Abstract
Background
older adults are known to have increased falls rates and functional decline following hospital discharge, with substantial economic healthcare costs. This systematic review aimed to synthesise the evidence for effective falls prevention interventions in older adults recently discharged from hospital.
Methods
literature searches of six databases of quantitative studies conducted from 1990 to June 2017, reporting falls outcomes of falls prevention interventions for community-dwelling older adults discharged from hospital were included. Study quality was assessed using a standardised JBI critical appraisal tool (MAStARI) and data pooled using Rev-Man Review Manager®
Results
sixteen studies (total sample size N = 3,290, from eight countries, mean age 77) comprising 12 interventions met inclusion criteria. We found home hazard modification interventions delivered to those with a previous falls history (1 study), was effective in reducing the number of falls (RR 0.63, 95%CI 0.43, 0.93, Low GRADE evidence). Home exercise interventions (3 studies) significantly increased the proportion of fallers (OR 1.74, 95%CI 1.17, 2.60, Moderate GRADE evidence), and did not significantly reduce falls rate (RR 1.27, 95%CI 0.99, 1.62, Very Low GRADE evidence) or falls injury rate (RR 1.16, 95%CI, 0.83,1.63, Low GRADE evidence). Nutritional supplementation for malnourished older adults (1 study) significantly reduced the proportion of fallers (HR 0.41, 95% CI 0.19, 0.86, Low GRADE evidence).
Conclusion
the recommended falls prevention interventions for older adults recently discharged from hospital are to provide home hazard minimisation particularly if they have a recent previous falls history and consider nutritional supplementation if they are malnourished.
Keywords: falls prevention interventions, after hospital discharge, falls outcomes, older people, systematic review
Introduction
Implementing effective strategies to reduce falls among older adults has become a world-wide health challenge as the global population continues to age [1]. Falls are a leading cause of hospitalisation for older adults [2, 3]. Hospital length of stay is decreasing, leaving older adults at risk of adverse events following hospital discharge. Falls are known to increase among older adults during the post-discharge period with an increased risk of hip fracture [4–6]. Compared to the average annual fall rate of 30% in the general older community with 10% of these falls resulting in a serious injury [7–9], 40% of older adults recently discharged from hospital fall at least once in the 6-month period following discharge and 54% of these falls result in a serious injury [10–14].
Several large systematic reviews have established evidence for the effectiveness of falls prevention interventions for older adults in the general community [15–20]. However, the studies included in these reviews did not specifically evaluate interventions in the post-discharge period and the findings may not translate to falls prevention among community-dwelling older adults recently discharged from hospital. Systematic reviews of interventions that provided broad discharge support for older adults showed limited reduction in falls or adverse events [21, 22]. One systematic review that evaluated falls prevention education for older adults concluded there was some evidence that education was effective in reducing falls rates during and after hospitalisation (risk ratio [RR] 0.77, 95% confidence interval 0.69–0.87), however other falls prevention interventions were not examined [23]. The lack of research evidence regarding effective falls prevention interventions in the period following hospitalisation needs to be addressed.
The primary objective of this review was to collate randomised controlled trials (RCTs) that delivered falls prevention interventions for older adults just prior or immediately following hospital discharge, and to synthesise the evidence regarding their effectiveness during the 6 months immediately following hospital discharge.
Methods
A review was undertaken according to a protocol published in JBI Register of Systematic Reviews and Implementation Reports [24], and reported in accordance with PRISMA guidelines [25].
Search strategy and information sources
The search was undertaken using a three-step strategy recommended by the JBI systematic review library [26], using MeSH terminology and keywords to ensure all relevant studies were captured. Full details of the search strategy and information sources can be found in Supplementary Appendix 1 available in Age and Ageing online from the journal website.
