Abstract
Background:
On July 21–22, 2012, Beijing, China, suffered its heaviest rainfall in 60 years. Two studies have estimated the fatality toll of this disaster using a traditional surveillance approach. However traditional surveillance can miss disaster-related deaths, including a substantial number of deaths from natural causes triggered by disaster exposure. Here we investigated community-wide mortality risk during this flood compared to rates in unexposed reference periods.
Methods:
We compared community-wide mortality rates on the peak flood day and the four following days to seasonally-matched non-flood days in previous years (2008–2011), controlling for potential confounders, to estimate the relative risks (RRs) of daily mortality among Beijing residents associated with this flood.
Results:
On July 21, 2012, the flood-associated RRs of all-cause, circulatory, and accidental mortality were 1.34 (95% confidence interval, 1.11–1.61), 1.37 (1.01–1.85), and 4.40 (2.98–6.51), respectively, compared to unexposed periods. No evidence of increased risk of respiratory mortality was observed. For the flood period of July 21–22, 2012, we estimated a total of 79 excess deaths among Beijing residents; by contrast, only 34 deaths were reported among Beijing residents in a study using a traditional surveillance approach.
Conclusions:
To our knowledge, this is the first study analyzing community-wide changes in mortality rates during the 2012 flood in Beijing, and one of the first to do so for any major flood worldwide. This study offers critical evidence on flood-related health impacts, as urban flooding is expected to become more frequent and severe in China.
Keywords: environmental health, natural disasters, floods, climate change
INTRODUCTION
On July 21, torrential rains fell from mid-day through the night, triggering flash floods.1–3 Almost 90% of the city experienced rainfall totals >100 millimeters (mm),2 and flooding was reported throughout the city.4 In some regions of the city, the disaster was particularly severe—for example, Fangshan District experienced >450 mm of rainfall.2 Flooding affected over 60 main roads at low-lying underpasses and bridges.2 Over 50,000 people were evacuated,3 and damages totaled over a billion dollars.2 As is often the case for urban flash floods,5 a key factor was that the rate of rainfall exceeded drainage capacity.3,4 Flood waters quickly receded after rainfall ended early on July 22,6 as drainage networks caught up, although clean-up of debris and mud was needed in following days, and some residents remained evacuated from their homes for several days.2,3,7
Two studies estimated the fatality toll from this flood,8,9 using a traditional surveillance approach of investigating each death that occurred in Beijing during the flood period, case-by-case, to identify which were flood-attributable. This surveillance approach searches death certificates for specific mentions of ties to a disaster and, in some cases, may draw on other available details on the circumstances of a specific death, including government and media reports, to determine if that death can be attributed to the disaster.8–10
Based on this approach, 60 or more of the deaths in Beijing on July 21–22, 2012, including 34 among Beijing residents, were attributable to the flood, mostly from drowning.8,9 Most deaths identified from the two surveillance studies were those caused by direct physical forces of the flood, such as drowning, or were from accidental causes linked to hazards created by the event, such as crushing by falling objects and electrical shocks.8,9 The traditional surveillance approach used for these estimates can, however, undercount disaster-associated deaths, especially from indirect causes that are also common outside of disaster periods.11 Further, this approach is unable to identify any patterns of potential avoided deaths during the disaster (e.g., a reduction in automobile fatalities related to people avoiding driving during severe weather conditions).12 Given these limitations in the traditional surveillance approach, an alternative approach that implements a counterfactual scenario in which mortality rates during the disaster are evaluated against mortality rates from comparable reference periods may provide more robust estimates of risk.
While assessments of community-wide mortality rates have been used to help understand the health impacts of other climate-related disasters, especially extreme temperature and heat waves,13,14 few studies worldwide have used a similar technique to better understand the mortality risks associated with floods. Several previous studies have explored large-scale, multi-year patterns in flood-related fatality tolls, including in the United States and Australia,15,16 but these employed a traditional surveillance approach. Worldwide, only a few studies have investigated flood-associated mortality risks by comparing the rate of community-wide mortality observed during the flood to rates in non-flooded periods or areas,17–21 making evidence on how community-wide mortality rates change during severe floods extremely limited, including in China.
Community-wide assessments can be particularly helpful in capturing changes in rates of circulatory and respiratory mortality during a disaster, as both are common mortality outcomes outside of disaster periods and so hard to attribute to a disaster on a case-by-case basis. Limited studies from outside China have found floods can substantially increase the risk of non-fatal cardiorespiratory outcomes, including risks of heart palpitations22 and heart attacks,23 making it plausible that major floods could also increase community-wide rates of circulatory and respiratory deaths. Beijing’s large population (> 21 million)24 provides the statistical power to investigate how a major flood changed community-wide mortality rates in a major Chinese city during and immediately after the event, both for deaths from all-causes and for deaths from several specific causes (circulatory, respiratory, and accidental).
