Abstract
Backgroud
The association between underlying comorbidities and cardiac injury and the prognosis in coronavirus disease 2019 (COVID‐19) patients was assessed in this study.
Hypothesis
The underlying comorbidities and cardiac injury may be associated with the prognosis in COVID‐19 patients.
Methods
A systematic search was conducted in PubMed, EMBASE, Web of science, and The Cochrane library from December 2019 to July 2020. The odds ratio (OR) and 95% confidence intervals (95% CI) were used to estimate the probability of comorbidities and cardiac injury in COVID‐19 patients with or without severe type, or in survivors vs nonsurvivors of COVID‐19 patients.
Results
A total of 124 studies were included in this analysis. A higher risk for severity was observed in COVID‐19 patients with comorbidities. The pooled result in patients with hypertension (OR 2.57, 95% CI: 2.12‐3.11), diabetes (OR 2.54, 95% CI: 1.89‐3.41), cardiovascular diseases (OR 3.86, 95% CI: 2.70‐5.52), chronic obstractive pulmonary disease (OR 2.71, 95% CI: 1.98‐3.70), chronic kidney disease (OR 2.20, 95% CI: 1.27‐3.80), and cancer (OR 2.42, 95% CI: 1.81‐3.22) respectively. All the comorbidities presented a higher risk of mortality. Moreover, the prevalence of acute cardiac injury is higher in severe group than in nonsevere group, and acute cardiac injury is associated with an increased risk for in‐hospital mortality.
Conclusion
Comorbidities and acute cardiac injury are closely associated with poor prognosis in COVID‐19 patients. It is necessary to continuously monitor related clinical indicators of organs injury and concern comorbidities in COVID‐19 patients.
Keywords: cardiac injury, comorbidities, COVID‐19, meta‐analysis, mortality, severity
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19) has emerged as a global pandemic and a public health event of widespread concern. 1 , 2 , 3 , 4 , 5 To date, more than 3.4 million individuals worldwide with confirmed COVID‐19, of whom more than 200 000 have lost their lives. The higher incidence of comorbidities in COVID‐19 patients, including hypertension, diabetes and cardiovascular disease et al, was reported in recent retrospective studies. Cardiovascular metabolic comorbidities may be a risk factor for poor prognosis. In addition, COVID‐19 patients have different degrees of myocardial damage in addition to respiratory symptoms, especially in critically ill patients.
Huang et al. 6 first reported that 32% of the cases had comorbidities, 8% developed myocardial injury, and the mortality rate as high as 15% in 41 confirmed patients. The study of Yang et al. 7 indicated that elderly critically ill patients (> 65 years old) with comorbidities and acute respiratory distress syndrome (ARDS) are at higher risk of death. In addition, Guo T et al 8 and Shi et al. 9 reported that COVID‐19 patients with myocardial injury had a significantly higher mortality rate than patients without myocardial injury. Given the worldwide pandemic of this infectious disease, it is necessary to identify the risk factors associated with increased risk of in‐hospital mortality in COVID‐19 patients. Although, some clinical case series studies demonstrated that comorbidities including hypertension, diabetes, and cardiovascular diseases (CVD), chronic obstractive pulmonary disease (COPD), chronic kidney disease (CKD), and cancer may be predictors for the poor prognosis in COVID‐19 patients, the number of enrolled patients was limited, and potential confounding factors were not excluded, so it still needs to be further confirmed. In this study, we conducted a systematic review of available studies to assess the association between underlying comorbidities and acute cardiac injury and the severity or the prognosis in COVID‐19 patients.
2. METHODS
2.1. Search strategy and study selection
We conducted systematic retrieval in PubMed, EMBASE (by Ovidsp), Web of Science and The Cochrane Library from December 2019 to July 2020. The free keywords included “comorbidities”, “hypertension”, “diabetes”, “cardiovascular disease”, “cardiac injury”, “chronic obstractive pulmonary disease”, “chronic kidney disease”, “cancer”, “novel coronavirus pneumonia”, “COVID‐19”, “2019‐nCoV” and “clinical characteristics”. Additionally, we checked the references of each cited manuscript to identify other possibly eligible studies. This pooled analysis was conducted and reported in compliance with the preferred reporting items for systematic reviews and meta‐analyses (PRISMA) guidelines. 10
Eligible studies should be written in English, and describe the relationship between age, gender, comorbidities and the prognosis of adult COVID‐19 patients. The number of enrolled patients is more than ten. Case reports, reviews, letters, family‐based studies, nonhuman studies, studies without adequate information, studies written not in English, studies focused only on children or pregnant women, and patients not stratified with the degree of severity or survivors were excluded. The inclusion of each study was determined by two researchers. Disagreements were resolved through a consensus.
2.2. Data extraction
Two reviewers independently extracted data from the included studies. Discrepancies were resolved by consensus between the two reviewers. Variables included authors, sample size, age, gender, relevant data on comorbidity of severe and nonsevere, and of survivors and nonsurvivors (including hypertension, diabetes, CVD, COPD, CKD, and cardiac injury). Cardiac injury was defined by elevation of Troponin I/T. The New castle Ottawa scale (NOS) was followed to assess the quality of studies. 11 The primary outcome was to explore the association between the comorbidities or acute cardiac injury and severity or mortality in confirmed COVID‐19 patients.
2.3. Statistical analysis
Pooled analysis was performed using STATA software (version 14.0). The odds ratio (OR) and 95% confidence intervals (95% CI) were used to estimate the probability of comorbidities or cardiac injury in COVID‐19 patients with or without severe type, or in survivors vs nonsurvivors of COVID‐19 patients. Magnitude of heterogeneity was calculated using the I2 statistic: 25%, 50%, and 75% representing low, medium, and high heterogeneity, respectively. Due to the heterogeneity between studies, a random effect model was performed to estimating the average effect. 12 In order to assess the impact of age (mean age or median age) and sex (percentage of males), univariable meta‐regression models were performed. Publication bias was evaluated by the Bgger's test, with P > .05 indicated no evidence of publication bias. 13
3. RESULTS
3.1. Search results and study characteristics
Initial database search identified 6196 studies and 34 additional records through reference and citation searches (Figure 1). Overall, 329 of them with full‐text were reviewed for eligibility, of which 124 studies were included in this analysis. 7 , 8 , 9 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 The NOS scores ranged between 5 and 8. The key characteristics of included studies were presented in Table S1. The majority of included studies were based in Asia, the minority was from the USA, Italy, Spain and other countries. With most studies including more males than females, and the mean age varied from a median of 40 to 84 years of age. 58 studies compared the incidence of hypertension or diabetes in severe vs nonsevere cases with COVID‐19 and 29 studies compared the prevalence of CVD. Eleven studies reported the association between acute cardiac injury and the severity of COVID‐19. Sixty three documents reported the incidence of cardiovascular metabolic diseases in nonsurvivors vs survivors.
FIGURE 1.
