Abstract
Introduction
There is strong evidence that exercise prevents falls in community-dwelling older people. This review summarises trial and participant characteristics, intervention contents and study quality of 108 randomised trials evaluating exercise interventions for falls prevention in community-dwelling older adults.
Methods
MEDLINE, EMBASE, CENTRAL and three other databases sourced randomised controlled trials of exercise as a single intervention to prevent falls in community-dwelling adults aged 60+ years to May 2018.
Results
108 trials with 146 intervention arms and 23 407 participants were included. Trials were undertaken in 25 countries, 90% of trials had predominantly female participants and 56% had elevated falls risk as an inclusion criterion. In 72% of trial interventions attendance rates exceeded 50% and/or 75% of participants attended 50% or more sessions. Characteristics of the trials within the three types of intervention programme that reduced falls were: (1) balance and functional training interventions lasting on average 25 weeks (IQR 16–52), 39% group based, 63% individually tailored; (2) Tai Chi interventions lasting on average 20 weeks (IQR 15–43), 71% group based, 7% tailored; (3) programmes with multiple types of exercise lasting on average 26 weeks (IQR 12–52), 54% group based, 75% tailored. Only 35% of trials had low risk of bias for allocation concealment, and 53% for attrition bias.
Conclusions
The characteristics of effective exercise interventions can guide clinicians and programme providers in developing optimal interventions based on current best evidence. Future trials should minimise likely sources of bias and comply with reporting guidelines.
Keywords: fall, exercise, evidence-based, senior, review
Summary box.
What is already known
Previous systematic reviews concluded exercise as a single intervention prevents falls in community-dwelling older adults.
Evidence-based practice requires clinicians and service providers to interpret, evaluate, adapt and integrate findings from clinical trials into their practice and policies.
Clinical trials of exercise intervention are heterogeneous in terms of participant characteristics, compliance, intervention content and risk of bias.
What are the new findings
A diversity of effective exercise interventions are available, offering clinicians an opportunity to implement shared decision-making with their patients.
Promotion of long-term exercise is needed.
Existing trials are prone to performance and ascertainment bias, which impedes the implementation of evidence-based medicine.
Further research is needed for interventions targeting males as well as low-income countries.
Introduction
Falls are a significant cause of mortality and can cause serious morbidity such as fracture and head injury in older adults.1 2 Falls substantially reduce the mobility and confidence of older people and impose a significant economic and social burden to society.2 3 Approximately one-third of people aged above 65 years living in the community fall each year4 and the incidence and healthcare cost associated with falls will increase with the ageing population.5 Thus, there is an urgent need for effective falls prevention strategies to be implemented.
Systematic reviews concluded that exercise programmes can reduce the rate of falls and risk of falling in community-dwelling older adults.6–8 In addition, two Cochrane systematic reviews concluded the falls prevention effect of stand-alone exercise interventions is similar to multifaceted interventions.7 9 Translating the research findings from stand-alone exercise intervention trials into clinical practice would therefore be a beneficial and potentially cost-effective public health solution to falls in community-dwelling older adults.10
Our recent Cochrane Review, including 108 trials, co-published in the British Journal of Sports Medicine,11 evaluated the effect of exercise on falls in people aged 60+ living in the community. Exercise interventions that reduced falls involved primarily balance and functional exercise (reduced fall rate by 24%, 95% CI 19% to 35%), Tai Chi (reduced fall rate by 19%, 95% CI 1% to 33%) or multiple exercise components, usually including balance and strength training (reduced fall rate by 34%, 95% CI 12% to 50%).8
Evidence-based practice requires clinicians to interpret, evaluate, adapt and integrate findings from clinical trials into their practice and policies.12 This is challenging with fall prevention trials, due to heterogeneity in participant characteristics and intervention content. Clinicians must consider whether results are generalisable to their patient population, by reviewing the type of exercise, duration, group-based versus individualised delivery and level of supervision provided.13 Considering participant adherence to intervention programmes also facilitates judgement on intervention effectiveness and acceptability.14 Assessment of risk of bias in a trial will also inform its validity.
Describing and understanding the characteristics of the trials included in the Cochrane Review8 evaluating the effectiveness of exercise on falls prevention, especially those studies contributing to effective intervention types, will guide evidence-based practice and future research. This paper aims to describe the following, in randomised controlled trials (RCT) of exercise as a single intervention for falls prevention in community-dwelling adults aged 60 years and older:
Trial and participant characteristics.
Components of exercise programmes that prevent falls (exercise type, duration and hours of intervention, delivery mode, level of supervision, tailored in intensity or type).
Risk of bias.
Methods
Searches
MEDLINE, EMBASE, CINAHL, Cochrane Bone, Joint and Muscle Trauma Group Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL) and the Physiotherapy Evidence Database (PEDro; http://www.pedro.org.au/) were searched from inception to 2 May 2018. The full search strategy is reported in detail in the Cochrane Review protocol15 and the search terms are included in online supplementary material A. The reference lists of previously published systematic reviews were screened and trial authors were contacted to identify additional studies.
bmjsem-2019-000663supp001.pdf (61.8KB, pdf)
Selection of studies
The detailed methodology for selection of studies was described in the Cochrane Review protocol.15 In brief, RCTs, individual or cluster randomised, evaluating the effect of exercise interventions on falls in older people living in the community were included. Eligible trials had exercise as a single intervention with the mean age minus 1 SD of the participants being greater than 60 years. Eligible trials reported either number or rate of falls. Trials using quasirandomisation were excluded. Studies were excluded if the target population had specified clinical conditions impacting falls, for example, dementia, stroke, Parkinson’s disease, multiple sclerosis, hip fracture and severe visual impairment.
The title, abstract and descriptors of identified studies were screened independently by pairs of review authors (ZAM, AT, NF, CS). From full text, the same two review authors (ZAM, AT, NF, CS) independently assessed each potentially eligible article with disagreements resolved through discussion. If needed, trial authors were contacted for additional information.
Data extraction
A pretested data extraction form based on an earlier Cochrane Review7 was used by pairs of review authors (ZAM, AT, NF, CS, GW, CAN) to independently extract data from all included trials. Disagreements were resolved through discussion. Review authors did not assess their own trials.
The items extracted from the trials included trial and participant characteristics (sample size at randomisation, trial location, age, gender, falls risk at enrolment, inclusion criteria related to falls, compliance) and intervention components (exercise type, duration of intervention, hours of intervention, delivery mode, level of supervision, tailored initially, progressed based on individual assessment, tailored in intensity or type). Falls risk at enrolment was classified as high if the trial’s inclusion criteria were based on specific fall risk factors such as previous falls, poor balance, recent hospitalisation, reduced lower strength, poor mobility, use of mobility aids, frail, prolonged bed rest, recent rehabilitation, functional limitation and all participants greater than age 80. Compliance was classified as good if the attendance rate exceeded 50% and/or 75% or more of the participants attended 50% or more sessions. The intervention type was classified based on taxonomy developed by the Prevention of Falls Network Europe (ProFaNE)16: balance, functional (task) and gait training; strengthening or resistance training; flexibility training; three-dimensional exercise (including Tai Chi and dance); general physical activity; endurance; and other exercises.
The methods for the estimate of the pooled treatment effect of exercise and the application of the Grading of Recommendations Assessment, Development and Evaluation system to establish certainty of evidence are described in detail in the Cochrane Review.8
Risk of bias of studies
Risk of bias was assessed independently by pairs of review authors (ZAM, AT, GW, NF) not blind to the trial authors or sources, using the Cochrane Risk of Bias tool.17 The criteria were: sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective reporting; and ascertainment bias. Disagreements were resolved through discussion. Review authors did not assess their own trials.
