Abstract
Out-of-office blood pressure measurement is an essential part of diagnosing and managing hypertension. In the era of advanced digital health information technology, the approach to achieving this is shifting from traditional methods (ambulatory and home blood pressure monitoring) to wearable devices and technology. Wearable blood pressure monitors allow frequent blood pressure measurements (ideally continuous beat-by-beat monitoring of blood pressure) with minimal stress on the patient. It is expected that wearable devices will dramatically change the quality of detection and management of hypertension by increasing the number of measurements in different situations, allowing accurate detection of phenotypes that have a negative impact on cardiovascular prognosis, such as masked hypertension and abnormal blood pressure variability. Frequent blood pressure measurements and the addition of new features such as monitoring of environmental conditions allows interpretation of blood pressure data in the context of daily stressors and different situations. This new digital approach to hypertension contributes to anticipation medicine, which refers to strategies designed to identify increasing risk and predict the onset of cardiovascular events based on a series of data collected over time, allowing proactive interventions to reduce risk. To achieve this, further research and validation is required to develop wearable blood pressure monitoring devices that provide the same accuracy as current approaches and can effectively contribute to personalized medicine.
Keywords: blood pressure, hypertension, phenotype, prognosis, wearable electronic devices
Out-of-office blood pressure (BP) determined using ambulatory BP monitoring (ABPM) and/or home BP monitoring (HBPM) is recommended for the diagnosis of hypertension in major international guidelines.1–11 Home and/or ambulatory BP readings have been shown to provide better prognostic information about target organ damage and cardiovascular risk than measurement of office BP.12–23 However, current approaches to ABPM and HBPM also have a number of well-known limitations, including patient comfort, sleep disturbance, availability, and cost.24–26
Newer information and communication technology (ICT)-based strategies provide options and solutions for self-monitoring of BP.27,28 These are designed to make it easier for patients to continuously monitor BP in a way that maximizes adherence. This approach has the potential to facilitate what has been defined as perfect 24-hour BP control: average 24-hour BP <130/80 mm Hg; normal circadian BP rhythm (including adequate dipping of nocturnal BP); and adequate BP variability (BPV).29 However, the vast majority are unregulated and unvalidated.30 There is therefore a need for more scientifically based and validated approaches to wearable BP technology to allow continuous monitoring of BP in an ambulatory setting. The optimal approach would be a wearable device that allows noninvasive cuff-less, beat-by-beat BP monitoring, with simultaneous determination of environmental conditions.31
The ultimate goal is that new information and communication technologies contribute to personalized solutions for hypertension management based on anticipation medicine with the goal of reducing cardiovascular risk (Figure 1).32 In addition, the availability of big data collected by wearable BP monitoring could facilitate time-series analyses and be used to inform artificial intelligence strategies to predict hypertension.33,34
Figure 1.
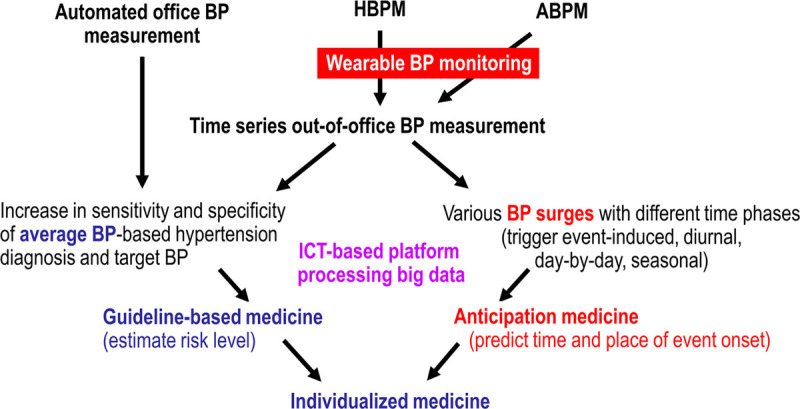
Time-series out-of-office blood-pressure (BP)-based anticipation management of hypertension.32 ABPM indicates ambulatory blood pressure monitoring; HBPM, home blood pressure monitoring; and ICT, information and communication technology. Reprinted from Kario et al32 with permission. Copyright© 2020, Wiley.
Wearable BP Monitoring Concept and Cardiovascular Risk
A wide variety of factors can influence BP at any time, highlighting the value of a wearable option that allows determination of associations between BP readings and potential triggers, such as environmental factors, physical activity, and psychological stress.33
Resonance Hypothesis of BPV, 24-Hour BP Profiles, and BP Surge
The synergistic resonance theory proposes that each form of BPV (beat-by-beat, diurnal, day-by-day, seasonal and yearly) has the potential to create dynamic surges in BP, which could coincide with peak BP and different external triggers (eg, temperature, mental stress, sleep apnea, exercise) to precipitate cardiovascular events (Figure 2), especially in patients with arterial stiffness who are less able to absorb BP surges in the peripheral arteries.29,35,36 Therefore, there are a variety of factors and triggers that contribute to the 24-hour BP profile and BP surges for each individual (Figure 3). There is also wide interindividual variation in daytime BP values, and in the response to stressful situations.37 In addition, actisensitivity (the slope of the regression line of ambulatory BP against the log of physical activity) in patients with hypertension varies by season, with higher trigger-specific surge in BP during exercise in winter compared with summer.33
Figure 2.
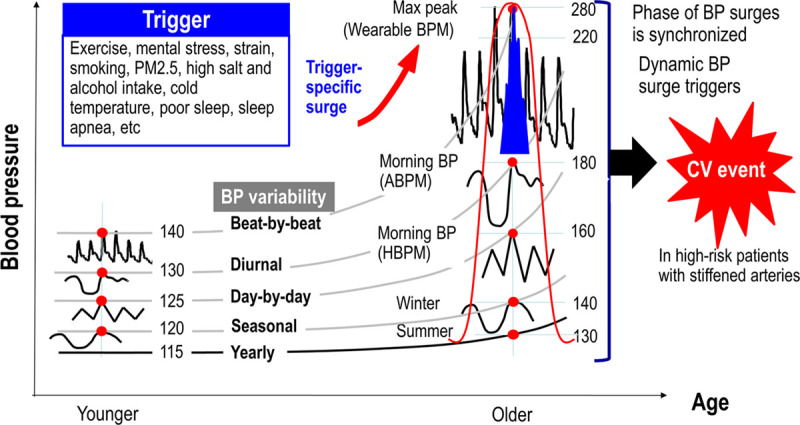
The resonance hypothesis of blood pressure (BP) variability. ABPM indicates ambulatory blood pressure monitoring; BPM, blood pressure monitoring; CV, cardiovascular; HBPM, home blood pressure monitoring; and PM2.5, particulate matter 2.5 micrometres or less in diameter. Reprinted from Kario31 with permission. Copyright ©2020, WKH.
Figure 3.
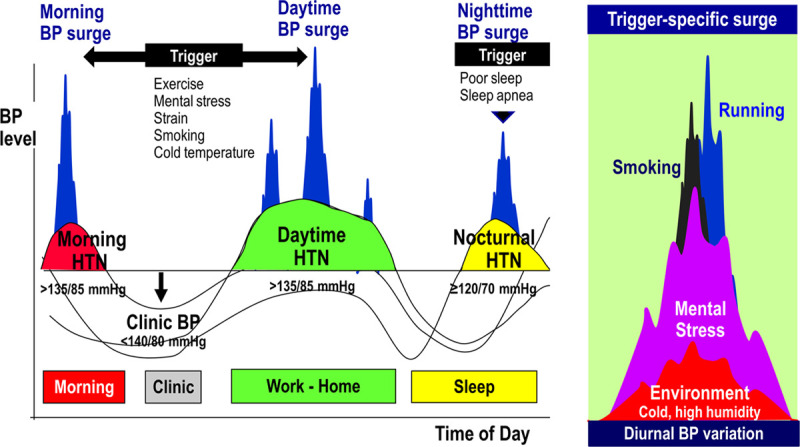
Synergistically accumulated trigger-specific blood pressure (BP) surges and diurnal variation. HTN indicates hypertension.