METHODS
Data
We obtained daily mortality counts from the Chinese Center for Disease Control and Prevention (CDC) for all Beijing residents from January 1, 2008, to December 31, 2012. Cause of death was coded according to the International Classification of Disease, Revision 10 (ICD-10, 2003 version).25 We aggregated data to create daily community-wide counts of deaths from four causes: all-cause, accidental (ICD-10: S00–Z99), circulatory (I00–I99), and respiratory (J00–J99). We obtained residential population data from the National Bureau of Statistics of China.24 We obtained daily temperature data from a weather station located in Nanjiao District (between Beijing’s fifth and sixth ring roads) and daily average concentrations of particulate matter with an aerodynamic diameter ≤ 2.5 micrometers (PM2.5) (used in sensitivity analysis) from a station in the Haidian District, both administrated by the Beijing Meteorological Bureau.
Statistical Analysis
The methodology of analyzing community-wide health risks from a disaster, by comparing the mortality rates observed during the disaster to the rates that would be expected had the disaster not occurred, is still in development. One potential approach is to use methods developed to study continuous ambient exposures like air pollution and temperature: time series analysis26 and time-stratified case-crossover.27 However, a potential limitation of both of these approaches to study the effects of discrete disaster periods is that they use, as controls, periods that are close in time to the event. While this implicitly helps control for long-term trends in baseline community mortality rates when studying continuous exposures, it could lead to biased estimates when studying disasters if disasters have extended impacts on community health risks and if this period of potential extended disaster effects is incorrectly specified in the model. A recent study provides a good example of the plausibility of such extended disaster effects: following Hurricane Maria’s landfall, the mortality rate in Puerto Rico for the next three months increased 62% compared with the same period of the previous year.28
Given these potential concerns with applying the time series or case-crossover study designs to analyze the effects of a disaster, we instead used a study design that matched the days of the flood disaster to similar unexposed days from the same time of the year in other years in Beijing, with control for long-term trends in mortality rates and the influence of temperature on mortality risk incorporated in the statistical model fit to this matched data. Previous studies have used similar study design to investigate hospitalization risk of other natural disasters, including heat waves29 and wildfires.30 As a sensitivity analysis, we also estimated risks based on time series and case-crossover designs,13,14,26,27 to help determine the sensitivity of estimates to the choice of study design.
While some floods can be long-lasting, this flash resulted from extreme rainfall from a single storm system, which began mid-day on July 21 and ended early in the morning of July 22.2,8 The flood waters receded in the hours following the rains,6 as the city’s drainage system caught up with the excess water. In heavily affected areas, many residents were evacuated within a day,2 limiting exposure to lingering flood waters in these districts. Given the rapid onset and dissipation of flooding, we classified the July 21 as the main exposed day (peak flood day). We also investigated potential changes in health risks in the four following days, which we modeled as lagged associations from the peak flood day. Such delayed associations could represent either delayed health effects from exposure on the peak flood day or health effects associated with exposure to mud, debris, lingering flood waters, or flood-associated infrastructure damage in the days following the peak flood day.
We matched the peak flood day (July 21, 2012), as well as four days after, with similar unexposed days. For the matched unexposed days, we selected days that were in: (1) a different year than the flood year; (2) the same month of year as the flood (July); and (3) the same day of week as the exposed day (e.g., the peak flood day, a Saturday, was matched to other Saturdays). To this matched data, we fit a model incorporating an unconstrained distributed lag while controlling for the potential confounders of long-term trends in mortality rates and temperature’s influence on mortality risk. We fit the following generalized linear model, using an over-dispersed Poisson distribution:
| (1) |
where:
Yt is the daily mortality among all Beijing residents on day t;
nYear(t) is the residential population of Beijing in the year of day t, included as an offset term to capture variation in Beijing’s population over the years included in the study period;
α is the model intercept;
β is a vector of length five (βl, l = 0,…, 4) of coefficients estimated from an unconstrained distributed lag function of flood exposure,31 where xt is 1 for the peak flood day and 0 for other days, and therefore xt-l is an indicator variable denoting whether a given day at lag l from day t is within the flood-exposed period or within the matched unexposed period;
Yeart is the year for day t, with γ as the coefficient for year, allowing control for a linear trend in mortality rates across study years;
Tt is the mean temperature for day t, with δ as the coefficient for Tt We also tested sensitivity to a more flexible control for temperature through a distributed lag non-linear function of daily temperature for lags 0–2.
With this unconstrained distributed lag model, separate associations are estimated for each lag; given the study design, data used in the analysis are matched on day of week for each lag-specific estimate, removing the need for further statistical control of day of week in the model.
The estimated lag-specific RRs of mortality on lag l from the peak flood day were calculated as RRl = exp(βl), based on the values of βl estimated from eq. 1. We estimated the flood-attributable number of deaths (El)as32
| (2) |
where Yl is the observed death count at lag l from the peak flood day.
Previous research, which calculated the fatality tolls for this flood using a traditional surveillance method,8,9 determined fatality tolls for the two days of July 21–22, 2012. To allow us to compare estimated flood-associated fatality tolls between our analysis approach and the traditional surveillance method, we also calculated excess deaths specifically for these two days. We calculated confidence interval for the estimate of total excess deaths on this two-day period using Monte Carlo simulations (details in Supplementary Material).
