Abstract
Background and Purpose:
An excess incidence of strokes among blacks vs whites has been shown, but data on disparities related to Hispanic ethnicity remains limited. This study examines race/ethnic differences in stroke incidence in the multi-ethnic, largely Caribbean Hispanic, Northern Manhattan Study (NOMAS), and whether disparities vary by age.
Methods:
The study population included participants in the prospective population-based NOMAS, followed for a mean of 14±7 years. Multivariable-adjusted Cox proportional hazards models were constructed to estimate the association between race/ethnicity and incident stroke of any subtype and ischemic stroke, stratified by age.
Results:
Among 3,298 participants (mean baseline age 69±10 years, 37% men, 24% black, 21% white, 52% Hispanic), 460 incident strokes accrued (400 ischemic, 43 ICH, 9 SAH). The most common ischemic subtype was cardioembolic, followed by lacunar infarcts, then cryptogenic. The greatest incidence rate was observed in blacks (13/1000 person-years), followed by Hispanics (10/1000 PY), and lowest in whites (9/1000 PY), and this order was observed for crude incidence rates until age 75. By age 85 the greatest incidence rate was in Hispanics. Blacks had an increased risk of stroke vs whites overall in multivariable models that included sociodemographics (HR=1.51, 95% CI=1.13–2.02), and stratified analyses showed that this disparirity was driven by women age ≥70. The increased rate of stroke among Hispanics (age/sex-adjusted HR=1.48, 1.13–1.93) was largely explained by education and insurance status (a proxy for socieoeconomic status; HR after further adjusting for these variables=1.17, 0.85–1.62), but remained significant for women age ≥70.
Conclusions:
This study provides novel data regarding the increased stroke risk among Caribbean Hispanics in this elderly population. Results highlight the need to create culturally-tailored campaigns to reach black and Hispanic populations to reduce race/ethnic stroke disparities, and support the important role of low socioeconomic status in driving an elevated risk among Caribbean Hispanics.
Keywords: Stroke, Race, Hispanic ethnicity, Epidemiology, Disparities
Subject terms: Race and ethnicity, Ischemic stroke, Epidemiology
Stroke mortality in the US has consistently been greater among blacks compared to whites. Data from our prior population-based case surveillance study in Northern Manhattan showed that blacks had a 2.4-fold and Hispanics a 2.0-fold increased incidence of stroke compared to whites living in the same urban community, a novel finding that suggested explanation for the similar disparities observed in stroke mortality rates1. Data from prospective cohort studies also suggest that the increased stroke incidence among blacks varies by age, with the strongest disparity observed in middle age2,3. Though the evidence is strong that the excess incidence of stroke among blacks is largely responsible for their increased stroke mortality, data for Hispanics remains relatively sparse and most data on stroke risk among Hispanics in the US comes from Mexican Americans. Mexican Americans have been shown to have an increased incidence of stroke compared to non-Hispanic whites, and this disparity also appears to be strongest during middle age and decline with age4,5. However, these findings may not generalize to other Hispanic subgroups, as the prevalence of vascular risk factors is known to vary across Hispanic subgroups, with Dominicans having a greater cardiovascular disease burden compared to other Hispanic subgroups such as Mexican Americans6.
The goal of the current study is to examine race/ethnic differences in stroke incidence in the diverse, yet largely Caribbean Hispanic, prospective population-based Northern Manhattan Study (NOMAS). The NOMAS cohort study, born out of a previous case-control study and initiated 26 years ago, now has a mean follow-up of 14 years, allowing for an analysis of racial and ethnic differences in stroke incidence overall and across stroke subtypes among this unique elderly population all residing in the same urban community.
