Abstract
Pilonidal sinus disease (PSD) is increasing globally. A recent meta-analysis and merged-data analysis showed that recurrence rates in PSD depend essentially on follow-up time and specific surgical procedures. However, the global distribution of surgical approaches and respective recurrence rates have never been studied in PSD. We aimed at studying the impact of geographic distribution of surgical approaches to treat PSD and subsequent geography-specific recurrence rates. We searched relevant databases as described previously. Recurrence rates were then associated with reported follow-up times and geographic origin. We simulated individual patients to enable analogy across data. Globally, recurrence rates range from 0.3% for Limberg/Dufourmentel approaches (95% CI 0.2–0.4) and flaps (95% CI 0.1–0.5) and up to 6.3% for incision (95% CI 3.2–9.3) at 12 months. Recurrence rates range from 0.3% for Karydakis/Bascom approaches (95% CI 0.0–0.8) up to 67.2% for incision (95% CI 7.5–100) in the USA, and 0.0% for primary asymmetric closure in Germany (95% CI 0.0–0.0). Our analysis shows that recurrence rates in PSD not only depend on therapeutic approaches and follow-up time but also on geography. Primary asymmetric closure and various flap techniques remain superior regardless of the geographical region. Some approaches have extraordinarily good outcomes in specific countries.
Subject terms: Gastroenterology, Health services
Introduction
The incidence of pilonidal sinus disease is increasing globally. About 100/100,000 inhabitants per year are affected in Germany1, with even higher numbers reported for Turkey2. Since 2013, American, German and Italian societies have published guidelines on best clinical practice3–5. While debate over the disease’s etiology and pathomechanisms is ongoing6–9, we showed recently that recurrence rates in PSD depend essentially on follow-up time and the specific surgical procedure used10. In a meta-analysis and merged-data analysis of surgical treatment options, follow-up times, and recurrence rates in 89,583 patients, recurrence after Limberg/Dufourmentel operations was as low as 0.6% at 12 months and 1.8% at 24 months postoperatively. Recurrence after Karydakis/Bascom procedures was 0.2% (95% CI 0.1–0.3%) at 12 months and 0.6% (95% CI 0.5–0.8%) at 24 months postoperatively. Primary midline closure after 240 months was associated with recurrence rates of 67.9% (95% CI 53.3–82.4%)10 (Table 1).
Table 1.
Recurrence rates (RR) in different surgical approaches deriving from including all available studies from all geographical regions for 12, 24, 60, and 120 months follow-up time.
| Surgical method (total patients included) | 12 months | 24 months | 60 months | 120 months | Citations | ||||
|---|---|---|---|---|---|---|---|---|---|
| RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | ||
| Primary open (6351) | 1.3 (1.0–1.7) | 5715 | 4.2 (3.6–4.8) | 3496 | 13.9 (12.2–15.6) | 1222 | 28.1* (23.9–32.4) | 241* | 20– 122 |
| Primary median closure (15011) | 3.1 (2.8–3.5) | 12,484 | 8 (7.4–8.6) | 6956 | 14.9 (13.8–15.9) | 2505 | 27.9 (25.5–30.4) | 631 | 20, 24, 27, 29, 31, 34– 38, 44, 46, 48, 52, 54, 56, 57, 59, 61– 66, 69, 73– 78, 81– 84, 86, 89– 91, 93– 100, 106– 108, 115, 118, 122– 248 |
| Primary asymmetric closure (2538) | 0.6 (0.3–0.9) | 2432 | 1.1 (0.7–1.6) | 1807 | 2.7 (1.9–3.6) | 1205 | 6.3* (4.8–7.7) | 937* | 65, 67, 100, 129, 183, 192, 249– 263 |
| Karydakis/Bascom (6276) | 0.5 (0.3–0.7) | 5868 | 1.6 (1.2–2.0) | 3630 | 6.3 (5.0–7.5) | 853 | NA | NA | 16, 21, 29, 41, 49, 66, 78, 88, 133, 163, 172, 184, 189, 192, 195, 199, 200, 202, 262– 316 |
| Limberg/Dufourmentel (11470) | 0.3 (0.2–0.4) | 10,937 | 1.5 (1.2–1.7) | 7527 | 5.9* (5.1–6.7) | 1638* | NA | NA | 25, 28, 31, 33, 52, 56, 67, 92, 100, 127, 128, 130, 131, 137, 139, 140, 148, 149, 163, 165, 170, 172, 174, 182, 190– 192, 201, 205, 207, 208, 231– 233, 243, 246, 267, 268, 270, 272– 274, 291, 292, 295, 297, 305– 309, 311– 313, 317– 398 |
| Marsupialization (1896) | 2.2 (1.4–2.9) | 1253 | 5.7 (4.2–7.1) | 800 | 7.8* (5.9–9.6) | 566* | NA | NA | 30, 37, 46, 60, 65, 69, 71, 77, 78, 89, 97, 104, 110, 137, 152, 156, 175, 207, 208, 332, 399– 416 |
| Limited excision (3346) | 5.1 (4.2–6.0) | 2746 | 7.4 (6.2–8.5) | 1810 | 13.1 (11.1–15.0) | 804 | NA | NA | 31, 34, 52, 60, 61, 69, 75, 82, 87, 96, 98, 103, 112, 116, 136, 138, 170, 187, 212, 220, 229, 241, 290, 299, 311, 344, 399, 414, 417– 436 |
| Pit picking (5432) | 2.8 (2.4–3.3) | 5221 | 6.6* (5.9–7.4) | 1962* | 14.2 (12.5–15.9) | 1401 | NA | NA | 16, 22, 55, 69, 109, 193, 216, 278, 298, 309, 437– 452 |
| Flaps (3073) | 0.3 (0.1–0.5) | 2902 | 1.1* (0.7–1.5) | 1687* | 6.4* (4.9–8.0) | 708* | NA | NA | 91, 98, 100, 108, 135, 173, 185, 191, 193, 227, 309, 322, 343, 362, 369, 375, 379, 424, 434, 453– 488 |
| Incision and drainage (293) | 6.3* (3.2–9.3) | 259* | 22.3 (15.8–28.9) | 243 | 36.8* (26.3–47.2) | 121* | NA | NA | 20, 52, 55, 77, 184, 212, 223, 253, 489 |
| Phenol only (1453) | 1.6* (0.9–2.3) | 1244* | 14.7 (12.1–17.3) | 687 | NA | NA | NA | NA | 53, 76, 114, 242, 363, 385, 490– 505 |
| Laser treatment (77) | 2.2* (0.0–4.8) | 74* | 11.8* (0.8–22.9) | 47* | NA | NA | NA | NA | 506– 508 |
| Others (1363) | 2.8 (1.9–3.8) | 1247 | 6.6* (4.8–8.4) | 624* | 19.8 (15.7–23.8) | 498 | NA | NA | 15, 16, 309, 430, 489, 509– 523 |
| Partial closure (202) | 0.6* (0.0–1.4) | 202* | 1.1* (0.0–2.5) | 201* | 11.2* (5.9–16.6) | 161* | NA | NA | 62, 98, 143 |
Geography – and thereby specific genetic mechanisms, healthcare settings and socioeconomic factors – has been shown to affect manifold diseases, and must be considered when studying a disease worldwide11,12. However, the global distribution of surgical approaches and the geography of recurrence rates have never been assessed in PSD, one of the most frequent surgical diagnoses1.
We therefore studied the impact of geographic distribution of surgical approaches on the treatment of PSD and the associated recurrence rates in order to evaluate the quality of selected procedures. We used our previously established database of publications from the years 1833–2017 to study PSD treatment strategies, follow-up time, and country of origin10. We hypothesized that geography affects recurrence rates in PSD and an extensive analysis of data will allow specific recommendations for different geographic regions.
Results
Our original search and processing strategy was described previously10. In brief, after exclusion of duplicates, we screened 5,768 studies across various databases. Data pertaining to malignancies, embryonic development, and body regions other than the presacral intergluteal location was additionally excluded, leaving 1,148 articles. Of these, 408 reports lacked data on follow-up time or on recurrence or both. Subsequently, data deriving from 740 studies was included in the merged data analysis10. The flow chart based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) can be found in our first study; the same applies for the heterogeneity analysis of the data involved10.
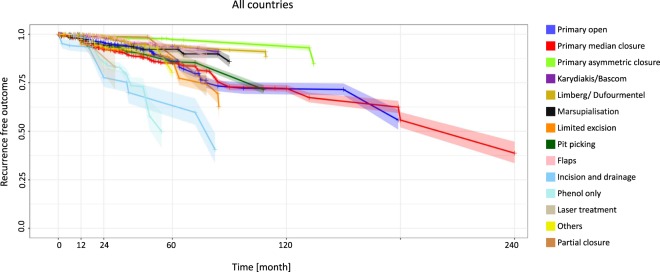
Looking at the overall results, the recurrence rates at 12 months ranged from 0.3% for the Limberg/Dufourmentel approach (95% CI 0.2–0.4) and the flaps approach (95% CI 0.1–0.5) to 6.3% for the incision and drainage approach (95% CI 3.2–9.3). At 60 months, the incision and drainage approach showed the highest recurrence rate: 36.8% (95% CI 26.3–47.2) (Fig. 1, Table 1).
Figure 1.
All countries: Kaplan-Meier-estimator depicting recurrence free outcome of the study population as a function of follow-up time. The data used include all available studies from all geographical regions. 95% confidence intervals are shown by shaded lines. The number of patients at risk for 12, 24, 60, and 120 months follow-up time are shown in Table 1.
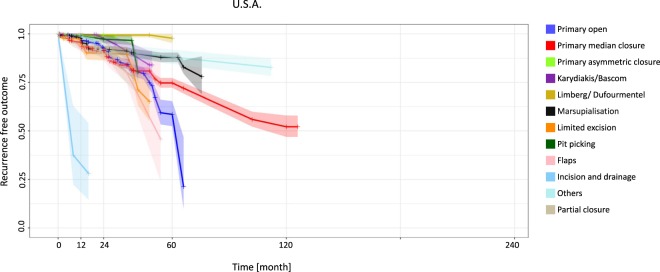
In the United States at 12 months the recurrence rates ranged from 0.3% for the Karydakis/Bascom approach (95% CI 0.0–0.8) to 67.2% for the incision and drainage approach (95% CI 7.5–100). The Limberg/Dufourmentel approach showed the lowest recurrence rate at 60 months, with 2.3% (95% CI 0.0–4.9) (Fig. 2, Table 2).
Figure 2.
United States: Kaplan-Meier estimator depicting recurrence-free outcome of the study population as a function of follow-up time. The data used include all available studies from the United States. 95% confidence intervals are shown by shaded lines. The number of patients at risk of recurrence at 12, 24, 60, and 120 months of follow-up is shown in Table 2.
Table 2.
Recurrence rates (RR) in different surgical approaches deriving from including available studies from the U.S.A. for 12, 24, 60, and 120 months follow-up time.
| USA | 12 months | 24 months | 60 months | 120 months | Citations | ||||
|---|---|---|---|---|---|---|---|---|---|
| Surgical method (total patients included) | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | |
| Primary open (2124) | 2.2 (1.5–2.8) | 1708 | 7.4 (5.7–9.1) | 734 | 41.5 (30.2–52.8) | 69 | NA | NA | 21, 37, 41, 43, 46, 57, 62, 63, 69, 77, 79, 104, 105, 107, 108, 111, 524– 540 |
| Primary median closure (3650) | 4.3 (3.6–5.1) | 2754 | 8.5 (7.4–9.7) | 2119 | 25.3 (21.9–28.7) | 388 | 47.9 (37.1–58.6) | 44 | 37, 46, 57, 62, 63, 69, 77, 107, 108, 152, 156, 157, 170, 175, 181, 185, 227, 237, 525– 529, 532, 533, 538, 540– 559 |
| Primary asymmetric closure (176) | 0.6* (0.0–1.7) | 170* | 0.6 (0.0–1.7) | 160 | NA | NA | NA | NA | 257, 560, 561 |
| Karydakis/Bascom (236) | 0.3* (0.0–0.8) | 236* | 2.4* (0.2–4.7) | 160* | NA | NA | NA | NA | 21, 41, 562– 565 |
| Limberg/Dufourmentel (164) | 0.6* (0.0–1.8) | 156* | 0.6* (0.0–1.8) | 145* | 2.3 (0.0–4.9) | 120 | NA | NA | 170, 351, 374, 566 |
| Marsupialization (1475) | 2.4 (1.4–3.3) | 933 | 8.0* (6.0–10.1) | 526* | 12.1* (9.2–15.0) | 332* | NA | NA | 37, 46, 69, 77, 104, 152, 156, 175, 399– 401, 404, 405, 410, 411, 416, 527, 532, 538, 549, 567– 571 |
| Limited excision (780) | 5.8 (3.3–8.3) | 301 | 10.1* (6.0–14.2) | 162* | NA | NA | NA | NA | 69, 170, 399, 430, 435, 527, 535, 572– 578 |
| Pit picking (328) | 0.9 (0.0–2.0) | 328 | 2.8 (0.6–4.9) | 213 | NA | NA | NA | NA | 69, 445, 579, 580 |
| Flaps (595) | 6.9 (4.6–9.3) | 517 | 10.7* (7.0–14.4) | 176* | NA | NA | NA | NA | 108, 185, 227, 485, 527, 533, 581– 583 |
| Incision and drainage (24) | 67.2* (7.5–100) | 16* | NA | NA | NA | NA | NA | NA | 77, 528 |
| Others (374) | 0.9* (0.0–1.9) | 364* | 8.2* (4.7–11.7) | 237* | 11.9* (7.5–16.3) | 234* | NA | NA | 430, 510, 520, 584, 585 |
| Partial closure (215) | 5.5* (2.2–8.8) | 199* | 8.9* (4.5–13.3) | 168* | NA | NA | NA | NA | 62, 526, 528, 533, 549, 586 |
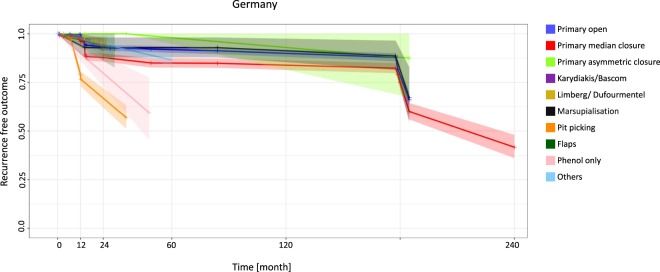
In Germany, patients undergoing the primary asymmetric closure approach had no recurrence at 12 months (95% CI 0.0–0.0), whereas patients undergoing the pit-picking approach had a much higher recurrence rate of 21.0% (95% CI 16.7–25.3). At 120 months four surgical approaches showed recurrence below 20%: the primary open approach (10.0%) (95% CI 7.9–12.1), the primary median closure approach (16.1%) (95% CI 13.1–19.2), the primary asymmetric closure approach (7.1%) (95% CI 0.0–22.1) and the marsupialization approach (8.8%) (95% CI 2.0–15.5) (Fig. 3, Table 3).
Figure 3.
Germany: Kaplan-Meier estimator depicting recurrence-free outcome of the study population as a function of follow-up time. The data used include all available studies from Germany. 95% confidence intervals are shown by shaded lines. The number of patients at risk of recurrence at 12, 24, 60, and 120 months of follow-up is shown in Table 3.
Table 3.
Recurrence rates (RR) in different surgical approaches deriving from including all available studies from Germany for 12, 24, 60, and 120 months follow-up time.
| Surgical method (total patients included) | 12 months | 24 months | 60 months | 120 months | Citations | ||||
|---|---|---|---|---|---|---|---|---|---|
| RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | ||
| Primary open (1457) | 0.5 (0.1–0.8) | 1263 | 6.9* (5.3–8.5) | 851* | 8.1* (6.3–9.9) | 752* | 10* (7.9–12.1) | 706* | 13, 26, 44, 54, 59, 64– 66, 92, 97, 115, 117, 122, 587, 588 |
| Primary median closure (1320) | 3.9 (2.7–5.1) | 1043 | 12.2 (9.8–14.6) | 655 | 15.0* (12.2–17.9) | 554* | 16.1* (13.1–19.2) | 507* | 13, 44, 54, 59, 64– 66, 97, 115, 122, 123, 180, 211, 588– 590 |
| Primary asymmetric closure (87) | 0.0* (0.0–0.0) | 48* | 0.0* (0.0–0.0) | 33* | 2.0* (0.0–6.3) | 26* | 7.1* (0.0–22.1) | 17* | 65, 588, 591, 592 |
| Karydakis/Bascom (332) | 1.5* (0.0–3.2) | 226* | 5.9 (2.0–9.8) | 151 | NA | NA | NA | NA | 66, 298, 587 |
| Limberg/Dufourmentel (434) | 1.9* (0.5–3.4) | 278* | 5.1* (1.2–8.9) | 54* | NA | NA | NA | NA | 92, 320, 357, 366, 394, 593– 595 |
| Marsupialization (98) | 6.0* (1.3–10.6) | 98* | 7.1* (1.5–12.7) | 93* | 7.1* (1.5–12.7) | 76* | 8.8* (2.0–15.5) | 57* | 13, 65, 97, 588 |
| Pit picking (676) | 21 (16.7–25.3) | 553 | 33.1* (25.2–41.1) | 158* | NA | NA | NA | NA | 298, 441, 447, 452 |
| Flaps (26) | 3.1* (0.0–7.6) | 26* | 6.2* (0.0–15.2) | 26* | NA | NA | NA | NA | 596 |
| Phenol only (37) | 10.1* (3.3–16.9) | 37* | 20.3* (6.7–33.8) | 37* | NA | NA | NA | NA | 497 |
| Others (498) | 2.7* (2.0–3.4) | 498* | 5.4* (4.0–6.8) | 498* | 13.5 (9.9–17.0) | 498 | NA | NA | 513 |
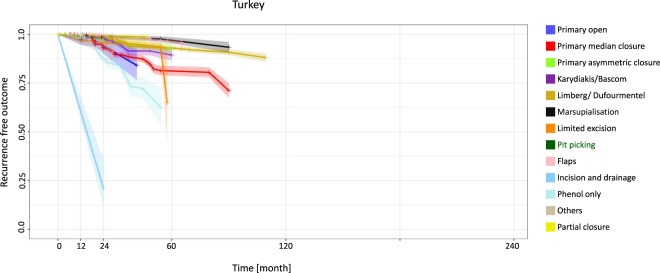
Patients in Turkey had very good outcomes with the flaps approach at 12 months (0.0% recurrence) (95% CI 0.0–0.0), but the incision and drainage approach was associated with recurrence of 39.4% at 12 months (95% CI 12.7–66.2) and 78.8% (95% CI 25.3–100) at 24 months (Fig. 4, Table 4).
Figure 4.
Turkey: Kaplan-Meier estimator depicting recurrence-free outcome of the study population as a function of follow-up time. The data used include all available studies from Turkey. 95% confidence intervals are shown by shaded lines. The number of patients at risk of recurrence at 12, 24, 60, and 120 months of follow-up is shown in Table 4.
Table 4.
Recurrence rates (RR) in different surgical approaches deriving from including all available studies from Turkey for 12, 24, 60, and 120 months follow-up time.
| Surgical method (total patients included) | 12 months | 24 months | 60 months | 120 months | Citations | ||||
|---|---|---|---|---|---|---|---|---|---|
| RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | ||
| Primary open (143) | 2.7* (0.0–5.5) | 143* | 5.9* (1.4–10.4) | 120* | NA | NA | NA | NA | 32, 114, 118 |
| Primary median closure (2902) | 0.8 (0.4–1.1) | 2818 | 7.0* (5.7–8.2) | 1383* | 18.8* (15.7–21.8) | 417* | NA | NA | 118, 127, 133, 136, 137, 139, 143, 148, 149, 158– 160, 169, 172– 174, 183, 192, 199– 201, 232, 242, 243, 246, 247, 597– 603 |
| Primary asymmetric closure (727) | 1.7 (0.7–2.8) | 621 | 2.5 (1.1–3.8) | 403 | 7.4 (4.4–10.4) | 257 | NA | NA | 183, 192, 253, 259, 261, 262 |
| Karydakis/Bascom (2471) | 0.8 (0.4–1.1) | 2356 | 1.7* (1.1–2.4) | 1343* | 10.7 (7.4–13.9) | 257 | NA | NA | 133, 172, 192, 199, 200, 262, 264, 267, 268, 270, 273, 274, 276, 279, 282, 284, 289– 292, 295, 296, 300, 305– 309, 603 |
| Limberg/Dufourmentel (7653) | 0.1 (0.0–0.2) | 7369 | 1.1 (0.8–1.4) | 5624 | 7.1* (5.9–8.2) | 988* | NA | NA | 127, 137, 139, 148, 149, 172, 174, 192, 201, 232, 243, 246, 267, 268, 270, 273, 274, 291, 292, 295, 305– 309, 317, 319, 321– 323, 327, 329, 330, 332, 338– 340, 342– 344, 346– 350, 352– 355, 359, 362– 364, 368, 369, 371– 373, 375, 379, 382, 385, 387, 395, 398, 600, 603– 607 |
| Marsupialisation (728) | 0.4 (0.0–0.9) | 688 | 1.3* (0.4–2.3) | 419* | 3.1* (1.4–4.7) | 358* | NA | NA | 137, 332, 402, 403, 415, 598, 599, 603, 606 |
| Limited excision (1402) | 3.1 (2.2–4.1) | 1402 | 4.1* (2.8–5.5) | 423* | NA | NA | NA | NA | 136, 290, 344, 417, 420, 424, 428, 429, 608 |
| Pit picking (204) | 0.4* (0.0–1.0) | 204* | 0.8* (0.0–2.0) | 204* | NA | NA | NA | NA | 309 |
| Flaps (2262) | 0 (0.0–0.0) | 2219 | 0.4* (0.1–0.8) | 1292* | 3.8* (2.5–5.2) | 670* | NA | NA | 173, 309, 322, 343, 362, 369, 375, 379, 424, 454– 456, 458, 459, 461, 462, 464, 466, 469– 471, 473, 475, 476, 478– 481, 599 |
| Incision and drainage (52) | 39.4* (12.7–66.2) | 52* | 78.8 (25.3–100) | 52 | NA | NA | NA | NA | 253 |
| Phenol only (1089) | 0.5 (0.1–0.9) | 990 | 12.6 (9.9–15.3) | 607 | NA | NA | NA | NA | 114, 242, 363, 385, 490– 496, 498, 504, 505, 609 |
| Others (103) | 2.6* (0.0–5.2) | 103* | 5.3* (0.1–10.4) | 56* | NA | NA | NA | NA | 309, 509, 521 |
| Partial closure (73) | 0.3* (0.0–1.1) | 73* | 0.7* (0.0–2.1) | 73* | NA | NA | NA | NA | 143 |
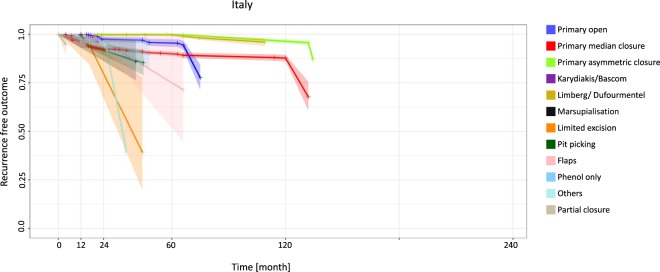
Italy delivered outstanding results at 12 months for four procedures: recurrence was 0.0% for the primary open approach (95% CI 0.0–0.0), the primary asymmetric closure approach (95% CI 0.0–0.0), the Limberg/Dufourmentel approach (95% CI 0.0–0.0) and the flaps approach (95% CI 0.0–0.0). Recurrence was relatively low with the marsupialization approach at 12 months (4.1%) (95% CI 0.5–7.7) and with the primary asymmetric closure approach at 120 months (3.6%) (95% CI 2.4–4.8) (Fig. 5, Table 5). Similar specifics can be shown for additional countries and regions such as Australia, New Zealand, Greece and Asia (Supplemental Figs 1–3, Supplemental Tables 1–3).
Figure 5.
Italy: Kaplan-Meier estimator depicting recurrence-free outcome of the study population as a function of follow-up time. The data used include all available studies from Italy. 95% confidence intervals are shown by shaded lines. The number of patients at risk of recurrence at 12, 24, 60, and 120 months of follow-up is shown in Table 5.
Table 5.
