Helicobacter pylori colonizes the stomach in about half of the world’s population. H. pylori strains containing the cag pathogenicity island (cag PAI) are associated with a higher risk of gastric adenocarcinoma or peptic ulcer disease than cag PAI-negative strains. The cag PAI encodes a type IV secretion system (T4SS) that mediates delivery of the CagA effector protein as well as nonprotein bacterial constituents into gastric epithelial cells.
KEYWORDS: Helicobacter pylori, ATPases, secretion systems, gastric cancer
ABSTRACT
Helicobacter pylori colonizes the stomach in about half of the world’s population. H. pylori strains containing the cag pathogenicity island (cag PAI) are associated with a higher risk of gastric adenocarcinoma or peptic ulcer disease than cag PAI-negative strains. The cag PAI encodes a type IV secretion system (T4SS) that mediates delivery of the CagA effector protein as well as nonprotein bacterial constituents into gastric epithelial cells. H. pylori-induced nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) activation and interleukin-8 (IL-8) secretion are attributed to T4SS-dependent delivery of lipopolysaccharide metabolites and peptidoglycan into host cells, and Toll-like receptor 9 (TLR9) activation is attributed to delivery of bacterial DNA. In this study, we analyzed the bacterial energetic requirements associated with these cellular alterations. Mutant strains lacking Cagα, Cagβ, or CagE (putative ATPases corresponding to VirB11, VirD4, and VirB4 in prototypical T4SSs) were capable of T4SS core complex assembly but defective in CagA translocation into host cells. Thus, the three Cag ATPases are not functionally redundant. Cagα and CagE were required for H. pylori-induced NF-κB activation, IL-8 secretion, and TLR9 activation, but Cagβ was dispensable for these responses. We identified putative ATP-binding motifs (Walker-A and Walker-B) in each of the ATPases and generated mutant strains in which these motifs were altered. Each of the Walker box mutant strains exhibited properties identical to those of the corresponding deletion mutant strains. These data suggest that Cag T4SS-dependent delivery of nonprotein bacterial constituents into host cells occurs through mechanisms different from those used for recruitment and delivery of CagA into host cells.
INTRODUCTION
Helicobacter pylori colonizes the stomach in about half of the human population (1–3), and the presence of these bacteria increases the risk of gastric adenocarcinoma, gastric lymphoma, and peptic ulceration (4, 5). H. pylori strains can potentially synthesize as many as four different type IV secretion systems (T4SSs) (6). One of these, the ComB T4SS, is present in nearly all H. pylori strains and mediates uptake of DNA (6, 7). T4SSs known as TFS3 and TFS4 are present in some H. pylori strains but absent from others; the functions of these T4SSs are unknown (6). The Cag T4SS is encoded by genes localized within a chromosomal region known as the cag pathogenicity island (cag PAI) (8–12). The proportion of H. pylori strains harboring the cag PAI varies from about 50% in the United States to nearly 100% in some parts of East Asia (13, 14). Individuals colonized with H. pylori strains containing the cag PAI have a higher risk of gastric adenocarcinoma or peptic ulcer disease than individuals colonized with cag PAI-negative strains (13, 14).
CagA is the only effector protein known to be translocated by the Cag T4SS (15, 16). Upon entry into gastric epithelial cells, CagA is phosphorylated by tyrosine kinases and interacts with multiple host cell proteins, altering their activity (15–18). Nonphosphorylated CagA also interacts with host cell proteins (15, 16, 18). The cellular alterations caused by CagA contribute to neoplastic transformation, and therefore, CagA has been designated as a “bacterial oncoprotein” (15, 16, 19).
The Cag T4SS is required not only for CagA translocation into host cells but also for H. pylori-induced cellular alterations attributed to the intracellular entry of nonprotein bacterial constituents. Nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) activation and stimulation of interleukin-8 (IL-8) production are attributed to the entry of H. pylori lipopolysaccharide metabolites (heptose 1,7-bisphosphate [HBP] [20–22] or ADP-glycero-β-d-manno-heptose [ADP heptose] [23]) and peptidoglycan (24) into host cells. Activation of Toll-like receptor 9 (TLR9) is attributed to the entry of H. pylori DNA into host cells (25, 26). Several publications reported that CagA can contribute to IL-8 induction and NF-κB activation (27–30). Conversely, these two cellular responses are elicited by mutant strains that do not produce CagA (31–34), which indicates that H. pylori can stimulate these responses through CagA-independent pathways.
About 17 of the 27 genes in the cag PAI are essential for CagA translocation into gastric epithelial cells, and about 14 are essential for H. pylori-induced IL-8 production by host cells (34). Five proteins encoded by genes in the cag PAI (CagY, CagX, CagT, CagM, and Cag3) assemble into a large core complex that spans the inner and outer membranes (35–38), and other cag PAI-encoded proteins assemble into an inner membrane complex (36). Three of the proteins localized to the Cag T4SS inner membrane complex are putative ATPases known as Cagα, Cagβ, and CagE (10, 34, 36). These correspond to VirB11, VirD4, and VirB4, respectively, in prototypical VirB/VirD4 T4SSs (E. coli conjugation systems and the Agrobacterium tumefaciens VirB/VirD4 system) (39–45).
H. pylori CagA, lipopolysaccharide metabolites, peptidoglycan, and DNA all enter host cells through Cag T4SS-dependent processes, but we speculate that these bacterial components are recruited and delivered into host cells through disparate mechanisms. In support of this view, a previous study showed that translocation of CagA into gastric epithelial cells requires several cag PAI-encoded proteins that are not required for H. pylori-induced IL-8 production (34). One of the proteins required for CagA translocation but not required for stimulation of IL-8 production is Cagβ (a VirD4 homolog) (34, 46). In Escherichia coli conjugation systems and the A. tumefaciens VirB/VirD4 system, VirD4 acts as a coupling protein that recruits DNA and the relaxosome from the cytoplasm to the T4SS (47–49). The role of Cagβ in H. pylori-induced TLR9 activation (a phenotype attributed to entry of bacterial DNA into host cells) has not yet been determined. Since VirD4 acts as a coupling protein required for recruitment and translocation of DNA in conjugative T4SSs and the A. tumefaciens T4SS (48, 50, 51), we hypothesized that Cagβ might be essential for recruitment and delivery of H. pylori DNA into host cells.
In the current study, we sought to further investigate the bacterial energetic requirements for T4SS-dependent, H. pylori-induced alterations in host cells. We generated unmarked cagα, cagβ, and cagE deletion mutants and genetically manipulated control strains containing the corresponding restored intact genes, as well as mutant strains containing substitution mutations in putative ATP-binding motifs (Walker-A and Walker-B boxes) of these ATPases. We then tested these mutants in cell culture assays to assess CagA translocation and CagA-independent cellular alterations (stimulation of IL-8 production, NF-κB activation, and TLR9 activation).
We report that the individual Cag ATPases are dispensable for assembly of the T4SS outer membrane core complex but essential for translocation of CagA into host cells. In addition, we report that strains containing mutations in Walker-A and Walker-B boxes of Cag ATPases exhibit the same phenotypes as corresponding deletion mutants. These findings indicate that the three Cag ATPases have nonredundant functions required for CagA translocation. Cagα and CagE, but not Cagβ, are required for H. pylori-induced NF-κB activation, IL-8 induction and TLR9 activation in host cells (three Cag T4SS-dependent phenotypes linked to cellular uptake of nonprotein bacterial components). The nonessentiality of Cagβ (a VirD4 homolog) for TLR9 activation contrasts the requirement of VirD4 for DNA transfer by conjugation systems and A. tumefaciens. Collectively, these data suggest that Cag T4SS-dependent delivery of nonprotein bacterial constituents into host cells occurs through mechanisms different from the mechanism used for the recruitment and delivery of CagA into host cells.
RESULTS
ATPases associated with the Cag T4SS.
Three genes within the cag PAI are predicted to encode ATPases (10). Cagα (encoded by the gene HP0525 in H. pylori strain 26695) is a VirB11 homolog, Cagβ (HP0524) is a VirD4 homolog, and CagE (HP0544) is a VirB4 homolog (39–43). The sequence relatedness of these H. pylori proteins to homologs in T4SSs of other bacterial species is relatively low. For example, in comparisons of H. pylori sequences with the homologous Agrobacterium VirB/VirD4 sequences, Cagα exhibits about 21% amino acid identity with VirB11 (GenBank accession no. P0A3F9 ), CagE exhibits about 17% identity with VirB4 (GenBank accession no. P17794), and Cagβ exhibits about 13% identity with VirD4 (GenBank accession no. P18594). To facilitate analysis of the Cag T4SS ATPases, we generated H. pylori mutant strains in which genes encoding each of the ATPases were individually disrupted or deleted, as described in Materials and Methods.
Cag T4SS ATPases are not required for outer membrane core complex assembly.
