ABSTRACT
Polycystic ovary syndrome (PCOS) affects ∼1 in 10 women worldwide. Hypomagnesemia may worsen insulin resistance (IR) due to the role magnesium (Mg) plays in glucose metabolism. This review explores the relation between serum Mg and IR among women with PCOS. A review of primary research focusing on both serum Mg and women with PCOS was conducted from 2011 to 2019. Studies reviewed included human subjects, written in the English language, and limited to community-dwelling women aged ≥18 y. A total of 7 articles were reviewed. The findings from 4 epidemiological analytic studies evaluating serum Mg status suggest there may be a relation between serum Mg concentrations and IR among women with PCOS. However, among the 3 experimental trials, Mg supplementation inconsistently impacted IR among women with PCOS. Women with PCOS are more likely to underconsume Mg-rich foods and have a greater likelihood of lower serum Mg concentrations. Although it remains unclear if dietary Mg and/or supplementation should be a nutritional strategy for all women with PCOS, current research indicates an association between adequate Mg status and improved IR. Further research evaluating dietary interventions and supplementation is warranted.
Keywords: polycystic ovary syndrome (PCOS), serum magnesium, insulin resistance, glycemic control, diet, supplementation
Introduction
Polycystic ovary syndrome
Polycystic ovary syndrome (PCOS) is a disease that affects 6–10% of females worldwide (1). Among women of reproductive age, PCOS is one of the most common endocrine disorders (2, 3). The diagnostic criteria for PCOS vary among organization recommendations. According to the NIH Consensus, the patient must present with clinical and/or biochemical hyperandrogenism as well as menstrual dysfunction (2). Whereas, the Rotterdam criteria states that patients must present with 2 out of the 3 symptoms: clinical and/or biochemical hyperandrogenism, oligo-ovulation or anovulation, or polycystic ovaries confirmed by ultrasound (4). The Androgen Excess Society's criteria for diagnosis includes clinical and/or biochemical hyperandrogenism and ovarian dysfunction and/or polycystic ovaries (5) (Table 1).
TABLE 1.
Criteria for the diagnosis of polycystic ovary syndrome
| NIH Consensus, 1990 (2) | Rotterdam criteria, 2003 (4) | Androgen Excess Society, 2006 (5) |
|---|---|---|
| Must include all: | Must include 2 out of 3: | Must include all: |
| Clinical and/or biochemical hyperandrogenism | Clinical and/or biochemical hyperandrogenism | Clinical and/or biochemical hyperandrogenism |
| Menstrual dysfunction | Oligo-ovulation or anovulation | Ovarian dysfunction and/or polycystic ovaries |
| Polycystic ovaries (ultrasound) | ||
| Exclusion of: | Exclusion of: | Exclusion of: |
| Nonclassic congenital adrenal hyperplasia | Other conditions mimicking PCOS | Other androgen excess or ovulatory disorders |
| Androgen-secreting tumors |
PCOS, polycystic ovary syndrome.
Signs and symptoms of PCOS may comprise of acne, excess hair or hirsutism, obesity or abdominal fat, alopecia, and acanthosis nigricans, as well as irregular menstrual cycles (2, 3, 6). Women with PCOS are at higher risk of developing obesity, insulin resistance (IR), type 2 diabetes mellitus, cardiovascular disease (CVD), cancer, infertility, and psychological disorders including depression and anxiety (3, 6). An accurate diagnosis of PCOS and early intervention aids in the reduction of reproductive, metabolic, and cardiovascular risks often noted within this population (2, 7). Although the exact pathogenesis of PCOS remains unknown (8, 9) researchers believe genetics, intrauterine factors such as androgen exposure and prenatal nutrition, environment and lifestyle, and obesity are all risk factors (8–10). Some risk factors, such as prenatal environment and genetics (10) cannot be changed; however, lifestyle factors, including diet, physical activity, and obesity (8, 9) may play a role in disease progression and are modifiable.
The treatment of PCOS is dependent upon the signs and symptoms, but current recommendations include weight loss as well as metformin for premenopausal women (7). Although weight loss, even as little as 5%, has been noted to restore normal menses and improve ovulation (7) additional cardiometabolic risk factors may still be present. Furthermore, weight loss may be inappropriate for women presenting as underweight or within a normal weight range or body composition. Therefore, it is critical to evaluate additional treatment options for women seeking disease control without medication or for those women who find weight loss difficult or potentially not appropriate.
Magnesium
Magnesium (Mg) is a cofactor in over 300 enzyme systems and is a required nutrient for both energy production and nucleic acid synthesis (11, 12). The normal blood serum concentration of Mg is between 0.76 and 1.15 mmol/L (1.85–3.65 mg/dL) (12), however, Mg researchers indicate the lower reference limit of serum Mg concentration should be 0.85 mmol/L (2.07 mg/dL), particularly for individuals with impaired glucose control (12, 13). The RDA for women aged ≥19 y is 320 mg (14). There is no evidence of adverse effects related to high intakes of naturally occurring magnesium in foods, thus no tolerable upper intake level (UL) is set for dietary Mg intake (14). However, excess supplemental Mg intake can produce diarrhea and rarely, more serious issues such as hypotension, weakness, and confusion (15). Therefore, a UL of 350 mg/d from supplemented Mg for women aged >14 y was established to reduce the risk of adverse reactions from excess intake (14).
Mg is an abundant mineral found in plant and animal sources as well as drinking water (16). Most foods containing dietary fiber also provide Mg, such as leafy green vegetables, whole grains, legumes, nuts, and seeds (16) (Table 2). Furthermore, some grains, including breakfast cereals, are fortified with Mg. Water, including tap, mineral, and bottled, is a source of Mg, but content varies from 1 mg/L to >120 mg/L depending upon the brand and source (17).
TABLE 2.
| Food | mg per serving |
|---|---|
| Almonds, ¼ cup | 96 |
| Spinach, cooked, ½ cup | 78 |
| Peanuts, oil roasted, ¼ cup | 63 |
| Snacks, trail mix, ¼ cup | 59 |
| Quinoa, cooked, ½ cup | 59 |
| Black beans, cooked, ½ cup | 60 |
| Edamame, shelled, cooked, ½ cup | 50 |
| Chocolate, dark, 1.0 ounce | 50 |
| Peanut butter, smooth, 2 tablespoons | 49 |
| Bread, whole wheat, 2 slices | 46 |
| Avocado, cubed, 1 cup | 44 |
| Potato, baked with skin, 3.5 ounces | 43 |
| Yogurt, plain, low fat, 8 ounces | 42 |
| Oatmeal, instant, 1 packet | 36 |
| Banana, 1 medium | 32 |
| Tomato products, canned, ½ cup | 29 |
| Salmon, Atlantic, farmed, 3 ounces | 26 |
| Milk, 1 cup | 24–27 |
It is estimated that over half of Americans do not obtain ample dietary Mg for various reasons, including low concentrations of Mg in processed foods and common dietary staples such as meat, sugar, and white flour (16, 18). Additionally, the cooking and boiling of produce diminishes the Mg content of food (16). Excessive doses of vitamin D may increase urinary Mg excretion, as Mg is necessary for the conversion of vitamin D into its active form (11, 19). Common medications, such as H2 blockers, proton pump inhibitors (PPIs), and diuretics, reduce the absorption of Mg (11). The FDA suggests clinicians should consider checking serum Mg concentrations prior to initiating PPI therapy for individuals requiring long-term therapy (≥1 y) or with polypharmacy (20). Prescription medications and over-the-counter medications, including PPIs and diuretics, in addition to diet history, should be evaluated as part of the clinician's assessment of the patient.
