Abstract
OBJECTIVES:
To examine the effects of high-fiber, isocaloric, macronutrient substitutions on bloating.
METHODS:
The OmniHeart study is a randomized 3-period crossover feeding trial conducted from April 2003 to June 2005. Participants were provided 3 isocaloric versions of high-fiber (∼30 g per 2,100 kcal) diet, each different in carbohydrate, protein, and unsaturated fat composition. Each feeding period lasted for 6 weeks with a 2- to 4-week washout period between diets. Participants reported the presence and severity of bloating at baseline (participants were eating their own diet) and at the end of each feeding period.
RESULTS:
One hundred sixty-four participants were included in the analysis (mean age: 53.1 years; 45% women; 55% black). The prevalence of bloating at baseline and at the end of the carbohydrate-rich, protein-rich, and unsaturated fat-rich diet period was 18%, 24%, 33%, and 30%, respectively. Compared with baseline, the relative risk of bloating for the carbohydrate-rich, protein-rich, and unsaturated fat-rich high-fiber diet was 1.34 (95% confidence interval [CI]: 0.93, 1.92), 1.78 (95% CI: 1.32, 2.40), and 1.63 (95% CI: 1.17, 2.26), respectively. The protein-rich diet increased the risk of bloating more than the carbohydrate-rich diet (relative risk = 1.40; 95% CI: 1.03, 1.88). Bloating did not significantly vary between protein-rich vs unsaturated fat-rich or unsaturated fat-rich vs carbohydrate-rich diets. Black participants compared with non-black participants had a higher risk of bloating after all 3 versions of the high-fiber OmniHeart diet (P-value for interaction = 0.012).
DISCUSSION:
Substitution of protein with carbohydrate may be an effective strategy to decrease bloating among individuals experiencing gastrointestinal bloating from a high-fiber diet.
INTRODUCTION
Bloating, a sensation of increased abdominal pressure (1), is one of the most common gastrointestinal (GI) symptoms in the United States, with 1 in 5 people reporting having had the symptom in the past week (2). Bloating is also the hallmark symptom of irritable bowel syndrome (IBS) (3), a highly prevalent condition in the United States (4). Diet is a modifiable cause of bloating. Bacteria in the colon produce gas by breaking down and fermenting incompletely digested food (e.g., fibers) (5). In addition, dietary fiber in food may impair gas transition and promote gas retention (6).
Few population studies have examined the effects of dietary fiber on bloating. We recently found in the Dietary Approaches to Stop Hypertension (DASH)-Sodium Trial that the DASH diet—a healthy dietary plan rich in fruits, vegetables, low-fat dairy food, and fiber—may increase the risk of bloating (7). However, Jarrar et al. (8) found that supplementation with a high-fiber cereal reduced bloating in a randomized trial. These discrepant findings may be due to the differential effects of fiber supplementation vs fiber from food. Alternatively, other aspects of diet, e.g., the macronutrient composition of the diet (carbohydrate, protein, and fat), might affect the occurrence and/or severity of bloating. To our knowledge, no trial has tested the effects of macronutrient composition on the symptom of bloating in the context of high fiber intake.
In this study, we examined the effects of 3 modified versions of the DASH diet, all high in fiber, on bloating. These diets were identical in calories but had different macronutrient compositions (one high in carbohydrate, another high in protein, and a third high in unsaturated fat). We hypothesized that, consistent with our previous work (7), all 3 high-fiber diets increase the risk of bloating, but the effect is modified by the type of macronutrient. We also evaluated whether the effects differed by race, sex, age, and obese status.
METHODS
Study design and participants
Participants are from the Optimal Macronutrient Intake Trial to Prevent Heart Disease (OmniHeart), a randomized 3-period crossover feeding trial. Detailed methods and the main results have been published elsewhere (9–11). The study was conducted from April 2003 to June 2005 at 2 study centers (the Johns Hopkins Medical Institutions and Brigham and Women's Hospital). Institutional review boards at each study center and an independent data and safety monitoring board approved the protocol and monitored the trial. Each participant provided written informed consent.
The study included generally healthy participants aged 30 years or older with prehypertension or hypertension (at the time of the trial, defined by systolic blood pressure of 120–159 mm Hg or diastolic blood pressure of 80–99 mm Hg), not on antihypertensive medication, and free of diabetes or other cardiovascular diseases. We assessed the participants' eligibility and collected baseline data at screening visits when participants were eating their own diet. We also used Food Frequency Questionnaires to collect information on participants' own diet during the screening visit. All eligible participants experienced a 6-day run-in period, during which they were introduced to the feeding protocol. Individuals who were not able adhere to the feeding regimen were identified and excluded. During the run-in period, the participants ate 2 days of meals from each of the 3 study diets and were then randomly assigned to one of the 6 sequences of the 3 diets. Each feeding period lasted 6 weeks and a washout period of 2–4 weeks separated each feeding period. Participants ate their own food during the washout period.
