Abstract
Background
The evidence of tapered methadone's efficacy in managing opioid withdrawal has been systematically evaluated in the previous version of this review that needs to be updated
Objectives
To evaluate the effectiveness of tapered methadone compared with other detoxification treatments and placebo in managing opioid withdrawal on completion of detoxification and relapse rate.
Search methods
We searched: Cochrane Central Register of Controlled Trials (The Cochrane Library 2012, Issue 4), PubMed (January 1966 to May 2012), EMBASE (January 1988 to May 2012), CINAHL (2003‐ December 2007), PsycINFO (January 1985 to December 2004), reference lists of articles.
Selection criteria
All randomised controlled trials that focused on the use of tapered methadone versus all other pharmacological detoxification treatments or placebo for the treatment of opiate withdrawal.
Data collection and analysis
Two review authors assessed the included studies. Any doubts about how to rate the studies were resolved by discussion with a third review author. Study quality was assessed according to the criteria indicated in the Cochrane Handbook for Systematic Reviews of Interventions.
Main results
Twenty‐three trials involving 2467 people were included. Comparing methadone versus any other pharmacological treatment, we observed no clinical difference between the two treatments in terms of completion of treatment, 16 studies 1381 participants, risk ratio (RR) 1.08 (95% confidence interval (CI) 0.97 to 1.21); number of participants abstinent at follow‐up, three studies, 386 participants RR 0.98 (95% CI 0.70 to 1.37); degree of discomfort for withdrawal symptoms and adverse events, although it was impossible to pool data for the last two outcomes. These results were confirmed also when we considered the single comparisons: methadone with: adrenergic agonists (11 studies), other opioid agonists (eight studies), anxiolytic (two studies), paiduyangsheng (one study). Comparing methadone with placebo (two studies) more severe withdrawal and more drop‐outs were found in the placebo group. The results indicate that the medications used in the included studies are similar in terms of overall effectiveness, although symptoms experienced by participants differed according to the medication used and the program adopted.
Authors' conclusions
Data from literature are hardly comparable; programs vary widely with regard to the assessment of outcome measures, impairing the application of meta‐analysis. The studies included in this review confirm that slow tapering with temporary substitution of long‐ acting opioids, can reduce withdrawal severity. Nevertheless, the majority of patients relapsed to heroin use.
Keywords: Humans, Methadone, Methadone/administration & dosage, Narcotics, Narcotics/administration & dosage, Narcotics/adverse effects, Opiate Substitution Treatment, Opiate Substitution Treatment/methods, Opioid‐Related Disorders, Opioid‐Related Disorders/rehabilitation, Randomized Controlled Trials as Topic, Substance Withdrawal Syndrome, Substance Withdrawal Syndrome/rehabilitation
Plain language summary
Methadone at tapered doses for the management of opioid withdrawal
Abuse of opioid drugs and dependence on them causes major health and social issues that include transmission of HIV and hepatitis C with injection, increased crime and costs for health care and law enforcement, family disruption and lost productivity. Addicts, particularly those aged 15 to 34 years, are also at higher risk of death. Managed withdrawal (or detoxification) is used as the first step in treatment. Withdrawal symptoms include anxiety, chills, muscle pain (myalgia) and weakness, tremor, lethargy and drowsiness, restlessness and irritability, nausea and vomiting and diarrhoea. Persisting sleep disturbances and drug craving can continue for weeks and months after detoxification and often lead to a return to opioid use. The number of addicts who complete detoxification tends to be low, and rates of relapse are high. For a tapered dose treatment to reduce withdrawal symptoms, illicit opioids are replaced by methadone or another agent using decreasing doses up to 30 days under medical supervision. The review authors searched the medical literature and identified 23 controlled trials involving 2467 adult opioid users in various countries. Trial participants were randomised to receive methadone or another pharmacological treatment. The other treatments were adrenergic agonists such as lofexidine, partial opioid agonists such as buprenorphine, opioid agonists such as LAAM (levo‐α‐acetyl‐methadol) and the anxiolytics chlordiazepoxide and buspirone. In the two studies that compared methadone with placebo, withdrawal symptoms were more severe and more people dropped out in the placebo group.
The studies included in this review confirmed that slow tapering with temporary substitution of long‐ acting opioids, could reduce withdrawal severity. Nevertheless, the majority of patients relapsed to heroin use. The medications used in the included studies were similar in terms of overall effectiveness, although symptoms experienced by participants differed according to the medication used and the program adopted.
The programs varied widely with regard to the assessment of outcome measures. Seventeen of the included trials were conducted in inpatient settings.
Summary of findings
Summary of findings for the main comparison. Tapered methadone versus any other treatment for the management of opioid withdrawal.
| Tapered methadone versus any other treatment for the management of opioid withdrawal | ||||||
| Patient or population: patients with the management of opioid withdrawal Settings: Inpatient and outpatient Intervention: Tapered methadone versus any other treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Tapered methadone versus any other treatment | |||||
| Completion of treatment Objective Follow‐up: mean 30 days | Study population | RR 1.08 (0.97 to 1.21) | 1381 (16 studies) | ⊕⊕⊕⊕ high | ||
| 547 per 1000 | 591 per 1000 (531 to 662) | |||||
| Moderate | ||||||
| 505 per 1000 | 545 per 1000 (490 to 611) | |||||
| Number of participants abstinent at follow‐up Objective Follow‐up: mean 1.5 months | Study population | RR 0.98 (0.7 to 1.37) | 386 (3 studies) | ⊕⊕⊕⊕ high | ||
| 255 per 1000 | 250 per 1000 (179 to 350) | |||||
| Moderate | ||||||
| 267 per 1000 | 262 per 1000 (187 to 366) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Background
Description of the condition
Recent figures for illicit drug use indicate that the prevalence of opiate abuse among persons from 15 to 64 years old is around 0.5% in most Western countries (EU, USA, Canada and Australia) (UNODC 2011). Opioid dependence is a worldwide health problem that has enormous economic, personal and public health consequences. There are an estimated 15.6 million illicit opioid users in the world, of whom 11 million use heroin (UNODC 2011). Opioids are the main drugs of abuse in Asia, Europe and much of Oceania, and it is estimated that globally the consumption of the opioid class of drugs is increasing (UNODC 2011).
In Europe heroin is still one of the main illegal substance recorded in indicators of problem drug use (EMCDDA 2011). Recent national estimates vary between one and eight cases per 1000 population aged 15–64 (EMCDDA 2011). The average prevalence of problem opioid use in the European Union and Norway, computed from national studies, is estimated to be between 3.6 and 4.4 cases per 1000 population aged 15–64 (EMCDDA 2011). The latest US data, show that, on average, three persons per 100 annual drug users had to undergo treatment for drug use in 2008. Opiates use is far more problematic than the use of other illicit drugs (UNODC 2011). Australia has an estimated 67,000–92,000 illicit heroin users (540–750 per 100,000 population aged 15 to 64) (Hall 1999).
Opioids, mainly heroin, were cited as the primary drug for entering treatment by around 216,000 or 51 % of all those reported entering specialist drug treatment in 29 European countries in 2009. The provision of treatment is central to the reduction of the harms to the individual and the community from opioid dependence.
The effect of chronic opioid exposure on opioid receptor levels has not been well‐defined in humans. Tolerance develops through multiple mechanisms, including an acute desensitisation of the opioid receptor (which develops within minutes of opioid use and resolves within hours after use), and a long‐term desensitisation of the opioid receptor (which persists for several days after removal of opioid agonists). Changes also occur in the number of opioid receptors (Williams 2001), and there is compensatory up‐regulation of the cyclic adenosine monophosphate (cAMP) producing enzymes. When the opioid is withdrawn, the cAMP cascade becomes overactive, leading to the “noradrenergic storm” seen clinically as opioid withdrawal, which may create a drive to reinstate substance use. The intensely dysphoric withdrawal syndrome is characterised by watery eyes, runny nose, yawning, sweating, restlessness, irritability, tremor, nausea, vomiting, diarrhoea, increased blood pressure, chills, cramps and muscles aches that can last seven days or even longer.
Description of the intervention
Treatment of opioid dependence is a set of pharmacological and psychosocial interventions aimed at reducing or ceasing opioid use, preventing future harms associated with opioid use, improving quality of life and well‐being of the opioid‐dependent patient. Opioid withdrawal can be managed by controlling the rate of cessation of opioids and by providing medication that relieves symptoms, or by a combination of the two. Methadone at adequate doses prevents or reverses withdrawal symptoms (Ward 1992), and thus reduces the need to use illegal heroin (Jaffe 1990). Methadone remains effective for approximately 24 hours, requiring a single daily dose rather than the more frequent administration of three to four times daily that occurs with the shorter‐acting heroin (Jaffe 1990).
How the intervention might work
Methadone can "block" the euphoric effects of heroin, discouraging illicit use and thereby relieving the user of the need or desire to seek heroin (Dole 1969). This allows the opportunity to engage in normative activities, and "rehabilitation" if necessary. Methadone can cause death in overdosage, like other similar medications such as morphine, and for this reason it is a treatment which is dispensed under medical supervision and relatively strict rules. In summary, methadone is a long‐acting opioid analgesic with well‐understood pharmacological characteristics, which make it suitable for stabilising opioid‐dependent patients in a maintenance treatment approach. Methadone was first used to treat heroin dependence as a tapering agent in US facilities after the second world war and had been introduced in the treatment of opioid dependence for maintenance purposes rather than detoxification until the 1960's. Even though now it is often used for detoxification, sometimes this occurs for economical reasons, sometimes for ideological ones. Despite the risk of relapse being high, detoxification with methadone is common in many countries. The upper limit of duration of the tapered methadone withdrawal period appears to be relatively arbitrary; a period of three to four weeks has been recommended and used in clinical practice (Gossop 1987).
Why it is important to do this review
Different pharmacological agents have been used as detoxification agents to ameliorate withdrawal symptoms, however, the rate of completion of detoxification tends to be low, and rates of relapse to opioid use following detoxification are high (Gossop 1989B; Valliant 1988). The present review focuses on detoxification from illicit opiate use through the use of tapered methadone.There are no systematic reviews already published on the effectiveness of methadone at tapered doses on completion of detoxification or relapse rate.
The previous version of this review was published in 2005 and an update is required.
Objectives
To assess the effectiveness of methadone at tapered doses versus placebo or other pharmacological treatments for the management of detoxification on completion and acceptability of the treatment and relapse rate.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials (RCTs) and controlled clinical trials (CCTs) on tapered methadone treatment (maximum 30 days) to manage withdrawal from opiates.
Types of participants
Opioid users enrolled in short‐term tapered methadone treatment to manage withdrawal from heroin or methadone or buprenorphine, no matter what the characteristic of the setting.Trials including patients with additional diagnoses such as benzodiazepine dependence were also eligible. Pregnant women, newborn infants with neonatal dependence and people with iatrogenic dependence (e.g. through treatment of chronic pain) were excluded. The absence in these patient groups of social and psychological factors that underlie opioid dependence makes for a substantially different approach to clinical management. This was the basis for excluding these groups from this review (Gowing 2008).
Types of interventions
Experimental Intervention
Methadone aimed at the detoxification from opiates, maximum length of treatment: 30 days
Control Interventions
Other opioid agonists (LAAM (levo‐α‐acetyl‐methadol), Buprenorphine, propoxyphene, etc).
Adrenergic agonists (clonidine, lofexidine, guanfacine).
Opioid antagonists (naltrexone, naloxone).
Placebo.
All aimed at the detoxification from opiate.
The setting in which withdrawal occurs is a factor that can be expected to influence outcomes. The degree of its effect has been explored by examining rate of completion of withdrawal.
Types of outcome measures
Primary outcomes
Completion of treatment as number of participants completing the detoxification program.
Acceptability of the treatment as a) duration and severity of signs and symptoms of withdrawal, including patient self‐rating, b) side effects.
Results at follow‐up as (a) number of participants abstinent at follow‐up, (b) naloxone challenge.
Secondary outcomes
Use of primary substance of abuse as a) number of participants who referred to the use of opioid during the treatment, b) number of participants with urine samples positive for opiate.
Different factors were considered as confounders and taken into account in the analysis wherever possible: setting ( inpatient or outpatient treatment); starting methadone dose/rate and pattern of dose reduction; scheduled duration of treatment; severity of dependence (duration of use, route of administration, frequency of assumption); health status; other treatment offered (psychosocial support); social status; number of previous treatment attempts and previous treatment outcomes.
Search methods for identification of studies
Electronic searches
We identified relevant studies that met the predefined inclusion criteria by searching the following sources from the earliest available date to December 2007. Relevant trials were obtained from the following sources:
Cochrane Central Register of Controlled Trials (The Cochrane Library 2012, Issue 4) which include the Cochrane Drugs and Alcohol Group's Register of Trials.
PubMed (from 2003 ‐ May 2012).
EMBASE (from 2003 ‐ May 2012).
CINAHL (from 2003 ‐ December 2011).
PsycINFO (January 1985 to December 2004).
To see the search strategies seeAppendix 1; Appendix 2; Appendix 3; Appendix 4.
There were no language or publication year restriction.
Searching other resources
We also searched:
Reference lists of all relevant papers to identify further studies.
Some of the main electronic sources of ongoing trials (meta‐Register of Controlled Trials; Clinical Trials.gov).
Conference proceedings likely to contain trials relevant to the review (College on Problems of Drug Dependence ‐CPDD).
National focal points for drug research (e.g., National Institute of Drug Abuse (NIDA), National Drug & Alcohol Research Centre (NDARC).
We contacted authors of included studies and experts in the field in various countries to find out if they know any other published or unpublished controlled trials
Data collection and analysis
Selection of studies
One review author (Amato) inspected the search hits by reading the titles and the abstracts. We obtained each potentially relevant study located in the search in full text and two review authors (Amato, Minozzi) independently assessed for inclusion. Doubts were resolved by discussion between the review authors.
Data extraction and management
Two review authors (Amato, Minozzi) independently extracted data from published sources using a data extraction form. Where differences in data extracted occurred this was resolved through discussion. Study quality was assessed by Silvia Minozzi according to the criteria indicated in Cochrane Handbook for Systematic Reviews of Interventions 4.2. (Higgins 2008)
Assessment of risk of bias in included studies
The risk of bias assessment for RCTs and CCTs in this review were performed using the five criteria recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). The recommended approach for assessing risk of bias in studies included in Cochrane reviews is a two‐part tool, addressing five specific domains (namely sequence generation, allocation concealment, blinding, incomplete outcome data, and other issues). The first part of the tool involves describing what was reported to have happened in the study. The second part of the tool involves assigning a judgement relating to the risk of bias for that entry. This is achieved by answering a pre‐specified question about the adequacy of the study in relation to the entry, such that a judgement of "Yes" indicates low risk of bias, "No" indicates high risk of bias, and "Unclear" indicates unclear or unknown risk of bias. To make these judgments we used the criteria indicated by the handbook adapted to the addiction field.
Blinding of participants, personnel and outcome assessor (avoidance of performance bias and detection bias) were considered separately for objective outcomes (e.g. drop‐out, use of substance of abuse measured by urinalysis, participants relapsed at the end of follow‐up, participants engaged in further treatments) and subjective outcomes (e.g. duration and severity of signs and symptoms of withdrawal, patient self‐reported use of substance, side effects, social functioning as integration at school or at work, family relationship).
Incomplete outcome data (avoidance of attrition bias) were considered for all outcomes except for the drop‐out from the treatment, which is very often the primary outcome measure in trials on addiction. It was assessed separately for results at the end of the study period and for results at follow‐up.
Grading of evidence
The quality of evidence was assessed according to a systematic and explicit method (Guyatt 2008). In order to indicate the extent to which one can be confident that an estimate of effect is correct, judgments about the quality of evidence are made for each comparison and outcome. These judgments consider study design (RCT, quasi‐RCT or observational study), study quality (detailed study design and execution), consistency of results (similarity of estimates of effect across studies), precision of estimates, and directness (the extent to which people, interventions and outcome measures are similar to those of interest). The following definitions in grading the quality of evidence for each outcome are used: High: further research is very unlikely to change our confidence in the estimate of effect. Moderate: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low: further research is very likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Very low: any estimate of effect is very uncertain.
Measures of treatment effect
We compared the treatment and control groups for outcomes at post‐test and at different follow‐up times. Post‐intervention data were collected immediately after the intervention ended. For continuous data it was not possible to pool data due to the heterogeneity of reporting in the included studies.
Dealing with missing data
Statisticians often use the terms ‘missing at random’, and ‘not missing at random’ to represent different scenarios. Data are said to be ‘missing at random’ if the fact that they are missing is unrelated to actual values of the missing data. Data are said to be ‘not missing at random’ if the fact that they are missing is related to the actual missing data. In cases where we assumed that data were missing at random, we analysed only the available data. If we assumed that the data were not missing at random, we planned to impute the missing data with replacement values, and to treat these as if they were observed. We planned to do this in different ways and compare the results (e.g. last observation carried forward, imputing an assumed outcome such as assuming all were poor outcomes, imputing the mean, imputing based on predicted values from a regression analysis). For the included studies in this review we did not impute data.
Assessment of heterogeneity
Statistically significant heterogeneity among primary outcome studies was assessed with Chi2 (Q) test and I2 (Higgins 2003). A significant Q ( P <.05) and I‐squared of at least 50% was considered as statistical heterogeneity.
Assessment of reporting biases
We used funnel plots for information about possible publication bias. But asymmetric funnel plots are not necessarily caused by publication bias (and publication bias does not necessarily cause asymmetry in a funnel plot). Whenever asymmetry was present, likely reasons were explored.
