Abstract
Objective
To evaluate and quantify the future risk of cardiovascular events in young adults with high blood pressure.
Design
Systematic review and meta-analysis.
Data sources
Medline, Embase, and Web of Science were searched from inception to 6 March 2020. Relative risks were pooled using a random effects model and expressed with 95% confidence intervals. Absolute risk difference was calculated. Dose-response relations between blood pressure and individual outcomes were assessed by a restricted cubic spline model.
Eligibility criteria for selecting studies
Studies were selected that investigated the adverse outcomes of adults aged 18-45 with raised blood pressure. The primary study outcome was a composite of total cardiovascular events. Coronary heart disease, stroke, and all cause mortality were examined as secondary outcomes.
Results
Seventeen observational cohorts consisting of approximately 4.5 million young adults were included in the analysis. The average follow-up was 14.7 years. Young adults with normal blood pressure had increased risk of cardiovascular events compared with those with optimal blood pressure (relative risk 1.19, 95% confidence interval 1.08 to 1.31; risk difference 0.37, 95% confidence interval 0.16 to 0.61 per 1000 person years). A graded, progressive association was found between blood pressure categories and increased risk of cardiovascular events (high normal blood pressure: relative risk 1.35, 95% confidence interval 1.22 to 1.49; risk difference 0.69, 95% confidence interval 0.43 to 0.97 per 1000 person years; grade 1 hypertension: 1.92, 1.68 to 2.19; 1.81, 1.34 to 2.34; grade 2 hypertension: 3.15, 2.31 to 4.29; 4.24, 2.58 to 6.48). Similar results were observed for coronary heart disease and stroke. Generally, the population attributable fraction for cardiovascular events associated with raised blood pressure was 23.8% (95% confidence interval 17.9% to 28.8%). The number needed to treat for one year to prevent one cardiovascular event was estimated at 2672 (95% confidence interval 1639 to 6250) for participants with normal blood pressure, 1450 (1031 to 2326) for those with high normal blood pressure, 552 (427 to 746) for those with grade 1 hypertension, and 236 (154 to 388) for those with grade 2 hypertension.
Conclusions
Young adults with raised blood pressure might have a slightly increased risk of cardiovascular events in later life. Because the evidence for blood pressure lowering is limited, active interventions should be cautious and warrant further investigation.
Introduction
Cardiovascular events are responsible for more than 18 million deaths each year, which is around one third of all global deaths.1 2 High blood pressure is a well recognised remediable risk factor for cardiovascular events. Currently, two different blood pressure thresholds are used to diagnose hypertension: the traditional threshold of 140/90 mm Hg3 and the newly recommended threshold of 130/80 mm Hg given in the 2017 guideline by the American College of Cardiology and American Heart Association.4 Although different criteria are implemented for diagnosing hypertension, their therapeutic recommendation is similar and largely driven by the risk of cardiovascular disease.3 4 Most randomised outcome studies have involved participants who are at high risk or are over the age of 55.5 Therefore frequently used risk prediction models or guidelines are mainly based on studies among older people,3 4 6 whereas the association between blood pressure and cardiovascular event risks among young adults is under studied. Although hypertension is traditionally a more prevalent disease in older people, recent epidemiological studies have shown that the incidence is progressively rising among the young.7
Further research is needed to determine whether cumulative exposure to raised blood pressure during young adulthood contributes to higher risks of cardiovascular events in later life. Systematic reviews or randomised control trials investigating the associations of raised blood pressure with risks of cardiovascular events among young adults are lacking. Only a limited number of observational studies exist.8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 However, substantial heterogeneity has been observed, varying in risk thresholds and the associations with different disease outcomes. An Indian cohort study showed that the risk of cardiovascular mortality increased in participants aged 34-44 years with systolic blood pressure from the category 140-159 mm Hg,21 while in several other cohorts, the blood pressure threshold associated with cardiovascular events was around 120/80 mm Hg.8 9 23 Additionally, Son and colleagues reported that higher measured blood pressure in early adulthood was associated with increased risks of all cardiovascular outcomes,8 whereas in the Harvard Alumni Health Study, the exposure-outcome association was exclusive of strokes.15
With these inconsistent findings in mind, an up-to-date understanding of the association of blood pressure with different cardiovascular outcomes is needed, which would help to refine strategies for primary prevention and to inform the design of future clinical trials. We conducted a systematic review and meta-analysis of published studies to quantify the association between blood pressure categories and the future risk of cardiovascular events in young adults. Additionally we assessed if increases in systolic and diastolic blood pressure differentially impacted distinctive clinical outcomes.
Methods
This study was conducted under a predefined protocol (supplementary appendix 1), following the recommendations of the Cochrane handbook25 and reporting in accordance with the PRISMA (preferred reporting items for systematic reviews and meta-analysis) statement.26 The protocol was amended once on 6 March 2020; the search end date and search strategies were updated. Extra statistical analyses were also performed. Additionally, the grading quality of this meta-analysis was reported and evaluated by using the GRADE (grading of recommendations assessment, Development and evaluation) approach.27 According to the protocol deviation process guide, these changes were considered minor protocol deviations.28
Inclusion and exclusion criteria
We considered studies to be eligible if they were longitudinal cohort studies that enrolled adults aged 18-45 years, and reported the association between increased blood pressure and the study outcomes. The primary study outcome was a composite of total cardiovascular events—coronary heart disease, stroke, heart failure, other types of cardiovascular diseases, and any cardiovascular deaths. We examined coronary heart disease, stroke, and all cause mortality as secondary outcomes.
We excluded studies if they were review articles, case reports, cross sectional studies, or randomised controlled trials comparing efficacy of antihypertensive medications; or if the study population was complicated with some other overt diseases, including cardiovascular diseases, kidney disease, diabetes, pulmonary hypertension, cancers, hyperthyroidism, connective tissue disease, rheumatoid arthritis, mental diseases or obstructive sleep apnoea. We also excluded studies involving pregnant participants, critically ill patients, or those admitted to hospital, studies recording fewer than three groups of blood pressure strata, or providing insufficient data to allow for risk estimates to be calculated.
Data sources and searches
We searched Medline, Embase, and Web of Science for articles from inception to 6 March 2020. Supplementary appendix 2 gives the detailed search strategy that used several search terms: (hypertension OR blood pressure) AND (cardiovascular disease OR coronary artery disease OR coronary heart disease OR myocardial infarction OR ischaemic heart disease OR acute coronary syndrome OR stroke OR cerebrovascular accident OR cerebrovascular disease OR cardiovascular events OR cardiovascular deaths OR heart failure OR diabetes OR renal failure OR chronic kidney disease) AND (cohort OR follow up) AND (age OR young). No restrictions were applied based on sex, location, languages, or duration of follow-up. We searched the reference lists of the included studies and relevant review articles, and contacted authors of potentially eligible articles to request additional data. Hand searching from the Google Scholar, China National Knowledge Infrastructure, or Wanfang datasets was conducted for additional grey literature, including government reports, insurance reports, conference proceedings, and digital dissertations. We also searched ClincalTrials.gov and the World Health Organization International Clinical Trials Registry Platform for ongoing or unpublished eligible studies. If duplicate studies were found from the same cohort that offered similar outcome measures, we included the studies reporting the most relevant data. However, if duplicate studies offered information for different outcomes, they were included in the pooled analysis for specific outcome analysis.
Two reviewers (DL and YC) screened all titles that met the inclusion criteria and then the remaining abstracts were screened. The full manuscripts were screened by the same reviewers to make the final decision for all included studies. Any disagreements were resolved by consensus.
Data extraction and quality assessment
Two reviewers (DL and YC) performed independent double data extraction. Core baseline and outcome data were extracted, including first author, year of publication, region/country, study type, year of enrolment, number and age of the included participants, follow-up duration, male sex proportion, body mass index, mean blood pressure level of each blood pressure stratum, the methods used for blood pressure measurement, and the study outcomes. Blood pressure was stratified into five subgroups: optimal blood pressure (systolic blood pressure <120 mm Hg and diastolic blood pressure <80 mm Hg), normal blood pressure (120-129 and 80-84 mm Hg), high normal blood pressure (130-139 and 85-89 mm Hg), grade 1 hypertension (140-159 and 90-99 mm Hg), and grade 2 hypertension (≥160 and ≥100 mm Hg) based on the 2018 European guideline.3 Optimal blood pressure was the reference category for relative risks. The information was obtained from published data or calculated by using the raw data.
We used the Newcastle-Ottawa scale to assess the characteristics and quality of included studies. Briefly, the scale is based on a star system and includes three broad perspectives: selection of the study groups, comparability of the groups, and ascertainment of the outcome of interest.29 Total score is calculated by summing the score for each answer. Studies are considered of good quality if the total score is at least 7/9. Two reviewers (DL and YC) independently conducted quality assessments of the included studies. Disagreements were resolved by discussion and further review. Publication bias was assessed by visual inspection of funnel plots and by Egger’s statistical tests.30 We considered a P value less than 0.05 to be evidence of small study effects.
