Abstract
Background:
Social determinants of health (SDoH) are socioeconomic factors that influence health outcomes. Guidelines recommend universal screening for SDoH at clinic visits, however, models that do not require additional resources are limited in subspecialty clinics. Individuals with sickle cell disease (SCD) face the burdens of chronic illness and often racial disparities, both of which may increase their vulnerability to adverse SDoH. Hematologists can impact both quality of life and clinical outcomes for their patients by implementing screening and referral programs addressing SDoH.
Methods:
Through prospective, quality improvement methods, we introduced universal screening for SDoH into our pediatric hematology clinic. The intervention was a paper screener followed by a referral to local community organizations for the specific needs endorsed. The aims of this study were to determine the feasibility of universal screening for SDoH in a busy subspeciality clinic using pre-existing resources, to identify the needs of our patients, and to facilitate referrals between our patients and community organizations via this low touch intervention.
Results:
Between August, 2017 and November, 2018, 156 screens were completed. Sixty-six percent were positive for at least one unmet social need for which 80% were referred to a relevant community organization. Forty-five percent of patients available via follow-up phone call reached out to the community organization.
Conclusions:
There is a high burden of SDoH in families of children with SCD. Universal screening in a pediatric hematology clinic with the subsequent connection of patients with SCD to community resources is feasible using existing clinic resources.
Keywords: Social determinants of health, sickle cell disease, poverty screening, health services, quality improvement
Introduction
Social determinants of health (SDoH) are socioeconomic factors that influence health and well-being.1 The World Health Organization identifies SDoH as “mostly responsible for health inequities – the unfair and avoidable differences in health status - seen within and between countries.”2 As examples, inadequate housing, food, and access to affordable medications are associated with lower quality of life, poor mental health, and worse outcomes from chronic medical illnesses.3–5 In the United States, SDoH are estimated to influence overall health outcomes more than medical care provided.6
The American College of Physicians and the American Academy of Pediatrics (AAP) recommend universal screening for SDoH to connect families with local resources.7,8, 9 In a randomized control trial, the Well Child Care, Evaluation, Community Resources, Advocacy, Referral, Education (WECARE) system utilized a self-reported screening tool for SDoH to connect families with local community organizations that address the specific socioeconomic need identified. This system resulted in a nearly 9-fold increase in referrals to community resources.10
The pediatric oncology community has also adopted screening for financial hardship as one of fifteen priority standards for the psychosocial care of children with cancer. The recommendations include an assessment of risk for financial hardship at time of diagnosis, targeted referral for financial counseling and supportive resources from governmental or charitable sources, and longitudinal reassessment and intervention throughout the clinical course.11 Feasibility has been demonstrated in pediatric oncology practices.12
While the health of all children is influenced by SDoH, patients with chronic illnesses, such as those with sickle cell disease (SCD), may be more affected. SCD is a red blood cell disorder that causes severe pain, increased risk of life-threatening infections, strokes, and early death.13 Of more than 100,000 Americans with SCD, the majority are African-American or from another racial minority background.14 In the United States, where a history of structural injustice has created concentrated cycles of poverty among racial and ethnic minorities, poverty disproportionately affects the same population as does SCD.15 The dual burdens of a chronic disease and racial inequity increase this population’s vulnerability to SDoH. Poverty in children with SCD is associated not only with lower quality of life, but also with higher healthcare utilization.16,17 Public health insurance, which is both a proxy for poverty and also has a causal link in health outcomes, has been associated with higher complication rates in youth with SCD.18
Although the psychosocial standards mentioned above are endorsed by the American Society of Pediatric Hematology/Oncology and the Association of Pediatric Hematology/Oncology Nurses regarding oncologic care, there are no recommended psychosocial guidelines for the care of pediatric hematology patients, and there are no published attempts to determine the feasibility of universal screening for SDoH in hematology clinics serving children or adults with SCD.
Despite an awareness of the detriments of poverty among patients with SCD, there are no published attempts to establish universal screening for SDoH in a clinic serving children with SCD. Therefore, we sought to emulate the systems developed in primary care and pediatric oncology clinics to improve the support provided to our patients via quality improvement (QI) methods. The aim of our initiative was to determine the feasibility of integrating universal screening for SDoH for patients with SCD into routine clinic flow using existing resources by screening 85% of eligible clinic patients per month. Secondarily, we sought to identify the socioeconomic needs of our patients and to facilitate referrals to community organizations via this low-touch intervention.
Materials and Methods
Setting/Population:
This QI initiative was implemented between August, 2017 and November, 2018 in the pediatric hematology clinic at BMC. BMC is an academic, urban, safety net hospital. Seventy-two percent of the hospital’s patients have public health insurance.19 The pediatric hematology clinic follows approximately 200 patients with SCD under 21 years of age.
