Abstract
A first episode of psychosis (FEP) can derail a patient’s educational goals, including attainment of a college education, and this can have lasting ramifications for socioeconomic and health outcomes. Despite this, few studies have examined return to college, which is an important index of real-world educational success after a FEP. In this study, we conducted a longitudinal medical record review of patients in a transdiagnostic outpatient FEP program and performed survival analysis, setting return to college as the endpoint, among the subset of patients whose college education was interrupted. We found that 82% (93/114) of college-enrolled FEP individuals experienced disruptions to their education after FEP, but that return to college also occurred in a substantial proportion (49/88, 56%) among those on leave who had follow-up data. In this sample, the median time to college return was 18 months. When separated by baseline diagnostic category, FEP patients with affective psychotic disorders (FEAP, n = 45) showed faster time to college return than those with primary psychotic disorders (FEPP, n = 43) (median 12 vs 24 mo; P = .024, unadjusted). When adjusted for having no more than 1 psychiatric hospitalization at intake and absence of cannabis use in the 6 months prior to intake (which were also significant predictors), differences by diagnostic category were more significant (hazard ratio 2.66, 95% CI 1.43–4.94, P = .002). Participation in education is an important outcome for stakeholders, and students with FEP can be successful in accomplishing this goal.
Keywords: schizophrenia, bipolar disorder, college reintegration, educational attainment, functional outcomes, recovery
Introduction
The first episode of psychosis (FEP) most commonly strikes during late adolescence or early adulthood,1,2 when young people are striving to establish identity and independence amid ongoing brain development3 and role and relational instability.4,5 The experience of new-onset psychotic symptoms such as hallucinations, delusions, and disordered thinking can be traumatic and disruptive in themselves.6–9 However, FEP often has far wider impact, disrupting multiple functional domains, including work, school, and interpersonal relationships.10 Such functional impairments during this transitional period can derail a young person’s attainment of his or her educational, career, and relational goals, leading to substantial personal costs,11,12 as well as high societal costs associated with lost productivity and potential.13,14
In industrialized societies, going to college (“college” in this paper refers to all postsecondary education—eg, community college, liberal arts college, or university—excluding graduate school) frequently marks an important developmental milestone in the transition to young adulthood. According to US Census Bureau data, the percentage of Americans who enroll in college after high school underwent a steady rise—from 14% in 19404 to 60% in 199015 and further to 70% in 200915—with the increase fueled in large part by the college-for-all ideal widely held in the United States.16 Rates have remained fairly stable in the past decade, with 69% of high school completers enrolling in college in 2018.17 A college education is considered to build human capital by providing knowledge, teaching critical thinking and problem-solving skills, providing socialization in the values and behaviors necessary for achievement, and widening access to diverse career and other opportunities.18 In addition, college promotes greater independence and self-direction compared to high school, providing opportunities for social and emotional growth.
Critically, the gains made during the college years can have enduring and potentially lifelong ramifications,19,20 as the level of education an individual attains lays the foundation for subsequent experiences. For one, education is a strong determinant of income and occupational achievements.21 While college is not the sole path to a desirable career and may not be appropriate for all high school graduates,16,22,23 there is evidence that average annual earnings increase with each educational level, and earnings differences by educational attainment compound over a lifetime.19 Improving school completion rates is also a matter of public health, as educational attainment is highly predictive of health outcomes18 and explains some of the health disparities prevalent in American society.24 In the United States, individuals with higher education have significantly lower mortality25–31 and better outcomes in a variety of health measures24,32 than those with lower educational levels.
Despite the public health and socioeconomic implications of higher education, few studies have examined return to college among young people after a FEP. There have been studies on educational attainment,11,12,33–36 rates of participation in or completion of postsecondary education,37–39 factors associated with school dropout,40 barriers to higher education,41–43 and barriers to utilization of campus disability services44–46 among individuals with psychiatric disabilities, as well as studies exploring the experiences of college students with mental illness47 including psychotic disorders.37,48–50 Recent studies also examined the prevalence and distribution of mental disorders among college students worldwide.51–53 However, the literature on the rates of college return or reintegration after a FEP is sparse. Zafran and colleagues reported on academic reintegration after a FEP, but this was a qualitative pilot study with only 5 patients,50 and investigation in a larger sample would provide greater insights about the rate and time course of return to college after a FEP as well as factors that facilitate or hinder return. Cognitive functioning in early psychosis has also been extensively investigated. However, cognitive capacity is not the only determinant of educational success.48,54 Though cognitive performance accounts for 23%–42% of the genetic contribution to educational attainment,55 genetic factors associated with traits other than intelligence, such as openness to experience55 and self-efficacy,56 also influence educational attainment. Importantly, educational attainment—more than performance on cognitive tests within a controlled setting—is the real-world outcome of greater interest for patients and their families.
In this study, we investigated the rates of successful return to college among patients in the McLean OnTrack outpatient FEP program (located at McLean Hospital in Belmont, MA, and henceforth abbreviated as OnTrack) and the factors that predict successful college return. Functional trajectories have historically been used to differentiate affective psychotic disorders, such as bipolar disorder (BP), from schizophrenia and other primary psychotic disorders.57 However, a growing body of evidence suggests that the clinical course of affective psychotic disorders is often cumulative and potentially deteriorating.58–60 As such, OnTrack takes a transdiagnostic approach to treating FEP. Yet, it remains unclear how patients with first-episode affective psychotic disorders (FEAP) compare to patients with first-episode primary psychotic disorders (FEPP) with respect to college-related outcomes. Cognitive deficits have been found in both FEPP and FEAP, but they typically emerge earlier, prior to illness onset, and are more severe in schizophrenia than BP.61–63 Given these differences in cognitive profiles, poorer college participation and performance might be expected in FEPP relative to FEAP. However, educational attainment in BP appears to be more complex, with studies discrepant on whether individuals with BP are at higher33,38 or lower risk36 of terminating education prior to college graduation relative to their healthy peers. More generally, the current literature on outcomes in FEP shows highly heterogenous patterns of recovery,64,65 and it is difficult to accurately predict which FEP patients are likely to do well with college reintegration. Therefore, we examined whether having a FEPP vs a FEAP diagnosis, along with other predictors, differentially impact the time to college return after FEP.
Methods
Medical Record Review
We conducted a medical record review of all patients (n = 219) admitted to McLean OnTrack during the program’s first 5.5 years. OnTrack treats young adults ages 18–30 years who have experienced a FEP, estimated by symptom onset, within the prior 12 months.66 OnTrack employs a multidisciplinary team-based model, integrating psychotherapy, recreational and process groups, peer support, family therapy/support, psychopharmacologic treatment, and case management. While OnTrack provides support toward the attainment of educational and other functional goals, the clinical team did not include licensed vocational counselors or supported education programs during the study period. As investigating the effect of specialized FEP care in OnTrack was not this study’s aim, we did not include a comparison group of FEP patients in standard, community care.
We extracted data from patients who entered OnTrack between May 3, 2012 (intake date of first patient) and October 1, 2017, following them through April 1, 2018 (6 mo after the cutoff date for study inclusion). We set the date of the intake evaluation date as the survival start time and extracted data about baseline characteristics from that visit. Using subsequent psychotherapy and psychopharmacology progress notes, we also extracted data for every 6-month period following intake (ie, 6, 12, 18, mo, etc.; see supplementary material for data dictionary.) We selected 6-month periods because most patients receiving treatment in OnTrack will have been seen at least once in a 6-month period, and we felt that 6-month intervals would capture the event of interest (return to college) for all students whether specific colleges adhered to a quarter or semester academic calendar. The duration of treatment in OnTrack over the study period ranged from <6 months to >60 months with a median of 18.2 (mean 22.4, SD 17.7 for n = 219).
Outpatient notes at McLean Hospital were written and maintained in paper charts until the hospital transitioned to the Meditech electronic health records system in October 2014 and then to EPIC in July 2017. We used all available sources of medical information, not just electronic health records. To ensure consistency and reliability, all record reviews were completed by P.B.C., a senior psychiatry resident under the supervision of a licensed and board-certified psychiatrist and researcher who specializes in psychosis (A.K.S.). All data were entered and managed in a database we custom-designed for this study using Research Electronic Data Capture (REDCap) tools67 hosted at Partners HealthCare. This study was approved by the Partners HealthCare Institutional Review Board, which granted a waiver of consent, given this research involved only health record review and no direct contact with study subjects.
