Abstract
Humankind has somewhat of a dark, yet almost fascinating, supernatural relationship with rabies. Even after Pasteur's rabies vaccine discovery, globally people continue to be stricken with it today. History has carried along the myths and legends that surround this diabolical virus. Some still believe that rabies treatment requires 20 or more shots to the stomach by some monstrously long needle. However, today's treatment regimen is typically only four vaccinations (five for immunocompromised) in the arm, plus human rabies immune globulin. This chapter explores the misunderstood concepts of rabies prevalence, signs and symptoms, exposures, and treatment protocols.
Keywords: Lyssavirus, Rabies, Rabies legends, Rabies myths, Rabies virus variants, Rhabdoviridae
Introduction
Rabies has been a part of human history for as long as it has been recorded in writing and art. From Odysseus’s story to Achilles, the actual word (term) that provoked and transformed Hector to a rage and frenzy, “lyssa,” is closely linked to the word “lykos” or “wolf” and is used to invoke images and feelings of an animal’s anger, madness, and wolfish rage.1 Lyssavirus is a genus of RNA viruses in the family Rhabdoviridae, order Mononegavirales. Lyssaviruses are bullet-shaped, single-stranded, negative-sense RNA viruses and the causative agents of the ancient zoonosis rabies. Africa is the likely home to the ancestors of taxa residing within the genus Lyssavirus, family Rhabdoviridae. Diverse lyssaviruses are envisioned as coevolving with bats, as the ultimate reservoirs, over seemingly millions of years (Fig. 5.1 ).2
Fig. 5.1.

A woodcut from the middle ages showing a rabid dog.
Reprinted with permission by source, fair use: https://en.wikipedia.org/wiki/Rabies#/media/File:Middle_Ages_rabid_dog.jpg.
Through eons of time, a wide range of myths and legends have developed pertaining to rabies. Many people still believe today that rabies treatment requires 20 or more shots into the stomach by some monstrously long needle. While in fact, today’s treatment regimen is typically only four vaccinations (five for immunocompromised individuals) in the arm, plus a dose of humane rabies immune globulin (HRIG). This myth is but one of a long list of questions, untruths, or exaggerations about the disease known as rabies.
-
•
Is there a way to vaccinate wildlife using a recombinant vaccine dropped from aircraft?3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14
-
•
Can scientists actually determine the origin of a rabies virus variant by way of genetic testing and methodologies?3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14
-
•
Are there special government laboratories that conduct specialized rabies testing?3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14
-
•
Can international public health teams actually halt and remove a moving viral epizootic outbreak in a geographical area?3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14
-
•
Is there a relationship between rabies and zombies?15
In this chapter, some of the more common misconceptions (and facts) about rabies will be described. These misconceptions are categorized under concepts of prevalence, signs and symptoms, exposure, treatment, and pop culture influence with respect to rabies.
Misunderstood Concepts of the Prevalence of Rabies
Where exactly do most cases of rabies occur in the world? Which type of animals are often more “at risk” for contracting rabies virus, otherwise known as high-risk animals? Are there places in the world where one might travel without worrying about rabies? Do cold-blooded animals, insects, or birds have a risk for acquiring this deadly disease? There are many untruths to unpack with respect to the prevalence of rabies. Learn more in the following accounts:
-
•
Many people believe that rabies infections only occur in poor, third-world countries. However, the truth is that rabies or rabies-like viruses are present on nearly every continent, with the exception of Antarctica. Numerous and diverse variants of lyssaviruses are found in a wide variety of animal species throughout the world, all of which may cause fatal human rabies. Rabies virus is by far the most common lyssavirus infection of humans. In the United States, only Hawaii is rabies free. Interestingly, in Hawaii and other rabies-free areas that are often islands, there are very strict laws and restrictions on the transport of animals from rabies-endemic states or countries to rabies-free geographic locations. In the United States, rabies as a disease is most prevalent along the East Coast (raccoon and bat rabies virus variants) from Florida to Maine and in Southern Arizona (Arizona gray fox) along the Mexican border. Rabies is also prevalent in Texas with south central skunk and bat rabies virus variants predominating.
