Abstract
Background
Guidelines recommend pulmonary rehabilitation (PR) after hospitalization for an exacerbation of COPD, but few patients enroll in PR. We explored whether density of PR programs explained regional variation and racial disparities in receipt of PR.
Methods
We used Centers for Medicare & Medicaid Services data from 223,832 Medicare beneficiaries hospitalized for COPD during 2012 who were eligible for PR postdischarge. We used Hospital-Referral Regions (HRR) as the unit of analysis. For each HRR, we calculated the density of PR programs as a measure of program access and estimated risk-standardized rates of PR within 6 months of discharge overall, and for non-Hispanic, white, and black beneficiaries. We used linear regression to examine the relationship between access to PR and HRR PR rates. We tested for racial disparity in PR rates among non-Hispanic white and black beneficiaries living in the same HRRs.
Results
Across 306 HRRs, the median number of PR programs per 1,000 Medicare beneficiaries was 0.06 (interquartile range [IQR], 0.04-0.10). Risk-standardized rates of PR ranged from 0.53% to 6.67% (median, 1.93%). Density of PR programs was positively associated with PR rates overall and among non-Hispanic white beneficiaries (P < .001), but this relationship was not observed among black beneficiaries. Rates were higher among non-Hispanic white beneficiaries (median, 2.08%; IQR, 1.54%-2.87%) compared with black beneficiaries (median, 1.19%; IQR, 1.15%-1.20%).
Conclusions
Greater PR program density was associated with higher rates of PR for non-Hispanic white but not black beneficiaries. Further research is needed to identify reasons for this discrepancy and strategies to increase receipt of PR for black patients.
Key Words: geographic analysis; Medicare; pulmonary disease, chronic obstructive; pulmonary rehabilitation; racial disparties
Abbreviations: FFS, fee-for-service; HCPCS, healthcare common procedure coding system; HRR, hospital referral region; PR, pulmonary rehabilitation
FOR EDITORIAL COMMENT, SEE PAGE 1070
More than 15 million individuals in the United States have been diagnosed with COPD, which was the fourth leading cause of death in 2017.1 In 2010, $32.1 billion was spent on COPD, and in 2020 those costs are projected to reach $49 billion.2 Although COPD has no cure, pulmonary rehabilitation (PR) improves patient outcomes and reduces hospital readmissions.3,4 Current guidelines recommend that patients hospitalized for COPD begin PR within 3 to 4 weeks of discharge.5,6 Despite its many benefits, PR is underused; fewer than 2% of patients receive PR within 6 months of hospitalization in the United States.7,8 Patient factors such as race and socioeconomic status are strongly associated with PR participation,8,9 and prior studies have found that black beneficiaries are less likely to receive PR than non-Hispanic white (NHW) beneficiaries.7, 8, 9
Where a patient lives is associated with his or her chances of receiving PR.10,11 This is at least partially driven by differences in access to PR; for example, 1,776 counties in the United States do not have a hospital outpatient PR program.12 Thus, there is reason to believe that differences in access to PR may contribute to the observed racial disparities in PR participation because black Medicare beneficiaries often reside in areas with different resources than NHW beneficiaries.13 Alternatively, disparities in PR participation could be driven by patient or physician behavior within the same geographic context, for example, physicians may be less likely to refer black patients to PR, or black patients may be less willing or able to attend.
In this study, we sought to determine whether access to PR, as measured by PR program density, was associated with rates of PR participation following a hospitalization. Further, we examined whether geographic variation in PR program density could account for previously observed differences in rates of PR participation between black and NHW Medicare beneficiaries.
Methods
Design, Setting, and Study Population
We conducted a retrospective study using the Centers for Medicare and Medicaid Services beneficiary summary files and standard analytic files that include individuals hospitalized in an acute care hospital in 2012. We selected patients with a principal diagnosis of COPD or a principal diagnosis of acute respiratory failure combined with a secondary diagnosis of COPD with acute exacerbation, defined in accordance with methods used by the Centers for Medicare and Medicaid Services.14
We restricted the cohort to individuals who were continuously enrolled in the Medicare fee-for-service (FFS) program for at least 1 year following their index admission to assess receipt of PR. We limited the study to individuals 66 or older to ensure that all subjects had at least 1 year of claims data before the index hospitalization to assess comorbidities and health-care use. To focus on those individuals who would likely benefit and be eligible to participate in PR, we excluded patients who were hospitalized for more than 30 days at their index hospitalization, died within 30 days of their index hospitalization, or were transferred to another acute care facility, hospice, long-term care facility, or court or law enforcement, or discharged against medical advice.
