Abstract
Background
Epidemiologic assessment of surgical admissions into intensive care units (ICU) provides a framework to evaluate healthcare system efficiency and project future healthcare needs.
Methods
We performed a 9-year (2008-2016), retrospective cohort analysis of all adult admissions to 88 SICUs using the prospectively and manually abstracted, Cerner APACHE Outcomes database. We stratified patients into 13 surgical cohorts and modeled temporal-trends in admission, mortality, SICU length of stay (LOS) and change in functional status (FS) using generalized mixed-effects and Quasi-Poisson models to obtain risk-adjusted outcomes.
Results
We evaluated 78,053 ICU admissions and observed a significant decrease in admissions after transplant and thoracic surgery, with a concomitant increase in admissions after otolaryngological and facial reconstructive procedures (all p < 0.05). While overall risk-adjusted mortality remained stable over the study period; mortality significantly declined in orthopedic, cardiac, urologic, and neurosurgical patients (all p < 0.05). Cardiac, urologic, gastrointestinal, neurosurgical, and orthopedic admissions showed significant reductions in LOS (all p < 0.05). The overall rate of FS deterioration increased per year, suggesting ICU-related disability increased over the study period.
Conclusion
Temporal analysis demonstrates a significant change in the type of surgical patients admitted to the ICU over the last decade, with decreasing mortality and LOS in selected cohorts, but an increasing rate of FS deterioration. Improvement in ICU outcomes may highlight the success of healthcare advancements within certain surgical cohorts, while simultaneously identifying cohorts that may benefit from future intervention. Our findings have significant implications in healthcare systems planning, including resource and personnel-allocation, education, and surgical training.
Level of Evidence:
IV
Study Type:
Economic/ Decision
Keywords: Surgical ICU, Incidence, Mortality, Length of Stay, Functional Status
Introduction
The field of critical care medicine is rapidly expanding in the United States.(1-5) Over a period of two decades, the total number of intensive care unit (ICU) beds has increased by over 35% (from 69,300 beds in 1985 to 93,955 in 2005) along with a 44% increase in ICU length of stay (LOS) (16.1 million inpatients days to 23.2 million inpatient days).(2,3) Mirroring these trends, the costs of providing critical care has also escalated disproportionately. From 2000 to 2005 there was a 44.2% rise in spending, with a total of $81.7 billion accounting of 0.66% of US gross domestic product spent in 2015.(3) The compounding effects of an aging population, increased insurance coverage, limited workforce, rising complexity of care and increasing severity of illness will exponentially increase the need for critical care services in the future.(6)
Despite the burden of disease and rising critical care exigency in the United States, the epidemiology of critical illness remains inadequately characterized, especially within the surgical literature.(6) Several authors attribute this to either the lack of a national, centralized, administrative or outcomes-based data repository that accurately captures critical care admissions or the inability of procedure or hospital-specific diagnosis codes to effectively identify the entire spectrum of critical illness.(6,7)
Several studies report temporal decreases in hospital mortality and morbidity for various disease processes that commonly require ICU level care, such as sepsis, coronary artery bypass graftings and other high-risk procedures.(8-11) Large ICU-based cohort studies from Australasia, England and Canada have demonstrated significant temporal reductions in risk-adjusted mortality and ICU LOS, and recent attempts from the United States also note similar trends.(12-15) However, these studies largely focus on medical ICU’s and non-surgical admissions; to our knowledge, no study has exclusively evaluated surgical ICU admissions within the United States. Such an appraisal helps characterize the variety of surgical patients admitted to ICU’s and can increase the efficiency of healthcare delivery by identifying needs for resource and personnel allocation. Furthermore, these efforts help identify priorities for training, education and outcomes-based research.(14,15)
In our current study, we leverage a national ICU outcomes database from the United States and model the temporal variation of surgical admissions within ICU’s, mortality, ICU LOS and the change of functional status (FS) over almost a decade. We hypothesize that the population of surgical patients admitted to ICU’s have increased over the last decade, with decreases in ICU mortality, ICU LOS, along with improvements to FS from baseline.
Methods
Data and Study Design
We performed a 9-year retrospective, temporal, cohort analysis using the APACHE outcomes database (Cerner Corporation, Kansas City, MO). This database includes prospectively collected clinical data from a cohort of 238 nonrandomized ICU’s across the United States from 2008-2016. The APACHE outcomes database compiles de-identified data from all participating ICU’s that voluntarily subscribe to its national benchmarking and quality improvement service.(16) It collects clinical, physiological and laboratory-based data including primary diagnosis for ICU admission, patient location prior to admission, severity scores, ventilator status, and duration of ICU LOS during the first 24-hours following admission, along with outcomes-based data from all patients admitted to the ICU.(16-18) APACHE outcomes use a combination of trained clinical-coordinators and an integrated electronic interface to abstract data.(19) Each coordinator is enrolled in a standardized, three-phase training session and automated software ensures that the data collected from the electronic interface is valid and devoid of incongruous or erroneous data points.(20) Details of data collection, validation, reliability and data-audit have been described elsewhere. (18-24) Our institutional ethical review board approved this study (UMN STUDY00001489).
Inclusion and Exclusion Criteria
The APACHE outcomes database included a total of 345,650 adult ICU admissions from 2008-2016, from 238 ICU’s. From this cohort, we included all individual patient encounters that had a primary surgical diagnosis on ICU admission from 2008 to 2016. We then excluded all patients who were <15 years of age. We also excluded any ICU with < 3 years of continuous, temporal data, OR any ICU with <25 patient admissions within any given year, during the study period (Figure 1).
Figure 1.