Sensitivity analysis.
In additional to our primary analysis, we also investigated the sensitivity of estimates to study design and modeling choices. First, we investigated whether results changed with differing selections of control days, changing to select from any day of the same month of year as the flood (July) in other years rather than restricting by day of week (referred to as “Matching by month” in results). Second, we changed the model’s control for potential confounders. We first adjusted for the daily average concentration of fine particulate matter (PM2.5) (“PM2.5-adjusted”). PM2.5 could be a potential confounder for the association between flooding and mortality. Ambient PM2.5 has been associated with increased mortality risk in China33 and can also influence summer rainfall frequency34 in China, a common cause of urban flooding in the country. We next fit a model that did not adjust for temperature as in the primary analysis (“Not temperature-adjusted”). Finally, we investigated the sensitivity of effect estimates to using time series and case-crossover designs rather than matching to similar days from other years. In the time series analysis (“Time series”), we used year-round data from the five-year study period, fitting a natural cubic spline function of time with 7 degree of freedom per year in the model to control for seasonal and long-term trends and, to control for temperature, a natural cubic spline with 3 degree of freedom. In the case-crossover analysis (“Case-crossover”), we used the time-stratified variant of this design,27 defining the case day as the peak flood day and control days as those days in the same year, month of year, and day of week as the case day. We analyzed the case-crossover data using a conditional Poisson generalized linear model,35 resulting in a risk ratio estimate that is directly comparable to the risk ratio estimates generated from the other study designs considered.
RESULTS
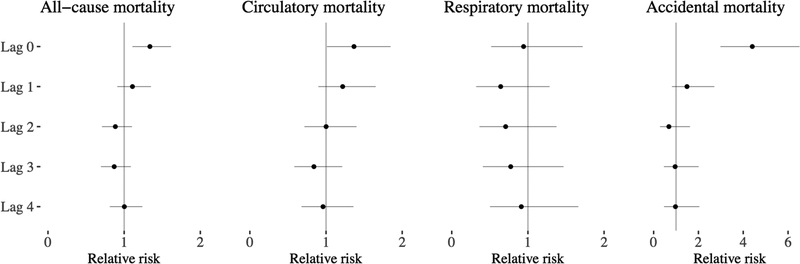
Compared to non-flood reference periods in other years, community-wide mortality rates were substantially higher among Beijing residents during the flood period for all-cause, circulatory, and accidental mortality compared to rates in matched unexposed periods (Figures 1 and 2). The highest increased risks were observed on the peak flood day (July 21, 2012) (Figures 1 and 2), when community-wide mortality rates were 34% higher for all-causes combined (relative risk [RR]: 1.34; 95% confidence interval [CI]: 1.11–1.61), 37% higher for cardiovascular causes (RR: 1.37; 95% CI: 1.01–1.85), and 340% higher for accidental causes (RR: 4.40; 95% CI: 2.98–6.51) (Figure 2). These estimated relative risks translated to 59 flood-related excess deaths overall on the peak flood day among Beijing residents, including 28 excess circulatory deaths and 24 excess accidental deaths (Table 1). For respiratory mortality, conversely, there was no evidence of an increase during the flood compared to matched unexposed days.
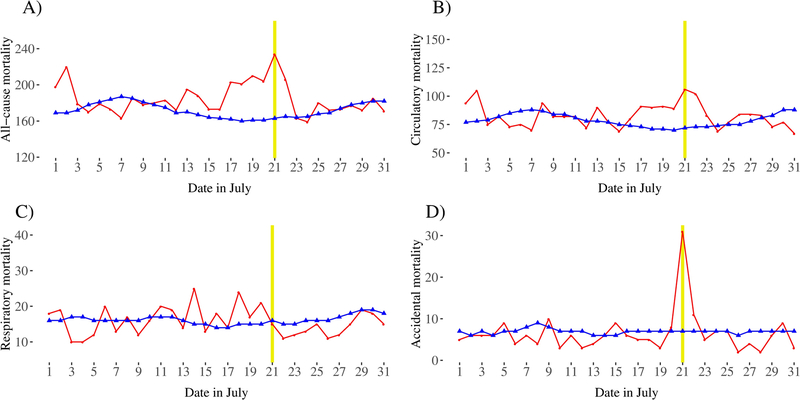
Figure 1.
Daily mortality counts for Beijing residents in July 2012 (red) compared with average mortality counts in July of previous years for (A) all-cause mortality, (B) circulatory mortality, (C) respiratory mortality, and (D) accidental mortality. Shown for comparison are the mean (blue line) of the five-day moving average of mortality, as well as the range (grey area) of daily mortality counts in July of the four previous years (2008–2011). The yellow vertical lines show the peak flood day (July 22).
Figure 2.
Estimates of the relative risk of mortality for four mortality outcomes on the peak flood day (lag 0) and on the four following days (lags 1–4) compared with matched unexposed days from other years, with modeled control for temperature and long-term mortality trends. Dots show point estimates and horizontal lines show 95% confidence intervals. The gray vertical line shows as a reference a relative risk of 1.