Materials and Methods
Study Population
The study population was comprised of participants in NOMAS, which is an ongoing prospective cohort study with the original goal of determining the incidence of and risk factors for stroke in a multi-ethnic urban population. As previously detailed7,8, participants were recruited between 1993–2001 with the following eligibility criteria: 1) age 40 or older; 2) clinically stroke free; 3) resident of Northern Manhattan for at least 3 months. Participants were selected using random-digit dialing (91% telephone response rate), and enrolled following an in-person baseline interview and assessment (75% enrollment response rate), with a final enrollment of 3,298 participants. The study was approved by the institutional review boards at Columbia University Medical Center and the University of Miami. All participants provided written informed consent. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Baseline Risk Factors
The baseline enrollment included a comprehensive assessment of vascular risk factors by self-report with interviews in English or Spanish as well as a physical examination by study physicians. Race-ethnicity was self-identified based on a questionnaire adapted from the 2000 U.S census and classified into four categories (white non-Hispanic; black non-Hispanic; Hispanic; non-Hispanic other race). Our Hispanics were predominately Caribbean Hispanics (61% Dominican, 14% Puerto Rican, 12% Cuban, 13% other). Standardized questions adapted from the Behavioral Risk Factor Surveillance System by the Centers for Disease Control were used to identify medical history, medication use, and health behaviors including hypertension, diabetes, cigarette smoking, alcohol intake and cardiac comorbidities. Smoking was categorized as current (within the past year), former, or never smoker of cigarettes, cigars or pipes. Classifications of moderate alcohol use, moderate to heavy physical activity, hypertension, diabetes mellitus, hypercholesterolemia, and body mass index (BMI) have been detailed previously9–11. Moderate alcohol use was defined as current drinking of more than one drink per month but less than three drinks per day. Moderate to heavy physical activity level was defined as participation in any of the selected rigorous physical activities during a typical 14-day period. Blood pressure was recorded as the average of two measurements taken before and after the examination. Fasting blood specimens were collected to measure blood glucose and lipid levels, analyzed at the Core Laboratory of the Irving Center for Clinical Research. Hypertension was defined as a blood pressure ≥140/90 mmHg, patient self-reported history of hypertension, or the use of anti-hypertensive medication. Diabetes mellitus was defined as a fasting glucose ≥126 mg/dl, patient self-reported history of diabetes, or the use of insulin or oral anti-diabetic medication. Hypercholesterolemia was defined as having a total cholesterol level of greater than 200 mg/dl, patient self-reported history of hypercholesterolemia, or use of cholesterol lowering medications. Height and weight were measured to determine BMI (as kg/m2).
Stroke Outcomes
Participants have been screened annually by telephone for new neurological symptoms and events/diagnoses, hospitalizations, or death. Suspected vascular events were followed with an in-person assessment by study physicians. The primary outcomes of interest were confirmed incident cases of any stroke type (infarcts, intracerebral hemorrhage, and subarachnoid hemorrhage). The secondary outcomes of interest were ischemic stroke subtypes, classified as lacunar infarct, extracranial atherosclerotic infarct, intracranial atherosclerotic infarct, cardioembolic infarct, and cryptogenic infarct/conflicting mechanisms. The follow-up procedures, outcomes classifications, and diagnostic criteria for each ischemic stroke subtype have been detailed previously7,8. Morbidity and mortality data were enhanced through local hospital surveillance of admission and discharge data, including ICD-9 codes. Cause of death was determined through correspondence with the participant’s family, review of medical records, and when available, a copy of the death certificate. A panel of NOMAS neurologists blinded to patient characteristics classified each case, with consensus reached by discussion, and adjudicated by the principal investigators as needed after review of all data.
Statistical analysis
A series of multivariable-adjusted Cox proportional hazards models were constructed to estimate hazard ratios and 95% confidence intervals (HR, 95% CI) for the relation between race/ethnicity with all stroke and ischemic stroke. The time scale was the interval from baseline to stroke, death, or the last recorded follow-up (through April, 2019), whichever occurred first. Complete loss to followup was <1% and unrelated to race/ethnicity. Proportional hazards assumptions were confirmed before running the Cox models. Model 1 was adjusted for age at baseline, and sex. Model 2 also included proxies for socioeconomic status including high school completion and medical insurance status. Model 3 additionally adjusted for smoking, moderate to heavy physical activity, moderate alcohol consumption, BMI, hypertension, diabetes, and hypercholesterolemia. These analyses were repeated stratifying by sex and age less than 70 and 70 or older at baseline, which was the mean baseline age among stroke cases. Analyses stratified by age at baseline and sex were determined a priori and not based on statistical tests of interaction as these were underpowered. All analyses were conducted using SAS version 9.4 (SAS institute).
