Abstract
Interethnic variability in drug response arises from genetic differences associated with drug metabolism, action and transport. These genetic variations can affect drug efficacy as well as cause adverse drug reactions (ADRs). We retrieved drug-response related single nucleotide polymorphism (SNP) associated data from databases and analyzed to elucidate population specific distribution of 159 drug-response related SNPs in twenty six populations belonging to five super-populations (African, Admixed Americans, East Asian, European and South Asian). Significant interpopulation differences exist in the minor (variant) allele frequencies (MAFs), linkage disequilibrium (LD) and haplotype distributions among these populations. 65 of the drug-response related alleles, which are considered as minor (variant) in global population, are present as the major alleles (frequency ≥0.5) in at least one or more populations. Populations that belong to the same super-population have similar distribution pattern for majority of the variant alleles. These drug response related variant allele frequencies and their pairwise LD measure (r2) can clearly distinguish the populations in a way that correspond to the known evolutionary history of human and current geographic distributions, while D' cannot. The data presented here may aid in identifying drugs that are more appropriate and/or require pharmacogenetic testing in these populations. Our findings emphasize on the importance of distinct, ethnicity-specific clinical guidelines, especially for the African populations, to avoid ADRs and ensure effective drug treatment.
Introduction
Pharmacogenomics studies interindividual variability in drug response, which is mainly caused by particular genetic variants associated with drug absorption, distribution, metabolism and elimination (ADME) [1, 2]. Differences in drug response can also be caused by variants in leukocyte antigen genes and drug targets [3]. These variants can modulate efficacy of drugs as well as result in ADRs, which are major causes of hospitalizations and mortalities in both adults and children [4–7]. Such adverse reactions not only exacerbate the patients’ illness, but also cause economic losses [8]. However, ADRs may be avoided in many cases if the genotypes of the patients at the drug-response related loci are known. For example, genotype-guided warfarin dosing was shown to significantly reduce warfarin-related internal bleeding and thromboembolism [9].
Except for a small fraction of the total genetic variants, the majority (genetic variants with minor allele frequencies > 0.05) are commonly shared across populations [10]. But this tiny fraction of the total genetic variants distinguish between metabolic phenotypes of the continental populations [11]. Besides, there is evidence of interethnic and intraethnic differences in the distribution of drug-response associated genetic variants and, as a consequence, variability in drug responses [12–14]. For example, rosuvastatin is commonly prescribed to prevent cardiovascular complications and treat abnormal lipid levels in the blood. Although its high efficacy and safety profile as a drug to tackle dyslipidemia are well-known, multiple studies have reported dose-dependent adverse effects of prolonged statin therapy [15–17]. Ethnic differences exist in the pharmacokinetics of rosuvastatin. The average systemic exposure to this drug among the individuals of Chinese ethnicity is 2.3-fold greater than the Caucasians, whereas Malays and Asian Indians have intermediate values [18].
Due to interpopulation genetic variations, drugs as well as markers used for pharmacogenotyping in one population may not be appropriate for another population. For example, HLA-b*58:01 allele is associated with allopurinol-induced severe cutaneous adverse reactions and rs9263726 can be used as a surrogate biomarker for the Japanese, but not the Australian and the Han Chinese populations [19, 20]. Population-based differences in the outcomes of anticancer treatments have also been reported. For example, discrepant responses to 5-Fluorouracil (5-FU) among different ethnicities of the South Asian population were attributed to genetic variations in the DPYD gene [21]. Analysis of population specific genetic structure, therefore, has many applications in medical and population genetic research as well as ensuring drug efficacy and development of pharmacogenetic tests [8, 22, 23].
Many aspects of the population history are reflected in genetic information [23]. SNPs and their allelic distribution provide important information about population structure, evolution and migration [24–29]. There are population-specific differences in the extent and pattern of linkage disequilibrium (LD) among genetic variants [11]. Levels and patterns of LD depend on a number of demographic factors such as population size and structure, population growth, admixture, migration and locus-specific factors such as mutation, selection, recombination, gene conversion and genetic drift [30, 31]. The application and transferability of surrogate biomarkers and/or tagSNPs from a particular genome wide association study (GWAS) depends on the genetic relatedness between the studied populations [32–35]. Hence, it is important to know population-specific LD patterns among different genetic variants before widely implementing results of GWAS.
Since allelic distribution and linkage disequilibrium (LD) of SNPs vary among populations, frequencies of different SNP alleles associated with drug response and patterns of LD should be analyzed separately for different populations. Here, we present the variant allele distribution, pairwise LD and haplotypes frequencies of 159 drug-response associated SNPs in five super-populations (African, Admixed Americans, East Asian, European and South Asian) and twenty six individual populations belonging to these super-populations.
Materials and methods
List of SNPs associated with drug response
The dbSNP database (https://www.ncbi.nlm.nih.gov/snp) at the National Center for Biotechnology Information (NCBI) was searched using the keyword ‘drug-response’. After filtering out the duplicates and insertion/deletion (indel) polymorphisms, 159 SNPs were selected for further analysis. Drugs related to these SNPs along with their applications were searched in ClinVar archive at NCBI (https://www.ncbi.nlm.nih.gov/clinvar) [36] and the PharmGKB (https://www.pharmgkb.org/) [37].
Allele frequency and pairwise LD calculation
We used the LDhap module at LDlink (https://ldlink.nci.nih.gov/) [38] to retrieve the population-specific allele and haplotype frequencies from the phase 3 (version 5) sequence data of the 1000 Genomes Project [39] for five super-populations (African, Admixed Americans, East Asian, European and South Asian) and twenty six individual populations belonging to these super-populations (Listed in Table 1). LDlink is a suite of web-based bioinformatics modules that provides an easy and user-friendly interface to investigate SNPs, LD and haplotypes in populations included in the 1000 Genomes Project [38]. The Reference SNP (rs) numbers of the SNPs were used as inputs. We used the LDmatrix module at LDlink to calculate the pairwise LD among the SNPs in different super- and sub-populations. SNPs that are located on the same chromosome were inputted together. SNP pairs that maintain a strong LD (r2≥ 0.8) were selected and compiled in a non-redundant list.
Table 1. List of drug-response related SNPs with MAF ≥0.5.
| SNP ID | Global major allele | Global minor allele | Associated drug | Drug used for | Population# | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALL | AFR | AMR | EAS | EUR | SAS | |||||||||||||||||||||||||||||||
| All pops |
AFR | YRI | LWK | GWD | MSL | ESN | ASW | ACB | AMR | MXL | PUR | CLM | PEL | EAS | CHB | JPT | CHS | CDX | KHV | EUR | CEU | TSI | FIN | GBR | IBS | SAS | GIH | PJL | BEB | STU | ITU | |||||
| rs1801133 | G | A | Cyclophosphamide, carboplatin, methotrexate | Precursor cell lymphoblastic leukemia-lymphoma, carcinoma, non-small-cell lung cancer, neoplasms | 0.25 | 0.54 | ||||||||||||||||||||||||||||||
| rs2297480 | T | G | Bisphosphonates | Postmenopausal osteoporosis | 0.37 | 0.69 | 0.76 | 0.74 | 0.75 | 0.66 | 0.54 | |||||||||||||||||||||||||
| rs1801274 | A | G | Trastuzumab | Breast neoplasms | 0.44 | 0.53 | 0.52 | 0.61 | 0.60 | 0.51 | 0.51 | 0.54 | 0.61 | 0.53 | ||||||||||||||||||||||
| rs1051740 | T | C | Carbamazepine | Epilepsy | 0.31 | 0.54 | ||||||||||||||||||||||||||||||
| rs1056836 | G | C | - | Congenital glaucoma | 0.39 | 0.82 | 0.88 | 0.79 | 0.82 | 0.87 | 0.84 | 0.70 | 0.79 | |||||||||||||||||||||||
| rs6166 | T | C | Follice-stimulating hormone | Ovarian hyperstimulation syndrome, ovarian response to FSH stimulation, ovarian dysgenesis | 0.41 | 0.50 | 0.51 | |||||||||||||||||||||||||||||
| rs6165 | C | T | Follice-stimulating hormone | Ovarian hyper-stimulation syndrome, ovarian response to FSH stimulation, ovarian dysgenesis | 0.49 | 0.58 | 0.67 | 0.56 | 0.66 | 0.66 | 0.67 | 0.64 | 0.67 | 0.67 | 0.65 | 0.55 | 0.59 | 0.53 | 0.50 | 0.56 | 0.57 | 0.54 | 0.52 | 0.63 | 0.55 | 0.54 | ||||||||||
| rs3812718 | C | T | Carbamazepine, phenytoin, anti-epileptics | Epilepsy | 0.49 | 0.56 | 0.60 | 0.51 | 0.62 | 0.68 | 0.70 | 0.54 | 0.53 | 0.53 | 0.57 | 0.61 | 0.58 | 0.58 | 0.58 | 0.60 | 0.59 | 0.55 | ||||||||||||||
| rs2952768 | T | C | Fentanyl, morphine, opioids | Pain | 0.39 | 0.54 | 0.51 | 0.51 | 0.52 | 0.57 | ||||||||||||||||||||||||||
| rs4673993 | T | C | Methotrexate | Rheumatoid arthritis | 0.29 | 0.56 | ||||||||||||||||||||||||||||||
| rs887829 | C | T | Atazanavir | Human immunodeficiency virus infection | 0.35 | 0.52 | 0.53 | |||||||||||||||||||||||||||||
| rs4961 | G | T | Furosemide, spironolactone | Liver cirrhosis | 0.21 | 0.54 | 0.56 | |||||||||||||||||||||||||||||
| rs145489027 | G | A | ACE inhibitor | 0.30 | 0.55 | 0.51 | ||||||||||||||||||||||||||||||
| rs1902023 | C | A | Oxazepam, lorazepam | Anxiety | 0.45 | 0.51 | 0.55 | 0.51 | 0.52 | 0.54 | 0.54 | 0.55 | 0.64 | 0.55 | ||||||||||||||||||||||
| rs4693075 | C | G | Atorvastatin, HMG CoA reductase inhibitors, rosuvastatin | Muscular diseases | 0.34 | 0.53 | 0.54 | |||||||||||||||||||||||||||||
| rs4444903 | G | A | Cetuximab | Colorectal neoplasms, rectal neoplasms | 0.40 | 0.61 | 0.60 | 0.62 | 0.63 | 0.59 | 0.61 | 0.51 | 0.52 | |||||||||||||||||||||||
| rs1801394 | A | G | Methotrexate | Burkitt lymphoma, T-cell precursor cell lymphoblastic leukemia-lymphoma, lymphoma, toxic liver disease, gastrointestinal stroma tumor, disorders of intracellular cobalamin metabolism | 0.36 | 0.52 | 0.56 | 0.62 | 0.57 | 0.52 | 0.51 | 0.54 | 0.51 | 0.59 | ||||||||||||||||||||||
| rs6295 | G | C | Paroxetine | Depressive disorder, panic disorder 1, major mood disorders | 0.45 | 0.57 | 0.59 | 0.61 | 0.56 | 0.55 | 0.54 | 0.57 | 0.57 | 0.58 | 0.52 | 0.54 | 0.51 | 0.59 | 0.61 | 0.53 | ||||||||||||||||
| rs17244841 | A | T | HMG CoA reductase inhibitors, pravastatin, simvastatin | Coronary artery disease, hyperlipidemias, coronary disease, myocardial infarction, hypercholesterolemia | 0.04 | |||||||||||||||||||||||||||||||
| rs1042713 | G | A | Salbutamol, salmeterol | Asthma | 0.48 | 0.52 | 0.53 | 0.53 | 0.52 | 0.52 | 0.55 | 0.51 | 0.52 | 0.55 | 0.55 | 0.61 | 0.58 | 0.57 | ||||||||||||||||||
| rs20455 | G | A | Pravastatin, atorvastatin | Coronary disease, myocardial infarction, hyperlipidemias | 0.46 | 0.67 | 0.68 | 0.59 | 0.62 | 0.79 | 0.52 | 0.51 | 0.64 | 0.63 | 0.65 | 0.66 | 0.66 | 0.59 | 0.54 | 0.54 | 0.55 | 0.56 | 0.52 | 0.52 | ||||||||||||