Table 1.
Estimates of relative risk of mortality compared to matched unexposed days, as well as the resulting estimates of flood-associated excess deaths, among Beijing residents on the peak flood day (July 21, 2012) and the following day. For each point estimate, 95% confidence intervals are shown in parentheses.
| Relative risk on July 21, 2012 (peak flood day) | Relative risk on July 22, 2012 | Excess deaths on peak flood daya | Excess deaths on July 21–22, 2012b | |
|---|---|---|---|---|
| All-cause mortality | 1.34 (1.11, 1.61) | 1.11 (0.91, 1.35) | 59 (23, 89) | 79 (22, 125) |
| Circulatory mortality | 1.37 (1.01, 1.85) | 1.22 (0.90, 1.65) | 28 (1, 49) | 46 (6, 79) |
| Respiratory mortality | 0.94 (0.52, 1.72) | 0.64 (0.32, 1.28) | −1 (−14, 6) | −7 (−29, 5) |
| Accidental mortality | 4.40 (2.98, 6.51) | 1.49 (0.82, 2.71) | 24 (21, 26) | 28 (20, 32) |
Confidence intervals were calculated based on the uncertainty of estimated relative risk on the peak flood day.
Confidence intervals were calculated using Monte Carlo simulation (details in the Supplementary Material).
The increases in community-wide rates for all-cause, circulatory, and accidental mortality were largest on the peak flood day (July 21, 2012), with some evidence of a continued increase on the following day (Figure 2). For the days considered further after the peak flood day (lags 2–4), we did not find evidence of significantly increased mortality risk for any cause considered. Since traditional surveillance considered the two-day period of July 21–22, 2012,8,9 we also estimated flood-associated deaths for this two-day period and estimated a total of 79 excess deaths in this period among Beijing residents (Table 1). Most of these deaths were from circulatory causes (an estimated 46 flood-related deaths) or accidental deaths (an estimated 28 flood-related deaths) (Table 1).
Estimates of RRs were robust to modeling choice and the matching method for selecting unexposed days for all-cause, circulatory, and respiratory mortality (Table 2). In all cases, we estimated increases of approximately 30% in all-cause mortality, increases of approximately 35% in circulatory mortality, and decreases of approximately 10% in respiratory mortality on the peak flood day compared to non-flood reference periods. However, when considering accidental mortality, results were somewhat sensitive to study design (Table 2). This could be because the accidental mortality rate in July across the years included in the study varied in a pattern that was difficult to capture using a linear control for long-term patterns in mortality rates (eFigure 1), as conducted in our primary analysis. When temperature was controlled with a more flexible control and to a longer lag, effect estimates were almost identical to the primary results (eFigure 2).
Table 2.
Sensitivity of estimates of relative risk on the peak flood day (July 21, 2012) to study design and modeling choices. The first row repeats the estimates generated based on our primary analysis (also shown in Table 1). All other rows show estimates based on alternative study design or modeling choices; see the Methods for descriptions of each. Shown in parentheses are the 95% confidence intervals for each estimate.
| All-cause mortality | Circulatory mortality | Respiratory mortality | Accidental mortality | |
|---|---|---|---|---|
| Primary analysis | 1.34 (1.11, 1.61) | 1.37 (1.01, 1.85) | 0.94 (0.52, 1.72) | 4.40 (2.98, 6.51) |
| Matching by month | 1.35 (1.11, 1.63) | 1.38 (1.01, 1.88) | 0.91 (0.50, 1.66) | 3.86 (2.70, 5.54) |
| PM2.5-adjusted | 1.33 (1.09, 1.62) | 1.32 (0.97, 1.79) | 0.90 (0.49, 1.66) | 4.55 (2.96, 6.98) |
| Not temperature-adjusted | 1.27 (1.02, 1.57) | 1.28 (0.92, 1.77) | 0.88 (0.48, 1.64) | 4.22 (2.87, 6.21) |
| Time series | 1.30 (1.11, 1.52) | 1.33 (1.06, 1.67) | 0.93 (0.55, 1.56) | 5.48 (3.73, 8.06) |
| Case-crossover | 1.33 (1.09, 1.62) | 1.38 (1.04, 1.83) | 0.85 (0.46, 1.57) | 6.64 (3.48, 12.67) |
DISCUSSION
Our results demonstrate this flood’s considerable impacts on public health in Beijing (79 deaths among Beijing residents), with over half of this impact resulting from increased risk of non-accidental mortality, in particular circulatory mortality (46 deaths among Beijing residents). The government of China, using a traditional surveillance approach of identifying flood-related deaths on a case-by-case basis, identified 60 flood-related deaths (among Beijing residents and non-residents combined) on July 21–22, 2012.8 Another study that similarly used a traditional surveillance approach—expanding on the government analysis by combining fatality information on specific deaths from different sources like government reports and site visitations— found 79 flood-related deaths, 71 of which could be identified as residents or non-residents, with 34 of these among Beijing residents.9 The estimated fatality toll among Beijing residents based on the traditional surveillance approach is therefore less than half the number of flood-related deaths we estimated based on an approach of comparing community-wide mortality rates during July 21–22, 2012, to the rates in comparable reference periods (Table 1).