Exposure: controlled feeding
Description of the OmniHeart diets.
We provided the participants 3 versions of the DASH diet with different macronutrient profiles: (i) a carbohydrate-rich diet (Carb diet) that provided 58% of calories as carbohydrate, 15% as protein, and 27% as fat; (ii) a protein-rich diet (Prot diet), with 10% of calories from carbohydrate replaced by protein (48% carbohydrate, 25% protein, and 27% fat); and (iii) an unsaturated fat-rich diet (Unsat diet), with 10% of calories from carbohydrate replaced by unsaturated fat (48% carbohydrate, 15% protein, and 37% fat). Table 1 shows the macronutrient targets of these diets. We will refer to these 3 diets as the OmniHeart diets.
Table 1.
Macronutrient targets the OmniHeart diets
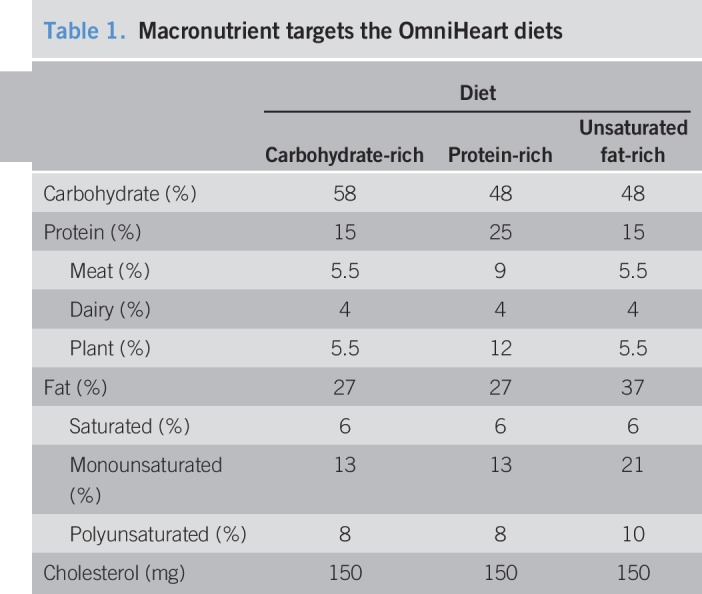
Each diet period contained different 7-day cycle menus with 5 caloric levels (1,600, 2,100, 2,600, 3,100, and 3,600 kcal). We estimated the initial caloric level at the start of the run-in period using the participant's sex, height, weight, and physical activity level. We measured participant's weight each weekday, and a dietitian adjusted caloric intake as needed to maintain the participant's weight within 2% of baseline weight. All 3 diets at each caloric level provided similar levels of dietary fiber and other nutrients—sodium, potassium, calcium, magnesium, and cholesterol. Detailed micronutrient targets, food group and subgroup servings, and sample menus have been provided in our previous publications (9,10).
Adherence to the OmniHeart diets.
We provided participants all of their food throughout the feeding periods. All food was prepared in the research kitchen in each institution with similar procedures for food production and distribution. Participants ate their main meal on-site on weekdays (Monday through Friday) and all other meals off-site. For each day of the controlled feeding periods, participants completed a diary in which they indicated whether they ate any nonstudy foods and whether they did not eat all study foods. According to these reports, adherence to the OmniHeart diets was high. All study food was consumed and no nonstudy food was eaten on 95%–96% of person-days on each diet.
Outcome: bloating symptom.
Participants completed a symptom checklist at baseline before feeding and once at the last week of each of the 3 diet periods. In the checklist, participants were asked if they felt “bloating/uncomfortably full in the past month” by rating the presence and severity as “symptom did not occur,” “mild symptom,” “moderate symptom,” or “severe symptom.” In the analysis, we dichotomized responses as “symptom did not occur” vs “symptom occurred.” We also dichotomized responses as “no to mild symptom” vs “moderate to severe symptom” in a sensitivity analysis.