Mg and IR
Mg directly influences glucose metabolism by acting as a cofactor for many enzymes involved in energy metabolism as well as being part of the Mg2+-ATP complex (21). Beyond the role as a cofactor for over 300 enzymes, Mg is essential for both aerobic and anaerobic energy production by glycolysis and oxidative phosphorylation via the Mg-ATP complex or directly as an enzyme activator (12, 16). The association between Mg and IR among individuals with diabetes mellitus (DM) and metabolic syndrome are well documented (22–25), with low concentrations of magnesium being associated with IR.
It is believed IR is the main pathogenic factor related to the increased rate of metabolic disturbances among women with PCOS (26). The exact underlying cause of IR remains unclear, however numerous mechanisms have been suggested, including oxidative stress and inflammation, endoplasmic reticulum stress, insulin receptor mutations, and mitochondrial dysfunction (3, 27).
Mg is required in the cellular absorption and conversion of glucose into energy (28, 29), and is essential for the autophosphorylation of the insulin receptor, tyrosine kinase (28, 29), which plays a crucial role in glucose uptake in muscular and adipose tissue (28, 29). The presence of Mg ultimately increases ATP receptor sensitivity by increasing tyrosine kinase activity (28, 29). Mg is also required in cellular glucose transport via glucose transporter protein activity-4 (GLUT-4) (28, 29). The autophosphorylation of tyrosine kinase influences the translocation of GLUT-4 to the plasma membrane. The facilitation of glucose transport thereby lowers blood glucose concentrations (28, 29).
It is theorized individuals with DM may benefit from Mg supplementation due to its insulin-sensitizing effect as well as its antagonistic effect with calcium (Ca) (30). Mg may also aid in regulating oxidative stress, thus reducing inflammation and thereby stabilizing the endothelium (30). As such, this benefit may translate to a similar population, such as women with PCOS, particularly women with IR.
Low dietary and serum Mg concentrations as well as an increased Mg urine output are frequently noted among individuals with IR and type 2 diabetes (31). In a 2016 systematic review and meta-analysis, researchers evaluated the effect of oral Mg supplementation on insulin sensitivity and glucose control among individuals presenting with and without DM (25). Mg supplementation doses ranged from 300 to 750 mg/d (25). Researchers found longer Mg supplementation duration, ≥4 mo when compared with <4 mo, significantly improved HOMA-IR (P = 0.001) and fasting glucose (P < 0.001) in both groups (25). A subgroup analysis of the Mg supplementation noted a significantly greater reduction in plasma glucose (P = 0.002) and HOMA-IR (P = 0.009) among individuals with low serum Mg concentrations when compared to individuals with normal serum Mg status (25).
Research evaluating the dietary habits of women with PCOS indicate 1 out of 4 women do not consume adequate amounts of dietary Mg (32). A study by Asemi et al. indicates women with PCOS consume an average of 233 mg/d of Mg, which is below the RDA of 320 mg/d for women aged ≥19 y (33).
With noted improvements among individuals with other metabolic disorders, such as DM, it is plausible to question if Mg may play a role in the nonpharmacologic treatment of IR among women with PCOS. The primary purpose of this review was to determine if there is a relation between serum Mg concentrations and IR among women with PCOS.
Methods
Search strategy
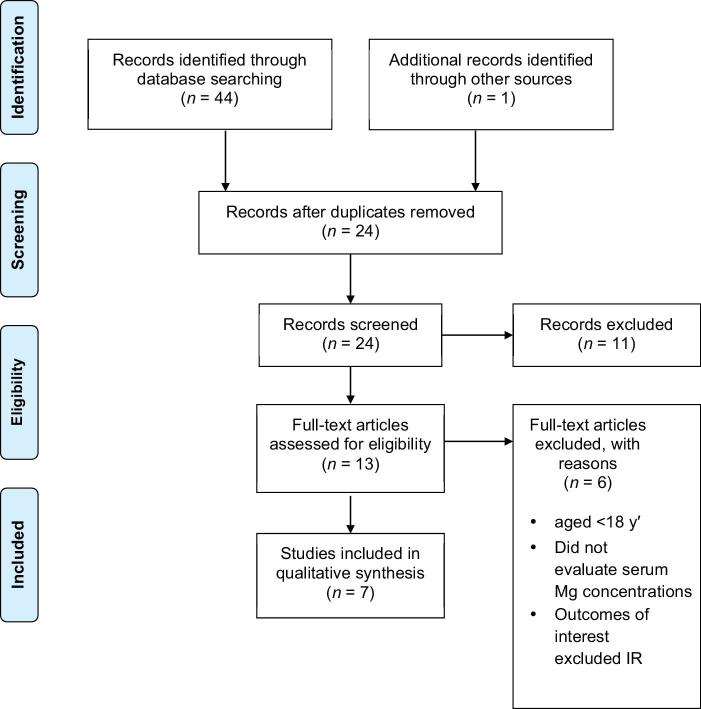
PubMed, the Cochrane Library, and Scopus were utilized to search the literature with keywords “PCOS” or “polycystic ovary syndrome and Mg”. Both medical subject headings (MeSH) terms and non-MeSH terms “magnesium” and “PCOS” were used. The articles included for the review were human, primary articles published within the previous 8 y, between 2011 and 2019, written in the English language, and limited to women aged ≥18 y. Studies involving participants with poor prognosis or acute, critical illness including HIV/AIDS, renal disease, cancer, organ transplant, hepatic disease, as well as those who were pregnant or breastfeeding were excluded. A total of 44 articles were identified from the search, with 1 additional source identified from a manual search of previously published articles. After eliminating duplicates and reviewing titles and abstracts of all articles, a total of 13 full-text articles were evaluated. Of those records, 6 full-text primary articles were excluded from the review, and 7 were included. Reasons for exclusion included participants aged <18 y, evaluation of dietary Mg excluding blood serum Mg concentrations, and outcomes of interest excluding IR (Figure 1).
FIGURE 1.
PRISMA flow diagram.
Data analysis and outcome measures
A total of 7 primary articles were reviewed and included in this state-of-the-art review. The Academy of Nutrition and Dietetics Evidence Analysis quality criteria checklist was utilized to evaluate all included studies (34). The relation between serum Mg concentrations and IR was evaluated utilizing glycemic parameters including, but not limited to, insulin, fasting blood glucose (FBG), and HOMA-IR, among women with PCOS. A full summary can be found in Tables 3 and 4.
TABLE 3.
