Abstract
This study reported cumulative 6-day (lag 0–5 days) relative risks (RR) and confidence intervals (CI) of daily outpatient visits for total respiratory disease (RD), asthma, and chronic airway obstruction not otherwise classified (CAO) associated with three ozone metrics (daily 1-h maximum (O3, 1 h max), 8-h average maximum (O3, 8 h max), 24-h average (O3, 24 h avg)), and an alternative oxidant indicator (Ox) in Taipei Metropolitan, using distributed lag non-linear models after controlling for potential confounders. The Ox showed the strongest association with outpatient visits for total RD (RR = 1.10, 95% CI: 1.10, 1.11) and asthma (RR = 1.18, 95% CI: 1.00, 1.39) in the cold season. The O3, 24 h avg appeared to be the optimal ozone metric associating with total RD than O3, 1 h max and O3, 8 h max based on model selection. In conclusion, outpatient visits for total RD associated with ozone vary with ozone metrics, disease and season.
Keywords: Ozone, Respiratory disease, Asthma, Chronic airway obstruction, Outpatient visit
Highlights
► The health risk of ozone varied by RD type and by the ozone metrics applied. ► O3, 24 h avg was a better metric to associate with outpatient visits of total RD. ► Ox most correlated with outpatient visits for total RD in the cold season.
The O3, 24 h avg was a better metric than O3, 1 h max and O3, 8 h max to associate with outpatient visits of total respiratory diseases.
1. Introduction
Tropospheric ozone (O3) is a common air pollutant in urban areas, with concentrations vary the most among ambient pollutants (Darrow et al., 2011). Meteorological factors (e.g., ambient temperature, wind speed and sunlight), geographical factors, and co-pollutants (e.g., nitrogen oxides and volatile organic compounds) affect the formation, concentration and spatial distribution of ozone (Hsu, 2007; Lin et al., 2010). Studies have shown that ambient ozone not only induces airway inflammation and decreases lung function but also associated with elevated mortality from and morbidity of respiratory disorders (Bell et al., 2004; Gryparis et al., 2004; Schwela, 2000).
Strong sunlight accelerates the photochemical reactions that cause ozone formation, raising concerns of adverse effects on mortality and morbidity in summers in the US and European (Gryparis et al., 2004; Lin et al., 2008; Samoli et al., 2009; Zanobetti and Schwartz, 2008). Pattenden et al. (2010) reported the synergistic health effects of high temperature and ozone levels in the summer season (Pattenden et al., 2010). But, some studies indicated that the effects of ozone are greater in cold weather than in hot weather (Linn et al., 2000; Wong et al., 1999).
Additionally, risk estimates vary by studied area and ozone metrics applied in ozone-related health studies (Bell and Dominici, 2008; Bell et al., 2004; Gryparis et al., 2004; Ji et al., 2011; Yang et al., 2012; Zanobetti and Schwartz, 2008). Three common ozone metrics have been used in regulatory (USEPA, 2012) and epidemiological studies (Bell and Dominici, 2008; Bell et al., 2004), i.e., daily 1-h maximum (O3, 1 h max), daily 8-h average maximum (O3, 8 h max), and daily 24-h average (O3, 24 h avg), representing different exposure time frames for health risk assessment. Concentration of ozone and the daily peak time of ozone formation are affected by traffic-related emissions; especially nitrogen oxides (NOx) emissions are considered a major precursor during ozone formation under strong sunlight. Therefore, total oxidant (Ox), which includes ozone and nitrogen dioxide (NO2), is a suggested alternative indictor of the health effects of ozone (Chou et al., 2006). Moreover, flux-based exposure metrics and exceedance of standard have also been used as ozone exposure indicators and to estimate the risk of ozone exposure for human health, plants and vegetation in Europe (Karlsson et al., 2007; Lin et al., 2008; Musselman et al., 2006). Although many different ozone indicators have been used, no gold standard or criteria for selecting ozone metrics have been established, especially for health risk studies.
Increasing ozone concentrations have tended to cause moderate to high oxidant episodes in the Taipei Metropolitan in the past two decades (Chang and Lee, 2008). Therefore, this study assessed the associations between three metrics (O3, 1 h max, O3, 8 h max, O3, 24 h avg) and an alternative oxidant indicator (Ox) and outpatient visits for total and cause-specific respiratory diseases (RD) of a population-based cohort in the subtropical climate of Taipei Metropolitan.
2. Methods
This study analyzed the data of Taipei Metropolitan from 2000 to 2009. Locating in the basin of northern Taiwan, Taipei Metropolitan (Taipei City and New Taipei City) is the economic and political center of Taiwan. Its population exceeds 6 million, which comprises near one-fourth of the total Taiwan population (Ministry of the Interior, 2006). Although the Mass Rapid Transit system provides over one million daily transportations for over 20 years, traffic emissions remain the major air pollution source.
2.1. Outpatient visits for total and case-specific respiratory disease
Electronic records for daily outpatient visits were obtained from the National Health Insurance (NHI) program, which covered 90.0% of the Taiwan population in 1995 and increased to 96.2% in 2000 (Bureau of National Health Insurance, 2001). We retrieved from the claims data patients' scrambled identification numbers, sex, date of birth, diagnoses, dates of admission and discharge, and information on hospitals and clinics. Of all those insured in 2000, one million people were randomly selected as a cohort by the National Health Research Institute, Taiwan. This cohort enrolled about 318,000 people residing in Taipei Metropolitan in 2000. Their records of outpatient visits for total RD (The 9th revision of International Classification of Diseases with clinical modification, ICD9 CM 460–519), asthma (ICD9 CM 493), and chronic airway obstruction not elsewhere classified (CAO) (ICD9 CM 496) were retrieved for further analyses.