Data Analysis
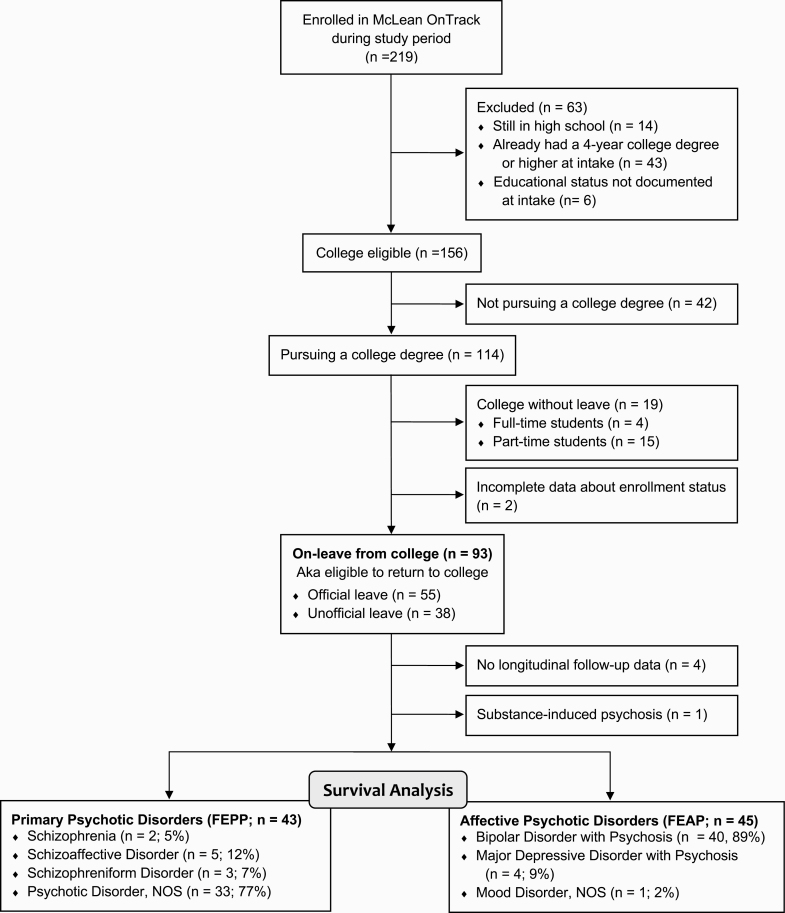
All analyses were performed in Stata version 15.1. Of the 219 patients on whom we conducted a medical record review, we performed survival analyses on the subset of 88 FEP individuals with a primary psychotic disorder (FEPP, n = 43) or affective psychotic disorder (FEAP, n = 45) who had their college experience interrupted by a leave of absence and for whom we had longitudinal data (ie, did not disengage from treatment immediately after the intake appointment). See figure 1 for reasons patients were excluded from analyses. The median duration of treatment in OnTrack for these 88 patients was 21.3 (mean 23.3, SD 16.1, range 0.23–60.7) months. Patients were categorized as FEPP if, at intake, they were given a primary psychiatric diagnosis of schizophrenia, schizoaffective disorder, schizophreniform disorder, or psychotic disorder not otherwise specified (NOS), and categorized as FEAP for BP, major depressive disorder, or mood disorder NOS, all with psychotic features. We compared the 43 FEPP and 45 FEAP eligible-to-return groups with respect to baseline demographic and clinical characteristics using t-tests for continuous variables and chi-square tests for categorical variables at a significance threshold of P < .05, 2-sided (table 1).
Fig. 1.
Flow diagram of patients.
Table 1.
Baseline Characteristics of First-Episode Primary Psychotic Disorder (FEPP) and First-Episode Affective Psychotic Disorder (FEAP) Patients With Longitudinal Data Who are Eligible to Return to College
| FEPP | FEAP | Statistic | P-value | |
|---|---|---|---|---|
| Sample size (N = 88) | n = 43 | n = 45 | ||
| Age, mean ± SD (range), y | 20.3 ± 1.8 (18–25) | 20.4 ± 1.9 (18–26) | t = −0.365 | .716 |
| Female, no. (%) | 9 (21%) | 12 (27%) | χ 2 = 0.398 | .528 |
| Race, no. (%) | χ 2 = 1.346 | .510 | ||
| White | 32 (74%) | 34 (76%) | ||
| Black | 3 (7%) | 1 (2%) | ||
| American Indian | 0 (0%) | 0 (0%) | ||
| Asian/Pacific Islander | 5 (12%) | 7 (16%) | ||
| Missing | 3 (7%) | 3 (7%) | ||
| Marital status, no. (%) | - | - | ||
| Never married | 43 (100%) | 44 (98%) | ||
| Married/sep/divorced | 0 (0%) | 0 (0%) | ||
| Missing | 0 (0%) | 1 (2%) | ||
| In a romantic relationship, no. (%) | 4 (9%) | 9 (20%) | χ 2 = 2.015 | .156 |
| Missing | 6 (14%) | 6 (13%) | ||
| Living at home with parents, no. (%) | 40 (93%) | 37 (82%) | χ 2 = 0.268 | .604 |
| Living with a roommate(s), no. (%) | 2 (5%) | 3 (7%) | ||
| Missing | 1 (2%) | 5 (11%) | ||
| Referral source, no. (%) | χ 2 = 1.678 | .795 | ||
| Inpatient hospital | 24 (56%) | 28 (62%) | ||
| Partial hospital | 9 (21%) | 7 (16%) | ||
| Outpatient provider | 5 (12%) | 3 (7%) | ||
| Family | 2 (2%) | 4 (9%) | ||
| Other | 1 (2%) | 1 (2%) | ||
| Missing | 2 (5%) | 2 (4%) | ||
| No. of prior hospitalizations, mean ± SD (range) | 1.5 ± 0.8 (0–4) | 1.6 ± 0.8 (0–3) | t = −0.517 | .606 |
| >1 hospitalization, no. (%) | 15 (35%) | 20 (44%) | χ 2 = 0.839 | .360 |
| Hospitalization at McLean prior to OnTrack, no. (%) | 27 (62.8%) | 29 (64.4%) | χ 2 = 0.025 | .875 |
| No. of prior suicide attempts, mean ± SD (range) | 0.14 ± 0.41 (0–2) | 0.16 ± 0.57 (0–3) | t = −0.183 | .855 |
| Suicide attempts, any lifetime, no. (%) | 5 (12%) | 4 (9%) | χ 2 = 0.180 | .672 |
| Suicide attempts, prior 6 mo, no. (%) | 3 (7%) | 3 (7%) | χ 2 = 0.003 | .954 |
| No. of antipsychotic medication trials, mean ± SD | 1.9 ± 1.0 (1–5) | 1.7 ± 1.1 (1–6) | t = 0.684 | .496 |
| >1 antipsychotic medication trial, no. (%) | 22 (51%) | 20 (44%) | χ 2 = 0.447 | .504 |
| Missing | 3 (7%) | 3 (7%) | ||
| Co-occurring psychiatric disorders, any, no. (%) | 19 (44%) | 11 (24%) | χ 2 = 3.814 | .051 |
| Mood disorder, not otherwise specified | 1 (2%) | 0 (0%) | χ 2 = 1.059 | .304 |
| Attention deficit hyperactivity disorder | 4 (9%) | 2 (4%) | χ 2 = 0.817 | .366 |
| Substance use disorder | 14 (33%) | 8 (18%) | χ 2 = 2.562 | .109 |
| Generalized anxiety disorder | 0 (0%) | 0 (0%) | - | - |
| Panic disorder | 0 (0%) | 0 (0%) | - | - |
| Obsessive-compulsive disorder | 1 (2%) | 2 (4%) | χ 2 = 0.300 | .584 |
| Posttraumatic stress disorder | 1 (2%) | 0 (0%) | χ 2 = 1.059 | .304 |
| Eating disorder | 0 (0%) | 1 (2%) | χ 2 = 0.967 | .326 |
| Co-occurring medical disorders, any, no. (%) | 11 (26%) | 12 (27%) | χ 2 = 0.013 | .908 |
| Thyroid disorders | 1 (2%) | 1 (2%) | χ 2 = 0.001 | .974 |
| Obesity | 0 (0%) | 1 (2%) | χ 2 = 0.967 | .326 |
| Dyslipidemia | 1 (2%) | 0 (0%) | χ 2 = 1.059 | .304 |
| Head injury requiring medical eval/tx | 9 (21%) | 6 (13%) | χ 2 = 0.898 | .343 |
| Substance use, prior 6 mo, any, no. (%) | 25 (58%) | 34 (76%) | χ 2 = 3.287 | .070 |
| Cannabis use, prior 6 mo | 24 (56%) | 33 (73%) | χ 2 = 2.958 | .085 |
| Stimulant use, prior 6 mo | 2 (5%) | 2 (4%) | χ 2 = 0.002 | .963 |
| Cocaine use, prior 6 mo | 1 (2%) | 3 (7%) | χ 2 = 0.955 | .328 |
| Hallucinogen use, prior 6 mo | 8 (19%) | 4 (9%) | χ 2 = 1.763 | .184 |
| Opioid use, prior 6 mo | 0 (0%) | 0 (0%) | - | - |
| Inhalant use, prior 6 mo | 0 (0%) | 0 (0%) | - | - |
| PCP use, prior 6 mo | 0 (0%) | 0 (0%) | - | - |
| Missing | 2 (5%) | 2 (4%) | ||
| Lifetime history of substance use | 34 (79%) | 40 (89%) | χ 2 = 1.585 | .208 |
| Lifetime history of trauma, no. (%) | 10 (23%) | 15 (33%) | χ 2 = 1.274 | .259 |
| Physical abuse | 5 (12%) | 1 (2%) | χ 2 = 3.062 | .080 |
| Emotional abuse | 5 (12%) | 4 (9%) | χ 2 = 0.180 | .672 |
| Sexual abuse | 3 (7%) | 6 (13%) | χ 2 = 0.968 | .325 |
| Missing | 3 (7%) | 4 (9%) | ||
| FH of psychotic disorder in first degree relative | 2 (5%) | 6 (13%) | χ 2 = 1.649 | .199 |
| First degree relative with schizophrenia | 0 (0%) | 1 (2%) | χ 2 = 0.967 | .326 |
| First degree relative with bipolar disorder | 2 (5%) | 5 (11%) | χ 2 = 1.253 | .263 |
| FH of any psychiatric disorder in first deg. relative | 19 (44%) | 17 (38%) | χ 2 = 0.374 | .541 |
| FH of completed suicide | 5 (12%) | 7 (16%) | χ 2 = 0.288 | .591 |
| Any psychiatric symptoms at intake, no. (%) | 35 (81%) | 18 (40%) | χ 2 = 15.730 | <.0001 |
| Any psychotic symptoms at intake, no. (%) | 34 (79%) | 15 (33%) | χ 2 = 18.639 | <.0001 |
| Insight into mental illness at intake, no. (%) | 6 (14%) | 11 (24%) | χ 2 = 1.688 | .194 |
| Missing | 0 (0%) | 1 (2%) | ||
| Medication adherence, prior 6 mo | χ 2 = 0.447 | .800 | ||
| Adherent (>90%) | 18 (42%) | 24 (53%) | ||
| Inconsistent (10%–90%) | 3 (7%) | 6 (13%) | ||
| Nonadherence (<10%) | 3 (7%) | 4 (7%) | ||
| Missing | 19 (44%) | 12 (27%) |
Note: Values in bold signify p-values that meet the significance threshold of P < .05, 2-sided. Values in italics indicate the no. (%) of patients with missing data for the variable indicated.
