Abstract
Introduction
Obesity is a worldwide public health issue with serious psychological and social impacts. Erectile dysfunction is also a common clinical condition, and obesity is one of its main risk factors.
Objective
The objective of this study was to systematically evaluate the effect of bariatric surgery on male sexual function.
Methods
A systematical research was carried out in Medline via PubMed, EMBASE, Cochrane Library, and Web of Science up to March 16, 2019, to identify published articles related to bariatric surgery and male sexual function in men. Two reviewers screened literature, extracted data, and assessed the quality of included studies. I2 index was applied to estimate the heterogeneity. All analyses were done using RevMan5.3 and Stata14.
Results
A total of 12 studies involving 420 participants were included. Analysis showed that bariatric surgery significantly reduced body mass index in morbidly obese patients (mean difference [MD] = -13.73; 95% CI -17.23 to -10.22; P < .00001). From 10 studies that reported the International Index of Erectile Function (IIEF) score, bariatric surgery led to a significant increase in IIEF-total score (MD = 8.2; 95% CI = 5.52−10.88; P < .00001), and erectile function score (MD = 3.76; 95% CI = 2.34−5.19; P < .00001), sexual desire (MD = 0.93; 95% CI = 0.55−1.32; P < .00001), sexual intercourse satisfaction (MD = 1.73; 95% CI = 0.43−3.03; P < .01), and total satisfaction (MD = 1.28; 95% CI = 0.56−2.00; P = .0005) were also significantly improved. However, bariatric surgery did not affect orgasm function (MD = 0.26; 95% CI = -0.15 to 0.68; P = .21). Three studies that reported the IIEF-5 score also showed a significant improvement of erectile function (MD = 5.45; 95% CI = 3.38−7.52; P < .00001).
Conclusions
Bariatric surgery could improve the erectile function, sexual desire, sexual intercourse satisfaction, and total satisfaction in morbidly obese men. Due to limited data on body mass index and hormone levels, our meta-analysis had some limitations. More clinical studies are needed to further explore the relationship between bariatric surgery and male sexual function.
Xu J, Wu Q, Zhang Y, et al. Effect of Bariatric Surgery on Male Sexual Function: A Meta-Analysis and Systematic Review. Sex Med 2019;7:270–281.
Key Words: Bariatric Surgery, Erectile Function, Obesity, Sexual Function, Systematic Review, Meta-Analysis
Introduction
The total number of overweight and obese people in the world reached 2.1 billion in 2013; the United States tops the list of the 671 million obese people in the world.1 Although the trend in average body mass index (BMI) has flattened out recently in high-income regions, it has accelerated in east and South Asia.2 Obesity is a worldwide public problem, often associated with diabetes, cardiovascular disease, depression, sleep apnea syndrome, and other chronic diseases.3 It severely affects the quality of life of patients and is associated with increased morbidity and mortality from a variety of chronic diseases.3, 4 Male sexual dysfunction is also common. Men’s inability to have satisfactory sex can cause a range of psychological problems, including depression, anxiety, poor body image, and low self-esteem.5
Erectile dysfunction is widely found in obese people, with 79% of patients with erectile dysfunction belonging to the overweight group.6 Abdominal obesity can increase the risk of erectile dysfunction by 50%,7 and the lack of confidence caused by obesity may also promote the occurrence of erectile dysfunction.8 At present, more and more attention has been paid to obesity-related sexual dysfunction. According to existing studies, mechanisms responsible for the independent influence of obesity on the erectile dysfunction may be hormonal imbalance, endothelial dysfunction, insulin resistance, psychological factors, and physical inactivity.8, 9 Low testosterone levels associated with obesity may lead to low sexual desire, whereas high reactive oxygen species production and the decrease in antioxidant capacity in obese patients will lead to endothelial dysfunction that can cause organic erectile dysfunction.10, 11 In addition to obesity itself, obesity-related comorbidities, such as diabetes, coronary heart disease, hypertension, and depression, are risk factors for male sexual dysfunction.8
Bariatric surgery has been widely used to treat morbidly obese patients and their associated complications, such as type 2 diabetes and sleep apnea syndrome,12, 13 as well as improve cardiovascular and renal functions.14, 15 Recent studies have shown that bariatric surgery for morbidly obese patients cannot only significantly reduce weight in a short period of time, but also significantly improve sexual function.16, 17, 18, 19 However, because the number of studies and the sample size are still small, and most of them are cohort studies, the effect of weight loss surgery on various domains of male sexual function is still controversial. In order to more accurately assess the relationship between bariatric surgery and male sexual function, we conducted a comprehensive systematic evaluation and meta-analysis of the existing studies in order to provide a basis for clinical decisions.
Materials and methods
Search Strategy
A systematic research was carried out in Medline via PubMed, EMBASE, Cochrane Library, and Web of Science up to March 16, 2019. The search terms used included bariatric surgery OR gastric bypass OR sleeve gastrectomy OR gastric banding OR gastroplasty OR jejunoileal bypass and erectile OR sexual. We also conducted a search of published research literature and a manual search of grey literature to ensure that no relevant articles were omitted. This system review and meta-analysis are reported in accordance with the preferred reporting items of the system review and meta-analysis (PRISMA).20
Inclusion and Exclusion Criteria
Inclusion criteria were as follows: (a) the study type was randomized controlled trial or observational study; (b) male obese patients who underwent weight-loss surgery were studied regardless of race, age, or course of disease; (c) the selected intervention was bariatric surgery, regardless of whether it was restrictive, malabsorptive, or mixed; (d) studies that compared patients before and after surgery or compared with control groups or patients underwent other interventions; and (e) outcomes were evaluated erectile function using International Index of Erectile Function (IIEF) score and Five-Item IIEF.
Exclusion criteria were as follows: (a) did not separate women and men; (b) did not define obesity; (c) did not use bariatric surgery as intervention; (d) outcomes are unclear and data are missing; and (e) republished literature.
Selection Process and Data Abstraction
Two reviewers reviewed the titles, abstracts, and full text independently according to inclusion and exclusion criteria. Disputes arising during the title and abstract screening phase are directly incorporated into the full text assessment to ensure that all relevant papers are not omitted. In the full text stage, the differences are resolved by negotiation between two reviewers. If there is no agreement, a third reviewer is consulted.
