Abstract
Autism research is heavily skewed towards western high-income countries. Culturally appropriate screening and diagnostic instruments for autism are lacking in most low- and middle-income settings where the majority of the global autism population lives. To date, a clear overview of the possible cultural and contextual factors that may affect the process of identifying and diagnosing individuals with ASD is missing. This study aims to outline these factors by proposing a conceptual framework. A multidisciplinary review approach was applied to inform the development of the conceptual framework, combining a systematic review of the relevant autism research literature with a wider literature search spanning key texts in global mental health, cultural psychiatry, cross-cultural psychology and intellectual disability research. The resulting conceptual framework considers the identification, help-seeking and diagnostic process at four interrelated levels: i) the expression, ii) recognition, iii) interpretation and iv) reporting of autism symptoms, and describes the cultural and contextual factors associated with each of these levels, including cultural norms of typical and atypical behaviour, culture-specific approaches to parenting, mental health literacy, cultural beliefs, attitudes and stigma, as well as the affordability, availability, accessibility and acceptability of services. This framework, mapping out the cultural and contextual factors that can affect the identification, help-seeking and diagnosis of ASD, may function as a springboard for the development of culturally appropriate autism screening and diagnostic instruments, and inform future cross-cultural autism research directions. The framework also has relevance for clinicians and policy makers aiming to improve support for underserved autism populations worldwide.
Keywords: autism, culture, low-and middle-income countries, screening, diagnosis
Introduction
Autism research is heavily skewed towards western high-income countries (Abubakar, Ssewanyana, de Vries, & Newton, 2016; de Vries, P.J., 2016; Durkin et al., 2015; Elsabbagh et al., 2012; Hahler & Elsabbagh, 2014). Fewer than 20% of the global population lives in these high-income countries (Durkin et al., 2015; World Bank, 2015), but autism studies are almost exclusively based on this selected population (de Vries, 2016; Durkin et al., 2015). Moreover, even within high-income countries ethnic minorities are underrepresented in autism research (West et al., 2016). As a result of this global imbalance our knowledge of the symptom expression of Autism Spectrum Disorders (ASD), the screening and diagnostic instruments used to aid ASD identification and referral and the interventions developed to support people with ASD are likely to be culturally and contextually biased (Durkin et al., 2015; Freeth, Sheppard, Ramachandran, & Milne, 2013). Only recently the call for a more global perspective on ASD has become more prominent (de Vries, 2016; Durkin et al., 2015; Munir et al., 2016; Rice & Lee, 2017; World Health Organization, 2013).
A global perspective on ASD is of urgent importance as the vast majority of the world autistic population today is severely overlooked and neglected (de Vries, 2016; Durkin et al., 2015). In low- and middle- income countries (LMIC) most individuals with ASD remain undiagnosed and the vast majority has no access to evidence-based support or education (Kieling et al., 2011). Developmental difficulties can be detected earlier through developmental monitoring and strengthening of developmental surveillance systems, an approach supported by the World Health Organization (WHO, 2012). To monitor developmental concerns, or to more specifically screen for autism, the development of culturally appropriate surveillance, screening and diagnostic tools is vital. Late or no diagnosis disadvantages individuals with ASD in distinct cultural or socioeconomic settings, and bars them from effective early intervention or educational support (Bakare & Munir, 2011; Bello-Mojeed, Omigbodun, Bakare, & Adewuya, 2017; Montiel-Nava, Chacín, & González-Ávila, 2017; Ruparelia et al., 2016). Moreover, little is known about the cultural and contextual adaptations required to make interventions feasible, acceptable and effective across low-resource settings (Al Maskari, Melville, & Willis, 2018; Franz, Chambers, von Isenburg, & de Vries, 2017; Guler, de Vries, Seris, Shabalala, & Franz, 2017). In addition to benefitting populations from LMIC, a better understanding of the cultural and contextual dimensions of ASD may also inform strategies to better support underserved communities within high-income countries.
In response to the call for more global representation in ASD research, over recent years there have been several attempts to develop or adapt screening instruments for use in different cultural or socioeconomic settings, however not always with the desired outcome. Screening instruments adapted for use in Uganda (Kakooza-Mwesige, Ssebyala, Karamagi, Kiguli, & et. al., 2014), Sri Lanka (Perera, Wijewardena, & Aluthwelage, 2009) and Japan (Kamio et al., 2014) for instance, reported low sensitivity. Studies using the Modified Checklist for Autism in Toddlers (MCHAT) in low socioeconomic or ethnically diverse settings within the USA, reported high false positive rates (Khowaja, Hazzard, & Robins, 2015; Scarpa et al., 2013) or low specificity and low positive predictive values in children of colour and children from lower-income households (Guthrie et al., 2019). A study using the Autism Diagnostic Interview-Revised (ADI-R) reported lower sensitivity and specificity on specific domains in Spanish speaking populations in the USA (Vanegas, Magaña, Morales, & McNamara, 2016). Cultural and contextual factors likely contributed to these issues (Kakooza-Mwesige et al., 2014; Samadi & McConkey, 2015; Scarpa et al., 2013). Thus, a worldwide scarcity of validated and culturally appropriate screening and diagnostic tools still exists (Abubakar, Ssewanyana, de Vries, et al., 2016; Barbaro & Halder, 2016).
Several previous review studies have considered the cultural adaptation process and psychometric properties of screening instruments for ASD (Al Maskari et al., 2018; Marlow, Servili, & Tomlinson, 2019; Soto et al., 2015; Stewart & Lee, 2017). However, these studies primarily focussed on the methodological adaptation of the tools, with little consideration of the underlying cultural or socioeconomic factors that may have necessitated the adaptation (Al Maskari et al., 2018). To date, a structured overview of the cultural and contextual factors that may affect the identification and diagnosis of autism globally is lacking.
The aim of this paper is to identify the possible cultural and contextual factors that may influence the identification, help-seeking and diagnosis of ASD and to propose a conceptual framework that maps out these factors. It is hoped that this conceptual framework can foster future cross-cultural autism research and guide the development or adaptation of culturally and contextually appropriate autism screening and diagnostic tools.
Methods
Given that global cross-cultural autism research is still in its infancy, the approach of this review study is multidisciplinary. Rather than solely considering autism studies, we drew on sociocultural research studies examining a wide range of mental health conditions and typical and atypical child development that may be informative for the global autism research field. We brought together literature from the fields of ASD, intellectual disability, cultural psychiatry, cross-cultural psychology and global mental health research, focusing on cultural and socioeconomic factors that may affect the identification and diagnosis of ASD. We also considered conceptual and systematic review papers exploring barriers and facilitators to mental health help-seeking (Jacobs, Ir, Bigdeli, Annear, & Van Damme, 2012; Reardon et al., 2017) and cultural and contextual factors influencing psychiatric diagnoses (Rogler, 1993) and help-seeking (Cauce et al., 2002) to inform the development of our conceptual framework. By taking this approach, potentially relevant factors that have as yet been understudied in autism research could be highlighted. Thus, the aim of this study was to map out what cultural and contextual factors could be of potential relevance in identifying and diagnosing ASD, rather than review evidence from previous autism studies of what are already known to be important factors. Since the overall aim is to improve early diagnosis worldwide, our primary focus is on autism in children rather than adults; the important role parents can play as their child’s advocates is considered as well. Throughout the development of the framework the focus was on the journey of identification, help-seeking and diagnosis from the perspective of the individual and their family.
The multidisciplinary literature that is of potential relevance for this study is wide ranging and too extensive to approach systematically, therefore a narrative approach was used. Nevertheless, to get an impression of the available literature to date in the field of cross-cultural ASD research, a search was conducted in the databases Medline (Pubmed), PsycInfo and the Cochrane Library. The final complete search was performed on 28 August 2019. MesH search terms were used relating to culture (‘culture’, ‘ethnology’) and ASD (‘Autism’, ‘Autism Spectrum Disorder’, ‘Asperger Syndrome’, ‘Pervasive Development Disorder’). The search produced 1104 articles. After screening these articles on title and abstract and excluding articles that were unrelated to ASD or culture, 231 relevant articles were identified and reviewed. This body of literature was subsequently combined with the authors’ own databases of a wider literature beyond autism research, spanning key texts in global mental health, cross-cultural psychiatry, cross-cultural psychology and global intellectual disability research. A snowballing method (Greenhalgh & Peacock, 2005) was used, manually examining reference lists and citations of the identified articles. The systematic search of autism literature together with the wider search covering other disciplines encompassed more than 800 papers, which informed the development of our conceptual framework. No restrictions regarding year of publication were made. No limitations to the design of the research reviewed were set; both qualitative and quantitative studies were included.
Results
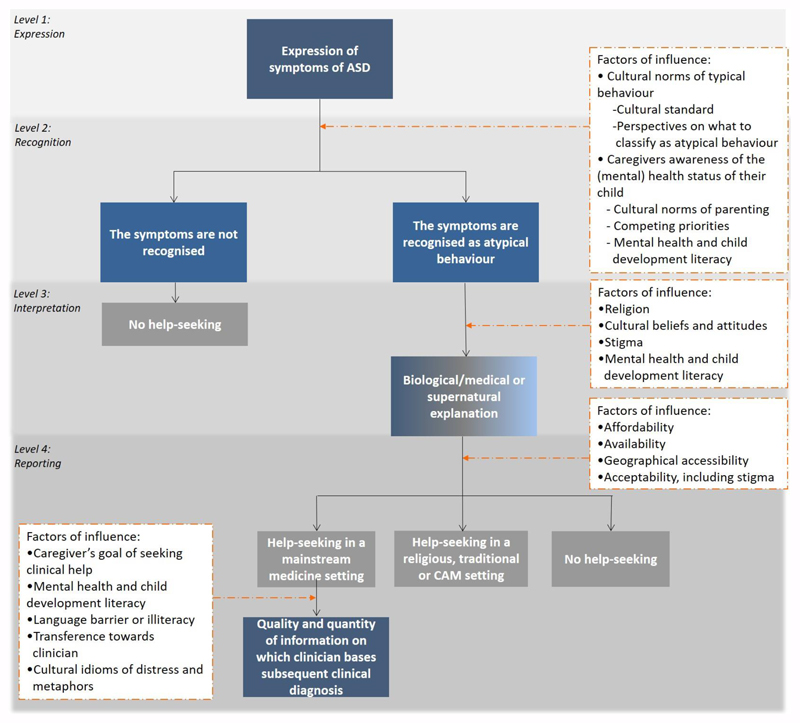
The conceptual framework is shown in Figure 1. The framework consists of four interrelated levels: i) the expression, ii) recognition, iii) interpretation, and iv) reporting of autism symptoms. Each level considers a specific question and subsequently outlines the associated potential cultural or contextual factors identified in our literature review. Each level in the framework and the factors relevant to this level will be discussed in turn.
Figure 1. The 4-level conceptual framework.
The conceptual framework considers the identification and diagnostic process at four levels: 1) the expression, 2) recognition, 3) interpretation and 4) reporting of autism symptoms. The possible cultural and socioeconomic factors that influence this process are presented in the white boxes. These factors of influence are further examined at its corresponding levels in the paper. The gradient box at level 3 in this framework illustrates that the biological or medical and supernatural causal explanations are not mutually exclusive. CAM = complementary alternative medicine.
Expression of symptoms
This first level of the conceptual framework addresses the question: To what extent is the expression of ASD symptoms, as defined in the DSM-5 (American Psychiatric Association, 2013) and the new ICD-11 (WHO, 2018) uniform across cultures?
The nosology of ASD across cultures
Following the DSM-5 diagnostic criteria for ASD there are three levels at which the behavioural aspects of ASD could differ cross-culturally: the broad domains (‘persistent deficits in social communication and social interaction’ and ‘restricted repetitive patterns of behaviour, interests, or activities’); the subdomains (e.g. ‘deficits in social-emotional reciprocity’, ‘hyper- or hyporeactivity to sensory input’); or the more narrowly described behavioural exemplars (e.g. ‘abnormal social approach’, ‘indifference to pain/temperature’) (American Psychiatric Association, 2013). The ASD criteria in the ICD-11 (WHO, 2018) follow the same two domain structure, but are less prescriptive in distinguishing narrow subdomains and behavioural exemplars (in line with the ICD classification system overall).
The broad domains defining ASD are found globally and across different ethnic groups (Lai, Lombardo, & Baron-Cohen, 2014; Lai, Lombardo, Chakrabarti, & Baron-Cohen, 2013; Zager, Cihak, & Stone-MacDonald, 2016). However, subtle differences may exist in the specific manifestations of autism symptoms, on the subdomain or behavioural exemplar level. At these levels, the symptoms of ASD may vary in four ways: 1) qualitative differences; 2) quantitative differences; 3) differences in the extent to which symptoms result in clinical impairment in day to day functioning; and 4) differences in how these symptoms cluster together in broad domains. When examining the ways in which the nosology of ASD may vary across cultures, two challenges should be kept in mind (see Box 1): the categorical fallacy that may affect cross-cultural research in psychiatry (Kleinman, 1987), and the intertwined relationship between autism’s nosology and its aetiology and developmental pathway (Lai et al., 2015).
Box 1. Two challenges in examining the nosology of autism across cultures.
Category fallacy
Kleinman (Kleinman, 1987) highlighted the pitfall of applying a nosological category developed for a particular cultural group to members of another culture, in which the category may lack coherence and may not be valid. A historical example of such a ‘category fallacy’ in cross-cultural psychiatry is Prince’s comparative study of the cultural syndrome ‘brain fag’. Prince (1960, 1985) first became aware of the brain fag syndrome amongst students in Nigeria, with complains such as ‘burning or crawling sensations’ and ‘feeling that words didn’t make sense when reading’. In this cultural group this category of symptoms was meaningful and locally recognised. However, when Prince subsequently assessed this constellation of symptoms in Canadian students, the number of students complaining of these symptoms was very low, suggesting these symptoms had no relevance in Canadian culture (Prince, 1960, 1985). To avoid this pitfall in autism research, it is important to carry out a range of qualitative and quantitative studies using ‘emic’ approaches (conducting research that takes culture as the starting point) to ensure that the construct ‘autism’ is theoretically meaningful and conceptually equivalent for members of a different culture (Cronbach & Meehl, 1955; Flaherty et al., 1988; Kirmayer & Swartz, 2014; Patel, 2003).