Results
Among 3,298 NOMAS participants, 460 incident strokes accrued over a mean follow-up time of 13.6±6.7 years. Of these 460 strokes, 400 were confirmed ischemic, 43 ICH, and 9 SAH. The mean age at baseline was 69±10 years, 37% were men, 24% black, 21% white, 52% Hispanic, and 3% other race. Table 1 describes the vascular risk factor profile of the study population at NOMAS baseline, overall and stratified by race/ethnicity.
Table 1.
Characteristics of the Northern Manhattan Study baseline cohort overall and by race and ethnicity
| Variable | Study population (N=3298) | White (N=690) | Black (N=803) | Hispanic (N=1728) |
|---|---|---|---|---|
| Age at baseline: mean (SD) | 69 (10) | 74 (10) | 72 (10) | 66 (9) |
| BMI: mean (SD) | 28 (6) | 26 (5) | 28 (6) | 28 (5) |
| Male: N (%) | 1227 (37) | 284 (41) | 263 (33) | 645 (37) |
| Highschool completion: N (%) | 1511 (46) | 566 (82) | 506 (63) | 384 (22) |
| Medicaid/no insurance: N (%) | 1436 (44) | 76 (11) | 202 (25) | 1138 (66) |
| Current | 560 (17) | 91 (13) | 180 (22) | 276 (16) |
| Moderate alcohol use: N (%) | 1083 (33) | 293 (42) | 256 (32) | 510 (30) |
| Moderate-heavy physical activity: N (%) | 282 (9) | 96 (14) | 72 (9) | 103 (6) |
| Hypertension: N (%) | 2430 (74) | 450 (65) | 638 (79) | 1297 (75) |
| Diabetes: N (%) | 715 (22) | 100 (14) | 196 (24) | 407 (24) |
| Hypercholesterolemia: N (%) | 2050 (62) | 465 (67) | 465 (58) | 1082 (63) |
The overall crude stroke incidence rate was 13/1000 person-years (PY) in blacks, 10/1000 PY in Hispanics, and 9/1000 PY in whites. The crude incidence rates of all stroke in each race/ethnic group, stratified by baseline age are shown in Figure 1. The greatest incidence rate was observed in blacks, followed by Hispanics, and lowest in whites, and this order was observed for the crude incidence rates until age 75. By age 85 the greatest incidence rate was observed for Hispanics.
Figure 1.
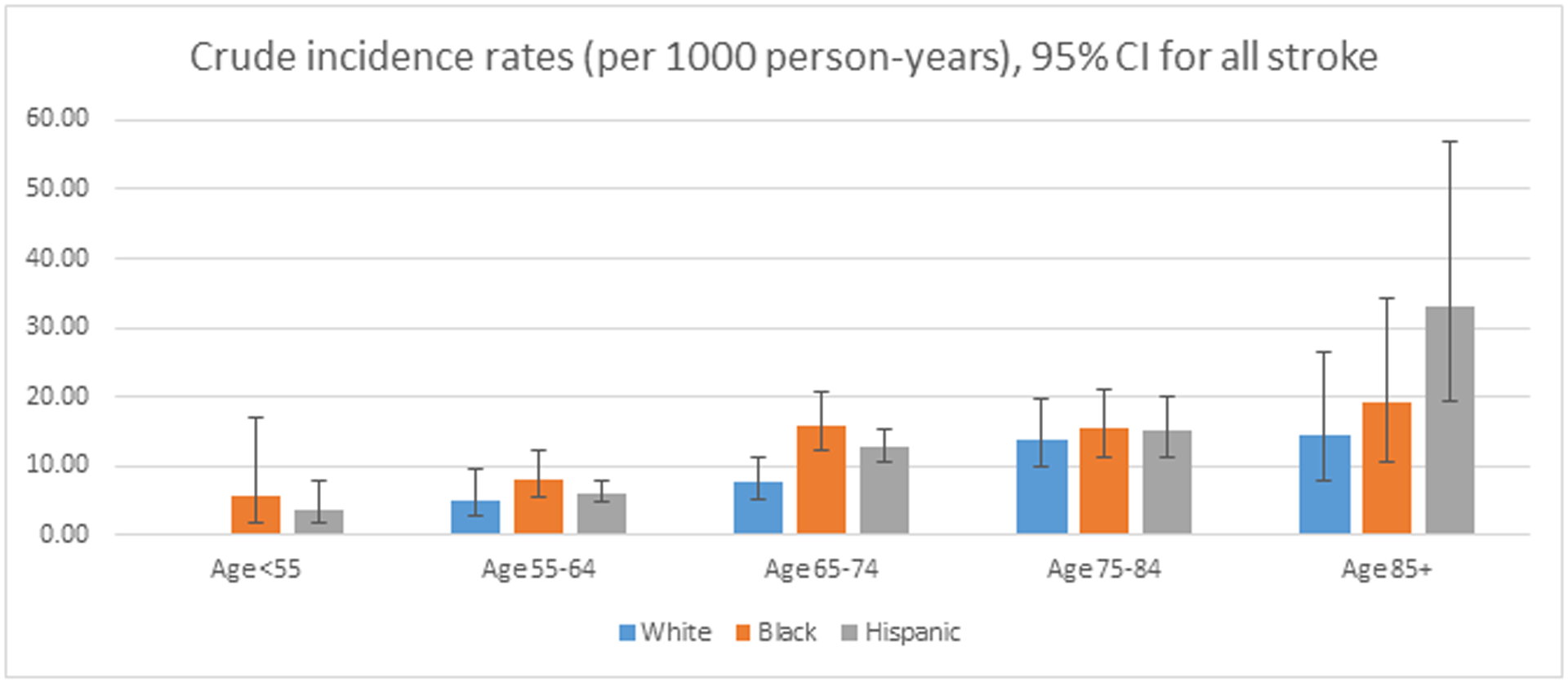
Crude stroke incidence rates by race/ethnicity, stratified by age category (with 95% confidence interval).