2.2. Air pollution and meteorological characteristics
The Taiwan Environmental Protection Administration (TEPA) has operated 74 monitoring stations distributed throughout Taiwan since 1993. Of these, 13 stations are in Taipei for monitoring the general ambient air pollution (Fig. 1 ). These stations measure and record hourly particulate matter <10 μm in aerodynamic diameter (PM10), nitric oxide (NO), NO2 and O3 concentrations. The hourly pollutants records were used to calculate 24 h (daily) concentrations of PM10, NO and NO2 for the present study period.
Fig. 1.
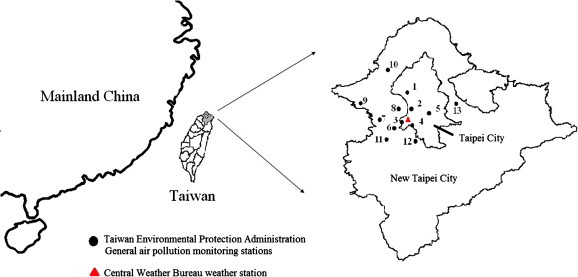
Ambient air monitoring stations and weather station in Taipei Metropolitan.
We used ozone metrics (O3, 1 h max, O3, 8 h max and O3, 24 h avg) and one total oxidant indicator (Ox) to represent ozone exposure during different exposure time frames. Briefly, the O3, 1 h max was calculated as the average maximum hourly ozone concentration in the study area. The O3, 8 h max was the daily average of the maximum 8-h moving average. The daily 24-h average value was calculated by averaging 24 hourly measurements. Finally, the total oxidant was an alternative metric, including daily 24-h ozone and daily 24-h NO2 concentrations. We used Ox to measure the combined effect of ozone and NO2 because NO rapidly forms NO2 by reacting with ozone (Chou et al., 2006). All ozone metrics were obtained by averaging the 13 monitoring values to obtain an overall daily representative ozone exposure in Taipei. Pollutants with missing data of longer than 6 h were not used for that day. The quality assurance and control were performed and operated by TEPA (Taiwan Environmental Protection Administration, 2011). The Central Weather Bureau provided 24-h data from 25 real-time weather monitoring stations in Taiwan (Taiwan Central Weather Bureau, 2013). Hourly weather measurements (average, maximum, and minimum temperatures, relative humility, dew point temperature, water vapor pressure, and wind speed) were recorded at five weather stations in Taipei Metropolitan. Daily weather measurements from the Taipei weather station located in the city center were used because they were considered representative of the ambient temperature exposures of the local population. Meteorological data for daily average temperature, relative humidity (RH) and wind speed (WS) were also retrieved.
2.3. Statistical analysis
This study applied Poisson regression models with dlnm (Gasparrini et al., 2010; Goldberg et al., 2011) to assess risk in four different ozone metrics associated with outpatient visits for total RD, asthma and CAO. Non-linear and delayed effects of ozone metrics and temperature were analyzed by natural cubic spline (NS) DLNM. The knots of variables were placed at equally spaced quantiles of the predictor. The knots of lag were set at equally spaced values on the log scale of lags.
Sensitivity analyses were performed to evaluate the covariates and their df in the model. We compared the risk estimates and model fittings for various combinations of relative humidity (NS, df set from 4 to 6), wind speed (NS, df set from 4 to 6), long-term time trend (NS, df set at 4, 7, and 14), cross-basis of ozone concentrations (NS, df set from 4 to 5), and cross-basis of average temperature (NS, df set from 4 to 6). The minimum Akaike information criterion was used for model selection (Akaike, 1973).
The model for expected number of cause-specific outpatient visits (Y) at day (t) was
Measurements of ozone metrics (Ozonei,t, in which i = 1–4 represented O3, 1 h max, O3, 8 h max, O3, 24 h avg, and Ox) were set at NS with 3 degrees of freedom (df) under 3 df lag space in models. Cumulative 6-day (from current day to maximum lag of 5 days) relative risks (RR) and 95% confidence intervals (CIs) of total RD, asthma and CAO were estimated by comparing ozone metrics for concentrations at the 75th (Q3) percentiles with that at the 25th (Q1) percentiles (Cheng et al., 2009). APj,t represented the linear effect of air pollutants (j = 1–2 for PM10 and NO2) on day t. Daily average temperature (T t) was set at NS with 6 df (approximately 4 °C for 1 df), and effects were accounted for 8 cumulative days (lag 0–7 days) with 3 df spline for lag. The model also controlled for the confounding effects of RH and WS using natural cubic spline with 5 df for daily measurements.
Moreover, the calendar year was treated as an additional categorical variable in models to control for annual variation in health outcomes (e.g., the sudden decrease in outpatient visits caused by the severe acute respiratory syndrome epidemic in 2003). The smoother term of time (“time” in the model) was set to 14 df per year. Other covariates, such as cumulative 15-day (from current day to maximum lag of 14 days) effect of outpatient visits for pneumonia and influenza (Flu, ICD9 CM codes 480–487), holidays, and day of the week (DOW) were also adjusted in the models. The relationships between outpatient visits of total and cause-specific respiratory diseases and three ozone metrics and Ox were determined for three time periods: the hot season (May–October), the cold season (November–April), and the entire year.
All data manipulations and statistical analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) and statistical environment R 2.12 (dlnm package).
3. Results
3.1. Ambient pollutants and weather characteristics
Table 1 shows the features of PM10, NO2, ozone metrics, temperature, RH, WS and daily outpatient visits for total RD, asthma and CAO in Metro Taipei from 2000 to 2009. Correlation coefficients for ozone metrics were 0.89 between O3, 1 h max and O3, 8 h max, 0.49 between O3, 1 h max and O3, 24 h avg, and 0.75 between O3, 8 h max and O3, 24 h avg. Supplementary Fig. S1 shows levels of O3, 1 h max and O3, 8 h max were higher in the hot season than in the cold season. However, O3, 24 h avg and Ox concentrations showed a bimodal annual distribution, and the average concentrations in hot and cold seasons were similar.
