Abstract
Objective
To test the hypothesis that life course patterns of employment, marriage, and childrearing influence later-life rate of memory decline among women, we examined the relationship of work-family experiences between ages 16 and 50 years and memory decline after age 55 years among US women.
Methods
Participants were women ages ≥55 years in the Health and Retirement Study. Participants reported employment, marital, and parenthood statuses between ages 16 and 50 years. Sequence analysis was used to group women with similar work-family life histories; we identified 5 profiles characterized by similar timing and transitions of combined work, marital, and parenthood statuses. Memory performance was assessed biennially from 1995 to 2016. We estimated associations between work-family profiles and later-life memory decline with linear mixed-effects models adjusted for practice effects, baseline age, race/ethnicity, birth region, childhood socioeconomic status, and educational attainment.
Results
There were 6,189 study participants (n = 488 working nonmothers, n = 4,326 working married mothers, n = 530 working single mothers, n = 319 nonworking single mothers, n = 526 nonworking married mothers). Mean baseline age was 57.2 years; average follow-up was 12.3 years. Between ages 55 and 60, memory scores were similar across work-family profiles. After age 60, average rate of memory decline was more than 50% greater among women whose work-family profiles did not include working for pay after childbearing, compared with those who were working mothers.
Conclusions
Women who worked for pay in early adulthood and midlife experienced slower rates of later-life memory decline, regardless of marital and parenthood status, suggesting participation in the paid labor force may protect against later-life memory decline.
Nearly two-thirds of Americans living with Alzheimer dementia are women,1,2 highlighting the importance of identifying modifiable determinants of later-life memory decline and dementia risk among women. Most research on sex/gender in Alzheimer dementia focuses on sex-linked biology; less research has considered social aspects of gender that could influence Alzheimer dementia risk.3,4
Life course patterns of employment, child-rearing, and marriage changed dramatically for US women over the past century.5 These changes may have implications for later-life cognitive health. For example, paid labor force participation could promote later-life cognitive health via cognitive stimulation,6–9 social engagement,10,11 and financial security.12 Conversely, prolonged stress from single motherhood could negatively affect later-life cognitive health.13–16 Prior studies evaluating relations between work-family profiles and health among US women suggest rates of cardiovascular disease, stroke, and mortality in later life are lowest among married mothers who participated in the paid labor force and highest among those with prolonged periods of single motherhood.17,18
Memory decline is the hallmark of Alzheimer dementia.2 Examining later-life memory enables disentanglement of factors influencing premorbid level of memory function and memory decline; the latter is more representative of accumulation of dementia-related neuropathology.19 Our objective was to estimate effects of work-family experiences between early adulthood and midlife (ages 16–50 years) on later-life rate of memory decline (ages 55 and older) among US women. We hypothesized that after accounting for education and other potential early-life confounders, later-life memory decline would be slowest among married mothers who participated in the paid labor force and fastest among women with prolonged periods of single motherhood, especially those who did not engage in paid work.
Methods
Standard protocol approvals, registrations, and patient consents
Health and Retirement Study (HRS) participants provided verbal informed consent. HRS data collection is approved by the University of Michigan Institutional Review Board. The present study used publicly available de-identified data and was certified exempt from review by the University of California Los Angeles Institutional Review Board.
Study population
The HRS is a national cohort representing noninstitutionalized adults over age 50 years in the United States.20 Biennial interviews are available through 2016. Our analyses included HRS participants who (1) were women born between January 1935 and February 1956, (2) participated in at least one memory assessment between 1995 and 2016 when they were age 55 years or older, (3) responded to study questions about dates of employment, marriage, and births of children, and (4) had complete covariate information. We excluded women without any memory assessments at ages ≥55 years to minimize potential reverse causation.
Life course work-family profiles
Life course work-family profiles were conceptualized and sequenced by Sabbath et al.17 Their methods are summarized here. Patterns and timing of work-family combinations were generated based on self-reported dates of employment, marital, and parenthood statuses between ages 16 and 50 years. For each woman, an individual work-family life trajectory was created from binary measures of waged employment (yes/no), marriage (yes/no), and children under 18 years (yes/no) at every age between 16 and 50. Sequence analysis21–23 was used to group women with similar work-family trajectories. The objective was to classify each woman by the prototypical sequence most closely resembling her work-family trajectory. Sequence analysis simultaneously accounts for order, timing, and duration of exposures, clustering individuals based on commonalities in timing of transition between elements and time spent in each element. It entails a 2-step data reduction technique: (1) optimal matching analysis to minimize the “cost” required to transform the work-family trajectories of any 2 given women to match and (2) hierarchical cluster analysis to identify the optimal number of work-family profile clusters by using the matrix of optimal matching distances.
