β-Lactam antibiotics have been widely used as therapeutic agents for the past 70 years, resulting in emergence of an abundance of β-lactam-inactivating β-lactamases. Although penicillinases in Staphylococcus aureus challenged the initial uses of penicillin, β-lactamases are most important in Gram-negative bacteria, particularly in enteric and nonfermentative pathogens, where collectively they confer resistance to all β-lactam-containing antibiotics.
KEYWORDS: ESBL, beta-lactamase, carbapenemase, epidemiology, resistance
SUMMARY
β-Lactam antibiotics have been widely used as therapeutic agents for the past 70 years, resulting in emergence of an abundance of β-lactam-inactivating β-lactamases. Although penicillinases in Staphylococcus aureus challenged the initial uses of penicillin, β-lactamases are most important in Gram-negative bacteria, particularly in enteric and nonfermentative pathogens, where collectively they confer resistance to all β-lactam-containing antibiotics. Critical β-lactamases are those enzymes whose genes are encoded on mobile elements that are transferable among species. Major β-lactamase families include plasmid-mediated extended-spectrum β-lactamases (ESBLs), AmpC cephalosporinases, and carbapenemases now appearing globally, with geographic preferences for specific variants. CTX-M enzymes include the most common ESBLs that are prevalent in all areas of the world. In contrast, KPC serine carbapenemases are present more frequently in the Americas, the Mediterranean countries, and China, whereas NDM metallo-β-lactamases are more prevalent in the Indian subcontinent and Eastern Europe. As selective pressure from β-lactam use continues, multiple β-lactamases per organism are increasingly common, including pathogens carrying three different carbapenemase genes. These organisms may be spread throughout health care facilities as well as in the community, warranting close attention to increased infection control measures and stewardship of the β-lactam-containing drugs in an effort to control selection of even more deleterious pathogens.
INTRODUCTION
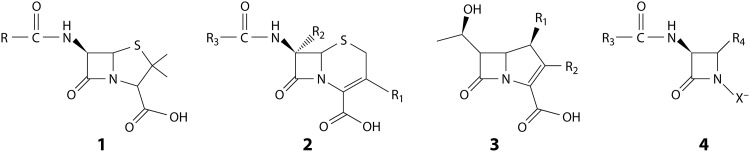
Antibiotics, specifically those in the β-lactam class, are essential to the practice of medicine in the 21st century, where almost two-thirds of recent hospital prescriptions include these agents (1). The most common β-lactam-containing agents belong to four major chemical classes, penicillins, cephalosporins, carbapenems, and monobactams (Fig. 1). Because these agents are so valuable, the medical community is quite alarmed that resistance to these drugs continues to increase in all parts of the world (1–4). Although resistance patterns may be geographically distinct, the threat remains that any new resistance mechanism may spread rapidly to other areas. For example, the gene encoding the New Delhi metallo-β-lactamase-1 (blaNDM-1), leading to resistance to most β-lactam antibiotics (5), was identified as early as 2006, with its occurrence initially confined to the Indian subcontinent (5–7). However, the gene became globally disseminated in fewer than 5 years of the first known occurrence, due in part to the travel of infected or colonized individuals to Europe, the Middle East, and North America (8). Thus, it is important to monitor resistance as a function of time and location, with the goal of containment of emerging resistance determinants to restricted geographical settings.
FIG 1.
Generic structures of β-lactams most important in clinical medicine. Structures include penicillin (1), cephalosporin (2), carbapenem (3), and monobactam (4).
Much of the resistance to β-lactams is due to the enzymes that inactivate these molecules, i.e., the β-lactamases, which are discussed in greater detail in this review (9). Both the Centers for Disease Control and Prevention, or CDC (10), and the World Health Organization, or WHO (11), have designated β-lactamase-producing Gram-negative bacteria some of the world’s most serious or critical threats. Pharmaceutical efforts to contain or subvert these enzymes by designing new molecules with expanded clinical applications have resulted in scientific, and some clinical, success. In the past decade, six new β-lactam-containing agents have been approved by the FDA: ceftaroline, ceftolozane-tazobactam, ceftazidime-avibactam, meropenem-vaborbactam, imipenem-cilastatin-relebactam, and cefiderocol (12, 13) (https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-complicated-urinary-tract-and-complicated-intra-abdominal-infections); four of these are β-lactam antibiotics paired with a β-lactamase-inhibitor to deter a β-lactamase from inactivating the antibiotic (13).
Although several recent reviews have described the almost 3,000 unique, naturally occurring β-lactamases in various epidemiological contexts (9, 13–20), this review contains updated information about the global prevalence of the most prominent of these enzymes. The kinds of organisms that produce β-lactamases include environmental bacteria, such as the Bacillus spp., but the role of these enzymes in clinical medicine is more relevant and far-reaching. Once thought to be primarily a concern in hospital-acquired infections, β-lactamases are now found in many community settings in patients of all ages. Colonization with β-lactamase-producing pathogens is found not only in hospitals but also in health care centers, as well as in the general population. Some specific β-lactamases, such as the plasmid-encoded TEM-, SHV-, and OXA-type enzymes, are ubiquitous, even in contemporary isolates (21). However, other enzymes have been identified only in one specific niche with little or no dissemination, such as the SPM-1 metallo-β-lactamase (MBL), which has not been identified outside Brazil, with the exception of a Swiss patient hospitalized initially in Brazil (22). It is important to note the sources and dissemination of the most prominent, and the most deleterious, β-lactamases in order to guide the most effective use of the β-lactam antibiotics in various geographical locations. In this review, the epidemiology of clinically relevant and widely dispersed β-lactamases is presented concerning present and past geographical and temporal differences of β-lactamase-producing human pathogens. Because of the breadth of the topic, only selected references have been cited, with an attempt to include more recent surveillance data when possible. Important trends and suggestions for the future are noted.
β-LACTAM RESISTANCE
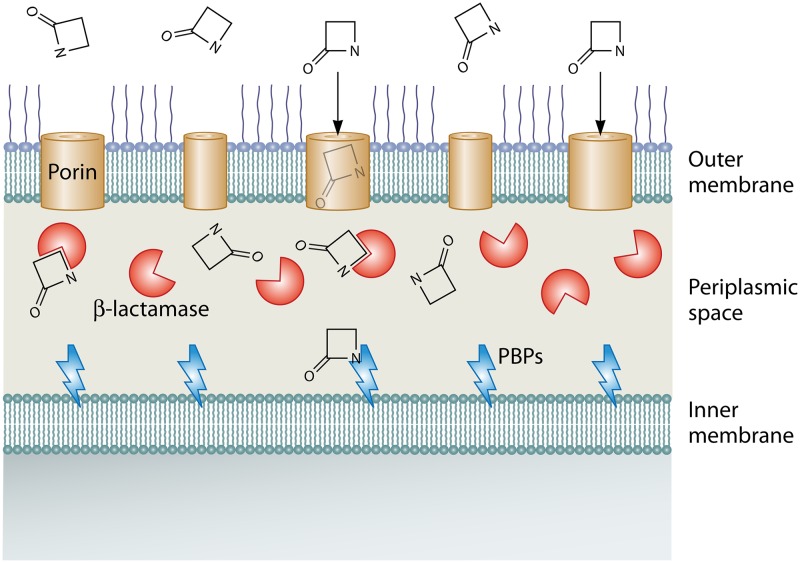
Resistance to the β-lactams can be manifest via multiple mechanisms related to the mechanism of action of these agents (23). β-Lactams serve as surrogate substrates for critical bacterial cell wall-synthesizing proteins, known as penicillin-binding proteins, or PBPs, that are responsible for the cross-linking of cell wall fragments before cell division can occur (24). Although PBPs differ structurally among various species of bacteria, the mechanism of killing is identical, with acylation of an active-site serine in the transpeptidase domain of the PBP as the definitive characteristic of the inhibitory activity (25). As penicillins became an essential component of the hospital armamentarium, Gram-positive pathogens were the first bacteria to exhibit resistance in outbreak proportions. After the introduction of cephalosporins and penicillinase-resistant penicillins, Gram-negative bacteria with their more complex cell wall structure were more likely to develop novel resistance mechanisms. In both sets of organisms, PBP modifications, as well as production of the hydrolytic β-lactamases, especially those that rely on an active serine for catalysis, have played critical roles in the emergence of resistant pathogens. The relationship between mechanism of action and the β-lactamase-associated mechanism of resistance is exemplified in the representation of a Gram-negative bacterial cell in Fig. 2. In this illustration, the β-lactam can bind to a PBP anchored on the inner membrane of the cell to prevent cell growth and division, unless it is intercepted and inactivated by a β-lactamase in the periplasmic space. In both cases, the β-lactam reacts to form a reactive intermediate that may be hydrolyzed rapidly, as in the case of the β-lactamases, with half-lives measured in fractions of a second (26), or slowly, as for PBPs that remain catalytically nonfunctional for sufficient periods to facilitate bacterial cell death; e.g., the half-life for a penicillin-transpeptidase complex in Streptomyces spp. has been recorded as high as 900 min (27). As discussed below, other mechanisms may also be operative.
FIG 2.
Schematic showing the interaction of β-lactam antibiotics with β-lactam interactive proteins in Gram-negative bacteria.
β-Lactamases
Several recent reviews have appeared describing the role of β-lactamases as the predominant β-lactam resistance determinant in Gram-negative bacteria (9, 13, 28, 29). Briefly, these enzymes eliminate the killing activity of β-lactams by binding the drug, breaking the amide bond of the four-membered azetidinone ring present in every β-lactam (Fig. 1), and adding a water molecule to the ring-opened molecule. Distinct mechanisms exist for β-lactamases that utilize an active-site serine for hydrolysis and enzymes that require at least one divalent Zn atom for hydrolysis. The serine β-lactamases function by initially forming a covalent acylated enzyme, whereas in MBLs, formation of a noncovalent reactive complex with the β-lactam is facilitated by Zn2+. Notably, the resulting product from both reactions is the identical microbiologically inactive molecule that is incapable of forming an enzymatically productive complex with a PBP. The result is continued survival of the bacterial cell. More detailed descriptions of the hydrolysis mechanisms for the two groups of enzymes have recently been reviewed (13, 30–32).
Nomenclature for β-lactamases is based on two major attributes of the physiologically important enzymes, i.e., structure and function. Structural classes were first defined by Ambler in 1980 (33), using the four β-lactamase amino acid sequences known at the time to describe class A enzymes, with a serine in the active site, and class B MBLs (33). Since then, class C and class D serine-based β-lactamases have been defined, based on molecular size and distinctive homologous motifs (34, 35). Modifications to the Ambler scheme were recently proposed by Philippon et al., who have suggested subclasses of class A β-lactamases (36). Functional classification schemes have been described for over 50 years based on biochemical attributes, such as substrate profiles, relative hydrolysis rates compared to that of reference β-lactams, and interactions with inhibitors (37). Updated functional nomenclature based on a combination of biochemical attributes and structural class assignments was proposed in 1995 by Bush et al. (38), with additional subgroups added in 2010 by Bush and Jacoby (39). Other functional names are widely used to describe β-lactamases that span more than one group or class. For example, carbapenemases, β-lactamases that are capable of hydrolyzing carbapenems at a rate that is clinically relevant, may belong to structural class A, B, or D, or they may belong to functional group 2df or 2f or group 3 (39). Extended-spectrum β-lactamases, or ESBLs, may include class A, C, or D enzymes, or they may be categorized as groups 1e, 2be, 2de, and 2e (39). A listing of the most important β-lactamases described in this review is shown in Table 1 together with the nomenclature used to describe these enzymes.
TABLE 1.
Nomenclature of clinically important enzymes named in this reviewd
| Molecular class or subclass | Functional group or subgroup | Common namea | Clinically relevant enzyme(s) or enzyme family(ies) | Characteristic substrate profileb | Characteristic inhibitor profilec |
|---|---|---|---|---|---|
| A | 2a | Penicillinase | PC1/blaZ | Narrow-spectrum PENs | CA, TZB |
| A | 2b | Penicillinase | TEM-1, SHV-1 | Narrow-spectrum PENs, early CEPHs | CA, TZB |
| A | 2be | ESBL | TEM-10, SHV-2, CTX-M-15 | Narrow-spectrum PENs, early CEPHs, ES-CEPHs, monobactams | CA, TZB, AVI |
| A | 2br | IRT | TEM-30 (IRT-2) | PENs, early CEPHs | TZB, AVI |
| A | 2e | ESBL cephalosporinase | CepA | ES-CEPHs | CA but not ATM |
| A | 2f | Carbapenemase | KPC | All FDA-approved β-lactams | AVI, REL, VAB |
| A | 2f | Carbapenemase | SME | PENs, early CEPHs, carbapenems, monobactams; not ES-CEPHS | CA, AVI, VAB |
| B1, B3 | 3a | MBL, carbapenemase | IMP, NDM, VIM, SPM | All PENs, CEPHs, carbapenems; not monobactams | EDTA; no clinically approved inhibitor |
| B2 | 3b | MBL, carbapenemase | L1, CphA | Carbapenems preferred | EDTA; no clinically approved inhibitor |
| C | 1 | Cephalosporinase | AmpC | CEPHs | ATM, AVI, VAB |
| D | 2d | Oxacillinase | OXA-1 | PENs, especially oxacillin/cloxacillin | Variable |
| D | 2df | Carbapenemase | OXA-23, OXA-48, OXA-181, OXA-232 | PENs, especially oxacillin/cloxacillin, carbapenems | AVI (OXA-48) |
ESBL, extended-spectrum β-lactamase; IRT, inhibitor-resistant TEM; MBL, metallo-β-lactamase.
CEPH, cephalosporin; ES-CEPHS, expanded-spectrum cephalosporins; PEN, penicillin.
ATM, aztreonam; AVI, avibactam; CA, clavulanic acid; REL, relebactam; TZB, tazobactam; VAB, vaborbactam.
Nomenclature is based on the Bush and Jacoby scheme (39).
Non-β-Lactamase-Mediated Resistance
Although β-lactam resistance is most commonly associated with β-lactamase production in Gram-negative bacteria, other resistance mechanisms may also be operative in both Gram-negative and Gram-positive organisms. The most obvious mechanism is due to production of low-affinity PBPs, which require large inhibitory amounts of β-lactams for bacterial killing. In Gram-positive bacteria, mosaic low-affinity PBPs may occur, as in Streptococcus pneumoniae (40), or there may be acquisition of a rogue PBP, such as PBP2a (or PBP2′), encoded by the mecA gene in Staphylococcus aureus and resulting in methicillin-resistant S. aureus, or MRSA (41, 42). Mutations in essential PBPs in Gram-negative bacteria occur less frequently than other resistance mechanisms but have been reported in Haemophilus influenzae, Pseudomonas aeruginosa, and E. coli clinical isolates (43–46).
In Gram-negative bacteria, non-β-lactamase-associated resistance mechanisms that limit intracellular drug concentrations are common. Decreased penetration into the cell can be caused by mutations in the genes encoding outer membrane proteins (OMPs) that serve as porins, the water-filled channels through which β-lactams can traverse the outer membrane (Fig. 2). These mutations may involve changes in the regulatory mechanisms affecting OMP production, or they may result in nonfunctional or deleted porins, as reported for OMPs in the Enterobacteriaceae and for OprD production in P. aeruginosa (47–50). Concurrent with defective porins, resistance may also occur due to the upregulation of efflux pumps, such as AcrAB-TolC in the enteric bacteria or the multidrug efflux (Mex) pumps in P. aeruginosa, and is exacerbated by the presence or hyperproduction of β-lactamases (51–54).
Resistance Emergence
Treatment with β-lactam antibiotics disrupts the microbial flora of the patient being treated, sometimes resulting in the development of resistance in not only the infection-causing pathogen but also in the organisms comprising the normal flora. This subsequently affects the environment and people surrounding the patient. This means that not only the hospital unit but also health care workers and, subsequently, their immediate contacts are affected by the development of resistance. Furthermore, groups of people in close proximity, such as in day care centers or in long-term care facilities, are affected by the use of antibiotics that select for transmissible β-lactam-resistant organisms, either as colonizing bacteria or as infecting pathogens that can freely move between the community and the hospital (55, 56).
Resistance to β-lactams can develop in previously susceptible organisms through mutations in genes encoding naturally occurring chromosomally encoded β-lactamases or by acquisition of foreign DNA encoding new β-lactamases (17, 23). As bacterial pathogens grow, chromosomal and plasmid DNA replicates through a process that is highly prone to errors concerning base incorporation, leading to nucleotide substitutions that occur randomly at a frequency of approximately 10−9 per gene (57). Exposure to the β-lactam antibiotic does not cause the mutations but rather selects for strains that mutate during normal replication cycles, thereby allowing the mutated bacterial cell to survive in the presence of the antibiotic. In β-lactamases, a single-nucleotide mutation leading to one amino acid change can greatly alter the functionality of an enzyme. Examples include the emergence of the first extended-spectrum β-lactamase (ESBL), in which glycine was substituted for Ser238 in the SHV-1 β-lactamase, resulting in SHV-2, which was resistant to expanded-spectrum cephalosporins (58, 59). A more recent example is the discovery of K. pneumoniae carbapenemase 35 (KPC-35), which contains a single leucine-to-proline substitution from KPC-2, resulting in reduced susceptibility to ceftazidime-avibactam (60).
In addition to random point mutations, replication errors may lead to deletions of a few base pairs of a gene, leading to inactive protein. Furthermore, mobile elements can insert DNA into genes or regulatory elements, thereby affecting the interaction of antibacterial agents with the bacterial target or altering the level of gene expression. Maintenance of a mutation causing antibiotic resistance in a bacterial pathogen is solely dependent upon how that mutation affects the fitness or virulence of that organism. When resistant mutants emerge that are still able to replicate and cause disease, they can gain a foothold in the population that is maintained by continued use of that antibiotic (61).
The most common way that bacteria become resistant to β-lactam antibiotics is through the acquisition of genes expressing β-lactamases (62). DNA transfer among bacteria primarily occurs through the acquisition of plasmids, some of which are self-transmissible, in that they carry genes to initiate the direct transfer to another bacterial cell. These large transferrable plasmids can accommodate multiple resistance genes and are the ideal vector for the dissemination of resistance genes. Within plasmids, resistance genes are often carried by transposons, which can transfer determinants between plasmids or transport them into and out of the chromosome (63). These genes are often a part of an integron that can acquire and express resistance determinants behind a single promoter. Many β-lactamase genes, particularly metallo-carbapenemases, can exist as gene cassettes inserted into integrons (63–65).
Among bacterial pathogens, dissemination of resistance genes contained in plasmids, transposons, and integrons has resulted in so-called gene epidemics (61). TEM-1, the first plasmid-encoded β-lactamase described in the literature, in 1965, originated in an E. coli isolate from a patient in Greece but has spread globally to multiple bacterial species (66, 67). It has been found in up to 70% of clinical isolates of Enterobacteriaceae, in a few Pseudomonas aeruginosa isolates, and in 30% of Neisseria gonorrhoeae isolates (67–69). In Japan and France, the prevalence of TEM-1 in H. influenzae declined after the adoption of the type B vaccine (70, 71), but the occurrence of TEM-1-producing strains in Sweden remained relatively constant between 2002 and 2010 (72). In all the reports, numbers of β-lactamase-negative, ampicillin-resistant isolates increased over time. In addition, multiple TEM-bearing plasmids in H. influenzae have been shown to affect fitness differently, also contributing to the loss of the TEM-1 enzyme (73).
Many of the β-lactamases now found on mobile elements are believed to have originated in the chromosomes of other bacterial species. A few examples include SHV-type β-lactamases, which are derived from a chromosomal SHV-1 β-lactamase of K. pneumoniae; the plasmid-encoded AmpC enzymes expressed in K. pneumoniae and E. coli, which are nearly identical to chromosomal AmpC genes found in Enterobacter cloacae complex (ACT-1 and MIR-1), Citrobacter freundii (CMY type), Hafnia alvei (ACC-1), and Morganella morganii (DHA-1); and the most common contemporary ESBL, the cefotaxime-hydrolyzing β-lactamase CTX-M type, which appears to have originated from Kluyvera spp. (59, 74–76).
Bacterial resistance to β-lactam antibiotics primarily results from modification of the target penicillin-binding proteins, decreased intracellular concentrations due to reduced permeability or efflux, or inactivation of the antibiotic from β-lactamases, which is the most common mechanism. Innate resistance to β-lactams occurs in certain pathogens. As a consequence, entire species of bacterial pathogens have been selected following repeated exposure to antibiotics due to this innate resistance. In addition, the introduction of new therapies has sometimes led to the unexpected consequence of shifting the etiology of some of the common hospital-based infections to species that are naturally more resistant than the pathogens they replaced. For example, carbapenemase-producing Acinetobacter baumannii and Stenotrophomonas maltophilia have become increasingly prevalent in many intensive care units (ICUs) following the increased use of carbapenems, especially among patients with mechanical ventilation (77–80).
EPIDEMIOLOGY OF β-LACTAMASE-PRODUCING PATHOGENS
Bacteria Producing Species-Specific β-Lactamases
Gram-positive bacteria.
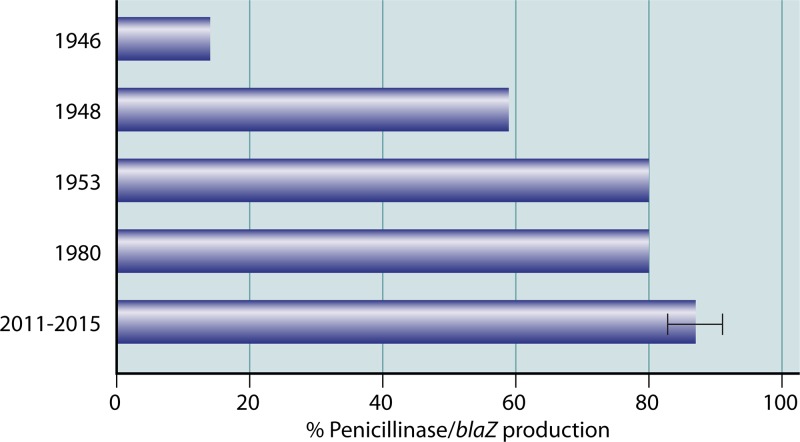
Penicillin was first utilized clinically to treat infections caused by streptococci, followed by its use against staphylococcal infections in the early 1940s. “Penicillinase” activity was first reported in 1940 in a “Bacillus” (Escherichia) coli strain but was not clinically relevant at the time (81). However, shortly thereafter, penicillin resistance was reported in the staphylococci due to a structurally different “penicillin inactivator” (82, 83). Resistant strains increased rapidly thereafter. In the late 1940s, penicillin resistance in S. aureus was monitored in St. Thomas’s Hospital in London over a 5-year period, with an increase from 14% in 1946 to 59% in 1948 (84). By 1953, 80% of hospital staphylococci were reported to be penicillin resistant, presumably due to penicillinase production (85). As shown in Fig. 3, penicillinase production in methicillin-susceptible S. aureus (MSSA) plateaued at approximately 80 to 85% by 1980 (86, 87). The most recent studies report between 83.8% and 91% of MSSA isolates producing the penicillinase gene blaZ from locations as diverse as Trinidad, Kuwait, China, and the United States (88–91). An exception to this trend is in Sweden, where only 43% of MSSA isolates in 2008 to 2009 were penicillinase producers, increasing to 71% in 2014 to 2015 (92). Note that essentially all MRSA isolates are penicillinase positive due to the close relationship between regulators of the defining MRSA mecA and the staphylococcal blaZ genes (93, 94). At least four different functional types of staphylococcal penicillinases have been described (95), but there has been only limited interest in the past 20 years in pursuing the molecular characteristics or additional epidemiology associated with these enzymes (96). Although the staphylococcal blaZ appeared briefly in rare Enterococcus faecalis isolates beginning in the 1980s (97, 98), the gene appears to have been lost from the enterococcal clonal complex responsible for multiple small outbreaks worldwide (99). There have been no recent reports of its presence (100). Likewise, no β-lactamases have been identified among the streptococci.
FIG 3.
Prevalence of penicillinase (blaZ)-producing staphylococci from global sources. Data for the years 1946 to 1980 were from references 84 and 85. Data for the years 2011 to 2017 include studies from Trinidad and Tobago (88), Kuwait (89), China (90), and the United States (91), with the range of percentages shown by the error bars.
Gram-negative fermentative bacteria.
AmpC β-lactamases belong to Ambler class C and Bush-Jacoby-Medeiros functional group 1. In addition to penicillins and early cephalosporins, they also confer resistance to the oxyimino-cephalosporins, such as ceftazidime, cefotaxime, and ceftriaxone, the monobactams, and cephamycins, such as cefoxitin (39, 101). Most class C enzymes are not inhibited by classical inhibitors clavulanate, sulbactam, and tazobactam; however, they are efficiently inhibited by the newer inhibitors avibactam, relebactam, and vaborbactam (102). In addition, class C enzymes are inhibited by aztreonam (38, 103). Class C β-lactamases tend to have a larger active site than do class A enzymes, which may allow them to bind the bulky side chains of the expanded-spectrum oxyiminocephalosporins (104).
AmpC enzymes are most often found as chromosomal β-lactamases that are produced by many species of Gram-negative bacteria (101). In clinical isolates of C. freundii, Enterobacter aerogenes, E. cloacae complex, and Serratia marcescens, AmpC enzymes are particularly important because they are inducible in these species. There is usually low-level basal expression of AmpC, which becomes high level upon exposure to certain β-lactams. In its natural state, the expression of AmpC is under the control of the repressor gene ampR, encoding a member of the LysR transcriptional regulator family. Repression and activation are closely linked to the processes of cell wall peptidoglycan synthesis and breakdown and involve a complex system with several additional genes, including ampD and ampG (105, 106). A mutation in any of the regulatory genes can result in constitutive upregulation of the AmpC β-lactamase. One or more mutations in ampD is the most common cause of constitutive high-level expression of AmpC hyperexpression in clinical isolates (107). Several species, including E. coli and Shigella spp., possess a chromosomally encoded AmpC but lack the repressor ampR gene, rendering the gene noninducible (101). The AmpC β-lactamase is usually produced at low levels in these organisms and rarely contributes to β-lactam resistance.
The genes encoding AmpC β-lactamases have been mobilized and are now widely found in plasmids. The first plasmid-encoded AmpC variant was identified in 1989 from K. pneumoniae isolated in South Korea from a patient with a wound infection. The isolate was notable because of its high degree of resistance to cefoxitin; the enzyme responsible for this resistance was named CMY-1, because phenotypically it was a cephamycinase (108). Within the next decade, several families of plasmid-encoded AmpC variants were reported, especially in clinical isolates, of K. pneumoniae and E. coli. Based on DNA sequence homology, the source of plasmid-based ampC genes has been attributed to several genera of bacteria, with a number of AmpC families reported (101). The following AmpC families have been described: two families of CMY β-lactamases (CMY-1 and CMY-2) originated from Aeromonas hydrophila and C. freundii, respectively; FOX- and MOX-type enzymes are derived from Aeromonas spp.; the ACC family originated from H. alvei; the LAT family of cephalosporinases arose from C. freundii; the MIR and ACT families originated from Enterobacter spp.; and the DHA family stemmed from M. morganii (74, 101, 109). These plasmid-mediated enzymes are often expressed constitutively at high levels due to strong promoters and high gene copy numbers. Plasmid-mediated class C β-lactamases have been detected in numerous genera of Enterobacteriaceae, including K. pneumoniae, E. aerogenes, Salmonella enterica serotype Senftenberg, E. coli, Proteus mirabilis, M. morganii, and Klebsiella oxytoca. Strains expressing plasmid-encoded AmpC enzymes can also become resistant to carbapenems with the loss of outer membrane porin proteins in clinical isolates of K. pneumoniae and S. enterica (75, 110–112).
Nonfermentative bacteria.
(i) Aeromonas spp.