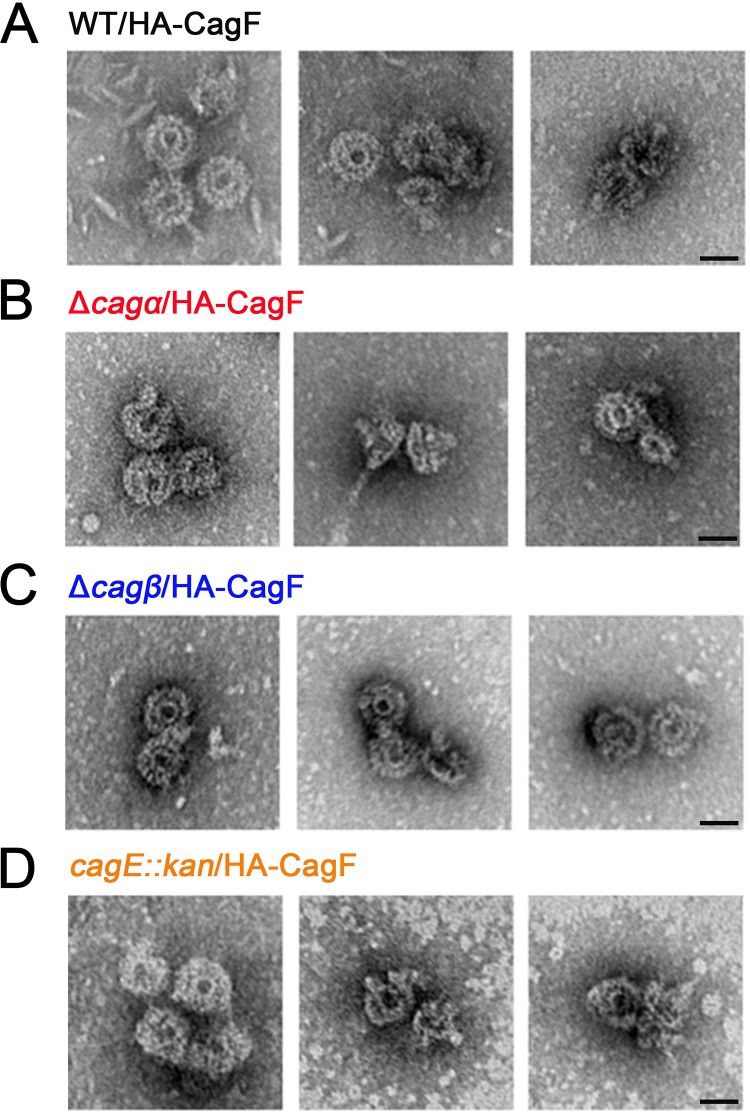
To evaluate whether the ATPases are required for T4SS core complex assembly, we conducted experiments to isolate core complexes from the ATPase mutants. To do this, we introduced a gene encoding HA-CagF into the ureAB chromosomal locus of strains harboring mutations in Cag ATPase-encoding genes. The resulting strains were designated FC1.1 (Δcagα/HA-CagF), FC2.1 (Δcagβ/HA-CagF), and FC3.1 (cagE::Kan/HA-CagF) (Table 1). We then immunopurified HA-CagF from these strains, which allows copurification of core complexes. Negative-stain electron microscopy (EM) analysis revealed successful isolation of core complexes from each of the mutant strains (Fig. 1). The structures of the core complexes isolated from the mutant strains appeared similar to structures of the core complex isolated from the corresponding strain containing a wild-type cag PAI (WT/HA-CagF) (Fig. 1). These results indicate that the individual Cag ATPases are not required for assembly of Cag T4SS outer membrane core complexes, a conclusion consistent with results of cryo-electron tomography experiments (36).
TABLE 1.
H. pylori strains used in this study
| H. pylori strain or plasmid | Description | Antibiotic resistance | Reference(s) |
|---|---|---|---|
| Straina | |||
| 26695 | Wild-type, intact cag PAI | None | 55 |
| ΔrdxA | Deletion of rdxA | Metronidazole | 52, 53 |
| rpsL-K43R | Codon 43 of rpsL harbors a lysine-to-arginine mutation | Streptomycin | 56, 68, 69 |
| Δcag PAI | Deletion of cag PAI | Chloramphenicol | 55 |
| Δcagα | Unmarked deletion of cagα | Metronidazole | 36 |
| ASL11.1 (cagα WB mutant)b | Introduced two point mutations in ATP-binding motifs of cagα (K184A, E248A) | Metronidazole | This study |
| ASL12.1 (restored WT cagα) | Restored two point mutations in cagα | Metronidazole | This study |
| Δcagβ | Unmarked deletion of cagβ | Metronidazole | 36 |
| ASL13.1 (cagβ WB mutant) | Introduced two point mutations in ATP-binding motifs of cagβ (K244A, D550A) | Streptomycin | This study |
| ASL14.1 (restored WT cagβ) | Restored two point mutations in cagβ | Streptomycin | This study |
| ΔcagE | Unmarked deletion of cagE | Metronidazole | 36 |
| ASL15.1 (cagE WB mutant) | Introduced two point mutations in ATP-binding motifs of cagE (K603A, D830A) | Streptomycin | This study |
| ASL16.1 (restored WT cagE) | Restored two point mutations in cagE | Streptomycin | This study |
| WT/HA-CagF | Introduced HA-cagF into ureAB locus | Chloramphenicol | 35 |
| FC1.1 (Δcagα/HA-CagF) | Introduced HA-cagF into ureAB locus | Metronidazole, chloramphenicol | This study |
| FC2.1 (Δcagβ/HA-CagF) | Introduced HA-cagF into ureAB locus | Metronidazole, chloramphenicol | This study |
| FC3.1 (cagE::kan/HA-CagF) | Introduced HA-cagF into ureAB locus | Kanamycin, chloramphenicol | This study |
| Plasmid | |||
| pΔcagα | Contains sequences from HP0524 and HP0526, and deletion of HP0525 (cagα) | Ampicillin | 36 |
| pΔcagα::cat-rdxA | cat-rdxA cassette cloned into BamHI site in HP0525 locus of pΔcagα | Ampicillin, chloramphenicol | 36 |
| pASL101.1 | Contains sequences from HP0524 to HP0526 in which two point mutations in ATP-binding motifs are introduced into cagα (K184A, E248A) | Ampicillin | This study |
| pASL102.1 | Restores the introduced point mutations in pASL101.1 | Ampicillin | This study |
| pΔcagβ | Contains sequences from HP0523 and HP0525, and deletion of HP0524 (cagβ) | Ampicillin | 36 |
| pΔcagβ::cat-rdxA | cat-rdxA cassette cloned into BamHI site in HP0524 locus of pΔcagβ | Ampicillin, chloramphenicol | 36 |
| pASL103.1 | cat-rpsL cassette cloned into ClaI site in HP0524 locus of pΔcagβ | Ampicillin, chloramphenicol | This study |
| pASL104.1 | Contains sequences from HP0523 to HP0525 in which two point mutations in ATP-binding motifs are introduced into cagβ (K244A, D550A) | Ampicillin | This study |
| pASL105.1 | Restored the introduced point mutations in pASL104.1 | Ampicillin | This study |
| pΔcagE | Contains sequences from HP0543 and HP0545, and deletion of HP0544 (cagE) | Ampicillin | 36 |
| pΔcagE::cat-rdxA | cat-rdxA cassette cloned into BamHI site in HP0544 locus of pΔcagE | Ampicillin, chloramphenicol | 36 |
| pASL106.1 | cat-rpsL cassette cloned into BamHI site in HP0544 locus of pΔcagE | Ampicillin, chloramphenicol | This study |
| pASL107.1 | Contains sequences from HP0543 to HP0545 in which two point mutations in ATP-binding motifs are introduced into cagE (K603A, D830A) | Ampicillin | This study |
| pASL108.1 | Restored the introduced point mutations in pASL107.1 | Ampicillin | This study |
| pAD-HA-CagF | Contains gene encoding HA-CagF and flanking ureAB sequences | Ampicillin, chloramphenicol | 35 |
All mutant strains were derived from H. pylori 26695.
WB, Walker box.
FIG 1.
Individual Cag T4SS ATPases are not required for assembly of the Cag T4SS core complex. H. pylori mutant strains lacking genes encoding individual ATPases (Δcagα, Δcagβ, and ΔcagE) were modified by introducing a gene encoding HA-CagF into the ureAB chromosomal locus, resulting in strains with the genotypes indicated in the figure (corresponding to FC1.1 [Δcagα/HA-CagF], FC2.1 [Δcagβ/HA-CagF], and FC3.1 [cagE::kan/HA-CagF] in Table 1). T4SS core complexes were immunopurified from these strains, and the preparations were analyzed and visualized by negative-stain electron microscopy (magnification, ×28,000). (A) Core complexes purified from a wild-type (WT) strain engineered to produce HA-CagF (WT/HA-CagF) (positive control). (B to D) Core complexes isolated from mutant strains engineered to produce HA-CagF (Δcagα/HA-CagF, Δcagβ/HA-CagF, and cagE::kan/HA-CagF). Scale bars, 25 nm.