In general, BP tends to be higher in the morning and lower at night. Variations from the normal physiological pattern include excessive morning BP surge, no decrease in BP at night (nondipper pattern), and increased nighttime BP (nocturnal hypertension, or riser pattern). Nocturnal hypertension is particularly associated with a salt-sensitive hypertension phenotype, as often seen in individuals of Asian ethnicity,38 and may be associated with sleep apnea.31
Excessive morning BP surge has been associated with increased stroke risk, cerebral hemorrhage, and a variety of forms of target organ damage.39–45 In addition, both nocturnal hypertension and a nondipper/riser pattern identified on ABPM have been shown to increase the risk of target organ damage and cardiovascular events.46–55 This means that accurate detection of perturbations in the BP profile and any associated triggers is important to reduce cardiovascular risk and the occurrence of adverse cardiovascular events. Wearable devices with beat-by-beat monitoring and sensors to determine environmental conditions are ideally suited to fulfill this role as part of the overall management of patients with hypertension.
Small Wearable Devices
App-based measurements are limited by reliability,56 and a large proportion of devices marketed for home BP monitoring are unvalidated.57 Nevertheless, there is a growing body of evidence to support wearable medical devices from experienced manufacturers. These use a variety of different approaches to determine BP, and some have recently been validated using currently accepted clinical standards.
Oscillometric Measurement at the Wrist
The oscillometric technique is widely used in current office, home, and ambulatory BP measurement devices. New wrist-cuff devices use the same technique but are expected to cause less discomfort and muscle compression than traditional upper arm cuffs. Two recent studies58,59 have validated watch-type wrist devices for BP measurement against the American National Standards Institute, Inc/Association for the Advancement of Medical Instrumentation/International Organization for Standardization (ANSI/American Association for the Advancement of Medical Instrumentation/ISO) 81060-2:2013 guidelines.60 The data showed that the HEM-6410T-ZM and HEM-6410T-ZL devices (Omron Healthcare, Kyoto, Japan) fulfilled the validation criteria when used in the sitting position with the wrist at heart level.59 Mean differences between reference BP values and HEM-6410T-ZM readings were −0.9±7.6/–1.1±6.1 mm Hg for SBP/DBP for criterion 1, and −0.9±6.8/–1.1±5.5 mm Hg for criterion 2; corresponding differences for HEM-6410T-ZL readings were 2.4±7.3/0.7±7.0 and 2.4±6.5/0.7±6.5 mm Hg.59 These seem to be the first wrist-type wearable devices validated against standardized criteria. Another Omron device (HEM9600T) also fulfilled the ANSI/American Association for the Advancement of Medical Instrumentation/ISO81060-2:2013 criteria when patients were in the sitting position, whereas accuracy in the supine position was only achieved when the palm was in the downward position.58
In addition to recognized standards, it is also of interest how wearable watch-type BP monitors compare with conventional out-of-office techniques (ABPM and HBPM). In outpatients, wearable watch-type BP monitor (HEM6410T) and ABPM device were simultaneously worn on the same arm. Mean difference in SBP values (average of 2 readings) between the wearable HEM6410T devices and ABPM were 0.8±12.8 mm Hg in the office (P=0.564) and 3.2±17.0 mm Hg outside the office (P<0.001).61 The proportion of differences that were within ±10 mm Hg was 58.7% in the office and 47.2% outside the office. In a mixed-effects model analysis, the temporal trend in the difference between the out-of-office BP values measured by the 2 devices was not statistically significant, indicating that there was an acceptable difference between the devices with respect to BP measurements.61 An example of BP readings taken using the wearable device from the above study and ABPM is shown in Figure 4. In another study, 24-hour BP measurements with the Model T2 wearable cuff-less device (TMART Technologies Ltd) in volunteers were within acceptable limits compared with ABPM, but BP measures showed systematic differences from HBPM determined over 7 days.62 Study participants did find the wearable device easy to wear and use.62
Figure 4.
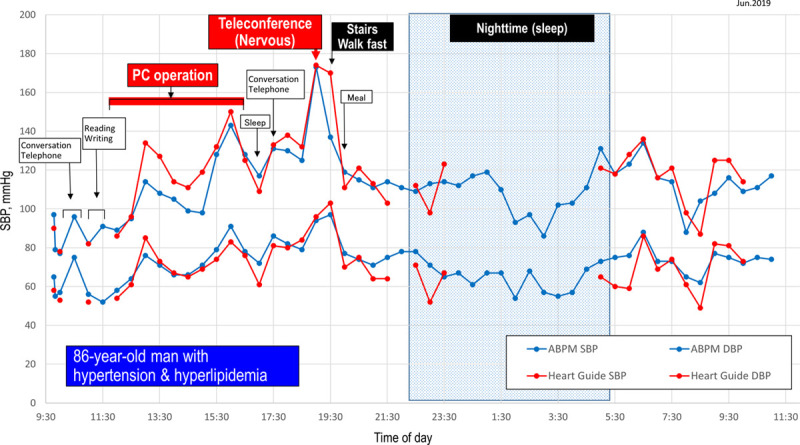
Comparison showing simultaneous monitoring with a wearable device (HeartGuide; Omron Healthcare Co, Ltd) and ambulatory blood pressure monitoring (ABPM). DBP indicates diastolic blood pressure; PC, personal computer; and SBP, systolic blood pressure.
The devices above were validated against current standards developed for traditional BP monitoring devices and were shown to perform adequately. However, there is not yet any standardized, specific approach to validating small wearable devices. It may be that the standards need to be modified and refined to provide the best data on wearable device performance, and this is an important area for future research in this developing field.
Applanation Tonometry Method
This approach uses arterial wall applanation to measure the waveform of arterial BP. The radial artery at the wrist is ideally suited for applanation because it is shallow beneath the skin and fixed on a radial bone.31 However, the sensor needs to be well secured so that it is in a stable position over the artery and does not move during measurements. Devices using this technology have been validated against ESH and American Association for the Advancement of Medical Instrumentation criteria under static conditions,63 but accuracy is lower under ambulatory conditions.64 Another limitation is that the positional relationship between the heart and the measurement site varies, which introduces an influence of hydrostatic pressure alternations on BP.31
Devices using the applanation tonometry method have been used to monitor nighttime BP and detect BP surges that are common in patients with sleep apnea.31 An algorithm to detect pathological surge BP (BP surge in seconds) was developed based on beat-by-beat BP readings obtained over one night.65 Figure 5 highlights successful use of this approach in a patient with diabetes mellitus, resistant hypertension, and sleep apnea, and suppression during treatment with a SGLT2 (sodium-glucose co-transporter 2) inhibitor. This case highlights a BPV profile detected using a new BP monitoring and BP surge detection algorithm.
Figure 5.