Measures
We identified patients who had initiated PR at both facility and office-based programs within 6 months of their index hospitalizations using health-care common procedure coding system codes (G0424, G0237, G0238, and G0239).
We used the Hospital Referral Region (HRR) as the geographic unit of analysis. The Dartmouth Atlas of Health Care divides the United States into 306 HRRs with the intention of defining local health-care markets. Boundaries were derived from Medicare beneficiary data and have been used extensively to study geographic variation in the quality and cost of care, including racial disparities.13,15 We used patients’ ZIP code of residence to determine in which HRR they lived.
To measure access to PR, we identified providers of PR on the basis of claims submitted for PR services using health-care common procedure coding system codes. Each provider was assigned to an HRR on the basis of ZIP code. If there were multiple providers at one address, we considered the additional provider(s) part of the same PR program. We created two measures of access to PR on the basis of PR program density. First, we calculated the number of PR programs per 1,000 Medicare FFS beneficiaries over the age of 65. Second, we calculated the number of PR programs per 1,000 patients hospitalized for COPD in our cohort.
To calculate risk-standardized, HRR-specific rates of PR participation within 6 months of hospital discharge, we developed a hierarchical model with random intercepts for HRR. The model adjusted for age, sex, comorbidity burden, number of admissions during the prior year, current tobacco use, and dual eligibility for Medicaid, a proxy for lower socioeconomic status.16 We repeated this analysis to calculate rates among NHW and black beneficiaries separately.
Statistical Analysis
To test the hypothesis that increased access to PR is associated higher PR rates, we fitted a linear regression model where the outcome variable was the HRR risk-standardized rate of PR. As our independent variable, we included the number of PR programs per 1,000 Medicare FFS beneficiaries. To control for confounding, additional variables in the model were the number of patients hospitalized with COPD per 1,000 Medicare FFS beneficiaries, percent of Medicare beneficiaries per HRR who are black, percent of HRR residents living at or below 200% of the federal poverty line, and unemployment rate. The region (West, Northeast, Midwest, or South) was included to help adjust for the fact that rates of PR clustered by region. To test the robustness of our findings related to access to PR providers, we also fitted a model in which we included number of PR programs per 1,000 Medicare FFS beneficiaries hospitalized for COPD in our cohort.
Next, we restricted our analysis to 177 HRRs, in which at least 2.5% of the Medicare population was black, to ensure greater stability in the risk-standardized rate estimates. To test the hypothesis that HRR risk-standardized rates of PR receipt among black Medicare beneficiaries are lower than rates among NHWs within the same region, we conducted a paired t-test for a difference in NHW and black risk-standardized rates of PR. Finally, grouping HRRs into tertiles on the basis of the density of PR programs, we compared PR rates among black and NHW beneficiaries within each tertile and tested for race differences using paired t-tests.
Results
Our study cohort included 223,832 Medicare beneficiaries hospitalized for COPD in 2012 who were potentially eligible to initiate PR following discharge, of whom 87% had a principal diagnosis of COPD. The median age was 77 (interquartile range [IQR], 71-83), 41% were men, 85% NHW, 8% black, and 5% Hispanic. Only 1.9% of patients received PR within 6 months of their hospital discharge.
Geographic Analysis
In 2012, the median number of Medicare FFS beneficiaries older than age 65 in an HRR was 63,912 (IQR, 34,930-109,982), 85.5% (IQR, 80.4-94.7) of beneficiaries were NHW, 3.4% (IQR, 1.1-8.6) were black, non-Hispanic, and 1.6% (IQR, 0.6-4.4) were Hispanic (Table 1).
Table 1.