Inclusion criteria
This review examined studies that evaluated any falls prevention intervention delivered to adults 60 years of age or older who were hospitalised and then discharged to the community. The interventions must have been delivered/commenced in hospital or in the first month after hospital discharge [24]. Studies eligible for the review were published and unpublished studies written in English from any country between January 1990 and June 2017, including RCTs and pseudo-RCTs comparing interventions against no intervention or placebo control. The start date of 1990 was considered appropriate as research concerning falls prevention is a relatively recent field and other large systematic reviews investigating falls interventions include RCTs dated from 1990 [20]. Studies needed to measure a falls outcome within at least 6 months after discharge from hospital including falls rate (expressed per 1,000-person days), proportion of people who fell one or more times, injurious falls rate (expressed per 1,000-person days) or proportion of people who had one or more injurious falls, with consideration of ProFANE common set of falls outcome definitions and measures [27–32].
Study quality
Papers selected for critical appraisal were assessed by three independent reviewers for risk of bias and methodological quality [26]. This was completed prior to inclusion in the review, using the standardised critical appraisal from JBI Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI), found in Supplementary Appendix 2 available in Age and Ageing online from the journal website.
Data synthesis and analysis
Data were collated by one reviewer then three reviewers independently confirmed accuracy of the data synthesis. Effectiveness of interventions was classified according to outcomes [30–33]. For outcomes reported as rates (rates of falls and rate of injurious falls), data were pooled using inverse variance DerSimonian and Laird method [34]. This produced a relative rate effect size with 95% confidence intervals (CI). For outcomes measured as proportions, the number of fallers and non-fallers in each group were entered and data pooled using Mantel–Haenszel model [35]. This produced an odds ratio (OR) with 95% confidence intervals. For studies that employed factorial designs, we extracted the main effect of each intervention if no interaction effect was identified. Quantitative data were pooled in statistical meta-analysis using Rev-Man Review Manager (Version 5.3.2014 TM) to generate forest plots [36]. All studies were analysed in terms of falls outcomes and subgroup meta-analyses based on pooling of comparable interventions. Heterogeneity was assessed using the I2 statistic and visual inspection of forest plots. A fixed-effects model was used to calculate estimates, based on examination of the literature [26, 37, 38]. The criteria that guided our decision to use the fixed-effect model in meta-analysis was the small number, size and heterogeneity of the studies evaluating each falls intervention. The included studies were clinical trials, methodologically homogenous, and measured one common true effect, a falls outcome. The only possible exception within this criterion was potential between-study heterogeneity of the participants. Notwithstanding fulfilment of our study sample inclusion criteria, we reasonably considered the participants to be similar enough to appropriately represent the population of older people recently discharged from hospital [38].
Results
Selected studies
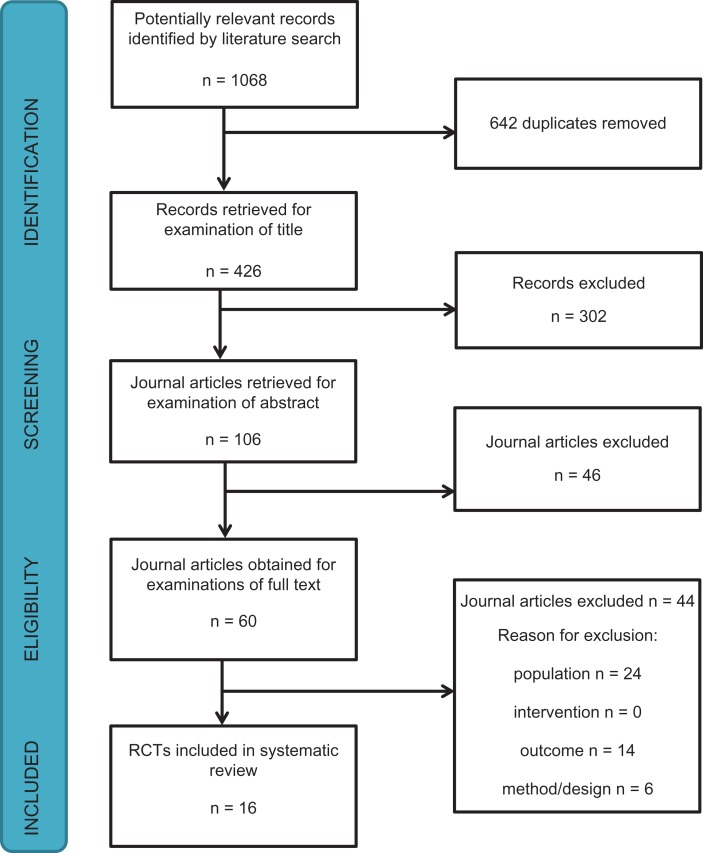
The search generated 1068 articles from the six databases. Figure 1 illustrates the study selection process. Supplementary Appendix 3, available in Age and Ageing online outlines the characteristics of included (N = 16) studies.