| rs1799971 | A | G | Ethanol, alfentanil, fentanyl, heroin, morphine, naltrexone, opioids, tramadol, buprenorphine, drugs used in opioid dependence | Alcohol dependence, heroin dependence, opioid-related disorders, pain | 0.22 | |||||||||||||||||||||||||||||||
| rs4880 | A | G | Cyclophosphamide | Breast neoplasms | 0.41 | 0.58 | 0.65 | 0.54 | 0.68 | 0.52 | 0.51 | 0.51 | 0.58 | |||||||||||||||||||||||
| rs37973 | A | G | Glucocorticoids | 0.40 | 0.51 | 0.51 | 0.52 | 0.51 | 0.53 | 0.59 | 0.52 | |||||||||||||||||||||||||
| rs7793837 | A | T | Salbutamol, selective beta-2-adrenoreceptor agonists | Drug reported used for: Asthma, Drug reported used for: Asthma | 0.42 | 0.86 | 0.91 | 0.84 | 0.87 | 0.86 | 0.91 | 0.76 | 0.81 | |||||||||||||||||||||||
| rs1045642 | G | A | Nevirapine, methotrexate, fentanyl, methadone, morphine, opioids, oxycodone, tramadol, digoxin | HIV Infections, toxic epidermal necrolysis, Burkitt lymphoma, precursor cell lymphoblastic leukemia-lymphoma, lymphoma, toxic liver disease, pain, heroin dependence | 0.40 | 0.52 | 0.57 | 0.58 | 0.53 | 0.58 | 0.57 | 0.51 | 0.61 | 0.59 | 0.59 | |||||||||||||||||||||
| rs776746 | C | T | Cyclosporine, tacrolimus, sirolimus | Organ transplantation, kidney transplantation, liver transplantation | 0.38 | 0.82 | 0.83 | 0.88 | 0.77 | 0.88 | 0.89 | 0.69 | 0.75 | |||||||||||||||||||||||
| rs2740574 | T | C | Condition: tacrolimus response—Dosage | Drug reported used for: Organ Transplantation | 0.23 | 0.77 | 0.76 | 0.83 | 0.79 | 0.84 | 0.77 | 0.67 | 0.66 | |||||||||||||||||||||||
| rs10246939 | C | T | Phenylthio-carbamide tasting | 0.48 | 0.52 | 0.54 | 0.51 | 0.58 | 0.51 | 0.53 | 0.54 | 0.54 | 0.57 | 0.62 | 0.58 | 0.50 | 0.64 | 0.58 | 0.59 | 0.67 | 0.70 | 0.66 | ||||||||||||||
| rs1726866 | G | A | Phenylthio-carbamide tasting | 0.43 | 0.54 | 0.57 | 0.62 | 0.58 | 0.64 | 0.58 | 0.59 | 0.67 | 0.70 | 0.66 | ||||||||||||||||||||||
| rs713598 | G | C | Phenylthio-carbamide tasting | 0.50 | 0.53 | 0.54 | 0.50 | 0.58 | 0.51 | 0.52 | 0.54 | 0.58 | 0.62 | 0.63 | 0.61 | 0.55 | 0.66 | 0.60 | 0.62 | 0.68 | 0.70 | 0.68 | ||||||||||||||
| rs6977820 | C | T | Antipsychotics | Metabolic syndrome X, schizophrenia, hyper-prolactinemia, tardive dyskinesia, weight gain, mental disorders | 0.42 | 0.83 | 0.88 | 0.83 | 0.84 | 0.85 | 0.90 | 0.68 | 0.74 | |||||||||||||||||||||||
| rs1041983 | C | T | Slow acetylator due to N-acetyl transferase enzyme variant, ethambutol, isoniazid, pyrazinamide, rifampin | Tuberculosis | 0.40 | 0.50 | 0.53 | 0.54 | 0.50 | |||||||||||||||||||||||||||
| rs6988229 | C | T | Salbutamol | Asthma | 0.24 | 0.60 | 0.62 | 0.57 | 0.62 | 0.59 | 0.59 | 0.57 | 0.60 | |||||||||||||||||||||||
| rs1695 | A | G | Platinum compounds, fluorouracil, oxaliplatin, cyclophosphamide, epirubicin, cisplatin | Neoplasms, ovarian neoplasms, colorectal neoplasms, breast neoplasms, osteosarcoma, urinary bladder neoplasms, medulloblastoma, brain neoplasms | 0.35 | 0.51 | 0.54 | 0.54 | 0.56 | 0.67 | ||||||||||||||||||||||||||
| rs716274 | A | G | Platinum compounds | Neoplasms, ovarian neoplasms | 0.44 | 0.50 | 0.54 | 0.51 | 0.59 | 0.58 | 0.63 | 0.59 | 0.57 | 0.60 | 0.51 | 0.50 | ||||||||||||||||||||
| rs11212617 | C | A | Metformin | Diabetes mellitus | 0.47 | 0.64 | 0.59 | 0.61 | 0.66 | 0.69 | 0.62 | 0.55 | 0.69 | 0.58 | 0.59 | 0.66 | 0.63 | 0.64 | 0.70 | 0.61 | 0.56 | 0.62 | ||||||||||||||
| rs1954787 | C | T | Antidepressants | Depression, depressive disorder, major depressive disorder, mood disorders | 0.50 | 0.90 | 0.93 | 0.86 | 0.95 | 0.94 | 0.90 | 0.83 | 0.83 | 0.52 | ||||||||||||||||||||||
| rs5443 | C | T | Sildenafil | Erectile dysfunction | 0.49 | 0.82 | 0.85 | 0.75 | 0.82 | 0.89 | 0.81 | 0.78 | 0.83 | 0.50 | 0.50 | 0.58 | 0.55 | |||||||||||||||||||
| rs11045879 | T | C | Methotrexate | Burkitt lymphoma, precursor cell lymphoblastic leukemia-lymphoma, toxic liver disease | 0.22 | 0.54 | ||||||||||||||||||||||||||||||
| rs7997012 | G | A | Antidepressants, citalopram, selective serotonin reuptake inhibitors | Depression, depressive disorder, major depressive disorder | 0.27 | 0.53 | 0.52 | |||||||||||||||||||||||||||||
| rs1719247 | T | C | HMG CoA reductase inhibitors, simvastatin | Muscular diseases, myopathy | 0.41 | 0.60 | 0.53 | 0.73 | 0.80 | 0.71 | 0.67 | 0.74 | 0.73 | 0.55 | 0.57 | 0.61 | 0.51 | 0.51 | 0.57 | |||||||||||||||||
| rs1346268 | T | C | HMG CoA reductase inhibitors, simvastatin | Muscular diseases, myopathy | 0.45 | 0.52 | 0.61 | 0.79 | 0.81 | 0.85 | 0.88 | 0.82 | 0.80 | 0.68 | ||||||||||||||||||||||
| rs578776 | A | G | Nicotine | Tobacco use disorder | 0.45 | 0.53 | 0.72 | 0.75 | 0.69 | 0.70 | 0.71 | 0.74 | 0.51 | 0.52 | 0.53 | 0.57 | 0.53 | |||||||||||||||||||
| rs7294 | C | T | Warfarin, acenocoumarol, phenprocoumon, vitamin K-dependent clotting factors | Heart diseases, atrial fibrillation, arteriosclerosis, hemorrhage, intracranial hemorrhages, myocardial infarction, peripheral vascular diseases, thromboembolism, venous thromboembolism, pulmonary embolism, stroke | 0.42 | 0.51 | 0.57 | 0.76 | 0.67 | 0.69 | 0.79 | 0.82 | 0.83 | |||||||||||||||||||||||
| rs2359612 | G | A | Warfarin | Heart diseases, atrial fibrillation, arteriosclerosis, hemorrhage, intracranial hemorrhages, myocardial infarction, peripheral vascular diseases, thromboembolism, venous thromboembolism, pulmonary embolism, stroke | 0.39 | 0.89 | 0.96 | 0.90 | 0.89 | 0.82 | 0.84 | |||||||||||||||||||||||||
| rs8050894 | C | G | Warfarin | Heart diseases, atrial fibrillation, arteriosclerosis, hemorrhage, intracranial hemorrhages, myocardial infarction, peripheral vascular diseases, thromboembolism, venous thromboembolism, pulmonary embolism, stroke | 0.42 | 0.51 | 0.89 | 0.96 | 0.90 | 0.89 | 0.82 | 0.84 | 0.50 | |||||||||||||||||||||||
| rs9934438 | G | A | Warfarin, acenocoumarol, phenprocoumon, vitamin K-dependent clotting factors | Heart diseases, atrial fibrillation, arteriosclerosis, hemorrhage, intracranial hemorrhages, myocardial infarction, peripheral vascular diseases, thromboembolism, venous thromboembolism, pulmonary embolism, stroke | 0.36 | 0.89 | 0.96 | 0.90 | 0.89 | 0.82 | 0.84 | |||||||||||||||||||||||||
| rs9923231 | C | T | Warfarin, acenocoumarol, phenprocoumon | Heart diseases, atrial fibrillation, arteriosclerosis, hemorrhage, intracranial hemorrhages, myocardial infarction, peripheral vascular diseases, thromboembolism, venous thromboembolism, pulmonary embolism, stroke | 0.36 | 0.89 | 0.96 | 0.90 | 0.89 | 0.82 | 0.84 | |||||||||||||||||||||||||
| rs7196161 | A | G | Warfarin | Heart diseases, atrial fibrillation, arteriosclerosis, hemorrhage, intracranial hemorrhages, myocardial infarction, peripheral vascular diseases, thromboembolism, venous thromboembolism, pulmonary embolism, stroke | 0.47 | 0.61 | 0.51 | 0.89 | 0.96 | 0.90 | 0.89 | 0.82 | 0.84 | |||||||||||||||||||||||
| rs1532624 | C | A | HMG CoA reductase inhibitors | Coronary artery disease, hyperlipidemias | 0.31 | 0.54 | 0.52 | |||||||||||||||||||||||||||||
| rs2232228 | A | G | Anthracyclines and related substances | Heart failure, cardiomyopathies, neoplasms | 0.34 | 0.50 | 0.52 | 0.54 | 0.50 | 0.57 | 0.51 | |||||||||||||||||||||||||
| rs1042522 | C | G | Antineoplastic agents, cisplatin, cyclophosphamide, fluorouracil, paclitaxel | Breast neoplasms, neoplasms, neutropenia, ovarian neoplasms, stomach neoplasms, non-small-cell lung carcinoma, colorectal neoplasms, esophageal neoplasms, mesothelioma, pancreatic neoplasms, uterine cervical neoplasms | 0.46 | 0.67 | 0.64 | 0.75 | 0.71 | 0.61 | 0.68 | 0.60 | 0.66 | 0.52 | 0.54 | 0.54 | ||||||||||||||||||||
| rs4149601 | G | A | Diuretics, hydrochlorothiazide | Hypertension, essential hypertension | 0.28 | 0.50 | ||||||||||||||||||||||||||||||
| rs17782313 | T | C | Antipsychotics | Metabolic syndrome X, schizophrenia, hyper-prolactinemia, tardive dyskinesia, weight gain, mental Disorders | 0.24 | |||||||||||||||||||||||||||||||
| rs489693 | C | A | Amisulpride, aripiprazole, clozapine, haloperidol, olanzapine, paliperidone, quetiapine, risperidone, ziprasidone | Autism spectrum disorder, schizoaffective disorder, schizophrenia. Metabolic syndrome X, hyper-prolactinemia, tardive dyskinesia, weight gain | 0.35 | 0.50 | 0.53 | 0.53 | 0.58 | 0.50 | ||||||||||||||||||||||||||
| rs12979860 | C | T | Peginterferon alfa-2a, peginterferon alfa-2b, and ribavirin, telaprevir, boceprevir | Hepatitis C, HIV infection, chronic Hepatitis C infection | 0.36 | 0.67 | 0.68 | 0.52 | 0.73 | 0.65 | 0.71 | 0.68 | 0.71 | |||||||||||||||||||||||
| rs3212986 | C | A | Cisplatin, platinum, platinum compounds | Neoplasms, osteosarcoma, urinary bladder neoplasms, ovarian neoplasms, medulloblastoma, brain neoplasms | 0.30 | 0.50 | ||||||||||||||||||||||||||||||
| rs11615 | G | A | Carboplatin, cisplatin, oxaliplatin, platinum compounds | Non-small-cell lung carcinoma, colorectal neoplasms, esophageal neoplasms, mesothelioma, ovarian neoplasms, pancreatic neoplasms, breast neoplasms, stomach neoplasms, cervical neoplasms | 0.33 | 0.62 | 0.64 | 0.54 | 0.63 | 0.68 | 0.63 | 0.52 | 0.51 | |||||||||||||||||||||||
| rs1056892 | G | A | Anthracyclines and related substances | Heart failure, cardiomyopathies, neoplasms | 0.43 | 0.51 | 0.51 | 0.53 | 0.52 | 0.57 | 0.53 | 0.53 | 0.54 | 0.59 | 0.53 | 0.52 | ||||||||||||||||||||
| rs4680 | G | A | Nicotine | Tobacco use disorder | 0.37 | 0.50 | 0.59 | 0.53 | 0.52 | |||||||||||||||||||||||||||
| rs2298383 | C | T | Caffeine | 0.40 | 0.52 | 0.65 | 0.50 | 0.51 | 0.52 | 0.56 | 0.59 | 0.59 | 0.58 | 0.57 | 0.63 | 0.57 | ||||||||||||||||||||
| rs1135840 | G | C | Debrisoquine | Ultra-rapid metabolism of debrisoquine | 0.40 | 0.52 | 0.60 | 0.51 | 0.61 | 0.50 | 0.53 | 0.57 | 0.50 | |||||||||||||||||||||||
| rs16947 | G | A | Debrisoquine | Ultra-rapid metabolism of debrisoquine | 0.36 | 0.55 | 0.56 | 0.65 | 0.54 | 0.61 | 0.57 | |||||||||||||||||||||||||
| rs1065852 | G | A | Debrisoquine | Ultra-rapid metabolism of debrisoquine | 0.24 | 0.57 | 0.60 | 0.61 | 0.63 | 0.66 | ||||||||||||||||||||||||||
# All populations (ALL); African super-population (AFR)- ((Yoruba in Ibadan, Nigeria (YRI); Luhya in Webuye, Kenya (LWK); Gambian in Western Divisions in the Gambia (GWD); Mende in Sierra Leone (MSL); Esan in Nigeria (ESN); Americans of African Ancestry in SW USA (ASW); African Caribbeans in Barbados (ACB)); Ad Mixed Americans (AMR)- ((Mexican Ancestry from Los Angeles USA (MXL); Puerto Ricans from Puerto Rico (PUR); Colombians from Medellin, Colombia (CLM); Peruvians from Lima, Peru (PEL)); East Asian (EAS)- ((Han Chinese in Beijing, China (CHB); Japanese in Tokyo, Japan (JPT); Southern Han Chinese (CHS); Chinese Dai in Xishuangbanna, China (CDX); Kinh in Ho Chi Minh City, Vietnam (KHV)); European (EUR)- ((Utah Residents (CEPH) with Northern and Western European Ancestry (CEU); Toscani in Italia (TSI); Finnish in Finland (FIN); British in England and Scotland (GBR); Iberian Population in Spain (IBS)); South Asian (SAS)- ((Gujarati Indian from Houston, Texas (GIH); Punjabi from Lahore, Pakistan (PJL); Bengali from Bangladesh (BEB); Sri Lankan Tamil from the UK (STU); Indian Telugu from the UK (ITU))
Statistical analyses
The statistical tools available at Metaboanalyst (https://www.metaboanalyst.ca/MetaboAnalyst/ModuleView.xhtml) [40] were used for multivariate principle component analysis (PCA), partial least square- discriminant analysis (PLS-DA) and hierarchical clustering based on the MAFs (defined based on frequencies in global population) of 159 drug-response related SNPs as well as pairwise LD measures (r2 and D'). Euclidean distance based Ward’s algorithm was applied in hierarchical clustering to generate population dendrogram. All graphs were generated using the GraphPad Prism® (Version 6) software.