Results
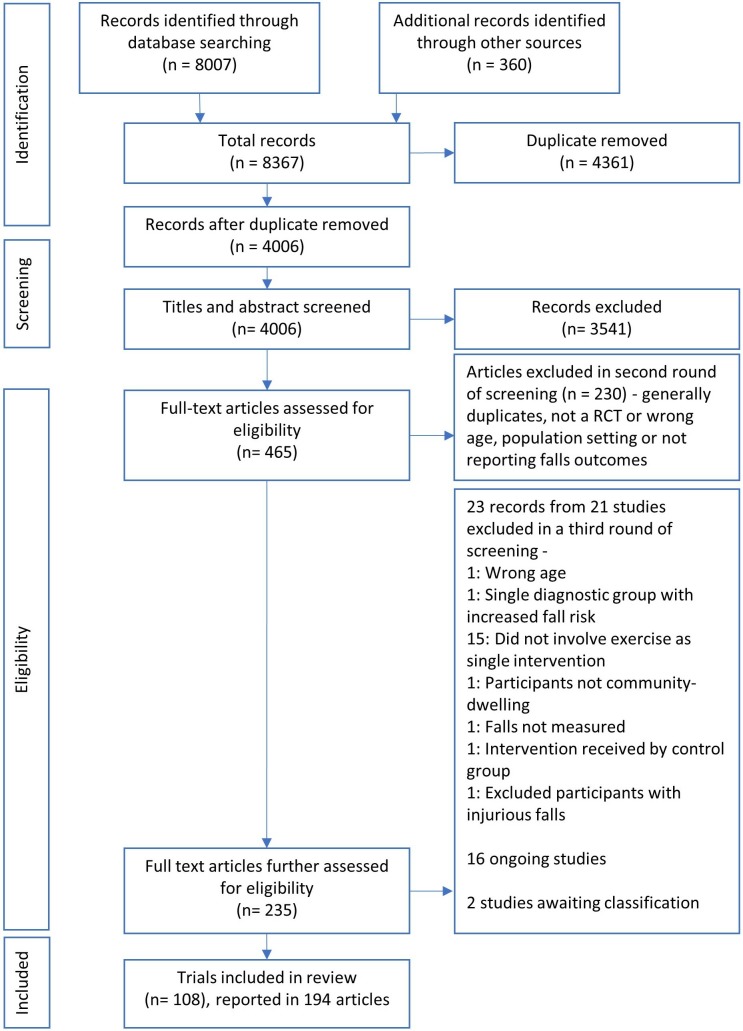
The search returned 4006 records, of which 108 trials involving 23 407 participants were eligible for inclusion (figure 1).18 The characteristics of the 108 included trials are summarised in online supplementary material B.10 19–125
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram18 summarising the study selection process. RCT, randomised controlled trial.
bmjsem-2019-000663supp002.pdf (77.2KB, pdf)
Trial and participant characteristics
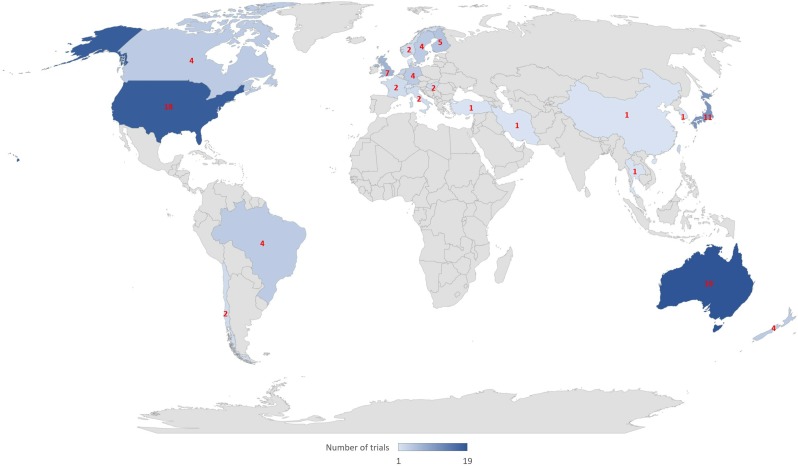
The sample size ranged from 2098 to 1635 participants.47 The included trials were undertaken in 25 countries (figure 2). The highest number of trials took place in Australia (19/108, 18%), followed by the USA (18/108, 17%), Japan (11/108, 10%) and the UK (7/108, 6%). There were three multinational trials.49 72 89 The mean participant age in the reviewed trials ranged from 65 to 88 years old. Ninety-seven (90%) trials had predominantly female participants; 28 (26%) trials were made up of entirely female participants with only one trial100 testing their intervention specifically on the male population. Sixty (56%) trials had elevated fall risk as an inclusion criterion, which was assessed as falls history (33 trials, 31%); poor balance (13 trials, 12%); poor mobility or use of mobility aid (4 trials, 4%); lower limb weakness (3 trials, 3%); functional limitation (3 trials, 3%); age greater than 80 years (3 trials, 3%); recent rehabilitation (2 trials, 2%); and 1 (1%) each for frail and prolonged bed rest, respectively. Fourteen of the trials had multiple inclusion criteria. Seventy-eight (72%) trials satisfied the criteria of good compliance with attendance rate exceeding 50% and/or 75% or more of the participants attending 50% or more sessions.
Figure 2.
Number of trials by country. Note: There are three multinational trials not included on the map: Australia and New Zealand by Latham et al72; Australia, Spain and Germany by Gschwind et al49; Belgium, Israel, Italy, the Netherlands and the UK by Mirelman et al.89
Intervention content and characteristics
There were 146 intervention arms in the 108 included trials. Using the ProFaNE taxonomy the primary intervention component was balance and functional exercise in 79 (54%) intervention arms; three-dimensional exercise (Tai Chi) in 16 (11%) intervention arms; and multiple categories of exercise in 34 (23%) intervention arms (the majority of these (n=19, 51%) included balance and functional exercise in addition to resistance exercise). These primary categories of exercise intervention significantly reduced falls in the Cochrane Review8 and the intervention characteristics are described in online supplementary material C. The remaining types of primary intervention, which did not significantly reduce falls, are described in online supplementary material D: strength or resistance training, 11 (8%) intervention arms; flexibility training, 1 (1%) intervention arm; general physical activity, 5 (3%) intervention arms. No intervention included endurance exercise as the primary component. The duration of the interventions varied from 2 to 130 weeks, with a median of 25 weeks (IQR 12–52) while 75 (51%) interventions lasted less than 24 weeks. The total hours of intervention varied from 6 to 1086 hours, with a median of 44 hours (IQR 24–87). There were 72 (49%) group-based interventions, 15 (10%) supervised individual-based interventions, 29 (20%) intervention arms were unsupervised individual exercise and 30 (21%) interventions were a mixture of group-based and individual exercise. The participant to instructor ratio was not clearly reported in 65 (45%) intervention arms. Of the 82 interventions that reported, 29 were not supervised, 15 had one-on-one intervention and 8 interventions had more than 10 participants per instructor. Eighty-one (55%) intervention arms were tailored to the individual initially and intervention was progressed based on individual assessment in 86 (59%) interventions. Ninety-three (64%) interventions were tailored in intensity or type.
bmjsem-2019-000663supp003.pdf (121.6KB, pdf)
bmjsem-2019-000663supp004.pdf (102.5KB, pdf)
Characteristics of studies where the primary exercise components wasere balance, functional and gait training
Compared with control, balance and functional exercises reduced the rate of falls by 24% (rate ratio 0.76, 95% CI 0.70 to 0.81; 7920 participants, 39 studies; high-certainty evidence). The median programme duration was 25 weeks (IQR 16–52). The median total hours of exercise was 52 hours (IQR 24–92). Twenty (39%) of the intervention arms were delivered in a group setting, 3 (6%) provided supervision to individuals, 15 (29%) were individually unsupervised and 13 (25%) involved a combination of group-based and individual exercise. In 20 (39%) interventions the participant-to-instructor ratio was not clearly reported. Of the 31 interventions, three had more than 10 participants per instructor. In 29 (57%) arms, the intervention was tailored to the individual initially and intervention was progressed based on individual assessment in 30 (59%) interventions. Thirty-two (63%) interventions were tailored in intensity or type and the remaining 19 (37%) were not tailored.