Recurrence rates (RR) in different surgical approaches deriving from including all available studies from Italy for 12, 24, 60, and 120 months follow-up time.
| Surgical method (total patients included) | 12 months | 24 months | 60 months | 120 months | Citations | ||||
|---|---|---|---|---|---|---|---|---|---|
| RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | RR in % (95% CI) | Nr. at risk | ||
| Primary open (1243) | 0 (0.0–0.0) | 1203 | 2.5* (1.2–3.8) | 441* | 4.5* (2.5–6.6) | 267* | NA | NA | 35, 56, 70, 72, 80, 91, 94– 96, 99, 100, 120, 610– 613 |
| Primary median closure (5583) | 3.3 (2.8–3.8) | 4184 | 7.6 (6.7–8.5) | 1939 | 10.1* (8.8–11.4) | 786* | 12.2 (10.3–14.2) | 382 | 35, 56, 91, 94– 96, 99, 100, 129, 144, 146, 161, 162, 165– 168, 171, 179, 182, 186, 197, 205, 209, 214, 215, 218– 222, 610– 621 |
| Primary asymmetric closure (1099) | 0.0* (0.0–0.0) | 1099* | 0.0* (0.0–0.0) | 1096* | 0.1* (0.0–0.2) | 1022* | 3.6* (2.4–4.8) | 937* | 100, 129, 256, 260, 622 |
| Karydakis/Bascom (109) | 3.7 (0.0–7.4) | 109 | NA | NA | NA | NA | NA | NA | 16, 622 |
| Limberg/Dufourmentel (944) | 0.0* (0.0–0.0) | 944* | 0.3* (0.0–0.7) | 891* | 0.3 (0.0–0.7) | 618 | NA | NA | 56, 100, 165, 182, 205, 328, 334, 336, 623 |
| Marsupialization (43) | 4.1* (0.5–7.7) | 43* | 8.2* (1.0–15.4) | 43* | NA | NA | NA | NA | 406 |
| Limited excision (18) | 4.0* (0.0–12.4) | 18* | 20.4* (0.0–47.3) | 16* | NA | NA | NA | NA | 96, 220 |
| Pit picking (2508) | 0.3 (0.1–0.5) | 2508 | 8.4* (5.4–11.3) | 1765* | NA | NA | NA | NA | 16, 439, 444, 451 |
| Flaps (13) | 0.0* (0.0–0.0) | 13* | 3.6* (0.0–9.6) | 12* | 25.0* (0.0–66.8) | 8* | NA | NA | 91, 100 |
| Phenol only (68) | 2.6* (0.5–4.6) | 68* | 5.1* (1.0–9.3) | 68* | NA | NA | NA | NA | 613 |
| Others (815) | 3.5 (2.1–4.9) | 728 | 5.2* (3.2–7.3) | 344* | NA | NA | NA | NA | 16, 182, 511, 514, 516, 523, 624 |
| Partial closure (58) | NA | NA | NA | NA | NA | NA | NA | NA612 | 625– 636 |
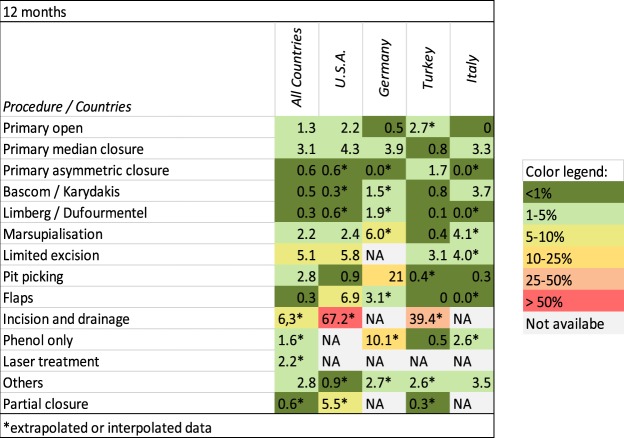
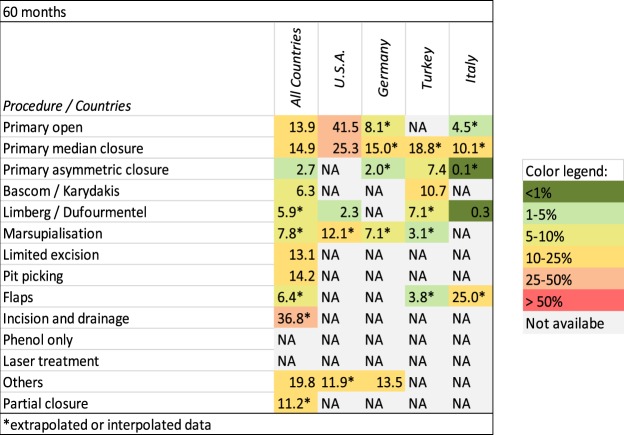
Figures 6 and 7 provide an overview of recurrence rates of all procedures studied after 12 and 60 months in various geographic settings.
Figure 6.
Procedure-specific recurrence rates in PSD [%] are shown at the time point 12 months. Extrapolated or interpolated data are marked with an asterisk (*).
Figure 7.
Procedure-specific recurrence rates in PSD [%] are shown at the time point 60 months. Extrapolated or interpolated data are marked with an asterisk (*).
Discussion
We analyzed global data of more than 80,000 PSD patients for the years 1833 to 2017. Whereas in our previous study we only looked at follow-up time dependent recurrence rates of different surgical procedures, we now analyzed the geography’s impact on recurrence rates. Most of the patients analyzed were from the US (8,017), Germany (4,965), Turkey (19,809) or Italy (12,443). Focusing on the surgical approaches used in different countries and regions of the world, we assessed the recurrence rates at different follow-up times and found a correlation between geography and PSD recurrence for a variety of surgical treatments.
Not all surgical approaches were used in all the countries analyzed, and certain preferences exist in the choice of surgical approach in each country, leading to differences in recurrence rates of specific surgical approaches between the geographical regions. Because not all nations and continents report PSD patient treatments in sufficient numbers, some geographical regions had to be excluded to ensure sufficient data quality. For example, countries in Africa, Asia and South America were not included due to missing data, and/or a very low disease burden.
The merged data analysis is potentially less powerful than a systematic review consisting entirely of randomized controlled trials (RCT’s). Many of the studies we cited could have qualified as RCT’s, but our approach enabled inclusion of enough patients to be able to compare all the surgical methods available in different geographical regions. Certain surgical approaches are not being used for treatment in all the analyzed geographical regions. This lack of data provides important information about established treatments in specific health care settings and geographic regions respectively. The patient number or number at risk also differs strongly between regions, probably pointing out specific economic and clinical peculiarities. Also, abrupt drops and interpolations in our figures need to be interpreted with caution because the curves about recurrence rates are influenced by the cohort sizes of underlying studies: The methodologies of the underlying studies may indirectly create a certain bias.
The primary open approach showed insufficient success in most geographical regions, with a recurrence rate of 41.5% being observed at 60 months in the US. This has not been shown before, and is appalling in its magnitude. Reasons for the high recurrence rate are not yet evident. Current evidence implies that non healing beyond 6 month post-surgery should be considered as recurrent disease13,14. The application of metronidazole 10% ointment has enabled a faster wound closure in patients15 and healing can be regularly expected within 6 months, however, some surgical wounds only close after 9 months or later. Further, non-healing wounds must not be confused with a scar overlying the sacral bone. By definition recurrent PSD is defined as a new sinus tract. Although stringent criteria to distinguish healing disorders versus recurrence are available, some variation in recurrence rate observation between countries might unfortunately have been published.
The primary midline closure, which is not recommended for use anymore, showed a recurrence rate of 25.3% at 60 months in the USA. The pit-picking approach had a high recurrence rate of 33.1% at 24 months in Germany and should therefore be used only selectively for the treatment of minor disease in PSD patients. Nevertheless, interim results of current studies on pit picking are more promising. In contrast to the finding in Germany, pit picking showed a very low recurrence rate of 0.8%* at 24 months in Turkey, justifying this treatment in the Turkish medical setting. Strikingly, the Karydakis/Bascom approach in Greek cohorts showed the lowest observed recurrence rate at the 120-month follow-up. Nevertheless, it should be kept in mind that Karydakis never fully disclosed his data details of several thousands of Greek recruits. In Italy, endoscopic therapy approaches of different names are emerging and first results appear to be very promissing16. Given our data base embracing evidence ranging from 1833 to 2017, it is currently too early, however, to comment on their long-term recurrence rate since our data base misses the most recent publications. This approach might become a very promising approach in PSD surgery.
Therapy of open wounds following surgery has not been standardized, and may be performed by either a doctor, a nurse or a family member. This is not sufficiently well described in most of the studies we cited. Even the most recently published US guidelines do not recommend a particular type of wound care for primary open treatment17. As increased duration of open wound treatment may increase recurrence rate14, and elevated body weight with consecutive metabolic derangements may prolong wound healing, body mass index (BMI) in relation to treatment applied may further influence recurrence rate in primary and secondary treatments.
Obviously, there is some mastery of certain surgical methods which are widely applied in some countries, and this contributes to better regional results. In other countries, the same methods used less often may show more dismal outcomes, contributing to the geographic differences in recurrence rates. Recently, Doll et al. have shown that patients with strong axial hair shafts are more prone to pilonidal sinus disease, and Bosche et al. found short cut hair less 2 cm length in the pilonidal nests18,19 indicating that both genetic disposition and cultural hair styles can contribute to regional variation of pilonidal sinus incidence and recurrence rate.
Furthermore, our current study analyzes results published in scientific journals. These studies are often run at large university hospitals. While industrialized countries have better resources and can document, study and report therapy outcomes, more rural countries with less funding may struggle to do so. In terms of economics, the costs of treatment may differ based on location, treating institution and type of therapy.
Our results allow a more differentiated view of PSD treatment. Surgical approaches should be selected carefully based on treatment efficacy in general, and geographical influences have to be taken into account when aiming for optimal treatment efficacy.
In summary, recurrence rates of different surgical approaches used in the treatment of PSD are influenced by geographical factors. Certain surgical approaches – such as primary asymmetric closure and different flap techniques – remain superior, regardless of the geographical region. This is powerful evidence since the clinical settings, the genetic background of the patient population and economic settings do vary between different countries. Methods such as limited excision and phenol treatment should be limited to selected settings due to their high recurrence rates. Under certain circumstances their use can be justified by the lack of need for a hospital stay or as low-cost variant of treatment. Geographic peculiarities were identified, such as high recurrence rates for the primary open approach in the US, suggesting that other methods should be preferred in the American setting. Pit picking should be selectively applied in Germany due to its high recurrence rate, and ways to improve this interesting minimal invasive procedure should be investigated. The same surgical method is already showing promising results in Turkey. In the future, detailed investigation into geographical differences in recurrence rates for the same surgical PSD method may lead to the identification of further co-factors for recurrence in pilonidal sinus disease. Therefore, the standardized definition of recurrence should uniformly be used13,14.
Methods
Our original search was described previously10. In brief, we searched for the NCBI Medical Subject Heading (MeSH) term “pilonid*”, as well as [“cyst” AND “dermoid”] in MEDLINE, Ovid, PubMed Central, PubMed, Scopus, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL) and other search engines to build the PSD database10. Publications from 1833 to 2017 in English, French, German, Italian, and Spanish were captured10. Reports in other languages were retrieved if recurrence at specific follow-up times and definitive treatment strategies were provided (National Health Service international prospective register of systematic reviews PROSPERO number 42016051588)10. Data were organized with Microsoft Excel (Version 2016, Microsoft Corp., Redmond, WA)10. Specific surgical approaches described in a report were listed in a data row, while columns included citation details (incl. country of origin), follow-up times, number of patients studied, recurrence, and study details10. Regularly recorded information included which hospital(s) participated and which region the patients came from. In the very few studies where this was not obvious, the patient’s country of origin was defined as where the first author’s hospital was located. If all other authors were from one hospital, and the first author exclusively was not, then the hospital of the last author defined the country. If an article addressed several surgical approaches, the data of each treatment strategy were managed separately10. Because the statistical measures were not standardized, mean and median reports were treated equally to take into account the cluster of affected patients who were young adults10. Data presented as range of follow-up times was managed by employing the center of the given time10.
Recurrence rates in each study were then associated with the reported follow-up time. Individual patients were statistically simulated to enable an analogy across all data10. Cochrane analysis and I2 calculation with Chi2 tests were employed to examine heterogeneity of the included data10.
Statistical analysis and figure generation were completed with the software “R” (version 3.1.0, R-studio framework version 0.98.982). Two-tailed statistical tests were performed10. Kaplan-Meier curves of recurrence-free outcome, including pointwise 95% confidence intervals (CI), were generated with ‘survival’ in “R” (version 2.40–1) and implemented in the R package for each therapeutic group in each geographic region.
Data with unknown geographical origin were excluded. The United States, Turkey, Italy, Germany and Greece were defined as single countries; other countries were grouped into regions (Northern Europe, the Mediterranean, North America, i.e. USA and Canada, Australia/New Zealand, Indo-Arabia, Asia and South America) to obtain sufficient sample sizes.
Category
Post hoc analyses of data for a systematic review and meta-analysis, no publication before. No submission in parallel. No full or partial presentation at a meeting or podium or conference.
Ethics
This article does not contain any studies with human participants. Therefore, no informed consent had to be obtained prior to preparation of the current manuscript.
Presentation
The manuscript has not been submitted elsewhere in parallel and has not been published previously. Some of the data were presented at the International Pilonidal Sinus Disease Conference in Berlin on Sept 23, 2017 and at the 2nd International Pilonidal Sinus Conference in Vienna on Sept 28th 2019.
Supplementary information
Acknowledgements
We acknowledge the editorial assistance of Jeannie Wurz, Science Writer in the Department of Anesthesiology and Pain Medicine, Inselspital, Bern University Hospital, University of Bern, 3010 Bern, Switzerland.
Author contributions
Statistical analysis and calculations: A.O., V.S., M.M.L., P.K., M.S. and D.D. Manuscript editing and interpretation of data: A.O., V.S., M.M.L., P.K., M.S., M.D., A.P.V., K.M.W. and D.D. Manuscript writing: A.O., V.S., M.M.L., A.P.V., P.K. and D.D. Graphic design: A.O., V.S., M.M.L., P.K., M.S. and D.D. Data acquisition: A.O., V.S., M.M.L., M.D., K.M.W. and D.D.
Data availability
All data and calculations are available to readers upon request to the corresponding author.
Competing interests
Dietrich Doll, Andriu Orlik, Katharina Maier, Peter Kauf, Marco Schmid, Maja Diekmann, Andreas P. Vogt, Verena K. Stauffer and Markus M. Luedi declare no competing financial interests. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. There are no relevant or minor financial relationships of authors, their relatives, or next of kin with external companies.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
is available for this paper at 10.1038/s41598-019-51159-z.
References
- 1.Doll DH, et al. Stop insulting the patient: neither incidence nor recurrence in pilonidal sinus disease is linked to personal hygiene. Pilonidal Sinus Journal. 2015;1:8. [Google Scholar]
- 2.Duman K, Girgin M, Harlak A. Prevalence of sacrococcygeal pilonidal disease in Turkey. Asian journal of surgery. 2017;40:434–437. doi: 10.1016/j.asjsur.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Segre D, Pozzo M, Perinotti R, Roche B. The treatment of pilonidal disease: guidelines of the Italian Society of Colorectal Surgery (SICCR) Tech Coloproctol. 2015;19:607–613. doi: 10.1007/s10151-015-1369-3. [DOI] [PubMed] [Google Scholar]
- 4.Steele SR, et al. Practice parameters for the management of pilonidal disease. Dis Colon Rectum. 2013;56:1021–1027. doi: 10.1097/DCR.0b013e31829d2616. [DOI] [PubMed] [Google Scholar]
- 5.Iesalnieks I, Ommer A, Petersen S, Doll D, Herold A. German national guideline on the management of pilonidal disease. Langenbecks Arch Surg. 2016;401:599–609. doi: 10.1007/s00423-016-1463-7. [DOI] [PubMed] [Google Scholar]
- 6.Doll D, et al. The presence of occipital hair in the pilonidal sinus cavity—a triple approach to proof. International Journal of Colorectal Disease. 2018;33:567–576. doi: 10.1007/s00384-018-2988-8. [DOI] [PubMed] [Google Scholar]
- 7.Stone HB. Pilonidal Sinus. Ann Surg. 1924;79:410–414. [PMC free article] [PubMed] [Google Scholar]
- 8.Davage ON. The Origin of Sacrococcygeal Pilonidal Sinuses. Am J Pathol. 1954;30:1191–1205. [PMC free article] [PubMed] [Google Scholar]
- 9.Sievert H, et al. The influence of lifestyle (smoking and body mass index) on wound healing and long-term recurrence rate in 534 primary pilonidal sinus patients. International Journal of Colorectal Disease. 2013;28:1555–1562. doi: 10.1007/s00384-013-1731-8. [DOI] [PubMed] [Google Scholar]
- 10.Stauffer VK, et al. Common surgical procedures in pilonidal sinus disease: A meta-analysis, merged data analysis, and comprehensive study on recurrence. Sci Rep. 2018;8:3058. doi: 10.1038/s41598-018-20143-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lessa FC, et al. Burden of Clostridium difficile infection in the United States. The New England journal of medicine. 2015;372:825–834. doi: 10.1056/NEJMoa1408913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crotty B. Ulcerative colitis and xenobiotic metabolism. Lancet (London, England) 1994;343:35–38. doi: 10.1016/S0140-6736(94)90882-6. [DOI] [PubMed] [Google Scholar]
- 13.Doll D, et al. Timeline of recurrence after primary and secondary pilonidal sinus surgery. Dis Colon Rectum. 2007;50:1928–1934. doi: 10.1007/s10350-007-9031-4. [DOI] [PubMed] [Google Scholar]
- 14.Allen-Mersh TG. Pilonidal sinus: finding the right track for treatment. Br J Surg. 1990;77:123–32. doi: 10.1002/bjs.1800770203. [DOI] [PubMed] [Google Scholar]
- 15.Ypsilantis E, Carapeti E, Chan S. The use of topical 10% metronidazole in the treatment of non-healing pilonidal sinus wounds after surgery. Int J Colorectal Dis. 2016;31:765–767. doi: 10.1007/s00384-015-2269-8. [DOI] [PubMed] [Google Scholar]
- 16.Milone M, Fernandez LM, Musella M, Milone F. Safety and Efficacy of Minimally Invasive Video-Assisted Ablation of Pilonidal Sinus: A Randomized Clinical Trial. JAMA Surg. 2016;151:547–553. doi: 10.1001/jamasurg.2015.5233. [DOI] [PubMed] [Google Scholar]
- 17.Johnson EK, Vogel JD, Cowan ML, Feingold DL, Steele SR. The American Society of Colon and Rectal Surgeons’ Clinical Practice Guidelines for the Management of Pilonidal Disease. Dis Colon Rectum. 2019;62:146–157. doi: 10.1097/dcr.0000000000001237. [DOI] [PubMed] [Google Scholar]
- 18.Doll D, et al. Strength of Occipital Hair as an Explanation for Pilonidal Sinus Disease Caused by Intruding Hair. Dis Colon Rectum. 2017;60:979–986. doi: 10.1097/DCR.0000000000000795. [DOI] [PubMed] [Google Scholar]
- 19.Bosche F, et al. The Hair in the Sinus: Sharp-Ended Rootless Head Hair Fragments can be Found in Large Amounts in Pilonidal Sinus Nests. World J Surg. 2018;42:567–573. doi: 10.1007/s00268-017-4093-5. [DOI] [PubMed] [Google Scholar]
- 20.Perruchoud C, Vuilleumier H, Givel JC. Pilonidal sinus: how to choose between excision and open granulation versus excision and primary closure? Study of a series of 141 patients operated on from 1991 to 1995. Swiss Surg. 2002;8:255–258. doi: 10.1024/1023-9332.8.6.255. [DOI] [PubMed] [Google Scholar]
- 21.Morden P, Drongowski RA, Geiger JD, Hirschl RB, Teitelbaum DH. Comparison of Karydakis versus midline excision for treatment of pilonidal sinus disease. Pediatr Surg Int. 2005;21:793–796. doi: 10.1007/s00383-005-1543-1. [DOI] [PubMed] [Google Scholar]
- 22.Mueller X, Rothenbuehler JM, Frede KE. Sacrococcygeal cysts. Is Lord Millar’s procedure an alternative to exeresis? J Chir (Paris) 1991;128:487–490. [PubMed] [Google Scholar]
- 23.Soll C, Hahnloser D, Dindo D, Clavien PA, Hetzer F. A novel approach for treatment of sacrococcygeal pilonidal sinus: less is more. Int J Colorectal Dis. 2008;23:177–180. doi: 10.1007/s00384-007-0377-9. [DOI] [PubMed] [Google Scholar]
- 24.al-Hassan HK, Francis IM, Neglen P. Primary closure or secondary granulation after excision of pilonidal sinus? Acta Chir Scand. 1990;156:695–699. [PubMed] [Google Scholar]
