Abstract
Objective
The study sought to determine which patient characteristics are associated with the use of patient-facing digital health tools in the United States.
Materials and Methods
We conducted a literature review of studies of patient-facing digital health tools that objectively evaluated use (eg, system/platform data representing frequency of use) by patient characteristics (eg, age, race or ethnicity, income, digital literacy). We included any type of patient-facing digital health tool except patient portals. We reran results using the subset of studies identified as having robust methodology to detect differences in patient characteristics.
Results
We included 29 studies; 13 had robust methodology. Most studies examined smartphone apps and text messaging programs for chronic disease management and evaluated only 1-3 patient characteristics, primarily age and gender. Overall, the majority of studies found no association between patient characteristics and use. Among the subset with robust methodology, white race and poor health status appeared to be associated with higher use.
Discussion
Given the substantial investment in digital health tools, it is surprising how little is known about the types of patients who use them. Strategies that engage diverse populations in digital health tool use appear to be needed.
Conclusion
Few studies evaluate objective measures of digital health tool use by patient characteristics, and those that do include a narrow range of characteristics. Evidence suggests that resources and need drive use.
Keywords: population health informatics, digital health, health equity, social determinants of health
INTRODUCTION
Background and significance
Availability of interactive digital health tools that enable patients to access health information and personal health data has increased rapidly over the past decade, alongside growing access to the Internet and smartphone ownership.1–4 These patient-facing tools, including smartphone apps, text messaging programs, and social media tools, among others, have been associated with improved clinical and behavioral outcomes, such as preventive health behaviors, chronic disease management, and patient-provider communication.3,5–8
Despite both high availability and interest in digital health tools among ethnically, economically, and linguistically diverse patient groups,9,10 adoption (or use) of these tools by patients is low.2,3,11 Furthermore, data from national patient surveys and evaluations of patient portals in the United States demonstrate differential adoption of digital health tools by various groups based on sociodemographics.2,3,12–22 Specifically, older adults, racial or ethnic minorities, and those with low socioeconomic status, low educational attainment, limited health literacy, and chronic illness use patient portals less often compared with advantaged populations.19–22 There is also research demonstrating that patient-facing digital health tools themselves are at risk of exacerbating health disparities23 but that little effort has been undertaken to address this. For example, despite lack of uptake by diverse populations, there is little evidence that health systems incorporate approaches to address health disparities in the development, implementation, and use of patient portals.19,24
In a conceptual model for understanding and preventing such disparities, Veinot et al23 proposed that differences in access, adoption or use, adherence, or effectiveness of digital health tools contribute to their risk of exacerbating health disparities. Moreover, the effectiveness of digital health tools depends largely on access, adoption or use, and adherence.23 As described previously, effectiveness of digital health tools on various behavioral and clinical outcomes has been evaluated, and there is a significant body of research examining adoption or use of patient portals linked to electronic health records.25–28 However, we lack a review of evidence on adoption or use for the vast array of digital health tools beyond patient portals.29–33 In particular, there is little understanding of which patient characteristics are associated with use of these digital health tools, which may differ from those associated with patient portal use because they feature greater flexibility in design with respect to patient needs and preferences. In the setting of increasing availability and prioritization of patient-facing digital health tools and the risk of these tools widening existing health disparities, it is critical to better understand factors influencing their uptake.23,34,35
Objective
We conducted a literature review of studies of patient-facing digital health tools (excluding patient portals) to identify which patient characteristics were associated with adoption or use of these digital health tools in the United States. We included only studies with objective (rather than self-reported) measures of use (eg, system or platform usage data representing frequency or duration of use).
METHODS
We adhered to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines36; however, we did not present data synthesis, as this is a literature review rather than a systematic review.
Search strategy
We developed a search strategy in collaboration with a clinical librarian (J.B.W.) that combined 2 main concepts: health information technology (including search terms reflecting mobile and smartphone, apps, texting, and other mobile health and digital health terminology) and patient engagement (including search terms reflecting uptake and participation; see Supplementary Appendix A1 for complete details). We intentionally omitted the word use from the search strategy, as it was nonspecific (given the lack of uniform terminology to describe this construct) and yielded a large number of irrelevant articles. We conducted a search using Boolean operators that combined keywords and MeSH (Medical Subject Headings) terms in PubMed on July 27, 2018. Because of our specific focus on implementation of digital tools in the health and medical fields, we chose to search within the biomedical literature in PubMed alone. Given the rapid change of technological advancements and our goal of understanding how technology is currently used to inform patient engagement efforts, we limited the search to articles published in the last 5 years (July 2013 to July 2018).