Characteristics of studies where the primary exercise component was Tai Chi
Compared with control, Tai Chi reduced the rate of falls by 19% (rate ratio 0.81, 95% CI 0.67 to 0.99; 2655 participants, 7 studies; low‐certainty evidence). The median programme duration was 20 weeks (IQR 15–43), with a median of 45 total hours of exercise (IQR 40–80). Tai Chi was delivered in a group in 10 (71%) intervention arms, delivered individually with supervision in 1 (7%) arm, individually without supervision in 1 (7%) arm; and with a combination of individual and group delivery in 2 (14%) arms. There was 1 (7%) intervention with one-on-one supervision and 7 (50%) interventions where the participant-to-instructor ratio was not clearly reported. Five Tai Chi intervention arms had more than 10 participants per instructor. None of the Tai Chi programmes were tailored to the individual initially and 1 (7%) intervention was progressed based on individual assessment. One (7%) intervention was tailored in intensity or type and the remaining 13 (93%) were not.
Characteristics of studies which involved multiple types of exercise
Multiple types of exercise (most commonly balance and functional exercises plus resistance exercises) reduced the rate of falls by 34% (rate ratio 0.66, 95% CI 0.50 to 0.88; 1374 participants, 11 studies; moderate-certainty evidence). The median programme duration was 25.5 weeks (IQR 12–52) and the median total hours of exercise was 54 hours (IQR 44–91). In 13 (54%) intervention arms, the multitype intervention was delivered in a group; in 5 (21%) arms, it was delivered individually without supervision; and in 6 (25%) there was a combination of individual and group delivery. There was 0 intervention with one-on-one supervision and 13 (54%) interventions where the participant-to-instructor ratio was not clearly reported. No interventions had more than 10 participants per instructor. The intervention was tailored to the individual initially in 18 (75%) and intervention was progressed based on individual assessment in 17 (71%) of interventions. Eighteen (75%) interventions were tailored in intensity or type and the remaining 5 (21%) were not tailored.
Components of studies in categories of exercise not found to prevent falls
The characteristics of studies in categories of exercise not found to be effective in preventing falls are outlined in online supplementary material D.
Risk of bias assessment
The summary of risk of bias is displayed in online supplementary material E. With regard to allocation, risk of selection bias for sequence generation was low in 67% (72/108) of the included trials, and unclear in the remaining 33% (36/108). Risk of selection bias for allocation concealment was low in 35% (38/108) of trials, high in 5% (5/108) and unclear in the remaining 60% (65/108). For blinding, participants and personnel delivering the intervention were potentially aware of their allocation status and falls were self-reported. The risk of performance bias (for blinding of participants and personnel) was low in 5% (5/108) of trials, high in 6% (6/108) and the remaining 89% (97/108) were unclear. The risk of detection bias (for ascertainment of falls) was low in 40% (43/108) of trials, high in 21% (23/108) and unclear in the remaining 39% (42/108). Risk of attrition bias, which may arise from incomplete outcome data, was low in 53% (57/108) of trials, high in 27% (29/108) and unclear in the remaining 20% (22/108). The risk of bias for selective outcome data was low in 12% (13/108) of trials, high in 48% (52/108) and unclear in the remaining 40% (43/108). The risk of ascertainment bias was low in 58% (63/108) of trials, high in 27% (29/108) and unclear in the remaining 15% (16/108).
bmjsem-2019-000663supp005.pdf (72.9KB, pdf)
Discussion
A variety of clinical trials of exercise as a single intervention for falls prevention in community-dwelling older people have been published. There are clear implications for practice and research. Descriptions of the characteristics of exercise programmes that contributed to effective intervention types may guide clinicians in developing optimal programmes for their patients. Identification of gaps and methodological flaws in fall prevention studies will guide future research.
In summary, most trials took place in developed countries, involved a wide age range and predominantly comprised female participants. Most trial populations had higher risk of falls, indicated by history of falls, poor balance, recent hospitalisation or poor mobility as inclusion criteria. Adherence to exercise was suboptimal. Balance and functional exercises were the most common primary intervention and had the greatest effect on falls. The duration and hours of intervention varied. While most interventions were group based and tailored to the individuals, the level of supervision was not clearly reported. Furthermore, the majority of trials did not clearly report allocation concealment and blinding of participants and personnel.
Implications for practice
Within the effective interventions, involving balance and functional exercises, Tai Chi and multiple types of exercise (typically incorporating balance and strength exercises), there are different ways the interventions can be delivered. Clinicians and exercise programme providers need to note the characteristics of trials that contributed to fall prevention effects, and work with patients to establish the most suitable exercise programme for the individual.126
The updated Cochrane Review8 is consistent with previous systematic reviews6 7 127 that identified greater falls prevention effects from exercise programmes that challenge balance. This element was present in all the effective interventions: balance and functional training, Tai Chi and multiple types of exercise. Challenge to balance can be achieved by progressively reducing the base of support, removing upper limb support and moving the centre of gravity to challenge balance. Strength training alone did not prevent falls, however when included in a programme with balance training, a fall prevention effect was evident. This is consistent with previous research that recommend exercise programmes targeting falls may include strength training in addition to balance training.6 127
For exercise to be effective a sufficient intensity and duration of exercise is required. In the trials with interventions classified primarily as balance and functional training, the median intervention duration was 6 months, with a total of 52 hours (approximately 2 hours per week). In trials with interventions classified primarily as Tai Chi, the median duration was 4 months, with a total of 45 hours (approximately 2.8 hours per week). For trials with interventions that included multiple primary components, the median intervention duration was 6 months, with a total of 54 hours. This is less than the 3 hours of exercises per week recommended for falls prevention, following a previous systematic review with meta-regression.6 In addition, ongoing exercise is needed to maintain the falls prevention benefit of exercise.6 The trial nature of these programmes limited their duration and clinicians need to discuss strategies with their patients to keep them exercising in the long term.
The Cochrane Review found there may be no difference in the effect of exercise on the rate of falls where interventions were delivered in a group setting compared with trials where interventions were delivered individually.8 In the effective intervention types, home-based interventions were frequently delivered as, or based on, the Otago Exercise Program. Home-based interventions, or group-based interventions with less than 10 participants, were mostly tailored in type or progression. For home-based programmes, the instructor usually makes an initial home visit to the participant’s residence to individually tailor the programme, with follow-up sessions for assessment and progression. For the group-based intervention, an instructor may adjust the individual’s tasks within a predefined programme. On the other hand, most group interventions with more than 10 participants per instructor were not tailored to individuals. Clinicians need to balance the increased social support and adherence from supervised group-based intervention with the sustainable self-motivation for exercise from individualised home-based intervention.128 129 Interventions combining both delivery modes have the potential to provide the benefit from both sides.
Optimising adherence is another important consideration during design and implementation of an intervention programme.130 Given the suboptimal level of compliance, clinicians should therefore incorporate effective strategies to promote adherence such as involving the patients in shared decision-making, goal setting and framing the interventions as life enhancing.128 130
There is sufficient evidence available to support the use of exercise to prevent falls, providing clinicians an opportunity to implement evidence-based shared decision-making. Evidence-based medicine requires clinicians to integrate the evidence with patient preferences.131 A decision aid could be developed to help clinicians and patients aware of the options and programmes available to them in the area.132
Implications for research
Several areas of deficiency in the arena of falls prevention research were identified in this review. There is a lack of clinical trials investigating the effect of exercise in preventing falls from the African continent and China, areas that represent a significant proportion of older adults in the world and are ageing rapidly.133 Low and middle-income countries and low-income countries are also under-represented, presenting a barrier in translating cost-effective exercise interventions to clinicians in these countries.12 Furthermore, exercise intervention trials that specifically target males are lacking with only one trial available. While the risk and incidence of falls are greater in females, the mortality rate due to falls is higher for males, suggesting more clinical trials for men are needed in preventing particular circumstances of falls.134 There was insufficient research evaluating programmes containing primarily flexibility and endurance exercise and little research evaluating only resistance training and only walking programmes. Finally, there is a need for cost-effectiveness analysis to investigate any economic benefit of home-based or individually tailored interventions for falls prevention.