Hospital Referral Region Summary Statistics, 2012 (n = 306)
| Variable | Median | Lower Quartile | Upper Quartile |
|---|---|---|---|
| Medicare FFS patients | 63,912 | 34,930 | 109,982 |
| Medicare FFS beneficiaries hospitalized for COPD | 483 | 290 | 851 |
| Share of Medicare FFS beneficiaries | |||
| Non-Hispanic white | 89.42% | 80.42% | 94.71% |
| Non-Hispanic black | 3.42% | 1.10% | 8.56% |
| Hispanic | 1.57% | 0.63% | 4.43% |
| Medicaid eligible | 13.01% | 10.15% | 16.47% |
| PR programs/HRR | 4 | 2 | 8 |
| PR programs/1,000 Medicare FFS beneficiaries | 0.06 | 0.04 | 0.10 |
| PR programs/1,000 Medicare FFS beneficiaries hospitalized for COPD | 7.96 | 5.24 | 13.16 |
| Share of HRR population | |||
| Unemployed | 8.96 | 7.53 | 10.40 |
| At or below 200% FPL | 37.19 | 32.07 | 41.63 |
| Risk-standardized rate pulmonary rehabilitation | 1.93% | 1.39% | 2.70% |
| Risk-standardized rate pulmonary rehabilitation, non-Hispanic white | 2.08% | 1.54% | 2.87% |
| Risk-standardized rate pulmonary rehabilitation, non-Hispanic black | 1.19% | 1.15% | 1.20% |
FFS = fee-for-service; FPL = federal poverty level; HRR = hospital referral region; PR = pulmonary rehabilitation.
Source: CMS files, 2012 CMS PUF, 2012-2014 American Community Survey. Note: Risk-standardized rates are adjusted for age, sex, comorbidity burden, admissions during prior year, current tobacco use, and Medicaid dual eligibility.
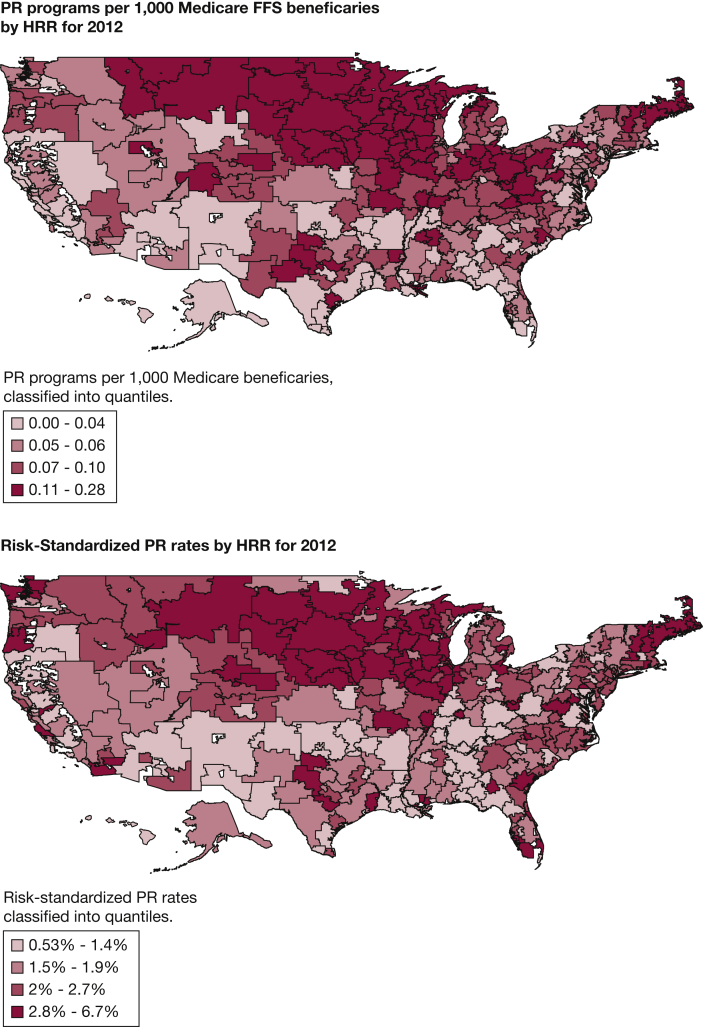
From our cohort, a median of 483 (IQR, 290-851) beneficiaries per HRR were hospitalized for COPD in 2012. The median number of PR programs per HRR was 4 (IQR, 2-8). The median PR density was 0.06 (IQR, 0.04-0.10) programs per 1,000 Medicare FFS beneficiaries and density ranged from a high of 0.28 PR programs per 1,000 in LaCrosse, Wisconsin, to a low of 0 in 12 HRRs with no PR programs. The HRRs with no PR programs were located in the South, Northeast, and Hawaii. The median HRR-specific risk-standardized rate of PR within 6 months of a hospitalization for COPD was 1.93% (IQR, 1.39-2.70). Risk-standardized rates ranged from a low of 0.53% in Oklahoma City to a high of 6.66% in Lincoln, Nebraska. Figure 1 presents maps of the overall, HRR-specific, risk-standardized rates of PR and the density of PR programs per 1,000 Medicare FFS Beneficiaries. These maps highlight the concentration of PR programs in the Midwest, as well as the higher rates of participation seen in that region.