Further, the previous surveillance-based research found the majority of flood-attributable deaths were due to drowning.8,9 The surveillance approach did identify two circulatory deaths from the flood—two people who died while conducting rescues because of excessive work and heart failure.9 While we similarly estimated a substantial toll from accidental deaths (28 excess accidental deaths estimated for July 21–22), we also found an important increase in non-accidental mortality during the flood period, with 46 excess circulatory deaths estimated for July 21–22 (Table 1), an impact largely missed through the traditional surveillance method. The increased risk during the flood for circulatory deaths, and its associated impact, can be much more difficult to capture using the traditional disaster surveillance method than accidental deaths (e.g., drowning deaths). This is in part because circulatory deaths are not directly caused by the physical forces of the flood and in part because circulatory deaths are not rare outside of flood periods, making it harder to declare that a specific circulatory death would not have occurred without the flood.
The flood-related circulatory deaths we observed could have resulted in part from the flood disrupting health services through associated damage to infrastructure (such as transportation and communications). During this period in Beijing, many roads and bridges were flooded (about 63 main roads in Beijing),2 crowded with fallen building and trees, or destroyed.2 Infrastructure damage can prevent residents from reaching healthcare resources, which is especially dangerous among people with pre-existing chronic medical conditions, or hinder medical personnel from offering services.36–38 Beijing’s dense population and heavy reliance on public transportation make it particularly susceptible to these complications. In addition, flooding can be an emotional trigger that exacerbates the initiating process of acute cardiac events,39 an effect that has been identified for other types of disasters including earthquakes and human-caused disasters.40,41 Flood-related deaths from circulatory causes have also been reported in flood events in England,23 Bangladesh,42 and France,43 and a retrospective study of 1997 floods in the Czech Republic found the rates of cardiac-related mortality in the month of flood was more than twice the rate in the two previous months.21
Conversely, we did not find a short-term association between respiratory mortality and this flood. Studies have found the likelihood of indoor mold growth increases in months following major floods,44 and indoor dampness or mold has been shown to be consistently associated with respiratory problems.45 Thus, while we found no evidence of an association between this flood and immediate respiratory mortality rates, the flood might have increased risk of respiratory mortality at a longer period (e.g., months) than that investigated here. A few epidemiological studies have found increased longer-term risk of respiratory problems and infections among people in flood-affected areas.43,46,47 For example, in Bangladesh, about half of respondents (46.8%) in two affected districts reported developing or suffering exacerbation of respiratory problems in the two months following the 1998 flood,42 and approximately 13% of reported deaths from the country’s 1988 flood were attributed to respiratory disease.47 Further, six months after the 2004 floods in rural Bangladesh, a substantial increase in risk of acute respiratory infection (RR = 1.25, 95% CI, 1.06–1.47) was observed in flooded versus unflooded areas.20 Other health outcomes could also have increased risk in the weeks and months following the flood, given previous research indicating increased risk for health outcomes including psychological outcomes following major disasters, and these could be explored in future research focusing on health risks in the weeks and months following this severe flash flood.48,49
The increased mortality risks we identified occurred primarily on the peak flood day (July 21), with lower mortality risks on the following day and little or no evidence of elevated risks on the days following that (Figure 2). This pattern may, however, be specific to this Beijing flood, which varied in some key characteristics from other major floods that have been studied. Although this flood was extreme for Beijing (the heaviest rainfall in six decades), it resulted from an extreme precipitation event that was much shorter (< 24 hours) and had a much lower total rainfall than other major flood events like the two-month flooding in Bangladesh in 1998.42 Further, in the most affected districts of Beijing (e.g., Fangshan District), most residents were evacuated within a day,2 which may have helped prevent additional flood-related deaths on following days. Flood characteristics can be important in determining patterns in flood-associated health risks;43,50 future research could explore whether community-wide flood mortality risks, including patterns in lagged effects following the flood, can be partially explained by variation in factors like the duration of rainfall and the community’s emergency response measures. Finally, here we take an approach of modeling associations at a lag from a single peak flood day. While appropriate given the characteristics of this flood, this approach would be less appropriate for other types of flood events. For example, river floods can have a slow onset, building over many days, and can persist for days or weeks.5 In that case, continuing flooding would have lasting impacts on human health, thus modeling associations based on lag from a single peak flood may be ambiguous.