The two reviewers independently extracted relevant data with the predesigned data extraction table. Baseline data extracted included: first author and publication time, country, number of cases, type of study, age, BMI, outcome measures, operation method, comparison, follow-up time, and quality score.
Outcomes Assessed and Risk of Bias Assessment
The included study should include at least one specific change of outcome index before and after surgery. The primary outcomes of our study include IIEF and its 5 domains (IIEF-Erectile Function; IIEF-Desire; IIEF-Orgasm Function; IIEF-Intercourse Satisfaction; and IIEF-Total Satisfaction) and Five-Item IIEF.21, 22 Although IIEF and Five-Item IIEF have similar functions, there are still differences in significance and scoring methods, therefore, we conducted meta-analysis on them separately to avoid bias. In order to more accurately understand the effect of surgery on each domain of IIEF, we conducted meta-analysis on the 5 domains of IIEF. The secondary outcomes include BMI, total testosterone, and free testosterone. The nonrandom study methodology index (MINORS) tool23 was used to assess the risk of bias in individual studies, with the Jadad Score24 and Agency for Healthcare Research and Quality Score25 also being used to assess the quality of 1 randomized clinical trial (RCT) and one cross-sectional study, respectively.
Statistical Analysis
All statistical analyses and meta-analyses were performed using Cochrane Review Manager 5.3 (China), and the significance level was set at P < 0.05. All results were continuous in nature. The effect size was estimated by calculating the mean difference (MD) of the results and their 95% CIs, and the combined effect was estimated. Heterogeneity was assessed using inconsistency (I2) statistics. We believe that if I2 is >50%, it represents considerable heterogeneity, and the random-effect model is used; if I2 is <50%, it represents heterogeneity within the acceptable range, and the fixed effect model is used. For studies that only reported the range of median and quartile, the estimation method proposed by Wan et al26 was used to estimate the mean and SD.
Sensitivity Analysis and Publication Bias
Sensitivity analysis was performed to identify the source of heterogeneity. The heterogeneity and pooled effect values after the removal of a single study were recalculated and recorded by eliminating each literature article one by one. We used Revman 5.3 to analyze the changes in I2 and Stata software to obtain the forest plots after each study was successively removed. After discovering the source of heterogeneity, the experiment design, sample size, evaluation criteria, and other aspects were analyzed to find out the reason why it became the source of heterogeneity.
We quantified publication bias by the egger method. When the P value obtained by the egger method was >0.05, it indicated that there was no significant publication bias; on the contrary, it indicated the existence of publication bias. If publication bias exists, we will test the influence of publication bias on the results by the rim and fill method. If it is found that publication bias has obvious influence on the results, we will discuss it in detail in the Discussion section.
Results
Literature Retrieval Results and Basic Characteristics
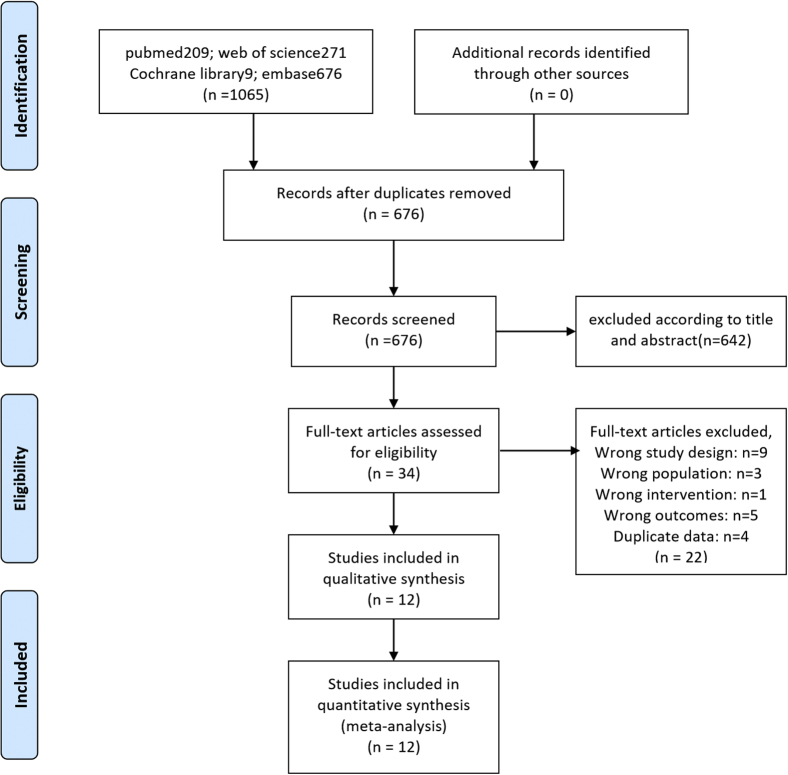
We have searched a large number of documents, carefully studied, and screened them, and the detailed process is shown in Figure 1. The results showed a total of 1,065 relevant studies chiefly from electronic databases. After removing duplicates, 642 references were excluded according to title and abstract because they were reviews or letters or irrelevant to the subject of this study. By reading the full text of 32 cations, 12 studies were eventually included,16, 17, 18, 19, 27, 28, 29, 30, 31, 32, 33, 34 including 420 participants. Among these studies, 3 were from Brazil, 6 from European countries, 2 from the United States, and 1 from China. Of the 12 studies, one was an RCT,28 1 was cross-sectional,17 and the rest were prospective cohort studies that were self-controlled. The included studies ranged from 2009 to 2017, with a median follow-up of 12 months (a range of 1 to 36 months). For studies reporting multiple time points, we selected the points closest to 12 months for analysis. In our meta-analysis, the main characteristics and data of each study are shown in Table 1.
Figure 1.
Literature search and selection process.
Table 1.