Statistical analysis
We used log-binomial regression models to estimate the relative risk (RR) of bloating for each diet (compared with baseline) and between each diet. We controlled for baseline bloating symptoms when comparing the RR between each diet. We used generalized estimating equations (exchangeable correlation structure with robust variance estimates) to account for within-individual correlations. To examine potential carryover effects, we conducted a sensitivity analysis by only analyzing data from the first diet period as if it was a 3-arm parallel trial. We also conducted an analysis using the nutrient substitution analysis method (12) to assess the effect on bloating symptoms when substituting 5%, 10%, and 15% of the total kcal from one type of macronutrient for another macronutrient while keeping the third macronutrient constant.
We assessed potential effect modifications by conducting subgroup analyses stratified by the following characteristics: sex (men; women), race (black; non-black), age (<50 years old; ≥50 years old), and baseline obese status (nonobese [body mass index < 30 kg/m2]; obese [body mass index ≥ 30 kg/m2]). We included interaction terms to test for differences between the strata. We conducted a sensitivity analysis adjusted for sex (if not stratified by sex) and race (if not stratified by race) when conducting the subgroup analyses.
We considered a 2-sided P-value < 0.05 as statistically significant. We conducted all data analysis using Stata 15.1 (StataCorp, College Station, TX).
RESULTS
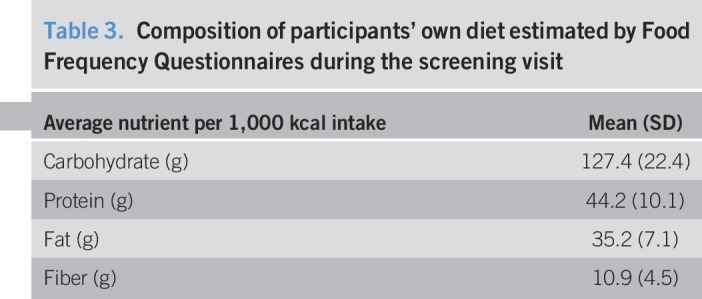
There were 164 randomized participants who completed 2 or more feeding periods and were included in the analysis (Table 2). The mean age of the participants was 53.1 years. Forty-five percent of the participants were women and 55% were black. Table 3 shows the average baseline carbohydrate, protein, fat, and fiber intake estimated by Food Frequency Questionnaire. Average baseline fiber intake was 10.9 g (SD: 4.5) per 1,000 kcal intake, 23.8% lower than the average fiber intake of ∼ 14.3 g per 1,000 kcal in the OmniHeart diets. Among all randomized participants, 162 completed the Carb diet period, 162 completed the Prot diet period, and 161 completed the Unsat diet period.