Individual Cag ATPases are required for CagA translocation.
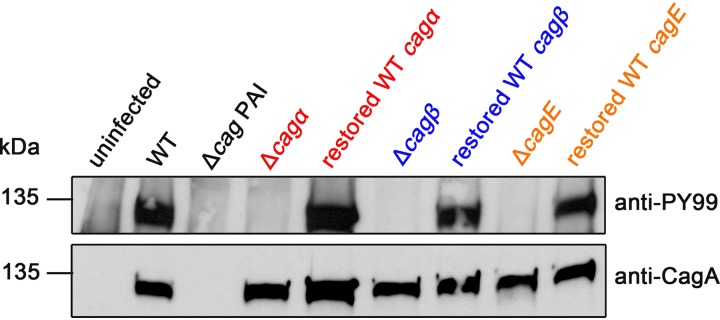
To assess if the individual Cag ATPases are required for CagA translocation into host cells, we cocultured H. pylori strains with AGS gastric epithelial cells and analyzed phosphorylation of CagA. For these experiments, we analyzed unmarked ATPase deletion mutant strains (Δcagα, Δcagβ, and ΔcagE) along with genetically manipulated control strains containing restored wild-type cagα, cagβ, and cagE sequences (named ASL12.1 [restored WT cagα], ASL14.1 [restored WT cagβ], and ASL16.1 [restored WT cagE]), generated as described in Materials and Methods (Table 1). Tyrosine-phosphorylated CagA was detected when the wild-type strain and control strains were cocultured with AGS cells but was not detected when any of the individual ATPase mutants were cocultured with AGS cells (Fig. 2). These results indicate that all three ATPases are required for CagA translocation into AGS cells.
FIG 2.
Individual Cag T4SS ATPases are essential for CagA translocation into AGS gastric epithelial cells. Wild-type (WT) strain 26695, a Δcag PAI mutant strain, and the indicated unmarked deletion mutant strains (Δcagα, Δcagβ, and ΔcagE) were cocultured with AGS cells. Genetically manipulated strains containing restored wild-type ATPase sequences (named ASL12.1 [restored WT cagα], ASL14.1 [restored WT cagβ], and ASL16.1 [restored WT cagE]; Table 1) were tested as controls. Extracts from H. pylori-gastric epithelial cell cocultures were immunoblotted with an anti-CagA antibody to detect CagA and an anti-phosphotyrosine antibody (anti-PY99) to detect phosphorylated CagA.
Cagβ is dispensable for H. pylori-induced NF-κB activation and IL-8 production.
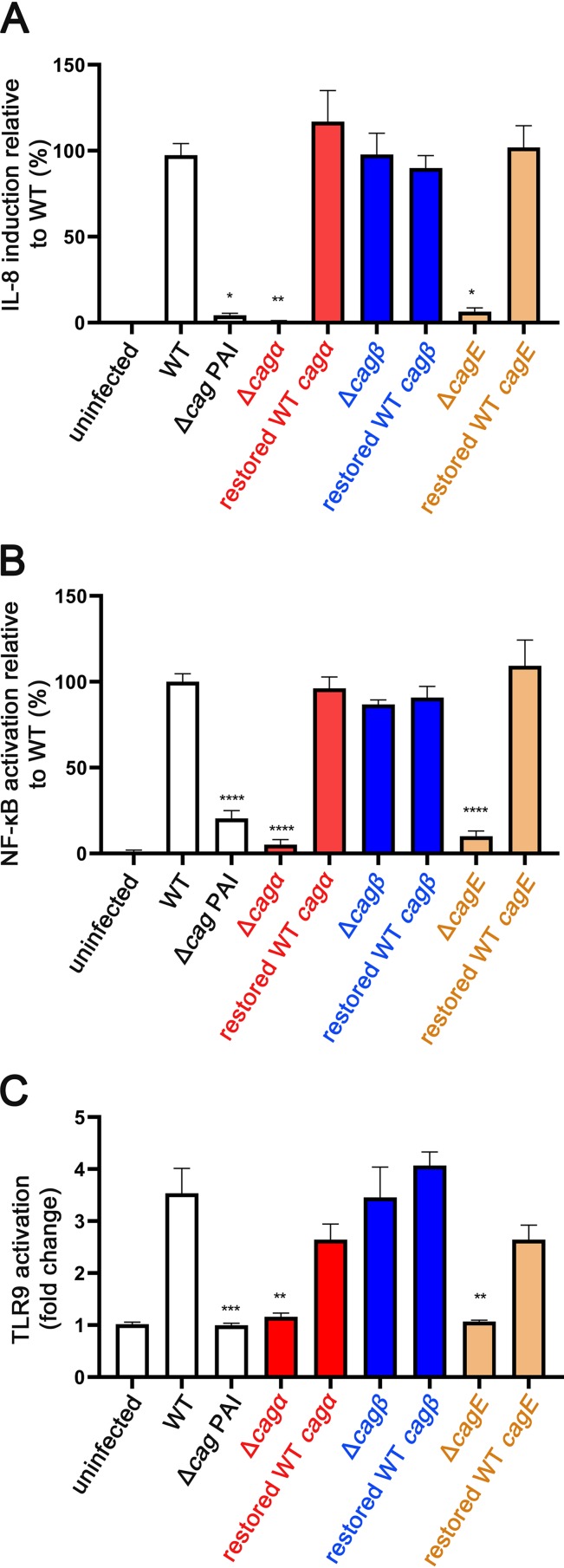
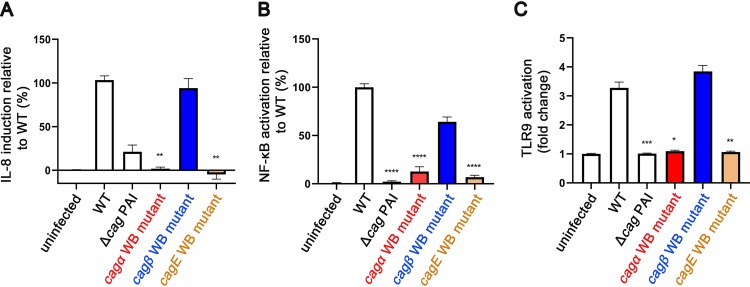
When cocultured with gastric epithelial cells, H. pylori strains containing an intact cag PAI stimulate activation of NF-κB and production of proinflammatory cytokines such as interleukin-8 (IL-8). Multiple genes encoding components of the Cag T4SS are required for these phenotypes (34, 35, 52, 53, 61). To investigate whether the individual ATPases are required for these phenotypes, we cocultured the wild-type and mutant H. pylori strains with AGS cells or AGS-NF-κB reporter cells and quantified IL-8 induction and NF-κB activation as described in Materials and Methods. The Δcagα and ΔcagE mutants were defective in both IL-8 induction and NF-κB activation, whereas the Δcagβ mutant stimulated IL-8 induction and NF-κB activation similar to the wild-type strain (Fig. 3A and B). The IL-8 induction and NF-κB phenotypes were intact in each of the control strains containing wild-type ATPase sequences (Fig. 3A and B). These data indicate that Cagα and CagE are each required for IL-8 secretion and NF-κB activation in gastric epithelial cells, but Cagβ is not required.
FIG 3.
Cagα and CagE, but not Cagβ, are required for three Cag T4SS-dependent alterations in host cells. Wild-type (WT) strain 26695, a Δcag PAI mutant strain, and the indicated unmarked deletion mutant strains (Δcagα, Δcagβ, and ΔcagE) were cocultured with AGS cells, AGS-NF-κB reporter cells, or HEK293-hTLR9 reporter cells. Genetically manipulated strains containing restored wild-type ATPase sequences (named ASL12.1, ASL14.1, and ASL16.1; Table 1) were tested as controls. IL-8 production, NF-κB activation, or TLR9 activation were quantified as described in Materials and Methods. (A, B) Cagα and CagE are required for IL-8 induction and NF-κB activation in AGS gastric epithelial cells. (C) Cagα and CagE are required for H. pylori-induced TLR9 activation in HEK293-hTLR9 reporter cells. The data represent results of three independent experiments with multiple technical replicates. Values represent means ± standard error of the mean (SEM). Statistical significance among groups was determined by Kruskal-Wallis test with Dunnett’s multiple comparison test. *, P ≤ 0.05; **, P ≤ 0.01; ***, P ≤ 0.001; ****, P ≤ 0.0001 compared to WT.
Cagα and CagE are required for H. pylori-induced TLR9 activation.