To examine the time it takes for FEP patients to return to college, irrespective of baseline diagnosis, we plotted a single Kaplan-Meier curve for all 88 eligible-to-return patients, with return to college as the endpoint. This endpoint was met if an individual returned to college and did not fail or drop out of college within the same 6-month period. To answer the question of whether FEPP and FEAP patients differ in the time to college return after a FEP, we plotted separate Kaplan-Meier curves for FEPP and FEAP and conducted a log-rank test to test the null hypothesis that the survival curves of the 2 groups did not significantly differ.
Next, we constructed Cox proportional hazards models to estimate the hazard ratio of return to college associated with psychosis category at intake (FEPP vs FEAP), first unadjusted, then adjusted for other clinical and demographic variables. We developed our model using purposeful selection of variables.68,69 To preserve the sample size, we considered only variables available for 95% or more of our sample. We identified candidate covariates as variables with P < .25 on univariate tests of each covariate against the outcome of college return and added these to our model. We retained only variables that were significant at an alpha level of 0.10 or were confounders (their removal changed any parameter estimate by ≥20%). The variables meeting these criteria were: (1) no more than 1 hospitalization prior to intake and (2) no cannabis use in the 6 months prior to intake. After this process, we returned to the variables that did not meet the P < .25 cutoff during univariate testing and added each, one at a time, to the existing model with the goal to retain any that were significant or a confounder. No additional variables were retained during this step. We did not include psychiatric or psychotic symptoms at intake in our purposeful selection process, as we considered these to be intermediary variables that might explain some of the relationship between psychosis category and college return. We assessed proportional hazards with Schoenfeld residual tests and found no evidence of a departure from proportional hazards for any of the variables in the final model or for the global test. We used Efron’s method for handling ties. We report the Wald P-value for each predictor of interest.
Students with psychiatric difficulties may be less likely to persist in school once they return. To address the issue of persistence in college, we reran analyses (ie, log-rank test, unadjusted Cox model, and the final adjusted model) after setting the endpoint as return to college with no subsequent failure or dropout. We also estimated the duration in college while in OnTrack, defined as the time between college return and either college graduation, failure or dropout from college, or termination from OnTrack. As we could not extract the exact date of college return from the medical records, we estimated the duration in college while in OnTrack in 6-month time units.
Finally, data extracted from records were limited to events that took place while patients received treatment in OnTrack. However, which patients disengage from treatment may not be random (eg, patients either doing very well or very poorly may be disproportionately represented among those who disengage early). To assess if early terminators differ from patients who stay in treatment, we compared these 2 groups with respect to baseline demographic and clinical variables. As OnTrack was offered to patients as a 2-year or more program, we defined early terminators as those who ended their treatment in OnTrack prior to 2 years.
Results
FEP Patients on Leave From College
Of the 114 patients in OnTrack who were pursuing a college degree, 93 (81.5%) took a leave of absence due to FEP, as of the time of intake. Only 19 patients (16.7%)—4 (3.5%) full-time and 15 (13.2%) part-time students—continued their education without a leave.
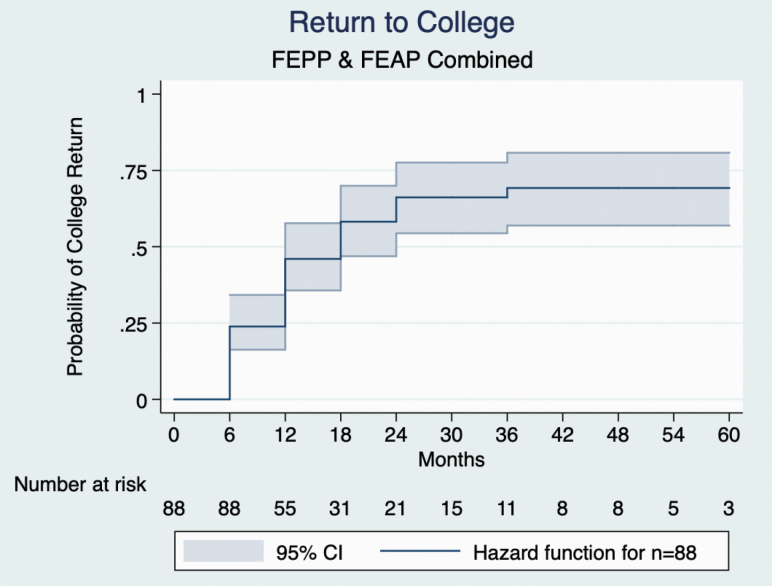
Survival Analysis: All FEP Patients on Leave
Of the 88 patients with FEAP or FEPP who were on leave and had follow-up data, 49 (55.7%) returned to college during the time they were in OnTrack (median 21.3, mean 23.3, SD 16.1 mo). The median time to college return for the group was 18 months (figure 2).
Fig. 2.
Kaplan-Meier curve for return to college for all first episode of psychosis (FEP) patients on leave (n = 88). A total of 46 patients (56%) returned to college while in OnTrack. The median time to college return was 18 months for the first-episode primary psychotic disorder (FEPP) and first-episode affective psychotic disorder (FEAP) combined.
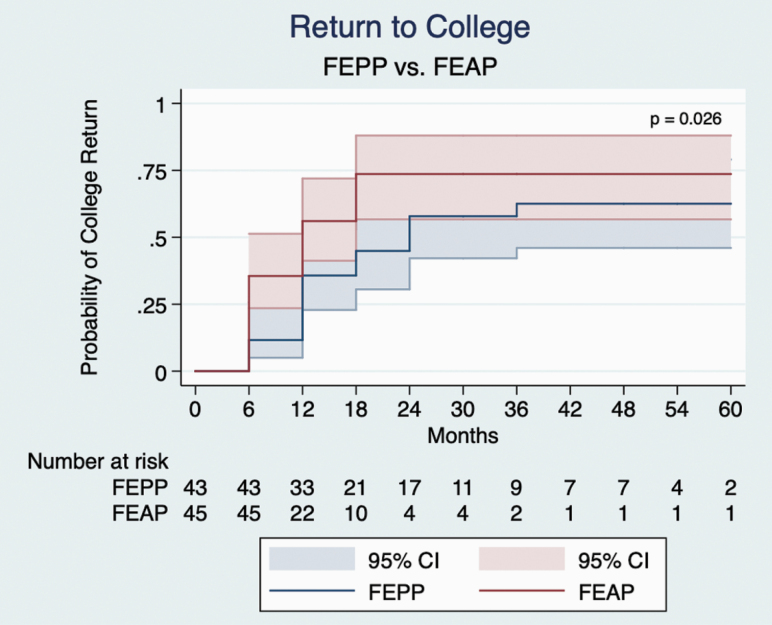
Survival Analysis: FEAP vs FEPP
Between-Group Differences in Baseline Characteristics.