Table 2.
Baseline characteristics of the participants in the OmniHeart study
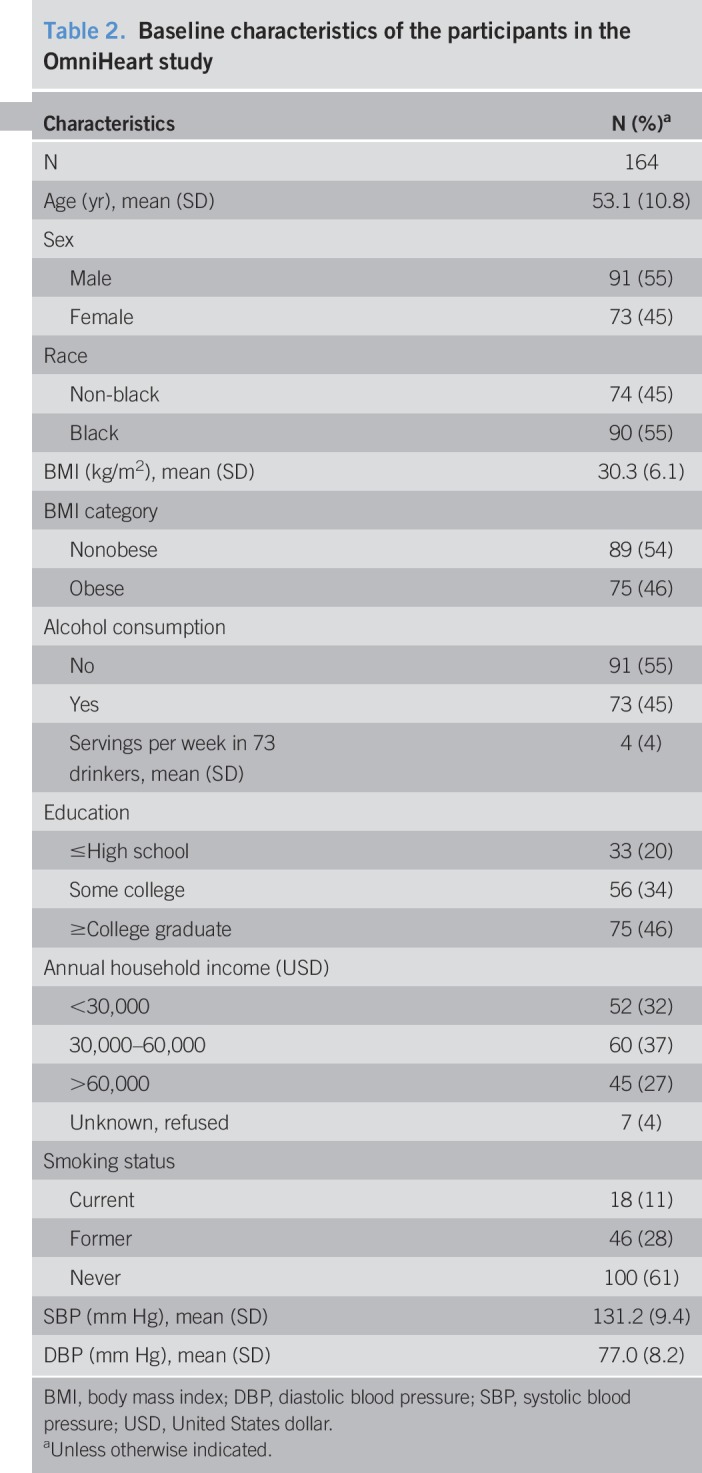
Table 3.
Composition of participants' own diet estimated by Food Frequency Questionnaires during the screening visit
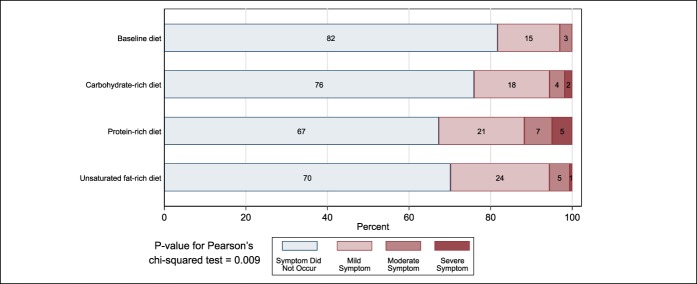
The percent of participants with no bloating, mild, moderate, and severe bloating differed by diets (P-value = 0.009) (Figure 1). At baseline and at the end of the Carb, Prot, and Unsat diet period, 30 (18%), 39 (24%), 53 (33%), and 48 (30%) participants reported bloating symptoms, respectively. Five (3%) participants had moderate to severe bloating symptoms at baseline, and 9 (6%), 19 (12%), and 9 (6%) had moderate to severe bloating at the end of the Carb, Prot, and Unsat diet periods, respectively.
Figure 1.
Percent of participants with no bloating, mild, moderate, and severe bloating at baseline and by diet.
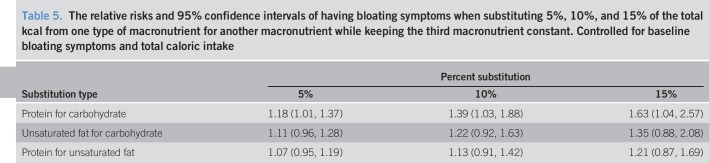
Compared with baseline, both the Prot diet (RR = 1.78; 95% confidence interval [CI]: 1.32, 2.40) and the Unsat diet (RR = 1.63; 95% CI: 1.17, 2.26) significantly increased the risk of bloating. The Carb diet did not significantly increase the risk of bloating (RR = 1.34; 95% CI: 0.93, 1.92). When comparing between diets, the Prot diet resulted in a higher risk of bloating than the Carb diet (RR = 1.40; 95% CI: 1.03, 1.88). However, bloating did not significantly vary between Prot vs Unsat or Unsat vs Carb diets (Table 4). Results were consistent using a nutrient substitution analysis (Table 5): substituting protein for carbohydrate resulted in the highest increase in bloating. Results were also consistent when we limited to the first diet period (see Supplemental Table 1, Supplementary Digital Content 1, http://links.lww.com/CTG/A162), and the bloating effect of the Prot diet compared with the other OmniHeart diets was stronger when we dichotomized responses as “no to mild symptom” vs “moderate to severe symptom” (Supplemental Table 1, Supplementary Digital Content 1, http://links.lww.com/CTG/A162).
Table 4.
