Abstract
Background
To understand better the success of self-management interventions and to enable tailoring of such interventions at specific subgroups of patients, the nurse-led Activate intervention is developed targeting one component of self-management (physical activity) in a heterogeneous subgroup (patients at risk of cardiovascular disease) in Dutch primary care.
Aim
The aim of this study was to evaluate the effectiveness of the Activate intervention and identifying which patient-related characteristics modify the effect.
Methods
A two-armed cluster-randomised controlled trial was conducted comparing the intervention with care as usual. The intervention consisted of four nurse-led behaviour change consultations within a 3-month period. Data were collected at baseline, 3 months and 6 months. Primary outcome was the daily amount of moderate to vigorous physical activity at 6 months. Secondary outcomes included sedentary behaviour, self-efficacy for physical activity, patient activation for self-management and health status. Prespecified effect modifiers were age, body mass index, level of education, social support, depression, patient provider relationship and baseline physical activity.
Results
Thirty-one general practices (n = 195 patients) were included (intervention group n = 93; control group n = 102). No significant between-group difference was found for physical activity (mean difference 2.49 minutes; 95% confidence interval -2.1; 7.1; P = 0.28) and secondary outcomes. Patients with low perceived social support (P = 0.01) and patients with a low baseline activity level (P = 0.02) benefitted more from the intervention.
Conclusion
The Activate intervention did not improve patients’ physical activity and secondary outcomes in primary care patients at risk of cardiovascular disease. To understand the results, the intervention fidelity and active components for effective self-management require further investigation.
Trial registration: ClinicalTrials.gov NCT02725203.
Keywords: Behaviour change wheel, cluster-randomised controlled trial, nurse-led intervention, physical activity, primary care, self-management
Introduction
Over the past decades, interventions to support the self-management of chronically ill patients are widely accepted given their potential to produce health benefits and reduced healthcare utilisation.1 Self-management interventions aim to support patients in acquiring skills to participate actively and take responsibility for self-managing their chronic condition and adopting healthy behaviours.2 Self-management interventions are considered complex because these interventions contain multiple interacting components3 and multiple behaviours, such as increasing physical activity, healthy nutrition and managing symptoms and medication.2 Individual patient meta-analyses have attempted to unravel the effectiveness of self-management interventions.4,5 Although these interventions have been shown to be effective and which patients benefit is not fully understood due to a wide variety in content, intensity, duration and delivery of interventions.6 Untangling these interventions contributes to a better understanding of the success of self-management interventions and enables the tailoring of such interventions to specific subgroups of patients.6 Therefore, the design of studies evaluating complex self-management interventions should be guided by understanding active ingredients, intervention fidelity and contextual factors of interventions.3,6 As a result, we developed the nurse-led Activate intervention, in which we deliberately broke down complexity into a single self-management component, namely increasing physical activity, rather than focussing on the multibehavioural concept of self-management as a whole. As is well established, patients at risk of cardiovascular disease (CVD) benefit from being active for 30 minutes or more of moderate to vigorous activity on at least 5 days weekly.7,8 Furthermore, patients often need to change their behaviour to reach this threshold9 due to, for example, physical constraints, seasonal changes, other priorities.10 Targeting the intervention to physical activity in a heterogeneous subgroup of primary care patients enables the identification of which patients benefit from the intervention.
The Activate intervention is designed to be delivered by primary care nurses in The Netherlands as they routinely monitor treatment outcomes, promote self-management and support healthy behaviour in patients at risk of CVD.11 Self-management support often requires nurses to change their consultation style from a traditional style of providing advice, informing and educating patients about their condition to a more coaching style of supporting patients in changing their behaviour including the use of behaviour change techniques (BCTs).1,12 This implies that nurses need to change their behaviour as well. Furthermore, healthcare providers play a vital role in the effectiveness of interventions, which emphasises the need for adequate intervention delivery. Therefore, the Activate intervention is targeted at both patients’ behaviour (increasing physical activity) and at nurses’ behaviour (acquiring the necessary skills to provide structured behaviour change support). To enhance replication and our understanding of its effectiveness, the behaviour change wheel (BCW) as a theoretical framework guided the design of the Activate intervention and the design of a thorough process evaluation.12,13 In this study we specifically determined the effectiveness of the intervention in patients and identified which patient-related characteristics modify the effect.
