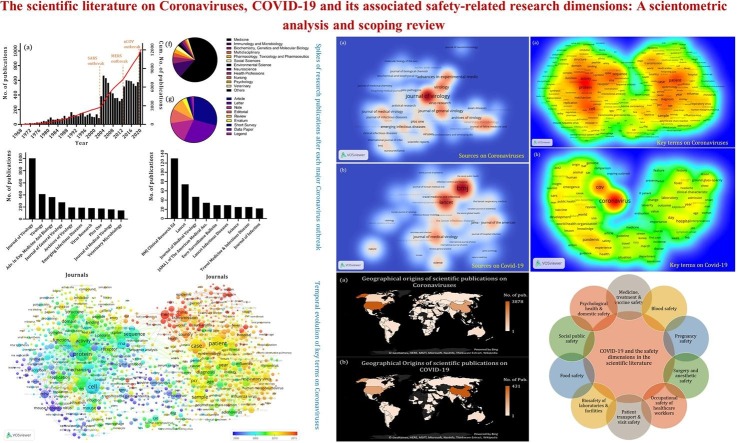
Graphical abstract
Keywords: Safety, Novel coronavirus, 2019-nCov, COVID-19
Highlights
-
•
Macro-analysing the scientific literature on Coronaviruses and Covid-19.
-
•
Identifying macro-level patterns of scholarly publications on Coronaviruses and Covid-19.
-
•
Scoping review of the safety-related research dimensions with respect to Covid-19.
-
•
Synthesising the current safety-related findings of the scientific studies on Covid-19.
-
•
Identifying underrepresented safety dimensions with respect to academic studies of Covid-19.
Abstract
The COVID-19 global pandemic has generated an abundance of research quickly following the outbreak. Within only a few months, more than a thousand studies on this topic have already appeared in the scientific literature. In this short review, we analyse the bibliometric aspects of these studies on a macro level, as well as those addressing Coronaviruses in general. Furthermore, through a scoping analysis of the literature on COVID-19, we identify the main safety-related dimensions that these studies have thus far addressed. Our findings show that across various research domains, and apart from the medical and clinical aspects such as the safety of vaccines and treatments, issues related to patient transport safety, occupational safety of healthcare professionals, biosafety of laboratories and facilities, social safety, food safety, and particularly mental/psychological health and domestic safety have thus far attracted most attention of the scientific community in relation to the COVID-19 pandemic. Our analysis also uncovers various potentially significant safety problems caused by this global health emergency which currently have attracted only limited scientific focus but may warrant more attention. These include matters such as cyber safety, economic safety, and supply-chain safety. These findings highlight why, from an academic research perspective, a holistic interdisciplinary approach and a collective scientific effort is required to help understand and mitigate the various safety impacts of this crisis whose implications reach far beyond the bio-medical risks. Such holistic safety-scientific understanding of the COVID-19 crisis can furthermore be instrumental to be better prepared for a future pandemic.
1. Introduction
The challenges of combating the novel Coronavirus pandemic have put a halt to many economic and socio-cultural activities in many societies across the globe. On the other hand, it has triggered an avalanche of scientific research, both within and outside the medical domain, in order to help communities overcome this challenge by minimising its adverse impacts. The enormity of these scientific efforts and the speed at which the knowledge on this topic has been generated pose significant difficulties for everyone to stay abreast of these developments. In an effort to address this challenge and to help better organise these emerging and rapidly developing scientific outcomes, in this short review, we conduct a macro-scale analysis of the scientific literature on Coronaviruses in general, as well as the novel Coronavirus (COVID-19) in particular. We also more closely examine the literature published on COVID-19 with safety components to identify the dimensions of research that have so far been addressed by the scientific community with respect to safety. Apart from the significance this may have to curb the impacts of the current crisis, a holistic view on what safety dimensions are relatively well covered scientifically and which have so far attracted less academic focus, can be instrumental to direct future research efforts. Scientifically analysing and understanding the various safety implications of the COVID-19 pandemic as widely as possible can furthermore help societies to be better prepared for future pandemic outbreaks, and ultimately support informed decision-making in light of societal values.
Research on Coronaviruses in general dates back to 1960s and the literature on this topic is quite well established. The sub-domain of this academic field of research focusing on COVID-19, however, is understandably just an emerging and fast developing field. In Section 2, we discuss the method by which the bibliometric data related to these segments of the literature has been obtained. It will be shown through the macro-level analysis of this literature in Section 3 that, within the last two decades, each major outbreak of a Coronavirus has been immediately followed by a quick surge in the number of scientific studies on the topic and a slow gradual decline afterwards. However, the surge of studies triggered by the latest outbreak, i.e. that of COVID-19, appears to be the largest of all by far, which may be a reflection of the magnitude of the crisis that this new disease has caused. Studies from various disciplines – far beyond medicine and immunology as central fields to understand and mitigate the disease itself – have already emerged on this topic. This includes fields within social sciences, environmental sciences, psychology and veterinary sciences (Decaro et al., 2020), and many more. Clearly, safety has been a distinct focus of interest among these studies. As the micro-level scoping analyses of this work in Section 4 demonstrate, at least ten major dimensions of safety research can be identified that have so far attracted the attention of the scientific community. The scholarly efforts on these safety dimensions and their findings and recommendations are synthesised here to help further invigorate academic investigations into the safety impacts of this pandemic. This can be important for informing policies in the face of this emergency. Section 5 concludes the findings while also identifying and discussing a selective list of potential safety-related dimensions with respect to this pandemic that are currently underrepresented in the scholarly domain. These may warrant further attention by the safety research community as the scale and scope of this crises become clearer, not in the least to facilitate wider understanding of the various safety implications as a basis for improved societal preparedness and response to future pandemic outbreaks.
2. Data and methods
Bibliographic details of the scientific literatures on Coronaviruses in general and COVID-19 in particular were retrieved from Scopus, one of the main databases of academic publication records (Mingers and Leydesdorff, 2015). The searches for establishing the datasets used in this article were last updated on 9 April 2020. To obtain the reference database for Coronaviruses the title and abstract of the scientific publications were searched for the term Coronavirus* (including its variations). A total of 12,109 items were obtained. In relation to the COVID-19 literature, the following combination of search terms was used in a title-abstract-keyword search to identify and retrieve the relevant literature: “COVID-19” OR “coronavirus disease 2019” OR “2019-nCov” OR “2019 Novel Coronavirus”. In total, 1,239 search outcomes were obtained.
The bibliographic details of both reference databases (i.e. 12,109 items associated with Coronaviruses and 1,239 items associated with COVID-19), including the list of authors, title, year of publication, source title, volume, issue, page numbers, author affiliations, abstracts, author keywords, index keywords, list of references, document type and some other details, were exported and analysed using scientometric methods. Both databases are accessible as Online Supplementary Material of this article. Table A1, Table A2 in the Appendix provide a list of authors, countries, funding sponsors, institutes and sources with the highest number of publications on these two topics respectively. The tables also provide a list of top subject areas in which these publications have been listed.
For the above datasets on Coronaviruses and COVID-19, scientometric methods are applied in Section 3 to obtain high-level insights in the development of these research domains. Apart from elementary statistics and standard visualization graphs, we apply the VOSviewer software (Van Eck and Waltman, 2010). This tool implements the visualization of similarities approach (Waltman et al., 2010) and is widely used in the wider academic and safety science literature to map clustered networks of authors, journals, collaborating countries, and co-citations. Moreover, VOSviewer also implements text mining algorithms to identify noun phrases from title and abstract of the publications, from which networks, clusters, and heatmaps can be constructed (van Eck et al., 2010). In Section 3, VOSviewer is used to map journal networks of the literature on Coronaviruses and COVID-19, as well as term clusters and heat maps of frequently occurring terms in these datasets.
Lastly, in order to identify the main dimensions of safety research that have thus far been addressed in the scholarly domain, a scoping review methodology is applied. Such review type is suitable for assessing what is the potential size and scope of the available research literature, and can primarily serve as a basis for directing further research efforts (Grant and Booth, 2009). To this effect, the aforementioned keyword search combination associated with COVID-19 was combined with the term “safety” through the AND-operator. The search included the title, abstract, and keywords of the articles. This search resulted in a total of 41 articles which were individually studied and filtered out depending on the extent of their relevance to safety research. Among those, 34 items were deemed relevant. Table A3 in the Appendix provides a synthesis of the methods, findings, and recommendations of these articles (where applicable) as well the safety dimensions to which they relate. These dimensions will be outlined in Section 4.
3. Macro-level analysis of the literature
All publications on COVID-19 expect for one item were listed as 2020 publications. As to the literature addressing Coronaviruses, the oldest items found was an item listed as short survey published by Nature in 1968. In that publication a group of virologists are named who recognised a then-new group of viruses called Coronaviruses (Almeida et al., 1968).
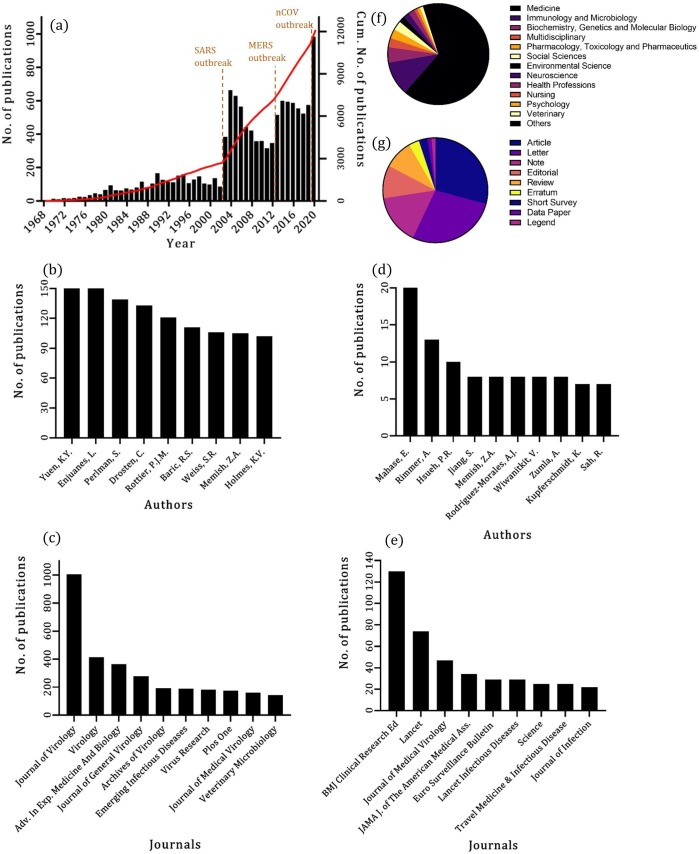
Fig. 1 (a) visualises the temporal development of the publications on Coronaviruses since 1968, i.e. the distribution of the scientific publications over the years, as well as the cumulative number of publications. Three clear spikes in the number of publications can be observed: one in 2003 (followed by another year of increased number of publication and then a gradual decline), one in 2013 (again, followed by another year of increased number of publication and then a slight decline), and the last one in 2020. The fist spike coincides with the SARS (Sever Acute Respiratory Syndrome) outbreak in 2002 and 2003 (Dodd and Stramer, 2020, Law et al., 2020). The second one is attributable to the MERS (Middle East Respiratory Syndrome) outbreak in 2012 (Sheng et al., 2020), which reinvigorated the scholarly attention to Coronaviruses. Evidently, the last spike follows the current COVID-19 outbreak. Fig. 1 (d) and (f) respectively illustrate the authors and journals with greatest number of publications on Coronaviruses. The Journal of Virology has published by far the most items on this topic, with journals such as Virology, Advances in Experimental Medicine and Biology following at a considerable distance. The figure also shows that the top-10 journals all focus on virological and medical topics.