A social worker provides psychosocial support for patients with SCD in the clinic, the emergency department, or the inpatient wards. At baseline, she met with patients for adjustment to diagnosis, management of chronic illness, and for socioeconomic needs if they were identified during the hematologist or social work visit. A patient navigator also helped families enroll in certain supports, specifically utility shutoff protection, the Massachusetts Medicaid transportation program, and BMC’s food pantry. Prior to this initiative, there was no systematic screening for SDoH in our hematology clinic; beyond the resources identified above, there was no database of resources to which our patients could be referred, and there was no streamlined process for making these referrals during the clinic visit.
Intervention
Screening:
We screened with WECARE, a one-page, self-reported questionnaire that was previously validated in BMC’s pediatric primary care network. The domains of SDoH screened for are adequate housing, food, employment, childcare, education, utilities, transportation to the hospital, and ability to pay for medications (Table 1). It was initially offered once every 3 months at non-sick visits and distributed by the physician or social worker. To identify patients with SCD who were due, the administrative coordinator initially tracked patients and noted on the electronic schedule that they needed a screener. The screening was offered in English, Spanish, Haitian Creole, and, in instances of low literacy, clinic staff read the screener to families. Families were given the option to decline the screener.
TABLE 1:
Screener for social determinants of health
| Housing | Do you currently live in a shelter or have no steady place to sleep at night? | Yes/No |
| Do you think you are at risk of becoming homeless? | Yes/No | |
| If yes, is this an emergency? | Yes/No | |
| Food | Within the past 12 months, the food you bought didn’t last and you didn’t have money to get more. | Often true/sometimes true/never true |
| Within the past 12 months, you worried whether your food would run out before you got money to buy more. | Often true/sometimes true/never true | |
| Is this an emergency? Do you need food for tonight? | Yes/No | |
| Medication | Do you have trouble paying for medicines? | Yes/No |
| Transportation | Do you have trouble getting transportation to medical appointments? | Yes/No |
| Utilities | Do you have trouble paying your heating or electricity bill? | Yes/No |
| If yes, are you at risk of having your utilities shut off in the next week? | Yes/No | |
| Daycare | Do you have trouble taking care of a child, family member, or friend? | Yes/No |
| Employment | Are you currently unemployed and looking for a job? | Yes/No |
| Education | Are you interested in more education? | Yes/No |
| Would you like help connecting to resources? Please circle below | |||
| Housing/shelter | Food | Paying for medication | Transportation to medical appointments |
| Utilities | Daycare | Job search/training | Education |
Referral:
A patient who reported a need or requested assistance for a need screened positive and subsequently was referred to a corresponding, local community organization aimed at addressing the specific needs (Example in Supplemental text Figure 3). The provider made the referral by inserting pre-existing ‘smart text’ phrases into the after-visit summary. Providers and patients decided if these families also needed to meet with the social worker. Certain questions asked if the family was in imminent need of assistance, in which case families were both given resources and scheduled with the social worker.
Aims:
Our specific aims were that 85% of children due for SDoH screening each month would have a screener documented in the medical record, and that 100% of patients with positive screens would be given a relevant resource sheet.
PDSA Methodology
Plan-do-study-act (PDSA) cycles were used to determine the most efficient way to introduce this screening into our clinic flow. In this QI framework, barriers are identified, changes are implemented, and the effects are monitored in a cyclic manner in order to improve a process.20
Our PDSA cycles were largely processed-focused, aiming to maximize the efficiency of screener distribution and documentation and of referral to resources. Examples of questions addressed in PDSA cycles included who distributed and recorded the screener, the frequency of screener distribution, which patients would be due for screening, and which socioeconomic needs were assessed (Table 2).