Risk of bias and deviation of clinical trials from study design and reporting guidelines reduces their credibility. The reporting of a substantial number of trials did not meet the standards of the Consolidated Standards of Reporting Trials statement,135 for example, one-third omitted a sufficient description of randomisation and almost two-thirds did not describe allocation concealment. Due to the nature of exercise interventions, it is extremely difficult to blind the participants or personnel. This amplifies the need to minimise the risk of ascertainment bias (bias in the recall of falls due to unreliable methods of ascertainment); yet 42% did not satisfy the criteria for low risk. Falls are under-reported when data are collected on a three monthly basis, compared with daily.136 To minimise bias, the ascertainment of falls should follow the ProFaNE consensus137 of daily recording of falls using falls calendars and monthly follow-up analysis performed by researchers blind to participants’ allocation. Almost half of the studies did not report participant-to-instructor ratio; consistent reporting guidelines on the level of supervision should be promoted. Evidence-based medicine is the implementation of high-quality evidence in clinical practice13; however, if the presentation of the evidence is not of high quality, then it would impede the utilisation of the findings by clinicians. Therefore, quality study methodology and satisfaction of the reporting guidelines should be promoted.
This report has limitations. This review did not include trials specifically recruiting older adults with dementia, stroke, Parkinson’s disease, multiple sclerosis or hip fracture. While these conditions are associated with a higher risk of falls, the effect of exercise on falls in these populations has been covered previously138 139 and we aim to make the study results generalisable to the community-dwelling older people. Exercise as part of a multicomponent intervention was excluded from this review as this is covered elsewhere.9 Coding of intervention type was limited to the information available in the papers or provided by the authors, which may be inaccurate. Multiple databases were searched and studies published in language other than English were included in an effort to minimise publication bias. More research is needed for categories of interventions not found to prevent falls and readers should be cautious to interpret it as ‘no evidence of effect’ rather than ‘evidence of no effect’.
Conclusion
This review identified the diversity of trials that evaluate the effect of exercise on falls in community-dwelling older people, in terms of participants’ age and baseline fall risk, intervention type, duration and delivery mode. Implications for clinicians include implementing balance challenging exercise programmes, of adequate duration, in a setting optimal for the patient, with strategies to promote exercise uptake. Further research is needed regarding exercise for fall prevention in low-income countries and in males. Future trials should minimise bias, comply with reporting guidelines and report factors relevant to facilitating translation to clinical practice.
Acknowledgments
We are very grateful for the extensive support from the Cochrane Bone, Joint and Muscle Trauma Group in the preparation of the Cochrane Review. The names of editorial base members, Cochrane editors, external referees, consumer peer referees, copyeditors and other contributors are listed in the Acknowledgements section in the full Cochrane Review.
Footnotes
Contributors: CAN was involved in data extraction, data analysis, and co‐led the writing of the review. NF was involved in screening, data extraction, data analysis, and co‐led the writing of the review. GW was involved in screening, data extraction, data analysis, and contributed to writing the review. AT and ZAM were involved in screening, data extraction, data analysis, and contributed to writing the review. CS was involved in screening, data extraction, data analysis, co‐led the writing of the review and acted as guarantor of the review.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer: No review author was involved in study selection or processing of any trials in which they were or are involved.
Competing interests: CS and AT are currently running trials of fall prevention interventions, funded by national grant agencies, which are not included in this review. CS is an author of several trials considered in this review, including four included trials (Merom et al (2016); Sherrington et al (2014); Vogler et al (2009); Voukelatos et al (2015)). CN, NF, GW, AT and ZAM have no known conflicts of interest.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Alamgir H, Muazzam S, Nasrullah M. Unintentional falls mortality among elderly in the United States: time for action. Injury 2012;43:2065–71. 10.1016/j.injury.2011.12.001 [DOI] [PubMed] [Google Scholar]
- 2.Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults — United States. J Safety Res 2016;58:99–103. 10.1016/j.jsr.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist 2002;42:17–23. 10.1093/geront/42.1.17 [DOI] [PubMed] [Google Scholar]
- 4.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006;35:ii37–41. 10.1093/ageing/afl084 [DOI] [PubMed] [Google Scholar]
- 5.Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. The Lancet 2012;380:2197–223. 10.1016/S0140-6736(12)61689-4 [DOI] [PubMed] [Google Scholar]
- 6.Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med 2017;51:1750–8. 10.1136/bjsports-2016-096547 [DOI] [PubMed] [Google Scholar]
- 7.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;85 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 2019;21 10.1002/14651858.CD012424.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hopewell S, Adedire O, Copsey BJ, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2018;32 10.1002/14651858.CD012221.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davis JC, Robertson MC, Ashe MC, et al. Does a home-based strength and balance programme in people aged >=80 years provide the best value for money to prevent falls? A systematic review of economic evaluations of falls prevention interventions. Br J Sports Med 2010;44:80–9. 10.1136/bjsm.2008.060988 [DOI] [PubMed] [Google Scholar]
- 11.Sherrington C, Fairhall N, Wallbank G, et al. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. Br J Sports Med 2019:bjsports-2019-101512. [DOI] [PubMed] [Google Scholar]
- 12.Grol R, Wensing M. What drives change? barriers to and incentives for achieving evidence‐based practice. Med J Aust 2004;180:S57–60. 10.5694/j.1326-5377.2004.tb05948.x [DOI] [PubMed] [Google Scholar]
- 13.Brownson RC, Jones E. Bridging the gap: translating research into policy and practice. Prev Med 2009;49:313–5. 10.1016/j.ypmed.2009.06.008 [DOI] [PubMed] [Google Scholar]
- 14.Cyarto EV, Brown WJ, Marshall AL. Retention, adherence and compliance: important considerations for home- and group-based resistance training programs for older adults. J Sci Med Sport 2006;9:402–12. 10.1016/j.jsams.2006.06.020 [DOI] [PubMed] [Google Scholar]
- 15.Sherrington C, Tiedemann A, Fairhall NJ, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 2016;34 Suppl 4 10.1002/14651858.CD012424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lamb SE, Becker C, Gillespie LD, et al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials 2011;12:125 10.1186/1745-6215-12-125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins J, Green S. Cochrane Handbook for systematic reviews of interventions version 5.1.0: the Cochrane collaboration 2011.