Figure 1.
Study selection flow chart.
The articles included in the review comprised one quasi RCT and 15 RCTs [39–53], refer to Supplementary Appendix 4 for the full reference list of included studies, available in Age and Ageing online. All the selected studies’ sample populations consisted of older adults recruited from inpatient wards. Participants’ mean age across the 16 studies were 77 years, with an age range of 70–84. Further details regarding the study population can be found in Supplementary Appendix 5, available in Age and Ageing online.
Study interventions
The interventions from nine studies were grouped according to a recommended taxonomy to describe falls prevention interventions [28], including home hazard modification interventions, home exercise programme, and cholecalciferol therapy. Two studies delivered exercise and cholecalciferol in factorial designed RCTs [47, 51]. One study provided a home exercise intervention as well as multi-factorial falls risk minimisation strategies based on falls risk factors [52], identified using a falls risk assessment tool for older people in the community (FROP-Com) [54, 55].
There were eight interventions included in the review that could not be pooled in meta-analysis because they only featured once across all the studies. These were geriatric team management, inpatient falls prevention education, tailored falls prevention education prior to discharge, a day hospital balance class, high-intensity quadriceps exercise, nutritional supplementation, discharge planning and an inpatient balance circuit class.
Quality of studies
The critical appraisal of all 16 included studies can be found in Supplementary Appendix 6, available in Age and Ageing online from the journal website.
Effectiveness of falls prevention interventions
Home hazard modification intervention
Three trials evaluated the effect of home hazard modification interventions on falls outcomes, however they differed in their presentation of effect estimates, therefore their results were analysed at the individual study level. One study dichotomised falls data, showing no significant effect on proportion of fallers (relative risk 1.06, 95%CI, 0.48, 2.34) [46]. Another study used the Andersen-Gill approach to describe falls as recurrent events and showed a significant reduction in proportion of fallers for the subgroup of participants with a previous falls history (HR 0.75, 95%CI 0.58, 0.96) [41]. (Supplementary Appendix seven Figure S1, available in Age and Ageing online)