Results
Distribution of drug-response related SNPs across populations
We compiled the allele frequencies of 159 drug-response related SNP loci in a total of 32 populations (one global, five super populations and twenty six individual populations) (S1 Table). Defining an allele as minor (frequency <0.5) based on its global distribution may not be always appropriate since globally defined minor alleles may be present as the more prevalent ones in certain populations [41]. 65 of these drug-response related alleles that are considered as minor (variant) in global population are present as the major alleles (frequency ≥0.5) in at least one population (Table 1). In fact, 14 of these drug-response related SNPs have MAFs ≥ 0.8 in at least one of the individual populations. 7 of these SNPs (rs1056836, rs7793837, rs776746, rs2740574, rs6977820, rs1954787 and rs5443) have MAFs ≥ 0.8 only in multiple African sub-populations and 6 (rs2359612, rs8050894, rs9934438, rs9923231, rs7196161 and rs1346268) have MAFs ≥ 0.8 only in several East Asian sub-populations. rs7294 has MAF ≥ 0.8 in only two South Asian populations (STU and ITU). MAFs at majority of the loci show similar distribution patterns among the individual sub-populations within each super-population (Table 1 and S1 Table). The drug-response related allele frequency distribution is different among super-populations indicating demographic effects (Fig 1).
Fig 1. Drug-response related minor (variant) allele frequency distribution in global and five super populations.
AFR = African, AMR = Admixed Americans, EAS = East Asian, EUR = European, SAS = South Asian.
SNPs can be arbitrarily divided into many classes based on their allele frequencies [42, 43]. In this study, we considered frequencies ≥ 0.2 to be comparatively high for the minor (variant) allele at any locus in any population. We observed 111 SNPs which have MAFs ≥ 0.2 in at least one of the super-populations (S1 Table). 31 of these 111 SNPs have MAFs ≥ 0.2 in all super-populations. MAFs at 13 SNP loci are ≥ 0.2 in all twenty-six individual sub-populations. These 13 SNPs are rs2297480, rs6166, rs3812718, rs2952768, rs2228001, rs1902023, rs1042713, rs1042522, rs3212986, rs4680, rs1135840, rs1041983 and rs5443. 18 SNPs have MAFs ≥ 0.2 in only one of the super-populations. These SNPs are rs7582141, rs6432512, rs264588, rs264631, rs2231142, rs7779029, rs2740574, rs6988229, rs885004, rs4917639, rs11045879, rs7297610, rs17708472, rs2884737, rs6065, rs1876828, rs16960228 and rs8099917. 28 SNPs are totally absent (MAF = 0) in all sub-populations belonging to at least any one of the super-populations. 72 SNPs have very low (≤ 0.05) MAFs in at least one of the super-populations. 23 of the drug-response related SNPs have MAF = 0 in majority (>13) of the 26 populations (S1 Table).
Private alleles, which are only present in a particular population among a broader collection of populations, are very useful in population genetics and human evolutionary genetics [44]. We found minor alleles of rs186335453 (T allele) and rs139801276 (C allele) to be private in LWK and all African sub-populations (except ACB), respectively. Minor alleles of rs111033610 (G allele) and rs5030865 (T allele) are private to the East Asian sub-populations (except JPT and CHS, respectively), and the T (variant) allele of rs56019966 is private to 3 European sub-populations (TSI, GBR and IBS).
LD patterns of the drug-response related SNPs
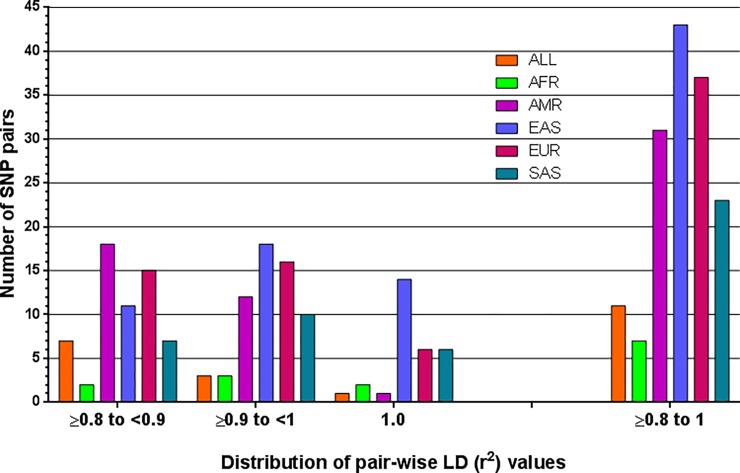
r2 and D' are the two most widely used measures of LD. r2 is more robust and correlates better among different population samples [45]. We found 48 SNP pairs with r2 ≥ 0.8 in at least one of the five super-populations (Table 2). 4 of these pairs have r2 values ≥ 0.8 in all super-populations. Interpopulation variability was observed at the levels of LD between drug-response associated SNP loci (Fig 2). 7 SNP pairs with r2 ≥ 0.8 are found in African, 31 in Admixed American, 43 in East Asian, 37 in European and 23 are in South Asian super-population (Table 2). East Asian super-population has very strong pairwise LD among 32 SNP pairs (r2 ≥ 0.9).
Table 2. List of drug-response related SNP pairs with r2 ≥ 0.8 in at least one of the five super-populations.
| SNP pairs | Chromosome | ALL | AFR | AMR | EAS | EUR | SAS | |
|---|---|---|---|---|---|---|---|---|
| rs264588 | rs7582141 | 2 | 0.816 | 0.929 | 0.979 | 0.857 | 0.953 | 0.239 |
| rs264588 | rs6432512 | 2 | 0.795 | 0.880 | 0.969 | 0.857 | 0.953 | 0.239 |
| rs264588 | rs10497203 | 2 | 0.414 | 0.196 | 0.802 | 0.829 | 0.790 | 0.122 |
| rs264588 | rs264651 | 2 | 0.564 | 0.230 | 0.833 | 0.972 | 0.859 | 0.846 |
| rs264631 | rs7582141 | 2 | 0.718 | 0.686 | 0.928 | 0.870 | 0.953 | 0.237 |
| rs264631 | rs6432512 | 2 | 0.699 | 0.642 | 0.919 | 0.870 | 0.953 | 0.237 |
| rs264631 | rs10497203 | 2 | 0.361 | 0.136 | 0.760 | 0.841 | 0.790 | 0.121 |
| rs264631 | rs264588 | 2 | 0.869 | 0.736 | 0.949 | 0.958 | 1.000 | 0.991 |
| rs264631 | rs264651 | 2 | 0.498 | 0.171 | 0.790 | 0.986 | 0.859 | 0.838 |
| rs264651 | rs10497203 | 2 | 0.684 | 0.714 | 0.965 | 0.854 | 0.873 | 0.144 |
| rs264651 | rs7582141 | 2 | 0.387 | 0.205 | 0.815 | 0.883 | 0.808 | 0.054 |
| rs264651 | rs6432512 | 2 | 0.377 | 0.194 | 0.807 | 0.883 | 0.808 | 0.054 |
| rs6165 | rs6166 | 2 | 0.630 | 0.208 | 0.783 | 0.880 | 0.992 | 0.940 |
| rs6432512 | rs7582141 | 2 | 0.976 | 0.949 | 0.990 | 1.000 | 1.000 | 1.000 |
| rs6432512 | rs10497203 | 2 | 0.510 | 0.204 | 0.816 | 0.972 | 0.829 | 0.477 |
| rs7582141 | rs10497203 | 2 | 0.523 | 0.216 | 0.825 | 0.972 | 0.829 | 0.477 |
| rs1142345 | rs1800460 | 6 | 0.318 | 0.043 | 0.687 | NA | 0.965 | 0.232 |
| rs1360780 | rs4713916 | 6 | 0.455 | 0.080 | 0.717 | 0.689 | 0.699 | 0.800 |
| rs713598 | rs10246939 | 7 | 0.931 | 0.970 | 0.865 | 0.996 | 0.855 | 0.927 |
| rs1726866 | rs10246939 | 7 | 0.799 | 0.446 | 0.878 | 0.996 | 0.992 | 1.000 |
| rs713598 | rs1726866 | 7 | 0.751 | 0.443 | 0.758 | 1.000 | 0.855 | 0.927 |
| rs1208 | rs1801280 | 8 | 0.823 | 0.611 | 0.904 | 0.948 | 0.918 | 0.914 |
| rs1799930 | rs1041983 | 8 | 0.532 | 0.317 | 0.504 | 0.439 | 0.887 | 0.743 |
| rs7853758 | rs885004 | 9 | 0.565 | 0.213 | 0.815 | 0.920 | 0.909 | 0.799 |
| rs4244285 | rs12777823 | 10 | 0.858 | 0.583 | 0.896 | 0.991 | 0.939 | 0.982 |
| rs10509681 | rs1799853 | 10 | 0.850 | 0.825 | 0.937 | 1.000 | 0.823 | 0.732 |
| rs75838422 | rs7900194 | 10 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| rs554405994 | rs116855232 | 13 | 0.217 | 0.000 | 0.800 | 0.233 | 0.000 | 0.000 |
| rs1719247 | rs1346268 | 15 | 0.537 | 0.099 | 0.849 | 0.950 | 0.946 | 0.744 |
| rs9934438 | rs2359612 | 16 | 0.863 | 0.265 | 0.948 | 1.000 | 1.000 | 1.000 |
| rs9923231 | rs2359612 | 16 | 0.862 | 0.265 | 0.943 | 1.000 | 1.000 | 1.000 |
| rs9923231 | rs9934438 | 16 | 0.999 | 1.000 | 0.994 | 1.000 | 1.000 | 1.000 |
| rs8050894 | rs2359612 | 16 | 0.646 | 0.003 | 0.833 | 1.000 | 0.951 | 0.976 |
| rs9934438 | rs8050894 | 16 | 0.774 | 0.167 | 0.884 | 1.000 | 0.951 | 0.976 |
| rs9923231 | rs8050894 | 16 | 0.774 | 0.167 | 0.878 | 1.000 | 0.951 | 0.976 |
| rs7196161 | rs8050894 | 16 | 0.720 | 0.323 | 0.827 | 1.000 | 0.899 | 0.921 |
| rs2359612 | rs7294 | 16 | 0.463 | 0.181 | 0.497 | 0.971 | 0.365 | 0.534 |
| rs8050894 | rs7294 | 16 | 0.511 | 0.279 | 0.525 | 0.971 | 0.379 | 0.547 |
| rs9934438 | rs7294 | 16 | 0.400 | 0.048 | 0.471 | 0.971 | 0.365 | 0.534 |
| rs9923231 | rs7294 | 16 | 0.399 | 0.048 | 0.469 | 0.971 | 0.365 | 0.534 |
| rs7196161 | rs7294 | 16 | 0.572 | 0.494 | 0.506 | 0.971 | 0.368 | 0.536 |
| rs7196161 | rs2359612 | 16 | 0.645 | 0.196 | 0.773 | 1.000 | 0.852 | 0.898 |
| rs7196161 | rs9934438 | 16 | 0.551 | 0.035 | 0.727 | 1.000 | 0.852 | 0.898 |
| rs7196161 | rs9923231 | 16 | 0.550 | 0.035 | 0.722 | 1.000 | 0.852 | 0.898 |
| rs12979860 | rs11881222 | 19 | 0.569 | 0.182 | 0.879 | 0.949 | 0.909 | 0.845 |
| rs8099917 | rs11881222 | 19 | 0.441 | 0.100 | 0.636 | 0.873 | 0.463 | 0.714 |
| rs8099917 | rs12979860 | 19 | 0.264 | 0.022 | 0.566 | 0.920 | 0.428 | 0.637 |
| rs1065852 | rs3892097 | 22 | 0.329 | 0.507 | 0.855 | 0.002 | 0.903 | 0.623 |
Fig 2. Distribution of pairwise LD (r2) values among the drug-response related minor (variant) alleles in global and 5 super populations.
AFR = African, AMR = Admixed Americans, EAS = East Asian, EUR = European, SAS = South Asian.
We found 10 haplotypes (2 in chromosome 8, 9 and 19 each, and 1 in chromosome 6, 7, 10 and 16 each) having ≥ 2 variant alleles as well as with frequencies ≥ 0.2 in at least one of the five super-populations (Table 3). All the alleles in the haplotype (T_A_C) on chromosome 7 are minor alleles at the corresponding loci in the global population. This haplotype is present in all five super-populations.