The nosology of autism may be intertwined with its aetiology and developmental pathway
If the aetiological causes of autism and/or the developmental pathway leading to autism as outcome are subtly different across different contexts, the behavioural expression of autism may be somewhat different too. For example, the greater prevalence of infectious diseases and increased exposure to environmental toxins and malnutrition in low-income settings may result in a behavioural phenotype of autism more frequently associated with general developmental delays. Vice versa, subtle cultural differences in what a society calls ‘autism’ are likely to result in slight differences in clinical groups, which may have somewhat different underlying aetiologies.
1). qualitative differences in symptom expression
While the broad symptom domains of autism are universally observed, differences may occur in the behavioural manifestations of autism. Previous research shows that specific manifestations vary according to age, intellectual ability and gender within a population (Lai et al., 2015; WHO, 2018). Whether this is also true for culture and context has not been studied in depth. Zhang et al. (2006) highlight possible cultural differences in the manifestation of autism in China compared to western cultures (Zhang, Wheeler, & Richey, 2006). In western cultural contexts a lack of eye contact is a common symptom of deficits in non-verbal communication. In the Chinese culture making direct eye contact with adults is considered impolite for children. Thus, in Chinese cultural context non-verbal communication difficulties characteristic for autism may manifest itself in atypical eye contact, rather than lack of eye contact.. A qualitative study exploring the expression of autism symptoms in Ethiopia (Hoekstra, Bayouh, et al., 2018) indicated that ‘greeting others well’ is reported by caregivers as something their autistic child does well, rather than a deficit. Social greetings are highly ritualised in Ethiopia and carry great social significance. Caregivers thus report this as their child’s strength, rather than as a difficulty indicative of ritualised behaviours or socio-communicative deficits characteristic of autism.
2). Quantitative differences in symptom expression
Even when the type of symptoms expressed are the same, there may be cultural differences in the frequency and severity of autistic traits or symptoms. In an early study of autism in African children, Lotter (1978) reported that most autistic children in his sample did not show hand flapping or rocking. A study comparing African American with White American children similarly reported differences in the frequency of presentation of ASD symptoms: non- functional routines or rituals and the preoccupation with parts of objects were significantly more often reported amongst white American children (Sell, Giarelli, Blum, Hanlon, & Levy, 2012). This echoes findings from a study in Nigeria finding that preoccupation with an interest or inappropriate object attachment was only present in a small minority of children with ASD (Bello-Mojeed et al., 2017). In a study comparing Latino adolescents and adults with their non-Latino counterparts in the USA, lower levels of restrictive –and- repetitive behaviours were found amongst the Latino participants (Magaña & Smith, 2013). Matson et al. (Matson et al., 2011) compared autism symptom expression in 145 autistic children across four western and eastern high-income countries, reporting cross-cultural differences in mean symptom expression scores for nonverbal communication/socialisation, verbal communication and insistence of sameness and restricted interests. The study’s relatively small sample size (27-40 participants per country) and possible cross-country differences in diagnostic practice precludes drawing strong conclusions, but provides some modest evidence of possible cultural divergence in the quantitative manifestation of ASD symptoms.
3). Differences in whether symptoms result in clinical impairment
One of the key ASD criteria in both DSM-5 and ICD-11 is that the symptoms cause “clinically significant impairment” in social, occupational, or other important areas of functioning (American Psychiatric Association, 2013; WHO, 2018). Cultural or socioeconomic variation in activities in day-to-day life may play a role in the extent to which difficulties are, or are perceived as, clinically significant impairments. For example, the socio-communicative and sensory demands placed on a subsistence farmer in a rural context are markedly different from the demands placed on an urban office worker required to work on collaborative projects in an open plan office. Little is known about how these cross-cultural and contextual differences may affect the degree of impairment induced by symptoms characteristic for ASD. Chen et al. (Chen, Bundy, Cordier, Chien, & Einfeld, 2017) compared everyday social participation of autistic individuals in Australia and Taiwan and reported that with similar ASD severity levels Taiwanese participants were more likely to stay at home compared to Australian participants, suggesting that cultural context may shape the degree of participation in day-to-day activities.
4). Differences in the factor analytic structure of autism symptoms
Both the DSM-5 and ICD-11 description of ASD include a two-domain structure, distinguishing social communicative difficulties from restricted and repetitive behaviours and interests. This two domain structure is largely supported by factor analytic studies of autism symptoms (Shuster, Perry, Bebko, & Toplak, 2014). However, the evidence for this structure comes almost exclusively from high-income countries (Shuster et al., 2014). A small number of factor analytic studies have been performed in non-western high-income countries. A study in Korea found the two- factor DSM-5 and ICD-10 structure measured by the Korean version of the ADI-R and Autism Diagnostic Observation Schedule (ADOS) well replicated in this Asian sample (Kim et al., 2016). A study examining the psychometric properties of the Chinese Autism-Spectrum Quotient in a Taiwanese sample reported a similar factor structure to those previously reported in western high-income countries (Lau et al., 2013). In sum, so far there is little evidence for clear cross-cultural differences in the latent structure of autism symptoms, but more research is needed, especially in low-income settings, before any firm conclusions can be drawn.
Recognition
The aim at this level of the conceptual framework is to clarify the process of recognition. The main question considered at this level is: What are the underlying cross-cultural and socioeconomic factors that influence whether and when atypical behaviour or traits relevant to ASD are recognised?
Global differences in age at first parental concern
The average age at which parents are first concerned in studies conducted in high-income western countries is often reported to be in the range of 14 to 19 months (Baghdadli, Picot, Pascal, Pry, & Aussilloux, 2003; Chawarska et al., 2006; Kishore & Basu, 2011; Matheis et al., 2017; Rosenberg, Landa, Law, Stuart, & Law, 2011). In countries with a different sociocultural or socioeconomic background, however, the reported age of first parental concerns tends to be higher. Studies conducted in India (Daley, 2004; Srinath, Seshadri, Girimaji, & Kommu, 2017), Latin America (Irarrazaval et al., 2017) and Hong Kong Chinese (Tait, Fung, Hu, Sweller, & Wang, 2016) reported mean ages of first parental concern of 24 to 26 months, 29 months and 31 months respectively. While these studies used somewhat different methodologies which may also account for some of the differences observed, possible cultural and contextual explanations for this gap will be discussed below.
Cultural norms of typical behaviour
A large study in typically developing children from four culturally and linguistically diverse countries (Argentina, India, South Africa and Turkey), reported that almost all milestones, with the exception of milestones related to self-help skills, are similarly attained in the first three years of life (Ertem et al., 2018). While this study provides little evidence for actual differences in reaching developmental milestones, cultural differences may exist in the levels of salience afforded to a specific behaviour by parents. Recognition of autism symptoms may be affected by cultural differences in what is considered typical behaviour. A behavioural characteristic seen as atypical in a western sociocultural context may not be deviating from the local norms in other sociocultural contexts. They may not deviate either because the behaviour is not salient in this culture and therefore tends to go unnoticed, or because the behaviour is interwoven with the cultural standard (Norbury & Sparks, 2013; Donohue, Childs, Richards, & Robins, 2017; Harrison, Long, Tommet, & Jones, 2017; Kirmayer & Swartz, 2014; Mandell & Novak, 2005).
As referred to earlier, eye contact with authorities is traditionally seen as shameful in Asian cultures and as disrespectful in some African or Latino cultures (Bernier, Mao, & Yen, 2010; Le Roux, 2002; Zhang et al., 2006). In these cultures a child that does not look their parent, teacher or a clinician in the eyes may be seen as obedient rather than displaying atypical behaviour characteristic of autism. The ‘abnormalities in eye contact’ as described in the DSM-5 (American Psychiatric Association, 2013; Zhang et al., 2006) may therefore be more subtle and difficult to recognise.
Imaginative play is another example of a symptom of autism where differences in cultural norms may be relevant (Norbury & Sparks, 2013; Freeth et al., 2013; Harrison et al., 2017; Smith, Malcolm-Smith, & Vries, 2017). The frequency with which children engage in pretend play and the degree of imagination used during this play is culturally influenced (Lillard & Pinkham, 2011; Weisberg, 2015). A study in South Africa aimed to ask caregivers what kind of pretend games their children play, but caregivers gave examples that did not include imaginary play, suggesting they were less familiar with this type of play (Smith et al., 2017). In most western societies parents think of young children as social partners and play with them, but caregivers in other societies often think that such behaviour serves no purpose and expect children to play with their siblings or peers (Bornstein, 2013). In general population samples from India, Kenya and Mexico, less than half of the children showed fantasy play (Edwards, 2000). Similarly, Anglo-American children were found to more often engage in pretend play during free play time than Korean American children (Farver & Shin, 1997). Thus, lack of imaginary play may be a more salient symptom of autism in high-income western countries than in other cultural contexts.
Quantitative evidence for possible cross-cultural differences in cultural norms come from studies using the Autism-Spectrum Quotient (AQ) (Baron-Cohen, Wheelwright, Skinner, Martin, & Clubley, 2001). Comparing AQ data from non-clinical student samples in the UK (where the instrument was developed) with data from students in Japan, Malaysia and India indicated that Japanese, Malaysian and Indian participants self-reported higher AQ scores than the UK sample (Freeth et al., 2013; Wakabayashi, Baron-Cohen, Wheelwright, & Tojo, 2006). These differences in mean scores may indicate differences in cultural norms of behaviours associated with autism. In a cross-cultural study using parent-reported AQ-Child data collected in the UK, India and Japan (Carruthers et al., 2018) most items showed similar performance in the ability to distinguish children with ASD from neurotypical children. There was some evidence for cultural divergence for four out of fifty items. The item ‘S/he enjoys doing things spontaneously’ for example, had very good discrimination properties in the UK, but poor discrimination properties in the Indian and Japanese samples, suggesting cultural norms may play a role in some specific autism characteristics.
Apart from differences in cultural standards, there may be variability in the boundaries of what is considered culturally acceptable behaviour: some cultures may be more forgiving of slight deviations of the typical norm than others. Cross-cultural psychology studies comparing perspectives on child behaviour (Lambert et al., 1992; Weisz et al., 1988) suggested that Thai and Jamaican adults were generally less concerned about problem behaviours compared to American adults. Similarly, immigrant mothers in the Netherlands perceived equivalent levels of child behaviour problems as less problematic compared to native Dutch mothers (Leijten, Raaijmakers, Orobio de Castro, & Matthys, 2016). In a study comparing reports of autism symptoms by Anglo and Latino mothers, the Latino mothers reported significantly fewer ASD symptoms, even though their children obtained higher ASD severity scores on the ADOS compared to the Anglo children (Blacher, Cohen, & Azad, 2014). A qualitative study (Daley, 2004) suggests similar cultural variation may be relevant to autism characteristics in rural India. In this study a psychiatrist is quoted: ‘There may be a tendency by our rural mass to accept and tolerate some degree of abnormality as normal’. Thus, cultural or contextual (urban vs rural) differences in tolerance and acceptance of deviating from the norm may influence whether symptoms of autism are regarded as atypical.
Caregivers’ awareness of the mental health and developmental status of their child
The degree of attention towards a child may differ across cultures or socioeconomic settings. The more attention is placed on a child’s cognitive and behavioural development and (mental) health, the easier and earlier atypical behaviour may be noticed. Cultural differences in parenting, and other priorities competing for the caregiver’s attention may influence a parent’s level of awareness of their child’s development.
Cultural norms of parenting
The concept of ‘parenting’ and how to fulfil this role is culture-dependent. In many cultures throughout the world people live in extended families with the responsibility for childcare distributed over multiple caregivers (Bornstein, 2013), including siblings (Gielen & Roopnarine, 2016). These shared responsibilities may influence the caregivers’ awareness of the (mental) health status and developmental trajectories of a child. Furthermore, culture influences parenting styles, what parents expect of their children and what behaviours they promote or discourage (Bornstein, 2005; Gielen & Roopnarine, 2016). Chinese parents tend to adhere to a highly child-centred strict way of parenting with a focus on achievement (Ashton-James, Kushlev, & Dunn, 2013; Chua, 2011). European American children are encouraged to discuss their own feelings and those of others, as a way to increase their understanding and regulation of emotions. In contrast, Chinese families tend to encourage their children to attune towards the feelings of others, but are expected to show restraint in the expression of their own feelings (Chao, 1995). American mothers try to promote self-actualisation, autonomy, assertiveness, and verbal competence in their children, whereas Japanese mothers tend to promote emotional maturity, self-control, interdependence and social courtesy (Bornstein, 2012). These cultural differences in parenting styles and in what parents expect of their children may affect whether and at what age a parent recognises aspects of atypical development in their child.
Competing priorities
Poor environmental circumstances or hazards can be root causes of physical health problems and can be related to living in poverty, war or hunger, especially in very low-income settings (WHO, 2008b). The priorities of caregivers may be mainly centred around social and financial stressors, resulting in decreased attention to the mental wellbeing and developmental trajectory of a child (Magnusson, Minkovitz, Kuhlthau, Caballero, & Mistry, 2017). As a consequence, atypical behaviour may be overlooked or there may be a delay in the process of recognition.
Literacy in mental health and the typical child developmental trajectory
Mental health literacy, the cognitive and social skills required to read, understand and gain access to basic mental health information (Jorm et al., 1997; Kutcher, Wei, & Coniglio, 2016), is found to be interrelated with mental health knowledge and awareness (Hoven et al., 2008) and may thus influence the process of recognising atypical behaviour. Similarly, this literacy may influence the caregivers’ awareness and attention towards the developmental trajectory of their child. Limited literacy around broad issues regarding mental health and development (Furnham & Hamid, 2014; Ganasen et al., 2008; Hoven et al., 2008), as well as limited autism awareness in specific (Abubakar, Ssewanyana, de Vries, et al., 2016; WHO, 2013), may affect if and when autism symptoms are recognised. A mother of a child with ASD in Malaysia was quoted (Ilias, Liaw, Cornish, Park, & Golden, 2017):
‘’I didn’t know she has autism until she got a fever. I sent her to the hospital. Then the doctor suspected that she is having autism. I said, ‘’What is autism?” Then he said this is a lifelong thing. Then I asked, ‘’Doctor, how to spell?” He said, ‘’A-u-t-i-s-m.”