The FEPP and FEAP patients differed significantly with respect to the presence of psychiatric symptoms, including psychotic symptoms, at intake, with fewer FEAP reporting symptoms (table 1). Trend-level differences (P = .051–.085) also existed in the proportion of patients with co-occurring psychiatric disorders, reporting cannabis use in the last 6 months, reporting any substance use in the last 6 months, and reporting a history of physical abuse. The 2 groups were comparable on all other baseline clinical and demographic characteristics.
Unadjusted Analyses.
The log-rank test showed a statistically significant difference between the 2 groups’ survival curves (P = .024) (figure 3). A higher overall proportion of FEAP patients (27/45, 60%) compared to FEPP patients (22/43, 51%) returned to college, and the FEAP curve was left-shifted, indicating that FEAP patients (median 12 mo) returned sooner than FEPP patients (median 24 mo). Similarly, unadjusted Cox hazard analysis using Efron’s method for ties showed FEAP with a higher hazard of college return than FEPP (hazard ratio [HR] 1.92, 95% CI 1.08–3.42, P = .026).
Fig. 3.
Kaplan-Meier curves for return to college by diagnostic group. The survival curves for the first-episode primary psychotic disorder (FEPP) and first-episode affective psychotic disorder (FEAP) were significantly different (log-rank test P = .024); more patients in the FEAP group (27/45, 60%) than the FEPP group (22/43, 51%) returned to college, and the median time to return was sooner in FEAP than FEPP (median 12 vs 24 mo).
Adjusted Hazard Analysis.
Using purposeful covariate selection, the variables we found to be significant covariates and/or confounders in addition to baseline diagnosis were: (1) no more than 1 psychiatric hospitalization prior to intake and (2) no cannabis use in the 6 months prior to intake. Adjusting for these covariates in our proportional hazards model, FEAP patients were 2.66 times more likely than FEPP patients to return to college (table 2).
Table 2.
Cox Proportional Hazards Modela for Return to College After a First Episode of Psychosis
| HR | SE | z-Statistic | P-value | 95% CI | |
|---|---|---|---|---|---|
| Affective psychotic disorder (FEAP) | 2.66 | 0.84 | 3.11 | .002 | 1.43–4.94 |
| Not more than 1 hospitalization | 2.16 | 0.68 | 2.44 | .015 | 1.16–4.00 |
| No cannabis use in the 6 mo prior to intake | 2.09 | 0.63 | 2.44 | .015 | 1.16–3.79 |
Note: HR, hazard ratio.
aUsing Efron’s method for handling ties.
Persistence in College
When we reran analyses using as our endpoint college return with no subsequent failures or dropouts, 46 (52.3%)—3 fewer patients—met the endpoint. The 3 patients who did not meet the more conservative endpoint consisted of 1 FEAP patient who returned to college at 12 months and dropped out at 24 months, 1 FEAP patient who returned at 18 months and dropped out at 24 months, and 1 FEPP patient who returned at 18 months and dropped out at 30 months. In addition, we identified 5 patients who made more than 1 attempt to return to college while in OnTrack (2 FEPP and 2 FEAP made 2 attempts, 1 FEAP made 3 attempts). Given that the final return attempt was the focus of this analysis, it was not surprising that the median time to return for the entire group became slightly longer, at 24 months (supplementary figure 1).
The log-rank test showed that more FEAP (25/45, 55.6%) than FEPP patients (21/43, 48.8%) returned to college without subsequent failures and that the median time to return was sooner in FEAP than FEPP patients (12 vs 24 mo) (P = .035) (supplementary figure 2). These results were similar to our original findings using return with no immediate failure or dropout within the same 6-month period as the outcome. The results of the unadjusted (HR 1.85, 95% CI 1.03–3.35, P = .040) and adjusted (HR 2.54, 95% CI 1.35–4.77, P = .004; supplementary table 1) Cox hazard analyses also did not substantially change from our original analyses.
When assessing duration in college while in OnTrack for all patients who returned to college (n = 49), we identified a total of 9 patients (all FEAP) who graduated from college after returning; all 9 graduated within the same 6-month period after their college return. For the remaining 40 patients, the median duration in college while in OnTrack was 12 (mean 12.9, SD 12.2, range 0–54) months (supplementary figure 3A for histogram). Of note, 8 patients ended treatment in OnTrack in the same 6-month period that they returned to college; excluding these individuals for n = 32, the median duration in college while in OnTrack was 12 (mean 16.1, SD 11.6, range 6–54). There was no significant difference in the proportion of patients in each 6-month time bin for college duration between the FEPP (n = 22) and FEAP (n = 18) patients who returned but had not graduated (χ 2 = 8.00, P = .333) (supplementary figure 3B).
Early Terminators (n = 41) vs Patients Treated ≥ 2 Years (n = 47)
Fewer early terminators had any co-occurring medical disorder (15% vs 36%; P = .022), and more early terminators used cannabis in the 6 months before intake (76% vs 55%; P = .047), compared to patients who stayed in treatment for ≥2 years. The 2 groups were otherwise comparable with respect to baseline clinical and demographic characteristics (supplementary table 2).
Exploration of Cognitive Functioning in a Limited Subset of Patients (n = 29)
Cognitive functioning can impact educational outcomes, even if cognitive capacity is not the only determinant of educational success. As such, we decided to conduct additional exploratory analysis to assess whether cognitive functioning could explain any of our findings. Because patients in OnTrack do not routinely undergo neuropsychological testing as part of their clinical care, systematic data on cognitive functioning were not available in the medical record for the vast majority of patients. However, patients in OnTrack had the opportunity to participate in a research study at McLean that aimed to collect clinical, cognitive, and multimodal neuroimaging measures in individuals with FEP. Cross-linking data from the FEP research study with patients in OnTrack, we found that cognitive measures collected using the MATRICS Cognitive Consensus Battery (MCCB)70 were available for 64 (29.2%) of all 219 OnTrack patients, and for 29 (33%) of the 88 patients in the survival analysis (who were eligible to return to college). Given the large number of patients with missing cognitive data, measures of cognitive functioning could not be included as covariates in the Cox proportional model. However, for the 29 patients for whom MCCB data were available, we explored whether there might be any differences in cognitive measures (ie, global cognition score as well as scores for the 7 cognitive domains assessed by the MCCB) by diagnostic group (n = 14 FEPP vs n = 15 FEAP), and also by whether patients did (n = 18) vs did not (n = 11) return to college during the study period (see supplementary material for details).
We found no differences between FEPP (n = 14) and FEAP (n = 15) in the global cognition (P = .594) or 7 domain scores (P = .113–.958) (supplementary table 3). We also found no differences in the global cognition (P = .857) or 7 domain scores (P = .525–.874) between the patients who did (n = 18) and did not (n = 11) return to college during the study period (supplementary table 4).
Discussion
Outcomes involving real-world functioning, such as engagement in work and school, may provide more meaningful indices of recovery than metrics focused solely on symptom severity. In this study, we conducted a longitudinal medical record review of all patients in a transdiagnostic outpatient FEP program. We found that the majority (81.5%) of individuals experienced disruptions to their college education due to FEP, but that return to college after a leave also occurred in substantial numbers. Within the subset of individuals whose college experience was disrupted, the median time to return to college was 18 months. Comparing individuals by baseline diagnostic category, we found that though a significant proportion of both FEPP (51%) and FEAP (60%) patients returned to college, there was a significant difference between the 2 groups’ survival curves, with time to college return being shorter in FEAP than in FEPP. Lastly, we found that in addition to having a FEAP diagnosis, having no cannabis use in the 6 months prior to intake and no more than 1 psychiatric hospitalization prior to intake increased the likelihood of returning to college after a FEP.