Methods
Study design
We designed a two-armed, unblinded, cluster-randomised controlled trial in primary care to compare the nurse-led Activate intervention with care as usual over a 6-month period. After formalisation of their participation, general practices (as clusters) were randomly allocated to the intervention group or control group to avoid contamination. Randomisation was performed using web-based software with a 1:1 ratio. A detailed study protocol has been published elsewhere13 (ClinicalTrials.gov NCT02725203). An informed consent to postponed information procedure was used in which patients were kept unaware of the major study aim, randomisation and allocation of their general practice until the end of the follow-up period.14 Written informed consent was received from all participants. The trial was approved by the ethics committee of the University Medical Center Utrecht (NL54286.041.15) and was conducted in accordance with the Declaration of Helsinki.
Setting and participants
General practices throughout The Netherlands were invited to participate when they reallocated the disease management for patients at risk of CVD to a primary care nurse. Patients were recruited from March 2016 to January 2017, follow-up was completed by November 2017. The study population consisted of adult patients supported by a primary care nurse working in a general practice. Patients were eligible when aged 40–75 years, at risk of CVD,15 did less than 30 minutes of moderate to vigorous physical activity on 5 or more days a week7 and mastered the Dutch language. Exclusion criteria were the inability to give informed consent, mental or physical impairment, participation in a structured physical activity programme in the past 2 years. Primary care nurses invited eligible patients to participate in agreement with the general practitioner.
Intervention
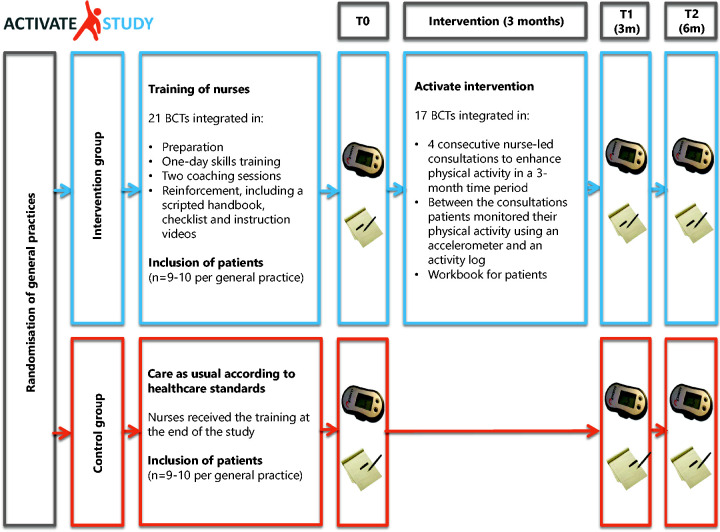
The Activate intervention was developed using the BCW to identify appropriate BCTs to enhance patients’ level of physical activity and understand nurses’ behaviour in delivering the Activate intervention.12 The development and content of the Activate intervention has been described in detail elsewhere.13 In short, as a result of the BCW 17 relevant BCTs were integrated into the Activate intervention and 21 relevant BCTs, such as goals setting, action planning, feedback on behaviour, self-monitoring and problem solving, were integrated into the training programme for nurses13 (Supplementary files 1 and 2).
The Activate intervention consisted of four prestructured, standardised nurse-led consultations to enhance patients’ level of physical activity. Consultations were offered at weeks 1, 3, 7 and 12 in patients’ own general practice, with a duration of 20–30 minutes. At the first consultation, patients received activity logs, forms for action planning, information about the trial, useful websites, apps and tips and tricks for physical activity. Nurses raised awareness about patients’ CVD risk profile and their physical activity level. Patients’ motivation to increase their physical activity was discussed and a personal outcome and activity goal was set. In the second consultation, nurses briefly repeated the information provided at the first consultation. In the second, third and fourth consultations, nurses reviewed and gave feedback on patients’ level of goal attainment and, when needed, adjusted the goals and action plans. In addition, in the third and fourth consultations, nurses discussed relapse prevention and the formation of new activity habits. During the intervention period, patients were asked to self-monitor their physical activity daily using an accelerometer (personal activity monitor; Pam AM300)16 and keeping an activity log.
