Abstract
Nonalcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver disease in the developed world, with a global prevalence of around 25%. NAFLD is considered to be the hepatic manifestation of metabolic syndrome and is strongly associated with obesity, insulin resistance and dyslipidemia. Insulin resistance plays a pivotal role in the development of NAFLD-related dyslipidemia, which ultimately increases the risk of premature cardiovascular diseases, a leading cause of morbidity and mortality in patients with NAFLD. Insulin affects hepatic glucose and lipid metabolism by hepatic or extrahepatic pathways. Aside from insulin resistance, several other factors also contribute to the pathogenesis of atherogenic dyslipidemia in patients with NAFLD. These include diet composition, gut microbiota and genetic factors, to name a few. The identification of potentially modifiable risk factors of NAFLD is of importance, so as to target those who may benefit from lifestyle changes and to help develop targeted therapies that decrease the risk of cardiovascular diseases in patients with NAFLD.
Keywords: Nonalcoholic fatty liver disease, Insulin resistance, Cardiovascular diseases, Dyslipidemia
Introduction
Nonalcoholic fatty liver disease (NAFLD) is a clinical spectrum of disease severity, ranging from isolated fatty infiltration of the liver (simple hepatic steatosis) to lobular inflammation, balloon degeneration, hepatic fibrosis, and cirrhosis. With epidemiological shifts due to lifestyle changes and modernization, NAFLD has become the most common cause of chronic liver disease in the developed world, with an estimated global prevalence of around 25%.1–3 NAFLD may be associated with features of metabolic syndrome, including obesity, insulin resistance, and atherogenic dyslipidemia, predisposing to an increased risk of progressive liver damage that can lead to nonalcoholic steatohepatitis (commonly known as NASH), cirrhosis, diabetes and premature cardiovascular disease (CVD).4–9 Insulin resistance plays a major role in the development of atherogenic dyslipidemia in NAFLD and the subsequent development of premature CVD.10 In this article, we will review the role of insulin in hepatic glucose and lipid metabolism, the mechanisms that may lead to NAFLD-related dyslipidemia and ectopic lipid deposition, and how these factors contribute to cardiovascular morbidity and mortality.
Hepatic glucose and lipid metabolism
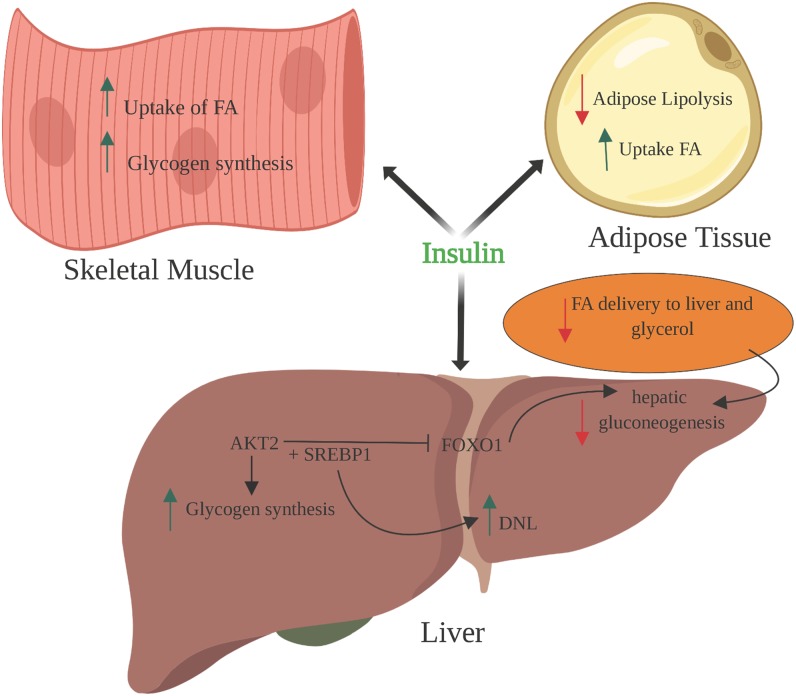
Liver plays a central role in the metabolism of carbohydrates, lipids and proteins under states of caloric excess and starvation. A key regulator of these homeostatic processes is insulin, which exerts its effects on hepatic glucose and lipid metabolism through a variety of different hepatic (direct) and extrahepatic (indirect) pathways. Fig. 1 illustrates these important pathways.
Fig. 1. Effects of Insulin on Glucose and Lipid metabolism.
Hepatic glucose metabolism
Direct insulin-mediated regulation of hepatic glucose metabolism begins with the activation of insulin receptor tyrosine kinase (IRTK), phosphoinositide-dependent kinase-1 (referred to as PDK1) and the mammalian target of rapamycin (referred to as mTORC)-2, and ends with protein kinase B (known as AKT) phosphorylation.11–13 Insulin, via this pathway, decreases hepatic gluconeogenesis by activating hepatocyte insulin receptors, which in turn trigger hepatic glycogen synthesis and downregulate the transcription of gluconeogenic enzymes through forkhead box protein O1 (referred to as FOXO1) phosphorylation.14,15 Indirectly, insulin further inhibits lipolysis in white adipose tissue, resulting in decreased fatty acid delivery to the liver by reducing hepatic acetyl-CoA content, an allosteric activator of pyruvate carboxylase. This occurs in conjunction with insulin-mediated suppression of glycerol conversion to glucose and delivery to the liver.16–18 The direct and indirect actions of insulin may play a role in different metabolic states, with glycogen replete states favoring direct insulin action and glycogen deplete states favoring the indirect effects of insulin.19–20
Hepatic lipid metabolism
Insulin directly regulates hepatic lipid metabolism by increasing mRNA expression of nuclear transcription factors, such as sterol regulatory element-binding protein-1c (referred to as SREBP-1c), which play a key role in the regulation of de novo lipogenesis (DNL) and triglyceride synthesis. This effect is amplified by an insulin-mediated increase in mTORC1 activity, which also activates SREBP1c mRNA expression and uncouples lipogenesis from gluconeogenesis. Indirectly, insulin acts peripherally by stimulating the uptake of fatty acids into muscle and adipose tissue that are produced by lipoprotein lipase-mediated triglyceride hydrolysis.21
Atherogenic dyslipidemia and ectopic lipid deposition
Atherogenic dyslipidemia and ectopic lipid deposition in NAFLD are multifactorial and occur broadly as a result of diet, skeletal muscle, hepatic and adipose insulin resistance, and genetic factors. Table 1 summarizes these factors.
Table 1. Summary of factors associated with atherogenic dyslipidemia in NAFLD.
| Factors involved in atherogenic dyslipidemia | Summary |
| Dietary content | Increases DNL and increases levels of hepatic inflammation |
| Skeletal insulin resistance | Increases hepatic DNL |
| Liver insulin resistance | Increases hepatic DNL and ectopic lipid deposition |
| Adipose insulin resistance | Increases inflammation, lipolysis, and incomplete fatty acid oxidation |
| Genetic factors | Unclear, but thought to be affected by genetic alterations that predispose to pro-inflammatory and profibrogenic mechanisms |
| Gut microbiota | Increases inflammation and increases production and absorption of gut-derived fatty acids, while also being associated with SIBO |
Abbreviations: DNL, de novo lipogenesis; NAFLD, nonalcoholic fatty liver disease; SIBO, small intestinal bacterial overgrowth.