Sequence analysis identified a solution of 7 work-family profile clusters, which produced maximum within-cluster homogeneity and maximum between-cluster heterogeneity: (1) women who did not have children and participated in the paid labor force (“working nonmothers”); (2) married women with children who continuously participated in the paid labor force (“working married mothers who continuously worked”); (3) married women with children who took a short amount of time out of the paid labor force when their children were young (“working married mothers who went back to work earlier”); (4) married women with children who took more time out of the paid labor force when their children were young (“working married mothers who went back to work later”); (5) women who experienced a long spell as a single mother not engaged in the paid labor force (“nonworking single mothers”); (6) women who experienced a long spell as a single mother who participated in the paid labor force (“working single mothers”); and (7) married women with children who never engaged in the paid labor force (“nonworking married mothers”). Figure e-1 (dataverse.ucla.edu/dataset.xhtml?persistentId=doi:10.25346/S6/ZR9FRC) visually displays the work-family profiles. Initial analyses showed very similar later-life memory trajectories for married women with children who participated in the paid labor force, regardless of whether they took time out of the labor force when their children were young. Thus, our primary results combine the 3 groups of married working mothers together (“working married mothers”), resulting in 5 prototypical work-family profiles. Results for all 7 prototypical work-family profiles are shown in appendix e-2.
Memory assessment
We used a previously developed memory composite score combining proxy and direct memory assessments for longitudinal analyses.24 For ease of interpretation, memory composite scores were standardized to the baseline analytic sample. All participants interviewed directly completed an immediate and delayed recall of a 10-word list. For individuals too impaired to participate, proxy informants, typically spouses, assessed the participants' memory on a 5-item Likert scale and completed the 16-item Informant Questionnaire for Cognitive Decline (IQCODE).25,26 A total of 1.7% of all memory assessments included in the study were based on proxy scores.
Death
At each biennial study wave, all previously surviving participants were contacted. If death was reported, date of death was obtained via interview with next of kin.27
Covariates
All models were adjusted for practice effects with an indicator variable for first memory assessment.28 We also included as covariates variables conceptualized as potential confounders of effects of work-family profiles on later-life memory trajectories. All potential confounders were temporally prior to the life course period included in work-family sequences (ages 16–50 years). Age at baseline memory assessment was considered as age in years at first memory assessment. Race/ethnicity was based on self-report (non-Latino Black/African American, non-Latino White, and Latino/Hispanic or other racial/ethnic group). Birth in the Southern United States (“Southern birth”), which has been shown to be associated with stroke29,30 and poorer later-life cognitive health,31–33 was self-reported state of birth classified by US Census region (Delaware; Maryland; Washington, DC; Virginia; West Virginia; North Carolina; South Carolina; Georgia; Florida; Kentucky; Tennessee; Mississippi; Alabama; Oklahoma; Texas; Arkansas; Louisiana). Childhood socioeconomic status was measured with a theoretically driven, validated index of self-reported factors.34 Self-reported educational attainment was dichotomized as <12 vs ≥12 years to minimize overlap between timing of educational attainment and work-family profiles.
To further characterize the sample, we examined 2 additional covariates that we did not conceptualize as potential confounders: number of children and household wealth calculated as the sum of all wealth components (excluding second home) less all debt reported at the HRS visit closest to age 55 years.35
Statistical analysis
We used linear mixed effects models36 to estimate effects of work-family profiles on later-life rate of memory decline starting at age 55. We used age centered at 65 years as the timescale and modeled the time trend with linear splines with knots every 5 years at ages 60, 65, 70, and 75 to accommodate nonlinearities and included interactions between work-family profile group and time trend splines. We included 3 correlated random effects: intercept, linear slope, and linear spline with a knot at age 65 years to model the within-person variance–covariance between observations. We considered models with covariate sets guided by our conceptual model with the goal of controlling for confounders of effects of work-family profiles on later-life memory decline. Model 1 adjusted for practice effects and age at baseline memory assessment. Model 2 in addition adjusted for race/ethnicity and Southern birth and interaction terms for both with the time trend splines. Model 3 in addition adjusted for childhood socioeconomic status and interaction terms between childhood socioeconomic status and the time trend splines. Model 4 in addition adjusted for educational attainment (<12 vs ≥12 years) and interaction terms with time trend splines.
To visually represent findings, we plotted estimated memory trajectories for each work-family profile holding covariates constant at reference values: age 55 at baseline memory assessment, non-Latino White, birth outside the Southern United States, childhood socioeconomic status score of 0, and ≥12 years of education for the fully adjusted model.