The main characteristics and data of each study
| Study | Country | Case | Study type | Age | BMI (kg/m2) | Outcome | Operation method | Comparison | Follow-up (mo) | Quality score |
|---|---|---|---|---|---|---|---|---|---|---|
| Araújo et al27 | Brazil | 21 | PC | 20−50 | 40 | BCDEFG | RYGB | Before vs after | 12 | 14 |
| Reis et al28 | Brazil | 10/10 | RCT | 36.7 ± 11.5/42.2 ± 11.0 | 55.7 ± 7.8/54.0 ± 6.1 | AHIJ | RYGB | Before vs after and between groups (MT NIP) | 24 | 3/5 |
| Ranasinghe et al29 | UK | 34 | PC | 52.8 ± 9.33 | 47.3 ± 12.67 | AB | LGB | Before vs after | 8 | 12 |
| Mora et al30 | Spain | 39 | PC | 18−65 | 46.90 ± 7.77 | ABCDEFGIJ | RYGB/LSG | Before vs after | 12 | 12 |
| Sarwer et al31 | USA | 27/20 | PC | 40−56 | 45.9 (3.0−94.3) | CDEFG | RYGB | Between groups (LM) | CS | 13 |
| Layus et al33 | Brazil | 14/14 | PC | CS | 44.9 ± 7.2 | BH | RYGB | Before vs after | 6 | 12 |
| Sarwer et al16 | USA | 32 | PC | 24−64 | 45.1 (42.0−52.2) | CDEFGIJ | RYGB | Before vs after | 36 | 13 |
| Efthymiou et al34 | Greece | 30 | PC | 37.30 ± 9.60 | 50.66 ± 7.90 | CDEFG | SG/RYGB/BPD+RY | Before vs after | 12 | 14 |
| Kun et al32 | China | 39 | RC | 45.20 ± 12.30 | 41.20 ± 8.50 | AHI | RYGB | Before vs after | 12 | 13 |
| Janik et al17 | Poland | 30/31 | CS∗ | 29 ± 2 | 43 ± 10 | ABCDEFG | LSG/RYGB | Between groups | 12–18 | 9/11 |
| Groutz et al18 | Israel | 39 | PC | 40.70 ± 12.40 | 42.80 ± 5.60 | ACDEFG | LSG | Before vs after | 3 | 14 |
| Aleid et al19 | UK | 30 | PC | 47.2 ± 8.1 | >35 | AB | LSG/LGB | Before vs after | 1−6 | 12 |
A = BMI change; B = IIEF-Total; C = IIEF-Erectile Function; D = IIEF-Sexual Desire; E = IIEF-Orgasm Function; F = IIEF-Intercourse Satisfaction; G = IIEF-Total Satisfaction; H = IIEF-5; I = Total testosterone; J = Free testosterone.
BMI = body mass index; BPD = biliary pancreatic diversion; CS = cannot say; IIEF = International Index of Erectile Function; IIEF-5 = 5-item International Index of Erectile Function; LGB = laparoscopic gastric-bypass; LM = lifestyle modification; LSG = laparoscopic sleeve gastrectomy; MT = multidisciplinary team; NIP = nonintensive program; PC = prospective cohort; RC = retrospective cohort RCT = randomized clinical trial; RY = Roux-en-Y; RYGB = Roux-en-Y gastric bypass; SG = sleeve gastrectomy.
CS = cross-sectional study.
Methodological Quality Assessment
The MINORS scale evaluation shows that 10 prospective cohort studies are of high grade and good quality. We used Jadad and Agency for Healthcare Research and Quality scales to evaluate Reis et al28 and Janik et al,17 respectively, and found that both of them had relatively high quality. Specific methodological quality evaluation results are shown in Table 2.
Table 2.
Quality assessment of included studies
| Study | MINORS criteria |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| A clearly stated aim | Inclusion of consecutive patients | Prospective collection of data | End points appropriate to the aims of the study | Unbiased assessment of the study end point | Follow-up period appropriate to the aim of the study | Loss to follow-up <5% | Prospective calculation of the study size | Total | |
| Araújo et al27 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 14 |
| Ranasinghe et al29 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 12 |
| Mora et al30 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 12 |
| Sarwer et al31 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 13 |
| Layus et al33 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 12 |
| Sarwer et al16 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 13 |
| Efthymiou et al34 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 14 |
| Kun et al32 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 13 |
| Groutz et al18 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 14 |
| Aleid et al19 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 12 |
| ∗Reis et al28 | Jadad scale: 3/5 | ∗Janik et al17 | AHRQ scale: 9/11 | ||||||
Meta-analysis results
Primary Outcomes
IIEF
A total of 10 studies reported the IIEF score. We analyzed the IIEF-Total Score and its 5 domains separately to obtain a comprehensive understanding of the effect of bariatric surgery on erectile function in men.
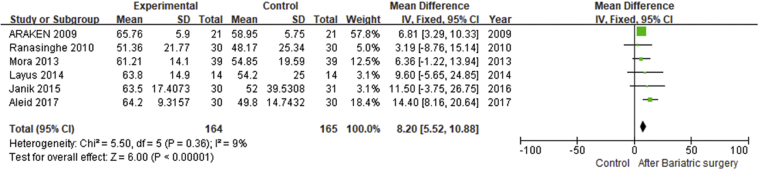
IIEF-Total Score
Six studies17, 19, 27, 29, 30, 33 reported the total score of the IIEF before and after surgery (75 points in total), and the meta-analysis results of the fixed-effect model showed that postoperative male erectile function was significantly improved compared with that before surgery (MD = 8.2; 95% CI = 5.52−10.88; P < .00001). For I2 = 9%, no significant heterogeneity was found (Figure 2.1).
Figure 2.1.
Forest plot-comparison of preoperative and postoperative International Index of Erectile Function-Total Score.
IIEF-Erectile Function
Six self-controlled prospective cohort studies16, 18, 27, 30, 31, 34 and 1 cross-sectional study17 reported the erectile function score of the patients. The meta-analysis results of the fixed-effect model showed that the erectile function score of the patients at 1 year after bariatric surgery was significantly higher than that before surgery, and the erectile function was significantly improved (MD = 3.76; 95% CI = 2.34−5.19; P < .00001). For I2 = 0, no significant heterogeneity was found (Figure 2.2).
Figure 2.2.
Forest plot-comparison of preoperative and postoperative International Index of Erectile Function score.