In another home hazard modification intervention study, results showed a reduction in falls using rate ratio (RR), also for a subgroup of participants with a previous history of frequent falls (RR 0.63, 95%CI 0.43, 0.93) [42]. (Supplementary Appendix 7 Figure S2, available in Age and Ageing online)
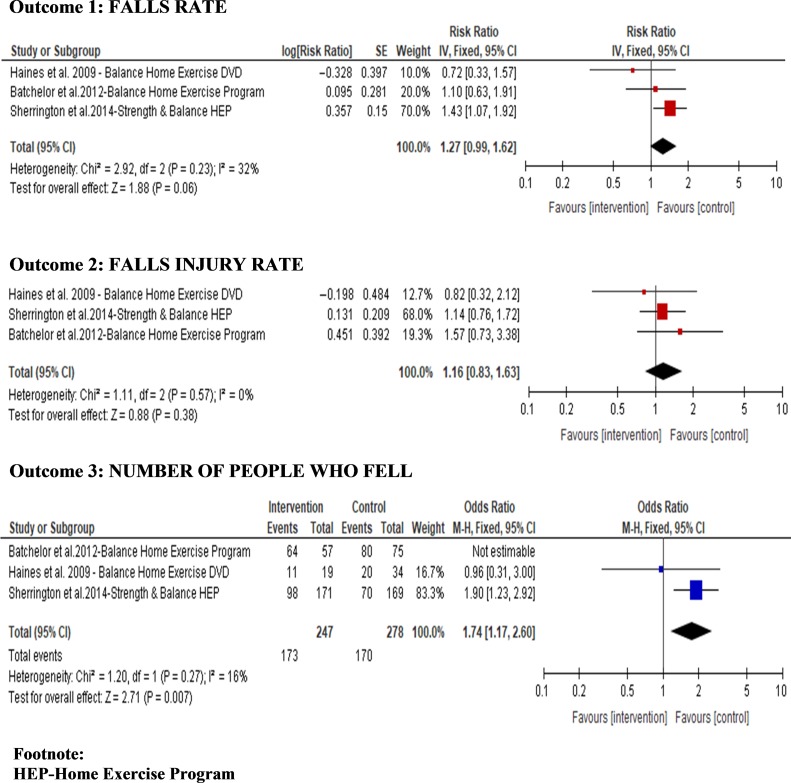
Home exercise intervention
Meta-analysis of falls rate data from three studies in the home exercise group of interventions showed moderate heterogeneity (I2 = 32% P = 0.23), this may have been due to the differing doses of intervention and clinical variation in the populations across the studies. Overall the intervention did not significantly reduce falls (RR 1.27, 95%CI, 0.99, 1.62), or falls injuries (RR 1.16, 95%CI, 0.83,1.63), however meta-analysis from two studies found a significant increase in proportion of fallers (OR 1.74, 95%CI, 1.17, 2.60) (Figure 2).
Figure 2.
Forest plots (pooled) overall effect of home exercise on falls outcomes.
Short-term nutritional supplementation intervention
A single study provided a multi-component nutritional intervention that included cholecalciferol supplementation for malnourished older adults commencing at hospital admission and continuing to 3 months after discharge. Falls rates were treated as binary data (participants did/did not fall), describing the hazard ratio of patients experiencing one or more falls, with an overall significant reduction in the number of people who fell (HR 0.41, 95% CI, 0.19, 0.86) at the study level.
There were six further interventions analysed at the study level, these are described in Supplementary Appendix 8 available in Age and Ageing online. The interventions included cholecalciferol therapy, inpatient falls prevention education and education provided at discharge, geriatric team management, inpatient balance circuit training, high-intensity quadriceps resistance training, and day hospital strength and balance training
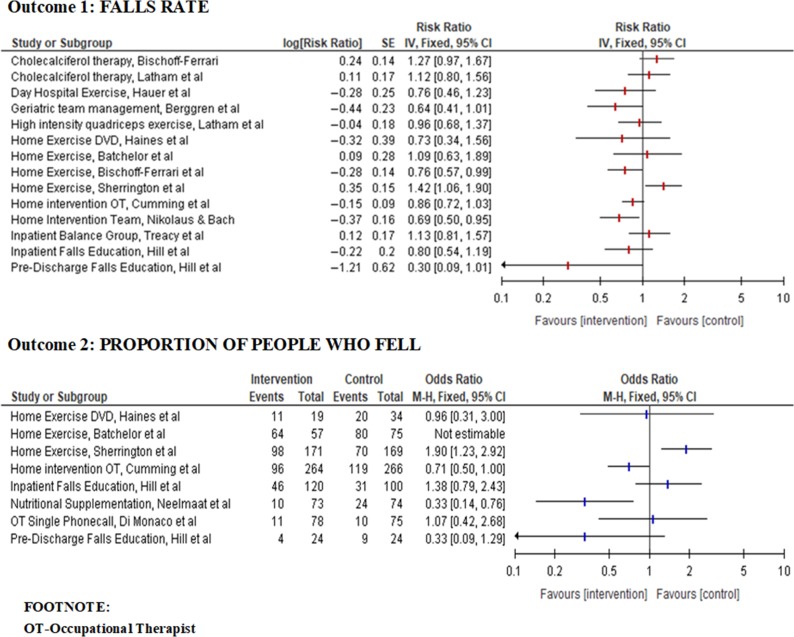
Overall comparison of effect of interventions (un-pooled)
The effects of all interventions, categorised according to studies, are presented using an un-pooled forest plot in Figure 3 (effect of all interventions on falls rates and proportion of people who fell). Six interventions were found to be ineffective in this population, including a single occupational therapist phone call, a balance home exercise programme using an instructional DVD, a non-supervised strength and balance home exercise programme, an inpatient balance home exercise programme, cholecalciferol therapy, and an inpatient falls education programme.