Table 1.
Characteristic of air pollutants, climate condition and daily outpatient visit for total respiratory disease, asthma and chronic airway obstruction not elsewhere classified (CAO) in Taipei Metropolitan during 2000–2009.
| Covariates | Minimum | 25% | 50% | 75% | Maximum | Mean |
|---|---|---|---|---|---|---|
| PM10 (μg/m3) | 10.7 | 31.4 | 43.6 | 60.1 | 286 | 48.4 |
| NO2 (ppb) | 3.90 | 23.1 | 30.1 | 39.5 | 119 | 33.0 |
| O3, max (ppb) | 9.65 | 36.8 | 46.8 | 65.2 | 143 | 52.9 |
| O3, 8 h (ppb) | 6.95 | 29.5 | 38.3 | 49.7 | 107 | 40.6 |
| O3, 24 h (ppb) | 4.53 | 19.0 | 24.9 | 31.2 | 73.1 | 25.5 |
| Ox (ppb) | 8.88 | 42.1 | 48.5 | 55.7 | 91.6 | 48.8 |
| Temperature (°C) | 8.30 | 19.3 | 23.9 | 28.0 | 33.0 | 23.4 |
| Relative humidity (%) | 37.0 | 69.0 | 75.0 | 83.0 | 98.0 | 75.7 |
| Wind speed (m/sec) | 0 | 1.60 | 2.40 | 3.60 | 7.90 | 2.61 |
| Daily hospital admissions | ||||||
| Respiratory diseases | 50 | 1750 | 2398 | 3096 | 6769 | 2443 |
| Asthma | 0 | 1 | 2 | 7 | 26 | 4 |
| Chronic airway obstruction not elsewhere classified | 0 | 7 | 16 | 22 | 51 | 15 |
| Pneumonia and influenza | 0 | 10 | 16 | 23 | 91 | 17 |
Fig. 2 shows the proportion of O3, 1 h max appearing in a day by hour. O3 levels were the highest from 8 AM to 6 PM in most of days. During the cold season, however, O3, 1 h max tended to peak at 0–7 AM.
Fig. 2.
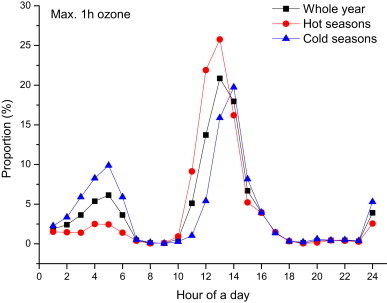
Proportion of 1-h maximum ozone (O3, 1 h max) occurred in a day by study periods, 2000–2009.
3.2. Cumulative relative risk of outpatient visits for respiratory disease
Fig. 3 shows the associations between ambient ozone levels and outpatient visits for total RD by ozone metric and study period. During hot seasons, outpatient visits for total RD were significantly and positively associated with O3, 24 h avg above 30 ppb and with Ox above 40 ppb. During cold seasons, on the other hand, the risk was also statistically significant in associations with O3, 1 h max above 40 ppb, O3, 8 h max above 30 ppb, and Ox above 45 ppb. The O3, 24 h avg had a significant positive association with outpatient visits for total RD in cold seasons; however, this study, as we observed the effects of ozone levels at 75th percentiles, obtained a lower risk estimate for O3, 24 h avg than other ozone metrics on associating with outpatient visits of total RD (Table 2 ).
Fig. 3.
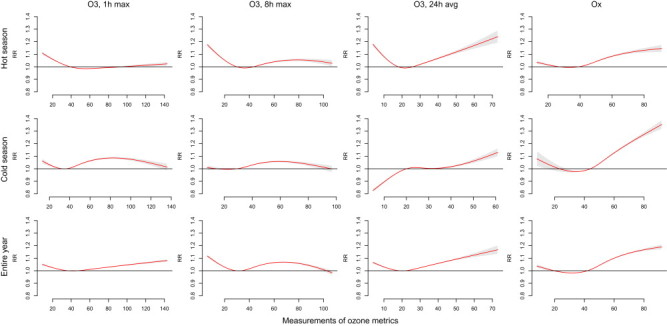
Cumulative 6-day relative risks of ozone metrics associated with outpatient visits for total respiratory disease using distributed lag non-linear model. Models included cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week; and long-term trends.
Table 2.
Cumulative six days (lag 0–5 days) relative risk and 95% confidence intervals for the ozone metrics associated with outpatient visits of total respiratory diseases (RD), asthma and chronic airway obstruction not elsewhere classified (CAO) using DLNM in Taipei Metropolitan, 2000–2009. Risks were estimated by comparing metrics for ozone concentrations at the 75th (Q3) percentiles with those at the 25th (Q1) percentiles.