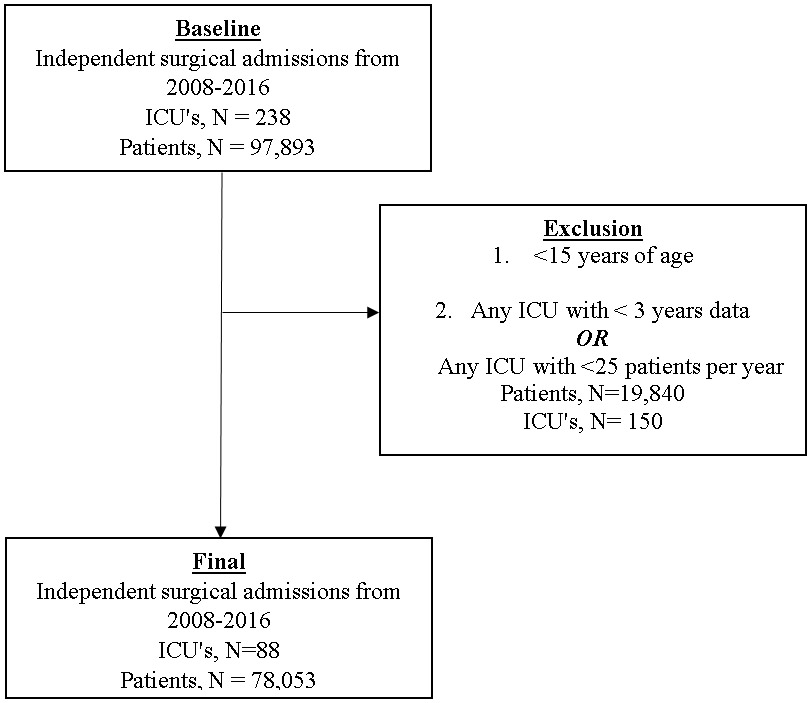
Inclusion and Exclusion Criteria
ICU= Intensive Care Unit
Epidemiological Classification
To facilitate temporal modeling, we classified all patients into 13 distinct surgical cohorts. The classification was based on the type of surgical procedure, the primary surgical team providing care, and the involved organ system. The surgical cohorts included: transplant; orthopedic; breast, soft-tissue, and extremity; vascular; hepatobiliary; cardiac; thoracic; gastrointestinal; urological; obstetric and gynecological; trauma; neurosurgery and spine; and facial and ear, nose and throat (ENT) surgery. Details of each surgical procedure and the diagnoses included under each cohort are provided in Supplementary Table 1.
Outcomes of Interest
Our primary outcome of interest was the temporal change in the incidence of surgical admissions within ICU’s. Our secondary outcomes included: the change in mortality, LOS, and the rate of change in functional status from baseline within each surgical cohort. Functional status was captured as an ordinal variable, both at ICU admission and at hospital discharge, and was assigned to one of three categories (independent, partially dependent and fully dependent). A designation of declined or remained stationary - functional status was based on the change, or lack thereof, in functional status from admission to hospital discharge.
Statistical Methods
Model Estimation
We used generalized mixed-effects regression to account for the clustered nature of the data and to adjust for potential hospital-specific variation. Mortality and ICU admission incidence rates were modeled at the hospital level using generalized negative-binomial models. Year was the predictor of interest, with a random intercept per ICU and an offset for the log number of cases per ICU per year in each epidemiologic category. Mortality models were additionally adjusted for severity of disease presentation using the validated APACHE III score.(23) All potential confounders were centered and scaled prior to fitting. We modeled ICU LOS using patient-level, generalized linear mixed-effects models with a random intercept for hospital, the year term as the predictor of interest, and adjusted for unscaled age, race, sex and APACHE III score. To model the rate of changing functional status, we used hospital-level Quasi-Poisson models with an offset of log cases per hospital per year per epidemiologic classification and year as the predictor of interest. For each functional status model, we adjusted for age, race, sex, and APACHE III score using centered and scaled covariates. Despite fitting a large number of models, we did not correct for multiple hypothesis testing as this study was primarily exploratory in nature. Incidence rate-ratios (IRR) for ICU admissions, mortality, and functional status, along with estimates for LOS are reported and graphed with 95% confidence intervals (CI) for a one-year increase. For the functional status models, the estimate denotes the IRR of declining, or stationary functional status during an ICU visit for a one-year increase in time.
Missing Variable Analysis
Missing variable analysis identified four variables with missing data; race (N = 1,179, 1.5%), APACHE III score (N = 104, 0.1%), hospital length of stay ( N = 6, <0.01 %) and discharge functional status (N = 19,290, N=24.7%). Little’s test determined that the data was not missing completely at random (MCAR), (χ2 = 64.4, P < 0.001). We did not utilize multiple imputation methods to account for missing data and instead chose complete case analysis for model creation as (i) three of the four variables with missing data had a very low percentages of data missing, (ii) functional status, which had the highest proportion of missing data, was an outcome/dependent variable; multiple imputation techniques are not recommended in these situations as they can inflate standard errors and introducing uncertainty into the models, (iii) pattern analysis of the missing data determined that data missing for functional status was unreported for all patients from certain participating hospitals; it is highly unlikely that this pattern of missingness would systemically bias our models.
Sensitivity Analysis
We performed a post-hoc, best- and worst-case sensitivity analysis for the overall change in discharge functional status, which had nearly 25% missing data. At the person level, we recoded those patients with a missing change in functional status as “stationary” or “independent to fully dependent” for best- and worst-case scenarios, respectively. We then modeled the rate of changing functional status using hospital-level Quasi-Poisson models with the same covariates described earlier.
All analyses were performed using R (version 3.4.0, R Core Team 2019, R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org) and STATA (StataCorp. LLC 2017. Stata Statistical Software: Release 15. College Station, TX).