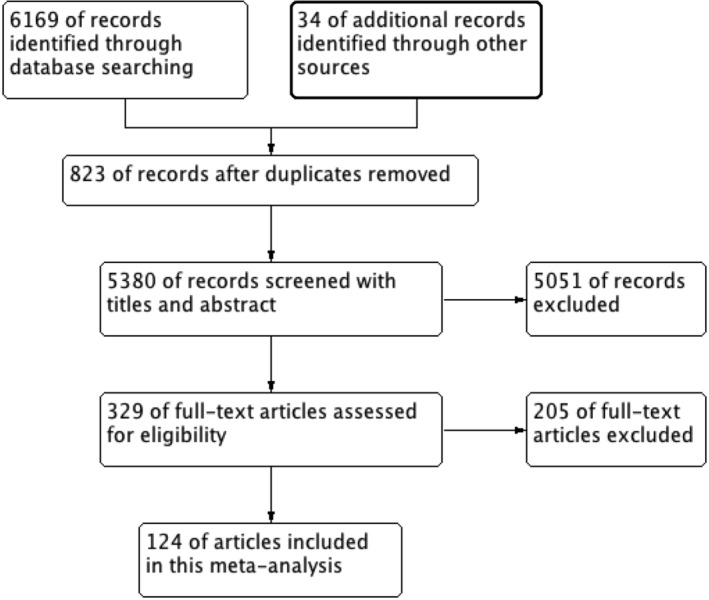
The flow of studies literature search and selection of studies
3.2. Meta‐analysis
The association between comorbidities and disease severity were presented in Figure 2. A heterogeneity between the studies varied from moderate to high. A higher risk for severity was observed in COVID‐19 patients with hypertension, diabetes, CVD, COPD, CKD or cancer, and the pooled result was (OR 2.57, 95% CI: 2.12‐3.11), (OR 2.54, 95% CI: 1.89‐3.41), (OR 3.86, 95% CI: 2.70‐5.52), (OR 2.71, 95% CI: 1.98‐3.70), (OR 2.20, 95% CI: 1.27‐3.80) and (OR 2.42, 95% CI: 1.81‐3.22) respectively (Figure 2, Table S2). At the same time, the risk for in‐hospital mortality was significantly increased in COVID‐19 patients with hypertension (OR 2.50, 95% CI: 2.02‐3.11), diabetes (OR 2.09, 95% CI: 1.80‐2.42), CVD (OR 2.65, 95% CI: 1.87‐3.77), COPD (OR 2.48, 95% CI: 2.05‐3.00), CKD (OR 3.07, 95% CI: 2.43‐3.88) or cancer (OR 1.90, 95% CI: 1.57‐2.30) (Figure 3, Table S2). Moreover, it is observed that the prevalence of acute cardiac injury is higher in severe group than in nonsevere group (OR:6.57; 95% CI 3.70‐11.65), and acute cardiac injury is associated with an increased risk for mortality (OR:16.96; 95% CI 7.89‐36.44) (Figure 4).
FIGURE 2.
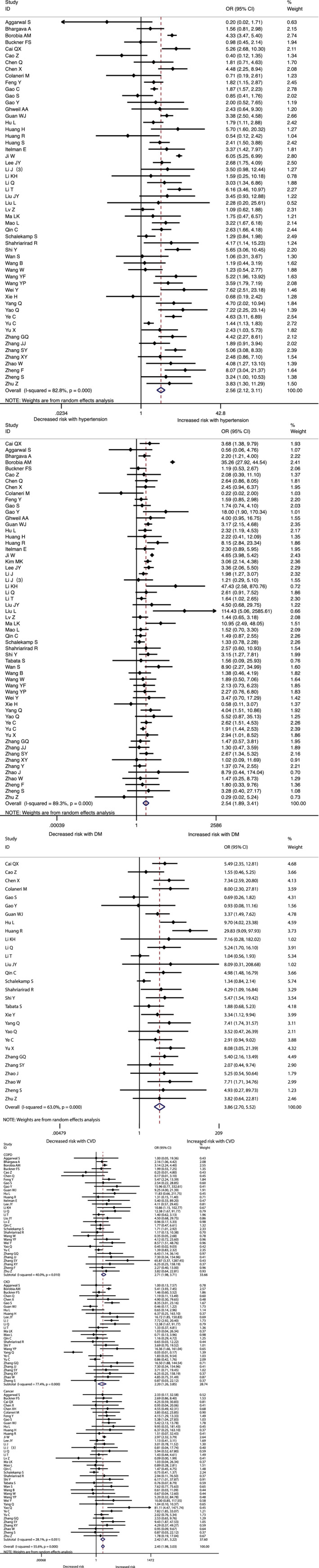
The association of comorbidities (hypertension, diabetes, and cardiovascular diseases(CVD), chronic obstractive pulmonary disease(COPD), chronic kidney disease(CKD), and cancer)with COVID‐19 severity
FIGURE 3.
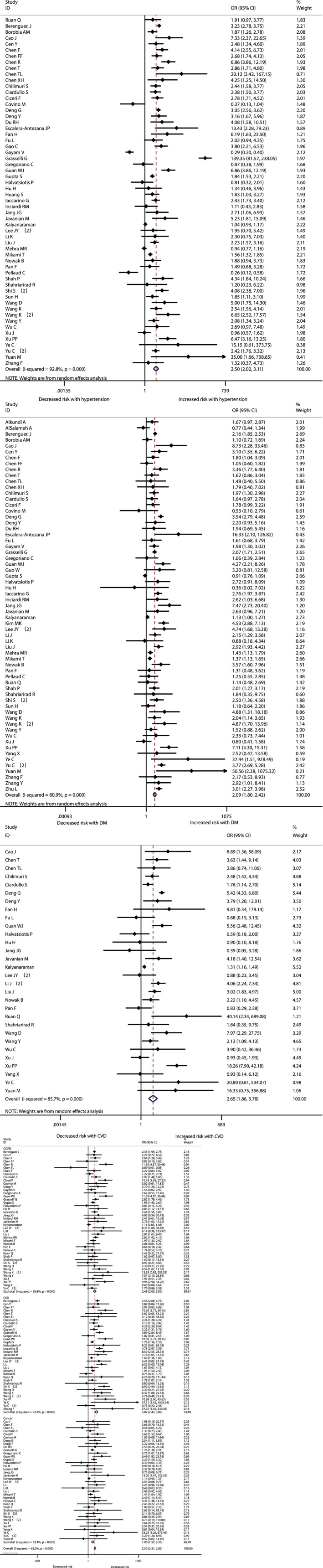
The association of comorbidities (hypertension, diabetes, and cardiovascular diseases(CVD), chronic obstractive pulmonary disease(COPD), chronic kidney disease(CKD), and cancer) with COVID‐19 mortality
FIGURE 4.