Table 3. Haplotypes with frequencies ≥ 0.2 as well as having ≥ 2 variant alleles in at least one of the five super-populations.
| Chromosome | SNP ID | Haplotypes*,# | Population | Frequency | Length, bp | Associated Drugs |
|---|---|---|---|---|---|---|
| 6 | rs1142345_ rs1800460_ rs1360780_ rs4713916 | T_C_T_A | AMR | 0.232 | 17571519 | Antidepressants, citalopram, fluoxetine, mirtazapine, paroxetine, selective serotonin reuptake inhibitors, venlafaxine |
| 6 | rs1142345_ rs1800460_ rs1360780_ rs4713916 | T_C_T_A | EUR | 0.268 | ||
| 6 | rs1142345_ rs1800460_ rs1360780_ rs4713916 | T_C_T_A | SAS | 0.308 | ||
| 7 | rs10246939_rs1726866_rs713598 | T_A_C | AFR | 0.330 | 741 | Phenylthiocarbamide tasting |
| 7 | rs10246939_rs1726866_rs713598 | T_A_C | AMR | 0.284 | ||
| 7 | rs10246939_rs1726866_rs713598 | T_A_C | EAS | 0.323 | ||
| 7 | rs10246939_rs1726866_rs713598 | T_A_C | EUR | 0.538 | ||
| 7 | rs10246939_rs1726866_rs713598 | T_A_C | SAS | 0.638 | ||
| 8 | rs1041983_rs1801280_rs1799930_rs1208 | C_C_G_G | AFR | 0.289 | 521 | Ethambutol, isoniazid, pyrazinamide, rifampin |
| 8 | rs1041983_rs1801280_rs1799930_rs1208 | T_T_A_A | AFR | 0.231 | ||
| 8 | rs1041983_rs1801280_rs1799930_rs1208 | C_C_G_G | AMR | 0.356 | ||
| 8 | rs1041983_rs1801280_rs1799930_rs1208 | T_T_A_A | EAS | 0.256 | ||
| 8 | rs1041983_rs1801280_rs1799930_rs1208 | C_C_G_G | EUR | 0.433 | ||
| 8 | rs1041983_rs1801280_rs1799930_rs1208 | T_T_A_A | EUR | 0.281 | ||
| 8 | rs1041983_rs1801280_rs1799930_rs1208 | T_T_A_A | SAS | 0.354 | ||
| 8 | rs1041983_rs1801280_rs1799930_rs1208 | C_C_G_G | SAS | 0.344 | ||
| 9 | rs7853758_rs885004 | A_G | AFR | 0.240 | 8624 | Anthracyclines and related substances |
| 9 | rs7853758_rs885004 | A_A | AMR | 0.200 | ||
| 10 | rs12777823_rs4244285_rs1799853_rs7900194_rs10509681_rs75838422 | A_A_C_G_G_T | EAS | 0.313 | 2056321 | Warfarin, proguanil, mephenytoin, amitriptyline, citalopram, clomipramine, clopidogrel |
| 10 | rs12777823_rs4244285_rs1799853_rs7900194_rs10509681_rs75838422 | A_A_C_G_G_T | SAS | 0.357 | ||
| 16 | rs7294_rs2359612_rs8050894_rs9934438_rs9923231_rs7196161 | C_A_G_A_T_G | AMR | 0.383 | 8660 | Warfarin, acenocoumarol, phenprocoumon, vitamin K-dependent clotting factors |
| 16 | rs7294_rs2359612_rs8050894_rs9934438_rs9923231_rs7196161 | C_A_G_A_T_G | EAS | 0.885 | ||
| 16 | rs7294_rs2359612_rs8050894_rs9934438_rs9923231_rs7196161 | C_A_G_A_T_G | EUR | 0.372 | ||
| 19 | rs11881222_rs12979860_rs8099917 | G_T_T | AFR | 0.256 | 8242 | Peginterferon alfa-2a, peginterferon alfa-2b, and ribavirin, telaprevir, boceprevir |
| 19 | rs11881222_rs12979860_rs8099917 | G_T_G | AMR | 0.275 |
*Order of the SNP alleles in the haplotypes are shown in the 2nd (SNP ID) column.
#Minor (variant) alleles are shown as bold italic font.
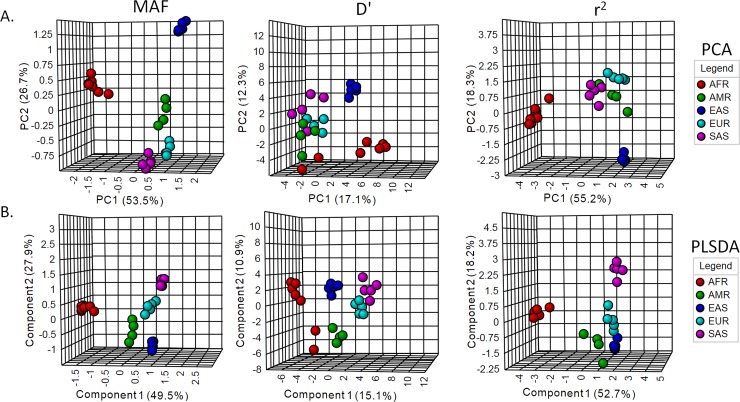
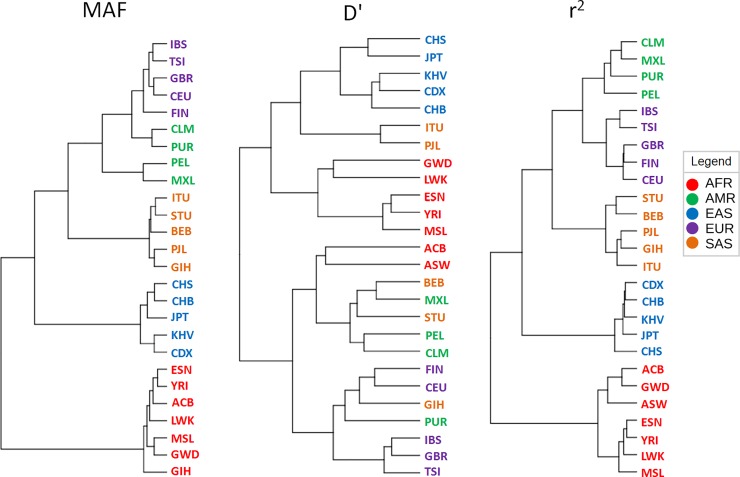
Geographic distribution of the drug-response related SNPs
We used MAFs (alleles that are considered as minor in global population) of the 159 SNPs, and both r2 and D' estimates of pairwise LD among these SNPs for multivariate clustering through principal component analysis (PCA), partial least square- discriminant analysis (PLS-DA), and hierarchical clustering (Figs 3 and 4). We used the first 2 components in PCA and PLS-DA to visualize the clustering pattern. With MAFs, the 1st and the 2nd components of both PCA and PLS-DA can explain more than 75% of the variations among the sub-populations (Fig 3A and 3B). The 1st and the 2nd components of both PCA and PLS-DA with r2 can explain > 70% variations among the populations (Fig 3A and 3B). As shown in the Fig 3A and 3B, component populations of the same super-populations cluster together. Americans of African ancestry in USA (ASW) and the African Caribbeans in Barbados are placed along with the African super-population. Hierarchical clustering of the MAF and r2 values using Euclidean distance measure and Ward’s algorithm cluster the component populations of each super-population in a similar way (Fig 4). In both MAF and r2 based dendrograms, African populations form a completely different branch from rest of the populations. In the other branch, the East Asian populations form a different clade from the Admixed American, European and South Asian populations. The other LD measure (D') cannot cluster the component populations as distinctively as in PCA and hierarchical clustering (Figs 3A and 4). Although D' places the component populations of super-populations in separate clusters in PLS-DA, their clustering is less obvious than the MAF and r2 based plots. Besides, in case of both PCA and PLS-DA using MAF and r2, but not D', the 1st component can distinctly separate African population cluster from clusters of other populations (Fig 3A and 3B). It is to be noted that PLS-DA is a supervised multivariate clustering method, which takes into consideration the data classes during the clustering process, while PCA is an unsupervised method.
Fig 3. Multivariate analysis using MAF, r2 and D' of the drug-response related SNPs in 26 populations.
A. Principle component analysis (PCA). B. Partial least square- discriminant analysis (PLS-DA).
Fig 4. Multivariate analysis using hierarchical clustering.
The dendrogram was constructed using the Ward clustering algorithm. The distances are not represented to scale on the tree.
Discussion
Drug-response related SNPs with high MAFs in global population and their clinical importance
Among the 159 drug-response related SNPs, we found 13 SNPs that have MAFs ≥ 0.2 in all super- and sub-populations. These SNPs are responsible for variable responses to bisphosphonates (rs2297480), carbamazepine, phenytoin and antiepileptics (rs3812718), fentanyl, morphine and opioids (rs2952768), cisplatin (rs2228001, rs1042522, rs3212986) oxazepam and lorazepam (rs1902023), salbutamol and salmeterol (rs1042713), antineoplastic agents such as cyclophosphamide, fluorouracil and paclitaxel (rs1042522), platinum and platinum compounds (rs3212986), nicotine (rs4680), debrisoquine (rs1135840), ethambutol, isoniazid, pyrazinamide and rifampin (rs1041983), and sildenafil (rs5443)- drugs that are prescribed for conditions like epilepsy, postmenopausal osteoporosis, pain relief, osteosarcoma, urinary bladder cancer, ovarian cancer, medulloblastoma, brain cancer, breast cancer, neutropenia, stomach cancer, non-small-cell lung carcinoma, colorectal cancer, esophageal cancer, pancreatic cancer, uterine cervical cancer, anxiety, insomnia, asthma, tuberculosis, etc [36, 37, 41]. rs6166 probably renders follicle-stimulating hormone receptor (FSHR) more sensitive to FSH by overcoming feedback inhibition [46]. Flurouracil (a common anti-cancer drug) and nicotine have been frequently reported to exhibit differences in drug response among different populations [8]. High MAF values at rs1042524 (also rs1042522) may play a role in such discrepancies.
One of these (rs2228001) variant-drug combinations has reached level 1B of clinical annotation [37]. Level 1B indicates annotation for a variant-drug combination in Clinical Pharmacogenomics Implementation Consortium (CPIC) or medical society-endorsed Pharmacogenomics (PGx) guideline, or implemented at a Pharmacogenomics Research Network (PGRN) site or in another major health system, for which the preponderance of evidences show an association. Patients with GG or GT genotype at rs2228001 may have an increased risk of cisplatin toxicity in comparison with those with TT genotype [37]. Another interesting variant-drug combination is rs4680-nicotine, which has level 2A clinical annotation evidence. The variants in level 2A are located in known pharmacogenes, and therefore, functional significance is more likely. rs4680 is located in the COMT gene. Individuals with the AA or AG genotype at rs4680, who are treated with nicotine replacement therapy (NRT), may have an increased likelihood of smoking cessation and decreased risk of relapse as compared to individuals with the GG genotype. Although A is the global minor allele at rs4680 (Table 1), its frequency is ≥ 0.5 in FIN, GBR and PJL sub-populations. The long term benefit of NRT is actually the requirement of modest and repeated episodes of such treatment [47]. Differences in the efficacy of NRT between men and women have been reported as well. Gains from long-term NRT decrease more rapidly for women than men [48]. Genotyping at the rs4680 locus may be considered while assessing the factors influencing NRT efficacy for the treatment of tobacco use disorder.
Drug-response related SNPs with high MAFs in individual populations and their clinical importance
18 SNPs have MAFs ≥ 0.2 in only one super-population (Table 1). 11 of these have MAFs ≥ 0.2 in African super-population. These are responsible for variable response to radiotherapy for prostate neoplasm (rs7582141, rs6432512, rs264588 and rs264631), irinotecan (rs7779029), tacrolimus (rs2740574), salbutamol (rs6988229), warfarin (rs4917639), hydrochlorothiazide (rs7297610 and rs16960228) and aspirin (rs6065). Four of these SNPs (rs7582141, rs6432512, rs264588 and rs264631) may be associated with variable risk of toxicity in response to radiotherapy for prostate neoplasm. There is level 2B clinical annotation evidence for these four variant-drug combinations [37]. Although data on prostate cancer treatment in Africa is under-reported [49], it is known that African men disproportionately suffer from prostate cancer compared to men from other parts of the world [50] and African American men have the highest rate of prostate cancer morbidity and mortality compared to men from any other race or ethnicity in the USA [51]. Socioeconomic and genetic factors are among the suggested explanations for such high burden of prostate cancer in African men [52]. There is no evidence that prostate cancer in African Americans is more virulent than in Caucasians [53]. But there are population-level genetic differences in androgen receptor signaling and DNA repair between African American and Caucasian men’s prostate cancer and African American men may harbor more radiosensitive tumors, which may result in better clinical outcomes from radiotherapy in African American patients with prostate cancer [54]. Since further studies are needed to conclusively find out all the factors affecting the efficacy of radiotherapy in African prostate cancer patients, the risk of increased toxicity of radiotherapy in prostate cancer patients with certain genotypes at rs7582141, rs6432512, rs264588 and rs264631 and their high (≥0.2) MAFs in African super-population should be considered. A discrete screening guideline may be helpful in treating African American men with prostate cancer [55] along with a distinct clinical guideline for radiotherapy.