Results
Of the 345,650 adult ICU admissions, 97,893 (28.3% of all ICU admissions) had a primary surgical diagnosis for ICU admission.. A total of 78,053 patient admissions, from 88 ICU’s across the United States, met our inclusion criteria (Figure 1). ICU and patient characteristics are shown in Table 1 and Table 2, respectively. On average, each participating hospital received 343 ± 204 ICU admissions annually. Geographically, the APACHE database captured data from all four major regions of the United States. However, in comparison with national metrics reported by the Centers for Medicare and Medicaid Services (CMS) Hospital Cost Report in the 2011, ICU’s from the South and Midwest regions were overrepresented in our current analysis (CMS data- proportion of ICU’s from national sample, South = 16.3%, Midwest = 22.6% vs. APACHE data- South= 40.9%, Midwest = 34.1%).(5)
Table 1.
Intensive Care Unit characteristics
| Covariate | 2008-2010 N=24 |
2011-2013 N=61 |
2014-2016 N=71 |
Overall N = 88 |
|---|---|---|---|---|
| Admissions per ICU, per year | 197 ± 175 | 195 ± 171 | 220 ± 163 | 343 ± 204 |
| Region | ||||
| Midwest | 12 (50%) | 27 (44.4%) | 24 (33.8%) | 30 (34.1%) |
| Northeast | 8 (33.3%) | 13 (21.3%) | 7 (9.9%) | 13(14.8%) |
| South | 1 (4.2%) | 14 (23%) | 32 (45.1%) | 36 (40.9(%) |
| West | 3 (12.5%) | 7 (11.5%) | 8 (11.3%) | 9 (10.2%) |
| Hospital Bed Size | 547 ± 287 | 538 ± 293 | 650 ± 406 | 641 ± 363 |
| Teaching Status | ||||
| Large teaching hospital | 15 (62.5%) | 25 (41%) | 24 (33.8%) | 34 (38.6%) |
| Small teaching hospital | 5 (20.8%) | 21 (34.4%) | 24 (33.8%) | 27 (30.7%) |
| Non-teaching hospital | 4 (16.7%) | 15 (24.5%) | 23 (32.4%) | 27 (30.7%) |
ICU = Intensive Care Unit
Descriptive statistics include N (Percent) or Mean ± Standard Deviation where indicated
Table 2.
Patient characteristics
| Variable | 2008-2010 N=10,432 |
2011-2013 N=24,046 |
2014-2016 N=43,575 |
Overall N = 78,053 |
|---|---|---|---|---|
| Age | 62.8 ± 15.9 | 62.9 ± 15.9 | 62.7 ± 15.8 | 62.8 ± 15.9 |
| Sex (Male) | 6,040 (57.9%) | 13,592 (56.5%) | 24,678 (56.6%) | 44,310 (56.8%) |
| Race | ||||
| White | 9,421 (90.3%) | 20,377 (84.7%) | 34,721 (79.7%) | 64,519 (83.9%) |
| Black or African American | 728 (7.0%) | 2,313 (9.6%) | 5,181 (11.9%) | 8,222 (10.5%) |
| Asian | 82 (0.8%) | 378 (1.6%) | 724 (1.7%) | 1,184 (1.5%) |
| Native American | 32 (0.3%) | 223 (0.9%) | 501 (1.1%) | 756 (1.0%) |
| Other | 91 (0.9%) | 467 (1.9%) | 1,635 (3.8%) | 2,193 (2.8%) |
| Admitting Location | ||||
| Home (Elective Surgery) | 6,559 (62.9%) | 13,648 (56.8%) | 25,605 (58.8%) | 45,812 (58.7%) |
| Emergency department (Emergency Surgery) | 448 (4.3%) | 1,117 (4.6%) | 4,064 (9.3%) | 5,629 (7.2%) |
| Another hospital/transfer | 333 (3.2%) | 1,370 (5.7%) | 3,239 (7.4%) | 4,942 (6.3%) |
| Othera | 3,092 (29.6%) | 7,911 (32.8%) | 10,667 (24.4%) | 3,041 (2.8%) |
| Discharge Location | ||||
| Floor | 4,365 (41.8%) | 7,161 (29.8%) | 10,337 (23.7%) | 21,863 (28.0%) |
| Floor with tele-monitoring | 1,215 (11.6%) | 5,241 (21.8%) | 13,314 (30.6%) | 19,770 (25.3%) |
| Step-down unit | 2,287 (21.9%) | 5,599 (23.3%) | 8,336 (19.1%) | 16,222 (20.8%) |
| Tele-unit | 1,379 (13.2%) | 3,263 (13.6%) | 6,516 (15.0%) | 11,158 (14.3%) |
| Home | 508 (4.9%) | 1,115 (4.9%) | 2,581 (5.9%) | 4,264 (5.5%) |
| Other | 678 (6.5%) | 1,667 (6.9%) | 2,491 (5.7%) | 4,776 (6.1%) |
| Admitting Specialty | ||||
| CT surgery | 2,603 (25.0%) | 6,090 (25.3%) | 10,012 (23%) | 18,705 (24.0%) |
| General surgery | 2,168 (20.8%) | 3,776 (15.7%) | 5,778 (12.9%) | 11,722 (15.0%) |
| Neurosurgery | 1,275 (12.2%) | 2,772 (11.5%) | 5,623 (12.9%) | 9,670 (12.4%) |
| Internal medicine | 248 (2.4%) | 737 (3.1%) | 4,720 (10.8%) | 5,705 (7.3%) |
| Vascular surgery | 900 (8.6%) | 1,762 (7.3%) | 2,459 (5.6%) | 5,121 (6.6%) |
| Anesthesia | 71 (0.7%) | 2,027 (8.4%) | 2,325 (5.3%) | 4,423 (5.7%) |
| Critical care | 157 (1.5%) | 737 (3.1%) | 2,392 (5.5%) | 3,286 (4.2%) |
| Trauma | 344 (3.3%) | 863 (3.6%) | 1,715 (3.9%) | 2,922 (3.7%) |
| Other | 2,666 (25.6%) | 5,282 (21.9%) | 8,551 (19.6%) | 16,499 (21.1%) |
| APACHE III Score | 48.5 ± 21.7 | 47.8 ± 21.6 | 47.6 ± 21.9 | 47.8 ± 21.8 |
| Discharge Functional Status | ||||
| Independent | 6,273 (60.1%) | 9,870 (41.0%) | 15,099 (34.7%) | 31,242 (40.0%) |
| Partially dependent | 2,915 (27.9%) | 6,343 (26.4%) | 11,213 (25.7%) | 20,471 (26.2%) |
| Fully dependent | 673 (6.5%) | 802 (3.3%) | 1,964 (4.5%) | 3,439 (4.4%) |
| ICU LOS | 1.7 [0.9, 3.1] | 3 [2,4] | 3 [2,4] | 1.7 [1, 3] |
| Mortality | 335 (3.2%) | 1,186 (4.9) | 1,857 (4.3%) | 3,611 (4.6%) |
ICU = Intensive Care Unit, CT = Cardiothoracic, APACHE = Acute Physiology and Chronic Health Evaluation Score, SAPS = Simplified Acute Physiology Score, LOS = Length of Stay Descriptive statistics include N (Percent), Mean ± Standard Deviation, or Median [Interquartile Range] where indicated
Other includes outpatient surgery center, outpatient clinic, long-term acute care hospital, psychiatric facility, other rehabilitation centers.