Data synthesis and analysis
We used the STATA version 15.0 (Stata Corp, College Station, TX) software package to conduct random effects meta-analysis by using the inverse variance method for pooling log relative risks. Random effects was used because the studies were conducted over a wide range of settings in different populations. This approach required that heterogeneity be considered when making the pooled effect estimate. If possible, we chose to pool the risk estimates from primary studies, and when these data were not available, raw data were used to calculate unadjusted risk estimates. Pooled relative risks were expressed with 95% confidence intervals. The absolute risk difference was calculated by using the formula [(RR−1)*I0], where RR indicates pooled relative risks and I0 is the incidence of cardiovascular events per 1000 person years among young adults with optimal blood pressure.31
We present benefit after one year of treatment in terms of number needed to treat for one year. This calculation assumed that the effect of treatment could help to lower the increased blood pressure to an optimal level and the event rate could be reduced to the same level as that in the population with optimal blood pressure. Number needed to treat was calculated directly as the reciprocal of the absolute risk difference between participants with increased blood pressure and optimal blood pressure.32 Additionally, we used the formula pdi*[(RR−1)/RR] to calculate the population attributable fractions for each categorical blood pressure level in comparison to the reference category of optimal blood pressure, where pdi represents the proportion of total events in the population arising from the ith exposure category.33
In the dose-response analysis, we used restricted cubic splines to assess the pooled dose-response relation between blood pressure and individual outcomes. Nonlinear models were fitted and the results presented with 95% confidence intervals.34 We used mean values of the systolic blood pressure or diastolic blood pressure reported by the original studies, or calculated the average level by estimating the midpoint in each category. To enable the total person years of observation to be calculated, we included data from reports that specified total person time of follow-up, or sample size and median follow-up per person.
We used the χ2 test to assess heterogeneity across studies, expressed as Cochran’s Q and I2 statistics, together with 95% confidence intervals. Values of 0-25% represented minimal heterogeneity, 26-75% represented moderate heterogeneity, and values greater than 75% represented substantial heterogeneity.35
We performed meta-regression and stratified analyses to assess the potential sources of heterogeneity. Studies were stratified into different subgroups based on age (younger than or older than 30 years); body mass index (≥25 or <25); sample size (≥100 000 or <100 000); median follow-up duration (>20 or ≤20 years); year of enrolment (before or after 1980); population regions (Asia, Europe, or North America); and Newcastle-Ottawa scale scores (>7 or ≤7). For studies reporting subgroups stratified by sex, we combined results from the male subgroups and studies that were all male, which were then compared with the pooling results of the female subgroups. We separated studies based on male proportion (≥90% or <90%) to further explore the potential effect of sex distribution on the associations of high blood pressure and cardiovascular risks.
We conducted further sensitivity analyses by leaving out studies with high risk of bias21; removing studies with only male participants10 13 15 17 22 23 24 or military members10; excluding studies of retrospective design8 19 24 or using non-equivalent outcome definitions9 24; or limiting studies to those involving only untreated participants,8 12 13 19 20 23 using a mercury sphygmomanometer for blood pressure measurements,12 13 14 21 22 23 or reporting some levels of adjustment.8 9 10 11 12 13 15 18 19 20 21 22 23 All statistical tests were two sided and a P value less than 0.05 was considered statistically significant.
Patient and public involvement
No patients or the public were involved in setting the research question or the outcome measures, nor were they involved in developing plans for recruitment, design, or implementation of the study. No patients or the public were asked to advise on interpretation or writing up of results. We had no way of directly contacting participants from the original studies.
Results
Description of studies included in the analysis
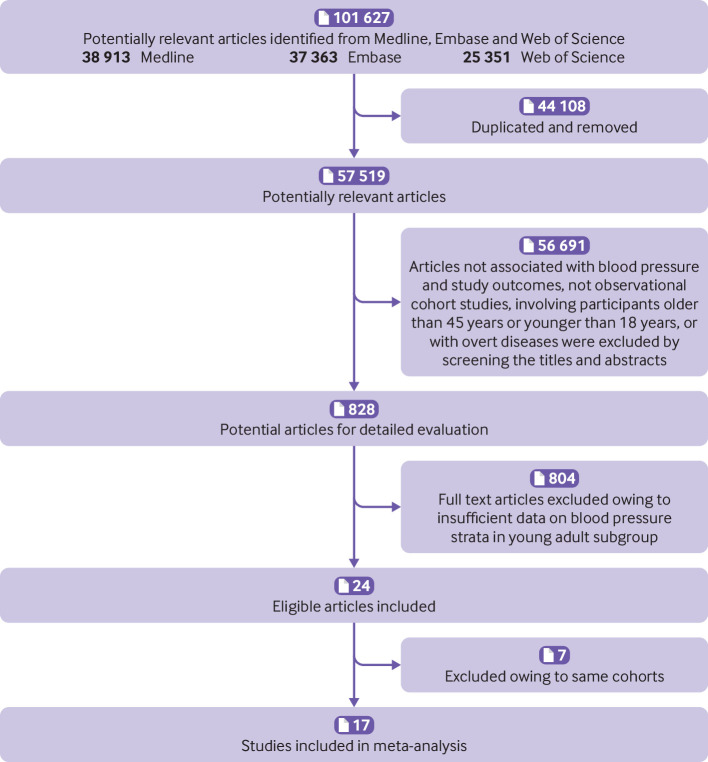
From 57 519 published records, 828 remained eligible for inclusion based on screening of the titles and abstracts. After reading the full manuscripts, a total of 17 studies were included in the analysis8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 (fig 1). The studies examined 4 533 292 young adults (ranging from 3490 to 2 488 101 in each study), with an average follow-up of 14.7 years (ranging from 4.3 to 56.3 years in each study). Table 1 gives details of the study characteristics. Three of the studies were retrospective cohort studies and 14 were prospective. All studies reported the outcome of cardiovascular events (coronary heart disease or stroke) and only eight reported the outcome of all cause mortality.
Fig 1.
Flowchart of selection of studies included in meta-analysis
Table 1.
Core characteristics of included studies
| Study | Region (country) | Study design (cohort) | Population at risk | Year of enrolment | Age (years) | Male sex (%) | Body mass index | Follow-up (years) | Study outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Selmer 199214 | Europe (Norway) | Prospective | 9827 | 1963 to 1964 | 35 | 43.0 | 25.3 | 20 | CV events, CHD, stroke, and all cause mortality |
| Glasgow Alumni 200017 | Europe (UK) | Prospective | 8345 | 1948 to 1968 | 20.5 | 100 | 21.7 | 41.3 | CV events, CHD, stroke, and all cause mortality |
| CHA 200123 | North America (US) | Prospective | 10 874 | 1967 to 1973 | 29.7 | 100 | 26 | 25 | CV events, CHD, and all cause mortality |
| Strandberg 200113 | Europe(Finland) | Prospective | 3490 | 1964 to 1973 | 37.5 | 100 | 25.9 | 27 | CV events and all cause mortality |
| MRFIT 200222 | North America (US) | Prospective | 148 204 | 1973 to 1975 | 40 | 100 | 27.7 | 22 | CV events |
| Falkstedt 200816 | Europe (Sweden) | Prospective | 47 873 | 1969 to 1970 | 19 | 100 | 21 | 18 | CHD and stroke |
| Sauvaget 201021 | Asia (India) | Prospective | 62 435 | 1996 to 2004 | 40 | 38.4 | 21.3 | 7 | CV events, CHD, and stroke |
| HAHS 201115 | North America (US) | Prospective | 18 881 | 1962 to 1966 | 18.3 | 100 | 21.7 | 56.3 | CV events, CHD, stroke, and all cause mortality |
| Sundström 201110 | Europe (Sweden) | Prospective | 1 207 141 | 1969 to 1995 | 18.4 | 100 | 21.7 | 24 | CV events and all cause mortality |
| CARDIA 20189 | North America (US) | Prospective | 4851 | 1985 to 1986 | 35.7 | 45.2 | 27.7 | 18.8 | CV events, CHD, stroke, and all cause mortality |
| CMCS 201820 | Asia (China) | Prospective | 8551 | 1992 to 1993 | 39.3 | 47.0 | 24.2 | 13.7 | CV events, CHD, and stroke |
| KNHI 20188 | Asia (Korea) | Retrospective | 2 488 101 | 2002 to 2005 | 31 | 68.3 | 23.1 | 10 | CV events, CHD, and stroke |
| EPOCH-JAPAN 201918 | Asia (Japan) | Prospective | 107 737 | 1980 to 2002 | 35 | 42.4 | 23.1 | 15.2 | CV events, CHD, and stroke |
| Jee 201924 | Asia (Korea) | Retrospective | 118 531 | 1992 to 1994 | 26.7 | 100 | 22.3 | 23 | CV events, CHD, and stroke |
| Kim 201919 | Asia (Korea) | Retrospective | 232 349 | 2011 to 2016 | 39 | 54.0 | 23.2 | 4.3 | CV events, CHD, and stroke |
| Liu 201911 | Asia (China) | Prospective | 20 072 | 2004 to 2006 | 41.5 | 49.9 | 24.1 | 12.5 | CV events, CHD, stroke, and all cause mortality |
| Zhang 201912 | North America (US) | Prospective | 36 030 | 1971 to 2002 | 30 | 44.5 | 26.8 | 17 | CV events, CHD, and stroke |
CHD=coronary heart disease; CV=cardiovascular.
We found no evidence of publication bias across different blood pressure categories based on visual inspection of funnel plots and the results from Egger’s tests (all P>0.05; supplementary appendix 3, fig S1). Table 2 reports Newcastle-Ottawa scale scores and quality assessment of the included studies; only one study scored lower than 7, indicating fair quality.21 All the other studies were recorded as good quality and low risk of bias based on total scores higher than 7. Most studies were rated as including representative participants for the general population. All but one study reported adequately on outcome ascertainment.19 According to the GRADE summary of evidence, the quality of evidence was rated as moderate to high for the outcomes of cardiovascular events, coronary heart disease and stroke, but low for all cause mortality except for the category of grade 2 hypertension (supplementary appendix 3, table S1).
