Abstract
Despite evidence of a strong relationship between BPD and substance use problems in general, little research has examined the associations of BPD symptoms with the misuse of sedatives or opioids, and no studies have explored possible factors that may underlie these associations. Thus, this study examined the relationships of BPD symptoms (i.e., the number of BPD criteria with threshold ratings on a diagnostic interview) to nonprescription sedative use, nonprescription opioid use, and prescription sedative/opioid misuse among 194 patients with alcohol and/or cocaine dependence in a residential substance use disorder treatment facility, as well as the roles of two theoretically-relevant factors in these relationships: emotion regulation (ER) difficulties and impulsivity facets. We found significant positive associations between BPD symptoms and nonprescription sedative use, nonprescription opioid use, and prescription sedative/opioid misuse. We also found significant positive indirect relationships of BPD symptoms to nonprescription sedative use through ER difficulties, ab = .04, 95% CI [.003, .09], and to prescription sedative/opioid misuse through two facets of impulsivity: lack of perseverance, ab = .05, 95% CI [.01, .11], and negative urgency, ab = .03, 95% CI [.002, .07]. Findings highlight the differential relevance of ER difficulties and impulsivity dimensions to the relationships of BPD symptoms to nonprescription sedative use and prescription sedative/opioid misuse, respectively, among patients with alcohol and/or cocaine dependence.
Keywords: emotion regulation, borderline personality disorder, impulsivity, sedatives, opioids, substance use
Borderline personality disorder (BPD) is characterized by severe emotional, behavioral, cognitive, and interpersonal dysregulation (American Psychiatric Association [APA], 2013; Linehan, 1993), as well as numerous co-occurring physical health (e.g., chronic pain, arthritis, cardiovascular disease; El-Gabalawy, Katz, & Sareen, 2010; Frankenburg & Zanarini, 2004; Lee at al., 2010; Sansone & Sansone, 2012) and mental health (e.g., anxiety disorders, posttraumatic stress disorder, major depressive disorder, risky behaviors; Kleindienst et al., 2008; Klonsky, 2007; McGlashan et al., 2000; Skodol et al., 1995, 2002; Svaldi, Phillipsen, & Matthies, 2012; Tomko, Trull, Wood, & Sher, 2014; Zanarini et al., 1998) problems. Although BPD is found at rates of 1–6% in the general population (Grant et al., 2008; Lenzenweger, Lane, Loranger, & Kessler, 2007; Tomko et al., 2014; Torgersen, Kringlen, & Cramer, 2001), BPD is the most common personality disorder among patients receiving mental health treatment, with 15–20% of inpatients and 8–10% of outpatients having a diagnosis of BPD (APA, 2013; Widiger & Weissman, 1991; Zimmerman, Rothschild, & Chelminski, 2005).
One mental health population with particularly high rates of BPD is patients with substance use disorders (SUDs). Rates of BPD range from 10–50% among individuals with SUDs (Cacciola, Alterman, McKay, & Rutherford, 2001; Trull et al., 2018; Trull, Sher, Minks-Brown, Durbin, & Burr, 2000), with rates as high as 61% among SUD inpatients (Trull et al., 2000). The co-occurrence of BPD and SUDs is related to worse outcomes than either disorder alone (Bornovalova et al., 2018), including increased risk for suicidal and nonsuicidal self-injury (Gunderson & Links, 2008; McMain & Ellery, 2008), greater variety of abused substances (Kruedelbach, McCormick, Schulz, & Grueneich, 1993), increased chronicity of BPD symptoms (Links, Heslegrave, Mitton, Van Reekum, & Patrick, 1995), and worse treatment outcomes (Pennay et al., 2011; Stone, 1990).
Notably, the majority of the research examining the association between BPD and substance use problems has focused on alcohol or cocaine use or examined substance use in general (vs. specific drug classes), with limited research examining central nervous system depressants (e.g., tranquilizers, sedatives, and opioids). However, there is considerable value in research focused on identifying the factors associated with the misuse of central system nervous depressants in particular. First, in recent years, these substances have become among the most frequently abused drugs within the general population (Jann, Kennedy, & Lopez, 2014; NIDA, 2018). Second, there is evidence that the misuse of central nervous system depressants may be particularly relevant to BPD. Given that individuals with BPD pathology have high rates of both physical health problems (including chronic pain) and anxiety disorders (see Frankenburg & Zanarini, 2004; Skodol et al., 1995; Zanarini et al., 1998) and are frequent utilizers of health care (see Bateman & Fonagy, 2003; Frankenburg & Zanarini, 2004), they may have increased access to both sedative and opioid prescription drugs that increase risk for abuse over time (see, e.g., Frankenburg, Fitzmaurice, & Zanarini, 2014). Moreover, given evidence that individuals with BPD tend to engage in a number of other health-risk behaviors (e.g., nonsuicidal self-injury) to escape or avoid negative affect (e.g., Hulbert & Thomas, 2010), they may be particularly motivated to use substances such as central nervous system depressants that function to reduce negative arousal. Finally, BPD pathology has been linked to dysregulation of the endogenous opioid system (Bandelow, Schmahl, Falkai, & Wedekind, 2010; Stanley & Siever, 2010), including deficits in endogenous opioids and more sensitive endogenous opioid system receptors. Thus, substances that activate this system may be more reinforcing for individuals with BPD pathology than those with typically developed endogenous opioid systems, increasing the frequency with which these substances are used.
Although considerable research has examined the association between BPD pathology and substance use in general (e.g., Grant et al., 2008; Maraz et al., 2016; Skodol, Oldham, & Gallaher, 1999; see also Trull et al., 2000, 2018), research examining the relationship of BPD pathology to sedative and opioid misuse (prescribed or non-prescribed) in particular is minimal. Nonetheless, the research that has been done demonstrates significant associations between BPD and both opioid and sedative use disorders (Carpenter, Wood, & Trull, 2016), as well as heightened rates of BPD among heroin users and individuals with opioid use disorders in general (Mackesy-Amiti, Donenberg, & Ouellet, 2012; Trull et al., 2000). Moreover, BPD features (specifically, self-harm/impulsivity features) have been found to be positively associated with risk for prescription opioid misuse (Tragesser, Jones, Robinson, Stutler, & Stewart, 2013).
Yet, despite this emerging support for an association between BPD pathology and the misuse of opioids and sedatives, the factors underlying this association remain unclear. Given the recent increase in abuse of opioids and sedatives within the U. S. population (Bachhuber, Hennessy, Cunningham, & Starrels, 2016; Compton & Volkow, 2006), as well as the high risk for accidental overdose with these substances (Florence, Zhou, Luo, & Zu, 2016; Jann et al., 2014; O’Brien, 2005), the misuse of these substances is a major public health concern (SAMHSA, 2017) and necessitates further research on the factors driving the misuse of these substances in high-risk populations, such as individuals with BPD pathology.
Two factors that may play a role in the association between BPD and sedative and opioid misuse are emotion regulation (ER) difficulties and impulsivity, both of which are theorized to underlie BPD, substance use difficulties, and their co-occurrence (Bornovalova, Lejuez, Daughters, Rosenthal, & Lynch, 2005; Maraz et al., 2016; Weiss et al., 2012). With regard to the former, ER difficulties refer to maladaptive ways of responding to emotions, including deficits in the understanding, acceptance, and effective use of emotions and modulation of emotions (Gratz, Moore, & Tull, 2016; Gratz, Dixon, Kiel, & Tull, 2018). Grounded in theory and research on the functionality of emotions (Cole, Michel, & Teti, 1994; Ekman & Davidson, 1994; Thompson, 1994) and paradoxical consequences of efforts to avoid or control emotions (e.g., Hayes, Luoma, Bond, Masuda, & Lillis, 2006), the conceptualization of ER difficulties used here proposes that responses to emotions are more important than the quality of those emotions. Notably, an extensive body of literature demonstrates that individuals with BPD pathology exhibit broad deficits in ER (Gratz et al., 2016; Salsman & Linehan, 2012), including greater nonacceptance and avoidance of emotions (Beblo et al., 2010; Gratz, Tull, & Gunderson, 2008; Yen, Zlotnick, & Costello, 2002), greater unwillingness to experience emotional distress (Bornovalova et al., 2008; Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006), and greater difficulties controlling behaviors in the context of emotional distress (Chapman, Dixon-Gordon, Layden, & Walters, 2010). The heightened levels of emotional unwillingness in BPD, combined with an absence of adaptive, non-avoidant strategies for tolerating and managing the elevated levels of emotional distress found in this population, may prompt individuals with BPD pathology to seek out alternative means for obtaining rapid relief from intense emotional distress, such as the use of substances. In particular, individuals with BPD pathology may be especially likely to abuse substances that bring about a sense of calm or result in feelings of euphoria that counter emotional distress, such as sedatives or opioids. The negative reinforcement provided by these substances may then result in an increased reliance on these substances to manage emotional distress, eventually contributing to sedative or opioid dependence (see Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). Indeed, this premise is further supported by research indicating that BPD features among college women are significantly associated with coping motives for prescription opioid use (Vest, Murphy, & Tragesser, 2018).