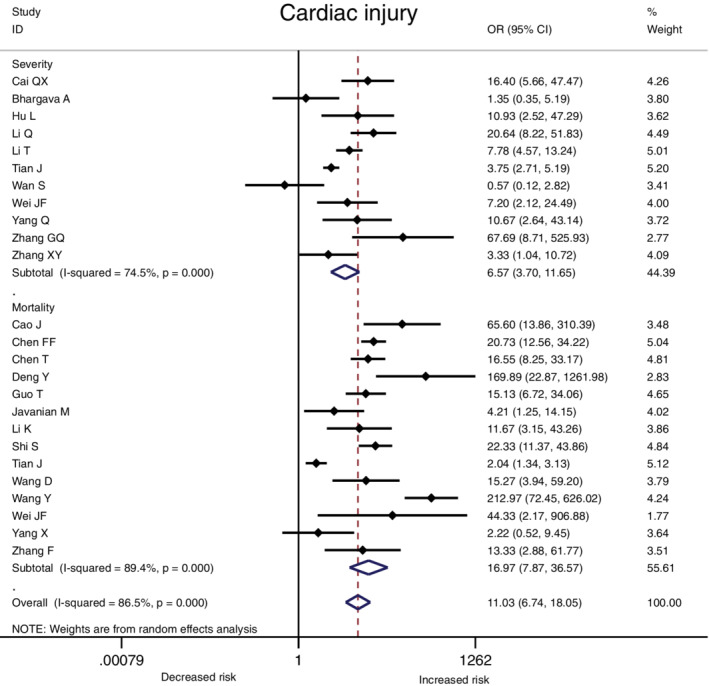
The association of cardiac injury with COVID‐19 severity and mortality
3.3. Meta‐regression analysis
The results of univariable meta‐regression analyses showed the impact of age and sex on the association between comorbidities or acute cardiac injury and the prognosis (severity and mortality) in COVID‐19 patients. There was a clearer effect of increasing age on the association between hypertesion and diabetes and severity of COVID‐19 (sFig1, sFig2). Conversely, there is no significant association between the proportion of males with the risk of severity or mortality. No obvious evidence of publication bias existed (Table S2).
4. DISCUSSION
The pandemic of COVID‐19 poses a huge challenge to countries all over the world. SARS‐CoV‐2 infection is more serious among individuals with immune deficiency and comorbidities. Reliable population epidemiology, clinical characteristics, and laboratory parameters can help distinguish high‐risk COVID‐19 patients and enable more active management of hospitalized or critically ill patients. At present, some laboratory indicators that may predict the deterioration of COVID‐19 have been identified, including leukocytosis, lymphopenia, thrombocytopenia, and cardiac injury biomarkers, elevated inflammatory cytokines. Notably, early studies reported some clinical indicators such as age, gender, as well as existing hypertension, diabetes and CVD can predict the prognosis of COVID‐19. CVD have the highest prevalence among potential patients at higher risk for severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection. 135 Comorbidities such as hypertension and diabetes are recognized as poor prognostic factors for ARDS and SIRS. 136 , 137 However, the relationship between these comorbidities and COVID‐19 severity or poor survival outcomes remains unclear.
This pooled analysis is based on data from 124 studies with confirmed COVID‐19. In this study, it is observed that the comorbidities makes COVID‐19 patients more likely to develop severe clinical type and increase the risk for in‐hospital death. Comorbidities may be a risk factor for critically ill patients with poor prognosis. Another important finding is that acute cardiac injury increased the risk of severity and in‐hospital death for patients with COVID‐19. According to the current research data, some patients with COVID‐19 suffered acute cardiac injury, and the incidence of acute cardiac injury is much higher in severe cases. 6 , 21 , 24 However, the pathogenesis of acute cardiac injury associated with COVID‐19 is still needs further investigation. The unique and significant affinity of SARS‐CoV‐2 for the host ACE2 receptor increases the possibility of direct infection of vascular endothelium and myocardium. Meanwhile, hypoxemia and cytokine storm may also be an important cause of acute cardiac injury. 6 Therefore, it is necessary to monitor acute cardiac injury markers and cardiac function during hospitalization, and pay more attention to heart damage related to SARS‐CoV‐2 infection in the course of disease treatment, and take more active treatment for patients with acute cardiac injury.
A recent study on influenza showed that patients with cardiovascular disease and hypertension have a higher risk of death than those without comorbidities. 138 Previous studies in patients with Middle East Respiratory Syndrome Coronavirus (MERS‐CoV) found that comorbidities were significantly associated with poor prognosis. 139 Recently, meta‐analysis have evaluated the impact of comorbidities in the population of COVID‐19, and the results are consistent with this review, 140 , 141 , 142 , 143 but with fewer the included studies. This pooled results are based on more data and included studies from many countries including China, the United States, Italy and so on. However, the local policy of COVID‐19 research and the time of patient enrollment is different, and some studies only included severely ill or elderly patients. Over time, people's attention to the epidemic, the implementation of related policies, and improvement of treatment plans may reduce the overall severity and mortality of COVID‐19. In addition, there are reports that some controversial studies of COVID‐19 patients have been withdrawn after the author failed to demonstrate the reliability of the data. This review included retrospective observational studies, which are prone to selection and recall bias in the collection and processing of data, and the definition of outcome may be different in each study. In order to make our results as accurate as possible, we removed studies that clearly had overlapping cohorts because they specified the same hospital and time period. However, we cannot be sure that the data among all studies does not overlap. The actual prevalence of comorbidities in COVID‐19 patients and their impact on prognosis remain unknown.
In summary, we updates the evidence on the association between comorbidities or cardiac injury and COVID‐19. The pooled result support that patients with comorbidities may increase the severity of SARS‐CoV‐2 infection, and may also greatly affect the survival outcome of COVID‐19 patients. The successful treatment of severe or critical cases is the key to reduce in‐hospital mortality. Prevention and intervention measures for these patients should be strengthened, and patients with underlying chronic diseases are strongly recommended to avoid any close contact with others in the community, especially in endemic areas. It is necessary to continuously monitor blood pressure, blood glucose, and related clinical indicators of organs injury in COVID‐19 patients with comorbidities.
Indeed, there are some limitations in this study. First, the baseline characteristics of included population in various studies may bias the results. Second, patients with one or more comorbidities and different clinical treatment strategies will lead to different survival outcomes. In addition, although we collect as much complete and reliable data as possible, most of the studies included are from China since it is the main focus of the pandemic rise. The actual prevalence and mortality rates may vary in different countries. Finally, we evaluated publication bias through Bgger regression test, but currently these common statistical methods (such as funnel plot, Bgger test and Egger test) are not considered to be useful evaluation tools. The influence of publication bias cannot be completely ruled out. Prospective randomized control trials are warranted to further confirm the conclusions in this study.
5. CONCLUSION
Comorbidities and acute cardiac injury are closely associated with poor prognosis in COVID‐19 patients. It is necessary to continuously monitor related clinical indicators of organs injury and concern comorbidities in COVID‐19 patients.