The RRs and 95% CIs of having bloating symptoms for each diet compared with baseline and between each diet
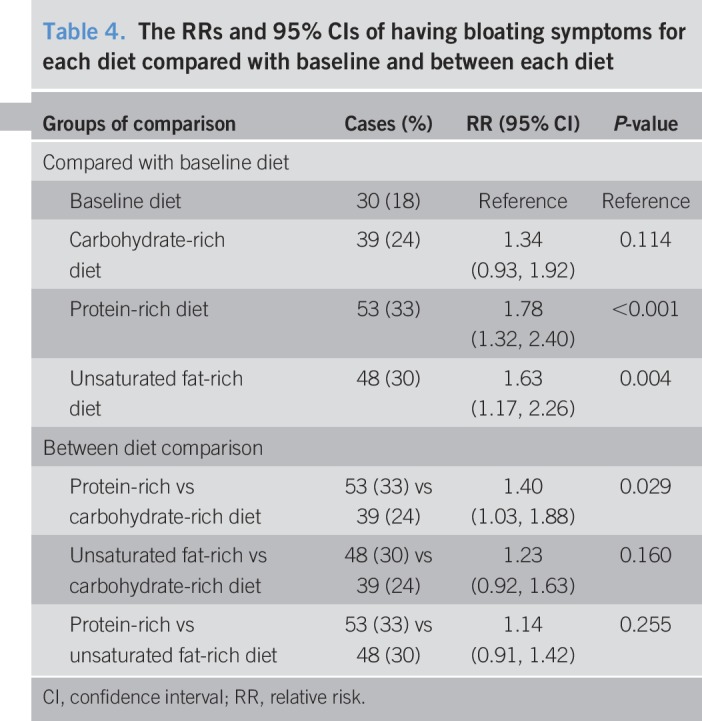
Table 5.
The relative risks and 95% confidence intervals of having bloating symptoms when substituting 5%, 10%, and 15% of the total kcal from one type of macronutrient for another macronutrient while keeping the third macronutrient constant. Controlled for baseline bloating symptoms and total caloric intake
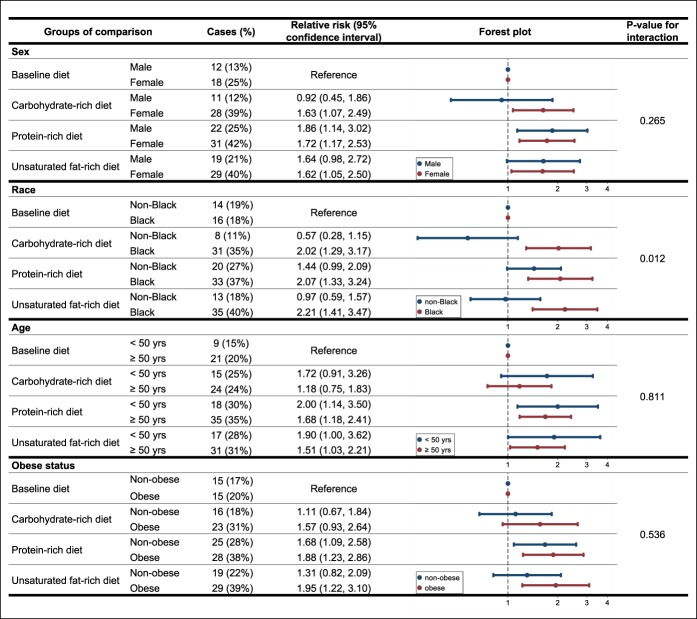
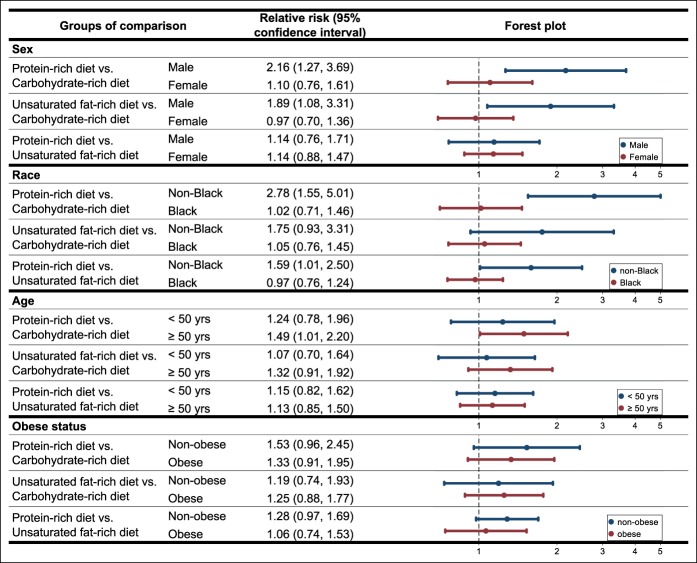
In the subgroup analyses, compared with baseline, all subgroups had a higher risk of bloating after the Prot diet; most subgroups had a higher risk of bloating after the Carb or the Unsat diet (Figure 2). The effect of each diet on bloating compared with baseline did not differ by sex, age, or obese status. Black participants, however, had significantly higher risk of bloating than non-black participants after all 3 versions of the high-fiber OmniHeart diet (P-value for interaction = 0.012). The between-diet effects on bloating varied by subgroups (Figure 3): non-black participants had stronger differences in bloating between all 3 diets and male participants had stronger differences in bloating between Prot vs Carb and Unsaturated Fat vs Carb diets. The effect of each diet on bloating compared with baseline (see Supplemental Table 2, Supplementary Digital Content 2, http://links.lww.com/CTG/A163) and the between-diet effects on bloating (see Supplemental Table 3, Supplementary Digital Content 3, http://links.lww.com/CTG/A164) did not markedly change when we adjusted for sex and race in the subgroup analyses.