Impulsivity is well documented as a mechanism driving the development and maintenance of substance use difficulties in general (Ouzir & Errami, 2016; Verdejo-García, Bechara, Rechnor, & Pérez-García, 2007), and has been implicated in the pathogenesis of BPD pathology (Crowell, Beauchaine, & Linehan, 2009). According to Whiteside and Lynam (2001), impulsivity is a multi-faceted construct consisting of negative urgency (i.e., the tendency to act impulsively when experiencing intense negative affect), lack of premeditation (i.e., the failure to consider the consequences of an action before engaging in that action), lack of perseverance (i.e., the inability to focus or follow through on difficult or boring tasks), and sensation seeking (i.e., the tendency to enjoy and pursue activities that are exciting). Notably, impulsivity among individuals with co-occurring BPD and substance use pathology is heightened relative to those with substance use problems or BPD alone (Links et al., 1995; Trull, Waudby, & Sher, 2004), which may partially explain the risk for more severe consequences among individuals with co-occurring BPD and substance use problems.
Previous research on impulsivity among individuals with BPD pathology suggests that the specific impulsivity facets of negative urgency and lack of perseverance are uniquely related to BPD symptoms (Bøen et al., 2015; DeShong, & Kurtz, 2013; Jacob et al., 2010; Peters, Upton, & Baer, 2013). Likewise, individuals with (vs. without) SUDs report higher levels of negative urgency and lack of perseverance, as well as greater lack of premeditation (Verdejo-García et al., 2007). Although few studies have examined the facets of impulsivity most relevant to opioid or sedative misuse, preliminary research suggests that negative urgency and sensation seeking may be related to misuse of prescription opioids among chronic pain patients (Vest, Reynolds, & Tragesser, 2016). Together, evidence for the converging relevance of negative urgency to BPD and both prescription opioid misuse and substance use pathology in general, as well as findings of the relevance of lack of perseverance to both BPD and substance use pathology, suggest that these particular facets of impulsivity could explain the association of BPD pathology with opioid and sedative misuse. Specifically, with regard to negative urgency, the intense negative emotions experienced by individuals with BPD pathology, combined with the higher levels of emotional unwillingness and avoidance in this population (see Gratz et al., 2006; Gratz, Tull, Baruch, Bornovalova, & Lejuez, 2008), may make it difficult to resist urges to seek out or use substances that could function to bring about rapid relief from those emotions. Perseverance, on the other hand, involves persistence on a task and the ability to continue or stay focused even when a task becomes difficult or boring, and corresponds with the personality traits of self-discipline and conscientiousness (Whiteside & Lynam, 2001). Thus, low perseverance among individuals with BPD pathology may interfere with their ability to take these medications as prescribed and/or persist through the unpleasant withdrawal symptoms associated with the recurrent use of these substances, resulting in the misuse of these substances.
Thus, given (a) the recent increase in abuse of opioids and sedatives within the U.S.; (b) the high risk for accidental overdose with these substances; (c) evidence for the particular relevance of sedatives and opioids to BPD pathology; and (d) the relative paucity of research on both the association between BPD pathology and the misuse of opioids and sedatives in particular and the factors underlying this association, the aims of the current study were to: 1) examine the associations between BPD symptoms (i.e., the number of BPD criteria with threshold ratings on a diagnostic interview) and sedative and opioid misuse (across nonprescription sedative use, nonprescription opioid use, and prescription sedative/opioid misuse) within an at-risk clinical population; and 2) explore the roles of ER difficulties and impulsivity facets in these associations. In particular, research highlights the importance of examining sedative and opioid misuse in the context of other SUDs (particularly alcohol and cocaine dependence) among individuals with BPD pathology. Not only are alcohol and cocaine dependence common among individuals with BPD (Carpenter et al., 2016), the use of opioids and sedatives in the context of alcohol and/or cocaine use is particularly risky. Specifically, research indicates that co-occurring sedative and opioid misuse in the context of alcohol or cocaine dependence is associated with a variety of negative outcomes, including heightened risk for overdose (Gudin, Mogali, Jones, & Comer, 2013), more severe drug use, risky behaviors, and substance use problems (e.g., injection drug use, risky sexual behavior; Leri, Bruneau, & Stewart, 2003; McCabe, Cranford, Morales, & Young, 2006; Subramaniam, Ives, Stitzer, & Dennis, 2010), and worse treatment outcomes (Leri et al., 2003). Thus, SUD patients with alcohol and/or cocaine dependence are a particularly relevant population for examining the associations between BPD pathology and sedative and opioid misuse.
We hypothesized that the relationships of BPD symptoms to all three sedative and opioid misuse outcomes within this population would be indirect through both ER difficulties and two particular facets of impulsivity: negative urgency and lack of perseverance.
Methods
Participants
Participants included in the current study (N = 194, 49.5% women) were those with complete data drawn from a larger sample of patients (N = 226) consecutively admitted to a residential SUD treatment facility located in the southern United States. This treatment facility is managed by the state department of mental health and located on the campus of the state’s primary psychiatric hospital. The treatment facility largely serves a rural population and accepts both voluntary and involuntary admissions. The majority (58.4%) of participants in this study were court-ordered to treatment. Following a short detoxification period, standard treatment at this facility involves a combination of strategies from Alcoholics Anonymous and Narcotics Anonymous, as well as groups focused on relapse prevention and life skills (e.g., stress management, social skills training). The facility requires complete abstinence from drugs (including nicotine) and alcohol, with the exception of caffeine. Aside from scheduled activities or medical appointments, residents are not permitted to leave the treatment facility. Contract duration is approximately 30 days for all patients.
The 194 participants included in this study ranged in age from 18 to 65 years (Mage = 34.22 ± 10.06) and were ethnically/racially diverse (59.3% White; 37.6% Black/African American; 1.5% Latinx). With regard to educational attainment, 33% had completed high school or received a GED, 28.9% had attended some college or technical school, and 9.7% had graduated from college. Most participants (74%) reported a household income of less than $30,000. With regard to SUD treatment history, 57.1% indicated previous treatment for alcohol use and 71.6% reported past treatment for drug use.
Measures
Borderline personality disorder symptoms
The BPD module of the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini, Frankenberg, Sickel, & Yong, 1996) was used to assess BPD symptoms (i.e., the number of BPD criteria with threshold ratings), as well as BPD diagnostic status. Interviews were conducted by bachelors- or masters-level clinical assessors trained to reliability with study investigators (diagnostic agreement > 88%). Detailed information on each criterion was collected by interviewers, and all ratings were reviewed by the study investigators. In the case of disagreements, ratings were discussed by the investigators and interviewer until a consensus was reached. The DIPD-IV has demonstrated good interrater and test-retest reliability (Carcone, Tokarz, & Ruocco, 2015; Grilo & McGlashan, 2000; Zanarini et al., 2000). Internal consistency in this sample was acceptable (α = .83).
Emotion regulation difficulties
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item measure that assesses dispositional ER difficulties across six domains: nonacceptance of negative emotions, inability to engage in goal-directed behaviors when experiencing negative emotions, difficulties controlling impulsive behaviors when experiencing negative emotions, lack of access to effective ER strategies, lack of emotional awareness, and lack of emotional clarity. Participants rate each item on a 5-point Likert-type scale (1 = “almost never” [0–10%], 2 = “sometimes” [11–35%], 3 = “about half the time” [36–65%], 4 = “most of the time” [66–90%], 5 = “almost always” [91–100%]). Factor analytic examinations of the DERS provide support for a meaningful overall factor represented by the DERS total score (Hallion, Steinman, Tolin, & Diefenbach, 2018; Osborne, Michonski, Sayrs, Welch, & Anderson, 2017). The DERS total score demonstrates good reliability and construct and convergent validity and is significantly associated with objective measures of ER and the unwillingness to experience emotions in particular (Gratz, Bornovalova, Delany-Brumsey, Nick, & Lejuez, 2007; Gratz & Roemer, 2004; Gratz et al., 2006; Vasilev, Crowell, Beauchaine, Mead, & Gatzke-Kopp, 2009). Internal consistency in this sample was acceptable (α = .93).