- 25.Fazeli MS, Adel MG, Lebaschi AH. Comparison of outcomes in Z-plasty and delayed healing by secondary intention of the wound after excision of the sacral pilonidal sinus: results of a randomized, clinical trial. Dis Colon Rectum. 2006;49:1831–1836. doi: 10.1007/s10350-006-0726-8. [DOI] [PubMed] [Google Scholar]
- 26.Menzel T, Dorner A, Cramer J. Excision and open wound treatment of pilonidal sinus. Rate of recurrence and duration of work incapacity. Dtsch Med Wochenschr. 1997;122:1447–1451. doi: 10.1055/s-2008-1047784. [DOI] [PubMed] [Google Scholar]
- 27.Rao MM, Zawislak W, Kennedy R, Gilliland R. A prospective randomised study comparing two treatment modalities for chronic pilonidal sinus with a 5-year follow-up. Int J Colorectal Dis. 2010;25:395–400. doi: 10.1007/s00384-009-0804-1. [DOI] [PubMed] [Google Scholar]
- 28.Jamal A, Shamim M, Hashmi F, Qureshi MI. Open excision with secondary healing versus rhomboid excision with Limberg transposition flap in the management of sacrococcygeal pilonidal disease. J Pak Med Assoc. 2009;59:157–160. [PubMed] [Google Scholar]
- 29.Dudink R, Veldkamp J, Nienhuijs S, Heemskerk J. Secondary healing versus midline closure and modified Bascom natal cleft lift for pilonidal sinus disease. Scand J Surg. 2011;100:110–113. doi: 10.1177/145749691110000208. [DOI] [PubMed] [Google Scholar]
- 30.Gupta PJ. Radiofrequency sinus excision: better alternative to marsupialization technique in sacrococcygeal pilonidal sinus disease. J Natl Med Assoc. 2005;97:998–1002. [PMC free article] [PubMed] [Google Scholar]
- 31.Holmebakk T, Nesbakken A. Surgery for pilonidal disease. Scand J Surg. 2005;94:43–46. doi: 10.1177/145749690509400111. [DOI] [PubMed] [Google Scholar]
- 32.Kement M, Oncel M, Kurt N, Kaptanoglu L. Sinus excision for the treatment of limited chronic pilonidal disease: results after a medium-term follow-up. Dis Colon Rectum. 2006;49:1758–1762. doi: 10.1007/s10350-006-0676-1. [DOI] [PubMed] [Google Scholar]
- 33.Kaser SA, Zengaffinen R, Uhlmann M, Glaser C, Maurer CA. Primary wound closure with a Limberg flap vs. secondary wound healing after excision of a pilonidal sinus: a multicentre randomised controlled study. Int J Colorectal Dis. 2015;30:97–103. doi: 10.1007/s00384-014-2057-x. [DOI] [PubMed] [Google Scholar]
- 34.Mohamed HA, Kadry I, Adly S. Comparison between three therapeutic modalities for non-complicated pilonidal sinus disease. Surgeon. 2005;3:73–77. doi: 10.1016/S1479-666X(05)80065-4. [DOI] [PubMed] [Google Scholar]
- 35.Testini M, et al. Treatment of chronic pilonidal sinus with local anaesthesia: a randomized trial of closed compared with open technique. Colorectal Dis. 2001;3:427–430. doi: 10.1046/j.1463-1318.2001.00278.x. [DOI] [PubMed] [Google Scholar]
- 36.Al-Salamah SM, Hussain MI, Mirza SM. Excision with or without primary closure for pilonidal sinus disease. J Pak Med Assoc. 2007;57:388–391. [PubMed] [Google Scholar]
- 37.Spivak H, Brooks VL, Nussbaum M, Friedman I. Treatment of chronic pilonidal disease. Dis Colon Rectum. 1996;39:1136–1139. doi: 10.1007/BF02081415. [DOI] [PubMed] [Google Scholar]
- 38.Aldaqal SM, Kensarah AA, Alhabboubi M, Ashy AA. A new technique in management of pilonidal sinus, a university teaching hospital experience. Int Surg. 2013;98:304–306. doi: 10.9738/INTSURG-D-13-00064.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soll C, et al. Sinusectomy for primary pilonidal sinus: less is more. Surgery. 2011;150:996–1001. doi: 10.1016/j.surg.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 40.Agren MS, et al. A randomized, double-blind, placebo-controlled multicenter trial evaluating topical zinc oxide for acute open wounds following pilonidal disease excision. Wound Repair Regen. 2006;14:526–535. doi: 10.1111/j.1743-6109.2006.00159.x. [DOI] [PubMed] [Google Scholar]
- 41.Gendy AS, et al. A comparison of the cleft lift procedure vs wide excision and packing for the treatment of pilonidal disease in adolescents. J Pediatr Surg. 2011;46:1256–1259. doi: 10.1016/j.jpedsurg.2011.03.062. [DOI] [PubMed] [Google Scholar]
- 42.Duxbury MS, Blake SM, Dashfield A, Lambert AW. A randomised trial of knife versus diathermy in pilonidal disease. R Coll Surg Engl. 2003;85:405–407. doi: 10.1308/003588403322520799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eftaiha M, Abcarian H. The dilemma of pilonidal disease: surgical treatment. Dis Colon Rectum. 1977;20:279–286. doi: 10.1007/BF02586423. [DOI] [PubMed] [Google Scholar]
- 44.Holzer B, et al. Efficacy and tolerance of a new gentamicin collagen fleece (Septocoll) after surgical treatment of a pilonidal sinus. Colorectal Dis. 2003;5:222–227. doi: 10.1046/j.1463-1318.2003.00471.x. [DOI] [PubMed] [Google Scholar]
- 45.Seleem MI, Al-Hashemy AM. Management of pilonidal sinus using fibrin glue: a new concept and preliminary experience. Colorectal Dis. 2005;7:319–322. doi: 10.1111/j.1463-1318.2005.00808.x. [DOI] [PubMed] [Google Scholar]
- 46.Solla JA, Rothenberger DA. Chronic pilonidal disease. An assessment of 150 cases. Dis Colon Rectum. 1990;33:758–761. doi: 10.1007/BF02052321. [DOI] [PubMed] [Google Scholar]
- 47.Spyridakis M, Christodoulidis G, Chatzitheofilou C, Symeonidis D, Tepetes K. The role of the platelet-rich plasma in accelerating the wound-healing process and recovery in patients being operated for pilonidal sinus disease: preliminary results. World J Surg. 2009;33:1764–1769. doi: 10.1007/s00268-009-0046-y. [DOI] [PubMed] [Google Scholar]
- 48.Chiedozi LC, Al-Rayyes FA, Salem MM, Al-Haddi FH, Al-Bidewi AA. Management of pilonidal sinus. Saudi Med J. 2002;23:786–788. [PubMed] [Google Scholar]
- 49.Keshvari A, et al. Karydakis flap versus excision-only technique in pilonidal disease. J Surg Res. 2015;198:260–266. doi: 10.1016/j.jss.2015.05.039. [DOI] [PubMed] [Google Scholar]
- 50.Biter LU, et al. The use of negative-pressure wound therapy in pilonidal sinus disease: a randomized controlled trial comparing negative-pressure wound therapy versus standard open wound care after surgical excision. Dis Colon Rectum. 2014;57:1406–1411. doi: 10.1097/DCR.0000000000000240. [DOI] [PubMed] [Google Scholar]
- 51.Viciano V, et al. Effect of hydrocolloid dressings on healing by second intention after excision of pilonidal sinus. Eur J Surg. 2000;166:229–232. doi: 10.1080/110241500750009339. [DOI] [PubMed] [Google Scholar]
- 52.Rabie ME, et al. Sacrococcygeal pilonidal disease: sinotomy versus excisional surgery, a retrospective study. ANZ J Surg. 2007;77:177–180. doi: 10.1111/j.1445-2197.2006.04002.x. [DOI] [PubMed] [Google Scholar]
- 53.Stansby G, Greatorex R. Phenol treatment of pilonidal sinuses of the natal cleft. Br J Surg. 1989;76:729–730. doi: 10.1002/bjs.1800760727. [DOI] [PubMed] [Google Scholar]
- 54.Ommer A, et al. Pilonidal Sinus–Primary Closure also in Case of Abscess? Zentralbl Chir. 2004;129:216–219. doi: 10.1055/s-2004-822742. [DOI] [PubMed] [Google Scholar]
- 55.Matter I, Kunin J, Schein M, Eldar S. Total excision versus non-resectional methods in the treatment of acute and chronic pilonidal disease. Br J Surg. 1995;82:752–753. doi: 10.1002/bjs.1800820612. [DOI] [PubMed] [Google Scholar]
- 56.Falco MD, et al. Il trattamento chirurgico del sinus pilonidalis con trasposizione di lembo secondo Dufourmentel Surgical treatment of sinus pilonidalis by Dufourmentel’s flap technique. Il Giornale di chirurgia. 2007;28:93–97. [PubMed] [Google Scholar]
- 57.Lukish JR, Kindelan T, Marmon LM, Pennington M, Norwood C. Laser epilation is a safe and effective therapy for teenagers with pilonidal disease. J Pediatr Surg. 2009;44:282–285. doi: 10.1016/j.jpedsurg.2008.10.057. [DOI] [PubMed] [Google Scholar]
- 58.Ghnnam WM, Hafez DM. Laser hair removal as adjunct to surgery for pilonidal sinus: our initial experience. J Cutan Aesthet Surg. 2011;4:192–195. doi: 10.4103/0974-2077.91251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baier PK, Baumgartner U, Furtwangler A, Holzinger F, Schoffel U. Therapy of the pilonidal sinus–Primary wound closure or open wound after excision. Zentralbl Chir. 2002;127:310–314. doi: 10.1055/s-2002-31557. [DOI] [PubMed] [Google Scholar]
- 60.Ortiz HH, Marti J, Sitges A. Pilonidal sinus: a claim for simple track incision. Dis Colon Rectum. 1977;20:325–328. doi: 10.1007/BF02586431. [DOI] [PubMed] [Google Scholar]
- 61.Goodall P. The aetiology and treatment of pilonidal sinus. A review of 163 patients. Br J Surg. 1961;49:212–218. doi: 10.1002/bjs.18004921421. [DOI] [PubMed] [Google Scholar]
- 62.Kooistra HP. Pilonidal sinuses. Review of the literature and report of three hundred fifty cases. Am J Surg. 1942;LV 1:3–17. doi: 10.1016/S0002-9610(42)90210-1. [DOI] [Google Scholar]
- 63.McKirdie M. Pilonidal Sinus. Ann Surg. 1938;107:389–399. doi: 10.1097/00000658-193803000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Iesalnieks I, Furst A, Rentsch M, Jauch KW. Primary midline closure after excision of a pilonidal sinus is associated with a high recurrence rate. Chirurg. 2003;74:461–468. doi: 10.1007/s00104-003-0616-8. [DOI] [PubMed] [Google Scholar]
- 65.Doll D, Matevossian E, Hoenemann C, Hoffmann S. Incision and drainage preceding definite surgery achieves lower 20-year long-term recurrence rate in 583 primary pilonidal sinus surgery patients. J Dtsch Dermatol Ges. 2013;11:60–64. doi: 10.1111/j.1610-0387.2012.08007.x. [DOI] [PubMed] [Google Scholar]
- 66.Iesalnieks I, Deimel S, Schlitt HJ. Karydakis flap for recurrent pilonidal disease. World J Surg. 2013;37:1115–1120. doi: 10.1007/s00268-013-1950-8. [DOI] [PubMed] [Google Scholar]
- 67.Hosseini M, Heidari A, Jafarnejad B. Comparison of Three Surgical Methods in Treatment of Patients with Pilonidal Sinus: Modified Excision and Repair/Wide Excision/Wide Excision and Flap in RASOUL, OMID and SADR Hospitals (2004–2007) Indian J Surg. 2013;75:395–400. doi: 10.1007/s12262-012-0713-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gupta PJ. Comparative study between radiofrequency sinus excision and open excision in sacro-coccygeal pilonidal sinus disease. Dig Surg. 2005;22:459–463. doi: 10.1159/000092034. [DOI] [PubMed] [Google Scholar]
- 69.Fitzpatrick EB, et al. Pilonidal disease in a military population: how far have we really come? Am J Surg. 2014;207:907–914. doi: 10.1016/j.amjsurg.2013.07.038. [DOI] [PubMed] [Google Scholar]
- 70.Patti R, et al. Use of fibrin glue in the treatment of pilonidal sinus disease: a pilot study. G Chir. 2006;27:331–334. [PubMed] [Google Scholar]
- 71.Nasr A, Ein SH. A pediatric surgeon’s 35-year experience with pilonidal disease in a Canadian children’s hospital. Can J Surg. 2011;54:39–42. doi: 10.1503/cjs.028509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Baldelli CM, et al. A short course of granulocyte-colony-stimulating factor to accelerate wound repair in patients undergoing surgery for sacrococcygeal pilonidal cyst: proof of concept. Cytotherapy. 2012;14:1101–1109. doi: 10.3109/14653249.2012.697147. [DOI] [PubMed] [Google Scholar]
- 73.Kareem TS. Surgical treatment of chronic sacrococcygeal pilonidal sinus. Open method versus primary closure. Saudi Med J. 2006;27:1534–1537. [PubMed] [Google Scholar]
- 74.Khawaja HT, Bryan S, Weaver PC. Treatment of natal cleft sinus: a prospective clinical and economic evaluation. BMJ (Clinical research ed.) 1992;304:1282–1283. doi: 10.1136/bmj.304.6837.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Notaras MJ. A review of three popular methods of treatment of postanal (pilonidal) sinus disease. Br J Surg. 1970;57:886–890. doi: 10.1002/bjs.1800571204. [DOI] [PubMed] [Google Scholar]
- 76.Oueidat D, et al. 25 years’ experience in the management of pilonidal sinus disease. Open Journal of Gastroenterology. 2014;4:5. doi: 10.4236/ojgas.2014.41001. [DOI] [Google Scholar]
- 77.Macfee WF. Pilonidal Cysts and Sinuses: A Method of Wound Closure: Review of 230 Cases. Ann Surg. 1942;116:687–699. doi: 10.1097/00000658-194211650-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kasim K, Abdlhamid NM, Badwan BR, Allowbany A. Is There a Relation Between Natal Cleft Depth and Post-Operative Morbidity After Different Methods of Excision of Sacro-Coccygeal Pilonidal Sinus? Indian J Surg. 2015;77:201–205. doi: 10.1007/s12262-012-0762-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Swenson SA, Harkins HN, Groesbeck HP. Pilonidal Sinus - Clinical Experiences with the Rogers Operation in thirty-five consecutive cases. Am J Surg. 1944;66:49–57. doi: 10.1016/S0002-9610(44)90226-6. [DOI] [Google Scholar]
- 80.Blanco G, Giordano M, Torelli I. Surgical treatment of pilonidal sinus with open surgical technique. Minerva Chir. 2003;58:181–187. [PubMed] [Google Scholar]
- 81.Hosseini SV, et al. The comparison between drainage, delayed excision and primary closure with excision and secondary healing in management of pilonidal abscess. Int J Surg. 2006;4:228–231. doi: 10.1016/j.ijsu.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 82.Fahrni GT, et al. Five-year Follow-up and Recurrence Rates Following Surgery for Acute and Chronic Pilonidal Disease: A Survey of 421 Cases. Wounds. 2016;28:20–26. [PubMed] [Google Scholar]
- 83.Kronborg O, Christensen K, Zimmermann-Nielsen C. Chronic pilonidal disease: a randomized trial with a complete 3-year follow-up. Br J Surg. 1985;72:303–304. doi: 10.1002/bjs.1800720418. [DOI] [PubMed] [Google Scholar]
- 84.Khatoon S, et al. Pilonidal sinus: Excision with primary midline closure versus open method. J. Liaquat Univ. Med. Health Sci. 2010;9:9–11. [Google Scholar]
- 85.Stelzmueller I, et al. Group Milleri Streptococci in perianal infections. Colorectal disease: the official journal of the Association of Coloproctology of Great Britain and Ireland. 2010;12:e121–127. doi: 10.1111/j.1463-1318.2009.01847.x. [DOI] [PubMed] [Google Scholar]
- 86.Sondenaa K, Nesvik I, Andersen E, Soreide JA. Recurrent pilonidal sinus after excision with closed or open treatment: final result of a randomised trial. Eur J Surg. 1996;162:237–240. [PubMed] [Google Scholar]
- 87.Shafik A. Electrocauterization in the treatment of pilonidal sinus. Int Surg. 1996;81:83–84. [PubMed] [Google Scholar]
- 88.Shah A, Waheed A, Malik A. Recurrence rates in pilonidal sinus surgery: Comparison of two techniques (Karydakis Versus Conventional Open Excision) Pak. J. Med. Health Sci. 2009;3:91–95. [Google Scholar]
- 89.Obedman M, Vaticon D. Pilonidal sinus: a high-incidence disease among adolescents. Int J Adolesc Med Health. 1993;6:21–36. doi: 10.1515/IJAMH.1993.6.1.21. [DOI] [PubMed] [Google Scholar]
- 90.Bracho Bracho, J. & Lira Soto, N. M. Enfermedad pilonidal: tecnica cerrada Vs. tecnica abierta con anestesia local. Boletin médico de postgrado (1996).
- 91.Coda A, Ferri F. Sinus pilonidalis: Removal and primary suture with aspirative draining [Sinus Pilonidalis: Escissione E Sutura Primaria Con Drenaggio Aspirativo] Chirurgia. 1990;3:433–437. [Google Scholar]
- 92.Dahmann S, Lebo PB, Meyer-Marcotty MV. Comparison of Treatments for an Infected Pilonidal Sinus: Differences in Scar Quality and Outcome Between Secondary Wound Healing and Limberg Flap in a Prospective Study. Handchir Mikrochir Plast Chir. 2016;48:111–119. doi: 10.1055/s-0041-111322. [DOI] [PubMed] [Google Scholar]
- 93.Sondenaa K, Nesvik I, Andersen E, Pollard ML, Soreide JA. Recurrent pilonidal sinus: Etiology and treatment. Dig. Surg. 1995;12:117–120. doi: 10.1159/000172329. [DOI] [Google Scholar]
- 94.Destito C, Romagnoli A, Pucello D, Mercuri M, Marin AW. Pilonidal sinus: long term results of excision and closure technic. Review of the literature. G Chir. 1997;18:441–446. [PubMed] [Google Scholar]
- 95.Donati A, et al. Heterologous lyophilized collagen in the secondary healing of pilonidal fistulae. Minerva Chir. 1993;48:141–145. [PubMed] [Google Scholar]
- 96.Leoni G, et al. Sinus pilonidalis. Critical review of our experience [Sinus pilonidalis. Revisione critica della nostra esperienza] Chirurgia. 1998;11:93–96. [Google Scholar]
- 97.Weckner W, Zorner M. Treatment of pilonidal sinus [Beitrag zur Behandlung der Pilonidalkrankheit] Z. Arztl. Fortbild. 1981;75:903–906. [PubMed] [Google Scholar]
- 98.Meier HP. Recurrence in sacral dermoid (sinusitis pilonidalis sacralis) Helv Chir Acta. 1983;49:645–649. [PubMed] [Google Scholar]
- 99.Rosato L, Fornero G, Luc AR, Clerico G. The radical treatment of sacrococcygeal pilonidal cysts. Minerva Chir. 1997;52:1277–1279. [PubMed] [Google Scholar]
- 100.Sturniolo G, Carditello A, Bonavita G, Bartolotta M, Saitta E. Evaluation of the results of different types of surgical intervention for pilonidal fistula. Minerva Chir. 1984;39:1161–1164. [PubMed] [Google Scholar]
- 101.Grandjean JP, Al Nashawati G. Pilonidal disease treated by wide excision and controlled cicatrisation. A report on 73 patients. Lyon Chir. 1996;92:292–295. [Google Scholar]
- 102.Garcia JC, Dupuis F. Surgical treatment of pilonidal disease. A new simplified technic. J Chir (Paris) 1983;120:347–350. [PubMed] [Google Scholar]
- 103.Gupta PJ. Radio surgery in pilonidal sinus: a new approach for the old problem. Acta Chir Belg. 2005;105:183–186. doi: 10.1080/00015458.2005.11679695. [DOI] [PubMed] [Google Scholar]
- 104.Rouch JD, et al. Short- and Long-term Results of Unroofing and Marsupialization for Adolescent Pilonidal Disease. JAMA Surg. 2016;151:877–879. doi: 10.1001/jamasurg.2016.0850. [DOI] [PubMed] [Google Scholar]
- 105.Houston HE. One-stage cure of infected pilonidal cysts. Am Surg. 1977;43:517–519. [PubMed] [Google Scholar]
- 106.Shah STA, Tahir M, Nasir M, Paracha SA, Wahab K. Outcome of open versus closed surgical technique for treatment of chronic pilonidal sinus: a randomized controlled trial. Khyber Med Univ J. 2013;5:146–151. [Google Scholar]
- 107.Tetirick JE. Limited excision of pilonidal cyst and sinus. Ohio State Med J. 1971;67:135–138. [PubMed] [Google Scholar]
- 108.Zagory JA, Golden J, Holoyda K, Demeter N, Nguyen NX. Excision and Primary Closure May Be the Better Option in the Surgical Management of Pilonidal Disease in the Pediatric Population. Am Surg. 2016;82:964–967. [PubMed] [Google Scholar]
- 109.Khodakaram K, Stark J, Hoglund I, Andersson RE. Minimal Excision and Primary Suture is a Cost-Efficient Definitive Treatment for Pilonidal Disease with Low Morbidity: A Population-Based Interventional and a Cross-Sectional Cohort Study. World J Surg. 2017;41:1295–1302. doi: 10.1007/s00268-016-3828-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gupta P. A comparison of two operations for pilonidal sinus disease. Nig J Surg Res. 2004;6:41–45. [Google Scholar]
- 111.Sasse, K. C., Brandt, J., Lim, D. C. & Ackerman, E. Accelerated healing of complex open pilonidal wounds using MatriStem extracellular matrix xenograft: nine cases. J Surg Case Rep2013, 10.1093/jscr/rjt025 (2013). [DOI] [PMC free article] [PubMed]
- 112.Elbanna HG, et al. Novel Approach of Treatment of Pilonidal Sinus Disease With Thrombin Gelatin Matrix as a Sealant. Dis Colon Rectum. 2016;59:775–780. doi: 10.1097/DCR.0000000000000604. [DOI] [PubMed] [Google Scholar]
- 113.Yamashita Y, Nagae H, Hashimoto I. Ambulatory Surgery for Pilonidal Sinus: Tract Excision and Open Treatment Followed by At-Home Irrigation. J Med Invest. 2016;63:216–218. doi: 10.2152/jmi.63.216. [DOI] [PubMed] [Google Scholar]
- 114.Calikoglu I, et al. Phenol Injection Versus Excision With Open Healing in Pilonidal Disease: A Prospective Randomized Trial. Dis Colon Rectum. 2017;60:161–169. doi: 10.1097/DCR.0000000000000717. [DOI] [PubMed] [Google Scholar]
- 115.Carstensen E, Keichel F. Etiology and therapy of pilonidal sinus. Chirurg. 1963;34:303–308. [PubMed] [Google Scholar]
- 116.Speter, C., Zmora, O., Nadler, R., Shinhar, D. & Bilik, R. Minimal incision as a promising technique for resection of pilonidal sinus in children. J Pediatr Surg, 10.1016/j.jpedsurg.2017.03.040 (2017). [DOI] [PubMed]
- 117.Gerhard H. On the understanding and treating coccygeal fustulae. Z. Arztl. Fortbild. 1963;57:841–843. [PubMed] [Google Scholar]
- 118.Ozcan, R. et al. Which treatment modality for pediatric pilonidal sinus: Primary repair or secondary healing? Asian J Surg, 10.1016/j.asjsur.2017.08.006 (2017). [DOI] [PubMed]
- 119.Shirah BH, Shirah HA. Factors affecting the outcome and duration of healing of the laid open wound for sacrococcygeal pilonidal sinus: A prospective cohort study of 472 patients. Wound Medicine. 2017;18:52–56. doi: 10.1016/j.wndm.2017.06.005. [DOI] [Google Scholar]
- 120.Zuin, M., Fogato, L. & Badin, A. Common risk factors for pilonidal sinus disease recurrence impact the onset of new cardiovascular disease in the longterm: a 5-year follow-up study. World J Surg (2017).