| Total RD |
Asthma |
CAO |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | AIC | RR | 95% CI | AIC | RR | 95% CI | AIC | |
| Hot season (May–October) | |||||||||
| O3, 1 h max | 0.99 | 0.99–1.00 | 147,400 | 1.06 | 0.93–1.22 | 7074 | 0.91 | 0.85–0.97 | 11,391 |
| O3, 8 h max | 1.03 | 1.02–1.04 | 147,209 | 1.08 | 0.91–1.28 | 7072 | 0.93 | 0.86–1.01 | 11,399 |
| O3, 24 h | 1.03 | 1.02–1.04 | 146,998 | 1.00 | 0.84–1.20 | 7073 | 0.92 | 0.85–1.00 | 11,389 |
| Ox | 1.06 | 1.05–1.07 | 149,709 | 1.03 | 0.87–1.21 | 7086 | 0.99 | 0.91–1.07 | 11,412 |
| Cold season (November–April) | |||||||||
| O3, 1 h max | 1.05 | 1.04–1.06 | 238,246 | 1.09 | 0.94–1.26 | 7264 | 0.92 | 0.85–0.99 | 12,023 |
| O3, 8 h max | 1.04 | 1.04–1.05 | 238,292 | 1.09 | 0.93–1.28 | 7262 | 0.88 | 0.81–0.96 | 12,016 |
| O3, 24 h | 1.00 | 1.00–1.01 | 236,878 | 0.96 | 0.81–1.13 | 7264 | 0.85 | 0.78–0.92 | 12,007 |
| Ox | 1.10 | 1.10–1.11 | 245,188 | 1.18 | 1.00–1.39 | 7285 | 0.97 | 0.89–1.06 | 12,051 |
| Whole year | |||||||||
| O3, 1 h max | 1.02 | 1.01–1.02 | 396,188 | 1.02 | 0.95–1.09 | 14,386 | 0.96 | 0.93–1.00 | 23,618 |
| O3, 8 h max | 1.05 | 1.04–1.05 | 395,751 | 1.03 | 0.93–1.14 | 14,384 | 0.97 | 0.92–1.02 | 23,629 |
| O3, 24 h | 1.03 | 1.02–1.03 | 395,064 | 1.00 | 0.90–1.11 | 14,384 | 0.94 | 0.90–0.99 | 23,625 |
| Ox | 1.08 | 1.08–1.08 | 405,065 | 1.08 | 0.97–1.20 | 14,397 | 1.02 | 0.97–1.08 | 23,667 |
Table 2 shows the cumulative 6-day RRs of outpatient visits of total RD, asthma and CAO associated with ozone metrics varied with study periods. Based on the AIC values for the models, the O3, 24 h avg was the optimal metric in associating with outpatient visits of total RD with RRs of 1.03 (95% CI: 1.02, 1.04) in the hot season and 1.00 (95% CI: 1.00, 1.01) in the cold season. During the hot season, the relative risks of outpatient visits for total RD were 0.99 (not significant) and 1.03 (95% CI: 1.02, 1.04) in association with O3, 1 h max and O3, 8 h max, respectively. In the cold season, the corresponding estimated RRs ranged between 1.04 and 1.05. The Ox had the strongest association with outpatients visits of total RD with a RR of 1.10 (95% CI: 1.10, 1.11) during cold seasons. Except for O3, 24 h avg, this study revealed a higher ozone risk in the cold season than in the hot season.
Fig. 4 shows the risk of outpatient visits of total RD by the lag effects of ozone metrics levels measured at 75th percentiles relative to that measured at 25th percentiles by season. The RR peaked at lag 0–1 days in association with Ox in the cold season and entire year. There were 2–3 days lag association with O3, 1 h max, O3, 8 h max and O3, 24 h avg, much more apparent in cold days and the risk increased with exposure hours.
Fig. 4.
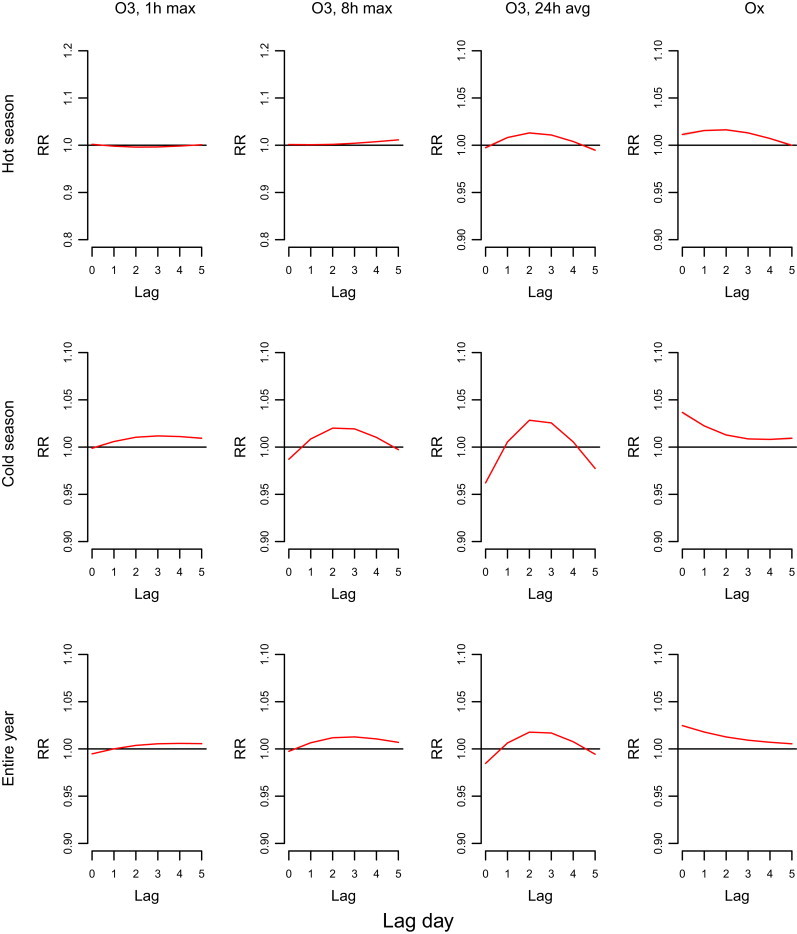
Risk of outpatient visits for total respiratory diseases in lag effects of ozone metrics measured at 75th percentile relative to 25th percentile. RRs were estimated using DLNM, which includes cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week, and long-term trends.