TABLE 2:
Plan-Do-Study-Act cycles
| Distribution of screener: Sept-Nov, 2017 | |
| Plan | Screeners were initially distributed by the hematologist or social worker depending on who saw the patient first. The perception of this strategy was that it was disruptive to clinic flow and did not allow patients enough time to complete the survey; therefore, we wanted to shift this task to the clinical assistants during rooming of the patient. |
| Do | A meeting was held with clinic staff to explain the importance of screening for social determinants of health, as well as the need for universal screening. A clinic flow diagram was created and available on the back of each paper screener to remind staff of the new flow with space to provide feedback on the process (Supplemental Figure 4A) |
| Study | Number of surveys distributed was the main outcome measure with no change or increased distribution being considered a successful transition. Feedback from clinicians and clinical assistants was elicited at meetings and via free text areas on the clinical flow diagram without any reported dissatisfaction or notable delays. Our additional balancing measure was the proportion of positive screens with a resultant resource sheet. |
| Act | After this PDSA cycle, clinical assistants were primarily responsible for survey distribution. |
| Timing of Screening: January, 2018 | |
| Plan | Because subspecialty care does not occur at pre-determined intervals the way that primary well child care does, the screening intervals did not have a natural pattern. We initially set out to screen families every three months because in our patient population socioeconomic needs, such as employment and housing can change rapidly. Many families, however, verbalized that screening every 3 months was too frequent. |
| Do | Screening was spaced to every 6 months. |
| Study | Proportions of surveys completed out of those that were due continued to be tracked. Clinical assistants felt positively about this change at staff meetings, and the social worker did not note any increase in unmet emergent needs. |
| Identification of patients due for screening, September, 2018 | |
| Plan | Initially, the administrative coordinator tracked screening of patients with SCD and designated that they were due every 3–6 months in the electronic schedule. |
| Do | To further reduce the administrative burden and to streamline the clinic flow, it was decided to distribute screening at all non-sick or non-urgent appointments. Clinic staff were updated during staff meetings and the clinic flow diagram was updated. |
| Study | The number of screeners documented in the EMR per patient with SCD per clinic visit was recorded, so the denominator of this process measure was adjusted. |
| Act | All patients with SCD are offered a screener at every non-sick or non-urgent care visit. |
| Documentation of screener results, September-November, 2018 | |
| Plan | Clinical assistants across the hospital had been trained to document a housing screener. Therefore, the clinic agreed that this should continue to be their role. |
| Do | When the clinic resumed the full SDoH screen, we designated it as the clinical assistants’ task to document the screener in the EMR. |
| Study | Process measures and balancing measures continued to be tracked. There was a sharp decline in distribution of resource referrals when providers were no longer recording the screener into the EMR themselves. This was reviewed and providers were reminded to review the flowsheets. Clinical assistants were also asked to page the social workers if there was a positive result. Clinical assistants reported some occasional lack of clarity in the process, but overall agreed with the change. |
| Act | Clinical assistants record screener results into the EMR and page SW for a positive screen. Physicians review all screening results in EMR. |
| Socioeconomic needs screened for: September-October, 2017 | |
| Plan | The initial screener was based on the WECARE screener that asked six questions. The primary care clinic at our hospital updated their screener to ask about ability to pay for medications and transportation to clinic. When considering adopting this change as well, we returned to our main criteria to guide which socioeconomic need to include which was that there was an available resource to address that need; this exists for these two questions. Patients with Massachusetts Medicaid and certain chronic medical conditions, including sickle cell disease, qualify for transportation to clinic visits and should have the majority of their medications covered. Prior to introducing WECARE, our clinic had been proactively setting up this transportation assistance for many families, particularly because many families in Boston do not have cars and the exposure to the cold winter while waiting for the bus can be detrimental to our patients. |
| Do | We adopted the updated screener and notified staff to discard the older version (which was printed on yellow rather than blue paper). |
| Study | This change was made relatively early in our study and changes in enrollment in transportation assistance were not tracked; however, there was no associated disruption in clinic flow with the addition of these questions reported on our clinical diagram or in clinical meetings. |
| Act | The 8-question screener was adopted. |
Measures:
During our PDSA cycles, we primarily tracked process measures, including the percentage of patients due who had a screener documented in their EMR and the percentage of patients who screened positive who received a referral in their AVS. We also tracked outcome measures- percentage of patients who screened positive who had connected with a community resource, and balancing measures-staff, patient, and provider satisfaction, including delays in work flow. Baseline clinic flow was diagramed and updated to reflect changes for tracking purposes, assessment of clinic flow, and staff education (Supplemental text Figure 4). Run charts were reviewed weekly at first and then monthly to inform further tests of change (Figure 1).