Similarly, our data sampled a higher proportion of teaching hospitals than CMS data (the proportion of ICU’s from national CMS sample: large teaching = 28.5%, small teaching = 31.5% vs. APACHE data: large teaching = 38.6%, small teaching = 30.7%.).(5) A higher percentage of patients were male (56.8%) with a mean age of 62.8 ± 15.9 years. While all racial groups were sampled, in comparison to the 2010 United States Census, a higher proportion of patients were White (72.4% vs. 83.9%) with a mean APACHE III score of (47.8 ± 21.8).(25) We observed that nearly 60% of patients were admitted to the ICU directly from home, while approximately 10% were referred from an outpatient clinic, and 7% transferred from the emergency department. Cardiothoracic surgery services admitted the highest volume of patients (N=18,705, 24 %) followed by general surgery (N=11,722, 15.0%). On admission, 40% (N=31,242) of patients had an independent functional status, with approximately 26% (N=20,471) being partially dependent and 4.4% (3,439) being fully dependent on external care.
Change in ICU Admissions
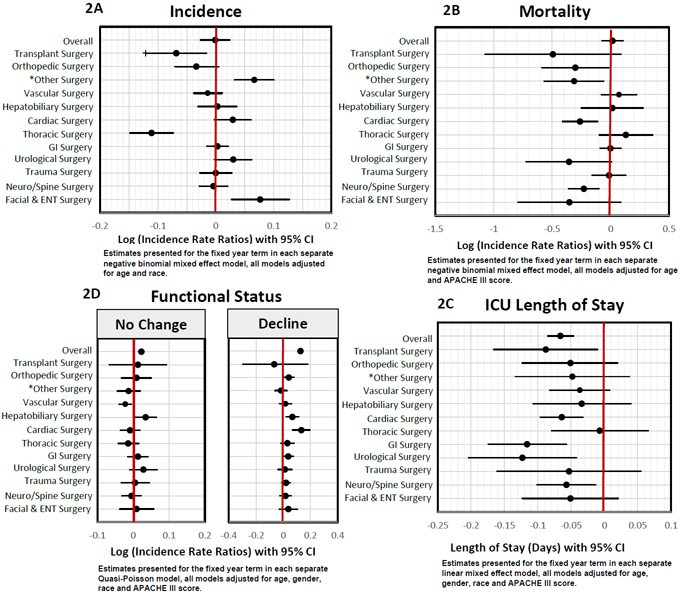
The overall incidence of surgical admissions to the ICU remained unchanged during the study period (IRR = 0.9, P = 0.961, Figure 2A and Supplementary Table 2). Transplant (IRR = 0.9, P = 0.001), and thoracic surgery admissions (IRR = 0.9, P < 0.001) decreased, while facial surgery & ENT (IRR = 1.1, P = 0.003) along with surgery for breast, soft tissue infections and extremity surgery (IRR = 1.1, P <0.001) admissions increased in incidence.
Figure 2.
(A) Log (Incidence rate-ratios) for surgical ICU incidence (B) Log (Incidence rate-ratios) for surgical ICU Mortality (C) Estimates for surgical ICU Length of Stay (D) Log (Incidence rate-ratios) for stationary and declining functional status.
Obstetrics and gynecological surgical models did not converge
*Breast, soft-tissue, extremity surgery
ICU= Intensive Care Unit, GI = Gastrointestinal surgery , ENT = Ear, nose and throat surgery, CI = Confidence interval.
Change in Hospital Mortality for Patients Admitted to the ICU
We observed no temporal change in the overall, risk-adjusted mortality over the 9-year study interval (Figure 2B and Supplementary Table 3). However, certain surgical cohorts such as cardiac surgery (IRR = 0.8, P = 0.001), neuro/spine surgery (IRR = 0.8, P = 0.001), orthopedic surgery (IRR = 0.7, P = 0.039), and breast, soft-tissue infection and extremity surgery (IRR = 0.7, P = 0.016) demonstrated a significant decrease in ICU mortality. Mortality after urological surgery also decreased but failed to achieve statistical significance (IRR = 0.7, P = 0.056).
Change in ICU Length of Stay
Our study showed a decrease in overall ICU LOS (Estimate −0.06, P < 0.001, Figure 2C and Supplementary Table 4) with significant reductions following gastrointestinal, urologic, transplant, cardiac, and neuro/spine surgery.