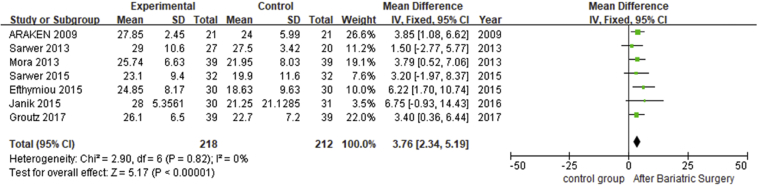
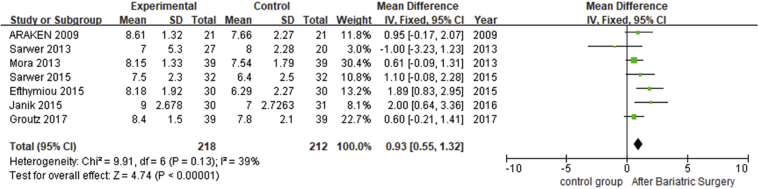
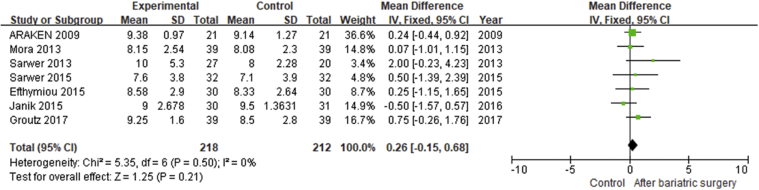
IIEF-Desire and IIEF-Orgasm Function
Seven studies16, 17, 18, 27, 30, 31, 34 reported preoperative and postoperative IIEF-Desire scores and IIEF-Orgasm Function scores in morbidly obese patients, with a total of 269 participants. The results of meta-analysis of fixed-effect model showed that the desire score of the patients after weight loss surgery was significantly higher 1 year after surgery than that before surgery (MD = 0.93; 95% CI = 0.55−1.32; P < .00001; Figure 2.3), and the orgasm function score was not significantly improved compared with that before surgery (MD = 0.26; 95% CI = -0.15 to 0.68; P = .21). For I2 <50%, no significant heterogeneity was found (Figure 2.4).
Figure 2.3.
Forest plot-comparison of preoperative and postoperative International Index of Erectile Function-Desire.
Figure 2.4.
Forest plot-comparison of preoperative and postoperative International Index of Erectile Function-Orgasm Function.
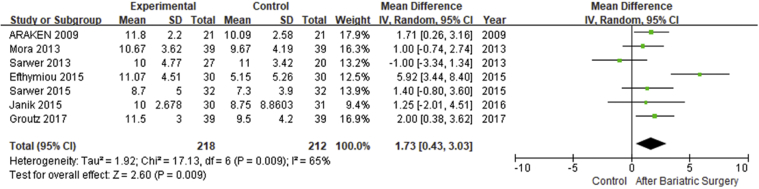
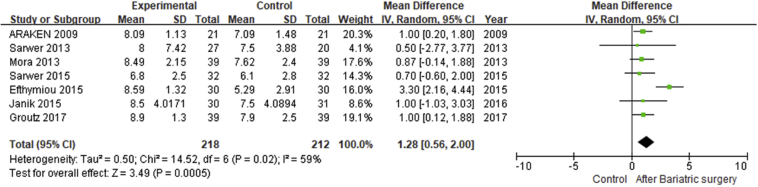
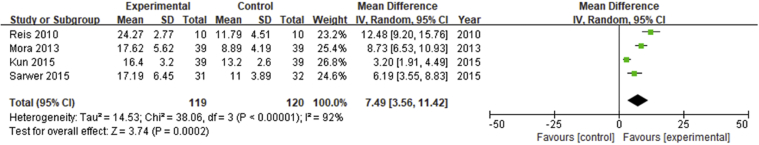
IIEF-Intercourse Satisfaction and IIEF-Total Satisfaction
7 studies16, 17, 18, 27, 30, 31, 34 reported preoperative and postoperative sexual satisfaction scores and total satisfaction scores in morbidly obese patients, with a total of 269 participants. The results of the meta-analysis of the random-effects model showed that patients’ intercourse satisfaction (MD = 1.73; 95% CI = 0.43−3.03; P < .01; Figure 2.5) and total satisfaction (MD = 1.28; 95% CI = 0.56−2.00; P = .0005; Figure 2.6) after bariatric surgery were significantly higher than before surgery. The I2 was 59% and 65%, respectively, indicating the presence of heterogeneity.
Figure 2.5.
Forest plot-comparison of preoperative and postoperative International Index of Erectile Function-Intercourse Satisfaction.
Figure 2.6.
Forest plot-comparison of preoperative and postoperative International Index of Erectile Function-Total Satisfaction.
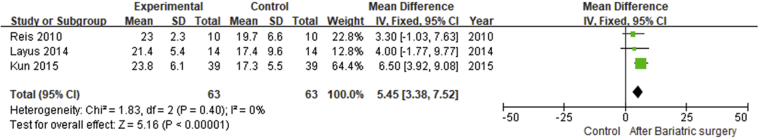
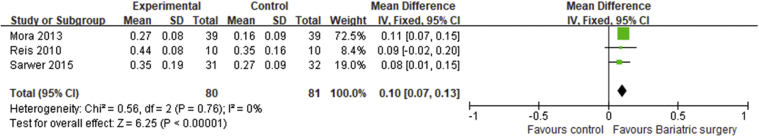
Five-Item IIEF
3 studies28, 32, 33 reported IIEF-5, including 87 participants. The meta-analysis of fixed-effect model showed that the erectile function of morbidly obese patients after bariatric surgery was significantly improved (MD = 5.45; 95% CI = 3.38−7.52; P < .00001). For I2 = 0, no significant heterogeneity was found (Figure 2.7).
Figure 2.7.
Forest plot-comparison of preoperative and postoperative Five-Item International Index of Erectile Function.
Secondary Outcomes
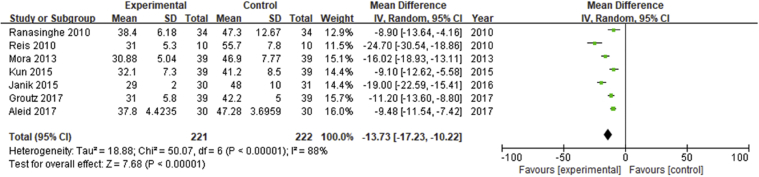
BMI
In the literature we included, a total of 7 studies17, 18, 19, 28, 29, 30, 32 gave explicit BMI changes. The random-effect model analysis showed that bariatric surgery could significantly reduce the BMI of patients (MD = -13.73; 95% CI = -17.23 to -10.22; P < .00001). I2 = 88%, indicating significant heterogeneity (Figure 3.1).
Figure 3.1.
Forest plot-comparison of preoperative and postoperative body mass index.