Impulsivity
Facets of impulsivity were measured using the UPPS Impulsive Behavior Scale (UPPS; Whiteside & Lynam, 2001; Whiteside, Lynam, Miller, & Reynolds, 2005). The UPPS assesses impulsivity as a multidimensional construct consisting of four facets: lack of premeditation, lack of perseverance, negative urgency, and sensation seeking. These scales have demonstrated good convergent and discriminant validity (Cyders & Smith, 2007). Participants rate 59 items on a 4-point Likert-type scale (1 = “agree strongly”, 2 = “agree some”, 3 = “disagree some”, 4 = “disagree strongly”). As the UPPS was designed to assess unique facets of impulsivity, a separate score is obtained for each facet and a total score is not calculated. Internal consistency of the subscales in this sample ranged from .77-.84.
Substance use
Substance use across the substances of interest (i.e., nonprescription sedatives, nonprescription opioids, and prescription sedatives and/or opioids) was assessed using the Drug Use Questionnaire (DUQ; Hien & First, 1991), a self-report measure of past-year frequency of alcohol and drug use. The DUQ characterizes frequency of use in a manner consistent with criteria for establishing the presence of a SUD in the Structured Clinical Interview for DSM-IV (SCID-IV; First, Spitzer, Gibbon, & Williams, 1996). Specifically, participants rate the frequency with which they used thirteen specific substances over the course of the past year on a 6-point Likert-type scale (0 = “never”, 1 = “one time”, 2 = “monthly or less”, 3 = “2–4 times a month”, 4 = “2–3 times a week”, and 5 = “4 or more times a week”). Of particular interest to this study were the items assessing the frequency of nonprescription sedative use, heroin use, and prescription drug misuse. Participants who endorsed prescription drug misuse were instructed to list the specific prescription drugs they had misused (i.e., used not as prescribed). Those endorsing misuse of prescription drugs other than sedatives or opioids were not included in this sample. This measure has demonstrated good construct validity (Bornovalova, Ouimette, Crawford, & Levy, 2009; Lejuez, Bornovalova, Reynolds, Daughters, Curtin, 2007; Tull, Kiel, McDermott, & Gratz, 2013) and convergence with SUD diagnoses from structured clinical interviews in associations with relevant outcomes (Lejuez et al., 2007).
Other psychopathology
Current mood and anxiety symptoms were assessed using the Depression Anxiety Stress Scales (DASS-21; Lovibond & Lovibond, 1995), a self-report measure that provides individual subscale scores of the severity of depression, anxiety, and stress symptoms. Participants rate the items on a 4-point Likert-type scale indicating how much each item applied to them in the past week (0 = “did not apply to me at all”, 1 = “applied to me some of the time”, 2 = “applied to me a good part of the time”, 3 = “applied to me most of the time”). This measure has demonstrated good reliability and validity (Lovibond & Lovibond, 1995). Internal consistency of these subscales ranged from .84-.90.
SUDs, including alcohol and cocaine dependence, were assessed using the SCID-IV (First et al., 1996). As with the DIPD-IV, interviews were conducted by bachelors- or masters-level clinical assessors trained to reliability with study investigators (diagnostic agreement > 88%). All interviews were reviewed by investigators, with disagreements discussed to reach a consensus.
Procedure
All procedures were reviewed and approved by the Institutional Review Boards of participating institutions. Data were collected between October 2011 and October 2013 as part of a larger study on risk-taking among patients with alcohol and/or cocaine dependence (the most common SUDs for which individuals sought treatment at the time in the state where data were collected; SAMHSA, 2015). Participants were recruited for this study no sooner than 72 hours after entry into the facility to limit the possible interference of withdrawal symptoms on study engagement. All patients at the treatment facility were provided with information about the study in group meetings and given the opportunity to meet with study personnel to learn more about the study and determine eligibility for the study. Participants interested in learning more about the study scheduled a time to meet in private with study personnel. During that meeting, eligibility was determined.
To be eligible for inclusion in the larger study, participants were required to: 1) be dependent on cocaine and/or alcohol (although participants could also be dependent on other substances in addition to cocaine and alcohol); 2) have a Mini-Mental Status Exam (Folstein, Folstein, & McHugh, 1975) score of ≥ 24 (indicative of no significant cognitive impairment); and 3) have no current psychotic disorder (as determined by the psychosis screener from the SCID-I; First et al., 1996). Those who met inclusion criteria were provided with information about study procedures and associated risks, following which written informed consent was obtained. Fewer than 5% of eligible patients refused to participate in this study. After providing written informed consent, participants completed a diagnostic interview, followed by a series of self-report questionnaires. Participants were reimbursed $25.
Analysis Plan
Mean replacement of individual items was used for cases with less than 20% missing data on any measure used in the analyses; cases with > 20% missing data on any included measure were excluded from analyses (resulting in the exclusion of 32 participants from the larger sample of 226). All analyses were conducted with the final sample of 194 participants. Using values recommended in Fritz and MacKinnon (2007), a sample size of 162 is adequate to detect a small to medium-sized effect (power = .80).
Correlation analyses were conducted to examine interrelations among the primary variables of interest. To identify covariates for primary analyses, associations between relevant demographic and clinical variables (i.e., age, racial/ethnic background, gender, depression symptoms, anxiety symptoms, alcohol dependence, and cocaine dependence) and the intervening and outcome variables of interest were examined using t tests and correlation analyses. Next, the PROCESS macro in SPSS (Model 4; Hayes, 2017), a tool that uses observed variable ordinary least squares regression to analyze path models, was used to examine relevant indirect relationships of BPD symptoms to past-year frequency of nonprescription sedative use, nonprescription opioid use, and prescription sedative/opioid misuse through ER difficulties (DERS total score) and impulsivity facets (UPPS subscales), as warranted by the initial correlation analyses. Specifically, only those intervening variables (i.e., UPPS subscales, DERS total score) significantly correlated with both the independent and dependent variables (i.e., BPD symptoms and the respective sedative or opioid use outcome variable) were included in each model. Each model also contained all identified relevant covariates (i.e., those associated with the intervening or outcome variables).
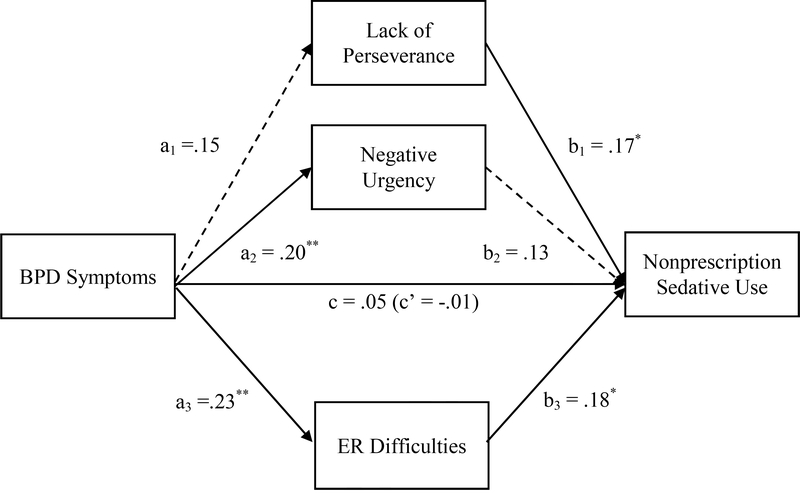
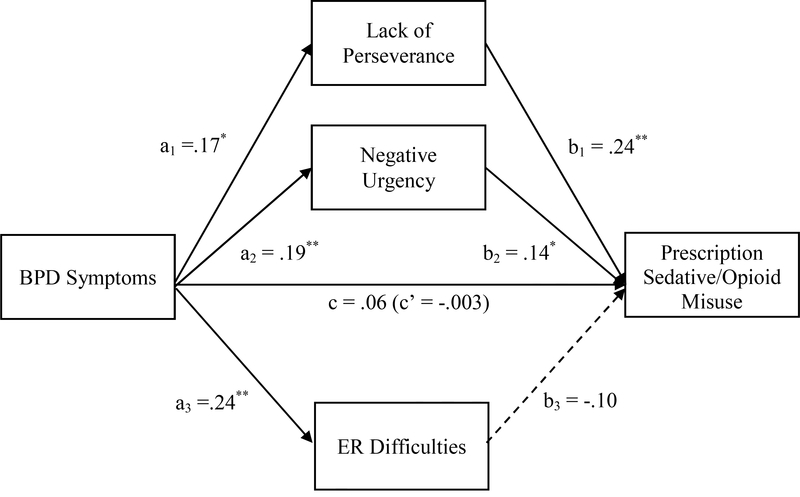
Specific paths tested in each examined model are presented in Figures 1 and 2. As depicted in Figures 1 and 2, path a captures the relationships between BPD symptoms and the intervening variable(s) (i.e., DERS and relevant UPPS scales), path b captures the relationships between the intervening variables and the outcome, and path c captures the relationship between BPD symptoms and the outcome variable. The indirect relationships of BPD symptoms to the sedative and opioid misuse outcomes are calculated as a x b (ab), and path c’ captures the direct relationship of BPD symptoms to the outcome variables (i.e., the remainder of the relationship not accounted for by the indirect relationship; Preacher & Hayes, 2008). Of note, all relevant intervening variables included in each model (i.e., those associated with both BPD pathology and the outcome of interest) were examined simultaneously as shown in Figures 1 and 2.