When cocultured with HEK293-hTLR9 reporter cells, H. pylori strains containing an intact cag PAI activate TLR9 through a process that requires multiple genes encoding components of the Cag T4SS (26). To determine if the individual ATPases are required for TLR9 activation, we cocultured the wild-type strain, mutant strains, and genetically manipulated control strains with the HEK293-hTLR9 reporter cells. The Δcagα and ΔcagE mutants were defective in activating TLR9, whereas the Δcagβ mutant retained the TLR9 activation phenotype (Fig. 3C). The genetically manipulated control strains containing restored wild-type ATPase sequences (ASL12.1, ASL14.1, and ASL16.1) exhibited an intact TLR9 activation phenotype (Fig. 3C). These data indicate that Cagα and CagE are required for H. pylori-induced TLR9 activation, but Cagβ is not required.
Putative ATP-binding motifs in Cag ATPases.
Previous cryo-electron tomography (cryo-ET) analyses revealed detectable differences in the structure of the Cag T4SS inner membrane complex in ATPase deletion mutants compared to the wild-type strain (36). Most notably, the inner membrane complex was almost completely absent in the ΔCagE mutant (36). This suggests that protein-protein interactions involving ATPases are important for assembly or stability of the Cag T4SS inner membrane complex. The ATPases (especially CagE) could potentially have important roles in assembly or stability of the T4SS inner membrane complex, independent of their enzymatic activity. Therefore, in addition to analyzing T4SS-dependent activities in ATPase deletion mutant strains, we undertook experiments to generate mutant strains containing substitution mutations in sites within the ATPases that are predicted to be required for enzymatic activity. By comparing the three H. pylori Cag ATPases to sequences of corresponding VirB11, VirB4, and VirD4 ATPases in T4SSs of other bacterial species, we identified putative ATP-binding motifs (Walker-A and Walker-B motifs) in Cagα, CagE, and Cagβ (Fig. S1 in the supplemental material). We introduced point mutations into the corresponding regions of the 3 individual chromosomal ATPase genes encoding the Walker-A and Walker-B motifs. The point mutations resulted in a change from a conserved lysine to alanine in the Walker-A motifs and a change from a conserved aspartic acid or glutamic acid to alanine in the Walker-B motifs (Table 1). The resulting mutant strains were named ASL11.1 (cagα Walker box [WB] mutant), ASL13.1(cagβ WB mutant), and ASL15.1 (cagE WB mutant) (Table 1). Proteomic analysis of membrane fractions allowed us to detect all three ATPase proteins in each of the mutant strains (Table 2). The proteomic data also allowed a semiquantitative assessment of ATPase abundance in the mutant strains compared to the WT strain. The number of CagE spectral counts detected in ASL15.1 was similar to the number of CagE spectral counts detected in the WT strain and other mutant strains (ASL11.1 and ASL13.1), which suggests that the introduction of Walker box mutations into CagE did not substantially alter CagE stability. The number of Cagα spectral counts detected in ASL11.1 was lower than the number of Cagα spectral counts detected in the WT strain or other mutants, and similarly, the number of Cagβ spectral counts was somewhat lower in ASL13.1 than in the other strains. Therefore, the introduction of mutations into Cagα (and possibly Cagβ) might diminish the stability of these proteins. The phenotypes of the latter two mutants are potentially attributable to both reduced abundance of Cagα or Cagβ as well as loss of enzymatic activity.
TABLE 2.
Mass spectrometric detection of Cag ATPases in wild-type and mutant strains
| Protein | Wild type | Δcag PAI | ASL11.1 | ASL13.1 | ASL15.1 |
|---|---|---|---|---|---|
| CagAa | 265 | 0 | 309 | 263 | 327 |
| Cagα | 11 | 0 | 2 | 8 | 10 |
| Cagβ | 19 | 0 | 26 | 10 | 23 |
| CagE | 25 | 0 | 22 | 15 | 21 |
| Fumarate reductasea | 142 | 172 | 148 | 174 | 175 |
| Acetyl-CoA synthetasea | 67 | 71 | 71 | 54 | 67 |
| Total spectral counts | 17,477 | 18,500 | 21,735 | 17,865 | 21,139 |
Numbers of spectral counts for CagA (encoded by the cag PAI), fumarate reductase, and acetyl-CoA synthetase (non-Cag proteins) are shown as controls for comparison.
Functional ATP-binding motifs in the Cag ATPases are required for CagA translocation.
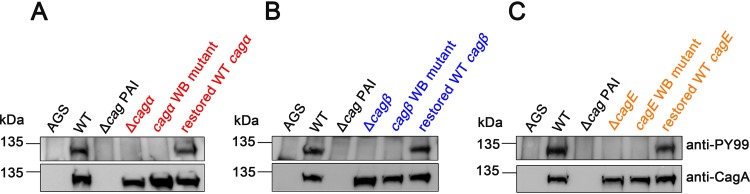
We then tested the capacity of the three Walker box mutant strains to translocate CagA into AGS gastric epithelial cells. None of the ATP-binding motif mutant strains (ASL11.1, ASL13.1, and ASL15.1) was able to translocate CagA into AGS cells (Fig. 4). Similar to the results shown in Fig. 2, all the engineered control strains containing wild-type ATPase sequences (ASL12.1, ASL14.1, and ASL16.1) exhibited an intact CagA translocation phenotype (Fig. 4). These data indicate that functional Walker motifs in each of the individual ATPases (Cagα, CagE, and Cagβ) are required for CagA translocation into host cells.
FIG 4.
Functional Walker motifs in individual Cag T4SS ATPases are required for CagA translocation into AGS gastric epithelial cells. Strains containing mutations in Walker motifs of Cagα, Cagβ, or CagE (cagα WB, cagβ WB, and cagE WB mutants, corresponding to ASL11.1, ASL13.1, or ASL 15.1, respectively, in Table 1) were generated as described in Materials and Methods. Wild-type (WT) strain 26695, a Δcag PAI mutant strain, and the indicated mutant strains were cocultured with AGS cells. Genetically manipulated strains containing restored wild-type ATPase sequences (named ASL12.1, ASL14.1, and ASL16.1; Table 1) were tested as controls. Extracts from H. pylori-gastric epithelial cell cocultures were immunoblotted with an anti-CagA antibody to detect CagA and an anti-phosphotyrosine antibody (anti-PY99) to detect phosphorylated CagA.
Functional ATP-binding motifs in Cagα and CagE are required for NF-κB activation, IL-8 induction, and TLR9 activation.
To test if functional Walker motifs in the ATPases are necessary for other Cag T4SS-dependent phenotypes, we analyzed IL-8 production, NF-κB activation, and TLR9 activation induced by the Walker box mutant strains (ASL11.1, ASL13.1, and ASL15.1). The cagα and cagE Walker box mutants were defective in inducing IL-8 and NF-κB, whereas the cagβ Walker box mutant stimulated IL-8 production and NF-κB activation similar to the WT strain (Fig. 5A and B). Similarly, the cagα and cagE Walker box mutants were defective in TLR9 activation compared to the WT strain (Fig. 5C). However, the cagβ Walker box mutant induced TLR9 activation similar to the wild-type strain (Fig. 5C). These data indicate that intact Walker box motifs in Cagα and CagE are required for all the phenotypes tested (NF-κB activation, IL-8 induction, and TLR9 activation), whereas intact Walker box motifs in Cagβ are not required for these phenotypes.
FIG 5.
Functional Walker motifs in Cagα and Cagβ are required for three Cag T4SS-dependent phenotypes. Wild-type strain 26695, a Δcag PAI mutant, and strains containing mutations in Walker motifs of Cagα, Cagβ, or CagE (ASL11.1, ASL13.1, or ASL 15.1; Table 1 and Fig. S1) were cocultured with AGS cells, AGS-NF-κB reporter cells, or HEK293-hTLR9 reporter cells. IL-8 production, NF-κB activation, or TLR9 activation were quantified as described in Materials and Methods. (A, B, and C) Functional Walker motifs in Cagα and CagE are essential for H. pylori-induced IL-8 induction, NF-κB activation, and TLR9 activation. The data represent results of three independent experiments with multiple technical replicates. Values represent mean ± standard error of the mean (SEM). Statistical significance among groups was determined by Kruskal-Wallis test with Dunnett’s multiple comparison test. *, P ≤ 0.05; **, P ≤ 0.01; ***, P ≤ 0.001; ****, P ≤ 0.0001 compared to WT.