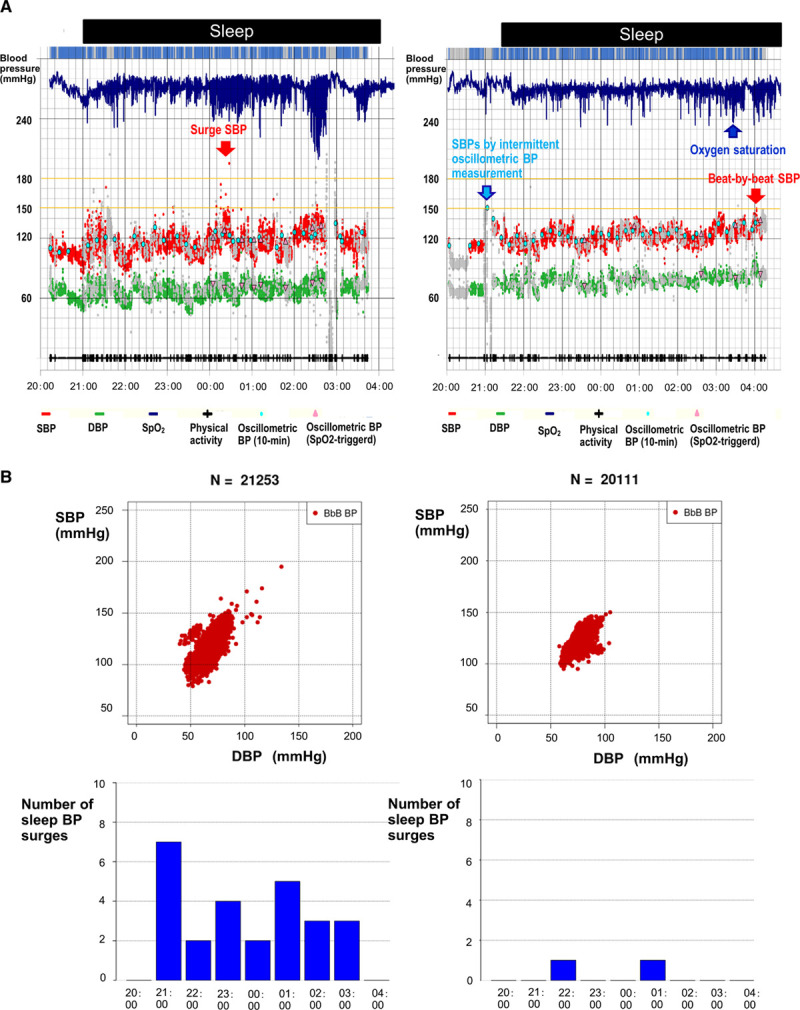
Pathological surge blood pressure (BP) detected by a new beat-by beat 'surge' BP monitoring and BP surge detection algorithm. A, Data showing suppression of BP surges trigged by apneic episodes during sleep in a 77-y-old woman with hypertension, diabetes mellitus, and obstructive sleep apnea. Sleep surge systolic (red dots) and diastolic (green dots) BP values were detected by the newly developed nocturnal beat-by-beat continuous BP monitoring (tonometry method) at baseline (treatment regimen: amlodipine 5 mg/d, aspirin 100 mg/d, and sitagliptin 25 mg/d) (left) and after 4 wk of add-on therapy with dapagliflozin 10 mg/d (right). B, The upper panels show the distribution of systolic BP (SBP) and diastolic BP (DBP) before (left) and after (right) 4 wk of dapagliflozin. The lower panels show nighttime BP surges detected by a newly developed surge autodetection algorithm.
Photoplethysmography
In this approach, a photoplethysmography sensor is worn over the finger and secured with a pressure cuff.66 Oscillations of pressure in the cuff are representative of the arterial pressure wave, allowing determination of SBP and DBP.67 Use of photoplethysmography has been shown to be suitable for use in wearable BP monitoring devices.68,69 Disadvantages of this approach include cuff pressure on the finger and sensitivity to movement.66
A device using a single photoplethysmography sensor has been validated against the Institute of Electrical and Electronics Engineers standard 1708-2014 under static and dynamic conditions and was able to document rapid changes in BP.70 In addition, sleep quality was better when the wearable device was used compared with cuff-based BP monitoring.70 Another device worn on the wrist that includes 2 photoplethysmography sensors was shown to have good accuracy compared with oscillometric-based devices but did not quite meet the American Association for the Advancement of Medical Instrumentation standard for nonautomated sphygmomanometers.71 A systematic review and meta-analysis concluded that although many studies have investigated the use of multisite photoplethysmography-based technologies for BP monitoring, there was not yet enough information to make a powerful and statistically significant contribution toward the reliable noninvasive measurement of arterial blood pressure.72
Pulse Transit Time
Pulse transit time is the interval of the pulse wave propagation between 2 arterial sites, is inversely proportional to BP, and has been shown to provide a good estimate of BP.73–77 Limitations of this approach include the ability to accurately estimate both SBP and DBP, and the influence of changes in arterial elasticity with age.78 Pulse transit time-based approaches to continuous BP monitoring often use an ECG provide and a finger photoplethysmography sensor, and can also provide information on heart rate.77,79,80
A device consisting of a finger photoplethysmography and 3 ECG leads connected to a watch-like device has been validated against the European Society of Hypertension International Protocol revision 2010 for the validation of BP measuring devices in adults.81,82 This is promising, but the device still needs to be tested outside laboratory conditions to provide its ability to continuously and reliably record 24-hour BP under real-life conditions. A device where the ECG and photoplethysmography signal detection systems are incorporated into a single wearable patch seems to have potential for real-time BP monitoring and would be convenient for patients.83
Another approach to measuring pulse transit time used an array of 2×2 bioimpedance sensors placed on the wrist and eliminates the need for ECG.84 This allowed continuous and accurate measurement of BP in a way that was comfortable for patients.84 Use of a bioimpedance system for BP monitoring was also investigated in another study. A wrist device with 4 bioimpedance sensors on the wrist in a horizontal structure showed good detection ratios for pulse wave velocity, and the estimated BP showed low root-mean-squared-errors of 7.47±2.15 mm Hg (SBP) and 5.17±1.81 mm Hg (DBP) compared with standard measurements.85 This suggests that such an approach is feasible for wearable BP devices, with refinement to reduce the estimated BP errors with the latter device.
Other Approaches
Several other techniques for measuring BP with a wearable device have been evaluated. One is a finger-wearable monitor consisting of a 2-dimensional, 30-element, capacitive tactile sensor array to measure contact pressure with the finger, a pump-driven pneumatic bladder to press the tactile array and the finger steadily toward each other; and a cuff that houses the sensor array and bladder.86 Mean±SD difference compared with brachial dual-observer auscultation was 0.9±6.9 mm Hg for SBP and –3.2±7.0 mm Hg for DBP, which is consistent with international standard validation requirements.86 Another device that was shown to perform well compared with standard criteria was a low-cost piezoelectric-based system worn on the wrist (mean absolute error of 1.52±0.30 and 1.83±0.50 for SBP and DBP, respectively).87 Soft pressure sensors using wrinkled thin films worn on the wrist have the benefit of being able to deform without breaking during normal force and movement.88 These have been shown to determine BP with similar accuracy to validated devices and therefore have potential for beat-to-beat BP monitoring.88
Machine Learning
The fact that BP is influenced by a variety of factors has driven research into use of machine learning technology based on big data to extract the optimal features required to monitor BP and develop algorithms that produce values that meet system validation requirements.89 The central concept is to examine time and frequency domains from physiological signals to extract BP-related features and then use machine learning to eliminate unwanted features and calculate BP from optimal data. The most common machine learning algorithms evaluated in the development of BP models to date include neural networks, linear regression, support vector machine, random forest, and deep learning. However, although these are showing promise, techniques need to be refined to improve and optimize accuracy before machine learning approaches are sufficiently precise to allow widespread clinical usage.89
Potential for Digital Platforms and Artificial Intelligence in Anticipation Medicine
The latest guidelines from the American College of Cardiology/American Heart Association highlight the important future role for health information technology solutions in hypertension diagnosis and management.7 In addition to wearable technologies, telemedicine solutions are also increasingly being used to manage hypertension. These have been shown to significantly reduce both SBP and DBP compared with usual care,90,91 but further research is needed to better define and standardize the optimal components and determine how interactive digital interventions might be widely incorporated into clinical practice across a range of healthcare settings.
Utilizing individual time-series data combined with data on environmental factors is increasingly being seen as important for taking a holistic approach to BP measurement (Figure 6).32 Cold temperatures may increase BP via sympathetic nervous system activation, vasoconstriction, and decreased endothelial function,92–94 and cold temperatures have consistently been shown to be associated with higher BP and greater BPV,95–101 and increased risk of cardiovascular disease events.96,102 A new semiautomatic HBPM device that automatically measures BP at fixed intervals during sleep has successfully been used to monitor nighttime BP in clinical trials103–108 and an updated version of this device that includes a temperature sensor has also been used in clinical trials of patients with uncontrolled nocturnal hypertension.109,110 However, this approach is resource intensive, meaning that initial usage may be limited and there would be challenges to overcome before widespread usage became possible.
Figure 6.