In addition to explaining global differences in recognition of autism symptoms, culture and context may also contribute to within-country differences in autism awareness. A recent study in a low-income sample of families in the USA suggested that compared to white parents racial/ethnic minority parents and especially Latino parents had less familiarity or personal experience with people with developmental disabilities, and were less aware of early signs of developmental disabilities (Zuckerman, Chavez, Murillo, Lindly, & Reeder, 2018). Limited awareness about autism and low mental health literacy may be directly related to the availability, accessibility and acceptability of healthcare professionals, a topic discussed in more detail under level 4 of this framework.
Interpretation
The emphasis at this level of the conceptual framework is on the process of interpretation: what kind of explanations may be given for the atypical behaviour (as observed and recognised in the second level of the conceptual framework), and what cultural and contextual factors may affect this interpretation?
Explanatory models of recognised atypical behaviour
Explanatory models are the individual’s perspectives on the nature, causes, course, diagnosis and treatment of illness (Kleinman, 1978), which can be culture bound. The causes of autism are complex and multi-factorial (Lai et al., 2013); most cases of autism are idiopathic and this uncertainty may add to the plethora of perceived causes reported by parents of children with ASD. Examples of biological or medical explanations attributed to ASD are hereditary factors (Gona et al., 2015; Heys et al., 2017), infectious disease (Gona et al., 2015; Tilahun et al., 2016), an accident (Al-Dababneh, Al-Zboon, & Baibers, 2016; Minhas et al., 2015; Shaked & Bilu, 2006; Tilahun et al., 2016), complications during pregnancy or birth (Al-Dababneh et al., 2016; Gona et al., 2015; Heys et al., 2017; Shaked & Bilu, 2006; Shyu, Tsai, & Tsai, 2010; Tilahun et al., 2016) or malnutrition (Gona et al., 2015; Heys et al., 2017). In the USA the most common perceived causes reported by parents are genetics/heritability and environmental risk factors, including heavy metals, food, pesticides, pollution and other exposures (Chaidez et al., 2018; Zuckerman, Lindly, & Sinche, 2016). Another explanation frequently offered, especially in North America, is childhood vaccinations (Bazzano, Zeldin, Schuster, Barrett, & Lehrer, 2012; Buehning & Peddecord, 2017; Decoteau, 2017; Goin-Kochel et al., 2016; Wolff & Madlon-Kay, 2014) even though a causal link between vaccinations and autism has been comprehensively scientifically rejected (Eggertson, 2010; Smeeth et al., 2004).
Cultural and contextual factors may affect the popularity of certain explanations. For example, while the belief that vaccines can cause autism is much more prevalent in North America than sub-Saharan Africa, within Somali communities living in the United States this belief appears particularly prevalent (Wolff & Madlon-Kay, 2014). Moreover, the Somali population in North America often sees autism as ‘the western disease’, as many do not believe autism exists in Somalia. One of their theories for the high rates of autism amongst Somali in America, is because of the American diet and environment exposures such as antibiotics in food production (Decoteau, 2017).
Supernatural explanations include attributing ASD to a curse, a sin or a punishment from God (Gona et al., 2015; Heys et al., 2017; Tilahun et al., 2016). The majority of mothers in a Jewish ultraorthodox sample in Israel reported the belief that the child with ASD has come to rectify a sin, paving the way to Paradise (Shaked & Bilu, 2006). In Pakistan neurodevelopmental disabilities are commonly believed to be the will of Allah, and caring for a child with ASD is a divine duty that will be rewarded in the afterlife (Minhas et al., 2015; Mirza, Tareen, Davidson, & Rahman, 2009). Other supernatural explanations particularly prevalent in African countries include witchcraft and the evil eye (Gona et al., 2015; Tilahun et al., 2016). Taken together, supernatural and traditional explanations tend to be more prevalent in LMIC (Gureje et al., 2015).
The various types of causal explanations are not mutually exclusive. For example, in a study in Ethiopia examining the explanatory models of caregivers of children with developmental disorders, 36% of the caregivers provided at least one biological/medical explanation as well as a supernatural explanation for their child’s condition (Tilahun et al., 2016). Similar co-existence of explanations has been reported in very different cultural settings including a Jewish ultraorthodox community in Israel (Shaked, 2005; Shaked & Bilu, 2006), in Taiwan (Shyu et al., 2010) and in a study of Indian parents who migrated abroad (Ravindran & Myers, 2013). A common thread in causal explanations for a child’s autism is that the perceived locus of control is laid with parents, especially mothers. The parents are seen as responsible for maternal malnutrition or alcohol use during pregnancy, a child’s head injury, or the cause of a sin placed on the family. Atypical development is also often attributed to bad parenting and spoiling the child (Heys et al., 2017). The parental feelings of guilt associated with these causal attributions may affect help-seeking.
Cultural beliefs or attitudes may also affect whether atypical development is perceived as problematic. In India, a common local cultural belief is that boys start to speak later than girls. A mother of a four-year-old boy in India was quoted: ‘It is well known that the Indian boy child speaks late’ (Daley, 2004). In China, a delay in speech is often interpreted as a good sign; there is an ancient saying that a child that speaks late will be more intelligent than its peers in the future (Sun et al., 2013). Thus, even if speech delay is recognised, cultural beliefs may affect the interpretation of this delay and may affect if and when help is sought.
The causal explanations for a child’s condition affect what type of support is sought and when this support is sought (Mandell & Novak, 2005; Yeh, Hough, McCabe, Lau, & Garland, 2004). There may be a delay or resistance to seek help in a mainstream medical setting if caregivers exclusively attribute the atypical behaviour of their child to supernatural or traditional explanations, or biological explanations not supported by mainstream evidence-based medicine. A study in Californian parents of children with autism found that parents endorsing causal beliefs relating to environmental risk exposures or vaccinations were more likely to seek complementary or alternative medicine support than families not endorsing such causal beliefs (Chaidez et al., 2018). Apart from perceived causal beliefs, factors that may influence this process of interpretation and subsequent help-seeking include stigma and mental health literacy.
Associated factors of influence
Stigma
Stigma towards individuals with autism and their families occurs globally and crosses culture and context (Grinker et al., 2012; Ha, Whittaker, Whittaker, & Rodger, 2014; Hsu et al., 2017; Manor-Binyamini & Shoshana, 2018; Mitter, Ali, & Scior, 2019; Someki, Torii, Brooks, Koeda, & Gillespie-Lynch, 2018; Tilahun et al., 2016). Two types of stigma can be distinguished; felt stigma (internal stigma rooted in fear of enacted stigma) and enacted stigma (external stigma, including overt ostracism or discrimination) (Brohan, Slade, Clement, & Thornicroft, 2010). Both types of stigma can be experienced by the individual with ASD themselves or by their caregivers or family members; the latter is referred to as affiliate stigma (Gaebel, Roessler, & Sartorius, 2017; Thornicroft et al., 2016; Werner & Shulman, 2015). A clear example of affiliate stigma is reported in a study of South Korean caregivers, who described the stigmatising consequences of having a child with ASD, including reduced career opportunities, marginalisation from socially desirable networks, and a decreased value of an apartment previously inhabited by a child with ASD (Grinker et al., 2012). In South Korea as well as India (Daley, Singhal, & Krishnamurthy, 2013; Divan, Vajaratkar, Desai, Strik-Lievers, & Patel, 2012; Grinker et al., 2012) the high heritability of autism adds a source of stigma; in both countries having a relative with autism may decrease marriage prospects due to a ‘genetic taint’ on the family, and in Korea beliefs about biological (including genetic) causes of autism are associated with increased stigmatising attitudes in the general population (Park, Lee, & Kim, 2018).
Stigma related to autism can be associated with the atypical behaviour itself (for example blaming the parent for bad parenting practices or spoiling the child; Heys et al., 2017) or can be directly associated with the diagnostic label of autism (for example, the genetic taint reported in Korea and India; Daley, Singhal, & Krishnamurthy, 2013; Divan, Vajaratkar, Desai, Strik-Lievers, & Patel, 2012; Grinker et al., 2012). Both types of stigma might affect parents’ interpretation of their child’s atypical behaviours and consequently influence if and when help is sought.
In a meta-synthesis of studies exploring parental experiences of autism, analysing 50 studies from across the globe, a common theme was that caregivers reported feeling socially excluded and negatively judged by others, even within their own extended family (Ooi, Ong, Jacob, & Khan, 2016). These felt or enacted stigma experiences may lead caregivers to favour alternative interpretations of their child’s atypical behaviour. In South Korea, parents prefer to call their child a ‘border child’. This substitute explanation focuses primarily on the social domain rather than on more generalised developmental problem, and frames the child’s symptoms as temporary difficulties rather than a long-term condition (Grinker et al., 2012; Grinker & Cho, 2013). Similarly, parents in Vietnam often prefer to refer to ASD as a disease rather than disorder, viewing the condition as temporary and emphasising the possibility of a cure (Ha et al., 2014).
In a study among Ethiopian caregivers, reported stigma was found to be associated with the type of causal explanations provided by caregivers (Tilahun et al., 2016). Caregivers providing a spiritual explanation for their child’s condition or seeking help from spiritual institutions reported higher experienced stigma.
Literacy in mental health and typical child developmental trajectories
Mental health and child developmental literacy is not only a key factor in recognising autism symptoms (as described at the second level of this conceptual framework), but also in the interpretation of these symptoms. For example, a belief commonly reported among parents in South Asian cultures is that children can grow out of their developmental problems; and as a result, these parents may be less likely to seek help, or may delay seeking help (Minhas et al., 2015).
Some studies suggest increased knowledge about ASD is associated with reduced stigmatising beliefs and attitudes (Milačić-Vidojević, Gligorović, & Dragojević, 2014; Obeid et al., 2015), and that autism training may improve knowledge and decrease stigmatising attitudes (Obeid et al., 2015; Tilahun et al., 2017). Similarly, parents of children with ASD found it easier to resist felt stigma when equipped with sufficient medical knowledge (Farrugia, 2009). However, the relationship between ASD knowledge and stigma is unlikely to be straightforward: as described above, knowledge of the genetic aetiology of autism may be related to increased stigma in some contexts (Daley, 2004; Divan et al., 2012; Grinker et al., 2012; Park et al., 2018). Research on mental health stigma suggests that knowledge about biogenetic causes of mental illness does not result in greater public acceptance of people with mental illness (Angermeyer, Holzinger, Carta, & Schomerus, 2011). Awareness of genetic influences may also be related to greater perceived seriousness of mental illness and reduced optimism about the long-term prognosis (Phelan, 2005; Phelan, Yang, & Cruz-Rojas, 2006). A study that evaluated the impact of a training on mental health and developmental disorders for Ethiopian community health workers reported decreased negative beliefs and stigmatising attitudes among trained health workers, but also a decrease in positive expectations of what children with autism can achieve (Tilahun et al., 2017).
Reporting
The fourth level of the conceptual framework focusses on the process of reporting symptoms to a health worker or clinical professional. Two underlying processes can be distinguished at this level: i) barriers to help-seeking; and ii) when help is sought, the factors influencing the quality and quantity of clinical information received by the clinician.
Barriers in help-seeking behaviour
Several previous studies have considered the barriers to accessing support for mental health problems (Cauce et al., 2002; Eaton et al., 2011; Prince et al., 2007; Reardon et al., 2017; Saxena, Thornicroft, Knapp, & Whiteford, 2007) or help for individuals with ASD (Abubakar, Ssewanyana, de Vries, et al., 2016; de Vries, 2016; Durkin et al., 2015; Masri, Al Suluh, & Nasir, 2013) around the globe. In addition to the factors outlined under the previous levels of the conceptual framework, four barriers to help-seeking can be distinguished: affordability, availability, geographical accessibility, and acceptability (Jacobs et al., 2012; Peters et al., 2008). These factors are discussed below in relation to mental health as well as to ASD. In contrast to the other levels of the framework, these factors primarily concern socioeconomic rather than cultural influences.
Affordability
The affordability of mental healthcare services comprises two perspectives: the actual cost of services and the user’s financial means (Peters et al., 2008). Service costs are associated with countries’ policies of financing mental healthcare. In 17% of all countries worldwide, and in over 40% of African and South East Asian countries, mental health services are primarily paid for by out of pocket payments (WHO, 2005). This type of mental health financing can result in ‘catastrophic payments’, in which costs are disproportionately high in relation to the income of a household. Households faced with these costs may therefore not seek help, or are pushed into (deeper) poverty (Hailemichael et al., 2019; World Health Organization, 2005). The second perspective concerns the financial means of a household. Across different geographical contexts, the access to and quality of ASD services is associated with income (Alnemary, Aldhalaan, Simon-Cereijido, & Alnemary, 2017; Bishop-Fitzpatrick & Kind, 2017; Colbert, Webber, & Graham, 2017; Dickerson et al., 2017), with parents of lower socioeconomic status reporting poorer access (Bishop-Fitzpatrick & Kind, 2017) and poorer quality (S. Magaña, Parish, & Son, 2015) of care for their child with ASD. In addition to direct healthcare expenditures, indirect expenditures, such as transportation costs or opportunity costs of the caregiver missing out on income-generating activities, play a role (Daley, 2004; Minhas et al., 2015; Peters et al., 2008; Tilahun et al., 2016). A mother of a seven-year-old girl with ASD in Pakistan was quoted (Minhas et al., 2015): ‘’We tried to visit the hospital once. It’s far off and expensive too; we can’t afford to take her frequently.”
Availability
Service provision in many LMIC is hampered by a lack of trained personnel, with most of these countries reporting shortages in psychiatrists, nurses and/or psychosocial care providers (Bruckner et al., 2011). Nearly half of the world’s population live in countries with fewer than one psychiatrist per 100 000 persons (WHO, 2014). Lack of diagnostic and intervention materials or instruments; poor quality or lack of experience of practicing clinicians; and long wait times for access to services have also been identified as barriers to receiving support (Durkin et al., 2015; Peters et al., 2008; Reardon et al., 2017). In Africa in particular, a shortage of basic knowledge about ASD amongst health professionals has been reported (Bakare & Munir, 2011; Eseigbe et al., 2015; Mitchell & Holdt, 2014; Ruparelia et al., 2016; Tekola et al., 2016; WHO, 2013), as well as a lack of appropriate diagnostic and screening tools (Abubakar, Ssewanyana, de Vries, et al., 2016; Abubakar, Ssewanyana, & Newton, 2016; Ruparelia et al., 2016; Tekola et al., 2016). Moreover, lack of consistently implemented developmental monitoring in the health system contributes to developmental delays being missed or identified late (Engle et al., 2011).