CONFLICT OF INTEREST
The authors declare they have no conflict of interest.
Supporting information
Figure S1 A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the hypertention‐related risk of COVID‐19 severity or mortality.
sFig 2. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the diabetes‐related risk of COVID‐19 severity or mortality.
sFig 3. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the cardiovascular disease‐related risk of COVID‐19 severity or mortality.
sFig 4. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the COPD‐related risk of COVID‐19 severity or mortality.
sFig 5. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the CKD‐related risk of COVID‐19 severity or mortality.
sFig 6. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the cancer‐related risk of COVID‐19 severity or mortality.
sFig 7. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the cardiac injury ‐related risk of COVID‐19 severity or mortality.
Table S1 Baseline characteristics of studies included in the systematic review.
Table S2: The pooled outcome in patients with comorbidities or cardiac injury.
Luo L, Fu M, Li Y, et al. The potential association between common comorbidities and severity and mortality of coronavirus disease 2019: A pooled analysis. Clin Cardiol. 2020;43:1478–1493. 10.1002/clc.23465
Contributor Information
Ling Tu, Email: lingtu@tjh.tjmu.edu.cn.
Xizhen Xu, Email: xzxu@tjh.tjmu.edu.cn.
DATA AVAILABILITY STATEMENT
The data supporting this systematic review are from previously reported studies and datasets, which have been cited.
REFERENCES
- 1. Hui DS, Azhar E, Madani TA, et al. The continuing 2019‐nCoV epidemic threat of novel coronaviruses to global health ‐ the latest 2019 novel coronavirus outbreak in Wuhan. China Int J Infect Dis. 2020;91:264‐266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lu H, Stratton CW, Tang YW. Outbreakof pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. J Med Virol. 2020;92(4):401‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wuhan Municipal Health Commission . Report of novel coronavirus‐infected pneumonia in China. Accessed January 31, 2020.
- 4. Paules CI, Marston HD, Fauci AS. Coronavirus infections—more than just the common cold. JAMA. 2020;323(8):707‐708. 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization . Coronavirus disease 2019 (COVID‐19) Situation Report – 66. World Health Organization, 27 March 2020.
- 6. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China the Lancet. 2020;395(10223):497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS‐CoV‐2 pneumonia in Wuhan, China: a single‐centered, retrospective, observational study. Lancet Respir Med. 2020;8:475‐481. 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID‐19). JAMA Cardiol. 2020;5:811 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shi S, Qin M, Shen B, et al. Associationof cardiac injury with mortality in hospitalized patients with COVID‐19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802‐810. 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stewart LA, Clarke M, Rovers M, et al. Preferred reporting items for system‐ atic review and meta‐analyses of individual participant data: the PRISMA‐IPD statement. Jama. 2015;313:1657‐1665. [DOI] [PubMed] [Google Scholar]
- 11. Morrison J, Pai M, Hopewell PC. Tuberculosis and latent tuberculosis infection in close contacts of people with pulmonary tuberculosis in lowincome and middleincome countries: a systematic review and metaanalysis. Lancet Infect Dis. 2008;8:359‐368. [DOI] [PubMed] [Google Scholar]
- 12. DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials. 1986;198(7):177‐188. 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 13. Duval S, Tweedie R. Trim and fill: a simple funnel‐plot‐based method of testing and adjusting for publication bias in meta‐analysis. Biometrics. 2000;56:455‐463. [DOI] [PubMed] [Google Scholar]
- 14. Wan S, Xiang Y, Fang W, et al. Clinical features and treatment of COVID‐19 patients in Northeast Chongqing. J Med Virol. 2020;92:797‐806. 10.1002/jmv.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan. ChinaAllergy. 2020;75:1730‐1741. 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 16. Aggarwal S, Garcia‐Telles N, Aggarwal G, Lavie C, Lippi G, Henry BM. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID‐19): first report from the United States. Diagnostics. 2020;7(2):91‐96. 10.1515/dx-2020-0046. [DOI] [PubMed] [Google Scholar]
- 17. Al‐Salameh A, Lanoix JP, Bennis Y, et al. Characteristics and outcomes of COVID‐19 in hospitalized patients with and without diabetes. Diabetes Metab Res Rev. 2020;e3388 10.1002/dmrr.3388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Alkundi A, Mahmoud I, Musa A, Naveed S, Alshawwaf M. Clinical characteristics and outcomes of COVID‐19 hospitalized patients with diabetes in the United Kingdom: a retrospective single Centre study. Diabetes Res Clin Pract. 2020;165:108263 10.1016/j.diabres.2020.108263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Almazeedi S, Al‐Youha S, Jamal MH, et al. Characteristics, risk factors and outcomes among the first consecutive 1096 patients diagnosed with COVID‐19 in Kuwait. EClinicalMedicine. 2020;24:100448 10.1016/j.eclinm.2020.100448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Berenguer J, Ryan P, Rodríguez‐Baño J, et al. Characteristics and predictors of death among 4,035 consecutively hospitalized patients with COVID‐19 in Spain. Clin Microbiol Infect. 2020;S1198‐743X(20):30431‐30436. 10.1016/j.cmi.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bhargava A, Fukushima EA, Levine M, et al. Predictors for severe COVID‐19 infection. Clin Infect Dis. 2020. 10.1093/cid/ciaa674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Borobia AM, Carcas AJ, Arnalich F, et al. A cohort of patients with COVID‐19 in a major teaching hospital in Europe. J Clin Med. 2020;9(6):1733 10.3390/jcm9061733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Buckner FS, McCulloch DJ, Atluri V, et al. Clinical features and outcomes of 105 hospitalized patients with COVID‐19 in Seattle, Washington. Clin Infect Dis. 2020;ciaa632 10.1093/cid/ciaa632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cai Q, Huang D, Ou P, et al. COVID‐19 in a designated infectious diseases hospital outside Hubei Province. China Allergy. 2020;75(7):1742‐1752. 10.1111/all.14309. [DOI] [PubMed] [Google Scholar]