Total Testosterone and Free Testosterone
To explore the changes in hormone levels before and after weight loss surgery was not our main purpose, so it was not searched as part of the retrieval strategy. Therefore, only 4 literatures16, 28, 30, 32 included in our study contained the data of changes in testosterone before and after surgery. The random-effect model analysis showed that bariatric surgery could significantly increase the level of total testosterone (MD = 7.49; 95% CI = 3.56−11.42; P = 0.0002; Figure 3.2) and free testosterone (MD = 0.1; 95% CI = 0.07−0.13; P < .0001; Figure 3.3). I2 was 92% and 0%, respectively, indicating significant heterogeneity only in the total testosterone outcome indicator group.
Figure 3.2.
Forest plot-comparison of preoperative and postoperative Total Testosterone.
Figure 3.3.
Forest plot-comparison of preoperative and postoperative Free Testosterone.
Subgroup Analysis
In addition to 1 cross-sectional study and 1 RCT, the studies we included were mainly prospective, cross-sectional, cohort studies. In order to verify whether different study types and comparisons would not produce significant bias in results, we conducted subgroup analysis on the study types and comparisons, and the results showed that the significance of major outcome indicators did not change. Nearly half of the included studies (5/12) had undergone >1 type of bariatric surgery, and no single result of specific bariatric surgery was reported. Gastric bypass was adopted as the surgical approach in all 6 studies. Therefore, we absolutely conducted a subgroup analysis of gastric-bypass (GB) alone, and the results showed that the significance of the other major outcome indicators remained unchanged except for the change of IIEF-Intercourse Satisfaction to no significant improvement (MD = 0.88; 95% CI = -0.69 to 2.45; P = .27; Table 3).
Table 3.
Subgroup analysis of study types, control methods, and operation method
| Subgroup analysis | IIEF-Total [95% CI] | IIEF-Erectile Function [95% CI] | IIEF-Sexual Desire [95% CI] | IIEF-Orgasm Function [95% CI] | IIEF-Intercourse Satisfaction [95% CI] | IIEF-Total Satisfaction [95% CI] |
|---|---|---|---|---|---|---|
| Comparison | ||||||
| Before vs after | 8.10 [5.38, 10.82] | 3.94 [2.39, 5.49] | 0.90 [0.49, 1.31] | 0.33 [-0.13, 0.79] | 2.23 [0.85, 3.62] | 1.35 [0.50, 2.20] |
| Study type | ||||||
| Prospective cohort | 8.10 [5.38, 10.82] | 3.66 [2.20, 5.11] | 0.84 [0.44, 1.24] | 0.40 [-0.05, 0.85] | 1.78 [0.34, 3.22] | 1.31 [0.51, 2.10] |
| Operation method | ||||||
| Gastric-bypass | 6.66 [3.37, 9.96] | 3.16 [1.04, 5.28] | 0.79 [0.02, 1.55] | 0.40 [-0.22, 1.02] | 0.88 [-0.69, 2.45] | 0.90 [0.24, 1.57] |
IIEF = International Index of Erectile Function.
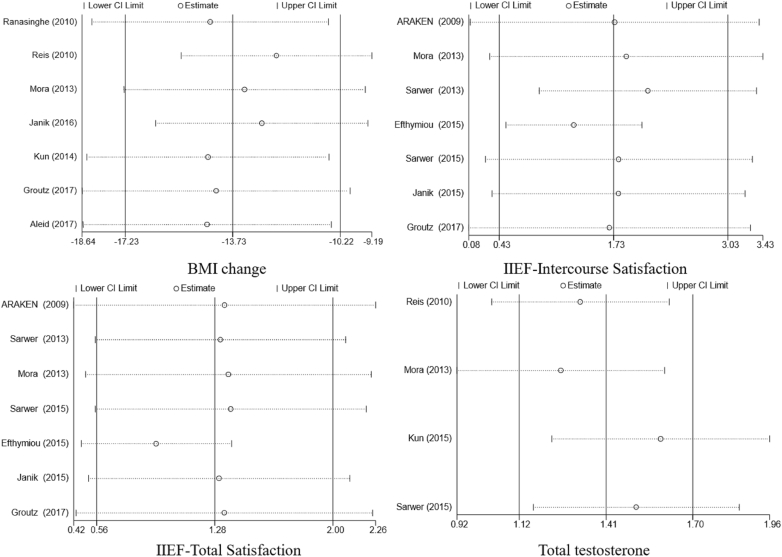
Sensitivity Analysis
There was moderate heterogeneity in the analysis of IIEF-Intercourse Satisfaction and IIEF-Total Satisfaction, 59% and 65%, respectively. To find the source of the heterogeneity, we removed each study in turn and found that when we removed Efthymiou et al,34 I2 became 0 (Table 4). This indicates that the source of heterogeneity in the two meta-analyses was Efthymiou et al.34 We also used the Stata software to get the forest plots after removing each study in turn (Figure 4). When we removed Efthymiou et al,34 we found that the result changed (from MD = 1.73; 95% CI = 0.43−3.03; P < .01 to MD = 1.28; 95% CI = 0.5−2.05; P = .001) in the IIEF-Intercourse Satisfaction outcome group and in the IIEF-Total Satisfaction outcome group, the result changed (from MD = 1.28; 95% CI = 0.56−2.00; P = .0005 to MD = 0.93; 95% CI = 0.47−1.38; P < .0001). In terms of data changes before and after the removal of Efthymiou et al,34 despite the heterogeneity, the final conclusions were not affected.
Table 4.
Sensitivity analysis
| Study omitted | Heterogeneity (A) |
Heterogeneity (B) |
||
|---|---|---|---|---|
| I2 | P value | I2 | P value | |
| Araújo et al27 | 71% | .04 | 64% | .004 |
| Sarwer et al31 | 57% | .0008 | 65% | .0007 |
| Mora et al30 | 70% | .02 | 64% | .002 |
| Sarwer et al16 | 71% | .004 | 64% | .001 |
| Efthymiou et al34 | 0% | .001 | 0% | < .0001 |
| Janik et al17 | 71% | .02 | 65% | .001 |
| Groutz et al18 | 71% | .04 | 65% | .004 |
A. IIEF-Contact Satisfaction. B. IIEF-Total Satisfaction.
IIEF = International Index of Erectile Function.
Figure 4.