Exclusion criteria
Articles were reviewed and excluded at 2 levels using criteria developed by all authors. At the first level, we reviewed titles and abstracts and excluded articles if they were not original research (eg, review articles, commentaries, study protocols, etc.), did not describe a patient-facing digital health tool, or were not conducted in the United States. We defined patient-facing digital health tools (hereafter also referred to as “digital health tools” or “tools”) as technologies with which patients could directly interact in order to enter and access personal health data, obtain health or disease-specific information, or monitor a health behavior or achieve a health goal (eg, text messaging app with reminders to take blood pressure medications).37 At the second screening level, we reviewed the full text of articles and excluded articles that did not evaluate use by patient characteristics (eg, age, gender, race or ethnicity, health literacy, health status), were studies of patient portals (as there are existing reviews focused on portals and other digital health tools are becoming increasingly ubiquitous), or included pediatric populations (as these evaluated surrogates’ rather than patients’ characteristics). Using DistillerSR (Evidence Partners, Ottawa, Ontario, Canada), title and abstract screening were completed by 1 reviewer (C.T.), with 2 additional reviewers (S.S.N. and C.L.) completing a subset of screening to ensure agreement on the categorization. Two reviewers (S.S.N. and C.T.) completed full text screening, with a subset double-screened to ensure concordance among reviewers. Any discordance (<5% of articles) was discussed in person among S.S.N., C.T., and C.L. until agreement was reached.
Data extraction: Outcome and predictor variables
We extracted only use measures that were evaluated by patient characteristics. Use was measured differently across studies, and included reach, retention over time, frequency of engagement (eg, number of times app was opened), and duration of engagement (eg, viewing time per link on a website).
We extracted patient characteristics that were included in the evaluations of use. In other words, we were not interested in the general description of the sample by patient demographics like age and gender, but rather in whether the study reported on use stratified by patient characteristics. The full list of patient characteristics extracted from each study included age, gender, race, health status, education, digital literacy, income, health literacy or numeracy, and limited English proficiency. We chose these variables based on previous research2,3,15 and a consensus approach of all authors in determining factors likely to influence digital health use. For each digital health tool, we determined which patient characteristics were statistically significantly associated or not associated with use, as well as the direction of the association, if any.
Data extraction: Determination of patient-level variations in use
Owing to the tremendous variation in how patient characteristics were measured, they were categorized into relative subgroups that could be applied to all studies (eg, age was divided into “older” vs “younger” subgroups). We then extracted whether the article reported a statistically significant (P < .05) vs nonsignificant association between any patient characteristic and the use outcomes. If there was a statistically significant association reported, we identified which patient subgroup was favored. For example, if use of a smartphone app was higher among younger compared with older individuals, the smartphone app was determined to favor younger individuals. If there was no statistically significant association between a patient characteristic and a use measure, this was reported as nonsignificant.
Selection of studies to support more robust subgroup analysis
As not all included studies were designed with the primary objective of evaluating use by patient characteristics, we identified the subset of included studies with a greater likelihood of internal validity in the examination of patient subgroup relationships. We did this to determine if there was a similar or stronger relationship between patient characteristics and use for studies that were more likely to support such inference. More specifically, we adapted criteria from a validated measure of risk of bias38 to evaluate whether included studies (1) clearly included and reported characteristics of nonusers of the digital health solution, (2) included ≥50 participants in analyses of use, and (3) presented multivariable relationships to assess whether a characteristic was predictive of use while holding all other characteristics constant. If a study met at least 2 of these 3 criteria, it was selected for subgroup analysis. We then replicated the data extraction described previously on this subset of studies.
Analyses
We took extracted data and first calculated descriptive statistics to summarize study and patient characteristics. Next, we determined the number of studies in which use outcomes were associated with each patient characteristic (including the direction of the association), as well as the number in which they were not associated with each patient characteristic. We did this analysis for all included studies and repeated it for the subgroup of studies described previously.