Summary of observational studies evaluating serum magnesium status among women with PCOS
| Author, year, study design | Study purpose | Study population | Intervention | Outcome data | Conclusions | Limitations of findings |
|---|---|---|---|---|---|---|
| Kauffman et al year: 2011study design: cross-sectional studycountry: USA funding source: nonequality grade: positive (+) | To determine if serum Mg concentrations correlate with IR, glucose intolerance, obesity, PCOS phenotype and other endocrine and metabolic parameters among women with PCOS | Premenopausal American women (n = 100)Aged: 18–42 yRecruitment: gynecology or re- productive endocrinology clinicsDx of PCOS: Rotterdam criteria | 100 women with PCOS were compared with 20 women without PCOS within the same age and weight range. Venous blood samples, were obtained between days 2 and 5 of the follicular phase postovernight fast. The follicular phase was not a variable for venous blood sample among women with prolonged amenorrhea | - Mg concentrations were similar between IR women and NIR women with PCOS (P = 0.34). - Mean serum Mg concentrations DM: 0.80 mmol/L; prediabetics: 0.85 mmol/L;euglycemic: 0.83 mmol/L, P = 0.13. - Mean serum Mg for both DM and euglycemic groups below the recommended Mg baseline concentration of 0.85 mmol/L (2.07 mg/dL) |
Mg concentrations were similar across PCOS phenotypes and were not significantly different from women without PCOS. Mg concentrations did not correspond to insulin sensitivity or glycemic concentrations in women with PCOS | - Limited demographics described. - 90% of women in study were anovulatory. - Small comparison group of 20 women |
| Chakraborty et al year: 2013study design: prospective cohort studycountry: Indiafunding source: unknownquality grade: positive (+) | To evaluate the serum concentrations of essential elements (Cu, Zn, Mg, Mn, Ca, and Cr) among IR and NIR women with PCOS | Premenopausal Indian women (n =132)Aged: <30 yRecruitment: outpatient infertility clinicDx of PCOS: Rotterdam criteria | Women with PCOS (n = 132) were stratified into 2 groups based upon IR. HOMA2-IR >2.1 were classified as IR. Group 1: IR with polycystic ovary morphology (n = 50) and Group 2: NIR (n = 82) and compared with control group (n = 46). Blood samples were collected between days 2 and 4 of the menstrual cycle at 09:00 h after an overnight fast | - PCOS vs. control fasting insulin (12.38 ± 0.83 vs. 8.12 ± 0.66, P < 0.004) concentrations and HOMA2-IR (2.21 ± 0.25 vs. 1.27 ± 0.37, P < 0.05). - IR PCOS vs. control serum Mg, P < 0.04. - Mg significantly correlated with fasting insulin concentrations in IR PCOS (r = −0.31; P < 0.03). - Mg of non-IR PCOS women similar to control, P > 0.05 |
There was association between serum elements, including Mg, and women with PCOS. Women with PCOS and IR are noted to have decreased serum Mg as well as higher Ca concentrations | - Limited demographics described. - Subjects were infertile for 5–10 y, which may pose systematic bias. - Stratified by IR; PCOS phenotype not evaluated |
| Rajeswari G et al year: 2016study design: case-control studycountry: Indiafunding source: unknownquality grade: neutral (Ø) | To analyze and compare biochemical markers (FBG, magnesium, uric acid. and lipid profile) that may aid in the identification of women with PCOS who are at risk of metabolic syndrome | Premenopausal Indian women (n = 80)Aged: 18–40 yRecruitment: outpatient OBGYN clinicDx of PCOS: per gynecology department | Intervention: 80 women with PCOS were compared with 40 women without PCOS within the same age range. Venous blood was collected to analyze serum magnesium, uric acid, FBG, lipid profile | - PCOS vs. control FBG: 116.65 ± 11.15 vs. 89.10 ± 5.89, P = 0.0001. - PCOS vs. control serum Mg: 1.210 ± 0.239 vs. 2.087 ± 0.189, P = 0.0001. - Significant negative correlation between glucose and Mg (r = −0.412, P = 0.0001) |
Women with PCOS were noted with lower serum Mg concentrations and higher FBG than women without PCOS | - Limited health and demographics described. - Control subjects only matched by age. - Statistically significant difference between BMI of control and PCOS group; sample size needs to be larger to infer women with PCOS have a higher BMI. - Did not compare PCOS phenotypes |
| Kanafchian et al year: 2019study design: case-control studycountry: Iranfunding source: grant from Babol University of Medical Sciences, Iranquality grade: Positive (+) | To evaluate serum Cu, Mg, and TAC concentrations among women with PCOS as compared with the control group | Premenopausal Iranian women (n = 60)Aged: 20–40 yRecruitment: outpatient infertility and reproductive health centerDx of PCOS: Rotterdam criteria | Women with PCOS (n = 60) were stratified into 2 groups based upon IR (n = 36) vs. NIR (n = 24). HOMA-IR >2.5 and QUICKI ≤0.333% were classified as IR. PCOS groups were compared with control (n = 90). Blood samples were collected after an overnight fast | - Mg concentrations were similar between PCOS vs. control (1.84 mg/dL vs. 1.83 mg/dL, P = 0.322) with no difference between groups based upon IR (P = 0.190). - Both groups were below the recommended Mg baseline concentration of 2.07 mg/dL. - Negative correlation between Mg and FBG among IR vs. NIR women with PCOS (r = −0.509, P = 0.002), HOMA-IR (r = −0.449, P = 0.006) and a positive correlation between Mg and QUICKI (r = 0.480, P = 0.003). - TAC significantly lower among IR vs. NIR and the control (P = 0.000). |
The results indicate a correlation between Mg and IR among women with PCOS, with a negative correlation between Mg and TAC that may contribute to oxidative stress and IR | - Limited health and demographics described. - Control subjects only matched by age. - Small sample size. - No postadjustment for differences between baseline variables. - Did not compare PCOS phenotypes |
Ca, calcium; Cr, chromium; Cu, copper; DM, diabetes mellitus; Dx, diagnosis; FBG, fasting blood glucose; IR, insulin resistance; Mg, magnesium; Mn, manganese; NIR, noninsulin resistant; OBGYN, obstetrics and gynecology; PCOS, polycystic ovary syndrome; QUACKI, quantitative insulin sensitivity check index; TAC, total antioxidant capacity; Zn, zinc.
TABLE 4.