Figure 1.
Indirect relationships of BPD symptoms to frequency of nonprescription sedative use through lack of perseverance, negative urgency, and ER difficulties
Note. β values are reported. Age, racial/ethnic background, income, depression symptoms, and anxiety symptoms were included as covariates in the model.
**p<.01, *p<.05
Figure 2.
Indirect relationships of BPD symptoms to prescription sedative/opioid misuse through lack of perseverance, negative urgency, and ER difficulties
Note. β values are reported. Age, racial/ethnic background, income, depression symptoms, and anxiety symptoms were included as covariates in the model.
**p<.01, *p<.05
Following recommendations by Preacher and Hayes (2008), the current study used a bootstrapping technique to estimate the indirect relationships. This approach is recommended over other approaches for examining indirect relationships (i.e., Sobel test, causal steps approach; MacKinnon, Lockwood, Hoffman, & West, 2002; MacKinnon, Lockwood, & Williams, 2004), as bootstrapping allows for better control of Type I error and provides greater power (Preacher & Hayes, 2008). In this study, as recommended by Hayes (2017) and Yzerbyt, Muller, Batailler, and Judd (2018), the estimates of the indirect relationships were derived from the mean of 5000 bootstrap samples. Bias corrected and accelerated 95% confidence intervals were calculated, and indirect relationship estimates were considered significant when the confidence intervals did not contain zero.
Results
Identification of Covariates
Participant age was negatively associated with ER difficulties, r = −.16, p = .03, and prescription sedative/opioid misuse, r = −.31, p < .001. Further, there were significant differences in negative urgency, t(180) = 3.32, p = .001, nonprescription sedative use, t(192) = 5.72, p < .001, and prescription sedative/opioid misuse, t(192) = 8.01, p < .001, as a function of racial/ethnic background, with White participants reporting greater negative urgency and more frequent drug misuse than participants who identified as a racial/ethnic minority. Likewise, there were significant differences in nonprescription sedative use, t(192) = −2.28, p = .02, and lack of perseverance, t(179) = 2.13, p = .03, between participants with an annual income below versus above $10,000, such that participants earning less than $10,000 annually reported significantly greater sedative use and significantly lower levels of lack of perseverance than those earning more than $10,000 annually. No significant gender differences were found for any intervening or outcome variable (ts <1.63, ps > .10). Depression symptoms were significantly related to ER difficulties, r = .44, p < .001, and negative urgency, r = .30, p < .001, and anxiety symptoms were significantly related to ER difficulties, r = .41, p < .001, negative urgency, r = .34, p < .001, nonprescription sedative use, r =.28, p = .01, and prescription sedative/opioid misuse, r= .20, p = .01. Finally, there were no significant differences in any of the intervening or outcome variables as a function of the presence (vs. absence) of either alcohol dependence or cocaine dependence (ts <|1.59|, ps > .13). Thus, age, racial/ethnic background, income, depression symptoms, and anxiety symptoms were included as covariates in all primary analyses.
Preliminary Analyses
Descriptive data on and correlations among the primary variables of interest are reported in Table 1. Consistent with past research on SUD samples (see Gratz et al., 2008; Trull et al., 2000), 34.1% of participants in this sample met criteria for BPD, 10.7% reported past-year use of nonprescription opioids, 51.7% reported past-year use of nonprescription sedatives, and 56.2% reported past-year prescription drug misuse. Of the participants reporting prescription drug misuse, 56.4% reported misusing prescription opioids and 24.8% reported misusing prescription sedatives. Current SUD diagnoses of participants are presented in Table 2.
Table 1.
Descriptive statistics for and correlations among primary study variables.
| Mean (SD) | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. BPD | 3.74 (2.41) | -- | -- | -- | -- | -- | -- | -- | -- | ||
| 2. DERS | 89.93 (24.99) | .34** | -- | -- | -- | -- | -- | -- | -- | ||
| 3. SS | 43.66 (7.34) | .11 | .18* | -- | -- | -- | -- | -- | -- | ||
| 4. NU | 45.21 (6.06) | .28** | .50** | .47** | -- | -- | -- | -- | -- | ||
| 5. PRE | 24.73 (5.37) | .09 | .26** | .06 | .04 | -- | -- | -- | -- | ||
| 6. PER | 24.05 (5.15) | .18* | .38* | −.02 | .18* | .58** | -- | -- | -- | ||
| 7. Sedative | 1.73 (1.96) | .14* | .21** | .25** | .25** | .25** | .22** | -- | -- | ||
| 8. Opioid | .29 (1.01) | .19** | .01 | .09 | −.06 | .19** | .09 | .18* | -- | ||
| 9. Rx | 2.26 (2.25) | .19* | .16* | .33** | .27** | .24** | .28** | .55** | .31** | -- | |
| 10. Depression | 12.28 (11.48) | .22** | .45** | .15* | .30** | .15* | .12 | .11 | .02 | .10 | -- |
| 11. Anxiety | 10.27 (9.97) | .24** | .41** | .12 | .34** | .15* | .09 | .18** | .07 | .18* | .75** |
Note. BPD = BPD symptoms, DERS = emotion regulation deficits, SS = sensation seeking subscale of UPPS, NU = negative urgency subscale of UPPS, PRE = lack of premeditation subscale of UPPS, PER = lack of perseverance subscale of UPPS, Sedative = past-year frequency of nonprescription sedative use, Opioid = past-year frequency of nonprescription opioid use, Rx = past-year frequency of prescription sedative/opioid misuse.
p< .0
p< .05
Table 2.
Participant substance use disorder (SUD) diagnoses.
| % Present (n) | |
|---|---|
| Alcohol Use Disorder | 67.5% (131) |
| Cocaine Use Disorder | 58.8% (114) |
| Cannabis Use Disorder | 29.4% (57) |
| Opioid Use Disorder | 22.7% (44) |
| Stimulant Use Disorder | 20.6% (40) |
| Sedative Use Disorder | 18.6% (36) |
| Polydrug Use Disorder | 9.3% (18) |
| Hallucinogen Use Disorder | 2.6% (5) |
| Two or more SUDs | 64.4% (125) |
| Three or more SUDs | 36.1% (70) |
Note. All diagnoses are current.
As expected, BPD symptoms were significantly positively correlated with past-year frequency of nonprescription sedative use, nonprescription opioid use, and prescription sedative/opioid misuse, as well as ER difficulties and the impulsivity facets of negative urgency and lack of perseverance (see Table 1). All associations were small in magnitude, with the exception of the correlation between BPD symptoms and ER difficulties, which was associated with a moderate effect size (see Table 1). Additionally, ER difficulties and the impulsivity facets of negative urgency, lack of perseverance, and sensation seeking were significantly positively associated with frequency of both nonprescription sedative use and prescription sedative/opioid misuse, and lack of premeditation was significantly associated with all three drug use outcomes (although all but the moderate-sized correlation between sensation seeking and prescription sedative/opioid misuse were small in magnitude).
Thus, primary analyses focused on the indirect relationships of BPD symptoms to frequency of nonprescription sedative use and prescription sedative/opioid misuse through ER difficulties and both negative urgency and lack of perseverance. Given that the only ER or impulsivity variable associated with nonprescription opioid use (i.e., lack of premeditation) was not significantly correlated with BPD symptoms, this particular outcome was not examined further.