Supplementary Figs. S2 and S3 present the ozone exposure–response curves for outpatient visits for asthma and CAO, respectively. Only Ox was significantly associated with increased asthma during the cold season, with a RR of 1.18 (95% CI: 1.00, 1.39) (Table 2). In addition, outpatient visits of CAO were partly negatively associated with levels of ozone, occurred mostly in the cold seasons. Supplementary Figs. S4 and S5 show the risk of outpatient visits for asthma and CAO associated with the lag effects of ozone metrics measured at the 75th percentiles relative to that measured at the 25th percentiles. The association between Ox and CAO risk appeared the greatest at the lag 0 day.
Sensitivity analyses show that the effects of ozone metrics on outpatient visits of RD were robust to alternative models (data not shown). However, the AIC values were lowest and risk estimates were higher as we set the time as 14 df per year.
4. Discussion
This was the first study to explore the association between various ozone metrics and daily outpatient visits for total and cause-specific RD in Taiwan. The results show that the association observed between outpatient visits for total RD and ozone varied with the ozone metric, the study period and the disease type. The Ox, which combines daily O3 and NO2 concentrations, is associated with the highest risk estimates for total RD. The O3, 24 h avg, which included daytime and nighttime ozone exposure, was a better metric compared to O3, 1 h max and O3, 8 h max in terms of its association with outpatient visits for total RD based on model selection (Paoletti et al., 2007).
Ambient ozone is typically measured using three ozone metrics. Daily O3, 1 h max and O3, 8 h max are included in the U.S. National Ambient Air Quality Standard (USEPA, 2012). Daily mortality from all causes, cardiovascular diseases and RD in the US have been associated with the levels of O3, 8 h max (Zanobetti and Schwartz, 2008). In Europe, the Air Pollution and Health – A European Approach (APHEA) project has reported that all-cause mortality and respiratory mortality increased 0.33% and 1.13%, respectively, for an increment of 10 μg/m3 ambient O3, 1 h max (Gryparis et al., 2004). The O3, 24 h avg metric is a daily ozone exposure index widely used in epidemiological studies (Bell and Dominici, 2008; Bell et al., 2004). However, no standard criterion has been developed for ozone-related health effect studies. Paoletti et al. (2007) reported strong correlations among ozone exposure metrics and suggested that air quality information should be provided with biologically meaningful metrics.
Among all ambient air pollutants, the ozone level changes rapidly as being affected by the complicated ambient ozone precursors and meteorological conditions varying with time (Darrow et al., 2011). Measurements of ozone metrics are affected by diurnal pattern of ozone, spatial representative of the ozone metrics, correlation between metrics and concentrations of co-pollutants (Darrow et al., 2011). Generally, the level of O3, 1 h max reaches the peak at noon (from 11 AM to 2 PM) because of strong sunlight (Lin et al., 2010) (Supplementary Fig. S1). During the cold seasons in Taipei, however, we found the highest O3, 1 h max level at nighttime (from 12 PM to 8 AM) (Fig. 2). This finding is consistent with previous studies (Chen et al., 2004; Hsu, 2007). Their results show a bimodal seasonality observed in monthly levels with the highest concentrations in autumn and late winter because of weather conditions and co-pollutant emissions.
The present study shows that the O3, 24 h avg is the optimal metric than O3, 1 h max and O3, 8 h max in association with total RD based on model selection, which is consistent with the findings reported in Suzhou. Although O3, 1 h max and O3, 8 h max apparently have a stronger association with mortality rate compared to O3, 24 h avg in the cool season, the AIC value for the O3, 24 h avg model is the lowest among the three ozone metrics (Yang et al., 2012). Moreover, this study observed the significant positive association between levels of O3, 24 h avg and outpatient visits of total RD in the cold season (Fig. 2) imply that this ozone metric may be optimal for use in health risk association studies. However, further study is needed for various health outcomes and study areas.
Studies in the U.S. and Europe show that the ozone exposure is associated with mortality from all causes and respiratory diseases (Bell et al., 2004; Samoli et al., 2009). However, the associations between ozone exposure and morbidity from RD have proven inconclusive. A multi-city meta-analysis found that emergency hospitalizations for total RD could increase by 2.97% per 10 ppb increase in O3, 24 h avg in the elderly population (Ji et al., 2011). Some studies have also reported a significant association between ozone levels and hospital admissions for chronic obstructive pulmonary disease (COPD) and asthma (Anderson et al., 1997; Ko et al., 2007a, 2007b; Lin et al., 2008; Sunyer et al., 1997). However, studies in Prague and Los Angeles showed no significant association between ozone and hospital admissions for RD (Hunova et al., 2013; Linn et al., 2000). In Metro Taipei, while outpatient visits for total RD is associated with ozone after adjusting for PM10 and NO2, the outpatient visits for asthma is associated with the combined effect of ozone and NO2 only in the cold season after adjusting for PM10. Our findings conflict with those of a Barcelona study, in which Ox is associated with the morbidity of COPD and asthma (Tobias Garces et al., 1998). However, because of depletion of ozone by NO, which is quickly oxidized by ozone to form NO2 in ambient atmosphere, total oxidant (Ox = O3 + NO2) is considered a better indicator for assessing the effects of both ozone and NO2 exposure (Chou et al., 2006). Ox appears the strongest association with outpatient visits for total RD in the present study. Therefore, Ox could be optional ozone metric for estimating health effects in metropolitan areas with strong sunlight and heavy traffic pollution.
The mortality risk associated with ozone exposure by season poses conflicting evidences. Some studies have found the highest risk in warmer months (Bell et al., 2004; Gryparis et al., 2004; Ito et al., 2005; Zanobetti and Schwartz, 2008). However, the mortality risk of ozone is unlikely confounded by temperature (Schwartz, 2005). The present study and previous studies conducted in Taipei and Shanghai (Liang et al., 2009; Yang et al., 2007; Zhang et al., 2006) found that the health risk of ozone was higher in cold days than in hot days. Therefore, assessments of the health risks of ozone should not be limited to the warm season.