The minor allele (C) at the rs4917639 locus- (located in CYP2C9 gene) is present with ≥0.2 frequency only in the African super-population. Individuals with the CA or CC genotype may require decreased dose of warfarin compared to those with the AA genotype and there is level 2A clinical annotation for this variant-drug combination [37]. An ethnicity-dependent CPIC guideline for warfarin dosing recommends a dose reduction of 10–25% in African Americans with AG or AA genotype at rs12777823, but not in patients with non-African ancestry [37]. Frequency of the A allele at rs12777823 is 0.251 in African super-population (Table 1). We did not find high pairwise LD between these 2 SNPs in African super-population. So, incorporation of rs4917639 into clinical guidelines may benefit individuals of African ancestry.
rs885004 and rs8099917 have MAFs ≥ 0.2 only in Admixed American super-population. These may cause variable response to anthracyclines and related substances (rs885004) and peginterferon alfa-2a, peginterferon alfa-2b, and ribavirin, telaprevir, boceprevir (rs8099917). There is level 1B clinical evidence for rs8099917 associated variable efficacy of peginterferon alfa-2a, peginterferon alfa-2b, ribavirin, telaprevir and boceprevir in chronic Hepatitis C treatment [37]. So, patients belonging to Admixed American super-population may benefit from dosing guidelines for these drugs based on the rs8099917 genotypes. In fact, it has been suggested that at least in HCV infected Caucasian patients simultaneous genotyping of rs12979860 and rs8099917 should be recommended prior to the initiation of pegylated interferons and ribavirin treatment [56]. The global minor allele (T) at rs12979860 has a frequency of 0.399 in Admixed American super-population (S1 Table). Determination of the rs8099917 genotype may benefit a significant proportion of heterozygous carriers of the rs12979860 T non-responder allele with respect to sustained virologic response prediction [57].
Two SNPs (rs2231142 and rs11045879) have MAFs ≥ 0.2 only in the East Asian super-population (Table 1). These may cause variable response to rosuvastatin and allopurinol (rs2231142) and methotrexate (rs11045879). There is level 2A clinical annotation for all these variant-drug combinations [37]. Ethnic differences in response to rosuvastatin (especially, the increased systemic exposure to this drug in people with Chinese ethnicity) have been mentioned earlier. FDA recommends Asian patients to initiate rosuvastatin at half of the normal dose for non-Asians [58].
rs17708472, rs2884737 and rs1876828 have MAFs ≥ 0.2 only in the European super-population. These SNPs may be responsible for variable response to warfarin (rs17708472 and rs2884737, which are located in VKORC1) and budesonide, corticosteroids, fluticasone propionate, fluticasone/salmeterol and triamcinolone (rs1876828). Genotype at rs17708472 and rs2884737 may influence warfarin dose requirement [37]. There is level 2A clinical evidence for the variant-drug combinations for these two SNPs [37]. Genotype at rs1876828 may affect the efficacy and, therefore, response to inhaled corticosteroids may influence resulting endogenous cortisol level [37]. rs1876828 is located in CHR1 gene, which is targeted with drugs to treat asthma. There is level 2B clinical annotation for these variant-drug combinations [37]. There is currently no clinical guideline for inhaled cortecosteroids that are used to treat asthma.
5 SNPs (rs2359612, rs8050894, rs9934438, rs9923231 and rs7196161) have MAF ≥ 0.8 in all East Asian sub-populations. These share absolute LD (r2 = 1) among them (S1 Fig). These SNPs cause variability in response to warfarin (rs2359612, rs8050894, rs9934438, rs9923231 and rs7196161), acenocoumarol and phenprocoumon (rs9934438 and rs9923231), and vitamin K-dependent clotting factors (rs9934438) [35,36]. As discussed earlier, there is level 1A clinical annotation for rs9923231-warfarin combination and level 1B clinical annotation for rs9934438-warfarin, rs9923231-acenocoumarol, and rs9923231-phenprocoumon combinations [37]. Individuals with CT genotype at rs9923231 may require a decreased dose of warfarin, acenocoumarol and phenprocoumon as compared to those with the CC genotype or an increased dose as compared to those with TT genotype [37]. Individuals with AA genotype at rs9934438 may require a lower dose of warfarin as compared to patients with the AG or GG genotype [37]. Chinese patients require lower dose of warfarin than Caucasian patients and VKORC1 genotype has already been suggested to be an important determinant of warfarin response in Chinese patients [59]. The same study reported the high frequencies (≥0.8) of the global minor alleles at rs9923231 and rs9934438 loci in Chinese population. So, reduced dosage of warfarin, acenocoumarol and phenprocoumon for individuals from East Asian populations may be recommended. High frequency of T allele at rs9923231 in East European populations may be the result of positive selection [60]. The absolute pairwise LD among rs2359612, rs8050894, rs9934438, rs9923231 and rs7196161 in East Asian populations is not an unusual finding. In fact, a 505 kb region of strong LD, which contains VKORC1 and 24 neighboring genes, is located on chromosome16 only in East Asian populations and this genomic region may have been submitted to a near complete selective sweep in all East Asian populations and only in this geographic area [61].
rs1954787 has MAF ≥ 0.8 in all African sub-populations and is responsible for variable response to antidepressants. Currently, there is level 2B clinical annotation for this variant-drug combination. Individuals with CT or TT genotype and depressive disorder or depression may be less likely to respond to antidepressant treatment as compared to those with CC genotype [37]. Major depressive disorder (MDD) usually remains untreated and is more severe and disabling in the African Americans and Caribbean Blacks compared with Anglo Americans [62]. Consequently, the burden of mental disorders, especially depressive disorders, may be higher in African Americans [62]. If the association between genotype at rs1954787 and variable response to antidepressants becomes strongly definitive, this marker may be employed in conjunction with other known predictors to anticipate the outcome of treatments with antidepressants [63] considering the fact that more than 80% patients with African ancestry may be less likely to respond to antidepressants.
In addition to these, level 1A clinical annotation is available for the following variant-drug combinations: rs887829-atazanavir; rs1142345-azathioprine, mercaptopurine, purine analogues, thioguanine; rs1800460-azathioprine, mercaptopurine, purine analogues, thioguanine; rs12248560-clopidogrel; rs28399504-clopidogrel; rs4986893- clopidogrel; rs1057910-warfarin; rs4149056-simvastatin; rs116855232-azathioprine, mercaptopurine; rs9923231- warfarin; and rs12979860-peginterferon alfa-2a, peginterferon alfa-2b, ribavirin [37]. Level 1B clinical annotation is available for the following variant-drug combinations and rs3745274-efavirenz [37].
SNPs in the Cytochrome P450 genes
Cytochrome P450 family genes (CYP) have been extensively studied in the context of pharmacogenomics because of their important roles in drug metabolism [64, 65]. Ethnic differences in these genes have been reported [14]. MAFs of CYP genes in all the super-populations are listed in S2 Table. Among these rs1135840, rs16947, rs1065852, rs12248560, rs4244285, rs4917639, rs3745274, rs776746, rs2740574, rs25487, rs2108622 and rs1056836 have MAF ≥ 0.2 in multiple super-populations. Level 1A clinical annotation is available for rs2108622-warfarin combination. Individuals with TT genotype at rs2108622 may require a higher dose of warfarin as compared to those with CC or CT genotype [37]. African populations stand out different from the other populations in terms of other SNPs in CYP genes as well. African populations are known to have different frequencies of certain ADRs than rest of the world [66]. The major alleles (frequency ≥ 0.5) at the rs16947, rs776746, rs2740574 and rs1056836 loci in most African subpopulations are actually global minor alleles. There are level 1A clinical annotations available for rs16947 (an SNP defining CYP2D6*2 allele)- paroxetine, nortriptyline, codeine, doxepin, trimipramine, clomipramine, atomoxetine and amitriptyline and rs776746- tacrolimus combinations [37]. T is the global minor allele at rs776746 and recipients of kidney, heart, lung or hematopoietic stem cell transplant, who have CT or TT genotype at rs776746 may require a higher dose of tacrolimus compared to those with CC genotype [37]. Differences in the allele frequencies at rs776746 between the European descendant and the African American individuals is partly responsible for the lower trough blood concentration of tacrolimus in African American kidney allograft recipients compared to the European descendants [67]. An African American-specific genotype-guided tacrolimus dosing model has recently been developed since African Americans have 20–50% lower bioavailability, higher clearance and lower blood concentration of tacrolimus and, as a result, require ~1.5–2 times higher doses than the Caucasians [68]. Other African populations may also benefit from this guideline. On the other hand, aroxetine, trimipramine, atomoxetine, clomipramine and amitriptyline are used to treat various mental disorders, especially depressive disorder [37]. It again shows the difficulty in selecting an efficacious drug to treat mental disorders in patients with African ancestry. There is level 1B clinical annotation for rs16947 (an SNP defining CYP2D6*2 allele)-tramadol combination. So, tramadol and codeine, both of which are used to treat pain, may have less than optimum response in the majority of individuals with African ancestry. It may have serious clinical implications as there are racial/ethnic disparities in pain epidemiology, access to quality pain care, pain assessments and treatments and pain-related outcomes [69]. rs16497 can reduce CYP2D6 expression by about 2 folds and thus may reduce overall CYP2D6 metabolic activity [70]. Incorporation of rs16947 along with another SNP into CYP2D6 biomarker panel may improve the accuracy of CYP2D6 metabolizer status prediction [71]. Poor metabolizers with less CYP2D6 activity may have very little analgesic efficacy for codeine [72]. Codeine is often prescribed to individuals with sickle cell disease (SCD) and precision medicine approach is necessary to maintain it as a safe option for pain control [73]. SCD is very common throughout much of sub-Saharan Africa [74]. African Americans with SCD are less genetically admixed than other African Americans and have an ancestry similar to Yorubans, Mandinkas and Bantu [75]. So, SCD may be more prevalent among individuals that are more closely related to sub-Saharan Africans. Moreover, the only two African sub-populations with MAF < 0.5 at rs16947 are ASW and ACB (Table 1). The sub-Saharan African populations have MAF ≥ 0.5 at rs16947. So, codeine may be less likely to be effective in individuals closely related to sub-Saharan Africa. Hence, alternative drugs may be considered for managing pain in SCD patients with African ancestry. Although we did not find extensive CYP allele frequency variations among the African populations as reported in a previous study [76], our results also emphasize the need for the population targeted optimization and development of drugs.
Drug-response related SNP haplotypes with high frequencies
Apart from the 10 haplotypes with at least two global minor alleles and frequencies ≥ 0.2 in at least one super-population (Table 3), there is an important haplotype (T_T_C_T_T_G_A_G) in the East Asian populations on chromosome 2. Although the frequency of this haplotype (0.1052) is < 0.2, all alleles except the first one are the minor (variant) alleles at the corresponding SNP loci (rs6166_ rs6165_ rs10497203_ rs7582141_ rs6432512_ rs264651_ rs264588_ rs264631) in the global population. All of these SNPs, except rs6166 and rs6165, are responsible for variable responses to radiotherapy for prostate cancer. However, currently none of these variant-drug combinations qualifies for level 1A or level 1B clinical annotation [37]. SNPs in other haplotypes (Table 3) with high prevalence cause variability in response to antidepressants, citalopram, fluoxetine, mirtazapine, paroxetine, selective serotonin reuptake inhibitors, venlafaxine (chromosome 6: T_C_T_A), phenylthiocarbamide tasting (chromosome 7: T_A_C), ethambutol, isoniazid, pyrazinamide, rifampin (chromosome 8: C_C_G_G and T_T_A_A), anthracyclines and related substances (chromosome 9: A_A), warfarin, proguanil, mephenytoin, amitriptyline, citalopram, clomipramine, clopidogrel (chromosome 10: A_A_C_G_G_T), warfarin, acenocoumarol, phenprocoumon, vitamin K-dependent clotting factors (chromosome 16: C_A_G_A_T_G) and peginterferon alfa-2a, peginterferon alfa-2b, and ribavirin, telaprevir, boceprevir (chromosome 19: G_T_T and G_T_G) [36, 37]. It is worth noting that multiple SNPs in the haplotype on chromosome 10 are located in CYP2C gene region and all except one SNP in the haplotype on chromosome 16 are located in VKORC1 gene region. These are two very important pharmacogenes. Both of these haplotypes (A_A_C_G_G_T and C_A_G_A_T_G, respectively) are present in global population with frequency ≥ 0.2. Clinical annotations for rs12777823-warfarin and rs9923231-warfarin combinations have already been discussed. Among the other SNPs in the haplotype on chromosome 10, level 1A clinical annotation is available for rs4244285-clopidogrel, rs4244285-amitriptyline and rs1799853-warfarin combinations [37]. On chromosome 16, level 1B clinical annotation is available for rs7294-warfarin, rs9934438-warfarin and rs9923231-acenocoumarol, phenprocoumon combinations [37].
LD patterns of the drug-response related SNPs across populations
Presence of long stretches of genomic regions with high LD in a particular population means that a number of neighboring SNPs are in strong or absolute pairwise LD with the functional or causal variant within that population. So, SNPs that are in strong or absolute pairwise LD with the causal variant will give similarly strong association signal. In that case, trans-population analysis, which utilizes differences in LD patterns across different populations, can be used to narrow the list of possible causal variants [77]. Hence, it is important to know the inter-population variability in LD pattern.