As a side note, one should always consider the risk of infectious disease when traveling to other countries by discussing travel plans with an appropriate person such as a travel physician or other health-care professional. There may be a need to plan for preexposure vaccinations (e.g., rabies, yellow fever, etc.) or medications (e.g., malaria, antibiotics) to take on their travels.16
-
•
A frequent belief is that this disease kills many people in the United States. However, approximately 95% of human deaths from the disease occur in Africa and Asia, where access to health-care facilities and treatment protocols is limited. The estimated annual figure of almost 59,000 rabies fatalities in humans is probably an underestimate. Almost all cases of rabies in humans worldwide result from bites from infected dogs.17, 18 Rabies cases in humans in the United States are rare, with only one to three cases reported annually. Forty three cases of rabies in humans have been reported in the United States and its territories from January 2003 through November 2018 (Table 5.1). Almost all of the cases are attributed to bat rabies with 11 of the total cases contracted outside of the United States and its territories. Of the 43 rabies cases, there were three survivors (40 deaths). For 2018, there have been three cases, with the most recent case (death) being a 74-year-old male from Utah from bat rabies (not included in Table 1).19
-
•
All warm-blooded animals can contract rabies, particularly mammals. A viral disease of the central nervous system, rabies transmits between animals, including humans, when saliva containing the virus enters an opening in the skin. Usually, the rabies virus enters through the bite of a rabid animal, but transmission can also occur when infected saliva enters through mucous membranes or a break in the skin. Viral familial relatives can be found with invertebrates and plants (distant hosts), but warm-blooded vertebrates are the hosts for the rabies virus. Among warm-blooded vertebrates, birds are susceptible to infection, but rabies predominates naturally among various mammalian populations. Only rare accounts occur in nonmammalian hosts, but in the Mammalia family, rabies cases have occurred from the armadillo to the zebra. Rabies is a significant disease of domestic and wild mammals alike, yet its zoonotic aspect is the cause of major historical infamy.2
Table 5.1.
| Date of onset | Date of death | Reporting state | Age (y) | Sex | Exposure∗ | RW† |
|---|---|---|---|---|---|---|
| 10 Feb 03 | 10 Mar 03 | VA | 25 | M | Unknown | Raccoon, eastern United States |
| 28 May 03 | 5 Jun 03 | PR | 64 | M | Bite, Puerto Rico | Dog-mongoose, Puerto Rico |
| 23 Aug 03 | 14 Sep 03 | CA | 66 | M | Bite | Bat. Ln |
| 9 Feb 04 | 15 Feb 04 | FL | 41 | M | Bite. Haiti | Dog, Haiti |
| 27 Apr 04 | 3 May 04 | AR | 20 | M | Bite (organ donor) | Bat. Tb |
| 25 May 04 | 31 May 04 | OK | 53 | M | Liver transplant | Bat. Tb |
| 27 May 04 | 21 Jun 04 | TX | 18 | M | Kidney transplant | Bat. Tb |
| 29 May 04 | 9 Jun 04 | TX | 50 | F | Kidney transplant | Bat. Tb |
| 2 Jun 04 | 10 Jun 04 | TX | 55 | F | Arterial transplant | Bat. Tb |
| 12 Oct 04 | Survived | WI | 15 | F | Bite | Bat, unknown |
| 19 Oct 04 | 26 Oct 04 | CA | 22 | M | Unknown. El Salvador | Dog. El Salvador |
| 27 Sep 05 | 27 Sep 05 | MS | 10 | M | Contact | Bat. unknown |
| 4 May 06 | 12 May 06 | TX | 16 | M | Contact | Bat. Tb |
| 30 Sep 06 | 2 Nov 06 | IN | 10 | F | Bite | Bat. Ln |
| 15 Nov 06 | 14 Dec 06 | CA | II | M | Bite, Philippines | Dog, Philippines |
| 19 Sep 07 | 20 Oct 07 | MN | 46 | M | Bite | Bat. unknown |
| 16 Mar 08 | 18 Mar 08 | CA | 16 | M | Bite. Mexico | Fox. Tb related |
| 19 Nov 08 | 30 Nov 08 | MO | 55 | M | Bite | Bat. Ln |
| 25 Feb 09 | Survived | TX | 17 | F | Contact | Bat. unknown |
| 5 Oct 09 | 20 Oct 09 | IN | 43 | M | Unknown | Bat. Ps |
| 20 Oct 09 | II Nov 09 | Ml | 55 | M | Contact | Bat, Ln |
| 23 Oct 09 | 20 Nov 09 | VA | 42 | M | Contact. India | Dog. India |
| 2 Aug 10 | 21 Aug 10 | LA | 19 | M | Bite, Mexico | Bat, Dr |
| 24 Dec 10 | 10 Jan 11 | WI | 70 | M | Unknown | Bat. Ps |
| 30 Apr II | Survived | CA | 8 | F | Unknown | Unknown |
| 30 Jun II | 20 Jul II | NJ | 73 | F | Bite. Haiti | Dog, Haiti |
| 14 Aug II | 31 Aug II | NY | 25 | M | Contact, Afghanistan | Dog, Afghanistan |
| 21 Aug II | 1 Sep 11 | NC | 20 | M | Unknown (organ donor)‡ | Raccoon, eastern United States |
| 1 Sep II | 14 Oct II | MA | 40 | M | Contact, Brazil | Dog, Brazil |
| 3 Dec II | 19 Dec II | SC | 46 | F | Unknown | Bat. Tb |
| 22 Dec II | 23 Jan 12 | MA | 63 | M | Contact | Bat, My sp |
| 6 Jul 12 | 31 Jul 12 | CA | 34 | M | Bite | Bat. Tb |
| 31 Jan 13 | 27 Feb 13 | MD | 49 | M | Kidney transplant | Raccoon, eastern United States |
| 16 May 13 | 11 Jun 13 | TX | 28 | M | Unknown, Guatemala | Dog, Guatemala |
| 12 Sep 14 | 26 Sep 14 | MO | 52 | M | Unknown | Bat. Ps |
| 30 Jul 15 | 24 Aug 15 | MA | 65 | M | Bite, Philippines | Dog, Philippines |
| 17 Sep 15 | 3 Oct 15 | WY | 77 | F | Contact | Bat. Ln |
| 25 Nov 15 | 1 Dec 15 | PR | 54 | M | Bite | Dog-mongoose, Puerto Rico |
| 5 May 17 | 21 May 17 | VA | 65 | F | Bite | Dog, India |
| 6 Oct 17 | 21 Oct 17 | FL | 56 | F | Bite | Bat. Tb |
