Abstract
Brugada phenocopies are interesting clinical entities with electrocardiographic (ECG) patterns indistinguishable from the inherited Brugada syndrome. In patients with Brugada phenocopies, these ECG patterns are expected to resolve with resolution of the underlying condition.
Keywords: brugada syndrome, brugada phenocopy, brugada pattern, pericarditis
Introduction
Brugada syndrome is an inherited cardiac channelopathy associated with a high risk of syncope and sudden cardiac death due to serious heart arrhythmias [1]. Patients with Brugada syndrome have characteristic electrocardiographic (ECG) patterns in the right precordial leads [1,2]. However, similar ECG patterns have been reported in a variety of other conditions, known as Brugada phenocopies, despite a lack of underlying genetic defects [2,3]. In Brugada phenocopies, the Brugada ECG pattern is expected to disappear within a few days of withdrawal of the provoking factor.
We report a case of a patient with acute pericarditis who developed a Brugada ECG pattern that completely resolved with the treatment of the underlying pericarditis.
Case presentation
A 35-year-old male patient without a significant medical history presented with substernal chest pain of one-day duration. The patient described his substernal chest pain as radiating to his back and worsening with inspiration and leaning forward. His history was remarkable for having a cold two weeks prior to his presentation.
Upon arrival to the hospital, his vital signs were unremarkable. Laboratory investigations showed normal while blood counts, normal lipid profile, and normal hemoglobin A1c. A chest X-ray didn’t show any evidence of pneumonia. A chest CT angiography was negative for pulmonary embolus or aortic dissection.
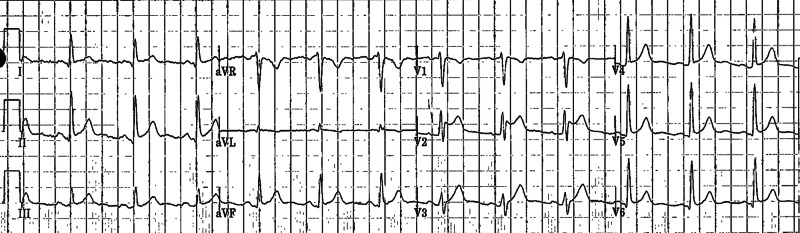
Two assays of troponin were performed six hours apart and were negative. His ECG showed diffuse ST-PR discordance, which was highly concerning of pericarditis, along with type II Brugada pattern, which manifested in lead V2 as a saddle-back pattern with at least 2-mm J-point elevation and at least 1-mm ST elevation with a positive T-wave (Figure 1). An echocardiogram was performed and showed normal left ventricular ejection fraction of 55% without regional wall motion abnormality or pericardial effusion.
Figure 1. ECG on presentation.
ECG showing diffuse ST-PR discordance secondary to acute pericarditis along with type II Brugada pattern, which manifested in lead V2 as a saddle-back pattern with at least 2-mm J-point elevation and at least 1-mm ST elevation with a positive T–wave
ECG, electrocardiogram
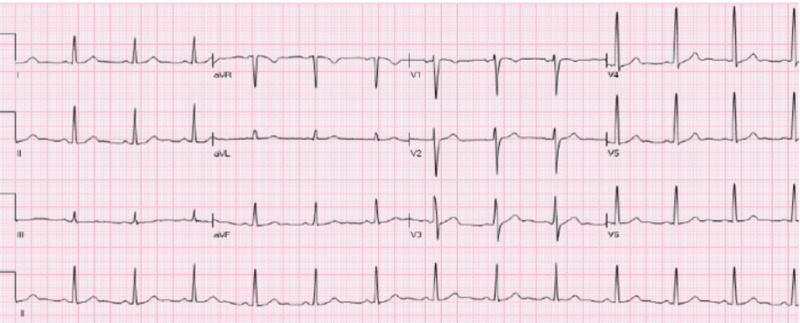
Given the history, clinical picture, and lack of family history of arrhythmias or sudden cardiac death, his ECG features in lead V2 were interpreted as Brugada phenocopy rather than Brugada syndrome. The patient was treated as a case of post-viral pericarditis. He was started on nonsteroidal anti-inflammatory drugs and colchicine, which lead to significant improvement in his symptoms and complete resolution of ECG features within two weeks (Figure 2) (Poster: Malik Shehadeh, John Costello, Vijaywant Brar, Susan O'Donoghue. Acute Pericarditis Mimicking Brugada Syndrome. Society of General Internal Medicine, May 2020, Birmingham, AL, USA).
Figure 2. ECG after two weeks of treatment.
Complete resolution of the type II Brugada pattern was noticed with resolving pericarditis after two weeks of treatment.