Fig. 1.
Summary statistics on bibliographic details of the studies published on Coronaviruses and COVID-19. (a) The temporal distribution of the publications on Coronaviruses as well as their cumulative number of publications (data for 2020 only represents the first three months). Plots (b) and (c) show most published authors and journals on Coronaviruses respectively. Plots (d) and (e) show authors and journals with the highest number of publications on COVID-19 respectively. Plots (f) and (g) respectively show the top subject areas and top document types for publications on COVID-19.
Focusing on the reference database of the studies on COVID-19, Fig. 1 shows the subject areas (part (b)), article types (part (c)), authors (part (e)) and journals (part (g)) with the highest number of publications on this topic. Understandably, most publications on COVID-19 have thus far appeared in journals listed under the field of Medicine, highlighting the concerted efforts on clinical aspects of the fight against this pandemic, compared to which all other aspects currently have received much less scientific attention. Interestingly, only under 40% of these publications are articles, whereas a substantial portion of the contributions to this domain are in the form of letters, notes, editorials and reviews. British Medical Journal (Clinical Research ed.) (BMJ) and Lancet have so far published the highest number of items on this topic, having collectively published nearly 37% of all publications on COVID-19 thus far.
The bibliographic coupling of the sources that have published studies on the Coronaviruses and COVID-19 is further analysed using VOSviewer (Van Eck and Waltman, 2013), an open-access software for bibliometric analysis as outlined in Section 2 (Mingers and Leydesdorff, 2015). Fig. 2 illustrates the outputs of this analysis. The bibliographic networks visualised in Fig. 2 through heat maps associated with each topic are based on the number of the references that publications of each source share with each other on each of the two topics of interest. Two journals are bibliographically coupled when their documents published on our topic of interest cite one or more document(s) in common, and the higher the number of their shared references, the stronger their coupling relationship. The more intensely the red shade corresponding to the journal name, the more dominant the journal as a knowledge outlet. The spatial closeness between journals corresponds to the number of references that publications of those sources share in each database. The results provide insights in the publication intensity across journals, complementary to Fig. 1(c) and (e).
Fig. 2.
Heat map of the sources that have published studies on (a) Coronaviruses and (b) COVID-19. In (a) and (b) the minimum number of documents of a journal to be visualised is respectively 20 and 5. The item weights are proportional to the number of documents published by each source.
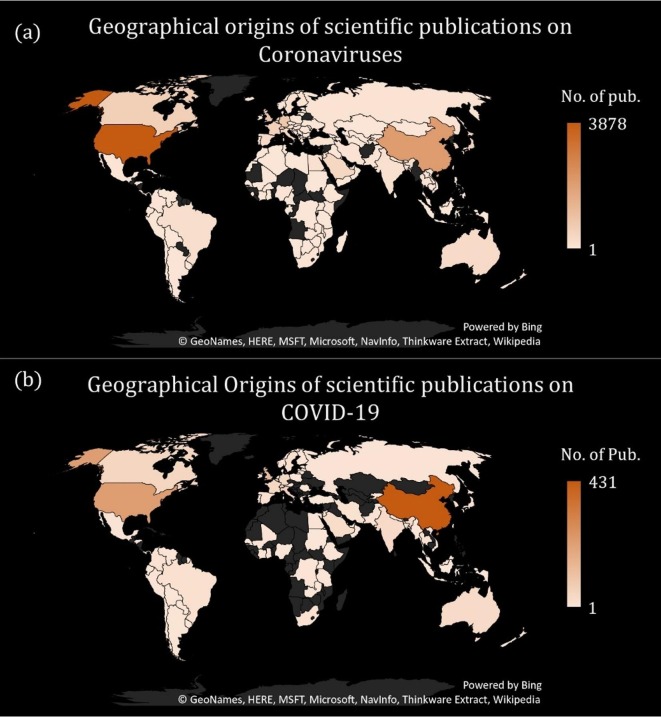
Fig. 3 visualises the number of publications originating from various geographical regions of the world based on the Scopus data on the country of submission. While researchers in the United States have contributed the highest number of research items to the topic of Coronaviruses, followed by Chinese authors, this order is reversed for the literature published on COVID-19. On COVID-19, nearly 30% of all published studies have thus far originated from China, with the United States accounting for nearly 14%. Research outputs originating from other geographical areas are currently significantly less voluminous, with gaps apparent especially in Africa, Eastern Europe, and Central Asia.
Fig. 3.
The distribution of the geographical origin of the scholarly publications (a) on Coronaviruses, (b) on COVID-19.
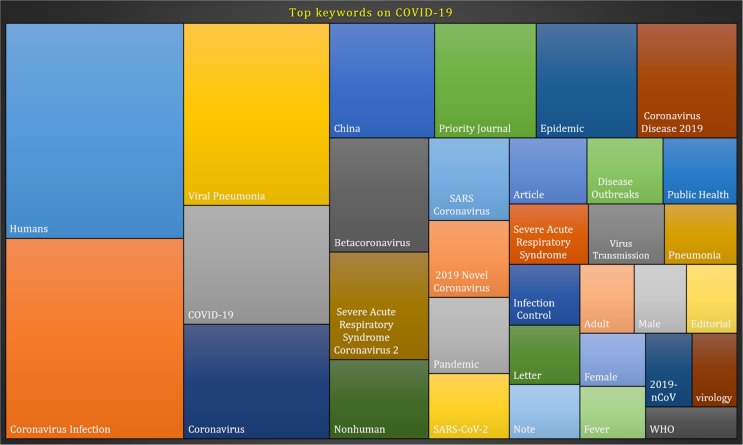
Finally, a keyword analysis is conducted using VOSviewer, on the terms appearing in the title and abstract of the publications on the datasets on Coronaviruses and COVID-19. The most frequently used keywords in title and abstract of the studies so far published on COVID-19 are illustrated in Fig. 4 where the size of each rectangle is proportional to the frequency of the term. The terms human* and Coronavirus infection* and viral pneumonia (including their variations, humans, Coronavirus infections and pneumonia virus) appear to be the most frequently used terms in the title and abstracts of publications on COVID-19. The fact that COVID-19 is from the family of the Coronaviruses has a clear reflection on the key terms of the publications with Coronavirus being also a top term. The relation of the virus to China as the geographical region where the outbreak began has also been reflected in the key terms with China being one of the most used terms.
Fig. 4.
Most frequent terms appeared in the title and abstract of the publications on COVID-19 based on the Scopus analyse search results.
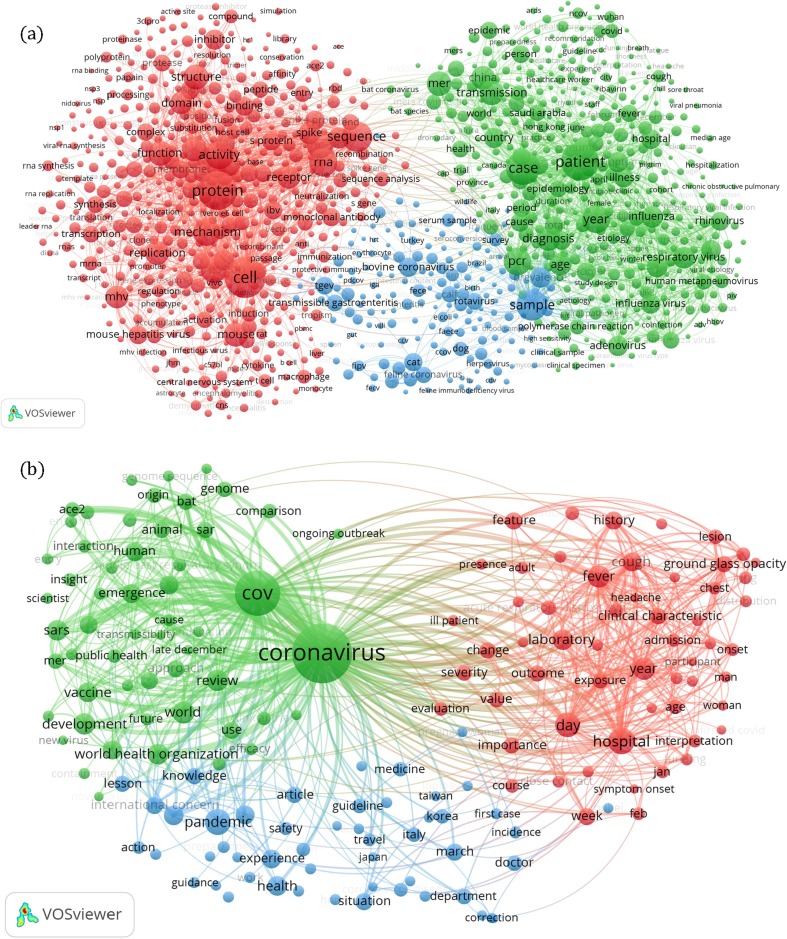
Fig. 5 presents a more detailed output of the scientometric mapping analysis for both Coronaviruses and COVID-19 topics. The network of most frequently occurring key terms are shown in Fig. 5, whereas the corresponding heat maps are shown in Fig. 6 . In the network images, the size of each node is proportional to the appearance frequency of associated term. The relatedness of the key terms is also based on the number of times that they appear in the same publication. More related key terms are generally visualised in closer proximity to each other, while the colours in the network visualisation represent the clusters of related key terms. In publications related to coronaviruses, as well as for the publications on COVID-19, three distinct clusters are detected.