| 28 Dec 17 | 14 Jan 18 | FL | 6 | M | Bite | Bat. Tb |
| 15 Jul 18 | 23 Aug 18 | DE | 69 | F | Unknown | Raccoon, eastern United States |
Dr = D rotundus. Ln = L noctivagans. My sp = Myotis species. Ps = P subflavus. Tb = T brasiliensis.
Data for exposure history are reported when plausible information was reported directly by the patient (if lucid or credible) or when a reliable account of an incident consistent with rabies virus exposure (eg, dog bite) was reported by an independent witness (usually a family member). Exposure histories are categorized as bite, contact (eg, waking to find bat on exposed skin) but no known bite was acknowledged, or unknown (ie, no known contact with an animal was elicited during case investigation). †Variants of the rabies virus associated with terrestrial animals in the United States and Puerto Rico are identified with the names of the reservoir animal (eg, dog or raccoon), followed by the name of the most definitive geographic entity (usually the country) from which the variant has been identified. Variants of the rabies virus associated with bats are identified with the names of the species of bats in which they have been found to be circulating. Because information regarding the location of the exposure and the identity of the exposing animal is almost always retrospective and much information is frequently unavailable, the location of the exposure and the identity of the animal responsible for the infection are often limited to deduction. ‡Infection was not identified until 2013. when an organ recipient developed rabies.19
Misunderstood Concepts on Clinical Signs and Symptoms of Rabies
According to the Centers for Disease Control and Prevention (CDC), the first clinical signs and symptoms of rabies may be very similar to those of the flu including general weakness or discomfort, fever, or headache. These clinical signs and symptoms may last for days and are directly related to the difficulty of a differential diagnosis of rabies in the absence of an obvious animal bite (or other) exposure.
There may be also discomfort or a prickling or itching sensation at the site of bite, progressing within days to signs and symptoms of cerebral dysfunction, anxiety, confusion, and agitation. As the disease progresses, the person may experience delirium, abnormal behavior, hallucinations, and insomnia. The acute period of disease typically ends after 2–10 days20 (see Chapter 2). Once clinical signs of rabies appear, the disease is nearly always fatal, and treatment is typically supportive. Disease prevention includes both passive immunity, through an injection of human rabies immune globulin, and active immunity produced via a round of injections with rabies vaccine. If a person has already begun to exhibit signs of the disease, survival is rare. To date, less than 10 documented cases of human survival from clinical rabies have been reported and only two have not had a history of pre- or postexposure prophylaxis.20
One of the more bizarre, but not uncommon, signs and symptoms of rabies that has been reported is male patients exhibiting hypersexual behavior. The virus sometimes acts on the limbic system of the brain causing men to show this behavior: increased sexual desire, involuntary erections, and in some reports continuous orgasms occurring at a rate of one per hour!1
In general, most people think of dogs when the topic of animals that can carry or transmit rabies is mentioned. This may be due to the long-standing fascination with the popular media (and ancient writings) that target the canine as the primary vector for rabies. For example, if you have seen the movie Old Yeller or Cujo, then you probably understand how the popular media can influence the public to fear rabies and scrutinize the family dog for any signs of “frothing or foaming” at the mouth.1 However, the disease affects both domestic and wild animals. Early clinical signs of the illness include fever, pain, and/or a tingling sensation around the wound.17 However, unlike the popular notion of Old Yeller or Cujo, the most typical clinical signs of rabies are unexplained paralysis and a change in behavior (refer to Chapter 2 for details). Still, there are many reports of other strange clinical behaviors by a rabid animal.21, 22
Misunderstood Concepts of What Classifies as an Exposure to Rabies
One of the difficult decisions about rabies, if not the most difficult, is “what constitutes an exposure” when trying to discern whether to treat or not to treat an individual. Likewise, there are important implications for the animal (domestic). For example, whether to quarantine the animal for observation or to euthanize an animal followed by laboratory testing for confirmation of rabies. The World Health Organization (WHO) has recommendations intended as a general guide.23 It is recognized that, in certain situations, modifications of these procedures are warranted. Such situations include exposure of infants or mentally disabled persons and other circumstances where a reliable history cannot be obtained, particularly in areas where rabies is enzootic, even though the animal is considered to be healthy at the time of exposure.