Figure 3.
Forest plots (un-pooled) effect of interventions on falls rate and proportion of people who fell.
There was between study variation in GRADE quality of evidence for the effect of home exercise intervention on falls outcomes (Table 1), despite heterogeneity scores during meta-analysis being low (Figure 2). This could be related to the clinical variation across the studies population, including older people diagnosed as high falls risk following a recent stroke, and discharged from general surgical and medical wards (Supplementary Appendix 3). We would advise caution against overinterpreting the GRADE recommendation, and guide readers to consider home exercise intervention content, dose, duration, delivery setting and supervision at the study level.
Table 1.
GRADE Summary of the evidence
| Number of Participants (studies) | Quality of the evidence (GRADE) | ANTICIPATED ABSOLUTE EFFECTS | ||
|---|---|---|---|---|
| Relative effects (%) | Absolute effect with intervention [95% CI] | |||
| HOME EXERCISE INTERVENTION | ||||
| Bibliography: Batchelor et al., (2012); Sherrington et al. (2014); Haines et al. (2009) | ||||
| Incident rate of falls Pooled | N = 525 participants (three studies) | ⊕⊝⊝⊝VERY LOW1,2 due to inconsistency and imprecision | – | Risk ratio for falls in the intervention groups was 1.27 [0.99–1.62] |
| Incident rate ratio of falls injury rate Pooled | N = 525 (three studies) | ⊕⊕⊝⊝LOW1 due to imprecision | – | Risk ratio for falls injuries in the intervention groups was 1.16 [0.83–1.63] |
| Proportion of fallers Pooled | N = 369 (two studies) | ⊕⊕⊕⊝ MODERATE | – | Odds ratio for proportion of fallers with intervention was 1.74 [1.17, 2.60] |
| NUTRITIONAL SUPPLEMENTATION | ||||
| Bibliography: Neelmaat et al. (2012) | ||||
| Proportion of fallers | N = 210 (one study) | ⊕⊕⊝⊝LOW due to only one study | – | Hazard ratio for proportion of fallers with intervention was 0.41 [0.19, 0.86] |
1Imprecision: the 95% CI of the pooled estimate included one or no effect.
2Inconsistency: heterogeneity may be explained by the differing characteristics of the populations, content and duration of the intervention across the studies.
GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate.
The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University, 2015 (developed by Evidence Prime, Inc.). http://www.gradepro.org [Accessed 16 March 2017].
Recommendations based on the evidence
Table 1 illustrates the summary of the evidence using the GRADE approach. [62]
Discussion
Summary of findings
The present systematic review and meta-analysis is the first to synthesise evidence of effective falls prevention interventions for older adults following recent hospital discharge. Overall results indicated there was limited evidence that home hazard modifications reduced falls outcomes, though the intervention was more effective among a subgroup of participants who had a frequent falls history. Home hazard modifications have previously been found to be effective in preventing falls among the general community population [16], and are frequently a component of hospital discharge plans [63–65]. These previous findings suggest that if these interventions were tailored and evaluated specifically for older adults recently discharged from hospital, there could be a greater amount of evidence of their effectiveness for falls prevention during the post-discharge period.