Summary of experimental trials evaluating supplemented Mg among women with PCOS
| Author, year, study design | Study purpose | Study population | Intervention | Outcome data | Conclusions | Limitations of findings |
|---|---|---|---|---|---|---|
| Muneyyirci-Delale et al year: 2013study design: RCTcountry: USAfunding source: unknownquality grade: positive (+) | To evaluate the effect of spironolactone, glucophage and magnesium on serum lipid profile, FFA concentrations and insulin sensitivity among women with PCOS | Premenopausal American women (n = 36)Aged: 18–42 yRecruitment: outpatient OBGYN clinicDx of PCOS: Rotterdam criteria | Group 1 (n = 14) 500 mg glucophage twice daily; Group 2 (n = 10) 400 mg magnesium oxide by mouth, twice daily; Group 3 (n = 12) 50 mg spironolactone twice daily x 12 wk. A glucose tolerance test with 75 g glucose load was performed at baseline and after treatment, collecting blood at 0, 1, and 2 h for insulin, glucose, FFA, and aldosterone. Subjects were asked not to change dietary habits or physical activity | - Mg supplementation did not significantly change weight, cholesterol, FFA, or insulin sensitivity. - The glucophage group significantly decreased BMI (33.3 ± 1.95 kg/m2 to 32.79 ± 1.95 kg/m2, P = 0.04). - The spironolactone group significantly decreased systolic blood pressure (P =0.04) and FFA concentrations (P < 0.03) with posttreatment basal aldosterone concentrations significantly increased (P < 0.001) |
While Mg supplementation did not result in significant improvements in the outcomes, supplementation may still be beneficial in the treatment of PCOS. However, future studies evaluating higher doses, longer durations, and potentially different preparations of magnesium are needed | -Very small sample size. - Lack of blinding. - Limited demographics described. - Lack of controls to assess FFA and aldosterone concentrations. - Only 20% of women in the study were anovulatory. - Phenotype not evaluated |
| Jamilian M et al year: 2017study design: RCTcountry: Iranfunding source: Grant from the Vice-chancellor for Research, AUMS, and Iran quality grade: positive (+) | To investigate the effects of Mg, Zn, Ca, and vitamin D supplementation on glycemic control and cardiometabolic risk markers among women with PCOS | Premenopausal Iranian women (n = 60)Aged: 18–40 yRecruitment: referral to the Research and Clinical Center for Infertility at the Kosar clinicDx of PCOS: Rotterdam criteria | Subjects were matched for BMI, age, and phenotypes of PCOS and then were randomly assigned into 2 groups to receive100 mg Mg, 4 mg Zn, 400 mg Ca plus 200 IU vitamin D (n = 30) or placebo (n = 30) twice daily x 12 wk. All consumed metformin tablet at the initial dose of 500 mg, which was increased in increments of 500 mg to 1500 mg/d x first 3 wk. All were advised to maintain their routine habits, 3-d food records and 3 physical activity records at weeks 0, 3, 6, 9, and 12 | Supplement vs. placebo: - Significantly increased serum Mg (+0.1 ± 0.1 vs. −0.1 ± 0.3 mg/dL, P = 0.002). - Significant decreased serum insulin concentrations (–1.9 ± 4.6 vs. +0.4 ± 2.8μIU/mL, P = 0.01), and HOMA-IR (-0.4 ± 1.0 vs. +0.1 ± 0.6, P = 0.02). - Significantly increased QUICKI (+0.01 ± 0.02 vs. −0.0003 ± 0.01, P = 0.02). - Significant difference in baseline FPG (P = 0.03), Mg (P < 0.001) and Ca (0.005). - Postadjustment of baseline variables, insulin (P = 0.10), HOMA-IR (P = 0.08) and QUICKI (P = 0.08) between groups were no longer significant |
Mg-Zn-Ca-vitamin D cosupplementation over 12 wk may have a beneficial effect on insulin metabolism and cardiometabolic risk, however, further investigation with comparisons of similar baseline controls are needed to confirm results | - Need for single supplementation of each compared with cosupplementation.- Baseline values of biochemical variables between placebo and intervention group significantly different. - Relatively small amount of Mg supplemented (100 mg/d). - Limited demographics described |
| Jamilian M et al year: 2019study design: RCTcountry: Iranfunding source: Grant from the Vice-chancellor for Research, AUMS, and Iranquality grade: Positive (+) | To investigate the effect of Mg and vitamin E cosupplementation on metabolic profiles of women with PCOS | Premenopausal Iranian women (n = 60)Aged: 18–40 yRecruitment: patients of the Clinical Center for Infertility at the Kossar clinicDx of PCOS: Rotterdam criteria | Subjects were randomly selected into 2 groups via computer; intervention 250 mg/d Mg plus 400 mg/d vitamin E (n = 30) or placebo (n = 30) x 12 wk. All participantscompleted 3-day food records and 3 physical activity records at weeks 0, 3, 6, 9, and 12 | Adjusted values supplementation vs. placebo: - Significantly reduced serum insulin concentrations (-1.0 ± 0.5 vs. 1.5 ± 0.5 μIU/mL, P = 0.002) and HOMA-IR (-0.2 ± 0.1 vs. 0.4 ± 0.1, P = 0.001). - Significantly increased QUICKI (0.003 ± 0.003 vs. −0.008 ± 0.003, P = 0.002). - Both groups were below the recommended Mg concentration of 2.07 mg/dL at baseline. - Posttrial, the cosupplementation group had serum Mg concentrations at 2.14 ± 0.8 mg/dL with a total change of (+0.09 ± 0.14) |
Mg and vitamin E cosupplementation over 12 wk among women with PCOS improves insulin metabolism but does not affect FPG concentrations | - Short duration. - Small sample size. - Need for single supplementation of each compared with cosupplementation. - Limited demographics described |
Ca, calcium; Dx, diagnosis; FFA, free fatty acid; FPG, fasting plasma glucose; Mg, magnesium; OBGYN, obstetrics and gynecology; PCOS, polycystic ovary syndrome; QUACKI, quantitative insulin sensitivity check index; RCT, randomized controlled trial; Zn, zinc.
Results
Of the 7 primary articles reviewed, 4 were epidemiological analytic studies that evaluated serum Mg status among women with PCOS compared with a control group (Table 3). The other 3 studies were randomized controlled trials (RCTs) evaluating Mg supplementation compared with a placebo group among women with PCOS (Table 4).
PCOS and serum Mg status
In the positively rated, 2011 cross-sectional study by Kauffman et al. researchers aimed to determine if serum Mg concentrations correlate with IR, glucose intolerance, obesity, PCOS phenotype, and other endocrine and metabolic parameters among women with PCOS (35). Premenopausal American women (n = 100) with PCOS were compared with women (n = 20) without PCOS within the same age and weight range (35). Except among women with prolonged amenorrhea, venous blood samples were obtained between days 2 and 5 of the follicular phase post overnight fast (35). For women with prolonged amenorrhea, the follicular phase was not taken into consideration for the venous blood draw (35). Mg concentrations were similar among women with IR + PCOS when compared with women with noninsulin resistant (NIR) + PCOS (0.82 mmol/L compared with 0.83 mmol/L, P = 0.34); however, both concentrations were below the recommended normal reference range (35). When comparing Mg concentrations to BMI status, no difference was found between the groups (P = 0.15). Participants with both DM + PCOS had a mean Mg concentration of 0.80 mmol/L, women classified as prediabetic had a mean Mg concentration of 0.85 mmol/L, and women with normal glucose concentrations had a mean Mg concentration of 0.83 mmol/L, thus there was no difference between groups (P = 0.13) (35). Mg concentrations were similar across all PCOS phenotypes and were not significantly different when compared with women without PCOS (35). Researchers concluded Mg concentrations do not correspond to insulin sensitivity or glycemic control in women with PCOS (35). Although researchers considered PCOS phenotype and the control was matched based upon age and weight, 90% of the women in the study were anovulatory and the comparison group was of small sample size (35).
Conversely, Chakraborty et al. completed a positively rated, prospective cohort study in 2013 (36). The researchers examined serum concentrations of essential elements, including copper (Cu), zinc (Zn), Mg, manganese (Mn), Ca, and chromium (Cr), among insulin resistant and NIR women with PCOS (36). Premenopausal Indian women with PCOS (n = 132) were separated into 2 groups, IR (n = 50) compared with NIR (n = 82) and compared to women (n = 46) of similar age and BMI who presented without a diagnosis of PCOS (36). Women with a HOMA2-IR >2.1 were classified as insulin resistant (36). Blood samples were collected between the second and fourth day of the menstrual cycles at 09:00 h, after an overnight fast (36). Fasting insulin (12.38 ± 0.83 compared with 8.12 ± 0.66 μIU/mL, P <0.004) concentrations and HOMA2-IR (2.21 ± 0.25 compared with 1.27 ± 0.37, P < 0.05) were significantly higher among women with PCOS compared with the control group (36). Women with IR + PCOS, when compared with the control group, had significantly lower concentrations of serum Mg (P < 0.04), whereas Mg concentrations among women with NIR + PCOS were similar to the control (P > 0.05) (raw data for Mg concentrations using mg/dL or mmol/L was not provided) (36). Researchers noted Mg to be significantly correlated with fasting insulin concentrations among women with IR + PCOS (r = −0.31; P < 0.03) (36). The authors concluded a possible association between serum elements and IR, including Mg, in women with PCOS (36). Furthermore, women with IR + PCOS had decreased Mg concentrations (36). Although the sample size was large and compared IR and NIR women with PCOS to the control sample, there were a few limitations (36). The subjects were infertile for 5–10 y and PCOS phenotype was not evaluated (36). Potential confounding factors, including dietary supplementation and diet, were not addressed (36).