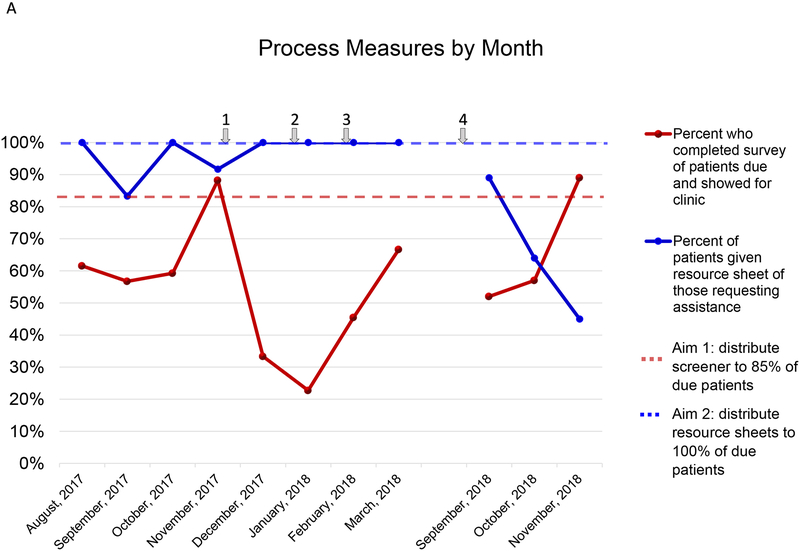
FIGURE 1A:
Run chart of process measures by month. PDSA cycles performed to improve process measures include: 1. Changed responsibility of survey distribution from physician to clinical assistant, resulting in increased survey distribution. 2. Winter holidays resulted in short-staffing and, because additional staff were not hired specifically for this survey, this resulted in decreased survey distribution 3. Staff meetings showing high level of needs and patient satisfaction. 4. Hospital roll-out of 2-question housing screen which briefly took the place of our survey; however, this did not meet the needs of our patients.
Results21
Between August, 2017 and November, 2018, 267 patient visits were eligible for screening. Of those 156 (58%) visits had a completed screen entered into the EMR, representing 132 unique patients (Table 3). The percentage per month varied from a low of 23% to improved high of 89% (Figure 1). Eighty percent of visits with positive screens had a targeted resource sheet included in their AVS. This work was done with existing clinic staff.
TABLE 3:
Demographics of patients screened
| Characteristic | Number (n=132) | % of screened |
|---|---|---|
| Sex | ||
| M | 65 | 49% |
| F | 67 | 51% |
| Age | ||
| 0–6 | 50 | 38% |
| 7–12 | 36 | 27% |
| 13–17 | 27 | 20% |
| 18+ | 19 | 14% |
| Genotype | ||
| HbSS | 98 | 74% |
| HbSC | 27 | 20% |
| HbS/Bo | 3 | 2% |
| HbS/B+ | 4 | 3% |
| Other | 0 | 0% |
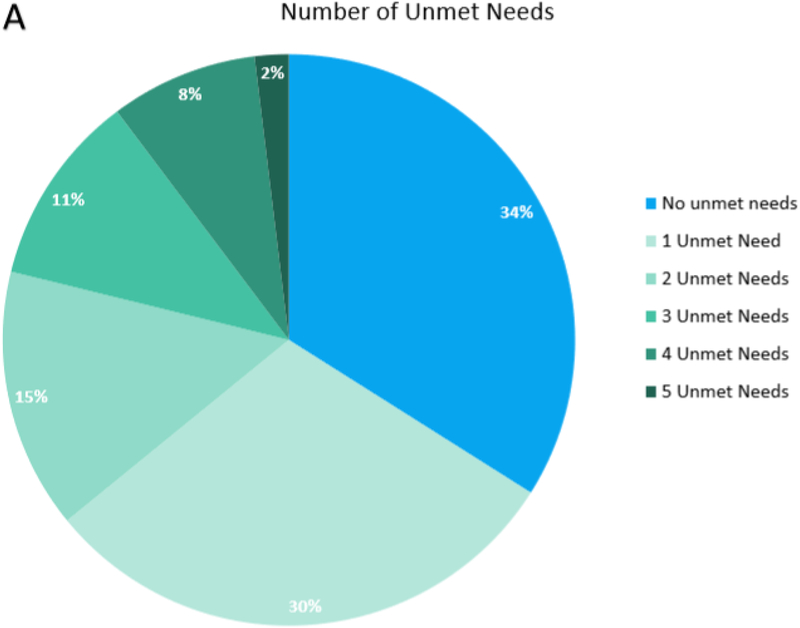
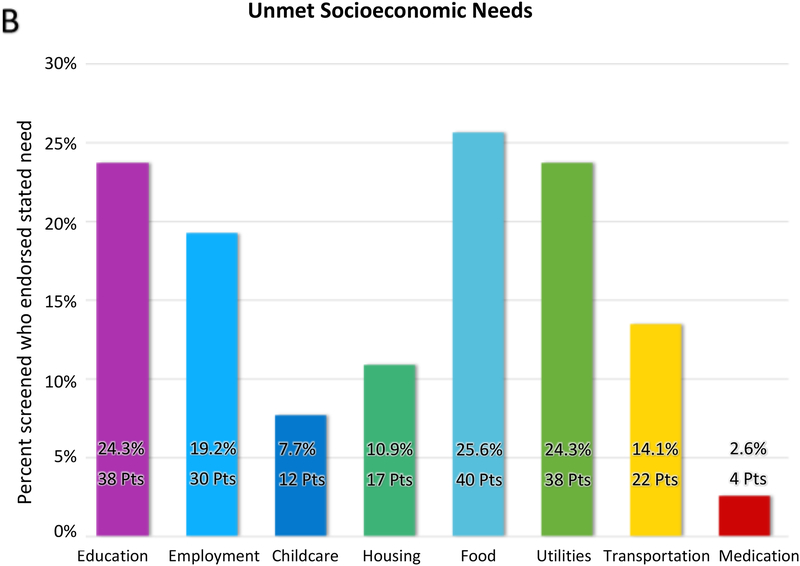
In 156 screens, 1.2 needs were identified per screener administered. Fifty-three (34%) reported no unmet socioeconomic needs and 103 (66%) were positive for at least 1 unmet socioeconomic need (Figure 2A). The most common unmet need was food insecurity, followed closely by difficulty paying utilities and a desire for more education (Figure 2B).