Data synthesis
Dichotomous outcomes (completion of treatment, number of participants with negative urinalysis) were analysed calculating the risk ratio (RR) for each trial with the uncertainty in each result being expressed by their confidence intervals (CIs). The RRs from the individual trials were combined through meta‐analysis where possible (comparability of intervention between trials) using a random‐effects model. The completion of the treatment was reported as the number of patients who completed the detoxification program. The use of primary substance was reported as the number of participants with consecutive negative urinalysis. The results at follow‐up were reported as the number of participants abstinent at the follow‐up interview (range of follow‐up period: one to six months). We used the Chi2 test to determine the heterogeneity of the results. A P value of the Chi2 test less than 0.005 indicated a significant heterogeneity.
Sensitivity analysis
The following sensitivity analyses were planned a priori: Generation of allocation sequence, concealment of allocation, blinding of patients and providers, blinding of assessors, incomplete outcome data addressed, selective reporting, and other bias.
Results
Description of studies
Results of the search
The literature searching process resulted in the identification of 8545 reports (6860 after duplicates removed), 6754 were excluded on the basis of title and abstract, 106 were retrieved in full text; 74 have been excluded and 23 (32 references) included, 17 studies included in quantitative synthesis (meta‐analysis). SeeFigure 1
1.

Flow chart of studies
Included studies
Twenty‐three studies (32 reports) meet the inclusion criteria for this review seeCharacteristics of included studies.
Duration of trials: range three to 30 days. Treatment regimens and setting: The countries in which the 23 studies were conducted are: USA (six studies), United Kingdom (five studies), Spain (four studies), China, Irane and Germany (two studies each), Austria and Italy (one study each). Eighteen trials were conducted with inpatients, five with outpatients. Information on methadone doses were available for 19 of the 23 included studies. The mean starting dose of methadone was 29 mg/day (range 15 to 60). The other four studies reported that the starting doses of methadone were variable, tailored on individual body weight or heroin consumption in the previous month.
Participants: 2467 opiate addicts. Age range was 18 to 70 years; one study (Howells 2002) did not report age characteristics only that participants were required to be under 55 years old.
Comparisons: In the 23 studies included in the review, tapered methadone was compared with the following.
Tapered methadone versus any other treatments: 23 studies, 2467 participants.
Tapered methadone versus adrenergic agonists: 11 studies, (Bearn 1996; Camí 1985; Dawe 1995; Gerra 2000; Howells 2002; Jiang 1993; Kleber 1985; San 1990; San 1994; Umbricht 2003; Washton 1981), 952 participants.
Tapered methadone versus other opioid agonists: eight studies, (Madlung‐Kratzer 2009; Seifert 2002; Sorensen 1982; Steinmann 2007;Tennant 1975; Umbricht 2003; Wright 2011; Zarghami 2012), 869 participants.
Tapered methadone versus anxiolytic: two studies (Buydens‐Branchey 2005; Drummond 1989), 47 participants.
Tapered methadone versus placebo: two studies (Buydens‐Branchey 2005; San 1992), 38 participants.
Tapered methadone versus paiduyangsheng: one study (Yang 2006), 580 participants.
One study (Umbricht 2003) has three arms, comparing methadone (arm 1) with buprenorphine (arm 2) and with clonidine (arm 3). For this study the participants in the methadone arm (21 people) are considered both in the comparison with adrenergic agonists and in the comparison with other opioid agonists. Another study (Buydens‐Branchey 2005) has four arms comparing methadone (arm 1) with placebo (arm 2), buspirone 30 mg (arm 3), buspirone 45 mg (arm 4). For this study the participants in the methadone arm (eight people) are considered in all the comparisons.
Two studies (Gerra 2000; San 1994) had three arms comparing methadone with different dosages of adrenergic agonist. For these studies we summarised the results of the two different dosages of adrenergic agonists. One study (San 1990) compared methadone with two different adrenergic agonists and we summarised the results of the two different adrenergic agonists.
Outcomes: Outcomes were either dichotomous or continuous, as reported by authors. The following principal outcomes were considered by the authors.
Completion of treatment as number of participants completing the detoxification program (16/23 studies).
Withdrawal scores (21/23 studies).
Side effects (16/23 studies).
Use of primary substance measured as number of opiate positive urine samples (3/23 studies).
Results at follow‐up as (a) number of participants abstinent at follow‐up (4/23 studies) and (b) naloxone challenge (2/23 studies).
Scales The 23 studies that used withdrawal scales to assess withdrawal symptoms used 22 different scales (see Table 2 ), of which 15 were published. Furthermore, four studies considered craving using four different methods to assess it: Craving questionnaire (Dawe 1995), Craving Scale (Gerra 2000), Severity of Dependence Scale (SDS) (Howells 2002) and Addiction Severity Index ( Kleber 1985). Five studies use questionnaires to assess psychological and behavioural characteristics: State Trait Anxiety Inventory (Camí 1985; San 1990; San 1994), Beck Depression Inventory (Kleber 1985, San 1994), Eysenck Personality Questionnaire (San 1994), Hamilton Anxiety Rating Scale (Yang 2006) Profile of Mood State (San 1990), Hospital Anxiety Depression (San 1994). One study used an Intelligence Quotient test: Wechsler Adult Intelligence Scale (San 1990).
1. Withdrawal scales.
| Author | Name of Scale | Published | n° items | n° scores |
| Bearn 1996 | Short Opiate Withdrawal Scale (Gossop 1990) | yes | 10 | 4 |
| Buydens‐Branchey 2005 | Subjective Opiate Withdrawal Scale (Handelsman 1987) | yes | 16 | 5 |
| Buydens‐Branchey 2005 | Objective Opiate Withdrawal Scale (Handelsman 1987) | yes | 13 | 3 |
| Camí 1985 | Abstinence Rating Scale | no | 17 | present/absent |
| Dawe 1995 | Symptom Checklist (Powell 1990) | yes | 10 | 4 |
| Drummond 1989 | Subjective Measures Questionnaire | no | 16 | not reported |
| Drummond 1989 | Objective Opiate Withdrawal Scale (Himmelsbach 1942) | yes | 10 | 4 |
| Gerra 2000 | List of Withdrawal Symptoms (Gerra 1995) | yes | 9 | 5 |
| Howells 2002 | Withdrawal Problem Scale (Gossop 1990) | yes | 20 | 4 |
| Howells 2002 | Short Opiate Withdrawal Scale (Gossop 1990) | yes | 8 | 4 |
| Jiang 1993 | Himmelsbach Drug Withdrawal Symptoms Assessment Chart (Himmelsbach 1941) | yes | 14 | 3 |
| Kleber 1985 | Himmelsbach Drug Withdrawal Symptoms Assessment Chart (Himmelsbach 1941) | yes | 14 | 3 |
| Kleber 1985 | Self Rated Withdrawal Scale (Haertzen 1968) | yes | 32 | 4 |
| Kleber 1985 | Observer rating scale (Kolb 1938) | yes | 10 | 3 |
| Madlung‐Kratzer 2009 | Short OpioidWithdrawal Scale [German version] (Gossop 1990) | yes | 12 | 4 |
| Salehi 2007 | Short Opioid Withdrawal Scale (Gossop 1990) | yes | 16 | 4 |
| San 1990 | Daily Abstinence Rating Scale | no | 21 | present/absent |
| San 1990 | Abstinence Signs | no | 11 | not reported |
| San 1990 | Abstinence Symptoms | no | 10 | not reported |
| San 1992 | Opiate Withdrawal Checklist (Schubert 1984) | yes | 21 | 3 |
| San 1994 | Opiate Withdrawal Checklist (Schubert 1984) | yes | 21 | 3 |
| San 1994 | Opiate Withdrawal Syndrome (Bradley 1987) | yes | not reported | 11 |
| Seifert 2002 | Short Opiate Witdrawal Scale (Gossop 1990) | yes | not reported | not reported |
| Sorensen 1982 | Detoxification Symptom Scale (Fulwiler 1979) | yes | 20 | not reported |
| Steinmann 2007 | Clinical Opiate Withdrawal Scale (Wesson 2003) | yes | 11 | not reported |
| Steinmann 2007 | Witdrawal Syndrome Scale | no | 24 | 4 |
| Tennant 1975 | Himmelsbach Drug Withdrawal Symptoms Assessment Chart (Himmelsbach 1941) | yes | 14 | 3 |
| Umbricht 2003 | Short Opiate Withdrawal Scale (Gossop 1990) | yes | 10 | 4 |
| Umbricht 2003 | Observer Opioid Withdrawal Scale (Peachey 1988) | yes | 11 | not reported |
| Yang 2006 | Opiate Withdrawal Scale | no | not reported | 4 |
| Zarghami 2012 | Objective Opioid Withdrawal Scale (Handelsman 1987) | yes | 13 | 3 |
Excluded studies
Seventhy‐four studies did not meet the criteria for inclusion in this review. The grounds for exclusion were: type of intervention: 39 studies; study design: 29 studies; study design and type of intervention: three studies; type of participants:one study; type of intervention and type of participants: one study, type of intervention and type of outcomes: one study; seeCharacteristics of excluded studies
Risk of bias in included studies
Overall the quality of the included studies was good, see Figure 2; Figure 3. Below the results of the single risk of bias are considered.
2.
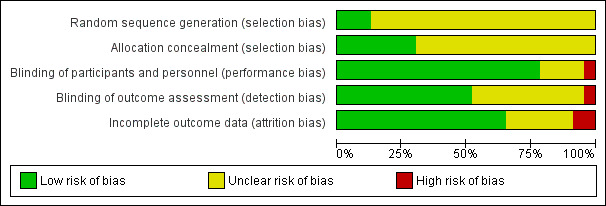
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
Random Sequence Generation: three studies (Madlung‐Kratzer 2009; Sorensen 1982; Wright 2011) were judged at low risk of selection bias because the investigators described a random component in the sequence generation process. The other 20 studies were judged as having an unclear risk of bias because there was insufficient information about the sequence generation process to permit judgement.
Allocation concealment: seven studies (Drummond 1989; Howells 2002; Madlung‐Kratzer 2009; San 1992; San 1994; Sorensen 1982; Wright 2011) were judged at low risk of selection bias because investigators enrolling participants could not foresee assignment and the method of allocation concealment was described. The other 16 studies were judged at unclear risk because they did not describe the method of concealment or did not describe it in sufficient detail to allow a definite judgement.
Blinding
Blinding of participants and personnel: 18 studies (Bearn 1996; Buydens‐Branchey 2005; Camí 1985; Dawe 1995; Drummond 1989; Howells 2002; Kleber 1985; Madlung‐Kratzer 2009; Salehi 2007; San 1990; San 1992; Seifert 2002; Sorensen 1982; Tennant 1975; Umbricht 2003; Washton 1981; Wright 2011; Yang 2006) were judged to be at low risk of performance bias because participants and providers were blinded and it was unlikely that the blinding could have been broken. One study (Gerra 2000) was judged at high risk of bias because it was not blinded and the remaining four studies (Jiang 1993; San 1994; Steinmann 2007; Zarghami 2012) were judged at unclear risk because it was not clear if a blinding condition had been undertaken.
Blinding of outcomes assessor: 12 studies (Bearn 1996; Buydens‐Branchey 2005; Camí 1985; Howells 2002; Kleber 1985; Salehi 2007; San 1990; San 1992; Sorensen 1982; Washton 1981; Wright 2011; Yang 2006) were judged at low risk of detection bias because it was specified that the outcome assessor was blinded. One study (Gerra 2000) was judged at high risk of bias because there was no blinding of outcome assessment. The remaining 10 studies were judged as having an unclear risk of bias because it was not clear if the outcome assessor was blind to treatment allocation.
Incomplete outcome data
Fiftheen studies (Bearn 1996; Camí 1985; Drummond 1989; Gerra 2000; Madlung‐Kratzer 2009; Salehi 2007; San 1990; San 1992; San 1994; Seifert 2002; Steinmann 2007; Tennant 1975; Umbricht 2003; Washton 1981; Wright 2011) were judged at low risk of attrition bias because all randomised patients were reported/analysed in the group to which they were allocated by randomisation, irrespective of non‐compliance and co‐interventions (intention‐to‐treat) or had no missing outcome data. Two studies (Buydens‐Branchey 2005; Zarghami 2012) were judged at high risk and the remaining six studies were judged at unclear risk.
Nevertheless, many outcomes could not be summarised because they were presented in graphical form or only provided statistical tests and P values. For most of the continuous variables standard deviation was not provided. Furthermore, the authors used different scales to compare the same or very similar outcomes and this makes it impossible to compare them. In particular for the outcomes which we considered as possible confounders such as setting, starting methadone dose, severity of dependence, health status etc. and for others for example, patients' motivation at enrolment, it was not possible to perform statistical analysis because many authors did not report the relevant data and, were these were available, the data were heterogeneously reported.
Effects of interventions
See: Table 1
The results were summarised, with comparison of quantitative data where possible, first for methadone versus any other treatment and then comparing separately methadone versus single different treatments.
1. Tapered methadone versus any other pharmacological treatment
1.1 Completion of treatment
Sixteen studies (Bearn 1996; Buydens‐Branchey 2005; Drummond 1989; Howells 2002; Kleber 1985; Madlung‐Kratzer 2009; Salehi 2007; San 1990; San 1994; Seifert 2002; Sorensen 1982; Steinmann 2007; Tennant 1975; Umbricht 2003; Washton 1981; Wright 2011), 1381 participants risk ratio (RR) 1.08 (95% confidence interval (CI) 0.97 to 1.21); the difference was not statistically significant, seeFigure 4 or Analysis 1.1,
4.

Forest plot of comparison: 1 Tapered methadone versus any other treatment, outcome: 1.1 Completion of treatment.
1.1. Analysis.

Comparison 1 Tapered methadone versus any other treatment, Outcome 1 Completion of treatment.
1.2 Results at follow‐up as number of participants abstinent at follow‐up
Three studies (Kleber 1985; Tennant 1975; Wright 2011), 386 participants (RR 0.98; 95% CI 0.70 to 1.37); the difference was not statistically significant, seeFigure 5 or Analysis 1.2
5.

Forest plot of comparison: 1 Tapered methadone versus any other treatment, outcome: 1.2 Number of participants abstinent at follow‐up.
1.2. Analysis.

Comparison 1 Tapered methadone versus any other treatment, Outcome 2 Number of participants abstinent at follow‐up.
Results at follow‐up as naloxone challenge
Two studies reported data on this outcome, but only Gerra 2000 reported the rate of participants who accepted and continued naltrexone treatment: in the methadone group 9/34, in clonidine five days 17/32; RR 0.50 (95% CI 0.26 to 0.95), the difference was statistically significant in favour of clonidine. Washton 1981 referred data for all the participants without distinction between the groups: of the eight participants who were opiate free at completion of the study, six began treatment with naltrexone.
Duration and severity of signs and symptoms of withdrawal
The diversity of approaches used for rating withdrawal severity, prevented a direct comparison of scores across studies. Different rating instruments were utilised and for many of them, the authors did not indicate the scores considered to represent boundaries of mild, moderate and severe to allow comparison of results between studies. The 21/23 studies that considered this outcome varied in how severity was rated and in the form in which results were reported. In some studies withdrawal was assessed by observers only, in others it was reported by participants and in others by both. In one study (Washton 1981), withdrawal was not systematically assessed and it was unclear how the assessment was undertaken. The diversity of approaches used for rating withdrawal severity prevented a direct comparison of scores across studies, consequently, we have not been able to make a quantitative analysis of the intensity of withdrawal. We tried to summarise the results in Table 3; Table 4; Table 5; Table 6; Table 7.