Among Hispanic participants, 61% were descended from the Dominican Republic (DR, mean baseline age=65±9), 14% from Puerto Rico (PR, mean baseline age=68±9), and 12% from Cuba (mean baseline age=72±10). The crude stroke IR was highest among those from Cuba (14/1000 PY, p=0.02 vs DR), followed by PR (10/1000 PY, p=0.53 vs DR), and DR (9/1000 PY). However, after adjusting for age and sex, there were no differences in the stroke incidence rate across Hispanic subgroups.
Figure 2 shows the age- and sex-adjusted incidence rates across the ischemic stroke subtypes in race-ethnic strata. The most common ischemic stroke subtype was cardioembolic, followed by lacunar infarcts, and then cryptogenic. The rate of cryptogenic infarcts exceeded lacunar infarcts only among whites.
Figure 2.
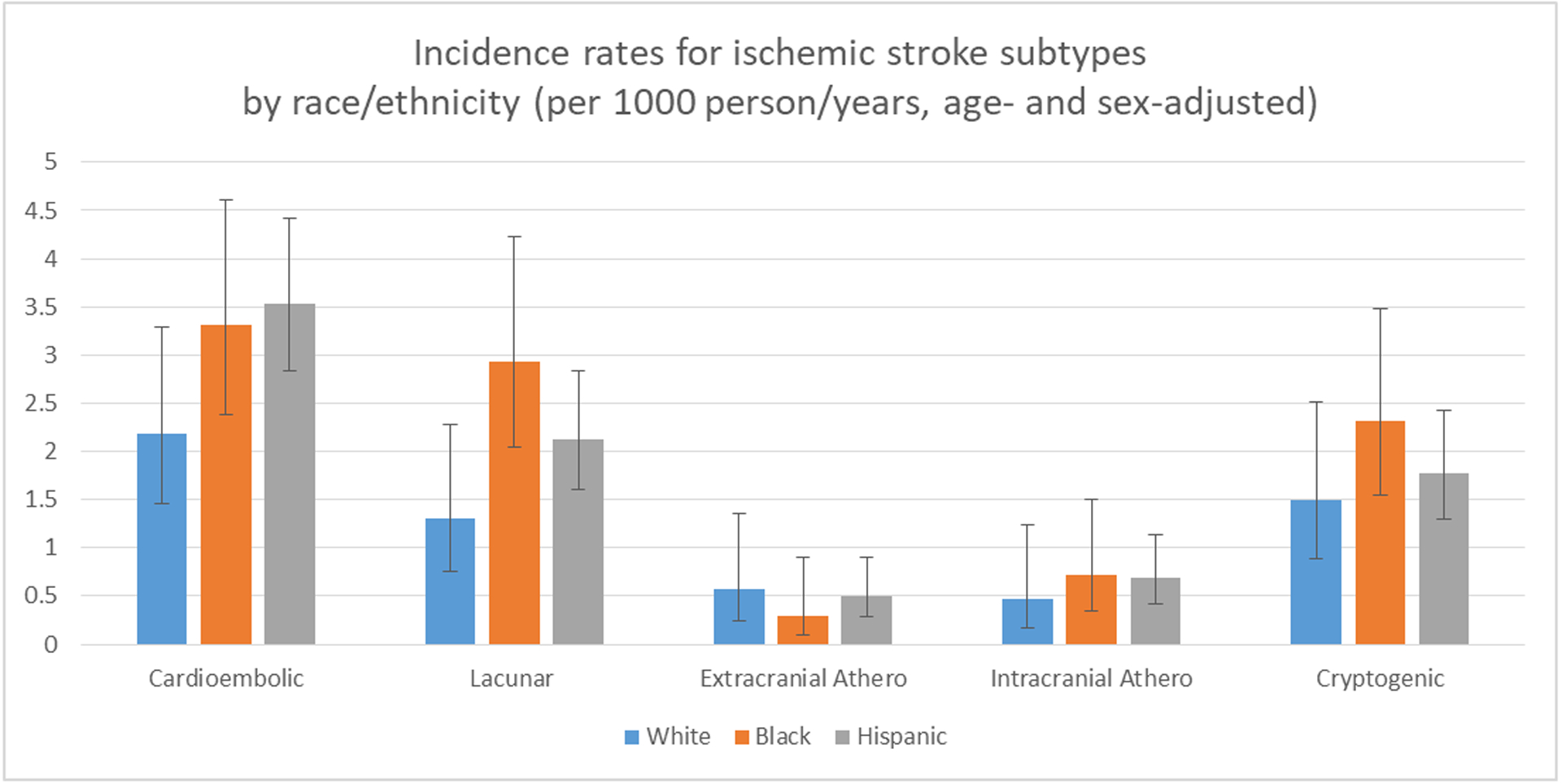
Age- and sex-adjusted incidence rates for each ischemic stroke subtype by race/ethnicity (with 95% confidence interval).
Table 2 shows the adjusted hazard ratios for all stroke, and Supplemental Table I for ischemic stroke, among blacks and Hispanics compared to whites in the series of multivariable adjusted models. Adjusting for age and sex in model 1, blacks and Hispanics had increased rates of stroke compared to whites, including ischemic stroke specifically. The effect estimates for blacks attenuated with further adjustment for proxy measures of SES and vascular risk factors, but remained significant in model 2 and was no longer significant in model 3. In contrast, the hazard ratios for Hispanics vs whites were substantially attenuated after adjustment for the proxy SES variables (education and insurance status) and were no longer significant in models 2 and 3.
Table 2.
Race and ethnic disparities in overall stroke incidence in NOMAS
| All Stroke HR (95% CI) | Black vs white | Hispanic vs white | |||
|---|---|---|---|---|---|
| All | Model 1 | 1.621 | (1.219, 2.155) | 1.478 | (1.132, 1.929) |
| Model 2 | 1.509 | (1.127, 2.020) | 1.173 | (0.850, 1.618) | |
| Model 3 | 1.329 | (0.988, 1.789) | 1.075 | (0.776, 1.489) | |
| <70 men | Model 1 | 1.479 | (0.750, 2.914) | 1.166 | (0.650, 2.093) |
| Model 2 | 1.346 | (0.676, 2.678) | 0.797 | (0.391, 1.627) | |
| Model 3 | 1.138 | (0.568, 2.278) | 0.701 | (0.343, 1.434) | |
| <70 women | Model 1 | 2.080 | (1.012, 4.273) | 1.424 | (0.729, 2.780) |
| Model 2 | 1.762 | (0.845, 3.672) | 0.893 | (0.409, 1.949) | |
| Model 3 | 1.468 | (0.683, 3.152) | 0.778 | (0.348, 1.742) | |