Forest plots for sensitivity analysis. BMI = body mass index; IIEF, International Index of Erectile Function.
There was high heterogeneity in the analysis of BMI and total testosterone, I2 = 88% and 92%, respectively. We removed each study in turn and observed heterogeneity changes and found that all I2 values were >80%. At the same time, the forest plots obtained by using Stata software also showed that the results obtained after removal of each study all deviated from the median line to a certain extent (Figure 4). By switching the random-effect model to the fixed-effect model, we found that the result changed (from MD = -13.73; 95% CI = -17.23 to -10.22; P < .00001 to MD = -12.38; 95% CI = -13.53 to -11.23; P < .00001) in the BMI outcome group and in the total testosterone outcome group, the result changed (from MD = 7.49; 95% CI = 3.56−11.42; P = .0002 to MD = 5.54; 95% CI = 4.56−6.52; P < .0001). The difference before and after switching was relatively small, and the conclusion was not changed, indicating that although heterogeneity existed, there was no obvious influence on the final results, and our results were relatively robust.
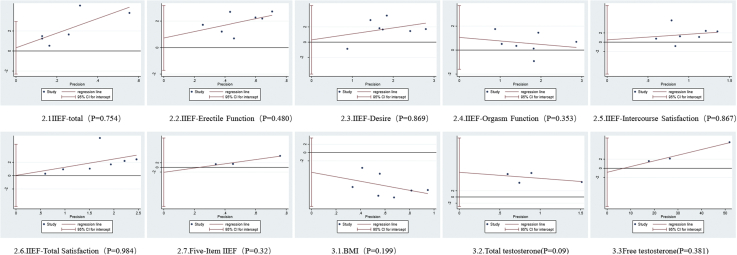
Publication Bias
We quantified publication bias by the Egger method and found that all P values of outcome indicator groups were >0.05, suggesting no significant publication bias (Figure 5).
Figure 5.
Publication bias - Egger graphs. BMI = body mass index; IIEF, International Index of Erectile Function.
Discussion
As far as we know, our study is the latest and most comprehensive meta-analysis on the effect of bariatric surgery on sexual function in morbidly obese patients. Current studies have shown that weight loss surgery can significantly improve men’s erectile function, but the current study sample size is small, and there is still a lack of large RCTs. Therefore, our meta-analysis integrated the data of all 420 participants and refined to every part of erectile function, and obtained results with strong demonstration effect, providing a strong basis for clinical decisions.
The results of our meta-analysis showed that the erectile function, sexual desire, and sexual satisfaction of obese patients after bariatric surgery were significantly improved, but there was no significant difference in the orgasmic function before and after surgery. Dallal et al35 evaluated 97 male patients using Brief Sexual Function Inventory score as the evaluation index of sexual function. The results showed that the average postoperative erectile function score was 2.5 points higher than that before the operation, and the average sexual desire score was 1.4 points higher than that before the operation. The results were consistent with the results of our meta-analysis. Because testosterone levels and BMI changes were not used as retrieval indicators, they were used as secondary outcome indicators in our study. The results of our meta-analysis showed that weight loss surgery could significantly reduce the BMI of patients, and the levels of total testosterone and free testosterone were also significantly increased. A previous meta-analysis on changes in hormone levels after weight loss surgery also reached the same conclusion as ours.36 Based on a careful study of the data, we found that the higher the initial value of BMI, the greater the decrease in BMI, and the changes in testosterone level were observed. We speculated that this trend might also occur in the 5 domains of IIEF. However, there are only 3 studies17, 18, 30 that contain both BMI reduction data and IIEF 5 domains data, and only 2 studies16, 30 that contain both hormone level changes and IIEF 5 domains data, so we can only guess the general trend and cannot get specific links through subgroup analysis and other methods. More large RCTs are needed to confirm this hypothesis.
The reasons for the significant improvement in erectile function, sexual desire, and sexual satisfaction may be related to the correction of postoperative vascular endothelial dysfunction and hormone imbalance in obese patients and the cure or improvement of obesity-related comorbidities.37, 38, 39 Obesity is thought to be a state of chronic oxidative stress and chronic inflammation, both of which interact in a vicious cycle.40 In obese patients, the production of a large amount of reactive oxygen species and the decline in the body's antioxidant capacity, as well as the decrease in blood flow and abnormal platelet agglutination in the body cause endothelial dysfunction, thereby causing erectile dysfunction.41 Weight loss improves endothelial function by increasing endothelium-dependent vasodilation, endothelial activation markers, and decreasing proinflammatory cytokine levels and insulin resistance.39, 42, 43 In terms of sex hormones, sexual desire and erectile function are significantly correlated with sex hormone balance, and androgens are indispensable in promoting male erectile function and maintaining sexual desire.44 The blocking of androgen can induce apoptosis of smooth muscle cells and increase of collagen.45 Rapid weight loss after bariatric surgery can increase androgen levels and improve endothelial function in obese patients.39 In addition to erectile dysfunction, diseases associated with obesity, such as diabetes, coronary heart disease, hypertension, and depression, can be controlled and alleviated to a certain extent.46 Lifestyle interventions can also reduce weight, but they are less effective than bariatric surgery.47 According to Sarwer et al,31 weight loss caused by lifestyle intervention can also improve sexual function, and there was no significant difference in the 5 structural domains of IIEF. There are still few studies comparing lifestyle intervention to bariatric surgery for sexual function improvement and further studies are needed.
According to the results of the subgroup analysis, we excluded the possible bias caused by different study types and control types, determined the stability of the results, and determined the effect of using only GB surgical method. Currently, there are 4 kinds of bariatric surgery, including GB, sleeve gastrectomy, and biliopancreatic diversion and gastric banding.48 It is worth noting that the improvement of sexual function in the 5 domains by only using the GB surgical method is lower than the overall result, which may indicate that the effect of the GB surgical method is inferior to other surgical methods. However, to our confusion, studies have shown that GB is not only as effective as or even better than other surgical methods in reducing weight and alleviating obesity-related complications, but also has a higher success rate.46, 48, 49 Due to the inadequacy of our data and the potential impact of ethnicity and initial BMI on outcomes, large RCTs are needed to further validate the effect of different surgical procedures on sexual function and its 5 domains.