Figure 2.
The relative risks and 95% confidence intervals of having bloating symptoms for each diet compared with baseline by sex, race, age, and obese status.
Figure 3.
The relative risks and 95% confidence intervals of having bloating symptoms between each diet by sex, race, age, and obese status.
DISCUSSION
In this 3-period crossover feeding trial, we found that switching from a low-fiber typical US diet to a higher fiber OmniHeart diet increased the occurrence of bloating. The protein-rich version of the OmniHeart diet increased the risk of bloating significantly more than the carbohydrate-rich version of the diet. Black participants were more likely than non-blacks to have bloating symptoms after switching from their baseline diet to each of the 3 higher-fiber OmniHeart diets.
Our finding that switching from a low-fiber to a high-fiber diet, irrespective of the macronutrient content, increases bloating and is consistent with several lines of evidence that dietary fiber can markedly affect the GI function (1). Dietary fiber is partially or totally fermented in the distal small bowel and colon, which leads to the production of a number of gases including carbon dioxide, hydrogen, and methane (13,14). Dietary fiber may also impair gas transition and promote gas retention by decreasing bolus propulsion to the rectum (6). Our recent study in 412 participants in the controlled-feeding DASH-Sodium Trial observed a 41% increase in the risk of bloating from a high-fiber (∼32 g per 2,100 kcal) DASH diet vs a low-fiber (∼11 g per 2,100 kcal) control diet over a 12-week period (7). By contrast, Jarrar el al. (8) found in a recent randomized controlled trial in the United Arab Emirates that the intervention group with 90 g/d high fiber cereal consumption (∼11 g fiber per 90 g cereal) had reduced bloating frequency compared with the control group with habitual diet after 20 days. This study, however, was not a controlled-feeding study. The supplemented fibers from cereals were largely insoluble (15) and low in gas production (13). Unlike OmniHeart diets, there were no supplemented fibers from fruits, beans, or seeds, the fiber of which are more soluble and fermentable, and thus higher in gas production (13,15).
To our knowledge, no studies have examined the effect of increasing dietary protein intake on bloating. Yancy et al. (16) found that a 26% protein diet compared with a 19% protein diet increased the risk of GI symptoms including constipation and diarrhea. However, the percent of carbohydrate and fat also differed between the 2 diets, and thus, it is unclear whether the differences in GI symptoms are entirely because of protein. The relatively higher risk of bloating after switching to the protein-rich diet vs the other high-fiber OmniHeart diets might not be due to protein per se, but rather the differential distribution of soluble and fermentable fibers in our version of the protein-rich diet. Although all OmniHeart diets were matched on fiber, the protein-rich OmniHeart diet emphasized plant protein, i.e., beans, legumes, nuts, seeds, wheat, and soy products in lieu of animal protein. Many of these food elements are rich sources of oligosaccharides, a soluble and highly fermentable fiber that is high in gas production (13). Legumes also contains many other soluble and fermentable fibers including resistant starch, pectin, guar gum, and inulin, which are moderate in gas production (13). To make the amount of fiber the same across all 3 diets, we also reduced some high-fiber grains in the protein-rich OmniHeart diet that are typically less soluble and fermentable and low in gas production.