There are other myths and legends surrounding the question of a true rabies exposure. The following are a few of the common ones:
-
•
On a given warm summer evening in areas of Texas just as dark approaches, bats start swooping in their feeding mode of eating insects, which is an ecologic and biologic benefit. This could initiate a warning from some folks about “bats getting tangled in your hair,” leading to being exposed to rabies. Of course, bats are not attracted to a person’s head of hair and do not try to “nest” there, but if a bat did get tangled in someone’s hair, they would receive PEP if the bat could not be tested as its too close a contact to rule out a bite occurring. However, contributing to this misconception could be media and historical writings with respect to vampire lore surrounding bats.1 Additionally, there were even popular television series like The Andy Griffith Show that had an episode with Barney Fife discussing bats in caves and their potential for laying “their eggs” in a person’s hair (Fig. 5.2 ).24
-
•
Can I get rabies if I handle blood, feces, or urine? The simple answer is no in this scenario. Rabies is not transmitted through the blood, urine, or feces of an infected animal, nor is it spread airborne through the open environment. Saliva provides the primary transmission medium when the animal is in the infectious stage of rabies. For the rabies virus to get to the salivary glands, it has to travel first from the site of entry (usually a bite wound) through the animal’s nervous system, then to the brain. This is what causes most rabid animals to exhibit abnormal behaviors, depending on what part of the brain is infected. Finally, the virus travels to the salivary glands during the terminal stage of rabies. It is this later stage of rabies when an animal is most infectious because the virus is in the saliva.21, 22, 25
Fig. 5.2.

Flying bats: this horde of flying bats could contain possible carriers of the rabies virus.
Reprinted with permission by source, fair use: Centers for Disease Control and Prevention (Public Health Image Library).
Misunderstood Concepts on Rabies Postexposure Prophylaxis and Treatment Protocols
Treatment for rabies, one of the world’s most diabolical viruses, has a long history of creative and bizarre origins. Rabies is a terrifying disease that dates as far back as the beginnings of humankind. In a sense, we humans fear rabies because it crosses the line between humanity and animal. Think about it, the disease is at the intersection of humans and animals. Somewhere deep in the psyche, one can become terrified by the thought of a bite from a rabid animal because it symbolizes the very metamorphosis of a human becoming that very rabid animal—a vampire or werewolf if you let your brain take you to that place.1
It should not be a surprise that humans have a longstanding and deep-seated fear of diseases with animal origins, or as science calls them, zoonotic diseases. A majority of new diseases are zoonotic. For example, swine flu, West Nile virus, anthrax, severe acute respiratory syndrome, tuberculosis, influenza, Ebola, nipah, powassan, and plague represent diseases from a wide range of eras. It is not a far reach to realize that the collective conscience of the general public has been swayed and biased by diseases with animal origins.1 So, along with that understanding comes an almost guttural need to find ways to treat or cure those diseases. This is where some of the earliest misconceptions for treating rabies originate in our history. Let us examine some of those treatments that seem to perpetuate in time regardless of the modern advances in medicine.