RESULTS
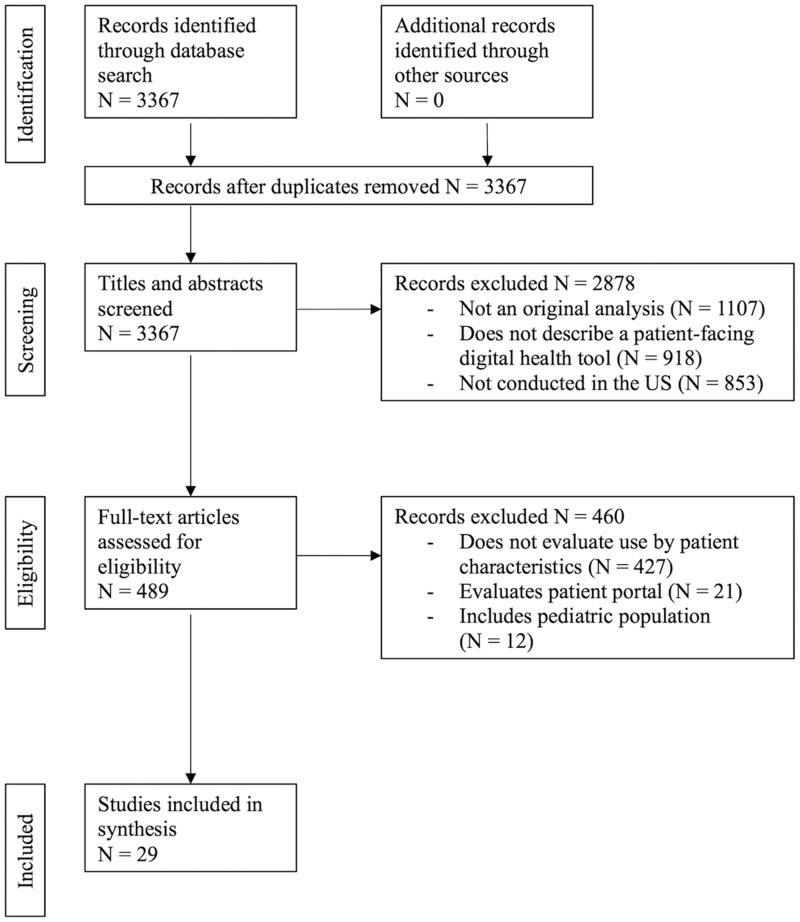
We identified 3367 studies using our search criteria; 29 studies met our final inclusion criteria (Figure 1, Supplementary Appendix A2).36
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram. US: United States.
Study and patient characteristics
Study and patient characteristics are summarized in Table 1, with additional details in Supplementary Appendix A3.
Table 1.
Study characteristics (N = 29)
| Patient characteristicsa | |
| Age | 21 (72.4) |
| Sex | 20 (69.0) |
| Race/ethnicity | 18 (62.1) |
| Health status or comorbidities | 15 (51.7) |
| Education | 9 (31.0) |
| Digital literacy | 5 (17.2) |
| Income | 5 (17.2) |
| Health literacy or numeracy | 4 (13.8) |
| Limited English proficiency | 1 (3.5) |
| Primary type of digital health toola | |
| Smartphone or tablet app | 11 (37.9) |
| Text messaging | 11 (37.9) |
| Interactive voice response | 4 (13.8) |
| Internet | 3 (10.4) |
| Social media | 2 (6.9) |
| Activity tracker | 1 (3.5) |
| Health area of focus | |
| Chronic disease management | 11 (37.9) |
| Tobacco or substance use | 7 (24.1) |
| Weight management | 5 (17.2) |
| Prevention/promotion | 4 (13.8) |
| Otherb | 2 (6.9) |
| Study settinga | |
| Academic medical center | 26 (89.7) |
| Community medical center | 6 (20.7) |
| Governmentc | 5 (17.2) |
| Tech company/organization | 5 (17.2) |
Values are n (%).
Twenty-four studies evaluated >1 patient characteristic. Three studies equally evaluated 2 types of digital health tool. Twelve studies included >1 setting.
Other includes hospital discharge planning and postoperative care.
Includes Veterans Health Administration, military bases and U.S. Army, and local departments of public health.
The most commonly included patient characteristics were age (21 studies), gender (20 studies), race (18 studies), and health status (15 studies). Definitions, measurement, and categorization of patient characteristics varied across studies (see Supplementary Appendix A4).
The digital health tools comprised 6 types of technologies: smartphone or tablet applications (11 studies), text messaging (11 studies), interactive voice response (IVR) (4 studies), Internet (3 studies), social media (2 studies), and activity-tracking devices (1 study). Eleven studies focused on chronic disease management. Twenty-six of the 29 studies were conducted at academic medical centers.
Studies selected for subgroup analysis
Supplementary Appendix A5 lists the studies that were selected for a more robust subgroup analysis and summarizes their appropriateness for subgroup analysis per each criterion and overall.
Thirteen of the 29 studies evaluating use met criteria for subgroup analysis. As an exemplar study of use that met criteria for appropriateness of subgroup analysis, Heminger et al39 evaluated use of Text2Quit, an interactive text messaging program aimed at smoking cessation, among 262 participants, including nonusers. They created a multivariable linear regression model that included all sociodemographic data to determine which patient characteristics were associated with use, which was defined as the sum of user-initiated survey responses, keyword usage, and web logins.