- 18.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Almeida TL, Alexander NB, Nyquist LV, et al. Minimally supervised multimodal exercise to reduce falls risk in Economically and educationally disadvantaged older adults. J Aging Phys Act 2013;21:241–59. 10.1123/japa.21.3.241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ansai JH, Aurichio TR, Gonçalves R, et al. Effects of two physical exercise protocols on physical performance related to falls in the oldest old: a randomized controlled trial. Geriatr Gerontol Int 2016;16:492–9. 10.1111/ggi.12497 [DOI] [PubMed] [Google Scholar]
- 21.Arantes PMM, Dias JMD, Fonseca FF, et al. Effect of a program based on balance exercises on gait, functional mobility, fear of falling, and falls in Prefrail older women. Top Geriatr Rehabil 2015;31:113–20. 10.1097/TGR.0000000000000056 [DOI] [Google Scholar]
- 22.Arkkukangas M, Johnson ST, Hellström K, et al. A feasibility study of a randomised controlled trial comparing fall prevention using exercise with or without the support of motivational interviewing. Prev Med Rep 2015;2:134–40. 10.1016/j.pmedr.2015.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ballard JE, McFarland C, Wallace LS, et al. The effect of 15 weeks of exercise on balance, leg strength, and reduction in falls in 40 women aged 65 to 89 years. J Am Med Womens Assoc 2004;59:255–61. [PubMed] [Google Scholar]
- 24.Barker AL, Talevski J, Bohensky MA, et al. Feasibility of Pilates exercise to decrease falls risk: a pilot randomized controlled trial in community-dwelling older people. Clin Rehabil 2016;30:984–96. 10.1177/0269215515606197 [DOI] [PubMed] [Google Scholar]
- 25.Barnett A, et al. Community-Based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing 2003;32:407–14. 10.1093/ageing/32.4.407 [DOI] [PubMed] [Google Scholar]
- 26.Beyer N, Simonsen L, Bülow J, et al. Old women with a recent fall history show improved muscle strength and function sustained for six months after finishing training. Aging Clin Exp Res 2007;19:300–9. 10.1007/BF03324706 [DOI] [PubMed] [Google Scholar]
- 27.Boongird C, Keesukphan P, Phiphadthakusolkul S, et al. Effects of a simple home-based exercise program on fall prevention in older adults: a 12-month primary care setting, randomized controlled trial. Geriatr Gerontol Int 2017;17:2157–63. 10.1111/ggi.13052 [DOI] [PubMed] [Google Scholar]
- 28.Brown A. Functional adaptation to exercise in elderly subjects. Curtin University of Technology, 2002. [Google Scholar]
- 29.Buchner DM, Cress ME, de Lateur BJ, et al. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol A Biol Sci Med Sci 1997;52A:M218–24. 10.1093/gerona/52A.4.M218 [DOI] [PubMed] [Google Scholar]
- 30.Bunout D, Barrera G, Avendaño M, et al. Results of a community-based weight-bearing resistance training programme for healthy Chilean elderly subjects. Age Ageing 2005;34:80–3. 10.1093/ageing/afi005 [DOI] [PubMed] [Google Scholar]
- 31.Campbell AJ, Robertson MC, Gardner MM, et al. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997;315:1065–9. 10.1136/bmj.315.7115.1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carter ND, Khan KM, McKay HA, et al. Community-Based exercise program reduces risk factors for falls in 65- to 75-year-old women with osteoporosis: randomized controlled trial. CMAJ 2002;167:997–1004. [PMC free article] [PubMed] [Google Scholar]
- 33.Cerny K, Blanks R, Mohamed O, et al. The effect of a multidimensional exercise program on strength, range of motion, balance and gait in the well elderly. Gait Posture 1998;7:185–6. 10.1016/S0966-6362(98)90283-1 [DOI] [Google Scholar]
- 34.Clegg A, Barber S, Young J, et al. The home-based older people's exercise (hope) trial: a pilot randomised controlled trial of a home-based exercise intervention for older people with frailty. Age Ageing 2014;43:687–95. 10.1093/ageing/afu033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clemson L, Singh MF, Bundy A, et al. Life pilot study: a randomised trial of balance and strength training embedded in daily life activity to reduce falls in older adults. Aust Occup Ther J 2010;57:42–50. 10.1111/j.1440-1630.2009.00848.x [DOI] [PubMed] [Google Scholar]
- 36.Clemson L, Fiatarone Singh MA, Bundy A, et al. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the life study): randomised parallel trial. BMJ 2012;345:e4547 10.1136/bmj.e4547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cornillon E, Blanchon MA, Ramboatsisetraina P, et al. [Effectiveness of falls prevention strategies for elderly subjects who live in the community with performance assessment of physical activities (before-after)]. Ann Readapt Med Phys 2002;45:493–504. 10.1016/s0168-6054(02)00302-1 [DOI] [PubMed] [Google Scholar]
- 38.Dadgari A, Aizan Hamid T, Hakim MN, et al. Randomized control trials on Otago exercise program (OEP) to reduce falls among elderly community dwellers in Shahroud, Iran. Iran Red Crescent Med J 2016;18:e26340 10.5812/ircmj.26340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dangour AD, Albala C, Allen E, et al. Effect of a nutrition supplement and physical activity program on pneumonia and walking capacity in Chilean older people: a factorial cluster randomized trial. PLoS Med 2011;8:e1001023 10.1371/journal.pmed.1001023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Day L, Fildes B, Gordon I, et al. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002;325:128 10.1136/bmj.325.7356.128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Day L, Hill KD, Stathakis VZ, et al. Impact of tai-chi on falls among preclinically disabled older people. A randomized controlled trial. J Am Med Dir Assoc 2015;16:420–6. 10.1016/j.jamda.2015.01.089 [DOI] [PubMed] [Google Scholar]
- 42.Duque G, Boersma D, Loza-Diaz G, et al. Effects of balance training using a virtual-reality system in older fallers. Clin Interv Aging 2013;8:257–63. 10.2147/CIA.S41453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ebrahim S, Thompson PW, Baskaran V, et al. Randomized placebo-controlled trial of brisk walking in the prevention of postmenopausal osteoporosis. Age Ageing 1997;26:253–60. 10.1093/ageing/26.4.253 [DOI] [PubMed] [Google Scholar]
- 44.El-Khoury F, Cassou B, Latouche A, et al. Effectiveness of two year balance training programme on prevention of fall induced injuries in at risk women aged 75-85 living in community: Ossébo randomised controlled trial. BMJ 2015;351 10.1136/bmj.h3830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Efficacy of home-based resistance training in frail elders Abstracts of the 16th Congress of the International association of gerontology. Bedford Park, South Australia: World Congress of Gerontology Inc, 1997. [Google Scholar]
- 46.Freiberger E, Menz HB, Abu-Omar K, et al. Preventing falls in physically active community-dwelling older people: a comparison of two intervention techniques. Gerontology 2007;53:298–305. 10.1159/000103256 [DOI] [PubMed] [Google Scholar]
- 47.Gill TM, Pahor M, Guralnik JM, et al. Effect of structured physical activity on prevention of serious fall injuries in adults aged 70-89: randomized clinical trial (life study). BMJ 2016;352 10.1136/bmj.i245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grahn Kronhed A-C, Hallberg I, Ödkvist L, et al. Effect of training on health-related quality of life, pain and falls in osteoporotic women. Adv Physiother 2009;11:154–65. 10.1080/14038190902896659 [DOI] [Google Scholar]