To assist with interpretation of the magnitude of the associations between work-family profiles and later-life memory decline, we translated group differences in average memory scores estimated from fully adjusted linear mixed effects models to risk ratios (RRs) and risk differences (RDs) for memory impairment at age 70. We computed the RR and risk difference estimates assuming 10% prevalence of memory impairment at age 70 among working married mothers based on the literature37; we repeated calculations assuming 5% prevalence (details provided in appendix e-3, dataverse.ucla.edu/dataset.xhtml?persistentId=doi:10.25346/S6/ZR9FRC).
Primary analyses evaluated the 5 work-family profiles. In a secondary analysis, we compared memory trajectories for the “working” profiles and “nonworking” profiles. Working profiles included working nonmothers, working married mothers, and working single mothers. Nonworking profiles included nonworking single mothers and nonworking married mothers.
Sensitivity analyses
To evaluate potential selective survival, we compared characteristics of participants who died during the study period, those lost to follow-up (i.e., those who did not participate in the 2016 memory assessment, but were presumed alive), and those who participated in the 2016 memory assessment. In addition, we repeated analyses using shared parameter (shared random intercept and slope terms) joint longitudinal-survival models to account for selective survival using the JMFit macro.38 Based on available software, we used study time as the timescale without splines.
We repeated analyses using time since baseline memory assessment as the timescale, with linear splines with knots at 4, 8, and 12 years and random effects for intercept and slope spline with a knot at 8 years.
Statistical analyses were performed in SAS version 9.4 (SAS Institute).
Data availability
The data used for analyses are available from the HRS website (hrs.isr.umich.edu/data-products).
Results
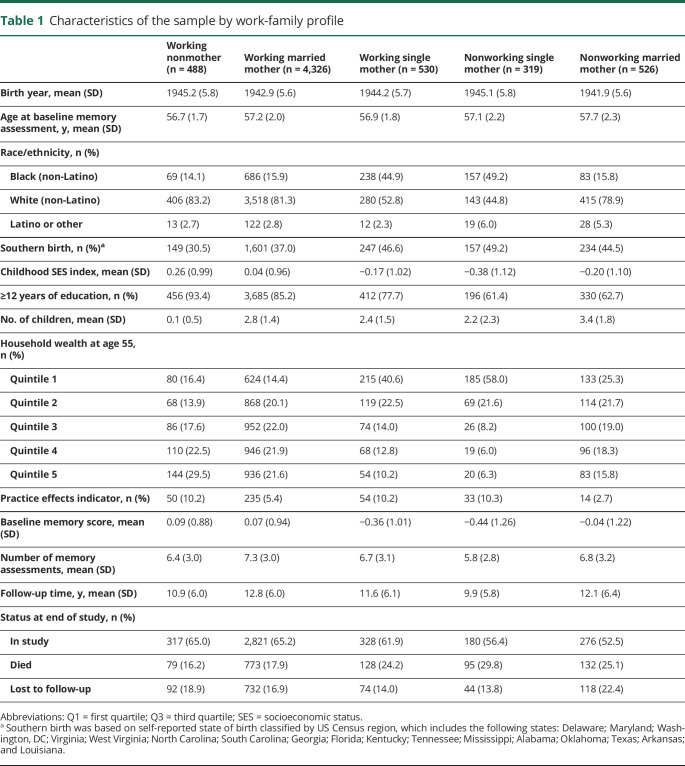
The analytic sample included 6,189 women. Mean age at baseline memory assessment was 57.2 years (range 55.0–74.5). Mean age at baseline memory assessment was oldest among nonworking married mothers and youngest among working nonmothers (table 1). As a group, working nonmothers had more advantaged backgrounds with regards to race/ethnicity, place of birth, childhood socioeconomic status index, and educational attainment. Single mothers, both working and nonworking, tended to have less advantaged backgrounds. Among mothers, average number of children ranged from 2.2 among nonworking single mothers to 3.4 among nonworking married mothers. At age 55, nonworking single mothers and working single mothers tended to have the lowest wealth, working nonmothers and working married mothers tended to have the highest wealth, and nonworking married mothers tended to have intermediate wealth.
Table 1.
Characteristics of the sample by work-family profile
Mean baseline memory scores were highest among working nonmothers and working married mothers and lowest among single mothers. Over an average follow-up of 12.3 years (range 0–21.2 years), participants participated in an average of 7.0 memory assessments (range 1–11). Average follow-up length and number of memory assessments was longest among working married mothers and shortest among nonworking single mothers.