The various species of Aeromonas produce multiple chromosomally mediated β-lactamases from molecular classes B, C, and D and can be uniquely species specific (113). A variety of class C AmpC-type β-lactamases have been characterized from Aeromonas spp., including CepS from A. hydrophila (originally misidentified as Aeromonas veronii bv. sobria), AsbA1 from Aeromonas jandaei, CepH from A. hydrophila, CAV-1 from Aeromonas caviae, MOX-4 from A. caviae, and TRU-1 from Aeromonas enteropelogenes (113). As with most other chromosomally encoded AmpC enzymes, these β-lactamases are under regulatory control that allows for induction of the enzyme and the selection of derepressed mutants that express high levels of enzyme (114). Many species of Aeromonas carry the metallo-β-lactamase CphA, which has a unique substrate profile, in that it inactivates penems and carbapenems but not penicillins and cephalosporins (115). CphA is discussed in more detail in the carbapenemase section.
(ii) Acinetobacter spp.
Acinetobacter spp., especially the Acinetobacter calcoaceticus-A. baumannii complex, also carries an intrinsic gene encoding AmpC, which is called blaADC, for Acinetobacter-derived cephalosporinase (116). The ampC gene of A. baumannii was first described and sequenced in 2000 (117). Increased resistance to expanded-spectrum cephalosporins can occur when ADC becomes overexpressed due to the acquisition of a strong promoter located on the insertion element ISAba1, which targets a specific position upstream of the intrinsic ampC gene of A. baumannii (118). The gene encoding ADC is highly variable, and the majority of the variations in the amino acid sequence do not alter the spectrum of resistance (119). A database has been established to track the various alleles of ADC (120).
Chromosomally encoded class D OXA-type β-lactamases are intrinsic to several species of Acinetobacter, including A. baumannii, A. calcoaceticus, Acinetobacter pittii, and Acinetobacter lwoffii (116). Virtually all A. baumannii isolates possess the gene encoding OXA-51 or one of its related variants that confer very low carbapenem resistance (121, 122). The expression of this β-lactamase becomes increased when mobile elements like the insertion sequence ISAba1 are positioned upstream of this gene in an opposite orientation and act as promoter sequences (121). OXA-23, the first OXA-type enzyme with higher carbapenemase activity discovered in A. baumannii, was described in 1985 and was originally named ARI-1 (123). Other OXA carbapenemases have been reported in A. baumannii, such as OXA-58, OXA-24/-40, and OXA-143, but other than OXA-51, OXA-23 remains the most common (121, 124). Sequencing and phylogenetic comparisons have revealed that these enzymes fall into 18 groups and that the acquisition of blaOXA genes by Acinetobacter spp. was ancient (116). A survey of clonality in 2013 reported that the predominant clonal type shifted from clonal cluster 3 to clonal cluster 2, a cluster highly associated with carbapenem resistance mediated by OXA-23 (125). A case-controlled study in Pittsburgh, where CC2 is prevalent, found that the mortality rate of patients with cancer and these multidrug-resistant A. baumannii infections was 41.9%, compared to 29.0% for the control group (126). Other localized health care sites have reported a greater diversity of infection-causing Acinetobacter clones depending on the source of the index cases, with as many as four different clonal types isolated from a single patient (127, 128).
(iii) Burkholderia spp.
The majority of clinical isolates of Burkholderia pseudomallei complex possess a chromosomally encoded class A β-lactamase called PenA, an enzyme that confers resistance to penicillins and early-generation cephalosporins (129). Although ceftazidime is the treatment of choice for this organism, mutations in PenA have led to resistance in both ceftazidime and clavulanate (130). PenA has also been described in the Burkholderia cepacia complex. In a study of clinical isolates of Burkholderia multivorans from cystic fibrosis patients, 90% of the strains were susceptible to ceftazidime-avibactam, suggesting that this combination is useful in treating strains expressing PenA (131).
(iv) Pseudomonas aeruginosa.
Chromosomally encoded inducible AmpC β-lactamases are also found in nonfermentative Gram-negative pathogens. In P. aeruginosa, the chromosomally encoded AmpC, called PDC, contributes to the natural resistance to aminopenicillins as well as early cephalosporins (132). Similar to what is seen in the Enterobacteriaceae, mutations in the regulatory genes involving peptidoglycan recycling can lead to the hyperproduction of AmpC, resulting in resistance to antipseudomonal penicillins, such ticarcillin, piperacillin, and aztreonam, and late-generation cephalosporins, such as ceftazidime and cefepime (133). Mutations in the genes encoding AmpC as well as changes in OMPs and efflux pumps can also contribute to resistance to cefepime (133). PDC enzymes are highly variable in sequence, which translates into variations in spectrum of activity. Some of the variants have been noted to provide resistance to imipenem and newer β-lactam–β-lactamase inhibitor combinations, such as ceftolozane-tazobactam (134). The chromosome of P. aeruginosa may also contain genes for OXA-type β-lactamases, including OXA-50 (135, 136).
(v) Stenotrophomonas maltophilia.
S. maltophilia produces two chromosomally encoded β-lactamases, L1, a metallo-β-lactamase, and L2, a class A cephalosporinase inhibited by clavulanate (137, 138). Both enzymes are inducible and utilize some of the same regulatory genes that control AmpC-type β-lactamases; however, the response to induction is different for the two enzymes (139, 140). The L1 and L2 β-lactamases confer resistance to virtually all β-lactams, although newer β-lactam–β-lactamase combinations, such as aztreonam-avibactam, may be useful in the future due to the stability of aztreonam to hydrolysis by L1 and the inhibition of L2 cephalosporinase by avibactam (141). There is an increased incidence of infections caused by S. maltophilia in the hospital setting, especially among immunocompromised patients, resulting in increased mortality attributed to this organism (142). A recent genetic study of 130 S. maltophilia clinical isolates from the United States revealed 90 different sequence types with 34 and 43 novel variants of the L1 and L2 β-lactamases, respectively (80). Unfortunately, functional information was not provided to describe the effects of the mostly conservative amino acid substitutions found in the variants.
Anaerobic bacteria.
Anaerobic bacteria produce several species-specific β-lactamases that confer resistance to many noncarbapenem β-lactams. A chromosomal class A β-lactamase, designated DES-1, has been identified in some, but not all, Desulfovibrio desulfuricans strains, an organism phylogenetically related to Bacteroides spp. (143). This enzyme is most closely related to PenA from Burkholderia pseudomallei and provides resistance to ureidopenicillins and expanded-spectrum cephalosporins. A class D β-lactamase named FUS-1 (OXA-85) has been characterized from Fusobacterium nucleatum subsp. polymorphum strains resistant to penicillin and amoxicillin (144). The blaFUS-1 gene is located on the chromosome and shares the closest ancestral relationship with OXA-63 from Brachyspira pilosicoli (53% identity). β-Lactamases have also been described for the anaerobic Gram-positive organism Clostridium difficile (145). Whole-genome sequencing revealed an open reading frame annotated as a putative β-lactamase gene with conserved amino acid sequence motifs characteristic of class D β-lactamases, which was subsequently named blaCDD. This β-lactamase is inducible and provides broad-spectrum activity against various β-lactam antibiotics, including penicillins and expanded-spectrum cephalosporins.
Gram-Negative Bacteria Producing Plasmid-Encoded ESBLs
Nomenclature.
In 1989, Bush defined group 2b′, subsequently called group 2be, enzymes as “β-lactamases that are capable of hydrolyzing aminothiazoleoxime β-lactam antibiotics, or the ‘extended-broad-spectrum’ antibiotics, at rates at least 10% that of benzylpenicillin and that are strongly inhibited by clavulanic acid” (38, 146). This definition originally included enzymes such as the chromosomal K1 β-lactamase from K. oxytoca; in 2010, the designation was expanded by Bush and Jacoby to include subgroups of class A, class C, and class D enzymes (39). However, other investigators believe the designation should refer to those plasmid-encoded β-lactamases that have emerged only from molecular class A enzymes belonging to functional group 2b, capable of hydrolyzing penicillins as well as narrow- and expanded-spectrum cephalosporins (38, 39). Traditional ESBLs are inhibited by the older β-lactamase inhibitors clavulanate, sulbactam, and tazobactam, as well as by more recently FDA-approved inhibitors, such as avibactam, relebactam, and vaborbactam. In the early ESBL definition, inhibition by clavulanate was a requirement for inclusion in this group, but in recent years, this prerequisite has been challenged by the diversity of the enzymes characterized that meet one or more of the attributes of the ESBL group (147). A recent literature survey of United States hospital infections caused by ESBL-producing E. coli and K. pneumoniae concluded that the rates of these infections were increasing, although specific data were difficult to assess due to differing definitions of ESBL (148).
ESBL variants.
Originally, ESBL enzymes were TEM and SHV variants displaying amino acid substitutions that changed their substrate profile to include the expanded-spectrum cephalosporins. The first ESBL (SHV-2) was described in 1985 and was found in a single strain of Klebsiella ozaenae isolated in Germany (149). Given the ease of whole-genome sequencing available today, multiple variants of the common TEM and SHV enzymes have been identified. There are now 183 nonduplicative variants of TEM and 178 variants of SHV, although not all of these possess the ESBL phenotype (https://www.ncbi.nlm.nih.gov/pathogens/isolates#/refgene/TEM; https://www.ncbi.nlm.nih.gov/pathogens/isolates#/refgene/SHV; https://externalwebapps.lahey.org/studies/). Changes at a limited number of amino acids are responsible for conferring the ESBL phenotype (59). Both TEM- and SHV-type ESBLs were described throughout the United States and Europe in the late 1980s and 1990s, with specific variants noted to be regional in distribution (150–152). For example, TEM-10 was responsible for several unrelated outbreaks of ESBL-producing organisms in the United States but was rarely seen in Europe (55). The prevalence of these enzymes has now diminished at the same time as the worldwide dissemination of isolates producing CTX-M-type β-lactamases (15).
CTX-M-type β-lactamases were also first reported in the 1980s. At first they were a curious addition to the list of ESBLs, but since the year 2000 they have spread worldwide and are now the most common type of ESBL (153). The CTX-M-type enzymes can be phylogenetically divided into five distinct clusters in which the group members share >94% identity (in contrast, ≤90% identity is observed between the members belonging to the other groups) (154). In general, CTX-M β-lactamases hydrolyze cefotaxime and ceftriaxone better than ceftazidime, although the spectrum varies by enzyme. CTX-M-15 can hydrolyze ceftazidime at higher rates than CTX-M-3, which may be a contributing factor for the successful spread of this enzyme (155). CTX-M-type enzymes are readily inhibited by all of the commercially available β-lactamase inhibitors, including the newest additions of avibactam and vaborbactam (102). The origin of the CTX-M-type enzymes is thought to be in Kluyvera spp., a rarely encountered environmental member of the Enterobacteriaceae (156). Genes presumed to be precursors of CTX-M-type enzymes have been identified among the chromosomes of Kluyvera cryocrescens (CTX-M-1 group), Kluyvera ascorbata (CTX-M-2 group), and Kluyvera georgiana (CTX-M-8, CTX-M-25, and CTX-M-9) (157). Plasmids and conjugative genetic elements such as ISEcp1-like, ISCR1, and class 1 integrons house the blaCTX-M genes and contribute to its mobilization (158). CTX-M β-lactamases are quite commonly found in E. coli and K. pneumoniae but are also found in other species of Enterobacteriaceae, including typhoidal and nontyphoidal Salmonella spp., Shigella spp., C. freundii, Enterobacter spp., and S. marcescens, as well as several species of nonfermenters (153, 157).
Although not classical ESBLs as defined by inhibition by clavulanate, a number of OXA-type β-lactamase variants, such as OXA-11 and OXA-14 to OXA-20, are associated with an ESBL phenotype in that they confer resistance to some of the late-generation cephalosporins (159). Many of these are derived from OXA-10 and OXA-2 and are commonly found in P. aeruginosa. OXA-163 is an interesting variant of OXA-48 in that it has an ESBL phenotype but is not a carbapenemase (160). In addition, OXA-1 (identical to OXA-30) hydrolyzes cefepime well and is prevalent among Enterobacteriaceae that also contain blaCTX-M-15 (161).
In recent years, multilocus sequence typing (MLST) has been used extensively to track and monitor the spread of resistance. As a result of these studies, several widely disseminated sequence types (ST) have been found in epidemics and outbreaks due to resistant organisms that are highly associated with certain resistance mechanisms. E. coli sequence type 131 (ST131, clade C) has been identified as the predominant lineage for E. coli causing extraintestinal infections, and the dissemination of CTX-M-15 has been driven in part by the spread of this successful clone (162). Isolates belonging to this lineage and phylogenetic group B2 have several virulence markers that contribute to its spread and can cause severe infections (163). The global dissemination of ST131, clade C, has led to an increase of fluoroquinolone-resistant and CTX-M-type β-lactamase-producing E. coli worldwide (153, 162–164). Prevalence studies showed that ST131 comprises up to 30% of all clinical isolates of extraintestinal E. coli clinical isolates and 40 to 80% of ESBL-producing isolates (153, 165).
Additional, less common ESBLs, other than TEM, SHV, and CTX-M, that have been found in clinically relevant settings include GES, PER, VEB, BES, BEL, SFO, and TLA β-lactamases (59). Once limited to the hospital setting, ESBL-producing isolates quickly expanded into nursing homes and community settings as well (55, 166). The impact of Enterobacteriaceae possessing ESBLs has had a significant impact on the choice of empirical antimicrobial therapy, driving the use of carbapenems in many institutions and resulting in increased resistance to carbapenems (167, 168).
Nonfermentative bacteria.
OXA-type extended-spectrum β-lactamases were originally found more commonly among P. aeruginosa isolates than in Enterobacteriaceae. Many of these were derived from OXA-2 or OXA-10 (169). In a recent study of P. aeruginosa isolated from patients in Tehran, 27.5% of the strains possessed a plasmid-mediated ESBL and were isolates found to contain genes for blaOXA-4, blaGES-1, and blaVEB-1 (170). VEB, GES, and OXA-type enzymes are also commonly found in Poland (171). In Saudi Arabia, VEB-1 and OXA-10 were found to be the most prevalent plasmid-mediated β-lactamases in P. aeruginosa (169).
ESBLs have been described among both environmental and clinical isolates of Aeromonas spp. There have been case reports of infections caused by A. hydrophila that carried blaTEM-24 and A. caviae with blaCTX-M-3 or blaPER-3 (172–174). Recently, CTX-M-3-producing A. salmonicida was isolated from the surgical site wound of a patient following leech therapy to restore blood flow to an amputated digit (175). It is likely that the presence of ESBLs in Aeromonas spp. is underreported, because the phenotypic testing would be masked by the presence of intrinsic AmpC and metallo-β-lactamases in this species (113).
Carbapenemase-Producing Bacteria
Species-specific serine carbapenemases.
(i) SME carbapenemases.
SME serine carbapenemases have been reported only in isolates of Serratia marcescens in which the relatively rare blaSME gene is located in the chromosome (176). An identifying characteristic of isolates expressing SME is that they are resistant to carbapenems but susceptible to expanded-spectrum cephalosporins like ceftazidime (177). To date, four variants of the original SME-1 enzyme have been reported (178–180). The first two SME-producing isolates were reported from England (177) but have not appeared to spread to the rest of Europe. Sporadic reports of these enzymes in the United States have occurred since 2004, with a relatively large outbreak of 19 SME-2-producing S. marcescens isolates appearing in Boston from 1994 to 1999 (176). Although most reported incidences of SME enzymes have been in the United States, these carbapenemases have also been reported in Argentina, Australia, Brazil, Canada, and Switzerland (176, 180–182). It is likely that SME enzymes are present in many other locations but have gone undetected because many laboratories do not test for a blaSME gene in their routine diagnostic testing for carbapenemases (176, 183).
Increasing numbers of SME enzymes have recently been reported from the Americas and the United Kingdom. In the United Kingdom, seven carbapenemase-producing S. marcescens isolates were identified in 2015 to 2016 after many years of no reported SME enzymes (183). Even greater numbers of these isolates were reported from Canada; the number of carbapenem-resistant S. marcescens isolates submitted to the National Microbiology Laboratory increased from 13 isolates in 2010 to 33 and 29 in 2012 and 2013, respectively. Among these 75 Canadian isolates, 30 of them (40%) carried a blaSME gene encoding either SME-1 (n = 24) or SME-2 (n = 6) enzymes (184). Genomic analyses of three native Canadian isolates, the UK isolates, and a United States isolate selected during antibiotic therapy revealed that the blaSME gene resided in a cryptic prophage genomic island, SmarGI1-1 (S. marcescens genomic island 1-1), inserted in the chromosome (183–185). In the U.S. isolate, both the SME and AmpC enzymes were inducible in the initial isolate and hyperproduced after several months of antibiotic treatment in the affected patient, due in part to missense and nonsense mutations in ampD (185).
(ii) IMI/NMC carbapenemases.
Other chromosomal serine carbapenemases include those in the IMI and NMC families identified to date only in isolates of the E. cloacae complex of organisms. Imipenem-resistant E. cloacae isolates from two California patients in 1984 were the original sources for the chromosomal IMI-1 enzyme (186). Like SME, the IMI β-lactamase confers resistance to carbapenems but not expanded-spectrum cephalosporins (186). Recently, IMI-type enzymes have been identified from China, Japan, and the French island of Mayotte (Indian Ocean) (187–189). In the latter two areas, the producing isolates were both carbapenem and colistin resistant. The NMC-A serine carbapenemase was first identified from a 1990 French isolate of E. cloacae (190) and shares 97% sequence identity with IMI-1 (186). At this time, the accepted nomenclature uses IMI as the family name for any new members of this set of related carbapenemases (https://ftp.ncbi.nlm.nih.gov/pathogen/betalactamases/Allele.tab, accessed 31 August 2019). NMC-A also has been reported occasionally in isolates of Enterobacter spp. from North America and in a Japanese tourist treated in Italy (191–194). Antonelli et al. have described an integrative mobile element that encoded an Xer tyrosine recombinase that was likely responsible for integration of the blaNMC-A carbapenemase gene into the chromosome of Enterobacter spp. (194). Recent genomic analyses of Canadian isolates have shown that both NMC-A and IMI genes were found on EludIMEX-1-like integrative mobile elements, most of which were integrated into the chromosome (193). The genes encoding IMI-5 and IMI-6 were found on IncFII-type plasmids, indicating that these currently Enterobacter-specific enzymes have the potential to spread to other genera (193).
Acquired serine carbapenemases.
(i) KPC carbapenemases.
In the late 1990s, the K. pneumoniae carbapenemase (KPC) family of β-lactamases began to emerge on the east coast of the United States and has become the most common carbapenemase detected globally (195–197). Characteristics of this family of acquired serine carbapenemases includes a molecular structure similar to that of other class A enzymes but with only 50%, 39%, and 35% amino acid sequence identity to the more common CTX-M-1, SHV-1, and TEM-1 enzymes, respectively (198). The KPC enzymes exist as one of at least 40 variants differing in most cases by less than five amino acids from the original KPC-2 and KPC-3 enzymes (https://www.ncbi.nlm.nih.gov/pathogens/isolates#/refgene/KPC, accessed 24 August 2019) and are found among many different genera of Enterobacteriaceae and P. aeruginosa (199, 200). KPC carbapenemases possess a large and shallow active site, allowing these enzymes to accommodate a wide range of β-lactam molecules, including cephalosporins, monobactams, and carbapenems (198). Isolates producing KPC-type enzymes not only are resistant to most β-lactams but also are often multidrug resistant, because they additionally encode a multitude of other resistance genes, rendering them virtually panresistant to many of the currently available first-line options for therapy (201–203). KPC-type β-lactamases are not inhibited by clavulanate or tazobactam; however, they are inhibited well by the newer β-lactamase inhibitors, such as avibactam, relebactam, and vaborbactam (199, 204, 205). However, strains harboring mutants of blaKPC can become resistant to ceftazidime-avibactam via increased catalytic activity for ceftazidime (206, 207).
The gene expressing KPC is usually found within a form of the composite transposon Tn4401 that may vary with length while retaining similar gene content (208). The successful spread of KPC has been due primarily to the spread of K. pneumoniae isolates belonging to the successful clonal complex 258 (CC258) or ST258 (clades I and II), found in both hospital and community isolates (202, 203, 209–212). In a survey of KPC-producing K. pneumoniae collected globally in 2012, Peirano et al. found that 290 of 522 (55.6%) isolates from 19 different countries belonged to CC258 (210). These isolates were divided between two clades, with both blaKPC-2 and blaKPC-3 located on IncFIIK2-like plasmids; ST258 clade I was more frequently associated with blaKPC-2, whereas clade II was more frequently associated with blaKPC-3 (210). Large outbreaks of KPC-producing K. pneumoniae in Poland and Colombia have also been attributed to strains belonging to ST258, with blaKPC often found inside the Tn4401 transposon (213, 214). In an extensive European genomic study of carbapenem-resistant K. pneumoniae from 244 hospitals in 32 countries, ST258/512 K. pneumoniae, originating in the United States, was identified as the likely progenitor of the large majority of European carbapenemase-producing isolates (215). Rojas et al. have proposed that the emergence of an epidemic KPC-producing K. pneumoniae ST258 clone in Colombia was due to the convergence of two different evolutionary pathways; one involved the horizontal transfer of blaKPC-2 mobile elements, and the other was due to the establishment of the highly virulent clonal group 258 (ST258) strain that carried blaKPC-3 (214). K. pneumoniae ST258 isolates containing blaKPC in the bacterial chromosome now have been reported by several different groups and may be more common than originally expected (216, 217). Sequence types other than ST258 have also been reported, with major representatives including ST11, the predominant type in China and Taiwan, and ST25, ST147, and ST512 in the Americas and Europe (210, 213, 217–220).
KPC was first identified in 1996 in North Carolina from an isolate of K. pneumoniae from a single patient (195). Although the next steps in dissemination were never identified, in the following decade, K. pneumoniae expressing KPC-2 gained a foothold and became endemic in New York City (221). Subsequently, the epidemiology of KPC-producing pathogens has expanded far beyond the northeast United States such that KPC enzymes have become the most common carbapenemases detected globally (222, 223). During the mid-2000s, several outbreaks of K. pneumoniae type ST258 were documented in hospitals in Israel caused by strains that were nearly identical to the KPC-producing strains detected in New York (224). This was attributed to the frequent travel back and forth of citizens of both countries. In a survey of Gram-negative pathogens collected from 2012 to 2014, KPC-producing isolates were found in 22 countries on four continents, as seen in Fig. 4 (199). In addition to K. pneumoniae, KPC-type β-lactamases were also found in E. aerogenes, E. coli, K. oxytoca, C. freundii, and several other species (199). Outside the United States, recent outbreaks of KPC-producing K. pneumoniae have been reported in Brazil, China, Ecuador, Germany, Greece, South Korea, Poland, Portugal, Switzerland, and Taiwan (213, 218–220, 225–232). A widely publicized outbreak of KPC-producing K. pneumoniae in the United States was documented in a clinical trial unit at the National Institutes of Health, resulting in the death of 11 of 18 infected patients as a result of infection-associated causes (233). Whole-genome sequencing was used to trace the infection to a single index case who left the unit 3 weeks prior to the next apparent case. The implementation of strict infection control practices subsequently halted the outbreak; however, sporadic cases still occur (233). The prevalence of KPC in K. pneumoniae isolates in New York City and Israel declined after the initial peak outbreaks, most likely due to strategic efforts to reduce the use of indwelling catheters plus increased infection control measures (234, 235). Carbapenem-resistant Enterobacteriaceae (CRE) bacteremia caused by KPC-producing K. pneumoniae is associated with high mortality rates and remains a problem in the New York-New Jersey area, which is the epicenter of CRE in the United States (211). However, the overall prevalence of clinical isolates expressing KPC has declined across New York City through massive infection control efforts (234). It is important to note that the promiscuous plasmids harboring blaKPC also commonly carry genes encoding resistance to aminoglycosides and additional β-lactamases, including ESBLs and metallo-β-lactamases (199, 200).
FIG 4.
Distribution of KPC-positive Enterobacteriaceae and P. aeruginosa collected in 2012 to 2014 from surveillance data. (Republished from reference 199.)
(ii) OXA carbapenemases.
Within the class D OXA family of β-lactamases, only a small fraction has a functional role as a carbapenemase. Among these are OXA-23, OXA-40, and the increasingly prevalent OXA-48, with its related variants, OXA-162, OXA-181, and OXA-232 (236). The OXA carbapenemases generally have hydrolytic activity against penicillins and broad-spectrum carbapenems and are poorly inhibited by β-lactamase inhibitors, except for avibactam (52, 237, 238). OXA-48 in particular hydrolyzes a narrower spectrum of β-lactams, with clinically relevant hydrolysis of penicillins and imipenem and lower hydrolysis of meropenem (239). The blaOXA-48 gene is often found in Tn1999 composite transposons that harbor copies of IS1999 flanking both sides of this β-lactamase gene (240). Isolates that express OXA-48 may be susceptible to cephalosporins and have only modestly elevated carbapenem MIC values, with many imipenem MICs of ≤2 μg/ml (241, 242). High-level resistance to carbapenems is usually due to a secondary nonenzymatic resistance mechanism in these isolates (239). The low levels of carbapenem resistance provided by this enzyme can make detection of strains harboring this resistance mechanism difficult.
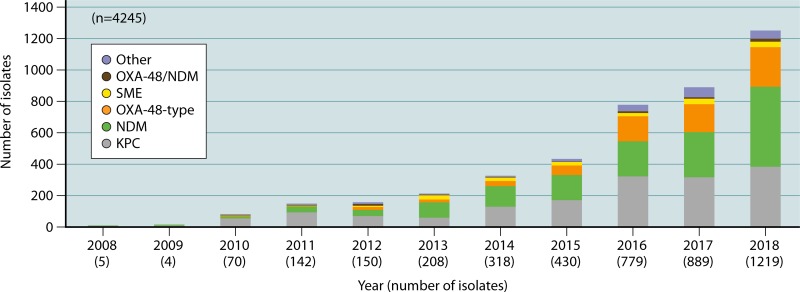
OXA-48 was first described among clinical isolates of K. pneumoniae from Turkey and has subsequently disseminated in Europe and the Mediterranean region, but it is found less frequently in the Americas (236, 239). In Spain, 72% of the 121 carbapenemase-producing E. coli isolates encoded OXA-48 in 2012 to 2014 (243); in a second Spanish study, 816 Enterobacteriaceae isolates producing OXA-48 were identified from 2013 to 2014, most frequently in K. pneumoniae (242). In a set of Spanish carbapenemase-producing Citrobacter species isolates collected between 2013 and 2015, 32% produced an OXA-48-type enzyme (244). A recent 2015 global survey of 11,559 Enterobacteriaceae isolates from 30 countries on five continents identified 40 OXA-48-producing strains; 95% were K. pneumoniae and all were from Europe, with 55% from Turkey (245). Another recent global surveillance study reported blaOXA-48 and blaOXA-48-like genes in 0.7% of 14 different species of Enterobacteriaceae collected from 2012 to 2015 in 20 countries (246). In addition, 8.7% of these isolates also coexpressed a metallo-β-lactamase. The incidence of OXA-48-type enzymes has been lower in Canada than in much of Europe but began to increase beginning in 2015. Throughout Canada, 67 OXA-48-like-producing isolates were collected in the 3-year period between 2011 and 2014, with many of these associated with international travel; in 2018, 21% (261/1,219) of the Canadian carbapenemase-producing enteric isolates were reported to produce OXA-48-like enzymes (247 and personal communication with M. Mulvey, Public Health Agency of Canada). The frequency of OXA-48 production in the United States has been low, with occasional localized isolates reported (248–250). Interestingly, OXA-23 is often found in P. mirabilis and was the causative pathogen in a cluster of community-onset infections in France (251). However, this provided only low-level resistance to carbapenems in this organism and may go undetected.
Species-specific metallo-β-lactamases.
(i) Aeromonas spp.