Fig. 5.
The network of the hot terms associated with publications on (a) Coronaviruses and (b) COVID-19.
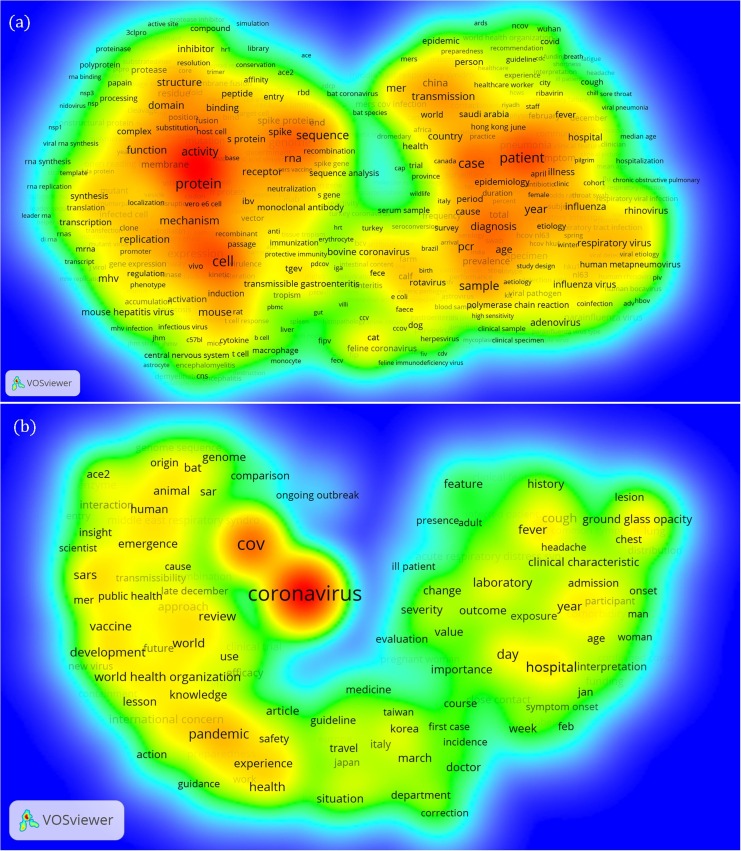
Fig. 6.
The heatmap of the network of the hot terms associated with publications on (a) Coronaviruses and (b) COVID-19.
In Fig. 5(a), which addresses Coronaviruses, the red cluster focuses on biomedical sciences, addressing aspects of medical microbiology and genetic epidemiology. As seen from Fig. 6(a), important terms in this cluster relate to phenomena at the cell level, with terms such as ‘gene’, ‘sequence’, ‘structure’, ‘protein’, ‘receptors’, and ‘rna’. The blue cluster appears to focus on veterinary virology, with terms such as ‘bovine coronavirus’, ‘feline coronavirus’, ‘cat’, ‘dog’, ‘transmissible gastroenteritis’, and ‘rotavirus’. Terms associated with lab animals (‘rat’, ‘mouse’) however appear in the red cluster. The green cluster focuses on medical science and patient and public health, with terms such as ‘patient’, ‘case’, ‘diagnosis’, ‘illness’, ‘hospital’, ‘influenza’, ‘transmission’, and ‘epidemic’. It also contains terms related to symptoms which are associated with Coronaviruses, such as ‘fever’, ‘cough’, ‘chill’, ‘sore throat’, and ‘viral pneumonia’. Finally, it contains names of countries, regions, or cities which play an important role in the outbreak, and/or from where significant research originates. Examples include ‘Hong Kong’, ‘Wuhan’, ‘Saudi Arabia’, and ‘Italy’.
The term cluster and heat maps on COVID-19 in Fig. 5(b) and Fig. 6(b) show a somewhat similar picture, although it is understandably somewhat less developed. The green cluster focuses on the origin and cause of the new Coronavirus, with terms such as ‘cause’, ‘bat’, ‘human’ and ‘interaction’. It also includes a narrative addressing the public health implications of the outbreak and the response of the medical sciences, with terms such as ‘vaccine’, ‘development’, ‘transmissibility’, ‘public health’, ‘scientist’, and ‘insight’. Comparisons with other viruses, such as ‘mer’, and ‘sars’ are also apparent. The red cluster in Fig. 5(b) focuses on the clinical characteristics of the disease, with terms such as ‘cough’, ‘fever’, ‘headache’, ‘chest’, and on differences between the sexes. Another apparent narrative includes the public health response, with terms such as ‘laboratory’, ‘hospital’, and ‘exposure’. The blue cluster appears to focus on the actions and response to the pandemic to ensure safety and health, with terms such as ‘knowledge’, ‘lesson’, ‘experience’, ‘guideline’, and ‘travel’. Overall, the term cluster and heat map of COVID-19 in Figs. 5(b) and 6(b) show narratives focusing more on the immediate response to the disease outbreak, whereas the maps in Figs. 5(a) and 6(a) for Coronaviruses include more established scientific knowledge.
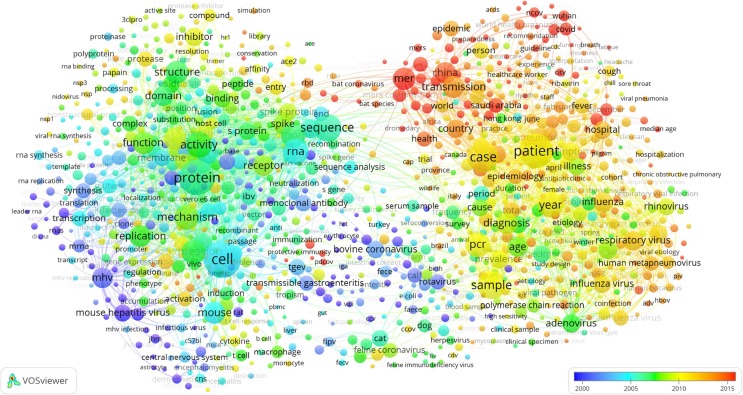
Fig. 7 visualises the network of key terms on Coronaviruses (corresponding to the network structure of Fig. 5(a)), overlaid with the colour-coding of the average year of publications when the terms have appeared. According to this map, the terms ‘MERS COV’, ‘COVID’ and ‘nCov’, ‘Wuhan’, ‘China’, and ‘bat coronavirus’ are all very recent terms in the scientific literature, for example compared to the terms ‘bovine coronavirus’ and ‘feline coronavirus’. Generally, it is apparent that the blue cluster from Fig. 5(a), focusing on veterinary virology, is the oldest. The red cluster from Fig. 5(a), which addresses aspects of biomedical sciences, is comparatively younger, while the green cluster, focusing on the public health implications, is comparatively the youngest. This suggests a scientific progress of discovery and study of Coronaviruses amongst animals, followed by viological, microbiological, genetic epidemiological, and medical studies, and finally clinical work and studies on public health. The fact that there is a sizeable body of academic literature on Coronaviruses, as observed from Fig. 1(c), with significant knowledge of their various biomedical aspects available since about 2005 as seen in Fig. 7, gives hope that clinical treatments for COVID-19 are attainable.
Fig. 7.
The network of the hot terms associated with publications on Coronaviruses overlaid with a colour-coding of the average year of publications in which each term has appeared. The minimum number of occurrences for each term to be included in the map is 30 times.
4. Scoping review of the COVID-19 literature in light of safety-related research dimensions
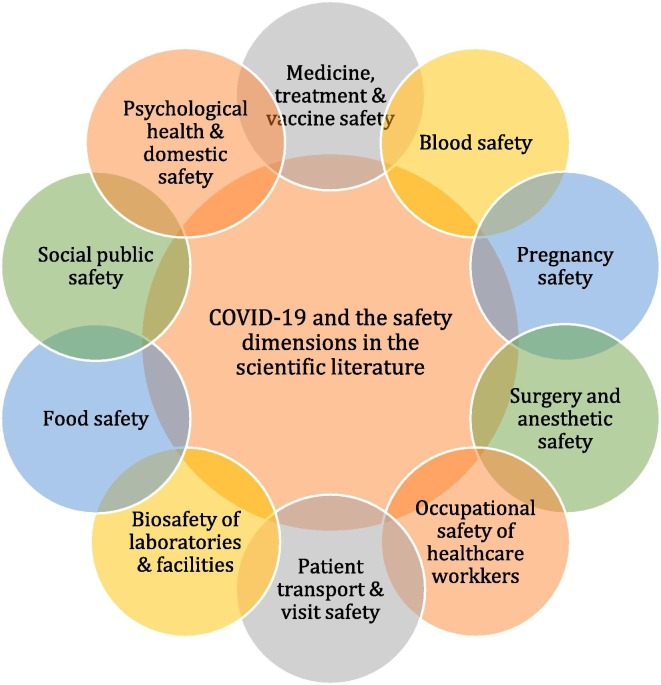
With a very high-level overview of the literature on Coronavirus and COVID-19 provided in Section 3, we turn in this Section to the safety-related aspects of COVID-19 on which scientific works have been published. Table A3 lists the studies on the COVID-19 pandemic where safety-related aspects were prominently considered, according to the search strategy outlined in Section 2. For each identified publication, the table lists the safety dimension in focus, the study method applied in the work, the key message or finding concluded from the work, and key recommendations given for practical implementation or further research. This information is extracted from the documents based on a close reading strategy (Paul and Elder, 2019) where the safety-related dimensions are interpreted and grouped based on the contents of the articles and the authors’ experiences with the safety sciences. Fig. 8 summarises the ten safety-related dimensions which were identified in the safety-focused publications related to COVID-19. These dimensions are briefly described in the following.
Fig. 8.
Research dimensions related to the safety impact of the COVID-19 pandemic addressed by academic studies.