Association of patient characteristics with use of digital health tools
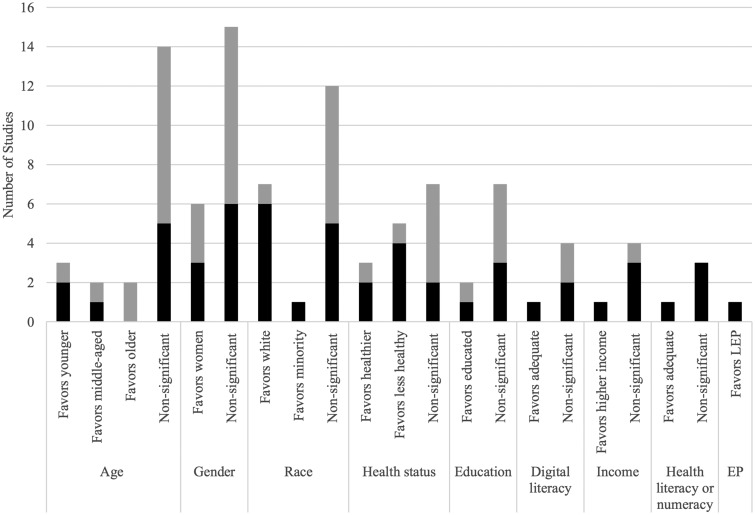
Figure 2 summarizes the association between use of digital health tools and patient characteristics, showing the overall number of studies per finding as well as the proportion of those that met criteria for a more robust analysis. Overall, among the studies evaluating use of digital health tools, most were not associated with age (n = 14 of 21), gender (n = 15 of 21), race (n = 12 of 20), health status (n = 7 of 15), education (n = 7 of 9), digital literacy (n = 4 of 5), income (n = 4 of 5), or health literacy or numeracy (n = 3 of 4). Only 1 study evaluated use by English proficiency and found that the digital health tool favored those with limited English proficiency (Spanish speakers spent more time per link on a website). However, this same study also found that white participants had more link views compared with racial or ethnic minority participants.40 The remaining studies of digital literacy, income, and health literacy or numeracy favored those with adequate digital or health literacy or numeracy and those with higher income.
Figure 2.
Patient characteristics associated with use, both among all included studies (entire bar) and within the subgroup of studies with more robust methodology (black). Studies that found no association (P ≥ .05) between use and patient characteristics were labeled “nonsignificant.” There were no tools that favored men or those with lower educational attainment, limited digital literacy, lower income, limited health literacy or numeracy, or English proficiency. Robust methodology was defined as meeting 2 of the following 3 criteria: (1) clearly included and reported characteristics of nonusers of the digital health solution, (2) included ≥50 participants in analyses, and (3) presented multivariable relationships to assess whether a characteristic was predictive of use holding all other characteristics constant. EP: English proficiency; LEP: limited English proficiency.
When considering only the 13 studies of use that met criteria for a more robust analysis, there appears to be a relationship between use and 2 characteristics: race and health status. Notably, half of digital health tools that examined use by race (n = 6 of 12) favored those who self-identify as white, while only 1 favored those who identify as a racial minority. Digital health tools that favored white populations compared with racial minorities included an Internet-based intervention for human immunodeficiency virus prevention among men who have sex with men,41 a text messaging program for assessing diabetes risk,42 a text messaging and IVR program for medication adherence among adults with diabetes,43 an Internet- and IVR-based program for weight management,44 a smartphone app for management of schizophrenia after hospital discharge,45 and an Internet program about nutrition.40 In these studies, use was measured as any adoption, retention over months, frequency of interactions with the digital health tool, or time spent using the digital health tool. Our subgroup analysis also found that half of the studies that examined use by health status (n = 4 of 8) favored those with poorer health status, while only 2 favored those with better health status. Digital health tools that favored those with poorer health status included a social media intervention for people living with human immunodeficiency virus,46 smartphone apps and an Internet-based program for mental health management,47,48 and a text messaging tool to improve postoperative care.49 Measures of use in these studies included any use of the tools and frequency of interactions with the tools.
DISCUSSION
In this review of recent evidence, we found only 29 studies evaluating use by patient characteristics. There was almost no uniformity across studies in how use was measured. The majority of studies included only 1-3 patient characteristics, primarily age and gender. For other factors, notably digital literacy and health literacy, the representation was extremely low, despite a growing body of work documenting barriers to digital health use by these factors.12,13,15,17,28,50 Moreover, the wide variability in measurement of patient characteristics represents the need for future work in digital health to not only include but also measure these variables in a standardized and validated manner.