DISCUSSION
H. pylori causes multiple alterations in gastric epithelial cells through processes dependent on the Cag T4SS (2, 9, 10, 12). Many Cag T4SS-dependent cellular alterations result from actions of CagA, whereas other Cag T4SS-dependent cellular alterations do not require CagA. For example, stimulation of IL-8 production by H. pylori has been attributed to the entry of lipopolysaccharide metabolites (HBP or ADP heptose) and/or peptidoglycan into host cells (20–24). HBP or ADP heptose activates alpha-kinase 1 (ALPK1) to phosphorylate tumor necrosis factor receptor-associated factor (TRAF)-interacting protein with forkhead-associated domain (TIFA) within host cells (20–22), and peptidoglycan is recognized by the intracellular host defense molecule NOD1 (24). Intracellular recognition of these pathogen-associated molecular patterns (PAMPs) leads to activation of multiple signaling pathways, including NOD1 signaling pathways and NOD-1 independent pathways that involve ALPK1 and TIFA, resulting in NF-κB activation (20–23). Activation of TLR9 has been attributed to the entry of bacterial DNA into host cells (26). Since the Cag T4SS is required for phenotypes linked to the entry of multiple different types of H. pylori constituents into host cells, this provides an opportunity to undertake a comparative analysis of the processes by which different bacterial constituents are delivered into host cells.
To investigate the bacterial energetic requirements for CagA translocation and Cag T4SS-dependent cellular alterations in gastric epithelial cells, we generated mutant strains lacking individual ATPase components of the Cag T4SS. As a first step in analyzing the mutant strains, we investigated their capacity to assemble Cag T4SS core complexes. The H. pylori Cag T4SS core complex contains five proteins, all of which are required for T4SS function (35–37). We successfully purified core complexes from each of the ATPase mutant strains, which indicates that these ATPases are not required for core complex assembly. This result is consistent with the results of recent cryo-electron tomography studies of the H. pylori Cag T4SS (36) and the Legionella Dot/Icm T4SS (62).
As a next step, we tested the ATPase mutant strains for the capacity to translocate CagA into host cells and found that all three ATPases are required for this activity. Previous studies used an insertional mutagenesis approach to disrupt Cag ATPases and reported that all three ATPases are required for the translocation of CagA protein into host cells (34). Analyses of unmarked deletion mutant strains (along with control strains) in the current study provide strong evidence that all three ATPases are required for CagA translocation, thereby indicating that the three ATPases are not functionally redundant.
We next tested the mutant strains for the capacity to stimulate IL-8 production. Consistent with the results of a previous study (34), we found that H. pylori-induced stimulation of IL-8 production requires CagE and Cagα but does not require Cagβ. The bacterial energetic requirements for H. pylori-induced NF-κB activation were identical to the requirements for IL-8 production, consistent with a current model in which NF-κB activation is required for IL-8 production (20, 32, 63–65).
A previous study reported that CagE was required for H. pylori-induced TLR9 activation (26), but the energetic requirements for this phenotype have not been previously studied in detail. We show that the energetic requirements for H. pylori-induced TLR9 activation are identical to requirements for IL-8 production and NF-κB activation (i.e., requiring CagE and Cagα but not Cagβ). This finding differs from a requirement of the Cagβ homolog (VirD4) for delivery of DNA into recipient cells by E. coli conjugative T4SSs or the A. tumefaciens VirB/VirD4 T4SS (48, 50).
The observation that a Cagβ mutant is defective in CagA translocation but still capable of stimulating IL-8 production, NF-κB activation, and TLR9 activation provides important insights into the mechanisms by which these processes occur. Specifically, these results suggest that the H. pylori substrates mediating IL-8 induction, NF-κB activation, or TLR9 activation are recruited or delivered to host cells through one or more Cag T4SS-dependent pathways different from those used for recruitment and delivery of CagA. A current model proposes that CagA is recruited from the cytoplasm to the inner membrane complex of the T4SS through interactions with Cagβ, a VirD4 homolog (46). Similarly, in E. coli conjugative T4SSs and the A. tumefaciens T4SS, VirD4 acts as a coupling protein, responsible for recruiting DNA and protein substrates (48, 50). Since H. pylori-induced IL-8 secretion, NF-κB activation, and TLR9 activation do not require Cagβ, we speculate that lipopolysaccharide (LPS) metabolites, peptidoglycan, or DNA fragments might diffuse from the cytoplasm or periplasm into the T4SS apparatus through a nonspecific process that does not require recruitment by a coupling protein. Alternatively, we speculate that LPS metabolites, peptidoglycan, or DNA might transit the bacterial cell envelope through one or more mechanisms different from those used for secretion of CagA. For example, these nonprotein H. pylori constituents could potentially be released into the extracellular environment through bacterial autolysis, as components of outer membrane vesicles, or through other processes, and the Cag T4SS may then facilitate the entry of these PAMPs into host cells. Consistent with the latter hypothesis, treatment of H. pylori-host cell cocultures with DNase I partially reduced the level of TLR9 activation (26). In addition to the Cag T4SS, the H. pylori strain used in these studies harbors a second T4SS (ComB system), which is required for natural transformation and conjugative transfer of DNA (6). Cross talk among H. pylori T4SSs could potentially occur (for example, an ATPase from the ComB system contributing to the function of the Cag T4SS), but there is no experimental evidence at present to support this possibility (26). In future studies, it will be important to determine whether H. pylori DNA, LPS metabolites, and peptidoglycan enter cells independently or if proteins analogous to the relaxosome utilized in conjugation systems and the A. tumefaciens VirB/VirD4 system are required.
ATPases (especially CagE) potentially have important roles in the assembly or stability of the T4SS inner membrane complex (36), independent of their enzymatic activity. If the ATPases contribute to T4SS activity through both enzymatic and nonenzymatic functions, it would not be possible to discriminate enzymatic and nonenzymatic functions through analysis of deletion mutant strains. In the current study, we generated H. pylori mutant strains harboring point mutations in sites predicted to be required for ATPase enzymatic activity and tested the hypothesis that these mutant strains might exhibit phenotypes different from those observed with deletion mutant strains. Previous studies have identified putative ATP-binding motifs in Cagα (66) and CagE (67), and mutagenesis of the Walker-A motif in the C-terminal portion of CagE abolished enzymatic activity of a recombinant protein produced in E. coli (67). Cag ATPase Walker box mutations have not previously been introduced into H. pylori chromosomal genes. In the current study, we found that each of the H. pylori mutant strains harboring point mutations in Walker boxes exhibited the same phenotypes as the deletion mutant strains. These data support a hypothesis that enzymatic activities of the three ATPases are required for Cag T4SS activities.
In summary, this study indicates that the three Cag ATPases have nonredundant functions required for delivery of CagA into host cells and indicates that the energetic requirements for phenotypes associated with intracellular entry of nonprotein H. pylori constituents into host cells differ from the energetic requirements for translocation of CagA. In future studies, it will be important to further elucidate differences in the mechanisms underlying the recruitment, secretion, and delivery of CagA into host cells compared to mechanisms underlying entry of nonprotein H. pylori constituents into host cells.
MATERIALS AND METHODS
Growth of H. pylori strains.
H. pylori 26695 and isogenic mutant strains were grown on Trypticase soy agar plates supplemented with 5% sheep blood at 37°C in room air containing 5% CO2. Antibiotic concentrations for the selection of H. pylori mutant strains were as follows: chloramphenicol (5 μg/ml), kanamycin (10 μg/ml), metronidazole (7.5 to 15 μg/ml), or streptomycin (25 or 50 μg/ml). The E. coli strain DH5α was used for plasmid propagation and was grown on Luria-Bertani agar plates or in Luria-Bertani liquid medium supplemented with appropriate antibiotics (ampicillin [50 μg/ml], kanamycin [25 μg/ml], or chloramphenicol [25 μg/ml]).
Generation of H. pylori mutant strains.
Unmarked deletion mutant strains (Δcagα, Δcagβ, and ΔcagE) were generated as described previously (36). To generate ATP-binding motif mutant strains, we introduced point mutations into sites encoding amino acids in Walker-A and Walker-B motifs (specifically, K184A and E248A in cagα; K244A and D550A in cagβ; and K603A and D830A in cagE) (Table 1 and Fig. S1 in the supplemental material). The three cag ATPase genes, including the point mutations described above, along with 0.5-kb flanking DNA, were synthesized (GenScript) and cloned into a pUC57 vector. ATP-binding motif mutant strains were generated by introducing plasmids (containing both Walker box mutations) into H. pylori strains containing either a cat-rdxA cassette (52) or a cat-rpsL cassette (53) in the genes of interest (Table 1). In parallel, we used site-directed mutagenesis to change the point mutations in plasmids back to wild-type nucleotides. Plasmids containing the corrected point mutations were transformed into strains containing cat-rdxA or cat-rpsL cassettes inserted in the genes of interest, resulting in control strains containing wild-type-like ATPase gene sequences (Table 1). PCR and sequencing of PCR products were used to confirm that the desired sequences were introduced into the appropriate cag ATPase genes.
Proteomic analysis of H. pylori membrane fractions.