Table 2.
Newcastle-Ottawa scale scores and quality assessment of included studies
| Study | Selection | Comparability | Outcome | Quality* | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness | Selection | Ascertainment | Outcome | Assessment | Follow-up | Adequacy | |||
| Selmer 199214 | * | * | * | — | ** | * | * | * | Good (8) |
| Glasgow Alumni 200017 | * | * | * | * | ** | * | * | * | Good (9) |
| CHA 200123 | * | * | * | * | ** | * | * | * | Good (9) |
| Strandberg 200113 | * | * | — | * | ** | * | * | * | Good (8) |
| MRFIT 200222 | * | * | * | * | ** | * | * | * | Good (9) |
| Falkstedt 200816 | * | * | * | * | ** | * | * | * | Good (9) |
| Sauvaget 201021 | — | * | * | — | * | * | * | * | Fair (6) |
| HAHS 201115 | * | * | * | * | ** | * | * | * | Good (9) |
| Sundstrom 201110 | * | * | * | * | ** | * | * | * | Good (9) |
| CARDIA 20189 | * | * | * | * | ** | * | * | * | Good (9) |
| CMCS 201820 | * | * | * | * | ** | * | * | * | Good (9) |
| KNHI 20188 | * | * | * | * | ** | * | * | * | Good (9) |
| EPOCH-JAPAN 201918 | * | — | * | * | ** | * | * | * | Good (8) |
| Jee 201924 | * | — | * | * | * | * | * | * | Good (7) |
| Kim 201919 | * | * | * | * | ** | * | — | * | Good (8) |
| Liu 201911 | * | * | — | * | * | * | * | * | Good (7) |
| Zhang, 201912 | * | — | * | * | * | * | * | * | Good (7) |
Total stars awarded.
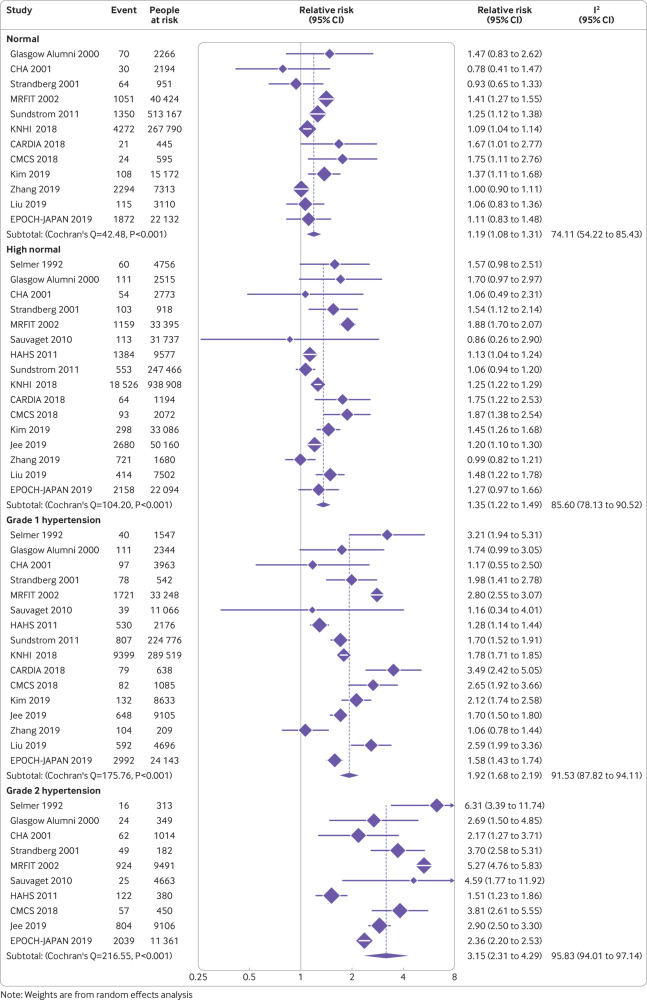
Increased blood pressure and primary study outcome
During follow-up, 85 674 cardiovascular events occurred. The event rate of cardiovascular events in young adults with optimal blood pressure was estimated to be 1.97 per 1000 person years (95% confidence interval 1.48 to 2.46). Figure 2 shows a graded, progressive association between blood pressure categories and the primary outcome. Young adults with normal blood pressure (relative risk 1.19, 95% confidence interval 1.08 to 1.31; risk difference 0.37, 95% confidence interval 0.16 to 0.61 per 1000 person years), high normal blood pressure (1.35, 1.22 to 1.49; 0.69, 0.43 to 0.97), grade 1 hypertension (1.92, 1.68 to 2.19; 1.81, 1.34 to 2.34), and grade 2 hypertension (3.15, 2.31 to 4.29; 4.24, 2.58 to 6.48 per 1000 person years) had increased risk of cardiovascular events compared with those with optimal blood pressure.
Fig 2.
Forest plot of relative risks of cardiovascular events across blood pressure categories compared with optimal blood pressure. RR=relative risk
The heterogeneity of relative risks was substantial and statistically significant across studies (Q=42.5, I2=74.1%, P<0.001 for normal blood pressure; Q=104.2, I2=85.6%, P<0.001 for high normal blood pressure; Q=175.8, I2=91.5%, P<0.001 for grade 1 hypertension; Q=216.6, I2=95.8%, P<0.001 for grade 2 hypertension; fig 2). Therefore, we conducted sensitivity analyses across various scenarios to assess whether and to what extent the heterogeneity could be reduced. As a result, the heterogeneity reduced from substantial to moderate (supplementary appendix 3, table S2) when the analyses were confined to studies including only untreated participants8 12 13 19 20 23 or when a mercury sphygmomanometer was used for blood pressure measurements.12 13 14 21 22 23
To further explore the source of heterogeneity, we performed stratified analyses in the predefined subgroups. The findings of increased cardiovascular risk associated with high blood pressure were consistently observed in most of the stratified analyses (table 3). Differences in study sample size, study quality, follow-up duration, population regions, or body mass index were not major sources of heterogeneity. Additionally, summary estimates of the risk increasing association were identical for both sexes. The stratification based on male proportion (≥90% v <90%) did not reveal a major difference in the exposure-outcome associations, which suggested that the disparity in sex proportion did not have an important effect on our findings. Also, the pattern of association did not change materially after removing studies that had all male participants10 13 15 17 22 23 24 or only military members.10 Although the year of enrolment for individual studies could be a source of heterogeneity, we did not observe important secular trends when pooling studies conducted before or after the 1980s (table 3). However, the associations of blood pressure above high normal blood pressure level and risks of cardiovascular events were more evident in young adults aged over 30 years, suggesting that age could be one of the sources of study heterogeneity.
Table 3.