Geographical accessibility
Geographical accessibility to services involves the travel distance, travel time, and the range and quality of the travel options (e.g. the quality of the road; availability of public transport services, etc) (Peters et al., 2008). Given the scarcity of mental health services and the often centralised location of services in or near larger cities (Saraceno et al., 2007), adequate access to diagnostic and intervention services is especially problematic for individuals living in more remote areas (Alnemary et al., 2017; Saxena et al., 2007). ASD studies from South Asian countries highlight how a limited number of specialists concentrated in big cities means it is prohibitively difficult for caregivers of children with ASD to seek help, with some families having to travel for days (Daley, 2004; Minhas et al., 2015). In Africa similar barriers were reported for individuals with intellectual disability (Adnams, 2010) and children with ASD (Tekola et al., 2016).
Cultural barriers in accessibility
Gender inequality can form a barrier to accessing services in some cultural contexts. A study among Bedouin mothers of children with autism in Israel (Manor-Binyamini & Shoshana, 2018) describes how in the strongly patriarchal society of the Bedouins, mothers are often unable to access services for their children by themselves and require the father as mediator. One mother was quoted:
“We missed many treatments because his father was busy, and I can’t travel without him, and sometimes he didn’t want to take us because he said it was useless.”
Acceptability
The acceptability of mental health services can be influenced by users’ attitudes and expectations of these services (Jacobs et al., 2012). A negative prior experience of the health service and knowledge and beliefs about -or expectations and quality standards of- the services can induce distrust in clinical help (Jacobs et al., 2012; Yeh et al., 2004). Distrust may cause caregivers to ‘shop’ from one clinician to the other (Daley, 2004; Minhas et al., 2015), to search for traditional and alternative help (Gureje et al., 2015; Lofthouse, Hendren, Hurt, Arnold, & Butter, 2012) or to seek no help at all. There is some evidence from ethnic minority populations in the USA that there are cultural differences in the acceptability of medical and psychosocial support services, with African American families in particular having little confidence in the impact of psychotherapy, and concern that contact with service providers may lead to institutionalisation (Cauce et al., 2002). Stigma can be considered under the broader dimension of acceptability (Jacobs et al., 2012). Since stigma features in several levels of our framework, its importance in help-seeking and reporting of autism symptoms is described separately below.
Stigma
In ASD research stigma is frequently reported as a barrier to seek help or to receiving a diagnosis (Grinker et al., 2012; Papadopoulos, Lodder, Constantinou, & Randhawa, 2019; Ruparelia et al., 2016; Zuckerman et al., 2014). This may be due to the fear of experienced shame, or the fear of a diagnostic label that has potential negative implications. As a mother in South Korea described (Grinker et al., 2012): ‘’Why, unless there was complete confidentiality, would any parent tell the truth about her child?” Affiliate stigma can cause caregivers in various cultural settings to keep the child secret from the community. These caregivers hide the child’s existence, keep the child at home, or send the child away to extended family living in more remote areas of the country (Hadidi & Khateeb, 2015; Tait et al., 2016; Tekola et al., 2016; Tilahun et al., 2016). This in turn may negatively influence the help-seeking behaviour and the awareness of ASD in these settings. An informant working for a community-based rehabilitation organisation in Ethiopia (Tekola et al., 2016) reported:
‘’Some of the children we see have not seen sunshine before….when we asked parents whether there are children who have problems in their house, they didn’t tell us about their child who has autism or intellectual disability. They only showed us their child who has a physical disability.”
In addition, even if help is sought, high levels of stigma may result in caregivers being reluctant to report symptoms that they view as socially undesirable (Grinker et al., 2012; Matson et al., 2017; Song et al., 2017). This may subsequently lead to a decrease in the quantity and quality of received clinical information – a topic addressed in the next section.
Factors of influence in the transfer of information
The quality and quantity of information a clinician receives from a caregiver to inform the diagnostic process can be influenced by cultural or contextual factors (Norbury & Sparks, 2013; Kirmayer & Swartz, 2014). In line with the scope of the conceptual framework, the focus here is on the factors of influence in the transference of information from the perspective of the caregivers and their child with ASD; the factors of influence on the side of the clinician (e.g. how the information is received) is an important topic but out of the scope of the current study.
Caregiver’s goal of seeking clinical help
A discordance in treatment goals or explanatory models between caregiver and clinician can cause misunderstandings in the clinician-caregiver relationship. In Pakistan, for example, caregivers often expect clinicians to be able to cure their child with ASD (Bernier et al., 2010; Minhas et al., 2015). Similarly, parents of children with ASD in Kenya reported they hoped for a cure and had sought treatment with this expectation in mind (Gona et al., 2015). This mismatch in caregiver expectation and what a clinician has to offer may result in caregivers seeking help elsewhere (Bernier et al., 2010; Klasen & Goodman, 2000; Minhas et al., 2015). Furthermore, there are cross-cultural differences in what is perceived as a ‘positive outcome’. Whereas the focus in western settings is often on the clinical outcome (e.g. decrease in severity of symptoms) in other cultural settings the emphasis may lie more strongly on an ‘existential’ outcome such as emotional wellbeing (Gureje et al., 2015; Kirmayer & Swartz, 2014).
Literacy in mental health and the typical child developmental trajectory
The possible influence of mental health and child developmental literacy on the recognition and interpretation of autism symptoms has already been discussed in level 2 and 3; in addition health literacy may affect the process of reporting. Limited health literacy may lead to difficulties in understanding questions or explanations from the clinician and difficulties gaining access to clinical information prior to visiting the clinic. Both may affect the quantity and quality of information as received by the clinician and as a result may influence the ability to identify and diagnose a child with ASD (Donohue et al., 2017).
Language barrier or low-literacy
Language barriers or low-literacy can induce difficulties in communication and are closely interlinked with health literacy. Language barriers may be especially relevant in multilingual countries where the diagnostician has a different mother tongue or dialect to that of the family. The high in- and outward migration rates globally may also contribute to language barriers (Rogler, 1993; United Nations, Department of Economic and Social Affairs, 2015). Latino parents living in the USA with poor proficiency in the English language report receiving poorer primary healthcare services than those with good English language proficiency (Pippins, Alegría, & Haas, 2007). Latino parents of children with ASD reported that a language barrier prevented them from expressing their concerns optimally (WHO, 2014). In addition, given that over 750 million adults globally are non-literate (UNESCO institute for statistics, 2017), illiteracy and low literacy should be considered as a factor of importance. Low literacy was offered as one explanation for the finding of high false positive rates in an autism screening study in ethnically diverse and low socioeconomic status families in the USA (Khowaja et al., 2015).
Caregivers’ perception of the clinician
The interaction between a clinician and the caregiver and child can be affected by the caregiver’s perception of the clinician. Some research suggests that the perceived personal similarities between patient and clinician with respect to their personal beliefs, values and communication style is associated with greater patient-reported trust and health care satisfaction (Street, O’Malley, Cooper, & Haidet, 2008).This is of particular importance in multicultural settings where cultural and linguistic barriers may reduce the experienced quality of care that families perceive (Alegría, Alvarez, & Falgas-Bague, 2017). Moreover, (perceived) differences in societal standing may affect the information exchange between clinician and caregiver. In India, clinicians are often perceived as ‘next to God’ (Daley, 2004); this view may affect the quality and quantity of information caregivers disclose.
Cultural idioms of distress and metaphors
The notion ‘cultural idioms of distress’ addresses the variety of ways in which cultural groups express or communicate their suffering (American Psychiatric Association, 2013; Kirmayer & Swartz, 2014; Nichter, 2010). Global mental health research shows that patients and their caregivers often express their (mental health) distress somatically or through the use of metaphors, and that some of these idioms may be culture-bound. African examples of metaphors used to describe mental distress are ‘a peppery feeling’, ‘heat in the head’ or ‘worms crawling in the head’ (Kirmayer & Swartz, 2014). Little is known about idioms of distress directly relevant to autism. In low awareness settings the main concerns highlighted by a parent of a child with autism may relate to challenging behaviour or lack of self-help skills of their child (e.g. difficulty in toilet training) (Hoekstra, Bayouh, et al., 2018). That is, rather than describing core autism diagnostic symptoms, caregivers may find difficulties that have a direct bearing on the practical day-to-day functioning of their family most salient and report these most prominently. A reciprocal understanding between caregiver and clinician of the cultural idioms of distress is likely to improve the clinician-caregiver communication and the clinical information that forms the basis for the clinical diagnosis and future care plan for the family.
Discussion
In this paper we proposed a 4-level conceptual framework, mapping out the possible cultural and contextual factors that may affect the identification and diagnosis of ASD. As far as we are aware, this is the first attempt to provide a structured overview of the cultural and contextual factors of influence in the process of identification, help-seeking and diagnosis of ASD globally, drawing on literature from different disciplines. Based on this framework, we suggest future research directions to build the urgently needed capacity for ASD research and services globally (Table 1), highlighting both fundamental research topics (F) as well as applied research to inform the development and implementation of interventions (I). Throughout all strands of future cross-cultural research suggested in Table 1, an important general guideline is to make sure that the cultural group under consideration is represented in the research group conducting the work, ensuring that the research uses culturally and contextually appropriate research methods, and that findings are interpreted with appreciation of the local context (Hoekstra, Girma, Tekola, & Yenus, 2018).
Table 1. Future research directions.
| RESEARCH TOPICS | METHODOLOGICAL APPROACH | |
|---|---|---|
| Level 1: Expression of symptoms | ||
|
| ||
| Cross-cultural reflection on the nosology of ASD | ||
|
| ||
| F | Qualitative symptom expression | Research into the qualitative manifestation of ASD symptoms in culturally diverse or specific non-western cultural settings, using not just etic, but also emic† approaches (Patel & Mann, 1997). In light of these findings, provide cultural and ethnic reflections on the criteria for ASD, on the narrow construct and behavioural exemplars |
|
| ||
| F | Quantitative symptom expression | Study of the cultural differences and commonalities in quantitative expression of ASD traits. Based on these findings, reflection on the threshold for defining clinical ASD |
|
| ||
| F | Clinical Impairment | Cross-cultural quantitative and qualitative research into the extent to which difficulties related to ASD result in impairment in day-to-day functioning. Based on these findings, reflection on the threshold for defining ASD |
|
| ||
| F | Factor analytic structure | Cross-cultural factor analytic studies of ASD symptoms. In light of these findings, reflection on broad and narrow symptom domain structure as described in current diagnostic manuals (American Psychiatric Association, 2013; WHO, 2018) |
|
| ||
| Level 2: Recognition | ||
|
| ||
| F | Age at first parental concern | Cross-cultural comparisons of age at first parental concern related to ASD and the associated socioeconomic and cultural factors that may explain cross-cultural variation |
|
| ||
| F | Cultural norms of typical behaviour | Cross-cultural comparisons of reports of autistic-like traits in typically developing children |
|
| ||
| F | Cultural norms of parenting | Cross-cultural comparisons of parenting styles, the distribution of responsibilities (e.g. extended families) and their potential influence on the age at first parental concern |
|
| ||
| F | Competing priorities | Explorative research into the influence of competing priorities such as poverty or war on caregivers' awareness of the mental health and developmental status of their child |
|
| ||
| F | Mental health and child development literacy | Cross-cultural comparisons of caregivers’ literacy on child mental health and child developmental trajectories, and the association between caregivers' awareness and age at first parental concern |
|
| ||
| I | Improving parental recognition of autism symptoms | Develop and evaluate culturally appropriate autism awareness interventions among parents |
|
| ||
| I | Improving recognition of autism symptoms by education and health workers | Develop and evaluate culturally appropriate training interventions to improve knowledge and awareness related to autism in teachers and/or health workers. Existing examples include Grinker et al. (2015) and Tilahun et al. (2017) (Grinker et al., 2015; Tilahun et al., 2017). |
|
| ||
| Level 3: Interpretation | ||
|
| ||
| F | Explanatory models | Cross-cultural comparisons of parental explanatory models and the associated socioeconomic and cultural factors that may explain cross-cultural variation |
|
| ||
| F | Help-seeking patterns | Cross-cultural comparisons of help-seeking behaviour and timing of help-seeking, and its association with parental causal explanations |
|
| ||
| I | Reduce barriers to help-seeking in mainstream medical settings due to stigma and/or alternative causal explanations | Develop and evaluate interventions aiming to decrease stigma and parental guilt. Where appropriate, co-develop and facilitate intervention in collaboration with alternative, religious or traditional healers (Gureje et al., 2015) |
|
| ||
| I | Improving awareness among mental health practitioners of the cultural background of their clients | Develop and evaluate training interventions to increase awareness among mental health practitioners of their clients’ explanatory models, concurrent alternative help-seeking behaviour, and cultural idioms of distress |
|
| ||
| Level 4: Reporting | ||
|
| ||
| F | Barriers to help-seeking | Identify the main local barriers of accessing services for ASD in specific cultural and socioeconomic settings |
|
| ||
| F | Timing of help-seeking from mainstream medical institutions | Cross-cultural comparisons of the age at which help is sought from mainstream medical institutions and its interrelationship with barriers to accessing services |
|
| ||
| F | Transference of clinical information | Cross-cultural exploration and comparison of the cultural and socioeconomic factors that may affect the transference of clinical information |
|
| ||
| I | Increase access to services | Develop and evaluate culturally and contextually appropriate service delivery models suitable for low-resource settings, for example using non-specialist training facilitators as currently tested in Pakistan (Hamdani et al., 2017; Hamdani, Minhas, Iqbal, & Rahman, 2015). |
| Develop and evaluate effective and feasible interventions to equip mental health professionals with the knowledge and skills required to identify, diagnose and/or manage ASD. Existing example includes the WHO mhGAP programme (WHO, 2008c). | ||
|
| ||
| Research straddling multiple framework levels | ||
|
| ||
| F | Stigma | Cross-cultural comparisons of felt, enacted and affiliate stigma related to ASD, and its association with explanatory models, health literacy and help-seeking behaviours |
|
| ||
| F | Improving the availability of cultural appropriate and validated screening and diagnostic instruments | Develop and validate culturally and contextually appropriate screening and diagnostic instruments |
|
| ||
| I | Improve public awareness of autism | Develop and evaluate interventions to improve public awareness of ASD, with autism literacy and stigma as focal points |
Note: F: fundamental research topics; I: research informing intervention development and implementation
Emic approach: conducting research taking the culture as starting point, seeking to understand the meaning of the phenotype under study and its associations with other factors using that cultural framework; vs etic approach, conducting an evaluation of a phenotype by attempting to use a more culturally neutral, universal or “objective” construct (Berry, 1969).