Dietary content
Diet may strongly influence the development of atherogenic dyslipidemia. Specifically, injurious effects of excess caloric intake are implicated in NAFLD, with one study demonstrating that patients with obesity and NAFLD may consume more calories than healthy lean individuals; in fact, a study examining patients with metabolic syndrome demonstrated a 3-fold higher rate of DNL.22,23 Furthermore, studies have shown that short-term caloric restriction can normalize hepatic insulin sensitivity and reverse NAFLD, thereby suggesting a causal role of ectopic lipids in insulin resistant states, such as NAFLD.24–26 It should be noted that excess fatty acid reservoirs (due to high-fat diets or increased caloric intake) promote hepatic lipid synthesis despite the presence of hepatic insulin resistance, as studies have shown that hepatic triglyceride synthesis is dependent on the rate of fatty acid delivery and independent of hepatocellular insulin signaling; on the contrary, DNL is insulin-dependent.27
In addition to excess caloric consumption and high-fat diets, simple sugars, such as fructose, can also promote lipogenesis. Fructose is exclusively metabolized by the liver and thus, is converted into triglycerides via DNL. At the cellular level, fructose and glucose both increase SREBP1c expression and enlist lipogenesis-favoring transcription factors, such as carbohydrate response element binding protein (ChREBP), peroxisome proliferator-activated receptor (referred to as PPARγ) coactivator 1-β, and liver X-receptor. Fructose-containing beverages have also been associated with the development of hyperlipidemia and insulin resistance.28,29 High-fructose diets also reduce PPARα activity and stimulate the expression of inflammatory regulators, such as nuclear factor kappa-light-chain-enhancer of activated B cells (referred to as NF-κB) and c-Jun N-terminal kinases (referred to as JNKs) which inhibit the phosphorylation of insulin receptor substrate-1 (referred to as IRS-1). This leads to insulin resistance and intrahepatic inflammation. Indeed, this is evident in rats that develop hepatic steatosis and hepatic fibrosis when fed high-fructose diets.30–32 To this end, multiple studies have demonstrated that diets with high saturated fat and simple carbohydrate content can significantly predispose individuals to a higher risk for ectopic lipid deposition and atherogenic dyslipidemia despite hepatic insulin resistance.33–35
Insulin resistance
The human body encompasses complex metabolic pathways that are fundamental to the interplay between glucose and insulin at the molecular level. Dysfunction of this interplay in states of nutritional imbalance is evident in metabolic syndrome. The inability of insulin to promote glucose uptake in muscle and the suppression of gluconeogenesis in the liver leads to a progressive reduction in beta cell function and ultimately insulin resistance. Insulin resistance plays a major role in the development of NAFLD and atherogenic dyslipidemia, and can manifest in multiple tissues, including skeletal muscle, liver, and adipose.36 Fig. 2 illustrates the mechanism of insulin resistance in skeletal muscle, liver and adipose tissue.
Fig. 2. Mechanism of insulin resistance in skeletal muscle, liver and adipose tissue.
Skeletal muscle insulin resistance
Skeletal muscle insulin resistance is caused by the accumulation of intramyocellular lipid (IMCL) content, which impairs insulin-stimulated glucose transport and glycogen synthesis. Studies examining skeletal muscle in the context of obesity have demonstrated that IMCL content predicts insulin resistance more accurately than fat mass in varying sedentary populations.37–39 Additional studies have further demonstrated that glucose transport is the rate-limiting step responsible for impaired insulin-stimulated glycogen synthesis and that IMCL accumulates when there is a mismatch between lipid oxidation and lipid delivery in muscle cells.16,40–44 These findings suggest an IMCL metabolite, such as diacylglycerol (DAG), acts as a potential mediator of insulin resistance, with high-fat fed and lipid-infused rats demonstrating DAG accumulation.45 Specifically, DAG accumulation has been shown to promote increased protein kinase C (PKC) translocation in skeletal muscle, resulting in the phosphorylation of IRS-1 at serine 1101, and this blocks the AKT pathway to cause impaired insulin signaling.46–48 This has been validated in genetic mouse models with IRTK and glucose transporter type 4 (referred to as GLUT4) mutations, which demonstrate a predisposition for hepatic steatosis and increased adiposity.49,50
Furthermore, progression to atherogenic dyslipidemia through increased liver triglyceride synthesis and plasma triglyceride concentrations with reduced high-density lipoprotein concentrations were observed in young, lean healthy humans with skeletal muscle insulin resistance. This illustrates that ingested glucose is diverted to the liver and not utilized by skeletal muscle in insulin-resistant states.49 These results suggest that in insulin responsive states, glucose is stored as muscle and liver glycogen; however, in insulin resistant states, defects in glycogen storage in muscle result in glucose being diverted to the liver. This resultant hyperglycemia and hyperinsulinemia further stimulate the enzymes involved in hepatic DNL, thereby promoting the conversion of glucose into fat. Ultimately, this increased plasma triglyceride level is the precursor to atherogenic dyslipidemia that leads to premature CVD and NAFLD.10,19,50
Liver insulin resistance
Many different models hypothesize on the mechanisms of hepatic insulin resistance. Initial studies involving patients with generalized lipodystrophy and lipodystrophic mouse models showed significant hepatic insulin resistance and recovery of insulin action post- leptin therapy and fat transplantation respectively.51,52 These findings were augmented by Kim et al.,53 who demonstrated that the overexpression of lipoprotein lipase and short-term high-fat diets in mouse models resulted in hepatic steatosis and hepatic insulin resistance without muscle lipid accumulation or peripheral insulin resistance. This highlights the specific association between ectopic lipid deposition in the liver and hepatic insulin resistance.
At the cellular level, current evidence indicates hepatic insulin resistance may share similarities with skeletal muscle insulin resistance, with evidence supporting a role for DAG accumulation and PKC activation.10,54 Specifically, studies examining fat-fed rats have shown that the intrahepatic accumulation of DAG promotes PKCɛ translocation in the liver and results in the increased phosphorylation of ISR-1 at threonine (Thr) 1160 (Thr1150 in mice). This subsequently results in impaired IRTK activation.55–59 Furthermore, these findings have been validated in studies in human patients undergoing bariatric surgery. Lipidomic analysis in these patients demonstrate increases in specific lipid metabolites, such as DAGs, while other studies show that hepatic DAG content and PKCɛ activity are the strongest predictors of insulin sensitivity.
These studies did not demonstrate any association between insulin sensitivity and other factors implicated in hepatic insulin resistance, such as ceramide content, endoplasmic reticulum stress markers, or inflammatory cytokine concentrations.60–63 Studies with mice lacking glycogen synthase demonstrate increased lipogenesis and NAFLD in the presence of hepatic insulin resistance.19,64 These findings may suggest a mechanism by which hepatic insulin resistance impairs glycogen synthesis and directs glucose into lipogenic pathways that lead to atherogenic dyslipidemia and the promotion of NAFLD.