Figure 1.
A, PR programs per 1,000 Medicare FFS beneficiaries by HRR for 2012. B, Risk-standardized PR rates for by HRR for 2012. Source: Authors’ calculations on the basis of Centers for Medicare & Medicaid Services public use files and fee-for-service files. Note: Risk-standardized rates are adjusted for age, sex, comorbidity burden, admissions during prior year, current tobacco use, and Medicaid dual eligibility. HRR = hospital referral region; PR = pulmonary rehabilitation.
Risk-standardized rates of PR were positively associated with the density of PR providers (Table 2). An increase in the density of PR of 1 SD, equivalent to adding 1 PR facility per 20,000 Medicare beneficiaries, was associated with a 0.55 percentage point increase in the rate of PR in an HRR, holding all else constant. Region was also associated with HRR rates, with the West having the lowest rates of participation. Compared with HRRs in the West, HRRs in the Northeast had PR rates 0.39 (P = .061) percentage points higher, Southern HRRs are 0.54 (P = .007) percentage points higher, and Midwestern HRRs are 0.55 (P = .006) percentage points higher. Although other HRR factors were statistically significant, the associations were not clinically meaningful.
Table 2.
Factors Associated with HRR-Specific Rates of PR after Hospitalization for COPD
| Variable | Model 1 |
Model 2 |
||
|---|---|---|---|---|
| Estimate | Pr > |t| | Estimate | Pr > |t| | |
| No. PR programs/1,000 Medicare FFS beneficiaries | 10.25 | <.001 | … | … |
| No. PR programs/1,000 Medicare FFS beneficiaries hospitalized for COPD | … | … | 0.06 | <.001 |
| No. of COPD hospitalized patients/1,000 Medicare FFS beneficiary | -0.11 | <.001 | -0.04 | 0.168 |
| Percent Medicare FFS beneficiary black | -0.02 | 0.017 | -0.02 | 0.018 |
| Percent of residents living at or below 200% federal poverty line | -0.03 | <.001 | -0.03 | <.01 |
| Percent of residents unemployed | 0.12 | <.001 | 0.10 | <.01 |
| Region (West referent) | ||||
| Northeast | 0.39 | 0.061 | 0.47 | 0.029 |
| Midwest | 0.55 | 0.006 | 0.71 | <.001 |
| South | 0.54 | 0.007 | 0.55 | <.01 |
| Intercept | 2.15 | <.001 | 1.74 | <.001 |
| N | 306 | … | 306 | … |
| R2 | 0.39 | … | 0.36 | … |
See Table 1 for expansion of abbreviations.
Note: Risk-standardized rates are adjusted for age, sex, comorbidity burden, admissions during prior year, current tobacco use, and Medicaid dual eligibility.