Similarly, Rajeswari et al. completed a neutral rated, prospective case-control study in 2016 (37). The researchers aimed to analyze biochemical parameters including FBG and serum Mg among women with PCOS (37). Premenopausal Indian women (n = 80) with PCOS were compared with Indian women (n = 40) without PCOS within the same age range (37). The study found significantly higher FBG concentrations in women with PCOS than the control (116.65 ± 11.15 compared with 89.10 ± 5.89 mg/dL, P = 0.0001), with a significantly lower serum Mg among women with PCOS than the control (1.210 mg/dL ± 0.239 compared with 2.087 mg/dL ± 0.189, P = 0.0001) (37). The serum Mg concentrations among women with PCOS were below the recommend normal reference range, whereas the control group was within the normal reference range (37). There was also a significant negative correlation between glucose and Mg (r = −0.412, P = 0.0001) (37). The researchers concluded women with PCOS present with lower serum Mg concentrations and higher FBG than women without PCOS. Limitations of the study included matching by age without consideration of weight or PCOS phenotypes and a small sample size (37). Furthermore, the authors did not adjust for potential confounders such as diet or supplementation (37).
Conversely, Kanafchian et al. completed a positively rated, case-control study in 2019 (38). The researchers evaluated serum copper (Cu), Mg, and total antioxidant capacity (TAC) concentrations in addition to biochemical glycemic parameters, among women with PCOS (38). Premenopausal Iranian women with PCOS (n = 60) were stratified into 2 groups based upon IR (n = 36) compared with NIR (n = 24) and compared Iranian women (n = 90) without PCOS of similar age (38). The study found Mg concentrations were similar between PCOS compared with the control (P = 0.322) with no difference between groups based upon IR (P = 0.190) (38). However, when the IR + PCOS group was compared with the NIR + PCOS group, researchers found a negative correlation between Mg and FBG (r = −0.509, P = 0.002), HOMA-IR (r = −0.449, P = 0.006), and a positive correlation between Mg and the quantitative insulin sensitivity check index (QUICKI) (r = 0.480, P = 0.003) (38). Additionally, TAC was significantly lower among women with IR + PCOS compared with NIR + PCOS and the control (P < 0.001) (38). The researchers indicated a correlation between Mg and IR among women with PCOS, with a negative correlation between Mg and TAC that may contribute to oxidative stress and IR (38). Limitations of the study included matching by age without consideration of weight or PCOS phenotypes, a relatively small sample size, and no adjustments for potential confounders such as diet or other baseline variables (38).
Out of the 4 studies evaluating serum Mg concentrations and glycemic control, only 2 (36, 37) studies found women with PCOS to have significantly lower Mg concentrations when compared with women without PCOS. In Rajeswari et al. (37), women with PCOS had statistically and clinically lower serum Mg concentrations, at 1.210 mg/dL (0.497 mmol/L), a value below the normal range of 0.76 to 1.15 mmol/L (12). Chakraborty et al. also found women with IR + PCOS to have a lower concentration of Mg when compared with the control group and women with NIR + PCOS (36). Kanafchian et al. did not find a statistically significant difference of serum Mg concentrations between the groups, however, they did note women with IR + PCOS had a negative correlation between Mg and FBG and HOMA-IR with a positive correlation between Mg and QUICKI (38). Finally, Kauffman et al. did not find statistically significant differences between the 2 groups, the women with IR + PCOS had a Mg concentration of 0.82 mmol/L (35). This finding may be of clinical significance as it is below 0.85 mmol/L, a proposed lower reference limit for individuals with impaired glucose control (12, 13). The results indicate women with IR + PCOS have a clinically significant lower serum Mg concentration than women with NIR + PCOS (35). The findings (35–38) suggest there may be a relation between serum Mg concentrations and IR among women with PCOS. Given this potential relation the supplementation of Mg may be beneficial in improving IR.
Effectiveness of Mg supplementation
In the positively rated 2013 randomized trial by Muneyyirci-Delale et al. researchers evaluated the effect of spironolactone, glucophage, and Mg on the serum lipid profile, free fatty acid (FFA) concentrations, and insulin sensitivity in women with PCOS (39). The researchers evaluated Mg oxide treatment compared with traditional medications as previous studies have indicated a low serum Mg status among women with PCOS (39). Premenopausal American women (n = 36) were randomly assigned to 1 of 3 groups: Group 1 (n = 14) 500 mg glucophage; Group 2 (n = 10) 400 mg Mg; Group 3 (n = 12) 50 mg spironolactone (39). All participants consumed the medication or supplement twice daily by mouth for 12 wk (39). A glucose tolerance test using a 75 g glucose load was performed at baseline and after treatment, collecting blood at 0, 1, and 2 h for insulin, glucose, FFA, and aldosterone determination (39). The subjects were asked to keep dietary habits and physical activity consistent for the duration of the study (39). Posttreatment, researchers found spironolactone to significantly decrease FFA concentrations (P < 0.3) and systolic blood pressure (P = 0.04) as well as significantly increase aldosterone concentrations (P < 0.001) (39). The glucophage group had a significantly decreased BMI (P < 0.04) (39). However, Mg supplementation did not significantly change baseline weight, cholesterol, FFA, or insulin sensitivity among participants (P > 0.05) when compared posttreatment (39). Although researchers noted Mg supplementation did not produce significant outcomes, the researchers did not evaluate baseline serum Mg among participants (39). This limitation, as well as the small sample size and relatively short duration of the study may also play a role in the outcome (39). Furthermore, the Mg supplementation was above the UL, however, no adverse events were reported (39). Mg may still be beneficial in the treatment of PCOS and future studies evaluating higher doses, longer durations, and potentially different preparations of Mg are needed (39).