Adipose insulin resistance
Insulin primarily functions to suppress lipolysis and promote lipid and glucose uptake in adipocytes. Adipose insulin resistance may be explained by reduced IRTK activity in combination with decreased plasma membrane insulin receptor content. Interestingly, weight loss corrected both adipose insulin resistance and defective adipocyte insulin receptor kinase activity. However, further research is warranted to better understand these mechanisms.54 An important regulator of adipose metabolism is ChREBP. ChREBP is directly related to insulin sensitivity in humans and has been implicated in the synthesis of fatty acid esters that are associated with improved glucose tolerance.65,66 Furthermore, patients with NASH and severe insulin resistance have lower levels of ChREBP on liver biopsy.67 Additionally, adipocytes can secrete adipocytokines, such as leptin and resistin (inflammatory), and adiponectin (anti-inflammatory), which exert their affects through cytokine signaling pathways. These adipocytokines are associated with increased insulin resistance and sensitivity respectively.32,68–71
Other factors that impact ectopic lipid deposition and affect the role of insulin in adipose lipolysis suppression include inflammatory agents involved in chemokine signaling, such as tumor necrosis factor (referred to as TNF)-alpha, interleukin (referred to as IL)-1B and interferon gamma (referred to as IFNγ), central nervous system-mediated pathways involving the hypothalamus, and reactive oxygen species produced as a result of increased mitochondrial fat oxidation.72–80 Conversely, abnormal hepatic mitochondrial function demonstrated in steatohepatitis can also result in reactive oxygen species due to the incomplete oxidation of fatty acids, which impairs insulin signaling.81 This resultant subclinical inflammation plays a role in the pathogenesis of NAFLD and may contribute to the development of atherogenic dyslipidemia with high-sensitivity C-reactive protein, a strong cardiovascular risk predictor, also shown to be elevated in patients with NAFLD.82 In combination, these factors all play a role in disrupting the effect of insulin on adipose tissue and may predispose to atherogenic-favoring metabolic states that precede NAFLD.
Genetic factors
Genetic variations in different populations have been shown to influence the risk of NAFLD. Genome-wide association studies have identified multiple genes with numerous polymorphisms that may be responsible for predisposing individuals to NAFLD and atherogenic dyslipidemia. The mechanism by which these genes influence the pathogenesis of NAFLD is unclear and may include inflammatory, profibrogenic, or energy regulating pathways. A recent systematic review highlighted six genes that were replicated in more than one histologically characterized cohort: patatin-like phospholipase domain-containing protein 3 (referred to as PNPLA3), apolipoprotein E (referred to as APOE), superoxide dismutase 2, mitochondrial (referred to as SOD2), TNF, transmembrane 6 superfamily member 2 (referred to as TM6SF2), and glucokinase regulator (referred to as GCKR). Only PNPLA3 (rs738409 variant) was consistently associated with NAFLD susceptibility, from among these genes.83 Polymorphisms in APOC3 have also been associated with NAFLD, which may predispose to dyslipidemia and insulin resistance through the inhibition of lipoprotein lipase activity.84–86 The membrane-bound O-acyltransferase domain-containing 7 gene and transmembrane channel-like 4 gene (referred to as MBOAT7-TMC4) and SCL16A11 are other examples of polymorphisms that may be associated with NAFLD.87–91 Further research is warranted to elucidate the role of genomic variations in NAFLD.
Gut microbiota
The gut microbiota is a growing area of research with regards to the development of metabolic diseases and associations with insulin resistance. Alterations in normal gut flora can lead to the increased production and absorption of gut short-chain fatty acids, altered dietary choline metabolism, altered bile acid pools, and changes in gut permeability.92 These changes are evident in disease states such as small intestinal bacterial overgrowth (commonly known as SIBO), where there is a higher prevalence of NAFLD. Specifically, SIBO induces hepatic expression of toll-like receptor 4 (referred to as TLR4), and release of IL-8 and TNF-alpha.93–95
Pederson et al.96 demonstrated an increased prevalence of Prevotella copri (P. copri) and Bacteriodes vulgatus in insulin-resistant subjects that was supported by mouse models in which P. copri had induced insulin resistance. These findings implicate gut microbiota with insulin resistance and suggest that gut microbiomes can influence disease severity in NAFLD. Further research is underway to better elucidate the role of gut microbiota on the pathogenesis of NAFLD.97,98
Cardiovascular risk
Patients with NAFLD are at an increased risk of mortality from cardiovascular events, including atherosclerosis, systolic or diastolic cardiac dysfunction, conduction abnormalities, and arrhythmias. Subclinical atherosclerosis begins as a result of endothelial dysfunction and can eventually manifest as carotid disease. Carotid disease can manifest as increased carotid intima-media thickness and the presence of carotid plaque on ultrasound, coronary artery calcification evident on computerized tomography, left ventricular hypertrophy seen on electrocardiogram and echocardiogram, and peripheral arterial disease seen on ankle-brachial pressure index.99 A plethora of studies report an association between NAFLD and these markers of preclinical atherosclerosis, with multiple systematic reviews and meta-analyses highlighting the association between NAFLD and carotid-artery intima-media-thickness, coronary artery calcification and endothelial dysfunction, independent of traditional risk factors.100–103
A recent systematic review and meta-analysis by Zhou et al.100 examining 26 observational studies further validated that the presence of NAFLD predisposes to a significantly higher risk of increased carotid artery intima-media thickness/plaques, arterial stiffness, coronary artery calcification and endothelial dysfunction, with odds ratios (95% confidence intervals) of 1.74 (1.47–2.06), 1.56 (1.24–1.96), 1.4 (1.22–1.60), and 3.73 (0.99–14.09) respectively. Case-control studies have also reported strong associations of NAFLD with early changes in left ventricular morphology and/or diastolic dysfunction with insulin resistance a likely key contributor. A prospective one-year follow-up study demonstrated that NAFLD is an independent risk factor for acute heart failure readmission rates.104
Besides cardiac dysfunction, significant ectopic lipid deposition seen in NAFLD can present as an increase in epicardial adipose tissue. Graner et al.105 illustrated this phenomenon in nondiabetic patients with NAFLD who exhibited higher amounts of epicardial adipose tissue. This increased epicardial adipose tissue is associated with sympathovagal imbalances that can predispose to cardiac arrhythmias, such as first degree heart block prolongation and atrial fibrillation.106–111 A prospective cohort study following diabetic patients for 10 years showed that patients with NAFLD developed atrial fibrillation more often than the controls.112 These findings suggest a potential role for screening and surveillance of atherogenic dyslipidemia in patients with NAFLD. Table 2 summarizes these studies mentioned above.
Table 2. Summary of studies examining the associations between NAFLD and cardiovascular disease.