For most patient characteristics, the majority of studies found no statistically significant association between the patient characteristic and use. For example, while older age is often assumed to be a barrier to engaging in digital health, our results suggest that for a range of digital health tools, age does not predict use. In fact, in some cases, use is higher among older adults. Nevertheless, among studies including large enough sample size of diverse subjects and nonusers, we did observe differences in digital health use by race and health status. These differences seemed to favor white participants and those with poorer health status more often. Literature evaluating patient portals has similarly found lower use among racial and ethnic minority populations20,32,51–53 but has not found an association between use and health status.30,54,55 Possible reasons for differences by race or ethnicity include cultural differences and patterns of use of digital health tools that may vary between social networks.23 For example, privacy concerns regarding electronic health records are expressed more frequently among African Americans compared with whites, and this may extend to other digital health tools.23 Additionally, people whose friends or social networks can help learn how to use digital health tools are more likely to use them.56,57 Our findings suggest that studies that prioritize inclusion of adequate sample sizes of diverse populations and of those with lived experiences with the health conditions of interest58 might be better positioned to provide greater generalizability about uptake of patient-facing digital health tools in real-world dissemination.59
Furthermore, despite the known high digital literacy, health literacy, numeracy, and language demands of many digital health tools, there were few studies examining use by these characteristics.60–63 It is imperative that these characteristics be included in evaluation studies of digital health tools in order to inform the real-world usefulness and likely uptake of such tools. Studies of usability of digital health tools, though few in number, have overwhelmingly found that adequate digital literacy, health literacy or numeracy, and English proficiency are associated with higher usability.31,64–66 This underscores the need not only to evaluate use by these patient characteristics but also to dedicate research to understanding usability by key patient characteristics, as usability predicts adherence to digital health tool use.23
Despite the large investment in an increasing number of digital health tools available to patients, few are using them, and this number has not grown appreciably over the past several years.67 Furthermore, while research has demonstrated the potential of these tools in widening existing health disparities,23 there has been little attention paid thus far to who users vs nonusers are. Our review underscores this and highlights that even among the studies that consider the relationship between patient characteristics and use, a wider range of patient characteristics and greater attention to robust methodology is needed. Some studies included in this review had robust methodology and did include a wide range of patient characteristics, demonstrating that it is possible to design and conduct such studies well. In fact, those studies that included digital literacy, health literacy, and English proficiency also tended to have more robust methodology. In order to understand why adoption of digital health tools remains so low, it is essential to consistently and deliberately assess their use. It is particularly necessary to do so among diverse populations that more accurately reflect the U.S. population, rather than among self-selecting, homogeneous, advantaged populations. Regardless of whether a digital health tool has been shown in a study to be effective in improving a behavioral or clinical outcome, these upstream factors of use and usability will ultimately determine whether it will be successful in improving health and ensuring health equity.23 As digital health tools continue to be rapidly developed and promoted, and patients are increasingly empowered to manage their personal health data,3,68 this becomes even more necessary.
This study has several limitations. Because of the wide variation in the definitions, measurements, and reporting of our outcome measures, we used terms capturing patient engagement in our search strategy for studies evaluating use—it is possible that we have not captured all relevant studies, particularly if they used different terminology for these measures. For the same reasons, we were unable to perform a meta-analysis of effect size or use a single validated tool to assess risk of bias or quality. However, we developed a set of proxy criteria to decide which of our included studies were methodologically appropriate for a subgroup analysis. We were similarly unable to assess publication bias; however, a large number of the included studies had negative (nonsignificant) findings. We limited our search to PubMed, given our specific focus on biomedical literature, and may therefore have missed studies available only in other databases. Finally, owing to the significant contribution of social factors (including patient characteristics highlighted in this study) to poor health outcomes in the United States compared with other high-income countries,69 we limited inclusion to U.S. studies, which could limit generalizability of results.
In conclusion, by specifically examining studies with objective measures of use, our results offer a substantially better understanding than provided by prior literature of patient adoption of digital health tools within different populations, including those vulnerable populations with high burden of disease and health inequity. Similar to studies of patient portal use, we found lower use of digital health tools among racial and ethnic minority populations. Evaluating use among diverse populations is critical in order to inform strategies to address low adoption of and adherence to patient-facing digital health tools. These efforts are important not only to increase patient uptake and sustained use of digital health tools, but also to identify inequities that may be perpetuated by growing availability of these tools.
FUNDING
This work was supported by The Commonwealth Fund (grant no. 20181504). SSN is funded in part by a National Research Service Award fellowship training grant (grant no.T32HP19025). CL and US are funded in part by the National Library of Medicine (grant no. R01LM013045); US is additionally funded in part by the National Cancer Institute (K24 CA212294-01). PA is funded in part by the Centers for Disease Control and Prevention (grant no.1 NB01OT009226-01-00) and the Health Resources and Services Administration (grant no. # 4 D33HP29250).
AUTHOR CONTRIBUTIONS
All authors contributed to the (1) conception or design of the work, (2) drafting or critically revising the work, (3) final approval of the version to be published, and (4) the accuracy and integrity of the work. SSN, CT, PA, and CL also contributed to the acquisition, analysis, and interpretation of the data.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Roy Cherian for his contributions to the literature search and development of inclusion and exclusion criteria.
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to declare.
REFERENCES
- 1.Pew Research Center. Mobile fact sheet. 2018. https://www.pewresearch.org/internet/fact-sheet/mobile/. Accessed December 1, 2018.