Research suggests that a college education can be more difficult for individuals with psychiatric disord-ers,11,33,38,41–43,51,53 and especially those with psychotic dis-rders,12,34,37,71,72 to attain. Young people with psychotic disorders participate in postsecondary education at much lower rates than their healthy peers,12,34,37 and those who do matriculate perform more poorly.37,39,49 For example, one study found that students with psychosis took more time-outs from school and longer to graduate compared to students with other psychiatric disorders, students with learning disorders, and students without disability.39 Reports of educational underachievement in students with psychotic disorders are unsurprising, as schizophrenia and related psychotic disorders are considered among the severest of mental illneses,73 and they are often preceded by a prodrome in which cognitive deficits are already present.74–76
On the other hand, it is now more possible for individuals with psychotic disorders to participate in higher education. US federal laws (ie, Section 504 of the Rehabilitation Act and the Americans with Disabilities Act, Amended Act [ADA-AA]) require colleges to ensure that students with psychiatric or other disabilities have equal access to academic programs.44,77 Treatments for mental illnesses have also resulted in individuals with psychotic disorders being less severely disabled by their illness.44,78–81 Importantly, while the expanded arsenal of antipsychotic and other psychotropic agents has given patients a way to alleviate symptoms, there is growing recognition that symptomatic recovery is distinct from functional recovery,82–84 and FEP programs have enhanced efforts to promote recovery of functioning as well as purpose and meaning in individuals with psychotic disorders.9,85 In this conceptualization of recovery,9,86–88 recovery is a journey toward attainment of meaningful goals and full human potential,89 not merely absence of symptoms. The role that education can play in developing human capital and in improving health is highly relevant within this framework, and consensus has been established that young people with psychosis should have the same educational opportunities as their nonpsychotic peers.90 Indeed, not only do many patients identify going back to school or getting more education as an important part of their recovery,50,91 education outranks symptomatic recovery among patient priorities.91
In our sample, 56% of FEP patients whose college education was interrupted returned to college while in OnTrack. That a considerable proportion of FEP individuals successfully return to college is consistent with literature pointing to the potential of some FEP patients to achieve successful educational outcomes.35,37,48,55 A study looking at the educational attainment of patients with psychotic disorders in relation to expected educational level as predicted by parental education found that, contrary to what the authors had hypothesized, patients with psychotic disorders had a higher level of education than their parents, even if the intergenerational increase was smaller than that made by healthy individuals.35 Successful return to college is also consistent with the small but positive genetic correlation that has been reported between schizophrenia risk and educational attainment55 (though also see ref.92) as well as with the finding that polygenic risk scores for schizophrenia and BP predict creativity.93
Research has shown that to successfully participate in higher education, students with FEP might rely on different motivational factors, supports, and strategies for managing their time and effort relative to students without FEP.37,50 Indeed, though our ability to interpret the findings from our exploratory analysis of cognitive functioning is severely limited by the small number of patients for whom cognitive measures were available, the lack of detectable differences in cognition (among the limited subset who did have cognitive data) by diagnostic group as well as by whether patients did or did not return to college suggests that successful return to college is unlikely to be determined by cognitive functioning alone. Rather, as proposed by the bioecological framework for understanding college mental health, a host of both immediate and broader contextual factors across the college mental health ecosystem influence educational outcomes.54 Relevant to factors at the level of the individual student, a meta-synthesis of qualitative research exploring the experiences of students with mental illness has shown that beyond the capacity to do the academic work, factors such as knowing oneself, managing one’s mental illness, and the ability to negotiate the social space are key to postsecondary educational success.48 The importance of engaging factors beyond cognitive capacity is further underscored by the finding that genetic factors associated with traits such as openness to experience55 and self-efficacy56 also influence educational attainment. It is also worth pointing out that the time it took for patients in our sample to return to college extends the expected time for college completion beyond the traditional college trajectory. Adjusting expectations amongst individuals with FEP, their family, and colleges—ie, that undergraduate trajectories after a FEP may be longer but that students with FEP can be successful—is pertinent. We would particularly recommend to families to adjust expectations around the timing for school return, and to schools that flexible policies during this process is essential to foster success.
Diagnosis was the strongest factor in our model for predicting a successful return to college. That the FEAP group showed faster time to college return than FEPP patients (median 12 vs 24 mo) is consistent with a recent study that showed that individuals with BP are more likely to complete university than individuals with schizophrenia (and even healthy controls).36 At the same time, it is important to recognize that the path back to college for those with FEAP is also frequently challenging and nonlinear.33,38 Though cognitive deficits in BP are less severe than in schizophrenia and there is no strong evidence for premorbid cognitive and academic difficulties in BP (in contrast to schizophrenia), it is increasingly recognized that cognitive impairment is present in the FEP of both FEAP and FEPP.61–63 There is a clear need for both groups to receive specialized accommodations as they transition back to school.
Having no more than 1 psychiatric hospitalization was also significantly associated with successful college return. Repeated hospitalizations may be a marker for more severe illness, unremitted symptoms, poor illness insight, and/or treatment nonadherence, all of which predict poorer functional outcome.94–96 Patients with multiple hospitalizations may need extra support and guidance around optimal timing and resources when attempting to return to campus. Our findings also highlight the need for better relapse prevention, with patients, schools, treaters, and families ideally working collaboratively to prevent relapse before a situation escalates into a crisis. It is worth noting that hospitalizations can themselves disrupt educational timelines, especially as many colleges mandate that students take a leave of absence following psychiatric hospitalization.97 While a leave from school may be appropriate in some cases, blanket policies that force all students to take a leave of absence after hospitalization or a psychotic episode may not be universally helpful.
Finally, return to college was also predicted by the absence of cannabis use in the 6 months prior to intake. The transition to college is a peak risk period for cannabis use, with peer influence being a potent predictor.98 Cannabis use among college students, even in nonpsychotic samples, is associated with a lower grade point average and higher risks of discontinuous enrollment and delayed graduation.99–102 Abundant evidence also points to the detrimental effects of cannabis on psychosis and psychosis risk, particularly during the critical period of adolescence, and especially among those with increased susceptibility to psychosis.103 These psychosis-related risks may be exacerbated with increasingly wider exposure (through the legalization of recreational cannabis in many states) and the increased availability of higher potency marijuana.104 Abstinence from cannabis is a potentially modifiable variable, and our findings suggest that FEP individuals who avoid cannabis are more likely to return to college.
Though OnTrack provides specialized treatment for FEP and general support toward the attainment of educational and vocational goals, the achievement of college return in our sample occurred in the absence of formal supported education services in OnTrack. Supported education is based on the principles of psychiatric rehabilitation and provides assistance, preparation, and supports to people with psychiatric disabilities who wish to pursue postsecondary education or training.105–107 Supported education and employment services are increasingly seen as critical components of coordinated specialty care programs for early psychosis, with evidence suggesting benefits for both educational and vocational outcomes when compared with standard care108–110 (though also see a systematic review111 which found benefits for employment but not education). Thus, we predict that college return rates in our sample might be even higher with supported education services. Unfortunately, despite the personal, public health, and socioeconomic importance of education and employment, neither supported education nor vocational counseling is currently reimbursed through third-party payers. Federal legislation enacted in 2014 provided funds to the Substance Abuse and Mental Health Services Administration (SAMHSA) to support the development of early psychosis treatment programs, including supported education and employment services, through mental health block grants.112 These grants have provided important stimulus and support for early psychosis programs across the United States. However, OnTrack has not been a recipient of this type of funding and thus has had to creatively utilize the resources already available, including asking clinicians to address the educational and vocational needs of patients while also providing psychotherapy, family support, and/or psychopharmacologic management. More recently, in 2018, OnTrack was fortunate to receive philanthropic funding to hire a certified peer specialist trained in the Individual Placement and Support (IPS) vocational model. OnTrack has also benefited from a weekly “jobs club” group run by a vocational specialist who works at an affiliated clubhouse program at McLean. In spite of these developments since the study period, there still remains a gap with respect to supported education in OnTrack. We believe that the experience of OnTrack highlights some of the practical and financial challenges faced by many early psychosis programs, even those like OnTrack that are embedded within academically affiliated private psychiatric hospitals.
Our findings should be considered in the context of several limitations. First, the sample of 88 patients included in our survival analysis is modest. Second, our study included limited data on cognitive impairments and no data on premorbid functioning. We were able to access systematic data about cognitive functioning through data sharing with another FEP research study. However, as only a third of the sample in the survival analysis underwent cognitive testing through voluntary research participation, we were constrained to only group-wise comparisons, rather than including cognitive measures as covariates in our Cox model. Given that cognitive data were available for a limited subset of patients, the findings from our exploratory analysis of cognitive functioning should be interpreted with caution.
Third, with the exception of the cognitive measures which were collected through data sharing with another study, all data were extracted from chart reviews, and such data are restricted to what clinicians document in their notes. However, the clinicians in the specialized FEP care environment of OnTrack are highly attuned to the importance of functional recovery in preventing negative outcomes and more often provided ample documentation of events such as return to college in their notes. Fourth, data are limited to events that took place while patients were treated in OnTrack. If a disproportionate number of patients dropped out of care because they were doing well and returning to college, our findings could underestimate college return rates. Conversely, if patients tended to drop out because of more severe illness, we would risk overestimation. However, our supplementary analysis shows that FEP patients who terminated early were comparable to those who stayed ≥2 years on most baseline characteristics, suggesting non-informative censoring. More importantly, our data, derived from chart review, includes clinically rich longitudinal data from patients who have ever been seen in the clinic, and are thus free from bias related to including only individuals who are willing and able to sign informed consent.113,114 That cognitive measures, collected through voluntary participation in a FEP research study, were available for only a third of the patients in the analysis underscores the advantages of medical record review in capturing a more representative sample.