CphA, the metallo-β-lactamase found in many waterborne Aeromonas spp., selectively hydrolyzes penems and carbapenems but no other β-lactams (115). CphA has been found in A. bestiarum, A. caviae, A. hydrophila, A. sobria, A. veronii, and A. jandaei but has not been identified in A. trota or A. schubertii (252, 253). The production of the MBL CphA is not readily detected by conventional in vitro susceptibility tests unless a large inoculum is used; only about 30% of Aeromonas spp. tested resistant to imipenem with the standard inoculum (254, 255). In contrast, the presence of CphA can be detected with the modified Hodge test (254). Sources for CphA-producing Aeromonas species isolates include Italian rivers and sewage from an urban wastewater treatment plant (256, 257). Aeromonas spp. are most often associated with isolates from aquatic animals, including fish, shrimp, and pet turtles, but increasing numbers of CphA-producing patient isolates are being described (253, 255, 258, 259). As a partial explanation, a genetic relationship between Aeromonas species fish isolates and CphA-producing patient isolates was recently demonstrated in Taiwan (255). The emergence of imipenem-resistant CphA-producing isolates of Aeromonas spp. following therapy with carbapenems has also been reported (260).
(ii) Bacteroides fragilis.
Carbapenem resistance in B. fragilis was first reported in 1983 in Japan (261), followed by a description of carbapenemase activity in similar isolates in the United States in 1986 (262). Conflicting nomenclature is used to describe this carbapenemase as either CfiA or CcrA, an enzyme also recognized for its ability to confer resistance to cefoxitin (263, 264). The cfiA-ccrA gene is usually silent and is expressed only if an insertion sequence has inserted upstream of this structural gene, and it has been reported to occur only in B. fragilis (265–267). Although the cfiA-ccrA gene occurs in <10% of B. fragilis isolates, it has been reported worldwide, including in Japan, Argentina, China, Slovenia, and the United States, where the incidence of carbapenem-resistant B. fragilis remained ≤2.5% during 2008 through 2012 (266–269).
(iii) Bacillus spp.
The Gram-positive bacilli Bacillus anthracis and Bacillus cereus are generally regarded as environmental bacteria but are responsible for occasional human infections in patients, including animal caretakers/herders, immunocompromised individuals, or neonates (270, 271). Each species produces both a chromosomal serine penicillinase and an MBL, both of which are species specific. However, the frequency of clinical resistance to penicillin and other β-lactam antibiotics in B. anthracis is low and has been reported to range from 2 to 16% in isolates from the United States, South Africa, or France (272). The bla2 MBL from B. anthracis has 92% sequence identity with the 569H MBL from B. cereus and has low affinity for β-lactams in multiple classes, including the carbapenem imipenem (273, 274). Gene expression of both the chromosomal bla1 penicillinase and the bla2 MBL may be either silent or constitutive and is controlled by the genes sigP, an extracytoplasmic function sigma factor, and rsiP (BA2503), an anti-sigma factor (275).
(iv) Elizabethkingia spp.
Elizabethkingia meningoseptica (formerly Chryseobacterium menigosepticum and Flavobacterium menigosepticum) is a Gram-negative bacterial pathogen that is increasingly reported in hospital-acquired outbreaks and is known to survive and thrive in the hospital environment (276). Although most commonly associated with immunocompromised patients, E. meningoseptica has been associated with pediatric infections with increased frequency (277). E. meningoseptica and the related species Elizabethkingia anophelis are intrinsically resistant to most β-lactams due to the presence of two metallo-β-lactamases, BlaB and GOB-type variants (278, 279).
(v) Stenotrophomonas maltophilia.
As described above, S. maltophilia produces the chromosomally encoded inducible metallo-β-lactamase L1 and the class A cephalosporinase L2 (137, 138). Production of the tetrameric L1 enzyme, inducible by imipenem, is associated with resistance to β-lactams, including the carbapenems (280). At least 34 novel variants of the L1 β-lactamase have been reported, distributed into four clades according to amino acid identities (80). Although patient isolates of S. maltophilia are highly heterogeneous concerning sequence type, genotypic associations between specific genomic groups and L1 clades have been reported (80). As antibiotic resistance in the pathogen has increased over the past 20 years, future therapeutic options may include the investigational siderophore cephalosporin cefiderocol, with in vitro inhibitory concentrations of ≤0.5 μg/ml (281).
Acquired metallo-β-lactamases.
(i) IMP carbapenemases.
In 1990, Japanese scientists identified the first IMP (active on imipenem) MBL in P. aeruginosa on a conjugative plasmid that soon appeared in S. marcescens and other Enterobacteriaceae in Japan (282–284). Both broad-host-range and narrow-host-range plasmids are associated with blaIMP genes, contributing to their continued dissemination (285). The IMP enzymes confer resistance to penicillins and cephalosporins as well as to carbapenems, but, like other MBLs, they do not hydrolyze aztreonam. In many isolates, only low-level carbapenem resistance is observed, with as many as 20% of IMP-producing Enterobacteriaceae testing susceptible to imipenem (286). IMP carbapenemases have remained continuing contributors to carbapenem resistance in Japan as well as in other regions of Southeast Asia (285–288). A recent global surveillance study showed a further spread of IMP-4-producing strains into Australia (289). In addition, a country-wide outbreak of P. aeruginosa expressing IMP-13 was detected in Italy (290, 291). Although they have not spread extensively throughout the rest of the world, they are being reported more frequently in Middle Eastern countries (292, 293).
(ii) VIM carbapenemases.
Two novel VIM (Verona integron-encoded metallo-β-lactamase) metallo-carbapenemases were first identified in Italy and France in 1997 and 1996, both from P. aeruginosa isolates containing blaVIM gene cassettes inserted into a class 1 integron (64, 294). Today, VIM MBLs are found globally, mainly in K. pneumoniae and E. cloacae complex (287, 295, 296). Although they are identified more frequently than IMP MBLs, they represent a minority of all carbapenemases in carbapenem-resistant pathogens (222, 223, 297). The enzymes were not closely related to other MBLs based on amino acid sequences, with only 28 to 31% sequence identity between the VIM-1/VIM-2 carbapenemases and IMP-1 (64, 294). Biochemically, VIM-2 has a broad substrate hydrolysis profile, which includes penicillins, carbapenems, and most cephalosporins but not aztreonam (294). Worldwide, VIM-2 is the most prevalent VIM-type metalloenzyme in P. aeruginosa (287).
Epidemiologically, the VIM carbapenemases initially spread rapidly throughout southern Europe, with major outbreaks of VIM-producing P. aeruginosa reported in Italy and Greece by 2006, followed by outbreaks of VIM-producing K. pneumoniae (298–301). Until 2008, carbapenemase production in Greece was primarily due to VIM MBLs, until a hyperepidemic KPC-encoding K. pneumoniae clone invaded their hospitals (302). By 2014, up to 80% of the carbapenemase-producing K. pneumoniae isolates from Greek hospitals produced KPC carbapenemases, with only 12 to 20% of the isolates producing VIM enzymes (303, 304). However, resurgence in the prevalence of VIM enzymes in a Greek university hospital was recently reported. Physicians began prescribing ceftazidime-avibactam in the intensive care unit for patients with KPC-producing bloodstream infections because of the activity of avibactam against the KPC β-lactamase and the reported clinical superiority and low resistance of the combination compared to that of colistin (305). From 2015 to 2017, 88% of carbapenem-resistant K. pneumoniae isolates harbored blaKPC; none produced blaVIM. At the end of 2018, the first year after ceftazidime-avibactam had been introduced, 51% of the carbapenem-resistant K. pneumoniae isolates tested positive for MBLs: 38% were blaVIM positive, and 11% were positive for both blaVIM and blaKPC. Of the 49% (22/45) of the isolates producing KPC enzymes, four isolates were resistant to ceftazidime-avibactam due to production of an MBL that is not inhibited by avibactam (199, 305). With the introduction of other serine β-lactamase inhibitor combinations into clinical practice, similar scenarios can be expected in the future.
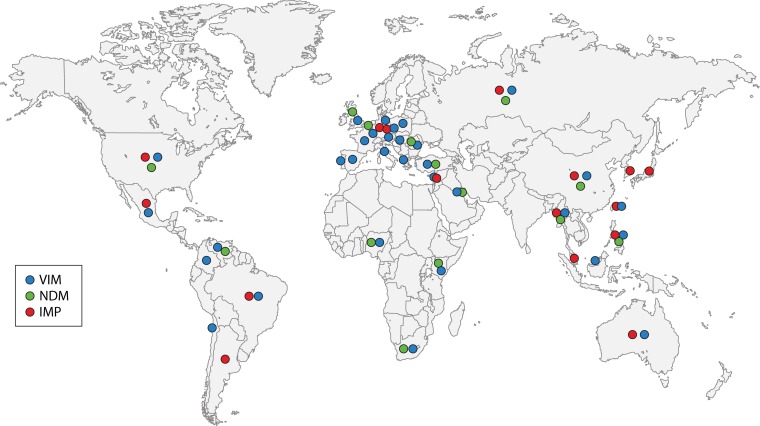
(iii) NDM carbapenemases.
The New Delhi metallo-β-lactamase (NDM) was first described in 2009 in an isolate of K. pneumoniae from a patient in Sweden that had previously been admitted to two different hospitals in India (5). NDM-1 shares very little sequence homology with the other MBLs commonly found in Enterobacteriaceae. The closest relative is VIM-1, with only 32.4% amino acid identity (306). A recent surveillance study of isolates collected from 40 countries in 2012 to 2014 showed that NDM-type enzymes accounted for 44.2% of all MBL-producing Enterobacteriaceae collected (287). Over 80% of recent E. coli isolates with NDM enzymes originated from Asia, predominantly from India, followed by China (307). Retrospective analyses of clinical isolates from India identified blaNDM-1 as early as 2006 (6). Within a few years, the gene had become endemic to all parts of India and Pakistan and had begun to spread into northern Europe (7). In less than a decade since those initial few reports, NDM-1 has spread across the globe (Fig. 5) and has been detected in many species of pathogenic enteric bacteria, foodborne Shigella spp. and Vibrio cholerae, and the nonfermenters A. baumannii and P. aeruginosa (287, 308). Isolates expressing NDM-1 are often multidrug resistant due to the movement of blaNDM genes with other resistance determinants. For example, there has been strong correlation with the presence of NDM-1 and the prevalent ArmA, RmtB, or RmtC 16S rRNA methylases that cause resistance to aminoglycosides, including the recently approved plazomicin (309, 310).
FIG 5.
Global distribution of metallo-β-lactamase-positive Enterobacteriaceae and P. aeruginosa, including NDM-type enzymes collected from 2012 to 2014 from surveillance. (Republished from reference 287).
In addition to the widespread presence of blaNDM on the Indian subcontinent, NDM now appears to be endemic to the Balkan countries, Northern Africa, and the Arabian Peninsula, where these countries may serve as a secondary reservoir for the enzyme (306). Recent outbreaks caused by NDM-producing Enterobacteriaceae have been reported in hospitals in Greece, Mexico, and the Netherlands and in a neonatal unit in China (311–313). Unlike the dissemination of KPC, high-risk clones and epidemic plasmids have not been widely implicated in the global spread of blaNDM genes (209). Although geographically localized outbreaks have been associated with a single clonal strain, little commonality has been seen, with multiple sequence types and plasmids involved, demonstrating the promiscuity of blaNDM genes. Examples just in Europe include a recent outbreak of NDM-producing K. pneumoniae isolates of sequence type 716 in Belgium (314); an outbreak in Italy due to NDM-producing K. pneumoniae ST16 (315); and outbreaks among eight Greek hospitals (2013 to 2016) related to ST11, the same sequence type as that seen in the first NDM-producing Greek outbreak and in a recent outbreak in Bulgaria (316). A recent global survey of pathogenic NDM-producing E. coli isolates identified a prevalence of sequence types ST101 and ST167 in multiple countries (307). Another study of GenBank sequences containing blaNDM genes reported more than 40 sequence types each for E. coli and K. pneumoniae in 2019 (317).
Bacteria Producing Inhibitor-Resistant β-Lactamases
Inhibitor-resistant β-lactamases belonging to functional group 2br are derivatives of TEM and SHV enzymes, with amino acid substitutions that make these enzymes refractory to inhibition by clavulanic acid and sulbactam; however, most remain susceptible to inhibition by tazobactam as well as the newer inhibitors, such as avibactam (38, 39, 221). Mutations responsible for this phenotype have been noted particularly at the following amino acid positions: Met69, Ser130, Arg244, Arg275, and Asn276 (318). Most inhibitor-resistant β-lactamases are variants of the TEM-1 enzyme. These were formerly called IRT (for inhibitor-resistant TEM) but are now given sequential TEM numbering. Only three SHV-type β-lactamases have been described as being inhibitor resistant, SHV-49, -56, and -107, all identified from European K. pneumoniae clinical isolates (319–321). A few TEM variants maintain the ESBL phenotype and also demonstrate inhibitor resistance and are referred to as complex TEM mutant (CMT) β-lactamases (318). The prevalence of organisms producing these inhibitor-resistant enzymes may be underestimated, because many laboratories do not identify these strains routinely (322). However, a strain of K. pneumoniae expressing the IRT TEM-30 was identified among KPC-producing isolates in an outbreak in New York (221).
Organisms with Multiple β-Lactamases
Production of multiple β-lactamases in a single organism has become common in contemporary nosocomial isolates, especially in Gram-negative pathogens, where mobile elements carrying a variety of resistance factors are freely transferred among species. In the Gram-positive world, penicillinase-producing staphylococci appear to produce only a single β-lactamase protein in each strain, although at least four types of penicillinases have been identified in this species (95). However, β-lactamases in S. aureus have not received the same molecular attention as β-lactamases in Gram-negative bacteria, so it is possible that greater heterogeneity exists than is currently realized. In Gram-negative bacteria, multiple reports of clinical isolates over the past 30 years document the production of more than one β-lactamase per strain (323–325). Of the baseline pathogens identified during the recent phase 3 pathogen-directed clinical trial of ceftazidime-avibactam, only 35/302 (11.6%) tested positive for a single β-lactamase gene; nine of those isolates (3.0% of the total) contained only a chromosomal ampC gene (21).
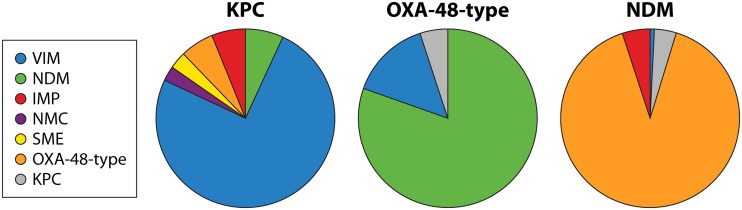
Multi-β-lactamase production can occur in all β-lactamase-producing Gram-negative species but is especially noticeable with a high frequency in carbapenemase-producing, multidrug-resistant bacteria (250, 326). In a survey of carbapenem-resistant Enterobacteriaceae from California (2013 to 2016), 79.2% of the carbapenemase gene-positive isolates compared to 60.5% of carbapenemase gene-negative isolates also tested positive for either an ESBL- or plasmid-encoded AmpC gene (250). Of greater concern is the coproduction of multiple carbapenemases in the same organism. A survey of 52 reports of the occurrence of multiple carbapenemases in a single organism (Table 2) showed that since 2008, KPC enzymes appeared in combination with another carbapenemase in at least 110 isolates, whereas OXA-48-related carbapenemases were named in carbapenemase combinations in over 130 isolates (Table 2 and Fig. 6). In these isolates, KPC β-lactamases were more likely to be identified in combination with VIM MBLs (75% of the isolates) than with other carbapenemases (Fig. 6). Many of these isolates originated from the Americas and Greece, although three isolates from Spain produced KPC-2/3 with VIM-1 (327, 328). Fewer isolates coproduced KPC enzymes with NDM-1 (7%), IMP (6%), or OXA-48 (6%) carbapenemases. The carbapenemases coproduced most frequently with OXA-48-type enzymes were MBLs; 81% of these isolates also produced NDM β-lactamases, whereas 14% of the OXA-producing isolates were associated with MBLs in the VIM family (Fig. 6). When NDM-type enzymes were coproduced with other carbapenemases, OXA-48-type enzymes were present in 90% of the isolates (Fig. 6), followed by IMP (5%) and KPC (4%). Although many of the organisms coproducing carbapenemases were K. pneumoniae isolates (60%), dual carbapenemase production was also reported in other enteric bacteria, including C. freundii (4.1%), Enterobacter spp. (3.7%), K. oxytoca (0.9%), and S. marcescens (11.1%) (Table 2). One of the more troublesome combinations reported recently was the triple threat of NDM-, VIM-, and OXA-48-encoding genes in a single K. pneumoniae isolate; this was identified from a U.S. patient who had undergone outpatient urodynamic studies in a hospital in India (329).
TABLE 2.
Production of multiple carbapenemases in the same Gram-negative pathogen, excluding Acinetobacter spp.
| Carbapenemase class |
Producing organism | No. of isolates | Yr of isolation | Location | Reference | ||
|---|---|---|---|---|---|---|---|
| Class A | Class B | Class D | |||||
| KPC-2 | IMP-8 or IMP-10 | NDa | S. marcescens, P. aeruginosa | 7 | 2009–2011 | Brazil, Puerto Rico | 362, 363 |
| KPC-2 or KPC-3 or KPC-17 | NDM-1 | ND | C. freundii, E. cloacae, Enterobacter hormaechei, K. pneumoniae | 9 | 2010–2016 | Brazil, China, Colombia, India, USA | 245, 364–370 |
| KPC-2 or KPC-3 or KPC-18 | VIM-1 or VIM-type | ND | C. freundii, E. cloacae, K. oxytoca, K. pneumoniae | 36 | 2008–2017 | Greece, Spain, USA | 304, 327, 328, 368, 371, 372 |
| KPC-type | VIM-type | ND | K. pneumoniae | 50 | 2013–2018 | Greece | 228, 305 |
| KPC-3, SME-1 | ND | ND | S. marcescens | 3 | 2015 | USA | 373 |
| KPC-2 or KPC-3, NMC-1 | ND | ND | K. pneumoniae | 4 | 2013–2017 | Malaysia, USA | 369, 374, 375 |
| KPC-2, NMC-1 | ND | OXA-48 | K. pneumoniae | 1 | 2013 | Malaysia, USA | 374 |
| KPC-type | ND | OXA-48 | K. pneumoniae | 7 | 2013–2014 | Malaysia, Taiwan | 304, 374, 376 |
| ND | IMP-4, VIM-2 | ND | S. marcescens | 15 | 2015 | Egypt | 292 |
| ND | IMP-4 or IMP-8, NDM-1 | ND | K. pneumoniae | 6 | 2013 | China, Malaysia | 226, 374 |
| ND | NDM-1 or NDM-type | OXA-48 or OXA-48-like | C. freundii, E. cloacae, Enterobacter ludwigii, E. coli, K. oxytoca, K. pneumoniae, Enterobacteriaceae | 91 | 2007–2018 | Belgium, England, France, Romania, India, Iran, Saudi Arabia, Spain, Tunisia, Turkey, USA | 215, 246, 297, 304, 377–387 |
| ND | NDM-type, VIM-type | OXA-48 | K. pneumoniae, Enterobacter spp. | 2 | 2011, 2018 | USA, Vietnam | 329, 370 |
| ND | NDM-1 or NDM-5 or NDM-7 | OXA-181 | E. coli, K. pneumoniae | 15 | 2010–2017 | Belgium, Canada, Egypt, India, Norway, South Korea, Sri Lanka | 388–395 |
| ND | NDM-1 | OXA-232 | K. pneumoniae | 4 | 2012–2018 | India, South Korea, USA | 361, 396, 397 |
| ND | VIM-type | OXA-48-type | C. freundii, Enterobacter spp., E. coli, K. pneumoniae, Enterobacteriaceae | 22 | 2006–2016 | Egypt, France, India, Kuwait, Spain, Turkey | 6, 244, 246, 370, 378, 383, 398 |
ND, not detected.
FIG 6.
Coproduction of carbapenemases in the same organism. Data for production of KPC β-lactamases, OXA-48-type β-lactamases, and NDM β-lactamases with other carbapenemases were compiled from Table 2.
Coproduction of multiple β-lactamases of different functionalities occurs frequently in Gram-negative bacteria that produce species-specific chromosomal enzymes (21). Enteric bacteria, such as Enterobacter spp., Citrobacter spp., and S. marcescens, and P. aeruginosa are affected. For example, K. oxytoca strains usually produce an OXY-type β-lactamase with an ESBL-like hydrolysis profile. Based on whole-genome sequencing, analysis of 12 carbapenemase-producing K. oxytoca isolates from Spain revealed three different blaOXY genes among the strains, together with genes encoding OXA-48, VIM-1, KPC-2, or KPC-3; two isolates carried genes for VIM-1, KPC-2/3, and an OXY enzyme of the blaOXY-2 genotype (328). Similarly, K. pneumoniae usually produces at least one SHV β-lactamase (330), together with β-lactamases from other molecular classes (21). Contemporary Enterobacter spp., Citrobacter spp., and P. mirabilis, with their own chromosomal AmpC cephalosporinases, all have a high probability of carrying another β-lactamase from molecular class A or D (246). Frequently these are TEM-1- or OXA-1-related enzymes (21, 246). These are narrow-spectrum β-lactamases with high catalytic efficiencies for commonly prescribed penicillins (331) and are likely retained to augment the cephalosporin-specific substrate profile provided by the AmpC enzymes (38).
TRANSMISSION OF β-LACTAMASE-PRODUCING PATHOGENS
Transmission of β-lactamase-producing bacterial pathogens is dependent upon multiple factors. The human reservoir in which the resistant organism emerges is affected by various elements, including geographical location, population density, hygiene, and use of antibiotics. For example, the prevalence of ESBL-producing E. coli is very high in Southeast Asia, Africa, and Central America and has a much lower prevalence in Europe (332). There is even variation within Europe, as the incidence of Enterobacteriaceae carrying ESBLs is higher in Western European countries that border the Mediterranean but is very low in the Netherlands and Scandinavia (333). In addition, we now live in a global society that is increasingly mobile, whether it is vacationers, medical tourists, or refugees. The rapid spread of NDM-producing Enterobacteriaceae was attributed in part to a large volume of medical tourism from northern Europe to India (7). All of these influences contribute to outbreaks and dissemination of β-lactamase-mediated resistance.
The epidemiology of β-lactamase-mediated resistance first and foremost follows the pathology of the bacterial pathogen in which the enzymes are found. Where you find the pathogen in a patient who requires heavy usage of β-lactam antibiotics, there too will you find various β-lactamases. For Enterobacteriaceae, the main reservoir of β-lactamase-producing pathogens is the digestive tract of colonized patients, with the majority of the infections caused by pathogens identical, or highly genetically related, to the colonizing organisms (334). Transmission of resistant Enterobacteriaceae occurs between patients with or without prior transmission to a health care worker. The rate of transmission of β-lactamase-producing pathogens can vary with species, likely according to differences in virulence factors. One study reported that the transmission rate of ESBL-producing organisms was 2-fold higher from patients colonized with K. pneumoniae than from those colonized with E. coli (335). Large-scale nosocomial outbreaks have been caused by highly virulent and transmissible isolates of ESBL- and carbapenemase-producing strains, such as E. coli ST131 and K. pneumoniae ST258 (209, 336). Although most outbreaks of β-lactamase producing Enterobacteriaceae occur in the ICU or in immunocompromised patients, neonates can also be affected. A recent report from Japan characterized an outbreak of ESBL-producing E. coli that was traced to shared breast milk from donor mothers (337).
The epidemiology of β-lactamase-producing Enterobacteriaceae has also changed over time. This is exemplified by the series of outbreak and endemic isolates of E. coli and K. pneumoniae expressing various β-lactamases that have been detected in the past 25 years in a single New York hospital. Ceftazidime was approved in 1984, and just a few years later, the ESBL era was born. An outbreak of ceftazidime-resistant K. pneumoniae that involved 155 patients during a 19-month period, from October 1988 to March 1990, was detected in The New York Hospital Medical Center of Queens (338, 339). Characterization of these isolates showed that they contained TEM-26 together with TEM-10, two of the first ESBLs to become endemic in the United States. Infection control measures resulted in the cessation of this outbreak; however, a low level of resistance to ceftazidime persisted. In 1993, several isolates of K. pneumoniae were noted that were not only ceftazidime resistant but also resistant to cefotaxime. These isolates produced the SHV-7 β-lactamase and were likely selected following increased prescribing of cefotaxime as a part of the effort to control the spread of TEM-26 (340). In response to the outbreak of ESBL-producing organisms, cephamycins, especially cefotetan, became the empirical treatment of choice. Subsequently, in 1995 there was an outbreak of E. coli and K. pneumoniae isolates that were resistant to cefoxitin and cefotetan by the acquisition of a novel plasmid-mediated AmpC-type β-lactamase, designated ACT-1 (75). As a result of this new wave of resistant organisms, the use of imipenem increased dramatically in the hospital. Immediately, K. pneumoniae isolates producing ACT-1 also became resistant to imipenem because of the loss of an outer membrane protein (75). However, the use of imipenem during these outbreaks also helped to select for the next wave of resistance. In the early 2000s, K. pneumoniae expressing KPC-2 became endemic across New York City, including in this hospital (221). In a 2009 study, K. pneumoniae isolates coproducing both KPC and CTX-M enzymes were isolated from nonhospitalized patients with urinary tract infections who presented at the emergency room or associated clinic of this hospital (341). Through massive infection control efforts across the city, the prevalence of KPC-producing K. pneumoniae has declined over the last decade, but the pathogen has not completely disappeared (211, 234).
P. aeruginosa is an opportunistic pathogen that causes a variety of infections, including sepsis, pneumonia, urinary tract infections, and soft-tissue infections (342). It is a leading cause of nosocomial infections, especially in the ICU, and is associated with immunocompromised patients due to solid-organ transplantation, invasive procedures, and immunosuppressive therapy (343). P. aeruginosa can survive well in the environment, particularly in water sources. Several outbreaks of carbapenem-resistant P. aeruginosa have been traced to an environmental reservoir within the hospital (344). Until very recently, most of the β-lactam resistance in P. aeruginosa was attributed to the loss of the OprD porin protein combined with high-level production of the naturally occurring AmpC β-lactamase, often in isolates that had upregulated efflux systems (345). However, in recent years, acquired β-lactamases have been responsible for outbreaks with increasing frequency. ESBLs such as PER-1 and OXA-10 are commonly found in P. aeruginosa (346). The increase in acquired β-lactamases has been especially noteworthy, as MBLs have moved into P. aeruginosa and have been the cause of outbreaks in many countries worldwide (347–350).
A. baumannii can cause a variety of acute hospital infections, including pneumonia (especially ventilator-associated pneumonia), bloodstream infections, urinary tract infections, skin and soft-tissue infections, burn and surgical wound infections, endocarditis, meningitis, and osteomyelitis (351). The majority of these are nosocomial infections, because the risk factors that make patients prone to the colonization and infection with A. baumannii include surgical procedures, major trauma, elderly patients, and prior antibacterial therapy. In addition, infections caused by A. baumannii are often associated with medical treatments that rely on some kind of indwelling hardware, including mechanical ventilators, intravascular catheters, urinary catheters, and drainage tubes (352). It has been reported that A. baumannii is the causative pathogen in 2 to 10% of all Gram-negative hospital infections, mainly affecting critically ill patients, especially in ICUs (351). Although β-lactamases of all classes contribute to resistance in Acinetobacter spp., A. baumannii is of particular concern when it becomes resistant to carbapenems. In these cases, health care-associated infections may increase the risk of mortality from 8% to 40% (353).
Nosocomial infections caused by β-lactamase-producing pathogens are associated with serious health and economic adverse outcomes, such as clinical failure with increased in-hospital mortality, prolonged length of stay, and increased direct and indirect costs (354). A meta-analysis showed that bacteremia caused by ESBL-producing Enterobacteriaceae was associated with a higher mortality than those caused by ESBL-negative isolates (355). Furthermore, infections caused by ESBL-producing E. coli and Klebsiella spp. were associated with increased health care costs due to prolonged infection-related length of stay and indirect care costs for enhanced infection control measures (356). An evaluation associated with an outbreak of carbapenemase-producing Enterobacteriaceae in London concluded that the overall economic costs were due not only to the expenses of treating infections but also to lost opportunities to treat other patients (357).