- 121.Danne J, Gwini S, McKenzie D, Danne P. A Retrospective Study of Pilonidal Sinus Healing by Secondary Intention Using Negative Pressure Wound Therapy Versus Alginate or Gauze Dressings. Ostomy Wound Manage. 2017;63:47–53. [PubMed] [Google Scholar]
- 122.Doll D, et al. Methylene Blue halves the long-term recurrence rate in acute pilonidal sinus disease. Int J Colorectal Dis. 2008;23:181–187. doi: 10.1007/s00384-007-0393-9. [DOI] [PubMed] [Google Scholar]
- 123.Bunke HJ, Schultheis A, Meyer G, Dusel W. Surgical revision of the pilonidal sinus with single shot antibiosis. Chirurg. 1995;66:220–223. [PubMed] [Google Scholar]
- 124.Kam BH. A simple surgical method of treating pilonidal sinus. Arch Chir Neerl. 1976;28:43–53. [PubMed] [Google Scholar]
- 125.Rainsbury RM, Southam JA. Radical surgery for pilonidal sinus. Annals of the Royal College of Surgeons of England. 1982;64:339–341. [PMC free article] [PubMed] [Google Scholar]
- 126.Sondenaa K, Andersen E, Nesvik I, Soreide JA. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995;10:39–42. doi: 10.1007/BF00337585. [DOI] [PubMed] [Google Scholar]
- 127.Akca T, Colak T, Ustunsoy B, Kanik A, Aydin S. Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary sacrococcygeal pilonidal disease. Br J Surg. 2005;92:1081–1084. doi: 10.1002/bjs.5074. [DOI] [PubMed] [Google Scholar]
- 128.Abu Galala KH, et al. Treatment of pilonidal sinus by primary closure with a transposed rhomboid flap compared with deep suturing: a prospective randomised clinical trial. Eur J Surg. 1999;165:468–472. doi: 10.1080/110241599750006721. [DOI] [PubMed] [Google Scholar]
- 129.Limongelli P, et al. D-shape asymmetric and symmetric excision with primary closure in the treatment of sacrococcygeal pilonidal disease. Am J Surg. 2014;207:882–889. doi: 10.1016/j.amjsurg.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 130.Khan PS, Hayat H, Hayat G. Limberg flap versus primary closure in the treatment of primary sacrococcygeal pilonidal disease; a randomized clinical trial. Indian J Surg. 2013;75:192–194. doi: 10.1007/s12262-012-0430-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Dass TA, Zaz M, Rather A, Bari S. Elliptical excision with midline primary closure versus rhomboid excision with limberg flap reconstruction in sacrococcygeal pilonidal disease: a prospective, randomized study. Indian J Surg. 2012;74:305–308. doi: 10.1007/s12262-011-0400-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Aldean I, Shankar PJ, Mathew J, Safarani N, Haboubi NY. Simple excision and primary closure of pilonidal sinus: a simple modification of conventional technique with excellent results. Colorectal Dis. 2005;7:81–85. doi: 10.1111/j.1463-1318.2004.00736.x. [DOI] [PubMed] [Google Scholar]
- 133.Can MF, Sevinc MM, Yilmaz M. Comparison of Karydakis flap reconstruction versus primary midline closure in sacrococcygeal pilonidal disease: results of 200 military service members. Surg Today. 2009;39:580–586. doi: 10.1007/s00595-008-3926-0. [DOI] [PubMed] [Google Scholar]
- 134.Gilani SN, et al. Excision and primary closure of pilonidal sinus disease: worthwhile option with an acceptable recurrence rate. Ir J Med Sci. 2011;180:173–176. doi: 10.1007/s11845-010-0532-0. [DOI] [PubMed] [Google Scholar]
- 135.Enshaei A, Motearefi S. Comparison of two surgical methods, primary closure and rotational flap, in patients with chronic pilonidal sinus. Glob J Health Sci. 2014;6:18–22. doi: 10.5539/gjhs.v6n7p18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Emir S, Topuz O, Kanat BH, Bali I. Sinotomy technique versus surgical excision with primary closure technique in pilonidal sinus disease. Bosn J Basic Med Sci. 2014;14:263–267. doi: 10.17305/bjbms.2014.4.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Osmanoglu G, Yetisir F. Limberg flap is better for the surgical treatment of pilonidal sinus. Results of a 767 patients series with an at least five years follow-up period. Chirurgia (Bucur) 2011;106:491–494. [PubMed] [Google Scholar]
- 138.Lorant T, Ribbe I, Mahteme H, Gustafsson UM, Graf W. Sinus excision and primary closure versus laying open in pilonidal disease: a prospective randomized trial. Dis Colon Rectum. 2011;54:300–305. doi: 10.1007/DCR.0b013e31820246bf. [DOI] [PubMed] [Google Scholar]
- 139.Onder A, et al. Pilonidal sinus disease: risk factors for postoperative complications and recurrence. Int Surg. 2012;97:224–229. doi: 10.9738/CC86.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Galal Elshazly W, Said K. Clinical trial comparing excision and primary closure with modified Limberg flap in the treatment of uncomplicated sacrococcygeal pilonidal disease. Alexandria Journal of Medicine. 2012;48:13–18. doi: 10.1016/j.ajme.2011.10.002. [DOI] [Google Scholar]
- 141.Al-Jaberi TM. Excision and simple primary closure of chronic pilonidal sinus. Eur J Surg. 2001;167:133–135. doi: 10.1080/110241501750070600. [DOI] [PubMed] [Google Scholar]
- 142.Khaira HS, Brown JH. Excision and primary suture of pilonidal sinus. Ann R Coll Surg Engl. 1995;77:242–244. [PMC free article] [PubMed] [Google Scholar]
- 143.Gencosmanoglu R, Inceoglu R. Modified lay-open (incision, curettage, partial lateral wall excision and marsupialization) versus total excision with primary closure in the treatment of chronic sacrococcygeal pilonidal sinus: a prospective, randomized clinical trial with a complete two-year follow-up. Int J Colorectal Dis. 2005;20:415–422. doi: 10.1007/s00384-004-0710-5. [DOI] [PubMed] [Google Scholar]
- 144.Tritapepe R, Di Padova C. Excision and primary closure of pilonidal sinus using a drain for antiseptic wound flushing. Am J Surg. 2002;183:209–211. doi: 10.1016/S0002-9610(01)00876-5. [DOI] [PubMed] [Google Scholar]
- 145.El-Shaer WM. The modified gluteal sliding plication closure in the treatment of chronic pilonidal sinus. Int J Colorectal Dis. 2010;25:887–894. doi: 10.1007/s00384-010-0911-z. [DOI] [PubMed] [Google Scholar]
- 146.Milone M, Musella M, Salvatore G, Leongito M, Milone F. Effectiveness of a drain in surgical treatment of sacrococcygeal pilonidal disease. Results of a randomized and controlled clinical trial on 803 consecutive patients. Int J Colorectal Dis. 2011;26:1601–1607. doi: 10.1007/s00384-011-1242-4. [DOI] [PubMed] [Google Scholar]
- 147.Serour F, Somekh E, Krutman B, Gorenstein A. Excision with primary closure and suction drainage for pilonidal sinus in adolescent patients. Pediatr Surg Int. 2002;18:159–161. doi: 10.1007/s003830100683. [DOI] [PubMed] [Google Scholar]
- 148.Ertan T, et al. Does technique alter quality of life after pilonidal sinus surgery? Am J Surg. 2005;190:388–392. doi: 10.1016/j.amjsurg.2004.08.068. [DOI] [PubMed] [Google Scholar]
- 149.Alptekin H, et al. Specimen index may be a predictive factor for recurrence after primary closure of pilonidal disease. J Korean Surg Soc. 2012;83:367–373. doi: 10.4174/jkss.2012.83.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Andersson RE, Lukas G, Skullman S, Hugander A. Local administration of antibiotics by gentamicin-collagen sponge does not improve wound healing or reduce recurrence rate after pilonidal excision with primary suture: a prospective randomized controlled trial. World J Surg. 2010;34:3042–3048. doi: 10.1007/s00268-010-0763-2. [DOI] [PubMed] [Google Scholar]
- 151.Badawy EA, Kanawati MN. Effect of hair removal by Nd:YAG laser on the recurrence of pilonidal sinus. J Eur Acad Dermatol Venereol. 2009;23:883–886. doi: 10.1111/j.1468-3083.2009.03147.x. [DOI] [PubMed] [Google Scholar]
- 152.Lee SL, Tejirian T, Abbas MA. Current management of adolescent pilonidal disease. J Pediatr Surg. 2008;43:1124–1127. doi: 10.1016/j.jpedsurg.2008.02.042. [DOI] [PubMed] [Google Scholar]
- 153.Othman I. Skin glue improves outcome after excision and primary closure of sacrococcygeal pilonidal disease. Indian J Surg. 2010;72:470–474. doi: 10.1007/s12262-010-0170-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Courtney SP, Merlin MJ. The use of fusidic acid gel in pilonidal abscess treatment: cure, recurrence and failure rates. Ann R Coll Surg Engl. 1986;68:170–171. [PMC free article] [PubMed] [Google Scholar]
- 155.Williams, R. S. A simple technique for successful primary closure after excision of pilonidal sinus disease. Ann R Coll Surg Engl72, 313–314; discussion 314–315 (1990). [PMC free article] [PubMed]
- 156.Tejirian T, Lee JJ, Abbas MA. Is wide local excision for pilonidal disease still justified? Am Surg. 2007;73:1075–1078. [PubMed] [Google Scholar]
- 157.Shons AR, Mountjoy JR. Pilonidal disease: the case for excision with primary closure. Dis Colon Rectum. 1971;14:353–355. doi: 10.1007/BF02553421. [DOI] [PubMed] [Google Scholar]
- 158.Terzi C, Canda AE, Unek T, Dalgic E, Fuzun M. What is the role of mechanical bowel preparation in patients with pilonidal sinus undergoing surgery? Prospective, randomized, surgeon-blinded trial. World J Surg. 2005;29:1465–1471. doi: 10.1007/s00268-005-0007-z. [DOI] [PubMed] [Google Scholar]
- 159.Aysan E, Basak F, Kinaci E, Sevinc M. Efficacy of local adrenalin injection during sacrococcygeal pilonidal sinus excision. Eur Surg Res. 2004;36:256–258. doi: 10.1159/000078861. [DOI] [PubMed] [Google Scholar]
- 160.Arda IS, Guney LH, Sevmis S, Hicsonmez A. High body mass index as a possible risk factor for pilonidal sinus disease in adolescents. World J Surg. 2005;29:469–471. doi: 10.1007/s00268-004-7533-y. [DOI] [PubMed] [Google Scholar]
- 161.Tocchi A, et al. Ambulatory closed surgery for the treatment of pilonidal sinus. G Chir. 2001;22:303–307. [PubMed] [Google Scholar]
- 162.Toccaceli S, Persico Stella L, Diana M, Dandolo R, Negro P. Treatment of pilonidal sinus with primary closure. A twenty-year experience. Chir Ital. 2008;60:433–438. [PubMed] [Google Scholar]
- 163.Örhalmi J, Sotona O, Dusek T, Ferko A. Pilonidal sinus - possibilities surgical treatment. Rozhl Chir. 2014;93:491–495. [PubMed] [Google Scholar]
- 164.Russell JL. A method of excision and primary closure of pilonidal cysts and sinuses. Can Med Assoc J. 1949;60:267–270. [PMC free article] [PubMed] [Google Scholar]
- 165.Muzi MG, et al. Randomized comparison of Limberg flap versus modified primary closure for the treatment of pilonidal disease. Am J Surg. 2010;200:9–14. doi: 10.1016/j.amjsurg.2009.05.036. [DOI] [PubMed] [Google Scholar]
- 166.Milone M, et al. Intradermal absorbable sutures to close pilonidal sinus wounds: a safe closure method? Surg Today. 2014;44:1638–1642. doi: 10.1007/s00595-013-0741-z. [DOI] [PubMed] [Google Scholar]
- 167.Gipponi M, Reboa G, Testa T, Giannini G, Strada P. Tension-free primary closure with autologous platelet gel versus Vivostat- for the definitive treatment of chronic sacrococcygeal pilonidal disease. In Vivo. 2010;24:583–589. [PubMed] [Google Scholar]
- 168.Biffoni M, et al. Pilonidal sinus. Outpatient treatment with local anesthesia. G Chir. 2009;30:173–176. [PubMed] [Google Scholar]
- 169.Inan A, Surgit O, Sen M, Bozer M, Dener C. One day surgery for pilonidal disease. Bratisl Lek Listy. 2011;112:572–574. [PubMed] [Google Scholar]
- 170.Lee HC, Ho YH, Seow CF, Eu KW, Nyam D. Pilonidal disease in Singapore: clinical features and management. Aust N Z J Surg. 2000;70:196–198. doi: 10.1046/j.1440-1622.2000.01785.x. [DOI] [PubMed] [Google Scholar]
- 171.Muzi MG, Milito G, Nigro C, Cadeddu F, Farinon AM. A modification of primary closure for the treatment of pilonidal disease in day-care setting. Colorectal Dis. 2009;11:84–88. doi: 10.1111/j.1463-1318.2008.01534.x. [DOI] [PubMed] [Google Scholar]
- 172.Sevinc B, et al. Randomized prospective comparison of midline and off-midline closure techniques in pilonidal sinus surgery. Surgery. 2016;159:749–754. doi: 10.1016/j.surg.2015.09.024. [DOI] [PubMed] [Google Scholar]
- 173.Nursal TZ, et al. Prospective randomized controlled trial comparing V-Y advancement flap with primary suture methods in pilonidal disease. Am J Surg. 2010;199:170–177. doi: 10.1016/j.amjsurg.2008.12.030. [DOI] [PubMed] [Google Scholar]
- 174.Yildiz T, Ilce Z, Kucuk A. Modified Limberg flap technique in the treatment of pilonidal sinus disease in teenagers. J Pediatr Surg. 2014;49:1610–1613. doi: 10.1016/j.jpedsurg.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 175.Cruz J, Ram MD. Sacrococcygeal pilonidal sinus. Dis Colon Rectum. 1971;14:356–359. doi: 10.1007/BF02553422. [DOI] [PubMed] [Google Scholar]
- 176.Kaya B, Uctum Y, Simsek A, Kutanis R. Primary closure in the treatment of pilonidal disease. An easy and effective method. Kolon Rektum Hast Derg. 2010;20:59–65. [Google Scholar]
- 177.Abbasi HR, Hosseini SV, Yarmohammadi H, Bolandparvaz S. Comparison between two methods of excision and primary closure of pilonidal sinus. Wound pain. 2007;9:143–146. [Google Scholar]
- 178.Braungart S, Powis M, Sutcliffe JR, Sugarman ID. Improving outcomes in pilonidal sinus disease. J Pediatr Surg. 2016;51:282–284. doi: 10.1016/j.jpedsurg.2015.10.076. [DOI] [PubMed] [Google Scholar]
- 179.Milone, M. et al. Pilonidal sinus surgery: could we predict postoperative complications? Int Wound J., 10.1111/iwj.12310 (2014). [DOI] [PMC free article] [PubMed]
- 180.Doll D, et al. Does gentamycin affect long term recurrence rate in pilonidal sinus surgery? European Surgery. 2011;43:236–243. doi: 10.1007/s10353-011-0615-9. [DOI] [Google Scholar]
- 181.Ferguson LK. Pilonidal Cysts: Treatment by Excision and Primary Suture in Ambulatory Patients. Ann Surg. 1935;101:469–477. doi: 10.1097/00000658-193501000-00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Galati G, Sterpetti AV, Tartaglia E. Therapeutic approaches to patients with pilonidal sinus based on specific clinical characteristic. Eur J Plast Surg. 2012;35:595–598. doi: 10.1007/s00238-011-0662-2. [DOI] [Google Scholar]
- 183.Talu M, Yücel O, User Y. Oblique excision with primary closure for the treatment of pilonidal sinus. Eur J Plast Surg. 1996;19:200–203. doi: 10.1007/BF00176279. [DOI] [Google Scholar]
- 184.Sakr, M. F., Hamed, H. H., Ramadan, M. A., Kantoush, H. E. & Al-Torky, H. M. Pilonidal sinus in Kuwait: Analysis of 801 consecutive patients (2012).
- 185.Washer JD, Smith DE, Carman ME, Blackhurst DW. Gluteal fascial advancement: an innovative, effective method for treating pilonidal disease. Am Surg. 2010;76:154–156. [PubMed] [Google Scholar]
- 186.Muzi MG, et al. Long-term results of pilonidal sinus disease with modified primary closure: new technique on 450 patients. Am Surg. 2014;80:484–488. [PubMed] [Google Scholar]
- 187.Miocinovic M, Horzic M, Bunoza D. The treatment of pilonidal disease of the sacrococcygeal region by the method of limited excision and open wound healing. Acta Med Croatica. 2000;54:27–31. [PubMed] [Google Scholar]
- 188.Sondenaa K, et al. Influence of failure of primary wound healing on subsequent recurrence of pilonidal sinus. combined prospective study and randomised controlled trial. Eur J Surg. 2002;168:614–618. doi: 10.1080/11024150201680007. [DOI] [PubMed] [Google Scholar]
- 189.Sakr MF, Elserafy ME, Hamed HM. Management of 634 Consecutive Patients with Chronic Pilonidal Sinus: A Nine-Year Experience of a Single Institute. Surgical. Science. 2012;3:145–154. [Google Scholar]
- 190.Youssef T, El-Awady S, Farid M. Tension-free primary closure compared with modified Limberg flap for pilonidal sinus disease: a prospective balanced randomized study. The Egyptian Journal of Surgery. 2015;34:85–89. doi: 10.4103/1110-1121.155716. [DOI] [Google Scholar]
- 191.Mahdy T. Surgical treatment of the pilonidal disease: primary closure or flap reconstruction after excision. Dis Colon Rectum. 2008;51:1816–1822. doi: 10.1007/s10350-008-9436-8. [DOI] [PubMed] [Google Scholar]
- 192.Saylam B, Balli DN, Duzgun AP, Ozer MV, Coskun F. Which surgical procedure offers the best treatment for pilonidal disease? Langenbecks Arch Surg. 2011;396:651–658. doi: 10.1007/s00423-011-0768-9. [DOI] [PubMed] [Google Scholar]
- 193.Smith CM, Jones A, Dass D, Murthi G, Lindley R. Early experience of the use of fibrin sealant in the management of children with pilonidal sinus disease. J Pediatr Surg. 2015;50:320–322. doi: 10.1016/j.jpedsurg.2014.11.022. [DOI] [PubMed] [Google Scholar]
- 194.Khanzada TW, Samad A. Recurrence after excision and primary closure of pilonidal sinus. Pak. J. Med. Sci. 2007;23:375–379. [Google Scholar]
- 195.Sakr MF, Moussa M. A prospective controlled randomized trial comparing Karydakis technique and midline closure in patients with recurrent chronic pilonidal sinus. Surg. Chronicles. 2011;16:84–90. [Google Scholar]
- 196.Siddiqui SS, Khan MA. Pilonidal sinus: Following the Aristotelian middle! Pak. J. Med. Sci. 2008;24:845–848. [Google Scholar]
- 197.Benfatto G, et al. Drainage useful in the excision and closure “per primam” of pilonidal sinus: technical notes. Chir Ital. 2003;55:621–624. [PubMed] [Google Scholar]
- 198.Bouq YA, Fazili FM, Fawzi HAG, Parvez T. Surgical management of pilonidal disease: Our experience. JK Pract. 2004;11:21–26. [Google Scholar]
- 199.Polat N, Albayrak D, Ibiş AC, Altan A. Comparison between karydakis flap repair and primary closure for surgical treatment of sacrococcygeal pilonidal sinus [Sakrokoksigeal pilonidal sinüsün cerrahi tedavisinde karydakis flep ameliyati ile primer kapamanin karşilaştirilmasi] Trakya Universitesi Tip Fakultesi Dergisi. 2008;25:87–94. [Google Scholar]
- 200.Toydemir T, Peşluk O, Ermeç ED, Turhan AN. Comparison of the clinical outcomes of karydakis flap versus primary closure procedures in the surgical treatment of sacrococcygeal pilonidal sinus disease [Sakrokosigeal pilonidal sinüs hastaliǧinin cerrahi tedavisinde karydakis flap ile primer kapama prosedürlerinin klinik sonuçlarinin karşilaştirilmasi] Med. J. Bakirkoy. 2012;8:78–81. doi: 10.5350/BTDMJB201208206. [DOI] [Google Scholar]
- 201.Çaglayan K, et al. The effect of different surgical methods on complications and on the quality of life in pilonidal sinus disease. Turk. J. Surg. 2011;27:94–97. doi: 10.5097/1300-0705.UCD.950-11.03. [DOI] [Google Scholar]
- 202.Sakr M, Habib M, Shaheed AA. Assessment of Karydakis technique as compared with midline closure for the management of chronic pilonidal sinus. J. Pelvic Med. Surg. 2006;12:201–206. doi: 10.1097/01.spv.0000217399.78641.43. [DOI] [Google Scholar]
- 203.Albahadili MA, Awazli LG. Pilonidal Sinus Excision Using Carbon Dioxide Laser 10600 nm. Iraqi J Laser. 2015;14:33–40. [Google Scholar]
- 204.Novotny GME. and Primary Closure of Pilonidal Sinus. A Critical Review of Forty-Five Cases. Med Serv J Can. 1964;20:352–354. [PubMed] [Google Scholar]
- 205.Maniscalco L, Speranza G, Maniscalco A. The pilonidal sinus: Which managment? [Il seno pilonidale: Come trattarlo?] Chirurgia. 2001;14:81–83. [Google Scholar]
- 206.Corsi, P. R., Corsi, R., Moura, L. F. R. A., Guerreiro, T. D. T. & Vasconcellos, L. P. Tratamento cirurgico do cisto pilonidal atraves de resseccao e fechamento primario com retalhos cutaneos. Revista brasileira de colo-proctologia (2004).
- 207.Jarufe CN, Bannura G, Contreras J, Saxton F, Marro P. Enfermedad pilonidal cronica sacrococcigea. Rev. Chil. Cir. 1999;51:66–71. [Google Scholar]
- 208.Blake P. P. et al. Tratamiento quirurgico del quiste pilonidal. Rev. Chil. Cir (1997).
- 209.Alberti P, Antoci G, Pasini M, Pasini GF. Pilonidal sinus: our experience in the surgical treatment by closed method. Minerva Chir. 1990;45:733–737. [PubMed] [Google Scholar]
- 210.Aaser P, Gruner OP. Pilonidal cysts. Excision and intracutaneous absorbable primary suture. Tidsskr Nor Laegeforen. 1992;112:206–207. [PubMed] [Google Scholar]
- 211.Klug W, Knoch HG, Holland-Moritz A. Sinus pilonidalis. Zeitschrift für ärztliche Fortbildung. 1984;78:711–714. [PubMed] [Google Scholar]
- 212.Bissett IP, Isbister WH. The management of patients with pilonidal disease - a comparative study. Aust N Z J Surg. 1987;57:939–942. doi: 10.1111/j.1445-2197.1987.tb01298.x. [DOI] [PubMed] [Google Scholar]
- 213.Sondenaa K, et al. The role of cefoxitin prophylaxis in chronic pilonidal sinus treated with excision and primary suture. J Am Coll Surg. 1995;180:157–160. [PubMed] [Google Scholar]
- 214.Palmieri B, Gozzi G, Rossi A. Pilonidal cysts: the state of the art and the authors’ personal experiences. Minerva Chir. 1994;49:377–382. [PubMed] [Google Scholar]
- 215.Diana G, Muscarella F, Pepe D, Speciale A. Primary closure in the treatment of pilonidal sinus. Evaluation of immediate and remote results [La chiusura per primam nel trattamento del sinus pilonidalis. Valutazione dei risultati immediati e a distanza]m. Minerva Chir. 1986;41:765–767. [PubMed] [Google Scholar]
- 216.Muller XM, Rothenbuhler JM, Frede KE. Sacro-coccygeal cyst: surgical techniques and results] Helv Chir Acta. 1992;58:889–892. [PubMed] [Google Scholar]
- 217.Angermann P, Beiter EC. [Pilonidal cyst. A sequence treated with excision and primary suture. Ugeskr Laeger. 1984;146:24–26. [PubMed] [Google Scholar]
- 218.Mecchia P, Tonizzo CA, Flamia M. Pilonidal cysts and fistulas: radical excision “en bloc” and closure “per primam”. Minerva Chir. 1995;50:553–556. [PubMed] [Google Scholar]
- 219.Rossi P, et al. The pilonidal sinus: its surgical treatment, our experience and a review of the literature. G Chir. 1993;14:120–123. [PubMed] [Google Scholar]
- 220.Sias F, Licheri S, Secci L, Loi R, Daniele GM. Ambulatory treatment of pilonidal sinus IL Trattamento Ambulatoriale Del Sinus Pilonidalis. Chirurgia. 1994;7:639–642. [Google Scholar]
- 221.Pozzi C, Tritapepe R. Healing of the operative wound after radical removal of the Sinus pilonidalis [Guarigione per prima intenzione dopo intervento radicale asportazione del Sinus Pilonidalis] Minerva Chir. 1989;44:2329–2332. [PubMed] [Google Scholar]
- 222.Virgillo, G., Mendicino, F. & Costanzo, A. Sinus pilonidalis. Brief review of literature and contribution to surgical therapy [Il Sinus Pilonidalis. Rivista sintetica della letteratura e contributo alla terapia chirugica]. 27, 1–40 (1975).
- 223.Christensen K, Kronborg O, Zimmermann-Nielsen C, Olsen H. Incision or primary suture in acute pilonidal abscesses. A prospective randomized study. Ugeskr Laeger. 1985;147:3479–3481. [PubMed] [Google Scholar]
- 224.Sarles JC, Sastre B, Delecourt P. Treatment of pilonidal cyst with radical excision and primary closure (author’s transl) Gastroenterol Clin Biol. 1977;1:929–932. [PubMed] [Google Scholar]
- 225.Verbeek HO, Bender J. Results of treatment of pilonidal sinus by block excision and primary suture. Arch Chir Neerl. 1974;26:311–318. [PubMed] [Google Scholar]
- 226.Schonk JW. Some aspects of the treatment of the pilonidal sinus. Arch Chir Neerl. 1971;23:297–302. [PubMed] [Google Scholar]
- 227.Powell BC, Webb CB, Ewing JA, Smith DE. Gluteal Fascial Advancement for Pilonidal Cyst Disease: A 10-year Review. Am Surg. 2016;82:622–625. [PubMed] [Google Scholar]
- 228.Ghnnam W, Ghazy H, Saed B, Farid M. Limited excision and primary closure for pilonidal sinus. Egypt J Surg. 2009;28:43–47. [Google Scholar]
- 229.Almajid FM, Alabdrabalnabi AA, Almulhim KA. The risk of recurrence of Pilonidal disease after surgical management. Saudi Med J. 2017;38:70–74. doi: 10.15537/smj.2017.1.15892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Liboni NS, Fregnani CHTG. Preliminary results from 28 cases of pilonidal cyst treated by excision and primary closure of the wound, reinforced with support suturing. Einstein. 2007;5:148–152. [Google Scholar]
- 231.Roshdy H, Ali Y, Askar W, Awad I, Farid M. Rhomboid flap versus primary closure after excision of saccrococcigeal pilonidal sinus (a prospective randomized study) Egypt J Surg. 2010;29:146–152. [Google Scholar]
- 232.Çaglayan K, et al. Investigation of Patient Dependent Factors Effecting Complications and Recurrence in Pilonidal Sinus Disease. Kolon Rektum Hast Derg. 2011;21:103–108. doi: 10.5505/KRHD.2011.43434. [DOI] [Google Scholar]
- 233.Pomazkin VI, Mansurov IV. Choice of operation for treatment of patients with pilonidal sinus. Vestn Khir Im I I Grek. 2008;167:85–87. [PubMed] [Google Scholar]
- 234.Grubnik, V. V. & Bakhar, G. A. The use of a laser in the surgical treatment of an epithelial coccygeal cyst. Klin Khir, 23–25 (1993). [PubMed]
- 235.de Quinta Frutosa R, et al. Enfermedad pilonidal. Tratamiento por exéresis en bloque con cierre primario. Cir Esp. 2000;68:570–572. [Google Scholar]
- 236.Wani, M., Shah, M., Wani, K. & Malik, A. Excision and primary closure of sacrococcygeal pilonidal sinus using suction drain. International Surgery Journal, 837–840, 10.18203/2349-2902.isj20161158 (2016).