| Study | Study description | Number of studies in meta-analysis | Results |
| Ampuero et al. (2015)99 | Meta-analysis showing an association between NAFLD and subclinical atherosclerosis and CAD | 14 studies were included, of which 10 were aimed at the presence of subclinical atherosclerosis and 4 studies at the presence of CAD | NAFLD showed a higher prevalence of pathological carotid intima-media thickness and carotid plaques; with regards to CAD, subjects with NAFLD were more likely to have CAD |
| Zhou et al. (2018)100 | Meta-analysis showing that NAFLD contributes to subclinical atherosclerosis | 26 studies were included in this meta-analysis, with a total participant size of 85,395 (including 29,493 with NAFLD) | The presence of NAFLD demonstrated a higher risk of increased carotid intima-media thickness/plaques, arterial stiffness, coronary artery calcification, and endothelial dysfunction |
| Jaruvongvanich et al. (2016)101 | Meta-analysis showing an association between NAFLD and coronary artery calcification | 12 studies involving 42,410 subjects were included in this meta-analysis | Mean coronary artery calcium scoring was significantly higher in subjects with NAFLD and higher aspartate aminotransferase levels were also associated with increased subclinical atherosclerosis |
| Fan et al. (2016)102 | Meta-analysis showing an association between NAFLD and impaired endothelial function | 11 observational studies were included, in which endothelial function was compared between NAFLD patients and healthy controls | NAFLD was associated with a reduction in brachial artery flow-mediated dilation |
| Cai et al. (2015)103 | Meta-analysis showing an association between NAFLD and carotid atherosclerosis | 9 studies were included involving 2446 subjects (925 with NAFLD) | The carotid intima-media thickness was increased 0.16 mm with a 95% confidence interval (0.11, 0.21) with a 3.73-times greater risk for carotid plaque |
| Valbusa et al. (2016)104 | Prospective study showing NAFLD is an independent risk factor for acute heart failure readmissions | Cohort study with a total sample of 314 elderly patients with confirmed consecutive admissions for acute heart failure | Patients with NAFLD had remarkably higher 1-year all-cause and cardiac rehospitalizations compared with their counterparts without NAFLD |
| Hung et al. (2015)108 | Cross-sectional analysis showing an association between NAFLD and QT prolongation in the general population | Observational study of 31,116 patients were included | Mild, moderate, and severe NAFLD was associated with increases in QTc interval (2.55, 6.59 and 12.14 ms) compared with no NAFLD (p < 0.001); NAFLD was also associated with an increased risk of QTc prolongation |
| Mantovani et al. (2017)109 | Retrospective cohort study showing an independent association between NAFLD and increased risk of heart block in hospitalized patients with type 2 diabetes mellitus | Retrospective study evaluating a cohort of 751 patients with type 2 diabetes mellitus during the years 2007-2014 | Overall, patients with NAFLD had a higher prevalence of persistent heart block than those without NAFLD (31.3% vs. 16.7%, p < 0.001). NAFLD was associated with a three-fold increased risk of prevalent heart block |
| Targher et al. (2013)110 | Retrospective cohort study showing an association between NAFLD and increased risk of atrial fibrillation in hospitalized patients with type 2 diabetes mellitus | 702 patients with type 2 diabetes mellitus were evaluated for the prevalence of atrial fibrillation during 2007-2011 | NAFLD was associated with an increased risk of prevalent atrial fibrillation |
| Targher et al. (2016)113 | Meta-analysis showing an association between NAFLD and an increased incidence of CVD | 16 observational prospective and retrospective studies with 34,043 individuals over a median period of 6.9 years were assessed in this meta-analysis | Patients with NAFLD had a higher risk of fatal and/or non-fatal CVD events that those without NAFLD, with patients with more severe NAFLD more likely to develop fatal and non-fatal events |
| Wu et al. (2016)114 | Meta-analysis showing an association of NAFLD with major adverse CVD events | 34 studies with a total of 164,494 participants were included; specifically, 21 cross-sectional studies and 13 cohort studies were examined in this meta-analysis | NAFLD was not associated with overall mortality and CVD mortality but was, however, associated with an increased risk of prevalence and incidence of CVD |
| Hagström et al. (2019)116 | Cohort study showing patients with NAFLD are at an increased risk for CVD | A large cohort of 603 biopsy-proven NAFLD patients free of baseline CVD were cross-linked to national registries to evaluate histological and traditional cardiovascular risk factors as predictors of cardiovascular outcomes | Patients with NAFLD are at an increased risk for CVD compared to matched controls but histological parameters do not seem to independently predict this risk |
Abbreviations: CAD, cardiac artery disease; CVD, cardiovascular disease; NAFLD, nonalcoholic fatty liver disease.
Cardiovascular outcomes and mortality in NAFLD
CVD has been incriminated as the leading cause of mortality among patients with NAFLD, even surpassing the mortality associated with chronic liver disease. Recently, a meta-analysis by Targher et al.113 demonstrated that NAFLD is associated with an increased risk of both fatal and nonfatal CVD events. Another meta-analysis by Wu et al.114 showed that NAFLD was associated with an increased prevalence of adverse cardiovascular events but did not show an association with overall or CVD mortality; similarly, NASH was not associated with overall or CVD mortality but was associated with an increased incidence of CVD. This increase in incidence may correlate with another systematic review by Dulai et al. that demonstrated an increased risk of mortality with increasing fibrosis severity in NAFLD.115 A recent Swedish cohort study in liver biopsy-diagnosed NAFLD with the longest documented follow-up time (of over 18 years) supported these findings by showing that patients with NAFLD are at an increased risk for CVD.116
Although more studies are needed to confirm a causal relationship between NAFLD and CVD, these findings highlight the importance of risk factor modification and interventions aimed at preventing CVD progression in NAFLD. Table 2 summarizes below the current literature evaluating the association between NAFLD and CVD.
Conclusions
The pathophysiological pathways that link NAFLD to premature CVD events result from the development of atherogenic dyslipidemia and ectopic lipid deposition. It involves an altered hepatic metabolism of lipids and glucose due to insulin resistance and a constellation pathogenetic factors associated with the gut microbiome, genetics, and individual lifestyle. The significant association between NAFLD and CVD warrants screening of NAFLD and its associated risk factors in high-risk patients in order to effectively intervene, with a focus on novel approaches that target insulin resistance and dyslipidemia. These novel approaches encompass both nonpharmacological approaches, such as weight loss, lifestyle modifications and bariatric surgery, as well as pharmacologic targets aimed at improving insulin sensitivity. A better understanding of the pathogenesis of insulin resistance will allow the development of newer treatment options that can address the growing health concerns posed by NAFLD and insulin resistance.