4.1. Medicine, treatment and vaccine safety
Among the emerging scholarly efforts in addressing the safety concerns of the COVID-19 global emergency, a significant portion of the studies have understandably focused on aspects related to the safety of medicine, treatment and vaccines as one of the most urgent matters in battling this pandemic (Cellina et al., 2020, Gray and Belessis, 2020, Schlagenhauf et al., 2020, Sodhi and Etminan, 2020, Zhang, 2020, Zheng et al., 2020a). In doing so, many studies have synthesised the scientific evidence regarding the safety and efficacy of various treatments based on experiences obtained from previous pandemics of similar nature, such as SARS and MERS. Highlighting the high degree of genetic similarity between SARS-COV and COVID-19, an overview by Chen et al. (2020d) outlines various vaccine development programs and different vaccine technologies that are currently being examined based on experiences with SARS. They emphasise that these vaccine strategies need to be evaluated for their safety and efficacy, with specific consideration for issues specific to vaccination of vulnerable populations such as elderly and those with debilitating chronic conditions. A considerable amount of scientific efforts is focused on the development of treatments, concerning which several studies appeared on the safety and efficacy of chloroquine and its variants such as hydroxychloroquine (Liu et al., 2020a) as potential treatment for COVID-19 (Cortegiani et al., 2020, Devaux et al., 2020). The study of Cortegiani et al. (2020) is a systematic review of the safety and efficacy of chloroquine for the treatment of COVID-19. It reflects the evidence from the ongoing clinical trials and suggests that the current promising evidence justify more clinical research into this potential treatment. Devaux et al. (2020) also suggest that the preliminary trials of chloroquine in China have been promising in terms of both safety and efficacy, which has led to several new trials.
4.2. Blood safety
Blood safety has been another matter of interest among the studies on COVID-19 that have emerged from the medical fields (Dodd and Stramer, 2020). The study of Chang et al. (2020) highlights the commonness of viral shedding in plasma or serum in coronaviruses, suggesting a transmission risk through transfusion of blood products. In their study, they review the existing evidence regarding the transmission of SARS, MERS and SARS-Cov2 through blood products and outline different methods for inactivation of coronavirus in blood products.
4.3. Pregnancy safety
A cohort of studies have investigated issues surrounding the safety of pregnancy in relation to COVID-19 (Al-Tawfiq, 2020, Chen et al., 2020a, Luo and Yin, 2020, Rasmussen et al., 2020, Schwartz and Graham, 2020, Zambrano et al., 2020). The study of Schwartz and Graham (2020) reviews the published data on epidemiological and clinical effect of SARS and MERS and other coronavirus infections on pregnant women and their infants. They provide recommendations for including pregnant women in the design of COVID-19 vaccine trials. Based on a retrospective review of the clinical records of pregnant women with confirmed COVID-19 pneumonia, Chen et al. (2020a) suggest that the clinical characteristics of these patients were similar to those non-pregnant adult patients with COVID-19. They furthermore find no evidence of vertical transmission from pregnant women to their infants who develop COVID-19 during late pregnancy. The study of Rasmussen et al. (2020) lays out various dimensions and principles of management of COVID-19 disease in pregnancy.
4.4. Surgery and anesthetic safety
Considerations have been given regarding safety of surgery and anesthesia (Aslam and Mehra, 2020, Kang et al., 2020b, Ng et al., 2020, Rasmussen and Koelling, 2020, Wang et al., 2020c) for COVID-19 patients, both from the perspective of patient safety (Chen et al., 2020b) and from the safety of medical staff (Givi et al., 2020). Based on the clinical records of 17 patients, the study of Chen et al. (2020b) discusses the management and safety of general anesthesia for Caesarean delivery in COVID-19 patients, including issues related to patient transfer, biosafety precautions, and the protection of the medical staff involved in the surgery. Based on a review of the literature and through communications with physicians, Givi et al. (2020) also provide a set of safety recommendations related to the diagnostic and therapeutic procedures of the neck and upper aerodigestive tract diseases (Lovato et al., 2020) in patients with COVID-19.
4.5. Occupational safety of healthcare workers
Considering that medical professionals are at a higher risk of exposure, the occupational safety of healthcare professionals has been a major focus of research in relation to COVID-19 (Ambigapathy et al., 2020, Belingheri et al., 2020, Chen et al., 2020e, Cheung et al., 2020, Joob and Wiwanitkit, 2020, Yifan et al., 2020). Cheung et al. (2020) argue that medical professionals who are involved in aerosol-generating procedures for COVID-19 patients, such as non-invasive ventilation or intubation, have a particularly higher infection risk. Based on their experience in an intensive care unit, they describe procedural safety recommendations which aim to help manage the risk to healthcare staff while maintaining quality care. Ambigapathy et al. (2020) provide a list of recommendations based on a review of the literature as to how front-line general practitioners should safely use Personal Protective Equipment (PPE) and discuss the importance of educating patients about PPE.
4.6. Patient transport and visit safety
A number of studies have discussed the issues related to the safety of patient transport. Based on the principles related to the influenza pandemic, Liew et al. (2020) outline a set of recommendations for safe patient transport for both suspected and confirmed cases, for both inter- and intra-hospital transports. To mitigate the risks involved in the transport of suspected COVID-19 cases, there have been models of care that avoid face-to-face contact between clinicians and patients which can also reduce the risk to the medical professionals. The method of video consultation has been discussed by Greenhalgh et al. (2020), who provide evidence from randomised trials showing that video consultations have been associated with high patient and staff satisfaction, lower care cost, and no significant difference in disease progression. They however highlight that such evidence underrepresents cases of patients with acute and potentially serious illness such as COVID-19. They compare the benefits and potential downsides of video consultations, in particular in relation to the COVID-19 disease.
4.7. Biosafety of medical facilities
The biosafety of laboratories and medical facilities has also attracted the attention of researchers in relation to COVID-19 pandemic (Hamzavi et al., 2020, Sultan et al., 2020, Xu et al., 2020). For example, the study of Kooraki et al. (2020) reviews precautions and safety measures specific to radiology departments in relation to dealing with known or suspected COVID-19 patients. These recommendations are meant to help manage the impact of the COVID-19 outbreak on the department and staff in the radiology departments and are thus also related to the topic of occupational safety. They argue that this requires a multidisciplinary committee to convene and outline such safeguarding guidelines. From a different perspective, Nie et al. (2020) discuss the biosafety considerations involved in the handling of the pseudo-virus for Coronaviruses. This requires level 3 biosafety facilities, which the authors highlight as one of the obstacles on the way of vaccine development. Consequently, they propose a series of pseudo-virus-based neutralisation assays and protocols for SARS-COV-2 which are safer and can be handled in biosafety level 2 facilities.
4.8. Food safety
Shariatifar and Molaee-aghaee (2019) highlight the food safety issues in relation to the COVID-19 pandemic. They list traditional and modern methods of inactivating viruses in food. Furthermore, they provide recommendations related to people’s behaviour, including both consumers and procedures, during the handling of the food product that can mitigate the risk of virus spread. From a different perspective, Yuan et al. (2020) provide recommendations regarding food safety, in order to prevent the exposure of humans to novel viruses from wild animals. This includes enhancing public awareness, establishing legislations on eating and trading wild animals, and putting in place mechanisms of market supervision to ensure food safety standards.
4.9. Social safety
The viewpoint written by Bachireddy et al. (2020) discusses the significant role of the Medicaid programs as an important social public safety net in the United States in the face of the COVID-19 pandemic. They argue how this pandemic has exposed gaps in the social safety net in the United States and discuss how through a series of actions, Medicaid programs could play a key role in protecting the public and supporting public health efforts in the battle with this pandemic. These recommendations cover dimensions such as the flexibility to maintain or increase enrolment, expanding the options to cover tele-visits, removing berries to billing related to diagnosis and treatment, expanding home-based care coverage, easing limits on prescription drugs, and assisting special segments of the population.
4.10. Mental/psychological health and domestic safety
In addition to the biological health and safety of the general population as well as healthcare professionals, a stream of research has also addressed potential threats to the mental/psychological health and domestic safety challenges posed by the COVID-19 crisis (Dalton et al., 2020, Davis et al., 2020, Joob and Wiwanitkit, 2020, Kang et al., 2020a, Liu et al., 2020b, Montemurro, 2020, Shi and Hall, 2020). It is clear that psychological well-being and physical safety are intrinsically interconnected and cannot be reasonably categorised as fully separate safety dimensions. Severe depression and anxiety can lead to self-harm and even suicide and domestic violence which all affect the physical well-being of individuals. Nevertheless, the focus of studies in this stream is on the indirect mental health impacts of this global epidemic rather than the biological and clinical aspects.
In line with these efforts, Li et al. (2020) conducted a machine learning and sentiment analysis of the Chinese microblogging website Weibo posts during the outbreak. Their observations indicate increased negative emotions including anxiety and depression, increased sensitivity to social risks, and declined happiness and life satisfaction in the population. Barari et al. (2020) also sampled and surveyed Italian population and concluded that people, even those who do not trust the government, generally accept the public health messages during this crisis. Compliance is generally high although slightly lower among young adults. Their survey also indicated that the quarantine has started to have serious negative effects on mental health. In light of their findings, they proposed that communications during the crisis should shift focus from mere advice to stay at home to more informative and constructive behavioural interventions, such as activities that can counter the impact of isolation. The study of Wang et al. (2020a) reports on another survey of the general public in China aiming to better understand the psychological impact of the COVID-19 outbreak. Their findings indicate that more than half of the studied population rated the psychological impact of the outbreak as moderate or severe. Women, students, and individuals with poor self-rated health were observed to be associated with greater levels of stress, anxiety, and depression.
In a letter to the editor, Alves et al. (2020) highlight the potential impact of this crisis on heightening the risk of family violence particularly in rural areas and especially in families with a history of recurrent domestic violence. They argue for intensifying protective measures during this pandemic. Along the same lines, another study has highlighted the potential effects of domestic violence on children during isolation (Bradbury-Jones and Isham).
Managing mental health challenges faced by healthcare workers during the pandemic has been another issue of concern in scholarly studies. Greenberg et al. (2020) highlight the problem of ‘moral injury’ that could potentially lead to suicide among healthcare workers. Cases of suicide have unfortunately already been recorded among healthcare professionals since the recent outbreak (Jun et al., 2020, Schwartz and Graham, 2020). Greenberg et al. (2020) provide a list of measures that can be taken in order to protect healthcare workers from the potentially harmful effect of moral injury during this emergency.
5. Discussion, future research directions, and conclusions
The unprecedented rate at which scientific publications related to the COVID-19 pandemic are emerging, and the large societal concerns related to many aspects related to the impacts of the pandemic, makes synthesising scientific knowledge more important than ever. In light of this, the aim of the current work was to capture, document and demonstrate the extent and scope of the scholarly research efforts that have been conducted on COVID-19 and the general class of coronaviruses. In particular, various relevant research dimensions of the interest to the safety research community are identified, which may help practitioners and decision makers understand relevant aspects of occupational, physical, medical, and public safety.