Finally, it could be argued that graduation from college might be a more valid measure of educational success than college return, as return to college does not guarantee a satisfactory grade point average or graduation. However, only 9 of the 49 patients who returned to college graduated during the study period. The median time to college return was 18 months, and the median duration in college among those who returned but had not yet graduated was 12 months. As a college education in the United States typically takes at least 4 years, the mean follow-up period of 22 months for patients in OnTrack is likely insufficient to capture graduation events. Though the number of graduation events in our sample was too small to meaningfully analyze time to graduation, to address the issue of persistence in college, we ran additional survival analyses using return to college with no subsequent failures or dropouts as the endpoint and found that the results did not substantially change from the original analyses which examined college return with no failure or dropout within the same 6-month period. Importantly, our study outcome of return to college is compatible with US federal laws pertaining to postsecondary educational settings (ie, ADA-AA), the goal of which is to provide students with equal access to academic programs.77 Not all the benefits of a college experience—eg, acquiring knowledge, practicing critical thinking and problem-solving skills, becoming acculturated to the values and behaviors necessary for achievement, and developing independence, among others—are contingent upon graduating, and returning to college represents more than just a step toward earning a degree. Participating in higher education facilitates the pursuit of personal development, career goals, and social inclusion.48,115 Moreover, returning to college has value in itself if it is a goal with personal meaning and purpose for a young person after a FEP.116
To conclude, the pursuit of higher education is well-aligned with the conceptualization of recovery as the attainment of meaningful goals and full human potential. Our findings indicate that interruption of college is very common after a FEP, but also provide evidence of the potential of both FEAP and FEPP patients for successful college return, albeit with longer trajectories than the conventional 4-year college timeline.
Supplementary Material
Acknowledgments
Special thanks to the clinical team at McLean OnTrack for their dedication to young people with first-episode psychosis. We thank Kathryn E. Lewandowski, PhD (as well as author Dost Öngür, MD, PhD) for sharing, and Andrea Wood, BA for assistance in compiling, the cognitive data we present in the supplementary materials. All authors have declared that there are no conflicts of interest in relation to the subject of this study. B.C.H. has received research support from Analysis Group, Verily Life Sciences, Novartis, Merck Serono, and Genzyme.
Funding
National Institutes of Health (P50MH115846 to D.O., A.K.S., and B.C.H.; K23MH100611 to A.K.S.; K08MH086846 and R01MH113858 to R.K.; R25MH094612 to P.B.C.).
References
- 1. Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20(4):359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McGorry PD, Purcell R, Goldstone S, Amminger GP. Age of onset and timing of treatment for mental and substance use disorders: implications for preventive intervention strategies and models of care. Curr Opin Psychiatry. 2011;24(4):301–306. [DOI] [PubMed] [Google Scholar]
- 3. Wilens TE, Rosenbaum JF. Transitional aged youth: a new frontier in child and adolescent psychiatry. J Am Acad Child Adolesc Psychiatry. 2013;52(9):887–890. [DOI] [PubMed] [Google Scholar]
- 4. Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 5. Arnett JJ, Žukauskienė R, Sugimura K. The new life stage of emerging adulthood at ages 18-29 years: implications for mental health. Lancet Psychiatry. 2014;1(7):569–576. [DOI] [PubMed] [Google Scholar]
- 6. Tarrier N, Khan S, Cater J, Picken A. The subjective consequences of suffering a first episode psychosis: trauma and suicide behaviour. Soc Psychiatry Psychiatr Epidemiol. 2007;42(1):29–35. [DOI] [PubMed] [Google Scholar]
- 7. Dunkley JE, Bates GW, Findlay BM. Understanding the trauma of first-episode psychosis. Early Interv Psychiatry. 2015;9(3):211–220. [DOI] [PubMed] [Google Scholar]
- 8. Rodrigues R, Anderson KK. The traumatic experience of first-episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2017;189:27–36. [DOI] [PubMed] [Google Scholar]
- 9. Wood L, Alsawy S. Recovery in psychosis from a service user perspective: a systematic review and thematic synthesis of current qualitative evidence. Community Ment Health J. 2018;54(6):793–804. [DOI] [PubMed] [Google Scholar]
- 10. Killackey E, Alvarez-Jimenez M, Allott K, Bendall S, McGorry P. Community rehabilitation and psychosocial interventions for psychotic disorders in youth. Child Adolesc Psychiatr Clin N Am. 2013;22(4):745–758. [DOI] [PubMed] [Google Scholar]
- 11. Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders, I: educational attainment. Am J Psychiatry. 1995;152(7):1026–1032. [DOI] [PubMed] [Google Scholar]
- 12. Isohanni I, Jones PB, Järvelin MR, et al. Educational consequences of mental disorders treated in hospital. A 31-year follow-up of the Northern Finland 1966 Birth Cohort. Psychol Med. 2001;31(2):339–349. [DOI] [PubMed] [Google Scholar]
- 13. Cloutier M, Aigbogun MS, Guerin A, et al. The Economic Burden of Schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77(6):764–771. [DOI] [PubMed] [Google Scholar]
- 14. Chong HY, Teoh SL, Wu DB, Kotirum S, Chiou CF, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:357–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kendig SM, Mattingly MJ, Bianchi SM. Childhood Poverty and the Transition to Adulthood. Fam Relat. 2014;63(2):271–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rosenbaum JE, Ahearn C, Becker K, Rosenbaum JE. The New Forgotten Half and Research Directions to Support Them. Washington, DC: William T. Grant Foundation; 2015. [Google Scholar]
- 17. National Center for Education Statistics. The Condition of Education in 2020: Immediate College Enrollment Rate.2020. https://nces.ed.gov/programs/coe/indicator_cpa.asp. Accessed May 21, 2020.
- 18. Ross CE, Mirowsky J. Refining the association between education and health: the effects of quantity, credential, and selectivity. Demography. 1999;36(4):445–460. [PubMed] [Google Scholar]
- 19. Day J, Newburger E. The Big Pay-off: Educational Attainment and Synthetic Estimates of Work-Life Earnings. Washington, DC: U.S. Department of Commerce, Economics, and Statistics. U.S. Census Bureau; 2002. [Google Scholar]
- 20. Halperin S. The Forgotten Half Revisited: American Youth and Young Families, 1988–2008. Washington, DC: American Youth Policy Forum; 1998. [Google Scholar]
- 21. Symonds WC, Schwartz R, Ferguson RF. Pathways to Prosperity: Meeting the Challenge of Preparing Young Americans for the 21st Century. Cambridge, MA: Pathways to Prosperity Project, Harvard University Graduate School of Education; 2011. [Google Scholar]
- 22. Boesel D, Fredland E. College for All? Is There Too Much Emphasis on Getting a 4-Year College Degree? Research Synthesis. Washington, DC: National Library of Education; 1999. [Google Scholar]
- 23. Rosenbaum JE, Stephan JL, Rosenbaum JE. Beyond one-size-fits-all college dreams: alternative pathways to desirable careers. American Educator. 2010;34(3):2–13. [Google Scholar]
- 24. Freudenberg N, Ruglis J. Reframing school dropout as a public health issue. Prev Chronic Dis. 2007;4(4):A107. [PMC free article] [PubMed] [Google Scholar]
- 25. Molla MT, Madans JH, Wagener DK. Differentials in adult mortality and activity limitation by years of education in the United States at the end of the 1990s. Population Devel Rev. 2004;30(4):625–646. [Google Scholar]