Ozone-related epidemiological studies generally assume a linear relationship between health risks and ozone levels (Bell et al., 2005). However, Lefohn et al. (2010) have reported a nonlinear relationship between ozone dose and pulmonary function. The lag effect of air pollutants is also considered a critical factor in health assessments. This study applied DLNM to calculate the nonlinear association and cumulative risks related to air pollutants at lag days. The findings enable greater flexibility when presenting the nonlinear ozone exposure–response curve for outpatient visits for total RD (Fig. 3) (Lefohn et al., 2010).
This study had some limitations. First, it used population-based outpatient visit data rather than individual-based data. That is, this ecological study did not collect information on personal ozone exposure and corresponding health response. Additionally, this study did not consider factors such as demography, personal lifestyle, socioeconomics, occupational exposure, air conditioner usage, and medical care provision, all of which can affect the ozone-health association. However, the risk of ozone on outpatient visits for total RD remains robust even after controlling for the potential effects of other air pollutants such as PM10 and NO2, meteorological conditions such as daily temperature, RH and WS, and respiratory tract infections and other potential confounders. Notably, the risk varies with the ozone metrics applied. This study agreed with previous findings that ozone metrics must be carefully manipulated when applying them to assess human exposure. Multiple ozone exposure metrics are recommended for health risk assessment (Anderson and Bell, 2010).
5. Conclusion
The health risk of RD related to ozone varies by the disease type and ozone metrics measured. The O3, 24 h avg, represented both daytime and nighttime ozone exposure, is the preferred metric instead of O3, 1 h max and O3, 8 h max for assessing the association with outpatient visits for total RD. The daily Ox levels of combined ozone and NO2 concentrations exhibit the strongest correlation with outpatient visits for total RD in the cold season in Metropolitan Taipei.
Fundings
This study was supported in part by the National Science Council of the Republic of China, Taiwan, under Contract Nos. NSC 100-2621-M-039-001 and NSC 99-2221-E-033-052.
Conflict of interest statement
All the authors declare that this study involves no conflict of interest.
Acknowledgments
The authors would like to thank the National Health Research Institute, Taiwan Environmental Protection Administration and Taiwan Central Weather Bureau for providing data. Interpretations and conclusions herein do not represent those of these agencies. Ted Knoy is appreciated for his editorial assistance.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.envpol.2012.12.010.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
Measurements of ozone metrics by month in Taipei from 2000 to 2009.
Cumulative 6-day relative risks of ozone metrics associated with outpatient visits of asthma using distributed lag non-linear model. Models included cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week, and long-term trends.
Cumulative 6-day relative risks of ozone metrics associated with outpatient visits of chronic airway obstruction not elsewhere classified using distributed lag non-linear model. Models included cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week, and long-term trends.
Lag effects of ozone metrics at measurements of 75th percentile compared with measurements of 25th percentile on the outpatient visits of asthma. RRs were estimated using DLNM, which includes cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week, and long-term trends.
Lag effects of ozone metrics at measurements of 75th percentile compared with measurements of 25th percentile on the outpatient visits of chronic airway obstruction not elsewhere classified. RRs were estimated using DLNM, which includes cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week, and long-term trends.
References
- Akaike H. 2nd International Symposium on Information Theory. 1973. Information theory and an extension of the maximum likelihood principle; pp. 267–281. [Google Scholar]
- Anderson G.B., Bell M.L. Does one size fit all? The suitability of standard ozone exposure metric conversion ratios and implications for epidemiology. J. Expo. Sci. Environ. Epidemiol. 2010;20:2–11. doi: 10.1038/jes.2008.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson H.R., Spix C., Medina S., Schouten J.P., Castellsague J., Rossi G., Zmirou D., Touloumi G., Wojtyniak B., Ponka A., Bacharova L., Schwartz J., Katsouyanni K. Air pollution and daily admissions for chronic obstructive pulmonary disease in 6 European cities: results from the APHEA project. Eur. Respir. J. 1997;10:1064–1071. doi: 10.1183/09031936.97.10051064. [DOI] [PubMed] [Google Scholar]
- Bell M.L., Dominici F. Effect modification by community characteristics on the short-term effects of ozone exposure and mortality in 98 US communities. Am. J. Epidemiol. 2008;167:986–997. doi: 10.1093/aje/kwm396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell M.L., Dominici F., Samet J.M. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study. Epidemiology. 2005;16:436–445. doi: 10.1097/01.ede.0000165817.40152.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell M.L., McDermott A., Zeger S.L., Samet J.M., Dominici F. Ozone and short-term mortality in 95 US urban communities, 1987–2000. JAMA. 2004;292:2372–2378. doi: 10.1001/jama.292.19.2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of National Health Insurance . Bureau of National Health Insurance, Department of Health, Executive Yuan, Republic of China; Taipei: 2001. National Health Insurance Profile. (in Chinese) [Google Scholar]