The standardised comprehensive training programme for nurses consisted of a one-day skills training supplemented with two individual coaching sessions from a health psychologist, instructional videos showing how to apply the BCTs in the consultations, a handbook which provided a structure of the consultations and included example sentences and checklists (what to do when).13
Care as usual
Patients in the control group received care as usual according to the Dutch guidelines for CVD risk management.15
Data collection
Trial procedures and data collection are summarised in Figure 1. Patients’ characteristics and outcomes were collected at baseline, at 3 and 6 months of follow-up using questionnaires and a small, valid and reliable blinded tri-axial accelerometer (Pam AM300).16 Patients were asked to wear the accelerometer for 7 consecutive days for 12 hours daily. In addition, patients were asked to report their daily amount of minutes of other activities besides walking, such as cycling, swimming and strength training, on an activity log, as the accelerometer cannot validly measure these activities. At baseline, questionnaires and accelerometers were given by the nurse during patients’ regular visits. For follow-up measurements, questionnaires and accelerometers were sent by post. If patients did not respond, patients were contacted within 3 weeks to diminish delay in follow-up measurement.
Figure 1.
Study design of the Activate cluster-randomised controlled trial.
Outcomes
The primary outcome was change (0–6 months) in minutes of moderate to vigorous physical activity (≥3–6 metabolic equivalents (METS)), assessed by the Pam AM300.16 For a valid measurement, the Pam AM300 had to be worn for at least 4 week days and one weekend day for 8 hours.
Secondary outcomes included change (0–6 months) in sedentary behaviour based on Pam AM300 data,16 as measured as the percentage of the wear time of the Pam AM300 spent in the sedentary category ( < 1.8 METS). Another secondary outcome was self-efficacy for physical activity, as being an intermediate for changing physical activity levels, measured with the exercise self-efficacy scale.17–19 Patients’ confidence to adhere to an exercise routine in 18 situations was measured on a 0 (‘I cannot do that) to 100 (‘I am certain that I can do that’) scale, with higher scores reflecting higher levels of exercise self-efficacy.19 The majority of patients were retired, therefore item 2 (‘When I am feeling under pressure from work’) was deleted from the analysis. The 13-item patient activation measure (PAM-13) was used to assess patient activation for self-management, including knowledge, skills and confidence in managing their personal health or illness on a 5-point scale.20 Higher scores are positively associated with self-management behaviours.20 The EQ-5D-3L was used to measure health status on five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression.21 The EQ-VAS was used to assess patients’ self-rated health on a vertical analogue scale with end points of 0 (‘worst imaginable health state’) and 100 (‘best imaginable health state’).21 Outcome data were collected at baseline (T0), at 3 months of follow-up (T1) and at 6 months of follow-up (T2), except for health status, which was collected at T0 and T2.
Prespecified potential effect modifiers were baseline age, body mass index (BMI), level of education, social support using the multidimensional scale of perceived social support,22 depression using the hospital anxiety and depression scale,23 patient–provider relationship using the communication assessment tool,24 and baseline level of physical activity.
Statistical analysis
The sample size calculation was based on the detection of a mean difference of 20% moderate to vigorous physical activity (minutes/day) between both groups at 6 months of follow-up.13 A sample of 279 patients (139–140 patients per group with a cluster size of nine to 10 patients per general practice) over 30–31 general practices was required with 80% power, alpha of 0.05, assuming an intraclass correlation of 0.05 and drop-out rate of 15%.13
Patients’ baseline characteristics were descriptively analysed. Subsequently, an intention-to-treat analysis and a per protocol analysis were performed. Patients who received at least three out of four consultations were included in the per protocol analysis and patients who did not complete the T1 measurement were excluded from this analysis. Multilevel repeated linear mixed models with three levels (time, patients and general practices) were used to analyse the effectiveness of the intervention. Random intercepts for time and general practice were included in all models and an interaction term was added for time and study arm. A significant group-by-time interaction (P < 0.05) means a significant difference between groups on the outcome over time. All models were adjusted for the baseline value. EQ-5D-3L data were analysed using analysis of covariance (ANCOVA). Standardised coefficients and 95% confidence intervals were used to estimate effect sizes.