FUTURE DIRECTIONS
β-Lactamase-producing pathogens will never disappear and can be expected to continue to increase with greater variety in the future. As an example, surveillance data from the Canadian Public Health Laboratory Network show the continuing increase in carbapenemase-producing nonduplicated pathogens since 2011 (Fig. 7), with greater numbers of enzymes and greater diversity among the kinds of carbapenemases over the past 9 years of surveillance (data used with permission from Michael Mulvey, Public Health Agency of Canada). Part of the reported increase may be due to better reporting of molecular data. However, it is also likely that increases in β-lactamase production are due to the ease with which these enzymes can travel between carriers and infected patients from all parts of the world. These pathogens have become well-established in both the community and in health care settings and will continue to exist as long as β-lactam antibiotics continue to be used. Although agents such as the newer β-lactamase inhibitor combinations, i.e., ceftazidime-avibactam, meropenem-vaborbactam, and imipenem-relebactam, have provided opportunities for safe and effective therapies to treat some of the most threatening carbapenemase-producing pathogens, they do not address the problems associated with metallo-β-lactamases. Even if some of the newer investigational agents are successful in treating MBL-producing pathogens, resistance to these new drugs also can be expected to emerge, as has been seen with ceftazidime-avibactam (45, 51). This resistance may be due to more than the known mechanisms of resistance, which include enzyme variants with decreased affinity for the inhibitors, altered PBPs, or decreased entry into the cell as a result of upregulated efflux pumps or changes in outer membrane proteins. Production of multiple β-lactamases from different classes, as exemplified in Table 2, will continue, so that cocktails of class-specific β-lactamase inhibitors may be required for effective treatment of serious infections.
FIG 7.
Surveillance of carbapenem-producing Enterobacteriaceae in Canada. Data were provided with the permission of Michael Mulvey, Public Health Agency of Canada.
Efforts to promote stewardship of these valuable agents are necessary and have been somewhat successful in localized areas. For example, Scandinavian countries exhibit lower resistance rates than much of the rest of Europe (2), due in part to increased use of narrow-spectrum penicillins and a reluctance to use the most advanced antibiotics in their health care centers (358, 359). As noted above, some hospitals have contained the spread of carbapenemases within their facilities as a result of stricter infection control measures (234, 235). In Israel, the reduction in the number of carbapenemase-producing Enterobacteriaceae required a successful effort to institute country-wide infection control measures that greatly diminished the number of new cases, but that did not entirely eradicate the causative pathogens (235). Notably, the model used to monitor and control resistance was extended to include other multidrug-resistant organisms and hospital-acquired infections (360). Thus, resistance may be confined on a national level with programs such as enhanced surveillance networks and promotion of good stewardship of the current antimicrobial agents.
Advances in molecular diagnostics are providing clinical microbiologists with the ability to define specific resistance mechanisms in clinical specimens at an early stage. Diagnostic kits that can test for multiple β-lactamases in a single assay mean that ESBL producers can be differentiated from carbapenemase- or metallo-β-lactamase-producing pathogens within hours of collecting a specimen. This allows a clinician to prescribe an appropriate antibiotic much sooner than previously possible. Another tool that is becoming more prominent is whole-genome sequencing, which provides in-depth knowledge of multiple resistance factors carried by pathogenic bacteria, thereby giving us greater insight into how therapies can be guided at an early stage (361). However, none of these approaches will eliminate the ubiquitous β-lactamase-producing bacteria that will continue to remain intimately associated with their human hosts.
ACKNOWLEDGMENT
We declare that we have no outside interests that influenced the content of this review article.
Biographies

Karen Bush received her BA in Chemistryxch (Monmouth College, IL) and Ph.D. in Biochemistry (Indiana University). She moved from the laboratory to supervisory/management positions at Squibb, Lederle, Astra, and Johnson & Johnson on teams that discovered and/or developed aztreonam, piperacillin-tazobactam, levofloxacin, ceftobiprole and doripenem. Since 1977, her main focus has been the study of β-lactamases. Her laboratory helped characterize the first KPC carbapenemases, and, with Patricia A. Bradford, some of the first ESBLs in the United States and the second plasmid-encoded AmpC cephalosporinase. She returned to Indiana University in 2009, where she is a Professor of Practice and Interim Director of the Biotechnology Program. Her laboratory currently tracks and characterizes carbapenem resistance in Indiana Gram-negative bacteria. She is a consultant for biotech companies and reviews for several granting agencies. She has served as an Editor of Antimicrobial Agents and Chemotherapy, EcoSal Plus, and mBio and is a Fellow of the American Academy of Microbiology.

Patricia A. Bradford is the owner of Antimicrobial Development Specialists, LLC, a consulting company focusing on the late-stage development of antibiotics. During tenures at AstraZeneca, Novartis, Wyeth Pharmaceuticals, and Lederle Laboratories, she worked on antibiotic projects that included development of piperacillin-tazobactam, tigecycline, and ceftazidime-avibactam. She is a Fellow of the American Academy of Microbiology, has over 100 publications in peer-reviewed journals, and has written several review articles and book chapters. She served as an editor for Antimicrobial Agents and Chemotherapy (2001 to 2011) and is currently a Senior Editor for ASM’s newest journal, mSphere. She is an active member of the Antimicrobial Susceptibility Testing subcommittee of the Clinical and Laboratory Standards Institute. Prior to working in industry, she was a clinical microbiologist at Nebraska Methodist Hospital in Omaha. She received a B.S. in Medical Technology from the University of Nebraska Medical School, Ph.D. in Medical Microbiology from Creighton University, and completed a postdoctoral fellowship with Karen Bush in β-lactamase research.
REFERENCES
- 1.Bush K, Bradford PA. 2016. β-Lactams and β-lactamase inhibitors: an overview, p 23–44. In Silver LL, Bush K (ed), Antibiotics and antibiotic resistance. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY. doi: 10.1101/cshperspect.a025247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ECDC. 2018. Surveillance of antimicrobial resistance in Europe–annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net) 2017. European Centre for Disease Prevention and Control, Stockholm, Sweden. [Google Scholar]
- 3.WHO. 2019. No time to wait: securing the future from drug-resistant infections. Report to the Secretary-General of the United Nations. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 4.Perez F, Bonomo RA. 2019. Carbapenem-resistant Enterobacteriaceae: global action required. Lancet Infect Dis 19:561–562. doi: 10.1016/S1473-3099(19)30210-5. [DOI] [PubMed] [Google Scholar]
- 5.Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, Walsh TR. 2009. Characterization of a new metallo-β-lactamase gene, blaNDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother 53:5046–5054. doi: 10.1128/AAC.00774-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castanheira M, Deshpande LM, Mathai D, Bell JM, Jones RN, Mendes RE. 2011. Early dissemination of NDM-1- and OXA-181-producing Enterobacteriaceae in Indian hospitals: report from the SENTRY Antimicrobial Surveillance Program (2006–2007). Antimicrob Agents Chemother 55:1274–1278. doi: 10.1128/AAC.01497-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, Chaudhary U, Doumith M, Giske CG, Irfan S, Krishnan P, Kumar AV, Maharjan S, Mushtaq S, Noorie T, Paterson DL, Pearson A, Perry C, Pike R, Rao B, Ray U, Sarma JB, Sharma M, Sheridan E, Thirunarayan MA, Turton J, Upadhyay S, Warner M, Welfare W, Livermore DM, Woodford N. 2010. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis 10:597–602. doi: 10.1016/S1473-3099(10)70143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khan AU, Nordmann P. 2012. Spread of carbapenemase NDM-1 producers: the situation in India and what may be proposed. Scand J Infect Dis 44:531–535. doi: 10.3109/00365548.2012.669046. [DOI] [PubMed] [Google Scholar]
- 9.Bush K. 2018. Past and present perspectives on β-lactamases. Antimicrob Agents Chemother 62:e01076-18. doi: 10.1128/AAC.01076-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. 2013. Antibiotic resistance threats in the United States, 2013. CDC, Atlanta, GA. [Google Scholar]
- 11.WHO. 2017. Prioritization of pathogens to guide discovery, research and development of new antibiotics for drug-resistant bacterial infections, including tuberculosis. World Health Organization, Geneva, Switzerland: www.who.int/medicines/areas/rational_use/PPLreport_2017_09_19.pdf?ua=1. [Google Scholar]
- 12.Theuretzbacher U, Bush K, Harbarth S, Paul M, Rex JH, Tacconelli E, Thwaites GE. Critical analysis of antibacterial agents in clinical development. Nat Rev Microbiol, in press. [DOI] [PubMed] [Google Scholar]
- 13.Bush K, Bradford PA. 2019. Interplay between β-lactamases and new β-lactamase inhibitors. Nat Rev Microbiol 17:295–306. doi: 10.1038/s41579-019-0159-8. [DOI] [PubMed] [Google Scholar]
- 14.Logan LK, Weinstein RA. 2017. The epidemiology of carbapenem-resistant Enterobacteriaceae: the impact and evolution of a global menace. J Infect Dis 215:S28–S36. doi: 10.1093/infdis/jiw282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doi Y, Iovleva A, Bonomo RA. 2017. The ecology of extended-spectrum beta-lactamases (ESBLs) in the developed world. J Travel Med 24:S44–S51. doi: 10.1093/jtm/taw102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bradford PA. 2018. Epidemiology of resistance In Fong IW, Shlaes D, Drlica K (ed), Antimicrobial resistance and implications for the 21st century, 2nd ed Springer International Publishing, New York, NY. doi: 10.1007/978-3-319-78538-7. [DOI] [Google Scholar]
- 17.Bradford PA, Castanheira M. 2018. Mechanisms of resistance In Jorgensen JH, Pfaller MA, Carroll KC, Funke G, Landry ML, Richter SS, Warnock DW (ed), Manual of clinical microbiology, 12th ed ASM Press, Washington, DC. [Google Scholar]
- 18.Livorsi DJ, Chorazy ML, Schweizer ML, Balkenende EC, Blevins AE, Nair R, Samore MH, Nelson RE, Khader K, Perencevich EN. 2018. A systematic review of the epidemiology of carbapenem-resistant Enterobacteriaceae in the United States. Antimicrob Resist Infect Control 7:55. doi: 10.1186/s13756-018-0346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eichenberger EM, Thaden JT. 2019. Epidemiology and mechanisms of resistance of extensively drug resistant Gram-negative bacteria. Antibiotics 8:37. doi: 10.3390/antibiotics8020037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Duin D, Doi Y. 2017. The global epidemiology of carbapenemase-producing Enterobacteriaceae. Virulence 8:460–469. doi: 10.1080/21505594.2016.1222343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mendes RE, Castanheira M, Woosley LN, Stone GG, Bradford PA, Flamm RK. 2019. Characterization of β-lactamase content of ceftazidime-resistant pathogens recovered during the pathogen-directed phase 3 REPRISE trial for ceftazidime-avibactam: correlation of efficacy against β-lactamase producers. Antimicrob Agents Chemother 63:e02655-18. doi: 10.1128/AAC.02655-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salabi AE, Toleman MA, Weeks J, Bruderer T, Frei R, Walsh TR. 2010. First report of the metallo-beta-lactamase SPM-1 in Europe. Antimicrob Agents Chemother 54:582. doi: 10.1128/AAC.00719-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.King DT, Sobhanifar S, Strynadka N. 2017. The mechanisms of resistance to β-lactam antibiotics In Gotte M, Berghuis A, Matlashewski G, Wainberg M, Sheppard D (ed), Handbook of antimicrobial resistance. Springer, New York, NY. [Google Scholar]
- 24.Izaki K, Matsuhashi M, Strominger JL. 1968. Biosynthesis of the peptidoglycan of bacterial cell walls. 8. Peptidoglycan transpeptidase and D-alanine carboxypeptidase: penicillin-sensitive enzymatic reaction in strains of Escherichia coli. J Biol Chem 243:3180–3192. [PubMed] [Google Scholar]
- 25.Yocum RR, Waxman DJ, Rasmussen JR, Strominger JL. 1979. Mechanism of penicillin action: penicillin and substrate bind covalently to the same active site serine in two bacterial D-alanine carboxypepdidases. Proc Natl Acad Sci U S A 76:2730–2734. doi: 10.1073/pnas.76.6.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fisher J, Belasco JG, Khosla S, Knowles JR. 1980. ß-Lactamase proceeds via an acyl-enzyme intermediate. Interaction of the Escherichia coli RTEM enzyme with cefoxitin. Biochemistry 19:2895–2901. doi: 10.1021/bi00554a012. [DOI] [PubMed] [Google Scholar]
- 27.Dusart J, Leyh-Bouille M, Ghuysen JM. 1977. The peptidoglycan crosslinking enzyme system in Streptomyces strains R61, K15 and rimosus. Kinetic coefficients involved in the interactions of the membrane-bound transpeptidase with peptide substrates and beta-lactam antibiotics. Eur J Biochem 81:33–44. doi: 10.1111/j.1432-1033.1977.tb11924.x. [DOI] [PubMed] [Google Scholar]
- 28.Tooke CL, Hinchliffe P, Bragginton EC, Colenso CK, Hirvonen VHA, Takebayashi Y, Spencer J. 2019. Beta-lactamases and beta-lactamase inhibitors in the 21st century. J Mol Biol 431:3472–3500. doi: 10.1016/j.jmb.2019.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meini S, Tascini C, Cei M, Sozio E, Rossolini GM. 2019. AmpC beta-lactamase-producing Enterobacterales: what a clinician should know. Infection 47:363–375. doi: 10.1007/s15010-019-01291-9. [DOI] [PubMed] [Google Scholar]
- 30.Bonomo RA. 2017. β-Lactamases: a focus on current challenges. Cold Spring Harb Perspect Med 7:a025239. doi: 10.1101/cshperspect.a025239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palzkill T. 2018. Structural and mechanistic basis for extended-spectrum drug-resistance mutations in altering the specificity of TEM, CTX-M, and KPC β-lactamases. Front Mol Biosci 5:16. doi: 10.3389/fmolb.2018.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salahuddin P, Kumar A, Khan AU. 2018. Structure, function of serine and metallo-β-lactamases and their inhibitors. Curr Protein Pept Sci 19:130–144. doi: 10.2174/0929866524666170724160623. [DOI] [PubMed] [Google Scholar]
- 33.Ambler RP. 1980. The structure of β-lactamases. Philos Trans R Soc Lond B Biol Sci 289:321–331. doi: 10.1098/rstb.1980.0049. [DOI] [PubMed] [Google Scholar]
- 34.Jaurin B, Grundstrom T. 1981. ampC cephalosporinase of Escherichia coli K-12 has a different evolutionary origin from that of β-lactamases of the penicillinase type. Proc Natl Acad Sci U S A 78:4897–4901. doi: 10.1073/pnas.78.8.4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huovinen P, Huovinen S, Jacoby GA. 1988. Sequence of PSE-2 beta-lactamase. Antimicrob Agents Chemother 32:134–136. doi: 10.1128/aac.32.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Philippon A, Jacquier H, Ruppe E, Labia R. 2019. Structure-based classification of class A beta-lactamases, an update. Curr Res Translation Med 31:31. doi: 10.1016/j.retram.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 37.Sawai T, Mitsuhashi S, Yamagishi S. 1968. Drug resistance of enteric bacteria. XIV. Comparison of β-lactamases in gram-negative rod bacteria resistant to α-aminobenzylpenicillin. Jpn J Microbiol 12:423–434. doi: 10.1111/j.1348-0421.1968.tb00415.x. [DOI] [PubMed] [Google Scholar]
- 38.Bush K, Jacoby GA, Medeiros AA. 1995. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob Agents Chemother 39:1211–1233. doi: 10.1128/aac.39.6.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bush K, Jacoby GA. 2010. Updated functional classification of β-lactamases. Antimicrob Agents Chemother 54:969–976. doi: 10.1128/AAC.01009-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Spratt BG. 1988. Hybrid penicillin-binding proteins in penicillin-resistant strains of Neisseria gonorrhoeae. Nature 332:173–176. doi: 10.1038/332173a0. [DOI] [PubMed] [Google Scholar]
- 41.Brown DF, Reynolds PE. 1980. Intrinsic resistance to beta-lactam antibiotics in Staphylococcus aureus. FEBS Lett 122:275–278. doi: 10.1016/0014-5793(80)80455-8. [DOI] [PubMed] [Google Scholar]
- 42.Hartman BJ, Tomasz A. 1984. Low-affinity penicillin-binding protein associated with β-lactam resistance in Staphylococcus aureus. J Bacteriol 158:513–516. doi: 10.1128/JB.158.2.513-516.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim IS, Ki CS, Kim S, Oh WS, Peck KR, Song JH, Lee K, Lee NY. 2007. Diversity of ampicillin resistance genes and antimicrobial susceptibility patterns in Haemophilus influenzae strains isolated in Korea. Antimicrob Agents Chemother 51:453–460. doi: 10.1128/AAC.00960-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clark ST, Sinha U, Zhang Y, Wang PW, Donaldson SL, Coburn B, Waters VJ, Yau YCW, Tullis DE, Guttman DS, Hwang DM. 2019. Penicillin-binding protein 3 is a common adaptive target among Pseudomonas aeruginosa isolates from adult cystic fibrosis patients treated with beta-lactams. Int J Antimicrob Agents 53:620–628. doi: 10.1016/j.ijantimicag.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 45.Alm RA, Johnstone MR, Lahiri SD. 2015. Characterization of Escherichia coli NDM isolates with decreased susceptibility to aztreonam/avibactam: role of a novel insertion in PBP3. J Antimicrob Chemother 70:1420–1428. doi: 10.1093/jac/dku568. [DOI] [PubMed] [Google Scholar]
- 46.Zhang Y, Kashikar A, Brown CA, Denys G, Bush K. 2017. Unusual Escherichia coli PBP 3 insertion sequence identified from a collection of carbapenem-resistant Enterobacteriaceae tested in vitro with a combination of ceftazidime-, ceftaroline-, or aztreonam-avibactam. Antimicrob Agents Chemother 61:e00389-17. doi: 10.1128/AAC.00389-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Boxtel R, Wattel AA, Arenas J, Goessens WH, Tommassen J. 2017. Acquisition of carbapenem resistance by plasmid-encoded-AmpC-epressing Escherichia coli. Antimicrob Agents Chemother 61:e01413-16. doi: 10.1128/AAC.01413-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wise MG, Horvath E, Young K, Sahm DF, Kazmierczak KM. 2018. Global survey of Klebsiella pneumoniae major porins from ertapenem non-susceptible isolates lacking carbapenemases. J Med Microbiol 67:289–295. doi: 10.1099/jmm.0.000691. [DOI] [PubMed] [Google Scholar]
- 49.Trias J, Nikaido H. 1990. Outer membrane protein D2 catalyzes facilitated diffusion of carbapenems and penems through the outer membrane of Pseudomonas aeruginosa. Antimicrob Agents Chemother 34:52–57. doi: 10.1128/aac.34.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shu JC, Kuo AJ, Su LH, Liu TP, Lee MH, Su IN, Wu TL. 2017. Development of carbapenem resistance in Pseudomonas aeruginosa is associated with OprD polymorphisms, particularly the amino acid substitution at codon 170. J Antimicrob Chemother 72:2489–2495. doi: 10.1093/jac/dkx158. [DOI] [PubMed] [Google Scholar]
- 51.Nelson K, Hemarajata P, Sun D, Rubio-Aparicio D, Tsivkovski R, Yang S, Sebra R, Kasarskis A, Nguyen H, Hanson BM, Leopold S, Weinstock G, Lomovskaya O, Humphries RM. 2017. Resistance to ceftazidime-avibactam is due to transposition of KPC in a porin-deficient strain of Klebsiella pneumoniae with increased efflux activity. Antimicrob Agents Chemother 61:e00989-17. doi: 10.1128/AAC.00989-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lomovskaya O, Sun D, Rubio-Aparicio D, Nelson K, Tsivkovski R, Griffith DC, Dudley MN. 2017. Vaborbactam: spectrum of β-lactamase inhibition and impact of resistance mechanisms on activity in Enterobacteriaceae. Antimicrob Agents Chemother 61:e01443-17. doi: 10.1128/AAC.01443-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Oliveira Santos IC, Albano RM, Asensi MD, D'Alincourt Carvalho-Assef AP. 2018. Draft genome sequence of KPC-2-producing Pseudomonas aeruginosa recovered from a bloodstream infection sample in Brazil. J Glob Antimicrob Resist 15:99–100. doi: 10.1016/j.jgar.2018.08.021. [DOI] [PubMed] [Google Scholar]
- 54.Wi YM, Greenwood-Quaintance KE, Schuetz AN, Ko KS, Peck KR, Song JH, Patel R. 2018. Activity of ceftolozane-tazobactam against carbapenem-resistant, non-carbapenemase-producing Pseudomonas aeruginosa and associated resistance mechanisms. Antimicrob Agents Chemother 62:e01970-17. doi: 10.1128/AAC.01970-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wiener J, Quinn JP, Bradford PA, Goering RV, Nathan C, Bush K, Weinstein RA. 1999. Multiple antibiotic-resistant Klebsiella and Escherichia coli in nursing homes. JAMA 281:517–523. doi: 10.1001/jama.281.6.517. [DOI] [PubMed] [Google Scholar]
- 56.Kim YA, Kim JJ, Kim H, Lee K. 2017. Community-onset extended-spectrum-beta-lactamase-producing Escherichia coli sequence type 131 at two Korean community hospitals: the spread of multidrug-resistant E. coli to the community via healthcare facilities. Int J Infect Dis 54:39–42. doi: 10.1016/j.ijid.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 57.Miller JH. 1983. Mutational specificity in bacteria. Annu Rev Genet 17:215–238. doi: 10.1146/annurev.ge.17.120183.001243. [DOI] [PubMed] [Google Scholar]
- 58.Barthélémy M, Péduzzi J, Yaghlane HB, Labia R. 1988. Single amino acid substitution between SHV-1 β-lactamase and cefotaxime-hydolyzing SHV-2 enzyme. FEBS Lett 231:217–220. doi: 10.1016/0014-5793(88)80734-8. [DOI] [PubMed] [Google Scholar]
- 59.Bradford PA. 2001. Extended-spectrum β-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev 14:933–951. doi: 10.1128/CMR.14.4.933-951.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hemarajata P, Humphries RM. 2019. Ceftazidime/avibactam resistance associated with L169P mutation in the omega loop of KPC-2. J Antimicrob Chemother 74:1241–1243. doi: 10.1093/jac/dkz026. [DOI] [PubMed] [Google Scholar]
- 61.Livermore DM. 2003. Bacterial resistance: origins, epidemiology, and impact. Clin Infect Dis 36:S11–S23. doi: 10.1086/344654. [DOI] [PubMed] [Google Scholar]
- 62.Jacoby GA. 1997. Extended-spectrum beta-lactamases and other enzymes providing resistance to oxyimino-beta-lactams. Infect Dis Clin North Am 11:875–887. doi: 10.1016/S0891-5520(05)70395-0. [DOI] [PubMed] [Google Scholar]
- 63.Hall RM. 2012. Integrons and gene cassettes: hotspots of diversity in bacterial genomes. Ann N Y Acad Sci 1267:71–78. doi: 10.1111/j.1749-6632.2012.06588.x. [DOI] [PubMed] [Google Scholar]
- 64.Lauretti L, Riccio ML, Mazzariol A, Cornaglia G, Amicosante G, Fontana R, Rossolini GM. 1999. Cloning and characterization of blaVIM, a new integron-borne metallo-β-lactamase gene from a Pseudomonas aeruginosa clinical isolate. Antimicrob Agents Chemother 43:1584–1590. doi: 10.1128/AAC.43.7.1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liapis E, Bour M, Triponney P, Jove T, Zahar JR, Valot B, Jeannot K, Plesiat P. 2019. Identification of diverse integron and plasmid structures carrying a novel carbapenemase among Pseudomonas species. Front Microbiol 10:404. doi: 10.3389/fmicb.2019.00404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Datta N, Kontomichalou P. 1965. Penicillinase synthesis controlled by infectious R factors in Enterobacteriaceae. Nature 208:239–241. doi: 10.1038/208239a0. [DOI] [PubMed] [Google Scholar]
- 67.Medeiros AA. 1984. β-Lactamases. Br Med Bull 40:18–27. doi: 10.1093/oxfordjournals.bmb.a071942. [DOI] [PubMed] [Google Scholar]
- 68.Bajpai T, Pandey M, Varma M, Bhatambare GS. 2017. Prevalence of TEM, SHV, and CTX-M β-lactamase genes in the urinary isolates of a tertiary care hospital. Avicenna J Med 7:12–16. doi: 10.4103/2231-0770.197508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yan J, Zhang J, van der Veen S. 2019. High prevalence of TEM-135 expression from the Asian plasmid in penicillinase-producing Neisseria gonorrhoeae from Hangzhou, China. Int J Antimicrob Agents 54:361–366. doi: 10.1016/j.ijantimicag.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 70.Qin L, Watanabe H, Asoh N, Watanabe K, Oishi K, Mizota T, Nagatake T. 2007. Short report: antimicrobial susceptibility and genetic characteristics of Haemophilus influenzae isolated from patients with respiratory tract infections between 1987 and 2000, including beta-lactamase-negative ampicillin-resistant strains. Epidemiol Infect 135:665–668. doi: 10.1017/S0950268806007023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dabernat H, Delmas C. 2012. Epidemiology and evolution of antibiotic resistance of Haemophilus influenzae in children 5 years of age or less in France, 2001–2008: a retrospective database analysis. Eur J Clin Microbiol Infect Dis 31:2745–2753. doi: 10.1007/s10096-012-1623-9. [DOI] [PubMed] [Google Scholar]