The framework is likely to be of relevance to a wide audience, including researchers conducting studies on the epidemiology, screening and diagnosis of autism or developing and evaluating interventions, but also to practitioners wishing to advance their knowledge about possible cultural factors affecting interaction with their clients. The framework may also be relevant for mental health service policy makers aiming to improve support for individuals with ASD globally.
Although the conceptual framework has specifically been developed for application in LMIC, it will have relevance too in culturally diverse settings in high-income countries. To illustrate, a study amongst a Somali population living in the UK (Fox, Aabe, Turner, Redwood, & Rai, 2016) reported findings that echo reports from populations resident in the horn or East of Africa (Gona et al., 2016; Tekola et al., 2016; Tilahun et al., 2016) regarding the perceptions of autism, experiences of stigma and unmet needs. Ethnic minority groups in high-income countries tend to be under-diagnosed for ASD and under-represented in autism research populations (Decoteau, 2017; Kawa et al., 2016; Sandy Magaña & Vanegas, 2017). Improving our understanding of the cultural dimensions of autism may thus inform initiatives to improve the identification, diagnosis and access to services of ethnic minority populations within high-income countries(La Roche, Bush, & D’Angelo, 2018).
An important limitation of this study is that the factors identified in the conceptual framework are of potential influence. This study aimed to set out which factors may influence the process of identification and diagnosis; it does not claim that each factor will play a role in all cultural settings. Future studies are warranted to examine the extent to which each of these factors are important across the globe. When examining cross-cultural differences across the globe, cultural and socioeconomic factors can be neatly intertwined. Therefore this paper has not tried to disentangle both types of influences. It is important to recognise that ‘culture’ does not follow country borders; large cultural differences may be observed within countries, and the cultural similarities may be smaller between neighbours than between diaspora groups living on different continents. Moreover, ‘culture’ is not static, and cultural differences or similarities may change over time (Kirmayer & Swartz, 2014). Kang-Yi et al (2018) for example highlight a diversity in attitudes within the Korean community in New York City, with some community members openly discussing autism and treating families with a child with autism like other families, while others are reluctant to talk about autism and are inclined to hide it (Kang-Yi et al., 2018). The study’s informants linked this diversity to generational differences, with the younger Korean immigrant population being more “open minded” about autism than the older generation. Thus, the salience of the factors identified in our conceptual framework are likely to be subject to change over time in any given population.
This framework was developed focusing on the cultural and contextual factors that may affect the family’s journey of identification, help-seeking and diagnosis of their child. This approach naturally emphasises individual and family-level factors; focusing instead on the health system would likely have identified additional clinician perspectives and systemic or macro factors not covered in our framework. Benefiting from a multidisciplinary approach, the paper sets out a conceptual framework covering both established cultural and contextual factors of influence on autism, as well as identifying factors that may be of influence based on sociocultural studies conducted in other disciplines. It is hoped that the framework and associated research suggestions may function as a springboard in the development of culturally and contextually appropriate screening and diagnostic instruments and interventions benefiting underserved populations across the world.
Lay summary.
The vast majority of autism research is conducted in western high-income settings. We therefore know relatively little of how culture and context can affect the identification, help-seeking and diagnosis of autism across the globe. This paper synthesises what is known from the autism research literature and a broader literature and maps out how culture and context may affect i) the expression, ii) recognition, iii) interpretation and iv) reporting of autism symptoms.
Acknowledgements
A. de Leeuw was supported by an Erasmus+ exchange programme grant while developing the conceptual framework presented. R.A. Hoekstra is supported by funding from Autism Speaks (#9817) and joint funding from the MRC (UK), DFID, Wellcome Trust and NIHR (#MR/P020844/1).
References
- Abubakar A, Ssewanyana D, de Vries PJ, Newton CR. Autism spectrum disorders in sub-Saharan Africa. The Lancet Psychiatry. 2016;3(9):800–802. doi: 10.1016/S2215-0366(16)30138-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abubakar A, Ssewanyana D, Newton CR. A Systematic Review of Research on Autism Spectrum Disorders in Sub-Saharan Africa. Behavioural Neurology. 2016;2:1–14. doi: 10.1155/2016/3501910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adnams CM. Perspectives of intellectual disability in South Africa: Epidemiology, policy, services for children and adults. Current Opinion in Psychiatry. 2010;23(5):436–440. doi: 10.1097/YCO.0b013e32833cfc2d. [DOI] [PubMed] [Google Scholar]
- Al Maskari TS, Melville CA, Willis DS. Systematic review: Cultural adaptation and feasibility of screening for autism in non-English speaking countries. International Journal of Mental Health Systems. 2018;12:22. doi: 10.1186/s13033-018-0200-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Dababneh KA, Al-Zboon EK, Baibers H. Jordanian parents’ beliefs about the causes of disability and the progress of their children with disabilities: Insights on mainstream schools and segregated centres. European Journal of Special Needs Education. 2016;32(3):362–376. doi: 10.1080/08856257.2016.1240341. [DOI] [Google Scholar]
- Alegría M, Alvarez K, Falgas-Bague I. Clinical Care Across Cultures: What Helps, What Hinders, What to Do. JAMA Psychiatry. 2017;74(9):865–866. doi: 10.1001/jamapsychiatry.2017.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alnemary FM, Aldhalaan HM, Simon-Cereijido G, Alnemary FM. Services for children with autism in the Kingdom of Saudi Arabia. Autism: The International Journal of Research and Practice. 2017;21(5):592–602. doi: 10.1177/1362361316664868. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edn. American Psychiatric Publishing; Arlington, VA: 2013. pp. 50–51. [Google Scholar]
- Angermeyer MC, Holzinger A, Carta MG, Schomerus G. Biogenetic explanations and public acceptance of mental illness: Systematic review of population studies. The British Journal of Psychiatry. 2011;199(5):367–372. doi: 10.1192/bjp.bp.110.085563. [DOI] [PubMed] [Google Scholar]
- Ashton-James CE, Kushlev K, Dunn EW. Parents Reap What They Sow: Child-Centrism and Parental Well-Being. Social Psychological and Personality Science. 2013;4(6):635–642. doi: 10.1177/1948550613479804. [DOI] [Google Scholar]
- Baghdadli A, Picot MC, Pascal C, Pry R, Aussilloux C. Relationship between age of recognition of first disturbances and severity in young children with autism. European Child & Adolescent Psychiatry. 2003;12(3):122–127. doi: 10.1007/s00787-003-0314-6. [DOI] [PubMed] [Google Scholar]
- Bakare MO, Munir KM. Excess of non-verbal cases of autism spectrum disorders presenting to orthodox clinical practice in Africa—A trend possibly resulting from late diagnosis and intervention. The South African Journal of Psychiatry: SAJP: The Journal of the Society of Psychiatrists of South Africa. 2011;17(4):118–120. [PMC free article] [PubMed] [Google Scholar]
- Barbaro J, Halder S. Early Identification of Autism Spectrum Disorder: Current Challenges and Future Global Directions. Current Developmental Disorders Reports. 2016;3(1):67–74. doi: 10.1007/s40474-016-0078-6. [DOI] [Google Scholar]
- Baron-Cohen S, Wheelwright S, Skinner R, Martin J, Clubley E. The autism-spectrum quotient (AQ): Evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. Journal of Autism and Developmental Disorders. 2001;31(1):5–17. doi: 10.1023/a:1005653411471. [DOI] [PubMed] [Google Scholar]
- Bazzano A, Zeldin A, Schuster E, Barrett C, Lehrer D. Vaccine-related beliefs and practices of parents of children with autism spectrum disorders. American Journal on Intellectual and Developmental Disabilities. 2012;117(3):233–242. doi: 10.1352/1944-7558-117.3.233. [DOI] [PubMed] [Google Scholar]
- Bello-Mojeed MA, Omigbodun OO, Bakare MO, Adewuya AO. Pattern of impairments and late diagnosis of autism spectrum disorder among a sub-Saharan African clinical population of children in Nigeria. Global Mental Health (Cambridge, England) 2017;4:e5. doi: 10.1017/gmh.2016.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernier R, Mao A, Yen J. Psychopathology, Families, and Culture: Autism. Child and Adolescent Psychiatric Clinics of North America. 2010;19(4):855–867. doi: 10.1016/j.chc.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Berry JW On Cross-Cultural Comparability. University of Sidney, Australia. International Journal of Psychology. 1969;4(2):119–128. [Google Scholar]
- Bishop-Fitzpatrick L, Kind AJH. A Scoping Review of Health Disparities in Autism Spectrum Disorder. Journal of Autism and Developmental Disorders. 2017;47(11):3380–3391. doi: 10.1007/s10803-017-3251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blacher J, Cohen SR, Azad G. In the eye of the beholder: Reports of autism symptoms by Anglo and Latino mothers. Research in Autism Spectrum Disorders. 2014;8(12):1648–1656. doi: 10.1016/j.rasd.2014.08.017. [DOI] [Google Scholar]
- Bornstein MH. Handbook of Parenting: Volume 4 Social Conditions and Applied Parenting. Psychology Press; 2005. [Google Scholar]
- Bornstein MH. Cultural Approaches to Parenting. Parenting, Science and Practice. 2012;12(2-3):212–221. doi: 10.1080/15295192.2012.683359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein MH. Parenting and child mental health: A cross-cultural perspective. World Psychiatry. 2013;12(3):258–265. doi: 10.1002/wps.20071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broady TR, Stoyles GJ, Morse C. Understanding carers’ lived experience of stigma: The voice of families with a child on the autism spectrum. Health & Social Care in the Community. 2017;25(1):224–233. doi: 10.1111/hsc.12297. [DOI] [PubMed] [Google Scholar]
- Brohan E, Slade M, Clement S, Thornicroft G. Experiences of mental illness stigma, prejudice and discrimination: A review of measures. BMC Health Services Research. 2010;10:80. doi: 10.1186/1472-6963-10-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruckner TA, Scheffler RM, Shen G, Yoon J, Chisholm D, Morris J, et al. Saxena S. The mental health workforce gap in low- and middle-income countries: A needs-based approach. Bulletin of the World Health Organization. 2011;89(3):184–194. doi: 10.2471/BLT.10.082784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buehning LJ, Peddecord KM. Vaccination Attitudes and Practices of Integrative Medicine Physicians. Alternative Therapies in Health and Medicine. 2017;23(1):46–54. [PubMed] [Google Scholar]
- Carruthers S, Kinnaird E, Rudra A, Smith P, Allison C, Auyeung B, et al. Hoekstra R. A cross-cultural study of autistic traits across India, Japan and the UK. Molecular Autism. 2018;9 doi: 10.1186/s13229-018-0235-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauce AM, Domenech-Rodríguez M, Paradise M, Cochran BN, Shea JM, Srebnik D, Baydar N. Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology. 2002;70(1):44–55. doi: 10.1037//0022-006x.70.1.44. [DOI] [PubMed] [Google Scholar]
- Chaidez V, Fernandez Y, Garcia E, Wang LW, Angkustsiri K, Krakowiak P, Hertz-Picciotto I, Hansen RL. Comparison of maternal beliefs about causes of autism spectrum disorder and association with utilization of services and treatments. Child: Care, Health and Development. 2018;44(6):916–925. doi: 10.1111/cch.12612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao R. Chinese and European-American cultural models of the self reflected in mothers’ child-rearing beliefs. Vol. 23. Ethos; 1995. pp. 328–54. (n.d.) [Google Scholar]
- Chawarska K, Paul R, Klin A, Hannigen S, Dichtel LE, Volkmar F. Parental Recognition of Developmental Problems in Toddlers with Autism Spectrum Disorders. Journal of Autism and Developmental Disorders. 2006;37(1):62–72. doi: 10.1007/s10803-006-0330-8. [DOI] [PubMed] [Google Scholar]
- Chen Y-W, Bundy AC, Cordier R, Chien Y-L, Einfeld SL. A cross-cultural exploration of the everyday social participation of individuals with autism spectrum disorders in Australia and Taiwan: An experience sampling study. Autism: The International Journal of Research and Practice. 2017;(2):231–241. doi: 10.1177/1362361316636756. [DOI] [PubMed] [Google Scholar]
- Chua A. Battle hymn of the tiger mom. NY: Penguin Press; 2011. [Google Scholar]
- Colbert AM, Webber J, Graham R. Factors that Influence Autism Knowledge in Hispanic Cultures: A Pilot Study. Journal of Racial and Ethnic Health Disparities. 2017;4(2):156–164. doi: 10.1007/s40615-016-0213-4. [DOI] [PubMed] [Google Scholar]
- Daley TC. From symptom recognition to diagnosis: Children with autism in urban India. Social Science & Medicine. 2004;58(7):1323–1335. doi: 10.1016/S0277-9536(03)00330-7. [DOI] [PubMed] [Google Scholar]