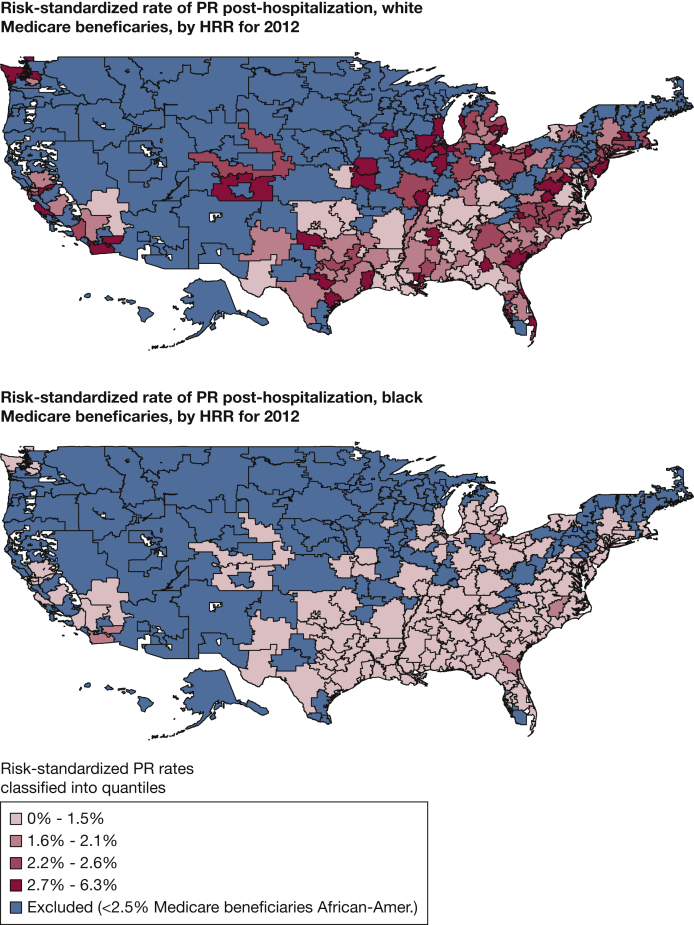
Risk-standardized, HRR-specific rates of PR participation following hospitalization for COPD were higher among NHW beneficiaries (2.08%; IQR, 1.54-2.87) compared with black beneficiaries (1.19%; IQR, 1.15-1.20) (Table 1). HRR risk-standardized rates of pulmonary rehabilitation among black Medicare beneficiaries were consistently lower than NHW beneficiaries. Furthermore, there was less variation across HRRs for black beneficiaries compared with NHW beneficiaries. In HRRs where at least 2.5% of the Medicare population older than age 65 was black, the mean difference between NHW and black risk-standardized HRR rates of PR was 0.96 percentage points (P < .001). Figure 2 illustrates that risk-standardized PR rates for black beneficiaries were consistently low across HRRs, even in HRRs where NHW beneficiary rates were above the national rate. For example, the Ormond Beach, Florida, HRR had the fourth highest PR rate overall of 6.03%. In this HRR, the PR rate for NHWs was 6.34% but the rate for black beneficiaries was 1.28%. The Blue Island, Illinois, HRR has the highest risk-standardized rate for black beneficiaries (1.84%); however, this was still lower than the national overall rate and lower than the rate among NHWs in the same HRR (3.33%).
Figure 2.
A, Risk-standardized rate of PR posthospitalization, non-Hispanic white Medicare beneficiaries, by HRR for 2012. B, Risk-standardized rate of PR posthospitalization, black Medicare beneficiaries, by HRR for 2012. Source: Authors’ calculations on the basis of Centers for Medicare & Medicaid Services public use files and fee-for-service files. Note: Risk-standardized rates are adjusted for age, sex, comorbidity burden, admissions during prior year, current tobacco use, and Medicaid dual eligibility. See Figure 1 legend for expansion of abbreviations.