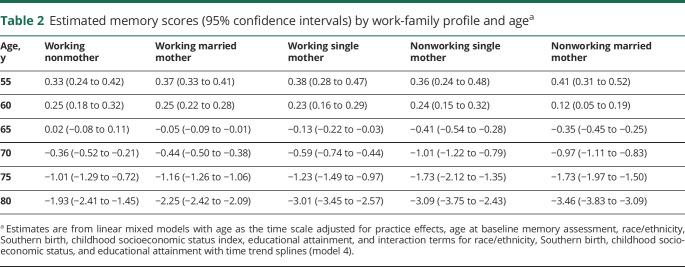
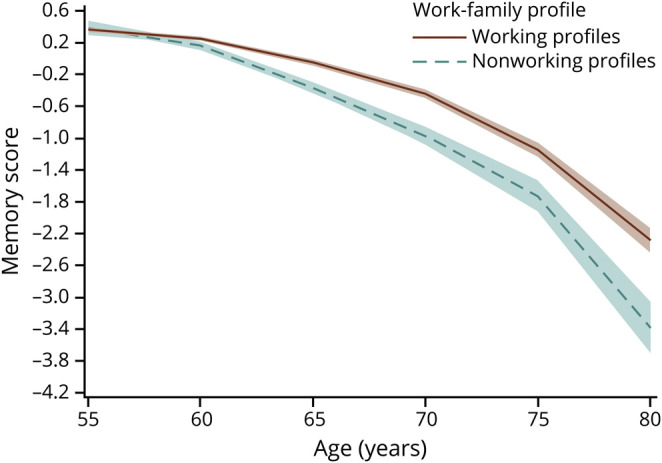
Estimates from linear mixed effects models adjusted for practice effects and age at first memory assessment (model 1) suggested lower average memory scores at age 55 years among single mothers (working and nonworking) than other work-family profile groups (figure e-3 and table e-2, dataverse.ucla.edu/dataset.xhtml?persistentId=doi:10.25346/S6/ZR9FRC). After adjusting for practice effects and potential confounders, there were no major differences in average memory scores at age 55 years by work-family profile group (figure 1, table 2, and table e-2). Average rate of memory score decline between ages 55 and 60 years may have been slightly faster among nonworking married mothers compared with working married mothers (table 2 and table e-2).
Figure 1. Estimated memory trajectories (95% confidence intervals) by work-family profile among women born between 1935 and 1956 in the Health and Retirement Study.
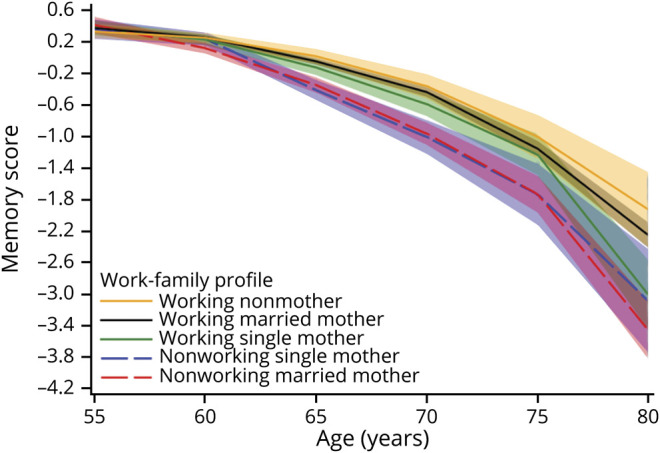
Table 2.
Estimated memory scores (95% confidence intervals) by work-family profile and agea
After age 60 years, average rate of memory score decline was on average slower for women who participated in the paid labor force compared with women who did not. For example, between ages 60 and 70, average memory score decline was 0.69 standardized units (95% confidence interval [CI] −0.75 to −0.63) among working married mothers. Over the same age span, average memory score decline was 1.25 standardized units (95% CI −1.46 to −1.03) among nonworking single mothers and 1.09 standardized units (95% CI −1.23 to −0.94) among nonworking married mothers (table 3). Thus, average memory score decline between ages 60 and 70 was more than 50% greater among women without paid labor force participation, compared with working married mothers. Overall, average rate of memory score decline was similar for the 2 groups who did not engage in paid work: nonworking single mothers and nonworking married mothers. There was some suggestion that after age 75, average rate of memory score decline was slightly faster for working single mothers vs working married mothers, although estimates after age 75 were imprecise due to small number of observations (table e-2, dataverse.ucla.edu/dataset.xhtml?persistentId=doi:10.25346/S6/ZR9FRC).
Table 3.