Extent of LD is lower in African in comparison to non-African populations [31, 78–84]. We found only 7 SNP pairs with strong pairwise LD (r2 ≥ 0.8) in African super-population, compared to 11 pairs in global population (Table 2). 4 SNP pairs were found to have strong LD (r2> 0.9) in all super-populations (Table 2). Among the individual super-populations, East Asian had the highest number of SNP loci (43) that maintain strong LD (r2≥0.8) with one another. Majority of these SNP pairs (32) maintain r2 ≥ 0.9, which is highly distinctive of the East Asian population (Fig 2). It is known that populations with higher extent of LD or background LD are more suitable for initial mapping in GWAS, whereas populations with lower level of LD or background LD are more suitable for subsequent fine mapping of causal variants [5, 85]. So, East Asian population might be investigated for initial mapping in future GWAS for pharmacognomic investigation.
Human evolution and geographic distribution of the drug-response related SNPs
Multiple studies have used allele frequencies for inferring human population structure [86–88]. We used the MAFs and pairwise LD measures (r2 and D') of 159 drug response-related SNPs for multivariate analysis using PCA, PLS-DA and hierarchical clustering (Figs 3 and 4). African populations appear completely distinct from the other populations. Similar results were obtained in previous studies using SNP loci, Alu insertion sites and D1S80 allele frequencies [86–89]. In these studies, the East Asian populations appear to be more distant from South Asian, European and Admixed American populations.
Fossil and genetic evidences suggest that anatomically modern humans evolved in Africa about 150,000 to 190,000 years ago and then migrated into Europe, Asia, and finally to the Americas in an approximately West-to-East pattern [82, 90, 91]. Geographic isolation, interbreeding, and adaptation in new environments differentiated human populations from each other [82]. Consistent with the out-of-Africa model of human origin, the Africans possess the oldest genetic pool and the highest level of genetic diversity [92]. Therefore, extent of LD is lower in African in comparison to non-African populations [31, 78–84]. There is more Neanderthal admixture into East Asian populations than into European populations and some extent of admixture occurred after the separation of East Asians and Europeans [93–97]. European and South Asian populations have been reported to be closely related in multiple studies [88, 89, 98]. South Asian populations also share Denisovan ancestry with the East Asians [96]. PCA, PLS-DA and dendrogram plotted with MAF and r2, but not D', of drug-response related SNPs could reproduce the human evolutionary history and geographic distribution.
Linkage disequilibrium (LD) that exists among DNA variants in the current human genome is the result of historical evolutionary forces, particularly finite population size, mutation, recombination rate, and natural selection [99]. LD between genetic variants is commonly measured as r2 (a squared correlation) or D′ (which is equal to D normalized by its maximum given the allele frequencies) [99, 100]. Though r2 or D' both depend on the allele frequencies, r2 is a more stringent measure and depends more on allele frequencies [101–103].
In PCA, PLS-DA and dendrogram with MAF and r2 values, Americans of African Ancestry (ASW) and African Caribbeans in Barbados (ACB) clustered with the African sub-populations. Based on the historical records, the African Americans and the African Caribbeans in Barbados are descended from slaves who were imported mostly from West Africa during the eighteenth century [27]. African Americans have genetic admixture with approximately 80% of their genome derived from their African ancestors and 20% from the Europeans [12, 82]. Among the African populations in this study, Mende (MSL) and Gambian (GWD) share mostly the Western African ancestry, Esan (ESN) and Yoruba (YRI) peoples from Nigeria share the West-Central African ancestry and the Luhya (LWK) people from Kenya belong to the Bantu-speaking Eastern African ancestry [104]. Since, the slaves in America and Carribeans were brought mostly from West Africa [27], they are supposed to carry more genetic similarity to the African populations than the Southern American ones [104, 105]. As shown in Figs 3 and 4, ASW and ACB populations form a distinct cluster with the other African populations, rather than with Admixed American populations. Admixed American populations appeared more closely genetically related with European populations in dendrogram with both MAF and r2.
Latin American populations- Colombia, Mexico, Peru, and Puerto Rico- have distinct patterns of continental genetic admixture [91]. Puerto Rico and Colombia are characterized by substantial ancestry contributions from African, European and Native American groups, whereas Mexico and Peru have primarily Native American and European ancestry [91]. Puerto Rico and Colombia inherited more genetic content from the European ancestry than Peru and Mexico [91, 106–108]. In the MAF based dendrogram, CEL and PUR form a closer branch with the European populations. Such finer distinctions were achieved with MAF and not r2. A dendrogram recapitulates the relationships among population groups. Individuals who cluster near each other in the tree could either share a recent common ancestry and/or experienced gene flow [84]. Finnish in Finland (FIN) are estimated to have obtained ~7% of their ancestry from East Asians and admixed American populations, whose Native American ancestors are related to East Asians [96]. MAF based dendrogram could figure out such finer genetic distinctions, which could not be detected with r2. So, human migration patterns and demographical history can be more accurately reconstructed with allele frequencies than pairwise LD measures. More dependency of r2 on allele frequencies in comparison to D' may explain why r2 is better than D' at reconstructing such patterns and history.
Although most of the large inter-continental differences in allele frequency may not result from positive selection [109], there may be numerous cases of recent positive selection of pharmacogenes [110]. We observed many drug-response related SNPs with higher MAFs in certain super- or subpopulations compared to other populations (S1 Table). There is evidence of natural selection for some of these SNPs, while the others require further investigations. For example, among the SNPs with MAFs ≥ 0.8 in at least one super- or subpopulation the possibility of natural selection has been suggested for rs776746 [111], rs2740574 [111], rs2359612 [61], rs8050894 [61], rs9934438 [61], rs9923231 [61], rs1346268 [112], rs7294 [61]. Hence, the pattern of allele frequency distribution observed for these 159 drug response-related SNPs may not be observed for any random 159 SNPs. Many of the SNPs chosen for this study may be under natural selection.
Can these findings be generalized?
Considering the high similarities of MAFs in sub-populations belonging to the same super-population, it may seem tempting to study only the super-populations to predict drug responses in all of its sub-populations. But such generalizations may not be appropriate. Only 26 sub-populations were included in this study and most of these samples cannot be considered representatives of their source populations. There can be marked differences in the allele frequencies of important pharmacogenes among the sub-populations belonging to the same super-population. Such differences were observed in the allele frequencies of CYP genes in African populations [76]. There may be large allele frequency differences even among groups of the same population. This phenomenon is observed in India where endogamy has maintained signatures of strong founder effects for thousands of years [113]. So, different Indian groups may show quite different drug responses. For example, there is a very high frequency of homozygous silent butyrylcholinesterase (BChE) in Vysya community of India [114]. Individuals with this particular genetic variant (BChE L307P) may have negligible activity due to its structural instability as compared to other BChE variants [115]. Administration of muscle relaxant succinylcholine to individuals carrying BChE variants with no or reduced activity may cause prolonged apnea [116]. Deficiency of BChE activity may also cause apnea after administration of neuromascular blocking drug mivacurium [117]. Furthermore, even two neighboring populations living in the same country may have differences in drug response if they have different ancestry or different level of admixture. For example, there are differences in allele frequencies of drug response-related SNPs between two neighboring Colombian populations- Antioquia and Chocó- owing to their distinct ancestry profiles [118].
In our study, we looked at only the SNPs that may cause variable drug responses. But other factors e.g., diet, chemical exposures from the environment, disease state, etc may be sources of variability in drug response as well [37, 119]. Epigenetic modulations of ADME genes and drug targets may be important determinant of responses to drugs [120]. Especially, epigenetics can play an important role in the acquired resistance to chemotherapy in cancer patients and epigenetic biomarkers may predict the outcomes of chemotherapy [121, 122]. In addition to drug-gene interactions, drug-gene-drug interactions may also cause differences in drug response and should be considered during prescribing drugs [123, 124].
Conclusion
There is a global concern to increase pharmacogenetic testing to ensure drug safety and enhance drug efficacy [125, 126]. However, most GWAS to identify drug-response related variants have been performed in the western populations and others have lagged behind [7, 127, 128]. It is important to understand the interpopulation or interethnic variability in drug response so that population/ethnicity-specific guidelines can be produced. Besides, knowing the SNP distribution and LD patterns of different populations will be helpful in causal variant discovery. In this study, we looked at the interpopulation similarities as well as differences in drug-response related minor (variant) allele frequencies, LD patterns and haplotype distributions. This study may be useful in comparative and evolutionary pharmacogenomics studies among populations in future.
Supporting information
(TIF)
(PDF)
(DOC)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This work was supported by the Ministry of Science and Technology, Bangladesh. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Brown AM, Renaud Y, Ross C, Hansen M, Mongrain I, Valois D, et al. Development of a broad-based ADME panel for use in pharmacogenomic studies. Pharmacogenomics. 2014;15(9):1185–95. 10.2217/pgs.14.81 [DOI] [PubMed] [Google Scholar]
- 2.Grossman I. ADME pharmacogenetics: current practices and future outlook. Expert Opin Drug Metab Toxicol. 2009;5(5):449–62. 10.1517/17425250902902322 [DOI] [PubMed] [Google Scholar]
- 3.Mukerjee G, Huston A, Kabakchiev B, Piquette-Miller M, van Schaik R, Dorfman R. User considerations in assessing pharmacogenomic tests and their clinical support tools. NPJ Genom Med. 2018;3(26). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Impicciatore P, Choonara I, Clarkson A, Provasi D, Pandolfini C, Bonati M. Incidence of adverse drug reactions in paediatric in/out-patients: a systematic review and meta-analysis of prospective studies. Br J Clin Pharmacol. 2001;52(1):77–83. 10.1046/j.0306-5251.2001.01407.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279(15):1200–5. 10.1001/jama.279.15.1200 [DOI] [PubMed] [Google Scholar]
- 6.Mouton JP, Mehta U, Parrish AG, Wilson DP, Stewart A, Njuguna CW, et al. Mortality from adverse drug reactions in adult medical inpatients at four hospitals in South Africa: a cross-sectional survey. Br J Clin Pharmacol. 2015;80(4):818–26. 10.1111/bcp.12567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanghera DK, Bejar C, Sapkota B, Wander GS, Ralhan S. Frequencies of poor metabolizer alleles of 12 pharmacogenomic actionable genes in Punjabi Sikhs of Indian Origin. Sci Rep. 2018;8(1):15742 10.1038/s41598-018-33981-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bachtiar M, Lee CGL. Genetics of population differences in drug response. Curr Genet Med Rep. 2013;1(3):162–70. [Google Scholar]
- 9.Goulding R, Dawes D, Price M, Wilkie S, Dawes M. Genotype-guided drug prescribing: a systematic review and meta-analysis of randomized control trials. Br J Clin Pharmacol. 2015;80(4):868–77. 10.1111/bcp.12475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nebert D, Menon A. Pharmacogenomics, ethnicity, and susceptibility genes. Pharmacogenomics J. 2001;1(1):19–22. 10.1038/sj.tpj.6500002 [DOI] [PubMed] [Google Scholar]
- 11.Suarez-Kurtz G, Parra EJ. Population Diversity in Pharmacogenetics: A Latin American Perspective. Adv Pharmacol. 2018;83:133–54. 10.1016/bs.apha.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 12.Ortega VE, Meyers DA. Pharmacogenetics: implications of race and ethnicity on defining genetic profiles for personalized medicine. J Allergy Clin Immunol. 2014;133(1):16–26. 10.1016/j.jaci.2013.10.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Claudio-Campos K, Duconge J, Cadilla CL, Ruaño G. Pharmacogenetics of drug-metabolizing enzymes in US Hispanics. Drug Metab Pers Ther. 2015;30(2):87–105. 10.1515/dmdi-2014-0023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGraw J, Waller D. Cytochrome P450 variations in different ethnic populations. Expert Opin Drug Metab Toxicol. 2012;8:371–82. 10.1517/17425255.2012.657626 [DOI] [PubMed] [Google Scholar]
- 15.Srivastava MR, Chandra A. STATINS-do we know them or are we Alice in wonderland? Endocrinol Metab Int J. 2017;5(3):241–3. [Google Scholar]