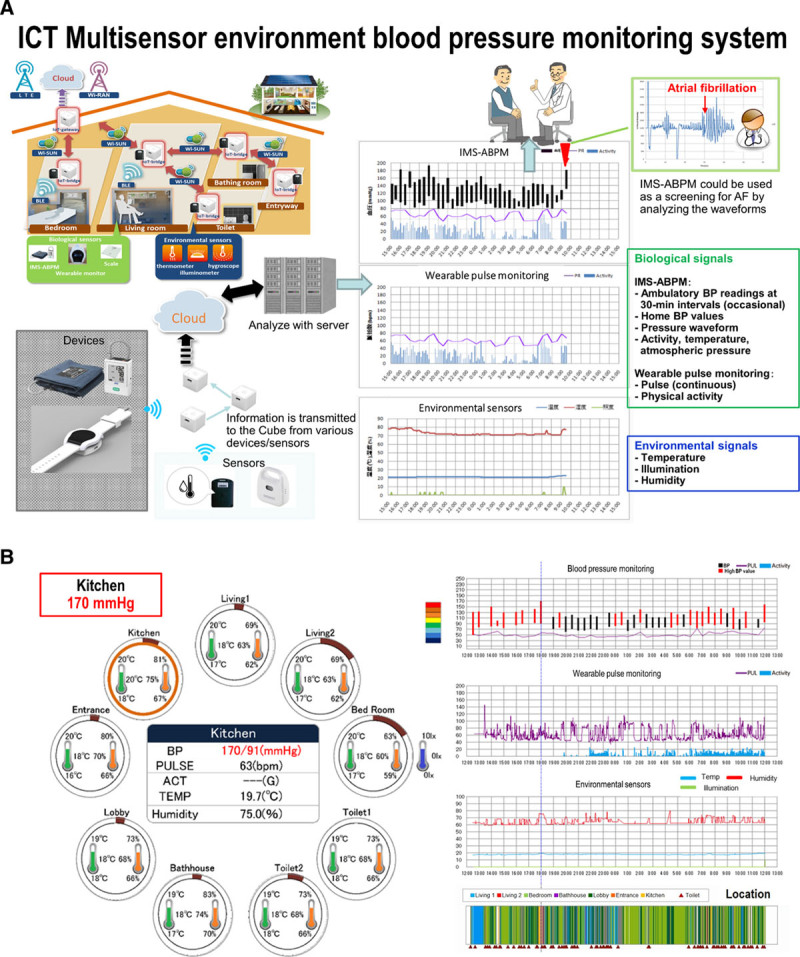
Information/communication technology (ICT) multisensor environment blood pressure monitoring system. A, A novel approach to individual management for hypertension. Biologic and environmental signals corresponding to an individual’s living conditions at home were simultaneously collected from multiple devices and sensors by an IoT (Internet of Things) gateway, and bridges based on the hybrid Wi-SUN/Wi-Fi transmission system. B, Time-trend reporting system of ambulatory blood pressure and environmental conditions along with an individual’s high-risk places and times. ABPM indicates ambulatory blood pressure monitoring; AF, atrial fibrillation; BLE, Bluetooth; BP, blood pressure; IMS, ICT-based multi-sensor; and PR, pulse rate. Reprinted from Kario et al32 with permission. Copyright ©2020. Wiley. http://www.jichi.ac.jp/usr/card/research/index_en.html
One example of putting remote management of hypertension into practice occurred during the aftermath of the Great East Japan Earthquake, which occurred on March 11, 2011. The Disaster Cardiovascular Prevention Network used a web-based HBPM system in a town devastated by the earthquake and subsequent tsunami.111 This enabled strict control of home BP to be achieved and seasonal variations in BP to be minimized over the months and years after the disaster and suggests that such an approach could be successfully applied for routine monitoring of BP in the wider community.
Anticipation medicine refers to approaches designed to identify increasing risk and predict the onset of cardiovascular events based on a series of data collected over time, allowing proactive interventions to reduce risk and eliminate events. Combining this with precision medicine, defined as customization of healthcare, with medical decisions, treatments and management tailored for each individual patient, offers the possibility of effectively managing hypertension to reduce cardiovascular risk.31 Effective utilization of digital platforms and solutions utilizing real-time data, such as that provided by wearable technologies, combined with artificial intelligence is another area with potential.31 Using data from 18 258 individuals, machine learning methods were able to develop a highly precise model to predict the development of hypertension in a general population.34 This could be used to identify individuals at risk of developing hypertension and allow early intervention with tools such as lifestyle modification to prevent future hypertension development. Another artificial intelligence-based prediction model using multi-input multi-output deep neural networks based on time-series BP data and related contextual information showed that this approach has the potential to predict both mean BP and BPV.112 Given that abnormal BPV is a known risk factor for CVD, the ability to predict BP over periods of 4 weeks using this model could have important clinical implications, although this remains to be determined.
While it is clear that wearable BP technologies have the potential to provide the types of data likely to be useful in developing cardiovascular risk reduction strategies, additional research is needed to determine whether more frequent and continuous monitoring using small wearable devices provides prognostic information that can be used to reduce cardiovascular event rates in clinical practice.
In conclusion, currently available data indicate that digital management of hypertension and wearable BP monitoring technology are the way of the future. These approaches make the aim of reducing, or even eliminating, the occurrence of cardiovascular events in patients with hypertension a realistic possibility. Using these approaches, it is possible to assess all types of BPV simultaneously, enabling a paradigm shift from BP management based on dots to seamless individualized anticipation medication for zero cardiovascular events. Smartphone apps are not yet useful in this setting, and none have currently been approved by the US FDA or European Commission.113 However, recent research shows that wearable devices produced by companies specializing in BP monitoring technology are validated and reliable,58,59,61,70,71,81,82 opening the way for their use in clinical practice. Wrist-worn wearable devices have also been shown to perform well against current out-of-office BP measurement approaches.61,62 Initial data suggest that wearable technology could also be useful for detecting arrhythmias, such as atrial fibrillation.114
The next important question is how best to incorporate the new technologies into clinical practice for both physicians and patients. Lower levels of technology literacy in some older patients may limit the usefulness of these approaches in an important subset of the population with hypertension, and this is something that needs to be considered as part of device development and implementation. Nevertheless, wearable BP monitoring technology is a promising and exciting field. Both current and future developments will ensure that wearable technologies become user-friendly, reliable, accurate, and flexible to provide real-time data to facilitate risk factor modification for the prevention of cardiovascular events.
Acknowledgments
Studies described in this paper was partly supported by Japan Agency for Medical Research and Development (AMED) under Grant Number JP17he1102002h0003; the Impulsing Paradigm Change through disruptive Technologies (IMPACT) program of the Cabinet Office, Government of Japan; and Omron Healthcare Co. We would like to thank IMPACT program collaborators, especially Dr Ryozo Nagai, Dr Hiroshi Harada, and Mrs Naoko Tomitani for their valuable contribution. Medical writing assistance was provided by Nicola Ryan, independent medical writer.
Sources of Funding
None.
Disclosures
K. Kario received independent principal investigator-initiated research grants from Omron Healthcare, Inc (Kyoto, Japan), and A&D, Inc (Tokyo, Japan).