Estimated mean change in memory scores at ages 60–70 (95% confidence interval [CI]) by work-family profile and estimated mean differences in change in memory scores at ages 60–70 (95% CI) between work-family profile groupsa
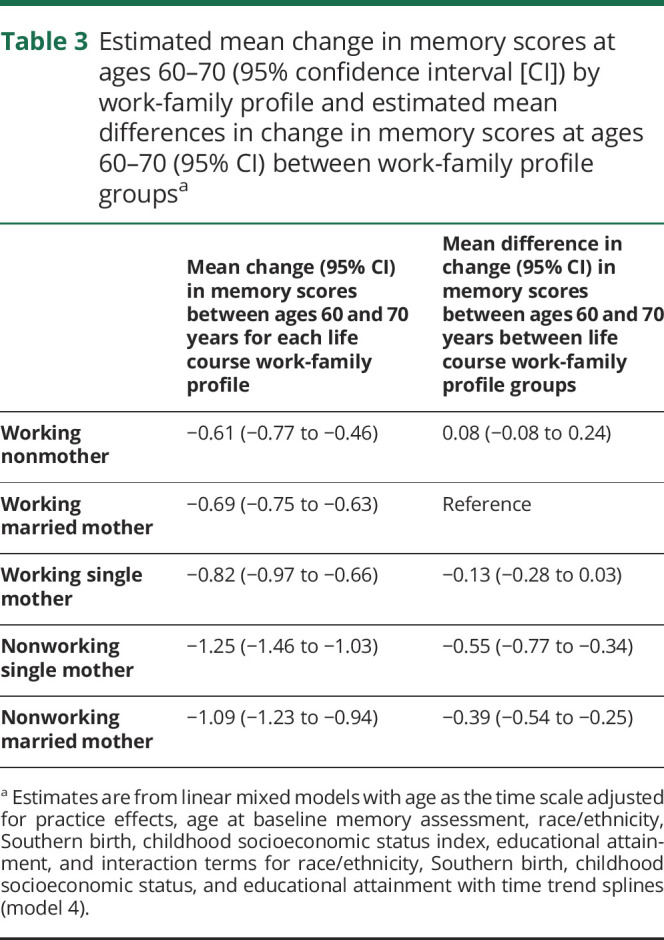
The 0.57 standardized unit difference in average memory scores at age 70 between nonworking single mothers and working married mothers translates to a 2.02 risk ratio for memory impairment and a 10.2% risk difference for memory impairment assuming 10% population prevalence of memory impairment among working married mothers (appendix e-3, dataverse.ucla.edu/dataset.xhtml?persistentId=doi:10.25346/S6/ZR9FRC). Similarly, the 0.53 standardized unit difference in average memory scores at age 70 between nonworking married mothers and working married mothers translates to a 1.94 RR for memory impairment and a 9.4% risk difference for memory impairment. Estimated RRs were larger and risk differences were smaller assuming 5% population prevalence of memory impairment among working married mothers (appendix e-3). In secondary analyses comparing memory trajectories for the 3 work-family profiles that included paid labor force participation and the 2 work-family profiles that did not include paid labor force participation, differences in average rates of memory decline were pronounced: between ages 60 and 70, average memory score decline was −0.44 standardized units (95% CI −0.56 to −0.32) greater among women without paid labor force participation compared with women who participated in the paid labor force (figure 2, table e-3, and table e-4, dataverse.ucla.edu/dataset.xhtml?persistentId=doi:10.25346/S6/ZR9FRC).
Figure 2. Estimated memory trajectories (95% confidence intervals) by working vs nonworking profiles among women born between 1935 and 1956 in the Health and Retirement Study.
In sensitivity analyses evaluating the potential influence of selective mortality on study results, we found that 63.4% of study participants remained in the study through the 2016 study wave, 19.5% died prior to 2016, and 17.1% were lost to follow-up (i.e., did not participate in the 2016 wave, but presumed alive). Cumulative mortality was highest among nonworking single mothers and lowest among working married mothers and working nonmothers. Loss to follow-up was highest among nonworking married mothers (table 1). Compared with women who remained in the study, those who died tended to be older at baseline, have lower baseline memory scores, and have less advantaged early-life backgrounds (table e-5, dataverse.ucla.edu/dataset.xhtml?persistentId=doi:10.25346/S6/ZR9FRC). Women lost to follow-up were similar to those who remained, although women lost to follow-up were on average slightly older at baseline and had higher childhood socioeconomic status. Results from joint-longitudinal models to account for selective survival were qualitatively similar to results from linear mixed effects models (table e-6), as were models using time since baseline instead of age as the time scale (figure e-4).