- 72.Resman F, Ristovski M, Forsgren A, Kaijser B, Kronvall G, Medstrand P, Melander E, Odenholt I, Riesbeck K. 2012. Increase of β-lactam-resistant invasive Haemophilus influenzae in Sweden, 1997 to 2010. Antimicrob Agents Chemother 56:4408–4415. doi: 10.1128/AAC.00415-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sondergaard A, Lund M, Norskov-Lauritsen N. 2015. TEM-1-encoding small plasmids impose dissimilar fitness costs on Haemophilus influenzae and Haemophilus parainfluenzae. Microbiology 161:2310–2315. doi: 10.1099/mic.0.000183. [DOI] [PubMed] [Google Scholar]
- 74.Philippon A, Arlet G, Jacoby GA. 2002. Plasmid-determined AmpC-type β-lactamases. Antimicrob Agents Chemother 46:1–11. doi: 10.1128/aac.46.1.1-11.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bradford PA, Urban C, Mariano N, Projan SJ, Rahal JJ, Bush K. 1997. Imipenem resistance in Klebsiella pneumoniae is associated with the combination of ACT-1, a plasmid-mediated AmpC β-lactamase, and the loss of an outer membrane protein. Antimicrob Agents Chemother 41:563–569. doi: 10.1128/AAC.41.3.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Oliver A, Pérez-Díaz JC, Coque TM, Baquero F, Cantón R. 2001. Nucleotide sequence and characterization of a novel cefotaxime-hydrolyzing b-lactamase (CTX-M-10) isolated in Spain. Antimicrob Agents Chemother 45:616–620. doi: 10.1128/AAC.45.2.616-620.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gomez J, Simarro E, Banos V, Requena L, Ruiz J, Garcia F, Canteras M, Valdes M. 1999. Six-year prospective study of risk and prognostic factors in patients with nosocomial sepsis caused by Acinetobacter baumannii. Eur J Clin Microbiol Infect Dis 18:358–361. doi: 10.1007/pl00015019. [DOI] [PubMed] [Google Scholar]
- 78.Elting LS, Khardori N, Bodey GP, Fainstein V. 1990. Nosocomial infection caused by Xanthomonas maltophilia: a case-control study of predisposing factors. Infect Control Hosp Epidemiol 11:134–138. doi: 10.1086/646136. [DOI] [PubMed] [Google Scholar]
- 79.Poirel L, Nordmann P. 2006. Carbapenem resistance in Acinetobacter baumannii: mechanisms and epidemiology. Clin Microbiol Infect 12:826–836. doi: 10.1111/j.1469-0691.2006.01456.x. [DOI] [PubMed] [Google Scholar]
- 80.Mojica MF, Rutter JD, Taracila M, Abriata LA, Fouts DE, Papp-Wallace KM, Walsh TJ, LiPuma JJ, Vila AJ, Bonomo RA. 2019. Population structure, molecular epidemiology, and β-lactamase diversity among Stenotrophomonas maltophilia isolates in the United States. mBio 10:e00405-19. doi: 10.1128/mBio.00405-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Abraham EP, Chain E. 1940. An enzyme from bacteria able to destroy penicillin. Nature 146:837–837. doi: 10.1038/146837a0. [DOI] [PubMed] [Google Scholar]
- 82.Rammelkamp CH, Maxon T. 1942. Resistance of Staphylococcus aureus to the action of penicillin. Proc Soc Exp Biol Med 51:386–389. doi: 10.3181/00379727-51-13986. [DOI] [Google Scholar]
- 83.Kirby WM. 1944. Extraction of a highly potent penicillin inactivator from penicillin resistant staphylococci. Science 99:452–453. doi: 10.1126/science.99.2579.452. [DOI] [PubMed] [Google Scholar]
- 84.Barber M, Whitehead JE. 1949. Bacteriophage types in penicillin-resistant staphylococcal infection. Br Med J 2:565–569. doi: 10.1136/bmj.2.4627.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Medeiros AA. 1997. Evolution and dissemination of β-lactamases accelerated by generations of beta-lactam antibiotics. Clin Infect Dis 24:S19–S45. doi: 10.1093/clinids/24.Supplement_1.S19. [DOI] [PubMed] [Google Scholar]
- 86.Chambers HF. 2001. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis 7:178–182. doi: 10.3201/eid0702.010204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Livermore DM. 2000. Antibiotic resistance in staphylococci. Int J Antimicrob Agents 16(Suppl 1):S3–S10. doi: 10.1016/S0924-8579(00)00299-5. [DOI] [PubMed] [Google Scholar]
- 88.Akpaka PE, Roberts R, Monecke S. 2017. Molecular characterization of antimicrobial resistance genes against Staphylococcus aureus isolates from Trinidad and Tobago. J Infect Public Health 10:316–323. doi: 10.1016/j.jiph.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 89.Vali L, Dashti AA, Mathew F, Udo EE. 2017. Characterization of heterogeneous MRSA and MSSA with reduced susceptibility to chlorhexidine in Kuwaiti hospitals. Front Microbiol 8:1359. doi: 10.3389/fmicb.2017.01359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yang Y, Hu Z, Shang W, Hu Q, Zhu J, Yang J, Peng H, Zhang X, Liu H, Cong Y, Li S, Hu X, Zhou R, Rao X. 2017. Molecular and phenotypic characterization revealed high prevalence of multidrug-resistant methicillin-susceptible Staphylococcus aureus in Chongqing, Southwestern China. Microb Drug Resist 23:241–246. doi: 10.1089/mdr.2016.0078. [DOI] [PubMed] [Google Scholar]
- 91.Richter SS, Doern GV, Heilmann KP, Miner S, Tendolkar S, Riahi F, Diekema DJ. 2016. Detection and prevalence of penicillin-susceptible Staphylococcus aureus in the United States in 2013. J Clin Microbiol 54:812–814. doi: 10.1128/JCM.03109-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hagstrand Aldman M, Skovby A, Påhlman LI. 2017. Penicillin-susceptible Staphylococcus aureus: susceptibility testing, resistance rates and outcome of infection. Infect Dis 49:454–460. doi: 10.1080/23744235.2017.1280617. [DOI] [PubMed] [Google Scholar]
- 93.Hiramatsu K, Asada K, Suzuki E, Okonogi K, Yokota T. 1992. Molecular cloning and nucleotide sequence determination of the regulator region of mecA gene in methicillin-resistant Staphylococcus aureus (MRSA). FEBS Lett 298:133–136. doi: 10.1016/0014-5793(92)80039-j. [DOI] [PubMed] [Google Scholar]
- 94.Arede P, Ministro J, Oliveira DC. 2013. Redefining the role of the beta-lactamase locus in methicillin-resistant Staphylococcus aureus: beta-lactamase regulators disrupt the MecI-mediated strong repression on mecA and optimize the phenotypic expression of resistance in strains with constitutive mecA expression. Antimicrob Agents Chemother 57:3037–3045. doi: 10.1128/AAC.02621-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zygmunt DJ, Stratton CW, Kernodle DS. 1992. Characterization of four β-lactamases produced by Staphylococcus aureus. Antimicrob Agents Chemother 36:440–445. doi: 10.1128/aac.36.2.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Voladri RKR, Tummuru MKR, Kernodle DS. 1996. Structure-function relationships among wild-type variants of Staphylococcus aureus β-lactamase: importance of amino acids 128 and 216. J Bacteriol 178:7248–7253. doi: 10.1128/jb.178.24.7248-7253.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Murray BE, Mederski-Samaroj B. 1983. Transferable beta-lactamase. A new mechanism for in vitro penicillin resistance in Streptococcus faecalis. J Clin Investig 72:1168–1171. doi: 10.1172/JCI111042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zscheck KK, Murray BE. 1991. Nucleotide sequence of the beta-lactamase gene from Enterococcus faecalis HH22 and its similarity to staphylococcal beta-lactamase genes. Antimicrob Agents Chemother 35:1736–1740. doi: 10.1128/aac.35.9.1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nallapareddy SR, Wenxiang H, Weinstock GM, Murray BE. 2005. Molecular characterization of a widespread, pathogenic, and antibiotic resistance-receptive Enterococcus faecalis lineage and dissemination of its putative pathogenicity island. J Bacteriol 187:5709–5718. doi: 10.1128/JB.187.16.5709-5718.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ceci M, Delpech G, Sparo M, Mezzina V, Sanchez Bruni S, Baldaccini B. 2015. Clinical and microbiological features of bacteremia caused by Enterococcus faecalis. J Infect Dev Ctries 9:1195–1203. doi: 10.3855/jidc.6587. [DOI] [PubMed] [Google Scholar]
- 101.Jacoby GA. 2009. AmpC β-lactamases. Clin Microbiol Rev 22:161–182. doi: 10.1128/CMR.00036-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Drawz SM, Papp-Wallace KM, Bonomo RA. 2014. New beta-lactamase inhibitors: a therapeutic renaissance in an MDR world. Antimicrob Agents Chemother 58:1835–1846. doi: 10.1128/AAC.00826-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bush K, Freudenberger JS, Sykes RB. 1982. Interaction of azthreonam and related monobactams with β-lactamases from Gram-negative bacteria. Antimicrob Agents Chemother 22:414–420. doi: 10.1128/aac.22.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Crichlow GV, Kuzin AP, Nukaga M, Mayama K, Sawai T, Knox JR. 1999. Structure of the extended-spectrum class C beta-lactamase of Enterobacter cloacae GC1, a natural mutant with a tandem tripeptide insertion. Biochemistry 38:10256–10261. doi: 10.1021/bi9908787. [DOI] [PubMed] [Google Scholar]
- 105.Holtje JV, Kopp U, Ursinus A, Wiedemann B. 1994. The negative regulator of β-lactamase induction AmpD is a N-acetyl-anhydromuramyl-L-alanine amidase. FEMS Microbiol Lett 122:159–164. doi: 10.1111/j.1574-6968.1994.tb07159.x. [DOI] [PubMed] [Google Scholar]
- 106.Korfmann G, Sanders CC. 1989. ampG is essential for high-level expression of AmpC β-lactamase in Enterobacter cloacae. Antimicrob Agents Chemother 33:1946–1951. doi: 10.1128/aac.33.11.1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hanson ND. 2003. AmpC β-lactamases: what do we need to know for the future? J Antimicrob Chemother 52:2–4. doi: 10.1093/jac/dkg284. [DOI] [PubMed] [Google Scholar]
- 108.Bauernfeind A, Stemplinger I, Jungwirth R, Wilhelm R, Chong Y. 1996. Comparative characterization of the cephamycinase blaCMY-1 gene and its relationship with other β-lactamase genes. Antimicrob Agents Chemother 40:1926–1930. doi: 10.1128/AAC.40.8.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Alvarez M, Tran JH, Chow N, Jacoby GA. 2004. Epidemiology of conjugative plasmid-mediated AmpC β-lactamases in the United States. Antimicrob Agents Chemother 48:533–537. doi: 10.1128/aac.48.2.533-537.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Armand-Lefèvre L, Leflon-Guibout V, Bredin J, Barguellil F, Amor A, Pagès JM, Nicolas-Chanoine M-H. 2003. Imipenem resistance in Salmonella enterica serovar Wien related to porin loss and CMY-4 β-lactamase production. Antimicrob Agents Chemother 47:1165–1168. doi: 10.1128/aac.47.3.1165-1168.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hamzaoui Z, Ocampo-Sosa A, Fernandez Martinez M, Landolsi S, Ferjani S, Maamar E, Saidani M, Slim A, Martinez-Martinez L, Boutiba-Ben Boubaker I. 2018. Role of association of OmpK35 and OmpK36 alteration and blaESBL and/or blaAmpC genes in conferring carbapenem resistance among non-carbapenemase-producing Klebsiella pneumoniae. Int J Antimicrob Agents 52:898–905. doi: 10.1016/j.ijantimicag.2018.03.020. [DOI] [PubMed] [Google Scholar]
- 112.Nicolas-Chanoine M-H, Mayer N, Guyot K, Dumont E, Pagès J-M. 2018. Interplay between membrane permeability and enzymatic barrier leads to antibiotic-dependent resistance in Klebsiella Pneumoniae. Front Microbiol 9:1422. doi: 10.3389/fmicb.2018.01422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chen P-L, Ko W-C, Wu C-J. 2012. Complexity of β-lactamases among clinical Aeromonas isolates and its clinical implications. J Microbiol Immunol Infect 45:398–403. doi: 10.1016/j.jmii.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 114.Walsh TR, Stunt RA, Nabi JA, MacGowan AP, Bennett PM. 1997. Distribution and expression of beta-lactamase genes among Aeromonas spp. J Antimicrob Chemother 40:171–178. doi: 10.1093/jac/40.2.171. [DOI] [PubMed] [Google Scholar]
- 115.Segatore B, Massidda O, Satta G, Setacci D, Amicosante G. 1993. High specificity of cphA-encoded metallo-beta-lactamase from Aeromonas hydrophila AE036 for carbapenems and its contribution to beta-lactam resistance. Antimicrob Agents Chemother 37:1324–1328. doi: 10.1128/aac.37.6.1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Périchon B, Goussard S, Walewski V, Krizova L, Cerqueira G, Murphy C, Feldgarden M, Wortman J, Clermont D, Nemec A, Courvalin P. 2014. Identification of 50 class D β-lactamases and 65 Acinetobacter derived cephalosporinases in Acinetobacter spp. Antimicrob Agents Chemother 58:936–949. doi: 10.1128/AAC.01261-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bou G, Martínez-Beltrán J. 2000. Cloning, nucleotide sequencing, and analysis of the gene encoding an AmpC β-lactamase in Acinetobacter baumannii. Antimicrob Agents Chemother 44:428–432. doi: 10.1128/aac.44.2.428-432.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hamidian M, Hall RM. 2013. ISAba1 targets a specific position upstream of the intrinsic ampC gene of Acinetobacter baumannii leading to cephalosporin resistance. J Antimicrob Chemother 68:2682–2683. doi: 10.1093/jac/dkt233. [DOI] [PubMed] [Google Scholar]
- 119.Rodríguez-Martínez J-M, Nordmann P, Ronco E, Poirel L. 2010. Extended-spectrum cephalosporinase in Acinetobacter baumannii. Antimicrob Agents Chemother 54:3484–3488. doi: 10.1128/AAC.00050-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Karah N, Jolley KA, Hall RM, Uhlin BE. 2017. Database for the ampC alleles in Acinetobacter baumannii. PLoS One 12:e0176695. doi: 10.1371/journal.pone.0176695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Héritier C, Poirel L, Lambert T, Nordmann P. 2005. Contribution of acquired carbapenem-hydrolyzing oxacillinases to carbapenem resistance in Acinetobacter baumannii. Antimicrob Agents Chemother 49:3198–3202. doi: 10.1128/AAC.49.8.3198-3202.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wang TH, Leu YS, Wang NY, Liu CP, Yan TR. 2018. Prevalence of different carbapenemase genes among carbapenem-resistant Acinetobacter baumannii blood isolates in Taiwan. Antimicrob Resist Infect Control 7:123. doi: 10.1186/s13756-018-0410-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Paton R, Miles RS, Hood J, Amyes SG, Miles RS, Amyes SG. 1993. ARI 1: β-lactamase-mediated imipenem resistance in Acinetobacter baumannii. Int J Antimicrob Agents 2:81–87. doi: 10.1016/0924-8579(93)90045-7. [DOI] [PubMed] [Google Scholar]
- 124.Higgins PG, Poirel L, Lehmann M, Nordmann P, Seifert H. 2009. OXA-143, a novel carbapenem-hydrolyzing class D β-Lactamase in Acinetobacter baumannii. Antimicrob Agents Chemother 53:5035–5038. doi: 10.1128/AAC.00856-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zarrilli R, Pournaras S, Giannouli M, Tsakris A. 2013. Global evolution of multidrug-resistant Acinetobacter baumannii clonal lineages. Int J Antimicrob Agents 41:11–19. doi: 10.1016/j.ijantimicag.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 126.Fukuta Y, Muder RR, Agha ME, Clarke LG, Wagener MM, Hensler AM, Doi Y. 2013. Risk factors for acquisition of multidrug-resistant Acinetobacter baumannii among cancer patients. Am J Infect Control 41:1249–1252. doi: 10.1016/j.ajic.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 127.Wendel AF, Malecki M, Otchwemah R, Tellez-Castillo CJ, Sakka SG, Mattner F. 2018. One-year molecular surveillance of carbapenem-susceptible A. baumannii on a German intensive care unit: diversity or clonality. Antimicrob Resist Infect Control 7:145. doi: 10.1186/s13756-018-0436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Granzer H, Hagen RM, Warnke P, Bock W, Baumann T, Schwarz NG, Podbielski A, Frickmann H, Koeller T. 2016. Molecular epidemiology of carbapenem-resistant Acinetobacter baumannii complex isolates from patients that were injured during the Eastern Ukrainian conflict. Eur J Microbiol Immunol 6:109–117. doi: 10.1556/1886.2016.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cheung TKM, Ho PL, Woo PCY, Yuen KY, Chau PY. 2002. Cloning and expression of class A beta-lactamase gene blaABPS in Burkholderia pseudomallei. Antimicrob Agents Chemother 46:1132–1135. doi: 10.1128/aac.46.4.1132-1135.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Rholl DA, Papp-Wallace KM, Tomaras AP, Vasil ML, Bonomo RA, Schweizer HP. 2011. Molecular investigations of PenA-mediated beta-lactam resistance in Burkholderia pseudomallei. Front Microbiol 2:139. doi: 10.3389/fmicb.2011.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Papp-Wallace KM, Becka SA, Zeiser ET, Ohuchi N, Mojica MF, Gatta JA, Falleni M, Tosi D, Borghi E, Winkler ML, Wilson BM, LiPuma JJ, Nukaga M, Bonomo RA. 2017. Overcoming an extremely drug resistant (XDR) pathogen: avibactam restores susceptibility to ceftazidime for Burkholderia cepacia complex isolates from cystic fibrosis patients. ACS Infect Dis 3:502–511. doi: 10.1021/acsinfecdis.7b00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Rodriguez-Martinez JM, Poirel L, Nordmann P. 2009. Extended-spectrum cephalosporinases in Pseudomonas aeruginosa. Antimicrob Agents Chemother 53:1766–1771. doi: 10.1128/AAC.01410-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Castanheira M, Mills JC, Farrell DJ, Jones RN. 2014. Mutation-driven β-lactam resistance mechanisms among contemporary ceftazidime-nonsusceptible Pseudomonas aeruginosa isolates from U.S. hospitals. Antimicrob Agents Chemother 58:6844–6850. doi: 10.1128/AAC.03681-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Berrazeg M, Jeannot K, Ntsogo Enguéné VY, Broutin I, Loeffert S, Fournier D, Plésiat P. 2015. Mutations in β-lactamase AmpC increase resistance of Pseudomonas aeruginosa isolates to antipseudomonal cephalosporins. Antimicrob Agents Chemother 59:6248–6255. doi: 10.1128/AAC.00825-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Girlich D, Naas T, Nordmann P. 2004. Biochemical characterization of the naturally occurring oxacillinase OXA-50 of Pseudomonas aeruginosa. Antimicrob Agents Chemother 48:2043–2048. doi: 10.1128/AAC.48.6.2043-2048.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Petrova A, Feodorova Y, Miteva-Katrandzhieva T, Petrov M, Murdjeva M. 2019. First detected OXA-50 carbapenem-resistant clinical isolates Pseudomonas aeruginosa from Bulgaria and interplay between the expression of main efflux pumps, OprD and intrinsic AmpC. J Med Microbiol 68:1723–1731. doi: 10.1099/jmm.0.001106. [DOI] [PubMed] [Google Scholar]
- 137.Walsh TR, Hall L, Assinder SJ, Nichols WW, Cartwright SJ, MacGowan AP, Bennett PM. 1994. Sequence analysis of the L1 metallo-beta-lactamase from Xanthomonas maltophilia. Biochim Biophys Acta 1218:199–201. doi: 10.1016/0167-4781(94)90011-6. [DOI] [PubMed] [Google Scholar]
- 138.Walsh TR, MacGowan AP, Bennett PM. 1997. Sequence analysis and enzyme kinetics of the L2 serine beta-lactamase from Stenotrophomonas maltophilia. Antimicrob Agents Chemother 41:1460–1464. doi: 10.1128/AAC.41.7.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Avison MB, Higgins CS, Ford PJ, von Heldreich CJ, Walsh TR, Bennett PM. 2002. Differential regulation of L1 and L2 β-lactamase expression in Stenotrophomonas maltophilia. J Antimicrob Chemother 49:387–389. doi: 10.1093/jac/49.2.387. [DOI] [PubMed] [Google Scholar]
- 140.Hu R-M, Huang K-J, Wu L-T, Hsiao Y-J, Yang T-C. 2008. Induction of L1 and L2 β-lactamases of Stenotrophomonas maltophilia. Antimicrob Agents Chemother 52:1198–1200. doi: 10.1128/AAC.00682-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mojica MF, Papp-Wallace KM, Taracila MA, Barnes MD, Rutter JD, Jacobs MR, LiPuma JJ, Walsh TJ, Vila AJ, Bonomo RA. 2017. Avibactam restores the susceptibility of clinical isolates of Stenotrophomonas maltophilia to aztreonam. Antimicrob Agents Chemother 61:e00777-17. doi: 10.1128/AAC.00777-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Brooke JS. 2012. Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Microbiol Rev 25:2–41. doi: 10.1128/CMR.00019-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Morin AS, Poirel L, Mory F, Labia R, Nordmann P. 2002. Biochemical-genetic analysis and distribution of DES-1, an Ambler class A extended-spectrum beta-lactamase from Desulfovibrio desulfuricans. Antimicrob Agents Chemother 46:3215–3222. doi: 10.1128/aac.46.10.3215-3222.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Voha C, Docquier J-D, Rossolini GM, Fosse T. 2006. Genetic and biochemical characterization of FUS-1 (OXA-85), a narrow-spectrum class D beta-lactamase from Fusobacterium nucleatum subsp. polymorphum. Antimicrob Agents Chemother 50:2673–2679. doi: 10.1128/AAC.00058-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Toth M, Stewart NK, Smith C, Vakulenko SB. 2018. Intrinsic class D β-lactamases of Clostridium difficile. mBio 9:e01803-18. doi: 10.1128/mBio.01803-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bush K. 1989. Classification of β-lactamases: groups 1, 2a, 2b, and 2b’. Antimicrob Agents Chemother 33:264–270. doi: 10.1128/aac.33.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Livermore DM. 2008. Defining an extended-spectrum β-lactamase. Clin Microbiol Infect 14(Suppl 1):3–10. doi: 10.1111/j.1469-0691.2007.01857.x. [DOI] [PubMed] [Google Scholar]
- 148.McDanel J, Schweizer M, Crabb V, Nelson R, Samore M, Khader K, Blevins AE, Diekema D, Chiang HY, Nair R, Perencevich E. 2017. Incidence of extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli and Klebsiella infections in the United States: a systematic literature review. Infect Control Hosp Epidemiol 38:1209–1215. doi: 10.1017/ice.2017.156. [DOI] [PubMed] [Google Scholar]
- 149.Kliebe C, Nies BA, Meyer JF, Tolxdorff-Neutzling RM, Wiedemann B. 1985. Evolution of plasmid-coded resistance to broad-spectrum cephalosporins. Antimicrob Agents Chemother 28:302–307. doi: 10.1128/aac.28.2.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sader HS, Pfaller MA, Jones RN. 1994. Prevalence of important pathogens and the antimicrobial activity of parenteral drugs at numerous medical centers in the United States. II. Study of the intra- and interlaboratory dissemination of extended-spectrum beta-lactamase-producing Enterobacteriaceae. Diagn Microbiol Infect Dis 20:203–208. doi: 10.1016/0732-8893(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 151.De Champs C, Sirot D, Chanal C, Bonnet R, Sirot J. 2000. A 1998 survey of extended-spectrum beta-lactamases in Enterobacteriaceae in France. The French Study Group. Antimicrob Agents Chemother 44:3177–3179. doi: 10.1128/aac.44.11.3177-3179.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Livermore DM, Canton R, Gniadkowski M, Nordmann P, Rossolini GM, Arlet G, Ayala J, Coque TM, Kern-Zdanowicz I, Luzzaro F, Poirel L, Woodford N. 2007. CTX-M: changing the face of ESBLs in Europe. J Antimicrob Chemother 59:165–174. doi: 10.1093/jac/dkl483. [DOI] [PubMed] [Google Scholar]
- 153.Peirano G, Pitout J. 2019. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: update on molecular epidemiology and treatment options. Drugs 79:1529–1541. doi: 10.1007/s40265-019-01180-3. [DOI] [PubMed] [Google Scholar]
- 154.Bonnet R. 2004. Growing group of extended-spectrum β-lactamases: the CTX-M enzymes. Antimicrob Agents Chemother 48:1–14. doi: 10.1128/aac.48.1.1-14.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Poirel L, Gniadkowski M, Nordmann P. 2002. Biochemical analysis of the ceftazidime-hydrolysing extended-spectrum beta-lactamase CTX-M-15 and of its structurally related β-lactamase CTX-M-3. J Antimicrob Chemother 50:1031–1034. doi: 10.1093/jac/dkf240. [DOI] [PubMed] [Google Scholar]
- 156.Rodriguez MM, Power P, Radice M, Vay C, Famiglietti A, Galleni M, Ayala JA, Gutkind G. 2004. Chromosome-encoded CTX-M-3 from Kluyvera ascorbata: a possible origin of plasmid-borne CTX-M-1-derived cefotaximases. Antimicrob Agents Chemother 48:4895–4897. doi: 10.1128/AAC.48.12.4895-4897.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Canton R, Gonzalez-Alba JM, Galan JC. 2012. CTX-M enzymes: origin and diffusion. Front Microbiol 3:110. doi: 10.3389/fmicb.2012.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Poirel L, Bonnin RA, Nordmann P. 2012. Genetic support and diversity of acquired extended-spectrum β-lactamases in Gram-negative rods. Infect Genet Evol 12:883–893. doi: 10.1016/j.meegid.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 159.Evans BA, Amyes S. 2014. OXA β-lactamases. Clin Microbiol Rev 27:241–263. doi: 10.1128/CMR.00117-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Poirel L, Castanheira M, Carrër A, Rodriguez CP, Jones RN, Smayevsky J, Nordmann P. 2011. OXA-163, an OXA-48-related class D β-lactamase with extended activity toward expanded-spectrum cephalosporins. Antimicrob Agents Chemother 55:2546–2551. doi: 10.1128/AAC.00022-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Castanheira M, Farrell SE, Deshpande LM, Mendes RE, Jones RN. 2013. Prevalence of β-lactamase-encoding genes among Enterobacteriaceae bacteremia isolates collected in 26 U.S. hospitals: report from the SENTRY Antimicrobial Surveillance Program (2010). Antimicrob Agents Chemother 57:3012–3020. doi: 10.1128/AAC.02252-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Peirano G, Pitout J. 2010. Molecular epidemiology of Escherichia coli producing CTX-M β-lactamases: the worldwide emergence of clone ST131 O25:H4. Int J Antimicrob Agents 35:316–321. doi: 10.1016/j.ijantimicag.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 163.Nicolas-Chanoine M-H, Bertrand X, Madec J-Y. 2014. Escherichia coli ST131, an intriguing clonal group. Clin Microbiol Rev 27:543–574. doi: 10.1128/CMR.00125-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Pitout JD, DeVinney R. 2017. Escherichia coli ST131: a multidrug-resistant clone primed for global domination. F1000Res 6:195. doi: 10.12688/f1000research.10609.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Banerjee R, Johnson JR. 2014. A new clone sweeps clean: the enigmatic emergence of Escherichia coli sequence type 131. Antimicrob Agents Chemother 58:4997–5004. doi: 10.1128/AAC.02824-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Pitout JD, Nordmann P, Laupland KB, Poirel L. 2005. Emergence of Enterobacteriaceae producing extended-spectrum β-lactamases (ESBLs) in the community. J Antimicrob Chemother 56:52–59. doi: 10.1093/jac/dki166. [DOI] [PubMed] [Google Scholar]