Rapid and timely accumulation of knowledge and empirical evidence is critical for policymakers and emergency managers faced with this crisis to maximally inform their decisions through scientific evidence. This also requires a systematic re-visiting of the existing knowledge to identify gaps and overlooked areas in order to better guide and mobilise the expertise of academics towards effective solutions. It is hoped that this study can contribute towards accelerating and facilitating these scientific efforts and bringing the safety-implications of this global emergency to the attention of the safety research community. Such implications, as demonstrated by the scientometric analyses and the scoping review, go far beyond the biological and immunological aspects and of the research on vaccines and medical treatment, which are obviously scientific priorities. Rather, these safety implications also include factors related to the non-physical safety and mental wellbeing of the public and particularly medical professionals, as well as issues related to the protection of social safety, food safety, patient transport safety and the biosafety of facilities and laboratories. As evidenced by this review, a great portion of the knowledge that is being leveraged today in the fight against the COVID-19 disease has been obtained as a result of the research efforts that were made in response to previous pandemics of similar nature (Bruinen de Bruin et al., 2020, De Giorgio, 2020, Feng et al., 2020, Hatchett et al., 2007, Lee et al., 2020, Viner et al., 2020, Wang et al., 2020d, Zhang and Qian, 2020).
Clearly, further accumulation of scientific research during and after the current epidemic could equip human societies and help them better prepare for health emergencies of global scale in the future. In this regard, the current work aims to highlight the safety dimensions related to which some research has already been published in connection to the COVID-19 pandemic. The authors hope that this can inspire other academics to identify gaps in the scope of the presented safety dimensions, in an effort to build an as diverse as possible picture of the safety implications of the current pandemic. Casting a wide net of pandemic-related safety research now can greatly facilitate societal and organizational learning in handling future pandemics. In this regard, it is highlighted that according to the Global Risks Report 2020 (WEF, 2020), infectious diseases is ranked the second-highest societal risk (after water crises), with only a few technological, geopolitical, and environmental risks higher rated. Thus, considering also that epidemic outbreaks have occurred relatively frequently in the past as shown e.g. in Fig. 1(a), building safety-related knowledge for the current pandemic now, may contribute to better preparedness and response for the next outbreak.
Moving beyond the obvious medical safety implications of the COVID-19 pandemic –such as the safety of vaccines, medicine, treatments, patient visits, laboratory testings– that have so far dominated the scholarly efforts in this domain, we would like to highlight a selective list of potential safety dimensions that, according to the presented scoping review, have not been represented in the published studies.
One example concerns the sudden shift of the educational, economic, business, clinical care and many other activities to the online domain during this global emergency, which could potentially create unprecedented concerns with respect to the cyber safety of both individuals and institutes. The physical isolation itself could potentially give rise to a sharp increase in the use of social media and even dating websites and online shopping. On such platforms, problems such as cyber bullying and information safety, are important emerging issues (Antoniadou and Kokkinos, 2015, Bi et al., 2019). Academics may pay more attention to this aspect of safety, which could affect individuals, institutes and businesses, under the unique circumstances this pandemic entail.
Our analysis alluded to a limited research effort on the implications of this epidemic on economic and social safety (Bayham and Fenichel, 2020), such as the study of Bachireddy et al. (2020) outlining how Medicaid programs could be utilised to act as a social safety net in the United States. However, more studies seem to be warranted on the effectiveness, equity, and sustainability of implemented policies and legislative actions to help protect the economic safety of societies at both micro and macro levels to mitigate or manage the financial fallouts caused by the epidemic (Hafiz et al., 2020, Kabir et al., 2020, Murphy et al., 2020, Van Lancker and Parolin, 2020). More also needs to be understood about the ways to protect the mental and physical health as well as social safety of vulnerable populations such as those of the low-income demographics (Van Lancker and Parolin, 2020), community dwelling older adults (Kuwahara et al., 2020), children and adolescents in temporary accommodations (Rosenthal et al., 2020), or migrants and refugees in temporary accommodations (Bozorgmehr et al., 2020, Daw, 2020, Kabir et al., 2020, Kluge et al., 2020).
In terms of occupational safety, the scoping review indicated that there has been some work addressing primarily the occupational safety of healthcare workers and staff in medical testing facilities. However, it is evident that in many countries, many workers in so-called essential services were tasked to remain professionally active to keep some key societal functions and utilities running. It is apparent that several such worker categories were exposed to higher infection risks than the general public, including grocery store staff, public transport and taxi drivers, and nursing home workers. With most of these workers having no prior knowledge of how to handle their personal safety in pandemics, anxiety and stress are important occupational hazards which would be important to build scientific evidence about. In addition, the effectiveness of safety measures in such different work environments, and their related training and behavioural implications, would be interesting areas of study.
Early media reporting indicated certain levels of societal anxiety in relation to the continuity and robustness of the supply chains—particularly those of food and essential products—which often manifested in the form of hoarding and so-called ‘panic shopping’. Although there is a well-established literature on this domain (Baghalian et al., 2013, Molero et al., 2017, Pan and Nagi, 2010, Tang, 2006, Yang, 2011), considering that this appeared to be a major concern of the public in the face of epidemics of this magnitude, further research seems to be needed on how to enhance the safety and robustness of supply chains while taking into account specific characteristics of the current health emergency. This may entail system-level studies of the disruptive effects of the impacts of the pandemic on essential multi-modal commodity supply chains by sea, land, or air freight. Furthermore, the occupational safety of port and aviation staff (Eldin et al., 2020), and seafarers and cruise line personnel are areas where research contributions are currently lacking. Many of these workers likely endured heightened levels of stress and anxiety due to prolonged periods at sea, sometimes onboard ships with confirmed infections and deaths, or in uncertain conditions far away from their families. Some work on occupational safety of these groups of workers exists, e.g. Useche et al., 2018, Shan and Lippel, 2019, but the authors are not aware of any research on occupational safety of these workers in a pandemic outbreak context.
Furthermore, while there is a substantial amount of scientific studies on crowd control and management (Feliciani and Nishinari, 2018, Haghani and Sarvi, 2018), not much appears to have been done to study specific characteristics of crowd control during health emergencies of this nature which require spatial distancing measures. At the early stages of the pandemic, before extreme lockdown measures were in place in many geographical regions, certain societies had introduced more moderate measures to mitigate the risk of potential outbreaks that involved keeping the density of human congregation in public spaces below certain thresholds. Similar measures could be expected during the transition from strict isolation measures back to more moderate measures once the acute severity of this public health emergency diminishes. We assume that these unprecedented challenges should require the expertise of the researchers active in this domain to propose methods and solutions for how to enforce such restrictions regarding crowd management and safety. Such research could be highly relevant in open public spaces such as parks, recreational areas, and beaches, in closed public spaces such as grocery shops, university buildings and particularly hospital emergency departments (Chen et al., 2020c), also in closed spaces such as office buildings, cruise vessels, or airplanes (Eldin et al., 2020) as well as public or shared transport vehicles (Zheng et al., 2020b).
On a similar note, it has been observed during this epidemic that the identification of positive cases of infected individuals has often resulted in the evacuation of the buildings, such as those of workplaces. It is assumed that, during the evacuation process, if appropriate measures are not taken to manage the evacuation process, a hasty unregulated evacuation in such instances could itself lead to heightened levels of spatial human concentration which can elevate the risk of contracting the virus for evacuees, particularly in high-occupancy buildings. In light of these concerns, we suggest that evacuation experts could revisit and further study the particular issues relevant to this problem and to propose appropriate methods and solutions for evacuation safety.
It is essential to emphasise that the above discussion only covers a selective list of potential ways by which further academic research could address perhaps less obvious safety implications of the epidemic. The scholarly literature that is being generated in response to this global emergency is immensely dynamic and rapidly developing. Therefore, it is expected that more scientific evidence and solutions be offered on these and other under-researched safety dimensions as new studies emerge.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssci.2020.104806.
Appendix A.
Table A1, Table A2, Table A3 .
Table A1.
Summary statistics on scholarly publications related to Coronaviruses.
| No. | Authors | Count | Country/Regions | Count | Funding sponsors | Count | Institutes | Count | Subject areas | Count | Sources | Count |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Yuen, K.Y. | 168 | United States | 3878 | National Institutes of Health | 643 | The University of Hong Kong | 441 | Medicine | 5168 | Journal of Virology | 1005 |
| 2 | Enjuanes, L. | 164 | China | 2020 | National Natural Science Foundation of China | 360 | Chinese Academy of Sciences | 285 | Immunology and Microbiology | 4923 | Virology | 414 |
| 3 | Perlman, S. | 139 | United Kingdom | 890 | National Institute of Allergy and Infectious Diseases | 253 | Utrecht University | 284 | Biochemistry, Genetics and Molecular Biology | 2744 | Advances in Experimental Medicine and Biology | 365 |
| 4 | Drosten, C. | 133 | Germany | 823 | National Basic Research Program of China (973 Program) | 128 | National Institutes of Health, Bethesda | 220 | Agricultural and Biological Sciences | 1794 | Journal of General Virology | 278 |
| 5 | Rottier, P.J.M. | 121 | The Netherlands | 660 | European Commission | 110 | Centers for Disease Control and Prevention | 212 | Veterinary | 1587 | Archives of Virology | 192 |
| 6 | Baric, R.S. | 111 | China | 625 | Deutsche Forschungsgemeinschaft | 89 | The University of North Carolina at Chapel Hill | 190 | Pharmacology, Toxicology and Pharmaceutics | 572 | Emerging Infectious Diseases | 188 |
| 7 | Weiss, S.R. | 106 | Canada | 614 | U.S. Public Health Service | 64 | Departement Infectieziekten en Immunologie, Universiteit Utrecht | 178 | Multidisciplinary | 477 | Virus Research | 182 |
| 8 | Memish, Z.A. | 105 | France | 553 | Chinese Academy of Sciences | 57 | Chinese University of Hong Kong | 177 | Chemistry | 223 | Plos One | 175 |
| 9 | Holmes, K.V. | 102 | Japan | 482 | National Science Council | 55 | University of Iowa | 154 | Environmental Science | 201 | Journal of Medical Virology | 161 |
| 10 | Makino, S. | 91 | South Korea | 403 | National Multiple Sclerosis Society | 52 | CSIC - Centro Nacional de Biotecnologia CNB | 150 | Neuroscience | 174 | Veterinary Microbiology | 143 |
| 11 | Peiris, J.S.M. | 91 | Saudi Arabia | 394 | University of Hong Kong | 52 | Ministry of Health Saudi Arabia | 148 | Engineering | 112 | Journal of Virological Methods | 134 |
| 12 | Woo, P.C.Y. | 91 | Italy | 362 | U.S. Department of Agriculture | 48 | Faculteit Diergeneeskunde, Universiteit Utrecht | 144 | Mathematics | 97 | Viruses | 132 |
| 13 | Talbot, P.J. | 89 | Taiwan, China | 336 | Biotechnology and Biological Sciences Research Council | 43 | Queen Mary Hospital Hong Kong | 139 | Computer Science | 96 | Journal of Clinical Microbiology | 127 |
| 14 | Jiang, S. | 88 | Singapore | 309 | Wellcome Trust | 42 | Julius-Maximilians-Universität Würzburg | 136 | Chemical Engineering | 85 | Journal of Infectious Diseases | 115 |
| 15 | Saif, L.J. | 88 | Spain | 294 | National Research Foundation of Korea | 41 | Academy of Military Medical Science China | 135 | Physics and Astronomy | 75 | Proceedings of The National Academy of Sciences Of The United States Of America | 101 |
| 16 | Stohlman, S.A. | 88 | Switzerland | 270 | National Science Foundation | 40 | Erasmus MC | 134 | Social Sciences | 70 | American Journal of Veterinary Research | 100 |
| 17 | Snijder, E.J. | 87 | Australia | 269 | National Institute of General Medical Sciences | 38 | Keck School of Medicine of USC | 129 | Health Professions | 62 | Antiviral Research | 89 |
| 18 | Lau, S.K.P. | 84 | Brazil | 201 | Natural Sciences and Engineering Research Council of Canada | 37 | Leiden University Medical Center - LUMC | 122 | Materials Science | 55 | Journal of Clinical Virology | 80 |
| 19 | Lai, M.M.C. | 81 | Belgium | 154 | Canadian Institutes of Health Research | 36 | The Ohio State University | 120 | Nursing | 37 | Vaccine | 80 |
| 20 | Denison, M.R. | 76 | Sweden | 147 | Japan Society for the Promotion of Science | 35 | Chinese Academy of Medical Sciences & Peking Union Medical College | 120 | Arts and Humanities | 25 | Virology Journal | 79 |
Table A2.