Change in Functional Status
Overall, we observed an increase in the IRR for declining and stationary functional status (Figure 2D and Supplementary Table 5 & 6). Orthopedic surgery (IRR = 1.04, P = 0.035), hepatobiliary surgery (IRR = 1.1, P = 0.004), and cardiac surgery (IRR = 1.1, P <0.001) demonstrated the greatest increase in declining functional status. Worst-case sensitivity analysis showed similar increases in IRR for stationary (IRR =1.023, P = <0.001) and declining functional status (IRR =1.094, P = <0.001). Similarly, sensitivity analysis for best-case scenarios demonstrated increases in IRR for stationary (IRR =1.030, P = <0.001) and declining functional status (IRR =1.135, P = <0.001, Supplementary Table 7).
Discussion
Our study is an early attempt to epidemiologically model surgical admissions and outcomes from multiple ICU’s within the United States using a non-administrative ICU database that has been used previously by other investigators(23,24). We demonstrate that after adjusting for center-specific variation, the overall cohort of surgical patients requiring critical care services have changed significantly from 2008 to 2016, with concomitant changes in mortality, ICU LOS and functional status.
Temporal Changes in ICU Admissions
An increasing amount of hospital resources are directed towards providing critical care services resulting in a disproportionate increase in the number of ICU beds nationwide. (1-4,26), Despite this increase, postoperative ICU utilization rates have decreased over time; in 2005, the utilization rates were 68% which decreased to approximately 66% in 2010.(27,28) We anticipated the incidence of surgical admissions in ICU’s to increase but our results demonstrate that apart from certain surgical cohorts, overall incidence remained static. While it may remain arduous to prove causality, the decrease in ICU utilization may partially explain our findings.
Other longitudinal ICU models have observed significant trends in medical admissions, where the frequency of certain disease processes such as sepsis, pneumonia, congestive heart failure, and diabetic ketoacidosis increased, while others such as asthma and gastrointestinal obstruction decreased in a temporal fashion.(29) However, a similar evaluation among surgical admissions is lacking. In our study, rates of ICU admissions for facial & ENT surgery, and surgery for necrotizing soft tissue infections increased. Similarly, rates of transplant and thoracic surgery decreased. While it is beyond the scope of this paper to review each trend in detail, our findings are congruent with recent epidemiological studies that document increases in the incidence of oropharyngeal cancers(30) and necrotizing soft tissue infections(31) and decreases in the incidence of lung, bronchus, and esophageal cancer for the past decade.(32,33) Epidemiologically monitoring ICU trends may help project future resource and personnel requirements. Such evaluations help ICU administrators and providers better anticipate cohort-specific needs, providing ample time for these systems to evolve and adapt.
Temporal Changes in Mortality
Hospital mortality after ICU admission has decreased temporally, however, these rates vary significantly based on geography, diagnosis, case-mix of the ICU, and time period of review.(12,13,15,29) An earlier review of US ICU’s that spanned over 24-years (1988-2012) noted a 35% relative reduction in unadjusted mortality(15), while a more contemporary analysis (2009-2013), observed a more modest decline (relative reduction of 3.3%).(29) While we observed a decrease in mortality within certain surgical cohorts, overall mortality rates remained stable. Several reasons may explain this discordance; aggregation of medical and surgical diagnosis (12-15,29), inclusion of patients with only high baseline-risk of mortality or high frequency of admission (15,29), inadequate risk-adjustment, and earlier time periods of review.(12,13,15) All these factors may affect the accuracy of temporal surgical models as surgical ICU admissions have a lower mortality than non-surgical ICU admissions(12) and a primary surgical diagnosis accounts for only 3 of the top 10 most frequent causes for ICU admissions. (29) Consequently, producing accurate estimates for surgical mortality would mandate and independent analysis.
A recent Canadian review reports outcomes analogous to ours.(34) Other publications have also observed decreases in ICU and non-ICU specific mortality following cardiac surgery (8,9,15,29), neuro/spine surgery (15,35), orthopedic surgery (15,36), and soft tissue/extremity surgery. (37) This decline in mortality is attributed to the general improvements made in healthcare delivery, along with the development of modern medical and surgical therapies.(15,29) Post-ICU mortality is an important marker of clinical care; our results aid in establishing benchmarks and help identify cohorts that may benefit from remedial quality improvement initiatives including prospective interventional studies.
Temporal Changes in ICU Length of Stay
We detected a fractional decrease in overall ICU LOS (6% decrease, which translates to 0.06 days or 1.6 hours) along with concurrent reductions within certain surgical cohorts. Despite achieving statistical significance, the clinical relevance of such a trend remains unclear. Earlier studies showed a more significant drop in ICU LOS, but more recent studies concur with our findings which may imply a plateauing effect.(15,29,38) Various political, economic and technologic incentives such as prospective payment systems, managed care plans, innovations in healthcare, adherence to standard practice guidelines, enhanced rehabilitation and mobilization efforts have all helped reduce hospital LOS, however, the complexity and ethical considerations of the ICU care have precluded it from following suit. (29,38-40) Moreover, regional and local studies have demonstrated the effect of operational changes, technologic advances and quality improvement efforts on ICU LOS reduction, but these have been yet to be demonstrated nationally. (29,38,40) This may explain why recent epidemiological reviews(29), including ours, fail to demonstrate significant clinical changes to ICU LOS.
Changes in Functional Status
A decrease in baseline functional status at hospital discharge is independently associated with increased risk of post-discharge mortality; improvements are associated with increased survival.(41) Along with decreases in patient mortality, we observed an increase in the rate of functional status deterioration. This association may allude to the increased burden of survivorship which is expected to grow in the US as a result of an increasing elderly population.(42) Our findings warrant concern, particularly considering the impact such deterioration would have on post-discharge outcomes.