- 25. Cao J, Tu WJ, Cheng W, et al. Clinical features and short‐term outcomes of 102 patients with Corona virus disease 2019 in Wuhan. China Clin Infect Dis. 2020;2:2‐755. 10.1093/cid/ciaa243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cao Z, Li T, Liang L, et al. Clinical characteristics of coronavirus disease 2019 patients in Beijing, China. PLoS One. 2020;15(6):e0234764 10.1371/journal.pone.0234764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cen Y, Chen X, Shen Y, et al. Risk factors for disease progression in patients with mild to moderate coronavirus disease 2019‐a multi‐Centre observational study. Clin Microbiol Infect. 2020;26(9):1242‐1247. 10.1016/j.cmi.2020.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen F, Sun W, Sun S, Li Z, Wang Z, Yu L. Clinical characteristics and risk factors for mortality among inpatients with COVID‐19 in Wuhan, China. Clin Transl Med. 2020;10(2):e40 10.1002/ctm2.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chen FF, Zhong M, Liu Y, et al. The characteristics and outcomes of 681 severe cases with COVID‐19 in China. J Crit Care. 2020;60:32‐37. 10.1016/j.jcrc.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chen Q, Zheng Z, Zhang C, et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID‐19) in Taizhou, Zhejiang. China Infection. 2020;48(4):543‐551. 10.1007/s15010-020-01432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chen R, Liang W, Jiang M, et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a Nationwide analysis in China. Chest. 2020;158(1):97‐105. 10.1016/j.chest.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1096 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chen T, Dai Z, Mo P, et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID‐19) in Wuhan, China (2019): a single‐centered, retrospective study. J Gerontol A Biol Sci Med Sci. 2020. 10.1093/gerona/glaa089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chen X, Zheng F, Qing Y, et al. Epidemiological and clinical features of 291 cases with coronavirus disease 2019 in areas adjacent to Hubei, China: a double‐center observational study. medRxiv. 2020. 10.1101/2020.03.03.20030353. [DOI] [Google Scholar]
- 35. Chen XF, Zhao B, Qu Y, et al. Detectable serum SARS‐CoV‐2 viral load (RNAaemia) is closely correlated with drastically elevated interleukin 6 (IL‐6) level in critically ill COVID‐19 patients. Clin Infect Dis. 2020. 10.1093/cid/ciaa449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chilimuri S, Sun H, Alemam A, et al. Predictors of mortality in adults admitted with COVID‐19: retrospective cohort Study from New York City. West J Emerg Med. 2020;21(4):779‐784. 10.5811/westjem.2020.6.47919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ciardullo S, Zerbini F, Perra S, et al. Impact of diabetes on COVID‐19‐related in‐hospital mortality: a retrospective study from northern Italy. J Endocrinol Invest. 2020;43:1‐8. 10.1007/s40618-020-01382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ciceri F, Castagna A, Rovere‐Querini P, et al. Early predictors of clinical outcomes of COVID‐19 outbreak in Milan. Italy Clin Immunol. 2020;217:108509 10.1016/j.clim.2020.108509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Colaneri M, Sacchi P, Zuccaro V, et al. Clinical characteristics of coronavirus disease (COVID‐19) early findings from a teaching hospital in Pavia, North Italy, 21 to February 28, 2020. Euro Surveill. 2020;25(16):2000460 10.2807/1560-7917.ES.2020.25.16.2000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Covino M, De Matteis G, Santoro M, et al. Clinical characteristics and prognostic factors in COVID‐19 patients aged ≥80 years. Geriatr Gerontol Int. 2020;20(7):704‐708. 10.1111/ggi.13960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Deng G, Yin M, Chen X, Zeng F. Clinical determinants for fatality of 44,672 patients with COVID‐19. Crit Care. 2020;24(1):179 10.1186/s13054-020-02902-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Deng Y, Liu W, Liu K, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID‐19) in Wuhan, China: a retrospective study. Chin Med J (Engl). 2020;133(11):1261‐1267. 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Du RH, Liang LR, Yang CQ, et al. Predictors of mortality for patients with COVID‐19 pneumonia caused by SARS‐CoV‐2: a prospective cohort study. Eur Respir J. 2020;55:2000524 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Escalera‐Antezana JP, Lizon‐Ferrufino NF, Maldonado‐Alanoca A, et al. Risk factors for mortality in patients with coronavirus disease 2019 (COVID‐19) in Bolivia: an analysis of the first 107 confirmed cases. Infez Med. 2020;28(2):238‐242. [PubMed] [Google Scholar]
- 45. Fan H, Zhang L, Huang B, et al. Cardiac injuries in patients with coronavirus disease 2019: not to be ignored. Int J Infect Dis. 2020;96:294‐297. 10.1016/j.ijid.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Feng Y, Ling Y, Bai T, et al. COVID‐19 with different severity: a multi‐center study of clinical features. Am J Respir Crit Care Med. 2020;30(9):4893‐4902. 10.1164/rccm.202002-0445OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Fu L, Fei J, Xiang H‐X, et al. Influence factors of death risk among COVID‐19 patients in Wuhan, China: a hospital‐based case‐cohort study. medRxiv. 2020;86:20035329. [Google Scholar]
- 48. Gao C, Cai Y, Zhang K, et al. Association of hypertension and antihypertensive treatment with COVID‐19 mortality: a retrospective observational study. Eur Heart J. 2020;41(22):2058‐2066. 10.1093/eurheartj/ehaa433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gao S, Jiang F, Jin W, et al. Risk factors influencing the prognosis of elderly patients infected with COVID‐19: a clinical retrospective study in Wuhan, China. Aging (Albany NY). 2020;12(13):12504‐12516. 10.18632/aging.103631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gao Y, Li T, Han M, et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID‐19. J Med Virol. 2020;92(7):791‐796. 10.1002/jmv.25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gayam V, Chobufo MD, Merghani MA, Lamichanne S, Garlapati PR, Adler MK. Clinical characteristics and predictors of mortality in African‐Americans with COVID‐19 from an inner‐city community teaching hospital in New York. J Med Virol. 2020. 10.1002/jmv.26306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ghweil AA, Hassan MH, Khodeary A, et al. Characteristics, outcomes and indicators of severity for COVID‐19 among sample of ESNA quarantine Hospital's patients, Egypt: a retrospective study. Infect Drug Resist. 2020;13:2375‐2383. 10.2147/IDR.S263489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Grasselli G, Greco M, Zanella A, et al. Risk factors associated with mortality among patients with COVID‐19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;e203539 10.1001/jamainternmed.2020.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Gregoriano C, Koch D, Haubitz S, et al. Characteristics, predictors and outcomes among 99 patients hospitalised with COVID‐19 in a tertiary care Centre in Switzerland: an observational analysis. Swiss Med Wkly. 2020;150:w20316 10.4414/smw.2020.20316. [DOI] [PubMed] [Google Scholar]
- 55. Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID‐19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Guo W, Li M, Dong Y, et al. Diabetes is a risk factor for the progression and prognosis of COVID‐19. Diabetes Metab Res Rev. 2020;32‐42. 10.1002/dmrr.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gupta S, Hayek SS, Wang W, et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020;e203596 10.1001/jamainternmed.2020.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Halvatsiotis P, Kotanidou A, Tzannis K, et al. Demographic and clinical features of critically ill patients with COVID‐19 in Greece: the burden of diabetes and obesity. Diabetes Res Clin Pract. 2020;166:108331 10.1016/j.diabres.2020.108331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hu L, Chen S, Fu Y, et al. Risk factors associated with clinical outcomes in 323 COVID‐19 hospitalized patients in Wuhan, China. Clin Infect Dis. 2020;ciaa539 10.1093/cid/ciaa539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hu H, Yao N, Qiu Y. Comparing rapid scoring Systems in Mortality Prediction of critically ill patients with novel coronavirus disease. Acad Emerg Med. 2020;27(6):461‐468. 10.1111/acem.13992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Huang H, Song B, Xu Z, et al. Predictors of coronavirus disease 2019 severity: a retrospective study of 64 cases. Jpn J Infect Dis. 2020. 10.7883/yoken.JJID.2020.298. [DOI] [PubMed] [Google Scholar]