We analyzed differences between heterogeneity sources and other studies to explore why these studies are sources of heterogeneity. Considering that the judgment of satisfaction was subjective, it may be related to the difference in the definition of “satisfaction” between the Greek population and other groups. By analyzing data from each study, we found that compared with patients with a lower baseline BMI, those with a higher baseline had a greater decrease in BMI and a greater increase in testosterone, which we speculated might be a source of heterogeneity.
Limitations
It is undeniable that this study also has several limitations. First, only 1 RCT was included, and the rest were observational studies. Second, although we had 420 participants, the sample size of a single study was small. Large RCTs are still needed. Third, although we discussed the effect of bariatric surgery on BMI and hormone levels, due to limited data, we were unable to further explore the specific impact of BMI changes and hormone levels on the 5 IIEF domains. Fourth, most of the follow-up time was about 1 year, lacking long-term efficacy indicators.
Conclusion
In conclusion, bariatric surgery could improve the erectile function, sexual desire, sexual intercourse satisfaction, and total satisfaction in morbidly obese men. Due to limited data on BMI and hormone levels, our meta-analysis had some limitations. More clinical studies are needed to further explore the relationship between bariatric surgery and male sexual function.
Data availability statement
All relevant data are within the paper and its Supporting Information files
Footnotes
Jiangnan Xu and Qian Wu contributed equally to this study.
Conflicts of Interest: The authors report not conflicts of interest.
Funding: None.
References
- 1.Ng M., Fleming T., Robinson M. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adams K.F., Schatzkin A., Harris T.B. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 4.LeBlanc E.S., Patnode C.D., Webber E.M. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018;320:1172–1191. doi: 10.1001/jama.2018.7777. [DOI] [PubMed] [Google Scholar]
- 5.Pastuszak A.W., Badhiwala N., Lipshultz L.I. Depression is correlated with the psychological and physical aspects of sexual dysfunction in men. Int J Impot Res. 2013;25:194–199. doi: 10.1038/ijir.2013.4. [DOI] [PubMed] [Google Scholar]
- 6.Bacon C.G., Mittleman M.A., Kawachi I. Sexual function in men older than 50 years of age: Results from the health professionals follow-up study. Ann Intern Med. 2003;139:161–168. doi: 10.7326/0003-4819-139-3-200308050-00005. [DOI] [PubMed] [Google Scholar]
- 7.Hadi H.A., Carr C.S., Al Suwaidi J. Endothelial dysfunction: Cardiovascular risk factors, therapy, and outcome. Vasc Health Risk Manag. 2005;1:183–198. [PMC free article] [PubMed] [Google Scholar]
- 8.Skrypnik D., Bogdanski P., Musialik K. [Obesity--significant risk factor for erectile dysfunction in men] Pol Merkur Lekarski. 2014;36:137–141. [in Polish] [PubMed] [Google Scholar]
- 9.Knoblovits P., Costanzo P.R., Valzacchi G.J. Erectile dysfunction, obesity, insulin resistance, and their relationship with testosterone levels in eugonadal patients in an andrology clinic setting. J Androl. 2010;31:263–270. doi: 10.2164/jandrol.109.007757. [DOI] [PubMed] [Google Scholar]
- 10.Silva F.H., Alexandre E.C., Calmasini F.B. Treatment with metformin improves erectile dysfunction in a murine model of obesity associated with insulin resistance. Urology. 2015;86:423.e1–423.e6. doi: 10.1016/j.urology.2015.04.035. [DOI] [PubMed] [Google Scholar]
- 11.Fernández-Sánchez A., Madrigal-Santillán E., Bautista M. Inflammation, oxidative stress, and obesity. Int J Mol Sci. 2011;12:3117–3132. doi: 10.3390/ijms12053117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aguiar I.C., Freitas W.R., Jr., Santos I.R. Obstructive sleep apnea and pulmonary function in patients with severe obesity before and after bariatric surgery: A randomized clinical trial. Multidiscip Respir Med. 2014;9:43. doi: 10.1186/2049-6958-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mingrone G., Panunzi S., De Gaetano A. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386:964–973. doi: 10.1016/S0140-6736(15)00075-6. [DOI] [PubMed] [Google Scholar]
- 14.Boido A., Ceriani V., Cetta F. Bariatric surgery and prevention of cardiovascular events and mortality in morbid obesity: Mechanisms of action and choice of surgery. Nutr Metab Cardiovasc Dis. 2015;25:437–443. doi: 10.1016/j.numecd.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Brethauer S.A., Aminian A., Romero-Talamás H. Can diabetes be surgically cured? Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258:628–636. doi: 10.1097/SLA.0b013e3182a5034b. [discussion: 636-637] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sarwer D.B., Spitzer J.C., Wadden T.A. Sexual functioning and sex hormones in men who underwent bariatric surgery. Surg Obes Relat Dis. 2015;11:643–651. doi: 10.1016/j.soard.2014.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janik M.R., Bielecka I., Podgórska L., Bujok J., Paśnik K. Male sexual function before and after bariatric surgery: A cross-sectional study. Obes Surg. 2015;25:S220. doi: 10.1007/s11695-015-1721-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Groutz A., Gordon D., Schachter P. Effects of bariatric surgery on male lower urinary tract symptoms and sexual function. Neurourol Urodyn. 2017;36:636–639. doi: 10.1002/nau.22980. [DOI] [PubMed] [Google Scholar]
- 19.Aleid M., Muneer A., Renshaw S. Early effect of bariatric surgery on urogenital function in morbidly obese men. J Sex Med. 2017;14:205–214. doi: 10.1016/j.jsxm.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Moher D., Liberati A., Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 21.Rosen R.C., Riley A., Wagner G. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 22.Rosen R.C., Cappelleri J.C., Smith M.D. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–326. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 23.Slim K., Nini E., Forestier D. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 24.Berger V.W. Is the Jadad score the proper evaluation of trials? J Rheumatol. 2006;33:1710–1711. [PubMed] [Google Scholar]