FIGURE 2A:
Number of reported unmet socioeconomic needs per screener completed. Approximately one-third (34%) of patients in our clinic reported no needs. A similar proportion (30%) endorsed one unmet need or 2 or more unmet needs (36%). The average needs identified per screener completed by all patients was 1.2.
FIGURE 2B:
Breakdown of unmet socioeconomic needs. Total exceeds 100% because patients were able to endorse multiple needs. Over one quarter of all patients surveyed endorsed food insecurity. Nearly this many endorsed difficulty paying for utilities and an interest in more education. Examples of solutions include referral to food pantries and providing utility shut-off protection letters. The rates of patients endorsing difficulty paying for medication is low (3%) likely because Massachusetts has universal health insurance, however, this shows that some patients remain underinsured.
The social worker called families with positive screens 2–3 weeks after their visit. Seventy-percent answered the phone, and 45% of those families reported reaching out to a community organization without any additional assistance from the clinic. Of those who reached out, 69% stated that the organization was helpful.
In terms of balancing measures, no additional clinic delays were submitted on our clinic flow diagrams. Our social worker did note a change in her work flow with more families identified to have socioeconomic needs requiring more in-person meetings and more follow-up phone calls, however, the screener provided her a streamlined approach to questioning and resource referral. Qualitatively, physicians, social work, and clinical assistants felt positively about the screening. One physician in our clinic stated, “I had a patient I’ve known for years who seems well-off in a two-parent household, and for the first time ever the mother told me that they often have trouble paying their utilities in the winter.” During follow-up phone calls, patients were asked how likely they were to continue discussing socioeconomic matters with the clinic on a 5-point Likert scale and the average response was 4.1.
Discussion
In this study we demonstrate that performing universal screening for SDoH among patients with SCD is feasible in a pediatric hematology clinic using existing resources and staff. This screening is viewed positively by patients. Furthermore, screening with the simple delivery of a pre-existing, targeted list of relevant resources is successful at connecting patients with local community organizations. This is the first study to demonstrate the feasibility of universal screening for SDoH for patients with SCD that we know of.
In our study, more than half of patients due for screening (58%) had a SDoH screener documented in their EMR, although many months did not reach our aim of screening 85% of patients. Several clinic-based factors contributed to this fluctuation, which we improved upon via process-focused PDSA cycles. Although our clinicians and social worker did not report delays in their workflow based on distributing and entering the screening results into the EMR, it was felt that this was not the most efficient use of clinician time; therefore, many PDSA cycles were aimed at optimizing these tasks for our clinical assistants. A main driver of this successful transition was showing our clinical assistants the significant socioeconomic needs reported and the positive patient responses to screening. Additionally, as many changes were made to clinic flow, occasionally the intended flow was unclear. A useful tool to address this was reminding all staff of changes in flow via updated clinic diagrams attached directly to the screener (Supplemental Figure 4B). In this transition, however, it remained important that the physicians and social workers continued to review the results and discuss socioeconomic challenges with their patients, so we did not transition the role of distributing resource referrals to our clinical assistants.
Notably, there are also many patient-based factors that may reduce the rates of completed screening. Patients were allowed to decline screening, and rates of refusal were not consistently tracked during this QI study. Offering universal screening is important to allow the families that need assistance to utilize it and to allow other families to opt out.