Missing outcome data were not imputed as linear mixed modelling handles missing outcome data. Two sensitivity analyses were performed: (a) outliers and (b) patients’ self-reported additional activities as covariate to the Pam AM300 data.
Effect modification was evaluated using the generalised estimating equation (GEE), including random intercepts. Effect modification is considered significant if the interaction between the outcome and a prespecified effect modifier is significant (P < 0.05).
Analyses and reporting followed CONSORT guidelines (Supplementary file 3). Analyses were performed using IBM SPSS statistics for Windows version 21.0 software (IBM, Armonk, NY, USA).
Results
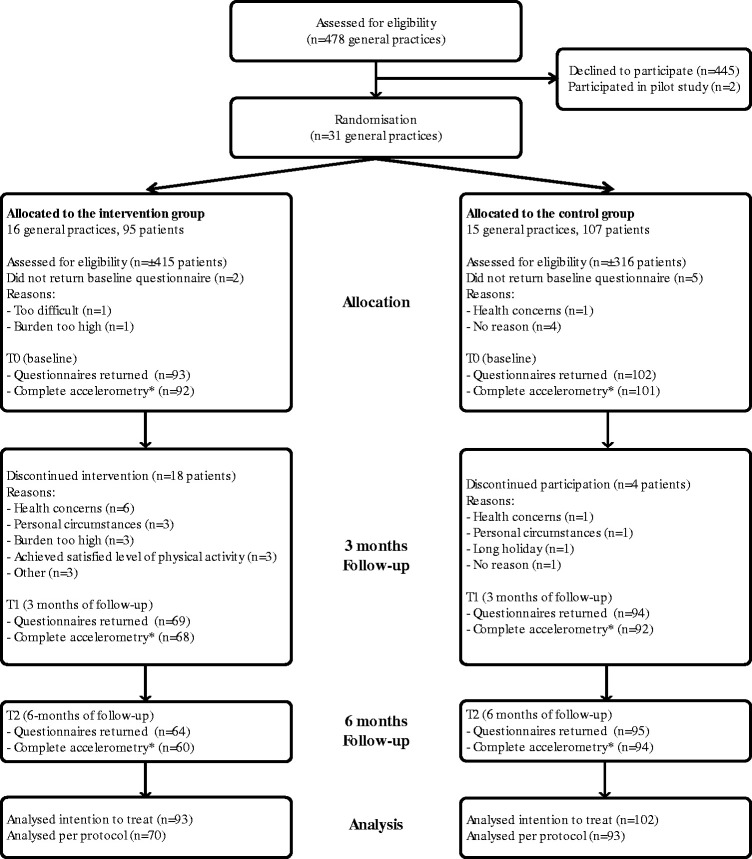
We invited 478 general practices until 31 agreed to participate (6.5%). Participating general practices were randomly allocated to the intervention group (n = 16) or control group (n = 15) (Figure 1). A total of 20 nurses participated in the intervention group and 16 nurses participated in the control group, including none to 12 patients (median 7.0; interquartile range (IQR) 7.0). Of the potential eligible patients (n = 731), 202 patients (27.6%) met the criteria to participate in this randomised controlled trial and after being fully informed gave their informed consent, 195 patients (26.7%) completed baseline questionnaires (intervention group n = 93; control group n = 102). In total, 73 patients (78.5%) attended all four consultations. At baseline, most patient characteristics were comparable between both groups; however, the intervention group had more women, had a higher BMI and had a slightly higher metabolic risk profile (Table 1). On average, patients were 62 years old and nearly half the patients had 30 or more minutes physical activity in the moderate to vigorous category on at least 5 days weekly (Table 1). Patients in the intervention group were slightly more active (Table 1).