Discussion
In a national cohort study of US women, rates of later-life memory decline were slower among women whose work-family trajectories included substantial periods of engagement in the paid labor force between ages 16 and 50 years. Conversely, rates of later-life memory decline were faster among women without paid labor force participation during early adulthood and midlife. In other words, results suggest that participating in the paid labor force protected against memory decline, regardless of family structure.
We hypothesized that after accounting for potential early-life confounders, rates of later-life memory decline would be slowest among married mothers who participated in the paid labor force and fastest among women who experienced prolonged periods of single motherhood, especially those who had not engaged in the paid labor force. Our hypothesis was based on literature linking labor force participation to later-life cognitive health6–9 and literature linking family structure to women's later-life health. The latter studies found that US and European women who experienced prolonged periods of single motherhood experienced greater risk of cardiovascular disease and stroke,18 physical disability,13 and mortality16,17 compared with working married mothers. However, the present study suggests that paid labor force participation protects against memory decline, regardless of family structure. Moreover, timing of labor force participation did not appear to matter: rates of memory decline were similar for married working mothers, including those who consistently worked, those who stayed home with children for a few years before reentering the paid labor force, and those who stayed home with children for many years before reentering the paid labor force. This suggests that the cognitive benefits of labor force participation may extend far into adulthood. This is consistent with a recent national study reporting that high-skill employment during working age predicted better numerical reasoning scores in later life, but this benefit plateaued after 4 years of high-skill employment.9
To our knowledge, this is the first study to evaluate the influence of work-family profiles on later-life cognitive decline, though our finding that paid labor force participation protects against later-life memory decline is supported by prior research. A recent study among European women found that partnered mothers who worked full- or part-time had the highest levels of cognitive performance in later life and women who spent most of their lives outside the paid labor force had the lowest levels of cognitive performance in later life.39 Interestingly, the authors found that women who worked part-time had higher levels of cognitive performance than women who worked full-time. However, this study examined cross-sectional cognitive performance, while the present study examined rates of cognitive change. Prior studies have documented protective associations between higher complexity of main lifetime occupation and later-life cognitive health6–9 and harmful associations between retirement and cognitive health40,41 in US and European cohorts. In addition to cognitive stimulation, paid labor force participation could promote later-cognitive health by promoting social engagement, which has been linked to later-life cognitive health.10,11
Our finding that women who participated in the paid labor force experienced slower later-life memory decline is unlikely to be completely attributable to confounding by early-life social factors. For example, in fully adjusted models, average rates of later-life memory decline were slower for working single mothers compared with nonworking married mothers, even though nonworking married mothers came from more privileged backgrounds. In addition, our analysis accounted for potential early-life confounders, including race/ethnicity, Southern birth, childhood socioeconomic status, and educational attainment. Notably, in models only adjusting for practice effects and age at baseline memory assessment, there were sizable differences in memory scores between work-family profiles: at age 55, average memory scores among single mothers (working and nonworking) were more than four-tenths of a standardized unit lower than average memory scores among working married mothers. In fully adjusted models, there were no differences in average memory scores between groups at age 55, suggesting that these models accounted for confounding by early-life factors that influence both work-family profiles and memory performance at age 55.
Strengths of our study include the large, national cohort study design with long follow-up, life course characterization of work-family profiles, and focus on women's social experiences. By evaluating rates of later-life memory decline, we were able to distinguish between premorbid memory function and later-life memory decline, which is more representative of accumulation of dementia-related pathology.19 Furthermore, we evaluated work-family profiles between ages 16 and 50 and memory decline starting at age 55, minimizing potential for reverse causation. While level of memory function in adulthood could influence work-family profiles, after adjusting for potential confounders, memory scores were similar across work-family profiles between ages 55 and 60. Our primary outcome was rate of memory decline, and it is unlikely that memory decline prior to age 50 had a significant influence on women's work-family profiles between ages 16 and 50.
This study has limitations. The present study assessed marriage, but did not assess nonmarital partnerships. Because same-sex marriages were not legal in the United States during the time of exposure assessment for the present study, this would particularly affect measurement of single motherhood among sexual minority women. The present study also lacks the capacity to disambiguate between cisgender and transgender women; thus, it is unclear to what degree work-family experiences affect later-life memory decline among transgender women. Characterization of work-family profiles relied on retrospective reporting of dates of employment, marriage, and parenthood. We did not examine nuances of the 3 elements of work-family profiles; most notably, we could not distinguish between full- and part-time employment. Memory performance was assessed using a brief assessment (immediate and delayed word recall), and we lack assessment of other cognitive domains. In addition, we focused exclusively on working for pay. If volunteering throughout early adulthood and midlife confers benefits to later-life cognitive health, including women who volunteered in the nonworking profiles would bias results towards the null. A potential confounder not measured in our analysis is rural residence in early adulthood and midlife, which could influence access to employment and childcare. If rural residence in this life course period made participation in the paid labor force more difficult for women and was also associated with faster later-life memory decline, this could contribute to observed associations between engagement in the paid labor force and slower later-life memory decline. In addition, residual confounding, particularly from time-dependent confounder mediators, cannot be ruled out. Development of methods for accounting for time-dependent confounder mediators in sequence analysis is an important area of future research.