| 70+ men | Model 1 | 1.264 | (0.707, 2.257) | 1.303 | (0.768, 2.210) |
| Model 2 | 1.090 | (0.593, 2.005) | 1.097 | (0.573, 2.102) | |
| Model 3 | 1.008 | (0.539, 1.885) | 1.047 | (0.538, 2.038) | |
| 70+ women | Model 1 | 1.740 | (1.104, 2.741) | 1.922 | (1.245, 2.968) |
| Model 2 | 1.758 | (1.103, 2.802) | 1.766 | (1.042, 2.993) | |
| Model 3 | 1.550 | (0.961, 2.501) | 1.612 | (0.943, 2.757) | |
Model 1: age, sex
Model 2: age, sex, highschool completion, insurance status
Model 3: age, sex, highschool completion, insurance status, smoking, physical activity, alcohol consumption, BMI, hypertension, diabetes, hypercholesterolemia
The disparity in stroke risk, and ischemic stroke in particular, observed among blacks vs whites was bigger in women. Adjusting for age and sex only, the disparity for blacks was large and significant in women of both age strata, though statistical significance was only achieved among women age 70 and older after adjustment for education and insurance. The difference between blacks and whites in stroke risk did not reach statistical significance among men in either age strata. Age- and sex-stratified analyses revealed that the stroke disparity for Hispanics was strongest among women age 70 and older, where it remained robust even after adjusting for education and insurance. Further adjustment for vascular risk factors slightly attenuated the association for Hispanics vs whites among older women and it lost statistical significance (p=0.08 for all stroke).
Race/ethnic disparities were not observed for ICH stroke subtype specifically, though the power with only 43 cases was minimal (Supplemental Table II).
Discussion
The results of the current study are consistent with previous studies that have shown an increased risk of stroke among blacks in the United States. In fact, the increased stroke incidence in blacks vs whites has been demonstrated repeatedly across many study populations12,13, including the Greater Cincinnati/Northern Kentucky Stroke Study3 and in the REasons for Geographic and Racial Differences in Stroke (REGARDS) national cohort study2. Data from these two cohort studies also suggest that the increased stroke incidence among blacks varies by age, with the strongest disparity observed in middle age. The