Primary Analyses
Results of the model examining the indirect relationships of BPD symptoms to frequency of nonprescription sedative use through ER difficulties, negative urgency, and lack of perseverance are shown in Figure 1. BPD symptoms were uniquely positively associated with ER difficulties and negative urgency, but not lack of perseverance (Figure 1). Conversely, ER difficulties and lack of perseverance (but not negative urgency) were uniquely positively associated with frequency of nonprescription sedative use (Figure 1). Finally, we found a significant indirect relationship of BPD symptoms to frequency of nonprescription sedative use through ER difficulties, F (5,193) = 4.84, p < .001, ab = .04, 95% CI [.003, .09], but not negative urgency, ab = −.03, 95% CI [−.08, .01], or lack of perseverance, ab = .01, 95% CI [−.02, .05].1
Results of the model examining the indirect relationships of BPD symptoms to frequency of prescription sedative/opioid misuse are shown in Figure 2. Consistent with the proposed model, BPD symptoms were uniquely positively associated with ER difficulties, negative urgency, and lack of perseverance (see Figure 2). However, only negative urgency and lack of perseverance were uniquely positively associated with frequency of prescription sedative/opioid misuse (Figure 2). Finally, we found a significant indirect relationship of BPD symptoms to frequency of prescription sedative/opioid misuse through both lack of perseverance, ab = .05, 95% CI [.01, .11], and negative urgency, ab = .03, 95% CI [.002, .07], F (5,184) = 10.45, p < .001, but not ER difficulties, ab = −.01, 95% CI [−.07, .05]. Of note, results did not change when covariates were excluded from the models.
Discussion
The present study examined the relationships of BPD symptoms to sedative and opioid misuse, as well as the roles of ER difficulties and impulsivity facets in these relationships, within a clinical sample of patients with alcohol and/or cocaine dependence. Extending past research on the association between BPD and substance use problems, we found significant zero-order associations between BPD symptoms and frequency of nonprescription sedative use, nonprescription opioid use, and prescription sedative/opioid misuse. These findings provide further support for the relevance of BPD pathology to the misuse of both sedatives and opioids in particular – two classes of drugs associated with elevated risk for both abuse and accidental poisoning and overdose in general (Coben et al., 2010; Florence et al., 2016; Jann et al., 2014; O’Brien, 2005) and among patients with alcohol and cocaine dependence in particular (Gudin et al., 2013; Subramaniam et al., 2010). The results of this study suggest that the presence of BPD symptoms may increase use of these substances among SUD patients.
Results of this study also highlight the differential relevance of ER difficulties and impulsivity dimensions to the relationships of BPD symptoms to nonprescription sedative use and prescription sedative/opioid misuse, respectively, among patients with alcohol and/or cocaine dependence. Specifically, we found a significant indirect relationship of BPD symptoms to nonprescription sedative use through ER difficulties. This finding is consistent with theoretical literature suggesting that the maladaptive behaviors commonly observed in BPD (including substance misuse) stem from the difficulties in ER that underlie this disorder (Gratz et al., 2016; Linehan, 1993). The results of this study suggest that the ER difficulties associated with BPD may be most strongly linked to the use of substances that down-regulate emotional distress and provide a sense of calm (i.e., sedatives), at least among SUD patients with alcohol and/or cocaine dependence. Interestingly, ER difficulties did not explain the relationship of BPD symptoms to nonprescription opioid use or prescription sedative/opioid misuse. This pattern of results may reflect the particular relevance of ER difficulties to the use of sedatives versus opioids, perhaps due to their intended targets. Specifically, given the strong associations between ER difficulties and anxiety (Campbell-Sills, Ellard, & Barlow, 2014), panic (Tull & Roemer, 2007), and other intense negative emotional states (Gupta, Rosenthal, Mancini, Cheavens, & Lynch, 2008; Shorey, Cornelius, & Idema, 2011), SUD patients with heightened ER difficulties may be more likely to seek out substances that are generally advertised or described as methods for alleviating anxiety or down-regulating negative emotions (i.e., sedatives such as benzodiazepines) than to seek out opioids, which are generally prescribed to alleviate somatic pain (even though opioids also have the ability to down-regulate negative affect; Martel, Dolman, Edwards, Jamison, & Wasan, 2014).
Conversely, we found significant indirect relationships of BPD symptoms to prescription sedative/opioid misuse through two facets of impulsivity: lack of perseverance and negative urgency. This finding is consistent with previous research indicating significant associations of negative urgency with prescription opioid misuse and both negative urgency and lack of perseverance with substance use problems in general (Verdejo-García et al., 2007; Vest et al., 2016). This finding suggests that it is the heightened impulsivity associated with BPD (rather than the ER difficulties associated with this disorder) that explains the association between BPD symptoms and prescription sedative/opioid misuse. Given the high opioid and benzodiazepine prescribing rates across the U.S. (Centers for Disease Control, 2018; Curtis et al., 2006; Olfson, King, & Schoenbaum, 2015), this finding may speak to the relevance of impulsivity to the misuse of easily accessible (i.e., prescribed) drugs versus illegal drugs that may be more difficult to obtain. The built-in delay associated with obtaining illicit sedatives and opioids may attenuate the strength of the relationship of impulsivity to these less accessible substances. Furthermore, a lack of perseverance in particular may make it more difficult to take medications as prescribed or persist through the experience of withdrawal symptoms once the prescription has ended.
Finally, it is important to note that neither ER difficulties nor any impulsivity facet explained the relationship of BPD symptoms to nonprescription opioid use. Future research is needed to examine other factors that may underlie the use of heroin and other nonprescription opioids among individuals with greater BPD symptoms. In particular, previous research has identified several risk factors for the abuse of nonprescription opioids, including poly-drug use (Wu & Howard, 2007), early onset of drug use (Storr, Westergaard, & Anthony, 2005), and personality characteristics such as neuroticism and anger (Kornør & Nordvik, 2007; Suh, Ruffinns, Robins, Albanese, & Khantzian, 2008), all of which are relevant to BPD (Franken & Hendriks, 2000; Hiebler-Ragger, Unterrainer, Rinner, & Kapfhammer, 2016; Mancke, Herpertz, Kleindienst, & Bertsch, 2017; Samuel, Carroll, Rounsaville, & Ball, 2013).
Several limitations warrant consideration. First, this study is limited by the use of cross-sectional data. Prospective, longitudinal studies are needed to clarify how co-occurring BPD and sedative/opioid misuse develop among SUD patients, as well as the specific roles of ER difficulties and impulsivity in this co-occurrence. In particular, such research would clarify the extent to which the ER difficulties and impulsivity associated with BPD actually drive the development of sedative and/or opioid misuse within this population (vs. being a consequence of the misuse of these substances). Indeed, although theory supports the direction of the associations examined here, the chronic use of sedatives and opioids could exacerbate ER difficulties and impulsivity, as well as BPD symptoms. Knowledge of the precise direction of the associations among BPD symptoms, ER difficulties, impulsivity, and sedative/opioid misuse among SUD patients would highlight relevant targets for prevention and early intervention efforts aimed at preventing the co-occurrence of BPD and sedative/opioid misuse among patients dependent on other substances.
This study is also limited by its reliance on a self-report measure of drug use frequency, which may be vulnerable to recall biases, social desirability concerns, and comprehension difficulties (Johnson & Fendrich, 2005). In addition, participants were asked to report on only the frequency with which they used each substance. Although substance use frequency and severity are likely highly correlated, our measure did not adequately assess specific substance use features that would provide a better index of substance use severity (e.g., cravings, drug-seeking behaviors). Future research would benefit from the use of more comprehensive interview-based measures of substance misuse, such as the Addiction Severity Index (McLellan et al., 1992), as well as ecological momentary assessment or timeline follow-back procedures, which may facilitate more accurate responding about the frequency and severity of drug use behaviors in daily life. Additionally, this study was conducted in a residential SUD treatment facility where the majority of patients were court-ordered to treatment; thus, findings may not generalize to other populations, including SUD outpatients, SUD patients voluntarily seeking treatment, non-SUD patients with BPD, or community samples. In addition, it is important to consider that patients in residential SUD treatment typically represent more severe SUD patient populations (Chen et al., 2011). Consistent with this, all participants in this study were dependent on alcohol and/or cocaine and many were dependent on multiple substances (including and/or instead of sedatives or opioids). Thus, it is possible that our findings are unique to this particular sample and may not generalize to individuals with primary sedative or opioid dependence (in the absence of alcohol or cocaine dependence). Future research examining the negative outcomes associated with opioid and sedative misuse among individuals with BPD pathology (e.g., risk-taking behavior, treatment failure, overdose, and relapse) should take into account the population in which these associations are examined, selecting the most applicable outcomes for the population in question. Moreover, future research is needed to examine the associations among BPD symptoms, ER difficulties, impulsivity dimensions, and sedative and opioid misuse within other relevant non-SUD samples, including individuals at risk for opioid and/or sedative misuse in particular (e.g., patients with severe anxiety disorders; chronic pain patients).