In a national study, women who participated in the paid labor force between early adulthood and midlife, regardless of family structure, experienced slower memory decline in later life than their nonworking peers, suggesting paid labor force participation plays a strong role in later-life cognitive health. These early findings suggest that policies that support paid labor force participation could be an effective population-level strategy to prevent later-life memory decline. Important areas of future research include disentangling potential mechanisms driving observed associations.
Glossary
- CI
confidence interval
- HRS
Health and Retirement Study
- IQCODE
Informant Questionnaire for Cognitive Decline
- RD
risk difference
- RR
risk ratio
Appendix. Authors
Footnotes
Editorial, page 1027
Study funding
This work was supported by National Institute on Aging grant numbers R00AG053410 and R01AG040248 and the Karen Toffler Charitable Trust.
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology 2013;80:1778–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alzheimer's Association. 2019 Alzheimer's disease facts and figures. Alzheimers Dement 2019;15:3. [Google Scholar]
- 3.Andrew MK, Tierney MC. The puzzle of sex, gender and Alzheimer's disease: why are women more often affected than men? Womens Health 2018;14:174550651881799. [Google Scholar]
- 4.Mayeda ER. Invited commentary: examining sex/gender differences in risk of Alzheimer disease and related dementias: challenges and future directions. Am J Epidemiol 2019;188:1224–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldin C. The quiet revolution that transformed women's employment, education, and family. Am Econ Rev 2006;96:1–21. [Google Scholar]
- 6.Kröger E, Andel R, Lindsay J, Benounissa Z, Verreault R, Laurin D. Is complexity of work associated with risk of dementia? Am J Epidemiol 2008;167:820–830. [DOI] [PubMed] [Google Scholar]
- 7.Vemuri P, Lesnick TG, Przybelski SA, et al. Association of lifetime intellectual enrichment with cognitive decline in the older population. JAMA Neurol 2014;71:1017–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pool LR, Weuve J, Wilson RS, Bültmann U, Evans DA, Mendes de Leon CF. Occupational cognitive requirements and late-life cognitive aging. Neurology 2016;86:1386–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kobayashi LC, Feldman JM. Employment trajectories in midlife and cognitive performance in later life: longitudinal study of older American men and women. J Epidemiol Community Health 2019;73:232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sommerlad A, Sabia S, Singh-Manoux A, Lewis G, Livingston G. Association of social contact with dementia and cognition: 28-year follow-up of the Whitehall II cohort study. PLoS Med 2019;16:e1002862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuiper JS, Zuidersma M, Zuidema SU, et al. Social relationships and cognitive decline: a systematic review and meta-analysis of longitudinal cohort studies. Int J Epidemiol 2016;45:1169–1206. [DOI] [PubMed] [Google Scholar]
- 12.Mani A, Mullainathan S, Shafir E, Zhao J. Poverty impedes cognitive function. Science 2013;341:976–980. [DOI] [PubMed] [Google Scholar]
- 13.Berkman LF, Zheng Y, Glymour MM. Mothering alone: cross-national comparisons of later-life disability and health among women who were single mothers. J Epidemiol Community Heal 2015;69:865–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berkman PL. Spouseless motherhood, psychological stress, and physical morbidity. J Health Soc Behav 1969;10:323–334. [PubMed] [Google Scholar]
- 15.Young LE, Cunningham SL, Buist DSM. Lone mothers are at higher risk for cardiovascular disease compared with partnered mothers. Data from the National Health and Nutrition Examination Survey III (NHANES III). Health Care Women Int 2005;26:604–621. [DOI] [PubMed] [Google Scholar]
- 16.McKetta S, Prins SJ, Platt J, Bates LM, Keyes K. Social sequencing to determine patterns in health and work–family trajectories for U.S. women, 1968–2013. SSM Popul Heal 2018;6:301–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sabbath EL, Guevara IM, Glymour MM, Berkman LF. Use of life course work–family profiles to predict mortality risk among US women. Am J Public Health 2015;105:e96–e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Hedel K, Mejía-Guevara I, Avendaño M, et al. Work-family trajectories and the higher cardiovascular risk of American women relative to women in 13 European countries. Public Health 2016;106:1449–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weuve J, Proust-Lima C, Power MC, et al. Guidelines for reporting methodological challenges and evaluating potential bias in dementia research. Alzheimers Dement 2015;11:1098–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort profile: the Health and Retirement Study (HRS). Int J Epidemiol 2014;43:576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abbott A. Sequence analysis: new methods for old ideas. Annu Rev Sociol 1995;21:93–113. [Google Scholar]