References
- 1.Chiang CE, Wang TD, Ueng KC, Lin TH, Yeh HI, Chen CY, Wu YJ, Tsai WC, Chao TH, Chen CH, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc 2015781–47doi: 10.1016/j.jcma.2014.11.005 [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Health and Care Excellence Hypertension in adults: diagnosis and management. NICE guideline [NG136]Aug 28, 2019Available at: https://www.nice.org.uk/guidance/ng136/resources/hypertension-in-adults-diagnosis-and-management-pdf-66141722710213. Accessed March 23, 2020 [PubMed]
- 3.Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, Harris KC, Nakhla M, Cloutier L, Gelfer M, et al. ; Hypertension Canada Hypertension Canada’s 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol 201834506–525doi: 10.1016/j.cjca.2018.02.022 [DOI] [PubMed] [Google Scholar]
- 4.O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, et al. ; European Society of Hypertension Working Group on Blood Pressure Monitoring European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 2013311731–1768doi: 10.1097/HJH.0b013e328363e964 [DOI] [PubMed] [Google Scholar]
- 5.Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, et al. ; European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 2014321359–1366doi: 10.1097/HJH.0000000000000221 [DOI] [PubMed] [Google Scholar]
- 6.Sharman JE, Howes FS, Head GA, McGrath BP, Stowasser M, Schlaich M, Glasziou P, Nelson MR. Home blood pressure monitoring: Australian Expert Consensus Statement. J Hypertens 2015331721–1728doi: 10.1097/HJH.0000000000000673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018712199–2269doi: 10.1016/j.jacc.2017.11.00529146533 [Google Scholar]
- 8.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, et al. ; ESC Scientific Document Group 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018393021–3104doi: 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 9.Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res 2019421235–1481doi: 10.1038/s41440-019-0284-9 [DOI] [PubMed] [Google Scholar]
- 10.Park S, Buranakitjaroen P, Chen CH, Chia YC, Divinagracia R, Hoshide S, Shin J, Siddique S, Sison J, Soenarta AA, et al. ; HOPE Asia Network Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network. J Hum Hypertens 201832249–258doi: 10.1038/s41371-017-0025-y [DOI] [PubMed] [Google Scholar]
- 11.Kario K, Shin J, Chen CH, Buranakitjaroen P, Chia YC, Divinagracia R, Nailes J, Hoshide S, Siddique S, Sison J, et al. Expert panel consensus recommendations for ambulatory blood pressure monitoring in Asia: the HOPE Asia Network. J Clin Hypertens (Greenwich) 2019211250–1283doi: 10.1111/jch.13652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, Menard J, Mallion JM. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA 20042911342–1349doi: 10.1001/jama.291.11.1342 [DOI] [PubMed] [Google Scholar]
- 13.Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, Matsui Y, Nakamura A, Fukutomi M, Eguchi K, et al. ; J-HOP Study Group Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese General Practice Population: The Japan Morning Surge-Home Blood Pressure Study. Hypertension 20166854–61doi: 10.1161/HYPERTENSIONAHA.116.07201 [DOI] [PubMed] [Google Scholar]
- 14.Kario K, Saito I, Kushiro T, Teramukai S, Ishikawa Y, Mori Y, Kobayashi F, Shimada K. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational study. Hypertension 201464989–996doi: 10.1161/HYPERTENSIONAHA.114.04262 [DOI] [PubMed] [Google Scholar]
- 15.Kario K, Saito I, Kushiro T, Teramukai S, Tomono Y, Okuda Y, Shimada K. Morning home blood pressure is a strong predictor of coronary artery disease: the HONEST Study. J Am Coll Cardiol 2016671519–1527doi: 10.1016/j.jacc.2016.01.037 [DOI] [PubMed] [Google Scholar]
- 16.Niiranen TJ, Hänninen MR, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension 2010551346–1351doi: 10.1161/HYPERTENSIONAHA.109.149336 [DOI] [PubMed] [Google Scholar]
- 17.Hara A, Tanaka K, Ohkubo T, Kondo T, Kikuya M, Metoki H, Hashimoto T, Satoh M, Inoue R, Asayama K, et al. Ambulatory versus home versus clinic blood pressure: the association with subclinical cerebrovascular diseases: the Ohasama Study. Hypertension 20125922–28doi: 10.1161/HYPERTENSIONAHA.111.174938 [DOI] [PubMed] [Google Scholar]
- 18.Ohkubo T, Hozawa A, Nagai K, Kikuya M, Tsuji I, Ito S, Satoh H, Hisamichi S, Imai Y. Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens 200018847–854doi: 10.1097/00004872-200018070-00005 [DOI] [PubMed] [Google Scholar]
- 19.Staessen JA, Thijs L, Fagard R, O’Brien ET, Clement D, de Leeuw PW, Mancia G, Nachev C, Palatini P, Parati G, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA 1999282539–546doi: 10.1001/jama.282.6.539 [DOI] [PubMed] [Google Scholar]
- 20.Fuchs SC, Mello RG, Fuchs FC. Home blood pressure monitoring is better predictor of cardiovascular disease and target organ damage than office blood pressure: a systematic review and meta-analysis. Curr Cardiol Rep. 2013;15:413. doi: 10.1007/s11886-013-0413-z. doi: 10.1007/s11886-013-0413-z. [DOI] [PubMed] [Google Scholar]
- 21.Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens 201230449–456doi: 10.1097/HJH.0b013e32834e4aed [DOI] [PubMed] [Google Scholar]
- 22.Stergiou GS, Asayama K, Thijs L, Kollias A, Niiranen TJ, Hozawa A, Boggia J, Johansson JK, Ohkubo T, Tsuji I, et al. ; International Database on HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) Investigators Prognosis of white-coat and masked hypertension: International Database of HOme blood pressure in relation to Cardiovascular Outcome. Hypertension 201463675–682doi: 10.1161/HYPERTENSIONAHA.113.02741 [DOI] [PubMed] [Google Scholar]
- 23.Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 199816971–975doi: 10.1097/00004872-199816070-00010 [DOI] [PubMed] [Google Scholar]
- 24.Little P, Barnett J, Barnsley L, Marjoram J, Fitzgerald-Barron A, Mant D. Comparison of acceptability of and preferences for different methods of measuring blood pressure in primary care. BMJ 2002325258–259doi: 10.1136/bmj.325.7358.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ernst ME, Bergus GR. Noninvasive 24-hour ambulatory blood pressure monitoring: overview of technology and clinical applications. Pharmacotherapy 200222597–612doi: 10.1592/phco.22.8.597.33212 [DOI] [PubMed] [Google Scholar]
- 26.Hinderliter AL, Voora RA, Viera AJ. Implementing ABPM into clinical practice. Curr Hypertens Rep. 2018;20:5. doi: 10.1007/s11906-018-0805-y. doi: 10.1007/s11906-018-0805-y. [DOI] [PubMed] [Google Scholar]
- 27.Logan AG. Community hypertension programs in the age of mobile technology and social media. Am J Hypertens 2014271033–1035doi: 10.1093/ajh/hpu125 [DOI] [PubMed] [Google Scholar]
- 28.Postel-Vinay N, Bobrie G, Savard S, Persu A, Amar L, Azizi M, Parati G. Home blood pressure measurement and digital health: communication technologies create a new context. J Hypertens 2018362125–2131doi: 10.1097/HJH.0000000000001860 [DOI] [PubMed] [Google Scholar]
- 29.Kario K. Essential Manual on Perfect 24-hour Blood Pressure Management from Morning to Nocturnal Hypertension: Up-to-date for Anticipation Medicine. Japan: Wiley Publishing; 2018. [Google Scholar]
- 30.Kumar N, Khunger M, Gupta A, Garg N. A content analysis of smartphone-based applications for hypertension management. J Am Soc Hypertens 20159130–136doi: 10.1016/j.jash.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 31.Kario K. Evidence and perspectives on the 24-hour management of hypertension: hemodynamic biomarker-initiated ‘anticipation medicine’ for zero cardiovascular event. Prog Cardiovasc Dis 201659262–281doi: 10.1016/j.pcad.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 32.Kario K, Tomitani N, Kanegae H, Yasui N, Nagai R, Harada H. The further development of out-of-office BP monitoring: Japan’s ImPACT Program Project’s achievements, impact, and direction. J Clin Hypertens(Greenwich) 201921344–349doi: 10.1111/jch.13495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kario K, Tomitani N, Kanegae H, Yasui N, Nishizawa M, Fujiwara T, Shigezumi T, Nagai R, Harada H. Development of a new ICT-based multisensor blood pressure monitoring system for use in hemodynamic biomarker-initiated anticipation medicine for cardiovascular disease: the National IMPACT Program Project. Prog Cardiovasc Dis 201760435–449doi: 10.1016/j.pcad.2017.10.002 [DOI] [PubMed] [Google Scholar]