Despite these limitations, the results of this study add to the small body of literature on the relationship of BPD to the use of sedatives and opioids, providing preliminary evidence for significant associations between BPD symptoms and both nonprescription and prescription sedative and opioid misuse among residential patients with alcohol and/or cocaine dependence. Extending past research in this area, results also suggest the relevance of ER difficulties and two facets of impulsivity (i.e., negative urgency and lack of perseverance), respectively, to the relationships of BPD symptoms to two of these drug use outcomes: nonprescription sedative use and prescription sedative/opioid misuse. As such, these findings highlight the potential role of emotional and behavioral dysregulation in sedative use and prescription sedative/opioid misuse among individuals with BPD pathology and co-occurring alcohol and/or cocaine dependence. Although in need of replication in larger and more comprehensive studies, further support for the role of ER difficulties, negative urgency, and lack of perseverance in nonprescription sedative use and prescription sedative/opioid misuse among individuals with BPD pathology could highlight the potential utility of targeting these mechanisms directly among alcohol and/or cocaine dependent patients with subthreshold or threshold BPD. Results also highlight the potential importance of assessing for BPD, ER difficulties, and impulsivity before prescribing sedatives or opioids to SUD patients dependent on other substances, as these factors may increase the potential for misuse of these drugs or contribute to other negative outcomes (e.g., increased risk for treatment failure or overdose).
Highlights.
Borderline personality disorder (BPD) is associated with substance use problems.
Little is known about the relation of BPD symptoms to sedative or opioid misuse.
We examined the roles of emotion regulation (ER) difficulties and impulsivity.
BPD symptoms were related to nonprescription sedative use through ER difficulties.
BPD symptoms were related to prescription sedative/opioid misuse via impulsivity.
Acknowledgments
This research was supported by National Institute on Drug Abuse Grant R21 DA030587, awarded to the second author (MTT).
Footnotes
Declaration of Interest
All authors declare that they have no conflicts of interest.
Declarations of interest: None.
The indirect relationships of BPD symptoms to frequency of nonprescription sedative use through each subscale of the DERS were also examined in a model including all subscales simultaneously. Notably, and providing support for the use of the total DERS score in the primary analyses, there were no significant indirect relationships through any of the individual subscales, including emotional nonacceptance, ab = .04, CI [−.01, .09], lack of awareness, ab = −.003, CI [−.04, .03], lack of clarity, ab = .01, CI [−.01, .03], difficulties engaging in goal directed behaviors, ab = .03, CI [−.01, .08], difficulties controlling impulsive behaviors, ab = .01, CI [−.04, .07], and lack of access to effective ER strategies, ab = −.01, CI [−.07, .05].
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Bachhuber MA, Hennessy S, Cunningham CO, & Starrels JL (2016). Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. American Journal of Public Health, 106, 686–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111, 33–51. [DOI] [PubMed] [Google Scholar]
- Bandelow B, Schmahl C, Falkai P, & Wedekind D (2010). Borderline personality disorder: a dysregulation of the endogenous opioid system?. Psychological Review, 117, 623–636. [DOI] [PubMed] [Google Scholar]
- Bateman A, & Fonagy P (2003). Health service utilization costs for borderline personality disorder patients treated with psychoanalytically oriented partial hospitalization versus general psychiatric care. American Journal of Psychiatry, 160, 169–171. [DOI] [PubMed] [Google Scholar]
- Beblo T, Pastuszak A, Griepenstroh J, Fernando S, Driessen M, Schütz A, … Schlosser N. (2010). Self-reported emotional dysregulation but no impairment of emotional intelligence in borderline personality disorder: An explorative study. Journal of Nervous and Mental Disease, 198, 385–388. [DOI] [PubMed] [Google Scholar]
- Bøen E, Hummelen B, Elvsåshagen T, Boye B, Andersson S, Karterud S, & Malt UF (2015). Different impulsivity profiles in borderline personality disorder and bipolar II disorder. Journal of Affective Disorders, 170, 104–111. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Nick B, Delany-Brumsey A, Lynch TR, … Lejuez CW (2008). A multimodal assessment of the relationship between emotion dysregulation and borderline personality disorder among inner-city substance users in residential treatment. Journal of Psychiatric Research, 42, 717–726. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Lejuez CW, Daughters SB, Rosenthal MZ, & Lynch TR (2005). Impulsivity as a common process across borderline personality and substance use disorders. Clinical Psychology Review, 25, 790–812. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Ouimette P, Crawford AV, & Levy R (2009). Testing gender effects on the mechanisms explaining the association between post-traumatic stress symptoms and substance use frequency. Addictive Behaviors, 34, 685–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Verhulst B, Webber T, McGue M, Iacono WG, & Hicks BM (2018). Genetic and environmental influences on the codevelopment among borderline personality disorder traits, major depression symptoms, and substance use disorder symptoms from adolescence to young adulthood. Development and Psychopathology, 30, 49–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, McKay JR, & Rutherford MJ (2001). Psychiatric comorbidity in patients with substance use disorders: Do not forget axis II disorders. Psychiatric Annals, 31, 321–331. [Google Scholar]
- Campbell-Sills L, Ellard KK, & Barlow DH (2014). Emotion regulation in anxiety disorders In Gross JJ (Ed.), Handbook of emotion regulation (pp. 393–412). New York: Guilford Press. [Google Scholar]
- Carcone D, Tokarz VL, & Ruocco AC (2015). A systematic review on the reliability and validity of semistructured diagnostic interviews for borderline personality disorder. Canadian Psychology, 56, 208–226. [Google Scholar]
- Carpenter RW, Wood PK, & Trull TJ (2016). Comorbidity of borderline personality disorder and lifetime substance use disorders in a nationally representative sample. Journal of Personality Disorders, 30, 336–350. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2018). U.S. opioid prescribing rate maps. Retrieved from https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html.
- Chapman AL, Dixon-Gordon KL, Layden BK, & Walters KN (2010). Borderline personality features moderate the effect of a fear induction on impulsivity. Personality Disorders: Theory, Research, and Treatment, 1, 139–152. [DOI] [PubMed] [Google Scholar]
- Chen KW, Banducci AN, Guller L, Macatee RJ, Lavelle A, Daughters SB, & Lejuez CW (2011). An examination of psychiatric comorbidities as a function of gender and substance type within an inpatient substance use treatment program. Drug and Alcohol Dependence, 118, 92–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coben JH, Davis SM, Furbee PM, Sikora RD, Tillotson RD, & Bossarte RM (2010). Hospitalizations for poisoning by prescription opioids, sedatives, and tranquilizers. American Journal of Preventive Medicine, 38, 517–524. [DOI] [PubMed] [Google Scholar]
- Cole PM, Michel MK, & Teti LO (1994). The development of emotion regulation and dysregulation: A clinical perspective. Monographs of the Society for Research in Child Development, 59, 73–100. [PubMed] [Google Scholar]
- Compton WM, & Volkow ND (2006). Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug and Alcohol Dependence, 81, 103–107. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, & Linehan MM (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135, 495–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis LH, Stoddard J, Radeva JI, Hutchison S, Dans PE, Wright A, … & Schulman KA (2006). Geographic variation in the prescription of schedule II opioid analgesics among outpatients in the United States. Health Services Research, 41, 837–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, & Smith GT (2007). Mood-based rash action and its components: Positive and negative urgency. Personality and Individual Differences, 43, 839–850. [Google Scholar]
- DeShong HL, & Kurtz JE (2013). Four factors of impulsivity differentiate antisocial and borderline personality disorders. Journal of Personality Disorders, 27, 144–156. [DOI] [PubMed] [Google Scholar]
- Ekman P, & Davidson RJ (1994). The nature of emotion: Fundamental questions. New York: Oxford University Press. [Google Scholar]
- El-Gabalawy R, Katz L, & Sareen J (2010). Comorbidity and associated severity of borderline personality disorder and physical health conditions in a nationally representative sample. Psychosomatic Medicine, 72, 641–647. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1996). Structured clinical interview for DSM-IV Axis I disorders – patient edition. New York: New York State Psychiatric Institute, Biometrics Research Department. [Google Scholar]
- Florence CS, Zhou C, Luo F, & Xu L (2016). The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Medical Care, 54, 901–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. [DOI] [PubMed] [Google Scholar]