- 62. Huang R, Zhu L, Xue L, et al. Clinical findings of patients with coronavirus disease 2019 in Jiangsu province, China: A retrospective, multi‐center study. PLoS Negl Trop Dis. 2020;14(5):e0008280 10.1371/journal.pntd.0008280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Huang S, Wang J, Liu F, et al. COVID‐19 patients with hypertension have more severe disease: a multicenter retrospective observational study. Hypertens Res. 2020;43(8):824‐831. 10.1038/s41440-020-0485-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Iaccarino G, Grassi G, Borghi C, et al. Age and multimorbidity predict death among COVID‐19 patients: results of the SARS‐RAS study of the Italian Society of Hypertension. Hypertension. 2020;76(2):366‐372. 10.1161/HYPERTENSIONAHA.120.15324. [DOI] [PubMed] [Google Scholar]
- 65. Inciardi RM, Adamo M, Lupi L, et al. Characteristics and outcomes of patients hospitalized for COVID‐19 and cardiac disease in northern Italy. Eur Heart J. 2020;41(19):1821‐1829. 10.1093/eurheartj/ehaa388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Itelman E, Wasserstrum Y, Segev A, et al. Clinical characterization of 162 COVID‐19 patients in Israel: preliminary report from a large tertiary center. Isr Med Assoc J. 2020;22(5):271‐274. [PubMed] [Google Scholar]
- 67. Jang JG, Hur J, Choi EY, Hong KS, Lee W, Ahn JH. Prognostic factors for severe coronavirus disease 2019 in Daegu, Korea. J Korean Med Sci. 2020;35(23):e209 10.3346/jkms.2020.35.e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Javanian M, Bayani M, Shokri M, et al. Clinical and laboratory findings from patients with COVID‐19 pneumonia in Babol north of Iran: a retrospective cohort study. Rom J Intern Med. 2020;58:161‐167. 10.2478/rjim-2020-0013. [DOI] [PubMed] [Google Scholar]
- 69. Ji W, Huh K, Kang M, et al. Effect of underlying comorbidities on the infection and severity of COVID‐19 in Korea: a Nationwide case‐control study. J Korean Med Sci. 2020;35(25):e237 10.3346/jkms.2020.35.e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Kalyanaraman Marcello R, Dolle J, Grami S, et al. Characteristics and outcomes of COVID‐19 patients in New York City's public hospital system. medRxiv. 2020;20086645 10.1101/2020.05.29.20086645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kim MK, Jeon JH, Kim SW, et al. The clinical characteristics and outcomes of patients with moderate‐to‐severe coronavirus disease 2019 infection and diabetes in Daegu, South Korea. Diabetes Metab J. 2020;44(4):602‐613. 10.4093/dmj.2020.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Lee JY, Hong SW, Hyun M, et al. Epidemiological and clinical characteristics of coronavirus disease 2019 in Daegu, South Korea. Int J Infect Dis. 2020;98:462‐466. 10.1016/j.ijid.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Lee JY, Kim HA, Huh K, et al. Risk factors for mortality and respiratory support in elderly patients hospitalized with COVID‐19 in Korea. J Korean Med Sci. 2020;35(23):e223 10.3346/jkms.2020.35.e223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Li J, Wang X, Chen J, Zhang H, Deng A. Association of reninangiotensin system inhibitors with severity or risk of death in patients with hypertension hospitalized for coronavirus disease 2019 (COVID‐19) infection in Wuhan, China. JAMA Cardiol. 2020;5(7):1‐6. 10.1001/jamacardio.2020.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Li J, Guo T, Dong D, et al. Defining heart disease risk for death in COVID‐19 infection. QJM. 2020;hcaa246 10.1093/qjmed/hcaa246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Li J, Xu G, Yu H, Peng X, Luo Y, Cao C. Clinical characteristics and outcomes of 74 patients with severe or critical COVID‐19. Am J Med Sci. 2020;360(3):229‐235. 10.1016/j.amjms.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Li K, Chen D, Chen S, Feng Y, Chang C. Radiographic findings and other predictors in adults with Covid‐19. medRxiv. 2020;2 10.1101/2020.03.23.20041673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Li KH, Wu J, Wu F, et al. The clinical and chest CT features associated with severe and critical COVID‐19 pneumonia. Invest Radiol. 2020;55(6):327‐331. 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Li Q, Ling Y, Zhang J, et al. Clinical characteristics of SARS‐CoV‐2 infections involving 325 hospitalized patients outside Wuhan. Infect Dis 2020. 10.21203/rs.3.rs-18699/v1. [DOI]
- 80. Li T, Lu L, Zhang W, et al. Clinical characteristics of 312 hospitalized older patients with COVID‐19 in Wuhan, China. Arch Gerontol Geriatr. 2020;91:104185 10.1016/j.archger.2020.104185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Liu J, Zhang S, Wu Z, et al. Clinical outcomes of COVID‐19 in Wuhan, China: a large cohort study. Ann Intensive Care. 2020;10(1):99 10.1186/s13613-020-00706-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Liu J, Liu Y, Xiang P, et al. Neutrophil‐to‐lymphocyte ratio predicts severe illness patients with 2019 novel coronavirus in the early stage. medRxiv. 10.1101/2020.02.10.20021584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Liu L, Gao J. Clinical characteristics of 51 patients discharged from hospital with COVID‐19 in Chongqing, China. MedRxiv. 2020. 10.1101/2020.02.20.20025536. [DOI] [Google Scholar]
- 84. Lv Z, Cheng S, Le J, et al. Clinical characteristics and co‐infections of 354 hospitalized patients with COVID‐19 in Wuhan, China: a retrospective cohort study. Microbes Infect. 2020;22(4–5):195‐199. 10.1016/j.micinf.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Ma KL, Liu Z‐H, Cao F‐C, et al. COVID‐19 myocarditis and severity factors: an adult cohort study. medRxiv. 2020. 10.1101/2020.03.19.20034124. [DOI] [Google Scholar]
- 86. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):1‐9. 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular disease, drug therapy, and mortality in Covid‐19. N Engl J Med. 2020;382(25):e102 10.1056/NEJMoa2007621. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 88. Mikami T, Miyashita H, Yamada T, et al. Risk factors for mortality in patients with COVID‐19 in New York City. J Gen Intern Med. 2020;1‐10. 10.1007/s11606-020-05983-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Nowak B, Szymański P, Pańkowski I, et al. Clinical characteristics and short‐term outcomes of patients with coronavirus disease 2019: a retrospective single‐center experience of a designated hospital in Poland. Pol Arch Intern Med. 2020;130(5):407‐411. 10.20452/pamw.15361. [DOI] [PubMed] [Google Scholar]