Stratification analysis of pooled relative risks for cardiovascular events
| Stratified by | Normal blood pressure | High normal blood pressure | Grade 1 hypertension | Grade 2 hypertension | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR (95% CI) | RD (95% CI)* | P value | RR (95% CI) | RD (95% CI)* | P value | RR (95% CI) | RD (95% CI)* | P value | RR (95% CI) | RD (95% CI)* | P value | |||||
| Mean age (years) | ||||||||||||||||
| >30 | 1.23 (1.07 to 1.41) | 0.37 (0.11 to 0.67) | 0.39 | 1.52 (1.30 to 1.78) | 0.85 (0.49 to 1.27) | 0.001 | 2.28 (1.90 to 2.73) | 2.09 (1.47 to 2.82) | 0.001 | 4.03 (2.56 to 6.36) | 4.94 (2.54 to 8.74) | 0.02 | ||||
| ≤30 | 1.12 (0.92 to 1.35) | 0.30 (−0.20 to 0.88) | — | 1.13 (1.05 to 1.21) | 0.33 (0.13 to 0.53) | — | 1.46 (1.24 to 1.72) | 1.15 (0.60 to 1.81) | — | 2.22 (1.46 to 3.39) | 3.06 (1.15 to 6.00) | — | ||||
| Mean body mass index | ||||||||||||||||
| ≥25 | 1.14 (0.89 to 1.46) | 0.36 (−0.28 to 1.17) | 0.62 | 1.46 (1.09 to 1.96) | 1.17 (0.23 to 2.45) | 0.31 | 2.12 (1.44 to 3.11) | 2.86 (1.12 to 5.38) | 0.35 | 4.12 (2.81 to 6.05) | 7.96 (4.62 to 12.88) | 0.07 | ||||
| <25 | 1.20 (1.08 to 1.33) | 0.33 (0.13 to 0.54) | — | 1.26 (1.17 to 1.36) | 0.43 (0.28 to 0.59) | — | 1.77 (1.60 to 1.96) | 1.26 (0.98 to 1.57) | — | 2.54 (2.01 to 3.21) | 2.53 (1.66 to 3.62) | — | ||||
| Sample size (people) | ||||||||||||||||
| ≥100 000 | 1.24 (1.09 to 1.42) | 0.39 (0.15 to 0.68) | 0.25 | 1.33 (1.15 to 1.54) | 0.54 (0.24 to 0.88) | 0.76 | 1.90 (1.62 to 2.23) | 1.47 (1.01 to 2.00) | 0.93 | 3.30 (1.96 to 5.57) | 3.75 (1.56 to 7.45) | 0.80 | ||||
| <100 000 | 1.13 (0.95 to 1.35) | 0.28 (−0.11 to 0.77) | — | 1.38 (1.17 to 1.62) | 0.83 (0.37 to 1.36) | — | 1.93 (1.43 to 2.61) | 2.04 (0.94 to 3.53) | — | 3.10 (2.00 to 4.79) | 4.60 (2.19 to 8.30) | — | ||||
| Follow-up duration (years) | ||||||||||||||||
| >20 | 1.25 (1.08 to 1.44) | 0.32 (0.10 to 0.56) | 0.52 | 1.33 (1.08 to 1.63) | 0.42 (0.10 to 0.81) | 0.74 | 1.76 (1.36 to 2.29) | 0.97 (0.46 to 1.65) | 0.37 | 2.84 (1.81 to 4.47) | 2.36 (1.04 to 4.44) | 0.40 | ||||
| ≤20 | 1.14 (1.03 to 1.27) | 0.35 (0.08 to 0.68) | — | 1.36 (1.21 to 1.53) | 0.90 (0.53 to 1.33) | — | 2.03 (1.73 to 2.39) | 2.58 (1.83 to 3.48) | — | 3.71 (2.29 to 6.02) | 6.78 (3.23 to 12.55) | — | ||||
| Year of enrolment | ||||||||||||||||
| >1980s | 1.14 (1.03 to 1.27) | 0.37 (0.08 to 0.72) | 0.52 | 1.31 (1.20 to 1.43) | 0.83 (0.53 to 1.15) | 0.82 | 1.90 (1.68 to 2.15) | 2.40 (1.82 to 3.07) | 0.90 | 2.86 (2.31 to 3.55) | 4.97 (3.50 to 6.81) | 0.95 | ||||
| ≤1980s | 1.25 (1.08 to 1.44) | 0.26 (0.08 to 0.46) | — | 1.39 (1.08 to 1.78) | 0.41 (0.08 to 0.81) | — | 1.90 (1.38 to 2.61) | 0.94 (0.40 to 1.67) | — | 3.19 (1.78 to 5.70) | 2.28 (0.81 to 4.89) | — | ||||
| Region | ||||||||||||||||
| North America | 1.19 (0.90 to 1.58) | 0.56 (−0.30 to 1.72) | — | 1.34 (0.97 to 1.84) | 1.01 (−0.09 to 2.49) | — | 1.77 (1.08 to 2.91) | 2.29 (0.24 to 5.67) | — | 2.61 (0.99 to 6.84) | 4.78 (−0.03 to 17.34) | — | ||||
| Europe | 1.19 (0.99 to 1.44) | 0.12 (−0.01 to 0.28) | 0.94† | 1.36 (1.03 to 1.79) | 0.23 (0.02 to 0.50) | 0.90† | 1.96 (1.54 to 2.50) | 0.60 (0.34 to 0.95) | 0.65† | 3.90 (2.58 to 5.89) | 1.83 (1.00 to 3.08) | 0.40† | ||||
| Asia | 1.18 (1.03 to 1.35) | 0.34 (0.06 to 0.67) | 0.97‡ | 1.33 (1.22 to 1.44) | 0.63 (0.42 to 0.84) | 0.90‡ | 1.87 (1.69 to 2.08) | 1.65 (1.31 to 2.05) | 0.70‡ | 2.86 (2.31 to 3.55) | 3.53 (2.49 to 4.85) | 0.66‡ | ||||
| Sex§ | ||||||||||||||||
| Male | 1.13 (1.00 to 1.28) | 0.31 (0.00 to 0.67) | 0.72 | 1.26 (1.12 to 1.42) | 0.62 (0.29 to 1.00) | 0.47 | 1.67 (1.42 to 1.97) | 1.60 (1.00 to 2.32) | 0.30 | 2.57 (1.75 to 3.78) | 3.75 (1.79 to 6.64) | 0.23 | ||||
| Female | 1.17 (0.99 to 1.39) | 0.65 (−0.04 to 1.49) | — | 1.25 (1.22 to 1.29) | 0.96 (0.84 to 1.11) | — | 1.90 (1.54 to 2.33) | 3.45 (2.07 to 5.09) | — | 5.84 (1.05 to 32.62) | 18.54 (0.19 to 121.10) | — | ||||
| Male proportion | ||||||||||||||||
| <90% | 1.14 (1.03 to 1.27) | 0.35 (0.08 to 0.68) | 0.52 | 1.36 (1.21 to 1.53) | 0.90 (0.53 to 1.33) | 0.74 | 2.03 (1.73 to 2.39) | 2.58 (1.83 to 3.48) | 0.37 | 3.71 (2.29 to 6.02) | 6.78 (3.23 to 12.55) | 0.40 | ||||
| ≥90% | 1.25 (1.08 to 1.44) | 0.32 (0.10 to 0.56) | — | 1.33 (1.08 to 1.63) | 0.42 (0.10 to 0.81) | — | 1.76 (1.36 to 2.29) | 0.97 (0.46 to 1.65) | — | 2.84 (1.81 to 4.47) | 2.36 (1.04 to 4.44) | — | ||||
| NOS score | ||||||||||||||||
| >7 | 1.26 (1.11 to 1.43) | 0.29 (0.12 to 0.47) | 0.06 | 1.42 (1.25 to 1.63) | 0.46 (0.28 to 0.69) | 0.19 | 2.06 (1.72 to 2.47) | 1.17 (0.79 to 1.62) | 0.19 | 3.27 (1.98 to 5.39) | 2.50 (1.08 to 4.83) | 0.72 | ||||
| ≤7 | 1.02 (0.93 to 1.12) | 0.08 (−0.27 to 0.46) | — | 1.21 (1.06 to 1.39) | 0.81 (0.23 to 1.51) | — | 1.65 (1.36 to 2.00) | 2.51 (1.39 to 3.86) | — | 2.66 (2.17 to 3.26) | 6.41 (4.52 to 8.72) | — | ||||
NOS=Newcastle-Ottawa scale; RD=risk difference; RR=relative risk.
Per 1000 person years.
P value for Europe versus North America subgroup.
P value for Asia versus North America subgroup.
Sex specific analyses available.
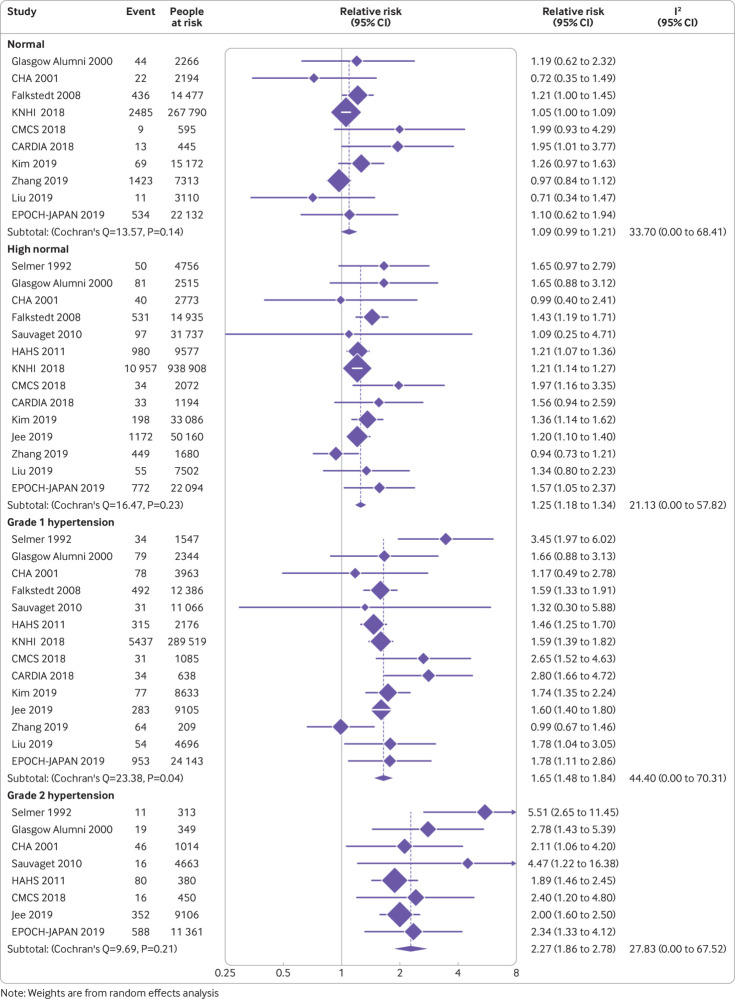
Increased blood pressure and secondary study outcomes
The event rates for coronary heart disease, stroke, and all cause mortality in young adults with optimal blood pressure level were estimated to be 1.07 (95% confidence interval 0.77 to 1.38), 0.94 (0.67 to 1.21), and 3.12 (1.40 to 4.84) per 1000 person years, respectively. The relative risk for coronary heart disease was 1.09 (95% confidence interval 0.99 to 1.21; risk difference 0.10, 95% confidence interval −0.01 to 0.22 per 1000 person years) for normal blood pressure, 1.25 (1.18 to 1.34; 0.27, 0.19 to 0.36) for high normal blood pressure, 1.65 (1.48 to 1.84; 0.70, 0.51 to 0.90 ) for grade 1 hypertension, and 2.27 (1.86 to 2.78; 1.36, 0.92 to 1.90) for grade 2 hypertension compared with optimal blood pressure (fig 3).