- 16.Rahal AJ, ElMallah AI, Poushuju RJ, Itani R. Do statins really cause diabetes? A meta-analysis of major randomized controlled clinical trials. Saudi Med J. 2016;37:1051–60. 10.15537/smj.2016.10.16078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sattar NA, Ginsberg H, Ray K, Chapman MJ, Arca M, Averna M, et al. The use of statins in people at risk of developing diabetes mellitus: evidence and guidance for clinical practice. Atheroscler Suppl. 2014;15(1):1–15. 10.1016/j.atherosclerosissup.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 18.Lee E, Ryan S, Birmingham B, Zalikowski J, March R, Ambrose H, et al. Rosuvastatin pharmacokinetics and pharmacogenetics in white and Asian subjects residing in the same environment. Clin Pharmacol Ther. 2005;78(4):330–41. 10.1016/j.clpt.2005.06.013 [DOI] [PubMed] [Google Scholar]
- 19.Dou Y, Peng P, Cai C, Ye A, Kong L, Zhang R. HLA-B*58:01 and rs9263726 have a linkage, but not absolute linkage disequilibrium in Han Chinese population. Drug Metab Pharmacokinet. 2018;33(5):228–31. 10.1016/j.dmpk.2018.08.001 [DOI] [PubMed] [Google Scholar]
- 20.Maekawa K, Nishikawa J, Kaniwa N, Sugiyama E, Koizumi T, Kurose K, et al. Development of a rapid and inexpensive assay for detecting a surrogate genetic polymorphism of HLA-B*58:01: a partially predictive but useful biomarker for allopurinol-related Stevens-Johnson syndrome/toxic epidermal necrolysis in Japanese. Drug Metab Pharmacokinet. 2012;27(4):447–50. 10.2133/dmpk.dmpk-11-nt-120 [DOI] [PubMed] [Google Scholar]
- 21.Hariprakash JM, Vellarikkal SK, Keechilat P, Verma A, Jayarajan R, Dixit V, et al. Pharmacogenetic landscape of DPYD variants in south Asian populations by integration of genome-scale data. Pharmacogenomics. 2018;19(3):227–41. 10.2217/pgs-2017-0101 [DOI] [PubMed] [Google Scholar]
- 22.Alhusain L, Hafez AM. Nonparametric approaches for population structure analysis. Human genomics. 2018;12(1):25 10.1186/s40246-018-0156-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paschou P, Ziv E, Burchard EG, Choudhry S, Rodriguez-Cintron W, Mahoney MW, et al. PCA-correlated SNPs for structure identification in worldwide human populations. PLoS genetics. 2007;3(9):1672–86. 10.1371/journal.pgen.0030160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taranto F, D’Agostino N, Greco B, Cardi T, Tripodi P. Genome-wide SNP discovery and population structure analysis in pepper (Capsicum annuum) using genotyping by sequencing. BMC Genomics. 2016;17:943 10.1186/s12864-016-3297-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pickrell JK, Pritchard JK. Inference of population splits and mixtures from genome-wide allele frequency data. PLoS Genet. 2012;8(11):e1002967 10.1371/journal.pgen.1002967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qin P, Zhou Y, Lou H, Lu D, Yang X, Wang Y, et al. Quantitating and dating recent gene flow between European and East Asian populations. Sci Rep. 2015;5:9500 10.1038/srep09500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chakraborty R. Gene admixture in human populations: models and predictions. Yearbook of physical anthopology 1986;29:1–43. [Google Scholar]
- 28.Excoffier L, Smouse PE. Using allele frequencies and geographic subdivision to reconstruct gene trees within a species: molecular variance parsimon. Genetics. 1994;136:343–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meisner J, Albrechtsen A. Inferring population structure and admixture proportions in low-depth NGS data. Genetics. 2018;10(2):719–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ardlie KG, Kruglyak L, Seielstad M. Patterns of linkage disequilibrium in the human genome. Nat Rev Genet. 2002;3(4):299–309. 10.1038/nrg777 [DOI] [PubMed] [Google Scholar]
- 31.Campbell MC, Tishkoff SA. African genetic diversity: implications for human demographic history, modern human origins, and complex disease mapping. Annu Rev Genomics Hum Genet. 2008;9:403–33. 10.1146/annurev.genom.9.081307.164258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim IW, Kim KI, Chang HJ, Yeon B, Bang SJ, Park T, et al. Ethnic variability in the allelic distribution of pharmacogenes between Korean and other populations. Pharmacogenetics and genomics. 2012;22(12):829–36. 10.1097/FPC.0b013e328358dd70 [DOI] [PubMed] [Google Scholar]
- 33.Mahasirimongkol S, Chantratita W, Promso S, Pasomsab E, Jinawath N, Jongjaroenprasert W, et al. Similarity of the allele frequency and linkage disequilibrium pattern of single nucleotide polymorphisms in drug-related gene loci between Thai and northern East Asian populations: Implications for tagging SNP selection in Thais. J Hum Genet. 2006;51(10):896–904. 10.1007/s10038-006-0041-1 [DOI] [PubMed] [Google Scholar]
- 34.Marigorta UM, Navarro A. High trans-ethnic replicability of GWAS results implies common causal variants. PLoS Genet. 2013;9(6):e1003566 10.1371/journal.pgen.1003566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mueller JC, Lõhmussaar E, Mägi R, Remm M, Bettecken T, Lichtner P, et al. Linkage disequilibrium patterns and tagSNP transferability among European populations. Am J Hum Genet. 2005;76(3):387–98. 10.1086/427925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Landrum MJ, Lee JM, Riley GR, Jang W, Rubinstein WS, Church DM, et al. ClinVar: public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res. 2014;42(Database issue):D980–5. 10.1093/nar/gkt1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Whirl-Carrillo M, McDonagh EM, Hebert JM, Gong L, Sangkuhl K, Thorn CF, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92(4):414–7. 10.1038/clpt.2012.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Machiela MJ, Chanock SJ. LDlink: A web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics. 2015;31:3555–7. 10.1093/bioinformatics/btv402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.1000 Genomes Project Consortium, Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, et al. A global reference for human genetic variation. Nature. 2015;526(7571):68–74. 10.1038/nature15393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xia J, Psychogios N, Young N, Wishart DS. MetaboAnalyst: a web server for metabolomic data analysis and interpretation. Nucleic Acids Res. 2009;37(Web Server issue):W652–60. 10.1093/nar/gkp356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahsan T, Sajib AA. Drug-response related genetic architecture of Bangladeshi population. Meta Gene. 2019;21:100585. [Google Scholar]
- 42.Luikart G, Allendorf FW, Cornuet JM, Sherwin WB. Distortion of allele frequency distributions provides a test for recent population bottlenecks. J Hered. 1998;89(3):238–47. 10.1093/jhered/89.3.238 [DOI] [PubMed] [Google Scholar]
- 43.He P, Lei X, Yuan D, Z Z, Huang S. Accumulation of minor alleles and risk prediction in schizophrenia. Scientific Reports. 2017;7:11661 10.1038/s41598-017-12104-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Szpiech ZA, Rosenberg NA. On the size distribution of private microsatellite alleles. Theor Popul Biol. 2011;80(2):100–13. 10.1016/j.tpb.2011.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Evans DM, Cardon LR. A comparison of linkage disequilibrium patterns and estimated population recombination rates across multiple populations. Am J Hum Genet. 2005;76(4):681–7. 10.1086/429274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rahman MS, Ahsan T, Hossain MR, Ahmed T, Sajib AA. Molecular mechanism of Metformin Associated Lactic Acidosis (MALA)- an in silico exploration. Current Pharmacogenomics and Personalized Medicine. 2018;16(3):199–209. [Google Scholar]
- 47.Etter JF, Stapleton JA. Nicotine replacement therapy for long-term smoking cessation: a meta-analysis. Tob Control. 2006;15(4):280–5. 10.1136/tc.2005.015487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cepeda-Benito A, Reynoso JT, Erath S. Meta-analysis of the efficacy of nicotine replacement therapy for smoking cessation: differences between men and women. J Consult Clin Psychol. 2004;72(4):712–22. 10.1037/0022-006X.72.4.712 [DOI] [PubMed] [Google Scholar]
- 49.Asamoah FA, Yarney J, Awasthi S, Vanderpuye V, Venkat PS, Fink AK, et al. Contemporary radiation treatment of prostate cancer in Africa: a Ghanaian experience. J Glob Oncol. 2018;4:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Adeloye D, David RA, Aderemi AV, Iseolorunkanmi A, Oyedokun A, Iweala EE, et al. An estimate of the incidence of prostate cancer in Africa: a systematic review and meta-analysis. PloS one. 2016;11(4):e0153496 10.1371/journal.pone.0153496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Odedina FT, Akinremi TO, Chinegwundoh F, Roberts R, Yu D, Reams RR, et al. Prostate cancer disparities in Black men of African descent: a comparative literature review of prostate cancer burden among Black men in the United States, Caribbean, United Kingdom, and West Africa. Infect Agent Cancer. 2009;4(Suppl I):S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hayes VM, Bornman MSR. Prostate cancer in Southern Africa: does Africa hold untapped potential to add value to the current understanding of a common disease? J Glob Oncol. 2018;4:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zagars GK, Pollack A, Pettaway CA. Prostate cancer in African-American men: outcome following radiation therapy with or without adjuvant androgen ablation. Int J Radiat Oncol Biol Phys. 1998;42(3):517–23. 10.1016/s0360-3016(98)00260-0 [DOI] [PubMed] [Google Scholar]
- 54.Spratt DE, Dess RT, Hartman HE, Mahal BA, Jackson WC, Soni PD, et al. Androgen receptor activity and radiotherapeutic sensitivity in African-American men with prostate cancer: a large scale gene expression analysis and meta-analysis of RTOG trials. International Journal of Radiation Oncology 2018;102(3):S3. [Google Scholar]
- 55.Shenoy D, Packianathan S, Chen AM, Vijayakumar S. Do African-American men need separate prostate cancer screening guidelines? BMC Urol. 2016;16:19 10.1186/s12894-016-0137-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sticchi L, Di Biagio A, Rappazzo E, Setti M, De Rosa G, De Hoffer L, et al. Rs12979860 and rs8099917 single nucleotide polymorphisms of interleukin-28B gene: simultaneous genotyping in caucasian patients infected with hepatitis C virus. J Prev Med Hyg. 2013;54(2):83–6. [PMC free article] [PubMed] [Google Scholar]
- 57.Fischer J, Böhm S, Scholz M, Müller T, Witt H, George J, et al. Combined effects of different interleukin-28B gene variants on the outcome of dual combination therapy in chronic hepatitis C virus type 1 infection. Hepatology. 2012;55(6):1700–10. 10.1002/hep.25582 [DOI] [PubMed] [Google Scholar]
- 58.Wu HF, Hristeva N, Chang J, Liang X, Li R, Frassetto L, et al. Rosuvastatin pharmacokinetics in Asian and white subjects wild type for both OATP1B1 and BCRP under control and inhibited conditions. J Pharm Sci. 2017;106(9):2751–7. 10.1016/j.xphs.2017.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lam MP, Cheung BM. The pharmacogenetics of the response to warfarin in Chinese. Br J Clin Pharmacol. 2012;73(3):340–7. 10.1111/j.1365-2125.2011.04097.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ross KA, Bigham AW, Edwards M, Gozdzik A, Suarez-Kurtz G, Parra EJ. Worldwide allele frequency distribution of four polymorphisms associated with warfarin dose requirements. J Hum Genet. 2010;55(9):582–9. 10.1038/jhg.2010.73 [DOI] [PubMed] [Google Scholar]
- 61.Patillon B, Luisi P, Blanché H, Patin E, Cann HM, Génin E, et al. Positive selection in the chromosome 16 VKORC1 genomic region has contributed to the variability of anticoagulant response in humans. PloS one. 2012;7(12):e53049 10.1371/journal.pone.0053049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Williams DR, Gonza´lez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites. Arch Gen Psychiatry. 2007;2007(64):305–15. [DOI] [PubMed] [Google Scholar]
- 63.Kawaguchi DM, Glatt SJ. GRIK4 polymorphism and its association with antidepressant response in depressed patients: a meta-analysis. Pharmacogenomics. 2014;15(11):1451–9. 10.2217/pgs.14.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aka I, Bernal CJ, Carroll R, Maxwell-Horn A, Oshikoya KA, Van Driest SL. Clinical Pharmacogenetics of Cytochrome P450-Associated Drugs in Children. J Pers Med. 2017;7(4):pii: E14 10.3390/jpm7040014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ingelman-Sundberg M. Pharmacogenetics of cytochrome P450 and its applications in drug therapy: the past, present and future. Trends Pharmacol Sci. 2004;25:193–200. 10.1016/j.tips.2004.02.007 [DOI] [PubMed] [Google Scholar]
- 66.Ampadu HH, Hoekman J, de Bruin ML, Pal SN, Olsson S, Sartori D, et al. Adverse Drug Reaction Reporting in Africa and a Comparison of Individual Case Safety Report Characteristics Between Africa and the Rest of the World: Analyses of Spontaneous Reports in VigiBase®. Drug Saf. 2016;39(4):335–45. 10.1007/s40264-015-0387-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Oetting WS, Schladt DP, Guan W, Miller MB, Remmel RP, Dorr C, et al. Genomewide association study of tacrolimus concentrations in African American kidney transplant recipients identifies multiple CYP3A5 alleles. Am J Transplant. 2016;16(2):574–82. 10.1111/ajt.13495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sanghavi K, Brundage RC, Miller MB, Schladt DP, Israni AK, Guan W, et al. Genotype-guided tacrolimus dosing in African-American kidney transplant recipients. Pharmacogenomics J. 2017;17(1):61–8. 10.1038/tpj.2015.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. The Journal of Pain. 2009;10(12):1187–204. 10.1016/j.jpain.2009.10.002 [DOI] [PubMed] [Google Scholar]