- Chang S.C., Lee C.T. Evaluation of the temporal variations of air quality in Taipei City, Taiwan, from 1994 to 2003. J. Environ. Manage. 2008;86:627–635. doi: 10.1016/j.jenvman.2006.12.029. [DOI] [PubMed] [Google Scholar]
- Chen K.S., Ho Y.T., Lai C.H., Tsai Y.A., Chen S.J. Trends in concentration of ground-level ozone and meteorological conditions during high ozone episodes in the Kao-Ping Airshed, Taiwan. J. Air Waste Manag. Assoc. 2004;54:36–48. doi: 10.1080/10473289.2004.10470880. [DOI] [PubMed] [Google Scholar]
- Cheng M.F., Tsai S.S., Chiu H.F., Sung F.C., Wu T.N., Yang C.Y. Air pollution and hospital admissions for pneumonia: are there potentially sensitive groups? Inhal. Toxicol. 2009;21:1092–1098. doi: 10.3109/08958370902744855. [DOI] [PubMed] [Google Scholar]
- Chou C.C.K., Liu S.C., Lin C.Y., Shiu C.J., Chang K.H. The trend of surface ozone in Taipei, Taiwan, and its causes: implications for ozone control strategies. Atmos. Environ. 2006;40:3898–3908. [Google Scholar]
- Darrow L.A., Klein M., Sarnat J.A., Mulholland J.A., Strickland M.J., Sarnat S.E., Russell A.G., Tolbert P.E. The use of alternative pollutant metrics in time-series studies of ambient air pollution and respiratory emergency department visits. J. Expo. Sci. Environ. Epidemiol. 2011;21:10–19. doi: 10.1038/jes.2009.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A., Armstrong B., Kenward M.G. Distributed lag non-linear models. Stat. Med. 2010;29:2224–2234. doi: 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg M.S., Gasparrini A., Armstrong B., Valois M.F. The short-term influence of temperature on daily mortality in the temperate climate of Montreal, Canada. Environ. Res. 2011;111:853–860. doi: 10.1016/j.envres.2011.05.022. [DOI] [PubMed] [Google Scholar]
- Gryparis A., Forsberg B., Katsouyanni K., Analitis A., Touloumi G., Schwartz J., Samoli E., Medina S., Anderson H.R., Niciu E.M., Wichmann H.E., Kriz B., Kosnik M., Skorkovsky J., Vonk J.M., Dortbudak Z. Acute effects of ozone on mortality from the “air pollution and health: a European approach” project. Am. J. Respir. Crit. Care Med. 2004;170:1080–1087. doi: 10.1164/rccm.200403-333OC. [DOI] [PubMed] [Google Scholar]
- Hsu K.J. Relationships between ten-year trends of tropospheric ozone and temperature over Taiwan. Sci. Total Environ. 2007;374:135–142. doi: 10.1016/j.scitotenv.2007.01.003. [DOI] [PubMed] [Google Scholar]
- Hunova I., Maly M., Rezacova J., Branis M. Association between ambient ozone and health outcomes in Prague. Int. Arch. Occup. Environ. Health. 2013;86:89–97. doi: 10.1007/s00420-012-0751-y. [DOI] [PubMed] [Google Scholar]
- Ito K., De Leon S.F., Lippmann M. Associations between ozone and daily mortality: analysis and meta-analysis. Epidemiology. 2005;16:446–457. doi: 10.1097/01.ede.0000165821.90114.7f. [DOI] [PubMed] [Google Scholar]
- Ji M., Cohan D.S., Bell M.L. Meta-analysis of the association between short-term exposure to ambient ozone and respiratory hospital admissions. Environ. Res. Lett. 2011;6 doi: 10.1088/1748-9326/6/2/024006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson P.E., Braun S., Broadmeadow M., Elvira S., Emberson L., Gimeno B.S., Le Thiec D., Novak K., Oksanen E., Schaub M., Uddling J., Wilkinson M. Risk assessments for forest trees: the performance of the ozone flux versus the AOT concepts. Environ. Pollut. 2007;146:608–616. doi: 10.1016/j.envpol.2006.06.012. [DOI] [PubMed] [Google Scholar]
- Ko F.W., Tam W., Wong T.W., Chan D.P., Tung A.H., Lai C.K., Hui D.S. Temporal relationship between air pollutants and hospital admissions for chronic obstructive pulmonary disease in Hong Kong. Thorax. 2007;62:780–785. doi: 10.1136/thx.2006.076166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko F.W., Tam W., Wong T.W., Lai C.K., Wong G.W., Leung T.F., Ng S.S., Hui D.S. Effects of air pollution on asthma hospitalization rates in different age groups in Hong Kong. Clin. Exp. Allergy. 2007;37:1312–1319. doi: 10.1111/j.1365-2222.2007.02791.x. [DOI] [PubMed] [Google Scholar]
- Lefohn A.S., Hazucha M.J., Shadwick D., Adams W.C. An alternative form and level of the human health ozone standard. Inhal. Toxicol. 2010;22:999–1011. doi: 10.3109/08958378.2010.505253. [DOI] [PubMed] [Google Scholar]
- Liang W.M., Wei H.Y., Kuo H.W. Association between daily mortality from respiratory and cardiovascular diseases and air pollution in Taiwan. Environ. Res. 2009;109:51–58. doi: 10.1016/j.envres.2008.10.002. [DOI] [PubMed] [Google Scholar]
- Lin S., Bell E.M., Liu W., Walker R.J., Kim N.K., Hwang S.A. Ambient ozone concentration and hospital admissions due to childhood respiratory diseases in New York State, 1991–2001. Environ. Res. 2008;108:42–47. doi: 10.1016/j.envres.2008.06.007. [DOI] [PubMed] [Google Scholar]
- Lin Y.K., Lin T.H., Chang S.C. The changes in different ozone metrics and their implications following precursor reductions over northern Taiwan from 1994 to 2007. Environ. Monit. Assess. 2010;169:143–157. doi: 10.1007/s10661-009-1158-4. [DOI] [PubMed] [Google Scholar]