In a 2017 positively rated, double-blind RCT, Jamilian et al. investigated the effects of Mg, Zn, Ca, and vitamin D supplementation on glycemic control (40). Premenopausal Iranian women (n = 60) were matched using BMI, age, and PCOS phenotype and randomly assigned into 2 groups: placebo or intervention to receive 100 mg Mg, 4 mg Zn, 400 mg Ca, and 200 IU vitamin D for 12 wk (40). Both the control group and the intervention group were prescribed metformin, starting with an initial dose of 500 mg, which was increased by 500 mg each week until reaching the target amount of 1500 mg/d (40). Participants were advised to maintain normal habits and track 3-d dietary and physical activity records at weeks 0, 3, 6, 9, and 12 (40). Upon completion of the 12-wk trial, the supplemented group, when compared with the placebo group, had significantly increased serum Mg concentrations (+0.1 ± 0.1 compared with −0.1 ± 0.3 mg/dL, P = 0.002) (40). The supplemented group compared with the placebo group also had a significant reduction in serum insulin concentrations (–1.9 ± 4.6 compared with +0.4 ± 2.8 μIU/mL, P = 0.01) as well as HOMA-IR (–0.4 ± 1.0 compared with +0.1 ± 0.6, P = 0.02) and a significant increase in the QUICKI (+0.01 ± 0.02 compared with −0.0003 ± 0.01, P = 0.02) (40). However, there was a significant difference in baseline values between the 2 groups for fasting plasma glucose (FPG) (P = 0.03), Mg (P < 0.001), and Ca (P = 0.005) (40). After the adjustment of baseline values of biochemical variables, age, and baseline BMI, the difference in changes of insulin (P = 0.10), HOMA-IR (P = 0.08), and QUICKI (P = 0.08) between the 2 groups were no longer significant; however cardiometabolic parameters including total cholesterol and triglycerides remained significantly lower (P < 0.05) (40). Despite lacking significant differences after the adjustment of baseline values for glycemic parameters, the authors suggested that Mg-Zn-Ca-vitamin D cosupplementation over 12 wk in women with PCOS may still have an advantageous effect on insulin sensitivity and markers of cardiometabolic risk (40). The study, however, had some limitations as the researchers failed to show the data for baseline serum values and did not note if the values were below the normal target range (40). Furthermore, much of the baseline values between the 2 groups were significantly different (40). Finally, since the intervention was a cosupplement, it is difficult to determine which, if any, of the nutrients may have exerted any beneficial effects (40).
Most recently, Jamilian et al. (2019), evaluated Mg and vitamin E cosupplementation on metabolic profiles of women with PCOS, in another positively rated, double-blind RCT (41). Subjects were randomly assigned into 2 groups via computer; the intervention group, receiving 250 mg/d Mg plus 400 mg/d vitamin E (n = 30) or the placebo group, receiving a similar shape and size capsule (n = 30) over 12 wk (41). All participants completed a 3-d food record with 3 physical activity records at weeks 0, 3, 6, 9, and 12 (41). Upon completion of the 12 wk study and after results were adjusted for baseline values, age, and BMI, the supplementation group compared with placebo had significantly reduced serum insulin concentrations (–1.0 ± 0.5 compared with 1.5 ± 0.5 μIU/mL, P = 0.002) and HOMA-IR (–0.2 ± 0.1 compared with 0.4 ± 0.1, P = 0.001), with significantly increased QUICKI (0.003 ± 0.003 compared with −0.008 ± 0.003, P = 0.002) (41). The researchers concluded the Mg and vitamin E cosupplementation over 12 wk among women with PCOS improved markers of cardiometabolic risk with a nonsignificant trend towards improved insulin sensitivity (41). Some limitations of the study included the duration and small sample size as well as the cosupplement invention, which similar to the previous study, remains unclear whether one single supplement improved the noted markers of IR or if improvement was due to the cosupplementation (41).
The effects of Mg supplementation among women with PCOS remain unclear. So far, only 3 RCTs (39–41) have evaluated the effects of Mg supplementation on glycemic control among women with PCOS. Although numerous studies have noted improved glycemic control with Mg supplementation among other populations, including type 2 diabetes (42) and gestational diabetes (43), current research has failed to associate Mg supplementation with significant glycemic improvements among women with PCOS (39). Whereas Jamilian et al. (2017 and 2019) found cosupplementation containing Mg significantly increased serum Mg concentrations (P = 0.002) (40, 41), only the cosupplementation of Mg and vitamin E has been noted to have a statistically significant effect on IR after adjusting for baseline values (41). However, despite not having statistical significance, the cosupplementation of Mg, Zn, Ca, and vitamin D, after adjusting for baseline values, actually resulted in a greater change in insulin (−1.6 ± 0.7 μIU/mL) (40) when compared with the statistically significant decrease in insulin (−1.0 ± 0.5 μIU/mL) with the Mg and vitamin E cosupplement over 12 wk (41).
Limitations
It is unclear if the association between IR and Mg supplementation is dose dependent, or rather, if IR is impacted by Mg deficiency. Furthermore, research has produced clinically significant results with the use of cosupplementation (40, 41) as well as a diet rich in Mg (33). Within the observational studies, only a few considered confounding variables such as supplemented Mg. One study failed to evaluate dietary supplementation (37), whereas others use supplementation exclusion criteria, but only if the supplement had been consumed 2 (36) or 3 (35) mo prior to enrollment. Muneyyirci-Delale et al. noted subjects were instructed to maintain normal dietary habits (39), however, they failed to evaluate the macro- and micronutrients within the “normal” diet. These confounding variables may have influenced the overall outcomes. All 3 RCTs were of short duration (39–41), however, studies evaluating insulin sensitivity and glucose control among both diabetic and nondiabetic individuals without PCOS noted Mg supplementation for >4 mo significantly improved HOMA-IR and fasting glucose (25). Research indicates women with PCOS are more likely to underconsume Mg-rich foods (32, 33) and have a greater likelihood of lower serum Mg (36, 37) when compared with women without PCOS. In 1 study, Mg cosupplementation was associated with improved IR and markers of cardiometabolic risk among women with PCOS (40).
Future research, including RCTs of larger sample size and longer duration, is needed to evaluate the effectiveness of single supplementation versus cosupplementation as well as to determine the optimal duration and dosage of supplementation.
There are some limitations within the research, particularly with regards to assessing serum Mg. Most of the body's Mg is located inside cells or in bone, thus the serum concentration may not accurately depict true Mg status (11, 12). Currently, there is no gold standard to assess Mg status, however, for the most comprehensive analysis, both laboratory tests and clinical assessment might be required (11, 12). Furthermore, only 3 (35, 36, 39) out of the 7 studies excluded individuals on medications, including PPIs. This confounding variable is of importance because chronic PPI-induced hypomagnesemia does not respond to Mg supplementation with an increase in Mg serum concentrations (11, 12, 20). Additionally, the research has not consistently matched women with PCOS upon BMI, age, phenotype, anovulation, or IR. Furthermore, biochemical parameters for serum concentrations were not routinely captured at baseline (40). Finally, there are limitations when using fasting values including HOMA-IR and QUICKI to measure IR and insulin sensitivity among women with PCOS, as the results are highly variable (44). Assessment measures found to be more accurate for the determination of IR and insulin sensitivity include the oral-glucose-tolerance test (OGTT) (44) and the gold standard, the hyperinsulinemic euglycemic glucose clamp technique (45).
Applications to Practice
Mg is a cofactor for numerous biochemical reactions (11, 12). Current research indicates women with PCOS are more likely to underconsume Mg-rich foods (32, 33) and have a greater likelihood of lower serum Mg (36, 37). However, serum Mg may not be the most reliable criteria for assessing Mg status (11, 12) and as such the use of a nutrition-focused medical history with dietary analysis as well as a physical examination should be utilized when assessing the overall status of the patient. Although it is uncommon for an individual to have a symptomatic Mg deficiency due to low dietary intake, health conditions such as type 2 diabetes, gastrointestinal diabetes, chronic alcoholism, and medications, including PPIs and diuretics, may increase the likelihood of deficiency (12).