- 167.Perez F, Endimiani A, Hujer KM, Bonomo RA. 2007. The continuing challenge of ESBLs. Curr Opin Pharmacol 7:459–469. doi: 10.1016/j.coph.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Paterson DL, Bonomo RA. 2005. Extended-spectrum β-lactamases: a clinical update. Clin Microbiol Rev 18:657–686. doi: 10.1128/CMR.18.4.657-686.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Tawfik AF, Shibl AM, Aljohi MA, Altammami MA, Al-Agamy MH. 2012. Distribution of Ambler class A, B and D beta-lactamases among Pseudomonas aeruginosa isolates. Burns 38:855–860. doi: 10.1016/j.burns.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 170.Amirkamali S, Naserpour-Farivar T, Azarhoosh K, Peymani A. 2017. Distribution of the blaOXA, blVEB-1, and blaGES-1 genes and resistance patterns of ESBL-producing Pseudomonas aeruginosa isolated from hospitals in Tehran and Qazvin, Iran. Rev Soc Bras Med Trop 50:315–320. doi: 10.1590/0037-8682-0478-2016. [DOI] [PubMed] [Google Scholar]
- 171.Laudy AE, Róg P, Smolińska-Król K, Ćmiel M, Słoczyńska A, Patzer J, Dzierżanowska D, Wolinowska R, Starościak B, Tyski S. 2017. Prevalence of ESBL-producing Pseudomonas aeruginosa isolates in Warsaw, Poland, detected by various phenotypic and genotypic methods. PLoS One 12:e0180121. doi: 10.1371/journal.pone.0180121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Fosse T, Giraud-Morin C, Madinier I, Mantoux F, Lacour JP, Ortonne JP. 2004. Aeromonas hydrophila with plasmid-borne class A extended-spectrum β-lactamase TEM-24 and three chromosomal class B, C, and D β-lactamases, isolated from a patient with necrotizing fasciitis. Antimicrob Agents Chemother 48:2342–2343. doi: 10.1128/AAC.48.6.2342-2343.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ye Y, Xu X-H, Li J-B. 2010. Emergence of CTX-M-3, TEM-1 and a new plasmid-mediated MOX-4 AmpC in a multiresistant Aeromonas caviae isolate from a patient with pneumonia. J Med Microbiol 59:843–847. doi: 10.1099/jmm.0.016337-0. [DOI] [PubMed] [Google Scholar]
- 174.Wu C-J, Chuang Y-C, Lee M-F, Lee C-C, Lee H-C, Lee N-Y, Chang C-M, Chen P-L, Lin Y-T, Yan J-J, Ko W-C. 2011. Bacteremia due to extended-spectrum-β-lactamase-producing Aeromonas spp. at a medical center in southern Taiwan. Antimicrob Agents Chemother 55:5813–5818. doi: 10.1128/AAC.00634-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ruppé E, Cherkaoui A, Wagner N, La Scala GC, Beaulieu JY, Girard M, Frey J, Lazarevic V, Schrenzel J. 2018. In vivo selection of a multidrug-resistant Aeromonas salmonicida during medicinal leech therapy. New Microbes New Infect 21:23–27. doi: 10.1016/j.nmni.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bush K, Pannell M, Lock JL, Queenan AM, Jorgensen JH, Lee RM, Lewis JS, Jarrett D. 2013. Detection systems for carbapenemase gene identification should include the SME serine carbapenemase. Int J Antimicrob Agents 41:1–4. doi: 10.1016/j.ijantimicag.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 177.Yang Y, Wu P, Livermore DM. 1990. Biochemical characterization of a β-lactamase that hydrolyzes penems and carbapenems for two Serratia marcescens isolates. Antimicrob Agents Chemother 34:755–758. doi: 10.1128/aac.34.5.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Queenan AM, Torres-Viera C, Gold HS, Carmeli Y, Eliopoulos GM, Moellering RC, Quinn JP, Hindler J, Medeiros AA, Bush K. 2000. SME-type carbapenem-hydrolyzing class A beta-lactamases from geographically diverse Serratia marcescens strains. Antimicrob Agents Chemother 44:3035–3039. doi: 10.1128/aac.44.11.3035-3039.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Queenan AM, Shang WC, Schreckenberger P, Lolans K, Bush K, Quinn J. 2006. SME-3, a novel member of the Serratia marcescens SME family of carbapenem-hydrolyzing beta-lactamases. Antimicrob Agents Chemother 50:3485–3487. doi: 10.1128/AAC.00363-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Cayo R, Leme RC, Streling AP, Matos AP, Nodari CS, Chaves JR, Brandao JL, de Almeida MF, Carrareto V, de Castro Pereira MA, de Almeida JP, Ferreira DC, Gales AC. 2017. Serratia marcescens harboring SME-4 in Brazil: a silent threat. Diagn Microbiol Infect Dis 87:357–358. doi: 10.1016/j.diagmicrobio.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 181.Sherry NL, Baines SL, Howden BP. 2018. Ceftazidime/avibactam susceptibility by three different susceptibility testing methods in carbapenemase-producing Gram-negative bacteria from Australia. Int J Antimicrob Agents 52:82–85. doi: 10.1016/j.ijantimicag.2018.02.017. [DOI] [PubMed] [Google Scholar]
- 182.Pollett S, Miller S, Hindler J, Uslan D, Carvalho M, Humphries RM. 2014. Phenotypic and molecular characteristics of carbapenem-resistant Enterobacteriaceae in a health care system in Los Angeles, California, from 2011 to 2013. J Clin Microbiol 52:4003–4009. doi: 10.1128/JCM.01397-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Hopkins KL, Findlay J, Meunier D, Cummins M, Curtis S, Kustos I, Mustafa N, Perry C, Pike R, Woodford N. 2017. Serratia marcescens producing SME carbapenemases: an emerging resistance problem in the UK? J Antimicrob Chemother 72:1535–1537. doi: 10.1093/jac/dkw567. [DOI] [PubMed] [Google Scholar]
- 184.Mataseje LF, Boyd DA, Delport J, Hoang L, Imperial M, Lefebvre B, Kuhn M, Van Caeseele P, Willey BM, Mulvey MR. 2014. Serratia marcescens harbouring SME-type class A carbapenemases in Canada and the presence of blaSME on a novel genomic island, SmarGI1-1. J Antimicrob Chemother 69:1825–1829. doi: 10.1093/jac/dku040. [DOI] [PubMed] [Google Scholar]
- 185.Hemarajata P, Amick T, Yang S, Gregson E, Holzmeyer C, Bush K, Humphries RM. 2018. Selection of hyperproduction of AmpC and SME-1 in a carbapenem-resistant Serratia marcescens isolate during antibiotic therapy. J Antimicrob Chemother 73:1256–1262. doi: 10.1093/jac/dky028. [DOI] [PubMed] [Google Scholar]
- 186.Rasmussen BA, Bush K, Keeney D, Yang Y, Hare R, O'Gara C, Medeiros AA. 1996. Characterization of IMI-1 beta-lactamase, a class A carbapenem-hydrolyzing enzyme from Enterobacter cloacae. Antimicrob Agents Chemother 40:2080–2086. doi: 10.1128/AAC.40.9.2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Huang L, Wang X, Feng Y, Xie Y, Xie L, Zong Z. 2015. First identification of an IMI-1 carbapenemase-producing colistin-resistant Enterobacter cloacae in China. Ann Clin Microbiol Antimicrob 14:51. doi: 10.1186/s12941-015-0112-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Miltgen G, Bonnin RA, Avril C, Benoit-Cattin T, Martak D, Leclaire A, Traversier N, Roquebert B, Jaffar-Bandjee MC, Lugagne N, Filleul L, Subiros M, de Montera AM, Cholley P, Thouverez M, Dortet L, Bertrand X, Naas T, Hocquet D, Belmonte O. 2018. Outbreak of IMI-1 carbapenemase-producing colistin-resistant Enterobacter cloacae on the French island of Mayotte (Indian Ocean). Int J Antimicrob Agents 52:416–420. doi: 10.1016/j.ijantimicag.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 189.Tarumoto N, Kodana M, Watanabe N, Sakai J, Imai K, Yamaguchi T, Taji Y, Ebihara Y, Murakami T, Maeda T, Mitsutake K, Maesaki S. 2018. First report of the isolation of blaIMI-1-producing colistin-heteroresistant Enterobacter cloacae in Japan, September 2016. J Infect Chemother 24:941–943. doi: 10.1016/j.jiac.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 190.Nordmann P, Mariotte S, Naas T, Labia R, Nicolas M-H. 1993. Biochemical properties of a carbapenem-hydrolyzing β-lactamase from Enterobacter cloacae and cloning of the gene into Escherichia coli. Antimicrob Agents Chemother 37:939–946. doi: 10.1128/aac.37.5.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Deshpande LM, Jones RN, Fritsche TR, Sader HS. 2006. Occurrence and characterization of carbapenemase-producing Enterobacteriaceae: report from the SENTRY Antimicrobial Surveillance Program (2000–2004). Microb Drug Resist 12:223–230. doi: 10.1089/mdr.2006.12.223. [DOI] [PubMed] [Google Scholar]
- 192.Pottumarthy S, Moland ES, Juretschko S, Swanzy SR, Thomson KS, Fritsche TR. 2003. NmcA carbapenem-hydrolyzing enzyme in Enterobacter cloacae in North America. Emerg Infect Dis 9:999–1002. doi: 10.3201/eid0908.030096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Boyd DA, Mataseje LF, Davidson R, Delport JA, Fuller J, Hoang L, Lefebvre B, Levett PN, Roscoe DL, Willey BM, Mulvey MR. 2017. Enterobacter cloacae complex isolates harboring blaNMC-A or blaIMI-type class A carbapenemase genes on novel chromosomal integrative elements and plasmids. Antimicrob Agents Chemother 61:e02578-16. doi: 10.1128/AAC.02578-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Antonelli A, D'Andrea MM, Di Pilato V, Viaggi B, Torricelli F, Rossolini GM. 2015. Characterization of a novel putative Xer-dependent integrative mobile element carrying the blaNMC-A carbapenemase gene, inserted into the chromosome of members of the Enterobacter cloacae complex. Antimicrob Agents Chemother 59:6620–6624. doi: 10.1128/AAC.01452-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, Alberti S, Bush K, Tenover FC. 2001. Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother 45:1151–1161. doi: 10.1128/AAC.45.4.1151-1161.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Yigit H, Queenan AM, Rasheed JK, Biddle JW, Domenech-Sanchez A, Alberti S, Bush K, Tenover FC. 2003. Carbapenem-resistant strain of Klebsiella oxytoca harboring carbapenem-hydrolyzing beta-lactamase KPC-2. Antimicrob Agents Chemother 47:3881–3889. doi: 10.1128/aac.47.12.3881-3889.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Woodford N, Tierno PM Jr, Young K, Tysall L, Palepou MF, Ward E, Painter RE, Suber DF, Shungu D, Silver LL, Inglima K, Kornblum J, Livermore DM. 2004. Outbreak of Klebsiella pneumoniae producing a new carbapenem-hydrolyzing class A beta-lactamase, KPC-3, in a New York Medical Center. Antimicrob Agents Chemother 48:4793–4799. doi: 10.1128/AAC.48.12.4793-4799.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Ke W, Bethel CR, Thomson JM, Bonomo RA, van den Akker F. 2007. Crystal structure of KPC-2: insights into carbapenemase activity in class A β-lactamases. Biochemistry 46:5732–5740. doi: 10.1021/bi700300u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Kazmierczak KM, Biedenbach DJ, Hackel M, Rabine S, de Jonge BLM, Bouchillon SK, Sahm DF, Bradford PA. 2016. Global dissemination of blaKPC into bacterial species beyond Klebsiella pneumoniae and in vitro susceptibility to ceftazidime-avibactam and aztreonam-avibactam. Antimicrob Agents Chemother 60:4490–4500. doi: 10.1128/AAC.00107-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Hu YY, Gu DX, Cai JC, Zhou HW, Zhang R. 2015. Emergence of KPC-2-producing Pseudomonas aeruginosa sequence type 463 isolates in Hangzhou, China. Antimicrob Agents Chemother 59:2914–2917. doi: 10.1128/AAC.04903-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Walther-Rasmussen J, Høiby N. 2007. Class A carbapenemases. J Antimicrob Chemother 60:470–482. doi: 10.1093/jac/dkm226. [DOI] [PubMed] [Google Scholar]
- 202.Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M, Cornaglia G, Garau J, Gniadkowski M, Hayden MK, Kumarasamy K, Livermore DM, Maya JJ, Nordmann P, Patel JB, Paterson DL, Pitout J, Villegas MV, Wang H, Woodford N, Quinn JP. 2013. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis 13:785–796. doi: 10.1016/S1473-3099(13)70190-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Pitout JD, Nordmann P, Poirel L. 2015. Carbapenemase-producing Klebsiella pneumoniae, a key pathogen set for global nosocomial dominance. Antimicrob Agents Chemother 59:5873–5884. doi: 10.1128/AAC.01019-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Carpenter J, Neidig N, Campbell A, Thornsberry T, Truex T, Fortney T, Zhang Y, Bush K. 2019. Activity of imipenem/relebactam against carbapenemase-producing Enterobacteriaceae with high colistin resistance. J Antimicrob Chemother 74:3260–3263. doi: 10.1093/jac/dkz354. [DOI] [PubMed] [Google Scholar]
- 205.Hackel MA, Lomovskaya O, Dudley MN, Karlowsky JA, Sahm DF. 2018. In vitro activity of meropenem-vaborbactam against clinical isolates of KPC-positive Enterobacteriaceae. Antimicrob Agents Chemother 62:e01904-17. doi: 10.1128/AAC.01904-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Haidar G, Clancy CJ, Shields RK, Hao B, Cheng S, Nguyen MH. 2017. Mutations in blaKPC-3 that confer ceftazidime-avibactam resistance encode novel KPC-3 variants that function as extended-spectrum β-lactamases. Antimicrob Agents Chemother 61:e02534-16. doi: 10.1128/AAC.02534-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Barnes MD, Winkler ML, Taracila MA, Page MG, Desarbre E, Kreiswirth BN, Shields RK, Nguyen MH, Clancy C, Spellberg B, Papp-Wallace KM, Bonomo RA. 2017. Klebsiella pneumoniae carbapenemase-2 (KPC-2), substitutions at Ambler position Asp179, and resistance to ceftazidime-avibactam: unique antibiotic-resistant phenotypes emerge from β-lactamase protein engineering. mBio 8:e00528-17. doi: 10.1128/mBio.00528-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Naas T, Cuzon G, Villegas MV, Lartigue MF, Quinn JP, Nordmann P. 2008. Genetic structures at the origin of acquisition of the beta-lactamase blaKPC gene. Antimicrob Agents Chemother 52:1257–1263. doi: 10.1128/AAC.01451-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Mathers AJ, Peirano G, Pitout JD. 2015. The role of epidemic resistance plasmids and international high-risk clones in the spread of multidrug-resistant Enterobacteriaceae. Clin Microbiol Rev 28:565–591. doi: 10.1128/CMR.00116-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Peirano G, Bradford PA, Kazmierczak KM, Chen L, Kreiswirth BN, Pitout JD. 2017. Importance of clonal complex 258 and IncFK2-like plasmids among a global collection of Klebsiella pneumoniae with blaKPC. Antimicrob Agents Chemother 61:e02610-16. doi: 10.1128/AAC.02610-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Satlin MJ, Chen L, Patel G, Gomez-Simmonds A, Weston G, Kim AC, Seo SK, Rosenthal ME, Sperber SJ, Jenkins SG, Hamula CL, Uhlemann AC, Levi MH, Fries BC, Tang YW, Juretschko S, Rojtman AD, Hong T, Mathema B, Jacobs MR, Walsh TJ, Bonomo RA, Kreiswirth BN. 2017. Multicenter clinical and molecular epidemiological analysis of bacteremia due to carbapenem-resistant Enterobacteriaceae (CRE) in the CRE epicenter of the United States. Antimicrob Agents Chemother 61:e02349-16. doi: 10.1128/AAC.02349-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Meletis G, Chatzopoulou F, Fragkouli A, Alexandridou M, Mavrovouniotis I, Chatzinikolaou A, Chatzidimitriou D. 2019. Whole genome approach study of KPC-encoding Klebsiella pneumoniae isolated in Greek private laboratories by non-hospitalized patients. J Glob Antimicrob Resist 20:78–81. doi: 10.1016/j.jgar.2019.07.027. [DOI] [PubMed] [Google Scholar]
- 213.Baraniak A, Izdebski R, Zabicka D, Bojarska K, Gorska S, Literacka E, Fiett J, Hryniewicz W, Gniadkowski M, KPC-PL2 Study Group. 2017. Multiregional dissemination of KPC-producing Klebsiella pneumoniae ST258/ST512 genotypes in Poland, 2010–14. J Antimicrob Chemother 72:1610–1616. doi: 10.1093/jac/dkx054. [DOI] [PubMed] [Google Scholar]
- 214.Rojas LJ, Weinstock GM, De La Cadena E, Diaz L, Rios R, Hanson BM, Brown JS, Vats P, Phillips DS, Nguyen H, Hujer KM, Correa A, Adams MD, Perez F, Sodergren E, Narechania A, Planet PJ, Villegas MV, Bonomo RA, Arias CA. 2017. An analysis of the epidemic of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: convergence of two evolutionary mechanisms creates the perfect storm. J Infect Dis 217:82–92. doi: 10.1093/infdis/jix524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.David S, Reuter S, Harris SR, Glasner C, Feltwell T, Argimon S, Abudahab K, Goater R, Giani T, Errico G, Aspbury M, Sjunnebo S, Koraqi A, Lacej D, Apfalter P, Hartl R, Glupczynski Y, Huang T-D, Strateva T, Marteva-Proevska Y, Andrasevic AT, Butic I, Pieridou-Bagatzouni D, Maikanti-Charalampous P, Hrabak J, Zemlickova H, Hammerum A, Jakobsen L, Ivanova M, Pavelkovich A, Jalava J, Österblad M, Dortet L, Vaux S, Kaase M, Gatermann SG, Vatopoulos A, Tryfinopoulou K, Tóth Á, Jánvári L, Boo TW, McGrath E, Carmeli Y, Adler A, Pantosti A, Monaco M, Raka L, Kurti A, Balode A, Saule M. 2019. Epidemic of carbapenem-resistant Klebsiella pneumoniae in Europe is driven by nosocomial spread. Nat Microbiol 4:1919–1929. doi: 10.1038/s41564-019-0492-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Chen L, Chavda KD, DeLeo FR, Bryant KA, Jacobs MR, Bonomo RA, Kreiswirth BN. 2015. Genome sequence of a Klebsiella pneumoniae sequence type 258 isolate with prophage-encoded K. pneumoniae carbapenemase. Genome Announc 3:e00659-15. doi: 10.1128/genomeA.00659-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Mathers AJ, Stoesser N, Chai W, Carroll J, Barry K, Cherunvanky A, Sebra R, Kasarskis A, Peto TE, Walker AS, Sifri CD, Crook DW, Sheppard AE. 2017. Chromosomal integration of the Klebsiella pneumoniae carbapenemase gene, blaKPC, in Klebsiella species is elusive but not rare. Antimicrob Agents Chemother 61:e01823-16. doi: 10.1128/AAC.01823-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Liang Y, Yin X, Zeng L, Chen S. 2017. Clonal replacement of epidemic KPC-producing Klebsiella pneumoniae in a hospital in China. BMC Infect Dis 17:363. doi: 10.1186/s12879-017-2467-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Chen CM, Guo MK, Ke SC, Lin YP, Li CR, Vy Nguyen HT, Wu LT. 2018. Emergence and nosocomial spread of ST11 carbapenem-resistant Klebsiella pneumoniae co-producing OXA-48 and KPC-2 in a regional hospital in Taiwan. J Med Microbiol 67:957–964. doi: 10.1099/jmm.0.000771. [DOI] [PubMed] [Google Scholar]
- 220.Prado-Vivar MB, Ortiz L, Reyes J, Villacis E, Fornasini M, Baldeon ME, Cardenas PA. 2019. Molecular typing of a large nosocomial outbreak of Klebsiella pneumoniae carbapenemase-producing bacteria in the biggest third level hospital of Quito, Ecuador. J Glob Antimicrob Resist 19:328–332. doi: 10.1016/j.jgar.2019.05.014. [DOI] [PubMed] [Google Scholar]
- 221.Bradford PA, Bratu S, Urban C, Visalli M, Mariano N, Landman D, Rahal JJ, Brooks S, Cebular S, Quale J. 2004. Emergence of carbapenem-resistant Klebsiella species possessing the class A carbapenem-hydrolyzing KPC-2 and inhibitor-resistant TEM-30 beta-lactamases in New York City. Clin Infect Dis 39:55–60. doi: 10.1086/421495. [DOI] [PubMed] [Google Scholar]
- 222.Castanheira M, Huband MD, Mendes RE, Flamm RK. 2017. Meropenem-vaborbactam tested against contemporary Gram-negative isolates collected worldwide during 2014, including carbapenem-resistant, KPC-producing, multidrug-resistant, and extensively drug-resistant Enterobacteriaceae. Antimicrob Agents Chemother 61:e00567-17. doi: 10.1128/AAC.00567-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Castanheira M, Deshpande LM, Mendes RE, Canton R, Sader HS, Jones RN. 2019. Variations in the occurrence of resistance phenotypes and carbapenemase genes among Enterobacteriaceae isolates in 20 years of the SENTRY antimicrobial surveillance program. Open Forum Infect Dis 6:S23–S33. doi: 10.1093/ofid/ofy347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Navon-Venezia S, Leavitt A, Schwaber MJ, Rasheed JK, Srinivasan A, Patel JB, Carmeli Y, Israeli KPC Kpn Study Group. 2009. First report on a hyperepidemic clone of KPC-3-producing Klebsiella pneumoniae in Israel genetically related to a strain causing outbreaks in the United States. Antimicrob Agents Chemother 53:818–820. doi: 10.1128/AAC.00987-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Palmeiro JK, de Souza RF, Schorner MA, Passarelli-Araujo H, Grazziotin AL, Vidal NM, Venancio TM, Dalla-Costa LM. 2019. Molecular epidemiology of multidrug-resistant Klebsiella pneumoniae isolates in a Brazilian tertiary hospital. Front Microbiol 10:1669. doi: 10.3389/fmicb.2019.01669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Liu L, Feng Y, Long H, McNally A, Zong Z. 2018. Sequence type 273 carbapenem-resistant Klebsiella pneumoniae carrying blaNDM-1 and blaIMP-4. Antimicrob Agents Chemother 62:e00160-18. doi: 10.1128/AAC.00160-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Schweizer C, Bischoff P, Bender J, Kola A, Gastmeier P, Hummel M, Klefisch FR, Schoenrath F, Fruhauf A, Pfeifer Y. 2019. Plasmid-mediated transmission of KPC-2 carbapenemase in Enterobacteriaceae in critically ill patients. Front Microbiol 10:276. doi: 10.3389/fmicb.2019.00276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Protonotariou E, Poulou A, Politi L, Sgouropoulos I, Metallidis S, Kachrimanidou M, Pournaras S, Tsakris A, Skoura L. 2018. Hospital outbreak due to a Klebsiella pneumoniae ST147 clonal strain co-producing KPC-2 and VIM-1 carbapenemases in a tertiary teaching hospital in northern Greece. Int J Antimicrob Agents 52:331–337. doi: 10.1016/j.ijantimicag.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 229.Kim JO, Song SA, Yoon EJ, Shin JH, Lee H, Jeong SH, Lee K. 2017. Outbreak of KPC-2-producing Enterobacteriaceae caused by clonal dissemination of Klebsiella pneumoniae ST307 carrying an IncX3-type plasmid harboring a truncated Tn4401a. Diagn Microbiol Infect Dis 87:343–348. doi: 10.1016/j.diagmicrobio.2016.12.012. [DOI] [PubMed] [Google Scholar]
- 230.Song JE, Jeong H, Lim YS, Ha EJ, Jung IY, Jeong W, Choi H, Jeong SJ, Ku NS, Park ES, Yong D, Lee K, Kim JM, Choi JY. 2019. An outbreak of KPC-producing Klebsiella pneumoniae linked with an index case of community-acquired KPC-producing isolate: rpidemiological investigation and whole genome sequencing analysis. Microb Drug Resist 25:1475–1483. doi: 10.1089/mdr.2018.0475. [DOI] [PubMed] [Google Scholar]
- 231.Vubil D, Figueiredo R, Reis T, Canha C, Boaventura L, Da Silva GJ. 2017. Outbreak of KPC-3-producing ST15 and ST348 Klebsiella pneumoniae in a Portuguese hospital. Epidemiol Infect 145:595–599. doi: 10.1017/S0950268816002442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Ruppe E, Olearo F, Pires D, Baud D, Renzi G, Cherkaoui A, Goldenberger D, Huttner A, Francois P, Harbarth S, Schrenzel J. 2017. Clonal or not clonal? Investigating hospital outbreaks of KPC-producing Klebsiella pneumoniae with whole-genome sequencing. Clin Microbiol Infect 23:470–475. doi: 10.1016/j.cmi.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 233.Snitkin ES, NISC Comparative Sequencing Program Group, Zelazny AM, Thomas PJ, Stock F, Group N, Henderson DK, Palmore TN, Segre JA. 2012. Tracking a hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with whole-genome sequencing. Sci Transl Med 4:148ra116. doi: 10.1126/scitranslmed.3004129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Abdallah M, Olafisoye O, Cortes C, Urban C, Landman D, Ghitan M, Collins B, Bratu S, Quale J. 2016. Rise and fall of KPC-producing Klebsiella pneumoniae in New York City. J Antimicrob Chemother 71:2945–2948. doi: 10.1093/jac/dkw242. [DOI] [PubMed] [Google Scholar]
- 235.Schwaber MJ, Israel Carbapenem-Resistant Enterobacteriaceae Working Group, Lev B, Israeli A, Solter E, Smollan G, Rubinovitch B, Shalit I, Carmeli Y. 2011. Containment of a country-wide outbreak of carbapenem-resistant Klebsiella pneumoniae in Israeli hospitals via a nationally implemented intervention. Clin Infect Dis 52:848–855. doi: 10.1093/cid/cir025. [DOI] [PubMed] [Google Scholar]
- 236.Mairi A, Pantel A, Sotto A, Lavigne JP, Touati A. 2018. OXA-48-like carbapenemases producing Enterobacteriaceae in different niches. Eur J Clin Microbiol Infect Dis 37:587–604. doi: 10.1007/s10096-017-3112-7. [DOI] [PubMed] [Google Scholar]
- 237.Ehmann DE, Jahic H, Ross PL, Gu RF, Hu J, Durand-Reville TF, Lahiri S, Thresher J, Livchak S, Gao N, Palmer T, Walkup GK, Fisher SL. 2013. Kinetics of avibactam inhibition against class A, C, and D β-lactamases. J Biol Chem 288:27960–27971. doi: 10.1074/jbc.M113.485979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Haidar G, Clancy CJ, Chen L, Samanta P, Shields RK, Kreiswirth BN, Nguyen MH. 2017. Identifying spectra of activity and therapeutic niches for ceftazidime-avibactam and imipenem-relebactam against carbapenem-resistant Enterobacteriaceae. Antimicrob Agents Chemother 61:e00642-17. doi: 10.1128/AAC.00642-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Poirel L, Heritier C, Tolun V, Nordmann P. 2004. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob Agents Chemother 48:15–22. doi: 10.1128/aac.48.1.15-22.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Aubert D, Naas T, Héritier C, Poirel L, Nordmann P. 2006. Functional characterization of IS1999, an IS4 family element involved in mobilization and expression of β-lactam resistance genes. J Bacteriol 188:6506–6514. doi: 10.1128/JB.00375-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Poirel L, Potron A, Nordmann P. 2012. OXA-48-like carbapenemases: the phantom menace. J Antimicrob Chemother 67:1597–1606. doi: 10.1093/jac/dks121. [DOI] [PubMed] [Google Scholar]