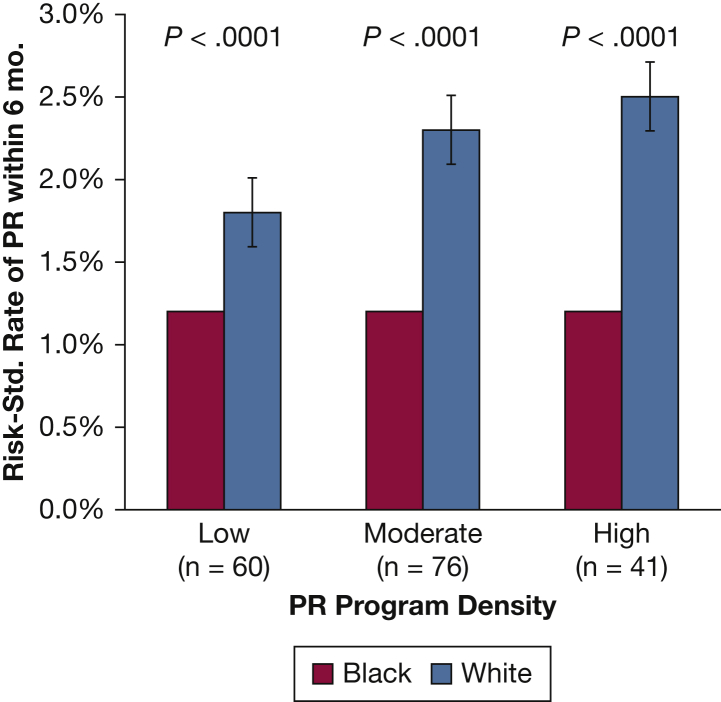
Among black COPD beneficiaries, PR rates were significantly lower than among NHW beneficiaries, regardless of the density of programs. This can be seen by comparing the upper map in Figure 1 to the lower map in Figure 2. In addition, when we divided HRRs into tertiles on the basis of program density, we found a positive association between density and participation among NHW patients with COPD, but no association between density of providers and rates among black patients with COPD. The relationship between the density of PR programs and rates of PR holds only for NHW beneficiaries (Fig 3).
Figure 3.
2012 risk-standardized PR rates, by HRR PR program density. Note: A total of 306 HRRs were divided into tertiles on the basis of PR program density; HRRs were then excluded, with less than 2.5% black Medicare fee-for-service beneficiaries. Risk-standardized rates are adjusted for age, sex, comorbidity burden, admissions during prior year, current tobacco use, and Medicaid dual eligibility. Program density is the number of PR programs divided by 1,000 Medicare FFS beneficiaries older than age 65 per HRR: Low was defined as 0 to 0.047 providers/1,000 Medicare FFS beneficiaries; moderate as 0.048 to 0.088; and high as 0.088 to 0.280. See Figure 1 legend for expansion of abbreviations.
Discussion
In this study of more than 220,000 US Medicare beneficiaries hospitalized for COPD in 2012, we found significant variation between HRRs in rates of PR after discharge, which was only partially explained by the availability of PR providers. Importantly, we found that although higher levels of PR program density were associated with higher rates of PR for NHW beneficiaries, this relationship did not hold for black beneficiaries. These findings suggest that disparity in the rate of PR participation according to race is not explained by regional differences in access to PR. Although in several HRRs, NHW Medicare beneficiaries are two to three times more likely to receive PR than the national average; regardless of where black beneficiaries live, their likelihood of receiving PR remains consistently below the national average and below NHW peers in the same HRR.
Our findings add to research on the causes of health disparities in COPD and are consistent with prior studies that have found black patients with COPD use fewer health-care services than NHW patients.17,18 More research is needed to understand the forces driving the disparity in receipt of PR among black and NHW Medicare beneficiaries. One possibility is that providers may be more likely to refer NHW patients to PR than black patients. Along these lines, studies examining smoking cessation have found that doctors are less likely to offer smoking cessation advice and interventions to black patients.19,20 Studies of systemic and liaison-facilitated referral for cardiac rehabilitation have shown promising results in reducing disparities in underserved groups.21,22 Further, there is a large body of evidence demonstrating that black patients have lower levels of trust in their physicians, which may reduce their willingness to participate.23 Additionally, other factors associated with race may explain lower rates of PR among black patients, such as access to transportation, economic status, health literacy, social and family situations, and cultural beliefs.24 In addition, because PR is an inherently social program in which patients interact with each other and the staff, some patients may feel less comfortable attending PR in an environment where they are the minority.25 Qualitative studies that focus on the experience of black patients with COPD and studies that examine providers’ referral behaviors will be essential in identifying barriers and reducing the disparity identified in this study.