Fig 3.
Forest plot of relative risks of coronary heart disease across blood pressure categories compared with optimal blood pressure. RR=relative risk
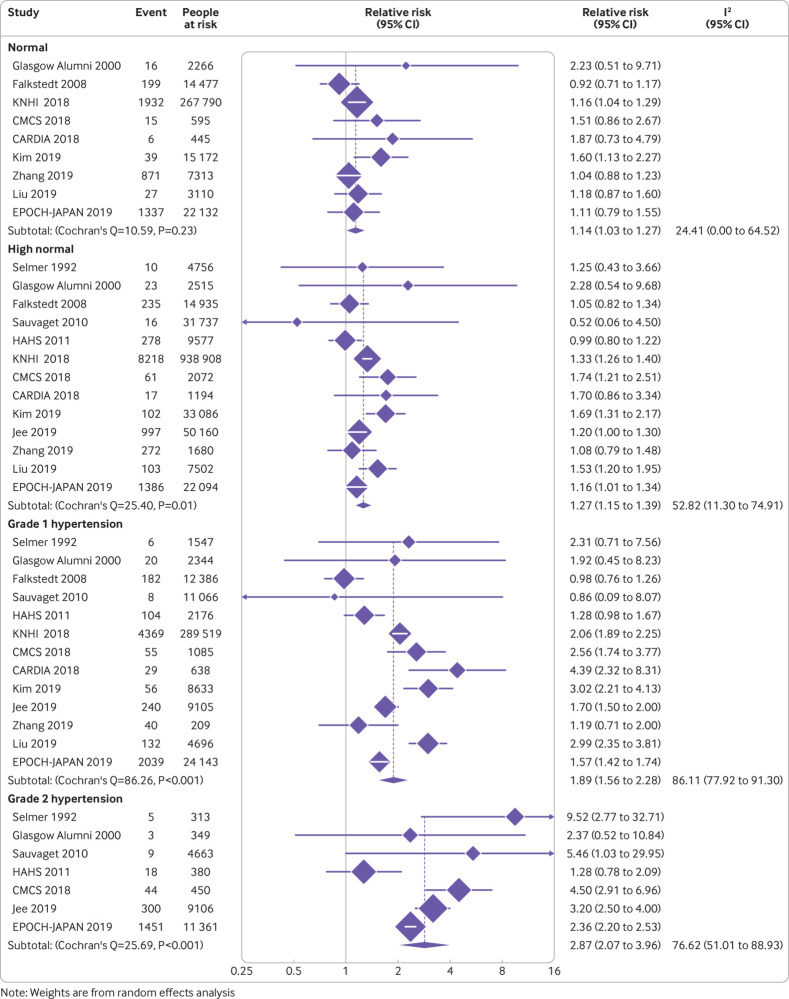
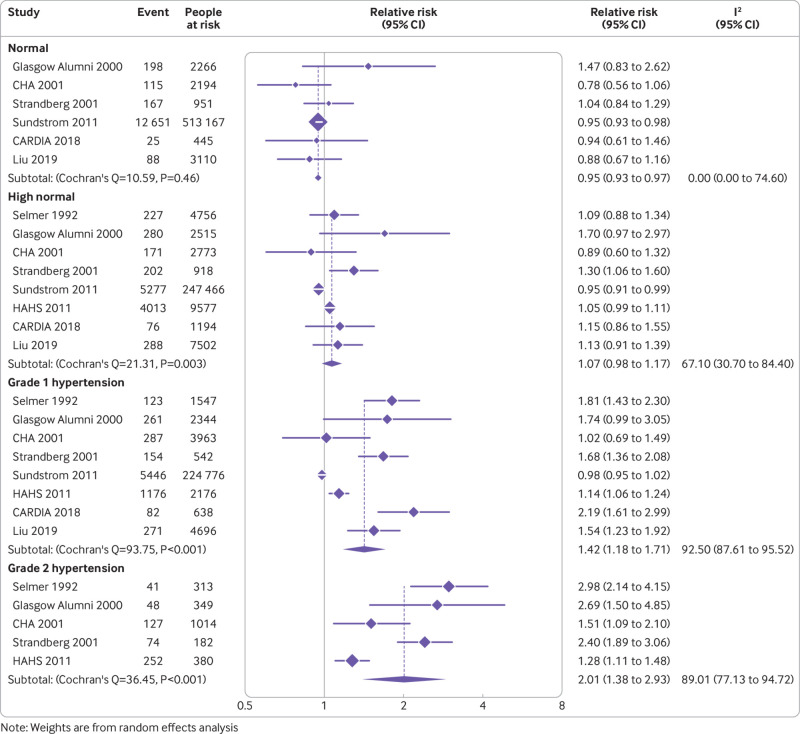
Similarly, young adults with normal blood pressure (relative risk 1.14, 95% confidence interval 1.03 to 1.27; risk difference 0.13, 95% confidence interval 0.03 to 0.25 per 1000 person years), high normal blood pressure (1.27, 1.15 to 1.39; 0.25, 0.14 to 0.37), grade 1 hypertension (1.89, 1.56 to 2.28; 0.84, 0.53 to 1.20), and grade 2 hypertension (2.87, 2.07 to 3.96; 1.76, 1.01 to 2.78) had increased risk of stroke compared with those with optimal blood pressure (fig 4). For all cause mortality, the risk increased above a blood pressure of 140/90 mm Hg, with a 42% higher risk for grade 1 hypertension (relative risk 1.42, 95% confidence interval 1.18 to 1.71; risk difference 1.31, 95% confidence interval 0.56 to 2.22 per 1000 person years) and a double risk for grade 2 hypertension (2.01, 1.38 to 2.93; 3.15, 1.19 to 6.02; fig 5).
Fig 4.
Forest plot of relative risks of stroke across blood pressure categories compared with optimal blood pressure. RR=relative risk
Fig 5.
Forest plot of relative risks of all cause mortality across blood pressure categories compared with optimal blood pressure. RR=relative risk
The heterogeneity of relative risks was moderate to substantial for the outcomes of stroke and all cause mortality across high normal blood pressure (Q=25.4, I2=52.8%, P=0.01 for stroke; Q=21.3, I2=67.1%, P=0.003 for all cause mortality; fig 4 and fig 5), grade 1 hypertension (Q=86.3, I2=86.1%, P<0.001 for stroke; Q=93.8, I2=92.5%, P<0.001 for all cause mortality; fig 4 and fig 5), and grade 2 hypertension strata (Q=25.7, I2=76.6%, P<0.001 for stroke; Q=36.5, I2=89.0%, P<0.001 for all cause mortality; fig 4 and fig 5). However, for the normal blood pressure stratum (Q=10.6, I2=24.4%, P=0.23 for stroke; Q=10.6, I2=0.0%, P=0.46 for all cause mortality; fig 4 and fig 5) and coronary heart disease outcome associated with normal blood pressure (Q=13.6, I2=33.7%, P=0.14; fig 3), high normal blood pressure (Q=16.5, I2=21.1%, P=0.23; fig 3), and grade 2 hypertension (Q=9.7, I2=27.8%, P=0.21; fig 3), we did not observe any significant heterogeneity.
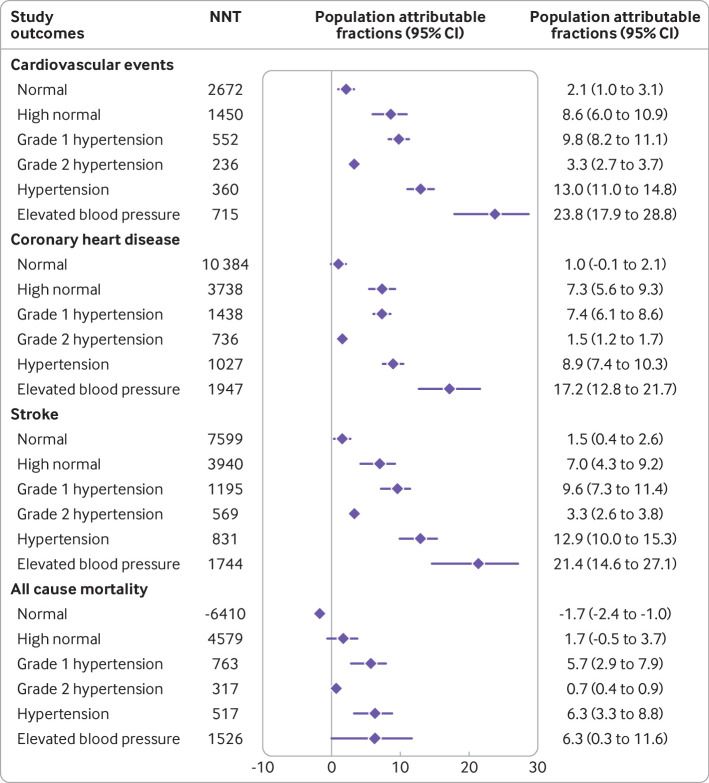
Number needed to treat and dose-response relation between blood pressure and all study outcomes
Assuming that the effect of treatment could help to lower increased blood pressure to the optimal level and the risk attributable to raised blood pressure was removed by treatment, the number needed to treat for one year to prevent one cardiovascular event was estimated to be 2672 (95% confidence interval 1639 to 6250) for those with normal blood pressure, 1450 (1031 to 2326) for those with high normal blood pressure, 552 (427 to 746) for those with grade 1 hypertension, and 236 (154 to 388) for those with grade 2 hypertension. Figure 6 shows the estimated number needed to treat to prevent one event of coronary heart disease, stroke, and all cause mortality. Generally, the population attributable fraction for the cardiovascular events associated with raised blood pressure was 23.8% (95% confidence interval 17.9% to 28.8%). The attributional effects increased across blood pressure increments: 2.1% (1.0% to 3.1%) for normal blood pressure, 8.6% (6.0% to 10.9%) for high normal blood pressure, and 13.0% (11.0% to 14.8%) for a hypertensive blood pressure level (fig 6). Similar results were observed for coronary heart disease and stroke (fig 6).