2. Withdrawal symptoms and side effects methadone versus adrenergic agonists.
| Study | Withdrawal symptoms | Side effects |
| Bearn 1996 | Mean scores higher for (1) on days 13‐21 and for (2) days 2‐12. Peak score on (1) day 13 and (2) day 10. | (2) 2 both female, experienced dizziness due to postural hypotension. |
| Camí 1985 | Muscular aching, flatulence and drowsiness more common in (1). Sleep disturbance & weeping in (2). | 1 of (2) had transferred loss of consciousness. (2) 4 (1) 1 experienced orthostatic hypotension. A graph shows a steady decline and similar magnitude in both groups regarding adverse effects, from days 1 to 6. After day 6, the scores for (1) increased, while in (2) continued to decline. |
| Dawe 1995 | Minimum withdrawal scores, mean (1) 25 (2) 33; maximum (1) 69 (2) 53. Time points minimum (1) day 1 (2) day 7, maximum (1) day 10 (2) day 2/3. | Not reported. |
| Gerra 2000 | In (2) mean scores slightly lower but not significantly lower than (3). During the last 4 days of treatment and after the first 4 days after methadone discontinuation; (1) mean scores significantly higher (2) than (3). | Mean daily blood pressure only for (2) & (3): no significant differences at any point. (2) 3 (3) 2 experienced side effects necessitate dose reduction. |
| Howells 2002 | Lowest daily score: mean (1) 49.4 (2) 50.0 ; Highest daily score: mean (1) 67.6 (2) 69.3; Total mean (1) 572.1 (2) 596.1 | Sitting blood pressure in (2) 4/32 lowest 61 mmHg, in (1) 3/36 lowest 80 mmHg, NS Depressive symptoms in 2 patients, one in each treatment group. |
| Jiang 1993 | On day 1 no significant differences in the two groups, between days 2 and 4 higher in (2), between days 8 and 12 lower in (2). | The scores higher in (2) compared to (1) from days 1 to 7, the greatest difference occurred on day 2 of treatment when the mean side effects scores was (1) 1.9 and (2) 8.2. The score subsequently declined in both groups. Comparison of each undesirable side effect suggests that general tiredness, weakness in walking, dizziness in standing position, dry mouth and lethargy are most common occurrences in (2), while in (1) only a small numbers of patients experienced general tiredness, weakness in walking, dry mouth and lethargy . In (2) 89 experienced dizziness on standing, mostly in the second and third days of treatment. Anxiety scores were significantly lower in (2) by day 11. |
| Kleber 1985 | Mean withdrawal scores at baseline and weeks 1‐2‐3‐4: at baseline no differences, during the first 2 weeks (1) 7.6, (2) 19.0, during the second two weeks (1) 13,0 (2) 12,0 ; Rates of withdrawal symptoms: (2) higher than (1); Comparison of withdrawal characteristics of success and failure in the groups were not statistically different. | Incidence of side effects, rated by physicians and nurses: (1) 11,5 (2) 16,8. Characteristics of side effects: for the majority of symptoms there were no differences among the two groups. Number using sleep medications: (1) 70% (2) 63%; Scores of Beck Depression Inventory between successfully drug‐free or not patients in the 2 groups were respectively: 54% and 17%. For the same groups, the percentage above the median for each ASI area were as follows: for medical area 62% and 46%, for employment 50% and 22%, for legal 35% and 22% , for family/social 31% and 28%, for psychological 31% and 28%. |
| San 1990 | Mean daily withdrawal scores (graph): Significant differences between (1) and (2) on days 2, 3, 4 and 5, higher in (1); between (1) and (3) on days 2, 3, 4 and 11, higher in (3); no significant differences between (2) and (3); the maximum mean was (1) 4.9, (2) 8.1, (3) 7.6 all on day 2. | Hypotensive effect more intense in (2); changes in heart rate more pronounced in (2) than in (3); (1) and (3) most frequent side effects: asthenia, dry mouth, flushing, mental clouding, thirst. . Differences in personality tests and patient's mood: NS |
| San 1994 | Mean daily withdrawal scores (graph): from day 9 higher in (2) and (3) for three days and in (1) after day 11, statistically significant between (1) and (3) on days 10,11 higher in (3); and between (1) and (2) on days 11,15, higher in (1); on day 20 higher in (3) compared with (1) and (2). | Differences in blood pressure and heart rate: for blood pressure, in (3) after day 13 grater decrease than in (1) and (2); for heart rate, in (3) bradycardia from day 9 with lowest rate on day 11, (62 beats per min); statistical significant difference between (3) compared with (1) and (2) in days 9, 10,11, 12,16, 17, 18, 19. Differences in personality tests and patient's mood: NS. |
| Umbricht 2003 | Mean withdrawal scores at baseline, after the first dose of medication and during the treatment no significant differences in the magnitude of the decrease in withdrawal between the groups. | 2 patients in (3) had to withdraw from the study because of decreased systolic blood pressure (< 90 mmHg) and bradycardia (HR < 50 BPM) |
| Washton 1981 | Major symptomatic complaints, specifically lethargy, restlessness and insomnia were identical for both groups. The main items contributing to scores in both groups were sleep problems, anxiety/nervousness, irritability, lack of energy, aches/pains and feeling cold. (2) reported symptoms during the 1° week of the study whereas (1) in the last week. | Lethargy and sluggishness most consistent complaints in (2). |
3. Withdrawal symptoms and side effects methadone versus other opioid agonists.
| Study | Withdrawal symptoms | Side effects |
| Madlung‐Kratzer 2009 | Changes in signs and symptoms of opioid withdrawal [12‐item German version of the Short Opioid Withdrawal Scale] assessed on days 0, 3, 7, 10, 14, 18 and 22 by patient self‐rating. At study entry signs and symptoms of withdrawal were mild but deteriorated steadily over time (day 0 versus day 22, P < 0.001). The only difference between the groups was found on day 18 (P = 0.022). All symptoms showed a homogeneous pattern of changes. (1) day 0 8.15 6.48 (7.00), day 22 16.00 7.81(15.00) P < 0.001; (2) day 0: 8.07 6.09 (7.00) day 22:18.32 8.98 (18.00) P < 0.001 |
The incidence of adverse events was low; 16 (16%) patients in the SRM group and 13 (13%) patients in the methadone group experienced at least one adverse event (c2 test, P = 0.586). Thirty of 45 (67%) of all adverse events were rated as being unrelated, nine (20%) as possibly related (SRM: six patients; methadone: three patients) and one (2%) (methadone group) as probably related to the study drug. The majority of adverse events (23 of 45) were gastrointestinal system disorders, such as nausea (three), vomiting (10), dentalgia (five), followed by psychiatric disorders (seven of 45, e.g. dysphoria, agitation, depression, panic attacks). |
| Seifert 2002 | SOWS score (days 0‐2): no differences; weeks 1‐2 (2) fewer symptoms than (1); no differences in self‐rating scales | Not assessed. |
| Sorensen 1982 | Mean symptom discomfort index initially declined then increased with drug taper. Initial, stabilisation and final ratings by graph: (1)18, 10, 15 (2) 16, 7, 16. | 1 overdose incident, possibly due to combination with alcohol. |
| Steinmann 2007 | Results in favour of buprenorphine only in the first day of treatment | Not assessed. |
| Tennant 1975 | Mean daily withdrawal scores (1) 6.6 (2) 9.6. Difference significant on days 8, 12, 15, 16, 17. | Only one statistically significant difference. (1)6 [16.7%], (2)17 [47%] reported euphoria. |
| Umbricht 2003 | Participant and observer rating scales: after first‐dose effect, further improvements were minimal, and overall mean scores during treatment were not significantly lower than scores after one treatment dose. The overall mean time averaged decreases ranged from‐5.1 to ‐6.0 for OOWS and ‐3.3 to ‐4.7 for SOWS. No significant differences in the magnitude of the decrease in the withdrawal between the treatment groups. At no time during treatment did withdrawal scores exceed baseline scores for any individual. | No major changes in blood pressure or heart rate during the observation time interval of the study. There was a trend (P = 0.06) toward myosis in the buprenorphine and methadone groups, consistent with a pharmacologic effect of treatment. Systolic blood pressure decreased significantly in the buprenorphine group. |
| Zarghami 2012 | Statistical analysis revealed that significant decreases (P ≤ .04) were found in the OOWS scores in both treatment methods up to day 14; no statistically significant difference was found between OOWS scores of the treatment methods at different intervals (P ≥ .1), except for day 6 of the study (P = .03) where results were in favour of tramadol. | No significant differences were observed in side effects scores for dizziness, somnolence, ataxia, constipation, nausea, seizures, and respiratory depression between two treatment methods, except for perspiration and pain, which were significantly higher in tramadol (P = .02) and methadone (P = 0.01) treatment methods, respectively |
OOWS: Objective Opioid Withdrawal Scale; SOWS: Short Opioid Withdrawal Scale
4. Withdrawal symptoms and side effects methadone versus anxiolytics.
| Study | Withdrawal symptoms | Side effects |
| Buydens‐Branchey 2005 | Subjective and Objective withdrawal scale: no significant differences between methadone and buspirone doses | Not assessed. |
| Drummond 1989 | Significant higher scores in the chlordiazepoxide group only on day 3; at the end of the study, the scores were higher in the methadone group but not statistically significant. Analysis of individual items in the OWS (Opiate Withdrawal Scale) failed to implicate any particular item as being responsible for the difference between the two groups. | In methadone group relative bradycardia is more present in the first days of treatment and the difference with respect to the chlordiazepoxide group became statistically significant on days 4 and 7. As methadone was gradually withdrawn, the mean heart rate returned to a level comparable to the beginning period. Mean pupil size was less in methadone group during the treatment period and the difference was statistically significant on day 5, similarly mean temperature was lower in this group on day 3. |
5. Withdrawal symptoms and side effects methadone versus placebo.
| Study | Withdrawal symptoms | Side effects |
| Buydens‐Branchey 2005 | Subjective and Objective scales: symptoms in placebo group were significantly more pronounced | Not assessed |
| San 1992 | Higher scores in the placebo groups, with the most severe symptoms on day 1 to 15. 8/11 placebo‐treated patients needed to be switched from placebo to methadone because the OWC (Opiate Withdrawal Checklist) daily score was > 15. With respect to features of the withdrawal syndrome in placebo patients, two stages were observed: anxiety, chills, gooseflesh, myalgia and weakness were the most common on day 1 to 5 and sleep disturbance persisted on day 6 to 13. | Not assessed |
6. Withdrawal symptoms and side effects methadone versus paiduyangsheng.
| Study | Withdrawal symptoms | Side effects |
| Yang 2006 | No differences between the two groups | Not assessed |
Side effects
Adverse effects were reported in 12/23 studies and assessed in different ways. This variability prevented quantitative analysis of this outcome. Data are reported in Table 3; Table 4; Table 5; Table 6.
Use of primary substance as Number of participants with opiate positive urinalysis during the treatment
Only 3/22 studies (Gerra 2000; Sorensen 1982; Tennant 1975) reported data on the use of opiate during the treatment but their modalities of reporting results of urinalysis was heterogeneous, making meta‐analysis difficult to be carried out. Results as reported in the articles are hardly informative, and data presented as number of positive tests over number of tests cannot be properly analysed through meta‐analysis. In fact using tests instead of the participants as the unit of analysis violates the hypothesis of independence among observations, and makes the results of tests done in each patient not independent.
2. Tapered methadone versus adrenergic agonists
2.1 Completion of treatment
Seven studies (Bearn 1996; Howells 2002; Kleber 1985; San 1990; San 1994; Umbricht 2003; Washton 1981), 577 participants RR 1.10 (95% CI 0.91to 1.32); the difference was not statistically significant, seeAnalysis 2.1,
2.1. Analysis.

Comparison 2 Tapered methadone versus adrenergic agonists, Outcome 1 Completion of treatment.
Use of primary substance as number of participants with opiate positive urinalysis during the treatment
One study (Gerra 2000), reported results of urine screening that showed a significantly higher rate of positive samples for morphine catabolites in the methadone and clonidine five‐days groups in respect of clonidine three days plus oxazepam, baclofen and ketoprofen group. No significant difference was found between the first two groups. In the methadone group, the positive urine rate increased significantly from day one to day 10.
Results at follow‐up as number of participants abstinent at follow‐up
One study (Kleber 1985), reported the number of participants abstinent at follow‐up at one month: 6/18 in methadone group and 4/15 in the clonidine group; at three months 5/19 in methadone and 4/15 in clonidine groups; at six months 7/18 in methadone and 3/13 in clonidine group. The differences were never statistically significant.
3. Tapered methadone versus any other opioid agonist
3.1 Completion of treatment
Seven studies (Madlung‐Kratzer 2009; Seifert 2002; Sorensen 1982; Steinmann 2007; Tennant 1975; Umbricht 2003; Wright 2011), 695 participants RR 1.10 (95% CI 0.89 to 1.37); the difference was not statistically significant, seeAnalysis 3.1.
3.1. Analysis.

Comparison 3 Tapered methadone versus other opioid agonists, Outcome 1 Completion of treatment methadone versus any other opioid agonist.
Use of primary substance as number of participants with opiate positive urinalysis during the treatment
Two studies (Sorensen 1982; Tennant 1975) considered this outcome.
Sorensen 1982, (tapered methadone versus LAAM) reported that the proportion of participants using opiates never dropped below 50% for any group at any time. Exact figures were not reported, data were presented only in a graph. The groups did not differ in the percentage of urine samples that contained opiates overall.
Tennant 1975, (tapered methadone versus propoxyphene) reported the number of participants who had opiate‐negative urine on at least one occasion: 27/36 (75%) in methadone group and 19/36 (53%) in propoxyphene group; the difference is not statistically significant.
Results at follow‐up as number of participants abstinent at follow‐up
Three studies reported this outcome.
Sorensen 1982: (tapered methadone versus LAAM), the data were reported for all the participants without distinction between the groups of treatment 57/61 participants gave consent to be interviewed: 24/49 reported that they abstained from heroin > one day after detoxification, at three months 2/49 abstinent, 25/49 sought further treatment and 9/49 enrolled in methadone maintenance treatment.
Tennant 1975: (tapered methadone versus propoxyphene) reported that at one month follow‐up the number of abstinent were 15/32 in the methadone group and 13/32 in propoxyphene group; the difference is not statistically significant.
Wright 2011: (tapered methadone versus tapered buprenorphine) reported that at eight days post detoxification, there was no statistically significant difference in the odds of achieving abstinence between the methadone and buprenorphine arms (odds ratio (OR) = 1.69; 95% CI = 0.81 to 3.51; P = 0.163). Similarly, there was no statistically significant difference at one month (OR = 0.38; 95% CI = 0.13 to 1.10; P = 0.074) or three months (OR = 0.38; 95% CI = 0.13 to 1.10; P = 0.074), and insufficient data at the six‐month time point to undertake statistical analysis.
3.2 Tapered methadone versus buprenorphine
Completion of treatment
Four studies (Seifert 2002; Steinmann 2007; Umbricht 2003; Wright 2011) 390 participants RR 0.97 (CI 95% 0.69 to 1.37), the difference was not statistically significant, seeAnalysis 3.2.
3.2. Analysis.

Comparison 3 Tapered methadone versus other opioid agonists, Outcome 2 Completion of treatment methadone versus buprenorphine.
3.3 Furthermore, single studies considered completion of treatment for the following comparisons
versus LAAM (Sorensen 1982), 5/15 patients in the methadone group and 4/13 in the LAAM group completed the treatment; RR 1.08 (CI 95% 0.37 to 3.21), the difference was not statistically significant but showed a trend in favour of LAAM;
versus propoxyphene (Tennant 1975), 25/36 in the methadone group and 15/36 in the propoxyphene group completed the treatment; RR 1.67 (CI 95% 1.07 to 2.60), the difference was statistically significant in favour of methadone group;
versus slow release morphine (Madlung‐Kratzer 2009), 49/100 in the methadone group and 50/102 in the slow release morphine group completed the treatment, RR 1.00 (CI 95% 0.75 to 1.32), the difference was not statistically significant.
4. Tapered methadone versus anxiolytic
4.1 Completion of treatment
Two studies (Buydens‐Branchey 2005; Drummond 1989), 47 participants RR 0.63 (CI 95% 0.18 to 2.24), the difference was not statistically significant and it should be considered that in one of the two studies (Buydens‐Branchey 2005) all the participants in both groups completed the treatment, seeAnalysis 4.1.
4.1. Analysis.

Comparison 4 Tapered methadone versus anxiolytic, Outcome 1 Completion of treatment.
5.Tapered methadone versus placebo
5.1 Completion of treatment
Two studies (Buydens‐Branchey 2005; San 1992), 38 participants RR 1.95 (CI 95% 1.21 to 3.13), in favour of methadone, see Analysis 5.1,
5.1. Analysis.
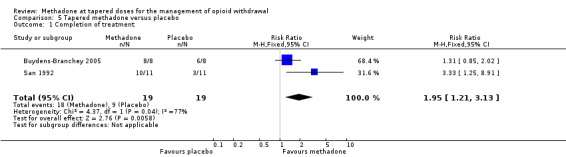
Comparison 5 Tapered methadone versus placebo, Outcome 1 Completion of treatment.
Discussion
Summary of main results
Comparing methadone with other pharmacological treatments aimed at detoxification, studies showed no substantial clinical difference between the treatments in terms of completion of treatment, 16 studies 1381 participants, risk ratio (RR) 1.08 (95% confidence interval (CI) 0.97 to 1.21), number of participants abstinent at follow‐up, three studies, 386 participants (RR 0.98; 95% CI 0.70 to 1.37) and degree of discomfort for withdrawal symptoms and adverse events.
Comparing methadone with adrenergic agonists, studies showed no substantial clinical difference between the treatments in terms of completion of treatment, seven studies, 577 participants RR 1.10 (95% CI 0.91 to 1.32). with regard to the withdrawal symptoms and side effects, early withdrawal symptoms were less adequately controlled with lofexidine than methadone; in the methadone groups the symptoms were experienced only in the latter stages of treatment when the dosage of the substance was drastically reduced. Only in two single studies (San 1990; San 1994) was methadone more effective than adrenergic agonists in decreasing withdrawal signs and symptoms and causing fewer side effects.
Comparing methadone with other opioid agonists, the results did not show differences between the groups with regard to completion of treatment, seven studies, 695 participants RR 1.10 (95% CI 0.89 to 1.37) and the acceptability of the treatment. Comparing methadone with buprenorphine, no differences were found for completion of treatment, four studies, 390 participants RR 0.97 (CI 95% 0.69 to 1.37).
Comparing methadone with the anxiolytic buspirone (Buydens‐Branchey 2005) and chlordiazepoxide (Drummond 1989) results did not show differences between the groups in terms of completion of treatment, two studies, 47 participants RR 0.91 (95% CI 0.47 to 1.77).
Comparing tapered methadone with placebo, studies showed, as expected, results in favour of methadone for completion of treatment, two studies, 38 participants RR1.95 (95% CI 1.21 to 3.13) and control of withdrawal symptoms.
Overall completeness and applicability of evidence
The extent to which a Cochrane review can draw conclusions about the effects of an intervention depends on whether the data and results from the included studies are valid. However, systematic reviews should evaluate and take into account not only the internal validity (i.e., the extent to which systematic errors or bias are avoided) of each trial included but also the applicability and generalisability or external validity (i.e., whether the results of a trial can be reasonably applied to a definable group of patients in a particular setting in routine practice) (Dekkers 2009). The main threat to external validity comes from the clinical setting, and the social and cultural context in which the studies were conducted, and this is particularly true in the field of addiction, where these contexts can actively affect the overall treatment outcome.