- 237.Bowers WF, Williamson WS. Pilonidal sinus; preliminary report on a fresh approach. AMA Arch Surg. 1956;73:931–935. doi: 10.1001/archsurg.1956.01280060031006. [DOI] [PubMed] [Google Scholar]
- 238.Abou-Zikry AS, Guindi A, Hashem M. Pilonidal sinus and cysts (sacro-coccygeal sinus); report of 22 cases treated by excision and primary suture. J Egypt Med Assoc. 1954;37:696–705. [PubMed] [Google Scholar]
- 239.Frostad H. Sacral dermoidcysts. Especially with a view to their treatment. Acta chir scand. 1946;93:23. [PubMed] [Google Scholar]
- 240.Muzi MG, et al. 389 - Muzi’s Tension Free Primary Closure of Pilonidal Sinus Disease: Long-Term Results on 450 Patients. Gastroenterology. 2017;152:S1212–S1213. doi: 10.1016/S0016-5085(17)34034-9. [DOI] [Google Scholar]
- 241.Darwish A, Eskandaros M, Hegab A. Sacrococcygeal pilonidal sinus: modified sinotomy versus lay-open, limited excision, and primary closure. The Egyptian Journal of Surgery. 2017;36:13–19. doi: 10.4103/1110-1121.199901. [DOI] [Google Scholar]
- 242.Ates, U. et al. Pilonidal sinus disease surgery in children: the first study to compare crystallized phenol application to primary excision and closure. J Pediatr Surg, 10.1016/j.jpedsurg.2017.05.012 (2017). [DOI] [PubMed]
- 243.Kose E, Hasbahceci M, Tonyali H, Karagulle M. Comparative analysis of the same technique-the same surgeon approach in the surgical treatment of pilonidal sinus disease: a retrospective cohort study. Ann Surg Treat Res. 2017;93:82–87. doi: 10.4174/astr.2017.93.2.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Ahmadinejad M, Ahmadi K, Ahmadinejad I, Masoud Hashemian A, Khademhoseini P. A Comparison between the Tie-over and Closed Suction Drainage Therapeutic Strategies in Patients Suffering from Sacral Pilonidal Sinus. Int J Biomed Sci. 2016;12:149–154. [PMC free article] [PubMed] [Google Scholar]
- 245.Hulten L. Sacral Dermoid–Pilonidal Sinus. Nord Med. 1965;74:699–703. [PubMed] [Google Scholar]
- 246.Okus A, Sevinc B, Karahan O, Eryilmaz MA. Comparison of Limberg flap and tension-free primary closure during pilonidal sinus surgery. World J Surg. 2012;36:431–435. doi: 10.1007/s00268-011-1333-y. [DOI] [PubMed] [Google Scholar]
- 247.Mentes O, et al. Management of pilonidal sinus disease with oblique excision and primary closure: results of 493 patients. Dis Colon Rectum. 2006;49:104–108. doi: 10.1007/s10350-005-0226-2. [DOI] [PubMed] [Google Scholar]
- 248.Akinci OF. Limited separate ellyptical excision for complicated pilonidal disease. Colorectal Dis. 2005;7:424–425. doi: 10.1111/j.1463-1318.2005.00824.x. [DOI] [PubMed] [Google Scholar]
- 249.Kitchen PR. Pilonidal sinus: experience with the Karydakis flap. Br J Surg. 1996;83:1452–1455. doi: 10.1002/bjs.1800831040. [DOI] [PubMed] [Google Scholar]
- 250.Marzouk DM, Abou-Zeid AA, Antoniou A, Haji A, Benziger H. Sinus excision, release of coccycutaneous attachments and dermal-subcuticular closure (XRD procedure): a novel technique in flattening the natal cleft in pilonidal sinus treatment. Ann R Coll Surg Engl. 2008;90:371–376. doi: 10.1308/003588408X285955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Senapati A, Cripps NP, Flashman K, Thompson MR. Cleft closure for the treatment of pilonidal sinus disease. Colorectal Dis. 2011;13:333–336. doi: 10.1111/j.1463-1318.2009.02148.x. [DOI] [PubMed] [Google Scholar]
- 252.Maghsoudi H, Nezami N, Ghamari AA. Ambulatory treatment of chronic pilonidal sinuses with lateral incision and primary suture. Can J Surg. 2011;54:78–82. doi: 10.1503/cjs.026309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Ciftci F, Abdurrahman I, Tosun M, Bas G. A new approach: oblique excision and primary closure in the management of acute pilonidal disease. Int J Clin Exp Med. 2014;7:5706–5710. [PMC free article] [PubMed] [Google Scholar]
- 254.Greenberg R, Kashtan H, Skornik Y, Werbin N. Treatment of pilonidal sinus disease using fibrin glue as a sealant. Tech Coloproctol. 2004;8:95–98. doi: 10.1007/s10151-004-0063-7. [DOI] [PubMed] [Google Scholar]
- 255.Kim JK, Jeong JC, Lee JB, Jung KH, Bae BK. S-plasty for pilonidal disease: modified primary closure reducing tension. J Korean Surg Soc. 2012;82:63–69. doi: 10.4174/jkss.2012.82.2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Brusciano L, et al. D-shape asymmetric excision of sacrococcygeal pilonidal sinus with primary closure, suction drain, and subcuticular skin closure: an analysis of risks factors for long-term recurrence. Surg Innov. 2015;22:143–148. doi: 10.1177/1553350614535856. [DOI] [PubMed] [Google Scholar]
- 257.Zimmerman CE. Outpatient excision and primary closure of pilonidal cysts and sinuses. Am J Surg. 1978;136:640–642. doi: 10.1016/0002-9610(78)90326-4. [DOI] [PubMed] [Google Scholar]
- 258.Ibrahim AMRR. Oblique excision and primary closure of pilonidal sinus (sacrococcygeal) Trends Med. Res. 2012;7:62–69. doi: 10.3923/tmr.2012.62.69. [DOI] [Google Scholar]
- 259.Bulus H, Coskun A. Is Asymmetric excision primary closure at treatment of pylonidal sinus disease an appropriate choice? J. Clin. Anal. Med. 2011;2:79–81. doi: 10.4328/jcam.279. [DOI] [Google Scholar]
- 260.Docimo L, et al. Primary closure of decentred wounds in surgical treatment of pilonidal sinus [La lateralizzazione della cicatrice nel trattamento chirurgico del sinus pilonidalis] Chirurgia. 1998;11:239–244. [Google Scholar]
- 261.Karip AB, et al. Effect of Triclosan-Coated Suture and Antibiotic Prophylaxis on Infection and Recurrence after Karydakis Flap Repair for Pilonidal Disease: A Randomized Parallel-Arm Double-Blinded Clinical Trial. Surg Infect (Larchmt) 2016;17:583–588. doi: 10.1089/sur.2015.207. [DOI] [PubMed] [Google Scholar]
- 262.Yildiz MK, et al. Karydakis flap procedure in patients with sacrococcygeal pilonidal sinus disease: experience of a single centre in Istanbul. Scientific World Journal. 2013;2013:807027. doi: 10.1155/2013/807027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Sewefy AM, Hassanen A, Atyia AM, Saleh SK. Karydakis Flap With Compressing Tie-over Interrupted Sutures Without Drain versus Standard Karydakis for Treatment of Sacrococcygeal Pilonidal Sinus Disease. Dis Colon Rectum. 2017;60:514–520. doi: 10.1097/DCR.0000000000000784. [DOI] [PubMed] [Google Scholar]
- 264.Akinci, O. F., Coskun, A. & Uzunkoy, A. Simple and effective surgical treatment of pilonidal sinus: asymmetric excision and primary closure using suction drain and subcuticular skin closure. Dis Colon Rectum43, 701–706; discussion 706–707 (2000). [DOI] [PubMed]
- 265.Anyanwu AC, Hossain S, Williams A, Montgomery AC. Karydakis operation for sacrococcygeal pilonidal sinus disease: experience in a district general hospital. Ann R Coll Surg Engl. 1998;80:197–199. [PMC free article] [PubMed] [Google Scholar]
- 266.Abdul-Ghani AK, Abdul-Ghani AN, Ingham Clark CL. Day-care surgery for pilonidal sinus. Ann R Coll Surg Engl. 2006;88:656–658. doi: 10.1308/003588406X149255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Guner A, et al. Limberg flap versus Bascom cleft lift techniques for sacrococcygeal pilonidal sinus: prospective, randomized trial. World J Surg. 2013;37:2074–2080. doi: 10.1007/s00268-013-2111-9. [DOI] [PubMed] [Google Scholar]
- 268.Arslan K, et al. Which flap method should be preferred for the treatment of pilonidal sinus? A prospective randomized study. Tech Coloproctol. 2014;18:29–37. doi: 10.1007/s10151-013-0982-2. [DOI] [PubMed] [Google Scholar]
- 269.Moran DC, Kavanagh DO, Adhmed I, Regan MC. Excision and primary closure using the Karydakis flap for the treatment of pilonidal disease: outcomes from a single institution. World J Surg. 2011;35:1803–1808. doi: 10.1007/s00268-011-1138-z. [DOI] [PubMed] [Google Scholar]
- 270.Ates M, Dirican A, Sarac M, Aslan A, Colak C. Short and long-term results of the Karydakis flap versus the Limberg flap for treating pilonidal sinus disease: a prospective randomized study. Am J Surg. 2011;202:568–573. doi: 10.1016/j.amjsurg.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 271.Bessa SS. Results of the lateral advancing flap operation (modified Karydakis procedure) for the management of pilonidal sinus disease. Dis Colon Rectum. 2007;50:1935–1940. doi: 10.1007/s10350-007-9049-7. [DOI] [PubMed] [Google Scholar]
- 272.Bessa SS. Comparison of short-term results between the modified Karydakis flap and the modified Limberg flap in the management of pilonidal sinus disease: a randomized controlled study. Dis Colon Rectum. 2013;56:491–498. doi: 10.1097/DCR.0b013e31828006f7. [DOI] [PubMed] [Google Scholar]
- 273.Can MF, Sevinc MM, Hancerliogullari O, Yilmaz M, Yagci G. Multicenter prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg. 2010;200:318–327. doi: 10.1016/j.amjsurg.2009.08.042. [DOI] [PubMed] [Google Scholar]
- 274.Karaca T, et al. Comparison of short-term results of modified Karydakis flap and modified Limberg flap for pilonidal sinus surgery. Int J Surg. 2012;10:601–606. doi: 10.1016/j.ijsu.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 275.Rushfeldt C, Bernstein A, Norderval S, Revhaug A. Introducing an asymmetric cleft lift technique as a uniform procedure for pilonidal sinus surgery. Scand J Surg. 2008;97:77–81. doi: 10.1177/145749690809700111. [DOI] [PubMed] [Google Scholar]
- 276.Gurer A, et al. Is routine cavity drainage necessary in Karydakis flap operation? A prospective, randomized trial. Dis Colon Rectum. 2005;48:1797–1799. doi: 10.1007/s10350-005-0108-7. [DOI] [PubMed] [Google Scholar]
- 277.Keshava A, Young CJ, Rickard MJ, Sinclair G. Karydakis flap repair for sacrococcygeal pilonidal sinus disease: how important is technique? ANZ J Surg. 2007;77:181–183. doi: 10.1111/j.1445-2197.2006.04003.x. [DOI] [PubMed] [Google Scholar]
- 278.Nordon IM, Senapati A, Cripps NP. A prospective randomized controlled trial of simple Bascom’s technique versus Bascom’s cleft closure for the treatment of chronic pilonidal disease. Am J Surg. 2009;197:189–192. doi: 10.1016/j.amjsurg.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 279.Sozen S, Emir S, Guzel K, Ozdemir CS. Are postoperative drains necessary with the Karydakis flap for treatment of pilonidal sinus? (Can fibrin glue be replaced to drains?) A prospective randomized trial. Ir J Med Sci. 2011;180:479–482. doi: 10.1007/s11845-010-0549-4. [DOI] [PubMed] [Google Scholar]
- 280.Al-Khayat H, et al. Risk factors for wound complication in pilonidal sinus procedures. J Am Coll Surg. 2007;205:439–444. doi: 10.1016/j.jamcollsurg.2007.04.034. [DOI] [PubMed] [Google Scholar]
- 281.Anderson JH, Yip CO, Nagabhushan JS, Connelly SJ. Day-case Karydakis flap for pilonidal sinus. Dis Colon Rectum. 2008;51:134–138. doi: 10.1007/s10350-007-9150-y. [DOI] [PubMed] [Google Scholar]
- 282.Kulacoglu H, Dener C, Tumer H, Aktimur R. Total subcutaneous fistulectomy combined with Karydakis flap for sacrococcygeal pilonidal disease with secondary perianal opening. Colorectal Dis. 2006;8:120–123. doi: 10.1111/j.1463-1318.2005.00872.x. [DOI] [PubMed] [Google Scholar]
- 283.Senapati, A., Cripps, N. P., Flashman, K. & Thompson, M. R. Cleft Closure for the Treatment of Pilonidal Sinus Disease. Colorectal Dis (2009). [DOI] [PubMed]
- 284.Tezel E, Bostanci H, Anadol AZ, Kurukahvecioglu O. Cleft lift procedure for sacrococcygeal pilonidal disease. Dis Colon Rectum. 2009;52:135–139. doi: 10.1007/DCR.0b013e31819734f8. [DOI] [PubMed] [Google Scholar]
- 285.Theodoropoulos GE, Vlahos K, Lazaris AC, Tahteris E, Panoussopoulos D. Modified Bascom’s asymmetric midgluteal cleft closure technique for recurrent pilonidal disease: early experience in a military hospital. Dis Colon Rectum. 2003;46:1286–1291. doi: 10.1097/01.DCR.0000084409.63183.5B. [DOI] [PubMed] [Google Scholar]
- 286.Bertelsen CA. Cleft-lift operation for pilonidal sinuses under tumescent local anesthesia: a prospective cohort study of peri- and postoperative pain. Dis Colon Rectum. 2011;54:895–900. doi: 10.1007/DCR.0b013e31820ee852. [DOI] [PubMed] [Google Scholar]
- 287.Buczacki S, Drage M, Wells A, Guy R. Sacrococcygeal pilonidal sinus disease. Colorectal Dis. 2009;11:657. doi: 10.1111/j.1463-1318.2009.01818.x. [DOI] [PubMed] [Google Scholar]
- 288.Cripps N, Evans J, Nordon I, Senapati A. Sacrococcygeal pilonidal sinus disease. Colorectal Dis. 2008;11:105–106. doi: 10.1111/j.1463-1318.2008.01741.x. [DOI] [PubMed] [Google Scholar]
- 289.Demircan F, et al. The effect of laser epilation on recurrence and satisfaction in patients with sacrococcygeal pilonidal disease: a prospective randomized controlled trial. Int J Clin Exp Med. 2015;8:2929–2933. [PMC free article] [PubMed] [Google Scholar]
- 290.Kanat BH, et al. Comparison of early surgery (unroofing-curettage) and elective surgery (Karydakis flap technique) in pilonidal sinus abscess cases. Ulus Travma Acil Cerrahi Derg. 2014;20:366–370. doi: 10.5505/tjtes.2014.62547. [DOI] [PubMed] [Google Scholar]
- 291.Bali I, et al. Effectiveness of Limberg and Karydakis flap in recurrent pilonidal sinus disease. Clinics (Sao Paulo) 2015;70:350–355. doi: 10.6061/clinics/2015(05)08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Ersoy E, et al. Comparison of the short-term results after Limberg and Karydakis procedures for pilonidal disease: randomized prospective analysis of 100 patients. Colorectal Dis. 2009;11:705–710. doi: 10.1111/j.1463-1318.2008.01646.x. [DOI] [PubMed] [Google Scholar]
- 293.Khan MI, Jawed M, Bhura S, Shaikh U, Arif A. To evaluate the outcome of sacrococcygeal pilonidal sinus excision using karydakis technique. Med. Forum Monthly. 2014;25:57–59. [Google Scholar]
- 294.Ortega PM, et al. Is the cleft lift procedure for non-acute sacrococcygeal pilonidal disease a definitive treatment? Long-term outcomes in 74 patients. Surg Today. 2014;44:2318–2323. doi: 10.1007/s00595-014-0923-3. [DOI] [PubMed] [Google Scholar]
- 295.Sit M, Aktas G, Yilmaz EE. Comparison of the three surgical flap techniques in pilonidal sinus surgery. Am Surg. 2013;79:1263–1268. [PubMed] [Google Scholar]
- 296.Guner A, Ozkan OF, Kece C, Kesici S, Kucuktulu U. Modification of the Bascom cleft lift procedure for chronic pilonidal sinus: results in 141 patients. Colorectal Dis. 2013;15:e402–406. doi: 10.1111/codi.12243. [DOI] [PubMed] [Google Scholar]
- 297.Iribarren BO, Barra MM, Lanzelotti GD, Rojas GM, Peña AE. Comparison between Limberg and Karydakis flap for wound closure after pilonidal cyst resection. Rev. Chil. Cir. 2015;67:399–406. doi: 10.4067/S0718-40262015000400009. [DOI] [Google Scholar]
- 298.Iesalnieks I, Deimel S, Zulke C, Schlitt HJ. Smoking increases the risk of pre- and postoperative complications in patients with pilonidal disease. J Dtsch Dermatol Ges. 2013;11:1001–1005. doi: 10.1111/ddg.12140. [DOI] [PubMed] [Google Scholar]
- 299.Patel LB, Allen M. Prolonged delay in healing after surgical treatment of pilonidal sinus is avoidable. Colorectal Dis. 1999;1:107–110. doi: 10.1046/j.1463-1318.1999.00030.x. [DOI] [PubMed] [Google Scholar]
- 300.Sahin A, Olcucuoglu E, Seker D, Kulacoglu H. The effect of using methylene blue in surgical treatments of pilonidal disease: a prospective randomized study. European Surgery. 2014;46:148–154. doi: 10.1007/s10353-014-0276-6. [DOI] [Google Scholar]
- 301.Kumar NA, Sutradhar P. Karydakis procedure for sacrococcygeal pilonidal sinus disease: Our experience. Indian J Plast Surg. 2014;47:402–406. doi: 10.4103/0970-0358.146615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Mohamed SJ, Kristensen BB, Lindgaard L, Bisgaard T. Acceptable effect of multimodal analgesic treatment after a Bascom cleft lift operation. Dan Med J. 2015;62:A4985. [PubMed] [Google Scholar]
- 303.Melkonian TE, et al. Short-and long-term results with Karydaki’s technique for sacrococcygeal pilonidal disease [Resultados a corto y largo plazo con la técnica de Karydakis para la enfermedad pilonidal sacrocoxígea] Rev. Chil. Cir. 2013;65:25–29. doi: 10.4067/S0718-40262013000100005. [DOI] [Google Scholar]
- 304.Abdelrazeq AS, Rahman M, Botterill ID, Alexander DJ. Short-term and long-term outcomes of the cleft lift procedure in the management of nonacute pilonidal disorders. Dis Colon Rectum. 2008;51:1100–1106. doi: 10.1007/s10350-008-9262-z. [DOI] [PubMed] [Google Scholar]
- 305.Bostanoglu S, Sakcak I, Avsar FM, Cosgun E, Hamamci EO. Comparison of Karydakis technique with Limberg Flap Procedure in Pilonidal Sinus Disease: Advantages of Karydakis technique. Pak. J. Med. Sci. 2010;26:773–777. [Google Scholar]
- 306.Piskin T, et al. Orifice location guided excision and flap procedures for treatment of sacrococcygeal pilonidal disease. Adv. Clin. Exp. Med. 2011;20:481–488. [Google Scholar]
- 307.Sözen S, et al. Comparison between Karydakis flap repair and Limberg flap for surgical treatment of sacrococcygeal pilonidal sinus (short term results) Turk. J. Surg. 2010;26:153–156. doi: 10.5097/1300-0705.UCD.609-10.01. [DOI] [Google Scholar]
- 308.Tokac M, Dumlu EG, Aydin MS, Yalcin A, Kilic M. Comparison of modified limberg flap and karydakis flap operations in pilonidal sinus surgery: prospective randomized study. Int Surg. 2015;100:870–877. doi: 10.9738/INTSURG-D-14-00213.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Guner A, Cekic AB, Boz A, Turkyilmaz S, Kucuktulu U. A proposed staging system for chronic symptomatic pilonidal sinus disease and results in patients treated with stage-based approach. BMC Surg. 2016;16:18. doi: 10.1186/s12893-016-0134-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Bannura C, Barrera E, Contreras P, Melo L, Soto C. Ambulatory karydakis procedure for sacrococcygeal pilonidal disease. Rev. Chil. Cir. 2009;61:256–260. [Google Scholar]
- 311.Larsson JC, Aliaga FD, Granero L, Cornet M. Tratamiento de la Enfermedad Pilonidal Crónica. Comparación de 3 Técnicas Quirúrgicas. Rev Argent Coloproct. 2014;25:64–70. [Google Scholar]
- 312.Guillermo Bannura C. Sacrococcygeal pilonidal disease. risks factors and surgical options [Enfermedad pilonidal sacro-coccígea: Factores de riesgo y tratamiento quirúrgico] Rev. Chil. Cir. 2011;63:527–533. doi: 10.4067/S0718-40262011000500016. [DOI] [Google Scholar]
- 313.Ochoa EM, Esquivel CM, Badra R, Cornet M. Sacrococcygeal pilonidal disease: results of karydakis flap vs. limberg flap. Prensa Med. Argent. 2009;96:31–37. [Google Scholar]
- 314.Ramzan M, Khalid Mirza M, Arif Ali M. Pilonidal Sinus; Experience with Modified Karydakis Procedure Using Subcuticular Skin Closure. The Professional Medical Journal. 2016;23:1499–1504. doi: 10.17957/tpmj/16.3602. [DOI] [Google Scholar]
- 315.Keshvari A, Keramati MR, Fazeli MS, Kazemeini A, Nouritaromlou MK. Risk factors for complications and recurrence after the Karydakis flap. J Surg Res. 2016;204:55–60. doi: 10.1016/j.jss.2016.04.035. [DOI] [PubMed] [Google Scholar]
- 316.Bannura G. Karydakis operation for sacrococcygeal pilonidal sinus disease. Rev Chil Cir. 2005;57:340–344. [Google Scholar]
- 317.Cubukcu A, et al. The role of obesity on the recurrence of pilonidal sinus disease in patients, who were treated by excision and Limberg flap transposition. Int J Colorectal Dis. 2000;15:173–175. doi: 10.1007/s003840000212. [DOI] [PubMed] [Google Scholar]
- 318.Arumugam PJ, Chandrasekaran TV, Morgan AR, Beynon J, Carr ND. The rhomboid flap for pilonidal disease. Colorectal Dis. 2003;5:218–221. doi: 10.1046/j.1463-1318.2003.00435.x. [DOI] [PubMed] [Google Scholar]
- 319.Mentes BB, et al. Modified Limberg transposition flap for sacrococcygeal pilonidal sinus. Surg Today. 2004;34:419–423. doi: 10.1007/s00595-003-2725-x. [DOI] [PubMed] [Google Scholar]