Our results show that patients with SCD in our clinic face a high SDoH burden. Sixty-six percent of screens report at least one unmet socioeconomic need, with an average of 2.1 unmet needs per patient with a need. There is not similar national data to compare to other SCD populations yet, however, the socioeconomic screening study from Dana Farber/Boston Children’s Cancer and Blood Disorders Center reported unmet socioeconomic needs in 44% of their pediatric oncology population.12 Ongoing research is needed to identify the national burden of socioeconomic needs among patients with SCD, and patients with SCD could likely benefit from SDoH screening guidelines similar to those in place for the oncology population. Until then, however, these numbers re-affirm to our clinic that it is imperative we continue improving this system to connect our patients with existing community resources.
This study also shows that our patients were pro-active once referred to community organizations, with nearly half of families reaching out to resources within two weeks (45%). This is higher than rates demonstrated in the BMC primary care clinic where 39% of families enrolled in a community program at their 12-month follow-up.18 This may be because our patients are eager to connect with assistance due to high socioeconomic burden or because they feel empowered to reach out. Overall, despite the high rates of unmet socioeconomic needs, screening did not overwhelm our existing staffing because, in this low-touch system, the referral information was well-integrated into the clinic flow and our families took action themselves to connect with community organizations.
Our next step for improvement is to assess and update our lists of community resources to ensure we are referring our patients to optimal agencies for their needs. Our social worker is leading this process with the creation of a database incorporating patient feedback regarding the effectiveness of each organization. Some needs are easily addressed; for example, concrete needs such as food insecurity and inability to pay for utilities can be improved with a food pantry or enrollment in a discount program. Other needs, such as unemployment or a desire for more education, either of which may underlie the remainder of the socioeconomic hardships, are not as tangibly fixed. Moreover, because the families at our clinic have children with chronic illnesses who have frequent clinic appointments or hospitalizations, it may be even harder for parents to remain employed or to consistently attend educational opportunities. For these problems it is especially beneficial to be able to refer families to organizations that are adept at addressing these unique challenges.
For the ongoing success of universal screening for SDoH in our clinic, we will continue working as a team with clinicians and the clinical assistants to distribute, record, review, and address the screener efficiently because efficient clinic flow is the key to sustainability of the screening. Several challenges in clinic flow remain, including that patients who arrive late are often roomed quickly resulting in missed screenings and that rates of screening decrease around staff vacations and holidays due to a reliance on a fixed number of staff members.
This study overcomes many potential barriers to physicians pro-actively asking their patients about SDoH. First, physicians may feel that they know which patients have socioeconomic needs; anecdotally, we have seen that universal screening captures needs that were not formerly recognized. Universal screening, by definition, attempts to screen everyone and, therefore, mitigates the role of provider perception in deciding which families should be asked about SDoH. In a population of patients with an already high burden of bias and stigma, the ability to remove provider-driven impetus for asking about needs may be beneficial.22 Another barrier to screening for SDoH may be that this is not currently a reimbursable action; therefore, additional staff cannot be hired to complete the task. We have introduced this screening successfully without any additional staff. Addressing SDoH may be actually be a cost-effective preventive measure by reducing the “revolving door” of recurrent hospitalizations and emergency room visits.23
Increasing awareness about the effects of poverty on a child’s health is elevating the importance of screening for and addressing SDoH in pediatrics. The AAP’s Task Force on Poverty identifies outpatient continuity providers as critical points-of-contact for mitigating the harms of unmet socioeconomic needs. They published a roadmap and framework for outpatient providers to address these needs. Direct, high-involvement strategies include hands-on, in-clinic help, such as social workers, medical legal partnerships, and organizations that help families complete applications. Indirect, low-involvement strategies screen families for needs and connect them with resources external to the clinic. The taskforce cites WECARE as an effective, and easily implemented, indirect strategy for improving care delivery to families living in poverty.24 Additional screeners are available and include the American Academy of Family Physician’s EveryONE project and the Centers for Medicare and Medicaid’s Health Related Social Needs screening tool.25,26
There are limitations to the generalizability of our single-center, QI study. Our clinic is fortunate to be located in an urban center with a high density of local organizations to whom we can refer our patients. We were also fortunate to have started the project with a pre-existing list of community resources. This should not be a limitation to replication, however, because many cities have pre-curated lists of community organizations which may be available through their local AAP chapters, UnitedWay211, or the EveryONE project.27 This is also a feasible volunteer project, which is where the database available at our hospital originated.28
Finally, this study was designed to directly improve the care of our patients and not to identify associations nor to prove causation. As such, areas of future study include assessing if our intervention reduces the rates of unmet socioeconomic needs and the determination of associations between universal screening and other outcomes, including the rates of missed clinic appointments, hospitalizations, re-admission rates, and perceived therapeutic alliance. Additionally, the screener could be used for more granular research into which specific unmet socioeconomic needs contribute to worse outcomes, which could then be used for targeted interventions. Currently, household income, zip code, and insurance type are proxies for poverty correlated with outcomes, but in many scenarios, they may be too blunt to identify a mechanism. Breaking poverty into more granular components might allow for an analysis of associations and causes, leading to concrete interventions through which we can improve our patients’ health and well-being.