- Daley TC, Singhal N, Krishnamurthy V. Ethical considerations in conducting research on autism spectrum disorders in low and middle income countries. Journal of Autism and Developmental Disorders. 2013;43(9):2002–2014. doi: 10.1007/s10803-012-1750-2. [DOI] [PubMed] [Google Scholar]
- de Vries PJ. Thinking globally to meet local needs. Current Opinion Neurology. 2016;29(0) doi: 10.1097/WCO.0000000000000297. [DOI] [PubMed] [Google Scholar]
- Decoteau CL. The “Western disease”: Autism and Somali parents’ embodied health movements. Social Science & Medicine (1982) 2017;177:169–176. doi: 10.1016/j.socscimed.2017.01.064. [DOI] [PubMed] [Google Scholar]
- Dickerson AS, Rahbar MH, Pearson DA, Kirby RS, Bakian AV, Bilder DA, et al. Slay Wingate M. Autism spectrum disorder reporting in lower socioeconomic neighborhoods. Autism: The International Journal of Research and Practice. 2017;21(4):470–480. doi: 10.1177/1362361316650091. [DOI] [PubMed] [Google Scholar]
- Divan G, Vajaratkar V, Desai MU, Strik-Lievers L, Patel V. Challenges, Coping Strategies, and Unmet Needs of Families with a Child with Autism Spectrum Disorder in Goa, India. Autism Research. 2012;5(3):190–200. doi: 10.1002/aur.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohue MR, Childs AW, Richards M, Robins DL. Race influences parent report of concerns about symptoms of autism spectrum disorder. Autism: The International Journal of Research and Practice. 2017 doi: 10.1177/1362361317722030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin MS, Elsabbagh M, Barbaro J, Gladstone M, Happe F, Hoekstra RA, et al. Shih A. Autism screening and diagnosis in low resource settings: Challenges and opportunities to enhance research and services worldwide. Autism Research: Official Journal of the International Society for Autism Research. 2015;8(5):473–476. doi: 10.1002/aur.1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton J, McCay L, Semrau M, Chatterjee S, Baingana F, Araya R, et al. Saxena S. Scale up of services for mental health in low-income and middle-income countries. The Lancet. 2011;378(9802):1592–1603. doi: 10.1016/S0140-6736(11)60891-X. [DOI] [PubMed] [Google Scholar]
- Edwards CP. Children’s Play in Cross-Cultural Perspective: A New Look at the Six Cultures Study. Cross-Cultural Research. 2000;34(4):318–338. doi: 10.1177/106939710003400402. [DOI] [Google Scholar]
- Eggertson L. Lancet retracts 12-year-old article linking autism to MMR vaccines. CMAJ : Canadian Medical Association Journal. 2010;182(4):E199–E200. doi: 10.1503/cmaj.109-3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsabbagh M, Divan G, Koh Y-J, Kim YS, Kauchali S, Marcín C, et al. Fombonne E. Global Prevalence of Autism and Other Pervasive Developmental Disorders. Autism Research. 2012;5(3):160–179. doi: 10.1002/aur.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engle PL, Fernald LC, Alderman H, Behrman J, O’Gara C, Yousafzai A, et al. Iltus S. Strategies for reducing inequalities and improving developmental outcomes for young children in low-income and middle-income countries. The Lancet. 2011;378(9799):1339–1353. doi: 10.1016/S0140-6736(11)60889-1. [DOI] [PubMed] [Google Scholar]
- Ertem IO, Krishnamurthy V, Mulaudzi MC, Sguassero Y, Balta H, Gulumser O, et al. Forsyth BWC. Similarities and differences in child development from birth to age 3 years by sex and across four countries: A cross-sectional, observational study. The Lancet Global Health. 2018;6(3):e279–e291. doi: 10.1016/S2214-109X(18)30003-2. [DOI] [PubMed] [Google Scholar]
- Eseigbe EE, Nuhu FT, Sheikh TL, Eseigbe P, Sanni KA, Olisah VO. Knowledge of Childhood Autism and Challenges of Management among Medical Doctors in Kaduna State, Northwest Nigeria. Autism Research and Treatment. 2015 doi: 10.1155/2015/892301. 892301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrugia D. Exploring stigma: Medical knowledge and the stigmatisation of parents of children diagnosed with autism spectrum disorder. Sociology of Health & Illness. 2009;31(7):1011–1027. doi: 10.1111/j.1467-9566.2009.01174.x. [DOI] [PubMed] [Google Scholar]
- Farver JA, Shin YL. Social pretend play in Korean- and Anglo-American preschoolers. Child Development. 1997;68(3):544–556. [PubMed] [Google Scholar]
- Fox F, Aabe N, Turner K, Redwood S, Rai D. “It was like walking without knowing where I was going”: A Qualitative Study of Autism in a UK Somali Migrant Community. Journal of Autism and Developmental Disorders. 2016;47(2):305–315. doi: 10.1007/s10803-016-2952-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz L, Chambers N, von Isenburg M, de Vries PJ. Autism spectrum disorder in sub-saharan africa: A comprehensive scoping review. Autism Research: Official Journal of the International Society for Autism Research. 2017;10(5):723–749. doi: 10.1002/aur.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeth M, Sheppard E, Ramachandran R, Milne E. A cross-cultural comparison of autistic traits in the UK, India and Malaysia. Journal of Autism and Developmental Disorders. 2013;43(11):2569–2583. doi: 10.1007/s10803-013-1808-9. [DOI] [PubMed] [Google Scholar]
- Furnham A, Hamid A. Mental health literacy in non-western countries: A review of the recent literature. Mental Health Review Journal. 2014;19(2):84–98. doi: 10.1108/MHRJ-01-2013-0004. [DOI] [Google Scholar]
- Gaebel W, Roessler W, Sartorius N. The Stigma of Mental Illness—End of the Story? Springer; 2017. [Google Scholar]
- Ganasen KA, Parker S, Hugo CJ, Stein DJ, Emsley RA, Seedat S. Mental health literacy: Focus on developing countries. African Journal of Psychiatry. 2008;11(1):23–28. doi: 10.4314/ajpsy.v11i1.30251. [DOI] [PubMed] [Google Scholar]
- Gielen UP, Roopnarine JL. Childhood and Adolescence: Cross-Cultural Perspectives and Applications, 2nd Edition: Cross-Cultural Perspectives and Applications. ABC-CLIO; 2016. [Google Scholar]
- Goin-Kochel RP, Mire SS, Dempsey AG, Fein RH, Guffey D, Minard CG, et al. Boom JA. Parental report of vaccine receipt in children with autism spectrum disorder: Do rates differ by pattern of ASD onset? Vaccine. 2016;34(11):1335–1342. doi: 10.1016/j.vaccine.2016.02.008. [DOI] [PubMed] [Google Scholar]
- Gona JK, Newton CR, Rimba KK, Mapenzi R, Kihara M, Vijver FV, Abubakar A. Challenges and coping strategies of parents of children with autism on the Kenyan coast. 2016;16(2):3517. [PMC free article] [PubMed] [Google Scholar]
- Gona Joseph K, Newton CR, Rimba K, Mapenzi R, Kihara M, Vijver de FJRV, Abubakar A. Parents’ and Professionals’ Perceptions on Causes and Treatment Options for Autism Spectrum Disorders (ASD) in a Multicultural Context on the Kenyan Coast. PLOS ONE. 2015;10(8):e0132729. doi: 10.1371/journal.pone.0132729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: Audit of primary sources. BMJ (Clinical Research Ed) 2005;331(7524):1064–1065. doi: 10.1136/bmj.38636.593461.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinker RR, Chambers N, Njongwe N, Lagman A, Guthrie Stronach, et al. Wetherby “Communities” in Community Engagement: Lessons Learned From Autism Research in South Korea and South Africa. Autism Research. 2012;5(3):201–210. doi: 10.1002/aur.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinker RR, Cho K. Border Children: Interpreting Autism Spectrum Disorder in South Korea. Ethos. 2013;41(1):46–74. doi: 10.1111/etho.12002. [DOI] [Google Scholar]
- Grinker RR, Kang-Yi CD, Ahmann C, Beidas RS, Lagman A, Mandell DS. Cultural Adaptation and Translation of Outreach Materials on Autism Spectrum Disorder. Journal of Autism and Developmental Disorders. 2015;45(8):2329–2336. doi: 10.1007/s10803-015-2397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guler J, de Vries PJ, Seris N, Shabalala N, Franz L. The importance of context in early autism intervention: A qualitative South African study. Autism: The International Journal of Research and Practice. 2017 doi: 10.1177/1362361317716604. 1362361317716604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gureje O, Nortje G, Makanjuola V, Oladeji BD, Seedat S, Jenkins R. The role of global traditional and complementary systems of medicine in the treatment of mental health disorders. Lancet Psychiatry. 2015;2:168–177. doi: 10.1016/S2215-0366(15)00013-9. [DOI] [PubMed] [Google Scholar]
- Guthrie W, Wallis K, Bennett A, Brooks E, Dudley J, Gerdes M, et al. Miller JS. Accuracy of Autism Screening in a Large Pediatric Network. Pediatrics. 2019;144(4) doi: 10.1542/peds.2018-3963. [DOI] [PubMed] [Google Scholar]
- Ha VS, Whittaker A, Whittaker M, Rodger S. Living with autism spectrum disorder in Hanoi, Vietnam. Social Science & Medicine. 2014;120:278–285. doi: 10.1016/j.socscimed.2014.09.038. [DOI] [PubMed] [Google Scholar]
- Hadidi MS, Khateeb JMA. Special Education in Arab Countries: Current challenges. International Journal of Disability, Development and Education. 2015;62(5):518–530. doi: 10.1080/1034912X.2015.1049127. [DOI] [Google Scholar]
- Hahler E-M, Elsabbagh M. Autism: A Global Perspective. Current Developmental Disorders Reports. 2014;2(1):58–64. doi: 10.1007/s40474-014-0033-3. [DOI] [Google Scholar]
- Hailemichael Y, Hailemariam D, Tirfessa K, Docrat S, Alem A, Medhin G, et al. Hanlon C. Catastrophic out-of-pocket payments for households of people with severe mental disorder: A comparative study in rural Ethiopia. International Journal of Mental Health Systems. 2019;13:39. doi: 10.1186/s13033-019-0294-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamdani SU, Akhtar P, Zill-E-Huma null, Nazir H, Minhas FA, Sikander S, et al. Rahman A. WHO Parents Skills Training (PST) programme for children with developmental disorders and delays delivered by Family Volunteers in rural Pakistan: Study protocol for effectiveness implementation hybrid cluster randomized controlled trial. Vol. 4. Global Mental Health (Cambridge, England); 2017. p. e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamdani SU, Minhas FA, Iqbal Z, Rahman A. Model for Service Delivery for Developmental Disorders in Low-Income Countries. Pediatrics. 2015;136(6):1166–1172. doi: 10.1542/peds.2015-0861. [DOI] [PubMed] [Google Scholar]
- Harrison AJ, Long KA, Tommet DC, Jones RN. Examining the role of race, ethnicity, and gender on social and behavioral ratings within the Autism Diagnostic Observation Schedule. Journal of Autism and Developmental Disorders. 2017;47(9):2770–2782. doi: 10.1007/s10803-017-3176-3. [DOI] [PubMed] [Google Scholar]
- Heys M, Alexander A, Medeiros E, Tumbahangphe KM, Gibbons F, Shrestha R, et al. Pellicano E. Understanding parents’ and professionals’ knowledge and awareness of autism in Nepal. Autism: The International Journal of Research and Practice. 2017;21(4):436–449. doi: 10.1177/1362361316646558. [DOI] [PubMed] [Google Scholar]
- Hoekstra RA, Bayouh FG, Gebru BT, Kinfe M, Mihretu A, Adamu W, et al. Hanlon C. The face of autism in Ethiopia: The expression, recognition, reporting and interpretation of autism symptoms in the Ethiopian context. International Society for Autism Research (INSAR) meeting; Rotterdam. 2018. May, [Google Scholar]
- Hoekstra RA, Girma F, Tekola B, Yenus Z. Nothing about us without us: The importance of local collaboration and engagement in the global study of autism. BJPsych International. 2018;15(2):40–43. doi: 10.1192/bji.2017.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoven CW, Doan T, Musa GJ, Jaliashvili T, Duarte CS, Ovuga E, et al. Force WAT. Worldwide child and adolescent mental health begins with awareness: A preliminary assessment in nine countries. International Review of Psychiatry. 2008;20(3):261–270. doi: 10.1080/09540260801995950. [DOI] [PubMed] [Google Scholar]
- Hsu Y, Tsai S, Hsieh M, Jenks MS, Tsai C, Hsu M. On my own: A qualitative phenomenological study of mothers of young children with autism spectrum disorder in Taiwan. Journal of Applied Research in Intellectual Disabilities. 2017;30(1):147–156. doi: 10.1111/jar.12229. [DOI] [PubMed] [Google Scholar]
- Ilias K, Liaw JHJ, Cornish K, Park MS-A, Golden KJ. Wellbeing of mothers of children with “A-U-T-I-S-M” in Malaysia: An interpretative phenomenological analysis study. Journal of Intellectual and Developmental Disability. 2017;42(1):74–89. doi: 10.3109/13668250.2016.1196657. [DOI] [Google Scholar]
- Irarrazaval M, García R, Riesle S, Moyano A, Cabezas M, Rattazzi A, et al. Rosoli A. 5.17 Access to Services, Priorities, and Challenges in Caregivers of Persons With Autism. Journal of the American Academy of Child & Adolescent Psychiatry. 2017;56(10):S259. doi: 10.1016/j.jaac.2017.09.300. [DOI] [Google Scholar]
- Jacobs B, Ir P, Bigdeli M, Annear PL, Van Damme W. Addressing access barriers to health services: An analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy and Planning. 2012;27(4):288–300. doi: 10.1093/heapol/czr038. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. “Mental health literacy”: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. The Medical Journal of Australia. 1997;166(4):182–186. doi: 10.5694/j.1326-5377.1997.tb140071.x. [DOI] [PubMed] [Google Scholar]
- K DP, Srinath DS, Seshadri DSP, Girimaji DSC, Kommu DJVS. Lost time-Need for more awareness in early intervention of autism spectrum disorder. Asian Journal of Psychiatry. 2017;25:13–15. doi: 10.1016/j.ajp.2016.07.021. [DOI] [PubMed] [Google Scholar]
- Kakooza-Mwesige A, Ssebyala K, Karamagi C, Kiguli S, et al. Adaptation of the “ten questions” to screen for autism and other neurodevelopmental disorders in Uganda. Autism. 2014;18(4):447–457. doi: 10.1177/1362361313475848. [DOI] [PubMed] [Google Scholar]