This study has several limitations. First, we do not have data on whether or not a patient was ever referred to PR; we only have information on whether a patient received PR. Thus, we were unable to determine whether the disparities in PR we observed were driven by physician or patient behavior. In addition, our primary outcome was participation in at least one session of PR; we did not examine likelihood to complete a full course of PR. Furthermore, the low rates of PR prevented us from conducting a more granular analysis of access to PR. Our results may have been different if we analyzed PR rates at a smaller geographic area, such as the neighborhood.26 Nonetheless, our analysis was the first to consider variation between HRRs, rather than Census regions or states. Unlike these political boundaries, HRRs were designed to reflect patterns of where patients seek medical care. Our measure of access, the density of PR programs, does not take into account differences in the size of programs, hours of operation, distance to programs, or travel time. In addition, density assigns the same level of access to all residents of an HRR regardless of where they live within the HRR; because HRRs span large geographic areas, two people living within the same HRR may have different abilities to access the same provider. We did not include a distance measure because we did not have access to beneficiaries’ home address, only ZIP code, making the calculation of a meaningful distance measure at the HRR level difficult. An additional limitation is that this study only includes data from 2012, and may not necessarily reflect current PR patterns. Finally, because our study relied on Medicare claims, our results may not be generalizable to younger populations. Nevertheless, examining patterns of care in the Medicare program is an advantage because it controls for differences in access to care among individuals related to insurance.
In conclusion, rates of PR participation following a hospitalization for COPD vary widely between regions the United States, and are only weakly associated with program density. Moreover, racial disparities in participation do not seem to be explained by differences in access, suggesting that simply building more PR programs will not mitigate this problem. Future research should explore why this is the case and identify strategies to increase PR participation among all patients with COPD, but particularly among black beneficiaries who may face additional barriers to accessing PR.
Acknowledgments
Author contributions: P. K. L., T. L., M. S. S, K. A. S., V. M. P.-P., Q. R. P., K. M., and P. S. P. conceived of and designed the study. P. S. P., A. P., and K. A. S. analyzed the data. All authors contributed to the interpretation of the results. K. A. S. drafted the manuscript. All authors contributed to revising the manuscript critically for important intellectual content. All authors give final approval of the version to be published. All authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Financial/nonfinancial disclosure: None declared.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Footnotes
FUNDING/SUPPORT: The research was supported by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH) [Grants K24 HL132008 and R01HL133046]. T.L. is supported by the NHLBI of the NIH [Grant K01HL114745]. Q.R.P. is supported by the NHLBI of the NIH [Grant K23HL135440]. The funders had no role in data collection, management, analysis; study design, conduct, or interpretation of study findings; or the preparation, review, or approval of the manuscript submitted for the publication.
References
- 1.National Heart, Lung, and Blood Institute What Is COPD? National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/health-topics/topics/copd/# Published April 28, 2017. Accessed November 29, 2017.
- 2.COPD Costs. Centers for Disease Control and Prevention. https://www.cdc.gov/copd/pubs/COPD-2014-Cost-Infographic-h.pdf
- 3.Puhan M.A., Gimeno-Santos E., Cates C.J., Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;12:CD005305. doi: 10.1002/14651858.CD005305.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. In: The Cochrane Collaboration, ed. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2015. [DOI] [PMC free article] [PubMed]
- 5.Criner G.J., Bourbeau J., Diekemper R.L. Prevention of acute exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest. 2015;147(4):894–942. doi: 10.1378/chest.14-1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wedzicha J.A., Miravitlles M., Hurst J.R. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2017;49(3) doi: 10.1183/13993003.00791-2016. [DOI] [PubMed] [Google Scholar]