- 26. Rogers RG, Everett BG, Zajacova A, Hummer RA. Educational degrees and adult mortality risk in the United States. Biodemography Soc Biol. 2010;56(1):80–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Miech R, Pampel F, Kim J, Rogers RG. The enduring association between education and mortality: the role of widening and narrowing disparities. Am Sociol Rev. 2011;76(6):913–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Montez JK, Hummer RA, Hayward MD. Educational attainment and adult mortality in the United States: a systematic analysis of functional form. Demography. 2012;49(1):315–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hummer RA, Hernandez EM. The effect of educational attainment on adult mortality in the United States. Popul Bull. 2013;68(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- 30. Hayward MD, Hummer RA, Sasson I. Trends and group differences in the association between educational attainment and U.S. adult mortality: implications for understanding education’s causal influence. Soc Sci Med. 2015;127:8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lawrence EM, Rogers RG, Zajacova A. Educational attainment and mortality in the united states: effects of degrees, years of schooling, and certification. Popul Res Policy Rev. 2016;35(4):501–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82(6):816–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Breslau J, Lane M, Sampson N, Kessler RC. Mental disorders and subsequent educational attainment in a US national sample. J Psychiatr Res. 2008;42(9):708–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tempelaar WM, Termorshuizen F, MacCabe JH, Boks MP, Kahn RS. Educational achievement in psychiatric patients and their siblings: a register-based study in 30 000 individuals in The Netherlands. Psychol Med. 2017;47(4):776–784. [DOI] [PubMed] [Google Scholar]
- 35. Frissen A, Lieverse R, Marcelis M, Drukker M, Delespaul P; GROUP Investigators Psychotic disorder and educational achievement: a family-based analysis. Soc Psychiatry Psychiatr Epidemiol. 2015;50(10):1511–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vreeker A, Boks MP, Abramovic L, et al. ; GROUP Investigators High educational performance is a distinctive feature of bipolar disorder: a study on cognition in bipolar disorder, schizophrenia patients, relatives and controls. Psychol Med. 2016;46(4):807–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Roy L, Rousseau J, Fortier P, Mottard JP. Postsecondary academic achievement and first-episode psychosis: a mixed-methods study. Can J Occup Ther. 2016;83(1):42–52. [DOI] [PubMed] [Google Scholar]
- 38. Hunt J, Eisenberg D, Kilbourne AM. Consequences of receipt of a psychiatric diagnosis for completion of college. Psychiatr Serv. 2010;61(4):399–404. [DOI] [PubMed] [Google Scholar]
- 39. McEwan RC, Downie R. Patterns of academic success and engagement among college students with psychiatric disabilities. J College Stud Psychother. 2019;33(3):257–272. [Google Scholar]
- 40. Esch P, Bocquet V, Pull C, et al. The downward spiral of mental disorders and educational attainment: a systematic review on early school leaving. BMC Psychiatry. 2014;14:237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Megivern D, Pellerito S, Mowbray C. Barriers to higher education for individuals with psychiatric disabilities. Psychiatr Rehabil J. 2003;26(3):217–231. [DOI] [PubMed] [Google Scholar]
- 42. Atkinson S, Bramley C, Schneider J. Professionals’ perceptions of the obstacles to education for people using mental health services. Psychiatr Rehabil J. 2009;33(1):26–31. [DOI] [PubMed] [Google Scholar]
- 43. Annapally SR, Jagannathan A, Kishore T, Thirthalli J, Daliboina M, Channaveerachari NK. Barriers to academic reintegration in students with severe mental disorders: thematic analysis. Asian J Psychiatr. 2019;45:107–112. [DOI] [PubMed] [Google Scholar]
- 44. Collins ME, Mowbray CT. Understanding the policy context for supporting students with psychiatric disabilities in higher education. Community Ment Health J. 2005;41(4):431–450. [DOI] [PubMed] [Google Scholar]
- 45. Collins ME, Mowbray CT. Higher education and psychiatric disabilities: National Survey of Campus Disability Services. Am J Orthopsychiatry. 2005;75(2):304–315. [DOI] [PubMed] [Google Scholar]
- 46. Mowbray CT, Megivern D, Mandiberg JM, et al. Campus mental health services: recommendations for change. Am J Orthopsychiatry. 2006;76(2):226–237. [DOI] [PubMed] [Google Scholar]
- 47. Salzer MS. A comparative study of campus experiences of college students with mental illnesses versus a general college sample. J Am Coll Health. 2012;60(1):1–7. [DOI] [PubMed] [Google Scholar]
- 48. Ennals P, Fossey E, Howie L. Postsecondary study and mental ill-health: a meta-synthesis of qualitative research exploring students’ lived experiences. J Ment Health. 2015;24(2):111–119. [DOI] [PubMed] [Google Scholar]
- 49. Sung KM, Puskar KR. Schizophrenia in college students in Korea: a qualitative perspective. Perspect Psychiatr Care. 2006;42(1):21–32. [DOI] [PubMed] [Google Scholar]
- 50. Zafran H, Tallant B, Gelinas I. A first-person exploration of the experience of academic reintegration after first episode psychosis. Int J Psychosoc Rehabilitation. 2012;16(1):27–43. [Google Scholar]
- 51. Auerbach RP, Alonso J, Axinn WG, et al. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med. 2016;46(14):2955–2970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Auerbach RP, Mortier P, Bruffaerts R, et al. ; WHO WMH-ICS Collaborators WHO World Mental Health Surveys International College Student Project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bruffaerts R, Mortier P, Kiekens G, et al. Mental health problems in college freshmen: prevalence and academic functioning. J Affect Disord. 2018;225:97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pinder-Amaker S, Bell C. A bioecological systems approach for navigating the college mental health crisis. Harv Rev Psychiatry. 2012;20(4):174–188. [DOI] [PubMed] [Google Scholar]
- 55. Okbay A, Beauchamp JP, Fontana MA, et al. ; LifeLines Cohort Study Genome-wide association study identifies 74 loci associated with educational attainment. Nature. 2016;533(7604):539–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Krapohl E, Rimfeld K, Shakeshaft NG, et al. The high heritability of educational achievement reflects many genetically influenced traits, not just intelligence. Proc Natl Acad Sci U S A. 2014;111(42):15273–15278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kraepelin E. Clinical Psychiatry: A Text-Book for Students and Physicians. New York and London: Macmillan; 1902. [Google Scholar]
- 58. Berk M, Berk L, Dodd S, et al. Stage managing bipolar disorder. Bipolar Disord. 2014;16(5):471–477. [DOI] [PubMed] [Google Scholar]
- 59. Magalhães PV, Dodd S, Nierenberg AA, Berk M. Cumulative morbidity and prognostic staging of illness in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Aust N Z J Psychiatry. 2012;46(11):1058–1067. [DOI] [PubMed] [Google Scholar]
- 60. Berk M, Kapczinski F, Andreazza AC, et al. Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress and neurotrophic factors. Neurosci Biobehav Rev. 2011;35(3):804–817. [DOI] [PubMed] [Google Scholar]
- 61. Sheffield JM, Karcher NR, Barch DM. Cognitive deficits in psychotic disorders: a lifespan perspective. Neuropsychol Rev. 2018;28(4):509–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Van Rheenen TE, Lewandowski KE, Bauer IE, et al. Current understandings of the trajectory and emerging correlates of cognitive impairment in bipolar disorder: an overview of evidence. Bipolar Disord. 2020;22(1):13–27. [DOI] [PubMed] [Google Scholar]
- 63. Green MF. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry. 2006;67(suppl 9):3–8; discussion 36–42. [PubMed] [Google Scholar]
- 64. Hall MH, Holton KM, Öngür D, Montrose D, Keshavan MS. Longitudinal trajectory of early functional recovery in patients with first episode psychosis. Schizophr Res. 2019;209:234–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Ayesa-Arriola R, Pelayo Terán JM, Setién-Suero E, et al. Patterns of recovery course in early intervention for FIRST episode non-affective psychosis patients: the role of timing. Schizophr Res. 2019;209:245–254. [DOI] [PubMed] [Google Scholar]
- 66. Shinn AK, Bolton KW, Karmacharya R, et al. McLean OnTrack: a transdiagnostic program for early intervention in first-episode psychosis. Early Interv Psychiatry. 2017;11(1):83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Hosmer DW, Lemeshow S. Applied Logistic Regression. New York, NY: Wiley; 2000. [Google Scholar]
- 70. Nuechterlein KH, Green MF, Kern RS, et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165(2):203–213. [DOI] [PubMed] [Google Scholar]
- 71. Bowman S, McKinstry C, McGorry P. Youth mental ill health and secondary school completion in Australia: time to act. Early Interv Psychiatry. 2017;11(4):277–289. [DOI] [PubMed] [Google Scholar]
- 72. Christianson L. Improving functional outcomes in college and university students with schizophrenia in the Western world. J Am Coll Health. 2018;66(1):61–68. [DOI] [PubMed] [Google Scholar]
- 73. Gore FM, Bloem PJ, Patton GC, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet. 2011;377(9783):2093–2102. [DOI] [PubMed] [Google Scholar]
- 74. Osler M, Lawlor DA, Nordentoft M. Cognitive function in childhood and early adulthood and hospital admission for schizophrenia and bipolar disorders in Danish men born in 1953. Schizophr Res. 2007;92(1-3):132–141. [DOI] [PubMed] [Google Scholar]