Summary statistics on scholarly publications related to COVID-19.
| No. | Authors | Count | Country/Region | Count | Funding sponsors | Count | Institutes | Count | Subject areas | Count | Sources | Count |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Mahase, E. | 20 | China | 431 | National Natural Science Foundation of China | 71 | The University of Hong Kong | 37 | Medicine | 1029 | BMJ Clinical Research Ed | 99 |
| 2 | Rimmer, A. | 13 | United States | 222 | National Basic Research Program of China (973 Program) | 17 | Huazhong University of Science and Technology | 33 | Immunology and Microbiology | 191 | Lancet | 74 |
| 3 | Hsueh, P.R. | 10 | United Kingdom | 132 | National Institutes of Health | 11 | Tongji Medical College | 31 | Biochemistry, Genetics and Molecular Biology | 90 | Journal of Medical Virology | 47 |
| 4 | Jiang, S. | 8 | Italy | 67 | Fundamental Research Funds for the Central Universities | 10 | Chinese Academy of Sciences | 31 | Multidisciplinary | 53 | JAMA Journal of The American Medical Association | 34 |
| 5 | Memish, Z.A. | 8 | Canada | 48 | Chinese Academy of Sciences | 9 | Chinese Academy of Medical Sciences & Peking Union Medical College | 26 | Pharmacology, Toxicology and Pharmaceutics | 47 | BMJ | 31 |
| 6 | Rodriguez-Morales, A.J. | 8 | China | 45 | Wellcome Trust | 8 | School of Medicine | 26 | Social Sciences | 43 | Euro Surveillance Bulletin Europeen Sur Les Maladies Transmissibles European Communicable Disease Bulletin | 29 |
| 7 | Wiwanitkit, V. | 8 | France | 42 | Centers for Disease Control and Prevention | 6 | Capital Medical University | 25 | Environmental Science | 31 | Lancet Infectious Diseases | 29 |
| 8 | Zumla, A. | 8 | Singapore | 41 | Science and Technology Major Project of Guangxi | 6 | London School of Hygiene & Tropical Medicine | 25 | Neuroscience | 28 | Science | 25 |
| 9 | Kupferschmidt, K. | 7 | Germany | 39 | Bill and Melinda Gates Foundation | 5 | National University of Singapore | 24 | Health Professions | 25 | Travel Medicine and Infectious Disease | 25 |
| 10 | Sah, R. | 7 | Switzerland | 37 | Chinese Academy of Medical Sciences | 5 | Chinese University of Hong Kong | 23 | Nursing | 21 | Journal of Infection | 22 |
| 11 | Baden, L.R. | 6 | Australia | 34 | European and Developing Countries Clinical Trials Partnership | 5 | Fudan University | 23 | Psychology | 15 | Nature | 21 |
| 12 | Drosten, C. | 6 | India | 31 | Health and Medical Research Fund | 5 | Wuhan University | 23 | Veterinary | 15 | New England Journal of Medicine | 18 |
| 13 | Eurosurveillance Editorial Team | 6 | Taiwan, China | 28 | National Institute of Allergy and Infectious Diseases | 5 | The University of Hong Kong Li Ka Shing Faculty of Medicine | 21 | Agricultural and Biological Sciences | 14 | Emerging Microbes and Infections | 16 |
| 14 | Iacobucci, G. | 6 | South Korea | 26 | National Major Science and Technology Projects of China | 5 | Zhongnan Hospital of Wuhan University | 21 | Computer Science | 14 | Lancet Respiratory Medicine | 15 |
| 15 | Iacobucci, G. | 6 | Saudi Arabia | 25 | National Science Fund for Distinguished Young Scholars | 5 | Zhejiang University | 19 | Mathematics | 13 | Journal of Korean Medical Science | 13 |
| 16 | Ippolito, G. | 6 | Sweden | 17 | Sanming Project of Medicine in Shenzhen | 5 | UCL | 19 | Engineering | 12 | Infection Control and Hospital Epidemiology | 11 |
| 17 | Kim, J.Y. | 6 | Thailand | 17 | Agence Nationale de la Recherche | 4 | University of Oxford | 19 | Chemistry | 9 | International Journal of Infectious Diseases | 11 |
| 18 | Morrissey, S. | 6 | Brazil | 16 | Canadian Institutes of Health Research | 4 | Zhejiang University School of Medicine | 19 | Business, Management and Accounting | 5 | Journal of Hospital Infection | 11 |
| 19 | Rubin, E.J. | 6 | Japan | 15 | China Scholarship Council | 4 | Ministry of Education China | 18 | Chemical Engineering | 5 | Journal of Microbiology Immunology and Infection | 11 |
| 20 | Angeletti, S. | 5 | The Netherlands | 15 | Horizon 2020 Framework Programme | 4 | University of Toronto | 17 | Dentistry | 5 | Veterinary Record | 11 |
Table A3.
Studies on the safety-related aspects of the COVID-19 pandemic.
| No. | Reference | Safety dimension* | Method of study | Key message/finding | Key recommendations |
|---|---|---|---|---|---|
| 1 | Devaux et al. (2020) | Medical | Preliminary trials |
|
|
| 2 | Liu et al. (2020a) | Medicine | Limited clinical trials |
|
|
| 3 | Chen et al. (2020d) | Medicine | Vaccine strategies related to SARS-CoV |
|
|
| 4 | Cortegiani et al. (2020) | Medicine | Existing medical evidence and ongoing clinical trials |
|
|
| 5 | Chang et al. (2020) | Blood | Relevant publications on previous coronaviruses |
|
|
| 6 | Dodd and Stramer (2020) | Blood | Relevant publications on previous coronaviruses |
|
|
| 7 | Schwartz and Graham (2020) | Pregnancy | Evidence from SARS and other Coronavirus Infections |
|
|
| 8 | Chen et al. (2020a) | Pregnancy | Retrospective review of medical records |
|
|
| 9 | Rasmussen et al. (2020) | Pregnancy | Evidence from similar pathogenic coronaviruses |
|
|
| 10 | Topalidou et al. (2020) | Pregnancy | Synthesising the scientific literature |
|
|
| 11 | Chen et al. (2020b) | Pregnancy, Surgery | Retrospective review of patients’ records |
|
|
| 12 | Givi et al. (2020) | Surgery | Review of the literature and communication with physicians with firsthand experience of treating COVID-19 patients |
|
|
| 13 | Kang et al. (2020b) | Pregnancy, Surgery | Medical practice experience in China |
|
|
| 14 | Fadel et al. (2020) | Occupational | N.A. |
|
|
| 15 | Chen et al. (2020e) | Occupational | Clinical practice in West China Hospital |
|
|
| 16 | Cheung et al. (2020) | Occupational | Clinal practice in Hong Kong |
|
|
| 17 | Ambigapathy et al. (2020) | Occupational | N.A. |
|
|
| 18 | Greenhalgh et al. (2020) | Transport & visit | Evidence from randomised trials |
|
|
| 19 | Liew et al. (2020) | Transport & visit | Evidence from influenza pandemic |
|
|
| 20 | Kooraki et al. (2020) | Laboratory, Occupational | N.A. |
|
|
| 21 | Nie et al. (2020) | Laboratory | Laboratory tests |
|
|
| 22 | Shariatifar and Molaee-aghaee (2019) | Food | N.A. |
|
|
| 23 | Yuan et al. (2020) | Food | Epidemiological evidence related to SARS and COVID-19 outbreaks |
|
|
| 24 | Bachireddy et al. (2020) | Social | N.A. |
|
|
| 25 | Jun et al. (2020) | Occupational, Mental | Evidence from previous epidemics |
|
|
| 26 | Wang et al. (2020a) | Mental | Survey the general public in China |
|
|
| 27 | Shigemura et al. (2020) | Mental | Evidence from previous pandemics and public emergencies |
|
|
| 28 | Li et al. (2020) | Mental | Analysis of social media feed (A Chinese microblogging website) |
|
|
| 29 | Alves et al. (2020) | Mental | N.A. |
|
|
| 30 | Van Bavel et al. (2020) | Mental | Evidence from a selection of research topics relevant to pandemics |
|
|
| 31 | Greenberg et al. (2020) | Mental, Occupational | N.A. |
|
|
| 32 | Wang et al. (2020b) | Mental | Evidence from previous outbreaks |
|
|
| 33 | Ornell et al. (2020) | Mental | Survey of recommendations from WHO and the US Centre for Disease Control and Prevention |
|
|
| 34 | Barari et al. (2020) | Mental | Public survey of Italian population sample |
|
|
*Medicine = “medicine, treatment and vaccine safety”, Blood = “blood safety”, Pregnancy = “pregnancy safety”, Surgery = “surgery and anesthetic safety”, Occupational = “occupational safety of healthcare workers”, Transport & visit = “patient transport and visit safety”, Laboratory = “biosafety of laboratories and facilities”, Food = “food safety”, Social = “Social public safety”, Mental = “mental/psychological health and domestic safety”.