-
•
In many of the earliest recordings of the disease, the treatments centered on the wound. This makes sense when you consider that humans from early in history understood that the origin of rabies manifested in humans after a canid bite, often while the animal was drooling copious amounts of saliva (frothing at the mouth). Without listing every single early thought on treatment of these wounds, the common thread is to “bleed and cauterize (burn) the wound.” For example, in early traditional Indian medicine, there is acknowledgment of the fatality of hydrophobia (fear of water in rabies patients) and a prescription of treatment for it—bleeding and cauterization of the wound. The process involved cauterizing the wound with clarified butter, which the patient is then asked to drink.1 It is accepted even today that after an animal bite, it is wise to let it bleed, followed by rigorous washing and flushing of the wound with soap and water. However, simply closing the wound or cauterizing it will not cure one from rabies.
-
•
Interestingly, the very pathogenesis of rabies in how it takes the central nervous system hostage to spread its deadly virions is now being studied to treat and possibly cure disease in brain cancer patients. The rabies virus, which kills tens of thousands of people a year, has a rare ability to enter nerve cells and use them as a conduit to infect brain tissue. Now, scientists are trying to mimic this strategy to ferry tumor-killing nanoparticles into brain tumors. In laymen’s terms, this means using viruses to carry tiny cancer killing agents to the tumor. So far, the approach has been shown to work only in mice. If successful in people, these nanoparticles could one day help doctors send treatment directly to tumors without harming healthy cells.26
-
•
Alarmingly, homeopathic and neuropathic treatments have gained some traction in the world in a variety of applications for mild to deadly diseases. Rabies is not immune to these “treatments.” While there is truth that some modern day medicines and drugs come from nature (e.g., penicillin is derived from the fungus Penicillium), in most instances it does not replace peer-reviewed and sound clinical trial-based medical treatments or procedures. Homeopathy principles roughly state that substances that produce similar symptoms of a particular ailment can cure said ailment (“like cures like”) and that diluting a substance increases its potency (“law of infinitesimals”), which brings to mind the “hair of the dog” remedy for some hangover sufferers. Recently, there was a report in which diluted saliva from a rabid dog was used to “treat” a 4-year-old boy for aggressive behavior. The first question that comes to mind is “where did the United Kingdom homeopathic pharmacy obtain rabid dog saliva?” Regardless, the rabid dog treatment, called lyssinum (aka lyssin or hydrophobinum), is one of more than 8500 homeopathic products approved by Health Canada. There is cause for concern, including those at the US Food and Drug Administration, that such homeopathic products can be harmful and/or delay actual medical interventions and treatments. The homeopath who administered the treatment admitted that “there is no common consensus about how the remedies work” and continued to claim that it was effective and safe, plus added that the saliva was diluted to the point that it would not contain any trace of rabies virus. Most rabies experts would have concerns about this treatment.27
-
•In an earlier section of this chapter, it was mentioned that some individuals (including some in health care or other biological science majors or backgrounds) incorrectly believe that rabies treatment requires 20 or more shots into the stomach by some monstrously long needle. Actually, almost all modern treatment regimens for rabies include four key features:
-
•Generous cleaning and lavage of the bite wound with soap or topical antiseptic and warm water.
-
•Avoidance of wound repair. Closed bite wounds from dogs (or other animals) often become bacterially infected with early closure. The recommendation is to use very few sutures early and wait 7–14 days to more definitively close the wound.2 Additionally, tetanus immunization boosters are indicated.
-
•Human rabies immune globulin (HRIG) is essential for bridging immunity until the response to rabies vaccination occurs 10–14 days later. The HRIG is most effective when infiltrated in the wound and not intramuscularly (IM) remote from the bite wound.