- Kamio Y, Inada N, Koyama T, Inokuchi E, Tsuchiya K, Kuroda M. Effectiveness of Using the Modified Checklist for Autism in Toddlers in Two-Stage Screening of Autism Spectrum Disorder at the 18-Month Health Check-Up in Japan. Journal of Autism and Developmental Disorders. 2014;44(1):194–203. doi: 10.1007/s10803-013-1864-1. [DOI] [PubMed] [Google Scholar]
- Kang-Yi CD, Grinker RR, Beidas R, Agha A, Russell R, Shah SB, et al. Mandell DS. Influence of Community-Level Cultural Beliefs about Autism on Families’ and Professionals’ Care for Children: Transcultural Psychiatry. 2018 doi: 10.1177/1363461518779831. 1363461518779831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawa R, Saemundsen E, Lóa Jónsdóttir S, Hellendoorn A, Lemcke S, Canal-Bedia R, et al. Moilanen I. European studies on prevalence and risk of autism spectrum disorders according to immigrant status-a review. European Journal of Public Health. 2016;27(1):101–110. doi: 10.1093/eurpub/ckw206. [DOI] [PubMed] [Google Scholar]
- Khowaja MK, Hazzard AP, Robins DL. Sociodemographic Barriers to Early Detection of Autism: Screening and Evaluation Using the M-CHAT, M-CHAT-R, and Follow-Up. Journal of Autism and Developmental Disorders. 2015;45(6):1797–1808. doi: 10.1007/s10803-014-2339-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Rahman A. Child and adolescent mental health worldwide: Evidence for action. Lancet (London, England) 2011;378(9801):1515–1525. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- Kim SH, Kim YS, Koh Y-J, Lim E-C, Kim S-J, Leventhal BL. Often Asked but Rarely Answered: Can Asians Meet DSM-5/ICD-10 Autism Spectrum Disorder Criteria? Journal of Child and Adolescent Psychopharmacology. 2016;26(9):835–842. doi: 10.1089/cap.2016.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirmayer LJ, Swartz L. In: Global Mental Health Principles and Practice. Patel V, Minas H, Cohen A, Prince MJ, editors. Oxford University Press; 2014. Culture and Global Mental Health (chapter 3) [Google Scholar]
- Kishore MT, Basu A. Early concerns of mothers of children later diagnosed with autism: Implications for early identification. Research in Autism Spectrum Disorders. 2011;5(1):157–163. doi: 10.1016/j.rasd.2010.03.005. [DOI] [Google Scholar]
- Klasen H, Goodman R. Parents and GPs at cross-purposes over hyperactivity: A qualitative study of possible barriers to treatment. The British Journal of General Practice. 2000;50(452):199–202. [PMC free article] [PubMed] [Google Scholar]
- Kleinman A. Concepts and a model for the comparison of medical systems as cultural systems. Social Science & Medicine. 1978;12(2B):85–95. doi: 10.1016/0160-7987(78)90014-5. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Anthropology and psychiatry. The role of culture in cross-cultural research on illness. The British Journal of Psychiatry: The Journal of Mental Science. 1987;151:447–454. doi: 10.1192/bjp.151.4.447. [DOI] [PubMed] [Google Scholar]
- Kutcher S, Wei Y, Coniglio C. Mental Health Literacy. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie. 2016;61(3):154–158. doi: 10.1177/0706743715616609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Roche MJ, Bush HH, D’Angelo E. The assessment and treatment of autism spectrum disorder: A cultural examination. Practice Innovations. 2018;3(2):107–122. doi: 10.1037/pri0000067. [DOI] [Google Scholar]
- Lai M-C, Lombardo MV, Auyeung B, Chakrabarti B, Baron-Cohen S. Sex/gender differences and autism: Setting the scene for future research. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(1):11–24. doi: 10.1016/j.jaac.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai M-C, Lombardo MV, Baron-Cohen S. Autism. Lancet (London, England) 2014;383(9920):896–910. doi: 10.1016/S0140-6736(13)61539-1. [DOI] [PubMed] [Google Scholar]
- Lai M-C, Lombardo MV, Chakrabarti B, Baron-Cohen S. Subgrouping the autism “spectrum”: Reflections on DSM-5. PLoS Biology. 2013;11(4):e1001544. doi: 10.1371/journal.pbio.1001544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert MC, Weisz JR, Knight F, Desrosiers MF, Overly K, Thesiger C. Jamaican and American adult perspectives on child psychopathology: Further exploration of the threshold model. Journal of Consulting and Clinical Psychology. 1992;60(1):146–149. doi: 10.1037//0022-006x.60.1.146. [DOI] [PubMed] [Google Scholar]
- Lau WY-P, Gau SS-F, Chiu Y-N, Wu Y-Y, Chou W-J, Liu S-K, Chou M-C. Psychometric properties of the Chinese version of the Autism Spectrum Quotient (AQ) Research in Developmental Disabilities. 2013;34(1):294–305. doi: 10.1016/j.ridd.2012.08.005. [DOI] [PubMed] [Google Scholar]
- Le Roux J. Effective educators are culturally competent communicators. Intercultural Education. 2002 [Google Scholar]
- Leijten P, Raaijmakers MAJ, Orobio de Castro B, Matthys W. Ethnic differences in problem perception: Immigrant mothers in a parenting intervention to reduce disruptive child behavior. The American Journal of Orthopsychiatry. 2016;86(3):323–331. doi: 10.1037/ort0000142. [DOI] [PubMed] [Google Scholar]
- Lillard A, Pinkham A. In: Blackwell Handbook of Childhood Cognitive Development. 2nd ed. Goswami U, editor. 2011. Pretend Play and Cognitive Development; pp. 285–311. [Google Scholar]
- Lofthouse N, Hendren R, Hurt E, Arnold LE, Butter E. A Review of Complementary and Alternative Treatments for Autism Spectrum Disorders. Autism Research and Treatment. 2012 doi: 10.1155/2012/870391. 87039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotter V. Childhood Autism in Africa. Journal of Child Psychology and Psychiatry. 1978;19(3):231–244. doi: 10.1111/j.1469-7610.1978.tb00466.x. [DOI] [PubMed] [Google Scholar]
- Magaña S, Parish SL, Son E. Have Racial and Ethnic Disparities in the Quality of Health Care Relationships Changed for Children With Developmental Disabilities and ASD? American Journal on Intellectual and Developmental Disabilities. 2015;120(6):504–513. doi: 10.1352/1944-7558-120.6.504. [DOI] [PubMed] [Google Scholar]
- Magaña S, Smith LE. The Use of the Autism Diagnostic Interview-Revised with a Latino Population of Adolescents and Adults with Autism. Journal of Autism and Developmental Disorders. 2013;43(5):1098–1105. doi: 10.1007/s10803-012-1652-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaña, Sandy, Vanegas SB. Diagnostic Utility of the ADI-R and DSM-5 in the Assessment of Latino Children and Adolescents. Journal of Autism and Developmental Disorders. 2017;47(5):1278–1287. doi: 10.1007/s10803-017-3043-2. [DOI] [PubMed] [Google Scholar]
- Magnusson DM, Minkovitz CS, Kuhlthau KA, Caballero TM, Mistry KB. Beliefs Regarding Development and Early Intervention Among Low-Income African American and Hispanic Mothers. Pediatrics. 2017;140(5) doi: 10.1542/peds.2017-2059. [DOI] [PubMed] [Google Scholar]
- Mak WWS, Cheung RYM. Affiliate stigma among caregivers of people with intellectual disability or mental illness. Journal of Applied Research in Intellectual Disabilities. 2008;21(6):532–545. doi: 10.1111/j.1468-3148.2008.00426.x. [DOI] [Google Scholar]
- Mandell DS, Novak M. The role of culture in families’ treatment decisions for children with autism spectrum disorders. Mental Retardation and Developmental Disabilities Research Reviews. 2005;11(2):110–115. doi: 10.1002/mrdd.20061. [DOI] [PubMed] [Google Scholar]
- Manor-Binyamini I, Shoshana A. Listening to Bedouin mothers of children with autism. Culture, Medicine, and Psychiatry: An International Journal of Cross-Cultural Health Research. 2018;42(2):401–418. doi: 10.1007/s11013-018-9567-x. [DOI] [PubMed] [Google Scholar]
- Marlow M, Servili C, Tomlinson M. A review of screening tools for the identification of autism spectrum disorders and developmental delay in infants and young children: Recommendations for use in low- and middle-income countries. Autism Research. 2019;12(2):176–199. doi: 10.1002/aur.2033. [DOI] [PubMed] [Google Scholar]
- Masri AT, Al Suluh N, Nasir R. Diagnostic delay of autism in Jordan: Review of 84 cases. The Libyan Journal of Medicine. 2013;8:21725. doi: 10.3402/ljm.v8i0.21725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheis M, Matson JL, Burns CO, Jiang X, Peters WJ, Moore M, et al. Estabillo J. Factors related to parental age of first concern in toddlers with autism spectrum disorder. Developmental Neurorehabilitation. 2017;20(4):228–235. doi: 10.1080/17518423.2016.1211186. [DOI] [PubMed] [Google Scholar]
- Matson JL, Matheis M, Burns CO, Esposito G, Venuti P, Pisula E, et al. Goldin RL. Examining cross-cultural differences in autism spectrum disorder: A multinational comparison from Greece, Italy, Japan, Poland, and the United States. European Psychiatry. 2017;42:70–76. doi: 10.1016/j.eurpsy.2016.10.007. [DOI] [PubMed] [Google Scholar]
- Matson J, Worley Fodstad, Chung Suh Jhin, et al. Furniss: A multinational study examining the cross cultural differences in reported symptoms of autism spectrum disorders: Israel, South Korea, the United Kingdom, and the United States of America. Research in Autism Spectrum Disorders. 2011;5(4):1598–1604. doi: 10.1016/j.rasd.2011.03.007. [DOI] [Google Scholar]
- Milačić-Vidojević I, Gligorović M, Dragojević N. Tendency towards stigmatization of families of a person with autistic spectrum disorders. The International Journal of Social Psychiatry. 2014;60(1):63–70. doi: 10.1177/0020764012463298. [DOI] [PubMed] [Google Scholar]
- Minhas A, Vajaratkar V, Divan G, Hamdani SU, Leadbitter K, Taylor C, et al. Rahman A. Parents’ perspectives on care of children with autistic spectrum disorder in South Asia – Views from Pakistan and India. International Review of Psychiatry. 2015;27(3):247–256. doi: 10.3109/09540261.2015.1049128. [DOI] [PubMed] [Google Scholar]
- Mirza I, Tareen A, Davidson LL, Rahman A. Community management of intellectual disabilities in Pakistan: A mixed methods study. Journal of Intellectual Disability Research : JIDR. 2009;53(6):559–570. doi: 10.1111/j.1365-2788.2009.01176.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell C, Holdt N. The search for a timely diagnosis: Parents’ experiences of their child being diagnosed with an Autistic Spectrum Disorder. Journal of Child & Adolescent Mental Health. 2014;26(1):49–62. doi: 10.2989/17280583.2013.849606. [DOI] [PubMed] [Google Scholar]
- Mitter N, Ali A, Scior K. Stigma experienced by families of individuals with intellectual disabilities and autism: A systematic review. Research in Developmental Disabilities. 2019;89:10–21. doi: 10.1016/j.ridd.2019.03.001. [DOI] [PubMed] [Google Scholar]
- Montiel-Nava C, Chacín JA, González-Ávila Z. Age of diagnosis of autism spectrum disorder in Latino children: The case of Venezuelan children. Autism. 2017;21(5):573–580. doi: 10.1177/1362361317701267. [DOI] [PubMed] [Google Scholar]
- Munir K, Lavelle TA, Helm DT, Thompson D, Prestt J, Azeem MW. Autism: A global framework for action. Report of the WISH Autism Forum. 2016 (n.d.) [Google Scholar]
- Nichter M. Idioms of Distress Revisited. Culture, Medicine, and Psychiatry. 2010;34(2):401–416. doi: 10.1007/s11013-010-9179-6. [DOI] [PubMed] [Google Scholar]
- Norbury, Sparks Difference or Disorder? Cultural Issues in Understanding Neurodevelopmental Disorders. Developmental Psychology. 2013;49(1):45–58. doi: 10.1037/a0027446. [DOI] [PubMed] [Google Scholar]
- Obeid R, Daou N, DeNigris D, Shane-Simpson C, Brooks PJ, Gillespie-Lynch K. A Cross-Cultural Comparison of Knowledge and Stigma Associated with Autism Spectrum Disorder Among College Students in Lebanon and the United States. Journal of Autism and Developmental Disorders. 2015;45(11):3520–3536. doi: 10.1007/s10803-015-2499-1. [DOI] [PubMed] [Google Scholar]
- Ooi KL, Ong YS, Jacob SA, Khan TM. A meta-synthesis on parenting a child with autism. Neuropsychiatric Disease and Treatment. 2016;12:745–762. doi: 10.2147/NDT.S100634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadopoulos C, Lodder A, Constantinou G, Randhawa G. Systematic review of the relationship between autism stigma and informal caregiver mental health. Journal of Autism and Developmental Disorders. 2019;49(4):1665–1685. doi: 10.1007/s10803-018-3835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S, Lee Y, Kim CE. Korean adults’ beliefs about and social distance toward attention-deficit hyperactivity disorder, Tourette syndrome, and autism spectrum disorder. Psychiatry Research. 2018;269:633–639. doi: 10.1016/j.psychres.2018.08.023. [DOI] [PubMed] [Google Scholar]
- Patel V, Mann A. Etic and emic criteria for non-psychotic mental disorder: A study of the CISR and care provider assessment in Harare. Social Psychiatry and Psychiatric Epidemiology. 1997;32(2):84–89. doi: 10.1007/BF00788925. [DOI] [PubMed] [Google Scholar]
- Perera H, Wijewardena K, Aluthwelage R. Screening of 18-24-month-old children for autism in a semi-urban community in Sri Lanka. Journal of Tropical Pediatrics. 2009;55(6):402–405. doi: 10.1093/tropej/fmp031. [DOI] [PubMed] [Google Scholar]
- Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Hafizur Rahman M. Poverty and Access to Health Care in Developing Countries. Annals of the New York Academy of Sciences. 2008;1136(1):161–171. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- Phelan JC. Geneticization of deviant behavior and consequences for stigma: The case of mental illness. Journal of Health and Social Behavior. 2005;46(4):307–322. doi: 10.1177/002214650504600401. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Yang LH, Cruz-Rojas R. Effects of attributing serious mental illnesses to genetic causes on orientations to treatment. Psychiatric Services (Washington, DC) 2006;57(3):382–387. doi: 10.1176/appi.ps.57.3.382. [DOI] [PubMed] [Google Scholar]