- 90. Pan F, Yang L, Li Y, et al. Factors associated with death outcome in patients with severe coronavirus disease‐19 (COVID‐19): a case‐control study. Int J Med Sci. 2020;17(9):1281‐1292. 10.7150/ijms.46614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Pellaud C, Grandmaison G, Pham Huu Thien HP, et al. Characteristics, comorbidities, 30‐day outcome and in‐hospital mortality of patients hospitalised with COVID‐19 in a Swiss area ‐ a retrospective cohort study. Swiss Med Wkly. 2020;150:w20314 10.4414/smw.2020.20314. [DOI] [PubMed] [Google Scholar]
- 92. Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID‐19 in Wuhan. China Clin Infect Dis. 2020;71:762‐768. 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID‐19 based on an analysis of data of 150 patients from Wuhan. China Intensive Care Med. 2020;46:846‐848. 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Schalekamp S, Huisman M, van Dijk RA, et al. Model‐based prediction of critical illness in hospitalized patients with COVID‐19. Radiology. 2020;202723 10.1148/radiol.2020202723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Shah P, Owens J, Franklin J, et al. Demographics, comorbidities and outcomes in hospitalized Covid‐19 patients in rural Southwest Georgia. Ann Med. 2020;1‐7. 10.1080/07853890.2020.1791356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Shahriarirad R, Khodamoradi Z, Erfani A, et al. Epidemiological and clinical features of 2019 novel coronavirus diseases (COVID‐19) in the south of Iran. BMC Infect Dis. 2020;20(1):427 10.1186/s12879-020-05128-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Shi S, Qin M, Cai Y, et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41(22):2070‐2079. 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Shi Y, Yu X, Zhao H, Wang H, Zhao R, Sheng J. Host susceptibility to severe COVID‐19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24(1):108 10.1186/s13054-020-2833-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Sun H, Ning R, Tao Y, et al. Risk factors for mortality in 244 older adults with COVID‐19 in Wuhan, China: a retrospective study. J Am Geriatr Soc. 2020;68(6):E19‐E23. 10.1111/jgs.16533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Tabata S, Imai K, Kawano S, et al. Clinical characteristics of COVID‐19 in 104 people with SARS‐CoV‐2 infection on the diamond princess cruise ship: a retrospective analysis. Lancet Infect Dis. 2020;20(9):1043‐1050. 10.1016/S1473-3099(20)30482-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Tian J, Yuan X, Xiao J, et al. Clinical characteristics and risk factors associated with COVID‐19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21(7):893‐903. 10.1016/S1470-2045(20)30309-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Wang B, Wang Z, Zhao J, et al. Epidemiological and clinical course of 483 patients with COVID‐19 in Wuhan, China: a single‐center, retrospective study from the mobile cabin hospital. Eur J Clin Microbiol Infect Dis. 2020;1‐7. 10.1007/s10096-020-03927-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Wang D, Yin Y, Hu C, et al. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS‐CoV‐2, discharged from two hospitals in Wuhan, China. Crit Care. 2020;24:188 10.1186/s13054-020-02895-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Wang K, Zhang Z, Yu M, et al. 15‐day mortality and associated risk factors for hospitalized patients with COVID‐19 in Wuhan, China: an ambispective observational cohort study. Intensive Care Med. 2020;46(7):1472‐1474. 10.1007/s00134-020-06047-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Wang K, Zuo P, Liu Y, et al. Clinical and laboratory predictors of in‐hospital mortality in patients with COVID‐19: a cohort study in Wuhan, China. Clin Infect Dis. 2020;ciaa538 10.1093/cid/ciaa538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Wang W, Xin C, Xiong Z, et al. Clinical characteristics and outcomes of 421 patients with coronavirus disease 2019 treated in a mobile cabin hospital. Chest. 2020;158(3):939‐946. 10.1016/j.chest.2020.05.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Wang Y, Lu X, Li Y, et al. Clinical course and outcomes of 344 intensive care patients with COVID‐19. Am J Respir Crit Care Med. 2020;201(11):1430‐1434. 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Wang YF, Zhou Y, Yang Z, Xia D, Hu Y, Geng S. Clinical characteristics of patients with severe pneumonia caused by the SARS‐CoV‐2 in Wuhan, China. Respiration. 2020;1‐9. 10.1159/000507940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Wang YP, Liao B, Guo Y, et al. Clinical characteristics of patients infected with the novel 2019 coronavirus (SARS‐Cov‐2) in Guangzhou, China. Open Forum Infect Dis. 2020;7(6):ofaa187 10.1093/ofid/ofaa187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Wei JF, Huang FY, Xiong TY, et al. Acute myocardial injury is common in patients with COVID‐19 and impairs their prognosis. Heart. 2020;106(15):1154‐1159. 10.1136/heartjnl-2020-317007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Wei Y, Zeng W, Huang X, et al. Clinical characteristics of 276 hospitalized patients with coronavirus disease 2019 in Zengdu District, Hubei Province: a single‐center descriptive study. BMC Infectious Diseases. 2020;20:549 10.1186/s12879-020-05252-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):1‐11. 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Xie H, Zhao J, Lian N, Lin S, Xie Q, Zhuo H. Clinical characteristics of non‐ICU hospitalized patients with coronavirus disease 2019 and liver injury: a retrospective study. Liver Int. 2020;40(6):1321‐1326. 10.1111/liv.14449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Xie Y, You Q, Wu C, et al. Impact of cardiovascular disease on clinical characteristics and outcomes of coronavirus disease 2019 (COVID‐19). Circ J. 2020;84(8):1277‐1283. 10.1253/circj.CJ-20-0348. [DOI] [PubMed] [Google Scholar]
- 115. Xu J, Yang X, Yang L, et al. Clinical course and predictors of 60‐day mortality in 239 critically ill patients with COVID‐19: a multicenter retrospective study from Wuhan, China. Crit Care. 2020;24(1):394 10.1186/s13054-020-03098-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Xu PP, Tian RH, Luo S, et al. Risk factors for adverse clinical outcomes with COVID‐19 in China: a multicenter, retrospective, observational study. Theranostics. 2020;10(14):6372‐6383. 10.7150/thno.46833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Yang Q, Xie L, Zhang W, et al. Analysis of the clinical characteristics, drug treatments and prognoses of 136 patients with coronavirus disease 2019. J Clin Pharm Ther. 2020;45(4):609‐616. 10.1111/jcpt.13170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Yao Q, Wang P, Wang X, et al. Retrospective study of risk factors for severe SARS‐Cov‐2 infections in hospitalized adult patients. Pol Arch Intern Med. 2020;130(5):390‐399. 10.20452/pamw.15312. [DOI] [PubMed] [Google Scholar]