- 320.Hegele A, Strombach FJ, Schonbach F. [Reconstructive surgical therapy of infected pilonidal sinus] Chirurg. 2003;74:749–752. doi: 10.1007/s00104-003-0657-z. [DOI] [PubMed] [Google Scholar]
- 321.Kaya B, et al. Modified Limberg transposition flap in the treatment of pilonidal sinus disease. Tech Coloproctol. 2012;16:55–59. doi: 10.1007/s10151-011-0799-9. [DOI] [PubMed] [Google Scholar]
- 322.Yildar M, Cavdar F. Comparison of the Limberg flap and bilateral gluteus maximus advancing flap following oblique excision for the treatment of pilonidal sinus disease. Surg Today. 2014;44:1828–1833. doi: 10.1007/s00595-013-0764-5. [DOI] [PubMed] [Google Scholar]
- 323.Kapan M, Kapan S, Pekmezci S, Durgun V. Sacrococcygeal pilonidal sinus disease with Limberg flap repair. Tech Coloproctol. 2002;6:27–32. doi: 10.1007/s101510200005. [DOI] [PubMed] [Google Scholar]
- 324.Müller K, et al. Prospective analysis of cosmesis, morbidity, and patient satisfaction following Limberg flap for the treatment of sacrococcygeal pilonidal sinus. Dis Colon Rectum. 2011;54:487–494. doi: 10.1007/DCR.0b013e3182051d96. [DOI] [PubMed] [Google Scholar]
- 325.Jimenez Romero C, Alcalde M, Martin F, Pulido A, Rico P. Treatment of pilonidal sinus by excision and rhomboid flap. Int J Colorectal Dis. 1990;5:200–202. doi: 10.1007/BF00303275. [DOI] [PubMed] [Google Scholar]
- 326.El-Khadrawy O, Hashish M, Ismail K, Shalaby H. Outcome of the rhomboid flap for recurrent pilonidal disease. World J Surg. 2009;33:1064–1068. doi: 10.1007/s00268-009-9920-x. [DOI] [PubMed] [Google Scholar]
- 327.Akin M, et al. Comparison of the classic Limberg flap and modified Limberg flap in the treatment of pilonidal sinus disease: a retrospective analysis of 416 patients. Surg Today. 2010;40:757–762. doi: 10.1007/s00595-008-4098-7. [DOI] [PubMed] [Google Scholar]
- 328.Milito G, et al. Modified Limberg’s transposition flap for pilonidal sinus. Long term follow up of 216 cases. Ann Ital Chir. 2007;78:227–231. [PubMed] [Google Scholar]
- 329.Daphan C, Tekelioglu MH, Sayilgan C. Limberg flap repair for pilonidal sinus disease. Dis Colon Rectum. 2004;47:233–237. doi: 10.1007/s10350-003-0037-2. [DOI] [PubMed] [Google Scholar]
- 330.Eryilmaz R, Sahin M, Alimoglu O, Dasiran F. Surgical treatment of sacrococcygeal pilonidal sinus with the Limberg transposition flap. Surgery. 2003;134:745–749. doi: 10.1016/s0039-6060(03)00163-6. [DOI] [PubMed] [Google Scholar]
- 331.Gwynn BR. Use of the rhomboid flap in pilonidal sinus. Ann R Coll Surg Engl. 1986;68:40–41. [PMC free article] [PubMed] [Google Scholar]
- 332.Karakayali F, et al. Unroofing and marsupialization vs. rhomboid excision and Limberg flap in pilonidal disease: a prospective, randomized, clinical trial. Dis Colon Rectum. 2009;52:496–502. doi: 10.1007/DCR.0b013e31819a3ec0. [DOI] [PubMed] [Google Scholar]
- 333.Lahooti M, Taheri PA, Nezami BG, Assa S. Sacrococcygeal pilonidal sinus treated by a new fascio-cutaneous flap. Dis Colon Rectum. 2008;51:588–592. doi: 10.1007/s10350-008-9211-x. [DOI] [PubMed] [Google Scholar]
- 334.Lieto E, et al. Dufourmentel rhomboid flap in the radical treatment of primary and recurrent sacrococcygeal pilonidal disease. Dis Colon Rectum. 2010;53:1061–1068. doi: 10.1007/DCR.0b013e3181defd25. [DOI] [PubMed] [Google Scholar]
- 335.Aithal SK, Rajan CS, Reddy N. Limberg flap for sacrococcygeal pilonidal sinus a safe and sound procedure. Indian J Surg. 2013;75:298–301. doi: 10.1007/s12262-012-0489-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Milito G, Cortese F, Casciani CU. Rhomboid flap procedure for pilonidal sinus: results from 67 cases. Int J Colorectal Dis. 1998;13:113–115. doi: 10.1007/s003840050146. [DOI] [PubMed] [Google Scholar]
- 337.Aslam MN, Shoaib S, Choudhry AM. Use of Limberg flap for pilonidal sinus - a viable option. J Ayub Med Coll Abbottabad. 2009;21:31–33. [PubMed] [Google Scholar]
- 338.Topgul K, Ozdemir E, Kilic K, Gokbayir H, Ferahkose Z. Long-term results of limberg flap procedure for treatment of pilonidal sinus: a report of 200 cases. Dis Colon Rectum. 2003;46:1545–1548. doi: 10.1097/01.DCR.0000089114.56612.06. [DOI] [PubMed] [Google Scholar]
- 339.Urhan MK, Kucukel F, Topgul K, Ozer I, Sari S. Rhomboid excision and Limberg flap for managing pilonidal sinus: results of 102 cases. Dis Colon Rectum. 2002;45:656–659. doi: 10.1007/s10350-004-6263-4. [DOI] [PubMed] [Google Scholar]
- 340.Kirkil C, et al. The effects of drainage on the rates of early wound complications and recurrences after Limberg flap reconstruction in patients with pilonidal disease. Tech Coloproctol. 2011;15:425–429. doi: 10.1007/s10151-011-0782-5. [DOI] [PubMed] [Google Scholar]
- 341.Darwish AM, Hassanin A. Reconstruction following excision of sacrococcygeal pilonidal sinus with a perforator-based fasciocutaneous Limberg flap. J Plast Reconstr Aesthet Surg. 2010;63:1176–1180. doi: 10.1016/j.bjps.2009.05.051. [DOI] [PubMed] [Google Scholar]
- 342.Altintoprak F, et al. Retrospective review of pilonidal sinus patients with early discharge after Limberg flap procedure. Int Surg. 2014;99:28–34. doi: 10.9738/INTSURG-D-13-00150.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Omer Y, Hayrettin D, Murat C, Mustafa Y, Evren D. Comparison of modified limberg flap and modified elliptical rotation flap for pilonidal sinus surgery: a retrospective cohort study. Int J Surg. 2015;16:74–77. doi: 10.1016/j.ijsu.2015.02.024. [DOI] [PubMed] [Google Scholar]
- 344.Yoldas T, et al. Recurrent pilonidal sinus: lay open or flap closure, does it differ? Int Surg. 2013;98:319–323. doi: 10.9738/INTSURG-D-13-00081.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Katsoulis IE, Hibberts F, Carapeti EA. Outcome of treatment of primary and recurrent pilonidal sinuses with the Limberg flap. Surgeon. 2006;4(7–10):62. doi: 10.1016/s1479-666x(06)80014-4. [DOI] [PubMed] [Google Scholar]
- 346.Erdem E, Sungurtekin U, Nessar M. Are postoperative drains necessary with the Limberg flap for treatment of pilonidal sinus? Dis Colon Rectum. 1998;41:1427–1431. doi: 10.1007/BF02237061. [DOI] [PubMed] [Google Scholar]
- 347.Tekin A. Pilonidal sinus: experience with the Limberg flap. Colorectal Dis. 1999;1:29–33. doi: 10.1046/j.1463-1318.1999.00007.x. [DOI] [PubMed] [Google Scholar]
- 348.Akin M, et al. Rhomboid excision and Limberg flap for managing pilonidal sinus: long-term results in 411 patients. Colorectal Dis. 2008;10:945–948. doi: 10.1111/j.1463-1318.2008.01563.x. [DOI] [PubMed] [Google Scholar]
- 349.Sabuncuoglu MZ, et al. Eyedrop-shaped, modified Limberg transposition flap in the treatment of pilonidal sinus disease. Asian J Surg. 2015;38:161–167. doi: 10.1016/j.asjsur.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 350.Afsarlar CE, et al. Treatment of adolescent pilonidal disease with a new modification to the Limberg flap: symmetrically rotated rhomboid excision and lateralization of the Limberg flap technique. J Pediatr Surg. 2013;48:1744–1749. doi: 10.1016/j.jpedsurg.2013.01.029. [DOI] [PubMed] [Google Scholar]
- 351.Yamout SZ, et al. Early experience with the use of rhomboid excision and Limberg flap in 16 adolescents with pilonidal disease. J Pediatr Surg. 2009;44:1586–1590. doi: 10.1016/j.jpedsurg.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 352.Altinli E, Koksal N, Onur E, Celik A, Sumer A. Impact of fibrin sealant on Limberg flap technique: results of a randomized controlled trial. Tech Coloproctol. 2007;11:22–25. doi: 10.1007/s10151-007-0320-7. [DOI] [PubMed] [Google Scholar]
- 353.Bozkurt MK, Tezel E. Management of pilonidal sinus with the Limberg flap. Dis Colon Rectum. 1998;41:775–777. doi: 10.1007/BF02236268. [DOI] [PubMed] [Google Scholar]
- 354.Colak T, Turkmenoglu O, Dag A, Akca T, Aydin S. A randomized clinical study evaluating the need for drainage after Limberg flap for pilonidal sinus. J Surg Res. 2010;158:127–131. doi: 10.1016/j.jss.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 355.Cihan A, et al. Superiority of asymmetric modified Limberg flap for surgical treatment of pilonidal disease. Dis Colon Rectum. 2006;49:244–249. doi: 10.1007/s10350-005-0253-z. [DOI] [PubMed] [Google Scholar]
- 356.Manterola C, Barroso M, Araya JC, Fonseca L. Pilonidal disease: 25 cases treated by the Dufourmentel technique. Dis Colon Rectum. 1991;34:649–652. doi: 10.1007/BF02050344. [DOI] [PubMed] [Google Scholar]
- 357.Ardelt M, et al. Sequential intervention with primary excision and Limberg plastic surgery procedure for treatment of sacrococcygeal pilonidal sinus: Results of a pilot study. Chirurg. 2015;86:771–775. doi: 10.1007/s00104-014-2963-z. [DOI] [PubMed] [Google Scholar]
- 358.Faux W, Pillai SC, Gold DM. Limberg flap for pilonidal disease: the “no-protractor” approach, 3 steps to success. Tech Coloproctol. 2005;9:153–155. doi: 10.1007/s10151-005-0216-3. [DOI] [PubMed] [Google Scholar]
- 359.Karakas, B. R. et al. Is the lateralization distance important in terms in patients undergoing the modified Limberg flap procedure for treatment of pilonidal sinus? Tech Coloproctol (2014). [DOI] [PubMed]
- 360.El-Tawil S, Carapeti E. Use of a double rhomboid transposition flap in the treatment of extensive complex pilonidal sinus disease. Colorectal Dis. 2009;11:313–317. doi: 10.1111/j.1463-1318.2008.01596.x. [DOI] [PubMed] [Google Scholar]
- 361.Sharma PP. Multiple Z-plasty in pilonidal sinus–a new technique under local anesthesia. World J Surg. 2006;30:2261–2265. doi: 10.1007/s00268-005-0632-6. [DOI] [PubMed] [Google Scholar]
- 362.Unalp HR, Derici H, Kamer E, Nazli O, Onal MA. Lower recurrence rate for Limberg vs. V-Y flap for pilonidal sinus. Dis Colon Rectum. 2007;50:1436–1444. doi: 10.1007/s10350-007-0276-8. [DOI] [PubMed] [Google Scholar]
- 363.Akan K, et al. Comparison of surgical Limberg flap technique and crystallized phenol application in the treatment of pilonidal sinus disease: a retrospective study. Ulus Cerrahi Derg. 2013;29:162–166. doi: 10.5152/UCD.2013.2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Yabanoglu H, Karagulle E, Belli S, Turk E. Results of modified Dufourmentel rhomboid flap in patients with extensive Sacrococcygeal pilonidal disease. Acta Chir Belg. 2014;114:52–57. doi: 10.1080/00015458.2014.11680977. [DOI] [PubMed] [Google Scholar]
- 365.Azizi R, Alemrajabi M, Naderan M, Shoar S. Efficacy of modified Limberg flap in surgical treatment of infected pilonidal abscess: a case–control study. European. Surgery. 2014;46:144–147. doi: 10.1007/s10353-014-0273-9. [DOI] [Google Scholar]
- 366.Jonas J, Blaich S, Bahr R. Surgery of pilonidal sinus using the Limberg flap. Zentralbl Chir. 2000;125:976–981. doi: 10.1055/s-2000-10076. [DOI] [PubMed] [Google Scholar]
- 367.Kicka M, Toporcer T, Radonak J. Pilonidal sinus–a classical plastic procedure according to Limberg (Limberg flap procedure) or its modified version? Rozhl Chir. 2011;90:482–487. [PubMed] [Google Scholar]
- 368.Karakas BR. Comparison of Z-plasty, limberg flap, and asymmetric modified Limberg flap techniques for the pilonidal sinus treatment: review of literature. Acta Chir Iugosl. 2013;60:31–37. doi: 10.2298/ACI1303031K. [DOI] [PubMed] [Google Scholar]
- 369.Saydam M, et al. Comparison of modified Limberg flap transposition and lateral advancement flap transposition with Burow’s triangle in the treatment of pilonidal sinus disease. Am J Surg. 2015;210:772–777. doi: 10.1016/j.amjsurg.2015.03.031. [DOI] [PubMed] [Google Scholar]
- 370.Misiakos EP, et al. Limberg flap reconstruction for the treatment of pilonidal sinus disease. Chirurgia (Bucur) 2006;101:513–517. [PubMed] [Google Scholar]
- 371.Karaca AS, Ali R, Capar M, Karaca S. Comparison of Limberg flap and excision and primary closure of pilonidal sinus disease, in terms of quality of life and complications. J Korean Surg Soc. 2013;85:236–239. doi: 10.4174/jkss.2013.85.5.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Yildar M, Cavdar F, Yildiz MK. The evaluation of a modified Dufourmentel flap after S-type excision for pilonidal sinus disease. ScientificWorldJournal. 2013;2013:459147. doi: 10.1155/2013/459147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Sungurtekin H, Sungurtekin U, Erdem E. Local anesthesia and midazolam versus spinal anesthesia in ambulatory pilonidal surgery. J Clin Anesth. 2003;15:201–205. doi: 10.1016/S0952-8180(03)00032-1. [DOI] [PubMed] [Google Scholar]
- 374.Roth RF, Moorman WL. Treatment of pilonidal sinus and cyst by conservative excision and W-plasty closure. Plast Reconstr Surg. 1977;60:412–415. [PubMed] [Google Scholar]
- 375.Altintoprak F, et al. Comparision of the Limberg flap with the V-Y flap technique in the treatment of pilonidal disease. J Korean Surg Soc. 2013;85:63–67. doi: 10.4174/jkss.2013.85.2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Dogra S, Rao PP. Z-Plasty a Rational and Effective Technique for Pilonidal Sinus. Hellenic Journal of Surgery. 2014;86:208–211. doi: 10.1007/s13126-014-0131-z. [DOI] [Google Scholar]
- 377.Rabbani, S. et al. Rhomboid excision with limberg transposition flap in the management of sacrococcygeal pilonidal sinus - a reliable surgical technique. Pakistan J of Medical and Health Sci8 (2014).
- 378.Madbouly KM. Day-case Limberg flap for recurrent pilonidal sinus: does obesity complicate the issue? Am Surg. 2010;76:995–999. [PubMed] [Google Scholar]
- 379.Öz, B. et al. A comparison of surgical outcome of fasciocutaneous V-Y advancement flap and Limberg transposition flap for recurrent sacrococcygeal pilonidal sinus disease. Asian J Surg6, 10.1016/j.asjsur.2015.10.002 (2015). [DOI] [PubMed]
- 380.Rao J, Deora H, Mandia R. A Retrospective Study of 40 Cases of Pilonidal Sinus with Excision of Tract and Z-plasty as Treatment of Choice for Both Primary and Recurrent Cases. Indian J Surg. 2013;77:691–693. doi: 10.1007/s12262-013-0983-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Moosavi SR, Kharazm P, Vaghardoost R. Surgical treatment of pilonidal sinus with a fasciocutaneous rotation flap based on an inferior pedicle. Scand J Plast Reconstr Surg Hand Surg. 2006;40:281–283. doi: 10.1080/02844310600869811. [DOI] [PubMed] [Google Scholar]
- 382.Das K, et al. Diathermy versus scalpel in Limberg flap in pilonidal sinus surgery. A prospective randomized trial. Ann Ital Chir. 2014;85:148–152. [PubMed] [Google Scholar]
- 383.Fahim M, et al. Limberg FLAP Reconstruction for Pilonidal Sinus Disease: An Experience. Ann Pak Inst Med Sci. 2013;9:215–218. [Google Scholar]
- 384.Shabir F, Khan BA, Mian MA. Rhomboid excision with Limberg flap a novel treatment for sacrococcygeal pilonidal sinus. Pak. J. Med. Health Sci. 2014;8:687–690. [Google Scholar]
- 385.Bayhan Z, et al. Crystallized phenol application and modified Limberg flap procedure in treatment of pilonidal sinus disease: A comparative retrospective study. Asian J Surg. 2016;39:172–177. doi: 10.1016/j.asjsur.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 386.Al-Haifi MB, et al. Rhomboid flap - A primary cure for pilonidal sinus. Kuwait Med. J. 2010;42:282–285. [Google Scholar]
- 387.Tardu, A., Haşlak, A., Özçinar, B. & Başak, F. Comparison of Limberg and Dufourmentel flap in surgical treatment of pilonidal sinus disease. Turk. J. Surg. 27, 35–40, 10.5097/1300-0705.UCD.659-11.04
- 388.Sellés R, et al. Complete excision and marsupialization of chronic pilonidal sacrococcygeal sinus: The ideal technique? Cir. Esp. 2002;72:92–94. doi: 10.1016/S0009-739X(02)72016-2. [DOI] [Google Scholar]
- 389.Tschudi J, Ris HB. Morbidity of Z-plasty in the treatment of pilonidal sinus. Chirurg. 1988;59:486–490. [PubMed] [Google Scholar]
- 390.Abu Galala KH, Salam IMA, El Ashaal YI, Chandran VP, Sim AJW. Excision of pilonidal sinus and primary closure by a rhomboid flap transposition. Asian J. Surg. 1996;19:305–308. [Google Scholar]
- 391.Ferreira Montero V, Garcia Fabian AP, Martinez Laganga A, Perez Ruiz L. Rhombic plastia in the form of an ‘L’ for treating pilonidal cysts [La plastia en “L” de Rombo para el tratamiento de los Quistes Pilonidales] Cir. Esp. 1977;31:153–158. [Google Scholar]
- 392.Kushwaha R, El-Tawil S, Hibberts F, Katsoulis IE, Carapeti E. Treatment of complex primary and recurrent pilonidal sinus with a Rhomboid Transposition Flap. Br J Surg. 2006;93:1–104. [Google Scholar]
- 393.Behdad A, Hosseinpoor M. Z-plasty for the treatment of residual cavity after pilonidal sinus excision. Medical Journal of the Islamic Republic of Iran. 2001;14:317–319. [Google Scholar]
- 394.Lauterbach HH, Konrad U. Zweiphasenkonzept zur Therapie des infizierten Sinus pilonidalis. Chir Praxis. 1999;55:623–628. [Google Scholar]
- 395.Mutaf M, Temel M, Koc MN. A New Surgical Technique for Closure of Pilonidal Sinus Defects: Triangular Closure Technique. Med Sci Monit. 2017;23:1033–1042. doi: 10.12659/MSM.899879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Raza MW, et al. Limberg flap for pilonidal sinus. J Rawal Med coll. 2012;16:132–134. [Google Scholar]
- 397.Khanna AK, Tiwary SK. Pilonidal sinus disease with especial reference to Limberg flap. Apollo Medicine. 2015;12:163–169. doi: 10.1016/j.apme.2015.07.013. [DOI] [Google Scholar]
- 398.Mentes O, Bagci M, Bilgin T, Ozgul O, Ozdemir M. Limberg flap procedure for pilonidal sinus disease: results of 353 patients. Langenbecks Arch Surg. 2008;393:185–189. doi: 10.1007/s00423-007-0227-9. [DOI] [PubMed] [Google Scholar]
- 399.Oncel M, et al. Excision and marsupialization versus sinus excision for the treatment of limited chronic pilonidal disease: a prospective, randomized trial. Tech Coloproctol. 2002;6:165–169. doi: 10.1007/s101510200037. [DOI] [PubMed] [Google Scholar]
- 400.Abramson DJ. An open, semiprimary closure operation for pilonidal sinuses, using local anesthesia. Dis Colon Rectum. 1970;13:215–219. doi: 10.1007/BF02617211. [DOI] [PubMed] [Google Scholar]
- 401.Abramson DJ, Cox PA. The marsupialization operation for pilonidal cysts and sinuses under local anesthesia with lidocaine; an ambulatory method of treatment. Ann Surg. 1954;139:341–349. doi: 10.1097/00000658-195403000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Aldemir M, Kara IH, Erten G, Tacyildiz I. Effectiveness of collagenase in the treatment of sacrococcygeal pilonidal sinus disease. Surg Today. 2003;33:106–109. doi: 10.1007/s005950300022. [DOI] [PubMed] [Google Scholar]
- 403.Ozbalci GS, Tuncal S, Bayraktar K, Tasova V, Ali Akkus M. Is gentamicin-impregnated collagen sponge to be recommended in pilonidal sinus patient treated with marsupialization? A prospective randomized study. Ann Ital Chir. 2014;85:576–582. [PubMed] [Google Scholar]
- 404.Zimmerman CE. Outpatient excision and primary closure of pilonidal cysts and sinuses. Long-term follow-up. Am J Surg. 1984;148:658–659. doi: 10.1016/0002-9610(84)90346-5. [DOI] [PubMed] [Google Scholar]
- 405.Brockbank MJ. Pilonidal Cyst. Am J Surg. 1945;68:4. doi: 10.1016/0002-9610(45)90422-3. [DOI] [Google Scholar]
- 406.Licheri S, et al. Radical treatment of acute pilonidal abscess by marsupialization. G Chir. 2004;25:414–416. [PubMed] [Google Scholar]
- 407.Gonzalo Inostroza L, et al. Pilonidal cyst abscess: Definitive treatment in a single time during the acute, short-term results [Quiste pilonidal abscedado: Tratamiento definitivo en un solo tiempo durante el episodio agudo, resultados a corto plazo] Rev. Chil. Cir. 2011;63:54–58. doi: 10.4067/S0718-40262011000100009. [DOI] [Google Scholar]
- 408.Perez Oberreuter, G. et al. Tecnica de marsupializacion en quiste pilonidal: 7 anos de experiencia. Rev. Chil. Cir. 50 (1998).