- 70.Wang D, Poi MJ, Sun X, Gaedigk A, Leeder JS, Sadee W. Common CYP2D6 polymorphisms affecting alternative splicing and transcription: long-range haplotypes with two regulatory variants modulate CYP2D6 activity. Hum Mol Genet. 2014;23(1):268–78. 10.1093/hmg/ddt417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ray B, Ozcagli E, Sadee W, Wang D. CYP2D6 haplotypes with enhancer single-nucleotide polymorphism rs5758550 and rs16947 (*2 allele): implications for CYP2D6 genotyping panels. Pharmacogenetics and genomics. 2019;29(2):39–47. 10.1097/FPC.0000000000000363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kirchheiner J, Schmidt H, Tzvetkov M, Keulen JT, Lötsch J, Roots I, et al. Pharmacokinetics of codeine and its metabolite morphine in ultra-rapid metabolizers due to CYP2D6 duplication. Pharmacogenomics J. 2007;7(4):257–65. 10.1038/sj.tpj.6500406 [DOI] [PubMed] [Google Scholar]
- 73.Gammal RS, Crews KR, Haidar CE, Hoffman JM, Baker DK, Barker PJ, et al. Pharmacogenetics for safe codeine use in sickle cell disease. Pediatrics. 2016;138(1):e20153479 10.1542/peds.2015-3479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Grosse SD, Odame I, Atrash HK, Amendah DD, Piel FB, Williams TN. Sickle cell disease in Africa: a neglected cause of early childhood mortality. Am J Prev Med. 2011;41(6 Suppl 4):S398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Solovieff N, Hartley SW, Baldwin CT, Klings ES, Gladwin MT, Taylor JG 6th, et al. Ancestry of African Americans with sickle cell disease. Blood Cells Mol Dis. 2011;47(1):41–5. 10.1016/j.bcmd.2011.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rajman I, Knapp L, Morgan T, Masimirembwa C. African Genetic Diversity: Implications for Cytochrome P450-mediated Drug Metabolism and Drug Development. EBioMedicine. 2017;17:67–74. 10.1016/j.ebiom.2017.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Teo YY, Ong RT, Sim X, Tai ES, Chia KS. Identifying candidate causal variants via trans-population fine-mapping. Genet Epidemiol. 2010;34(7):653–64. 10.1002/gepi.20522 [DOI] [PubMed] [Google Scholar]
- 78.González-Neira A, Calafell F, Navarro A, Lao O, Cann H, Comas D, et al. Geographic stratification of linkage disequilibrium: a worldwide population study in a region of chromosome 22. Human genomics. 2004;1(6):399–409. 10.1186/1479-7364-1-6-399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Teo YY, Fry AE, Bhattacharya K, Small KS, Kwiatkowski DP, Clark TG. Genome-wide comparisons of variation in linkage disequilibrium. Genome research. 2009;19(10):1849–60. 10.1101/gr.092189.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vernot B, Stergachis AB, Maurano MT, Vierstra J, Neph S, Thurman RE, et al. Personal and population genomics of human regulatory variation. Genome Res 2012;22(9):1689–97. 10.1101/gr.134890.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Campbell MC, Hirbo JB, Townsend JP, Tishkoff SA. The peopling of the African continent and the diaspora into the new world. Curr Opin Genet Dev. 2014;29:120–32. 10.1016/j.gde.2014.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hellwege JN, Keaton JM, Giri A, Gao X, Edwards DRV, Edwards TL. Population Stratification in Genetic Association Studies. Current protocols in human genetics. 2017;95:1.22.1–1..3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lambert CA, Tishkoff SA. Genetic structure in African populations: implications for human demographic history. Cold Spring Harb Symp Quant Biol. 2009;74:395–402. 10.1101/sqb.2009.74.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fan S, Kelly DE, Beltrame MH, Hansen MEB, Mallick S, Ranciaro A, et al. African evolutionary history inferred from whole genome sequence data of 44 indigenous African populations. Genome Biol. 2019;20(1):82 10.1186/s13059-019-1679-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Katoh T, Mano S, Ikuta T, Munkhbat B, Tounai K, Ando H, et al. Genetic isolates in East Asia: a study of linkage disequilibrium in the X chromosome. Am J Hum Genet. 2002;71(2):395–400. 10.1086/341608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Antunez-de-Mayolo G, Antunez-de-Mayolo A, Antunez-de-Mayolo P, Papiha SS, Hammer M, Yunis JJ, et al. Phylogenetics of worldwide human populations as determined by polymorphic Alu insertions. Electrophoresis. 2002;23(19):3346–56. [DOI] [PubMed] [Google Scholar]
- 87.Duncan G, Thomas E, Gallo JC, Baird LS, Garrison J, Herrera RJ. Human phylogenetic relationships according to the D1S80 locus. Genetica. 1996;98(3):277–87. 10.1007/bf00057592 [DOI] [PubMed] [Google Scholar]
- 88.Li JZ, Absher DM, Tang H, Southwick AM, Casto AM, Ramachandran S, et al. Worldwide human relationships inferred from genome-wide patterns of variation. Science. 2008;319(5866):1100–4. 10.1126/science.1153717 [DOI] [PubMed] [Google Scholar]
- 89.Visscher H, Ross CJ, Dubé MP, Brown AM, Phillips MS, Carleton BC, et al. Application of principal component analysis to pharmacogenomic studies in Canada. Pharmacogenomics J. 2009;9(6):362–72. 10.1038/tpj.2009.36 [DOI] [PubMed] [Google Scholar]
- 90.Tishkoff SA, Reed FA, Friedlaender FR, Ehret C, Ranciaro A, Froment A, et al. The genetic structure and history of Africans and African Americans. Science. 2009;324(5930):1035–44. 10.1126/science.1172257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Norris ET, Wang L, Conley AB, Rishishwar L, Mariño-Ramírez L, Valderrama-Aguirre A, et al. Genetic ancestry, admixture and health determinants in Latin America. BMC Genomics. 2018;19(Suppl 8):861 10.1186/s12864-018-5195-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rotimi CN, Bentley AR, Doumatey AP, Chen G, Shriner D, Adeyemo A. The genomic landscape of African populations in health and disease. Hum Mol Genet. 2017;26(R2):R225–R36. 10.1093/hmg/ddx253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wall JD, Yang MA, Jay F, Kim SK, Durand EY, Stevison LS, et al. Higher levels of neanderthal ancestry in East Asians than in Europeans. Genetics. 2013;194(1):199–209. 10.1534/genetics.112.148213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kim BY, Lohmueller KE. Selection and reduced population size cannot explain higher amounts of Neandertal ancestry in East Asian than in European human populations. American journal of human genetics. 2015;96(3):454–61. 10.1016/j.ajhg.2014.12.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Villanea FA, Schraiber JG. Multiple episodes of interbreeding between Neanderthal and modern humans. Nature ecology & evolution. 2019;3(1):39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Browning SR, Browning BL, Zhou Y, Tucci S, Akey JM. Analysis of human sequence data reveals two pulses of Archaic Denisovan admixture. Cell. 2018;173(1):53–61.e9. 10.1016/j.cell.2018.02.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Laval G, Patin E, Barreiro LB, Quintana-Murci L. Formulating a historical and demographic model of recent human evolution based on resequencing data from noncoding regions. PloS one. 2010;5(4):e10284 10.1371/journal.pone.0010284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Xu S. Human population admixture in Asia. Genomics Inform. 2012;10(3):133–44. 10.5808/GI.2012.10.3.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Visscher PM, Wray NR, Zhang Q, Sklar P, McCarthy MI, Brown MA, et al. 10 Years of GWAS Discovery: Biology, Function, and Translation. American journal of human genetics. 2017;101(1):5–22. 10.1016/j.ajhg.2017.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.VanLiere JM, Rosenberg NA. Mathematical properties of the r2 measure of linkage disequilibrium. Theor Popul Biol. 2008;74(1):130–7. 10.1016/j.tpb.2008.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shifman S, Kuypers J, Kokoris M, Yakir B, Darvasi A. Linkage disequilibrium patterns of the human genome across populations. Hum Mol Genet. 2003;12(7):771–6. 10.1093/hmg/ddg088 [DOI] [PubMed] [Google Scholar]
- 102.Pittman AM, Myers AJ, Abou-Sleiman P, Fung HC, Kaleem M, Marlowe L, et al. Linkage disequilibrium fine mapping and haplotype association analysis of the tau gene in progressive supranuclear palsy and corticobasal degeneration. J Med Genet. 2005;42:837–46. 10.1136/jmg.2005.031377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wray NR. Allele frequencies and the r2 measure of linkage disequilibrium impact on design and interpretation of association studies. Twin Research and Human Genetics. 2005;8(2):87–94. 10.1375/1832427053738827 [DOI] [PubMed] [Google Scholar]
- 104.Rotimi CN, Tekola-Ayele F, Baker JL, Shriner D. The African diaspora: history, adaptation and health. Curr Opin Genet Dev. 2016;41:77–84. 10.1016/j.gde.2016.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Montinaro F, Busby GB, Pascali VL, Myers S, Hellenthal G, Capelli C. Unravelling the hidden ancestry of American admixed populations. Nat Commun. 2015;6:6596 10.1038/ncomms7596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ruiz-Linares A, Adhikari K, Acuña-Alonzo V, Quinto-Sanchez M, Jaramillo C, Arias W, et al. Admixture in Latin America: geographic structure, phenotypic diversity and self-perception of ancestry based on 7,342 individuals. PLoS Genet. 2014;10(9):e1004572 10.1371/journal.pgen.1004572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Homburger JR, Moreno-Estrada A, Gignoux CR, Nelson D, Sanchez E, Ortiz-Tello P, et al. Genomic insights into the ancestry and demographic history of South America. PLoS Genet. 2015;11(12):e1005602 10.1371/journal.pgen.1005602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Salzano FM, Sans M. Interethnic admixture and the evolution of Latin American populations. Genet Mol Biol. 2014;37(1 Suppl):151–70. 10.1590/s1415-47572014000200003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hofer T, Ray N, Wegmann D, Excoffier L. Large allele frequency differences between human continental groups are more likely to have occurred by drift during range expansions than by selection. Ann Hum Genet. 2009;73(1):95–108. 10.1111/j.1469-1809.2008.00489.x [DOI] [PubMed] [Google Scholar]
- 110.Li J, Zhang L, Zhou H, Stoneking M, Tang K. Global patterns of genetic diversity and signals of natural selection for human ADME genes. Hum Mol Genet. 2011;20(3):528–40. 10.1093/hmg/ddq498 [DOI] [PubMed] [Google Scholar]
- 111.Mustafina OE, Tuktarova IA, Karimov DD, Somova Rs, Nasibullin TR. CYP2D6, CYP3A5, and CYP3A4 gene polymorphism in Russian, Tatar, and Bashkir populations. Genetika. 2015;51(1):109–19. [PubMed] [Google Scholar]
- 112.Khan A, Tian L, Zhang C, Yuan K, Xu S. Genetic diversity and natural selection footprints of the glycine amidinotransferase gene in various human populations. Scientific Reports. 2016;6:18755 10.1038/srep18755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Reich D, Thangaraj K, Patterson N, Price AL, Singh L. Reconstructing Indian population history. Nature. 2009;461(7263):489–94. 10.1038/nature08365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Manoharan I, Wieseler S, Layer PG, Lockridge O, Boopathy R. Naturally occurring mutation Leu307Pro of human butyrylcholinesterase in the Vysya community of India. Pharmacogenetics and genomics. 2006;16(7):461–8. 10.1097/01.fpc.0000197464.37211.77 [DOI] [PubMed] [Google Scholar]
- 115.David SM, Venkatesan SK, Boopathy R. An Indian butyrylcholinesterase variant L307P is not structurally stable: a molecular dynamics simulation study. Chem Biol Interact. 2013;203(1):30–5. 10.1016/j.cbi.2012.10.010 [DOI] [PubMed] [Google Scholar]
- 116.Çokuğraş AN. Butyrylcholinesterase: structure and physiological importance. Turk J Biochem. 2003;28(2):54–61. [Google Scholar]
- 117.Zencirci B. Pseudocholinesterase enzyme deficiency: a case series and review of the literature. Cases J. 2009;2:9148 10.1186/1757-1626-2-9148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nagar SD, Moreno AM, Norris ET, Rishishwar L, Conley AB, O'Neal KL, et al. Population pharmacogenomics for precision public health in Colombia. Front Genet. 2019;10:241 10.3389/fgene.2019.00241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Thummel KE, Lin YS. Sources of interindividual variability. Methods Mol Biol. 2014;1113:363–415. 10.1007/978-1-62703-758-7_17 [DOI] [PubMed] [Google Scholar]
- 120.Ivanov M, Kacevska M, Ingelman-Sundberg M. Epigenomics and interindividual differences in drug response. Clin Pharmacol Ther. 2012;92(6):727–36. 10.1038/clpt.2012.152 [DOI] [PubMed] [Google Scholar]
- 121.Glasspool RM, Teodoridis JM, Brown R. Epigenetics as a mechanism driving polygenic clinical drug resistance. Br J Cancer. 2006;94(8):1087–92. 10.1038/sj.bjc.6603024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Losi L, Fonda S, Saponaro S, Chelbi ST, Lancellotti C, Gozzi G, et al. Distinct DNA methylation profiles in ovarian tumors: opportunities for novel biomarkers. Int J Mol Sci. 2018;19(6):pii: E1559 10.3390/ijms19061559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bahar MA, Setiawan D, Hak E, Wilffert B. Pharmacogenetics of drug-drug interaction and drug-drug-gene interaction: a systematic review on CYP2C9, CYP2C19 and CYP2D6. Pharmacogenomics. 2017;18(7):701–39. 10.2217/pgs-2017-0194 [DOI] [PubMed] [Google Scholar]
- 124.Knisely MR, Carpenter JS, Draucker CB, Skaar T, Broome ME, Holmes AM, et al. CYP2D6 drug-gene and drug-drug-gene interactions among patients prescribed pharmacogenetically actionable opioids. Appl Nurs Res. 2017;38:107–10. 10.1016/j.apnr.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gross T, Daniel J. Overview of pharmacogenomic testing in clinical practice. Ment Health Clin. 2018;8(5):235–41. 10.9740/mhc.2018.09.235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Moaddeb J, Haga SB. Pharmacogenetic testing: Current Evidence of Clinical Utility. Ther Adv Drug Saf. 2013;4(4):155–69. 10.1177/2042098613485595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lee YF, Kwok RCC, Wong ICK, Lui VWY. The Pharmacogenomic Era in Asia: Potential Roles and Challenges for Asian Pharmacists J Pharmacogenomics Pharmacoproteomics. 2017;8(1):1000164. [Google Scholar]
- 128.Yang Y, Peter I, Scott SA. Pharmacogenetics in Jewish populations. Drug Metabol Drug Interact. 2014;29(4):221–33. 10.1515/dmdi-2013-0069 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(PDF)
(DOC)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.