The effect of functional status deterioration on long-term outcomes has garnered national interest, and efforts to better characterize the prevalence, etiology and associated risk factors are underway.(42) Several risk factors like increased age, comorbidities, baseline cognition, prolonged immobilization and mechanical ventilation affect both discharge functional status and the propensity to develop chronic critical illness.(42-44) Identifying patients at higher risk, and targeting modifiable risk factors such as early mobilization, may help reduce subsequent disability.(42) For example, the effective implementation of the “ABCDE” bundles have helped double the rates of mobilization, independently improving functional status.(45) However, studies have largely analyzed the effects of poor functional status; little, to no research has evaluated temporal trends in changing functional status.
It is possible, considering our timeline of review, that our results are reflective of trends prior to the clinical emphasis on chronic critical illness and early mobilization. Currently, there is heightened awareness of the clinical impact of chronic critical illness and early mobilization; expert consensus statements and critical care guidelines all currently recommend daily functional and cognitive assessments.(42) Monitoring these trends in the future may more accurately reflect the effectiveness and success of such interventions. Moreover, identifying patients who are at highest risk for functional status deterioration may enhance resource allocation and encourage quality improvement initiatives.
We acknowledge several limitations of our study. First, this was a retrospective review of a self-selected cohort of ICU’s that used the APACHE system to audit outcomes. Despite observing great variation in geographic distribution, hospital-size, and teaching status, our sample accounted for only 1.4% of all ICU’s in the United States (N=6,119). (27,46) Second, all the ICU’s that met our inclusion criteria did not serially collect data for the entire 9-year duration of the study, which may have introduced bias due to data not missing completely at random. Third, our criteria for classifying patients into distinct epidemiological cohorts was based on a simple yet pragmatic clinical stratification scheme that accounted for the primary surgical team and underlying disease process. It is common clinical practice to aggregate outcomes to the primary team providing care; however, we acknowledge that in an ICU setting, such an approach may be suboptimal as patient care is more often a multidisciplinary effort. Fourth, we were unable to capture outcomes following hospital discharge; certain outcomes including mortality and functional status are known to vary significantly following discharge. For example, patients who survive hospitalizations after the initial ICU admission report higher mortality rates in the 6 months following discharge.(47) To this regard, we were unable to discern the location of hospital discharge and rates of readmission, which may additionally confound our results. Several authors have observed an increasing trend to transfer patients to post-acute care facilities, acute-care hospitals, or other long-term, acute-care facilities, which may all spuriously reduce hospital mortality and LOS.(48,49) Fifth, we were unable to assess the accuracy of diagnostic codes and ICU prognostic tools used by the database as these may have changed with time.(50) Older prediction models have documented a decrease in accuracy and calibration when used with more contemporary datasets, as a result, it is possible that the APACHE III system, may have over predicted mortality outcomes.(50) Sixth, as with any ecologic or epidemiologic study, we cannot discern the presence of incongruous empirical correlations at the individual- or aggregate level. Nonetheless, despite these ecologic or individualistic fallacies, contemporary evidence mandates a comprehensive evaluation of multilevel models. Lastly, while we were able to adjust for center-specific random effects (between centers), we were unable to independently adjust for within center variation and other potential confounders like ICU structure (open vs. closed, medical, mixed, surgical, etc.), ICU staffing, teaching status of hospitals, use and adoption of disease-specific therapies, social determinant of health and adherence to standard of care guidelines.
Conclusions
In summary, the paradigm of surgical critical care is evolving in the United States. Our epidemiological assessment demonstrates that the population of surgical patients requiring critical care services is changing over time. We identify critical trends in ICU mortality, ICU length of stay, and demonstrate that functional status is deteriorating at an increased rate among surgical patients. Our results provide valuable insights into practice trends nationwide, help establish specialty-specific ICU benchmarks, and may have implications in healthcare systems planning, including resource and personnel-allocation, education, and surgical training.
Supplementary Material
Acknowledgments
We would like to thank Cerner Corporation and Laura Freeseman-Freeman for providing us with the APACHE Outcomes data for research.
Disclosures and Conflicts of Interest
This research was supported by the National Institutes of Health’s National Center for Advancing Translational Sciences, grant UL1TR002494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health’s National Center for Advancing Translational Sciences. We have no conflicts of interests to disclose.
Footnotes
Disclosures and Conflicts of Interest
Victor Vakayil, MBBS, MS - None
Nicholas E. Ingraham, MD - None
Alexandria J. Robbins, MD - None
Rebecca Freese, MS - None
Elise F. Northrop, BA - None
Kathryn Pendleton, MD - None
Melissa Brunsvold, MD - None
Anthony Charles, MD, MPH – None
Jeffrey G. Chipman, MD - None
Christopher J. Tignanelli, MD – None
Contributor Information
Victor Vakayil, Department of Surgery, University of Minnesota Medical School, Minneapolis, MN.; School of Public Health, University of Minnesota, Minneapolis MN..
Nicholas E. Ingraham, Department of Medicine, University of Minnesota Medical School, Minneapolis, MN..
Alexandria J. Robbins, Department of Surgery, University of Minnesota Medical School, Minneapolis, MN..
Rebecca Freese, Biostatistical Design and Analysis Center, Clinical and Translational Science Institute, University of Minnesota, Minneapolis, MN..
Elise F. Northrop, Biostatistical Design and Analysis Center, Clinical and Translational Science Institute, University of Minnesota, Minneapolis, MN..
Melissa E. Brunsvold, Department of Surgery, University of Minnesota Medical School, Minneapolis, MN..
Kathryn M. Pendleton, Department of Medicine, University of Minnesota Medical School, Minneapolis, MN..
Anthony Charles, Department of Surgery, University of North Carolina School of Medicine, Chapel Hill, NC.; School of Public Health, University of North Carolina School of Medicine, Chapel Hill, NC..