Fig 6.
Population attributable fraction and number needed to treat for one year for different study outcomes across blood pressure categories. NNT=number needed to treat
The risk increasing associations of blood pressure categories with cardiovascular events, coronary heart disease, and stroke were similar when using mean systolic and diastolic blood pressure values. Figure 7 shows that systolic blood pressure higher than 120-129 mm Hg was associated with an increased risk of cardiovascular events, coronary heart disease, and stroke in a dose responsive manner (fig 7, top panel). Similarly, the association of diastolic blood pressure with risk of cardiovascular events, coronary heart disease, and stroke monotonically increased from a level of 80 mm Hg (fig 7, bottom panel). For all cause mortality, the risk associated with systolic blood pressure increased from a level above 150-160 mm Hg, and an association with diastolic blood pressure was observed above 80-90 mm Hg. Independently, every 10 mm Hg increment of systolic blood pressure was associated with a 5% increased risk of cardiovascular events (relative risk 1.05, 95% confidence interval 1.03 to 1.06), a 3% increased risk of coronary heart disease (1.03, 1.02 to 1.04), a 4% increased risk of stroke (1.04, 1.02 to 1.05), and a 2% increased risk of all cause mortality (1.02, 1.01 to 1.03). For diastolic blood pressure, each 5 mm Hg increment resulted in a 4% increased risk of cardiovascular events (1.04, 1.03 to 1.05), a 2% increased risk of coronary heart disease (1.02, 1.02 to 1.03), a 3% increased risk of stroke (1.03, 1.02 to 1.04), and a 2% increased risk of all cause mortality (1.02, 1.01 to 1.03).
Fig 7.
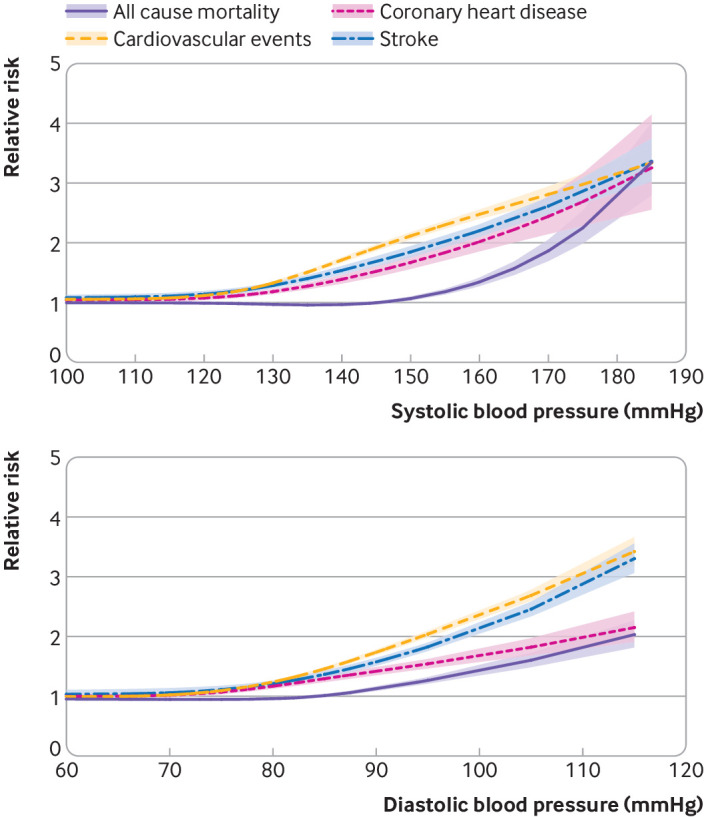
Nonlinear dose-response analysis of systolic blood pressure (top panel) and diastolic blood pressure (bottom panel) and risk of cardiovascular events, coronary heart disease, stroke, and all cause mortality. Shaded areas indicate 95% confidence intervals for corresponding coloured lines
Discussion
Principal findings
Limited evidence exists of an association between higher blood pressure and the risk of clinically manifest cardiovascular events in young adults. A systematic review of the literature provided insight into this process. Our study was based on 17 studies with approximately 4.5 million young adults and yielded three main findings. Firstly, we observed continuous and graded associations between categorical blood pressure increments and increasing risks of cardiovascular events, coronary heart disease, stroke, and all cause mortality. The risk increasing association with cardiovascular events was consistent in participants across different regions, but it was more evident in those older than 30 years. Secondly, the population attributable fractions for cardiovascular events from increased blood pressure were high, contributing to nearly a quarter of cardiovascular events in young adults. Thirdly, a similar pattern of the associations with different study outcomes was observed in the dose-response relation of systolic and diastolic blood pressure.
Strengths and limitations of the study
The strengths of the present study are the large sample size and the long follow-up duration, with a total of approximately 4.5 million participants at risk and an average follow-up of 14.7 years. The associations of high blood pressure with various study outcomes were examined across different blood pressure categories in our study. Unlike most of the previous studies assessing only normotension and hypertension,36 37 the use of comprehensive blood pressure strata enabled healthcare workers to determine a detailed association of blood pressure with cardiovascular events. Additionally, restricted cubic spline models were used to assess the dose-response relation between blood pressure and future risk of individual outcomes, providing an estimate of the independent associations of systolic and diastolic blood pressure with different study outcomes. Moreover, consistent results of the pooled estimates from the stratified and sensitivity analyses across various scenarios supported the robustness of the study findings.
However, limitations also exist. Firstly, this review was not preregistered. However, it was conducted under a predefined protocol and followed the guidance of the Cochrane handbook.25 The items recommended by the PRISMA statement were also provided, which reduced the manipulation and improved the transparency.26 Secondly, considerable heterogeneity was observed in the design of the included studies. The protocols for blood pressure measurement were not equivalent in different cohorts. Population characteristics, including age range, treated or untreated status, presence or absence of hyperglycaemia, hyperuricaemia, and dyslipidaemia might also have contributed to the heterogeneity of the included studies. As a result, although the risk increasing association remained robust across various scenarios, high levels of statistical heterogeneity generally persisted and could not be reduced in stratified and sensitivity analyses. Finally, pooling results from studies that were all male with other mixed studies could have biased the results. However, stratification analyses by sex distribution (male proportion) were conducted and showed that the summary estimates of the risk increasing association were identical for both sexes and in studies with different proportions of male participants. However, analysis of the female population was based on only four studies and the calculated estimates for women were highly uncertain.
Comparison with other studies
Associations between high blood pressure and cardiovascular risk have long been recognised and found to be age specific, but most of the outcome studies were carried out in middle aged or older populations.38 39 40 Previous cohort studies and overviews have shown that high blood pressure is robustly associated with increased risk of total cardiovascular events and all cause mortality in middle aged or older populations.1 23 38 41 42 The Suita Study reported that the cardiovascular risk was 2.04 (95% confidence interval 1.19 to 3.48) for normal blood pressure, 2.46 (1.46 to 4.14) for high normal blood pressure, 2.62 (1.59 to 4.32) for grade 1 hypertension, and 3.95 (2.37 to 6.58) for grade 2 hypertension compared with optimal blood pressure in a population over 50 years old. Additionally, each 10 mm Hg decrement in systolic blood pressure was predicted to result in a reduction in cardiovascular events of around 25-40%.43 Our findings further support the idea that the relative risks for cardiovascular events associated with various blood pressure categories vary among different age groups.39 We show that the relative risks for cardiovascular events in each blood pressure category were all lower among young adults. For every 10 mm Hg increment of systolic blood pressure and every 5 mm Hg increment of diastolic blood pressure, a 4-5% increase in risk was found.
Relative risk estimates for disease incidence are of limited clinical utility given the uncertainty about the incidence rate of the reference group, referring to the optimal blood pressure sample in our study.44 The absolute risk for cardiovascular events in young adults with optimal blood pressure is low compared with the older population. The Multi-Ethnic Study of Atherosclerosis, a population based study that enrolled adults aged 45-84 years who were free of clinical cardiovascular diseases, showed that the event rates for all cardiovascular events in participants with a blood pressure of 120-139 mm Hg were 5.6-24.3 per 1000 person years. For those with a blood pressure of 140-159 mm Hg, the event rates were 7.4-36.9 per 1000 person years and rose to a level of 16.7-37.1 per 1000 person years when blood pressure was higher than 160 mm Hg.45 Despite the relatively low absolute risk, the difference in absolute risk (at least four additional cardiovascular events per 10 000 person years in those with increased blood pressure) should not be overlooked owing to an increasing prevalence of hypertension in young adults.7 46 47
The population attributable fraction for cardiovascular events from raised blood pressure in young adults was higher than the corresponding blood pressure levels in older people.20 48 This finding suggests that the impact of high blood pressure on cardiovascular events is more detrimental among young people, especially above the level of 140/90 mm Hg. The reason for this effect is probably driven by age. The contributing impacts of other risk factors, including previous cardiovascular disease, impaired lung function, or longer duration of diabetes could make a greater difference at an older age and so the contributing role of hypertension diminishes48 49; however, for young adults, with fewer comorbidities or risk factors, the role of increased blood pressure dominates.