We unexpectedly found that participants who self-reported as black vs non-black were more likely to have bloating symptoms after switching from baseline diet to all 3 versions of the high-fiber OmniHeart diet. One potential explanation may be that the contrast in fiber intake between participants' baseline diet and high-fiber OmniHeart diet was greater for blacks than for non-blacks in our study. This theory is supported by the data from the 2015–2016 National Health and Nutrition Examination Survey, from which non-Hispanic blacks, on average, have lower fiber intake (13.7 g/d) than other groups (non-Hispanic white: 16.5 g/d; non-Hispanic Asian: 18.6 g/d; and Hispanic: 17.5 g/d) (17). Another hypothesis is that blacks have a different GI response to the same diet patterns than non-blacks. Previous studies have explored and found marked differences in the gut microbiome composition between blacks and whites (18) and also in GI response to the same diet between blacks and African natives (19).
Our study has a number of strengths. First, this is the first study that tested the effects of macronutrient composition on bloating symptoms using data from a randomized trial. This was also a crossover trial in which each participant served as his or her own control, which minimized potential confounding. Second, adherence to the diets and completion of data collection in each diet period was high, thereby minimizing the potential biases due to attrition and missing data. Third, the macronutrients in each of the 3 diets are precisely calculated and highly controlled, which allowed us to make comparisons between diets and draw inferences on the effect of macronutrients on bloating. Fourth, the wash-out period is long (2–4 weeks, compared with the 6-week diet period) and the symptom questionnaire was administered at the end of each diet period. This minimized the potential carryover effect of the previous diet, which was also supported by our sensitivity analysis.
Our study has limitations. First, we did not have detailed information on the presence and absence of IBS and were not able to examine if IBS modified the associations of macronutrients and bloating. Second, despite the high diversity of our study population (>50% black), we lacked ethnicity breakdown for non-black participants. Third, the symptom of bloating was self-reported only at baseline and once at the end of each diet period, thus misclassification of the outcome cannot be ruled out. We were also not able to assess the weekly change in bloating symptoms. Fourth, we were not able to control for and did not measure the composition of soluble vs insoluble fibers or animal vs plant-based protein in each of the 3 diets, which may have contributed to the between diet differences in bloating. Other unmeasured food elements may also have contributed to the differences.
Switching from a low-fiber typical US diet to a higher fiber diet increased occurrence of bloating. However, the increase in bloating was attenuated by substituting high-fiber sources of protein with high-fiber sources of carbohydrate. Future research is needed to replicate and better understand our finding that blacks experienced more bloating on high-fiber diets than non-blacks. In conclusion, substitution of protein with carbohydrate may be an effective strategy to decrease bloating among individuals experiencing GI bloating from a high-fiber diet.
CONFLICTS OF INTEREST
Guarantor of the article: Noel T. Mueller, PhD, MPH.
Specific author contributions: M.Z.: conception and design of the manuscript, analysis and interpretation of the data, drafting the manuscript, and revision of the manuscript. S.P.J.: conception and design of the manuscript, interpretation of the data, and revision of the manuscript. L.J.A.: conception and design of the manuscript, acquisition and interpretation of the data, and revision of the manuscript. P.J.P.: interpretation of the data and revision of the manuscript. E.R.M.: interpretation of the data and revision of the manuscript. N.T.M.: conception and design of the manuscript, outlining of the manuscript, interpretation of the data, and revision of the manuscript. All authors have approved the final draft submitted.
Financial support: Funding for the OmniHeart study was provided through grant R01HL67098 from the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH/NHLBI). N.T.M. is supported by the NIH/NHLBI under award number K01HL141589. S.P.J. is supported by the NIH/NHLBI under award number K23HL135273. L.J.A. is supported by the Mid-Atlantic Nutrition Obesity Research Center (NORC) by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (NIH/NIDDK) under award number P30DK072488.
Potential competing interests: None to report.
Trial registration: ClinicalTrials.gov Identifier: NCT00051350.
Study Highlights.
WHAT IS KNOWN
✓ Bloating is one of the most common GI symptoms and the hallmark of IBS.
✓ Dietary fiber may increase bloating by promoting gas production.
✓ Evidence from population studies on the effects of high-fiber diets on bloating has been limited, and no trials have specifically examined if macronutrient composition modifies the effects a high-fiber diet intake on bloating.
WHAT IS NEW HERE
✓ The symptom of bloating increased when participants switched from their habitual diet to the 3 high-fiber dietary patterns, each with a different macronutrient composition.
✓ A high-fiber diet enriched in protein (mostly plant-based) increased bloating more than a high-fiber diet enriched in carbohydrate.
✓ Bloating did not significantly differ between the protein-rich and unsaturated fat-rich diets, and between the unsaturated fat-rich and carbohydrate-rich diets.