In this review, besides the limits in external validity due to the general requirement of RCTs in terms of strict inclusion criteria, highly homogenous study groups, limitations in dose adjustment, etc., the types of participants (adults abusers/dependents on opioids) are quite representative of the general population of opioid dependents. Moreover, the interventions, the settings and the outcomes investigated (completion of treatment, abstinence during the treatment and at follow‐up, adverse events) are important to populations, practitioners and decision makers, and relevant for the context of current practice.
However, there are general questions difficult to answer on the basis of our results such as what are the treatment expectations? what defines treatment success? is success strictly limited to suppression of withdrawal symptoms? The studies included did not examine any carried over effects bearing on sustained abstinence or eventual remission of disease and this certanly is a limit. Furthermore onether important limitation to the generalisation of the evidence is the impossibility to cumulate results of very important outcomes such as abstinence at follow‐up and control of withdrawal symptoms due the different ways in which these outcomes are rated and reported in the single studies. Finally 17 out of 22 included trials were conducted in an inpatients' setting, which is probably not the most common setting in clinical practice for this type of intervention, and this could act as an effect modifier in the estimation of efficacy of treatment.
Quality of the evidence
The quality of evidence, assessed according to the GRADE method, may be judged as high for the efficacy of tapered methadone versus any other treatment for the management of opioid withdrawal, see Summary of findings table 1. In respect of risk of bias, the quality of evidence was moderate to high, the percentage of included studies judged at low risk of bias were as follow: selection bias 13% for sequence generation and 30% for allocation concealment; performance bias 78%; detection bias 52% and 65% for attrition bias.
Finally, the great heterogeneity of the scales used in the primary studies and the way in which results were reported made it not possible to undertake a cumulative analysis.
Potential biases in the review process
None known.
Authors' conclusions
Implications for practice.
The results indicate that tapered methadone and the other substances used in the included studies are effective in the treatment of heroin withdrawal syndrome, although symptoms presented by participants differed according to the drug used. The studies confirm the issue that with the increasing availability of substances that allow slow tapering and temporary substitution of long‐acting narcotics, with good medical supervision and ancillary medications for tranquillisation and sleep, withdrawal can be relatively painless. Managed withdrawal, or detoxification, is not in itself a treatment for dependence but detoxification remains a required first step for many forms of longer‐term treatment. Moreover, different conditions of detoxification can affect at least an immediate outcome: heroin use during treatment and produce different responses in terms of intensity and time course of withdrawal response. Nevertheless, a majority of patients relapsed in heroin use, and relapse from the drug‐free state to re‐addiction is the main problem in heroin addiction.
Research suggests that for some important outcomes such as withdrawal symptoms, treatment programs are difficult to compare due to the variability of the methods used to assess them. Withdrawal limited to 30 days has the disadvantage that many persons, due to the rapid tapering, are prematurely withdrawn and consequently resume heroin use. There has been a general pessimism among both clinicians and researchers about the utility of brief detoxification treatment because many patients soon returned to regular heroin use. This pessimism is probably based on the unrealistic expectation that a brief, inexpensive intervention could dramatically alter the course of a chronic, relapsing disorder such as heroin addiction. Whether people relapse to heroin use again has no bearing on the success or otherwise of a detoxification procedure and the investment in methadone detoxification could be justified if more modest goals were being achieved for example, the reduction, even temporarily, of the daily heroin dosage, with its consequent reduction of dependence on illegal income and the possibility of reaching drug addicts who would otherwise not have applied for treatment.
Implications for research.
To enable comparison and pooling of results, standardised criteria for reporting urinalysis results should be used, data should be reported as number of participants with positive or negative samples instead of mean number of positive/negative tests for each group. When different rating instruments are used, researchers should try to utilise only published instruments, indicate the scores to represent boundaries of mild, moderate and severe withdrawal to allow comparison of results between studies and report the standard deviation of the means.
What's new
| Date | Event | Description |
|---|---|---|
| 20 July 2012 | New citation required but conclusions have not changed | New search, new studies, new assessment of risk of bias |
| 20 July 2012 | New search has been performed | Substantially updated |
| 20 October 2008 | Amended | Contact details amended |
History
Protocol first published: Issue 1, 2001 Review first published: Issue 1, 2002
| Date | Event | Description |
|---|---|---|
| 21 July 2008 | Amended | Minor changes |
| 2 July 2008 | Amended | Minimal changes in the abstract |
| 28 March 2008 | Amended | Inserted GRADE summary of findings table |
| 27 March 2008 | New search has been performed | The search strategy was updated and launched for all the database, we found four new trials to be included. Conclusions did not changed |
| 26 March 2008 | New search has been performed | Converted to new review format. |
| 18 May 2005 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We would like to thank Zuzana Mitrova for help in searching and retrieving articles.
Appendices
Appendix 1. CENTRAL search strategy
MeSH descriptor Substance‐Related Disorders explode all trees
((drug or substance) next (Abus* or addict* or dependen* or disorder*)):ti,ab
((opioid* or opiate*) next (withdraw* or detox*)):ti,ab,kw
(Overdos* or Over‐do*):ti,ab
(Intoxicat* or abstin* or abstain* or withdr* or detox*):ti,ab
(#1 OR #2 OR #3 OR #4 OR #5)
MeSH descriptor Heroin explode all trees
(heroin):ti,ab,kw
(Opioid* or Opiat*) :ti,ab,kw
(morphine*):ti,ab,kw
MeSH descriptor Methadone explode all trees
(methadone):ti,ab,kw
(#7 OR #8 OR #9 OR #10 OR #11 OR #12)
(#6 AND #13)
Appendix 2. PubMed search strategy
Opioid‐Related Disorders[Mesh]
((substance*[tiab] or drug[tiab]) AND (abuse*[tiab] or dependen*[tiab] or use* or disorder* or addict*[tiab]))
intoxicat*[tiab] or detox*[tiab] or disintox*[tiab] or withdraw*[tiab] or abstinen*[tiab] or abstain*[tiab])
#2 OR #3 OR #4
opiat*[tiab] OR opioid*[tiab] OR morphin*[tiab]
Heroin[MeSH Terms] OR heroin
Methadone[Mesh]
methadone [tiab]
#5 OR #6 OR #7 OR #8
#4 AND #9
randomized controlled trial [pt]
controlled clinical trial [pt]
randomized [tiab]
placebo [tiab]
clinical trials as topic [mesh: noexp]
randomly [tiab]
trial [tiab]
#11 or #12 or #13 or #14 or #15 or #16 or #17
#10 and #18
Appendix 3. EMBASE search strategy
'addiction'/exp
substance:ab,ti OR drug:ab,ti AND (abuse*:ab,ti OR dependen*:ab,ti OR use*:ab,ti OR disorder*:ab,ti OR addict*:ab,ti)
'detoxification'/exp
intoxicat*:ab,ti OR detox*:ab,ti OR disintox*:ab,ti OR withdraw*:ab,ti OR abstinen*:ab,ti OR abstain*:ab,ti
#1 OR #2 OR #3 OR #4
opiat*:ab,ti OR opioid*:ab,ti
heroin:ab,ti
morphine:ab,ti
'dimorphine'/exp
'methadone'/exp
methadone:ab,ti
#6 OR #7 OR #8 OR #9 OR #10
'crossover procedure'/exp
'double blind procedure'/exp
'single blind procedure'/exp
'controlled clinical trial'/exp
'clinical trial'/exp
placebo:ab,ti OR 'double blind':ab,ti OR 'single blind':ab,ti OR assign*:ab,ti OR allocat*:ab,ti OR volunteer*:ab,ti
random*:ab,ti OR factorial*:ab,ti OR crossover:ab,ti OR (cross:ab,ti AND over:ab,ti)
'randomized controlled trial'/exp
#13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20
#5 AND #12 AND #21 AND [humans]/lim AND [embase]/lim AND [2008‐2012]/py
Appendix 4. CINAHL search strategy
(MH "Substance Use Disorders+")
TX ((drug or substance) and (addict* or dependen* or abuse*or disorder*))
TX ((opioid* or opiate*) and (abuse* or addict* or dependen*))
S3 or S2 or S1
TX (opioid* or opiate*)
TX methadone or MH methadone
TX heroin or NT heroin
S7 or S6 or S5
TX random*
TX (clin* and trial*)
TX (singl* or doubl* or tripl* or trebl*) and (mask* or blind*)
TX crossover*
TX allocate*
TX assign*
TX ((random*) and (allocate* or assign*))
(MH "Random Assignment")
(MH "Clinical Trials+")
S17 or S16 or S15 or S14 or S13 or S12 or S11 or S10 or S9
S8 and S4
S18 and S19
Data and analyses
Comparison 1. Tapered methadone versus any other treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Completion of treatment | 16 | 1381 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.97, 1.21] |
| 2 Number of participants abstinent at follow‐up | 3 | 386 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.70, 1.37] |
Comparison 2. Tapered methadone versus adrenergic agonists.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Completion of treatment | 7 | 577 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.91, 1.32] |
Comparison 3. Tapered methadone versus other opioid agonists.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Completion of treatment methadone versus any other opioid agonist | 7 | 695 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.89, 1.37] |
| 2 Completion of treatment methadone versus buprenorphine | 4 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.69, 1.37] |
Comparison 4. Tapered methadone versus anxiolytic.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Completion of treatment | 2 | 47 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.47, 1.77] |
Comparison 5. Tapered methadone versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Completion of treatment | 2 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.95 [1.21, 3.13] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bearn 1996.
| Methods | Randomised controlled trial. Setting: inpatient treatment. | |
| Participants | 86 users of heroin, methadone or both; opioid dependent by DSM‐IV, drug use confirmed by urine test. (1) 44, (2) 42; (1) 86%, (2) 74% male. 37/86 also used benzodiazepines. Mean duration opioid use 10.5 Y. Mean age 31.7 Y. Groups similar. Excl. cr: major psychiatric or physical illness, pregnant or taking neuroleptic or antidepressant medication. | |
| Interventions | Stabilised on methadone (around 60 mg/day) for 3 days prior to detoxification, then: (1) Methadone, starting dose variable, tapered over 10 days. (2) Lofexidine,initial dose 0.6 mg/day until day 4, maintained at 2 mg/day for 3 days, then tapered over 3 days. Both drugs administered twice daily. Diazepam 3 days stabilisation then tapered over 21 days for those co dependent on benzodiazepines. Scheduled duration of the study 20 days (10‐day treatment program followed by 10 day‐rehabilitation program). Country of origin: Europe (UK). | |
| Outcomes | Completion rate as number completing 20 days treatment. Acceptability of the treatment as daily withdrawal score (graph) and as mean morning and evening daily blood pressure (graph) and number experiencing dizziness. | |
| Notes | SOWS (10 items, 0‐3 severity) completed daily by participants. Compliance corroborate by urine screening three times/week. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "after the stabilisation period, ..patients randomly assigned to either methadone syrup and placebo tablets or placebo syrup and lofexidine tablet". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "a dedicated worker who did not have clinical contact with the patients had exclusive knowledge of urine drug screen.." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Buydens‐Branchey 2005.
| Methods | Randomised controlled trial. Setting: inpatient | |
| Participants | 31 hospitalised heroin addicts (DSM IV), all males. 31 randomised, data presented on 29: 2 participants in the placebo group requested to discontinue. Age 48.3 years.12 Afroamerican, 10 Caucasian, 7 Hispanic. Mean age of starting regular heroin use: 24.6 years 15 iv; mean daily heroin use 0.62 g. 14 in the past had participated in MMT. Incl.c: used heroin daily for at least the prior 6 months, using al least 2.5 g/week of heroin; physical dependence on opiates; urine samples positive for opiates; expressed willingness to participate in an RCT. Excl. c: current or past psychiatric disorder; evidence of significant neurologic, gastrointestinal, hepatic, cardiovascular, renal, endocrine or haematologic disease; seropositive status for HIV. | |
| Interventions | (1) methadone, 8 participants; (2) placebo, 8 participants; (3) buspirone 30 mg, 8 participants; (4) buspirone 75 mg, 7 participants. Scheduled duration of the study 12 days. Country of origin: USA | |
| Outcomes | Completion of treatment; Assessment of withdrawal symptoms (SOWS and OOWS) | |
| Notes | 31 randomised, data presented on 29: 2 participants in the placebo group requested to discontinue. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method of allocation not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | staff, participants blind to treatment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | outcome assessors blind to treatment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | data presented for the 29/31 participants who remained in the study |
Camí 1985.
| Methods | Controlled clinical trial. Setting: inpatient treatment, no phone calls or visitors. Detoxification preceded admission to drug‐free therapeutic community. | |
| Participants | 45 users of heroin, dependent by DSM‐III‐R. Of 30 who completed study, 24 male. (1) 15, (2) 15. Mean age 23.5 Y. Mean heroin use 4.2 Y. Mean previous supervised withdrawal attempts 1.8. | |
| Interventions | (1) Methadone 30‐45 mg/day. Initial dose based on patient's weight and heroin consumed in last month.(2) Clonidine 0.9‐1.35 mg/day, Both drugs given every 8 hours and tapered over 10 days. Flunitrazepam and acetylsalicylic acid as adjunct medications. Psychoterapeutic support for all. Naloxone challenges (0.4 mg ) on day of discharge. Scheduled duration of the study 8‐10 days. Country of origin: Europe (Spain) | |
| Outcomes | Analysis based on 30/45 who completed 12 days of treatment. Acceptability of the treatment as percentage of mean positive symptoms and as mean adverse effects and mean changes in heart rates 2/daily. | |
| Notes | Withdrawal rated daily by nurses (19 withdrawal signs, 17 adverse effects rated present/absent). Patients completed State‐Trait Anxiety Inventory Questionnaire on days 1, 2, 3, 4, 7 & 10. Nurses measured blood pressure, heart rate and axillary temperature daily at 9 AM and 5 PM. Participants monitored by random urine screening. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | stated as double blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | stated as blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Dawe 1995.
| Methods | Randomised controlled trial. Setting: inpatient treatment. | |
| Participants | 16 users of heroin, (1) 7 (2) 9. Mean age 29 Y., mean use of heroin 8 Y. Groups stated as similar. | |
| Interventions | (1) Methadone tapered by linear reduction, mean starting dose 57.2 (range 35‐85) mg/day. (2) Clonidine oral, maximum 0.12 mg/day. (1) detoxification ward (2) behavioural psychotherapy ward. Scheduled duration of the study 13 days. Country of origin: Europe (UK) | |
| Outcomes | Acceptability of the treatment as min & max withdrawal scores; mean of withdrawal symptoms, negative and positive craving at time of maximum and minimum withdrawal. Drop‐outs rates not reported. | |
| Notes | Symptom Checklist used to assess physical symptoms of opiate withdrawal. Craving Questionnaire. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | clinical staff and patients blind to treatment, blind maintained with placebo syrup and tablets |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | results on all randomised participants |
Drummond 1989.
| Methods | Randomised controlled trial. Randomisation: Blindness: Placebos used to maintain blind. Setting: inpatient treatment, 3 hospitals involved. | |
| Participants | 33 heroin users selected, 9 excluded, 24 treated; 85% injectors, mean dose 0.8 +/‐ 0.6 g/day. 54.2% male, most used cannabis regularly or occasionally, 3/24 used benzodiazepines regularly. Mean age 24.9 Y., mean duration of drug use 4.7 Y.; Excl. cr.= serious physical illness. Groups similar. | |
| Interventions | (1) Methadone, initial dose 20 mg/day plus more if needed. (2) Chlordiazepoxide, initial dose 200 mg/day plus more if needed. Patients chose rate of dose reduction, discharge 2 days after final dose. Scheduled duration of the study 14 days. Country of origin: Europe (UK). | |
| Outcomes | Completion rate as rate of drop‐outs and length of treatment. Acceptability of the treatment as mean total subjective and objective withdrawal scores and as mean heart rate, mean pupil size, mean temperature (all graph). Results at follow‐up as urine screening, craving and mood measures, naltrexone compliance and relapse rate for 6 months. | |
| Notes | Patients rated expected withdrawal at entry, 16‐item SMQ daily. In addiction Objective Opiate Withdrawal scale. Nurses recorded physiological measures & 10 items scale daily. Rating instruments completed by subjects & nurses. Random urine testing. Study across 3 hospitals. Rating reliability confirmed, training to ensure consistent application. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Low risk | random allocation by pharmacist |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | staff and patients blind to medication and urine screening results |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Gerra 2000.