Acknowledgments
The authors would like to acknowledge everyone who contributed to the completion of this project.
Abbreviations
- ChREBP
carbohydrate response element binding protein
- CVD
cardiovascular disease
- DAG
diacylglycerol
- DNL
de novo lipogenesis
- IMCL
intramyocellular lipid
- IRTK
insulin receptor tyrosine kinase
- NAFLD
nonalcoholic fatty liver disease
- PKC
protein kinase C
References
- 1.Younossi Z, Henry L. Contribution of alcoholic and nonalcoholic fatty liver disease to the burden of liver-related morbidity and mortality. Gastroenterology. 2016;150:1778–1785. doi: 10.1053/j.gastro.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 3.Younossi ZM, Stepanova M, Afendy M, Fang Y, Younossi Y, Mir H, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9:524–530.e1. doi: 10.1016/j.cgh.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 4.Marchesini G, Moscatiello S, Di Domizio S, Forlani G. Obesity-associated liver disease. J Clin Endocrinol Metab. 2008;93:S74–S80. doi: 10.1210/jc.2008-1399. [DOI] [PubMed] [Google Scholar]
- 5.Lallukka S, Yki-Järvinen H. Non-alcoholic fatty liver disease and risk of type 2 diabetes. Best Pract Res Clin Endocrinol Metab. 2016;30:385–395. doi: 10.1016/j.beem.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 6.Yki-Järvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2:901–910. doi: 10.1016/S2213-8587(14)70032-4. [DOI] [PubMed] [Google Scholar]
- 7.Firneisz G. Non-alcoholic fatty liver disease and type 2 diabetes mellitus: the liver disease of our age? World J Gastroenterol. 2014;20:9072–9089. doi: 10.3748/wjg.v20.i27.9072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Alwis NM, Day CP. Non-alcoholic fatty liver disease: the mist gradually clears. J Hepatol. 2008;48(Suppl 1):S104–S112. doi: 10.1016/j.jhep.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 9.Targher G, Marra F, Marchesini G. Increased risk of cardiovascular disease in non-alcoholic fatty liver disease: causal effect or epiphenomenon? Diabetologia. 2008;51:1947–1953. doi: 10.1007/s00125-008-1135-4. [DOI] [PubMed] [Google Scholar]
- 10.Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. J Clin Invest. 2016;126:12–22. doi: 10.1172/JCI77812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guertin DA, Sabatini DM. Defining the role of mTOR in cancer. Cancer Cell. 2007;12:9–22. doi: 10.1016/j.ccr.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Alessi DR, James SR, Downes CP, Holmes AB, Gaffney PR, Reese CB, et al. Characterization of a 3-phosphoinositide-dependent protein kinase which phosphorylates and activates protein kinase Balpha. Curr Biol. 1997;7:261–269. doi: 10.1016/s0960-9822(06)00122-9. [DOI] [PubMed] [Google Scholar]
- 13.Stephens L, Anderson K, Stokoe D, Erdjument-Bromage H, Painter GF, Holmes AB, et al. Protein kinase B kinases that mediate phosphatidylinositol 3,4,5-trisphosphate-dependent activation of protein kinase B. Science. 1998;279:710–714. doi: 10.1126/science.279.5351.710. [DOI] [PubMed] [Google Scholar]
- 14.Petersen KF, Laurent D, Rothman DL, Cline GW, Shulman GI. Mechanism by which glucose and insulin inhibit net hepatic glycogenolysis in humans. J Clin Invest. 1998;101:1203–1209. doi: 10.1172/JCI579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakae J, Kitamura T, Silver DL, Accili D. The forkhead transcription factor Foxo1 (Fkhr) confers insulin sensitivity onto glucose-6-phosphatase expression. J Clin Invest. 2001;108:1359–1367. doi: 10.1172/JCI12876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Previs SF, Cline GW, Shulman GI. A critical evaluation of mass isotopomer distribution analysis of gluconeogenesis in vivo. Am J Physiol. 1999;277:E154–E160. doi: 10.1152/ajpendo.1999.277.1.E154. [DOI] [PubMed] [Google Scholar]
- 17.Perry RJ, Zhang XM, Zhang D, Kumashiro N, Camporez JP, Cline GW, et al. Leptin reverses diabetes by suppression of the hypothalamic-pituitary-adrenal axis. Nat Med. 2014;20:759–763. doi: 10.1038/nm.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perry RJ, Camporez JG, Kursawe R, Titchenell PM, Zhang D, Perry CJ, et al. Hepatic acetyl CoA links adipose tissue inflammation to hepatic insulin resistance and type 2 diabetes. Cell. 2015;160:745–758. doi: 10.1016/j.cell.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samuel VT, Shulman GI. Nonalcoholic fatty liver disease as a nexus of metabolic and hepatic diseases. Cell Metab. 2018;27:22–41. doi: 10.1016/j.cmet.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wan M, Leavens KF, Hunter RW, Koren S, von Wilamowitz-Moellendorff A, Lu M, et al. A noncanonical, GSK3-independent pathway controls postprandial hepatic glycogen deposition. Cell Metab. 2013;18:99–105. doi: 10.1016/j.cmet.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wehmeyer MH, Zyriax BC, Jagemann B, Roth E, Windler E, Schulze Zur Wiesch J, et al. Nonalcoholic fatty liver disease is associated with excessive calorie intake rather than a distinctive dietary pattern. Medicine (Baltimore) 2016;95:e3887. doi: 10.1097/MD.0000000000003887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lambert JE, Ramos-Roman MA, Browning JD, Parks EJ. Increased de novo lipogenesis is a distinct characteristic of individuals with nonalcoholic fatty liver disease. Gastroenterology. 2014;146:726–735. doi: 10.1053/j.gastro.2013.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petersen KF, Dufour S, Befroy D, Lehrke M, Hendler RE, Shulman GI. Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes. 2005;54:603–608. doi: 10.2337/diabetes.54.3.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor R, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, et al. Clinical and metabolic features of the randomised controlled Diabetes Remission Clinical Trial (DiRECT) cohort. Diabetologia. 2018;61:589–598. doi: 10.1007/s00125-017-4503-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perry RJ, Peng L, Cline GW, Wang Y, Rabin-Court A, Song JD, et al. Mechanisms by which a very-low-calorie diet reverses hyperglycemia in a rat model of type 2 diabetes. Cell Metab. 2018;27:210–217.e3. doi: 10.1016/j.cmet.2017.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vatner DF, Majumdar SK, Kumashiro N, Petersen MC, Rahimi Y, Gattu AK, et al. Insulin-independent regulation of hepatic triglyceride synthesis by fatty acids. Proc Natl Acad Sci U S A. 2015;112:1143–1148. doi: 10.1073/pnas.1423952112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hudgins LC, Parker TS, Levine DM, Hellerstein MK. A dual sugar challenge test for lipogenic sensitivity to dietary fructose. J Clin Endocrinol Metab. 2011;96:861–868. doi: 10.1210/jc.2010-2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lecoultre V, Egli L, Carrel G, Theytaz F, Kreis R, Schneiter P, et al. Effects of fructose and glucose overfeeding on hepatic insulin sensitivity and intrahepatic lipids in healthy humans. Obesity (Silver Spring) 2013;21:782–785. doi: 10.1002/oby.20377. [DOI] [PubMed] [Google Scholar]
- 30.Spruss A, Bergheim I. Dietary fructose and intestinal barrier: potential risk factor in the pathogenesis of nonalcoholic fatty liver disease. J Nutr Biochem. 2009;20:657–662. doi: 10.1016/j.jnutbio.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 31.Roglans N, Vilà L, Farré M, Alegret M, Sánchez RM, Vázquez-Carrera M, et al. Impairment of hepatic Stat-3 activation and reduction of PPARalpha activity in fructose-fed rats. Hepatology. 2007;45:778–788. doi: 10.1002/hep.21499. [DOI] [PubMed] [Google Scholar]