risk of stroke in blacks under age 65 has been estimated to be up to three-fold higher than that in whites of similar age, but this disparity has previously been shown to diminish significantly with increasing age, with overall relative risks in the 1.5–2.5 range2,12. In the REGARDS cohort, blacks age 45–54 had a four-fold increased incidence of stroke compared to whites, but there was no disparity observed among those age 85 and older2. Overall, in models that account only for age and sex, the disparity observed for blacks does appear to decrease with advancing age in NOMAS. However, sex-stratified analyses suggested that the race disparity was pronounced and significant in women specifically, and that among women the disparity does not in fact decrease with age. The current study provides novel evidence for a strong and persistent disparity in stroke risk for blacks vs. whites among elderly women. The absence of a reduced race disparity with age observed among women underscores the importance of examining sex differences in trends over age. It is also important to note that the current study population is elderly, and previously observed trends in slightly younger populations may not exist in this older population at a higher stroke risk.
Ethnic disparities in stroke risk are less well understood, and those of Hispanic ethnicity in the United States represent a heterogeneous population in terms of origin and vascular risk profile. In our primarily Caribbean Hispanic population we found an increased risk of stroke for Hispanics vs non-Hispanic whites that was largely explained by SES proxies, education level and insurance status. The elevated risk of stroke among Hispanics was also strongest among women, and particularly elderly women. Among women age 70 and over there was a nearly two-fold increased risk of stroke among Hispanics vs whites, a finding that remained strong and significant after adjusting for education and insurance status. Therefore, as mentioned above, the current study provides novel insight into the important, persistent and increasing disparities in stroke risk in elderly minorities, specifically among women, and shows that race/ethnic disparities are not just evident in the young as suggested in previous studies.