| Methods | Randomised controlled trial. Setting: inpatient. | |
| Participants | 98 heroin users by DSM‐IV, 71 males, aged 18 to 36 years, use of heroin from 2 to 6 years. (1) 34 (2) 32 (3) 32, (1) 24 (2) 23 (3) 24 male. Excl. c.: double dependence or prolonged use of drugs other than heroin, chronic physical disorders, psychosis, recent weight loss or obesity, endocrine‐neopathies and immuno deficiencies. | |
| Interventions | Intravenous heroin was administered to all participants until 12 hours before treatment. (1) Methadone oral tapered from 40 mg to zero in 10 days. (2) Clonidine iv 0.150 mg in 100 mL saline/three/morning and three/afternoon for 2 days, in the following 3 days, 0.150 mg three times/day. At 11 PM clonidine 0.150 mg orally every evening/5 days. (3) Clonidine at the same doses and with the same procedures of (2) for 2 days, and oral 0.150 mg/3 on the third day; oxazepam 60 mg/day, oral baclofen 10 mg/3/day and ketoprofen 400 mg daily. During the first day of treatment naloxone injections until the full dose of 0.4 mg was attained and 5 mg orally of naltrexone syrup. In the day 2, 50 mg of oral naltrexone. In (2) & (3) blood pressure was measured every 2 hours during detoxification procedure. Scheduled duration of the study 10 days. Country of origin: Europe (Italy). | |
| Outcomes | Acceptability of the treatment as mean scores of withdrawal symptoms daily and negative and positive craving scores. Use of primary substance as percentage of positive urine controls. (All graph). Results at follow‐up as rate of patients who accepted and continued naltrexone treatment (graph) and percentage of patients who relapsed in heroin dependence. All participants were admitted to extended naltrexone treatment after detoxification. | |
| Notes | Urinary tests performed daily during detox. period. Withdrawal symptoms evaluated by the same observer daily (9 signs, severity 0‐5). Craving Scale rated from patients at the beginning and following the treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | no information, apparently no blindness |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | no information, apparently no blindness |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Howells 2002.
| Methods | Randomised controlled trial. Setting: inpatient treatment. | |
| Participants | 76 heroin‐dependent by DSM IV, were eligible, 68 treated. (1) 36 (2) 32. Mean age (1) 30.5 years, (2) 29.8; time from first use of heroin (1) 9.5 (2) 8.8. Past month use of other substances for all participants: benzodiazepine 67.6%, amphetamine, 5%, non prescribed methadone 5%, cocaine 1%, crack 2%. Excl c.: serious major psychiatric illness, serious physical illness. | |
| Interventions | (1) Methadone 30 mg/day 1, 25 mg/day days 2 and 3, 20 mg/day days 4 and 5, then tapered to 0 in 10 days. (2) Lofexidine 0.6 mg day 1, increased of 0.4 mg/day until day 4, 2 mg/day for three days, next 3 days dose tapered by 0.4 mg/day. Scheduled duration of the study 10 days. Country of origin: Europe (UK). | |
| Outcomes | Completion rate as failure to complete detoxification. Acceptability of the treatment as withdrawal symptom severity, rates and timing of withdrawal. Other: severity of psychological aspects of drug dependence. | |
| Notes | Withdrawal Problems Scale, Short Opiate Withdrawal Scale both self‐rated daily. Severity of Dependency Scales. Hypotension, lying and sitting blood pressure, heart rate measured twice daily. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Low risk | random allocation by pharmacist |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | staff and patients blind to medication |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | stated as blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | results on all randomised participants |
Jiang 1993.
| Methods | Randomised controlled trial. Not all participants had entered treatment voluntarily. Setting: inpatient treatment in 5 different rehabilitation centres. | |
| Participants | 200 heroin users, dependent by DSM‐III‐R. 100 allocated to each group. (1) 73% (2) 82% male. (1) 80 (2) 67 using orally only, others iv or iv and oral. Men age (1) 24.9 (2) 24.7. No previous treatments (1) 79% (2) 63%. Duration of addiction (1) 16.1 (2) 15.2 months. At admission time since last drug intake (1) 8.7 hours(2) 10.7. No demographics differences. Excl. cr.: concurrent medical condition, infectious diseases, mental illnesses. | |
| Interventions | (1) Methadone, max days 1‐2 then tapered and ceased after day 12; mean max dose day 2 = 21.6 mg. (2) Clonidine, "sufficient" dose days 1‐4, tapered days 5‐8, ceased after day 11; mean max dose day 2 = 1.05 mg. For both drugs initial dose dependent on body weight, physical condition, heroin intake previous week. Dose titrated against withdrawal and side effects. Scheduled duration of the study: 12 days. Country of origin: China | |
| Outcomes | Acceptability of the treatment as mean daily withdrawal score and as total scores of undesirable side effects. Other: score variation in Hamilton Anxiety test. No drop outs reported. Endpoint of naloxone challenge used for only half of participants. | |
| Notes | Report in Chinese, English translation obtained. Symptoms and vital signs assessed daily using Himmelsbach scale as guide; 21 designated symptoms and vital signs also assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | no information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | no information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | results on all randomised participants |
Kleber 1985.
| Methods | Randomised controlled trial. Setting: outpatient treatment; component of multi‐centre study. | |
| Participants | 49 opiate addicts >‐ 6 mo. receiving methadone 20 mg/day or less, (1) 25 (2) 24, 76% males, mean age 29.5 Y., mean length of addiction 10.0 Y. Groups similar. | |
| Interventions | (1) Methadone, initial dose 20 mg/day, single daily oral dose tapered by 1 mg/day. (2) Clonidine oral, initial dose 0.3 mg/day in 3 divided doses; by day 6, gradual increase to max 1 mg/day; from day 11, tapered by 20‐25% per day. Chloral hydrate as adjunct medication. Scheduled duration of the study 30 days. Country of origin: USA. | |
| Outcomes | Completion rate as number of drop‐outs and percentages of success rates. Acceptability of the treatment as mean withdrawal scores at baseline and weeks 1‐2‐3‐4; rates of withdrawal symptoms (graph), comparison of withdrawal characteristics of success and failure in the two groups, incidence and characteristics of side effects and number using sleep medication. Results at follow‐up at 1, 3, 6 months as naloxone challenge rates. Other: Scores of Beck Depression inventory and of ASI. | |
| Notes | Withdrawal rated by nurses (24 items, 0‐3 severity) and participants (31 items, 1‐4 severity). Side effects rated by physicians and nurses. Successful detoxification, the main outcome, was defined as a) having 10 days following the last dose of study methadone in which no illicit opiate use is reported, or b) passing a naloxone test. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | participants and staff blind to treatment, blind maintained with placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | stated as blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis |
Madlung‐Kratzer 2009.
| Methods | Randomised controlled trial. Setting : inpatient at 3 psychiatric hospitals. | |
| Participants | 202 patients male and female opioid dependents (age > 18 years) willing to undergo detoxification from maintenance therapy in order to reach abstinence.who (confirmed diagnosis of opioid addiction according to ICD‐10 criteria) Incl.c: alcohol consumption of < 100 g/day during the last 4 weeks; reliable contraceptive methods (hormonal,non‐hormonal) for female patients of childbearing potential. Occasional (but not daily) consumption of cocaine was acceptable. Exc criteria: Patients were excluded from the study if they had clinically significant somatic illness (except hepatitis), acute psychotic illnesses (i.e. known schizophrenia or major depression with suicidal intent) or known contraindications to morphine or methadone. Patients were also excluded if they had received maintenance treatment with other opioids (e.g. buprenorphine, codeine derivatives) or were unwilling to follow investigator instructions. | |
| Interventions | (1) SROM: N= 102; (2) methadone: N = 100 both tapered. Scheduled duration of the study: 16 days. Country of origin: Austria. | |
| Outcomes | Completion rate, changes in signs and symptoms of opioid withdrawal [12‐item German version of the Short Opioid Withdrawal Scale (SOWS)] [20] assessed on days 0, 3, 7, 10, 14, 18 and 22 by patient self‐rating; somatic and psychological symptoms [Symptom Checklist (SCL‐90‐R)] [21] assessed on days 0, 7, 14 and 22,from which global symptom scale scores were calculated; craving for heroin, alcohol, benzodiazepines, cocaine and cannabis (rated by patients on a visual analogue scale: 0 mm = no craving, 100 mm = most intense craving) assessed on days 0, 3, 7, 10, 14, 18 and 22; adverse events. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | central stratified randomisation |
| Allocation concealment (selection bias) | Low risk | random allocation by pharmacist |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | participants and staff blind to treatments |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis |
Salehi 2007.
| Methods | Randomised controlled trial. Setting: outpatient | |
| Participants | 70 participants, all males, mean age 37 years; n. 60 married: 60; n. 33 elementary education, n. 26 high school, n.11 university degree. Duration of dependence mean 12.8 years. Groups similar. Exc cr: presence of any medical disease that prohibited using tramadol and methadone, taking extra medication, polysubstance dependence, presence of any major psychiatric disorder. | |
| Interventions | (1) methadone, starting dose 15 mg/day, 36 participants, ; (2) tramadol, starting dose 450 mg/day, 34 participants. Both groups were treated with 0.3 mg/day of clonidine and 10 to 30 mg/day oxazepam. Scheduled duration of the study 7 days. Country of origin: Iran | |
| Outcomes | Completion of treatment, Withdrawal symptoms (SOWS) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | participants and staff blind to medication |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | outcome assessors blind to medication |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
San 1990.
| Methods | Randomised controlled trial. Randomisation: method of allocation not reported. Blindness: Setting: inpatient treatment. | |
| Participants | 170 heroin dependent by DSM‐III‐R entered trial, analysis based on 90/170 who completed >‐12 days of treatment. (1) 30, (2) 30, (3) 30. In each group around 80% male, mean age around 24 Y. and mean duration of opiate use around 5 Y. No differences between groups Excl. c.: psychopathological antecedents before opioid addiction, signs cardiovascular diseases, previous participation in clinical trial. Country of origin: Europe (Spain) | |
| Interventions | Initial dose of medication dependent on weight and heroin use in previous week. (1) Methadone, mean max dose 37.3 mg/day. (2) Clonidine, mean max dose 1.05 mg/day, (3) Guanfacine, mean max dose 3.58 mg/day. For all max dose given on days 2 & 3. Drugs tapered over 11 days. Benzodiazepines as adjunct medication as needed. Scheduled duration of the study 14 days. | |
| Outcomes | Completion rate as mean duration in treatment, number completing detoxification, causes of failure. comparison of success and failure. Acceptability of the treatment as time course of withdrawal scores (graph), min & max withdrawal scores time, course of cardiovascular effects, mydriasis and other side effects (all graph). Other: Scores of EPQ and MMPI. Some data confounded by exclusion of early drop‐outs. | |
| Notes | Withdrawal and side effects rated by observers. Participants completed psychometric evaluation (MMPI, State Trait Anxiety Inventory and Eysenck Personality Questionnaire) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | participants and staff blind to medication, placebo used to maintain blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | outcome assessors blind to medication |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
San 1992.
| Methods | Randomised controlled trial. Blindness: double blind. Setting: inpatient treatment. | |
| Participants | 22 opioid dependent by DSM‐III‐R, using buprenorphine mean dose (1) 2.0 (2) 1.7 mg/day; route of assumption (1) 81.8% (2) 100% iv (1) 11 (2) 11 patients, 17 male, mean age (1) 28.0 (2) 29.7 Y. No differences in groups. Excl. cr.: patients with methadone or heroin use detected by urine testing in 2 weeks prior to admission. | |
| Interventions | (1) Methadone max dose 20 mg/day, tapered over 9‐11 days. (2) Placebo. Scheduled duration of study 13 days Country of origin: Europe (Spain). | |
| Outcomes | Completion rate as number who completed and numbers of patients who shifted from (2) to (1). Acceptability of the treatment as individual mean daily withdrawal scores in placebo group (graph). Study confounded by 8/11 placebo‐treated group being switched to methadone. | |
| Notes | Opiate Withdrawal Checklist (21 items, 0‐3 severity) administered by nursing staff. Data provided for placebo‐treated patients only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Low risk | allocation by pharmacy prior to admission |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | participants and staff blind to medication |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | outcome assessors blind to medication |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
San 1994.
| Methods | Randomised controlled trial. Setting: inpatient treatment. Trial in two phases. | |
| Participants | 144 heroin dependent by DSM‐III‐R, mean heroin dose 656 mg/day; Group (3) introduced in phase 2. (1) 75 (2) 43 (3) 26, 102 male, mean age 27.1 Y., 52% HIV+. Stated no differences between groups. Excl. cr.: history of psychiatric disorders, liver dysfunction, cardiovascular diseases, other addiction, pregnancy. | |
| Interventions | Methadone, 3 divided doses, initial dose based on body weight & heroin consumption, tapered over 8 days to (1) 10% (2&3) 50% of initial dose. From day 9: (1) Continued methadone taper, others switched to (2) 3 or (3)4 mg guanfacine. 59% given benzodiazepines 32% hypnotics as adjunct medication. Scheduled duration of the study 18 days. Country of origin: Europo (Spain) | |
| Outcomes | Completion rate as percentage of participants remaining in the study (graph). Acceptability of the treatment as mean daily withdrawal scores (graph) and differences in blood pressure and heart rate. Other: mean dose diazepam, personality tests, patients' mood between groups. | |
| Notes | Opiate withdrawal symptoms were measured by means of the Opiate Withdrawal Checklist which was completed by nursing staff three times a day and the Opiate Withdrawal Syndrome which was self‐ completed by patients once a day. Nursing staff monitored heart rate and blood pressure daily. Urine screening days 1, 4, 7, 14, 17. Psychometric tests were performed in all participants. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Low risk | allocation by pharmacy |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | double blind, treating doctor blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not stated if observer blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Seifert 2002.
| Methods | Randomised controlled trial. Randomisation: Blindness: Setting: inpatient treatment. | |
| Participants | 26 opioid dependent (DSM IV criteria) and abused various additional drugs. (1) 12 (2) 14; Mean age (1) 31.8 (2) 31.1; Male (1) 9 (2) 13; Years of opioid abuse (1) 10.5 (2) 8.6. Excl cr: people who had participated in a structured drug research program within the previous 6 months or had active schizophrenia, active bipolar affective disorder, active hepatic disease, active cardiovascular disease, abnormal ECG, chronic obstructive pulmonary disease, pregnancy. | |
| Interventions | (1) Methadone tapered, starting dose 20 mg/day, last dose 2.5 mg/day. (2) Buprenorphine tapered starting dose 4 mg/day, last dose 0.4 mg/day. For both groups carbamazepine: days 1‐6: 900 mg/day; days 7‐10: 400 mg/day; days 11‐14: 200 mg/day. Scheduled duration of the study 14 days. Country of origin: Europe (Germany). | |
| Outcomes | Completion rate as number of non completer. Acceptability of the treatment as mean scores of SOWS and as scores of a visual analogue scale. | |
| Notes | SOWS self‐rate and examiner rating using a visual analogue scale. Urine sample randomly once a week. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | double blind, placebo used to maintain blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not stated if observer blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Sorensen 1982.
| Methods | Randomised controlled trial. Setting: outpatient treatment. | |
| Participants | 61 heroin dependent > 80/day. All male. 53% white, 36% Hispanic, 11% other. Mean age 28.9; 33% employed; 28% married; 57% arrested in last 2 Y.; 90% had prior treatment. (1A) 18 (1B) 15 (2A) 15 (2B) 13 . Groups similar on all except arrests in last 2 years. Excl. c.: life‐threatening medical conditions. | |
| Interventions | (1A) Methadone 30 mg increasing to 40 mg, then tapered in 6 weeks, (2A) LAAM, doses to parallel methadone.,(1B) & (2B) same but active treatment only 3 weeks. For all, 1 week stabilisation. Scheduled duration of the study 21 days. Country of origin: USA | |
| Outcomes | Completion rate as percentage of retention in treatment. Acceptability of the treatment as mean symptom discomfort index (graph). Use of primary substance of abuse as percentage of patients with urine samples positive for opiate (graph). Initial, stabilization and final ratings. Results at follow‐up as number of abstinent > 1 day after detoxification and at follow‐up at 3 months: number of abstinent, sought further treatment, enrolled in MMT. | |
| Notes | Profile of Mood State (POMS) completed wk prior treatment & day 14. Detoxification Symptom Scale (20 items) administered by researchers daily, reported as discomfort index combining frequency and severity. Two urine screens per week (random). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified by employment status |
| Allocation concealment (selection bias) | Low risk | random allocation by pharmacist |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | double blind, doses prepared by pharmacist; placebo used to maintain blind, staff and participants blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | outcome assessors blind to medication |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | results on 86% of participants available 12 weeks after intake |
Steinmann 2007.
| Methods | Randomised controlled trial. Setting: inpatient | |
| Participants | 39 opioid dependent, 31 males, mean age 27 years. EXC cr: previous detoxification treatments | |
| Interventions | (1) methadone 21 participants, starting dose 60 mg/day, tapered of 2.5‐5 mg/day; (2) buprenorphine, 18 participants, starting dose 12‐16 mg/day, tapered of 0.8‐1.2 mg/day. Scheduled duration of the study 28 days. Country of origin: Europe (Germany) | |
| Outcomes | Completion of treatment, withdrawal symptoms (OOWS), craving. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Tennant 1975.
| Methods | Randomised controlled trial. Setting: outpatient treatment, daily clinic attendance for supervised dosing. | |
| Participants | 72 heroin addict > 18 Y.; dependent by history, needle marks, positive urine test, observation of withdrawal symptoms. (1) 36 (2) 36; (1) 80.6% (2) 77.7% male; (1) 50% (2) 56% white; mean age (1) 27.1 (2) 28.5 ; mean duration heroin use years (1) 7.8 (2) 9.1; mean current daily heroin use months (1) 8.8 (2) 7.0; (1) 5.0% (2) 3.2% urine positive for amphetamines or barbiturates during treatment . No differences between groups. | |
| Interventions | (1) Methadone, initial dose 24 mg daily tapered. (2) Propoxyphene napsylate, initial dose 800 mg daily, tapered. Scheduled duration of the study 21 days. Country of origin: USA. | |
| Outcomes | Completion rate as number not completed treatment and mean days in treatment. Acceptability of the treatment as mean daily withdrawal scores (graph). Use of primary substance of abuse as percentage of patients with urine samples positive/negative during treatment. Results at follow‐up as at 1 month: patients abstinent, relapsed, entered in MMT. | |
| Notes | Intensity of withdrawal assessed daily using Himmelsbach scale (0‐2+severity). 16 side effects assessed each day by same scoring system. Observed urine 2x weeks. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | staff and patients blind; medication dispensed in identical capsules and placebos used to conceal tapering |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Umbricht 2003.