One limitation of this study is that we were unable to explore district-level mortality risks and impacts of this flood, as mortality data at the district level were not available. The intensity of this rainfall was heterogeneous across Beijing;4,8 for example, the average hourly precipitation on July 21–22 in the Fangshan District (in the southwest of Beijing) was 15.2 mm, while in the Huairou District (northeast of Beijing) it was 5.7 mm.8 Based on one of the studies that analyzed this event using a traditional disaster surveillance method,8 the amount of rainfall in a person’s neighborhood was found to be an important factor in the risks of flood-related mortality, a pattern we are unable to explore using city-level data. A second limitation stems from the difficulty of estimating increases in community-wide mortality rates compared to reference periods. However, we found our key conclusions (an approximately 30% increased risk in all-cause mortality associated with the flood, with important contributions from both circulatory and accidental deaths) were robust across several study designs considered, all of which compare mortality rates during the flood to different non-flood reference periods, adding weight to these conclusions, although choices among study design added some uncertainty to the exact quantitative estimates of risks and associated impacts, particularly for accidental mortality outcomes. Finally, while the sensitivity analysis suggested that the main results were not confounded by PM2.5, we were not able to test for potential confounding by another air pollutant, ground-level ozone, which can reach concentrations dangerous to human health in Beijing.51 Since the formation of ozone is a function of sunlight and temperature,52 its concentration was likely lower on the peak flood day, when torrential rainfall occurred, than on other summer days, and so failure to control for ozone pollution may bias our estimates towards the null if some of the unexposed days were characterized by high ozone levels. We lacked complete ozone data from 2012 and other study years to test for such confounding, but with the recent implementation of wide-scale ozone monitoring in China,51 future research on more recent flood events could investigate this.
Recent and expected climate trends make it critical to improve our understanding of the health risks associated with climate-related disasters, including floods, in order to mitigate the health impacts of future events. Our study city, Beijing, is located in the North China Plain, where although the amount and frequency of rainfall have decreased over the last decades,53 the intensity of heavy rainfall is projected to increase substantially over the next few decades.54 Although flood events as severe as the one investigated in this study have to date been rare in Beijing, floods of similar magnitude may be more common in the coming decades. Throughout China, most regions have experienced an increase in extreme rainfall events and are expected to experience an increased frequency of severe flood events through the end of the 21st century,53,54 as are many other locations worldwide (e.g., Europe and the Midwest and Northeast regions of the U.S.).55,56 This study, and similar studies estimating the community-wide change in mortality rates during flood events, can add to existing studies of flood-related mortality based on a traditional surveillance method to offer critical evidence in assessing flood-related health impacts and crafting strategies to limit or prevent flood-related deaths during future events.
Supplementary Material
Sources of financial support:
This research was supported by a R00ES022631 from National Institute of Environmental Health Science as well as grants from the National Natural Science Foundation of China (Grant: 21277135), Beijing Natural Science Foundation (7172145), and the National High-level Talents Special Support Plan of China for Young Talents.
Footnotes
Declaration of competing financial interests: None.
Data and code availability: Data used in this paper were obtained from Chinese Center of Disease Control and Prevention and Beijing Meteorological Bureau. Due to data protection regulations of these two agencies, data is not publicly available. Interested researchers can contact the authors for further details on accessing the data. All computing code used for this analysis is available at https://gitlab.com/MeilinYan/2012_flood_mortality_risk.
REFERENCES
- 1.Chen S, Liu H, You Y, et al. Evaluation of high-resolution precipitation estimates from satellites during July 2012 Beijing flood event using dense rain gauge observations. PLoS One 2014;9(4):e89681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang K, Wang L, Wei Y-M, Ye M. Beijing storm of July 21, 2012: Observations and reflections. Natural Hazards 2013;67(2):969–74. [Google Scholar]
- 3.Andrew Jacobs. Heavy Rains Blamed for at Least 37 Deaths in Beijing. The New York Times 2012. July https://www.nytimes.com/2012/07/23/world/asia/beijing-rains-leave-dozens-dead.html. Accessed 17 Sept 2019. [Google Scholar]
- 4.Hénonin J, Hongtao M, Zheng-Yu Y, et al. Citywide multi-grid urban flood modelling: the July 2012 flood in Beijing. Urban Water Journal 2015;12(1):52–66. [Google Scholar]
- 5.Doswell III CA. Flooding. Encyclopedia of Atmospheric Sciences 2003. Elsevier Science Ltd, Amsterdam. [Google Scholar]
- 6.Yin Z, Guo W, Li N, and Xie Y. Numerical Simulation of Urban Ponding in Beijing. Meteorological Monthly 2015;41(9):1111–1118. (In Chinese). [Google Scholar]
- 7.Zhen X, Tan Z. Beijing Flood Death Toll Hit 77. China Daily 2012. http://www.chinadaily.com.cn/china/2012-07/27/content_15622158.htm. Accessed 17 Sept 2019. [Google Scholar]
- 8.Liu J, Wang S-Y. Analysis of human vulnerability to the extreme rainfall event on 21–22 July 2012 in Beijing, China. Natural Hazards and Earth System Sciences 2013;13(11):2911–26. [Google Scholar]
- 9.Du W, FitzGerald G, Hou X-Y, Zhu W. A case study in flood fatality: Beijing July 2012 flood. 2013. Available from: http://eprints.qut.edu.au/76146/. Accessed 22 Jan 2019.