Jeffrey G. Chipman, Department of Surgery, University of Minnesota Medical School, Minneapolis, MN..
Christopher J. Tignanelli, Department of Surgery, University of Minnesota Medical School, Minneapolis, MN.; Department of Surgery, North Memorial Health Hospital, Robbinsdale, MN; Institute of Health Informatics, University of Minnesota, Minneapolis, MN..
Bibliography
- 1.Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985-2000: an analysis of bed numbers, use, and costs. Crit Care Med. 2004. June;32(6):1254–9. [DOI] [PubMed] [Google Scholar]
- 2.Halpern NA, Pastores SM, Thaler HT, Greenstein RJ. Changes in critical care beds and occupancy in the United States 1985-2000: Differences attributable to hospital size. Crit Care Med. 2006. August;34(8):2105–12. [DOI] [PubMed] [Google Scholar]
- 3.Halpern NA, Pastores SM. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010. January;38(1):65–71. [DOI] [PubMed] [Google Scholar]
- 4.Wallace DJ, Angus DC, Seymour CW, Barnato AE, Kahn JM. Critical care bed growth in the United States. A comparison of regional and national trends. Am J Respir Crit Care Med. 2015. February 15;191(4):410–6. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25522054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wallace DJ, Seymour CW, Kahn JM. Hospital-Level Changes in Adult ICU Bed Supply in the United States. Crit Care Med. 2017. January;45(1):e67–76. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27661861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adhikari NKJ, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults Lancet (London, England: ). 2010. October;376(9749):1339–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wunsch H, Harrison DA, Rowan K. Health services research in critical care using administrative data. J Crit Care. 2005. September;20(3):264–9. [DOI] [PubMed] [Google Scholar]
- 8.Hines AL, Heslin KC, Jiang HJ, Coffey R. Trends in Observed Adult Inpatient Mortality for High-Volume Conditions, 2002-2012 HCUP Statistical Brief# 194. Rockville, MD: Agency Healthc Res Qual; 2015; [PubMed] [Google Scholar]
- 9.Weiss AJ, Elixhauser A, Andrews RM. Characteristics of operating room procedures in US hospitals, 2011: statistical brief# 170 Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency Healthc Res Qual; 2006; [PubMed] [Google Scholar]
- 10.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011. June;364(22):2128–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003. April;348(16):1546–54. [DOI] [PubMed] [Google Scholar]
- 12.Moran JL, Bristow P, Solomon PJ, George C, Hart GK. Mortality and length-of-stay outcomes, 1993-2003, in the binational Australian and New Zealand intensive care adult patient database. Crit Care Med. 2008. January;36(1):46–61. [DOI] [PubMed] [Google Scholar]
- 13.Hutchings A, Durand MA, Grieve R, Harrison D, Rowan K, Green J, Cairns J, Black N. Evaluation of modernisation of adult critical care services in England: time series and cost effectiveness analysis. BMJ. 2009. November;339:b4353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garland A, Olafson K, Ramsey CD, Yogendran M, Fransoo R. Epidemiology of critically ill patients in intensive care units: a population-based observational study. Crit Care. 2013;17(5):R212 Available from: 10.1186/cc13026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zimmerman JE, Kramer AA, Knaus WA. Changes in hospital mortality for United States intensive care unit admissions from 1988 to 2012. Crit Care. 2013;17(2):R81 Available from: 10.1186/cc12695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Apache Outcomes [Internet]. [cited 2019 Aug 1]. Available from: https://apacheoutcomes.cernerworks.com/criticaloutcomes-home/
- 17.Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med. 2006. May;34(5):1297–310. [DOI] [PubMed] [Google Scholar]
- 18.Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991. December;100(6):1619–36. [DOI] [PubMed] [Google Scholar]
- 19.Wallace DJ, Angus DC, Barnato AE, Kramer AA, Kahn JM. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012/05/21. 2012. May 31;366(22):2093–101. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22612639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD. Hospital Volume and the Outcomes of Mechanical Ventilation. N Engl J Med. 2006. July 6;355(1):41–50. Available from: 10.1056/NEJMsa053993 [DOI] [PubMed] [Google Scholar]
- 21.Damiano AM, Bergner M, Draper EA, Knaus WA, Wagner DP. Reliability of a measure of severity of illness: acute physiology of chronic health evaluation--II. J Clin Epidemiol. 1992. February;45(2):93–101. [DOI] [PubMed] [Google Scholar]
- 22.Sirio CA, Shepardson LB, Rotondi AJ, Cooper GS, Angus DC, Harper DL, Rosenthal GE. Community-wide assessment of intensive care outcomes using a physiologically based prognostic measure: implications for critical care delivery from Cleveland Health Quality Choice. Chest. 1999. March;115(3):793–801. [DOI] [PubMed] [Google Scholar]
- 23.Zimmerman JE, Wagner DP, Draper EA, Wright L, Alzola C, Knaus WA. Evaluation of acute physiology and chronic health evaluation III predictions of hospital mortality in an independent database. Crit Care Med. 1998. August;26(8):1317–26. [DOI] [PubMed] [Google Scholar]
- 24.Zimmerman JE, Kramer AA, McNair DS, Malila FM, Shaffer VL. Intensive care unit length of stay: Benchmarking based on Acute Physiology and Chronic Health Evaluation (APACHE) IV. Crit Care Med. 2006. October;34(10):2517–29. [DOI] [PubMed] [Google Scholar]
- 25.United States Census -2010. . Available from: https://www.census.gov/programs-surveys/decennial-census/decade.2010.html
- 26.Ward NS, Chong DH. Critical Care Beds and Resource Utilization: Current Trends and Controversies. Semin Respir Crit Care Med. 2015. December;36(6):914–20. [DOI] [PubMed] [Google Scholar]