- 2. Kontos E, Blake KD, Chou WY, Prestin A.. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res 2014; 16 (7): e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lustria MLA, Smith SA, Hinnant CC.. Exploring digital divides: an examination of eHealth technology use in health information seeking, communication and personal health information management in the USA. Health Informatics J 2011; 17 (3): 224–43. [DOI] [PubMed] [Google Scholar]
- 4. Singh K, Meyer SR, Westfall JM.. Consumer-facing data, information, and tools: self-management of health in the digital age. Health Aff (Millwood) 2019; 38 (3): 352–8. [DOI] [PubMed] [Google Scholar]
- 5. Anglada-Martinez H, Riu-Viladoms G, Martin-Conde M, Rovira-Illamola M, Sotoca-Momblona JM, Codina-Jane C.. Does mHealth increase adherence to medication? Results of a systematic review. Int J Clin Pract 2015; 69 (1): 9–32. [DOI] [PubMed] [Google Scholar]
- 6. Rathbone AL, Prescott J.. The use of mobile apps and SMS messaging as physical and mental health interventions: systematic review. J Med Internet Res 2017; 19 (8): e295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Whitehead L, Seaton P.. The effectiveness of self-management mobile phone and tablet apps in long-term condition management: a systematic review. J Med Internet Res 2016; 18 (5): e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wu Y, Yao X, Vespasiani G, et al. Mobile app-based interventions to support diabetes self-management: a systematic review of randomized controlled trials to identify functions associated with glycemic efficacy. JMIR Mhealth Uhealth 2017; 5 (3): e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cohen AB, Safavi K. The oversell and undersell of digital health. Health Affairs Blog Bethesda,MD; February 27, 2019. https://www.healthaffairs.org/do/10.1377/hblog20190226.63748/full/. Accessed October 1, 2019.
- 10. Schickedanz A, Huang D, Lopez A, et al. Access, interest, and attitudes toward electronic communication for health care among patients in the medical safety net. J Gen Intern Med 2013; 28 (7): 914–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Health Information Technology: HHS Should Assess the Effectiveness of Its Efforts to Enhance Patient Access to and Use of Electronic Health Information Washington, DC: U.S. Government Accountability Office; 2017.
- 12. Broderick JD, T., Langhans E, Lemerise AJ, Lier S, Harris L. Designing health literate mobile apps. Discussion Paper. 2013. https://nam.edu/wp-content/uploads/2015/06/HealthLiterateApps.pdf. Accessed October 1, 2019.
- 13. Chakkalakal RJ, Kripalani S, Schlundt DG, Elasy TA, Osborn CY.. Disparities in using technology to access health information: race versus health literacy. Diabetes Care 2014; 37 (3): e53–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gordon NP, Hornbrook MC.. Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: a database and survey study of seniors in a large health plan. J Med Internet Res 2016; 18 (3): e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mackert M, Mabry-Flynn A, Champlin S, Donovan EE, Pounders K.. Health literacy and health information technology adoption: the potential for a new digital divide. J Med Internet Res 2016; 18 (10): e264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ray R, Sewell AA, Gilbert KL, Roberts JD.. Missed opportunity? Leveraging mobile technology to reduce racial health disparities . J Health Polit Policy Law 2017; 42 (5): 901–24. [DOI] [PubMed] [Google Scholar]
- 17. Sarkar U, Karter AJ, Liu JY.. The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system-results from the diabetes study of northern California (DISTANCE). J Health Commun 2010; 15 (Suppl 2): 183–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhang Y, Lauche R, Sibbritt D, Olaniran B, Cook R, Adams J.. Comparison of health information technology use between American Adults with and without chronic health conditions: findings from The National Health Interview Survey 2012. J Med Internet Res 2017; 19 (10): e335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Grossman LV, Masterson Creber RM, Benda NC, Wright D, Vawdrey DK, Ancker JS.. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inform Assoc 2019; 26 (8–9): 855–70. doi: 10.1093/jamia/ocz023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ancker JS, Hafeez B, Kaushal R.. Socioeconomic disparities in adoption of personal health records over time. Am J Manag Care 2016; 22 (8): 539–40. [PMC free article] [PubMed] [Google Scholar]
- 21. Anthony DL, Campos-Castillo C, Lim PS.. Who isn’t using patient portals and why? Evidence and implications from a national sample of US adults. Health Aff (Millwood) 2018; 37 (12): 1948–54. [DOI] [PubMed] [Google Scholar]