- 10.Rocha LA, Fromknecht CQ, Redman SD, Brady JE, Hodge SE, and Noe RS. Medicolegal death scene investigations after natural disaster-and weather-related events: A review of the literature.” Academic Forensic Pathology 2017;7(2): 221–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKinney N, Houser C, Meyer-Arendt K. Direct and indirect mortality in Florida during the 2004 hurricane season. International Journal of Biometeorology 2011;55(4):533–46. [DOI] [PubMed] [Google Scholar]
- 12.Naumann RB, Dellinger AM, Kresnow M-J. Driving self-restriction in high-risk conditions: How do older drivers compare to others? Journal of Safety Research 2011;42(1):67–71. [DOI] [PubMed] [Google Scholar]
- 13.Anderson GB, Bell ML. Heat waves in the United States: Mortality risk during heat waves and effect modification by heat wave characteristics in 43 US communities. Environmental Health Perspectives 2011;119(2):210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gasparrini A, Guo Y, Hashizume M, et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. The Lancet 2015;386(9991):369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ashley ST, Ashley WS. Flood fatalities in the United States. Journal of Applied Meteorology and Climatology 2008;47(3):805–18. [Google Scholar]
- 16.FitzGerald G, Du W, Jamal A, Clark M, Hou X-Y. Flood fatalities in contemporary Australia (1997–2008). Emergency Medicine Australasia 2010;22(2):180–6. [DOI] [PubMed] [Google Scholar]
- 17.Milojevic A, Armstrong B, Kovats S, et al. Long-term effects of flooding on mortality in England and Wales, 1994–2005: Controlled interrupted time-series analysis. Environmental Health 2011;10(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stephens KU, Grew D, Chin K, et al. Excess mortality in the aftermath of Hurricane Katrina: A preliminary report. Disaster Medicine and Public Health Preparedness 2007;1(1):15–20. [DOI] [PubMed] [Google Scholar]
- 19.Bennet G. Bristol floods 1968. Controlled survey of effects on health of local community disaster. British Medical Journal 1970;3(5720):454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milojevic A, Armstrong B, Hashizume M, et al. Health effects of flooding in rural Bangladesh. Epidemiology 2012;23(1):107–15. [DOI] [PubMed] [Google Scholar]
- 21.Obrová J, Sovová E, Ivanová K, Táborsky M, Loyka S. Effects of the July 1997 floods in the Czech Republic on cardiac mortality. Disaster Medicine and Public Health Preparedness 2014;8(6):492–6. [DOI] [PubMed] [Google Scholar]
- 22.Chae E-H, Kim TW, Rhee S-J, Henderson TD. The impact of flooding on the mental health of affected people in South Korea. Community Mental Health Journal 2005;41(6):633–45. [DOI] [PubMed] [Google Scholar]
- 23.Carroll B, Balogh R, Morbey H, Araoz G. Health and social impacts of a flood disaster: Responding to needs and implications for practice. Disasters 2010;34(4):1045–63. [DOI] [PubMed] [Google Scholar]
- 24.National Bureau of Statistics of China. National data [Internet]. 2016. [cited 2018 Jun 1];Available from: http://data.stats.gov.cn/english/easyquery.htm?cn=E0103. Accessed 22 Jan 2019
- 25.World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision [Internet]. World Health Organization; 2003. Available from: http://apps.who.int/classifications/apps/icd/icd10online2003/fr-icd.htm. Accessed 22 Jan 2019. [Google Scholar]
- 26.Schwartz J, Marcus A. Mortality and air pollution in London: a time series analysis. American Journal of Epidemiology 1990;131(1): 185–194. [DOI] [PubMed] [Google Scholar]
- 27.Levy D, Lumley T, Sheppard L, Kaufman J, Checkoway H. Referent selection in case-crossover analyses of acute health effects of air pollution. Epidemiology 2001;12(2): 186–192. [DOI] [PubMed] [Google Scholar]
- 28.Kishore N, Marqués D, Mahmud A, et al. Mortality in Puerto Rico after Hurricane Maria. New England Journal of Medicine 2018;379(2): 162–170. [DOI] [PubMed] [Google Scholar]
- 29.Bobb JF, Obermeyer Z, Wang Y, Dominici F. Cause-specific risk of hospital admission related to extreme heat in older adults. Journal of the American Medical Association 2014;312(24): 2659–2667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu JC, Wilson A, Mickley LJ, et al. Wildfire-specific fine particulate matter and risk of hospital admissions in urban and rural counties. Epidemiology 2017;28(1): 77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gasparrini A. Modeling exposure–lag–response associations with distributed lag non-linear models. Statistics in Medicine 2014;33(5):881–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Steenland K, Armstrong B. An overview of methods for calculating the burden of disease due to specific risk factors. Epidemiology 2006;17(5):512–9. [DOI] [PubMed] [Google Scholar]