- Linn W.S., Szlachcic Y., Gong H., Jr., Kinney P.L., Berhane K.T. Air pollution and daily hospital admissions in metropolitan Los Angeles. Environ. Health Perspect. 2000;108:427–434. doi: 10.1289/ehp.00108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of the Interior . Department of Statistics, Ministry of the Interior, ROC; Taipei: 2006. Land Area and Population Density in Taiwan Area. [Google Scholar]
- Musselman R.C., Lefohn A.S., Massman W.J., Heath R.L. A critical review and analysis of the use of exposure- and flux-based ozone indices for predicting vegetation effects. Atmos. Environ. 2006;40:1869–1888. [Google Scholar]
- Paoletti E., De Marco A., Racalbuto S. Why should we calculate complex indices of ozone exposure? Results from Mediterranean background sites. Environ. Monit. Assess. 2007;128:19–30. doi: 10.1007/s10661-006-9412-5. [DOI] [PubMed] [Google Scholar]
- Pattenden S., Armstrong B., Milojevic A., Heal M.R., Chalabi Z., Doherty R., Barratt B., Kovats R.S., Wilkinson P. Ozone, heat and mortality: acute effects in 15 British conurbations. Occup. Environ. Med. 2010;67:699–707. doi: 10.1136/oem.2009.051714. [DOI] [PubMed] [Google Scholar]
- Samoli E., Zanobetti A., Schwartz J., Atkinson R., LeTertre A., Schindler C., Perez L., Cadum E., Pekkanen J., Paldy A., Touloumi G., Katsouyanni K. The temporal pattern of mortality responses to ambient ozone in the APHEA project. J. Epidemiol. Community Health. 2009;63:960–966. doi: 10.1136/jech.2008.084012. [DOI] [PubMed] [Google Scholar]
- Schwartz J. How sensitive is the association between ozone and daily deaths to control for temperature? Am. J. Respir. Crit. Care Med. 2005;171:627–631. doi: 10.1164/rccm.200407-933OC. [DOI] [PubMed] [Google Scholar]
- Schwela D. Air pollution and health in urban areas. Rev. Environ. Health. 2000;15:13–42. doi: 10.1515/reveh.2000.15.1-2.13. [DOI] [PubMed] [Google Scholar]
- Sunyer J., Spix C., Quenel P., Ponce-de-Leon A., Ponka A., Barumandzadeh T., Touloumi G., Bacharova L., Wojtyniak B., Vonk J., Bisanti L., Schwartz J., Katsouyanni K. Urban air pollution and emergency admissions for asthma in four European cities: the APHEA Project. Thorax. 1997;52:760–765. doi: 10.1136/thx.52.9.760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taiwan Central Weather Bureau . 2013. Illustrations of Surface Observation Data.http://www.cwb.gov.tw/V7e/observe/ Available at: (accessed 01.04.13.) [Google Scholar]
- Taiwan Environmental Protection Administration . 2011. Taiwan Air Quality Monitoring Network.http://taqm.epa.gov.tw/taqm/en/PsiAreaHourly.aspx Available at: (accessed 12.05.11.) [Google Scholar]
- Tobias Garces A., Sunyer Deu J., Castellsague Pique J., Saez Zafra M., Anto Boque J.M. Impact of air pollution on the mortality and emergencies of chronic obstructive pulmonary disease and asthma in Barcelona. Gac. Sanit. 1998;12:223–230. doi: 10.1016/s0213-9111(98)76476-3. [DOI] [PubMed] [Google Scholar]
- USEPA . 2012. National Ambient Air Quality Standards (NAAQS)http://www.epa.gov/air/criteria.html Available at: (accessed 09.12.12.) [Google Scholar]
- Wong T.W., Lau T.S., Yu T.S., Neller A., Wong S.L., Tam W., Pang S.W. Air pollution and hospital admissions for respiratory and cardiovascular diseases in Hong Kong. Occup. Environ. Med. 1999;56:679–683. doi: 10.1136/oem.56.10.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C., Yang H., Guo S., Wang Z., Xu X., Duan X., Kan H. Alternative ozone metrics and daily mortality in Suzhou: the China Air Pollution and Health Effects Study (CAPES) Sci. Total Environ. 2012;426:83–89. doi: 10.1016/j.scitotenv.2012.03.036. [DOI] [PubMed] [Google Scholar]
- Yang C.Y., Chen C.C., Chen C.Y., Kuo H.W. Air pollution and hospital admissions for asthma in a subtropical city: Taipei, Taiwan. J. Toxicol. Environ. Health A. 2007;70:111–117. doi: 10.1080/15287390600755059. [DOI] [PubMed] [Google Scholar]
- Zanobetti A., Schwartz J. Is there adaptation in the ozone mortality relationship: a multi-city case-crossover analysis. Environ. Health. 2008;7:22. doi: 10.1186/1476-069X-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Huang W., London S.J., Song G., Chen G., Jiang L., Zhao N., Chen B., Kan H. Ozone and daily mortality in Shanghai, China. Environ. Health Perspect. 2006;114:1227–1232. doi: 10.1289/ehp.9014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Measurements of ozone metrics by month in Taipei from 2000 to 2009.
Cumulative 6-day relative risks of ozone metrics associated with outpatient visits of asthma using distributed lag non-linear model. Models included cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week, and long-term trends.
Cumulative 6-day relative risks of ozone metrics associated with outpatient visits of chronic airway obstruction not elsewhere classified using distributed lag non-linear model. Models included cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week, and long-term trends.
Lag effects of ozone metrics at measurements of 75th percentile compared with measurements of 25th percentile on the outpatient visits of asthma. RRs were estimated using DLNM, which includes cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week, and long-term trends.
Lag effects of ozone metrics at measurements of 75th percentile compared with measurements of 25th percentile on the outpatient visits of chronic airway obstruction not elsewhere classified. RRs were estimated using DLNM, which includes cumulative 6-day effects of PM10 and NO2, cumulative 8-day effects of average temperature, cumulative 15-day effects of outpatient visits for pneumonia and influenza, relative humidity, wind speed, holiday effects, day of the week, and long-term trends.