- 25.Fu R, Holmer HK. Change score or followup score? An empirical evaluation of the impact of choice of mean difference estimates [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2015 Apr. Report No.: 15-EHCV016-EF. [PubMed]
- 26.Wan X., Wang W., Liu J. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Araújo A.A., Brito A.M., Ferreira Mde N., Petribú K. [Changes the sexual quality of life of the obeses submitted Fobi-Capella gastroplasty surgery] Rev Col Bras Cir. 2009;36:42–48. doi: 10.1590/s0100-69912009000100009. [in Portuguese] [DOI] [PubMed] [Google Scholar]
- 28.Reis L.O., Favaro W.J., Barreiro G.C. Erectile dysfunction and hormonal imbalance in morbidly obese male is reversed after gastric bypass surgery: A prospective randomized controlled trial. Int J Androl. 2010;33:736–744. doi: 10.1111/j.1365-2605.2009.01017.x. [DOI] [PubMed] [Google Scholar]
- 29.Ranasinghe W.K., Wright T., Attia J. Effects of bariatric surgery on urinary and sexual function. BJU Int. 2011;107:88–94. doi: 10.1111/j.1464-410X.2010.09509.x. [DOI] [PubMed] [Google Scholar]
- 30.Mora M., Aranda G.B., de Hollanda A. Weight loss is a major contributor to improved sexual function after bariatric surgery. Surg Endosc. 2013;27:3197–3204. doi: 10.1007/s00464-013-2890-y. [DOI] [PubMed] [Google Scholar]
- 31.Sarwer D.B., Spitzer J.C., Wadden T.A. Sexual functioning and sex hormones in persons with extreme obesity and seeking surgical and nonsurgical weight loss. Surg Obes Relat Dis. 2013;9:997–1007. doi: 10.1016/j.soard.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kun L., Pin Z., Jianzhong D. Significant improvement of erectile function after Roux-en-Y gastric bypass surgery in obese Chinese men with erectile dysfunction. Obes Surg. 2014;25:838–844. doi: 10.1007/s11695-014-1465-x. [DOI] [PubMed] [Google Scholar]
- 33.Layus A., Costanzo P., Rey Valzacchi G. Changes in erectile function and “hormonogram” in obese patients treated with bariatric surgery (Preliminary report) J Sex Med. 2014;11:244. [Google Scholar]
- 34.Efthymiou V., Hyphantis T., Karaivazoglou K. The effect of bariatric surgery on patient HRQOL and sexual health during a 1-year postoperative period. Obes Surg. 2015;25:310–318. doi: 10.1007/s11695-014-1384-x. [DOI] [PubMed] [Google Scholar]
- 35.Dallal R.M., Chernoff A., O'Leary M.P. Sexual dysfunction is common in the morbidly obese male and improves after gastric bypass surgery. J Am Coll Surg. 2008;207:859–864. doi: 10.1016/j.jamcollsurg.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 36.Lee Y., Dang J.T., Switzer N. Impact of bariatric surgery on male sex hormones and sperm quality: A systematic review and meta-analysis. Obes Surg. 2019;29:334–346. doi: 10.1007/s11695-018-3557-5. [DOI] [PubMed] [Google Scholar]
- 37.Hutter M., Greene M.E., Chang D. The development of patient reported outcomes for national implementation in the MBSAQIP -- The first report from the PCORI funded LOBSTER PROMs study. Surg Obes Relat Dis. 2016;12:S101. [Google Scholar]
- 38.Botella-Carretero J.I., Balsa J.A., Gómez-Martin J.M. Circulating free testosterone in obese men after bariatric surgery increases in parallel with insulin sensitivity. J Endocrinol Invest. 2013;36:227–232. doi: 10.3275/8469. [DOI] [PubMed] [Google Scholar]
- 39.Csipo T., Fulop G.A., Lipecz A. Short-term weight loss reverses obesity-induced microvascular endothelial dysfunction. Geroscience. 2018 doi: 10.1007/s11357-018-0028-9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bondia-Pons I., Ryan L., Martinez J.A. Oxidative stress and inflammation interactions in human obesity. J Physiol Biochem. 2012;68:701–711. doi: 10.1007/s13105-012-0154-2. [DOI] [PubMed] [Google Scholar]
- 41.Antkowiak M.C., Rao Y., Suratt B.T. Association of obesity with markers of endothelial dysfunction and inflammation in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2017;195:A4263. [Google Scholar]
- 42.Osto E., Corteville C., Spliethoff K. Roux-En-Y gastric bypass improves obesity-induced endothelial dysfunction by a glucagon like peptide-1 mediated body weight loss independent effect. J Am Coll Cardiol. 2013;61:E2065. [Google Scholar]
- 43.Pontiroli A.E., Pizzocri P., Paroni R. Sympathetic overactivity, endothelial dysfunction, inflammation, and metabolic abnormalities cluster in grade III (World Health Organization) obesity: Reversal through sustained weight loss obtained with laparoscopic adjustable gastric banding. Diabetes Care. 2006;29:2735–2738. doi: 10.2337/dc06-1417. [DOI] [PubMed] [Google Scholar]
- 44.Aversa A., Isidori A.M., De Martino M.U. Androgens and penile erection: Evidence for a direct relationship between free testosterone and cavernous vasodilation in men with erectile dysfunction. Clin Endocrinol (Oxf) 2000;53:517–522. doi: 10.1046/j.1365-2265.2000.01118.x. [DOI] [PubMed] [Google Scholar]
- 45.Traish A.M., Park K., Dhir V. Effects of castration and androgen replacement on erectile function in a rabbit model. Endocrinology. 1999;140:1861–1868. doi: 10.1210/endo.140.4.6655. [DOI] [PubMed] [Google Scholar]
- 46.Salminen P., Helmiö M., Ovaska J. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: The SLEEVEPASS Randomized Clinical Trial. JAMA. 2018;319:241–254. doi: 10.1001/jama.2017.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Avenell A., Robertson C., Skea Z. Bariatric surgery, lifestyle interventions and orlistat for severe obesity: The REBALANCE mixed-methods systematic review and economic evaluation. Health Technol Assess. 2018;22:1–246. doi: 10.3310/hta22680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Azagury D., Mokhtari T.E., Garcia L. Heterogeneity of weight loss after gastric bypass, sleeve gastrectomy, and adjustable gastric banding. Surgery. 2019;165:565–570. doi: 10.1016/j.surg.2018.08.023. [DOI] [PubMed] [Google Scholar]
- 49.Ahmed B., King W.C., Gourash W. Long-term weight change and health outcomes for sleeve gastrectomy (SG) and matched Roux-en-Y gastric bypass (RYGB) participants in the Longitudinal Assessment of Bariatric Surgery (LABS) study. Surgery. 2018;164:774–783. doi: 10.1016/j.surg.2018.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files