- 32.Tilg H, Moschen AR. Inflammatory mechanisms in the regulation of insulin resistance. Mol Med. 2008;14:222–231. doi: 10.2119/2007-00119.Tilg. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Assy N, Nasser G, Kamayse I, Nseir W, Beniashvili Z, Djibre A, et al. Soft drink consumption linked with fatty liver in the absence of traditional risk factors. Can J Gastroenterol. 2008;22:811–816. doi: 10.1155/2008/810961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ouyang X, Cirillo P, Sautin Y, McCall S, Bruchette JL, Diehl AM, et al. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J Hepatol. 2008;48:993–999. doi: 10.1016/j.jhep.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, Webb M, Blendis L, Halpern Z, et al. Long term nutritional intake and the risk for non-alcoholic fatty liver disease (NAFLD): a population based study. J Hepatol. 2007;47:711–717. doi: 10.1016/j.jhep.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 36.Shulman GI. Cellular mechanisms of insulin resistance. J Clin Invest. 2000;106:171–176. doi: 10.1172/JCI10583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sinha R, Dufour S, Petersen KF, LeBon V, Enoksson S, Ma YZ, et al. Assessment of skeletal muscle triglyceride content by (1)H nuclear magnetic resonance spectroscopy in lean and obese adolescents: relationships to insulin sensitivity, total body fat, and central adiposity. Diabetes. 2002;51:1022–1027. doi: 10.2337/diabetes.51.4.1022. [DOI] [PubMed] [Google Scholar]
- 38.Perseghin G, Scifo P, De Cobelli F, Pagliato E, Battezzati A, Arcelloni C, et al. Intramyocellular triglyceride content is a determinant of in vivo insulin resistance in humans: a 1H-13C nuclear magnetic resonance spectroscopy assessment in offspring of type 2 diabetic parents. Diabetes. 1999;48:1600–1606. doi: 10.2337/diabetes.48.8.1600. [DOI] [PubMed] [Google Scholar]
- 39.Krssak M, Falk Petersen K, Dresner A, DiPietro L, Vogel SM, Rothman DL, et al. Intramyocellular lipid concentrations are correlated with insulin sensitivity in humans: a 1H NMR spectroscopy study. Diabetologia. 1999;42:113–116. doi: 10.1007/s001250051123. [DOI] [PubMed] [Google Scholar]
- 40.Dresner A, Laurent D, Marcucci M, Griffin ME, Dufour S, Cline GW, et al. Effects of free fatty acids on glucose transport and IRS-1-associated phosphatidylinositol 3-kinase activity. J Clin Invest. 1999;103:253–259. doi: 10.1172/JCI5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roden M, Price TB, Perseghin G, Petersen KF, Rothman DL, Cline GW, et al. Mechanism of free fatty acid-induced insulin resistance in humans. J Clin Invest. 1996;97:2859–2865. doi: 10.1172/JCI118742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petersen KF, Hendler R, Price T, Perseghin G, Rothman DL, Held N, et al. 13C/31P NMR studies on the mechanism of insulin resistance in obesity. Diabetes. 1998;47:381–386. doi: 10.2337/diabetes.47.3.381. [DOI] [PubMed] [Google Scholar]
- 43.Cline GW, Petersen KF, Krssak M, Shen J, Hundal RS, Trajanoski Z, et al. Impaired glucose transport as a cause of decreased insulin-stimulated muscle glycogen synthesis in type 2 diabetes. N Engl J Med. 1999;341:240–246. doi: 10.1056/NEJM199907223410404. [DOI] [PubMed] [Google Scholar]
- 44.Perseghin G, Price TB, Petersen KF, Roden M, Cline GW, Gerow K, et al. Increased glucose transport-phosphorylation and muscle glycogen synthesis after exercise training in insulin-resistant subjects. N Engl J Med. 1996;335:1357–1362. doi: 10.1056/NEJM199610313351804. [DOI] [PubMed] [Google Scholar]
- 45.Yu C, Chen Y, Cline GW, Zhang D, Zong H, Wang Y, et al. Mechanism by which fatty acids inhibit insulin activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3-kinase activity in muscle. J Biol Chem. 2002;277:50230–50236. doi: 10.1074/jbc.M200958200. [DOI] [PubMed] [Google Scholar]
- 46.Itani SI, Ruderman NB, Schmieder F, Boden G. Lipid-induced insulin resistance in human muscle is associated with changes in diacylglycerol, protein kinase C, and IkappaB-alpha. Diabetes. 2002;51:2005–2011. doi: 10.2337/diabetes.51.7.2005. [DOI] [PubMed] [Google Scholar]
- 47.Szendroedi J, Yoshimura T, Phielix E, Koliaki C, Marcucci M, Zhang D, et al. Role of diacylglycerol activation of PKCθ in lipid-induced muscle insulin resistance in humans. Proc Natl Acad Sci U S A. 2014;111:9597–9602. doi: 10.1073/pnas.1409229111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li Y, Soos TJ, Li X, Wu J, Degennaro M, Sun X, et al. Protein kinase C Theta inhibits insulin signaling by phosphorylating IRS1 at Ser(1101) J Biol Chem. 2004;279:45304–45307. doi: 10.1074/jbc.C400186200. [DOI] [PubMed] [Google Scholar]
- 49.Petersen KF, Dufour S, Savage DB, Bilz S, Solomon G, Yonemitsu S, et al. The role of skeletal muscle insulin resistance in the pathogenesis of the metabolic syndrome. Proc Natl Acad Sci U S A. 2007;104:12587–12594. doi: 10.1073/pnas.0705408104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Flannery C, Dufour S, Rabøl R, Shulman GI, Petersen KF. Skeletal muscle insulin resistance promotes increased hepatic de novo lipogenesis, hyperlipidemia, and hepatic steatosis in the elderly. Diabetes. 2012;61:2711–2717. doi: 10.2337/db12-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Petersen KF, Oral EA, Dufour S, Befroy D, Ariyan C, Yu C, et al. Leptin reverses insulin resistance and hepatic steatosis in patients with severe lipodystrophy. J Clin Invest. 2002;109:1345–1350. doi: 10.1172/JCI15001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim JK, Gavrilova O, Chen Y, Reitman ML, Shulman GI. Mechanism of insulin resistance in A-ZIP/F-1 fatless mice. J Biol Chem. 2000;275:8456–8460. doi: 10.1074/jbc.275.12.8456. [DOI] [PubMed] [Google Scholar]
- 53.Kim JK, Fillmore JJ, Chen Y, Yu C, Moore IK, Pypaert M, et al. Tissue-specific overexpression of lipoprotein lipase causes tissue-specific insulin resistance. Proc Natl Acad Sci U S A. 2001;98:7522–7527. doi: 10.1073/pnas.121164498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Petersen MC, Shulman GI. Mechanisms of insulin action and insulin resistance. Physiol Rev. 2018;98:2133–2223. doi: 10.1152/physrev.00063.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Qu X, Seale JP, Donnelly R. Tissue and isoform-selective activation of protein kinase C in insulin-resistant obese Zucker rats - effects of feeding. J Endocrinol. 1999;162:207–214. doi: 10.1677/joe.0.1620207. [DOI] [PubMed] [Google Scholar]
- 56.Samuel VT, Liu ZX, Qu X, Elder BD, Bilz S, Befroy D, et al. Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J Biol Chem. 2004;279:32345–32353. doi: 10.1074/jbc.M313478200. [DOI] [PubMed] [Google Scholar]
- 57.Samuel VT, Liu ZX, Wang A, Beddow SA, Geisler JG, Kahn M, et al. Inhibition of protein kinase Cepsilon prevents hepatic insulin resistance in nonalcoholic fatty liver disease. J Clin Invest. 2007;117:739–745. doi: 10.1172/JCI30400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Raddatz K, Turner N, Frangioudakis G, Liao BM, Pedersen DJ, Cantley J, et al. Time-dependent effects of Prkce deletion on glucose homeostasis and hepatic lipid metabolism on dietary lipid oversupply in mice. Diabetologia. 2011;54:1447–1456. doi: 10.1007/s00125-011-2073-0. [DOI] [PubMed] [Google Scholar]