- 33.Chen R, Yin P, Meng X, et al. “Fine particulate air pollution and daily mortality. A nationwide analysis in 272 Chinese cities.” American Journal of Respiratory and Critical Care Medicine 2017;196(1): 73–81. [DOI] [PubMed] [Google Scholar]
- 34.Choi Y, Ho C, Kim J, Gong D, Park RJ. “The impact of aerosols on the summer rainfall frequency in China.” Journal of Applied Meteorology and Climatology 2008;47(6): 1802–1813. [Google Scholar]
- 35.Armstrong BG, Gasparrini A, Tobias A. Conditional Poisson models: a flexible alternative to conditional logistic case cross-over analysis. BMC Medical Research Methodology 2014;14(1):122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Du W, FitzGerald GJ, Clark M, Hou X-Y. Health impacts of floods. Prehospital and Disaster Medicine 2010;25(3):265–72. [DOI] [PubMed] [Google Scholar]
- 37.Schatz JJ. Floods hamper health-care delivery in southern Africa. The Lancet 2008; 371(9615):799–800. [DOI] [PubMed] [Google Scholar]
- 38.Axelrod C, Killam PP, Gaston MH, Stinson N. Primary health care and the Midwest flood disaster. Public Health Reports 1994;109(5):601. [PMC free article] [PubMed] [Google Scholar]
- 39.Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nature Reviews Cardiology 2012;9(6):360. [DOI] [PubMed] [Google Scholar]
- 40.Leor J, Kloner RA. The Northridge earthquake as a trigger for acute myocardial infarction. American Journal of Cardiology 1996;77(14):1230–2. [DOI] [PubMed] [Google Scholar]
- 41.Steinberg JS, Arshad A, Kowalski M, et al. Increased incidence of life-threatening ventricular arrhythmias in implantable defibrillator patients after the World Trade Center attack. Journal of the American College of Cardiology 2004;44(6):1261–4. [DOI] [PubMed] [Google Scholar]
- 42.Kunii O, Nakamura S, Abdur R, Wakai S. The impact on health and risk factors of the diarrhoea epidemics in the 1998 Bangladesh floods. Public Health 2002;116(2):68–74. [DOI] [PubMed] [Google Scholar]
- 43.Ruin I, Creutin J-D, Anquetin S, Lutoff C. Human exposure to flash floods—Relation between flood parameters and human vulnerability during a storm of September 2002 in Southern France. Journal of Hydrology 2008;361(1–2):199–213. [Google Scholar]
- 44.Barbeau DN, Grimsley LF, White LE, El-Dahr JM, Lichtveld M. Mold exposure and health effects following Hurricanes Katrina and Rita. Annual Review of Public Health 2010;31:165–78. [DOI] [PubMed] [Google Scholar]
- 45.Mendell MJ, Mirer AG, Cheung K, Douwes J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: A review of the epidemiologic evidence. Environmental Health Perspectives 2011;119(6):748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Biswas R, Pal D, Mukhopadhyay S. A community-based study on health impact of flood in a vulnerable district of West Bengal. Indian Journal of Public Health 1999;43(2):89–90. [PubMed] [Google Scholar]
- 47.Siddique A, Baqui A, Eusof A, Zaman K. 1988 floods in Bangladesh: Pattern of illness and causes of death. Journal of Diarrhoeal Diseases Research 1991;310–4. [PubMed] [Google Scholar]
- 48.Ahern M, Kovats RS, Wilkinson P, Few R, & Matthies F. Global health impacts of floods: epidemiologic evidence. Epidemiologic Reviews 2005;27(1):36–46. [DOI] [PubMed] [Google Scholar]
- 49.Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiologic Reviews 2005;27(1):78–91. [DOI] [PubMed] [Google Scholar]
- 50.Jonkman SN, Maaskant B, Boyd E, Levitan ML. Loss of life caused by the flooding of New Orleans after Hurricane Katrina: Analysis of the relationship between flood characteristics and mortality. Risk Analysis 2009;29(5):676–98. [DOI] [PubMed] [Google Scholar]
- 51.Lu X, Hong J, Zhang L, et al. Severe surface ozone pollution in China: A global perspective. Environmental Science & Technology Letters 2018;5(8): 487–494. [Google Scholar]
- 52.Stathopoulou E, Mihalakakou G, Santamouris M, Bagiorgas HS. On the impact of temperature on tropospheric ozone concentration levels in urban environments. Journal of Earth System Science 2008;117(3):227–36. [Google Scholar]
- 53.Fu G, Yu J, Yu X, et al. Temporal variation of extreme rainfall events in China, 1961–2009. Journal of Hydrology 2013;487:48–59. [Google Scholar]
- 54.Chen H, Sun J, Chen X. Future changes of drought and flood events in China under a global warming scenario. Atmospheric and Oceanic Science Letters 2013;6(1):8–13. [Google Scholar]
- 55.Alfieri L, Feyen L, Dottori F, Bianchi A. Ensemble flood risk assessment in Europe under high end climate scenarios. Global Environmental Change 2015;35:199–212. [Google Scholar]
- 56.Melillo JM, Richmond T, Yohe GW, Eds. Highlights of climate change impacts in the United States: The Third National Climate Assessment [Internet] U.S. Global Change Research Program; 2014. Available from: http://s3.amazonaws.com/nca2014/high/NCA3_Highlights_HighRes.pdf?download=1. Accessed 22 Jan 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.