- 34.Kanegae H, Suzuki K, Fukatani K, Ito T, Harada N, Kario K. Highly precise risk prediction model for new-onset hypertension using artificial intelligence techniques. J Clin Hypertens (Greenwich) 202022445–450doi: 10.1111/jch.13759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kario K. New insight of morning blood pressure surge into the triggers of cardiovascular disease-synergistic resonance of blood pressure variability. Am J Hypertens 20162914–16doi: 10.1093/ajh/hpv114 [DOI] [PubMed] [Google Scholar]
- 36.Kario K, Chirinos JA, Townsend RR, Weber MA, Scuteri A, Avolio A, Hoshide S, Kabutoya T, Tomiyama H, Node K, et al. Systemic hemodynamic atherothrombotic syndrome (SHATS) - coupling vascular disease and blood pressure variability: proposed concept from pulse of Asia. Prog Cardiovasc Dis 20206322–32doi: 10.1016/j.pcad.2019.11.002 [DOI] [PubMed] [Google Scholar]
- 37.Kario K, Schwartz JE, Gerin W, Robayo N, Maceo E, Pickering TG. Psychological and physical stress-induced cardiovascular reactivity and diurnal blood pressure variation in women with different work shifts. Hypertens Res 200225543–551doi: 10.1291/hypres.25.543 [DOI] [PubMed] [Google Scholar]
- 38.Kario K, Chen CH, Park S, Park CG, Hoshide S, Cheng HM, Huang QF, Wang JG. Consensus document on improving hypertension management in Asian patients, taking into account Asian characteristics. Hypertension 201871375–382doi: 10.1161/HYPERTENSIONAHA.117.10238 [DOI] [PubMed] [Google Scholar]
- 39.Chen CT, Li Y, Zhang J, Wang Y, Ling HW, Chen KM, Gao PJ, Zhu DL. Association between ambulatory systolic blood pressure during the day and asymptomatic intracranial arterial stenosis. Hypertension 20146361–67doi: 10.1161/HYPERTENSIONAHA.113.01838 [DOI] [PubMed] [Google Scholar]
- 40.Kaneda R, Kario K, Hoshide S, Umeda Y, Hoshide Y, Shimada K. Morning blood pressure hyper-reactivity is an independent predictor for hypertensive cardiac hypertrophy in a community-dwelling population. Am J Hypertens 20051812 Pt 11528–1533doi: 10.1016/j.amjhyper.2005.06.015 [DOI] [PubMed] [Google Scholar]
- 41.Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, Murata M, Kuroda T, Schwartz JE, Shimada K. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation 20031071401–1406doi: 10.1161/01.cir.0000056521.67546.aa [DOI] [PubMed] [Google Scholar]
- 42.Kuwajima I, Mitani K, Miyao M, Suzuki Y, Kuramoto K, Ozawa T. Cardiac implications of the morning surge in blood pressure in elderly hypertensive patients: relation to arising time. Am J Hypertens 1995829–33doi: 10.1016/0895-7061(94)00154-4 [DOI] [PubMed] [Google Scholar]
- 43.Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension 200647149–154doi: 10.1161/01.HYP.0000198541.12640.0f [DOI] [PubMed] [Google Scholar]
- 44.Shimizu M, Ishikawa J, Yano Y, Hoshide S, Shimada K, Kario K. The relationship between the morning blood pressure surge and low-grade inflammation on silent cerebral infarct and clinical stroke events. Atherosclerosis 2011219316–321doi: 10.1016/j.atherosclerosis.2011.06.030 [DOI] [PubMed] [Google Scholar]
- 45.Yano Y, Hoshide S, Inokuchi T, Kanemaru Y, Shimada K, Kario K. Association between morning blood pressure surge and cardiovascular remodeling in treated elderly hypertensive subjects. Am J Hypertens 2009221177–1182doi: 10.1038/ajh.2009.162 [DOI] [PubMed] [Google Scholar]
- 46.Acciaroli G, Facchinetti A, Pillonetto G, Sparacino G. Non-invasive continuous-time blood pressure estimation from a single channel PPG signal using regularized ARX models. Conf Proc IEEE Eng Med Biol Soc 201820183630–3633doi: 10.1109/EMBC.2018.8512944 [DOI] [PubMed] [Google Scholar]
- 47.Hoshide S, Kario K, Hoshide Y, Umeda Y, Hashimoto T, Kunii O, Ojima T, Shimada K. Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensives. Am J Hypertens 200316434–438doi: 10.1016/s0895-7061(03)00567-3 [DOI] [PubMed] [Google Scholar]
- 48.Kario K, Matsuo T, Kobayashi H, Imiya M, Matsuo M, Shimada K. Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippers. Hypertension 199627130–135doi: 10.1161/01.hyp.27.1.130 [DOI] [PubMed] [Google Scholar]
- 49.Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension 200138852–857doi: 10.1161/hy1001.092640 [DOI] [PubMed] [Google Scholar]
- 50.Kario K, Shimada K. Risers and extreme-dippers of nocturnal blood pressure in hypertension: antihypertensive strategy for nocturnal blood pressure. Clin Exp Hypertens 200426177–189doi: 10.1081/ceh-120028556 [DOI] [PubMed] [Google Scholar]
- 51.Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens 2002202183–2189doi: 10.1097/00004872-200211000-00017 [DOI] [PubMed] [Google Scholar]
- 52.Kabutoya T, Hoshide S, Ishikawa J, Eguchi K, Shimada K, Kario K. The effect of pulse rate and blood pressure dipping status on the risk of stroke and cardiovascular disease in Japanese hypertensive patients. Am J Hypertens 201023749–755doi: 10.1038/ajh.2010.45 [DOI] [PubMed] [Google Scholar]
- 53.Komori T, Eguchi K, Saito T, Hoshide S, Kario K. Riser pattern: another determinant of heart failure with preserved ejection fraction. J Clin Hypertens (Greenwich) 201618994–999doi: 10.1111/jch.12818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Komori T, Eguchi K, Saito T, Hoshide S, Kario K. Riser pattern is a novel predictor of adverse events in heart failure patients with preserved ejection fraction. Circ J 201781220–226doi: 10.1253/circj.CJ-16-0740 [DOI] [PubMed] [Google Scholar]
- 55.Kario K. Nocturnal hypertension: new technology and evidence. Hypertension 201871997–1009doi: 10.1161/HYPERTENSIONAHA.118.10971 [DOI] [PubMed] [Google Scholar]
- 56.Burke LE, Ma J, Azar KM, Bennett GG, Peterson ED, Zheng Y, Riley W, Stephens J, Shah SH, Suffoletto B, Turan TN, Spring B, Steinberger J, Quinn CC; American Heart Association Publications Committee of the Council on Epidemiology and Prevention, Behavior Change Committee of the Council on Cardiometabolic Health, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, Council on Quality of Care and Outcomes Research, and Stroke Council Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation 20151321157–1213doi: 10.1161/CIR.0000000000000232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Picone DS, Deshpande RA, Schultz MG, Fonseca R, Campbell NRC, Delles C, Hecht Olsen M, Schutte AE, Stergiou G, Padwal R, et al. Nonvalidated home blood pressure devices dominate the online marketplace in Australia: major implications for cardiovascular risk management. Hypertension 2020751593–1599doi: 10.1161/HYPERTENSIONAHA.120.14719 [DOI] [PubMed] [Google Scholar]
- 58.Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of a wrist-type home nocturnal blood pressure monitor in the sitting and supine position according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-9600T. J Clin Hypertens (Greenwich) 201921463–469doi: 10.1111/jch.13464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of two watch-type wearable blood pressure monitors according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-6410T-ZM and HEM-6410T-ZL. J Clin Hypertens (Greenwich) 201921853–858doi: 10.1111/jch.13499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Association for the Advancement of Medical Instrumentation American National Standard: Non-Invasive Sphygmomanometers - Part 2: Clinical Validation of Automated Measurement Type; ANSI/AAMI/ISO. 201381060–81062Available at: https://my.aami.org/aamiresources/previewfiles/8106002_1306_preview.pdf. Accessed April 2, 2020