- 75. Woodberry KA, Giuliano AJ, Seidman LJ. Premorbid IQ in schizophrenia: a meta-analytic review. Am J Psychiatry. 2008;165(5):579–587. [DOI] [PubMed] [Google Scholar]
- 76. Trotta A, Murray RM, MacCabe JH. Do premorbid and post-onset cognitive functioning differ between schizophrenia and bipolar disorder? A systematic review and meta-analysis. Psychol Med. 2015;45(2):381–394. [DOI] [PubMed] [Google Scholar]
- 77. Gotlib D, Saragoza P, Segal S, Goodman L, Schwartz V. Evaluation and Management of Mental Health Disability in Post-secondary Students. Curr Psychiatry Rep. 2019;21(6):43. [DOI] [PubMed] [Google Scholar]
- 78. Harding CM, Brooks GW, Ashikaga T, Strauss JS, Breier A. The Vermont longitudinal study of persons with severe mental illness, II: long-term outcome of subjects who retrospectively met DSM-III criteria for schizophrenia. Am J Psychiatry. 1987;144(6):727–735. [DOI] [PubMed] [Google Scholar]
- 79. Harrison G, Hopper K, Craig T, et al. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry. 2001;178:506–517. [DOI] [PubMed] [Google Scholar]
- 80. Harrow M, Grossman LS, Jobe TH, Herbener ES. Do patients with schizophrenia ever show periods of recovery? A 15-year multi-follow-up study. Schizophr Bull. 2005;31(3):723–734. [DOI] [PubMed] [Google Scholar]
- 81. Harrow M, Jobe TH. Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: a 15-year multifollow-up study. J Nerv Ment Dis. 2007;195(5):406–414. [DOI] [PubMed] [Google Scholar]
- 82. Wunderink L, Sytema S, Nienhuis FJ, Wiersma D. Clinical recovery in first-episode psychosis. Schizophr Bull. 2009;35(2):362–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Wunderink L, Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy: long-term follow-up of a 2-year randomized clinical trial. JAMA Psychiatry. 2013;70(9):913–920. [DOI] [PubMed] [Google Scholar]
- 84. Van Eck RM, Burger TJ, Vellinga A, Schirmbeck F, de Haan L. The relationship between clinical and personal recovery in patients with schizophrenia spectrum disorders: a systematic review and meta-analysis. Schizophr Bull. 2018;44(3):631–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Silverstein SM, Bellack AS. A scientific agenda for the concept of recovery as it applies to schizophrenia. Clin Psychol Rev. 2008;28(7):1108–1124. [DOI] [PubMed] [Google Scholar]
- 86. Deegan PE. Recovery: the lived experience of rehabilitation. Psychosocial Rehabilitation Journal. 1988;9(4):11–19. [Google Scholar]
- 87. Bellack AS. Scientific and consumer models of recovery in schizophrenia: concordance, contrasts, and implications. Schizophr Bull. 2006;32(3):432–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Law H, Morrison AP. Recovery in psychosis: a Delphi study with experts by experience. Schizophr Bull. 2014;40(6):1347–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Buckley PF, Fenley G, Mabe A, Peeples S. Recovery and schizophrenia. Clin Schizophr Relat Psychoses. 2007;1:96–100. [Google Scholar]
- 90. International First Episode Vocational Recovery G. Meaningful lives: supporting young people with psychosis in education, training and employment: an international consensus statement. Early Interv Psychiatry. 2010;4(4):323–326. [DOI] [PubMed] [Google Scholar]
- 91. Ramsay CE, Broussard B, Goulding SM, et al. Life and treatment goals of individuals hospitalized for first-episode nonaffective psychosis. Psychiatry Res. 2011;189(3):344–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Stefansson H, Meyer-Lindenberg A, Steinberg S, et al. CNVs conferring risk of autism or schizophrenia affect cognition in controls. Nature. 2014;505(7483):361–366. [DOI] [PubMed] [Google Scholar]
- 93. Power RA, Steinberg S, Bjornsdottir G, et al. Polygenic risk scores for schizophrenia and bipolar disorder predict creativity. Nat Neurosci. 2015;18(7):953–955. [DOI] [PubMed] [Google Scholar]
- 94. Bodén R, Sundström J, Lindström E, Lindström L. Association between symptomatic remission and functional outcome in first-episode schizophrenia. Schizophr Res. 2009;107(2-3):232–237. [DOI] [PubMed] [Google Scholar]
- 95. García-Cabeza I, Díaz-Caneja CM, Ovejero M, de Portugal E. Adherence, insight and disability in paranoid schizophrenia. Psychiatry Res. 2018;270:274–280. [DOI] [PubMed] [Google Scholar]
- 96. Haddad PM, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014;5:43–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Paul S. Appelbaum MD. Law & Psychiatry: “Depressed? Get Out!”: dealing with suicidal students on college campuses. Psychiatr Serv. 2006;57(7):914–916. [DOI] [PubMed] [Google Scholar]
- 98. Kirst M, Mecredy G, Borland T, Chaiton M. Predictors of substance use among young adults transitioning away from high school: a narrative review. Subst Use Misuse. 2014;49(13):1795–1807. [DOI] [PubMed] [Google Scholar]
- 99. Suerken CK, Reboussin BA, Egan KL, et al. Marijuana use trajectories and academic outcomes among college students. Drug Alcohol Depend. 2016;162:137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Bell R, Wechsler H, Johnston LD. Correlates of college student marijuana use: results of a US National Survey. Addiction. 1997;92(5):571–581. [PubMed] [Google Scholar]
- 101. Arria AM, Garnier-Dykstra LM, Caldeira KM, Vincent KB, Winick ER, O’Grady KE. Drug use patterns and continuous enrollment in college: results from a longitudinal study. J Stud Alcohol Drugs. 2013;74(1):71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Arria AM, Caldeira KM, Bugbee BA, Vincent KB, O’Grady KE. The academic consequences of marijuana use during college. Psychol Addict Behav. 2015;29(3): 564–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to Pot - A Review of the Association between Cannabis and Psychosis. Front Psychiatry. 2014;5:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Cascini F, Aiello C, Di Tanna G. Increasing delta-9-tetrahydrocannabinol (Δ-9-THC) content in herbal cannabis over time: systematic review and meta-analysis. Curr Drug Abuse Rev. 2012;5(1):32–40. [DOI] [PubMed] [Google Scholar]
- 105. Unger KV, Anthony WA, Sciarappa K, Rogers ES. A supported education program for young adults with long-term mental illness. Hosp Community Psychiatry. 1991;42(8):838–842. [DOI] [PubMed] [Google Scholar]
- 106. Mowbray CT, Collins M, Bybee D. Supported education for individuals with psychiatric disabilities: long-term outcomes from an experimental study. Social Work Research. 1999;23(2):89–100. [Google Scholar]
- 107. Mueser KT, Cook JA. Supported employment, supported education, and career development. Psychiatr Rehabil J. 2012;35(6):417–420. [DOI] [PubMed] [Google Scholar]
- 108. Rosenheck R, Mueser KT, Sint K, et al. Supported employment and education in comprehensive, integrated care for first episode psychosis: effects on work, school, and disability income. Schizophr Res. 2017;182:120–128. [DOI] [PubMed] [Google Scholar]
- 109. Humensky JL, Nossel I, Bello I, Dixon LB. supported education and employment services for young people with early psychosis in OnTrackNY. J Ment Health Policy Econ. 2019;22(3):95–108. [PMC free article] [PubMed] [Google Scholar]
- 110. Nuechterlein KH, Subotnik KL, Turner LR, Ventura J, Becker DR, Drake RE. Individual placement and support for individuals with recent-onset schizophrenia: integrating supported education and supported employment. Psychiatr Rehabil J. 2008;31(4):340–349. [DOI] [PubMed] [Google Scholar]
- 111. Bond GR, Drake RE, Luciano A. Employment and educational outcomes in early intervention programmes for early psychosis: a systematic review. Epidemiol Psychiatr Sci. 2015;24(5):446–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Heinssen RK, Goldstein AB, Azrin ST. Evidence-based treatments for first episode psychosis: components of coordiated specialty care.2014. https://www.nimh.nih.gov/health/topics/schizophrenia/raise/evidence-based-treatments-for-first-episode-psychosis-components-of-coordinated-specialty-care.shtml. Accessed May 20, 2020.
- 113. Kline E, Hendel V, Friedman-Yakoobian M, et al. A comparison of neurocognition and functioning in first episode psychosis populations: do research samples reflect the real world? Soc Psychiatry Psychiatr Epidemiol. 2019;54(3):291–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Shah JL, Peters MI. Early intervention in psychiatry: scotomas, representativeness, and the lens of clinical populations. Soc Psychiatry Psychiatr Epidemiol. 2019;54(9):1019–1021. [DOI] [PubMed] [Google Scholar]
- 115. Ennals P, Fossey EM, Harvey CA, Killackey E. Postsecondary education: kindling opportunities for people with mental illness. Asia Pac Psychiatry. 2014;6(2):115–119. [DOI] [PubMed] [Google Scholar]
- 116. Harvey PD, Bellack AS. Toward a terminology for functional recovery in schizophrenia: is functional remission a viable concept? Schizophr Bull. 2009;35(2):300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.