- Pippins JR, Alegría M, Haas JS. Association between language proficiency and the quality of primary care among a national sample of insured Latinos. Medical Care. 2007;45(11):1020–1025. doi: 10.1097/MLR.0b013e31814847be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental health. Lancet (London, England) 2007;370(9590):859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- Ravindran N, Myers BJ. Beliefs and Practices Regarding Autism in Indian Families Now Settled Abroad An Internet Survey. Focus on Autism and Other Developmental Disabilities. 2013;28(1):44–53. doi: 10.1177/1088357612458970. [DOI] [Google Scholar]
- Reardon T, Harvey K, Baranowska M, O’Brien D, Smith L, Creswell C. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. European Child & Adolescent Psychiatry. 2017;26(6):623–647. doi: 10.1007/s00787-016-0930-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice CE, Lee L-C. Expanding the global reach of research in autism. Autism: The International Journal of Research and Practice. 2017;21(5):515–517. doi: 10.1177/1362361317704603. [DOI] [PubMed] [Google Scholar]
- Rogler LH. Culturally sensitizing psychiatric diagnosis. A framework for research. The Journal of Nervous and Mental Disease. 1993;181(7):401–408. doi: 10.1097/00005053-199307000-00001. [DOI] [PubMed] [Google Scholar]
- Rosenberg RE, Landa R, Law JK, Stuart EA, Law PA. Factors affecting age at initial autism spectrum disorder diagnosis in a national survey. Autism Research and Treatment. 2011;2011 doi: 10.1155/2011/874619. 874619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruparelia K, Abubakar A, Badoe E, Bakare M, Visser K, Chugani DC, et al. Newton CR. Autism Spectrum Disorders in Africa: Current Challenges in Identification, Assessment, and Treatment. Journal of Child Neurology. 2016;31(8):1018–1026. doi: 10.1177/0883073816635748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samadi SA, McConkey R. Screening for Autism in Iranian Preschoolers: Contrasting M-CHAT and a Scale Developed in Iran. Journal of Autism and Developmental Disorders. 2015;45(9):2908–2916. doi: 10.1007/s10803-015-2454-1. [DOI] [PubMed] [Google Scholar]
- Saraceno B, Ommeren M, van Batniji R, Cohen A, Gureje O, Mahoney J, et al. Underhill C. Barriers to improvement of mental health services in low-income and middle-income countries. The Lancet. 2007;370(9593):1164–1174. doi: 10.1016/S0140-6736(07)61263-X. [DOI] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: Scarcity, inequity, and inefficiency. Lancet (London, England) 2007;370(9590):878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- Scale up services for mental disorders: A call for action. The Lancet. 2007;370(9594):1241–1252. doi: 10.1016/S0140-6736(07)61242-2. [DOI] [PubMed] [Google Scholar]
- Scambler G, Hopkins A. Being epileptic: Coming to terms with stigma. Sociology of Health & Illness. 1986;8(1):26–43. doi: 10.1111/1467-9566.ep11346455. [DOI] [Google Scholar]
- Scarpa A, Reyes NM, Patriquin MA, Lorenzi J, Hassenfeldt TA, Desai VJ, Kerkering KW. The modified checklist for autism in toddlers: Reliability in a diverse rural American sample. Journal of Autism and Developmental Disorders. 2013;43(10):2269–2279. doi: 10.1007/s10803-013-1779-x. [DOI] [PubMed] [Google Scholar]
- Sell NK, Giarelli E, Blum N, Hanlon AL, Levy SE. A comparison of autism spectrum disorder DSM-IV criteria and associated features among African American and white children in Philadelphia County. Disability and Health Journal. 2012;5(1):9–17. doi: 10.1016/j.dhjo.2011.08.002. [DOI] [PubMed] [Google Scholar]
- Shaked M. The social trajectory of illness: Autism in the ultraorthodox community in Israel. Social Science & Medicine. 2005;61(10):2190–2200. doi: 10.1016/j.socscimed.2005.04.022. [DOI] [PubMed] [Google Scholar]
- Shaked M, Bilu Y. Grappling with affliction: Autism in the Jewish ultraorthodox community in Israel. Culture, Medicine and Psychiatry. 2006;30(1):1–27. doi: 10.1007/s11013-006-9006-2. [DOI] [PubMed] [Google Scholar]
- Shuster J, Perry A, Bebko J, Toplak ME. Review of Factor Analytic Studies Examining Symptoms of Autism Spectrum Disorders. Journal of Autism and Developmental Disorders. 2014;44(1):90–110. doi: 10.1007/s10803-013-1854-3. [DOI] [PubMed] [Google Scholar]
- Shyu Y-IL, Tsai J-L, Tsai W-C. Explaining and Selecting Treatments for Autism: Parental Explanatory Models in Taiwan. Journal of Autism and Developmental Disorders. 2010;40(11):1323–1331. doi: 10.1007/s10803-010-0991-1. [DOI] [PubMed] [Google Scholar]
- Smeeth L, Cook C, Fombonne E, Heavey L, Rodrigues LC, Smith PG, Hall AJ. MMR vaccination and pervasive developmental disorders: A case-control study. Lancet (London, England) 2004;364(9438):963–969. doi: 10.1016/S0140-6736(04)17020-7. [DOI] [PubMed] [Google Scholar]
- Smith L, Malcolm-Smith S, Vries de PJ. Translation and cultural appropriateness of the Autism Diagnostic Observation Schedule-2 in Afrikaans. Autism. 2017;21(5):552–563. doi: 10.1177/1362361316648469. [DOI] [PubMed] [Google Scholar]
- Someki F, Torii M, Brooks PJ, Koeda T, Gillespie-Lynch K. Stigma associated with autism among college students in Japan and the United States: An online training study. Research in Developmental Disabilities. 2018;76:88–98. doi: 10.1016/j.ridd.2018.02.016. [DOI] [PubMed] [Google Scholar]
- Song J, Leventhal BL, Koh YJ, Cheon KA, Hong HJ, Kim YK, et al. Kim YS. Cross-Cultural Aspect of Behavior Assessment System for Children-2, Parent Rating Scale-Child: Standardization in Korean Children. Yonsei Medical Journal. 2017;58(2):439–448. doi: 10.3349/ymj.2017.58.2.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soto S, Linas K, Jacobstein D, Biel M, Migdal T, Anthony BJ. A review of cultural adaptations of screening tools for autism spectrum disorders. Autism: The International Journal of Research and Practice. 2015;19(6):646–661. doi: 10.1177/1362361314541012. [DOI] [PubMed] [Google Scholar]
- Stewart LA, Lee L-C. Screening for autism spectrum disorder in low- and middle-income countries: A systematic review. Autism. 2017 doi: 10.1177/1362361316677025. 1362361316677025. [DOI] [PubMed] [Google Scholar]
- Street RL, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: Personal and ethnic dimensions of shared identity. Annals of Family Medicine. 2008; 6(3):198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X, Allison C, Auyeung B, Matthews FE, Baron-Cohen S, Brayne C. Service provision for autism in mainland China: Preliminary mapping of service pathways. Social Science & Medicine. 2013;98:87–94. doi: 10.1016/j.socscimed.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tait K, Fung F, Hu A, Sweller N, Wang W. Understanding Hong Kong Chinese Families’ Experiences of an Autism/ASD Diagnosis. Journal of Autism and Developmental Disorders. 2016;46(4):1164–1183. doi: 10.1007/s10803-015-2650-z. [DOI] [PubMed] [Google Scholar]
- Tekola B, Baheretibeb Y, Roth I, Tilahun D, Fekadu A, Hanlon C, Hoekstra RA. Challenges and opportunities to improve autism services in low-income countries: Lessons from a situational analysis in Ethiopia. Global Mental Health. 2016;1(3):e21. doi: 10.1017/gmh.2016.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, et al. Henderson C. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet. 2016;387(10023):1123–1132. doi: 10.1016/S0140-6736(15)00298-6. [DOI] [PubMed] [Google Scholar]
- Tilahun D, Fekadu A, Tekola B, Araya M, Roth I, Davey B, et al. Hoekstra RA. Ethiopian community health workers’ beliefs and attitudes towards children with autism: Impact of a brief training intervention. Autism: The International Journal of Research and Practice. 2017 doi: 10.1177/1362361317730298. [DOI] [PubMed] [Google Scholar]
- Tilahun D, Hanlon C, Fekadu A, Tekola B, Baheretibeb Y, Hoekstra RA. Stigma, explanatory models and unmet needs of caregivers of children with developmental disorders in a low-income African country: A cross-sectional facility-based survey. BMC Health Services Research. 2016;16:152. doi: 10.1186/s12913-016-1383-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNESCO institute for statistics. Literacy Rates Continue to Rise from One Generation to the Next. 2017 September; Factsheet no. 45. [Google Scholar]
- United Nations, Department of Economic and Social Affairs. Trends in International Migrant Stock: Migrants by Destination and Origin (United Nations database, POP/DB/MIG/Stock/Rev) 2015 [Google Scholar]
- United Nations Economic and Social Council. ECOSOC Annual Ministerial Review. Regional Preparatory Meeting on Promoting Health Literacy Beijing; China. 2009. Apr, pp. 29–30. (n.d.) [Google Scholar]
- Vanegas SB, Magaña S, Morales M, McNamara E. Clinical Validity of the ADI-R in a US-Based Latino Population. Journal of Autism and Developmental Disorders. 2016;46(5):1623–1635. doi: 10.1007/s10803-015-2690-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakabayashi A, Baron-Cohen S, Wheelwright S, Tojo Y. The Autism-Spectrum Quotient (AQ) in Japan: A cross-cultural comparison. Journal of Autism and Developmental Disorders. 2006;36(2):263–270. doi: 10.1007/s10803-005-0061-2. [DOI] [PubMed] [Google Scholar]
- Weisberg DS. Pretend play. Wiley Interdisciplinary Reviews: Cognitive Science. 2015;6(3):249–261. doi: 10.1002/wcs.1341. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Suwanlert S, Chaiyasit W, Weiss B, Walter BR, Anderson WW. Thai and American perspectives on over- and undercontrolled child behavior problems: Exploring the threshold model among parents, teachers, and psychologists. Journal of Consulting and Clinical Psychology. 1988;56(4):601–609. doi: 10.1037//0022-006x.56.4.601. [DOI] [PubMed] [Google Scholar]
- Werner S, Shulman C. Does type of disability make a difference in affiliate stigma among family caregivers of individuals with autism, intellectual disability or physical disability? Journal of Intellectual Disability Research. 2015;59(3):272–283. doi: 10.1111/jir.12136. [DOI] [PubMed] [Google Scholar]
- West EA, Travers JC, Kemper TD, Liberty LM, Cote DL, McCollow MM, Brusnahan LLS. Racial and Ethnic Diversity of Participants in Research Supporting Evidence-Based Practices for Learners With Autism Spectrum Disorder. The Journal of Special Education. 2016;50(3):151–163. doi: 10.1177/0022466916632495. [DOI] [Google Scholar]
- WHO. Developmental difficulties in early childhood: Prevention, early identification, assessment and intervention in low- and middle-income countries: a review. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- WHO. ICD-11 International Classification of Diseases for Mortality and Morbidity Statistics, Eleventh Revision. 2018. Jun, [Google Scholar]
- WHO/UNEP Health and Environment Linkages Initiative (HELI) Health Environment: Managing the linkages for sustainable development: A toolkit for decision-makers: Synthesis report. 2008. [Google Scholar]
- Wolff ER, Madlon-Kay DJ. Childhood vaccine beliefs reported by Somali and non-Somali parents. Journal of the American Board of Family Medicine: JABFM. 2014;27(4):458–464. doi: 10.3122/jabfm.2014.04.130275. [DOI] [PubMed] [Google Scholar]
- World Bank. World Development Indicators. Washington, DC: The World Bank; 2015. (n.d.) [Google Scholar]
- World Health Organization. Technical Briefs for Policy-Makers: Designing health financing systems to reduce catastrophic health expenditure. Number 2. 2005 [Google Scholar]
- World Health Organization. mhGAP: Mental Health Gap Action Programme: Scaling Up Care for Mental, Neurological and Substance Use Disorders. WHO Guidelines Approved by the Guidelines Review Committee; Geneva: 2008. [PubMed] [Google Scholar]
- World Health Organization. Global Health Observatory (GHO) data: Psychiatrists and nurses working in mental health sector. 2014 (n.d.-a) [Google Scholar]
- World Health Organization. Mental Health Atlas. Geneva: 2017. (n.d.-b), Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- World Health Organization. From raising awareness to building capacity. Geneva, Switzerland: 2013. Meeting report: Autism spectrum disorders and other developmental disorders. (n.d.) [Google Scholar]
- Yeh M, Hough RL, McCabe K, Lau A, Garland A. Parental Beliefs About the Causes of Child Problems: Exploring Racial/Ethnic Patterns. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(5):605–612. doi: 10.1097/00004583-200405000-00014. [DOI] [PubMed] [Google Scholar]
- Zager D, Cihak DF, Stone-MacDonald A. Autism Spectrum Disorders: Identification, Education, and Treatment. Chapter 5, Global Perspectives. Routledge; 2016. [Google Scholar]
- Zhang J, Wheeler J, Richey D. Cultural Validity in Assessment Instruments for Children with Autism from a Chinese Cultural Perspective. International Journal of Special Education. 2006;21:109–114. [Google Scholar]
- Zuckerman KE, Chavez AE, Murillo CR, Lindly OJ, Reeder JA. Disparities in Familiarity with Developmental Disabilities among Low-Income Parents. Academic Pediatrics. 2018 doi: 10.1016/j.acap.2018.06.011. pii: S1876-2859(18)30422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Lindly OJ, Sinche B. Parent Beliefs About the Causes of Learning and Developmental Problems Among Children With Autism Spectrum Disorder: Results From a National Survey. American Journal on Intellectual and Developmental Disabilities. 2016;121(5):432–447. doi: 10.1352/1944-7558-121.5.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Sinche B, Mejia A, Cobian M, Becker T, Nicolaidis C. Latino Parents’ Perspectives of Barriers to Autism Diagnosis. Academic Pediatrics. 2014;14(3):301–308. doi: 10.1016/j.acap.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]