- 59.Petersen MC, Madiraju AK, Gassaway BM, Marcel M, Nasiri AR, Butrico G, et al. Insulin receptor Thr1160 phosphorylation mediates lipid-induced hepatic insulin resistance. J Clin Invest. 2016;126:4361–4371. doi: 10.1172/JCI86013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kumashiro N, Erion DM, Zhang D, Kahn M, Beddow SA, Chu X, et al. Cellular mechanism of insulin resistance in nonalcoholic fatty liver disease. Proc Natl Acad Sci U S A. 2011;108:16381–16385. doi: 10.1073/pnas.1113359108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Magkos F, Su X, Bradley D, Fabbrini E, Conte C, Eagon JC, et al. Intrahepatic diacylglycerol content is associated with hepatic insulin resistance in obese subjects. Gastroenterology. 2012;142:1444–1446.e2. doi: 10.1053/j.gastro.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Luukkonen PK, Zhou Y, Sädevirta S, Leivonen M, Arola J, Orešič M, et al. Hepatic ceramides dissociate steatosis and insulin resistance in patients with non-alcoholic fatty liver disease. J Hepatol. 2016;64:1167–1175. doi: 10.1016/j.jhep.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 63.Ter Horst KW, Gilijamse PW, Versteeg RI, Ackermans MT, Nederveen AJ, la Fleur SE, et al. Hepatic diacylglycerol-associated protein kinase Cɛ translocation links hepatic steatosis to hepatic insulin resistance in humans. Cell Rep. 2017;19:1997–2004. doi: 10.1016/j.celrep.2017.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Irimia JM, Meyer CM, Segvich DM, Surendran S, DePaoli-Roach AA, Morral N, et al. Lack of liver glycogen causes hepatic insulin resistance and steatosis in mice. J Biol Chem. 2017;292:10455–10464. doi: 10.1074/jbc.M117.786525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Herman MA, Peroni OD, Villoria J, Schön MR, Abumrad NA, Blüher M, et al. A novel ChREBP isoform in adipose tissue regulates systemic glucose metabolism. Nature. 2012;484:333–338. doi: 10.1038/nature10986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yore MM, Syed I, Moraes-Vieira PM, Zhang T, Herman MA, Homan EA, et al. Discovery of a class of endogenous mammalian lipids with anti-diabetic and anti-inflammatory effects. Cell. 2014;159:318–332. doi: 10.1016/j.cell.2014.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Benhamed F, Denechaud PD, Lemoine M, Robichon C, Moldes M, Bertrand-Michel J, et al. The lipogenic transcription factor ChREBP dissociates hepatic steatosis from insulin resistance in mice and humans. J Clin Invest. 2012;122:2176–2194. doi: 10.1172/JCI41636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tilg H. The role of cytokines in non-alcoholic fatty liver disease. Dig Dis. 2010;28:179–185. doi: 10.1159/000282083. [DOI] [PubMed] [Google Scholar]
- 69.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89:2548–2556. doi: 10.1210/jc.2004-0395. [DOI] [PubMed] [Google Scholar]
- 70.Asano T, Watanabe K, Kubota N, Gunji T, Omata M, Kadowaki T, et al. Adiponectin knockout mice on high fat diet develop fibrosing steatohepatitis. J Gastroenterol Hepatol. 2009;24:1669–1676. doi: 10.1111/j.1440-1746.2009.06039.x. [DOI] [PubMed] [Google Scholar]
- 71.Nawrocki AR, Rajala MW, Tomas E, Pajvani UB, Saha AK, Trumbauer ME, et al. Mice lacking adiponectin show decreased hepatic insulin sensitivity and reduced responsiveness to peroxisome proliferator-activated receptor gamma agonists. J Biol Chem. 2006;281:2654–2660. doi: 10.1074/jbc.M505311200. [DOI] [PubMed] [Google Scholar]
- 72.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW., Jr Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–1808. doi: 10.1172/JCI19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003;112:1821–1830. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Laurencikiene J, van Harmelen V, Arvidsson Nordström E, Dicker A, Blomqvist L, Näslund E, et al. NF-kappaB is important for TNF-alpha-induced lipolysis in human adipocytes. J Lipid Res. 2007;48:1069–1077. doi: 10.1194/jlr.M600471-JLR200. [DOI] [PubMed] [Google Scholar]
- 75.Ranjit S, Boutet E, Gandhi P, Prot M, Tamori Y, Chawla A, et al. Regulation of fat specific protein 27 by isoproterenol and TNF-α to control lipolysis in murine adipocytes. J Lipid Res. 2011;52:221–236. doi: 10.1194/jlr.M008771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Scherer T, O’Hare J, Diggs-Andrews K, Schweiger M, Cheng B, Lindtner C, et al. Brain insulin controls adipose tissue lipolysis and lipogenesis. Cell Metab. 2011;13:183–194. doi: 10.1016/j.cmet.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Scherer T, Lindtner C, Zielinski E, O’Hare J, Filatova N, Buettner C. Short term voluntary overfeeding disrupts brain insulin control of adipose tissue lipolysis. J Biol Chem. 2012;287:33061–33069. doi: 10.1074/jbc.M111.307348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Iwen KA, Scherer T, Heni M, Sayk F, Wellnitz T, Machleidt F, et al. Intranasal insulin suppresses systemic but not subcutaneous lipolysis in healthy humans. J Clin Endocrinol Metab. 2014;99:E246–E251. doi: 10.1210/jc.2013-3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brands M, Verhoeven AJ, Serlie MJ. Role of mitochondrial function in insulin resistance. Adv Exp Med Biol. 2012;942:215–234. doi: 10.1007/978-94-007-2869-1_9. [DOI] [PubMed] [Google Scholar]
- 80.Bugianesi E, Gastaldelli A, Vanni E, Gambino R, Cassader M, Baldi S, et al. Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: sites and mechanisms. Diabetologia. 2005;48:634–642. doi: 10.1007/s00125-005-1682-x. [DOI] [PubMed] [Google Scholar]
- 81.Koliaki C, Szendroedi J, Kaul K, Jelenik T, Nowotny P, Jankowiak F, et al. Adaptation of hepatic mitochondrial function in humans with non-alcoholic fatty liver is lost in steatohepatitis. Cell Metab. 2015;21:739–746. doi: 10.1016/j.cmet.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 82.Yeniova AO, Küçükazman M, Ata N, Dal K, Kefeli A, Başyiğit S, et al. High-sensitivity C-reactive protein is a strong predictor of non-alcoholic fatty liver disease. Hepatogastroenterology. 2014;61:422–425. [PubMed] [Google Scholar]
- 83.Wood KL, Miller MH, Dillon JF. Systematic review of genetic association studies involving histologically confirmed non-alcoholic fatty liver disease. BMJ Open Gastroenterol. 2015;2:e000019. doi: 10.1136/bmjgast-2014-000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Peter A, Kantartzis K, Machicao F, Machann J, Wagner S, Templin S, et al. Visceral obesity modulates the impact of apolipoprotein C3 gene variants on liver fat content. Int J Obes (Lond) 2012;36:774–782. doi: 10.1038/ijo.2011.154. [DOI] [PubMed] [Google Scholar]
- 85.Petersen KF, Dufour S, Hariri A, Nelson-Williams C, Foo JN, Zhang XM, et al. Apolipoprotein C3 gene variants in nonalcoholic fatty liver disease. N Engl J Med. 2010;362:1082–1089. doi: 10.1056/NEJMoa0907295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang RN, Zheng RD, Mi YQ, Zhou D, Shen F, Chen GY, et al. APOC3 rs2070666 is associated with the hepatic steatosis independently of PNPLA3 rs738409 in Chinese Han patients with nonalcoholic fatty liver diseases. Dig Dis Sci. 2016;61:2284–2293. doi: 10.1007/s10620-016-4120-7. [DOI] [PubMed] [Google Scholar]
- 87.Mahdessian H, Taxiarchis A, Popov S, Silveira A, Franco-Cereceda A, Hamsten A, et al. TM6SF2 is a regulator of liver fat metabolism influencing triglyceride secretion and hepatic lipid droplet content. Proc Natl Acad Sci U S A. 2014;111:8913–8918. doi: 10.1073/pnas.1323785111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Luukkonen PK, Zhou Y, Hyötyläinen T, Leivonen M, Arola J, Orho-Melander M, et al. The MBOAT7 variant rs641738 alters hepatic phosphatidylinositols and increases severity of non-alcoholic fatty liver disease in humans. J Hepatol. 2016;65:1263–1265. doi: 10.1016/j.jhep.2016.07.045. [DOI] [PubMed] [Google Scholar]