| Methods | Randomised controlled trial. Randomisation: Blindness: Setting: inpatient treatment. | |
| Participants | 63 heroin dependent: (1) 21, (2) 21, (3) 21,. Mean age: (1) 40.0, (2) 39.6, (3) 40.0, ; Afro‐American: (1) 21, (2) 20, (3) 21; Male (1) 9, (2) 15, (3) 14. Incl c.: current heroin dependent, HIV seropositivity, 18 years or more, hospitalisation for an acute medical illness. Excl c.: concurrent alcohol dependence, inability to give informed consent, acute psychosis or AIDS dementia, hypotension, bradycardia, coagulopathy or severe thrombocytopenia precluding intramuscular injections, enrolment in methadone maintenance treatment. | |
| Interventions | (1) Methadone orally once a day, 30 mg on day 1, 20 mg on day 2, 10 mg on day 3. (2) Buprenorphine intramuscularly 0.6 mg every 4 h on day 1, every 6 h on day 2, every 8 h on day 3. (3) Clonidine orally, a loading dose of 0.2 mg followed by 0.1 mg every 4 h on day 1, every 6 h on day 2 and every 8 h on day 3. Scheduled duration of the study 3 days. Country of origin: USA. | |
| Outcomes | Completion rate as number who completed the study and number of drop‐outs who voluntarily left the study. Acceptability of the treatment as mean participant‐ and observer‐rated opioid withdrawal scores and pupil size. Craving. | |
| Notes | SOWS twice a day rated by participants, nurses rated opioid withdrawal scale three times a day. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | double blind, placebo used to maintain blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Washton 1981.
| Methods | Randomised controlled trial. Setting: outpatient treatment, 3‐5 clinic visits/week. | |
| Participants | 26 patients, 19/26 MMT (15‐30 mg/day), 7/26 illicit heroin and/or methadone, stabilised for 3 weeks on 15‐30 mg/day methadone. 22 male, 18 white, 5 black, 3 Hispanic, mean age 31 (range 22‐49) Y , mean duration of addiction 10 Y (range 3 mo‐25 Y.) (1) 13 (2) 13. Groups stated as similar. Excl. c.: evidence of serious medical or psychiatric illness. | |
| Interventions | (1) Methadone 20 mg/day reduced by 1 mg/day. (2) Clonidine, dose titrated against symptoms and side effects to max 1.2 mg/day. Scheduled duration of the study 30 days. Country of origin: USA | |
| Outcomes | Completion rate as number completing detoxification. Results at follow‐up as number initiating naltrexone maintenance treatment. | |
| Notes | Ratings of withdrawal not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | participants and staff blind to medication |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | investigators not informed of blood pressure measurements to avoid breaking blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | results on all randomised participants |
Wright 2011.
| Methods | Randomised controlled trial. Setting: prison. | |
| Participants | 289 prisoners, all male. Incl.c: 21–65 years old; using illicit opiates as confirmed by urine test; expressing a wish to detoxify and remain abstinent; willing to give informed consent; and remaining in custody for at least 28 days. Excl. c: contraindications to methadone or buprenorphine; medical conditions requiring emergency admission to hospital, thus precluding detoxification; currently undergoing detoxification from other addictive drugs whereby concurrent opiate detoxification would not be clinically indicated; and previously randomised into the trial. | |
| Interventions | (1) Methadone, n = 148, starting dose 30 mg (2) Buprenorphine, n = 141, starting dose 8 mg. Scheduled duration of the study: 20 days. Country of origin: UK. | |
| Outcomes | Post detoxification abstinence across time; completion rate. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | randomisation sequence (with random block size) was generated using Microsoft Excel RAND function |
| Allocation concealment (selection bias) | Low risk | sealed, opaque, consecutively numbered envelopes concealing the name of the allocated intervention were prepared by a researcher who had no contact with participants |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | participants and staff blind to medication |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | outcome assessors blind to medication |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis |
Yang 2006.
| Methods | Randomised controlled trial. Setting: inpatient. | |
| Participants | 580 opioid dependents; (1) 278, (2) 302. Mean age: 23 years; Male 381. | |
| Interventions | (1) Methadone, starting dose 40‐50 mg/day then tapered 20% per day. (2) Paidu capsules, starting dose 3‐5 twice a day, then tapered. Scheduled duration of the study 10 days. Country of origin: China. | |
| Outcomes | Withdrawal symptoms (OOWS); Anxiety (Hamilton Anxiety Rating Scale). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | staff and participants blind to treatment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | outcome assessors blind to treatment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not clear |
Zarghami 2012.
| Methods | Randomised controlled trial. Setting: inpatient. | |
| Participants | 70 patients, all men; age range, 18–46 years, with a confirmed diagnosis of opioid dependence according to DSM‐IV‐TR criteria. Excl. c: clinically significant somatic illness (e.g., hepatitis, tuberculosis, acquired immune deficiency syndrome), a history of seizures, acute psychotic illnesses (e.g., known schizophrenia or major depression with suicidal intent), and using other substances except nicotine (e.g., other opioids, monoamine oxidase (MAO) inhibitors, doxepin, anti‐spastic drugs, beta blockers, known inducers or inhibitors of CYP3A and CYP2D6, cannabinoids, and alcohol). No significant differences were found in baseline demographics and drug use history between the two patient cohorts. | |
| Interventions | (1) methadone, N = 35; (2) tramadol N = 35. The dose reduction regimens were based on an oral dose of either 600 mg/day of tramadol (200 mg three times daily) or 60 mg/day of methadone (20 mg three times daily). These starting doses were maintained for three consecutive days under double‐blind conditions. Thereafter, detoxifications were initiated by tapered dose reductions (20% every 2 days) over a period of 11 days to reach abstinence. At the end of second week, the medications were discontinued. |
|
| Outcomes | Withdrawal scores; side effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not reported |
| Allocation concealment (selection bias) | Unclear risk | method of allocation not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | method not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | method not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | nine patients in the methadone group and five patients in the tramadol group were excluded from the study |
ASI: Addiction Severity Index; DSM: Diagnostical and Statistical Manual of Mental Disorders; ECG: Electrocardiogram; EPQ: Esenck Personality Questionnary; Excl. c: Exclusion criteria; HIV: Human Immunodeficency Virus; h: hour; Incl.c: Inclusion criteria; ITT: intention‐to‐treat; iv: intravenous; MMPI: Minnesota Multiphasic Personality Inventory; MMT: Methadone Maintenance Treatment; mo: months; OOWS: Objective Opiate Withdrawal Scale; RCT: Randomised Controlled Trial; SOWS: Subjective Opiate Withdrawal Scale; SMQ: Subjective Measures Questionnairewks: weeks; Y: years
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Albizu‐Garcia 2012 | Excludes as study design was not in the inclusion criteria: survey report |
| Bakhshani 2008 | Excluded as type of intervention was not in the inclusion criteria: evaluation of the efficacy of transcutaneous electrical stimulation added or not to methadone |
| Bearn 1998 | Excluded as the study design was not in the inclusion criteria of the review: open design with a patient preference allocation |
| Bearn 2008 | Excluded as type of intervention was not in the inclusion criteria: auricular acupuncture as an adjunct to opiate detoxification treatment |
| Bell 2009 | Excluded as type of intervention was not in the inclusion criteria: investigate the pharmacokinetics and pharmacodynamics of orally administered methadone‐naloxone |
| Bickel 1988 | Excluded as type of intervention was not in the inclusion criteria: length of treatment 90 days |
| Brewin 1989 | Excluded as the study design was not in the inclusion criteria: review article |
| Bux 1993 | Excluded as the study design was not in the inclusion criteria: no randomised controlled trial |
| Byrne 2006 | Excluded as the study design was not in the inclusion criteria: letter |
| Cameron 2006 | Excluded as type of intervention was not in the inclusion criteria: length of treatment 12 weeks |
| Critchlow 2006 | Excluded as the study design was not in the inclusion criteria: letter |
| Dawe 1991 | Excluded as type of intervention was not in the inclusion criteria: length of treatment 70 days |
| De Los Cobos 2000 | Excluded as the study design was not in the inclusion criteria: no randomised controlled trial |
| Deniker 1975 | Excluded as the study design was not in the inclusion criteria: no randomised controlled trial |
| Dijkstra 2010 | Excluded as type of intervention was not in the inclusion criteria: rapid detoxification with naltrexone |
| Ebner 2004 | Excluded as the study design was not in the inclusion criteria: no randomised controlled trial |
| Fulwiler 1979 | Excluded as the type of intervention was not in the inclusion criteria: two different modalities of tapering methadone (1) physician regulated, (2) self‐regulated |
| Gerra 2004 | Excluded as the type of intervention was not in the inclusion criteria: methadone and buprenorphine both as maintenance treatments |
| Gerra 2007 | Excluded as type of intervention (maintenance) and type of participants (include also healthy participants ) were not in the inclusion criteria |
| Glasper 2008 | Excluded as the type of intervention was not in the inclusion criteria: both groups received methadone at different dosages to investigate influence of methadone doses on the Severity of Opiate Withdrawal Symptoms |
| Goldstein 1972 | Excluded as the study design was not in the inclusion criteria: theoretical and descriptive study |
| Gossop 1989A | Excluded as the study design was not in the inclusion criteria: retrospective analysis |
| Green 1988 | Excluded as the type of intervention was not in the inclusion criteria: methadone tapered in both groups plus (1) 15‐30 min interview with detailed information about the withdrawal regimen likely length and intensity of symptoms. (2) regular information about their admission and ward routine |
| Greenwald 2006 | Excluded as type of participants not in the inclusion criteria: volunteers no opioid dependent |
| Gruber 2008 | Excluded as the type of intervention was not in the inclusion criteria: methadone maintenance with standard or minimal counselling versus 21‐day methadone detoxification |
| Hall 1979 | Excluded as the type of intervention not in the inclusion criteria: methadone tapered in both groups plus (1) paid for drug‐free urine 6 times during treatment and brief counselling weekly. (2) Paid $1 for each urine sample given |
| Hall 2008 | Excluded as the study design was not in the inclusion criteria: letter |
| Hasson 2007 | Excluded as type of intervention was not in the inclusion criteria: length of treatment 24 weeks |
| Highfield 2007 | Excluded as type of intervention was not in the inclusion criteria: length of treatment 120 days |
| Hser 2012 | Excluded as type of intervention was not in the inclusion criteria: MMT |
| Jaffe 1972 | Excluded as type of intervention was not in the inclusion criteria: length of treatment 15 weeks |
| JI 2007 | Excluded as type of intervention was not in the inclusion criteria: tapered methadone in both groups |
| Johnson 1992 | Excluded as type of intervention was not in the inclusion criteria: length of treatment 17 weeks |
| Kheirabadi 2008 | Excluded as type of intervention was not in the inclusion criteria: efficacy of gabapentin added to methadone |
| Krabbe 2003 | Excluded as the study design not in the inclusion criteria of the review: prospective clinical trial |
| Kristensen 2005 | Excluded as type of intervention was not in the inclusion criteria: length of treatment 26 weeks |
| Lal 1976 | Excluded as the type of intervention not in the inclusion criteria: two different modalities of tapering methadone (1) methadone tapered over 10 days (2) abrupt cessation day 11 |
| Liu 2009 | Excludes as study design and type of intervention not in the inclusion criteria: review of randomised trials comparing acupuncture combined with opioid agonist treatment versus opioid agonists alone for treating symptoms of opioid withdrawal |
| Liu 2009a | Excludes as study design and type of intervention not in the inclusion criteria: review of randomised trials comparing Chinese herbal medicine to either alpha2‐adrenergic agonists or opioid agonists for heroin detoxification |
| Lobmaier 2010 | Excludes as study design not in the inclusion criteria: article that reviews the main pharmacotherapies that are currently being used to treat opioid addiction |
| Madden 1986 | Excluded as the type of intervention not in the inclusion criteria of the review: methadone tapered in both groups plus (1) "standard detoxification" (2) "cordial substitution" |
| Maddux 1980 | Excluded as the study design was not in the inclusion criteria: longitudinal study |
| Mannelli 2008 | Excluded as type of intervention not in the inclusion criteria: very low dose naltrexone addition in opioid detoxification |
| McCambridge 2006 | Excluded as type of intervention was not in the inclusion criteria: random allocation only for groups without methadone |
| McCaul 1984 | Excluded as the study design, the type of intervention not in the inclusion criteria: no RCT, three different modalities of tapering methadone, 6 weeks of treatment |
| Meader 2010 | Excluded as the study design was not in the inclusion criteria of the review: systematic review |
| Mintz 1975 | Excluded as the type of intervention not in the inclusion criteria: methadone maintenance patients were assigned to (1) decreasing dose or (2) continued methadone maintenance |
| Mitchell 2012 | Excluded as the study design was not in the inclusion criteria: the study compares the characteristics of patients entering methadone treatment vs. buprenorphine treatment to determine whether BT was attracting different types of patients |
| Mokhber 2008 | Excluded as the type of intervention not in the inclusion criteria: efficacy of totipalmate as an adjunct medication in heroin withdrawal |
| Neale 2005 | Excluded as study design not in the inclusion criteria: cross sectional data from a longitudinal study |
| O'Connor 1997 | Excluded as the type of intervention was not in the inclusion criteria: no methadone in the three detoxification protocols (clonidine, combined clonidine and naltrexone, buprenorphine) |
| Pjrek 2012 | Excluded as study design not in the inclusion criteria: naturalistic study |
| Rawson 1983 | Excluded as the type of intervention was not in the inclusion criteria: methadone tapered in both groups plus (1) with counselling sessions (2) without counselling |
| Reed 2007 | Excluded as study design not in the inclusion criteria: not RCT, allocation to detoxification condition was by patient choice |
| Reilly 1995 | Excluded as the study design was not in the inclusion criteria: not RCT |
| Sees 2000 | Excluded as the type of intervention was not in the inclusion criteria: (1) methadone maintenance treatment, (2) methadone tapered; outcomes at six months |
| Semba 2007 | Excluded as the study design was not in the inclusion criteria: not RCT |
| Shaygani 2009 | Excluded as the study design was not in the inclusion criteria: not RCT |
| Sheard 2006 | Excluded as the type of intervention not in the inclusion criteria: no methadone |
| Soyka 2009 | Excluded as the study design was not in the inclusion criteria: not RCT, open study |
| Stimmel 1982 | Excluded as the study design was not in the inclusion criteria: not RCT |
| Stotts 2012 | Excluded as type of intervention not in the inclusion criteria: study developed and tested an ACT‐based opioid detoxification behavioral therapy study developed and tested an ACT‐based opioid detoxification behavioural therapy |
| Strain 1993 | Excluded as type of intervention not in the inclusion criteria: the length of treatment (15 weeks) was too long |
| Strang 1990 | Excluded as the type of intervention was not in the inclusion criteria: two different modalities of tapered methadone on (1) linear (2) inverse exponential curve |
| Strang 1997 | Excluded as the type of intervention and the outcomes measures were not in the inclusion criteria: groups differed in duration of detoxification, intensity & duration of adjunct & follow‐up care, no rating instruments used, no urinalysis reported, endpoint is vague |
| Sullivan 2004 | Excluded as study design not in the inclusion criteria: cross‐ sectional survey |
| Teesson 2006 | Excluded as the study design was not in the inclusion criteria: not RCT |
| Tennant 1978 | Excluded as type of intervention was not in the inclusion criteria: length of treatment 42 days |
| Van Beek‐Verbeek 1983 | Excluded as the type of intervention was not in the inclusion criteria: methadone tapered in both groups plus (1) placebo (2) desglycinamide9‐arginine 8‐vasopressin |
| Veilleux 2010 | Excluded as the study design was not in the inclusion criteria: not RCT, review of opioid dependence treatment |
| Wang 1982 | Excluded as the type of intervention was not in the inclusion criteria: methadone not tapered |
| Yang 2008 | Excluded as the type of intervention was not in the inclusion criteria: the study examines the effects of levotetrahydropalmatine (l‐THP) on reducing heroin craving and increasing the abstinence rate among heroin‐dependent patients |
| Zeng 2005 | Excluded as type of intervention was not in the inclusion criteria: tapered methadone in both groups |
| Ziaadini 2011 | Excluded as the study design was not in the inclusion criteria: not RCT, cohort prospective study |
ACT‐based: acceptance and commitment therapy‐based; BT: behavioural therapy; MMT: Methadone Maintenance Treatment; RCT= Randomised Controlled Trial.
Contributions of authors
Marica Ferri drafted the original protocol. Laura Amato and Silvia Minozzi searched and selected trials, extracted data and wrote the review. Silvia Minozzi evaluated the methodological quality of the studies and commented on the updated version of the review. Marina Davoli supervised the entire review and Robert Ali commented on the draft. Laura Amato updated the review.
Sources of support
Internal sources
Department of Epidemiology, ASL RM E, Italy.