H. pylori were cultured in Brucella broth containing 10% fetal bovine serum for 24 h at 37°C in room air containing 5% CO2. The bacteria were harvested by centrifugation and then were washed in buffer (50 mM Tris, 100 mM NaCl, 27 mM KCl, 1 mM CaCl2, 0.5 mM MgCl2 [pH 7.4]) and centrifuged at 4,500 × g for 10 min. After two additional washing steps, the pelleted bacteria were resuspended in lysis buffer (50 mM Tris, 1 mM MgCl2, protease inhibitor [cOmplete protease inhibitor cocktail tablets, Roche] [pH 7.4]) and then sonicated on ice. The lysate was centrifuged at 4,500 × g for 10 min to remove any remaining intact bacteria, and the resulting supernatant was centrifuged at 10,000 × g for 1 h at 4°C. The pellet (membrane fraction) was then resuspended in RIPA buffer (50 mM Tris-HCl, 150 mM NaCl, 1 mM EDTA, 1% NP40, 0.25% sodium deoxycholate, protease inhibitor [pH 8.0]). The membrane fraction was solubilized by rotating the sample on a rotisserie for 1 h at 4°C. The solubilized membrane fraction was then collected after centrifugation at 21,000 × g for 10 min at 4°C. The membrane fraction was then subjected to proteomic analysis.
Samples prepared as described above were run 2 cm into a 10% Bis-Tris NuPAGE gel. Gels were stained with Coomassie blue, and an in-gel trypsin digest was performed. Single-dimensional liquid chromatography-tandem mass spectrometry (LC-MS/MS) was performed using Thermo Fisher QExactive Plus equipped with a nano-electrospray source and attached to an LC3000 (Thermo Fisher) high-pressure liquid chromatography (HPLC) unit with an autosampler. Peptides were resolved via reversed-phase separation (90 min total cycle time). Full MS (MS1) were collected at 70,000 resolution with an automatic gain control (AGC) target of 3e6, and MS/MS were collected at 17,500 resolution with an AGC target of 1e5, excluding unassigned charge states and requiring an intensity threshold of 2e4. Fifteen MS/MS were collected for each MS1 with a dynamic exclusion window of 10 s. Peptides were resolved via reversed-phase separation (90-min total cycle time). Peptide MS/MS spectra were acquired data dependently with 2 full-scan MS followed by 5 MS/MS scans. The peptide MS/MS spectral data were queried using SEQUEST (full tryptic specificity) and searched against the H. pylori 26695 protein database, to which both common contaminants and reversed versions of H. pylori protein sequences had been added. Peptide identifications were filtered and collated to proteins using Scaffold 4 (Proteome Systems). Protein identifications required a minimum of 2 unique peptides per protein and were filtered to a 5% false discovery rate (both peptide and protein).
Isolation of the H. pylori Cag T4SS outer membrane core complex.
The Cag T4SS outer membrane core complex was isolated from H. pylori strains producing HA-tagged forms of CagF (designated HA-CagF) using a previously described immunoprecipitation approach (35). We first transformed Δcagα, Δcagβ, or cagE::kan (kanamycin cassette inserted within the cagE gene) mutant strains with plasmids containing a gene encoding CagF with an HA-epitope tag at the N terminus and containing a chloramphenicol cassette (35). This approach introduced sequences encoding HA-tagged CagF into the H. pylori ureAB chromosomal locus (35). Outer membrane core complexes were isolated as previously described (35). Briefly, strains were grown in liquid cultures for 16 h, pelleted at 3,300 × g for 15 min at 4°C, resuspended in RIPA buffer (50 mM HEPES, 100 mM NaCl, 1% NP-40, and 0.25% deoxycholate supplemented with 1 mM phenylmethylsulfonyl fluoride and protease inhibitors [Roche]), sonicated on ice, and then incubated for 1 h at 4°C; bacterial lysates were collected and then incubated with anti-HA antibodies noncovalently linked to protein G Dynabeads for 30 min; HA peptide was utilized to selectively elute the proteins. Samples were analyzed by negative-stain EM, as described previously (54).
CagA translocation assay.
Translocation of oncoprotein CagA into AGS human gastric epithelial cells was assessed using previously described methodology (52, 55–59). Briefly, we cocultured H. pylori strains with AGS cells at a multiplicity of infection (MOI) of 100:1 for 5 to 6 h at 37°C. CagA translocation was evaluated by detecting tyrosine phosphorylation of CagA, using an anti-phosphotyrosine antibody (α-PY99, Santa Cruz Biotechnology), and CagA was detected using anti-CagA antibody (Santa Cruz Biotechnology).
IL-8 induction assay.
AGS cells were seeded at 2 × 105 cells per well in a 12-well culture dish overnight and then cocultured with H. pylori strains at an MOI of 100:1 for 5 to 6 h at 37°C with 5% CO2. The supernatants were collected after being centrifuged at 15,000 × g for 5 min. IL-8 induction was quantified by using Human CXCL8 enzyme-linked immunosorbent assay (ELISA) (R&D systems), following the manufacturer’s protocol.
NF-κB activation assay.
NF-κB activity was quantified by coculturing an NF-κB luciferase reporter cell line (in an AGS gastric epithelial cell background) with H. pylori strains, as previously described (60). Briefly, the reporter cell line was seeded in a 96-well plate overnight and then infected with H. pylori strains at an MOI of 100:1 for 2.5 h. The luciferase activity of cell lysates was measured using a Steady-Glo luciferase assay substrate (Promega).
TLR9 activation assay.
TLR9 activation by H. pylori strains was analyzed by coculturing the bacteria with TLR9 reporter cells for 24 h, using the approach described previously (26). Briefly, TLR9+ (HEK-Blue-hTLR9) and parental (HEK-Blue-Null1) cells (InvivoGen) were seeded in 96-well plates and cocultured with H. pylori strains at an MOI of 100:1 at 37°C with 5% CO2 for 24 h. The resulting supernatants were mixed with HEK-Blue detection media (InvivoGen), and the signals in the plates were measured by spectrophotometer at 650 nm.
Supplementary Material
ACKNOWLEDGMENTS
The work described in this paper was supported by the National Institutes of Health (AI118932, CA116087, AI039657, and T32AI112541) and the Department of Veterans Affairs (1I01BX004447). Proteomic studies were supported by the Digestive Disease Research Center (P30DK058404) and the Vanderbilt Ingram Cancer Institute (P30CA068485).
Footnotes
Supplemental material is available online only.