-
•Rabies vaccine should be a modern cell-based, inactivated vaccine. Rabies vaccine is effective when given intradermally or IM, although only the latter route is licensed in the United States. The WHO recommends several schemata for rabies immunization. In the United States, only four doses (from the original five) are now recommended (0, 3, 7, and 14 days) because an immune response is invariably present by day 14.28 However, a fifth dose is still recommended on day 28 for individuals who are immunocompromised.2
-
•
Simply put, rabies usually kills its victims without early intervention. With the recent and increased attention from stories of survivors of rabies, there have been recent reports from India of natural survivors, but most often with poor functional outcomes.29, 30 The exciting new Milwaukee Protocol and its use globally has produced four survivors who have had excellent cognitive recovery and outcomes. However, two had spastic diplegia that has been described in animal survivor models of rabies.31
Influence of Rabies on Pop Culture
It really should not be a surprise that rabies, a disease that goes back to the dawn of human civilization, continues to influence our pop culture (movies, television, art and literature, and tales told over generations). Perhaps it is because rabies has always been known to be the very transformation of a disease from animal to man that is easily observed. The CDC estimates that zoonotic diseases are very common, both in America and globally. They estimate that more than 6 out of every 10 known infectious diseases in people are derived from animals and 3 out of every 4 new or emerging infectious diseases in people are transmitted from animals.32
Historically, humans just did not see the connection of infectious disease to animals. Scientists and scholars blamed nearly everything but animals. Even some of the nastiest culprits of disease like smallpox (albeit this infection is not zoonotic) or Black Death (bubonic plague), which spreads to humans via respiratory droplets or by way of hitching a ride on a rat or other rodents via a flea vector, were often misunderstood regarding transmission or cause. Usually, this meant that things such as demons, bad air (literal meaning of malaria), heavenly bodies/stars, and even human behavior were the root of disease. Almost all of them were blamed on nonhuman hosts, except for rabies and anthrax. Regardless of how far one goes back in time, one did not need to look further than the consequences of what happened after a human was bitten by a “mad dog” or other animal. In addition, to add insult to injury (literally), it was often the owner’s very own best friend—the dog.1
If one looks to the time of Greek myth, we find Lycaon, king of Arcadia, transforming into a slavering wolf with rabid and foamy jaws. In fifteenth century Spain, we read about witch-hunters called saludadores and they were known as healers of rabies. During the interim of the 15th and 18th centuries, our European counterparts were building two well-known legends—the werewolf and vampire—which had the ability to be human and animal and pass on this ability via the bite. Even as we approach the 19th century with viruses becoming more understood by science and the discovery of Pasteur’s rabies vaccine, people of France were still transfixed and terrified by the fantasy and horror that a rabies infection converted people into maddened animals. Ironically, their horror (fantasy) had some foundation.1
Even after Pasteur’s vaccine, which miraculously could save one from certain death by rabies if given prior to signs and symptoms, humankind’s ongoing rabid fantasy about possible monster metamorphoses with rabies continues in the pop culture and is going strong to this day. One needs to look no further than even possibly American’s most trusted media icon, Walt Disney, when he released Old Yeller or about 24 years later when the novel Cujo (and later film) transfixed audiences to fear rabies (Fig. 5.3, Fig. 5.4 ).
Fig. 5.3.
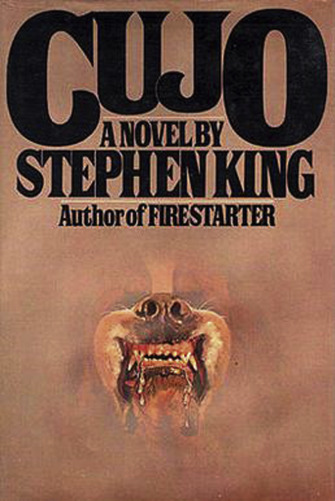
Cujo book cover.
Reprinted with permission by source, fair use: https://en.wikipedia.org/wiki/Cujo#/media/File:Cujo_(book_cover).jpg.
Fig. 5.4.
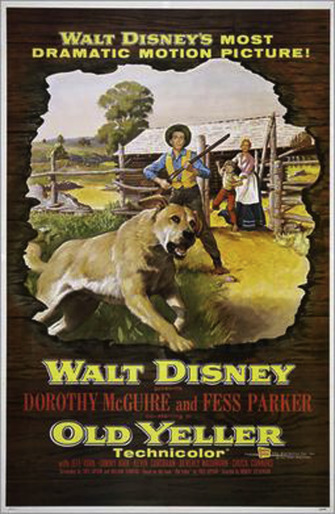
Old Yeller movie poster.
Reprinted with permission by source, fair use: https://en.wikipedia.org/w/index.php?curid=41973841.
Vampire movie after vampire movie arrived followed by zombie movies (I Am Legend, World War Z, etc.) and the more current television series (The Walking Dead, Fear the Walking Dead, etc.) (Fig. 5.5 ).
Fig. 5.5.
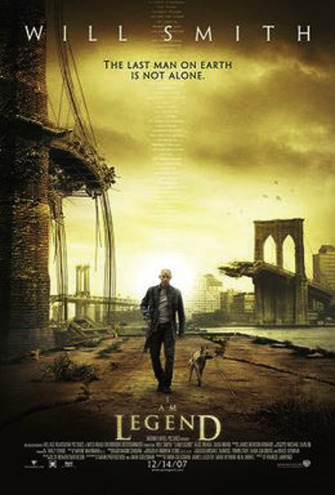
I Am Legend movie teaser poster.
Reprinted with permission by source, fair use: https://en.wikipedia.org/w/index.php?curid=11659226.