ECG, electrocardiogram
Discussion
Brugada syndrome is an autosomal dominant genetic disorder with incomplete penetrance characterized by disturbances affecting the electrical activity within the heart. Patients with Brugada syndrome might experience syncope or sudden cardiac death due to serious abnormal heart rhythms such as ventricular fibrillation. Genetic analysis revealed that most of the causative mutations involve the cardiac sodium channel genes [1,4]. More than 100 mutations have been described so far in the literature [1]. The relationship between the sodium channel abnormalities and characteristic ECG patterns seen in the right precordial leads in patients with Brugada syndrome is not fully understood.
The ECG features for patients with Brugada syndrome can be divided into two distinct patterns: one with a coved-type ST segment elevation (type I Brugada pattern) and the other one with a saddle-back ST segment elevation (type II Brugada pattern).
Diagnosis of Brugada syndrome requires a characteristic type I Brugada pattern and clinical findings (i.e., arrhythmia, syncope, sudden cardiac death). However, some patients may be diagnosed based on relevant family history of sudden cardiac death or coved-type ECGs in family members. In patients with type II Brugada pattern, diagnosis is considered positive when conversion to the diagnostic type I Brugada pattern occurs after a sodium channel blocker drug challenge test [1-3]. Once diagnosis is made, these patients will need follow-up on a regular basis and family screening in first-degree relatives, and might benefit from an implantable cardioverter-defibrillator (ICD) placement.
The term “Brugada phenocopy” is proposed to describe clinical conditions with Brugada ECG patterns in patients without underlying genetic defect or family history of sudden cardiac death. There are hundreds of published cases of Brugada phenocopies due to various clinical conditions such as metabolic derangements, myocardial ischemia, infiltrative cardiomyopathy, pericardial disease, mechanical mediastinal compression, and pulmonary embolism [3]. Aiming the clarification of this topic, the International Registry of Brugada phenocopies maintains an online database for the documentation of these patients. It is crucial to recognize that in all these clinical entities, the Brugada ECG patterns are expected to resolve with resolution of the underlying condition [3].
Only five cases of pericarditis-induced Brugada phenocopy have been reported in the literature [5-8]. Three of these cases presented with type II Brugada pattern and the other two presented with type I Brugada pattern (Table 1). In all these patients, the ECG patterns completely resolved with resolution of underlying pericarditis.
Table 1. Reported cases of pericarditis-induced Brugada phenocopy in the literature.
We reported the sixth case of acute pericarditis-induced Brugada phenocopy. Our patient presented with Brugada-type II pattern and his ECG features resolved completely with resolution of underlying pericarditis.
Conclusions
Acute pericarditis may mimic Brugada syndrome. The ECG patterns of Brugada syndrome shouldn’t be considered as a specific marker of the syndrome but rather as a sign of electrical heart disease that can be due to various other conditions. To make a definitive diagnosis in patients with a high clinical pretest probability of Brugada syndrome, further workup such as drug challenge with sodium channel blocker and genetic analysis might be required.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Brugada syndrome 2012. Berne P, Brugada J. Circ J. 2012;76:1563–1571. doi: 10.1253/circj.cj-12-0717. [DOI] [PubMed] [Google Scholar]
- 2.Proposed diagnostic criteria for the Brugada syndrome: consensus report. Wilde AA, Antzelevitch C, Borggrefe M, et al. Circulation. 2002;106:2514–2519. doi: 10.1161/01.cir.0000034169.45752.4a. [DOI] [PubMed] [Google Scholar]
- 3.Brugada phenocopy: a new electrocardiogram phenomenon. Anselm DD, Evans JM, Baranchuk A. World J Cardiol. 2014;6:81–86. doi: 10.4330/wjc.v6.i3.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.An international compendium of mutations in the SCN5A-encoded cardiac sodium channel in patients referred for Brugada syndrome genetic testing. Kapplinger JD, Tester DJ, Alders M, et al. Heart Rhythm. 2010;7:33–46. doi: 10.1016/j.hrthm.2009.09.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brugada-like early repolarisation pattern associated with acute pericarditis. Ozeke O, Selcuk MT, Topaloglu S, Maden O, Aras D. Emerg Med J. 2006;23:64. doi: 10.1136/emj.2006.040634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drug-induced pericarditis mimicking Brugada syndrome. Hermida JS, Six I, Jarry G. Europace. 2007;9:66–68. doi: 10.1093/europace/eul140. [DOI] [PubMed] [Google Scholar]
- 7.Pericarditis mimicking Brugada syndrome. Monti M, Olivi G, Francavilla F, Borgognoni F. Am J Emerg Med. 2017;35:669. doi: 10.1016/j.ajem.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Type 1 Brugada phenocopy in a patient with acute pericarditis. Yu M, Zhang Q, Huang X, Zhao X. J Electrocardiol. 2018;51:1121–1123. doi: 10.1016/j.jelectrocard.2018.10.087. [DOI] [PubMed] [Google Scholar]