REFERENCES
- 1.Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, Malfertheiner P, Graham DY, Wong VWS, Wu JCY, Chan FKL, Sung JJY, Kaplan GG, Ng SC. 2017. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology 153:420–429. doi: 10.1053/j.gastro.2017.04.022. [DOI] [PubMed] [Google Scholar]
- 2.Brown LM. 2000. Helicobacter pylori: epidemiology and routes of transmission. Epidemiol Rev 22:283–297. doi: 10.1093/oxfordjournals.epirev.a018040. [DOI] [PubMed] [Google Scholar]
- 3.Gilbreath JJ, Cody WL, Merrell DS, Hendrixson DR. 2011. Change is good: variations in common biological mechanisms in the epsilonproteobacterial genera Campylobacter and Helicobacter. Microbiol Mol Biol Rev 75:84–132. doi: 10.1128/MMBR.00035-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suerbaum S, Michetti P. 2002. Helicobacter pylori infection. N Engl J Med 347:1175–1186. doi: 10.1056/NEJMra020542. [DOI] [PubMed] [Google Scholar]
- 5.Cover TL, Blaser MJ. 2009. Helicobacter pylori in health and disease. Gastroenterology 136:1863–1873. doi: 10.1053/j.gastro.2009.01.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rohrer S, Holsten L, Weiss E, Benghezal M, Fischer W, Haas R. 2012. Multiple pathways of plasmid DNA transfer in Helicobacter pylori. PLoS One 7:e45623. doi: 10.1371/journal.pone.0045623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hofreuter D, Odenbreit S, Haas R. 2001. Natural transformation competence in Helicobacter pylori is mediated by the basic components of a type IV secretion system. Mol Microbiol 41:379–391. doi: 10.1046/j.1365-2958.2001.02502.x. [DOI] [PubMed] [Google Scholar]
- 8.Backert S, Haas R, Gerhard M, Naumann M. 2017. The Helicobacter pylori type iv secretion system encoded by the cag pathogenicity island: architecture, function, and signaling. Curr Top Microbiol Immunol 413:187–220. doi: 10.1007/978-3-319-75241-9_8. [DOI] [PubMed] [Google Scholar]
- 9.Fischer W. 2011. Assembly and molecular mode of action of the Helicobacter pylori Cag type IV secretion apparatus. FEBS J 278:1203–1212. doi: 10.1111/j.1742-4658.2011.08036.x. [DOI] [PubMed] [Google Scholar]
- 10.Terradot L, Waksman G. 2011. Architecture of the Helicobacter pylori Cag-type IV secretion system. FEBS J 278:1213–1222. doi: 10.1111/j.1742-4658.2011.08037.x. [DOI] [PubMed] [Google Scholar]
- 11.Olbermann P, Josenhans C, Moodley Y, Uhr M, Stamer C, Vauterin M, Suerbaum S, Achtman M, Linz B. 2010. A global overview of the genetic and functional diversity in the Helicobacter pylori cag pathogenicity island. PLoS Genet 6:e1001069. doi: 10.1371/journal.pgen.1001069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bourzac KM, Guillemin K. 2005. Helicobacter pylori–host cell interactions mediated by type IV secretion. Cell Microbiol 7:911–919. doi: 10.1111/j.1462-5822.2005.00541.x. [DOI] [PubMed] [Google Scholar]
- 13.Park JY, Forman D, Waskito LA, Yamaoka Y, Crabtree JE. 2018. Epidemiology of Helicobacter pylori and CagA-positive infections and global variations in gastric cancer. Toxins 10:163. doi: 10.3390/toxins10040163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cover TL. 2016. Helicobacter pylori diversity and gastric cancer risk. mBio 7:e01869. doi: 10.1128/mBio.01869-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatakeyama M. 2014. Helicobacter pylori CagA and gastric cancer: a paradigm for hit-and-run carcinogenesis. Cell Host Microbe 15:306–316. doi: 10.1016/j.chom.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Tegtmeyer N, Neddermann M, Asche CI, Backert S. 2017. Subversion of host kinases: a key network in cellular signaling hijacked by Helicobacter pylori CagA. Mol Microbiol 105:358–372. doi: 10.1111/mmi.13707. [DOI] [PubMed] [Google Scholar]
- 17.Backert S, Tegtmeyer N. 2017. Type IV secretion and signal transduction of Helicobacter pylori CagA through interactions with host cell receptors. Toxins 9:115. doi: 10.3390/toxins9040115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatakeyama M. 2004. Oncogenic mechanisms of the Helicobacter pylori CagA protein. Nat Rev Cancer 4:688–694. doi: 10.1038/nrc1433. [DOI] [PubMed] [Google Scholar]
- 19.Ohnishi N, Yuasa H, Tanaka S, Sawa H, Miura M, Matsui A, Higashi H, Musashi M, Iwabuchi K, Suzuki M, Yamada G, Azuma T, Hatakeyama M. 2008. Transgenic expression of Helicobacter pylori CagA induces gastrointestinal and hematopoietic neoplasms in mouse. Proc Natl Acad Sci U S A 105:1003–1008. doi: 10.1073/pnas.0711183105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gall A, Gaudet RG, Gray-Owen SD, Salama NR. 2017. TIFA signaling in gastric epithelial cells initiates the cag type 4 secretion system-dependent innate immune response to Helicobacter pylori infection. mBio 8:e01168-17. doi: 10.1128/mBio.01168-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stein SC, Faber E, Bats SH, Murillo T, Speidel Y, Coombs N, Josenhans C. 2017. Helicobacter pylori modulates host cell responses by CagT4SS-dependent translocation of an intermediate metabolite of LPS inner core heptose biosynthesis. PLoS Pathog 13:e1006514. doi: 10.1371/journal.ppat.1006514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zimmermann S, Pfannkuch L, Al-Zeer MA, Bartfeld S, Koch M, Liu J, Rechner C, Soerensen M, Sokolova O, Zamyatina A, Kosma P, Mäurer AP, Glowinski F, Pleissner K-P, Schmid M, Brinkmann V, Karlas A, Naumann M, Rother M, Machuy N, Meyer TF. 2017. ALPK1- and TIFA-dependent innate immune response triggered by the Helicobacter pylori type IV secretion system. Cell Rep 20:2384–2395. doi: 10.1016/j.celrep.2017.08.039. [DOI] [PubMed] [Google Scholar]
- 23.Pfannkuch L, Hurwitz R, Traulsen J, Sigulla J, Poeschke M, Matzner L, Kosma P, Schmid M, Meyer TF. 2019. ADP heptose, a novel pathogen-associated molecular pattern identified in Helicobacter pylori. FASEB J 33:9087–9099. doi: 10.1096/fj.201802555R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Viala J, Chaput C, Boneca IG, Cardona A, Girardin SE, Moran AP, Athman R, Mémet S, Huerre MR, Coyle AJ, DiStefano PS, Sansonetti PJ, Labigne A, Bertin J, Philpott DJ, Ferrero RL. 2004. Nod1 responds to peptidoglycan delivered by the Helicobacter pylori cag pathogenicity island. Nat Immunol 5:1166–1174. doi: 10.1038/ni1131. [DOI] [PubMed] [Google Scholar]
- 25.Varga MG, Peek RM. 2017. DNA transfer and Toll-like receptor modulation by Helicobacter pylori. Curr Top Microbiol Immunol 400:169–193. doi: 10.1007/978-3-319-50520-6_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Varga MG, Shaffer CL, Sierra JC, Suarez G, Piazuelo MB, Whitaker ME, Romero-Gallo J, Krishna US, Delgado A, Gomez MA, Good JAD, Almqvist F, Skaar EP, Correa P, Wilson KT, Hadjifrangiskou M, Peek RM. 2016. Pathogenic Helicobacter pylori strains translocate DNA and activate TLR9 via the cancer-associated cag type IV secretion system. Oncogene 35:6262–6269. doi: 10.1038/onc.2016.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lai C-H, Wang H-J, Chang Y-C, Hsieh W-C, Lin H-J, Tang C-H, Sheu JJ-C, Lin C-J, Yang M-S, Tseng S-F, Wang W-C. 2011. Helicobacter pylori CagA-mediated IL-8 induction in gastric epithelial cells is cholesterol-dependent and requires the C-terminal tyrosine phosphorylation-containing domain. FEMS Microbiol Lett 323:155–163. doi: 10.1111/j.1574-6968.2011.02372.x. [DOI] [PubMed] [Google Scholar]
- 28.Lim JW, Kim KH, Kim H. 2009. αPix interacts with Helicobacter pylori CagA to induce IL-8 expression in gastric epithelial cells. Scand J Gastroenterol 44:1166–1172. doi: 10.1080/00365520903144398. [DOI] [PubMed] [Google Scholar]
- 29.Kim S-Y, Lee Y-C, Kim HK, Blaser MJ. 2006. Helicobacter pylori CagA transfection of gastric epithelial cells induces interleukin-8. Cell Microbiol 8:97–106. doi: 10.1111/j.1462-5822.2005.00603.x. [DOI] [PubMed] [Google Scholar]
- 30.Brandt S, Kwok T, Hartig R, König W, Backert S. 2005. NF-κB activation and potentiation of proinflammatory responses by the Helicobacter pylori CagA protein. Proc Natl Acad Sci U S A 102:9300–9305. doi: 10.1073/pnas.0409873102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gorrell RJ, Guan J, Xin Y, Tafreshi MA, Hutton ML, McGuckin MA, Ferrero RL, Kwok T. 2013. A novel NOD1- and CagA-independent pathway of interleukin-8 induction mediated by the Helicobacter pylori type IV secretion system. Cell Microbiol 15:554–570. doi: 10.1111/cmi.12055. [DOI] [PubMed] [Google Scholar]
- 32.Sokolova O, Borgmann M, Rieke C, Schweitzer K, Rothkötter H-J, Naumann M. 2013. Helicobacter pylori induces type 4 secretion system-dependent, but CagA-independent activation of IκBs and NF-κB/RelA at early time points. Int J Med Microbiol 303:548–552. doi: 10.1016/j.ijmm.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 33.Crabtree JE, Xiang Z, Lindley IJ, Tompkins DS, Rappuoli R, Covacci A. 1995. Induction of interleukin-8 secretion from gastric epithelial cells by a cagA negative isogenic mutant of Helicobacter pylori. J Clin Pathol 48:967–969. doi: 10.1136/jcp.48.10.967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fischer W, Püls J, Buhrdorf R, Gebert B, Odenbreit S, Haas R. 2001. Systematic mutagenesis of the Helicobacter pylori cag pathogenicity island: essential genes for CagA translocation in host cells and induction of interleukin-8. Mol Microbiol 42:1337–1348. doi: 10.1046/j.1365-2958.2001.02714.x. [DOI] [PubMed] [Google Scholar]