Rabies even shows up in our comedy with appearances in shows like King of the Hill and Beavis and Butt-Head, as well as in an episode of The Office. In the popular Seinfeld episode—classic TV—one of the main characters, Elaine, gets bitten by a dog, the owner evades her, she has to get PEP (the doctor tells her the shot will hurt very much), and she keeps thinking she is showing signs of rabies (spitting back water, frothing at the mouth, etc.).1 It seems that rabies will always have a place in shaping pop culture, especially in the realm of the horror and science fiction genre. One can assume that because of this ongoing fascination with rabies in the arts and in our passing on of stories, often handing them down from one generation to the next, that we will continue to be fed misconceptions (although often based on science) about this diabolical virus known as rabies.
Conclusions
It is incumbent for all of us in the modern era to dispel these myths and legends so that we can move forward in our efforts to assist humankind and downplay the sometimes-misguided fascination with this ongoing threat. Realistically, those in the rabies medical, public health, and research community have a long way to go for increased disease survivorship and increased health literacy between health-care professionals and the public. To give just one example about our need to learn and communicate in the world of rabies, one needs to look no further than the variances in virulence and possible better outcomes from rabies virus variant phylogeny differences—the reasons for the overrepresentation of the silver-haired bat, Lasionycteris noctivagans (Fig. 5.6 ) rabies virus variant in human infections are unclear. The frequency of infection, shedding, and dissemination of rabies virus in L. noctivagans, compared with Myotis lucifugus and Eptesicus fuscus, suggests the discrepancy of human rabies cases may be due to increased infectivity in heterospecific hosts, human susceptibility, and/or behavioral factors.33 In the interim, misconceived notions will most likely continue to be generated regarding the prevalence, signs and symptoms, diagnosis, and treatment protocols pertaining to this notorious and ancient killer known as rabies. It is incumbent upon all of us to be better stewards in the art of science communication with respect to decreasing the misunderstanding and sometimes panic surrounding this ancient disease.
Fig. 5.6.

A silver-haired bat, the type that has been responsible for numerous human rabies cases and deaths.
Reprinted with pemission by source, fair use: https://commons.wikimedia.org/wiki/File:Silver-haired_bat.JPG.
References
- 1.Wasik B., Rabid M.M. Penguin Books; New York, NY: 2012. A Cultural History of the World’s Most Diabolical Virus. [Google Scholar]
- 2.Rupprecht C., Kuzmin I., Meslin F. Lyssaviruses and rabies: current conundrums, concerns, contradictions and controversies. F1000Res. 2017;6:184. doi: 10.12688/f1000research.10416.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finley D. Texas A&M University Press; College Station, TX: 1998. Mad Dogs: The New Rabies Plague. [Google Scholar]
- 4.Rohde R.E., Neill S.U., Clark K.A. Molecular epidemiology of rabies epizootics in Texas. J Clin Virol. 1997;8:209–217. doi: 10.1016/s0928-0197(97)10003-4. [DOI] [PubMed] [Google Scholar]
- 5.Sabouraud A., Smith J.S., Orciari L.A. Typing of rabies virus isolates by DNA enzyme immunoassay. J Clin Virol. 1999;12:9–19. doi: 10.1016/s1386-6532(98)00006-7. [DOI] [PubMed] [Google Scholar]
- 6.Rohde R.E., Wilson P.J., Mayes B.C. 2004. Rabies: methods and Guidelines for Assessing a Clinical Rarity. pp. 21–29. (ASCP Microbio No. MB-4 Tech Sample). [Google Scholar]
- 7.Rohde R.E., Mayes B.C., Smith J.S. Bat rabies, Texas, 1996–2000. Emerg Infect Dis. 2004;10(5):948–952. doi: 10.3201/eid1005.030719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sidwa T., Wilson P.J., Moore G. Evaluation of oral rabies vaccination programs for control of rabies epizootics in coyotes and gray foxes: 1995–2003. JAVMA. 2005;227(5):785–792. doi: 10.2460/javma.2005.227.785. [DOI] [PubMed] [Google Scholar]
- 9.Leslie M.J., Messenger S., Rohde R.E. Bat-associated rabies virus in skunks. Emerg Infect Dis. 2006;12(8):1274–1277. doi: 10.3201/eid1208.051526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rohde R.E. Rabies: an old disease for a new generation. ASCLS Today Newsl. 2007;21(8):14–15. [Google Scholar]
- 11.Rohde R.E. Controlling rabies at its source: the Texas experience – oral rabies vaccination program. ASCLS Today. 2008;22(5):14–15. [Google Scholar]
- 12.Oertli E.H., Wilson P.J., Hunt P.R. Rabies in skunks in Texas. JAVMA. 2009;234(5):1–5. doi: 10.2460/javma.234.5.616. [DOI] [PubMed] [Google Scholar]
- 13.Mayes B.C., Wilson P.J., Oertli E.H. Epidemiology of rabies in bats in Texas, 2001–2010. JAVMA. 2013;243(8):1129–1137. doi: 10.2460/javma.243.8.1129. [DOI] [PubMed] [Google Scholar]
- 14.Rohde R.E., Mayes B.C. Molecular diagnosis and epidemiology of rabies. In: Hu P., Hedge M., Lennon P.A., editors. Modern Clinical Molecular Techniques. Springer Press; New York: 2012. pp. 199–211. [Google Scholar]
- 15.Rohde R.E. 2018. Invited Interview for Outbreak News Today Radio Podcast – Rabies: History, Myths and Diagnosis on Outbreak News This Week.http://outbreaknewstoday.com/rabies-history-myths-and-diagnosis-on-outbreak-news-this-week-96853/ [Google Scholar]
- 16.Centers for Diseases Control and Prevention – Explore Travel Health With the CDC Yellow Book. Petersen BW, Wallace RM, Shlim DR. Chapter 3 – Infectious diseases related to travel: rabies. https://wwwnc.cdc.gov/travel/yellowbook/2018/infectious-diseases-related-to-travel/rabies.