Previous evidence has shown that falls prevention exercise programmes are beneficial for older adults in the community setting, however, the findings of this review indicate they may have a different effect in older adults recently discharged from hospital. There are many precipitating factors to be considered in providing home exercise falls interventions to older adults following hospital discharge, including the likely need for regular supervision over an extended period to increase safety, challenge balance and maintain compliance [43, 66–69]. A large meta-analysis led by Sherrington et al. [18] concluded that falls prevention programmes that include a moderate to high challenge to balance are associated with a reduction in falls among community-dwelling older adults. However, when these exercise parameters were introduced to older adults recently discharged from hospital [43], this led to an increase in the number of falls, falls injuries, and proportion of fallers. The components of the home exercise programmes that may assist to explain this effect include no direct supervision or limited one-on-one supervision of the exercises, and recommended frequencies of 30–40 min at least 3–6 days per week. Since this population is generally functionally declined, participants may have required more supervision initially, and a lower commencement dosage of exercise.
This review found that cholecalciferol therapy did not significantly reduce falls in older adults discharged from hospital. Although previous reviews have demonstrated a protective effect of cholecalciferol therapy on falls in community-dwelling and institutionalised older adults [16, 70], some more recent RCTs have concluded a higher risk of falls at higher doses, particularly for older adults with a previous falls history [71]. Despite the lack of evidence for falls prevention following hospital discharge, falls prevention guidelines recommend at least 800 international units of vitamin D per day for those with proven or suspected vitamin D deficiency, abnormal gait and risk of falls [72].
Previous reviews have indicated that patient population may impact outcomes of falls prevention interventions, such as older adults who are frail and at risk of functional decline following recent hospital discharge [15, 19, 22, 64]. Critical elements of frailty, such as muscle weakness and malnutrition are associated with falls and functional decline [73]. A multi-factorial intervention incorporating an individualised home programme for frail older adults improved risk factors for falls but did not reduce rate of falls [74]. One study in this review that provided nutrition supplementation for malnourished older adults was effective in reducing the proportion of people who fell post-discharge [42], indicating interventions that target elements of frailty are likely to have a positive effect on falls risk factors and falls outcomes. This result is consistent with previous RCTs and systematic reviews [21, 64, 75–77].
Study strengths and limitations
This systematic review was a comprehensive undertaking with a large range of falls prevention interventions analysed. Falls prevention interventions that are effective in the general older population may require tailoring to be effective for older adults recently discharged from hospital. There are additional and possibly specific factors to be considered in delivering interventions to this population, including the need for regular supervision and support to aid functional recovery and prevention of hospital re-admission.
Although this review did not find one falls prevention intervention was significantly effective overall, there is a possibility that tailoring different components of the interventions to the identified falls risks, physical and social needs of the older person, could lead to better uptake of falls prevention strategies. Although a large systematic review investigating falls prevention found multi-factorial interventions were implemented in 19 trials, [16] we found no trials that evaluated multi-factorial falls interventions in the post-discharge setting. Targeted multi-dimensional falls risk assessment and management offered by multi-disciplinary specialists for older adults following hospital discharge is warranted. Especially considering current healthcare services tend to discharge older adults from hospital with ongoing medical illnesses, frailty and risk of further falls. This is a consideration for future research as multi-factorial falls interventions have been shown to be effective for falls prevention of older adults in the community setting [16].
A possible limitation of this review is the grouping of interventions that necessitated simplification of often complex interventions. The analysis is based on overall effects of the intervention categories, without consideration of characteristics of individual participants, modification of intervention doses, or adherence to interventions.
Despite efforts to be comprehensive in our choice of search terms, we did not cover all MeSH terms such as ‘elderly’ and ‘seniors’, and so there is potential that studies were not found during our search strategy and screening process. However, the MeSH terms used in our search include ‘frail elderly’ as well as people ‘aged 65–79 years’, and during the final search phase, we hand-searched reference lists of all studies examined in full text to strengthen our search.
Conclusion
Falls is a serious problem for older adults who have recently been discharged from hospital, with associated decline in quality of life and functional independence [9–13]. Falls prevention interventions found to be effective in the general older population are not necessarily transferrable to older adults following hospital discharge.