Evidence regarding disparities in stroke incidence among Hispanics living in the United States remains limited and was the primary goal of NOMAS. Data from the Brain Attack Surveillance in Corpus Christi study showed that stroke incidence was higher among Mexicans than non-Hispanic whites in southeast Texas, and that this disparity decreased with increasing age. An increased incidence of ischemic stroke was observed among Mexicans vs whites among those age 45–59 and 60–74, but not along those over age 7514. Another analysis in the Health and Retirement Study (HERS) found that US-born Hispanics were at elevated risk of stroke compared to non-Hispanic whites, but that after adjusting for demographic and socioeconomic factors, the difference was attenuated15. The HERS study had a different study design and a smaller number of Hispanics, predominantly of Mexican descent. In 1998 NOMAS investigators reported that blacks had a 2.4-fold increased incidence of stroke compared to whites and Hispanics a two-fold increased incidence compared to whites, in the population-based surveillance study that gave rise to the Northern Manhattan Study cohort1. It has now been over 25 years since the NOMAS cohort began recruitment, allowing for a more refined and well-controlled analysis of these racial and ethnic disparities in stroke incidence in the unique, older, primarily Caribbean Hispanic, urban, low SES population. The overall conclusions remain consistent, with blacks and Hispanics having an increased incidence of stroke compared to non-Hispanic whites in northern Manhattan, though the hazard ratios after adjusting for age and sex were not as strong as those observed in the original study. At that time it was hypothesized that SES and education differences might account for a portion of the observed disparities, a finding confirmed in the current analysis, particularly among those in the younger age category at baseline (<70 years). The substantial increased incidence of stroke observed in subsets of the black and Hispanic population in NOMAS supports the importance of culturally-tailored stroke education and prevention campaigns aimed at these minority populations.
An increased incidence of stroke among blacks and Hispanics is largely explained by the increased burden of vascular disease risk factors. The final multivariable models included behavioral risk factors such as physical activity, smoking, and alcohol consumption, as well as important traditional stroke risk factors including BMI, diabetes, hypertension, and hypercholesterolemia, and in these models the effect estimates were attenuated, resulting in a loss of statistical significance. These observations confirm our understanding that these vascular risk factors are important explanatory factors in the observed race/ethnic disparities and aggressively addressing these risk factors could reduce race-ethnic disparities in stroke risk. In the NOMAS cohort, race/ethnic differences in vascular risk profile have been observed in the current study as well as numerous others10,16. Complete data on stroke risk factor trajectories over the course of follow-up was not available, and race/ethnic differences in these trajectories over time may help explain observed stroke disparities. In addition, other less traditional vascular disease risk factors (e.g. inflammation, diet, psychosocial factors, lifestyle behaviors) may also account for some of the observed disparity and require further investigation. The importance of examining ethnic differences in stroke incidence in this largely Caribbean population is highlighted by previous findings that suggest that Dominicans have more vascular disease risk factors compared to other Hispanic populations in the US, including Mexican Americans, who have been better represented in other studies6.
Our study also provides novel data on the variability in incidence of ischemic stroke subtypes across strata defined race/ethnicity with up to 25 years of follow-up. Race and ethnic incidence data on ischemic stroke subtypes is very limited. In the current study, cardioembolic stroke was the most common subtype of ischemic stroke among all race/ethnic groups. In our prior stroke surveillance study in northern Manhattan cryptogenic strokes were most common, with cardioembolic strokes the second most frequent in whites, while in blacks and Hispanics the frequency of lacunar stroke was slightly but not significantly higher7. Recently the proportion of patients diagnosed with cardioembolic stroke due to discovery of occult paroxysmal atrial fibrillation has increased, but this was not true throughout the duration of NOMAS, which began recruitment in 1993. In blacks, atherosclerotic subtypes also summed to be nearly as common as cardioembolic. Though the previous study suggested that the increased incidence of ischemic stroke in blacks and Hispanics vs whites may be present across all ischemic stroke subtypes, the results of the current study do not clearly support this disparity, particularly for extracranial atherosclerotic stroke. However, the current study is underpowered to reliably estimate the relative disparities between race/ethnic groups across the ischemic stroke subtypes.
Strengths of this study include the long follow-up with limited attrition in a well-defined population-based cohort, confirmed and adjudicated data on ischemic stroke subtypes, and measured vascular risk factors at study baseline. An additional strength is the mutually exclusive stratified analyses by sex and age, though the statistical power within strata was limited. An important strength is the examination of a multi-ethnic population living in the same urban community, and one with a majority of participants of Caribbean Hispanic descent, a growing population that has traditionally been underrepresented in epidemiological research. However, our findings may not generalize to other populations with different compositions, particularly in relation to SES and vascular risk factors, as ours was a notably low SES and generally high vascular risk elderly population. An important limitation is that the current study lacked sufficient power to detect significant race/ethnic disparities in stroke risk over multiple strata at the low range of clinical relevance, and therefore the importance of future analyses in other large multiethnic prospective cohorts is underscored. Similarly, it lacked sufficient power to reliably estimate race/ethnic disparities in ischemic stroke subtypes and hemorrhagic stroke subtypes, particularly by age category. As mentioned, we used medical insurance status and high school completion as imperfect proxy measures of SES. We dichotomized education in this manner in our multivariable models after careful examination of its relationship with both race/ethnicity and stroke risk in our cohort (not shown).