The clinician should evaluate for potential Mg deficiency via food- and nutrition-related history, reviewing sources of Mg, including legumes, leafy greens, potatoes, and quinoa. An assessment of medications and supplements, biochemical data, and physical findings should also be conducted. Excessive vitamin D supplementation, chronic diarrhea, fat malabsorption, and medications, particularly long-term use of PPIs, may increase the risk of Mg deficiency (11). Patients with mild Mg deficiency may have no significant signs or symptoms. However, symptoms of Mg deficiency may include a decreased appetite, nausea, vomiting, fatigue, and weakness (11, 12). With more severe deficiencies, individuals may experience numbness, tingling, muscle cramping, seizures, and changes in personality, as well as arrhythmia, coronary spasms, and hypocalcemia or hypokalemia (11, 12).
Finally, it appears dietary Mg may not be the only or best solution for improving glucose metabolism and insulin sensitivity among women with PCOS. Utilizing a nutrient-dense diet, such as the Dietary Approaches to Stop Hypertension (DASH) eating pattern (33) that is high in Mg, potassium (K), Ca, and low in sodium, is associated with improved health outcomes including CVD, DM, and metabolic syndrome (33). Micronutrients often underconsumed among women with PCOS include Mg, K, Ca, vitamin D, and folate (32, 33). Furthermore, lower serum concentrations of essential elements including Mg (35–37), Mn (36, 46), and Cr (36) are noted among women with PCOS when compared with women without PCOS. An individualized plan for the supplementation of micronutrients may be warranted for women who struggle to meet their micronutrient needs.
Conclusion
Women with PCOS are more likely to underconsume Mg-rich foods (32, 33) and have a greater likelihood of lower serum Mg concentrations (36, 37). The results of the observational studies indicate an association between Mg and IR among women with PCOS (35–38). It remains unclear whether adequate dietary Mg or supplementation improves insulin sensitivity among all women with PCOS, however, there is some evidence to suggest that improved IR can be obtained in women with PCOS as a result of Mg cosupplementation (39, 40). Dietary interventions and micronutrient supplementation may prove to be a viable treatment option for women seeking disease control without medication, however, more research is needed.
Although research has made great strides with regards to the evaluation and treatment of PCOS, the etiology, progression throughout the lifespan, spectrum of symptoms, and various morbidities still remain rather elusive. Furthermore, the true pathogenesis of disease is still unknown. Although unregulated steroidogenesis, IR, genetics, and oxidative stress likely play a role, additional studies are needed to better understand the disease in order to prevent comorbidities and treat PCOS. Larger studies of longer duration, evaluating both IR + PCOS compared with NIR + PCOS women and PCOS phenotypes are necessary. Moving forward, the relation between supplementation of micronutrients, particularly those consumed in lower quantities within this population, such as Mg, vitamin D, Ca, K, folate, and antioxidants, would also be of value. Although it remains unclear if dietary Mg and/or Mg supplementation should be a nutritional strategy encouraged for all women with PCOS, current research indicates an association between achieving adequate Mg status and improved IR.
Acknowledgements
The authors’ responsibilities were as follows—KPH, RZ, and ARP: were involved in the conception and design of the review article; KPH: drafted the article; all authors were involved in the critical revision of the article, and read and approved the final manuscript.
Notes
The authors reported no funding received for this review.
Author disclosures: KPH, RZ, ARP, and AH, no conflicts of interest.
Abbreviations used: Ca, calcium; Cr, chromium; Cu, copper; CVD, cardiovascular disease; DM, diabetes mellitus; Dx, diagnosis; FBG, fasting blood glucose; FFA, free fatty acid; FPG, fasting plasma glucose; GLUT-4, glucose transporter protein activity-4; IR, insulin resistance; K, potassium; Mg, magnesium; Mn, manganese; NIR, noninsulin resistant; OGBYN, obstetrics and gynecology; PCOS, polycystic ovary syndrome; PPI, proton pump inhibitor; QUICKI, quantitative insulin sensitivity check index; RCT, randomized controlled trial; TAC, total antioxidant capacity; UL, tolerable upper intake level; Zn, zinc.
References
- 1. Bozdag G, Mumusoglu S, Zengin D, Karabulut E, Yildiz BO. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod 2016;31(12):2841–55. [DOI] [PubMed] [Google Scholar]
- 2. Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E, American Association of Clinical Endocrinologists (AACE); American College of Endocrinology (ACE); Androgen Excess and PCOS Society (AES). American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society Disease State Clinical Review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome–Part 1. Endocr Pract 2015;21(11):1291–300. [DOI] [PubMed] [Google Scholar]
- 3. El Hayek S, Bitar L, Hamdar LH, Mirza FG, Daoud G. Polycystic ovarian syndrome: an updated overview. Front Physiol 2016;7:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rotterdam EA-SPCWG. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25. [DOI] [PubMed] [Google Scholar]
- 5. Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, Janssen OE, Legro RS, Norman RJ, Taylor AE et al.. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril 2009;91(2):456–88. [DOI] [PubMed] [Google Scholar]
- 6. Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, Welt CK, Endocrine Society. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2013;98(12):4565–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E, American Association of Clinical Endocrinologists (AACE); American College of Endocrinology (ACE); Androgen Excess and PCOS Society. American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society Disease State Clinical Review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome - part 2. Endocr Pract 2015;21(12):1415–26. [DOI] [PubMed] [Google Scholar]
- 8. Bednarska S, Siejka A.. The pathogenesis and treatment of polycystic ovary syndrome: what's new? Adv Clin Exp Med 2017;26(2):359–67. [DOI] [PubMed] [Google Scholar]
- 9. Ibanez L, Oberfield SE, Witchel SF, Auchus RJ, Chang RJ, Codner E, Dabadghao P, Darendeliler F, Elbarbary NS, Gambineri A et al.. An international consortium update: pathophysiology, diagnosis, and treatment of polycystic ovarian syndrome in adolescence. Horm Res Paediatr 2017;88(6):371–95. [DOI] [PubMed] [Google Scholar]
- 10. Rosenfield RL, Ehrmann DA.. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev 2016;37(5):467–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schwalfenberg GK, Genuis SJ.. The importance of magnesium in clinical healthcare. Scientifica (Cairo) 2017;2017:4179326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grober U, Schmidt J, Kisters K. Magnesium in prevention and therapy. Nutrients 2015;7(9):8199–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Elin RJ. Assessment of magnesium status for diagnosis and therapy. Magnes Res 2010;23(4):S194–8. [DOI] [PubMed] [Google Scholar]
- 14. Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, DC: National Academies Press; 1997. [PubMed] [Google Scholar]