- 7.Spitzer K.A., Stefan M.S., Priya A. Participation in pulmonary rehabilitation after hospitalization for chronic obstructive pulmonary disease among Medicare beneficiaries. Ann Am Thorac Soc. 2018;16(1):99–106. doi: 10.1513/AnnalsATS.201805-332OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nishi S.P.E., Zhang W., Kuo Y.-F., Sharma G. Pulmonary rehabilitation utilization in older adults with chronic obstructive pulmonary disease, 2003 to 2012. J Cardiopulm Rehabil Prev. 2016;36(5):375–382. doi: 10.1097/HCR.0000000000000194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vercammen-Grandjean C., Schopfer D.W., Zhang N., Whooley M.A. Participation in pulmonary rehabilitation by Veterans Health Administration and Medicare Beneficiaries after hospitalization for chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2018;38(6):406–410. doi: 10.1097/HCR.0000000000000357. [DOI] [PubMed] [Google Scholar]
- 10.Fan V.S., Giardino N.D., Blough D.K., Kaplan R.M., Ramsey S.D. Costs of pulmonary rehabilitation and predictors of adherence in the National Emphysema Treatment Trial. COPD J Chronic Obstr Pulm Dis. 2008;5(2):105–116. doi: 10.1080/15412550801941190. [DOI] [PubMed] [Google Scholar]
- 11.Oates G.R., Hamby B.W., Stepanikova I. Social determinants of adherence to pulmonary rehabilitation for chronic obstructive pulmonary disease. COPD. 2017;14(6):610–617. doi: 10.1080/15412555.2017.1379070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moscovice I.S., Casey M.M., Wu Z. Disparities in geographic access to hospital outpatient pulmonary rehabilitation programs in the United States. Chest. 2019;156(2):308–315. doi: 10.1016/j.chest.2019.03.031. [DOI] [PubMed] [Google Scholar]
- 13.Baicker K., Chandra A., Skinner J.S. Geographic variation in health care and the problem of measuring racial disparities. Perspect Biol Med. 2005;48(1 Suppl):S42–S53. [PubMed] [Google Scholar]
- 14.Dorsey K., Grady J.N., Desai N. 2016 Condition-Specific Measures Updates and Specifications Report Hospital-Level 30-Day Risk-Standardized Readmission Measures for Chronic Obstructive Pulmonary Disease (Version 5.0). Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE) http://aann.org/uploads/Condition_Specific_Readmission_Measures.pdf
- 15.Skinner J., Weinstein J.N., Sporer S.M., Wennberg J.E. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349(14):1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 16.Normand S.T., Shahian D.M. Statistical and clinical aspects of hospital outcomes profiling. Stat Sci. 2007;22(2):206–226. [Google Scholar]
- 17.Pleasants R., Riley I., Mannino D. Defining and targeting health disparities in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2016;11:2475–2496. doi: 10.2147/COPD.S79077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaya F.T., Maneval M.S., Gbarayor C.M. Burden of COPD, asthma, and concomitant COPD and asthma among adults. Chest. 2009;136(2):405–411. doi: 10.1378/chest.08-2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cokkinides V.E., Halpern M.T., Barbeau E.M., Ward E., Thun M.J. Racial and ethnic disparities in smoking-cessation interventions: analysis of the 2005 National Health Interview Survey. Am J Prev Med. 2008;34(5):404–412. doi: 10.1016/j.amepre.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Browning K.K., Ferketich A.K., Salsberry P.J., Wewers M.E. Socioeconomic disparity in provider-delivered assistance to quit smoking. Nicotine Tob Res. 2008;10(1):55–61. doi: 10.1080/14622200701704905. [DOI] [PubMed] [Google Scholar]
- 21.Grace S.L., Leung Y.W., Reid R. The role of systematic inpatient cardiac rehabilitation referral in increasing equitable access and utilization. J Cardiopulm Rehabil Prev. 2012;32(1):41–47. doi: 10.1097/HCR.0b013e31823be13b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gravely S., Anand S.S., Stewart D.E., Grace S.L., CRCARE Investigators Effect of referral strategies on access to cardiac rehabilitation among women. Eur J Prev Cardiol. 2014;21(8):1018–1025. doi: 10.1177/2047487313482280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Musa D., Schulz R., Harris R., Silverman M., Thomas S.B. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health. 2009;99(7):1293–1299. doi: 10.2105/AJPH.2007.123927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schraufnagel D.E., Blasi F., Kraft M., Gaga M., Finn P.W., Rabe K.F. An Official American Thoracic Society/European Respiratory Society Policy Statement: disparities in respiratory health. Am J Respir Crit Care Med. 2013;188(7):865–871. doi: 10.1164/rccm.201308-1509ST. [DOI] [PubMed] [Google Scholar]
- 25.Levack W.M., Jones B., Grainger R., Boland P., Brown M., Ingham T.R. Whakawhanaungatanga: the importance of culturally meaningful connections to improve uptake of pulmonary rehabilitation by Māori with COPD - a qualitative study. Int J Chron Obstruct Pulmon Dis. 2016;11:489–501. doi: 10.2147/COPD.S97665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kwan M.-P. The uncertain geographic context problem. Ann Assoc Am Geogr. 2012;102(5):958–968. [Google Scholar]