- 27.Halpern NA, Pastores SM. Critical Care Medicine Beds, Use, Occupancy, and Costs in the United States: A Methodological Review. Crit Care Med. 2015. November;43(11):2452–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26308432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halpern NA, Goldman DA, Tan KS, Pastores SM. Trends in Critical Care Beds and Use Among Population Groups and Medicare and Medicaid Beneficiaries in the United States: 2000-2010. Crit Care Med . 2016. August;44(8):1490–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27136721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lilly CM, Swami S, Liu X, Riker RR, Badawi O. Five-Year Trends of Critical Care Practice and Outcomes. Chest. 2017. October;152(4):723–35. [DOI] [PubMed] [Google Scholar]
- 30.Cancer Stat Facts: Oral Cavity and Pharynx Cancer . [cited 2019 Dec 8]. Available from: https://seer.cancer.gov/statfacts/html/oralcav.html
- 31.Soltani AM, Best MJ, Francis CS, Allan BJ, Askari M, Panthaki ZJ. Trends in the incidence and treatment of necrotizing soft tissue infections: an analysis of the National Hospital Discharge Survey. J Burn Care Res. 2014;35(5):449–54. [DOI] [PubMed] [Google Scholar]
- 32.Cancer Stat Facts: Esophageal Cancer [Internet]. [cited 2019 Dec 8]. Available from: https://seer.cancer.gov/statfacts/html/esoph.html
- 33.Cancer Stat Facts: Lung and Bronchus Cancer [Internet]. [cited 2019 Dec 8]. Available from: https://seer.cancer.gov/statfacts/html/lungb.html
- 34.Garland A, Olafson K, Ramsey CD, Yogendran M, Fransoo R. A population-based observational study of intensive care unit-related outcomes. With emphasis on post-hospital outcomes. Ann Am Thorac Soc. 2015. February;12(2):202–8. [DOI] [PubMed] [Google Scholar]
- 35.Qureshi AI, Suri MFK, Nasar A, Kirmani JF, Divani AA, He W, Hopkins LN. Trends in hospitalization and mortality for subarachnoid hemorrhage and unruptured aneurysms in the United States. Neurosurgery. 2005. July;57(1):1–8. [DOI] [PubMed] [Google Scholar]
- 36.Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR, Li Y. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991-2008. JAMA. 2011. April;305(15):1560–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Psoinos CM, Flahive JM, Shaw JJ, Li Y, Ng SC, Tseng JF, Santry HP. Contemporary trends in necrotizing soft-tissue infections in the United States. Surgery. 2013. June;153(6):819–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rosenberg AL, Zimmerman JE, Alzola C, Draper EA, Knaus WA. Intensive care unit length of stay: recent changes and future challenges. Crit Care Med. 2000. October;28(10):3465–73. [DOI] [PubMed] [Google Scholar]
- 39.Rogers WH, Draper D, Kahn KL, Keeler EB, Rubenstein L V, Kosecoff J, Brook RH. Quality of care before and after implementation of the DRG-based prospective payment system. A summary of effects. JAMA. 1990. October;264(15):1989–94. [PubMed] [Google Scholar]
- 40.van der Sluijs AF, van Slobbe-Bijlsma ER, Chick SE, Vroom MB, Dongelmans DA, Vlaar APJ. The impact of changes in intensive care organization on patient outcome and cost-effectiveness—a narrative review. J Intensive Care [Internet]. 2017;5(1):13 Available from: 10.1186/s40560-016-0207-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rydingsward JE, Horkan CM, Mogensen KM, Quraishi SA, Amrein K, Christopher KB. Functional Status in ICU Survivors and Out of Hospital Outcomes: A Cohort Study. Crit Care Med. 2016. May;44(5):869–79. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26929191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brummel NE, Balas MC, Morandi A, Ferrante LE, Gill TM, Ely EW. Understanding and reducing disability in older adults following critical illness. Crit Care Med. 2015. June;43(6):1265–75. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25756418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haas JS, Teixeira C, Cabral CR, Fleig AHD, Freitas APR, Treptow EC, Rizzotto MI, Machado AS, Balzano PC, Hetzel MP, et al. Factors influencing physical functional status in intensive care unit survivors two years after discharge. BMC Anesthesiol. 2013. June 18;13:11 Available from: https://www.ncbi.nlm.nih.gov/pubmed/23773812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nelson JE, Cox CE, Hope AA, Carson SS. Chronic critical illness. Am J Respir Crit Care Med. 2010/05/06. 2010. August 15;182(4):446–54. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20448093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Balas MC, Vasilevskis EE, Olsen KM, Schmid KK, Shostrom V, Cohen MZ, Peitz G, Gannon DE, Sisson J, Sullivan J, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014. May;42(5):1024–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.American Hospital Association- Hospital Statistics. 2015.
- 47.Wunsch H, Guerra C, Barnato AE, Angus DC, Li G, Linde-Zwirble WT. Three-Year Outcomes for Medicare Beneficiaries Who Survive Intensive Care. JAMA. 2010. March 3;303(9):849–56. Available from: 10.1001/jama.2010.216 [DOI] [PubMed] [Google Scholar]
- 48.Vasilevskis EE, Kuzniewicz MW, Dean ML, Clay T, Vittinghoff E, Rennie DJ, Dudley RA. Relationship between discharge practices and intensive care unit in-hospital mortality performance: evidence of a discharge bias. Med Care. 2009. July;47(7):803–12. [DOI] [PubMed] [Google Scholar]
- 49.Kahn JM, Kramer AA, Rubenfeld GD. Transferring critically ill patients out of hospital improves the standardized mortality ratio: a simulation study. Chest. 2007. January;131(1):68–75. [DOI] [PubMed] [Google Scholar]
- 50.Kramer AA. Predictive mortality models are not like fine wine. Crit Care. 2005/October/26 2005;9(6):636–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16356253 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.