- 242.Pérez-Blanco V, Redondo-Bravo L, Ruíz-Carrascoso G, Paño-Pardo JR, Gómez-Gil R, Robustillo-Rodela A, García-Rodríguez J, Mingorance J, Herruzo R. 2018. Epidemiology and control measures of an OXA-48-producing Enterobacteriaceae hospital-wide oligoclonal outbreak. Epidemiol Infect 146:656–662. doi: 10.1017/S0950268818000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Ortega A, Sáez D, Bautista V, Fernández-Romero S, Lara N, Aracil B, Pérez-Vázquez M, Campos J, Oteo J, Spanish Collaborating Group for the Antibiotic Resistance Surveillance Programme. 2016. Carbapenemase-producing Escherichia coli is becoming more prevalent in Spain mainly because of the polyclonal dissemination of OXA-48. J Antimicrob Chemother 71:2131–2138. doi: 10.1093/jac/dkw148. [DOI] [PubMed] [Google Scholar]
- 244.Arana DM, Ortega A, González-Barberá E, Lara N, Bautista V, Gómez-Ruíz D, Sáez D, Fernández-Romero S, Aracil B, Pérez-Vázquez M, Campos J, Oteo J, Spanish Antibiotic Resistance Surveillance Programme Collaborating Group. 2017. Carbapenem-resistant Citrobacter spp. isolated in Spain from 2013 to 2015 produced a variety of carbapenemases including VIM-1, OXA-48, KPC-2, NDM-1 and VIM-2. J Antimicrob Chemother 72:3283–3287. doi: 10.1093/jac/dkx325. [DOI] [PubMed] [Google Scholar]
- 245.Pfaller MA, Huband MD, Mendes RE, Flamm RK, Castanheira M. 2018. In vitro activity of meropenem/vaborbactam and characterisation of carbapenem resistance mechanisms among carbapenem-resistant Enterobacteriaceae from the 2015 meropenem/vaborbactam surveillance programme. Int J Antimicrob Agents 52:144–150. doi: 10.1016/j.ijantimicag.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 246.Kazmierczak KM, Bradford PA, Stone GG, de Jonge BLM, Sahm DF. 2018. In vitro activity of ceftazidime-avibactam and aztreonam-avibactam against OXA-48-carrying Enterobacteriaceae isolated as part of the International Network for Optimal Resistance Monitoring (INFORM) global surveillance program from 2012 to 2015. Antimicrob Agents Chemother 62:12. doi: 10.1128/AAC.00592-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Mataseje LF, Boyd DA, Fuller J, Haldane D, Hoang L, Lefebvre B, Melano RG, Poutanen S, Van Caeseele P, Mulvey MR. 2018. Characterization of OXA-48-like carbapenemase producers in Canada, 2011–14. J Antimicrob Chemother 73:626–633. doi: 10.1093/jac/dkx462. [DOI] [PubMed] [Google Scholar]
- 248.Lascols C, Peirano G, Hackel M, Laupland KB, Pitout JD. 2013. Surveillance and molecular epidemiology of Klebsiella pneumoniae isolates that produce carbapenemases: first report of OXA-48-like enzymes in North America. Antimicrob Agents Chemother 57:130–136. doi: 10.1128/AAC.01686-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Lutgring JD, Zhu W, de Man TJB, Avillan JJ, Anderson KF, Lonsway DR, Rowe LA, Batra D, Rasheed JK, Limbago BM. 2018. Phenotypic and genotypic characterization of Enterobacteriaceae producing oxacillinase-48-like carbapenemases, United States. Emerg Infect Dis 24:700–709. doi: 10.3201/eid2404.171377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Senchyna F, Gaur RL, Sandlund J, Truong C, Tremintin G, Kultz D, Gomez CA, Tamburini FB, Andermann T, Bhatt A, Tickler I, Watz N, Budvytiene I, Shi G, Tenover FC, Banaei N. 2019. Diversity of resistance mechanisms in carbapenem-resistant Enterobacteriaceae at a health care system in Northern California, from 2013 to 2016. Diagn Microbiol Infect Dis 93:250–257. doi: 10.1016/j.diagmicrobio.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Potron A, Hocquet D, Triponney P, Plésiat P, Bertrand X, Valot B. 2019. Carbapenem-susceptible OXA-23-producing Proteus mirabilis in the French community. Antimicrob Agents Chemother 63:e00191-19. doi: 10.1128/AAC.00191-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Rossolini GM, Zanchi A, Chiesurin A, Amicosante G, Satta G, Guglielmetti P. 1995. Distribution of cphA or related carbapenemase-encoding genes and production of carbapenemase activity in members of the genus Aeromonas. Antimicrob Agents Chemother 39:346–349. doi: 10.1128/aac.39.2.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Sinclair HA, Heney C, Sidjabat HE, George NM, Bergh H, Anuj SN, Nimmo GR, Paterson DL. 2016. Genotypic and phenotypic identification of Aeromonas species and CphA-mediated carbapenem resistance in Queensland, Australia. Diagn Microbiol Infect Dis 85:98–101. doi: 10.1016/j.diagmicrobio.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 254.Wu C-J, Chen P-L, Wu J-J, Yan J-J, Lee C-C, Lee H-C, Lee N-Y, Chang C-M, Lin Y-T, Chiu Y-C, Ko W-C. 2012. Distribution and phenotypic and genotypic detection of a metallo-β-lactamase, CphA, among bacteraemic Aeromonas isolates. J Med Microbiol 61:712–719. doi: 10.1099/jmm.0.038323-0. [DOI] [PubMed] [Google Scholar]
- 255.Wu CJ, Ko WC, Lee NY, Su SL, Li CW, Li MC, Chen YW, Su YC, Shu CY, Lin YT, Chen PL. 2019. Genotypic and phenotypic characteristics of Aeromonas isolates from fish and patients in Tainan City. Appl Environ Microbiol 16:16. doi: 10.1128/AEM.01360-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Piccirilli A, Pompilio A, Rossi L, Segatore B, Amicosante G, Rosatelli G, Perilli M, Di Bonaventura G. 2019. Identification of CTX-M-15 and CTX-M-27 in antibiotic-resistant Gram-negative bacteria isolated from three rivers running in central Italy. Microb Drug Resist 25:1041–1049. doi: 10.1089/mdr.2019.0016. [DOI] [PubMed] [Google Scholar]
- 257.Piotrowska M, Przygodzińska D, Matyjewicz K, Popowska M. 2017. Occurrence and variety of beta-lactamase genes among Aeromonas spp. isolated from urban wastewater treatment plant. Front Microbiol 8:863. doi: 10.3389/fmicb.2017.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Wimalasena S, De Silva BCJ, Hossain S, Pathirana H, Heo GJ. 2017. Prevalence and characterisation of quinolone resistance genes in Aeromonas spp. isolated from pet turtles in South Korea. J Glob Antimicrob Resist 11:34–38. doi: 10.1016/j.jgar.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 259.De Silva BCJ, Hossain S, Dahanayake PS, Heo GJ. 2018. Frozen white-leg shrimp (Litopenaeus vannamei) in Korean markets as a source of Aeromonas spp. harboring antibiotic and heavy metal resistance genes. Microb Drug Resist 24:24. doi: 10.1089/mdr.2018.0035. [DOI] [PubMed] [Google Scholar]
- 260.Sánchez-Céspedes J, Figueras MJ, Aspiroz C, Aldea MJ, Toledo M, Alperí A, Marco F, Vila J. 2009. Development of imipenem resistance in an Aeromonas veronii biovar sobria clinical isolate recovered from a patient with cholangitis. J Med Microbiol 58:451–455. doi: 10.1099/jmm.0.47804-0. [DOI] [PubMed] [Google Scholar]
- 261.Yotsuji A, Minami S, Inoue M, Mitsuhashi S. 1983. Properties of novel β-lactamase produced by Bacteroides fragilis. Antimicrob Agents Chemother 24:925–929. doi: 10.1128/aac.24.6.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Cuchural GJ Jr, Malamy MH, Tally FP. 1986. β-Lactamase-mediated imipenem resistance in Bacteroides fragilis. Antimicrob Agents Chemother 30:645–648. doi: 10.1128/aac.30.5.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Thompson JS, Malamy MH. 1990. Sequencing the gene for an imipenem-cefoxitin-hydrolyzing enzyme (CfiA) from Bacteroides fragilis TAL2480 reveals strong similarity between CfiA and Bacillus cereus β-lactamase II. J Bacteriol 172:2584–2593. doi: 10.1128/jb.172.5.2584-2593.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Rasmussen BA, Gluzman Y, Tally FP. 1990. Cloning and sequencing of the class B β-lactamase gene (ccrA) from Bacteroides fragilis TAL3636. Antimicrob Agents Chemother 34:1590–1592. doi: 10.1128/aac.34.8.1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Podglajen I, Breuil J, Collatz E. 1994. Insertion of a novel DNA sequence, 1S1186, upstream of the silent carbapenemase gene cfiA, promotes expression of carbapenem resistance in clinical isolates of Bacteroides fragilis. Mol Microbiol 12:105–114. doi: 10.1111/j.1365-2958.1994.tb00999.x. [DOI] [PubMed] [Google Scholar]
- 266.Gao Q, Wu S, Xu T, Zhao X, Huang H, Hu F. 2019. Emergence of carbapenem resistance in Bacteroides fragilis in China. Int J Antimicrob Agents 53:859–863. doi: 10.1016/j.ijantimicag.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 267.Jeverica S, Soki J, Premru MM, Nagy E, Papst L. 2019. High prevalence of division II (cfiA positive) isolates among blood stream Bacteroides fragilis in Slovenia as determined by MALDI-TOF MS. Anaerobe 58:30–34. doi: 10.1016/j.anaerobe.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 268.Litterio MR, Cejas D, Gutkind G, Radice M. 2017. Identification of CfiA coding genes in Bacteroides fragilis isolates recovered in Argentina. Inconsistencies in CfiA organization and nomenclature. Anaerobe 48:257–261. doi: 10.1016/j.anaerobe.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 269.Snydman DR, Jacobus NV, McDermott LA, Goldstein EJ, Harrell L, Jenkins SG, Newton D, Patel R, Hecht DW. 2017. Trends in antimicrobial resistance among Bacteroides species and Parabacteroides species in the United States from 2010–2012 with comparison to 2008–2009. Anaerobe 43:21–26. doi: 10.1016/j.anaerobe.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 270.Carlson CJ, Kracalik IT, Ross N, Alexander KA, Hugh-Jones ME, Fegan M, Elkin BT, Epp T, Shury TK, Zhang W, Bagirova M, Getz WM, Blackburn JK. 2019. The global distribution of Bacillus anthracis and associated anthrax risk to humans, livestock and wildlife. Nat Microbiol 4:1337–1343. doi: 10.1038/s41564-019-0435-4. [DOI] [PubMed] [Google Scholar]
- 271.Lewin A, Quach C, Rigourd V, Picaud JC, Perreault T, Frange P, Domingo MC, Lalancette C, Delage G, Germain M. 2019. Bacillus cereus infection in neonates and the absence of evidence for the role of banked human milk: case reports and literature review. Infect Control Hosp Epidemiol 40:787–793. doi: 10.1017/ice.2019.110. [DOI] [PubMed] [Google Scholar]
- 272.Chen Y, Succi J, Tenover FC, Koehler TM. 2003. Beta-lactamase genes of the penicillin-susceptible Bacillus anthracis Sterne strain. J Bacteriol 185:823–830. doi: 10.1128/jb.185.3.823-830.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Lim HM, Pene JJ, Shaw R. 1988. Cloning, nucleotide sequence, and expression of the Bacillus cereus 5/B/6 ß-lactamase II structural gene. J Bacteriol 170:2873–2878. doi: 10.1128/jb.170.6.2873-2878.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Materon IC, Queenan AM, Koehler TM, Bush K, Palzkill T. 2003. Biochemical characterization of beta-lactamases Bla1 and Bla2 from Bacillus anthracis. Antimicrob Agents Chemother 47:2040–2042. doi: 10.1128/aac.47.6.2040-2042.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Ross CL, Thomason KS, Koehler TM. 2009. An extracytoplasmic function sigma factor controls beta-lactamase gene expression in Bacillus anthracis and other Bacillus cereus group species. J Bacteriol 191:6683–6693. doi: 10.1128/JB.00691-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Jean SS, Lee WS, Chen FL, Ou TY, Hsueh PR. 2014. Elizabethkingia meningoseptica: an important emerging pathogen causing healthcare-associated infections. J Hosp Infect 86:244–249. doi: 10.1016/j.jhin.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 277.Mirza HC, Tuncer Ö, Ölmez S, Şener B, Tuğcu GD, Özçelik U, Gürsoy NC, Otlu B, Büyükçam A, Kara A, Sancak B. 2018. Clinical strains of Chryseobacterium and Elizabethkingia spp. isolated from pediatric patients in a university hospital: performance of MALDI-TOF MS-based identification, antimicrobial susceptibilities, and baseline patient characteristics. Microb Drug Resist 24:816–821. doi: 10.1089/mdr.2017.0206. [DOI] [PubMed] [Google Scholar]
- 278.González LJ, Vila AJ. 2012. Carbapenem resistance in Elizabethkingia meningoseptica is mediated by metallo-β-lactamase BlaB. Antimicrob Agents Chemother 56:1686–1692. doi: 10.1128/AAC.05835-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Morán-Barrio J, Lisa M-N, Larrieux N, Drusin SI, Viale AM, Moreno DM, Buschiazzo A, Vila AJ. 2016. Crystal structure of the metallo-β-lactamase GOB in the periplasmic dizinc form reveals an unusual metal site. Antimicrob Agents Chemother 60:6013–6022. doi: 10.1128/AAC.01067-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Mercuri P, Ishii Y, Ma L, Rossolini G, Luzzaro F, Amicosante G, Franceschini N, Frere J, Galleni M. 2002. Clonal diversity and metallo-beta-lactamase production in clinical isolates of Stenotrophomonas maltophilia. Microb Drug Resist 8:193–200. doi: 10.1089/107662902760326904. [DOI] [PubMed] [Google Scholar]
- 281.Karlowsky JA, Hackel MA, Tsuji M, Yamano Y, Echols R, Sahm DF. 2019. In vitro activity of cefiderocol, a siderophore cephalosporin, against Gram-negative bacilli isolated by clinical laboratories in North America and Europe in 2015–2016: SIDERO-WT-2015. Int J Antimicrob Agents 53:456–466. doi: 10.1016/j.ijantimicag.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 282.Watanabe M, Iyobe S, Inoue M, Mitsuhashi S. 1991. Transferable imipenem resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother 35:147–151. doi: 10.1128/aac.35.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Queenan AM, Bush K. 2007. Carbapenemases: the versatile β-lactamases. Clin Microbiol Rev 20:440–458. doi: 10.1128/CMR.00001-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Osano E, Arakawa Y, Wacharotayankun R, Ohta M, Horii T, Ito H, Yoshimura F, Kato N. 1994. Molecular characterization of an enterobacterial metallo beta-lactamase found in a clinical isolate of Serratia marcescens that shows imipenem resistance. Antimicrob Agents Chemother 38:71–78. doi: 10.1128/aac.38.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Matsumura Y, Peirano G, Bradford PA, Motyl MR, DeVinney R, Pitout J. 2018. Genomic characterization of IMP and VIM carbapenemase-encoding transferable plasmids of Enterobacteriaceae. J Antimicrob Chemother 73:3034–3038. doi: 10.1093/jac/dky303. [DOI] [PubMed] [Google Scholar]
- 286.Karlowsky JA, Lob SH, Kazmierczak KM, Badal RE, Young K, Motyl MR, Sahm DF. 2017. In vitro activity of imipenem against carbapenemase-positive Enterobacteriaceae isolates collected by the SMART global surveillance program from 2008 to 2014. J Clin Microbiol 55:1638–1649. doi: 10.1128/JCM.02316-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Kazmierczak KM, Rabine S, Hackel M, McLaughlin RE, Biedenbach DJ, Bouchillon SK, Sahm DF, Bradford PA. 2016. Multiyear, multinational survey of the incidence and global distribution of metallo-β-lactamase-producing Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother 60:1067–1078. doi: 10.1128/AAC.02379-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Malchione MD, Torres LM, Hartley DM, Koch M, Goodman J. 2019. Carbapenem and colistin resistance in Enterobacteriaceae in Southeast Asia: review and mapping of emerging and overlapping challenges. Int J Antimicrob Agents 54:381–399. doi: 10.1016/j.ijantimicag.2019.07.019. [DOI] [PubMed] [Google Scholar]
- 289.Matsumura Y, Peirano G, Motyl MR, Adams MD, Chen L, Kreiswirth B, DeVinney R, Pitout JD. 2017. Global molecular epidemiology of IMP-producing Enterobacteriaceae. Antimicrob Agents Chemother 61:e02729-16. doi: 10.1128/AAC.02729-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Pagani L, Colinon C, Migliavacca R, Labonia M, Docquier J-D, Nucleo E, Spalla M, Li Bergoli M, Rossolini GM. 2005. Nosocomial outbreak caused by multidrug-resistant Pseudomonas aeruginosa producing IMP-13 metallo-beta-lactamase. J Clin Microbiol 43:3824–3828. doi: 10.1128/JCM.43.8.3824-3828.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Rossolini GM, Luzzaro F, Migliavacca R, Mugnaioli C, Pini B, De Luca F, Perilli M, Pollini S, Spalla M, Amicosante G, Toniolo A, Pagani L. 2008. First countrywide survey of acquired metallo-beta-lactamases in gram-negative pathogens in Italy. Antimicrob Agents Chemother 52:4023–4029. doi: 10.1128/AAC.00707-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Ghaith DM, Zafer MM, Ismail DK, Al-Agamy MH, Bohol MFF, Al-Qahtani A, Al-Ahdal MN, Elnagdy SM, Mostafa IY. 2018. First reported nosocomial outbreak of Serratia marcescens harboring blaIMP-4 and blaVIM-2 in a neonatal intensive care unit in Cairo, Egypt. Infect Drug Resist 11:2211–2217. doi: 10.2147/IDR.S174869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Yaghi J, Fattouh N, Akkawi C, Chamy LE, Maroun RG, Khalil G. 2019. Unusually high prevalence of cosecretion of Ambler class A and B carbapenemases and nonenzymatic mechanisms in multidrug-resistant cinical isolates of Pseudomonas aeruginosa in Lebanon. Microb Drug Resist 19:19. doi: 10.1089/mdr.2019.0040. [DOI] [PubMed] [Google Scholar]
- 294.Poirel L, Naas T, Nicolas D, Collet L, Bellais S, Cavallo JD, Nordmann P. 2000. Characterization of VIM-2, a carbapenem-hydrolyzing metallo-beta-lactamase and its plasmid- and integron-borne gene from a Pseudomonas aeruginosa clinical isolate in France. Antimicrob Agents Chemother 44:891–897. doi: 10.1128/aac.44.4.891-897.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Matsumura Y, Peirano G, Devinney R, Bradford PA, Motyl MR, Adams MD, Chen L, Kreiswirth B, Pitout J. 2017. Genomic epidemiology of global VIM-producing Enterobacteriaceae. J Antimicrob Chemother 72:2249–2258. doi: 10.1093/jac/dkx148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Leung GH, Gray TJ, Cheong EY, Haertsch P, Gottlieb T. 2013. Persistence of related blaIMP-4 metallo-beta-lactamase producing Enterobacteriaceae from clinical and environmental specimens within a burns unit in Australia–a six-year retrospective study. Antimicrob Resist Infect Control 2:35. doi: 10.1186/2047-2994-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Findlay J, Hopkins KL, Alvarez-Buylla A, Meunier D, Mustafa N, Hill R, Pike R, McCrae LX, Hawkey PM, Woodford N. 2017. Characterization of carbapenemase-producing Enterobacteriaceae in the West Midlands region of England: 2007–14. J Antimicrob Chemother 72:1054–1062. doi: 10.1093/jac/dkw560. [DOI] [PubMed] [Google Scholar]
- 298.Lagatolla C, Edalucci E, Dolzani L, Riccio ML, De Luca F, Medessi E, Rossolini GM, Tonin EA. 2006. Molecular evolution of metallo-beta-lactamase-producing Pseudomonas aeruginosa in a nosocomial setting of high-level endemicity. J Clin Microbiol 44:2348–2353. doi: 10.1128/JCM.00258-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Pournaras S, Maniati M, Petinaki E, Tzouvelekis LS, Tsakris A, Legakis NJ, Maniatis AN. 2003. Hospital outbreak of multiple clones of Pseudomonas aeruginosa carrying the unrelated metallo-beta-lactamase gene variants blaVIM-2 and blaVIM-4. J Antimicrob Chemother 51:1409–1414. doi: 10.1093/jac/dkg239. [DOI] [PubMed] [Google Scholar]
- 300.Tokatlidou D, Tsivitanidou M, Pournaras S, Ikonomidis A, Tsakris A, Sofianou D. 2008. Outbreak caused by a multidrug-resistant Klebsiella pneumoniae clone carrying blaVIM-12 in a university hospital. J Clin Microbiol 46:1005–1008. doi: 10.1128/JCM.01573-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Cagnacci S, Gualco L, Roveta S, Mannelli S, Borgianni L, Docquier JD, Dodi F, Centanaro M, Debbia E, Marchese A, Rossolini GM. 2008. Bloodstream infections caused by multidrug-resistant Klebsiella pneumoniae producing the carbapenem-hydrolysing VIM-1 metallo-beta-lactamase: first Italian outbreak. J Antimicrob Chemother 61:296–300. doi: 10.1093/jac/dkm471. [DOI] [PubMed] [Google Scholar]
- 302.Giakoupi P, Maltezou H, Polemis M, Pappa O, Saroglou G, Vatopoulos A, Greek System for the Surveillance of Antimicrobial Resistance. 2009. KPC-2-producing Klebsiella pneumoniae infections in Greek hospitals are mainly due to a hyperepidemic clone. Euro Surveill 14:19218. doi: 10.2807/ese.14.21.19218-en. [DOI] [PubMed] [Google Scholar]
- 303.Spyropoulou A, Papadimitriou-Olivgeris M, Bartzavali C, Vamvakopoulou S, Marangos M, Spiliopoulou I, Anastassiou ED, Christofidou M. 2016. A ten-year surveillance study of carbapenemase-producing Klebsiella pneumoniae in a tertiary care Greek university hospital: predominance of KPC- over VIM- or NDM-producing isolates. J Med Microbiol 65:240–246. doi: 10.1099/jmm.0.000217. [DOI] [PubMed] [Google Scholar]
- 304.Galani I, Nafplioti K, Adamou P, Karaiskos I, Giamarellou H, Souli M, Study Collaborators. 2019. Nationwide epidemiology of carbapenem resistant Klebsiella pneumoniae isolates from Greek hospitals, with regard to plazomicin and aminoglycoside resistance. BMC Infect Dis 19:167. doi: 10.1186/s12879-019-3801-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Papadimitriou-Olivgeris M, Bartzavali C, Lambropoulou A, Solomou A, Tsiata E, Anastassiou ED, Fligou F, Marangos M, Spiliopoulou I, Christofidou M. 2019. Reversal of carbapenemase-producing Klebsiella pneumoniae epidemiology from blaKPC- to blaVIM-harbouring isolates in a Greek ICU after introduction of ceftazidime/avibactam. J Antimicrob Chemother 74:2051–2054. doi: 10.1093/jac/dkz125. [DOI] [PubMed] [Google Scholar]
- 306.Nordmann P, Poirel L. 2014. The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin Microbiol Infect 20:821–830. doi: 10.1111/1469-0691.12719. [DOI] [PubMed] [Google Scholar]
- 307.Dadashi M, Yaslianifard S, Hajikhani B, Kabir K, Owlia P, Goudarzi M, Hakemivala M, Darban-Sarokhalil D. 2019. Frequency distribution, genotypes and the most prevalent sequence types of New Delhi metallo-beta-lactamase-producing Escherichia coli among clinical isolates around the world; a review. J Glob Antimicrob Resist 19:284–293. doi: 10.1016/j.jgar.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 308.Walsh TR, Weeks J, Livermore DM, Toleman MA. 2011. Dissemination of NDM-1 positive bacteria in the New Delhi environment and its implications for human health: an environmental point prevalence study. Lancet Infect Dis 11:355–362. doi: 10.1016/S1473-3099(11)70059-7. [DOI] [PubMed] [Google Scholar]
- 309.Livermore DM, Mushtaq S, Warner M, Zhang JC, Maharjan S, Doumith M, Woodford N. 2011. Activity of aminoglycosides, including ACHN-490, against carbapenem-resistant Enterobacteriaceae isolates. J Antimicrob Chemother 66:48–53. doi: 10.1093/jac/dkq408. [DOI] [PubMed] [Google Scholar]
- 310.Serio AW, Keepers T, Andrews L, Krause KM. 2018. Aminoglycoside revival: review of a historically important class of antimicrobials undergoing rejuvenation. EcoSal Plus 8:10.1128/ecosalplus.ESP-0002-2018. doi: 10.1128/ecosalplus.ESP-0002-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Bocanegra-Ibarias P, Garza-González E, Morfín-Otero R, Barrios H, Villarreal-Treviño L, Rodríguez-Noriega E, Garza-Ramos U, Petersen-Morfin S, Silva-Sanchez J. 2017. Molecular and microbiological report of a hospital outbreak of NDM-1-carrying Enterobacteriaceae in Mexico. PLoS One 12:e0179651. doi: 10.1371/journal.pone.0179651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Bosch T, Lutgens SPM, Hermans MHA, Wever PC, Schneeberger PM, Renders NHM, Leenders A, Kluytmans J, Schoffelen A, Notermans D, Witteveen S, Bathoorn E, Schouls LM. 2017. An outbreak of NDM-1 producing Klebsiella pneumoniae in a Dutch hospital with interspecies transfer of the resistance plasmid and unexpected occurrence in unrelated healthcare centers. J Clin Microbiol 55:2380–2390. doi: 10.1128/jcm.00535-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Cai J, Cheng Q, Shen Y, Gu D, Fang Y, Chan EW, Chen S. 2017. Genetic and functional characterization of blaCTX-M-199, a novel tazobactam and sulbactam resistance-encoding gene located in a conjugative mcr-1-bearing IncI2 plasmid. Antimicrob Agents Chemother 61:e00562-17. doi: 10.1128/AAC.00562-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Heinrichs A, Argudin MA, De Mendonca R, Deplano A, Roisin S, Dodemont M, Coussement J, Filippin L, Dombrecht J, De Bruyne K, Huang TD, Supply P, Byl B, Glupczynski Y, Denis O. 2019. An outpatient clinic as a potential site of transmission for an outbreak of New Delhi metallo-β-lactamase-producing Klebsiella pneumoniae sequence type 716: a study using whole-genome sequencing. Clin Infect Dis 68:993–1000. doi: 10.1093/cid/ciy581. [DOI] [PubMed] [Google Scholar]
- 315.Espinal P, Nucleo E, Caltagirone M, Mattioni Marchetti V, Fernandes MR, Biscaro V, Rigoli R, Carattoli A, Migliavacca R, Villa L. 2019. Genomics of Klebsiella pneumoniae ST16 producing NDM-1, CTX-M-15, and OXA-232. Clin Microbiol Infect 25:385.e1–385.e5. doi: 10.1016/j.cmi.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 316.Politi L, Gartzonika K, Spanakis N, Zarkotou O, Poulou A, Skoura L, Vrioni G, Tsakris A. 2019. Emergence of NDM-1-producing Klebsiella pneumoniae in Greece: evidence of a widespread clonal outbreak. J Antimicrob Chemother 74:2197–2202. doi: 10.1093/jac/dkz176. [DOI] [PubMed] [Google Scholar]
- 317.Wu W, Feng Y, Tang G, Qiao F, McNally A, Zong Z. 2019. NDM metallo-β-lactamases and their bacterial producers in health care settings. Clin Microbiol Rev 32:e00115-18. doi: 10.1128/CMR.00115-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Cantón R, Morosini MI, Martín O, de la Maza OMS, de la Pedrosa EGG. 2008. IRT and CMT β-lactamases and inhibitor resistance. Clin Microbiol Infect 14(Suppl 1):53–62. doi: 10.1111/j.1469-0691.2007.01849.x. [DOI] [PubMed] [Google Scholar]