Appendix B. Supplementary data
The following are the Supplementary data to this article:
References
- Al-Tawfiq J.A. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) and COVID-19 infection during pregnancy. Travel Med. Infect. Dis. 2020;101641 doi: 10.1016/j.tmaid.2020.101641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida J., Berry D., Cunningham C., Hamre D., Hofstad M., Mallucci L., McIntosh K., Tyrrell D. Coronaviruses. Nature. 1968;220:2. [Google Scholar]
- Alves P.M.R., de Oliveira C.J.B., de Oliveira T.R.N., Barbosa K.B., Marcene H.C., de Oliveira S.V. COVID-19: isolations, quarantines and domestic violence in rural areas. SciMedicine J. 2020;2:44–45. [Google Scholar]
- Ambigapathy S., Rajahram G.S., Shamsudin U.K., Khoo E.M., Cheah W.K., Peariasamy K.M., Goh P.P., Khor S.K. How should front-line general practitioners use personal protective equipment (PPE)? Malaysian Family Physician. 2020;15:2–5. [PMC free article] [PubMed] [Google Scholar]
- Antoniadou N., Kokkinos C.M. Cyber and school bullying: same or different phenomena? Aggression Violent Behav. 2015;25:363–372. [Google Scholar]
- Aslam S., Mehra M.R. 19: Yet another coronavirus challenge in transplantation. J. Heart Lung Transplant. 2020 doi: 10.1016/j.healun.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachireddy, C., Chen, C., Dar, M., 2020. Securing the safety net and protecting public health during a pandemic: medicaid's response to COVID-19. JAMA – J. Am. Med. Assoc. [DOI] [PubMed]
- Baghalian A., Rezapour S., Farahani R.Z. Robust supply chain network design with service level against disruptions and demand uncertainties: a real-life case. Eur. J. Oper. Res. 2013;227:199–215. [Google Scholar]
- Barari, S., Caria, S., Davola, A., Falco, P., Fetzer, T., Fiorin, S., Hensel, L., Ivchenko, A., Jachimowicz, J., King, G., 2020. Evaluating COVID-19 public health messaging in Italy: self-reported compliance and growing mental health concerns. medRxiv.
- Bayham J., Fenichel E.P. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modelling study. The Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belingheri M., Paladino M.E., Riva M.A. Beyond the assistance: additional exposure situations to COVID-19 for healthcare workers. J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi X., Shi X., Zhang Z. Cognitive machine learning model for network information safety. Saf. Sci. 2019;118:435–441. [Google Scholar]
- Bozorgmehr K., Saint V., Kaasch A., Stuckler D., Kentikelenis A. COVID and the convergence of three crises in Europe. The Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30078-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury-Jones, C., Isham, L., n/a. The pandemic paradox: the consequences of COVID-19 on domestic violence. J. Clin. Nursing. [DOI] [PMC free article] [PubMed]
- Bruinen de Bruin Y., Lequarre A.-S., McCourt J., Clevestig P., Pigazzani F., Zare Jeddi M., Colosio C., Goulart M. Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Saf. Sci. 2020;104773 doi: 10.1016/j.ssci.2020.104773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellina, M., Orsi, M., Bombaci, F., Sala, M., Marino, P., Oliva, G., 2020. Favorable changes of CT findings in a patient with COVID-19 pneumonia after treatment with tocilizumab. Diagnostic and Interventional Imaging. [DOI] [PMC free article] [PubMed]
- Chang Le, Yan Ying, Wang Lunan. Coronavirus Disease 2019: coronaviruses and blood safety. Transfus. Med. Rev. 2020 doi: 10.1016/j.tmrv.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., Li J., Zhao D., Xu D., Gong Q., Liao J., Yang H., Hou W., Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Zhang Y., Huang L., Cheng B.H., Xia Z.Y., Meng Q.T. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery: a case series of 17 patients. Canadian J. Anesthesia. 2020 doi: 10.1007/s12630-020-01630-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T.-Y., Lai H.-W., Hou I.L., Lin C.-H., Chen M.-K., Chou C.-C., Lin Y.-R. Buffer areas in emergency department to handle potential COVID-19 community infection in Taiwan. Travel Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W.H., Strych U., Hotez P.J., Bottazzi M.E. The SARS-CoV-2 vaccine pipeline: an overview. Curr. Tropical Med. Reports. 2020 doi: 10.1007/s40475-020-00201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Pradhan S., Xue S. What are we doing in the dermatology outpatient department amidst the raging of the 2019 novel coronavirus? J. Am. Acad. Dermatol. 2020;82:1034. doi: 10.1016/j.jaad.2020.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung J.C.H., Ho L.T., Cheng J.V., Cham E.Y.K., Lam K.N. Staff safety during emergency airway management for COVID-19 in Hong Kong. The Lancet Resp. Med. 2020;8 doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortegiani A., Ingoglia G., Ippolito M., Giarratano A., Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J. Crit. Care. 2020 doi: 10.1016/j.jcrc.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton L., Rapa E., Stein A. Protecting the psychological health of children through effective communication about COVID-19. The Lancet Child & Adolescent Health. 2020 doi: 10.1016/S2352-4642(20)30097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C., Chong N.K., Oh J.Y., Baeg A., Rajasegaran K., Elaine Chew C.S. Caring for children and adolescents with eating disorders in the current COVID-19 pandemic: a Singapore perspective. J. Adolesc. Health. 2020 doi: 10.1016/j.jadohealth.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daw M.A. Corona virus infection in Syria, Libya and Yemen; an alarming devastating threat. Travel Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Giorgio A. COVID-19 is not just a flu. Learn from Italy and act now. Travel Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decaro N., Martella V., Saif L.J., Buonavoglia C. COVID-19 from veterinary medicine and one health perspectives: what animal coronaviruses have taught us. Res. Vet. Sci. 2020;131:21–23. doi: 10.1016/j.rvsc.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devaux Christian A., Rolain Jean-Marc, Colson Philippe, Raoult Didier. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int. J. Antimicrob. Agents. 2020:105938. doi: 10.1016/j.ijantimicag.2020.105938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd R.Y., Stramer S.L. COVID-19 and blood safety: help with a dilemma. Transfus. Med. Rev. 2020 doi: 10.1016/j.tmrv.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldin C., Lagier J.-C., Mailhe M., Gautret P. Probable aircraft transmission of Covid-19 in-flight from the Central African Republic to France. Travel Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadel M., Salomon J., Descatha A. Coronavirus outbreak: the role of companies in preparedness and responses. The Lancet Public Health. 2020;5 doi: 10.1016/S2468-2667(20)30051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feliciani C., Nishinari K. Measurement of congestion and intrinsic risk in pedestrian crowds. Transp. Res. Part C: Emerg. Technol. 2018;91:124–155. [Google Scholar]
- Feng Z.-H., Cheng Y.-R., Ye L., Zhou M.-Y., Wang M.-W., Chen J. Is home isolation appropriate for preventing the spread of COVID-19? Public Health. 2020 doi: 10.1016/j.puhe.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Givi B., Schiff B.A., Chinn S.B., Clayburgh D., Iyer N.G., Jalisi S., Moore M.G., Nathan C.A., Orloff L.A., O'Neill J.P., Parker N., Zender C., Morris L.G.T., Davies L. Safety Recommendations for Evaluation and Surgery of the Head and Neck during the COVID-19 Pandemic. JAMA. Otolaryngol. Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- Grant M.J., Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inform. Libraries J. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- Gray P.E., Belessis Y. The use of Traditional Chinese Medicines to treat SARS-CoV-2 may cause more harm than good. Pharmacol. Res. 2020;156 doi: 10.1016/j.phrs.2020.104776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ (Clinical research ed.) 2020:368. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- Greenhalgh, T., Wherton, J., Shaw, S., Morrison, C., 2020. Video consultations for covid-19. The BMJ 368. [DOI] [PubMed]
- Hafiz, H., Oei, S.-Y., Ring, D.M., Shnitser, N., 2020. Regulating in Pandemic: Evaluating Economic and Financial Policy Responses to the Coronavirus Crisis. Boston College Law School Legal Studies Research Paper.