- 22. Peacock S, Reddy A, Leveille SG, et al. Patient portals and personal health information online: perception, access, and use by US adults. J Am Med Inform Assoc 2017; 24 (e1): e173–e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Veinot TC, Mitchell H, Ancker JS.. Good intentions are not enough: how informatics interventions can worsen inequality. J Am Med Inform Assoc 2018; 25 (8): 1080–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Antonio MG, Petrovskaya O, Lau F.. Is research on patient portals attuned to health equity? A scoping review. J Am Med Inform Assoc 2019; 26 (8–9): 871–83. doi: 10.1093/jamia/ocz054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Irizarry T, DeVito Dabbs A, Curran CR.. Patient portals and patient engagement: a state of the science review. J Med Internet Res 2015; 17 (6): e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wildenbos GA, Peute L, Jaspers M.. Facilitators and barriers of electronic health record patient portal adoption by older adults: a literature study. Stud Health Technol Inform 2017; 235: 308–12. [PubMed] [Google Scholar]
- 27. Fraccaro P, Vigo M, Balatsoukas P, Buchan IE, Peek N, van der Veer SN.. Patient portal adoption rates: a systematic literature review and meta-analysis. Stud Health Technol Inform 2017; 245: 79–83. [PubMed] [Google Scholar]
- 28. Coughlin SS, Stewart JL, Young L, Heboyan V, De Leo G.. Health literacy and patient web portals. Int J Med Inform 2018; 113: 43–8. [DOI] [PubMed] [Google Scholar]
- 29. Lyles CR, Nelson EC, Frampton S, Dykes PC, Cemballi AG, Sarkar U.. Using electronic health record portals to improve patient engagement: research priorities and best practices. Ann Intern Med 2019; 17 (6): e148. doi:10.7326/M19-0876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Turvey C, Klein D, Fix G, et al. Blue Button use by patients to access and share health record information using the Department of Veterans Affairs’ online patient portal. J Am Med Inform Assoc 2014; 21 (4): 657–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Taha J, Sharit J, Czaja SJ.. The impact of numeracy ability and technology skills on older adults’ performance of health management tasks using a patient portal. J Appl Gerontol 2014; 33 (4): 416–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Graetz I, Gordon N, Fung V, Hamity C, Reed ME.. The digital divide and patient portals: internet access explained differences in patient portal use for secure messaging by age, race, and income. Med Care 2016; 54 (8): 772–9. [DOI] [PubMed] [Google Scholar]
- 33. Price-Haywood EG, Harden-Barrios J, Ulep R, Luo Q.. eHealth literacy: patient engagement in identifying strategies to encourage use of patient portals among older adults. Popul Health Manag 2017; 20 (6): 486–94. [DOI] [PubMed] [Google Scholar]
- 34. Hung M, Conrad J, Hon SD, Cheng C, Franklin JD, Tang P.. Uncovering patterns of technology use in consumer health informatics. Wires Comput Stat 2013; 5 (6): 432–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yen PY, Walker DM, Smith JMG, Zhou MP, Menser TL, McAlearney AS.. Usability evaluation of a commercial inpatient portal. Int J Med Inform 2018; 110: 10–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Moher D, Liberati A, Tetzlaff J, Altman DG, Group atP. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA StatementThe PRISMA statement. Ann Intern Med 2009; 151 (4): 264–9. [DOI] [PubMed] [Google Scholar]
- 37.Food and Drug Administration. Digital health. 2020. https://www.fda.gov/medical-devices/digital-health. Accessed December 9, 2019.
- 38. Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355: i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Heminger CL, Boal AL, Zumer M, Abroms LC.. Text2Quit: an analysis of participant engagement in the mobile smoking cessation program. Am J Drug Alcohol Abuse 2016; 42 (4): 450–8. [DOI] [PubMed] [Google Scholar]
- 40. Brusk JJ, Bensley RJ.. A comparison of mobile and fixed device access on user engagement associated with women, infants, and children (WIC) online nutrition education. JMIR Res Protoc 2016; 5 (4): e216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Khosropour CM, Johnson BA, Ricca AV, Sullivan PS.. Enhancing retention of an internet-based cohort study of men who have sex with men (MSM) via text messaging: randomized controlled trial. J Med Internet Res 2013; 15 (8): e194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Buis LR, Hirzel L, Turske SA, Des Jardins TR, Yarandi H, Bondurant P.. Use of a text message program to raise type 2 diabetes risk awareness and promote health behavior change (Part I): assessment of participant reach and adoption. J Med Internet Res 2013; 15 (12): e281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nelson LA, Mulvaney SA, Gebretsadik T, Ho YX, Johnson KB, Osborn CY.. Disparities in the use of a mHealth medication adherence promotion intervention for low-income adults with type 2 diabetes. J Am Med Inform Assoc 2016; 23 (1): 12–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wolin KY, Steinberg DM, Lane IB, et al. Engagement with eHealth self-monitoring in a primary care-based weight management intervention. PLoS One 2015; 10 (10): e0140455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ben-Zeev D, Scherer EA, Gottlieb JD, et al. mHealth for schizophrenia: patient engagement with a mobile phone intervention following hospital discharge. JMIR Ment Health 2016; 3 (3): e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Flickinger TE, DeBolt C, Wispelwey E, et al. Content analysis and user characteristics of a smartphone-based online support group for people living with HIV. Telemed J E Health 2016; 22 (9): 746–54. [DOI] [PubMed] [Google Scholar]