- 61.Kario K, Shimbo D, Tomitani N, Kanegae H, Schwartz JE, Williams B. The first study comparing a wearable watch-type blood pressure monitor with a conventional ambulatory blood pressure monitor on in-office and out-of-office settings. J Clin Hypertens (Greenwich) 202022135–141doi: 10.1111/jch.13799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Islam SMS, Cartledge S, Karmakar C, Rawstorn JC, Fraser SF, Chow C, Maddison R. Validation and acceptability of a cuffless wrist-worn wearable blood pressure monitoring device among users and health care professionals: mixed methods study. JMIR Mhealth Uhealth. 2019;7:e14706. doi: 10.2196/14706. doi: 10.2196/14706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nair D, Tan SY, Gan HW, Lim SF, Tan J, Zhu M, Gao H, Chua NH, Peh WL, Mak KH. The use of ambulatory tonometric radial arterial wave capture to measure ambulatory blood pressure: the validation of a novel wrist-bound device in adults. J Hum Hypertens 200822220–222doi: 10.1038/sj.jhh.1002306 [DOI] [PubMed] [Google Scholar]
- 64.Komori T, Eguchi K, Hoshide S, Williams B, Kario K. Comparison of wrist-type and arm-type 24-h blood pressure monitoring devices for ambulatory use. Blood Press Monit 20131857–62doi: 10.1097/MBP.0b013e32835d124f [DOI] [PubMed] [Google Scholar]
- 65.Kokubo A, Kuwubara M, Nakajima H, Tomitani N, Yamashita S, Shiga T, Kario K. Automatic detection algorithm for establishing standard to identify “surge blood pressure.” Med Biol Eng Comput 2020581393–1404doi: 10.1007/s11517-020-02162-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Arakawa T. Recent research and developing trends of wearable sensors for detecting blood pressure. Sensors (Basel) 2018;18:2772. doi: 10.3390/s18092772. doi: 10.3390/s18092772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Penaz J.Photo-electric measurement of blood pressure, volume and flow in the finger.. In Proceedings of the Digest of Tenth International Conference on Medical Biological Engineering; August 13–17, 1973; Dresden, Germany. [Google Scholar]
- 68.Liu J, Yan BP, Zhang YT, Ding XR, Su P, Zhao N. Multi-wavelength photoplethysmography enabling continuous blood pressure measurement with compact wearable electronics. IEEE Trans Biomed Eng 2019661514–1525doi: 10.1109/TBME.2018.2874957 [DOI] [PubMed] [Google Scholar]
- 69.Rachim VP, Chung WY. Multimodal wrist biosensor for wearable cuff-less blood pressure monitoring system. Sci Rep. 2019;9:7947. doi: 10.1038/s41598-019-44348-3. doi: 10.1038/s41598-019-44348-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Watanabe N, Bando YK, Kawachi T, Yamakita H, Futatsuyama K, Honda Y, Yasui H, Nishimura K, Kamihara T, Okumura T, et al. Development and validation of a novel cuff-less blood pressure monitoring device. JACC Basic Transl Sci 20172631–642doi: 10.1016/j.jacbts.2017.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lazazzera R, Belhaj Y, Carrault G. A new wearable device for blood pressure estimation using photoplethysmogram. Sensors (Basel) 2019;19:2557. doi: 10.3390/s19112557. doi: 10.3390/s19112557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chan G, Cooper R, Hosanee M, et al. Multi-site photoplethysmography technology for blood pressure assessment: challenges and recommendations. J Clin Med. 2019;8:1827. doi: 10.3390/jcm8111827. doi: 10.3390/jcm8111827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mukkamala R, Hahn JO, Inan OT, Mestha LK, Kim CS, Töreyin H, Kyal S. Toward ubiquitous blood pressure monitoring via pulse transit time: theory and practice. IEEE Trans Biomed Eng 2015621879–1901doi: 10.1109/TBME.2015.2441951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Geddes LA, Voelz MH, Babbs CF, Bourland JD, Tacker WA. Pulse transit time as an indicator of arterial blood pressure. Psychophysiology 19811871–74doi: 10.1111/j.1469-8986.1981.tb01545.x [DOI] [PubMed] [Google Scholar]
- 75.Smith RP, Argod J, Pépin JL, Lévy PA. Pulse transit time: an appraisal of potential clinical applications. Thorax 199954452–457doi: 10.1136/thx.54.5.452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Thomas SS, Nathan V, Chengzhi Zong, Akinbola E, Aroul AL, Philipose L, Soundarapandian K, Xiangrong Shi, Jafari R. BioWatch - a wrist watch based signal acquisition system for physiological signals including blood pressure. Conf Proc IEEE Eng Med Biol Soc 201420142286–2289doi: 10.1109/EMBC.2014.6944076 [DOI] [PubMed] [Google Scholar]
- 77.Thomas SS, Nathan V, Zong C, Soundarapandian K, Shi X, Jafari R. BioWatch: a noninvasive wrist-based blood pressure monitor that incorporates training techniques for posture and subject variability. IEEE J Biomed Health Inform 2016201291–1300doi: 10.1109/JBHI.2015.2458779 [DOI] [PubMed] [Google Scholar]
- 78.Huynh TH, Jafari R, Chung WY. Noninvasive cuffless blood pressure estimation using pulse transit time and impedance plethysmography. IEEE Trans Biomed Eng 201966967–976doi: 10.1109/TBME.2018.2865751 [DOI] [PubMed] [Google Scholar]
- 79.Zhang Q, Zhou D, Zeng X. Highly wearable cuff-less blood pressure and heart rate monitoring with single-arm electrocardiogram and photoplethysmogram signals. Biomed Eng Online. 2017;16:23. doi: 10.1186/s12938-017-0317-z. doi: 10.1186/s12938-017-0317-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zheng Y, Poon CC, Yan BP, Lau JY. Pulse arrival time based cuff-less and 24-h wearable blood pressure monitoring and its diagnostic value in hypertension. J Med Syst. 2016;40:195. doi: 10.1007/s10916-016-0558-6. doi: 10.1007/s10916-016-0558-6. [DOI] [PubMed] [Google Scholar]
- 81.Bilo G, Zorzi C, Ochoa Munera JE, Torlasco C, Giuli V, Parati G. Validation of the Somnotouch-NIBP noninvasive continuous blood pressure monitor according to the European Society of Hypertension International Protocol revision 2010. Blood Press Monit 201520291–294doi: 10.1097/MBP.0000000000000124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.O’Brien E, Atkins N, Stergiou G, Karpettas N, Parati G, Asmar R, Imai Y, Wang J, Mengden T, Shennan A; Working Group on Blood Pressure Monitoring of the European Society of Hypertension European Society of Hypertension International Protocol revision 2010 for the validation of blood pressure measuring devices in adults. Blood Press Monit 20101523–38doi: 10.1097/MBP.0b013e3283360e98 [DOI] [PubMed] [Google Scholar]
- 83.Qiu C, Wu T, Redoute JM, Yuce MR. A wireless wearable sensor patch for the real-time estimation of continuous beat-to-beat blood pressure. Conf Proc IEEE Eng Med Biol Soc 201920196842–6845doi: 10.1109/EMBC.2019.8857446 [DOI] [PubMed] [Google Scholar]
- 84.Ibrahim B, Jafari R. Continuous blood pressure monitoring using wrist-worn bio-impedance sensors with wet electrodes. IEEE Biomed Circuits Syst Conf. 2018;2018 doi: 10.1109/BIOCAS.2018.8584783. doi: 10.1109/BIOCAS.2018.8584783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Huynh TH, Jafari R, Chung WY. A robust bioimpedance structure for smartwatch-based blood pressure monitoring. Sensors (Basel) 2018;18:2095. doi: 10.3390/s18072095. doi: 10.3390/s18072095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Narasimhan R, Parlikar T, Verghesel G, McConnell MV. Finger-wearable blood pressure monitor. Conf Proc IEEE Eng Med Biol Soc 201820183792–3795doi: 10.1109/EMBC.2018.8513065 [DOI] [PubMed] [Google Scholar]
- 87.Wang TW, Lin SF. Wearable piezoelectric-based system for continuous beat-to-beat blood pressure measurement. Sensors (Basel) 2020;20:851. doi: 10.3390/s20030851. doi: 10.3390/s20030851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kim J, Chou EF, Le J, Wong S, Chu M, Khine M. Soft wearable pressure sensors for beat-to-beat blood pressure monitoring. Adv Healthc Mater. 2019;8:e1900109. doi: 10.1002/adhm.201900109. doi: 10.1002/adhm.201900109. [DOI] [PubMed] [Google Scholar]
- 89.Rastegar S, GholamHosseini H, Lowe A. Non-invasive continuous blood pressure monitoring systems: current and proposed technology issues and challenges [published online ahead of print November 1, 2019]. Australas Phys Eng Sci Med. 2019 doi: 10.1007/s13246-019-00813-x. doi: 10.1007/s13246-13019-00813-x. [DOI] [PubMed] [Google Scholar]