- Franken IA, & Hendriks VM (2000). Early-onset of illicit substance use is associated with greater axis-II comorbidity, not with axis-I comorbidity. Drug and Alcohol Dependence, 59, 305–308. [DOI] [PubMed] [Google Scholar]
- Frankenburg FR, Fitzmaurice GM, & Zanarini MC (2014). The use of prescription opioid medication by patients with borderline personality disorder and axis II comparison subjects: A 10-year follow-up study. Journal of Clinical Psychiatry, 75, 357–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankenburg FR, & Zanarini MC (2004). The association between borderline personality disorder and chronic medical illnesses, poor health-related lifestyle choices and costly forms of health care utilization. Journal of Clinical Psychiatry, 65, 1660–1665. [DOI] [PubMed] [Google Scholar]
- Fritz MS, & MacKinnon DP (2007). Required sample size to detect the mediated effect. Psychological Science, 18, 233–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, & … Ruan WJ (2008). Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 69, 533–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Bornovalova MA, Delany-Brumsey A, Nick B, & Lejuez CW (2007). A laboratory-based study of the relationship between childhood abuse and experiential avoidance among inner-city substance users: The role of emotional nonacceptance. Behavior Therapy, 38, 256–268. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Dixon LJ, Kiel EJ, & Tull MT (2018). Emotion regulation: Theoretical models, associated outcomes, and recent advances In Zeigler-Hill V & Shackelford TK (Eds.), The SAGE handbook of personality and individual differences (pp. 63–89). London: SAGE Publications. [Google Scholar]
- Gratz KL, Moore KE, & Tull MT (2016). The role of emotion dysregulation in the presence, associated difficulties, and treatment of borderline personality disorder. Personality Disorders: Theory, Research, and Treatment, 7, 344–353. [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26, 41–54. [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, & Gunderson JG (2006). An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology, 115, 850–855. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Baruch DE, Bornovalova MA, & Lejuez CW (2008). Factors associated with co-occurring borderline personality disorder among inner-city substance users: The roles of childhood maltreatment, negative affect intensity/reactivity, and emotion dysregulation. Comprehensive Psychiatry, 49, 603–615. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, & Gunderson JG (2008). Preliminary data on the relationship between anxiety sensitivity and borderline personality disorder: The role of experiential avoidance. Journal of Psychiatric Research, 42, 550–559. [DOI] [PubMed] [Google Scholar]
- Grilo CM, & McGlashan TH (2000). Convergent and discriminant validity of DSM-IV axis II personality disorder criteria in adult outpatients with binge eating disorder. Comprehensive Psychiatry, 41, 163–166. [DOI] [PubMed] [Google Scholar]
- Gudin JA, Mogali S, Jones JD, & Comer SD (2013). Risks, management, and monitoring of combination opioid, benzodiazepines, and/or alcohol use. Postgraduate Medicine, 125, 115–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunderson JG, & Links PS (2008). Borderline personality disorder: A clinical guide, 2nd ed Arlington: American Psychiatric Publishing. [Google Scholar]
- Gupta S, Rosenthal MZ, Mancini AD, Cheavens JS, & Lynch TR (2008). Emotion regulation skills mediate the effects of shame on eating disorder symptoms in women. Eating Disorders: The Journal of Treatment & Prevention, 16, 405–417. [DOI] [PubMed] [Google Scholar]
- Hallion LS, Steinman SA, Tolin DF, & Diefenbach GJ (2018). Psychometric properties of the Difficulties in Emotion Regulation Scale (DERS) and its short forms in adults with emotional disorders. Frontiers in Psychology, 9, 539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press. [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, & Lillis J (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44, 1–25. [DOI] [PubMed] [Google Scholar]
- Hiebler-Ragger M, Unterrainer H, Rinner A, & Kapfhammer H (2016). Insecure attachment styles and increased borderline personality organization in substance use disorders. Psychopathology, 49, 341–344. [DOI] [PubMed] [Google Scholar]
- Hien DA, & First M (1991). Drug Use Questionnaire. Unpublished scale, Columbia College of Physicians and Surgeons, New York State Psychiatric Institute. [Google Scholar]
- Hulbert C, & Thomas R (2010). Predicting self-injury in BPD: an investigation of the experiential avoidance model. Journal of Personality Disorders, 24, 651–663. [DOI] [PubMed] [Google Scholar]
- Jacob GA, Gutz L, Bader K, Lieb K, Tusher O, & Stahl C (2010). Impulsivity in borderline personality disorder: Impairment in self-report measures, but not behavioral inhibition. Psychopathology, 43, 180–188. [DOI] [PubMed] [Google Scholar]
- Jann M, Kennedy WK, & Lopez G (2014). Benzodiazepines: A major component in unintentional prescription drug overdoses with opioid analgesics. Journal of Pharmacy Practice, 27, 5–16. [DOI] [PubMed] [Google Scholar]
- Johnson T, & Fendrich M (2005). Modeling sources of self-report bias in a survey of drug use epidemiology. Annals of Epidemiology, 15, 381–389. [DOI] [PubMed] [Google Scholar]
- Kleindienst N, Bohus M, Ludascher P, Limberger MF, Kuenkele K, Ebner-Priemer, & … Schmahl C (2008). Motives for nonsuicidal self-injury among women with borderline personality disorder. Journal of Nervous and Mental Disease, 196, 230–236. [DOI] [PubMed] [Google Scholar]
- Klonsky ED (2007). The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review, 27, 226–239. [DOI] [PubMed] [Google Scholar]
- Kornør H, & Nordvik H (2007). Five-factor model personality traits in opioid dependence. BMC Psychiatry, 7, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruedelbach N, McCormick RA, Schulz SC, & Grueneich R (1993). Impulsivity, coping styles, and triggers for craving in substance abusers with borderline personality disorder. Journal of Personality Disorders, 7, 214–222. [Google Scholar]
- Lee H, Bienvenu J, Cho S, Ramsey C, Bandeen-Roche K, Eaton WW, & Nestadt G (2010). Personality disorders and traits as predictors of incident cardiovascular disease: Findings from the 23-yearfollow-up of the Baltimore ECA Study. Psychosomatics: Journal of Consultation Liaison Psychiatry, 51, 289–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Bornovalova MA, Reynolds EK, Daughters SB, & Curtin JJ (2007). Risk factors in the relationship between gender and crack/cocaine. Experimental and Clinical Psychopharmacology, 15, 165–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzenweger MF, Lane MC, Loranger AW, & Kessler RC (2007). DSM-IV personality disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 62, 553–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leri F, Bruneau J, & Stewart J (2003). Understanding polydrug use: review of heroin and cocaine co-use. Addiction, 98, 7–22. [DOI] [PubMed] [Google Scholar]
- Linehan MM (1993). Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press. [Google Scholar]
- Links PS, Heslegrave RJ, Mitton JE, Van Reekum R, & Patrick J (1995). Borderline personality disorder and substance abuse: Consequences of comorbidity. The Canadian Journal of Psychiatry, 40, 9–14. [DOI] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33, 335–343. [DOI] [PubMed] [Google Scholar]
- Mackesy-Amiti ME, Donenberg GR, & Ouellet LJ (2012). Prevalence of psychiatric disorders among young injection drug users. Drug and Alcohol Dependence, 124, 70–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancke F, Herpertz SC, Kleindienst N, & Bertsch K (2017). Emotion dysregulation and trait anger sequentially mediate the association between borderline personality disorder and aggression. Journal of Personality Disorders, 31, 256–272. [DOI] [PubMed] [Google Scholar]
- Maraz A, Andó B, Rigó P, Harmatta J, Takách G, Zalka Z, & … Demetrovics Z (2016). The two-faceted nature of impulsivity in patients with borderline personality disorder and substance use disorder. Drug and Alcohol Dependence, 163, 48–54. [DOI] [PubMed] [Google Scholar]
- Martel MO, Dolman AJ, Edwards RR, Jamison RN, & Wasan AD (2014). The association between negative affect and prescription opioid misuse in patients with chronic pain: the mediating role of opioid craving. The Journal of Pain, 15, 90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, Morales M, & Young A (2006). Simultaneous and concurrent polydrug use of alcohol and prescription drugs: prevalence, correlates, and consequences. Journal of Studies on Alcohol, 67, 529–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, Zanarini MC, & Stout RL (2000). The collaborative longitudinal personality disorders study: Baseline axis I/II and II/II diagnostic co-occurrence. Acta Psychiatrica Scandinavica, 102, 256–264. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, … & Argeriou M (1992). The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment, 9, 199–213. [DOI] [PubMed] [Google Scholar]
- McMain S, & Ellery M (2008). Screening and assessment of personality disorders in addiction treatment settings. International Journal of Mental Health and Addiction, 6, 20–31. [Google Scholar]
- National Institute on Drug Abuse (NIDA). (2018). Misuse of prescription drugs. Retrieved from https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs on 2019, January 22
- O’Brien CP (2005). Benzodiazepine use, abuse, and dependence. The Journal of Clinical Psychiatry, 66, 28–33. [PubMed] [Google Scholar]