External sources
No sources of support supplied
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Bearn 1996 {published data only}
- Bearn J, Gossop M, Strang J. Randomised double‐blind comparison of lofexidine and methadone in the in‐patient treatment of opiate withdrawal. Drug and Alcohol Dependence 1996;43(1‐2):87‐91. [DOI] [PubMed] [Google Scholar]
Buydens‐Branchey 2005 {published data only}
- Buydens‐Branchey L, Branchey M, Reel‐Brander C. Efficacy of buspirone in the treatment of opioid withdrawal. Journal of Clinical Psychopharmacology 2005;25(3):230‐6. [DOI] [PubMed] [Google Scholar]
Camí 1985 {published data only}
- Cami J, Torres S, San L, Sole A, Guerra D, Ugena B. Efficacy of clonidine and of methadone in the rapid detoxification of patients dependent on heroin. Clinical Pharmacology and Therapeutics 1985;38(3):336‐41. [DOI] [PubMed] [Google Scholar]
Dawe 1995 {published data only}
- Dawe S, Gray JA. Craving and drug reward: a comparison of methadone and clonidine in detoxifying opiate addicts. Drug and Alcohol Dependence 1995;39(3):207‐12. [DOI] [PubMed] [Google Scholar]
Drummond 1989 {published data only}
- Drummond DC, Turkington D, Rahman MZ, Mullin PJ, Jackson P. Chlordiazepoxide versus Methadone in opiate withdrawal: a preliminary double blind trial. Drug and Alcohol Dependence 1989;23(1):63‐71. [DOI] [PubMed] [Google Scholar]
Gerra 2000 {published data only}
- Gerra G, Zaimovic A, Rustichelli P, Fontanesi B, Zambelli U, Timpano M, et al. Rapid opiate detoxification in outpatient treatment: relationship with naltrexone compliance. Journal of Substance Abuse Treatment 2000;18(2):185‐91. [DOI] [PubMed] [Google Scholar]
Howells 2002 {published data only}
- Howells C, Allen S, Gupta J, Stillwell G, Marsden J, Farrel M. Prison based detoxification for opioid dependence: a randomised double blind controlled trial of lofexidine and methadone. Drug and Alcohol Dependence 2002;67:169‐76. [DOI] [PubMed] [Google Scholar]
Jiang 1993 {published data only}
- Jiang Z. Rapid detoxification with clonidine for heroin addiction. A comparative study on its efficacy vs methadone. Chinese Journal of Neurology and Psychiatry 1993;26(1):10‐3. [Google Scholar]
Kleber 1985 {published data only}
- Kleber HD, Riordan CE, Rounsaville B, Kosten T, Charney D, Gaspari J, et al. Clonidine in outpatient detoxification from methadone maintenance. Archives of General Psychiatry 1985;42(4):391‐4. [DOI] [PubMed] [Google Scholar]
- Kosten RT, Rounsaville J, Kleber HD. Relationship of depression to clonidine detoxification of opiate addicts. Comprehensive Psychiatry 1984;25(5):503‐8. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Rounsaville BJ, Kleber HD. Comparison of clinician ratings to self reports of withdrawal during clonidine detoxification of opiate addicts. American Journal of Drug and Alcohol Abuse 1985;11(1‐2):1‐10. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Kosten T, Kleber H. Success and failure at outpatient opioid detoxification. Evaluating the process of clonidine and methadone assisted withdrawal. Journal of Nervous and Mental Disease 1985;173(2):103‐10. [DOI] [PubMed] [Google Scholar]
Madlung‐Kratzer 2009 {published data only}
- Madlung‐Kratzer E, Spitzer B, Brosch R, Dunkel D, Haring C. A double‐blind, randomised, parallel group study to compare the efficacy, safety and tolerability of slow‐release oral morphine versus methadone in opioid‐dependent in‐patients willing to undergo detoxification. Addiction 2009; Vol. 104, issue 9:1549‐57. [DOI] [PMC free article] [PubMed]
Salehi 2007 {published data only}
- Salehi M, Amanatkar M, Barekatain M. Comparison of the efficacy of methadone and tramadol in opioid‐assisted detoxification. Iranian Journal of Medical Science 2007;32(1):28‐31. [Google Scholar]
- Salehi M, Amanatkar M, Barekatain M. Tramadol versus methadone for the management of acute opioid withdrawal: An add‐on study. Journal of Research in Medical Sciences 2006;11(3):185‐9. [Google Scholar]
San 1990 {published data only}
- San L, Camì J, Peri JM, Mata R, Porta M. Efficacy of clonidine, guanfacine and methadone in the rapid detoxification of heroin addicts: a controlled clinical trial. British Journal of Addiction 1990;85(1):141‐7. [DOI] [PubMed] [Google Scholar]
- San L, Camì J, Peri JM, Mata R, Porta M. Success and Failure at inpatient heroin detoxification. British Journal of Addiction 1989;84(1):81‐7. [DOI] [PubMed] [Google Scholar]
San 1992 {published data only}
- San L, Camì J, Fernandez T, Olle JM, Peri JM, Torrens M. Assessment and management of opioid withdrawal symptoms in buprenorphine‐dependent subjects. British Journal of Addiction 1992;87(1):55‐62. [DOI] [PubMed] [Google Scholar]
San 1994 {published data only}
- San L, Fernandez T, Camì J, Gossop M. Efficacy of methadone versus methadone and guanfacine in the detoxification of heroin addicted patients. Journal of Substance Abuse Treatment 1994;11(5):463‐9. [DOI] [PubMed] [Google Scholar]
Seifert 2002 {published data only}
- Seifert J, Metzner C, Paetzold W, Borsutzky M, Ohlmeir M, Passie T, et al. Mood and affect during detoxification of opiate addicts: a comparison of buprenorphine versus methadone. Addiction Biology 2005;10(2):157‐64. [DOI] [PubMed] [Google Scholar]
- Seifert J, Metzner C, Paetzold W, Borsutzky M, Passle T, Rollnik J, et al. Detoxification of opiate addicts with multiple drug abuse: a comparison of buprenorphine vs methadone. Pharmacopsychiatry 2002;35:159‐64. [DOI] [PubMed] [Google Scholar]
Sorensen 1982 {published data only}
- Sorensen JL, Hargreaves WA, Weinberg JA. Withdrawal from heroin in three or six weeks. Comparison of methadyl acetate and methadone. Archives of General Psychiatry 1982;39(2):167‐71. [DOI] [PubMed] [Google Scholar]
Steinmann 2007 {published data only}
- Steinmann C, Artmann S, Henneberg B, Paul HW. Should methadone or buprenorphine be preferred for opiate detoxification?: [Methadon‐Racemat versus Buprenorphin zur stationären Entgiftungsbehandlung Opiatabhängiger]. Psychiatrische Praxis 2007;34(S1):103‐5. [Google Scholar]
- Steinmann C, Artmann S, Schachtschneider A, Paul HW. Methadone versus buprenorphine for inpatient detoxification treatment [Methadon‐Racemat versus Buprenorphin zur stationaren Entgiftungsbehandlung]. Sucht 2008;54(4):217‐21. [Google Scholar]
Tennant 1975 {published data only}
- Tennant S Jr, Russel BA, Casas SK, Bleick RN. Heroin detoxification. A comparison of propoxyphene and methadone. JAMA 1975;232(10):1019‐23. [DOI] [PubMed] [Google Scholar]
Umbricht 2003 {published data only}
- Umbricht A, Hoover DR, Tucker MJ, Leslie JM, Chaisson RE, Preston KL. Opioid detoxification with buprenorphine, clonidine or methadone in hospitalized heroin dependent patients with HIV infection. Drug and Alcohol Dependence 2003;69:263‐72. [DOI] [PubMed] [Google Scholar]
Washton 1981 {published data only}
- Washton AM, Resnick RB. Clonidine versus methadone for opiate detoxification. Lancet 1980;2(8207):1297. [DOI] [PubMed] [Google Scholar]
- Washton AM, Resnick RB. Clonidine vs methadone for opiate detoxification: double‐blind outpatient trials. In: Harris LS editor(s). NIDA Research Monograph. Vol. 34, Washington DC: Department of Health and Human Services, 1981:89‐94. [PubMed] [Google Scholar]
Wright 2011 {published data only}
- Sheard L, Wright NM, Adams CE, Bound N, Rushforth B, Hart R, et al. The Leeds Evaluation of Efficacy of Detoxification Study (LEEDS)Prisons Project Study: protocol for a randomised controlled trial comparing methadone and buprenorphine for opiate detoxification. Trials 2009;10:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright NM, Sheard L, Adams CE, Rushforth BJ, Harrison W, Bound N, et al. Comparison of methadone and buprenorphine for opiate detoxification (LEEDS trial): a randomised controlled trial. The British Journal of General Practice: the journal of the Royal College of General Practitioners 2011;61(593):772‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yang 2006 {published data only}
- Yang L, Chen J, Li L, Wen P, Zhang X. Controlled clinical study on Paiduyangsheng capsule in detoxification of heroin abuse. Chinese Journal of Drug Abuse Prevention 2006;12(2):86‐8. [Google Scholar]
Zarghami 2012 {published data only}
- Zarghami M, Masoum B, Shiran MR. Tramadol versus methadone for treatment of opiate withdrawal: a double blind, randomised, clinical trial. Journal of Addictive Diseases 2012;31:112‐7. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Albizu‐Garcia 2012 {published data only}
- Albizu‐Garcia CE, Caraballo JN, Caraballo‐Correa G, Hernandez‐Viver A, Roman‐Badenas L. Assessing need for medication‐assisted treatment for opiate‐dependent prison inmates. Substance Abuse 2012;33(1):60‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bakhshani 2008 {published data only}
- Bakhshani NM, Lashkaripour K, Sadjadi SA. A randomised effectiveness trial of methadone, TENS and methadone plus TENS in management of opiate withdrawal symptoms. Journal of the Pakistan Medical Association 2008; Vol. 58, issue 12:667‐71. [PubMed]
Bearn 1998 {published data only}
- Bearn J, Gossop M, Strang J. Accelerated lofexidine treatment regimen compared with conventional lofexidine and methadone treatment for inpatient opiate detoxification. Drug and Alcohol Dependence 1998;50(3):227‐32. [DOI] [PubMed] [Google Scholar]
Bearn 2008 {published data only}
Bell 2009 {published data only}
Bickel 1988 {published data only}
- Bickel WK, Stitzer ML, Bigelow GE, Liebson IA, Jasinski DR, Johnson RE. A clinical trial of buprenorphine: comparison with methadone in the detoxification of heroin addicts. Clinical Pharmacology and Therapeutics 1988;43(1):72‐8. [DOI] [PubMed] [Google Scholar]
Brewin 1989 {published data only}
- Brewin CR, Bradley C. Patient preference and randomised clinical trials. BMJ 1989;299:313‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bux 1993 {published data only}
- Bux DA, Iguchi MY, Lidz V, Baxter RC, Platt JJ. Participation in an outreach‐based coupon distribution program for free methadone detoxification. Hospital and Community Psychiatry 1993;44(11):1066‐72. [DOI] [PubMed] [Google Scholar]
Byrne 2006 {published data only}
- Byrne A, Hallinan R. Is methadone too dangerous for opiate addiction? Methadone is still needed in addiction treatments. BMJ 2006;332(7532):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cameron 2006 {published data only}
- Cameron IM, Matheson CI, Bond CM, McNamee P, Lawrie T, Robinson A, et al . Pilot randomised controlled trial of community pharmacy administration of buprenorphine versus methadone. International Journal of Pharmacy Practice 2006;14(4):243‐8. [Google Scholar]
Critchlow 2006 {published data only}
- Critchlow G, Nadeem H. Abstinence‐oriented treatment for opiate addiction. British Journal of Psychiatry 2006;188:292‐3. [DOI] [PubMed] [Google Scholar]
Dawe 1991 {published data only}
- Dawe S, Griffiths P, Gossop M, Strang J. Should opiate addicts be involved in controlling their own detoxification? A comparison of fixed versus negotiable schedules. British Journal of Addiction 1991;86(8):977‐82. [DOI] [PubMed] [Google Scholar]
De Los Cobos 2000 {published data only}
- Cobos JP, Duro P, Trujols J, Tejero A, Batle F, Ribalta E, et al. Methadone tapering plus amantadine to detoxify heroin dependent inpatients with or without an active cocaine use disorder: two randomised controlled trials. Drug and Alcohol Dependence 2001;63:187‐95. [DOI] [PubMed] [Google Scholar]
Deniker 1975 {published data only}
- Deniker P, Loo H, Zarifian E, Cuche H. A french experience with methadone [A propos d'une expèrience française de la mèthadone]. Encéphale 1975;1(1):75‐91. [PubMed] [Google Scholar]
Dijkstra 2010 {published data only}
- Dijkstra BA, Jong CA, Wensing M, Krabbe PF, Staak CP. Opioid detoxification: from controlled clinical trial to clinical practice. The American Journal on Addictions 2010;19(3):283‐90. [DOI] [PubMed] [Google Scholar]
Ebner 2004 {published data only}
- Ebner R, Schreiber W, Zierer C. Buprenorphine or methadone for detoxification of young opioid addicts? [Buprenorphin oder methadon im entzug junger opiatabhangiger?]. Psychiatrische Praxis 2004;31(S1):108‐10. [DOI] [PubMed] [Google Scholar]
Fulwiler 1979 {published data only}
- Fulwiler RL, Hargreaves WA, Bortman RA. Detoxification from heroin using self vs physician regulation of methadone dose. The International Journal of the Addictions 1979;14(2):289‐98. [DOI] [PubMed] [Google Scholar]
Gerra 2004 {published data only}
- Gerra G, Borella F, Zaimovic A, Moi G, Bussandri M, Bubici C, et al. Buprenorphine versus methadone for opioid dependence: predictor variables for treatment outcome. Drug and Alcohol Dependence 2004;75:37‐45. [DOI] [PubMed] [Google Scholar]
Gerra 2007 {published data only}
- Gerra G, Zaimovic A, Raggi MA, Moi G, Branchi B, Moroni M, et al. Experimentally induced aggressiveness in heroin‐dependent patients treated with buprenorphine: comparison of patients receiving methadone and healthy subjects. Psychiatry Research 2007;149(1‐3):201‐13. [DOI] [PubMed] [Google Scholar]
Glasper 2008 {published data only}
- Glasper A, Gossop M, Wet C, Reed L, Bearn J. Influence of the dose on the severity of opiate withdrawal symptoms during methadone detoxification. Pharmacology 2008;81(2):92‐6. [DOI] [PubMed] [Google Scholar]
Goldstein 1972 {published data only}
- Goldstein A. Heroin addiction and the role of methadone in its treatment. Archives of General Psychiatry 1972;26:291‐7. [DOI] [PubMed] [Google Scholar]
Gossop 1989A {published data only}
- Gossop M, Griffiths P, Bradley B, Strang J. Opiate withdrawal symptoms in response to 10 day and 21 day methadone withdrawal programmes. British Journal of Psychiatry 1989;154:360‐3. [DOI] [PubMed] [Google Scholar]
Green 1988 {published data only}
- Green L, Gossop M. Effects of information on the opiate withdrawal syndrome. British Journal of Addiction 1988;83(3):305‐9. [DOI] [PubMed] [Google Scholar]
Greenwald 2006 {published data only}
- Greenwald MK. Early impact of methadone induction for heroin dependence: differential effects of two dose sequences in a randomised controlled study. Experimental and Clinical Psychopharmacology 2006;14(1):52‐67. [DOI] [PubMed] [Google Scholar]
Gruber 2008 {published data only}
- Gruber VA, Delucchib KL, Kielsteinc A, Batkid SL. A randomised trial of six‐month methadone maintenance with standard or minimal counselling versus 21‐day methadone detoxification. Drug and Alcohol Dependence 2008;94(1‐3):199‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hall 1979 {published data only}
- Hall SM, Bass A, Hargreaves WA, Loeb P. Contingency management and information feedback in outpatient heroin detoxification. Behavior Therapy 1979;10:443‐51. [Google Scholar]
Hall 2008 {published data only}
- Hall WD, Mattick RP. Oral substitution treatments for opioid dependence. Lancet 2008;371(9631):2150‐1. [DOI] [PubMed] [Google Scholar]
Hasson 2007 {published data only}
- Hasson A, Thomas C, Jenkins J, Ling W. Buprenorphine retention in the CTN START study: an unexpected observation. 69th Annual Scientific Meeting of the College on Problems of Drug Dependence. 2007.