✓ The effect of the higher-fiber diets on of bloating was greater in black participants than in non-black participants, raising the possibility that GI responses to diet may be race-specific.
TRANSLATIONAL IMPACT
✓ Among individuals experiencing GI discomfort from a high-fiber diet, substitution of protein with carbohydrate may be an effective strategy to decrease GI discomfort.
Supplementary Material
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at http://links.lww.com/CTG/A162, http://links.lww.com/CTG/A163, and http://links.lww.com/CTG/A164
REFERENCES
- 1.Malagelada JR, Accarino A, Azpiroz F. Bloating and abdominal distension: Old misconceptions and current knowledge. Am J Gastroenterol 2017;112(8):1221–31. [DOI] [PubMed] [Google Scholar]
- 2.Almario CV, Ballal ML, Chey WD, et al. Burden of gastrointestinal symptoms in the United States: Results of a nationally representative survey of over 71,000 Americans. Am J Gastroenterol 2018;113(11):1701–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ringel Y, Williams RE, Kalilani L, et al. Prevalence, characteristics, and impact of bloating symptoms in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 2009;7(1):68–72. [DOI] [PubMed] [Google Scholar]
- 4.Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol 2014;6:71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lacy BE, Gabbard SL, Crowell MD. Pathophysiology, evaluation, and treatment of bloating: Hope, hype, or hot air? Gastroenterol Hepatol 2011;7(11):729–39. [PMC free article] [PubMed] [Google Scholar]
- 6.Gonlachanvit S, Coleski R, Owyang C, et al. Inhibitory actions of a high fibre diet on intestinal gas transit in healthy volunteers. Gut 2004;53(11):1577–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peng AW, Juraschek SP, Appel LJ, et al. Effects of the DASH diet and sodium intake on bloating: Results from the DASH-sodium trial. Am J Gastroenterol 2019;114:1109–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jarrar AH, Beasley JM, Ohuma EO, et al. Effect of high fiber cereal intake on satiety and gastrointestinal symptoms during Ramadan. Nutrients 2019;11(4):939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swain JF, McCarron PB, Hamilton EF, et al. Characteristics of the diet patterns tested in the optimal macronutrient intake trial to prevent heart disease (OmniHeart): Options for a heart-healthy diet. J Am Diet Assoc 2008;108(2):257–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Appel LJ, Sacks FM, Carey VJ, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum LipidsResults of the OmniHeart randomized trial. J Am Med Assoc 2005;294(19):2455–64. [DOI] [PubMed] [Google Scholar]
- 11.Carey VJ, Bishop L, Charleston J, et al. Rationale and design of the optimal macro-nutrient intake heart trial to prevent heart disease (OMNI-Heart). Clin Trials 2005;2(6):529–37. [DOI] [PubMed] [Google Scholar]
- 12.Færch K, Lau C, Tetens I, et al. A statistical approach based on substitution of macronutrients provides additional information to models analyzing single dietary factors in relation to type 2 diabetes in Danish adults: The Inter99 study. J Nutr 2005;135(5):1177–82. [DOI] [PubMed] [Google Scholar]
- 13.Eswaran S, Muir J, Chey WD. Fiber and functional gastrointestinal disorders. Am J Gastroenterol 2013;108(5):718–27. [DOI] [PubMed] [Google Scholar]
- 14.Marthinsen D, Fleming SE. Excretion of breath and flatus gases by humans consuming high-fiber diets. J Nutr 1982;112(6):1133–43. [DOI] [PubMed] [Google Scholar]
- 15.Howarth NC, Saltzman E, Roberts SB. Dietary fiber and weight regulation. Nutr Rev 2001;59(5):129–39. [DOI] [PubMed] [Google Scholar]
- 16.Yancy WS, Jr, Olsen MK, Guyton JR, et al. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: A randomized, controlled trial. Ann Intern Med 2004;140(10):769–77. [DOI] [PubMed] [Google Scholar]
- 17.U.S. Department of Agriculture, Agricultural Research Service. Nutrient intakes from food and beverages: Mean amounts consumed per individual, by race/ethnicity and age, what we eat in America, NHANES 2015-2016 (https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/1516/Table_2_NIN_RAC_15.pdf). Published 2018. Accessed April 30, 2019.
- 18.Farhana L, Antaki F, Murshed F, et al. Gut microbiome profiling and colorectal cancer in African Americans and Caucasian Americans. World J Gastrointest Pathophysiol 2018;9(2):47–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Keefe SJD, Li JV, Lahti L, et al. Fat, fibre and cancer risk in African Americans and rural Africans. Nat Commun 2015;6:6342. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.