- 49.Gschwind YJ, Eichberg S, Ejupi A, et al. ICT-based system to predict and prevent falls (iStoppFalls): results from an international multicenter randomized controlled trial. Eur Rev Aging Phys Act 2015;12 10.1186/s11556-015-0155-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haines TP, Russell T, Brauer SG, et al. Effectiveness of a video-based exercise programme to reduce falls and improve health-related quality of life among older adults discharged from Hospital: a pilot randomized controlled trial. Clin Rehabil 2009;23:973–85. 10.1177/0269215509338998 [DOI] [PubMed] [Google Scholar]
- 51.Halvarsson A, Franzén E, Farén E, et al. Long-Term effects of new progressive group balance training for elderly people with increased risk of falling – a randomized controlled trial. Clin Rehabil 2013;27:450–8. 10.1177/0269215512462908 [DOI] [PubMed] [Google Scholar]
- 52.Halvarsson A, Oddsson L, Franzén E, et al. Long-Term effects of a progressive and specific balance-training programme with multi-task exercises for older adults with osteoporosis: a randomized controlled study. Clin Rehabil 2016;30:1049–59. 10.1177/0269215515605553 [DOI] [PubMed] [Google Scholar]
- 53.Hamrick I, Mross P, Christopher N, et al. Yoga's effect on falls in rural, older adults. Complement Ther Med 2017;35:57–63. 10.1016/j.ctim.2017.09.007 [DOI] [PubMed] [Google Scholar]
- 54.Hauer K, Rost B, Rütschle K, et al. Exercise training for rehabilitation and secondary prevention of falls in geriatric patients with a history of injurious falls. J Am Geriatr Soc 2001;49:10–20. 10.1046/j.1532-5415.2001.49004.x [DOI] [PubMed] [Google Scholar]
- 55.Helbostad JL, Sletvold O, Moe-Nilssen R. Effects of home exercises and group training on functional abilities in home-dwelling older persons with mobility and balance problems. A randomized study. Aging Clin Exp Res 2004;16:113–21. 10.1007/BF03324539 [DOI] [PubMed] [Google Scholar]
- 56.Hirase T, Inokuchi S, Matsusaka N, et al. Effects of a balance training program using a foam rubber pad in community-based older adults. Journal of Geriatric Physical Therapy 2015;38:62–70. 10.1519/JPT.0000000000000023 [DOI] [PubMed] [Google Scholar]
- 57.Huang H-C, Liu C-Y, Huang Y-T, et al. Community-based interventions to reduce falls among older adults in Taiwan - long time follow-up randomised controlled study. J Clin Nurs 2010;19:959–68. 10.1111/j.1365-2702.2009.02834.x [DOI] [PubMed] [Google Scholar]
- 58.Hwang H-F, Chen S-J, Lee-Hsieh J, et al. Effects of home-based tai chi and lower extremity training and self-practice on falls and functional outcomes in older fallers from the emergency department-a randomized controlled trial. J Am Geriatr Soc 2016;64:518–25. 10.1111/jgs.13952 [DOI] [PubMed] [Google Scholar]
- 59.Iliffe S, Kendrick D, Morris R, et al. Multicentre cluster randomised trial comparing a community group exercise programme and home-based exercise with usual care for people aged 65 years and over in primary care. Health Technol Assess 2014;18:1–106. 10.3310/hta18490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Irez GB, Ozdemir RA, Evin R, et al. Integrating Pilates exercise into an exercise program for 65+ year-old women to reduce falls. J Sports Sci Med 2011;10:105–11. [PMC free article] [PubMed] [Google Scholar]
- 61.Iwamoto J, Suzuki H, Tanaka K, et al. Preventative effect of exercise against falls in the elderly: a randomized controlled trial. Osteoporos Int 2009;20:1233–40. 10.1007/s00198-008-0794-9 [DOI] [PubMed] [Google Scholar]
- 62.Kamide N, Shiba Y, Shibata H. Effects on balance, falls, and bone mineral density of a home-based exercise program without home visits in community-dwelling elderly women: a randomized controlled trial. J Physiol Anthropol 2009;28:115–22. 10.2114/jpa2.28.115 [DOI] [PubMed] [Google Scholar]
- 63.Karinkanta S, Heinonen A, Sievänen H, et al. A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: randomized, controlled trial. Osteoporos Int 2007;18:453–62. 10.1007/s00198-006-0256-1 [DOI] [PubMed] [Google Scholar]
- 64.Kemmler W, von Stengel S, Engelke K, et al. Exercise effects on bone mineral density, falls, coronary risk factors, and health care costs in older women: the randomized controlled senior fitness and prevention (SEFIP) study. Arch Intern Med 2010;170:179–85. 10.1001/archinternmed.2009.499 [DOI] [PubMed] [Google Scholar]
- 65.Kerse N, Hayman KJ, Moyes SA, et al. Home-Based activity program for older people with depressive symptoms: DeLLITE-a randomized controlled trial. The Annals of Family Medicine 2010;8:214–23. 10.1370/afm.1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kim H, Yoshida H, Suzuki T. Falls and fractures in participants and excluded non-participants of a fall prevention exercise program for elderly women with a history of falls: 1-year follow-up study. Geriatr Gerontol Int 2014;14:285–92. 10.1111/ggi.12095 [DOI] [PubMed] [Google Scholar]
- 67.Korpelainen R, Keinänen-Kiukaanniemi S, Heikkinen J, et al. Effect of exercise on extraskeletal risk factors for hip fractures in elderly women with low BMD: a population-based randomized controlled trial. J Bone Miner Res 2006;21:772–9. 10.1359/jbmr.060116 [DOI] [PubMed] [Google Scholar]
- 68.Kovács E, Prókai L, Mészáros L, et al. Adapted physical activity is beneficial on balance, functional mobility, quality of life and fall risk in community-dwelling older women: a randomized single-blinded controlled trial. Eur J Phys Rehabil Med 2013;49:301–10. [PubMed] [Google Scholar]
- 69.Kwok BC, Pua YH. Effects of WiiActive exercises on fear of falling and functional outcomes in community-dwelling older adults: a randomised control trial. Age Ageing 2016;45:621–7. 10.1093/ageing/afw108 [DOI] [PubMed] [Google Scholar]
- 70.Kyrdalen IL, Moen K, Røysland AS, et al. The Otago exercise program performed as group training versus home training in fall-prone older people: a randomized controlled trial. Physiother. Res. Int. 2014;19:108–16. 10.1002/pri.1571 [DOI] [PubMed] [Google Scholar]
- 71.LaStayo P, Marcus R, Dibble L, et al. Eccentric versus traditional resistance exercise for older adult fallers in the community: a randomized trial within a multi-component fall reduction program. BMC Geriatr 2017;17:149 10.1186/s12877-017-0539-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Latham NK, Anderson CS, Lee A, et al. A randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail older people: the frailty interventions trial in elderly subjects (fitness). J Am Geriatr Soc 2003;51:291–9. 10.1046/j.1532-5415.2003.51101.x [DOI] [PubMed] [Google Scholar]
- 73.Lehtola S, Hanninen L, Paatalo M. The incidence of falls during a six month exercise trial and four month follow-up among home dwelling persons aged 70–75 years. Liikunta Tiede 2000;6:41–7. [Google Scholar]
- 74.Li F, Harmer P, Fisher KJ, et al. Tai chi and fall reductions in older adults: a randomized controlled trial. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2005;60:187–94. 10.1093/gerona/60.2.187 [DOI] [PubMed] [Google Scholar]
- 75.Lin M-R, Wolf SL, Hwang H-F, et al. A randomized, controlled trial of fall prevention programs and quality of life in older fallers. J Am Geriatr Soc 2007;55:499–506. 10.1111/j.1532-5415.2007.01146.x [DOI] [PubMed] [Google Scholar]
- 76.Liston MB, Alushi L, Bamiou D-E, et al. Feasibility and effect of supplementing a modified Otago intervention with multisensory balance exercises in older people who fall: a pilot randomized controlled trial. Clin Rehabil 2014;28:784–93. 10.1177/0269215514521042 [DOI] [PubMed] [Google Scholar]