We found low to moderate quality GRADE evidence following data-analysis from studies grouped according to interventions. The recommended falls prevention interventions for older adults recently discharged from hospital are to provide home hazard minimisation particularly if they have a recent previous falls history and consider nutritional supplementation if they are malnourished. Future randomised controlled trials to investigate the post-discharge falls prevention effects of tailored education, multi-factorial falls interventions and structured supervised exercise programmes are warranted. Falls prevention interventions for this population may need to be tailored to the individual older patient, with planned review after hospital discharge to support uptake of falls prevention strategies.
Key points.
There is a range of falls interventions delivered in a limited number of small studies for the post-discharge older population with potential high risk of bias.
Falls prevention interventions effective in the general older population are not automatically transferrable in the post-discharge setting and may need to be tailored to the individual older patient, with post-discharge review to support uptake.
Recommendations based on the evidence are to implement home hazard minimisation particularly if there is a history of recent falls and consider nutritional supplementation if the older adult is malnourished.
Future research to investigate the post-discharge falls prevention effects of tailored education, multi-factorial interventions, and structured supervised exercise programmes is warranted.
Supplementary Material
Supplementary data
Supplementary data mentioned in the text are available here.
Conflict of interest
Ms. Naseri reports a stipend from Curtin University (2016–2019) to undertake a PhD and received as part of a Project grant (App1078918) from the National Health and Medical Research Council of Australia.
Funding
Authors SM, TH, MEM, JF-C, CE-B, D-CAL, LF, AMH have received a grant from the National Health and Medical Research Council (Australia) to conduct a trial which investigates how to reduce falls and promote independence in older people after hospital discharge (Project App no:1078918). CN receives a post graduate student stipend as part of the grant. This grant funding has not been received directly to the authors rather to the institutions they represent. SM receives funding support from the National Health and Medical Research Council (Australia, APP). The authors have not received financial support for this study.
References
- PLEASE NOTE: The very long list of references has meant that only the most important are listed here and are represented by bold type throughout the text. The full list of references is available in Appendix 4, available in Age and Ageing online.
- *denotes study included in the systematic review
- 2. Bradley C. Hospitalisations due to falls in older people, Australia 2008-09. Injury research and statistics series no. 62. Cat. no. INJCAT 138. Canberra: Australian Institute of Health and Welfare, 2012. Canberra: Australia. http://www.aihw.gov.au/publication-detail/?id=10737421923
- 4. Wolinsky FD, Bentler SE, Liu L et al. Recent hospitalization and the risk of hip fracture among older Americans. J Gerontol A Biol Sci Med Sci 2009; 64: 249–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mahoney JE, Palta M, Johnson J et al. Temporal association between hospitalization and rate of falls after discharge. Arch Intern Med 2000; 160: 2788–95. [DOI] [PubMed] [Google Scholar]
- 10. Sager MA, Franke T, Inouye SK et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 1996; 156: 645–52. [PubMed] [Google Scholar]
- 14. Hill AM, Hoffmann T, McPhail S et al. Evaluation of the sustained effect of inpatient falls prevention education and predictors of falls after hospital discharge-follow-up to a randomized controlled trial. J Gerontol A Biol Sci Med Sci 2011; 66: 1001–12. [DOI] [PubMed] [Google Scholar]
- 16. Gillespie LD, Robertson MC, Gillespie WJ et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012; 9: Cd007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sherrington C, Tiedemann A, Fairhall N et al. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. NSW Public Health Bull 2011; 22: 78–83. [DOI] [PubMed] [Google Scholar]