- 47. Frisbee KL. Variations in the use of mHealth Tools: The VA mobile health study. JMIR Mhealth Uhealth 2016; 4 (3): e89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Toscos T, Carpenter M, Drouin M, Roebuck A, Kerrigan C, Mirro M.. College students’ experiences with, and willingness to use, different types of telemental health resources: do gender, depression/anxiety, or stress levels matter? Telemed J E Health 2018. Apr 16; doi: 10.1089/tmj.2017.0243. [DOI] [PubMed] [Google Scholar]
- 49. Sosa A, Heineman N, Thomas K, et al. Improving patient health engagement with mobile texting: a pilot study in the head and neck postoperative setting. Head Neck 2017; 39 (5): 988–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. O’Connor S, Hanlon P, O’Donnell CA, Garcia S, Glanville J, Mair FS.. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: a systematic review of qualitative studies. BMC Med Inform Decis Mak 2016; 16 (1): 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gerber DE, Laccetti AL, Chen B, et al. Predictors and intensity of online access to electronic medical records among patients with cancer. J Oncol Pract 2014; 10 (5): e307–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Graetz I, Huang J, Brand RJ, Hsu J, Yamin CK, Reed ME.. Bridging the digital divide: mobile access to personal health records among patients with diabetes. Am J Manag Care 2018; 24 (1): 43–8. [PMC free article] [PubMed] [Google Scholar]
- 53. Shimada SL, Allison JJ, Rosen AK, Feng H, Houston TK.. Sustained use of patient portal features and improvements in diabetes physiological measures. J Med Internet Res 2016; 18 (7): e179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Griffin A, Skinner A, Thornhill J, Weinberger M.. Patient portals: who uses them? What features do they use? And do they reduce hospital readmissions? Appl Clin Inform 2016; 7 (2): 489–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wallace LS, Angier H, Huguet N, et al. Patterns of electronic portal use among vulnerable patients in a nationwide practice-based research network: from the OCHIN Practice-based Research Network (PBRN). J Am Board Fam Med 2016; 29 (5): 592–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Jensen JD, King AJ, Davis LA, Guntzviller LM.. Utilization of internet technology by low-income adults: the role of health literacy, health numeracy, and computer assistance. J Aging Health 2010; 22 (6): 804–26. [DOI] [PubMed] [Google Scholar]
- 57. Rogers EM. Diffusion of Innovations. New York, NY: Free Press, 1962. [Google Scholar]
- 58. Anthony DL, Campos-Castillo C.. Patient portals and disparities: the authors reply. Health Aff (Millwood) 2019; 38 (3): 510. [DOI] [PubMed] [Google Scholar]
- 59. Toscos T, Drouin M, Pater J, Flanagan M, Pfafman R, Mirro MJ.. Selection biases in technology-based intervention research: patients’ technology use relates to both demographic and health-related inequities. J Am Med Inform Assoc 2019; 26 (8–9): 835–9. doi: 10.1093/jamia/ocz058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Berland GE, Morales LS, Algazy JI, et al. Health information on the Internet: accessibility, quality, and readability in English and Spanish. JAMA 2001; 285 (20): 2612–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Colorafi K, Greenes RA, Kates M.. Preferences of older adults and their families for Meaningful Use clinical summaries. Mhealth 2018; 4: 8–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Irizarry TS, Nilsen ML, Czaja S, Beach S, DeVito Dabbs A.. Patient portals as a tool for health care engagement: a mixed-method study of older adults with varying levels of health literacy and prior patient portal use. J Med Internet Res 2017; 19 (3): e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mishuris RG, Stewart M, Fix GM, et al. Barriers to patient portal access among veterans receiving home-based primary care: a qualitative study. Health Expect 2015; 18 (6): 2296–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Tieu L, Schillinger D, Sarkar U, et al. Online patient websites for electronic health record access among vulnerable populations: portals to nowhere? J Am Med Inform Assoc 2017; 24 (e1): e47–e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Crosier BS, Brian RM, Ben-Zeev D.. Using Facebook to reach people who experience auditory hallucinations. J Med Internet Res 2016; 18 (6): e160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Bravo C, O’Donoghue C, Kaplan C, Luce J, Ozanne E.. Can mHealth improve risk assessment in underserved populations? Acceptability of a breast health questionnaire app in ethnically diverse, older, low-income women. J Health Dispar Res Pract 2014; 7 (4). [PMC free article] [PubMed] [Google Scholar]
- 67.Rock Health. Digital Health Consumer Adoption Report 2019. https://rockhealth.com/reports/digital-health-consumer-adoption-report-2019/. Accessed December 9, 2019.
- 68. Kreps GL, Neuhauser L.. New directions in eHealth communication: opportunities and challenges. Patient Educ Couns 2010; 78 (3): 329–36. [DOI] [PubMed] [Google Scholar]
- 69.National Research Council, Institute of Medicine; Woolf SH, Aron L, eds. U.S. Health in International Perspective: Shorter Lives, Poorer Health. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.