Table 1.
Baseline characteristics of participants of the Activate trial.
| Control (n = 102) | Intervention (n = 93) | |
|---|---|---|
| Female, n (%) | 35 (34.3) | 41 (44.1) |
| Age in years, mean ± SD | 63.4 ± 8.3 | 61.9 ± 9.1 |
| Employed, n (%) | 33 (32.4) | 34 (36.6) |
| Living with others, n (%) | 87 (85.3) | 76 (81.7) |
| Level of education, n (%) | ||
| Primary education or below | 6 (5.9) | 3 (3.3) |
| Secondary education | 69 (68.3) | 67 (72.8) |
| Higher education | 26 (25.7) | 22 (23.9) |
| Smoking, n (%) | 11 (10.8) | 14 (15.1) |
| Body mass index, mean ± SD | 29.7 ± 4.8 | 32.7 ± 5.4 |
| <25, n (%) | 15 (14.7) | 3 (3.2) |
| 25–29.99, n (%) | 47 (46.1) | 30 (32.3) |
| ≥30, n (%) | 40 (39.2) | 60 (64.5) |
| Cardiovascular risk factors, n (%) | ||
| Hypertension only | 23 (22.5) | 13 (14.0) |
| Hypercholesterolemia only | 7 (6.9) | 5 (5.4) |
| DM2 only | 4 (3.9) | 3 (3.2) |
| Hypertension and hypercholesterolemia | 20 (19.6) | 25 (26.9) |
| Hypertension and DM2 | 9 (8.8) | 8 (8.6) |
| Hypertension, hypercholesterolemia and DM2 | 25 (24.5) | 32 (34.4) |
| Hypercholesterolemia and DM2 | 11 (10.8) | 4 (4.3) |
| Risk unknown | 3 (2.9) | 3 (3.2) |
| Health literacy (HLS-EU-Q), mean ± SD | 35.2 ± 6.9 | 33.9 ± 7.9 |
| Social support (MSPSS), mean ± SD | 65.5 ± 14.8 | 63.8 ± 13.8 |
| Depression (HADS), mean ± SD | 3.9 ± 3.3 | 5.5 ± 3.6 |
| Patient-provider relationship (CAT) | 4.1 ± 0.8 | 4.1 ± 0.7 |
| Meet Dutch physical activity guideline,a n (%) | 43 (43.0) | 52 (55.9) |
CAT: communication assessment tool; DM2: diabetes mellitus type 2; HADS: hospital anxiety and depression scale; HLS-EU-Q: European health literacy survey questionnaire; MSPSS: multidimensional scale of perceived social support.
aDutch physical activity guideline consists of at least 30 minutes of moderate to vigorous activity on at least 5 days weekly, measured with the accelerometer.
Primary outcome (intention-to-treat)
After 6 months, the level of physical activity did not significantly differ in both groups; see Table 2. However, the level of physical activity in the intervention group was higher (15.3%) after 6 months. At 6 months, 20 patients (33.3%) in the intervention group gained the clinically relevant 20% increase of their physical activity from baseline, compared with 22 patients (23.7%) in the control group. The intraclass correlation coefficient was 0.12.
Table 2.
Treatment effect for the primary and secondary outcome measures (intention-to-treat).