- 89.Mancina RM, Dongiovanni P, Petta S, Pingitore P, Meroni M, Rametta R, et al. The MBOAT7-TMC4 variant rs641738 increases risk of nonalcoholic fatty liver disease in individuals of European descent. Gastroenterology. 2016;150:1219–1230.e6. doi: 10.1053/j.gastro.2016.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Williams AL, Jacobs SB, Moreno-Macías H, Huerta-Chagoya A, Churchhouse C, Márquez-Luna C, et al. Sequence variants in SLC16A11 are a common risk factor for type 2 diabetes in Mexico. Nature. 2014;506:97–101. doi: 10.1038/nature12828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rusu V, Hoch E, Mercader JM, Tenen DE, Gymrek M, Hartigan CR, et al. Type 2 diabetes variants disrupt function of SLC16A11 through two distinct mechanisms. Cell. 2017;170:199–212.e20. doi: 10.1016/j.cell.2017.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yu J, Marsh S, Hu J, Feng W, Wu C. The pathogenesis of nonalcoholic fatty liver disease: Interplay between diet, gut microbiota, and genetic background. Gastroenterol Res Pract. 2016;2016:2862173. doi: 10.1155/2016/2862173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ferolla SM, Armiliato GN, Couto CA, Ferrari TC. The role of intestinal bacteria overgrowth in obesity-related nonalcoholic fatty liver disease. Nutrients. 2014;6:5583–5599. doi: 10.3390/nu6125583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wigg AJ, Roberts-Thomson IC, Dymock RB, McCarthy PJ, Grose RH, Cummins AG. The role of small intestinal bacterial overgrowth, intestinal permeability, endotoxaemia, and tumour necrosis factor alpha in the pathogenesis of non-alcoholic steatohepatitis. Gut. 2001;48:206–211. doi: 10.1136/gut.48.2.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Boursier J, Mueller O, Barret M, Machado M, Fizanne L, Araujo-Perez F, et al. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota. Hepatology. 2016;63:764–775. doi: 10.1002/hep.28356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pedersen HK, Gudmundsdottir V, Nielsen HB, Hyotylainen T, Nielsen T, Jensen BA, et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature. 2016;535:376–381. doi: 10.1038/nature18646. [DOI] [PubMed] [Google Scholar]
- 97.Abdel-Razik A, Mousa N, Shabana W, Refaey M, Elzehery R, Elhelaly R, et al. Rifaximin in nonalcoholic fatty liver disease: hit multiple targets with a single shot. Eur J Gastroenterol Hepatol. 2018;30:1237–1246. doi: 10.1097/MEG.0000000000001232. [DOI] [PubMed] [Google Scholar]
- 98.Borrelli A, Bonelli P, Tuccillo FM, Goldfine ID, Evans JL, Buonaguro FM, et al. Role of gut microbiota and oxidative stress in the progression of non-alcoholic fatty liver disease to hepatocarcinoma: Current and innovative therapeutic approaches. Redox Biol. 2018;15:467–479. doi: 10.1016/j.redox.2018.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ampuero J, Gallego-Durán R, Romero-Gómez M. Association of NAFLD with subclinical atherosclerosis and coronary-artery disease: meta-analysis. Rev Esp Enferm Dig. 2015;107:10–16. [PubMed] [Google Scholar]
- 100.Zhou YY, Zhou XD, Wu SJ, Fan DH, Van Poucke S, Chen YP, et al. Nonalcoholic fatty liver disease contributes to subclinical atherosclerosis: A systematic review and meta-analysis. Hepatol Commun. 2018;2:376–392. doi: 10.1002/hep4.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jaruvongvanich V, Wirunsawanya K, Sanguankeo A, Upala S. Nonalcoholic fatty liver disease is associated with coronary artery calcification: A systematic review and meta-analysis. Dig Liver Dis. 2016;48:1410–1417. doi: 10.1016/j.dld.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 102.Fan Y, Wei F, Zhou Y, Zhang H. Association of non-alcoholic fatty liver disease with impaired endothelial function by flow-mediated dilation: A meta-analysis. Hepatol Res. 2016;46:E165–E173. doi: 10.1111/hepr.12554. [DOI] [PubMed] [Google Scholar]
- 103.Cai J, Zhang S, Huang W. Association between nonalcoholic fatty liver disease and carotid atherosclerosis: a meta-analysis. Int J Clin Exp Med. 2015;8:7673–7678. [PMC free article] [PubMed] [Google Scholar]
- 104.Valbusa F, Bonapace S, Grillo C, Scala L, Chiampan A, Rossi A, et al. Nonalcoholic fatty liver disease is associated with higher 1-year all-cause rehospitalization rates in patients admitted for acute heart failure. Medicine (Baltimore) 2016;95:e2760. doi: 10.1097/MD.0000000000002760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Granér M, Nyman K, Siren R, Pentikäinen MO, Lundbom J, Hakkarainen A, et al. Ectopic fat depots and left ventricular function in nondiabetic men with nonalcoholic fatty liver disease. Circ Cardiovasc Imaging. 2014;8:e001979. doi: 10.1161/CIRCIMAGING.114.001979. [DOI] [PubMed] [Google Scholar]
- 106.Balcioğlu AS, Çiçek D, Akinci S, Eldem HO, Bal UA, Okyay K, et al. Arrhythmogenic evidence for epicardial adipose tissue: heart rate variability and turbulence are influenced by epicardial fat thickness. Pacing Clin Electrophysiol. 2015;38:99–106. doi: 10.1111/pace.12512. [DOI] [PubMed] [Google Scholar]
- 107.Targher G, Valbusa F, Bonapace S, Bertolini L, Zenari L, Pichiri I, et al. Association of nonalcoholic fatty liver disease with QTc interval in patients with type 2 diabetes. Nutr Metab Cardiovasc Dis. 2014;24:663–669. doi: 10.1016/j.numecd.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 108.Hung CS, Tseng PH, Tu CH, Chen CC, Liao WC, Lee YC, et al. Nonalcoholic fatty liver disease is associated with QT prolongation in the general population. J Am Heart Assoc. 2015;4:e001820. doi: 10.1161/JAHA.115.001820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mantovani A, Rigolon R, Pichiri I, Bonapace S, Morani G, Zoppini G, et al. Nonalcoholic fatty liver disease is associated with an increased risk of heart block in hospitalized patients with type 2 diabetes mellitus. PLoS One. 2017;12:e0185459. doi: 10.1371/journal.pone.0185459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Targher G, Mantovani A, Pichiri I, Rigolon R, Dauriz M, Zoppini G, et al. Non-alcoholic fatty liver disease is associated with an increased prevalence of atrial fibrillation in hospitalized patients with type 2 diabetes. Clin Sci (Lond) 2013;125:301–309. doi: 10.1042/CS20130036. [DOI] [PubMed] [Google Scholar]
- 111.Ozveren O, Izgi C, Eroglu E, Simsek MA, Turer A, Kucukdurmaz Z, et al. Doppler tissue evaluation of atrial conduction properties in patients with non-alcoholic fatty-liver disease. Ultrason Imaging. 2016;38:225–235. doi: 10.1177/0161734615595015. [DOI] [PubMed] [Google Scholar]
- 112.Targher G, Valbusa F, Bonapace S, Bertolini L, Zenari L, Rodella S, et al. Non-alcoholic fatty liver disease is associated with an increased incidence of atrial fibrillation in patients with type 2 diabetes. PLoS One. 2013;8:e57183. doi: 10.1371/journal.pone.0057183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: A meta-analysis. J Hepatol. 2016;65:589–600. doi: 10.1016/j.jhep.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 114.Wu S, Wu F, Ding Y, Hou J, Bi J, Zhang Z. Association of non-alcoholic fatty liver disease with major adverse cardiovascular events: A systematic review and meta-analysis. Sci Rep. 2016;6:33386. doi: 10.1038/srep33386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Dulai PS, Singh S, Patel J, Soni M, Prokop LJ, Younossi Z, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: Systematic review and meta-analysis. Hepatology. 2017;65:1557–1565. doi: 10.1002/hep.29085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hagström H, Nasr P, Ekstedt M, Hammar U, Stål P, Askling J, et al. Cardiovascular risk factors in non-alcoholic fatty liver disease. Liver Int. 2019;39:197–204. doi: 10.1111/liv.13973. [DOI] [PubMed] [Google Scholar]