- 90.McLean G, Band R, Saunderson K, Hanlon P, Murray E, Little P, McManus RJ, Yardley L, Mair FS; DIPSS Co-Investigators Digital interventions to promote self-management in adults with hypertension systematic review and meta-analysis. J Hypertens 201634600–612doi: 10.1097/HJH.0000000000000859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Milani RV, Lavie CJ, Bober RM, Milani AR, Ventura HO. Improving hypertension control and patient engagement using digital tools. Am J Med 201713014–20doi: 10.1016/j.amjmed.2016.07.029 [DOI] [PubMed] [Google Scholar]
- 92.Jehn M, Appel LJ, Sacks FM, Miller ER 3rd; DASH Collaborative Research Group The effect of ambient temperature and barometric pressure on ambulatory blood pressure variability. Am J Hypertens 200215941–945doi: 10.1016/s0895-7061(02)02999-0 [DOI] [PubMed] [Google Scholar]
- 93.Park S, Kario K, Chia YC, Turana Y, Chen CH, Buranakitjaroen P, Nailes J, Hoshide S, Siddique S, Sison J, et al. ; HOPE Asia Network The influence of the ambient temperature on blood pressure and how it will affect the epidemiology of hypertension in Asia. J Clin Hypertens (Greenwich) 202022438–444doi: 10.1111/jch.13762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Widlansky ME, Vita JA, Keyes MJ, Larson MG, Hamburg NM, Levy D, Mitchell GF, Osypiuk EW, Vasan RS, Benjamin EJ. Relation of season and temperature to endothelium-dependent flow-mediated vasodilation in subjects without clinical evidence of cardiovascular disease (from the Framingham Heart Study). Am J Cardiol 2007100518–523doi: 10.1016/j.amjcard.2007.03.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lewington S, Li L, Sherliker P, Guo Y, Millwood I, Bian Z, Whitlock G, Yang L, Collins R, Chen J, et al. ; China Kadoorie Biobank Study Collaboration Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens 2012301383–1391doi: 10.1097/HJH.0b013e32835465b5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yang L, Li L, Lewington S, Guo Y, Sherliker P, Bian Z, Collins R, Peto R, Liu Y, Yang R, et al. ; China Kadoorie Biobank Study Collaboration Outdoor temperature, blood pressure, and cardiovascular disease mortality among 23 000 individuals with diagnosed cardiovascular diseases from China. Eur Heart J 2015361178–1185doi: 10.1093/eurheartj/ehv023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hanazawa T, Asayama K, Watabe D, Hosaka M, Satoh M, Yasui D, Obara T, Inoue R, Metoki H, Kikuya M, et al. Seasonal variation in self-measured home blood pressure among patients on antihypertensive medications: HOMED-BP study. Hypertens Res 201740284–290doi: 10.1038/hr.2016.133 [DOI] [PubMed] [Google Scholar]
- 98.Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, Giglio A, Bilo G, Caldara G, Lonati L, et al. Weather-related changes in 24-hour blood pressure profile: effects of age and implications for hypertension management. Hypertension 200647155–161doi: 10.1161/01.HYP.0000199192.17126.d4 [DOI] [PubMed] [Google Scholar]
- 99.Sega R, Cesana G, Bombelli M, Grassi G, Stella ML, Zanchetti A, Mancia G. Seasonal variations in home and ambulatory blood pressure in the PAMELA population. Pressione Arteriose Monitorate E Loro Associazioni. J Hypertens 1998161585–1592doi: 10.1097/00004872-199816110-00004 [DOI] [PubMed] [Google Scholar]
- 100.Sheng CS, Cheng YB, Wei FF, Yang WY, Guo QH, Li FK, Huang QF, Thijs L, Staessen JA, Wang JG, et al. Diurnal blood pressure rhythmicity in relation to environmental and genetic cues in untreated referred patients. Hypertension 201769128–135doi: 10.1161/HYPERTENSIONAHA.116.07958 [DOI] [PubMed] [Google Scholar]
- 101.Tabara Y, Matsumoto T, Murase K, Nagashima S, Hirai T, Kosugi S, Nakayama T, Wakamura T, Chin K, Matsuda F; The Nagahama Study Group Seasonal variation in nocturnal home blood pressure fall: the Nagahama study. Hypertens Res 201841198–208doi: 10.1038/s41440-017-0003-3 [DOI] [PubMed] [Google Scholar]
- 102.Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, Tobias A, Tong S, Rocklöv J, Forsberg B, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 2015386369–375doi: 10.1016/S0140-6736(14)62114-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ishikawa J, Hoshide S, Eguchi K, Ishikawa S, Shimada K, Kario K; Japan Morning Surge-Home Blood Pressure Study Investigators Group Nighttime home blood pressure and the risk of hypertensive target organ damage. Hypertension 201260921–928doi: 10.1161/HYPERTENSIONAHA.112.198101 [DOI] [PubMed] [Google Scholar]
- 104.Ishikawa J, Shimizu M, Sugiyama Edison E, Yano Y, Hoshide S, Eguchi K, Kario K; J-TOP (Japan Morning Surge-Target Organ Protection) Study Investigators Group Assessment of the reductions in night-time blood pressure and dipping induced by antihypertensive medication using a home blood pressure monitor. J Hypertens 20143282–89doi: 10.1097/HJH.0b013e328365c8a8 [DOI] [PubMed] [Google Scholar]
- 105.Kario K, Hoshide S, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, Yano Y, Eguchi K, Matsui Y, Shimizu M, et al. ; J-HOP Study Group Sleep blood pressure self-measured at home as a novel determinant of organ damage: Japan Morning Surge Home Blood Pressure (J-HOP) Study. J Clin Hypertens (Greenwich) 201517340–348doi: 10.1111/jch.12500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kario K, Hoshide S, Shimizu M, Yano Y, Eguchi K, Ishikawa J, Ishikawa S, Shimada K. Effect of dosing time of angiotensin II receptor blockade titrated by self-measured blood pressure recordings on cardiorenal protection in hypertensives: the Japan Morning Surge-Target Organ Protection (J-TOP) study. J Hypertens 2010281574–1583doi: 10.1097/HJH.0b013e3283395267 [DOI] [PubMed] [Google Scholar]
- 107.Kario K, Kanegae H, Tomitani N, Okawara Y, Fujiwara T, Yano Y, Hoshide S. Nighttime blood pressure measured by home blood pressure monitoring as an independent predictor of cardiovascular events in general practice. Hypertension 2019731240–1248doi: 10.1161/HYPERTENSIONAHA.118.12740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hoshide S, Kario K, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, Matsui Y, Nakamura A, Fukutomi M, et al. ; J-HOP Study Group Association of morning and evening blood pressure at home with asymptomatic organ damage in the J-HOP Study. Am J Hypertens 201427939–947doi: 10.1093/ajh/hpt290 [DOI] [PubMed] [Google Scholar]
- 109.Fujiwara T, Tomitani N, Kanegae H, Kario K. Comparative effects of valsartan plus either cilnidipine or hydrochlorothiazide on home morning blood pressure surge evaluated by information and communication technology-based nocturnal home blood pressure monitoring. J Clin Hypertens (Greenwich) 201820159–167doi: 10.1111/jch.13154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kario K, Tomitani N, Kanegae H, Ishii H, Uchiyama K, Yamagiwa K, Shiraiwa T, Katsuya T, Yoshida T, Kanda K, et al. Comparative effects of an angiotensin II receptor blocker (ARB)/diuretic vs. ARB/calcium-channel blocker combination on uncontrolled nocturnal hypertension evaluated by information and communication technology-based nocturnal home blood pressure monitoring-the NOCTURNE Study. Circ J 201781948–957doi: 10.1253/circj.CJ-17-0109 [DOI] [PubMed] [Google Scholar]
- 111.Nishizawa M, Hoshide S, Okawara Y, Matsuo T, Kario K. Strict blood pressure control achieved using an ICT-based home blood pressure monitoring system in a catastrophically damaged area after a disaster. J Clin Hypertens (Greenwich) 20171926–29doi: 10.1111/jch.12864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Koshimizu H, Kojima R, Kario K, Okuno Y. Prediction of blood pressure variability using deep neural networks. Int J Med Inform. 2020;136:104067. doi: 10.1016/j.ijmedinf.2019.104067. doi: 10.1016/j.ijmedinf.2019.104067. [DOI] [PubMed] [Google Scholar]
- 113.Kitt J, Fox R, Tucker KL, McManus RJ. New approaches in hypertension management: a review of current and developing technologies and their potential impact on hypertension care. Curr Hypertens Rep. 2019;21:44. doi: 10.1007/s11906-019-0949-4. doi: 10.1007/s11906-019-0949-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kabutoya T, Takahashi S, Watanabe T, et al. Diagnostic accuracy of an algorithm for detecting atrial fibrillation in a wrist-type pulse wave monitor. J Clin Hypertens (Greenwich) 2019211393–1398 [DOI] [PMC free article] [PubMed] [Google Scholar]