- 77.Liu-Ambrose T, Khan KM, Eng JJ, et al. Resistance and Agility training reduce fall risk in women aged 75 to 85 with low bone mass: a 6-month randomized, controlled Trial*. J Am Geriatr Soc 2004;52:657–65. 10.1111/j.1532-5415.2004.52200.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Liu-Ambrose T, Donaldson MG, Ahamed Y, et al. Otago home-based strength and balance retraining improves executive functioning in older fallers: a randomized controlled trial. J Am Geriatr Soc 2008;56:1821–30. 10.1111/j.1532-5415.2008.01931.x [DOI] [PubMed] [Google Scholar]
- 79.Logghe IHJ, Zeeuwe PEM, Verhagen AP, et al. Lack of effect of tai chi Chuan in preventing falls in elderly people living at home: a randomized clinical trial. J Am Geriatr Soc 2009;57:70–5. 10.1111/j.1532-5415.2008.02064.x [DOI] [PubMed] [Google Scholar]
- 80.Lord SR, Ward JA, Williams P, et al. The effect of a 12-month exercise trial on balance, strength, and falls in older women: a randomized controlled trial. J Am Geriatr Soc 1995;43:1198–206. 10.1111/j.1532-5415.1995.tb07394.x [DOI] [PubMed] [Google Scholar]
- 81.Lord SR, Castell S, Corcoran J, et al. The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: a randomized, controlled trial. J Am Geriatr Soc 2003;51:1685–92. 10.1046/j.1532-5415.2003.51551.x [DOI] [PubMed] [Google Scholar]
- 82.Lurie JD, Zagaria AB, Pidgeon DM, et al. Pilot comparative effectiveness study of surface perturbation treadmill training to prevent falls in older adults. BMC Geriatr 2013;13:49 10.1186/1471-2318-13-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Luukinen H, Lehtola S, Jokelainen J, et al. Pragmatic exercise-oriented prevention of falls among the elderly: a population-based, randomized, controlled trial. Prev Med 2007;44:265–71. 10.1016/j.ypmed.2006.09.011 [DOI] [PubMed] [Google Scholar]
- 84.Madureira MM, Takayama L, Gallinaro AL, et al. Balance training program is highly effective in improving functional status and reducing the risk of falls in elderly women with osteoporosis: a randomized controlled trial. Osteoporos Int 2007;18:419–25. 10.1007/s00198-006-0252-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.McMurdo MET, Mole PA, Paterson CR. Controlled trial of weight bearing exercise in older women in relation to bone density and falls. BMJ 1997;314:569 10.1136/bmj.314.7080.569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Means KM, Rodell DE, O'Sullivan PS. Balance, mobility, and falls among community-dwelling elderly persons: effects of a rehabilitation exercise program. Am J Phys Med Rehabil 2005;84:238–50. 10.1097/01.phm.0000151944.22116.5a [DOI] [PubMed] [Google Scholar]
- 87.Merom D, Mathieu E, Cerin E, et al. Social dancing and incidence of falls in older adults: a cluster randomised controlled trial. PLoS Med 2016;13:e1002112 10.1371/journal.pmed.1002112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mikó I, Szerb I, Szerb A, et al. Effectiveness of balance training programme in reducing the frequency of falling in established osteoporotic women: a randomized controlled trial. Clin Rehabil 2017;31:217–24. 10.1177/0269215516628616 [DOI] [PubMed] [Google Scholar]
- 89.Mirelman A, Rochester L, Maidan I, et al. Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): a randomised controlled trial. The Lancet 2016;388:1170–82. 10.1016/S0140-6736(16)31325-3 [DOI] [PubMed] [Google Scholar]
- 90.Morgan RO, Virnig BA, Duque M, et al. Low-Intensity exercise and reduction of the risk for falls among at-risk elders. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2004;59:M1062–7. 10.1093/gerona/59.10.M1062 [DOI] [PubMed] [Google Scholar]
- 91.Morone G, Paolucci T, Luziatelli S, et al. Wii fit is effective in women with bone loss condition associated with balance disorders: a randomized controlled trial. Aging Clin Exp Res 2016;28:1187–93. 10.1007/s40520-016-0578-6 [DOI] [PubMed] [Google Scholar]
- 92.Morrison S, Simmons R, Colberg SR, et al. Supervised balance training and Wii Fit–Based exercises lower falls risk in older adults with type 2 diabetes. J Am Med Dir Assoc 2018;19:185.e7–185.e13. 10.1016/j.jamda.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 93.Ng TP, Feng L, Nyunt MSZ, et al. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: a randomized controlled trial. Am J Med 2015;128:1225–36. 10.1016/j.amjmed.2015.06.017 [DOI] [PubMed] [Google Scholar]
- 94.Nitz JC, Choy NL. The efficacy of a specific balance-strategy training programme for preventing falls among older people: a pilot randomised controlled trial. Age Ageing 2004;33:52–8. 10.1093/ageing/afh029 [DOI] [PubMed] [Google Scholar]
- 95.Okubo Y, Osuka Y, Jung S, et al. Walking can be more effective than balance training in fall prevention among community-dwelling older adults. Geriatr Gerontol Int 2016;16:118–25. 10.1111/ggi.12444 [DOI] [PubMed] [Google Scholar]
- 96.Park H, Kim KJ, Komatsu T, et al. Effect of combined exercise training on bone, body balance, and gait ability: a randomized controlled study in community-dwelling elderly women. J Bone Miner Metab 2008;26:254–9. 10.1007/s00774-007-0819-z [DOI] [PubMed] [Google Scholar]
- 97.Reinsch S, MacRae P, Lachenbruch PA, et al. Attempts to prevent falls and injury: a prospective community study. Gerontologist 1992;32:450–6. 10.1093/geront/32.4.450 [DOI] [PubMed] [Google Scholar]
- 98.Resnick B. Testing the effect of the WALC intervention on exercise adherence in older adults. J Gerontol Nurs 2002;28:40–9. 10.3928/0098-9134-20020601-10 [DOI] [PubMed] [Google Scholar]
- 99.Robertson MC, et al. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: randomised controlled trial. BMJ 2001;322:697–701. 10.1136/bmj.322.7288.697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rubenstein LZ, Josephson KR, Trueblood PR, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2000;55:M317–21. 10.1093/gerona/55.6.M317 [DOI] [PubMed] [Google Scholar]
- 101.Sakamoto K, Endo N, Harada A, et al. Why not use your own body weight to prevent falls? A randomized, controlled trial of balance therapy to prevent falls and fractures for elderly people who can stand on one leg for ≤15s. Journal of Orthopaedic Science 2013;18:110–20. 10.1007/s00776-012-0328-3 [DOI] [PubMed] [Google Scholar]
- 102.Sales M, Polman R, Hill KD, et al. A novel exercise initiative for seniors to improve balance and physical function. J Aging Health 2017;29:1424–43. 10.1177/0898264316662359 [DOI] [PubMed] [Google Scholar]
- 103.Sherrington C, Lord SR, Vogler CM, et al. A post-hospital home exercise program improved mobility but increased falls in older people: a randomised controlled trial. PLoS One 2014;9:e104412 10.1371/journal.pone.0104412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Shigematsu R, Okura T, Nakagaichi M, et al. Square-stepping exercise and fall risk factors in older adults: a single-blind, randomized controlled trial. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2008;63:76–82. 10.1093/gerona/63.1.76 [DOI] [PubMed] [Google Scholar]
- 105.Siegrist M, Freiberger E, Geilhof B, et al. Fall prevention in a primary care setting: the effects of a targeted complex exercise intervention in a cluster randomized trial. Dtsch Arztebl Int 2016;113:365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Skelton D, Dinan S, Campbell M, et al. Tailored group exercise (falls management exercise — fame) reduces falls in community-dwelling older frequent fallers (an RCT). Age Ageing 2005;34:636–9. 10.1093/ageing/afi174 [DOI] [PubMed] [Google Scholar]
- 107.Smulders E, Weerdesteyn V, Groen BE, et al. Efficacy of a short multidisciplinary falls prevention program for elderly persons with osteoporosis and a fall history: a randomized controlled trial. Arch Phys Med Rehabil 2010;91:1705–11. 10.1016/j.apmr.2010.08.004 [DOI] [PubMed] [Google Scholar]