Systolic and diastolic blood pressure each independently influenced cardiovascular outcomes in young adults. The pathophysiological basis of high blood pressure in young adults and older people seems to be different.5 50 White coat hypertension, a hyperadrenergic state, a higher prevalence of secondary hypertension, and hypertension caused by peripheral blood pressure amplification are more commonly seen in young adults. Conversely, loss of arterial compliance and increased arterial stiffness are often found in older people, concurrent with increasing systolic blood pressure and decreasing diastolic blood pressure.5 50 51 Understanding such pathophysiological links among different age groups could help us to better understand what we found in this study. The Monica, Risk, Genetics, Archiving and Monograph project, a large population based cohort, found a gradual age related shift from diastolic blood pressure to both diastolic blood pressure and systolic blood pressure, and eventually to systolic blood pressure as a risk factor for cardiovascular events.52 This finding is consistent with our results, with systolic and diastolic blood pressure independently and comparatively associated with the risk of cardiovascular events. However, outcome specific association was observed in terms of systolic blood pressure and diastolic blood pressure. For systolic blood pressure, the risk of stroke and coronary heart disease was identical in pattern and increased from the level of 120 mm Hg, while for all cause mortality the risk apparently rose from the level of 150-160 mm Hg. For diastolic blood pressure, the burden for stroke was more evident than coronary heart disease and all cause mortality. Given that the prevalence of isolated diastolic hypertension is more pronounced in young adults, special attention should be paid to this population.53
Implications of the study
Uncertainty remains about antihypertensive treatments in young adults with increased blood pressure. Because our findings were based on observational studies, not interventional, no direct data were yielded relating to antihypertensive treatment. According to the hypertension guidelines, antihypertensive treatment is beneficial for those with a 10 year atherosclerotic cardiovascular disease risk of more than 10%.3 4 However, the frequently used risk prediction models have not been validated in young adults and evidence to support the recommendation of starting antihypertensive drugs is insufficient.54 55 Therefore, active interventions should be cautious. Based on our findings, to prevent one cardiovascular event, the number needed to treat for one year was estimated to be 2672, 1450, 552, and 236 for normal blood pressure, high normal blood pressure, grade 1 hypertension, and grade 2 hypertension, respectively. These data suggest a lower likelihood of treatment benefit, especially for those with normal and high normal blood pressure. Our results could inform healthcare professionals about the effort needed to achieve a particular outcome and provide insights into the design of future clinical trials.31
Without a defined association between high blood pressure and cardiovascular risks, developing and implementing standardised treatment advice and guidelines that include young adults is challenging. Although ongoing studies for young adults are currently being investigated, most are still at the initial stages and the long term impact on cardiovascular end points remains to be determined.56 57 58 Therefore, the insights provided in our study could help to refine strategies for primary prevention and might have important implications for future research.
Conclusion
We performed a meta-analysis of blood pressure and cardiovascular events data from approximately 4.5 million young adults. Importantly, cardiovascular risk was found to be increased at a normal blood pressure level. Despite the relatively low absolute risk, in this analysis the difference in absolute risk above normal blood pressure in comparison to optimal blood pressure was persistent and should not be ignored. Additionally, systolic and diastolic blood pressure each independently influenced cardiovascular outcomes, and so both should be considered when assessing risks in young adults. However, based on the high number needed to treat and probably low likelihood for treatment benefit, active interventions should be cautious and warrant further investigation.
What is already known on this topic
Associations between high blood pressure and cardiovascular risk have long been recognised, but most outcome studies included middle aged or older populations
The prevalence of hypertension among young adults has been increasing
Further research is needed to determine whether cumulative exposure to raised blood pressure during young adulthood contributes to higher risks of cardiovascular events in later life
What this study adds
A graded, progressive association between blood pressure categories and risk of cardiovascular events was observed in young adults
Systolic and diastolic blood pressure each independently influenced cardiovascular outcomes in young adults
Acknowledgments
We thank Yuli Huang from Shunde Hospital, Southern Medical University for his helpful comments on this study.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary appendix 1
Web appendix: Supplementary appendix 2
Web appendix: Supplementary appendix 3
Web appendix: Supplementary appendix 4
Contributors: DL, YC, and HZ contributed equally to this work. HC, CZ, and WS are senior and corresponding authors who also contributed equally to this study. DL, YC, HZ, HC, CZ, and WS have full access to all the data in this study and take full responsibility as guarantors for the integrity of the data and the accuracy of the data analysis. DL and YC contributed to studies selection, data extraction, data analyses, and manuscript drafting. HZ, MB, PC, HL, and KC contributed to data analyses, data interpretation, and manuscript drafting. HC, CZ, and WS contributed to study design, data interpretation, and final approval of the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This work was supported by the National Natural Science Foundation of China (grant No 81300279, 81741067, 81701396, and 81870334), Guangdong Province Natural Science Foundation (grant No 2016A030313815, 2017A030313464, and 2017A030313512), Science and Technology Planning Project of Guangdong Province (grant No 2015A020212029), Science and Technology Program of Guangzhou (grant No 201707010419 and 201804010050), and High-level Hospital Construction Project (grant No DFJH201803). The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: support from the National Natural Science Foundation of China, Guangdong Province Natural Science Foundation, Science and Technology Planning Project of Guangdong Province, Science and Technology Program of Guangzhou, and High-level Hospital Construction Project for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Ethical approval for this evidence synthesis was not required.
Data sharing: No additional data available.
The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: The authors plan to disseminate these findings to appropriate audiences such as academia, clinicians, policy makers, and the general public through various channels including press release, social media, or e-newsletter.
References
- 1. Han M, Li Q, Liu L, et al. Prehypertension and risk of cardiovascular diseases: a meta-analysis of 47 cohort studies. J Hypertens 2019;37:2325-32. 10.1097/HJH.0000000000002191. [DOI] [PubMed] [Google Scholar]
- 2. GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736-88. 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Williams B, Mancia G, Spiering W, et al. ESC Scientific Document Group 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021-104. 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 4. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018;138:e426-83. 10.1161/CIR.0000000000000597. [DOI] [PubMed] [Google Scholar]
- 5. Bursztyn M. Isolated systolic hypertension in young adults: a heterogeneous finding. J Hypertens 2018;36:1791-2. 10.1097/HJH.0000000000001763. [DOI] [PubMed] [Google Scholar]
- 6. Kjeldsen SE. Hypertension and cardiovascular risk: general aspects. Pharmacol Res 2018;129:95-9. 10.1016/j.phrs.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 7. De Venecia T, Lu M, Figueredo VM. Hypertension in young adults. Postgrad Med 2016;128:201-7. 10.1080/00325481.2016.1147927. [DOI] [PubMed] [Google Scholar]
- 8. Son JS, Choi S, Kim K, et al. Association of blood pressure classification in Korean young adults according to the 2017 American College of Cardiology/American Heart Association guidelines with subsequent cardiovascular disease events. JAMA 2018;320:1783-92. 10.1001/jama.2018.16501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yano Y, Reis JP, Colangelo LA, et al. Association of blood pressure classification in young adults using the 2017 American College of Cardiology/American Heart Association blood pressure guideline with cardiovascular events later in life. JAMA 2018;320:1774-82. 10.1001/jama.2018.13551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sundström J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ 2011;342:d643. 10.1136/bmj.d643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu S, Wang Y, Xie Y, et al. The association of stage 1 hypertension defined by the 2017 ACC/AHA hypertension guideline and subsequent cardiovascular events among adults <50 years. J Hum Hypertens 2020;34:233-40. 10.1038/s41371-019-0242-7. [DOI] [PubMed] [Google Scholar]
- 12. Zhang Y, Vittinghoff E, Pletcher MJ, et al. Associations of blood pressure and cholesterol levels during young adulthood with later cardiovascular events. J Am Coll Cardiol 2019;74:330-41. 10.1016/j.jacc.2019.03.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Strandberg TE, Salomaa VV, Vanhanen HT, Pitkälä K. Blood pressure and mortality during an up to 32-year follow-up. J Hypertens 2001;19:35-9. 10.1097/00004872-200101000-00005. [DOI] [PubMed] [Google Scholar]