- 21. Mistiaen P, Francke AL, Poot E. Interventions aimed at reducing problems in adult patients discharged from hospital to home: a systematic meta-review. BMC Health Serv Res 2007; 7: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Conroy SP, Stevens T, Parker SG et al. A systematic review of comprehensive geriatric assessment to improve outcomes for frail older people being rapidly discharged from acute hospital: ‘interface geriatrics’. Age Ageing 2011; 40: 436–43. [DOI] [PubMed] [Google Scholar]
- 23. Lee D-CA, Pritchard E, McDermott F et al. Falls prevention education for older adults during and after hospitalization: a systematic review and meta-analysis. Health Educ J 2014; 73: 530–44. [Google Scholar]
- 24. Naseri C, McPhail S, Francis-Coad J et al. Effectiveness of falls prevention interventions for older adults newly discharged from hospital: a systematic review protocol. JBI Database System Rev Implement Rep 2017; 15: 686–93. [DOI] [PubMed] [Google Scholar]
- 28. Lamb S, Becker C, Gillespie L et al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials 2011; 12: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Higgins J, Thompson S, Deeks J et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tufanaru C, Munn Z, Stephenson M, Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int J Evid Based Healthc 2015; 13: 196–207. [DOI] [PubMed] [Google Scholar]
- 39. *Di Monaco M, Vallero F, De Toma E et al. A single home visit by an occupational therapist reduces the risk of falling after hip fracture in elderly women: a quasi-randomized controlled trial. J Rehabil Med 2008; 40: 446–50. [DOI] [PubMed] [Google Scholar]
- 40. *Hill AM, Etherton-Beer C, Haines TP. Tailored education for older patients to facilitate engagement in falls prevention strategies after hospital discharge-a pilot randomized controlled trial. PLoS One 2013; 8: e63450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. *Sherrington C, Lord SR, Vogler CM et al. A post-hospital home exercise program improved mobility but increased falls in older people: a randomised controlled trial. PLoS One 2014; 9: e104412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. *Hauer K, Rost B, Rűtschle K et al. Exercise training for rehabilitation and secondary prevention of falls in geriatric patients with a history of injurious falls. J Am Geriatr Soc 2001; 49: 10–20. [DOI] [PubMed] [Google Scholar]
- 48. *Berggren M, Stenvall M, Olofsson B, Gustafson Y. Evaluation of a fall-prevention program in older people after femoral neck fracture: a one-year follow-up. Osteoporos Int 2008; 19: 801–9. [DOI] [PubMed] [Google Scholar]
- 52. *Haines TP, Russell T, Brauer SG et al. Effectiveness of a video-based exercise programme to reduce falls and improve health-related quality of life among older adults discharged from hospital: a pilot randomized controlled trial. Clin Rehabil 2009; 23: 973–85. [DOI] [PubMed] [Google Scholar]
- 55. Russell M, Hill K, Day L et al. Development of the falls risk for older people in the community (FROP-Com) screening tool. Age Ageing 2009; 38: 40–6. [DOI] [PubMed] [Google Scholar]
- 58. Porritt K, Gomersall J, Lockwood C. JBI’s systematic reviews: study selection and critical appraisal. Am J Nurs 2014; 114: 47–52. [DOI] [PubMed] [Google Scholar]
- 62. Guyatt GH, Oxman AD, Vist GE et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336: 924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Shepperd S, Lannin NA, Clemson LM et al. Discharge planning from hospital to home. Cochrane Database Syst Rev 2013; 1: Cd000313. [DOI] [PubMed] [Google Scholar]
- 66. Nyman SR, Victor CR. Older people’s participation in and engagement with falls prevention interventions in community settings: an augment to the Cochrane systematic review. Age Ageing 2012; 41: 16–23. [DOI] [PubMed] [Google Scholar]
- 70. Glendenning P, Zhu K, Inderjeeth C et al. Effects of three-monthly oral 150,000 IU cholecalciferol supplementation on falls, mobility, and muscle strength in older postmenopausal women: a randomized controlled trial. J Bone Miner Res 2012; 27: 170–6. [DOI] [PubMed] [Google Scholar]
- 71. Bruyere O, Cavalier E, Souberbielle JC et al. Effects of vitamin D in the elderly population: current status and perspectives. Arch Public Health 2014; 72: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011; 59: 148–57. [DOI] [PubMed] [Google Scholar]
- 73. Gill TM, Williams CS, Tinetti ME. The combined effects of baseline vulnerability and acute hospital events on the development of functional dependence among community-living older persons. J Gerontol A Biol Sci Med Sci 1999; 54: M377–83. [DOI] [PubMed] [Google Scholar]
- 77. Chang JT, Morton SC, Rubenstein LZ et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ 2004; 328: 680. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.