Supplementary Material
FIGURE 3: Example resource sheets
FIGURE 4A: Clinic flow diagrams were updated to inform clinic staff of the screening process. Changes were made in concordance with PDSA cycles. A table to elicit feedback was included, but was most often left blank or was used to re-iterate the need endorsed.
FIGURE 4B: CA- clinical assistant, MD- medical doctor, SW- social worker. This is the most current clinic flow diagram and represents the results of several PDSA cycles to maximize efficiency.
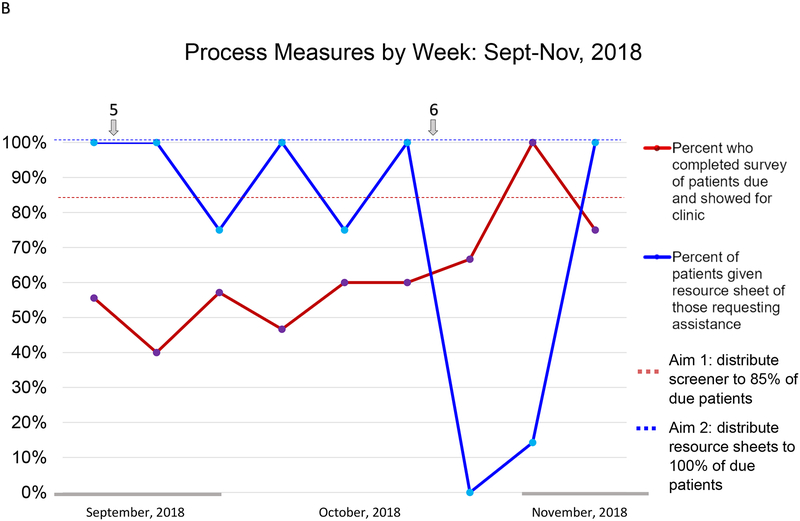
FIGURE 1B:
Run chart of process measures by week. An analysis of process measure by week shows more detailed trends for this time period. 5. All patients with SCD presenting for a non-sick or non-urgent clinic appointment were given screeners. This did not result in significant change in the numbers of screeners that were completed or documented. 6. Clinical assistants entered screener results into EMR at increasing rates, but were not explicitly asked to page social work for positive results to not overburden the clinical assistants. This resulted in decreased distribution of resource sheets. Changes were made to the clinic flow to ask clinical assistants to page SW for positive results. Reminders were posted in exam rooms and a new clinic flow diagram was distributed. Physicians were reminded to continue reviewing the screening results.
Acknowledgments:
Thank you to Dr. Arvin Garg for creating the initial We Care survey and for lending your advice as we expand its impact. Dr. Sobota is funded through an ASH Scholar Award and NHLBI 1K23HL135436-01
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Abbreviation
- SDoH
Social determinants of health
- SCD
Sickle cell disease
- EMR
Electronic medical record
- BMC
Boston Medical Center
Footnotes
Conflict of Interest Statement: The authors have no conflicts of interest to disclose
References
- 1.Marmot M, Wilkinson R. Social Determinants of Health: The Solid Facts. World Health Organization; 2006. [Google Scholar]
- 2.World Health Organization. About social determinants of health. [online] https://www.who.int/social_determinants/sdh_definition/en/ Accessed March, 2019
- 3.Bonnefoy X Inadequate housing and health: an overview. Int J Environ Pollut. 2007;30(3):411–429. 2. [Google Scholar]
- 4.Gundersen C, Kreider B. Bounding the effects of food insecurity on children’s health outcomes. J Health Econ. 2009;28(5):971–983. [DOI] [PubMed] [Google Scholar]
- 5.Mojtabai R, Olfson M. Medication costs, adherence and health outcomes among medicare beneficiaries. Health Aff. 2003;22(4):220–229. [DOI] [PubMed] [Google Scholar]
- 6.Artiga S, Hinton E. Beyond Health Care: The Role Of Social Determinants in Promoting Health and Health Equity. Kaiser Family Foundation; https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/. Accessed March, 2019. [Google Scholar]
- 7.Daniel H, Bornstein SS, Kane GC. Addressing social determinants to improve patient care and promote health equity: an American College of Physicians position paper. Ann Intern Med. 2018;168(8):577–578. doi: 10.7326/M17-2441 [DOI] [PubMed] [Google Scholar]
- 8.Council on Community Pediatrics. Poverty and child health in the United States. Pediatrics. 2016; 137(4):e20160339. [DOI] [PubMed] [Google Scholar]
- 9.Berman R, Patel M, Belamarich P, Gross R. Screening for Poverty and Poverty-Related Social Determinants of Health. Pediatrics in Review. 2018;39(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garg A, Toy S, Tripodis Y, Silverstein M, et al. Addressing social determinants of health at well child care visits: A cluster RCT. Pediatrics. 2015;(135)2:e296–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pelletier W, Bona K. Assessment of financial burden as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62(S5): S619–S631 [DOI] [PubMed] [Google Scholar]