Highfield 2007 {published data only}
- Highfield DA, Schwartz RP, Jaffe JH, O'Grady KE. Intravenous and intranasal heroin‐dependent treatment‐seekers: Characteristics and treatment outcome. Addiction 2007;102(11):1816‐23. [DOI] [PubMed] [Google Scholar]
Hser 2012 {published data only}
- Hser YI, Fu L, Wu F, Du J, Zhao, M. Pilot trial of a recovery management intervention for heroin addicts released from compulsory rehabilitation in China. Journal of Substance Abuse Treatment 2012 April 18 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
Jaffe 1972 {published data only}
- Jaffe JH, Senay EC, Schuster CR, Renault PR, Smith B, DiMenza S. Methadyl acetate vs methadone. A double‐blind study in heroin users. JAMA 1972;222(4):437‐42. [PubMed] [Google Scholar]
JI 2007 {published data only}
- JI H, YE S, NIE Z, Zeng Y, Liu Y, XIE L, et al. Clinical research of withdrawal syndrome treatment with phenytoin in heroin addicts. Chinese Journal of Drug Abuse Prevention and Treatment 2006;12(1):28‐30. [Google Scholar]
Johnson 1992 {published data only}
- Johnson RE, Jaffe JH, Fudala PJ. A controlled trial of buprenorphine treatment for opioid dependence. JAMA 1992;267(20):2750‐5. [PubMed] [Google Scholar]
Kheirabadi 2008 {published data only}
Krabbe 2003 {published data only}
- Krabbe PF, Koning JP, Heinen N, Laheij RJ, Cauter V, Jong CA. Rapid detoxification from opioid dependence under general anaesthesia versus standard methadone tapering: abstinence rates and withdrawal distress experiences. Addiction Biology 2003;8:349‐56. [DOI] [PubMed] [Google Scholar]
Kristensen 2005 {published data only}
- Kristensen O, Espegren O, Asland R, Jakobsen E, Lie O, Seiler S. A randomised clinical trial of methadone vs. buprenorphine to opioid dependants [Buprenorfin og metadon til opiatavhengige‐ en randomisert studie]. Tidsskrift for Den Norske Laegeforening 2005;125(2):148‐51. [PubMed] [Google Scholar]
Lal 1976 {published data only}
- Lal B, Singh G. Experiences of a methadone detoxification programme for opium addicts. Drug and Alcohol Dependence 1976;1(6):391‐8. [DOI] [PubMed] [Google Scholar]
Liu 2009 {published data only}
- Liu TT, Shi J, Epstein DH, Bao YP, Lu L. A meta‐analysis of acupuncture combined with opioid receptor agonists for treatment of opiate‐withdrawal symptoms. Cellular and Molecular Neurobiology 2009;29(4):449‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2009a {published data only}
- Liu TT, Shi J, Epstein DH, Bao YP, Lu L. A meta‐analysis of Chinese herbal medicine in treatment of managed withdrawal from heroin. Cellular and Molecular Neurobiology 2009;29(1):17‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lobmaier 2010 {published data only}
- Lobmaier P, Gossop M, Waal H, Bramness J. The pharmacological treatment of opioid addiction‐‐a clinical perspective. European Journal of Clinical Pharmacology 2010;66(6):537‐45. [DOI] [PubMed] [Google Scholar]
Madden 1986 {published data only}
- Madden C, Singer G, Jagoda J, Jetwa J, Croxford R. Opiate‐seeeking behavior under conditions of methadone detoxification and removal. The International Journal of the Addictions 1986;21(8):947‐53. [DOI] [PubMed] [Google Scholar]
Maddux 1980 {published data only}
- Maddux J, Desmond DP, Esaquivel M. Outpatient methadone withdrawal for heroin dependence. American Journal of Drug and Alcohol Abuse 1980;7:323‐33. [DOI] [PubMed] [Google Scholar]
Mannelli 2008 {published data only}
- Mannelli P, Patkar AA, Peindl K, Gorelick DA, Wu LT, Gottheil E. Very low dose naltrexone addition in opioid detoxification: a randomized, controlled trial. Addiction Biology 2008;14(2):204‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
McCambridge 2006 {published data only}
- McCambridge J, Gossop M, Beswick T, Best D, Bearn J, Rees S, et al. In‐patient detoxification procedures, treatment retention, and post‐treatment opiate use: comparison of lofexidine + naloxone, lofexidine + placebo, and methadone. Drug and Alcohol Dependence 2007;88(1):91‐5. [DOI] [PubMed] [Google Scholar]
McCaul 1984 {published data only}
- Caul ME, Stitzer ML, Bigelow GE, Liebson IA. Methadone detoxification: effects of methadone dose versus time in treatment. NIDA Research Monograph 1984;49:269‐74. [PubMed] [Google Scholar]
Meader 2010 {published data only}
- Meader N. A comparison of methadone, buprenorphine and alpha2 adrenergic agonists for opioid detoxification: A mixed treatment comparison meta‐analysis. Drug Alcohol Dependence 2010;108(1‐2):110‐4. [DOI] [PubMed] [Google Scholar]
Mintz 1975 {published data only}
- Mintz J, O'Brien CP, O'Hare K, Goldschimidt J. Double‐blind detoxification of methadone maintenance patients. The International Journal of the Addictions 1975;10(5):815‐24. [DOI] [PubMed] [Google Scholar]
Mitchell 2012 {published data only}
- Mitchell SG, Kelly SM, Gryczynski J, Myers CP, Jaffe JH, O'Grady KE, et al. African American patients seeking treatment in the public sector: Characteristics of buprenorphine vs. methadone patients. Drug and Alcohol Dependence 2012;122(1‐2):55‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mokhber 2008 {published data only}
- Mokhber N, Soltanifar A, Talebi M. Efficacy of topiramate as an adjunct medication in heroin withdrawal: A randomized control trial. Journal of Pakistan Psychiatric Society 2008;5(1):22‐6. [Google Scholar]
Neale 2005 {published data only}
- Neale J, Robertson M. Recent life problems and non‐fatal overdose among heroin users entering treatment. Addiction 2005;100(2):168‐75. [DOI] [PubMed] [Google Scholar]
O'Connor 1997 {published data only}
- O'Connor PG, Carroll KM, Shi JM, Schottenfeld RS, Kosten TR, Rounsaville BJ. Three methods of opioid detoxification in a primary care setting. Annals of Internal Medicine 1997;127(7):526‐30. [DOI] [PubMed] [Google Scholar]
Pjrek 2012 {published data only}
- Pjrek E, Frey R, Naderi‐Heiden A, Strnad A, Kowarik A, Kasper S, et al. Actigraphic measurements in opioid detoxification with methadone or buprenorphine. Journal of Clinical Psychopharmacology 2012;32(1):75‐82. [DOI] [PubMed] [Google Scholar]
Rawson 1983 {published data only}
- Rawson RA, Mann AJ, Tennant FS Jr, Clabough D. Efficacy of psychotherapeutic counselling during 21‐day ambulatory heroin detoxification. NIDA Research Monograph 1983;43:310‐4. [PubMed] [Google Scholar]
Reed 2007 {published data only}
- Reed LJ, Glasper A, Wet CJ, Bearn J, Gossop M. Comparison of buprenorphine and methadone in the treatment of opiate withdrawal: possible advantages of buprenorphine for the treatment of opiate‐benzodiazepine co dependent patients?. Journal of Clinical Psychopharmacology 2007;27(2):188‐92. [DOI] [PubMed] [Google Scholar]
Reilly 1995 {published data only}
- Reilly PM, Banys P, Tusel DJ, Sees KL, Krumenaker CL, Shopshire MS. Methadone transition treatment: a treatment model for 180‐day methadone detoxification. The International Journal of the Addictions 1995;30(4):387‐402. [DOI] [PubMed] [Google Scholar]
Sees 2000 {published data only}
- Sees LK, Delucchi KL, Masson C, Rosen A, Clark HW, Robillard H, et al. Methadone maintenance vs 180‐day psychosocially enriched detoxification for treatment of opioid dependence. JAMA 2000;283(10):1303‐10. [DOI] [PubMed] [Google Scholar]
Semba 2007 {published data only}
- Semba RD, Ricketts EP, Mehta SF, Kirk GD, Latkin C, Galai N, et al. Adherence and retention of female injection drug users in a phase III clinical trial in inner city Baltimore. American Journal of Drug and Alcohol Abuse 2007;33(1):71‐80. [DOI] [PubMed] [Google Scholar]
Shaygani 2009 {published data only}
- Shaygani S, Waal H. Treatment of opioid withdrawal. Tidsskr Nor Laegeforen 2009;129(2):114‐5. [DOI] [PubMed] [Google Scholar]
Sheard 2006 {published data only}
- Sheard L, Adams CE, Wright NM, El‐Sayeh H, Dalton R, Tompkins CNE. The Leeds Evaluation of Efficacy of Detoxification Study (LEEDS) prisons project pilot study: Protocol for a randomised controlled trial comparing dihydrocodeine and buprenorphine for opiate detoxification. Trials 2007;8(8):1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Soyka 2009 {published data only}
- Soyka M, Zingg C. Feasability and safety of transfer from racemic methadone to (R)‐methadone in primary care: Clinical results from an open study. World Journal of Biological Psychiatry 2009;10(3):217‐24. [DOI] [PubMed] [Google Scholar]
Stimmel 1982 {published data only}
- Stimmel B, Hanbury R, Cohen M. Factors affecting detoxification from methadone. Journal of Psychiatric Treatment and Evaluation 1982;4:377‐81. [Google Scholar]
Stotts 2012 {published data only}
- Stotts AL, Green C, Masuda A, Grabowski J, Wilson K, Northrup TF, et al. A Stage I pilot study of acceptance and commitment therapy for methadone detoxification. Drug and Alcohol Dependence 2012;Mar 14:Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
Strain 1993 {published data only}
- Strain EC, Stitzer M, Liebson IA, Bigelow GE. Dose response effects of methadone in the treatment of opioid dependence. Annals of Internal Medicine 1993;119(1):23‐7. [DOI] [PubMed] [Google Scholar]
Strang 1990 {published data only}
- Strang J, Gossop M. Comparison of linear versus inverse exponential methadone reduction curves in the detoxification of opiate addicts. Addiction Behaviors 1990;15(6):541‐7. [DOI] [PubMed] [Google Scholar]
Strang 1997 {published data only}
- Strang J, Marks I, Dawe S, Powell J, Gossop M, Richards D, et al. Type of hospital setting and treatment outcome with heroin addicts. British Journal of Psychiatry 1997;171:335‐9. [DOI] [PubMed] [Google Scholar]
Sullivan 2004 {published data only}
- Sullivan LE, Chawarski M, O'Connor PG, Schottenfeld RS, Fiellin DA. The practice of office‐based buprenorphine treatment of opioid dependence: is it associated with new patients entering into treatment?. Drug and Alcohol Dependence 2005;79(1):113‐6. [DOI] [PubMed] [Google Scholar]
Teesson 2006 {published data only}
- Teesson M, Havard A, Ross J, Darke S. Outcomes after detoxification for heroin dependence: findings from the Australian Treatment Outcome Study (ATOS). Drug and Alcohol Review 2006;25(3):241‐7. [DOI] [PubMed] [Google Scholar]
Tennant 1978 {published data only}
- Tennant FS Jr, Shannon J A. Detoxification from methadone maintenance: double blind comparison of two methods. Drug and Alcohol Dependence 1978;3:85‐92. [DOI] [PubMed] [Google Scholar]
Van Beek‐Verbeek 1983 {published data only}
- Beek‐Verbeek G, Fraenkel HM, Ree JM. Des‐gly9‐[arg8]‐vasopressin may facilitate methadone detoxification of heroin addicts. Substance and Alcohol Actions/Misuse 1983;4(5):375‐82. [PubMed] [Google Scholar]
Veilleux 2010 {published data only}
- Veilleux JC, Colvin PJ, Anderson J, York C, Heinz AJ. A review of opioid dependence treatment: pharmacological and psychosocial interventions to treat opioid addiction. Clinical Psychology Review 2010;30(2):155‐66. [DOI] [PubMed] [Google Scholar]
Wang 1982 {published data only}
- Wang RI, Kochar C, Hasegawa AT, Roh BL. Clinical comparison of propoxyphene napsylate and methadone in the treatment of opiate dependence. NIDA Research Monograph 1982;41:253‐60. [PubMed] [Google Scholar]
Yang 2008 {published data only}
- Yang Z, Shao YCC, Li S J, Qi JLL, Zhang MJJ, Hao W, et al. Medication of l‐tetrahydropalmatine significantly ameliorates opiate craving and increases the abstinence rate in heroin users: a pilot study. Acta Pharmacologica Sinica 2008;29(7):781‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zeng 2005 {published data only}
- Zeng X, Lei L, Lu Y, Wang Z. Treatment of heroinism with acupuncture at points of the Du Channel. Journal of Traditional Chinese Medicine 2005;25(3):166‐70. [PubMed] [Google Scholar]
Ziaadini 2011 {published data only}
- Ziaadini H, Parvaresh N, Afshar N, Hoseinian SM, Sarhadi R, Hahdoost AA. Comparison of the outcomes of three detoxification methods (clonidin, methadon, rapid) in opioid‐dependents referred to kerman shaheed beheshti hospital in a 6‐month follow‐ up. Journal of Kerman University of Medical Sciences 2011;18(3):246‐59. [Google Scholar]
Additional references
Bradley 1987
- Bradley BP, Gossop M, Phillips GT, Legarda JJ. The development of an Opiate Withdrawal Scale (OWS). British Journal of Addiction 1987;82:1139‐42. [DOI] [PubMed] [Google Scholar]
Dekkers 2009
- Dekkers OM, Elm E, Algra A, Romijn JA, Vandenbroucke JP. How to assess the external validity of therapeutic trials: a conceptual approach. International Journal of Epidemiology 2009;39:89‐94. [DOI] [PubMed] [Google Scholar]
EMCDDA 2011
- European Monitoring Centre for Drugs and Drug Addiction Annual report 2011: the state of the drugs problem in EuropeLuxembourg. Publications Office of the European Union, available at www.emcdda.europa.eu. [DOI: 10.2810/44330] [DOI]
Gerra 1995
- Gerra G, Marcato A, Cavaccari R, Fontanesi B, Delsignore R, Fertonani G, et al. Clonidine and opiate receptor antagonists in the treatment of heroin addiction. Journal of Substance Abuse treatment 1995;12:35‐41. [PubMed] [Google Scholar]
Gossop 1987
- Gossop M, Bradley B, Phillips GT. Investigation of withdrawal symptoms shown by opiate addicts during and subsequent to a 21 day inpatient methadone detoxification procedure. Addictive Behaviors 1987;12:1‐6. [DOI] [PubMed] [Google Scholar]
Gossop 1989B
- Gossop M, Green L, Phillips G, Bradley B. Lapse, relapse and survival among opiate addicts after treatment. British Journal of Psychiatry 1989;154:348‐53. [DOI] [PubMed] [Google Scholar]
Gossop 1990
- Gossop M. The development of a Short Opiate Withdrawal Scale (SOWS). Addictive Behaviors 1990;15:487‐90. [DOI] [PubMed] [Google Scholar]
Gowing 2008
- Gowing L, Ali R, White J. Alpha2 adrenergic agonists for the management of opioid withdrawal. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD002024.pub3] [DOI] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haertzen 1968
- Haertzen CA, Meketon MJ. Opiate withdrawal measured by the Addiction Research Center Inventory (ARCI). Diseases of the Nervous sSystem 1968;29:450‐5. [PubMed] [Google Scholar]
Hall 1999
- Hall W, Lynskey M, Degenhardt L. Heroin use in Australia: its impact on public health and public order. NDARC Monograph No. 42. Sydney, National Drug and Alcohol Research Centre 1999.
Handelsman 1987
- Handelsman L, Cochrane KJ, Aronson M. Two new rating scales for opiate withdrawal. American Journal of Drug and Alcohol Abuse 1987;13:293‐308. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). The Cochrane Collaboration, 2008. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. Available from www.cochrane‐handbook.org..
Himmelsbach 1941
- Himmelsbach CK. The morphine abstinence syndrome, its nature and treatment. Annals of Internal Medicine 1941;15:829‐39. [Google Scholar]
Himmelsbach 1942
- Himmelsbach CK. Clinical studies of drug addiction: physical dependence, withdrawal and recovery. Archives of Internal Medicine 1942;69:766‐72. [Google Scholar]
Jaffe 1990
- Jaffe J. Drug addiction and drug abuse. In: A Gilman, T Rall, A Nies, P Taylor editor(s). The Pharmacological Basis of Therapeutics. 8th edition. New York: Pergamon Press, 1990:522‐73. [Google Scholar]
Kolb 1938
- Kolb L, Himmelsbach CK. Clinical studies of drug addiction III. American journal of Psichiatry 1938;94:759‐99. [Google Scholar]
Peachey 1988
- Peachey J, Lei H. Assessment of opioid dependence with naloxone. British Journal of Addictions 1988;83:193‐201. [DOI] [PubMed] [Google Scholar]
Powell 1990
- Powell J, Gray JA, Bradley BP, Kasvikis Y, Strang J, Barratt L, et al. The effects of cue exposure to drug‐related cues in detoxified opiate addicts: a theoretical review and some new data. Addictive Behavior 1990;15:339‐54. [DOI] [PubMed] [Google Scholar]
Schubert 1984
- Schubert H, Fleischacker W, Meise V, Theohar C. Preliminary results of guanfacine treatment of acute opiate withdrawal. American Journal of Psichiatry 1984;141:1271‐3. [DOI] [PubMed] [Google Scholar]
UNODC 2011
- UNODC, World Drug Report, 2011. Retrieved May 18, 2012, from the United Nation Office on Drug and Crime web site at: http://www.unodc.org.
Valliant 1988
- Valliant GE. What does long‐term follow‐up teach us about relapse and prevention of relapse in addiction?. British Journal of Addiction 1988;83:1147‐57. [DOI] [PubMed] [Google Scholar]
Ward 1992
- Ward J, Mattick RP, Hall W. Key Issues in Methadone Maintenance Treatment. Sydney: New South Wales University Press, 1992. [Google Scholar]
Wesson 2003
- Wesson DR, Ling W. The Clinical Opiate Withdrawal Scale (COWS). Journal of Psychoactive Drugs 2003;35(2):253‐9. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Amato 2003
- Amato L, Davoli M, Ferri M, Ali R. Methadone at tapered doses for the management of opioid withdrawal. Cochrane Database of Systematic Reviews 2003, Issue 2. [DOI: 10.1002/14651858.CD003409.pub2] [DOI] [PubMed] [Google Scholar]
Amato 2005
- Amato L, Davoli M, Minozzi S, Ali R, Ferri M. Methadone at tapered doses for the management of opioid withdrawal. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD003409.pub3] [DOI] [PubMed] [Google Scholar]