- 409.Duchateau J, De Mol J, Bostoen H, Allegaert W. Pilonidal sinus. Excision–marsupialization–phenolization? Acta Chir Belg. 1985;85:325–328. [PubMed] [Google Scholar]
- 410.Abramson DJ. Excision and delayed closure of pilonidal sinuses. Surg Gynecol Obstet. 1977;144:205–207. [PubMed] [Google Scholar]
- 411.Abramson DJ. Outpatient management of pilonidal sinuses: excision and semiprimary closure technic. Mil Med. 1978;143:753–757. doi: 10.1093/milmed/143.11.753. [DOI] [PubMed] [Google Scholar]
- 412.Struijk DG, Krediet RT, de Glas-Vos JW, Boeschoten EW, Arisz L. Experiences with acute peritoneal dialysis in adults. Ned Tijdschr Geneeskd. 1984;128:751–755. [PubMed] [Google Scholar]
- 413.Sahsamanis G, et al. Semi-closed surgical technique for treatment of pilonidal sinus disease. Ann Med Surg (Lond) 2017;15:47–51. doi: 10.1016/j.amsu.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Arauz S, Yamaguchi N, Schmidt Goffi F, Zanoto A. Tratamento cirúrgico da doença pilonidal sacrococcígea: estudo comparativo entre as técnicas de marsupialização e de incisão e curetagem [Surgical treatment of sacrococcigeal pilonidal disease: a comparative study between marsupialization and incision plus curettage techniques] Rev Col Bras Cir. 2002;29:659–662. doi: 10.1590/S0100-69912002000500008. [DOI] [Google Scholar]
- 415.Yildirim D, Sunamak O, Pergel A, Mounla M. Combined single step definitive treatment in acute pilonidal sinus abscess. Surg Sci. 2010;1:24–26. doi: 10.4236/ss.2010.11005. [DOI] [Google Scholar]
- 416.Cavanagh CR, Schnug GE. Definitive Treatment of the Pilonidal Abscess. Northwest Med. 1964;63:449–451. [PubMed] [Google Scholar]
- 417.Olmez A, Kayaalp C, Aydin C. Treatment of pilonidal disease by combination of pit excision and phenol application. Tech Coloproctol. 2013;17:201–206. doi: 10.1007/s10151-012-0903-9. [DOI] [PubMed] [Google Scholar]
- 418.Al-Naami MY. Outpatient pilonidal sinotomy complemented with good wound and surrounding skin care. Saudi Med J. 2005;26:285–288. [PubMed] [Google Scholar]
- 419.Gupta PJ. Radiofrequency incision and lay open technique of pilonidal sinus (clinical practice paper on modified technique) Kobe J Med Sci. 2003;49:75–82. [PubMed] [Google Scholar]
- 420.Kepenekci I, Demirkan A, Celasin H, Gecim IE. Unroofing and curettage for the treatment of acute and chronic pilonidal disease. World J Surg. 2010;34:153–157. doi: 10.1007/s00268-009-0245-6. [DOI] [PubMed] [Google Scholar]
- 421.Al Homoud SJ, Habib ZS, Abdul Jabbar AS, Isbister WH. Management of sacrococcygeal pilonidal disease. Saudi. Med. J. 2001;22:762–764. [PubMed] [Google Scholar]
- 422.Elsey E, Lund JN. Fibrin glue in the treatment for pilonidal sinus: high patient satisfaction and rapid return to normal activities. Tech Coloproctol. 2013;17:101–104. doi: 10.1007/s10151-012-0956-9. [DOI] [PubMed] [Google Scholar]
- 423.Gidwani AL, Murugan K, Nasir A, Brown R. Incise and lay open: an effective procedure for coccygeal pilonidal sinus disease. Ir J Med Sci. 2010;179:207–210. doi: 10.1007/s11845-009-0450-1. [DOI] [PubMed] [Google Scholar]
- 424.Oram Y, Kahraman F, Karincaoglu Y, Koyuncu E. Evaluation of 60 patients with pilonidal sinus treated with laser epilation after surgery. Dermatol Surg. 2010;36:88–91. doi: 10.1111/j.1524-4725.2009.01387.x. [DOI] [PubMed] [Google Scholar]
- 425.Klin B, Heller ON, Kaplan I. The use of the CO2 laser in pilonidal sinus disease: preliminary results of an ambulatory prospective study. J Clin Laser Med Surg. 1990;8:31–37. doi: 10.1089/clm.1990.8.19. [DOI] [PubMed] [Google Scholar]
- 426.Jensen SL, Harling H. Prognosis after simple incision and drainage for a first-episode acute pilonidal abscess. Br J Surg. 1988;75:60–61. doi: 10.1002/bjs.1800750122. [DOI] [PubMed] [Google Scholar]
- 427.Garg P, Garg M, Gupta V, Mehta SK, Lakhtaria P. Laying open (deroofing) and curettage under local anesthesia for pilonidal disease: An outpatient procedure. World J Gastrointest Surg. 2015;7:214–218. doi: 10.4240/wjgs.v7.i9.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Yalcin S, Ergul E. A single-surgeon, single-institute experience of 59 sinotomies for sacrococcygeal pilonidal disease under local anesthesia. Bratisl Lek Listy. 2010;111:284–285. [PubMed] [Google Scholar]
- 429.Sozen S, Ozturk V, Das V. Day–Care Surgery for Pilonidal Sinus Using Sinotomy Technique and Fibrin Glue Injection. Arch Clin Exp Surg. 2012;1:138–141. doi: 10.5455/aces.20120625121721. [DOI] [Google Scholar]
- 430.Qayyum I, Bai D, Tsoraides SS. Loop drainage after debridement (LDAD): minimally invasive treatment for pilonidal cyst. Tech Coloproctol. 2016;20:591–594. doi: 10.1007/s10151-016-1469-8. [DOI] [PubMed] [Google Scholar]
- 431.Isbister WH, Prasad J. Pilonidal disease. Aust N Z J Surg. 1995;65:561–563. doi: 10.1111/j.1445-2197.1995.tb01695.x. [DOI] [PubMed] [Google Scholar]
- 432.Mikkelsen K. Pilonidal sinus. A follow-up study of out-patients treated by simple incision. Ugeskr Laeger. 1975;137:789–791. [PubMed] [Google Scholar]
- 433.Shirah B, Shirah H. The Effect of Hydrogen Peroxide on the Healing of the Laid Open Wound in the Treatment of Chronic Sacrococcygeal Pilonidal Sinus: A Retrospective Database Analysis of 500 Patients. International Journal of Surgery and Medicine. 2016;2:17. doi: 10.5455/ijsm.woundhealing. [DOI] [Google Scholar]
- 434.Malik GA, Choudary TH, Wahab A. Pilonidal Sinus; Prevalence and comparison of excision and primary closure with lay open procedure. Professional Med J. 2009;16:297–298. [Google Scholar]
- 435.Goswitz JT. Sacrococcygeal Pilonidal Sinus Disease. Treatment and Long-Term Follow-up in a Military Hospital Serving Combat-Ready Units. Arch Surg. 1965;90:890–892. doi: 10.1001/archsurg.1965.01320120092007. [DOI] [PubMed] [Google Scholar]
- 436.Gillquist J. Prevention of the recurrence of so-called sacral dermoid. Nord Med. 1965;74:1315. [PubMed] [Google Scholar]
- 437.Senapati A, Cripps NP, Thompson MR. Bascom’s operation in the day-surgical management of symptomatic pilonidal sinus. Br J Surg. 2000;87:1067–1070. doi: 10.1046/j.1365-2168.2000.01472.x. [DOI] [PubMed] [Google Scholar]
- 438.Gips, M., Melki, Y., Salem, L., Weil, R. & Sulkes, J. Minimal surgery for pilonidal disease using trephines: description of a new technique and long-term outcomes in 1,358 patients. Dis Colon Rectum51, 1656–1662; discussion 1662–1653, 10.1007/s10350-008-9329-x (2008). [DOI] [PubMed]
- 439.Zorcolo L, Capra F, Scintu F, Casula G. Surgical treatment of pilonidal disease. Results with the Bascom’s technique. Minerva Chir. 2004;59:387–395. [PubMed] [Google Scholar]
- 440.Edwards MH. Pilonidal sinus: a 5-year appraisal of the Millar-Lord treatment. Br J Surg. 1977;64:867–868. doi: 10.1002/bjs.1800641209. [DOI] [PubMed] [Google Scholar]
- 441.Iesalnieks I, Deimel S, Kienle K, Schlitt HJ, Zulke C. Pit-picking surgery for pilonidal disease. Chirurg. 2011;82:927–931. doi: 10.1007/s00104-011-2077-9. [DOI] [PubMed] [Google Scholar]
- 442.Colov EP, Bertelsen CA. Short convalescence and minimal pain after out-patient Bascom’s pit-pick operation. Danish medical bulletin. 2011;58:A4348. [PubMed] [Google Scholar]
- 443.Mosquera DA, Quayle JB. Bascom’s operation for pilonidal sinus. J R Soc Med. 1995;88:45P–46P. [PMC free article] [PubMed] [Google Scholar]
- 444.Neola, B., Capasso, S., Caruso, L., Falato, A. & Ferulano, G. P. Scarless outpatient ablation of pilonidal sinus: a pilot study of a new minimally invasive treatment. Int Wound J, 10.1111/iwj.12350 (2014). [DOI] [PMC free article] [PubMed]
- 445.Majeski J, Stroud J. Sacrococcygeal pilonidal disease. Int Surg. 2011;96:144–147. doi: 10.9738/1393.1. [DOI] [PubMed] [Google Scholar]
- 446.Lund JN, Leveson SH. Fibrin glue in the treatment of pilonidal sinus: results of a pilot study. Dis Colon Rectum. 2005;48:1094–1096. doi: 10.1007/s10350-004-0905-4. [DOI] [PubMed] [Google Scholar]
- 447.Iesalnieks I, Deimel S, Schlitt HJ. “Pit picking” surgery for patients with pilonidal disease: mid-term results and risk factors. Chirurg. 2015;86:482–485. doi: 10.1007/s00104-014-2776-0. [DOI] [PubMed] [Google Scholar]
- 448.Klaiber C, Staub A, Ackermann D, Akovbiantz A. The Lord-Millar operation of pilonidal sinus [Die Sakraldermoidoperation nach Lord-Millar] Helv. Chir. Acta. 1982;49:221–222. [Google Scholar]
- 449.Froidevaux A, Marti MC. Sacro coccygeal cysts. Results of a new series of 51 cases [Kystes Sacro Coccygiens. Resultats d´une nouvelle serie de 51 cas] Lyon Chir. 1977;73:269–271. [Google Scholar]
- 450.Jensen SL, Nielsen OV. Lord-Millar brush method in ambulatory treatment of pilonidal cysts. Ugeskr Laeger. 1988;150:98–100. [PubMed] [Google Scholar]
- 451.Di Castro A, Guerra F, Sandri GB, Maria Ettorre G. Minimally invasive surgery for the treatment of pilonidal disease. The Gips procedure on 2347 patients. Int J Surg. 2016;36:201–205. doi: 10.1016/j.ijsu.2016.10.040. [DOI] [PubMed] [Google Scholar]
- 452.Petersen S. Skin preserving pit excision, so-called pit picking. Pilonidal Sinus Journal. 2017;3:1–7. [Google Scholar]
- 453.Awad MM, Saad KM. Does closure of chronic pilonidal sinus still remain a matter of debate after bilateral rotation flap? (N-shaped closure technique) Indian J Plast Surg. 2006;39:157–162. doi: 10.4103/0970-0358.29545. [DOI] [Google Scholar]
- 454.Polat C, et al. Is oval flap reconstruction a good modification for treating pilonidal sinuses? Am J Surg. 2011;201:192–196. doi: 10.1016/j.amjsurg.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 455.Krand O, Yalt T, Berber I, Kara VM, Tellioglu G. Management of pilonidal sinus disease with oblique excision and bilateral gluteus maximus fascia advancing flap: result of 278 patients. Dis Colon Rectum. 2009;52:1172–1177. doi: 10.1007/DCR.0b013e31819ef582. [DOI] [PubMed] [Google Scholar]
- 456.Nessar G, Kayaalp C, Seven C. Elliptical rotation flap for pilonidal sinus. Am J Surg. 2004;187:300–303. doi: 10.1016/j.amjsurg.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 457.El-Khatib HA, Al-Basti HB. A perforator-based bilobed fasciocutaneous flap: an additional tool for primary reconstruction following wide excision of sacrococcygeal pilonidal disease. J Plast Reconstr Aesthet Surg. 2009;62:494–498. doi: 10.1016/j.bjps.2007.11.043. [DOI] [PubMed] [Google Scholar]
- 458.Dizen H, Yoldas O, Yildiz M, Cilekar M, Dilektasli E. Modified elliptical rotation flap for sacrococcygeal pilonidal sinus disease. ANZ J Surg. 2014;84:769–771. doi: 10.1111/ans.12818. [DOI] [PubMed] [Google Scholar]
- 459.Turan A, Isler C, Bas SC, Genc B, Ozsoy Z. A new flap for reconstruction of pilonidal sinus: lumbar adipofascial turnover flap. Ann Plast Surg. 2007;58:411–415. doi: 10.1097/01.sap.0000243999.36577.3f. [DOI] [PubMed] [Google Scholar]
- 460.Schrogendorfer KF, et al. Prospective evaluation of a single-sided innervated gluteal artery perforator flap for reconstruction for extensive and recurrent pilonidal sinus disease: functional, aesthetic, and patient-reported long-term outcomes. World J Surg. 2012;36:2230–2236. doi: 10.1007/s00268-012-1639-4. [DOI] [PubMed] [Google Scholar]
- 461.Berkem H, et al. V-Y advancement flap closures for complicated pilonidal sinus disease. Int J Colorectal Dis. 2005;20:343–348. doi: 10.1007/s00384-004-0699-9. [DOI] [PubMed] [Google Scholar]
- 462.Acarturk TO, Parsak CK, Sakman G, Demircan O. Superior gluteal artery perforator flap in the reconstruction of pilonidal sinus. J Plast Reconstr Aesthet Surg. 2010;63:133–139. doi: 10.1016/j.bjps.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 463.Schoeller T, Wechselberger G, Otto A, Papp C. Pilonidal sinus: experience with the Karydakis flap. Br J Surg. 1997;84:890–891. doi: 10.1002/bjs.1800840650. [DOI] [PubMed] [Google Scholar]
- 464.Dylek ON, Bekereciodlu M. Role of simple V-Y advancement flap in the treatment of complicated pilonidal sinus. Eur J Surg. 1998;164:961–964. doi: 10.1080/110241598750005147. [DOI] [PubMed] [Google Scholar]
- 465.Mackowski, A. & Levitt, M. Outcomes of the house advancement flap for pilonidal sinus. ANZ J Surg, 10.1111/ans.13077 (2015). [DOI] [PubMed]
- 466.Ekci B, Gokce O. A new flap technique to treat pilonidal sinus. Tech Coloproctol. 2009;13:205–209. doi: 10.1007/s10151-009-0500-8. [DOI] [PubMed] [Google Scholar]
- 467.Lasheen AE, Saad K, Raslan M. Crossed triangular flaps technique for surgical treatment of chronic pilonidal sinus disease. Arch Surg. 2008;143:503–505. doi: 10.1001/archsurg.143.5.503. [DOI] [PubMed] [Google Scholar]
- 468.Awad MM, Saad KM, Tolba AM, Gharib OH. A simple novel technique for closure of simple and complex pilonidal sinus with either simple (tongue-shaped) or bilobed rotation flap. Indian J Plast Surg. 2007;44:47–50. doi: 10.4103/0970-0358.32663. [DOI] [Google Scholar]
- 469.Eryilmaz R, Okan I, Coskun A, Bas G, Sahin M. Surgical treatment of complicated pilonidal sinus with a fasciocutaneous V-Y advancement flap. Dis Colon Rectum. 2009;52:2036–2040. doi: 10.1007/DCR.0b013e3181beb537. [DOI] [PubMed] [Google Scholar]
- 470.Basterzi Y, et al. Reconstruction of extensive pilonidal sinus defects with the use of S-GAP flaps. Ann Plast Surg. 2008;61:197–200. doi: 10.1097/SAP.0b013e3181587a06. [DOI] [PubMed] [Google Scholar]
- 471.Saray A, Dirlik M, Caglikulekci M, Turkmenoglu O. Gluteal V-Y advancement fasciocutaneous flap for treatment of chronic pilonidal sinus disease. Scand J Plast Reconstr Surg Hand Surg. 2002;36:80–84. doi: 10.1080/028443102753575211. [DOI] [PubMed] [Google Scholar]
- 472.Venus, M. R. & Titley, O. G. Outcomes in the repair of pilonidal sinus disease excision wounds using a parasacral perforator flap. Ann R Coll Surg Engl94, 12–16, 10.1308/003588412X13171221499748, 10.1308/003588412X13373405387339 (2012). [DOI] [PMC free article] [PubMed]
- 473.Yuksel BC, Berkem H, Ozel H, Hengirmen S. A new surgical method of pilonidal sinus treatment: a bilaterally paralel elliptic fascio-cutaneous advancement flap technique. Bratisl Lek Listy. 2012;113:728–731. doi: 10.4149/bll_2012_165. [DOI] [PubMed] [Google Scholar]
- 474.Sahasrabudhe P, Panse N, Waghmare C, Waykole P. V-y advancement flap technique in resurfacing postexcisional defect in cases with pilonidal sinus disease-study of 25 cases. Indian J Surg. 2012;74:364–370. doi: 10.1007/s12262-011-0403-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Ozdemir H, Unal Ozdemir Z, Tayfun Sahiner I, Senol M. Whole natal cleft excision and flap: an alternative surgical method in extensive sacrococcygeal pilonidal sinus disease. Acta Chir Belg. 2014;114:266–270. doi: 10.1080/00015458.2014.11681024. [DOI] [PubMed] [Google Scholar]
- 476.Kayaalp C, Olmez A, Aydin C, Piskin T. Tumescent local anesthesia for excision and flap procedures in treatment of pilonidal disease. Dis Colon Rectum. 2009;52:1780–1783. doi: 10.1007/DCR.0b013e3181b553bb. [DOI] [PubMed] [Google Scholar]
- 477.Onishi K, Maruyama Y. Sacral adipofascial turn-over flap for the excisional defect of pilonidal sinus. Plast Reconstr Surg. 2001;108:2006–2010. doi: 10.1097/00006534-200112000-00026. [DOI] [PubMed] [Google Scholar]
- 478.Sungur N, et al. V-Y rotation advancement fasciocutaneous flap for excisional defects of pilonidal sinus. Plast Reconstr Surg. 2006;117:2448–2454. doi: 10.1097/01.prs.0000219170.74059.94. [DOI] [PubMed] [Google Scholar]
- 479.Demiryilmaz I, et al. Application of fasciocutaneous V-Y advancement flap in primary and recurrent sacrococcygeal pilonidal sinus disease. Med Sci Monit. 2014;20:1263–1266. doi: 10.12659/MSM.890752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Yucel, E., Tezcan, L. & Yilmaz, O. C. “Flag Excision an Flap” Procedure: a Novel Modification for Off-Midline Closure After Pilonidal Sinus Excision. Indian J Surg (2015). [DOI] [PMC free article] [PubMed]
- 481.Yazar M, et al. Cosmetic closure of pilonidal sinus defects with bilateral transpositional adipofascial flaps. J Plast Surg Hand Surg. 2013;47:292–296. doi: 10.3109/2000656X.2013.765884. [DOI] [PubMed] [Google Scholar]
- 482.Elalfy K, Emile S, Lotfy A, Youssef M, Elfeki H. Bilateral gluteal advancement flap for treatment of recurrent sacrococcygeal pilonidal disease: A prospective cohort study. Int J Surg. 2016;29:1–8. doi: 10.1016/j.ijsu.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 483.Al Najjar MJ, Al-Helfy SHA. Elliptical Rotation Flap for Complicated Pilonidal Sinus. Iraqi JMS. 2015;13:56–63. [Google Scholar]
- 484.Kauer OG, Correa VR, Rojas PH. Utilizacion del colgajo romboidal simple en el tratamiento quirurgico de la enfermedad pilonidal. Rev. Chil. Cir. 1999;51:623–626. [Google Scholar]
- 485.Trooskin SZ. Pilonidal cyst: wide excision and primary closure with an advancement flap. J Med Soc N J. 1985;82:367–370. [PubMed] [Google Scholar]
- 486.Stroosma OC. Gluteal fasciaplasty as a method of primary closure in the treatment of pilonidal sinus. Arch Chir Neerl. 1978;30:61–64. [PubMed] [Google Scholar]
- 487.Schoeller T, Wechselberger G, Otto A, Papp C. Definite surgical treatment of complicated recurrent pilonidal disease with a modified fasciocutaneous V-Y advancement flap. Surgery. 1997;121:258–263. doi: 10.1016/S0039-6060(97)90354-8. [DOI] [PubMed] [Google Scholar]
- 488.Fjermeros H. Pilonidal cysts; treatment by Holman’s operation. Acta Chir Scand. 1957;113:374–379. [PubMed] [Google Scholar]
- 489.Javed MA, et al. Comparison of conventional incision and drainage for pilonidal abscess versus novel endoscopic pilonidal abscess treatment (EPAT) Tech Coloproctol. 2016;20:871–873. doi: 10.1007/s10151-016-1546-z. [DOI] [PubMed] [Google Scholar]
- 490.Kayaalp C, Olmez A, Aydin C, Piskin T, Kahraman L. Investigation of a one-time phenol application for pilonidal disease. Med Princ Pract. 2010;19:212–215. doi: 10.1159/000285291. [DOI] [PubMed] [Google Scholar]
- 491.Kaymakcioglu N, et al. Treatment of pilonidal sinus by phenol application and factors affecting the recurrence. Tech Coloproctol. 2005;9:21–24. doi: 10.1007/s10151-005-0187-4. [DOI] [PubMed] [Google Scholar]
- 492.Sakcak I, Avsar FM, Cosgun E. Comparison of the application of low concentration and 80% phenol solution in pilonidal sinus disease. JRSM Short Rep. 2010;1:5. doi: 10.1258/shorts.2009.100047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493.Girgin M, et al. Minimally invasive treatment of pilonidal disease: crystallized phenol and laser depilation. Int Surg. 2012;97:288–292. doi: 10.9738/CC130.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 494.Aygen E, Arslan K, Dogru O, Basbug M, Camci C. Crystallized phenol in nonoperative treatment of previously operated, recurrent pilonidal disease. Dis Colon Rectum. 2010;53:932–935. doi: 10.1007/DCR.0b013e3181d8283b. [DOI] [PubMed] [Google Scholar]
- 495.Dag A, Colak T, Turkmenoglu O, Sozutek A, Gundogdu R. Phenol procedure for pilonidal sinus disease and risk factors for treatment failure. Surgery. 2012;151:113–117. doi: 10.1016/j.surg.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 496.Dogru O, Camci C, Aygen E, Girgin M, Topuz O. Pilonidal sinus treated with crystallized phenol: an eight-year experience. Dis Colon Rectum. 2004;47:1934–1938. doi: 10.1007/s10350-004-0720-y. [DOI] [PubMed] [Google Scholar]
- 497.Schneider IH, Thaler K, Kockerling F. Treatment of pilonidal sinuses by phenol injections. Int J Colorectal Dis. 1994;9:200–202. doi: 10.1007/BF00292250. [DOI] [PubMed] [Google Scholar]
- 498.Aksoy HM, Aksoy B, Egemen D. Effectiveness of topical use of natural polyphenols for the treatment of sacrococcygeal pilonidal sinus disease: a retrospective study including 192 patients. Eur J Dermatol. 2010;20:476–481. doi: 10.1684/ejd.2010.0978. [DOI] [PubMed] [Google Scholar]
- 499.Girgin M, Kanat BH. The results of a one-time crystallized phenol application for pilonidal sinus disease. Indian J Surg. 2014;76:17–20. doi: 10.1007/s12262-012-0548-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 500.Kelly SB, Graham WJ. Treatment of pilonidal sinus by phenol injection. Ulster Med J. 1989;58:56–59. [PMC free article] [PubMed] [Google Scholar]
- 501.Maurice BA, Greenwood RK. A Conservative Treatment of Pilonidal Sinus. Br J Surg. 1964;51:510–512. doi: 10.1002/bjs.1800510711. [DOI] [PubMed] [Google Scholar]
- 502.Stewart TJ, Bell M. The treatment of pilonidal sinus by phenol injection. Ulster Med J. 1969;38:167–171. [PMC free article] [PubMed] [Google Scholar]
- 503.Hegge HG, Vos GA, Patka P, Hoitsma HF. Treatment of complicated or infected pilonidal sinus disease by local application of phenol. Surgery. 1987;102:52–54. [PubMed] [Google Scholar]
- 504.Yuksel ME. Pilonidal sinus disease can be treated with crystallized phenol using a simple three-step technique. Acta Dermatovenerol Alp Pannonica Adriat. 2017;26:15–17. doi: 10.15570/actaapa.2017.4. [DOI] [PubMed] [Google Scholar]
- 505.Emiroglu, M. et al. The effect of phenol concentration on the treatment of pilonidal sinus disease: Early results of a prospective randomized study. Int Surg, 10.9738/INTSURG-D-15-00120.1 (2016). [DOI] [PubMed]
- 506.Lindholt-Jensen CS, Lindholt JS, Beyer M. Nd-YAG laser treatment of primary and recurrent pilonidal sinus. Lasers Med Sci. 2012;27:505–508. doi: 10.1007/s10103-011-0990-2. [DOI] [PubMed] [Google Scholar]
- 507.Landa N, Aller O, Landa-Gundin N, Torrontegui J, Azpiazu JL. Successful treatment of recurrent pilonidal sinus with laser epilation. Dermatol Surg. 2005;31:726–728. doi: 10.1097/00042728-200506000-00024. [DOI] [PubMed] [Google Scholar]
- 508.Shafigh Y, Beheshti A, Charkhchian M, Rad FS. Successful treatment of pilonidal disease by intense pulsed light device. Adv Clin Exp Med. 2014;23:277–282. doi: 10.17219/acem/37077. [DOI] [PubMed] [Google Scholar]
- 509.Isik A, et al. The use of fibrin glue without surgery in the treatment of pilonidal sinus disease. Int J Clin Exp Med. 2014;7:1047–1051. [PMC free article] [PubMed] [Google Scholar]
- 510.Rao AC. Cutting seton for pilonidal disease: a new approach. Tech Coloproctol. 2006;10:242–244. doi: 10.1007/s10151-006-0287-9. [DOI] [PubMed] [Google Scholar]
- 511.Meinero P, Mori L, Gasloli G. Endoscopic pilonidal sinus treatment (E.P.Si.T.) Tech Coloproctol. 2014;18:389–392. doi: 10.1007/s10151-013-1016-9. [DOI] [PubMed] [Google Scholar]
- 512.Hussain ZI, Aghahoseini A, Alexander D. Converting emergency pilonidal abscess into an elective procedure. Dis Colon Rectum. 2012;55:640–645. doi: 10.1097/DCR.0b013e31824b9527. [DOI] [PubMed] [Google Scholar]