- Haghani M., Sarvi M. Crowd behaviour and motion: empirical methods. Transp. Res. Part B: Methodol. 2018;107:253–294. [Google Scholar]
- Hamzavi I.H., Lyons A.B., Kohli I., Narla S., Parks-Miller A., Gelfand J.M., Lim H.W., Ozog D. Ultraviolet germicidal irradiation: possible method for respirator disinfection to facilitate reuse during COVID-19 pandemic. J. Am. Acad. Dermatol. 2020 doi: 10.1016/j.jaad.2020.03.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatchett R.J., Mecher C.E., Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc. Natl. Acad. Sci. 2007;104:7582. doi: 10.1073/pnas.0610941104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joob, B., Wiwanitkit, V., 2020. Traumatization in medical staff helping with COVID-19 control. Brain, Behavior, and Immunity. [DOI] [PMC free article] [PubMed]
- Jun, J., Tucker, S., Melnyk, B., 2020. Clinician Mental Health and Well‐Being During Global Healthcare Crises: Evidence Learned From Prior Epidemics for COVID‐19 Pandemic. Worldviews on Evidence‐Based Nursing. [DOI] [PubMed]
- Kabir M., Afzal M.S., Khan A., Ahmed H. COVID-19 pandemic and economic cost; impact on forcibly displaced people. Travel Med. Infect. Dis. 2020:101661. doi: 10.1016/j.tmaid.2020.101661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang C., Yang S., Yuan J., Xu L., Zhao X., Yang J. Patients with chronic illness urgently need integrated physical and psychological care during the COVID-19 outbreak. Asian J. Psych. 2020;51 doi: 10.1016/j.ajp.2020.102081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang, X., Zhang, R., He, H., Yao, Y., Zheng, Y., Wen, X., Zhu, S., 2020b. Anesthesia management in cesarean section for a patient with coronavirus disease 2019. Zhejiang da xue xue bao. Yi xue ban = J. Zhejiang Univ. Med. Sci. 49, 0. [DOI] [PMC free article] [PubMed]
- Kluge H.H.P., Jakab Z., Bartovic J., D'Anna V., Severoni S. Refugee and migrant health in the COVID-19 response. The Lancet. 2020;395:1237–1239. doi: 10.1016/S0140-6736(20)30791-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kooraki S., Hosseiny M., Myers L., Gholamrezanezhad A. Coronavirus (COVID-19) outbreak: what the department of radiology should know. J. Am. College Radiol. 2020;17:447–451. doi: 10.1016/j.jacr.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuwahara K., Kuroda A., Fukuda Y. COVID-19: Active measures to support community-dwelling older adults. Travel Med. Infect. Dis. 2020:101638. doi: 10.1016/j.tmaid.2020.101638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law S., Leung A.W., Xu C. Severe Acute Respiratory Syndrome (SARS) and Coronavirus disease-2019 (COVID- 19): from causes to preventions in Hong Kong. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee V.J., Ho M., Kai C.W., Aguilera X., Heymann D., Wilder-Smith A. Epidemic preparedness in urban settings: new challenges and opportunities. Lancet. Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30249-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Wang Y., Xue J., Zhao N., Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int. J. Environ. Res. Public Health. 2020;17:2032. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liew Mei Fong, Siow Wen Ting, Yau Ying Wei, See Kay Choong. Safe patient transport for COVID-19. Crit. Care. 2020;24(1) doi: 10.1186/s13054-020-2828-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Jia, Cao Ruiyuan, Xu Mingyue, Wang Xi, Zhang Huanyu, Hu Hengrui, Li Yufeng, Hu Zhihong, Zhong Wu, Wang Manli. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6(1) doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.J., Bao Y., Huang X., Shi J., Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolescent Health. 2020 doi: 10.1016/S2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovato Andrea, de Filippis Cosimo, Marioni Gino. Upper airway symptoms in coronavirus disease 2019 (COVID-19) Am. J. Otolaryngol. 2020:102474. doi: 10.1016/j.amjoto.2020.102474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., Yin K. Management of pregnant women infected with COVID-19. Lancet. Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30191-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mingers J., Leydesdorff L. A review of theory and practice in scientometrics. Eur. J. Oper. Res. 2015;246:1–19. [Google Scholar]
- Molero G.D., Santarremigia F.E., Aragonés-Beltrán P., Pastor-Ferrando J.-P. Total safety by design: Increased safety and operability of supply chain of inland terminals for containers with dangerous goods. Saf. Sci. 2017;100:168–182. [Google Scholar]
- Montemurro, N., 2020. The emotional impact of COVID-19: From medical staff to common people. Brain, Behav., Immunity. [DOI] [PMC free article] [PubMed]
- Murphy A., Abdi Z., Harirchi I., McKee M., Ahmadnezhad E. Economic sanctions and Iran's capacity to respond to COVID-19. The Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30083-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng J.J., Ho P., Dharmaraj R.B., Wong J.C.L., Choong A.M.T.L. The global impact of COVID-19 on vascular surgical services. J. Vasc. Surg. 2020 doi: 10.1016/j.jvs.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie J., Li Q., Wu J., Zhao C., Hao H., Liu H., Zhang L., Nie L., Qin H., Wang M., Lu Q., Li X., Sun Q., Liu J., Fan C., Huang W., Xu M., Wang Y. Establishment and validation of a pseudovirus neutralization assay for SARS-CoV-2. Emerging Microbes Infect. 2020;9:680–686. doi: 10.1080/22221751.2020.1743767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. “Pandemic fear” and COVID- 19: mental health burden and strategies. Brazil. J. Psych. 2020 doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan F., Nagi R. Robust supply chain design under uncertain demand in agile manufacturing. Comput. Oper. Res. 2010;37:668–683. [Google Scholar]
- Paul, R., Elder, L., 2019. How to read a paragraph: The art of close reading. Rowman & Littlefield.
- Rasmussen S.A., Smulian J.C., Lednicky J.A., Wen T.S., Jamieson D.J. Coronavirus Disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am. J. Obstet. Gynecol. 2020 doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen T.E., Koelling E.E. A military perspective on the vascular surgeon’s response to the COVID-19 pandemic. J. Vasc. Surg. 2020 doi: 10.1016/j.jvs.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal D.M., Ucci M., Heys M., Hayward A., Lakhanpaul M. Impacts of COVID-19 on vulnerable children in temporary accommodation in the UK. The Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30080-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlagenhauf P., Grobusch M.P., Maier J.D., Gautret P. Repurposing antimalarials and other drugs for COVID-19. Travel Med. Infect. Dis. 2020:101658. doi: 10.1016/j.tmaid.2020.101658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz D.A., Graham A.L. Potential maternal and infant outcomes from coronavirus 2019-NCOV (SARS-CoV-2) infecting pregnant women: Lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020;12 doi: 10.3390/v12020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shan D., Lippel K. Occupational health and safety challenges from employment-related geographical mobility among Canadian seafarers on the Great Lakes and St. Lawrence Seaway. NEW SOLUTIONS: J. Environ. Occup. Health Policy. 2019;29:371–396. doi: 10.1177/1048291119870762. [DOI] [PubMed] [Google Scholar]
- Shariatifar N., Molaee-aghaee E. A Novel coronavirus 2019 (COVID-19): important tips on food safety. J. Food Safety Hygiene. 2019;5:58–59. [Google Scholar]
- Sheng Wang-Huei, Ko Wen-Chien, Huang Yhu-Chering, Hsueh Po-Ren. SARS-CoV-2 and COVID-19. J. Microbiol. Immunol. Infect. 2020 doi: 10.1016/j.jmii.2020.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi W., Hall B.J. What can we do for people exposed to multiple traumatic events during the coronavirus pandemic? Asian J. Psych. 2020;51 doi: 10.1016/j.ajp.2020.102065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psych. Clin. Neurosci. 2020 doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sodhi M., Etminan M. Safety of ibuprofen in patients with COVID-19: causal or confounded? Chest. 2020 doi: 10.1016/j.chest.2020.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultan S., Lim J.K., Altayar O., Davitkov P., Feuerstein J.D., Siddique S.M., Falck-Ytter Y., El-Serag H.B. AGA institute rapid recommendations for gastrointestinal procedures during the COVID-19 pandemic. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang C.S. Robust strategies for mitigating supply chain disruptions. Int. J. Logistics: Res. Appl. 2006;9:33–45. [Google Scholar]
- Topalidou, A., Thomson, G., Downe, S., 2020. COVID-19 and maternal mental health: Are we getting the balance right? medRxiv.
- Useche S.A., Gómez V., Cendales B., Alonso F. Working conditions, job strain, and traffic safety among three groups of public transport drivers. Safety Health Work. 2018;9:454–461. doi: 10.1016/j.shaw.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bavel, J.J., Boggio, P., Capraro, V., Cichocka, A., Cikara, M., Crockett, M., Crum, A., Douglas, K., Druckman, J., Drury, J., 2020. Using social and behavioural science to support COVID-19 pandemic response. [DOI] [PubMed]
- Van Eck, N., Waltman, L., 2010. Software survey: VOSviewer, a computer program for bibliometric mapping. scientometrics 84, 523–538. [DOI] [PMC free article] [PubMed]
- van Eck, N., Waltman, L., Noyons, E., Buter, R., 2010. Automatic term identification for bibliometric mapping. scientometrics 82, 581–596. [DOI] [PMC free article] [PubMed]
- Van Eck, N.J., Waltman, L., 2013. VOSviewer manual, vol. 1. Univeristeit Leiden, Leiden, pp. 1–53.
- Van Lancker W., Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. The Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner R.M., Russell S.J., Croker H., Packer J., Ward J., Stansfield C., Mytton O., Bonell C., Booy R. School closure and management practices during coronavirus outbreaks including COVID- 19: a rapid systematic review. The Lancet Child & Adolescent Health. 2020 doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waltman L., Van Eck N.J., Noyons E.C. A unified approach to mapping and clustering of bibliometric networks. J. Informetrics. 2010;4:629–635. [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in china. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. The Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Li X., Cao G., Wu X., Wang Z., Yan T. COVID-19 in a kidney transplant patient. Eur. Urol. 2020 doi: 10.1016/j.eururo.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Jingzhong, Liao Yi, Wang Xiaoyang, Li Yichong, Jiang Dan, He Jianfan, Zhang Shunxiang, Xia Junjie. Incidence of novel coronavirus (2019-nCoV) infection among people under home quarantine in Shenzhen, China. Travel Med. Infect. Dis. 2020:101660. doi: 10.1016/j.tmaid.2020.101660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WEF, 2020. The global risks report 2020. World Economic Forum, Geneva, Switzerland, p. 102.
- Xu C., Jin J., Song J., Yang Y., Yao M., Zhang Y., Zhao R., Chen Z. Application of refined management in prevention and control of the coronavirus disease 2019 epidemic in non-isolated areas of a general hospital. Int. J. Nursing Sci. 2020 doi: 10.1016/j.ijnss.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y.-C. Risk management of Taiwan’s maritime supply chain security. Saf. Sci. 2011;49:382–393. [Google Scholar]
- Yifan T., Ying L., Chunhong G., Jing S., Rong W., Zhenyu L., Zejuan G., Peihung L. Symptom Cluster of ICU nurses treating COVID-19 pneumonia patients in Wuhan, China. J. Pain Symptom Manage. 2020 doi: 10.1016/j.jpainsymman.2020.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J., Lu Y., Cao X., Cui H. Regulating wildlife conservation and food safety to prevent human exposure to novel virus. Ecosystem Health Sustain. 2020:1741325. [Google Scholar]
- Zambrano L.I., Fuentes-Barahona I.C., Bejarano-Torres D.A., Bustillo C., Gonzales G., Vallecillo-Chinchilla G., Sanchez-Martínez F.E., Valle-Reconco J.A., Sierra M., Bonilla-Aldana D.K., Cardona-Ospina J.A., Rodríguez-Morales A.J. A pregnant woman with COVID-19 in Central America. Travel Med. Infect. Dis. 2020;101639 doi: 10.1016/j.tmaid.2020.101639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang K. Is traditional Chinese medicine useful in the treatment of COVID-19? Am. J. Emerg. Med. 2020 doi: 10.1016/j.ajem.2020.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W., Qian B.-Y. Making decisions to mitigate COVID-19 with limited knowledge. Lancet. Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30280-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng C., Wang J., Guo H., Lu Z., Ma Y., Zhu Y., Xia D., Wang Y., He H., Zhou J., Wang Y., Fei M., Yin Y., Zheng M., Xu Y. Risk-adapted treatment strategy For COVID-19 patients. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng R., Xu Y., Wang W., Ning G., Bi Y. Spatial transmission of COVID-19 via public and private transportation in China. Travel Med. Infect. Dis. 2020:101626. doi: 10.1016/j.tmaid.2020.101626. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.