- 108.Steadman J, Donaldson N, Kalra L. A randomized controlled trial of an enhanced balance training program to improve mobility and reduce falls in elderly patients. J Am Geriatr Soc 2003;51:847–52. 10.1046/j.1365-2389.2003.51268.x [DOI] [PubMed] [Google Scholar]
- 109.Suzuki T, Kim H, Yoshida H, et al. Randomized controlled trial of exercise intervention for the prevention of falls in community-dwelling elderly Japanese women. J Bone Miner Metab 2004;22:602–11. 10.1007/s00774-004-0530-2 [DOI] [PubMed] [Google Scholar]
- 110.Taylor D, Hale L, Schluter P, et al. Effectiveness of tai chi as a community-based falls prevention intervention: a randomized controlled trial. J Am Geriatr Soc 2012;60:841–8. 10.1111/j.1532-5415.2012.03928.x [DOI] [PubMed] [Google Scholar]
- 111.Trombetti A, Hars M, Herrmann FR, et al. Effect of Music-Based Multitask training on gait, balance, and fall risk in elderly people. Arch Intern Med 2011;171:525–33. 10.1001/archinternmed.2010.446 [DOI] [PubMed] [Google Scholar]
- 112.Uusi-Rasi K, Patil R, Karinkanta S, et al. Exercise and vitamin D in fall prevention among older women: a randomized clinical trial. JAMA Intern Med 2015;175:703–11. 10.1001/jamainternmed.2015.0225 [DOI] [PubMed] [Google Scholar]
- 113.Verrusio W, Gianturco V, Cacciafesta M, et al. Fall prevention in the young old using an exoskeleton human body posturizer: a randomized controlled trial. Aging Clin Exp Res 2017;29:207–14. 10.1007/s40520-016-0540-7 [DOI] [PubMed] [Google Scholar]
- 114.Vogler CM, Sherrington C, Ogle SJ, et al. Reducing risk of falling in older people discharged from Hospital: a randomized controlled trial comparing seated exercises, weight-bearing exercises, and social visits. Arch Phys Med Rehabil 2009;90:1317–24. 10.1016/j.apmr.2009.01.030 [DOI] [PubMed] [Google Scholar]
- 115.Voukelatos A, Cumming RG, Lord SR, et al. A randomized, controlled trial of tai chi for the prevention of falls: the central Sydney tai chi trial. J Am Geriatr Soc 2007;55:1185–91. 10.1111/j.1532-5415.2007.01244.x [DOI] [PubMed] [Google Scholar]
- 116.Voukelatos A, Merom D, Sherrington C, et al. The impact of a home-based walking programme on falls in older people: the easy steps randomised controlled trial. Age Ageing 2015;44:377–83. 10.1093/ageing/afu186 [DOI] [PubMed] [Google Scholar]
- 117.Weerdesteyn V, Rijken H, Geurts ACH, et al. A five-week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerontology 2006;52:131–41. 10.1159/000091822 [DOI] [PubMed] [Google Scholar]
- 118.Wolf SL, Barnhart HX, Kutner NG, et al. Reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training. Atlanta FICSIT group. frailty and injuries: cooperative studies of intervention techniques. J Am Geriatr Soc 1996;44:489–97. 10.1111/j.1532-5415.1996.tb01432.x [DOI] [PubMed] [Google Scholar]
- 119.Wolf SL, Sattin RW, Kutner M, et al. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc 2003;51:1693–701. 10.1046/j.1532-5415.2003.51552.x [DOI] [PubMed] [Google Scholar]
- 120.Woo J, Hong A, Lau E, et al. A randomised controlled trial of tai chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing 2007;36:262–8. 10.1093/ageing/afm005 [DOI] [PubMed] [Google Scholar]
- 121.Wu G, Keyes L, Callas P, et al. Comparison of telecommunication, community, and home-based tai chi exercise programs on compliance and effectiveness in elders at risk for falls. Arch Phys Med Rehabil 2010;91:849–56. 10.1016/j.apmr.2010.01.024 [DOI] [PubMed] [Google Scholar]
- 122.Yamada M, Aoyama T, Arai H, et al. Complex obstacle negotiation exercise can prevent falls in community-dwelling elderly Japanese aged 75 years and older. Geriatr Gerontol Int 2012;12:461–7. 10.1111/j.1447-0594.2011.00794.x [DOI] [PubMed] [Google Scholar]
- 123.Yamada M, Higuchi T, Nishiguchi S, et al. Multitarget stepping program in combination with a standardized multicomponent exercise program can prevent falls in community-dwelling older adults: a randomized, controlled trial. J Am Geriatr Soc 2013;61:1669–75. 10.1111/jgs.12453 [DOI] [PubMed] [Google Scholar]
- 124.Yamada M, Tanaka B, Nagai K, et al. Trail-walking exercise and fall risk factors in community-dwelling older adults: preliminary results of a randomized controlled trial. J Am Geriatr Soc 2010;58:1946–51. 10.1111/j.1532-5415.2010.03059.x [DOI] [PubMed] [Google Scholar]
- 125.Yang XJ, Hill K, Moore K, et al. Effectiveness of a targeted exercise intervention in reversing older people's mild balance dysfunction: a randomized controlled trial. Phys Ther 2012;92:24–37. 10.2522/ptj.20100289 [DOI] [PubMed] [Google Scholar]
- 126.Montgomery K. How doctors think: clinical judgement and the practice of medicine. New York, NY: Oxford University Press, 2006. [Google Scholar]
- 127.Power V, Clifford AM. Characteristics of optimum falls prevention exercise programmes for community-dwelling older adults using the FITT principle. Eur Rev Aging Phys Act 2013;10:95–106. 10.1007/s11556-012-0108-2 [DOI] [Google Scholar]
- 128.Bunn F, Dickinson A, Barnett-Page E, et al. A systematic review of older people's perceptions of facilitators and barriers to participation in falls-prevention interventions. Ageing Soc 2008;28:449–72. 10.1017/S0144686X07006861 [DOI] [Google Scholar]
- 129.Jang H, Clemson L, Lovarini M, et al. Cultural influences on exercise participation and fall prevention: a systematic review and narrative synthesis. Disabil Rehabil 2016;38:724–32. 10.3109/09638288.2015.1061606 [DOI] [PubMed] [Google Scholar]
- 130.McPhate L, Simek EM, Haines TP. Program-related factors are associated with adherence to group exercise interventions for the prevention of falls: a systematic review. J Physiother 2013;59:81–92. 10.1016/S1836-9553(13)70160-7 [DOI] [PubMed] [Google Scholar]
- 131.Wade DT, Smeets RJEM, Verbunt JA. Research in rehabilitation medicine: methodological challenges. J Clin Epidemiol 2010;63:699–704. 10.1016/j.jclinepi.2009.07.010 [DOI] [PubMed] [Google Scholar]
- 132.Stiggelbout AM, Weijden TVd, Wit MPTD, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ 2012;344 10.1136/bmj.e256 [DOI] [PubMed] [Google Scholar]
- 133.He W, Goodkind D, Kowal P, et al. An ageingg world: 2015. Washington DC: United States Census Bureau, 2015. [Google Scholar]
- 134.Chang VC, Do MT. Risk factors for falls among seniors: implications of gender. Am J Epidemiol 2015;181:521–31. 10.1093/aje/kwu268 [DOI] [PubMed] [Google Scholar]
- 135.Schulz KF, Altman DG, Moher D, et al. Consort 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hannan MT, Gagnon MM, Aneja J, et al. Optimizing the tracking of falls in studies of older participants: comparison of quarterly telephone recall with monthly falls calendars in the mobilize Boston study. Am J Epidemiol 2010;171:1031–6. 10.1093/aje/kwq024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lamb SE, Jørstad-Stein EC, Hauer K, et al. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc 2005;53:1618–22. 10.1111/j.1532-5415.2005.53455.x [DOI] [PubMed] [Google Scholar]
- 138.Canning CG, Allen NE, Bloem BR, et al. Interventions for preventing falls in Parkinson's disease. Cochrane Database Syst Rev 2015;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Verheyden G, Weerdesteyn V, Pickering RM, et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev 2013;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2019-000663supp001.pdf (61.8KB, pdf)
bmjsem-2019-000663supp002.pdf (77.2KB, pdf)
bmjsem-2019-000663supp003.pdf (121.6KB, pdf)
bmjsem-2019-000663supp004.pdf (102.5KB, pdf)
bmjsem-2019-000663supp005.pdf (72.9KB, pdf)