- 513.Evers T, et al. Trends in incidence and long-term recurrence rate of pilonidal sinus disease and analysis of associated influencing factors. Zhonghua Wai Ke Za Zhi. 2011;49:799–803. [PubMed] [Google Scholar]
- 514.Milone M, et al. Video-assisted ablation of pilonidal sinus: a new minimally invasive treatment–a pilot study. Surgery. 2014;155:562–566. doi: 10.1016/j.surg.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 515.Chia CL, Tay VW, Mantoo SK. Endoscopic pilonidal sinus treatment in the Asian population. Surg Laparosc Endosc Percutan Tech. 2015;25:e95–97. doi: 10.1097/SLE.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 516.Meinero, P. et al. Endoscopic pilonidal sinus treatment (EPSiT): a prospective multicentre trial. Colorectal Dis, 10.1111/codi.13322 (2016). [DOI] [PubMed]
- 517.Hemanta P, Kumar RR, Rao MM. Ksharasutra therapy - a minimal invasive parasurgical method in the treatment of sacrococcygeal pilonidal sinus (Nadi vrana): Result of a pilot study. Intern. J. Res. Ayurveda Pharm. 2012;3:668–670. doi: 10.7897/2277-4343.03518. [DOI] [Google Scholar]
- 518.Borde CM, Bruck HG. The indications for split thickness skin grafting in recurrent pilonidal sinus [Die Indikation zur Spalthautplastik bei rezidivierendem pilonidalem Sinus (Sakraldermoid)] Wiener Klinische Wochenschrift. 1973;85:624–628. [PubMed] [Google Scholar]
- 519.Jain Y, et al. Endoscopic pilonidal abscess treatment: a novel approach for the treatment of pilonidal abscess. Ann R Coll Surg Engl. 2017;99:134–136. doi: 10.1308/rcsann.2016.0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 520.Berger H. The medical treatment of pilonidal disease. N Y State J Med. 1949;49:1313. [PubMed] [Google Scholar]
- 521.Gecim IE, Goktug UU, Celasin H. Endoscopic Pilonidal Sinus Treatment Combined With Crystalized Phenol Application May Prevent Recurrence. Dis Colon Rectum. 2017;60:405–407. doi: 10.1097/DCR.0000000000000778. [DOI] [PubMed] [Google Scholar]
- 522.Suarez Valladares, M. J. & Rodriguez-Prieto, M. A. Laser Nd:YAG to treat primary pilonidal cysts: an alternative treatment. Br J Dermatol, 10.1111/bjd.15929 (2017). [DOI] [PubMed]
- 523.Giarratano, G. et al. Endoscopic Pilonidal Sinus Treatment: Long-Term Results of a Prospective Series. JSLS21, 10.4293/JSLS.2017.00043 (2017). [DOI] [PMC free article] [PubMed]
- 524.Rogers H, Dwight RW. Pilonidal Sinus: Observations on One Hundred Forty Cases Treated by Cautery Excision. Ann Surg. 1938;107:400–418. doi: 10.1097/00000658-193803000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 525.Close AS. Pilonidal cysts: an analysis of surgical failures. Ann Surg. 1955;141:523–526. doi: 10.1097/00000658-195504000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 526.Hoffert PW, Healy MJ., Jr. Pilonidal sinus and cyst: an analysis of the results of surgical therapy in 229 consecutive cases. Bull N Y Acad Med. 1952;28:612. [PubMed] [Google Scholar]
- 527.Dwight RW, Maloy JK. Pilonidal sinus; experience with 449 cases. N Engl J Med. 1953;249:926–930. doi: 10.1056/NEJM195312032492303. [DOI] [PubMed] [Google Scholar]
- 528.Breidenbach L, Wilson HL. Pilonidal Cysts and Sinuses. Ann Surg. 1935;102:455–463. doi: 10.1097/00000658-193509000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 529.Palumbo LT, Larimore OM, Katz IA. Pilonidal cysts and sinuses; a statistical review. AMA Arch Surg. 1951;63:852–857. doi: 10.1001/archsurg.1951.01250040868016. [DOI] [PubMed] [Google Scholar]
- 530.Kleckner MS. Pilonidal Sinus: Its surgical management. Trans Am Proctol Soc. 1936;36:166. [Google Scholar]
- 531.Mathesheimer JL. An ambulant method for the treatment of pilonidal disease. Am J Surg. 1945;69:230–231. doi: 10.1016/S0002-9610(45)90377-1. [DOI] [Google Scholar]
- 532.Lawrence KB, Baker WJ. The marsupialization operation for pilonidal sinus; a comparison with other surgical methods in 359 cases. N Engl J Med. 1951;245:134–139. doi: 10.1056/NEJM195107262450403. [DOI] [PubMed] [Google Scholar]
- 533.Kleiman A. Pilonidal cyst; follow-up studies on 481 patients. US Armed Forces Med J. 1952;3:575–580. [PubMed] [Google Scholar]
- 534.Guyuron B, Dinner MI, Dowden RV. Excision and grafting in treatment of recurrent pilonidal sinus disease. Surg Gynecol Obstet. 1983;156:201–204. [PubMed] [Google Scholar]
- 535.Jordan MH, Meinecke HM. Ambulatory surgery for pilonidal disease. Am Surg. 1979;45:360–363. [PubMed] [Google Scholar]
- 536.Feigenbaum HA. Excision of acute pilonidal cyst abscess; a preliminary report. Am J Surg. 1957;94:636–637. doi: 10.1016/0002-9610(57)90595-0. [DOI] [PubMed] [Google Scholar]
- 537.Brust JC, Sarner JB. Pilonidal cyst. N Y State J Med. 1948;48:2138–2144. [PubMed] [Google Scholar]
- 538.Larsen BB. Comparative results-in operations for pilonidal cysts. Arch Surg. 1948;56:516–521. doi: 10.1001/archsurg.1948.01240010524006. [DOI] [PubMed] [Google Scholar]
- 539.Heaton, J. R. Surgical treatment of pilonidal disease. J Mich State Med Soc56, 1566–1567 passim (1957). [PubMed]
- 540.Grau HR. Pilonidal sinus; etiology of recurrence. J Int Coll Surg. 1951;15:591–604. [PubMed] [Google Scholar]
- 541.Heifetz CJ. Pilonidal disease; a study of fifty consecutive cases treated successfully by excision and primary closure. Am J Surg. 1958;96:405–410. doi: 10.1016/0002-9610(58)90934-6. [DOI] [PubMed] [Google Scholar]
- 542.Comarr AE. Pilonidal cysts and/or sinuses: primary closure with the wirebution retention technic. Am J Surg. 1959;97:328–330. doi: 10.1016/0002-9610(59)90310-1. [DOI] [PubMed] [Google Scholar]
- 543.Ross RL. Recurrent pilonidal cyst and sinus; a plan of preoperative preparation, operation and postoperative care. Calif Med. 1956;85:183–186. [PMC free article] [PubMed] [Google Scholar]
- 544.Leichtling JJ. Simple primary closure for sacrococcygeal pilonidal disease. Am J Surg. 1967;113:441–444. doi: 10.1016/0002-9610(67)90298-X. [DOI] [PubMed] [Google Scholar]
- 545.Larsen BB. Pilonidal cysts and sinuses; a technic for excision and primary closure. Ann Surg. 1946;123:1090–1100. doi: 10.1097/00000658-194606000-00012. [DOI] [PubMed] [Google Scholar]
- 546.Hamilton JE, Cattanach LM. Comparative study of chemotherapies in the surgery of pilonidal sinus. Am J Surg. 1947;74:449–454. doi: 10.1016/0002-9610(47)90138-4. [DOI] [PubMed] [Google Scholar]
- 547.Goldman B. Combined therapy for pilonidal (sacrococcygeal) cyst and sinus; roentgen epilation of operative field prior to surgical excision with primary closure. J Int Coll Surg. 1952;18:903–909. [PubMed] [Google Scholar]
- 548.Ferguson LK, Mecray PM. Pilonidal Cysts: Excision and primary suture in ambulatory patients. Am J Surg. 1937;36:270–277. doi: 10.1016/S0002-9610(37)90829-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 549.Larkin LC. Pilonidal cyst; analysis of 100 consecutive cases, emphasizing treatment by radical excision, primary closure and penicillin therapy. Surg Gynecol Obstet. 1946;82:694–704. [PubMed] [Google Scholar]
- 550.Bear NE, Woldman VF. Treatment of pilonidal cysts. Wis Med J. 1945;44:1166–1169. [PubMed] [Google Scholar]
- 551.Bentivegna SS, Procario P. Primary closure of pilonidal cystectomy. Am Surg. 1977;43:214–216. [PubMed] [Google Scholar]
- 552.Laforet EG. Pilonidal sinus; a method of treatment by primary closure. Am J Surg. 1957;93:873–875. doi: 10.1016/0002-9610(57)90566-4. [DOI] [PubMed] [Google Scholar]
- 553.Finestone EO. Technic of excision and primary closure of pilonidal sinus. N Y State J Med. 1952;52:1291–1294. [PubMed] [Google Scholar]
- 554.Turner FP, O’Neil JW. Treatment of pilonidal sinus by primary closure; a seven-year study. AMA Arch Surg. 1959;78:398–405. doi: 10.1001/archsurg.1959.04320030042008. [DOI] [PubMed] [Google Scholar]
- 555.Hamilton JE, Stephens G, Claugus CE. Pilonidal Sinus: Excision and Primary Closure. Surgery. 1963;54:597–603. [PubMed] [Google Scholar]
- 556.Beardsley JM. Treatment of pilonidal cyst and sinus. AMA Arch Surg. 1954;68:608–611. doi: 10.1001/archsurg.1954.01260050610004. [DOI] [PubMed] [Google Scholar]
- 557.Ziegler HR, Murphey DR, Jr., Meek EM. Pilonidal cyst and sinus; a new method of excision with primary closure. Surgery. 1946;20:690–703. [PubMed] [Google Scholar]
- 558.Bellis CJ. Pilonidal cyst; treatment by a uniformly successful method. J Int Coll Surg. 1950;13:334–337. [PubMed] [Google Scholar]
- 559.Kleitsch WP, Cherry LD. Pilonidal sinus; a rational scheme of treatment. Mil Surg. 1952;111:96–106. [PubMed] [Google Scholar]
- 560.Casten DF, Tan BY, Ayuyao A. A technique of radical excision of pilonidal disease with primary closure. Surgery. 1973;73:109–114. [PubMed] [Google Scholar]
- 561.Brezin D, Love C, Lawrence J. Pilonidal cyst. Am J Surg. 1943;60:264–266. doi: 10.1016/S0002-9610(43)90662-2. [DOI] [Google Scholar]
- 562.Bascom, J. & Bascom, T. Failed pilonidal surgery: new paradigm and new operation leading to cures. Arch Surg137, 1146–1150; discussion 1151 (2002). [DOI] [PubMed]
- 563.Bascom, J. & Bascom, T. Utility of the cleft lift procedure in refractory pilonidal disease. Am J Surg193, 606–609; discussion 609, 10.1016/j.amjsurg.2007.01.008 (2007). [DOI] [PubMed]
- 564.Immerman SC. Treatment of pilonidal disease using the Bascom ‘Cleft-Lift’ procedure. Am Surg. 2014;80:E49–50. [PubMed] [Google Scholar]
- 565.Bascom JU. Repeat pilonidal operations. Am J Surg. 1987;154:118–122. doi: 10.1016/0002-9610(87)90300-X. [DOI] [PubMed] [Google Scholar]
- 566.Mansoory A, Dickson D. Z-plasty for treatment of disease of the pilonidal sinus. Surg Gynecol Obstet. 1982;155:409–411. [PubMed] [Google Scholar]
- 567.Abramson DJ. A simple marsupialization technic for treatment of pilonidal sinus: long-term follow up. Ann Surg. 1960;151:261–267. doi: 10.1097/00000658-196002000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 568.Neumeister CA. A modification of the marsupialization operation for pilonidal disease. South Med J. 1963;56:730–732. doi: 10.1097/00007611-196307000-00006. [DOI] [PubMed] [Google Scholar]
- 569.Cavanagh CR, Schnug GE, Girvin GW, McGonigle DJ. Definitive marsupialization of the acute pilonidal abscess. Am Surg. 1970;36:650–651. [PubMed] [Google Scholar]
- 570.van Ess LJ. Surgical management of pilonidal disease. Am J Proctol. 1965;16:389–393. [PubMed] [Google Scholar]
- 571.Uhle AO. Eventration of pilonidal cysts and sinuses. Northwest Med. 1957;56:687–690. [PubMed] [Google Scholar]
- 572.Gage AA, Dutta P. Cryosurgery for pilonidal disease. Am J Surg. 1977;133:249–254. doi: 10.1016/0002-9610(77)90093-9. [DOI] [PubMed] [Google Scholar]
- 573.O’Connor JJ. Surgery plus freezing as a technique for treating pilonidal disease. Dis Colon Rectum. 1979;22:306–307. doi: 10.1007/BF02609310. [DOI] [PubMed] [Google Scholar]
- 574.Miller RJ. Pilonidal disease. A logical approach. Postgrad Med. 1967;41:382–385. doi: 10.1080/00325481.1967.11696173. [DOI] [PubMed] [Google Scholar]
- 575.Matino JJ, Banerjee S, Brown SH, Waldron JE. Human dermal tissue allograft use in treating chronic pilonidal sinus. Conn Med. 2010;74:393–398. [PubMed] [Google Scholar]
- 576.Shafiroff BG, Doubilet H. The conservative treatment of pilonidal cyst. N Y State J Med. 1946;46:891–893. [PubMed] [Google Scholar]
- 577.Crile G., Jr. A definitive ambulatory treatment for infected pilonidal cysts. Surgery. 1948;24:677–679. [PubMed] [Google Scholar]
- 578.Korb JH. Infected pilonidal cysts; a simplified method of treatment. Mil Surg. 1951;108:29–34. [PubMed] [Google Scholar]
- 579.Bascom J. Pilonidal disease: long-term results of follicle removal. Dis Colon Rectum. 1983;26:800–807. doi: 10.1007/BF02554755. [DOI] [PubMed] [Google Scholar]
- 580.Bascom J. Pilonidal disease: origin from follicles of hairs and results of follicle removal as treatment. Surgery. 1980;87:567–572. [PubMed] [Google Scholar]
- 581.Turner FP. Pilonidal sinus: primary closure with equal musculofascial flaps and removable far-and-near sutures; analysis of fifty-nine consecutive cases. Ann Surg. 1954;140:687–694. doi: 10.1097/00000658-195411000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 582.Cherry JK. Primary closure of pilonidal sinus. Surg Gynecol Obstet. 1968;126:1263–1269. [PubMed] [Google Scholar]
- 583.Dwight RW. Pilonidal sinus; an evaluation of plastic closure using flaps of gluteal muscle. AMA Arch Surg. 1952;64:438–442. doi: 10.1001/archsurg.1952.01260010454003. [DOI] [PubMed] [Google Scholar]
- 584.Feit HL. The use of thorium X in treatment of pilonidal cyst: a preliminary report. Dis Colon Rectum. 1960;3:61–64. doi: 10.1007/BF02616500. [DOI] [PubMed] [Google Scholar]
- 585.Armstrong, J. H. & Barcia, P. J. Pilonidal sinus disease. The conservative approach. Arch Surg129, 914–917 discussion 917–919 (1994). [DOI] [PubMed]
- 586.Pyrtek LJ, Bartus SA. Excision of Pilonidal Cyst with Simplified Partial Wound Closure. Surg Gynecol Obstet. 1964;118:605–608. [PubMed] [Google Scholar]
- 587.Petersen S, et al. Short-term results of Karydakis flap for pilonidal sinus disease. Tech Coloproctol. 2007;11:235–240. doi: 10.1007/s10151-007-0357-7. [DOI] [PubMed] [Google Scholar]
- 588.Doll D, Luedi MM, Evers T, Kauf P, Matevossian E. Recurrence-free survival, but not surgical therapy per se, determines 583 patients’ long-term satisfaction following primary pilonidal sinus surgery. Int J Colorectal Dis. 2015;30:605–611. doi: 10.1007/s00384-015-2130-0. [DOI] [PubMed] [Google Scholar]
- 589.Vogel P, Lenz J. Treatment of pilonidal sinus with excision and primary suture using a local, resorbable antibiotic carrier. Results of a prospective randomized study. Chirurg. 1992;63:748–753. [PubMed] [Google Scholar]
- 590.Denkers D, Girona J. Der abszedierte Sinus pilonidalis der Steißbeinregion - Möglichkeiten der chirurgischen Versorgung. Coloproctology. 1996;18:257–259. [Google Scholar]
- 591.Eichfuss HP, Eichen R, Koch G, Eckert P. Primary closure of the sinus pilonidalis. Chirurg. 1978;49:124–126. [PubMed] [Google Scholar]
- 592.Eichfuss HP, Schontag H, Pfeiffer M. A new surgical procedure for treating sacrococcygeal fistulas and cysts. [Ein neues Operationsverfahren der Steissbeinfisteln und -zysten] Aktuel Chir. 1982;17:138–140. [Google Scholar]
- 593.Hasse FM, Rademacher C, Bingham K, Lohlein D. The Dufourmentel flap-plasty for treatment of chronic pilonidal sinus. Chirurg. 1998;69:663–666. doi: 10.1007/s001040050472. [DOI] [PubMed] [Google Scholar]
- 594.Jaschke CW, Mahrlein R, Mangold G. Results of the Limberg transposition flap in the treatment of pilonidal sinus. Zentralbl Chir. 2002;127:712–715. doi: 10.1055/s-2002-33579. [DOI] [PubMed] [Google Scholar]
- 595.Friedl PG, Rappold EM, Jager C. Effective and minimally painful surgery of pilonidal sinus - asymmetric transposition flap according to Dufourmentel. J Dtsch Dermatol Ges. 2011;9:333–335. doi: 10.1111/j.1610-0387.2011.07662.x. [DOI] [PubMed] [Google Scholar]
- 596.Geuenich A, Hannekum A. Primary closure of pilonidal sinus through a slide-swing operation. Chirurg. 1981;52:114–117. [PubMed] [Google Scholar]
- 597.Akinci OF, Coskun A, Ozgonul A, Terzi A. Surgical treatment of complicated pilonidal disease: limited separate elliptical excision with primary closure. Colorectal Dis. 2006;8:704–709. doi: 10.1111/j.1463-1318.2006.01022.x. [DOI] [PubMed] [Google Scholar]
- 598.Fuzun M, et al. Which technique for treatment of pilonidal sinus–open or closed? Dis Colon Rectum. 1994;37:1148–1150. doi: 10.1007/BF02049819. [DOI] [PubMed] [Google Scholar]
- 599.Aydede H, Erhan Y, Sakarya A, Kumkumoglu Y. Comparison of three methods in surgical treatment of pilonidal disease. ANZ J Surg. 2001;71:362–364. doi: 10.1046/j.1440-1622.2001.02129.x. [DOI] [PubMed] [Google Scholar]
- 600.Cihan A, et al. Modified Limberg flap reconstruction compares favourably with primary repair for pilonidal sinus surgery. ANZ J Surg. 2004;74:238–242. doi: 10.1111/j.1445-2197.2004.02951.x. [DOI] [PubMed] [Google Scholar]
- 601.Yetim I, Ozkan OV, Dervisoglu A, Erzurumlu K, Canbolant E. Effect of gentamicin-absorbed collagen in wound healing in pilonidal sinus surgery: a prospective randomized study. J Int Med Res. 2010;38:1029–1033. doi: 10.1177/147323001003800329. [DOI] [PubMed] [Google Scholar]
- 602.Kaya B, Uctum Y, Simsek A, Kutanis R. Treatment of Pilonidal Sinus with Primary Closure. A Simple and Effective Method. Kolon Rektum Hast Derg. 2010;20:59–65. [Google Scholar]
- 603.Kücükkartallar T, Tekin A, Vatansev C. The comparison of the results of different operation techniques for pilonidal sinus disease. Genel Tip Derg. 2007;17:95–97. [Google Scholar]
- 604.Ozgultekin R, et al. Therapy of pilonidal sinus with the Limberg transposition flap. Chirurg. 1995;66:192–195. [PubMed] [Google Scholar]
- 605.Yilmaz S, Kirimlioglu V, Katz D. RAm. Eur J Surg. 2000;166:269. doi: 10.1080/110241500750009410. [DOI] [PubMed] [Google Scholar]
- 606.Yetişir F, Kaya O, Baran I. The comparison of marsupialization and Limberg flap in the treatment of pilonidal disease. Turk. J. Surg. 2005;21:184–190. [Google Scholar]
- 607.Zorlu M, et al. Early results with the Mutaf technique: a novel off-midline approach in pilonidal sinus surgery. Ann Surg Treat Res. 2016;90:265–271. doi: 10.4174/astr.2016.90.5.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 608.Arik MK, Borazan E. Phenol application combined with minimally invasive surgery for pilonidal sinus treatment [Pi̇loni̇dal si̇nüste mi̇ni̇mal i̇nvazi̇v cerrahi̇ i̇le kombi̇ne fenol uygulamalarimiz] Anatolian J. Clin. Invest. 2011;5:165–168. [Google Scholar]
- 609.Yilmaz M, Engin O, Uyar ME. Crystalline Phenol Practices and Clinical Results in our Patients with Pilonidal Sinus. J Universal Surg. 2015;3:1–4. [Google Scholar]
- 610.Castronovo G, Ciulla A, Urso G, Tomasello G, Damiani S. Pilonidal sinus: an retrospective analysis of 205 cases. Ann Ital Chir. 2003;74:559–563. [PubMed] [Google Scholar]
- 611.Bianco V, Basile C, Tortorella M. Sacrococcygeal pilonidal sinus disease. Treatment by “open” and “closed” technique: personal experience. G Chir. 2003;24:145–147. [PubMed] [Google Scholar]
- 612.Cimarelli S, Magnano G. Treatment of pilonidal sinus. Our experience. Minerva Chir. 1989;44:1131–1134. [PubMed] [Google Scholar]
- 613.Pezzangora V, Averno V, Barina R. Treatment of fistulized pilonidal sinuses by phenol injection. Chir Ital. 1980;32:848–854. [PubMed] [Google Scholar]
- 614.Ciccolo A, et al. Treatment of pilonidal disease in short-stay surgery: personal method. Ann Ital Chir. 2004;75:603–605. [PubMed] [Google Scholar]
- 615.Filingeri V, Gravante G. Radiofrequency sinus excision. Dig. Surg. 2006;23:125. doi: 10.1159/000094136. [DOI] [PubMed] [Google Scholar]
- 616.Brearley R. Treatment of pilonidal sinus. Br Med J. 1959;2:1256. doi: 10.1136/bmj.2.5161.1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 617.Del Papa, M., Mobili, M., Attardo, S., Paolucci, G. & Braccioni, U. Radical excision and primary suture of pilonidal sinus: our experience. Ann Ital Chir63, 507–509; discussion 509–510 (1992). [PubMed]
- 618.Cianci F, Marinaccio F. Treatment of pilonidal sinus by radical excision and primary closure. Our experience. Minerva Chir. 1984;39:1111–1115. [PubMed] [Google Scholar]
- 619.Cortese M, Benedetti Valentini G, Giacomini S. Personal experience in the treatment of pilonidal sinus. Minerva Chir. 1985;40:1137–1139. [PubMed] [Google Scholar]
- 620.Vitale A, Barberis G, Maida P, Salzano A. Use of biological glue in the surgical treatment of sacrococcygeal fistulas. G Chir. 1992;13:271–272. [PubMed] [Google Scholar]
- 621.Muzi MG, et al. Muzi’s Tension Free Primary Closure of Pilonidal Sinus Disease: Long-Term Results on 450 Patients. Gastroenterology. 2017;152:S1212–S1213. doi: 10.1016/s0016-5085(17)34034-9. [DOI] [Google Scholar]
- 622.De Nardi P, Gazzetta PG, Fiorentini G, Guarneri G. The cleft lift procedure for complex pilonidal disease. European Surgery. 2016;48:250–257. doi: 10.1007/s10353-016-0428-y. [DOI] [Google Scholar]
- 623.Casula G, Uccheddu A, Figus M. Long term results of the Z-plasty method in the treatment of pilonidal sinus. Minerva Chir. 1983;38:617–620. [PubMed] [Google Scholar]
- 624.Meinero P, Mori L. Endoscopic pilonidal sinus treatment (E.P.Si.T): a new mininvasive procedure. Journal of the American College of Surgeons. 2014;219:e75. doi: 10.1016/j.jamcollsurg.2014.07.583. [DOI] [Google Scholar]
- 625.Roberton HR. Pilonidal surgery. Med J Aust. 1981;1:375–376. doi: 10.5694/j.1326-5377.1981.tb135941.x. [DOI] [PubMed] [Google Scholar]
- 626.Thomas D. Pilonidal sinus: a review of the literature and a report of 100 cases. Med J Aust. 1968;2:184–188. doi: 10.5694/j.1326-5377.1968.tb29395.x. [DOI] [PubMed] [Google Scholar]
- 627.Kitchen PRB. Pilonidal sinus: Excision and primary closure with a lateralised wound - the Karydakis operation. Aust. New Zealand J. Surg. 1982;52:302–305. doi: 10.1111/j.1445-2197.1982.tb05405.x. [DOI] [PubMed] [Google Scholar]
- 628.McDermott FT. Pilonidal sinus treated by Z-plasty. Aust N Z J Surg. 1967;37:64–69. doi: 10.1111/j.1445-2197.1967.tb06989.x. [DOI] [PubMed] [Google Scholar]
- 629.Hobbs AF. An operative technique for the treatment of pilonidal sinus. Aust N Z J Surg. 1967;36:337–342. doi: 10.1111/j.1445-2197.1967.tb05545.x. [DOI] [PubMed] [Google Scholar]
- 630.Stephens FO, Sloane DR. Management of pilonidal sinus–a modern approach. Med J Aust. 1968;1:395–396. doi: 10.5694/j.1326-5377.1968.tb28590.x. [DOI] [PubMed] [Google Scholar]
- 631.Owen Smith, M. S. Phenol irrigation for pilonidal sinus. 121, 79–86 (1975).
- 632.Evangelou G, Tiniakos G. Treatment of pilonidal sinus disease based on pathological observations. Int Surg. 1974;59:493–496. [PubMed] [Google Scholar]
- 633.Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992;62:385–389. doi: 10.1111/j.1445-2197.1992.tb07208.x. [DOI] [PubMed] [Google Scholar]
- 634.Karydakis GE. New approach to the problem of pilonidal sinus. Lancet. 1973;2:1414–1415. doi: 10.1016/S0140-6736(73)92803-1. [DOI] [PubMed] [Google Scholar]
- 635.Toubanakis G. Treatment of pilonidal sinus disease with the Z-plasty procedure (modified) Am Surg. 1986;52:611–612. [PubMed] [Google Scholar]
- 636.Zambouras DH, Karavas N. Operative Behandlung des Sakraldermoids durch eine neue modifizierte Marsupialisationsmethode. Chirurg. 1971;7:330–331. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data and calculations are available to readers upon request to the corresponding author.