- 319.Dubois V, Poirel L, Arpin C, Coulange L, Bebear C, Nordmann P, Quentin C. 2004. SHV-49, a novel inhibitor-resistant β-lactamase in a clinical isolate of Klebsiella pneumoniae. Antimicrob Agents Chemother 48:4466–4469. doi: 10.1128/AAC.48.11.4466-4469.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Dubois V, Poirel L, Demarthe F, Arpin C, Coulange L, Minarini LA, Bezian MC, Nordmann P, Quentin C. 2008. Molecular and biochemical characterization of SHV-56, a novel inhibitor-resistant beta-lactamase from Klebsiella pneumoniae. Antimicrob Agents Chemother 52:3792–3794. doi: 10.1128/AAC.00387-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Mendonca N, ARSIP Participants, Ferreira E, Louro D, Canica M. 2009. Molecular epidemiology and antimicrobial susceptibility of extended- and broad-spectrum beta-lactamase-producing Klebsiella pneumoniae isolated in Portugal. Int J Antimicrob Agents 34:29–37. doi: 10.1016/j.ijantimicag.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 322.Kaye KS, Gold HS, Schwaber MJ, Venkataraman L, Qi Y, De Girolami PC, Samore MH, Anderson G, Rasheed JK, Tenover FC. 2004. Variety of β-lactamases produced by amoxicillin-clavulanate-resistant Escherichia coli isolated in the northeastern United States. Antimicrob Agents Chemother 48:1520–1525. doi: 10.1128/aac.48.5.1520-1525.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Chanal CM, Sirot DL, Labia R, Petit A, Morand A, Sirot JL, Cluzel RA. 1988. Comparative study of a novel plasmid-mediated β-lactamase, CAZ-2, and the CTX-1 and CAZ-1 enzymes conferring resistance to broad spectrum cephalosporins. Antimicrob Agents Chemother 32:1660–1665. doi: 10.1128/aac.32.11.1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Bradford P, Cherubin CE, Idemyor V, Rasmussen BA, Bush K. 1994. Multiply resistant Klebsiella pneumoniae from two Chicago hospitals: identification of the extended spectrum TEM-12 and TEM-10 ceftazidime-hydrolyzing β-lactamases in a single isolate. Antimicrob Agents Chemother 38:761–766. doi: 10.1128/aac.38.4.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Moland ES, Black JA, Hossain A, Hanson ND, Thomson KS, Pottumarthy S. 2003. Discovery of CTX-M-like extended-spectrum beta-lactamases in Escherichia coli isolates from five US States. Antimicrob Agents Chemother 47:2382–2383. doi: 10.1128/aac.47.7.2382-2383.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Bush K. 2013. Carbapenemases: partners in crime. J Glob Antimicrob Resist 1:7–16. doi: 10.1016/j.jgar.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 327.Hernández-García M, Pérez-Viso B, Carmen Turrientes M, Díaz-Agero C, López-Fresneña N, Bonten M, Malhotra-Kumar S, Ruiz-Garbajosa P, Cantón R. 2018. Characterization of carbapenemase-producing Enterobacteriaceae from colonized patients in a university hospital in Madrid, Spain, during the R-GNOSIS project depicts increased clonal diversity over time with maintenance of high-risk clones. J Antimicrob Chemother 73:3039–3043. doi: 10.1093/jac/dky284. [DOI] [PubMed] [Google Scholar]
- 328.Perez-Vazquez M, Oteo-Iglesias J, Sola-Campoy PJ, Carrizo-Manzoni H, Bautista V, Lara N, Aracil B, Alhambra A, Martinez-Martinez L, Campos J, Spanish Antibiotic Resistance Surveillance Program Collaborating Group. 2019. Characterization of carbapenemase-producing Klebsiella oxytoca in Spain, 2016–2017. Antimicrob Agents Chemother 63:e02529-18. doi: 10.1128/AAC.02529-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Vannice K, Benoliel E, Kauber K, Brostrom-Smith C, Montgomery P, Kay M, Walters M, Tran M, D'Angeli M, Duchin J. 2019. Notes from the field: clinical Klebsiella pneumoniae isolate with three carbapenem resistance genes associated with urology procedures–King County, Washington, 2018. MMWR Morb Mortal Wkly Rep 68:667–668. doi: 10.15585/mmwr.mm6830a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Babini GS, Livermore DM. 2000. Are SHV beta-lactamases universal in Klebsiella pneumoniae? Antimicrob Agents Chemother 44:2230. doi: 10.1128/aac.44.8.2230-2230.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Fisher JF, Knowles JR. 1978. Bacterial resistance to β-lactams: the β-lactamases. Ann Rep Med Chem 13:239–248. [Google Scholar]
- 332.Woerther PL, Burdet C, Chachaty E, Andremont A. 2013. Trends in human fecal carriage of extended-spectrum beta-lactamases in the community: toward the globalization of CTX-M. Clin Microbiol Rev 26:744–758. doi: 10.1128/CMR.00023-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Reuland EA, Al Naiemi N, Kaiser AM, Heck M, Kluytmans JA, Savelkoul PH, Elders PJ, Vandenbroucke-Grauls CM. 2016. Prevalence and risk factors for carriage of ESBL-producing Enterobacteriaceae in Amsterdam. J Antimicrob Chemother 71:1076–1082. doi: 10.1093/jac/dkv441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Tschudin-Sutter S, Lucet JC, Mutters NT, Tacconelli E, Zahar JR, Harbarth S. 2017. Contact precautions for preventing nosocomial transmission of extended-spectrum beta lactamase-producing Escherichia coli: a point/counterpoint review. Clin Infect Dis 65:342–347. doi: 10.1093/cid/cix258. [DOI] [PubMed] [Google Scholar]
- 335.Hilty M, Betsch BY, Bögli-Stuber K, Heiniger N, Stadler M, Küffer M, Kronenberg A, Rohrer C, Aebi S, Endimiani A, Droz S, Mühlemann K. 2012. Transmission dynamics of extended-spectrum beta-lactamase-producing Enterobacteriaceae in the tertiary care hospital and the household setting. Clin Infect Dis 55:967–975. doi: 10.1093/cid/cis581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Marsh JW, Mustapha MM, Griffith MP, Evans DR, Ezeonwuka C, Pasculle AW, Shutt KA, Sundermann A, Ayres AM, Shields RK, Babiker A, Cooper VS, Van Tyne D, Harrison LH. 2019. Evolution of outbreak-causing carbapenem-resistant Klebsiella pneumoniae ST258 at a tertiary care hospital over 8 years. mBio 10:3. doi: 10.1128/mBio.01945-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Nakamura K, Kaneko M, Abe Y, Yamamoto N, Mori H, Yoshida A, Ohashi K, Miura S, Yang TT, Momoi N, Kanemitsu K. 2016. Outbreak of extended-spectrum beta-lactamase-producing Escherichia coli transmitted through breast milk sharing in a neonatal intensive care unit. J Hosp Infect 92:42–46. doi: 10.1016/j.jhin.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 338.Meyer KS, Urban C, Eagan JA, Berger BJ, Rahal JJ. 1993. Nosocomial outbreak of Klebsiella infection resistant to late-generation cephalosporins. Ann Intern Med 119:353–358. doi: 10.7326/0003-4819-119-5-199309010-00001. [DOI] [PubMed] [Google Scholar]
- 339.Urban CM, Meyer KS, Mariano N, Rahal JJ, Flamm R, Rasmussen BA, Bush K. 1994. Identification of TEM-26 ß-lactamase responsible for a major outbreak of ceftazidime resistant Klebsiella pneumoniae. Antimicrob Agents Chemother 38:392–395. doi: 10.1128/aac.38.2.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Bradford PA, Urban C, Jaiswal A, Mariano N, Rasmussen BA, Projan SJ, Rahal JJ, Bush K. 1995. SHV-7, a novel cefotaxime-hydrolyzing beta-lactamase, identified in Escherichia coli isolates from hospitalized nursing home patients. Antimicrob Agents Chemother 39:899–905. doi: 10.1128/aac.39.4.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Kopacz J, Mariano N, Colon-Urban R, Sychangco P, Wehbeh W, Segal-Maurer S, Urban C. 2013. Identification of extended-spectrum-beta-lactamase-positive Klebsiella pneumoniae urinary tract isolates harboring KPC and CTX-M beta-lactamases in nonhospitalized patients. Antimicrob Agents Chemother 57:5166–5169. doi: 10.1128/AAC.00043-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Rosenthal VD, INICC Members, Bijie H, Maki DG, Mehta Y, Apisarnthanarak A, Medeiros EA, Leblebicioglu H, Fisher D, Alvarez-Moreno C, Khader IA, Del Rocio Gonzalez Martinez M, Cuellar LE, Navoa-Ng JA, Abouqal R, Guanche Garcell H, Mitrev Z, Pirez Garcia MC, Hamdi A, Duenas L, Cancel E, Gurskis V, Rasslan O, Ahmed A, Kanj SS, Ugalde OC, Mapp T, Raka L, Yuet Meng C, Thu Le TA, Ghazal S, Gikas A, Narvaez LP, Mejia N, Hadjieva N, Gamar Elanbya MO, Guzman Siritt ME, Jayatilleke K. 2012. International Nosocomial Infection Control Consortium (INICC) report, data summary of 36 countries, for 2004–2009. Am J Infect Control 40:396–407. doi: 10.1016/j.ajic.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 343.Hong DJ, Bae IK, Jang IH, Jeong SH, Kang HK, Lee K. 2015. Epidemiology and characteristics of metallo-beta-lactamase-producing Pseudomonas aeruginosa. Infect Chemother 47:81–97. doi: 10.3947/ic.2015.47.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Schneider H, Geginat G, Hogardt M, Kramer A, Durken M, Schroten H, Tenenbaum T. 2012. Pseudomonas aeruginosa outbreak in a pediatric oncology care unit caused by an errant water jet into contaminated siphons. Pediatr Infect Dis J 31:648–650. doi: 10.1097/INF.0b013e31824d1a11. [DOI] [PubMed] [Google Scholar]
- 345.Quale J, Bratu S, Gupta J, Landman D. 2006. Interplay of efflux system, ampC, and oprD expression in carbapenem resistance of Pseudomonas aeruginosa clinical isolates. Antimicrob Agents Chemother 50:1633–1641. doi: 10.1128/AAC.50.5.1633-1641.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Farshadzadeh Z, Khosravi AD, Alavi SM, Parhizgari N, Hoveizavi H. 2014. Spread of extended-spectrum beta-lactamase genes of blaOXA-10, blaPER-1 and blaCTX-M in Pseudomonas aeruginosa strains isolated from burn patients. Burns 40:1575–1580. doi: 10.1016/j.burns.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 347.Lucena A, Dalla Costa LM, Nogueira KS, Matos AP, Gales AC, Paganini MC, Castro ME, Raboni SM. 2014. Nosocomial infections with metallo-beta-lactamase-producing Pseudomonas aeruginosa: molecular epidemiology, risk factors, clinical features and outcomes. J Hosp Infect 87:234–240. doi: 10.1016/j.jhin.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 348.Al-Charrakh AH, Al-Awadi SJ, Mohammed AS. 2016. Detection of metallo-beta-lactamase producing Pseudomonas aeruginosa isolated from public and private hospitals in Baghdad, Iraq. Acta Med Iran 54:107–113. [PubMed] [Google Scholar]
- 349.Mikucionyte G, Zamorano L, Vitkauskiene A, Lopez-Causape C, Juan C, Mulet X, Oliver A. 2016. Nosocomial dissemination of VIM-2-producing ST235 Pseudomonas aeruginosa in Lithuania. Eur J Clin Microbiol Infect Dis 35:195–200. doi: 10.1007/s10096-015-2529-0. [DOI] [PubMed] [Google Scholar]
- 350.Rankin D, Caicedo L, Dotson N, Gable P, Chu A. 2018. Notes from the field: Verona integron-encoded metallo-beta-lactamase-producing Pseudomonas aeruginosa outbreak in a long-term acute care hospital–Orange County, Florida, 2017. MMWR Morb Mortal Wkly Rep 67:611–612. doi: 10.15585/mmwr.mm6721a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Antunes LC, Visca P, Towner KJ. 2014. Acinetobacter baumannii: evolution of a global pathogen. Pathog Dis 71:292–301. doi: 10.1111/2049-632X.12125. [DOI] [PubMed] [Google Scholar]
- 352.Dijkshoorn L, Nemec A, Seifert H. 2007. An increasing threat in hospitals: multidrug-resistant Acinetobacter baumannii. Nat Rev Microbiol 5:939–951. doi: 10.1038/nrmicro1789. [DOI] [PubMed] [Google Scholar]
- 353.Lemos EV, de la Hoz FP, Einarson TR, McGhan WF, Quevedo E, Castañeda C, Kawai K. 2014. Carbapenem resistance and mortality in patients with Acinetobacter baumannii infection: systematic review and meta-analysis. Clin Microbiol Infect 20:416–423. doi: 10.1111/1469-0691.12363. [DOI] [PubMed] [Google Scholar]
- 354.Stewardson AJ, Allignol A, Beyersmann J, Graves N, Schumacher M, Meyer R, Tacconelli E, De Angelis G, Farina C, Pezzoli F, Bertrand X, Gbaguidi-Haore H, Edgeworth J, Tosas O, Martinez JA, Ayala-Blanco MP, Pan A, Zoncada A, Marwick CA, Nathwani D, Seifert H, Hos N, Hagel S, Pletz M, Harbarth S, TIMBER Study Group. 2016. The health and economic burden of bloodstream infections caused by antimicrobial-susceptible and non-susceptible Enterobacteriaceae and Staphylococcus aureus in European hospitals, 2010 and 2011: a multicentre retrospective cohort study. Euro Surveill 21:18. doi: 10.2807/1560-7917.ES.2016.21.33.30319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Rottier WC, Ammerlaan HS, Bonten MJ. 2012. Effects of confounders and intermediates on the association of bacteraemia caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae and patient outcome: a meta-analysis. J Antimicrob Chemother 67:1311–1320. doi: 10.1093/jac/dks065. [DOI] [PubMed] [Google Scholar]
- 356.Maslikowska JA, Walker SA, Elligsen M, Mittmann N, Palmay L, Daneman N, Simor A. 2016. Impact of infection with extended-spectrum beta-lactamase-producing Escherichia coli or Klebsiella species on outcome and hospitalization costs. J Hosp Infect 92:33–41. doi: 10.1016/j.jhin.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 357.Otter JA, Burgess P, Davies F, Mookerjee S, Singleton J, Gilchrist M, Parsons D, Brannigan ET, Robotham J, Holmes AH. 2017. Counting the cost of an outbreak of carbapenemase-producing Enterobacteriaceae: an economic evaluation from a hospital perspective. Clin Microbiol Infect 23:188–196. doi: 10.1016/j.cmi.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 358.Mölstad S, Löfmark S, Carlin K, Erntell M, Aspevall O, Blad L, Hanberger H, Hedin K, Hellman J, Norman C, Skoog G, Stålsby-Lundborg C, Tegmark Wisell K, Åhrén C, Cars O. 2017. Lessons learnt during 20 years of the Swedish strategic programme against antibiotic resistance. Bull World Health Organ 95:764–773. doi: 10.2471/BLT.16.184374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Aabenhus R, Hansen MP, Saust LT, Bjerrum L. 2017. Characterisation of antibiotic prescriptions for acute respiratory tract infections in Danish general practice: a retrospective registry based cohort study. NPJ Prim Care Respir Med 27:37. doi: 10.1038/s41533-017-0037-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Schwaber MJ, Carmeli Y. 2017. The impact of a carbapenem-resistant Enterobacteriaceae outbreak on facilitating development of a national infrastructure for infection control in Israel. Clin Infect Dis 65:2144–2149. doi: 10.1093/cid/cix615. [DOI] [PubMed] [Google Scholar]
- 361.Contreras DA, Fitzwater SP, Nanayakkara DD, Schaenman J, Aldrovandi GM, Garner OB, Yang S. 16 September 2019. Co-infections of two strains of NDM-1 and OXA-232 co-producing Klebsiella pneumoniae in a kidney transplant patient. Antimicrob Agents Chemother doi: 10.1128/AAC.00948-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Martinez T, Vazquez GJ, Aquino EE, Ramirez-Ronda R, Robledo IE. 2012. First report of a Pseudomonas aeruginosa clinical isolate co-harbouring KPC-2 and IMP-18 carbapenemases. Int J Antimicrob Agents 39:542–543. doi: 10.1016/j.ijantimicag.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 363.Silva KE, Cayo R, Carvalhaes CG, Patussi Correia Sacchi F, Rodrigues-Costa F, Ramos da Silva AC, Croda J, Gales AC, Simionatto S. 2015. Coproduction of KPC-2 and IMP-10 in carbapenem-resistant Serratia marcescens isolates from an outbreak in a Brazilian teaching hospital. J Clin Microbiol 53:2324–2328. doi: 10.1128/JCM.00727-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Kumarasamy K, Kalyanasundaram A. 2012. Emergence of Klebsiella pneumoniae isolate co-producing NDM-1 with KPC-2 from India. J Antimicrob Chemother 67:243–244. doi: 10.1093/jac/dkr431. [DOI] [PubMed] [Google Scholar]
- 365.Feng J, Qiu Y, Yin Z, Chen W, Yang H, Yang W, Wang J, Gao Y, Zhou D. 2015. Coexistence of a novel KPC-2-encoding MDR plasmid and an NDM-1-encoding pNDM-HN380-like plasmid in a clinical isolate of Citrobacter freundii. J Antimicrob Chemother 70:2987–2991. doi: 10.1093/jac/dkv232. [DOI] [PubMed] [Google Scholar]
- 366.Pereira PS, Borghi M, Albano RM, Lopes JC, Silveira MC, Marques EA, Oliveira JC, Asensi MD, Carvalho-Assef AP. 2015. Coproduction of NDM-1 and KPC-2 in Enterobacter hormaechei from Brazil. Microb Drug Resist 21:234–236. doi: 10.1089/mdr.2014.0171. [DOI] [PubMed] [Google Scholar]
- 367.Du H, Chen L, Chavda KD, Pandey R, Zhang H, Xie X, Tang YW, Kreiswirth BN. 2016. Genomic characterization of Enterobacter cloacae isolates from China that coproduce KPC-3 and NDM-1 carbapenemases. Antimicrob Agents Chemother 60:2519–2523. doi: 10.1128/AAC.03053-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Zhang Y, Lin X, Bush K. 2016. In vitro susceptibility of beta-lactamase-producing carbapenem-resistant Enterobacteriaceae (CRE) to eravacycline. J Antibiot (Tokyo) 69:600–604. doi: 10.1038/ja.2016.73. [DOI] [PubMed] [Google Scholar]
- 369.Sader HS, Castanheira M, Duncan LR, Flamm RK. 2018. Antimicrobial susceptibility of Enterobacteriaceae and Pseudomonas aeruginosa isolates from United States medical centers stratified by infection type: results from the International Network for Optimal Resistance Monitoring (INFORM) surveillance program, 2015–2016. Diagn Microbiol Infect Dis 92:69–74. doi: 10.1016/j.diagmicrobio.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 370.Peirano G, Matsumura Y, Adams MD, Bradford P, Motyl M, Chen L, Kreiswirth BN, Pitout J. 2018. Genomic epidemiology of global carbapenemase-producing Enterobacter spp., 2008–2014. Emerg Infect Dis 24:1010–1019. doi: 10.3201/eid2406.171648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Poulou A, Voulgari E, Vrioni G, Xidopoulos G, Pliagkos A, Chatzipantazi V, Markou F, Tsakris A. 2012. Imported KPC-producing Klebsiella pneumoniae clones in a Greek hospital: impact of infection control measures to restrain their dissemination. J Clin Microbiol 50:2618–2623. doi: 10.1128/JCM.00459-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Pournaras S, Poulou A, Voulgari E, Vrioni G, Kristo I, Tsakris A. 2010. Detection of the new metallo-β-lactamase VIM-19 along with KPC-2, CMY-2 and CTX-M-15 in Klebsiella pneumoniae. J Antimicrob Chemother 65:1604–1607. doi: 10.1093/jac/dkq190. [DOI] [PubMed] [Google Scholar]
- 373.Fortney T, Zhang Y, Campbell A, Carpenter J, Sultana R, Bush K. 2018. Microbiological response of Serratia marcescens isolates to β-lactamase inhibitor combinations in the presence of KPC and SME carbapenemases, Sunday-484. Abstr ASM Microbe 2018. American Society for Microbiology, Washington, DC. [Google Scholar]
- 374.Low YM, Yap PS, Abdul Jabar K, Ponnampalavanar S, Karunakaran R, Velayuthan R, Chong CW, Bakar S, Md Yusof MY, Teh CS. 2017. The emergence of carbapenem resistant Klebsiella pneumoniae in Malaysia: correlation between microbiological trends with host characteristics and clinical factors. Antimicrob Resist Infect Control 6:5. doi: 10.1186/s13756-016-0164-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Sader HS, Castanheira M, Mendes RE, Flamm RK. 2018. Frequency and antimicrobial susceptibility of Gram-negative bacteria isolated from patients with pneumonia hospitalized in ICUs of US medical centres (2015–17). J Antimicrob Chemother 73:3053–3059. doi: 10.1093/jac/dky279. [DOI] [PubMed] [Google Scholar]
- 376.Wang Y-C, Tang H-L, Liao Y-C, Chiou C-S, Chen Y-T, Chiang M-K, Lu M-C, Lai Y-C. 2019. Cocarriage of distinct blaKPC-2 and blaOXA-48 plasmids in a single sequence type 11 carbapenem-resistant Klebsiella pneumoniae isolate. Antimicrob Agents Chemother 63:e02282-18. doi: 10.1128/AAC.02282-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.De Geyter D, Blommaert L, Verbraeken N, Sevenois M, Huyghens L, Martini H, Covens L, Pierard D, Wybo I. 2017. The sink as a potential source of transmission of carbapenemase-producing Enterobacteriaceae in the intensive care unit. Antimicrob Resist Infect Control 6:24. doi: 10.1186/s13756-017-0182-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Dortet L, Cuzon G, Ponties V, Nordmann P. 2017. Trends in carbapenemase-producing Enterobacteriaceae, France, 2012 to 2014. Euro Surveillance 22:30461. doi: 10.2807/1560-7917.ES.2017.22.6.30461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Khajuria A, Praharaj AK, Kumar M, Grover N. 2014. Emergence of Escherichia coli, co-producing NDM-1 and OXA-48 carbapenemases, in urinary isolates, at a tertiary care centre at Central India. J Clin Diagn Res 8:DC01-4. doi: 10.7860/JCDR/2014/7952.4413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Solgi H, Badmasti F, Aminzadeh Z, Giske CG, Pourahmad M, Vaziri F, Havaei SA, Shahcheraghi F. 2017. Molecular characterization of intestinal carriage of carbapenem-resistant Enterobacteriaceae among inpatients at two Iranian university hospitals: first report of co-production of blaNDM-7 and blaOXA-48. Eur J Clin Microbiol Infect Dis 36:2127–2135. doi: 10.1007/s10096-017-3035-3. [DOI] [PubMed] [Google Scholar]
- 381.Khajuria A, Praharaj AK, Grover N, Kumar M. 2013. First report of an Enterobacter ludwigii isolate coharboring NDM-1 and OXA-48 carbapenemases. Antimicrob Agents Chemother 57:5189–5190. doi: 10.1128/AAC.00789-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Ben Nasr A, Decre D, Compain F, Genel N, Barguellil F, Arlet G. 2013. Emergence of NDM-1 in association with OXA-48 in Klebsiella pneumoniae from Tunisia. Antimicrob Agents Chemother 57:4089–4090. doi: 10.1128/AAC.00536-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Cizmeci Z, Aktas E, Otlu B, Acikgoz O, Ordekci S. 2017. Molecular characterization of carbapenem-resistant Enterobacteriaceae yields increasing rates of NDM-1 carbapenemases and colistin resistance in an OXA-48-endemic area. J Chemother 29:344–350. doi: 10.1080/1120009X.2017.1323149. [DOI] [PubMed] [Google Scholar]
- 384.Memish ZA, Assiri A, Almasri M, Roshdy H, Hathout H, Kaase M, Gatermann SG, Yezli S. 2015. Molecular characterization of carbapenemase production among Gram-negative bacteria in Saudi Arabia. Microb Drug Resist 21:307–314. doi: 10.1089/mdr.2014.0121. [DOI] [PubMed] [Google Scholar]
- 385.Zaman TU, Alrodayyan M, Albladi M, Aldrees M, Siddique MI, Aljohani S, Balkhy HH. 2018. Clonal diversity and genetic profiling of antibiotic resistance among multidrug/carbapenem-resistant Klebsiella pneumoniae isolates from a tertiary care hospital in Saudi Arabia. BMC Infect Dis 18:205. doi: 10.1186/s12879-018-3114-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Hamzaoui Z, Ocampo-Sosa A, Maamar E, Fernandez Martinez M, Ferjani S, Hammami S, Harbaoui S, Genel N, Arlet G, Saidani M, Slim A, Boutiba-Ben Boubaker I, Martinez-Martinez L. 2018. An outbreak of NDM-1-producing Klebsiella pneumoniae, associated with OmpK35 and OmpK36 porin loss in Tunisia. Microb Drug Resist 24:1137–1147. doi: 10.1089/mdr.2017.0165. [DOI] [PubMed] [Google Scholar]
- 387.Solgi H, Badmasti F, Giske CG, Aghamohammad S, Shahcheraghi F. 2018. Molecular epidemiology of NDM-1- and OXA-48-producing Klebsiella pneumoniae in an Iranian hospital: clonal dissemination of ST11 and ST893. J Antimicrob Chemother 73:1517–1524. doi: 10.1093/jac/dky081. [DOI] [PubMed] [Google Scholar]
- 388.Huang TD, Bogaerts P, Berhin C, Hoebeke M, Bauraing C, Glupczynski Y, a Multicentre Study Group. 2017. Increasing proportion of carbapenemase-producing Enterobacteriaceae and emergence of a MCR-1 producer through a multicentric study among hospital-based and private laboratories in Belgium from September to November 2015. Euro Surveill 22:30530. doi: 10.2807/1560-7917.ES.2017.22.19.30530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Samuelsen O, Naseer U, Karah N, Lindemann PC, Kanestrom A, Leegaard TM, Sundsfjord A. 2013. Identification of Enterobacteriaceae isolates with OXA-48 and coproduction of OXA-181 and NDM-1 in Norway. J Antimicrob Chemother 68:1682–1685. doi: 10.1093/jac/dkt058. [DOI] [PubMed] [Google Scholar]
- 390.Peirano G, Ahmed-Bentley J, Fuller J, Rubin JE, Pitout JD. 2014. Travel-related carbapenemase-producing Gram-negative bacteria in Alberta, Canada: the first 3 years. J Clin Microbiol 52:1575–1581. doi: 10.1128/JCM.00162-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Hall JM, Corea E, Sanjeewani HD, Inglis TJ. 2014. Molecular mechanisms of β-lactam resistance in carbapenemase-producing Klebsiella pneumoniae from Sri Lanka. J Med Microbiol 63:1087–1092. doi: 10.1099/jmm.0.076760-0. [DOI] [PubMed] [Google Scholar]
- 392.Gamal D, Fernández-Martínez M, El-Defrawy I, Ocampo-Sosa AA, Martínez-Martínez L. 2016. First identification of NDM-5 associated with OXA-181 in Escherichia coli from Egypt. Emerg Microbes Infect 5:e30. doi: 10.1038/emi.2016.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Baek JY, Cho SY, Kim SH, Kang CI, Peck KR, Song JH, Chung DR, Ko KS. 2019. Plasmid analysis of Escherichia coli isolates from South Korea co-producing NDM-5 and OXA-181 carbapenemases. Plasmid 104:102417. doi: 10.1016/j.plasmid.2019.102417. [DOI] [PubMed] [Google Scholar]
- 394.Rojas LJ, Hujer AM, Rudin SD, Wright MS, Domitrovic TN, Marshall SH, Hujer KM, Richter SS, Cober E, Perez F, Adams MD, van Duin D, Bonomo RA. 2017. NDM-5 and OXA-181 β-lactamases, a significant threat continues to spread in the Americas. Antimicrob Agents Chemother 61:e00454-17. doi: 10.1128/AAC.00454-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Hammerum AM, Littauer P, Hansen F. 2015. Detection of Klebsiella pneumoniae co-producing NDM-7 and OXA-181, Escherichia coli producing NDM-5 and Acinetobacter baumannii producing OXA-23 in a single patient. Int J Antimicrob Agents 46:597–598. doi: 10.1016/j.ijantimicag.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 396.Al-Marzooq F, Ngeow YF, Tay ST. 2015. Emergence of Klebsiella pneumoniae producing dual carbapenemases (NDM-1 and OXA-232) and 16S rRNA methylase (armA) isolated from a Malaysian patient returning from India. Int J Antimicrob Agents 45:445–446. doi: 10.1016/j.ijantimicag.2014.12.013. [DOI] [PubMed] [Google Scholar]
- 397.Lee H, Baek JY, Kim SY, Jo H, Kang K, Ko JH, Cho SY, Chung DR, Peck KR, Song JH, Ko KS. 2018. Comparison of virulence between matt and mucoid colonies of Klebsiella pneumoniae coproducing NDM-1 and OXA-232 isolated from a single patient. J Microbiol 56:665–672. doi: 10.1007/s12275-018-8130-3. [DOI] [PubMed] [Google Scholar]
- 398.Poirel L, Abdelaziz MO, Bernabeu S, Nordmann P. 2013. Occurrence of OXA-48 and VIM-1 carbapenemase-producing Enterobacteriaceae in Egypt. Int J Antimicrob Agents 41:90–91. doi: 10.1016/j.ijantimicag.2012.08.015. [DOI] [PubMed] [Google Scholar]