- 35.Frick-Cheng AE, Pyburn TM, Voss BJ, McDonald WH, Ohi MD, Cover TL. 2016. Molecular and structural analysis of the Helicobacter pylori type iv secretion system core complex. mBio 7:e02001. doi: 10.1128/mBio.02001-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu B, Khara P, Song L, Lin AS, Frick-Cheng AE, Harvey ML, Cover TL, Christie PJ. 2019. In situ molecular architecture of the Helicobacter pylori Cag type IV secretion system. mBio 10:e00849-19. doi: 10.1128/mBio.00849-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chung JM, Sheedlo MJ, Campbell AM, Sawhney N, Frick-Cheng AE, Lacy DB, Cover TL, Ohi MD. 2019. Structure of the Helicobacter pylori Cag type IV secretion system. Elife 8:e47644. doi: 10.7554/eLife.47644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang Y-W, Shaffer CL, Rettberg LA, Ghosal D, Jensen GJ. 2018. In vivo structures of the Helicobacter pylori cag type IV secretion system. Cell Rep 23:673–681. doi: 10.1016/j.celrep.2018.03.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alvarez-Martinez CE, Christie PJ. 2009. Biological diversity of prokaryotic type IV secretion systems. Microbiol Mol Biol Rev 73:775–808. doi: 10.1128/MMBR.00023-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wallden K, Rivera-Calzada A, Waksman G. 2010. Microreview: type IV secretion systems: versatility and diversity in function. Cell Microbiol 12:1203–1212. doi: 10.1111/j.1462-5822.2010.01499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fronzes R, Christie PJ, Waksman G. 2009. The structural biology of type IV secretion systems. Nat Rev Microbiol 7:703–714. doi: 10.1038/nrmicro2218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Christie PJ, Whitaker N, González-Rivera C. 2014. Mechanism and structure of the bacterial type IV secretion systems. Biochim Biophys Acta 1843:1578–1591. doi: 10.1016/j.bbamcr.2013.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ilangovan A, Connery S, Waksman G. 2015. Structural biology of the Gram-negative bacterial conjugation systems. Trends Microbiol 23:301–310. doi: 10.1016/j.tim.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 44.Galán JE, Waksman G. 2018. Protein-injection machines in bacteria. Cell 172:1306–1318. doi: 10.1016/j.cell.2018.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Savvides SN, Yeo H-J, Beck MR, Blaesing F, Lurz R, Lanka E, Buhrdorf R, Fischer W, Haas R, Waksman G. 2003. VirB11 ATPases are dynamic hexameric assemblies: new insights into bacterial type IV secretion. EMBO J 22:1969–1980. doi: 10.1093/emboj/cdg223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jurik A, Hausser E, Kutter S, Pattis I, Prassl S, Weiss E, Fischer W. 2010. The coupling protein Cagβ and its interaction partner CagZ are required for type IV secretion of the Helicobacter pylori CagA protein. Infect Immun 78:5244–5251. doi: 10.1128/IAI.00796-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cascales E, Christie PJ. 2004. Definition of a bacterial type IV secretion pathway for a DNA substrate. Science 304:1170–1173. doi: 10.1126/science.1095211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Christie PJ, Gomez Valero L, Buchrieser C. 2017. Biological diversity and evolution of type IV secretion systems. Curr Top Microbiol Immunol 413:1–30. doi: 10.1007/978-3-319-75241-9_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Redzej A, Ukleja M, Connery S, Trokter M, Felisberto-Rodrigues C, Cryar A, Thalassinos K, Hayward RD, Orlova EV, Waksman G. 2017. Structure of a VirD4 coupling protein bound to a VirB type IV secretion machinery. EMBO J 36:3080–3095. doi: 10.15252/embj.201796629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Waksman G. 2019. From conjugation to T4S systems in Gram-negative bacteria: a mechanistic biology perspective. EMBO Rep 20:e47012. doi: 10.15252/embr.201847012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Grohmann E, Christie PJ, Waksman G, Backert S. 2018. Type IV secretion in Gram-negative and Gram-positive bacteria. Mol Microbiol 107:455–471. doi: 10.1111/mmi.13896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shaffer CL, Gaddy JA, Loh JT, Johnson EM, Hill S, Hennig EE, McClain MS, McDonald WH, Cover TL. 2011. Helicobacter pylori exploits a unique repertoire of type IV secretion system components for pilus assembly at the bacteria-host cell interface. PLoS Pathog 7:e1002237. doi: 10.1371/journal.ppat.1002237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnson EM, Gaddy JA, Voss BJ, Hennig EE, Cover TL. 2014. Genes required for assembly of pili associated with the Helicobacter pylori cag type IV secretion system. Infect Immun 82:3457–3470. doi: 10.1128/IAI.01640-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ohi M, Li Y, Cheng Y, Walz T. 2004. Negative staining and image classification – powerful tools in modern electron microscopy. Biol Proced Online 6:23–34. doi: 10.1251/bpo70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Busler VJ, Torres VJ, McClain MS, Tirado O, Friedman DB, Cover TL. 2006. Protein-protein interactions among Helicobacter pylori cag proteins. J Bacteriol 188:4787–4800. doi: 10.1128/JB.00066-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Loh JT, Torres VJ, Cover TL. 2007. Regulation of Helicobacter pylori cagA expression in response to salt. Cancer Res 67:4709–4715. doi: 10.1158/0008-5472.CAN-06-4746. [DOI] [PubMed] [Google Scholar]
- 57.Stein M, Rappuoli R, Covacci A. 2000. Tyrosine phosphorylation of the Helicobacter pylori CagA antigen after cag-driven host cell translocation. Proc Natl Acad Sci U S A 97:1263–1268. doi: 10.1073/pnas.97.3.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Odenbreit S, Püls J, Sedlmaier B, Gerland E, Fischer W, Haas R. 2000. Translocation of Helicobacter pylori CagA into gastric epithelial cells by type IV secretion. Science 287:1497–1500. doi: 10.1126/science.287.5457.1497. [DOI] [PubMed] [Google Scholar]
- 59.Backert S, Ziska E, Brinkmann V, Zimny-Arndt U, Fauconnier A, Jungblut PR, Naumann M, Meyer TF. 2000. Translocation of the Helicobacter pylori CagA protein in gastric epithelial cells by a type IV secretion apparatus. Cell Microbiol 2:155–164. doi: 10.1046/j.1462-5822.2000.00043.x. [DOI] [PubMed] [Google Scholar]
- 60.Barrozo RM, Cooke CL, Hansen LM, Lam AM, Gaddy JA, Johnson EM, Cariaga TA, Suarez G, Peek RM Jr, Cover TL, Solnick JV. 2013. Functional plasticity in the type IV secretion system of Helicobacter pylori. PLoS Pathog 9:e1003189. doi: 10.1371/journal.ppat.1003189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Censini S, Lange C, Xiang Z, Crabtree JE, Ghiara P, Borodovsky M, Rappuoli R, Covacci A. 1996. cag, a pathogenicity island of Helicobacter pylori, encodes type I-specific and disease-associated virulence factors. Proc Natl Acad Sci U S A 93:14648–14653. doi: 10.1073/pnas.93.25.14648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ghosal D, Jeong KC, Chang Y-W, Gyore J, Teng L, Gardner A, Vogel JP, Jensen GJ. 2019. Molecular architecture, polar targeting and biogenesis of the Legionella Dot/Icm T4SS. Nat Microbiol 4:1173–1182. doi: 10.1038/s41564-019-0427-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu T, Zhang L, Joo D, Sun S-C. 2017. NF-κB signaling in inflammation. Signal Transduct Target Ther 2:17023. doi: 10.1038/sigtrans.2017.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang Q, Lenardo MJ, Baltimore D. 2017. 30 Years of NF-κB: a blossoming of relevance to human pathobiology. Cell 168:37–57. doi: 10.1016/j.cell.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Keates S, Hitti YS, Upton M, Kelly CP. 1997. Helicobacter pylori infection activates NF-kappa B in gastric epithelial cells. Gastroenterology 113:1099–1109. doi: 10.1053/gast.1997.v113.pm9322504. [DOI] [PubMed] [Google Scholar]
- 66.Yeo H-J, Savvides SN, Herr AB, Lanka E, Waksman G. 2000. Crystal structure of the hexameric traffic ATPase of the Helicobacter pylori type IV secretion system. Mol Cell 6:1461–1472. doi: 10.1016/s1097-2765(00)00142-8. [DOI] [PubMed] [Google Scholar]
- 67.Shariq M, Kumar N, Kumari R, Kumar A, Subbarao N, Mukhopadhyay G. 2015. Biochemical analysis of CagE: a VirB4 homologue of Helicobacter pylori Cag-T4SS. PLoS One 10:e0142606. doi: 10.1371/journal.pone.0142606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Loh JT, Lin AS, Beckett AC, McClain MS, Cover TL. 2018. Role of a stem-loop structure in Helicobacter pylori cagA transcript stability. Infect Immun 87:e00692-18. doi: 10.1128/IAI.00692-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Styer CM, Hansen LM, Cooke CL, Gundersen AM, Choi SS, Berg DE, Benghezal M, Marshall BJ, Peek RM, Borén T, Solnick JV. 2010. Expression of the BabA adhesin during experimental infection with Helicobacter pylori. Infect Immun 78:1593–1600. doi: 10.1128/IAI.01297-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.