- 22.Aisenbrey S, Fasang AE. New life for old ideas: the “second wave” of sequence analysis bringing the “course” back into the life course. Sociol Methods Res 2009;38:420–462. [Google Scholar]
- 23.Wu LL. Some comments on “sequence analysis and optimal matching methods in sociology: review and prospect. Sociol Methods Res 2000;29:41–64. [Google Scholar]
- 24.Wu Q, Tchetgen Tchetgen EJ, Osypuk TL, White K, Mujahid M, Maria Glymour M. Combining direct and proxy assessments to reduce attrition bias in a longitudinal study. Alzheimer Dis Assoc Disord 2013;27:207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jorm AF. A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): development and cross-validation. Psychol Med 1994;24:145–153. [DOI] [PubMed] [Google Scholar]
- 26.Jorm AF, Christensen H, Korten AE, Jacomb PA, Henderson AS. Informant ratings of cognitive decline in old age: validation against change on cognitive tests over 7 to 8 years. Psychol Med 2000;30:981–985. [DOI] [PubMed] [Google Scholar]
- 27.Health and Retirement Study. Health and Retirement Study 2016 Tracker Early, Version 3.0 Data Description and Usage [online]. 2019. Available at: hrs.isr.umich.edu/news/hrs-tracker-2016-early-version-30. Accessed November 27, 2019. [Google Scholar]
- 28.Vivot A, Power MC, Glymour MM, et al. Jump, hop, or skip: modeling practice effects in studies of determinants of cognitive change in older adults. Am J Epidemiol 2016;183:302–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glymour MM, Kosheleva A, Boden-Albala B. Birth and adult residence in the Stroke Belt independently predict stroke mortality. Neurology 2009;73:1858–1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Howard VJ, McClure LA, Maria Glymour M, et al. Effect of duration and age at exposure to the stroke belt on incident stroke in adulthood. Neurology 2013;80:1655–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glymour MM, Kosheleva A, Wadley VG, Weiss C, Manly JJ. Geographic distribution of dementia mortality. Alzheimer Dis Assoc Disord 2011;25:196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu SY, Glymour MM, Zahodne LB, Weiss C, Manly JJ. Role of place in explaining racial heterogeneity in cognitive outcomes among older adults. J Int Neuropsychol Soc 2015;21:677–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilsanz P, Mayeda ER, Glymour MM, Quesenberry CP, Whitmer RA. Association between birth in a high stroke mortality state, race, and risk of dementia. JAMA Neurol 2017;74:1056–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vable AM, Gilsanz P, Nguyen TT, Kawachi I, Glymour MM. Validation of a theoretically motivated approach to measuring childhood socioeconomic circumstances in the Health and Retirement Study. PLoS One 2017;12:e0185898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bugliari D, Campbell N, Chan C, et al. RAND HRS Longitudinal File 2016 (V1) Documentation; 2019. [Google Scholar]
- 36.Weiss RE. Modeling Longitudinal Data. New York: Springer Science & Business Media; 2005. [Google Scholar]
- 37.Petersen RC, Lopez O, Armstrong MJ, et al. Practice guideline update summary: mild cognitive impairment: report of the guideline development, dissemination, and implementation. Neurology 2018;90:126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang D, Chen MH, Ibrahim JG, Boye ME, Shen W. JMFit: a SAS macro for joint models of longitudinal and survival data. J Stat Softw 2016;71:1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ice E, Ang S, Greenberg K, Burgard S. Women's work-family histories and cognitive performance in later life. Am J Epidemiol 2020;189:922–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dufouil C, Pereira E, Ve Chêne G, et al. Older age at retirement is associated with decreased risk of dementia. Eur J Epidemiol 2014;29:353–361. [DOI] [PubMed] [Google Scholar]
- 41.Xue B, Cadar D, Fleischmann M, et al. Effect of retirement on cognitive function: the Whitehall II cohort study. Eur J Epidemiol 2018;33:989–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used for analyses are available from the HRS website (hrs.isr.umich.edu/data-products).