- 119. Ye C, Zhang S, Zhang X, et al. Impact of comorbidities on patients with COVID‐19: a large retrospective study in Zhejiang, China. J Med Virol. 2020. 10.1002/jmv.26183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Yu C, Lei Q, Li W, et al. Epidemiological and clinical characteristics of 1663 hospitalized patients infected with COVID‐19 in Wuhan, China: a single‐center experience. J Infect Public Health. 2020;13(9):1202‐1209. 10.1016/j.jiph.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Yu C, Lei Q, Li W, et al. Clinical characteristics, associated factors, and predicting COVID‐19 mortality risk: a retrospective study in Wuhan, China. Am J Prev Med. 2020;59(2):168‐175. 10.1016/j.amepre.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Yu X, Sun X, Cui P, et al. Epidemiological and clinical characteristics of 333 confirmed cases with coronavirus disease 2019 in Shanghai. China Transbound Emerg Dis. 2020;67(4):1697‐1707. 10.1111/tbed.13604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Yuan M, Yin W, Tao Z, Tan W, Hu Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS One. 2020;15(3):e0230548 10.1371/journal.pone.0230548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Zhang F, Yang D, Li J, et al. Myocardial injury is associated with in‐hospitalmortality of confirmed or suspected COVID‐19 in Wuhan, China: a single center retrospective cohort study. medRxiv. 2020. 10.1101/2020.03.21.20040121. [DOI] [Google Scholar]
- 125. Zhang GQ, Hu C, Luo L, et al. Clinical features and outcomes of 221 patients with COVID‐19 in Wuhan, China. medRxiv. 2020. 10.1101/2020.03.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Zhang SY, Lian JS, Hu JH, et al. Clinical characteristics of different subtypes and risk factors for the severity of illness in patients with COVID‐19 in Zhejiang, China. Infect Dis Poverty. 2020;9(1):85 10.1186/s40249-020-00710-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Zhao XY, Xu XX, Yin HS, et al. Clinical characteristics of patients with 2019 coronavirus disease in a non‐Wuhan area of Hubei Province, China: a retrospective study. BMC Infect Dis. 2020;20(1):311 10.1186/s12879-020-05010-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Zhang Y, Cui Y, Shen M, et al. Association of diabetes mellitus with disease severity and prognosis in COVID‐19: a retrospective cohort study. Diabetes Res Clin Pract. 2020;165:108227 10.1016/j.diabres.2020.108227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Zhao J, Gao HY, Feng ZY, Wu QJ. A retrospective analysis of the clinical and epidemiological characteristics of COVID‐19 patients in Henan provincial People's hospital, Zhengzhou, China. Front Med (Lausanne). 2020;7:286 10.3389/fmed.2020.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Zhao W, Yu S, Zha X, et al. Clinical characteristics and durations of hospitalized patients with COVID‐19 in Beijing: a retrospective cohort study. medRxiv. 2017;21(1):1‐9. [Google Scholar]
- 131. Zheng F, Tang W, Li H, Huang YX, Xie YL, Zhou ZG. Clinical characteristics of 161 cases of corona virus disease 2019 (COVID‐19) in Changsha. Eur Rev Med Pharmacol Sci. 2020;24(6):3404‐3410. 10.26355/eurrev_202003_20711. [DOI] [PubMed] [Google Scholar]
- 132. Zheng S, Fan J, Yu F, et al. Viral load dynamics and disease severity in patients infected with SARS‐CoV‐2 in Zhejiang province, China, January‐march 2020: retrospective cohort study. BMJ. 2020;369:m1443 10.1136/bmj.m1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Zhu L, She ZG, Cheng X, et al. Association of blood glucose control and outcomes in patients with covid‐19 and pre‐existing type 2 diabetes. Cell Metabol. 2020;31(6):1068‐1077. 10.1016/j.c-met.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Zhu Z, Cai T, Fan L, et al. Clinical value of immune‐inflammatory parameters to assess the severity of coronavirus disease 2019. Int J Infect Dis. 2020;95:332‐339. 10.1016/j.ijid.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Onder G, Rezza G, Brusaferro S. Case‐fatality rate and characteristics of patients dying in relation to COVID‐19 in Italy. JAMA. 2020;323(18):1775‐1776. 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 136. Azoulay E, Lemiale V, Mourvillier B, et al. Management and outcomes of acute respiratory distress syndrome patients with and without comorbid conditions. Intensive Care Med. 2018;44(7):1050‐1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Chakraborty RK, Burns B. Systemic inflammatory response syndrome. Treasure Island (FL): StatPearls Publishing; http://www.ncbi.nlm.nih.gov/books/NBK547669/. [PubMed] [Google Scholar]
- 138. Mertz D, Kim TH, Johnstone J, et al. Populations at risk for severe or complicated influenza illness: systematic review and meta‐analysis. BMJ. 2013;347:f5061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Alraddadi BM, Watson JT, Almarashi A, et al. Risk factors for primary Middle East respiratory syndrome coronavirus illness in humans, Saudi Arabia. Emerging Infectious Diseases. 2016;22:49‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Singh AK, Gillies CL, Singh R, et al. Prevalence of co‐morbidities and their association with mortality in patients with COVID‐19: a systematic review and meta‐analysis. Diabetes Obes Metab. 2020. 10.1111/dom.14124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Toraih EA, Elshazli RM, Hussein MH, et al. Association of cardiac biomarkers and comorbidities with increased mortality, severity, and cardiac injury in COVID‐19 patients: a meta‐regression and decision tree analysis. J Med Virol. 2020. 10.1002/jmv.26166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Mantovani A, Byrne CD, Zheng MH, Targher G. Diabetes as a risk factor for greater COVID‐19 severity and in‐hospital death: a meta‐analysis of observational studies. Nutr Metab Cardiovasc Dis. 2020;30(8):1236‐1248. 10.1016/j.numecd.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Matsushita K, Ding N, Kou M, et al. The relationship of COVID‐19 severity with cardiovascular disease and its traditional risk factors: a systematic review and meta‐analysis. medRxiv. 10.1101/2020.04.05.20054155. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the hypertention‐related risk of COVID‐19 severity or mortality.
sFig 2. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the diabetes‐related risk of COVID‐19 severity or mortality.
sFig 3. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the cardiovascular disease‐related risk of COVID‐19 severity or mortality.
sFig 4. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the COPD‐related risk of COVID‐19 severity or mortality.
sFig 5. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the CKD‐related risk of COVID‐19 severity or mortality.
sFig 6. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the cancer‐related risk of COVID‐19 severity or mortality.
sFig 7. A Univariable linear meta‐regression analyses of the association of either age (panels A and C) or sex (panels B and D) the cardiac injury ‐related risk of COVID‐19 severity or mortality.
Table S1 Baseline characteristics of studies included in the systematic review.
Table S2: The pooled outcome in patients with comorbidities or cardiac injury.
Data Availability Statement
The data supporting this systematic review are from previously reported studies and datasets, which have been cited.