- 14. Selmer R. Blood pressure and twenty-year mortality in the city of Bergen, Norway. Am J Epidemiol 1992;136:428-40. 10.1093/oxfordjournals.aje.a116516. [DOI] [PubMed] [Google Scholar]
- 15. Gray L, Lee IM, Sesso HD, Batty GD. Blood pressure in early adulthood, hypertension in middle age, and future cardiovascular disease mortality: HAHS (Harvard Alumni Health Study). J Am Coll Cardiol 2011;58:2396-403. 10.1016/j.jacc.2011.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Falkstedt D, Koupil I, Hemmingsson T. Blood pressure in late adolescence and early incidence of coronary heart disease and stroke in the Swedish 1969 conscription cohort. J Hypertens 2008;26:1313-20. 10.1097/HJH.0b013e3282ffb17e. [DOI] [PubMed] [Google Scholar]
- 17. McCarron P, Smith GD, Okasha M, McEwen J. Blood pressure in young adulthood and mortality from cardiovascular disease. Lancet 2000;355:1430-1. 10.1016/S0140-6736(00)02146-2. [DOI] [PubMed] [Google Scholar]
- 18. Satoh M, Ohkubo T, Asayama K, et al. EPOCH-JAPAN Research Group Lifetime risk of stroke and coronary heart disease deaths according to blood pressure level: EPOCH-JAPAN (Evidence for Cardiovascular Prevention From Observational Cohorts in Japan). Hypertension 2019;73:52-9. 10.1161/HYPERTENSIONAHA.118.11635. [DOI] [PubMed] [Google Scholar]
- 19. Kim S, Chang Y, Kang J, et al. Relationship of the blood pressure categories, as defined by the ACC/AHA 2017 blood pressure guidelines, and the risk of development of cardiovascular disease in low-risk young adults: insights from a retrospective cohort of young adults. J Am Heart Assoc 2019;8:e011946. 10.1161/JAHA.119.011946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Qi Y, Han X, Zhao D, et al. Long-term cardiovascular risk associated with stage 1 hypertension defined by the 2017 ACC/AHA hypertension guideline. J Am Coll Cardiol 2018;72:1201-10. 10.1016/j.jacc.2018.06.056. [DOI] [PubMed] [Google Scholar]
- 21. Sauvaget C, Ramadas K, Thomas G, Thara S, Sankaranarayanan R. Prognosis criteria of casual systolic and diastolic blood pressure values in a prospective study in India. J Epidemiol Community Health 2010;64:366-72. 10.1136/jech.2008.086777. [DOI] [PubMed] [Google Scholar]
- 22. Domanski M, Mitchell G, Pfeffer M, et al. MRFIT Research Group Pulse pressure and cardiovascular disease-related mortality: follow-up study of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA 2002;287:2677-83. 10.1001/jama.287.20.2677. [DOI] [PubMed] [Google Scholar]
- 23. Miura K, Daviglus ML, Dyer AR, et al. Relationship of blood pressure to 25-year mortality due to coronary heart disease, cardiovascular diseases, and all causes in young adult men: the Chicago Heart Association Detection Project in Industry. Arch Intern Med 2001;161:1501-8. 10.1001/archinte.161.12.1501. [DOI] [PubMed] [Google Scholar]
- 24. Jee Y, Jung KJ, Lee S, Back JH, Jee SH, Cho SI. Smoking and atherosclerotic cardiovascular disease risk in young men: the Korean Life Course Health Study. BMJ Open 2019;9:e024453. 10.1136/bmjopen-2018-024453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Higgins J, Green S. Cochrane handbook for systematic review of interventions. [Version 5.1.0] Cochrane Collaboration, 2011. [Google Scholar]
- 26. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Guyatt GH, Oxman AD, Vist GE, et al. GRADE Working Group GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924-6. 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.TransCelerate BioPharma,Inc. Protocol Deviation Process Guide https://transceleratebiopharmainc.com/wp-content/uploads/2019/08/TransCelerate_ProtocolDeviation_ProcessGuide_ForPublicComment_August2019.pdf. Accessed 28 April 2020.
- 29. Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute. oxford. asp, 2011. [Google Scholar]
- 30. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ray WA, Murray KT, Hall K, Arbogast PG, Stein CM. Azithromycin and the risk of cardiovascular death. N Engl J Med 2012;366:1881-90. 10.1056/NEJMoa1003833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tramèr MR, Walder B. Number needed to treat (or harm). World J Surg 2005;29:576-81. 10.1007/s00268-005-7916-8. [DOI] [PubMed] [Google Scholar]
- 33. Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health 1998;88:15-9. 10.2105/AJPH.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med 1989;8:551-61. 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 35. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Satoh M, Ohkubo T, Asayama K, et al. Evidence for Cardiovascular Prevention From Observational Cohorts in Japan (EPOCH–JAPAN) Research Group Combined effect of blood pressure and total cholesterol levels on long-term risks of subtypes of cardiovascular death: evidence for cardiovascular prevention from observational cohorts in Japan. Hypertension 2015;65:517-24. 10.1161/HYPERTENSIONAHA.114.04639. [DOI] [PubMed] [Google Scholar]
- 37. Satoh M, Asayama K, Kikuya M, et al. Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: the Ohasama Study. Hypertension 2016;67:48-55. 10.1161/HYPERTENSIONAHA.115.06461. [DOI] [PubMed] [Google Scholar]
- 38. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903-13. 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 39. Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet 2014;383:1899-911. 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation 2001;103:1245-9. 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- 41. Yano Y, Franklin SS, Greenland P, Lloyd-Jones D. Reply: interpreting blood pressure in young adults. J Am Coll Cardiol 2015;66:330-1. 10.1016/j.jacc.2015.05.019. [DOI] [PubMed] [Google Scholar]
- 42. Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA 1996;275:1571-6. 10.1001/jama.1996.03530440051036 [DOI] [PubMed] [Google Scholar]
- 43. Lawes CM, Bennett DA, Lewington S, Rodgers A. Blood pressure and coronary heart disease: a review of the evidence. Semin Vasc Med 2002;2:355-68. 10.1055/s-2002-36765. [DOI] [PubMed] [Google Scholar]
- 44. Lloyd-Jones DM, Braun LT, Ndumele CE, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American Heart Association and American College of Cardiology. Circulation 2019;139:e1162-77. 10.1161/CIR.0000000000000638. [DOI] [PubMed] [Google Scholar]
- 45. McEvoy JW, Martin SS, Dardari ZA, et al. Coronary artery calcium to guide a personalized risk-based approach to initiation and intensification of antihypertensive therapy. Circulation 2017;135:153-65. 10.1161/CIRCULATIONAHA.116.025471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Williamson W, Foster C, Reid H, et al. Will exercise advice be sufficient for treatment of young adults with prehypertension and hypertension? A systematic review and meta-analysis. Hypertension 2016;68:78-87. 10.1161/HYPERTENSIONAHA.116.07431. [DOI] [PubMed] [Google Scholar]
- 47. Scarborough Pa Bhatnagar P, Wickramasinghe K, Smolina K, Mitchell C, Rayner M. Coronary heart disease statistics 2010 edition. British Health Foundation Health Promotion research group. Department of Public Health, University of Oxford, 2010. [Google Scholar]
- 48. Whelton PK. Epidemiology of hypertension. Lancet 1994;344:101-6. 10.1016/s0140-6736(94)91285-8. [DOI] [PubMed] [Google Scholar]
- 49. Duong M, Islam S, Rangarajan S, et al. PURE investigators Mortality and cardiovascular and respiratory morbidity in individuals with impaired FEV1 (PURE): an international, community-based cohort study. Lancet Glob Health 2019;7:e613-23. 10.1016/S2214-109X(19)30070-1. [DOI] [PubMed] [Google Scholar]
- 50. Vasan RS. High blood pressure in young adulthood and risk of premature cardiovascular disease: calibrating treatment benefits to potential harm. JAMA 2018;320:1760-3. 10.1001/jama.2018.16068. [DOI] [PubMed] [Google Scholar]
- 51. Franklin SS, Gustin W, 4th, Wong ND, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation 1997;96:308-15. 10.1161/01.cir.96.1.308. [DOI] [PubMed] [Google Scholar]
- 52. Vishram JK, Borglykke A, Andreasen AH, et al. MORGAM Project Do other cardiovascular risk factors influence the impact of age on the association between blood pressure and mortality? The MORGAM Project. J Hypertens 2014;32:1025-33. 10.1097/HJH.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 53. McEvoy JW, Daya N, Rahman F, et al. Association of isolated diastolic hypertension as defined by the 2017 ACC/AHA blood pressure guideline with incident cardiovascular outcomes. JAMA 2020;323:329-38. 10.1001/jama.2019.21402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lamprea-Montealegre JA, Zelnick LR, Hall YN, Bansal N, de Boer IH. Prevalence of hypertension and cardiovascular risk according to blood pressure thresholds used for diagnosis. Hypertension 2018;72:602-9. 10.1161/HYPERTENSIONAHA.118.11609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lee CJ, Ryu J, Kim HC, et al. Clinical benefit of treatment of stage-1, low-risk hypertension. Hypertension 2018;72:1285-93. 10.1161/HYPERTENSIONAHA.118.11787. [DOI] [PubMed] [Google Scholar]
- 56. Koskinen JS, Kytö V, Juonala M, et al. Childhood risk factors and carotid atherosclerotic plaque in adulthood: The Cardiovascular Risk in Young Finns Study. Atherosclerosis 2020;293:18-25. 10.1016/j.atherosclerosis.2019.11.029. [DOI] [PubMed] [Google Scholar]
- 57. Nardin C, Maki-Petaja KM, Miles KL, et al. Enigma Study Investigators Cardiovascular phenotype of elevated blood pressure differs markedly between young males and females: the Enigma Study. Hypertension 2018;72:1277-84. 10.1161/HYPERTENSIONAHA.118.11975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Zheng W, Mu J, Chu C, et al. Association of blood pressure trajectories in early life with subclinical renal damage in middle age. J Am Soc Nephrol 2018;29:2835-46. 10.1681/ASN.2018030263. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary appendix 1
Web appendix: Supplementary appendix 2
Web appendix: Supplementary appendix 3
Web appendix: Supplementary appendix 4