- Olfson M, King M, & Schoenbaum M (2015). Benzodiazepine use in the United States. Journal of the American Medical Association Psychiatry, 72, 136–142. [DOI] [PubMed] [Google Scholar]
- Osborne TL, Michonski J, Sayrs J, Welch SS, & Anderson LK (2017). Factor structure of the Difficulties in Emotion Regulation Scale (DERS) in adult outpatients receiving dialectical behavior therapy (DBT). Journal of Psychopathology and Behavioral Assessment, 39, 355–371. [Google Scholar]
- Ouzir M, & Errami M (2016). Etiological theories of addiction: A comprehensive update on neurobiological, genetic and behavioural vulnerability. Pharmacology, Biochemistry and Behavior, 148, 59–68. [DOI] [PubMed] [Google Scholar]
- Pennay A, Cameron J, Reichert T, Strickland H, Lee NK, Hall K, & Lubman DI (2011). A systematic review of interventions for co-occurring substance use disorder and borderline personality disorder. Journal of Substance Abuse Treatment, 41, 363–373. [DOI] [PubMed] [Google Scholar]
- Peters JR, Upton BT, & Baer RA (2013). Brief report: relationships between facets of impulsivity and borderline personality features. Journal of Personality Disorders, 27, 547–552. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Salsman NL, & Linehan MM (2012). An investigation of the relationships among negative affect, difficulties in emotion regulation, and features of borderline personality disorder. Journal of Psychopathology and Behavioral Assessment, 34, 260–267. [Google Scholar]
- Samuel DB, Carroll KM, Rounsaville BJ, & Ball SA (2013). Personality disorders as maladaptive, extreme variants of normal personality: Borderline personality disorder and neuroticism in a substance using sample. Journal of Personality Disorders, 27, 625–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansone RA, & Sansone LA (2012). Chronic pain syndromes and borderline personality disorder. Innovations in Clinical Neuroscience, 9, 10–14. [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, Cornelius TL, & Idema C (2011). Trait anger as a mediator of difficulties with emotion regulation and female-perpetrated psychological aggression. Violence and Victims, 26, 271–282. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, & Siever LJ (2002). The borderline diagnosis I: Psychopathology, comorbidity, and personality structure. Biological Psychiatry, 51, 936–950. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Oldham JM, & Gallaher PE (1999). Axis II comorbidity of substance use disorders among patients referred for treatment of personality disorders. American Journal of Psychiatry, 156, 733–738. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Oldham JM, Hyler SE, Stein DJ, Hollander E, Gallaher PE, & Lopez AE (1995). Patterns of anxiety and personality disorder comorbidity. Journal of Psychiatric Research, 29, 361–374. [DOI] [PubMed] [Google Scholar]
- Stanley B, & Siever LJ (2009). The interpersonal dimension of borderline personality disorder: toward a neuropeptide model. American Journal of Psychiatry, 167, 24–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone MH (1990). The fate of borderline patients: Successful outcome and psychiatric practice. New York: Guilford Press. [Google Scholar]
- Storr CL, Westergaard R, & Anthony JC (2005). Early onset inhalant use and risk for opiate initiation by young adulthood. Drug and Alcohol Dependence, 78, 253–261. [DOI] [PubMed] [Google Scholar]
- Subramaniam GA, Ives ML, Stitzer ML, & Dennis ML (2010). The added risk of opioid problem use among treatment-seeking youth with marijuana and/or alcohol problem use. Addiction, 105, 686–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2017). Key substance use and mental health indicators in the United States: Results from the 2016 national survey on drug use and health (HHS Publication No. SMA 17–5044, NSDUH Series H-52). Retrieved from https://www.samhsa.gov/data/
- Substance Abuse and Mental Health Services Administration (SAMHSA), Center for Behavioral Health Statistics and Quality (2015). Treatment Episode Data Set (TEDS): 2003–2013. State Admissions to Substance Abuse Treatment Services. BHSIS Series S-80, HHS Publication No. (SMA) 16–4964. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Suh JJ, Ruffins S, Robins CE, Albanese MJ, & Khantzian EJ (2008). Self-medication hypothesis: Connecting affective experience and drug choice. Psychoanalytic Psychology, 25, 518–532. [Google Scholar]
- Svaldi J, Philipsen A, & Matthies S (2012). Risky decision-making in borderline personality disorder. Psychiatry Research, 197, 112–118. [DOI] [PubMed] [Google Scholar]
- Thompson RA (1994). Emotion regulation: A theme in search of definition. Monographs of the Society for Research in Child Development, 59, 25–52. [PubMed] [Google Scholar]
- Tomko RL, Trull TJ, Wood PK, & Sher KJ (2014). Characteristics of borderline personality disorder in a community sample: Comorbidity, treatment utilization, and general functioning. Journal of Personality Disorders, 28, 734–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torgersen S, Kringlen E, & Cramer V (2001). The prevalence of personality disorders in a community sample. Archives of General Psychiatry, 58, 590–596. [DOI] [PubMed] [Google Scholar]
- Tragesser SL, Jones RE, Robinson RJ, Stutler A, & Stewart A (2013). Borderline personality disorder features and risk for prescription opioid use disorders. Journal of Personality Disorders, 27, 427–441. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Freeman LK, Vebares TJ, Choate AM, Helle AC, & Wycoff AM (2018). Borderline personality disorder and substance use disorders: an updated review. Borderline Personality Disorder and Emotion Dysregulation, 5, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Sher KJ, Minks-Brown C, Durbin J, & Burr R (2000). Borderline personality disorder and substance use disorders: A review and integration. Clinical Psychology Review, 20, 235–253. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Waudby CJ, & Sher KJ (2004). Alcohol, tobacco, and drug use disorders and personality disorder symptoms. Experimental & Clinical Psychopharmacology, 12, 65–75. [DOI] [PubMed] [Google Scholar]
- Tull MT, Kiel EJ, McDermott MJ, & Gratz KL (2013). The effect of trauma cue exposure on cocaine cravings among cocaine dependent inpatients with and without posttraumatic stress disorder: Exploring the mediating role of negative affect and discrete negative emotional states. Journal of Experimental Psychopathology, 4, 485–501. [Google Scholar]
- Tull MT, & Roemer L (2007). Emotion regulation difficulties associated with the experience of uncued panic attacks: Evidence of experiential avoidance, emotional nonacceptance, and decreased emotional clarity. Behavior Therapy, 38, 378–391. [DOI] [PubMed] [Google Scholar]
- Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, & Gatzke-Kopp LM (2009). Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry, 50, 1357–1364. [DOI] [PubMed] [Google Scholar]
- Verdejo-García A, Bechara A, Recknor EC, & Pérez-García M (2007). Negative emotion-driven impulsivity predicts substance dependence problems. Drug and Alcohol Dependence, 91, 213–219. [DOI] [PubMed] [Google Scholar]
- Vest NA, Murphy KT, & Tragesser SL (2018). Borderline personality disorder features and drinking, cannabis, and prescription opioid motives: Differential associations across substance and sex. Addictive Behaviors, 87, 46–54. [DOI] [PubMed] [Google Scholar]
- Vest N, Reynolds CJ, & Tragesser SL (2016). Impulsivity and risk for prescription opioid misuse in a chronic pain patient sample. Addictive Behaviors, 60, 184–190. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, & Gratz KL (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26, 453–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30, 669–689. [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, & Reynolds SK (2005). Validation of the UPPS impulsive behaviour scale: A four-factor model of impulsivity. European Journal of Personality, 19, 559–574. [Google Scholar]
- Widiger TA, & Weissman MM (1991). Epidemiology of borderline personality disorder. Hospital & Community Psychiatry, 42, 1015–1021. [DOI] [PubMed] [Google Scholar]
- Wu LT & Howard MO (2007). Is inhalant use a risk factor for heroin and injection drug use among adolescents in the United States? Addictive Behaviors, 32, 265–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen S, Zlotnick C, & Costello E (2002). Affect regulation in women with borderline personality disorder traits. Journal of Nervous and Mental Disease, 190, 693–696. [DOI] [PubMed] [Google Scholar]
- Yzerbyt V, Muller D, Batailler C, & Judd CM (2018). New recommendations for testing indirect effects in mediational models: The need to report and test component paths. Journal of Personality and Social Psychology, 115, 929–943. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, & Reynolds V (1998). Axis I comorbidity of borderline personality disorder. The American Journal of Psychiatry, 155, 1733–1739. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, & Young L (1996). Diagnostic interview for DSM-IV personality disorders. Unpublished measure. Boston, MA: McLean Hospital. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, & … Gunderson JG (2000). The collaborative longitudinal personality disorders study: Reliability of axis I and II diagnoses. Journal of Personality Disorders, 14, 291–299. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Rothschild L, & Chelminski I (2005). The prevalence of DSM-IV personality disorders in psychiatric outpatients. American Journal of Psychiatry, 162, 1911–1918. [DOI] [PubMed] [Google Scholar]