- 15. Weiss D, Brunk DK, Goodman DA. Scottsdale magnesium study: absorption, cellular uptake, and clinical effectiveness of a timed-release magnesium supplement in a standard adult clinical population. J Am Coll Nutr 2018;37(4):316–27. [DOI] [PubMed] [Google Scholar]
- 16. Tarleton EK. Factors influencing magnesium consumption among adults in the United States. Nutr Rev 2018;76(7):526–38. [DOI] [PubMed] [Google Scholar]
- 17. Azoulay A, Garzon P, Eisenberg MJ. Comparison of the mineral content of tap water and bottled waters. J Gen Intern Med 2001;16(3):168–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cifelli CJ, Houchins JA, Demmer E, Fulgoni VL. Increasing plant based foods or dairy foods differentially affects nutrient intakes: dietary scenarios using NHANES 2007–2010. Nutrients 2016;8(7):E422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rosanoff A, Dai Q, Shapses SA. Essential nutrient interactions: does low or suboptimal magnesium status interact with vitamin D and/or calcium status? Adv Nutr 2016;7(1):25–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Florentin M, Elisaf MS. Proton pump inhibitor-induced hypomagnesemia: a new challenge. World J Nephrol 2012;1(6):151–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Morais JBS, Severo JS, de Alencar GRR, de Oliveira ARS, Cruz KJC, Marreiro DDN, Freitas BJESA, de Carvalho CMR, Martins MDCCE, Frota KMG. Effect of magnesium supplementation on insulin resistance in humans: a systematic review. Nutrition 2017;38:54–60. [DOI] [PubMed] [Google Scholar]
- 22. Hruby A, Meigs JB, O'Donnell CJ, Jacques PF, McKeown NM. Higher magnesium intake reduces risk of impaired glucose and insulin metabolism and progression from prediabetes to diabetes in middle-aged Americans. Diabetes Care 2014;37(2):419–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chutia H, Lynrah KG.. Association of serum magnesium deficiency with insulin resistance in type 2 diabetes mellitus. J Lab Physicians 2015;7(2):75–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sarrafzadegan N, Khosravi-Boroujeni H, Lotfizadeh M, Pourmogaddas A, Salehi-Abargouei A. Magnesium status and the metabolic syndrome: a systematic review and meta-analysis. Nutrition 2016;32(4):409–17. [DOI] [PubMed] [Google Scholar]
- 25. Simental-Mendia LE, Sahebkar A, Rodriguez-Moran M, Guerrero-Romero F. A systematic review and meta-analysis of randomized controlled trials on the effects of magnesium supplementation on insulin sensitivity and glucose control. Pharmacol Res 2016;111:272–82. [DOI] [PubMed] [Google Scholar]
- 26. Siklar Z, Berberoglu M, Camtosun E, Kocaay P. Diagnostic characteristics and metabolic risk factors of cases with polycystic ovary syndrome during adolescence. J Pediatr Adolesc Gynecol 2015;28(2):78–83. [DOI] [PubMed] [Google Scholar]
- 27. Yaribeygi H, Farrokhi FR, Butler AE, Sahebkar A. Insulin resistance: review of the underlying molecular mechanisms. J Cell Physiol 2019;234(6):8152–61. [DOI] [PubMed] [Google Scholar]
- 28. Gommers LM, Hoenderop JG, Bindels RJ, de Baaij JH. Hypomagnesemia in type 2 diabetes: a vicious circle? Diabetes 2016;65(1):3–13. [DOI] [PubMed] [Google Scholar]
- 29. Kostov K. Effects of magnesium deficiency on mechanisms of insulin resistance in type 2 diabetes: focusing on the processes of insulin secretion and signaling. Int J Mol Sci 2019;20(6):E1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Von Ehrlich E, Barbagallo M, Classen HG, Guerrero-Romero F, Morren FC, Rodriguez-Moran M, Vierling W, Vormann J, Kisters K. The significance of magnesium in insulin resistance, metabolic syndrome, and diabetes–recommendations of the Association of Magnesium Research. Diabetol Stoffwechs 2014;9:96–100. [Google Scholar]
- 31. Chaudhary DP, Sharma R, Bansal DD.. Implications of magnesium deficiency in type 2 diabetes: a review. Biol Trace Elem Res 2010;134(2):119–29. [DOI] [PubMed] [Google Scholar]
- 32. Szczuko M, Skowronek M, Zapalowska-Chwyc M, Starczewski A. Quantitative assessment of nutrition in patients with polycystic ovary syndrome (PCOS). Rocz Panstw Zakl Hig 2016;67(4):419–26. [PubMed] [Google Scholar]
- 33. Asemi Z, Esmaillzadeh A. DASH diet, insulin resistance, and serum hs-CRP in polycystic ovary syndrome: a randomized controlled clinical trial. Horm Metab Res 2015;47(3):232–8. [DOI] [PubMed] [Google Scholar]
- 34. Evidence Analysis Manual: Steps in the Academy Evidence Analysis Process April 2016. [Available from: www.andeal.org].
- 35. Kauffman RP, Tullar PE, Nipp RD, Castracane VD. Serum magnesium concentrations and metabolic variables in polycystic ovary syndrome. Acta Obstet Gynecol Scand 2011;90(5):452–8. [DOI] [PubMed] [Google Scholar]
- 36. Chakraborty P, Ghosh S, Goswami SK, Kabir SN, Chakravarty B, Jana K. Altered trace mineral milieu might play an aetiological role in the pathogenesis of polycystic ovary syndrome. Biol Trace Elem Res 2013;152(1):9–15. [DOI] [PubMed] [Google Scholar]
- 37. Rajeswari G GP, Veerabhadrudu B, Suresh E. Study of magnesium levels in polycystic ovarian syndrome. Int J App Res 2016;2(3):610–3. [Google Scholar]
- 38. Kanafchian M, Esmaeilzadeh S, Mahjoub S, Rahsepar M, Ghasemi M. Status of serum copper, magnesium, and total antioxidant capacity in patients with polycystic ovary syndrome. Biol Trace Elem Res 2019[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 39. Muneyyirci-Delale O, Kaplan J, Joulak I, Yang L, Von Gizycki H, Nacharaju VL. Serum free fatty acid levels in PCOS patients treated with glucophage, magnesium oxide and spironolactone. Gynecol Endocrinol 2013;29(5):474–7. [DOI] [PubMed] [Google Scholar]
- 40. Jamilian M, Maktabi M, Asemi Z. A trial on the effects of magnesium-zinc-calcium-vitamin D co-supplementation on glycemic control and markers of cardio-metabolic risk in women with polycystic ovary syndrome. Arch Iran Med 2017;20(10):640–5. [PubMed] [Google Scholar]
- 41. Jamilian M, Sabzevar NK, Asemi Z. The effect of magnesium and vitamin E co-supplementation on glycemic control and markers of cardio-metabolic risk in women with polycystic ovary syndrome: a randomized, double-blind, placebo-controlled trial. Horm Metab Res 2019;51(2):100–5. [DOI] [PubMed] [Google Scholar]
- 42. Veronese N, Watutantrige-Fernando S, Luchini C, Solmi M, Sartore G, Sergi G, Manzato E, Barbagallo M, Stubbs B. Effect of magnesium supplementation on glucose metabolism in people with or at risk of diabetes: a systematic review and meta-analysis of double-blind randomized controlled trials. Eur J Clin Nutr 2016;70(12):1463. [DOI] [PubMed] [Google Scholar]
- 43. Asemi Z, Karamali M, Jamilian M, Foroozanfard F, Bahmani F, Heidarzadeh Z, Esmailzadeh A. Magnesium supplementation affects metabolic status and pregnancy outcomes in gestational diabetes: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr 2015;102(1):222–9. [DOI] [PubMed] [Google Scholar]
- 44. Lewandowski KC, Plusajska J, Horzelski W, Bieniek E, Lewinski A. Limitations of insulin resistance assessment in polycystic ovary syndrome. Endocr Connect 2018;7(3):403–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Polak K, Czyzyk A, Simoncini T, Meczekalski B. New markers of insulin resistance in polycystic ovary syndrome. J Endocrinol Invest 2017;40(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kurdoglu Z, Kurdoglu M, Demir H, Sahin HG. Serum trace elements and heavy metals in polycystic ovary syndrome. Hum Exp Toxicol 2012;31(5):452–6. [DOI] [PubMed] [Google Scholar]