- 12.Zheng D, Shyr D, Ma C, Muriel A, Wolfe J, Bona K. Feasibility of systematic poverty screening in a pediatric oncology referral center. Pediatr Blood Cancer. 2018;65:e27380. doi: 10.1002/pbc.27380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Powars D, Chan L, Hiti A, Ramicone E, Johnson C. Outcome of sickle cell anemia: a 4-decade observational study of 1056 patients. Medicine. 2005;84(6):363–376. doi: 10.1097/01.md.0000189089.45003.52. [DOI] [PubMed] [Google Scholar]
- 14.Hassell K Population estimates of sickle cell disease in the U.S. American Journal of Preventive Medicine. 2010; 38(4), S512–S521. [DOI] [PubMed] [Google Scholar]
- 15.The Kaiser Family Foundation State Health Facts. National Vital Statistics Reports. 2017;66(1). https://www.cdc.gov/nchs/data/nvsr/nvsr66/nvsr66_01.pdf. Accessed March, 2019. [Google Scholar]
- 16.Panepinto J, Foerster L, Sabnis S, Pajewski N, Hoffmann R. Impact of poverty and sickle cell disease on the health-related quality of life of children. Blood. 2007;110(11):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raphael J, Dietrich C, Whitmire D, Mahoney D. Healthcare utilization and expenditures for low income children with sickle cell disease. Pediatric Blood and Cancer. 2009;52(2):263–7. doi: 10.1002/pbc.21781. [DOI] [PubMed] [Google Scholar]
- 18.Robinson M, Daniel L, O’Hara E, Szabo M, Barakat L. Insurance status as a sociodemographic risk factor for functional outcomes and health-related quality of life among youth with sickle cell disease. J Pediatr Hematol Oncol. 2014;36(1):51–6. doi: 10.1097/MPH.0000000000000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boston Medical Center. BMC-Facts. 2017. www.bmc.org/sites/default/files/For_Medical_Professionals/BMC-Facts.pdf. Accessed March, 2019.
- 20.Murtagh Kurowski E, Schondelmeyer AC, Brown C et al. Curr Treat Options Peds (2015) 1: 380 10.1007/s40746-015-0027-3 [DOI] [Google Scholar]
- 21.The data that support the findings of this study are available from the corresponding author upon reasonable request.
- 22.Wakefield E, Popp J, Dale L, Santanelli J. Perceived racial bias and health-related stigma among youth with sickle cell disease. Journal of Developmental & Behavioral Pediatrics. 2017;38(2):1. [DOI] [PubMed] [Google Scholar]
- 23.Andermann A Screening for social determinants of health in clinical care: moving the margins to the mainstream. Public Health Rev. 2018;39(19). doi: 10.1186/s40985-018-0094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beck A, Tschudy M, Coker T, Mistry K, et al. Determinants of Health and Pediatric Primary Care Practices. Pediatrics. 2016;137(3). [DOI] [PubMed] [Google Scholar]
- 25.The EveryONE Project Toolkit. https://www.aafp.org/patient-care/social-determinants-of-health/everyone-project/eop-tools.html. Accessed July 31, 2019.
- 26.The Accountable Health Communities Health-Related Social Needs Screening Tool. https://innovation.cms.gov/Files/worksheets/ahcm-screeningtool.pdf. Accessed July 31, 2019.
- 27.2-1-1. Available at: www.211.org/. Accessed July 31, 2019.
- 28.Health Leads. https://healthleadsusa.org/. Accessed April 30, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FIGURE 3: Example resource sheets
FIGURE 4A: Clinic flow diagrams were updated to inform clinic staff of the screening process. Changes were made in concordance with PDSA cycles. A table to elicit feedback was included, but was most often left blank or was used to re-iterate the need endorsed.
FIGURE 4B: CA- clinical assistant, MD- medical doctor, SW- social worker. This is the most current clinic flow diagram and represents the results of several PDSA cycles to maximize efficiency.