In conclusion, this study provides unique evidence of race and ethnic disparities in stroke risk, and the role of advancing age in modifying these disparities. Most importantly, we showed an increased risk of stroke among Hispanics of Caribbean descent compared to non-Hispanic whites, consistent with evidence from other Hispanic populations of Mexican descent. Our results highlight the persistent disparities in stroke risk among elderly minorities. Future studies are needed in larger cohorts to further elucidate the three way interactions between race and ethnicity, sex, and age in determining stroke risk, which can inform stroke prevention efforts and public policy recommendations regarding community risk factor management.
Supplementary Material
Acknowledgements
Funding: This study was supported by National Institutes of Health/National Institute of Neurological Disorders and Stroke (R01 NS 29993). Support was also provided from the National Center for Advancing Translational Sciences, Clinical Translational Science Institute (UL1TR000460).
Footnotes
Disclosures: Hannah Gardener, Ralph L Sacco, and Tatjana Rundek receive funding from the Florida Department of Health for the Florida Stroke Registry. Ralph L Sacco receives funding support from Boehringer Ingelheim for the RESPECT-ESUS trial.
References
- 1.Sacco RL, Boden-Albala B, Gan R, Chen X, Kargman DE, Shea S, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am J Epidemiol. 1998;147:259–68. [DOI] [PubMed] [Google Scholar]
- 2.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69:619–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kissela B, Schneider A, Kleindorfer D, Khoury J, Miller R, Alwell K, et al. Stroke in a biracial population: the excess burden of stroke among blacks. Stroke. 2004;35:426–31. [DOI] [PubMed] [Google Scholar]
- 4.Morgenstern LB, Smith MA, Lisabeth LD, Risser JM, Uchino K, Garcia N, et al. Excess stroke in Mexican Americans compared with non-Hispanic Whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004;160:376–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgenstern LB, Smith MA, Sánchez BN, Brown DL, Zahuranec DB, Garcia N, et al. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. Ann Neurol. 2013;74:778–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daviglus ML, Talavera GA, Avilés-Santa ML, Allison M, Cai J, Criqui MH, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wright CB, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111:1327–31. [DOI] [PubMed] [Google Scholar]
- 8.Sacco RL, Anand K, Lee HS, Boden-Albala B, Stabler S, Allen R, et al. Homocysteine and the risk of ischemic stroke in a triethnic cohort: the NOrthern MAnhattan Study. Stroke. 2004;35:2263–9. [DOI] [PubMed] [Google Scholar]
- 9.Boden-Albala B, Cammack S, Chong J, Wang C, Wright C, Rundek T, et al. Diabetes, fasting glucose levels, and risk of ischemic stroke and vascular events: findings from the Northern Manhattan Study (NOMAS). Diabetes Care 2008;31:1132–1137. [DOI] [PubMed] [Google Scholar]
- 10.Willey JZ, Paik MC, Sacco R, Elkind MS, Boden-Albala B. Social determinants of physical inactivity in the Northern Manhattan Study (NOMAS). J Community Health 2010;35:602–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monteith TS, Gardener H, Rundek T, Elkind MS, Sacco RL. Migraine and risk of stroke in older adults: Northern Manhattan Study. Neurology. 2015;85:715–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30:736–43. [DOI] [PubMed] [Google Scholar]
- 13.Appelros P, Stegmayr B, Terént A. Sex differences in stroke epidemiology: a systematic review. Stroke. 2009;40:1082–90 [DOI] [PubMed] [Google Scholar]
- 14.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moon JR, Capistrant BD, Kawachi I, Avendaño M, Subramanian SV, Bates LM, et al. Stroke incidence in older US Hispanics: is foreign birth protective? Stroke. 2012;43:1224–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: the northern Manhattan study. Circulation. 2012;125:2975–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