- 17.Haugh L. 15 Obscure and Little Known Facts About Rabies. https://guardianlv.com/2016/06/obscure-and-little-known-facts-about-rabies/.
- 18.Fooks A.R., Banyard A.C., Horton D.L. Current status of rabies and prospects for elimination. Lancet. 2014;384:1389–1399. doi: 10.1016/S0140-6736(13)62707-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma X., Monroe B.P., Cleaton J.M. Rabies surveillance in the United States during 2017. JAVMA. 2018;253(12):1555–1568. doi: 10.2460/javma.253.12.1555. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. What are the Signs and Symptoms of Rabies? https://www.cdc.gov/rabies/symptoms/index.html.
- 21.Wilson P.J., Rohde R.E. Elsevier Connect; 2016. The Many Faces of Rabies.htpps://www.elsevier.com/connect/the-many-faces-of-rabies [Google Scholar]
- 22.Wilson P.J., Rohde R.E. Elsevier Connect; 2015. 8 Things You May Not Know About Rabies – But Should.https://www.elsevier.com/connect/8-things-you-may-not-know-about-rabies-but-should [Google Scholar]
- 23.World Health Organization. Rabies – Guide for Post-exposure Prophylaxis. http://www.who.int/rabies/human/postexp/en/.
- 24.Barney Fife – Bat eggs. https://www.youtube.com/watch?v=lrb3zoeKiGM.
- 25.911Wildlife. Common Misconceptions About Rabies. http://www.911wildlife.com/animals/common-misconceptions-about-rabies/.
- 26.Blois M. How to stop brain cancer—with rabies. Science. 2017 http://www.sciencemag.org/news/2017/02/how-stop-brain-cancer-rabies [Google Scholar]
- 27.Mole B. Homeopath “Treated” 4-yr-old Boy’s Behavior Problems With Saliva From Rabid Dog. https://arstechnica.com/science/2018/04/homeopath-treated-4-yr-old-boys-behavior-problems-with-saliva-from-rabid-dog/.
- 28.Willoughby R., Jr. Rabies: rare human infection – common questions. Infect Dis Clin. 2015;29:637–650. doi: 10.1016/j.idc.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 29.de Souza A., Madhusudana S.N. Survival from rabies encephalitis. J Neurol Sci. 2014;339:8–14. doi: 10.1016/j.jns.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 30.Karande S., Muranjan M., Mani R.S. Atypical rabies encephalitis in a six-year old boy: clinical, radiological, and laboratory findings. Int J Infect Dis. 2015;36:1–3. doi: 10.1016/j.ijid.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 31.Feder H.M., Jr., Petersen B.W., Robertson K.L. Rabies: still a uniformly fatal disease? Historical occurrence, epidemiological trends, and paradigm shifts. Curr Infect Dis Rep. 2012;14:408–422. doi: 10.1007/s11908-012-0268-2. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Zoonotic Diseases. https://www.cdc.gov/onehealth/basics/zoonotic-diseases.html.
- 33.Davis A.D., Morgan S.M.D., Dupuis M. Overwintering of rabies virus in silver haired bats (Lasionycteris noctivagans) PLoS One. 2016;11(5):e0155542. doi: 10.1371/journal.pone.0155542. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0155542 [DOI] [PMC free article] [PubMed] [Google Scholar]