| Outcome measure |
Control group (n = 102) |
Intervention group (n = 93) |
Treatment effect (6 months) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Mean ± SD (linear mixed models) |
Unadjusted |
Adjusted* |
||||||||
| Baseline | 3 months | 6 months | Baseline | 3 months | 6 months | MD (95% CI) | P value | MD (95% CI) | P value | |
| Physical activitya | 38.9 ± 22.6 | 39.8 ± 25.9 | 39.9 ± 26.1 | 37.5 ± 21.1 | 43.3 ± 20.7 | 44.2 ± 24.4 | 2.92 (–6.2; 12.1) | 0.52 | 2.49 (–2.1; 7.1) | 0.28 |
| Physical activityb | 50.7 ± 33.4 | 52.3 ± 35.4 | 65.4 ± 48.8 | 49.4 ± 29.6 | 56.8 ± 29.7 | 69.4 ± 46.8 | 3.57 (–8.4; 15.5) | 0.55 | 2.41 (–4.3; 9.1) | 0.48 |
| Daily sedentary timec | 82.6 ± 5.7 | 82.5 ± 5.8 | 82.9 ± 5.9 | 83.3 ± 5.5 | 83.0 ± 5.9 | 83.3 ± 5.3 | 0.54 (–1.5; 2.6) | 0.60 | 0.31(–0.6; 1.9) | 0.50 |
| Exercise Self-efficacy Scale | 51.8 ± 17.7 | 57.7 ± 16.8 | 59.0 ± 16.7 | 49.4 ± 17.1 | 57.0 ± 17.3 | 58.8 ± 16.0 | –0.82 (–5.8; 4.2) | 0.75 | –0.79 (–4.6; 3.0) | 0.68 |
| PAM-13 | 59.2 ± 12.2 | 60.1 ± 14.0 | 61.6 ± 11.9 | 57.2 ± 12.2 | 59.9 ± 12.7 | 59.7 ± 14.0 | –1.59 (–5.4; 2.2) | 0.41 | 0.03 (–2.9; 3.0) | 0.99 |
|
Mean ± SD (ANCOVA) |
|
|
Standardised coefficients (95% CI) |
P value |
||||||
| EQ-5D-3L | 0.8 ± 0.2 | NA | 0.8 ± 0.2 | 0.8 ± 0.2 | NA | 0.8 ± 0.2 | 0.02 (0.0; 0.05) | 0.17 | ||
| EQ VAS score | 73.6 ± 14.1 | NA | 75.2 ± 14.6 | 67.3 ± 14.7 | NA | 70.0 ± 12.4 | 0.16 (–3.2; 3.5) | 0.92 | ||
CI: confidence interval; MD: mean difference; NA: not applicable; PAM-13: patient activation measure short form; VAS: visual analogue scale.
aDaily minutes of moderate to vigorous physical activity.
bObjective daily minutes of moderate to vigorous physical activity measured with the accelerometer added with self-reported cycling, swimming, strength training.
cPercentage of the wear time spent in the sedentary category (<1.8 METS).
*Adjusted for baseline measurement.
Secondary outcomes
The intention-to-treat analyses showed no statistical differences at 6 months with respect to sedentary behaviour, self-efficacy for physical activity, patient activation for self-management and health status (Table 2). In both groups, patients’ self-efficacy increased during the intervention period and stabilised at 6 months. Patients in the intervention group were slightly less activated compared with patients in the control group. Patients in the intervention group graded their health status lower compared with patients in the control group, although patients’ visual analogue scale score increased in both groups.
Data from 163 patients (Figure 2) were included in the per protocol analyses. The per protocol analyses confirmed the results of the intention-to-treat analyses (Table 3).
Figure 2.
CONSORT flowchart of general practices and participants assigned to the intervention and control group.
*Data available for at least 4 week days and one weekend day for 8 hours.
Table 3.
Treatment effect for the primary and secondary outcome measures (per protocol).
| Outcome measure |
Control group (n = 93) |
Intervention group (n = 70) |
Treatment effect (6 months) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Mean ± SD (linear mixed models) |
Unadjusted |
Adjusted* |
||||||||
| Baseline | 3 months | 6 months | Baseline | 3 months | 6 months | MD (95% CI) | P value | MD (95% CI) | P value | |
| Physical activitya | 38.7 ± 22.8 | 39.8 ± 25.9 | 39.1 ± 25.4 | 40.8 ± 21.3 | 43.3 ± 20.7 | 44.7 ± 24.3 | 3.98 (–5.0; 12.9) | 0.52 | 2.55 (–2.0; 7.2) | 0.26 |
| Physical activityb | 51.6 ± 33.3 | 52.3 ± 35.4 | 65.4 ± 49.2 | 54.1 ± 30.1 | 56.8 ± 29.7 | 70.1 ± 46.8 | 4.00 (–8.0; 16.0) | 0.51 | 2.43 (–4.3; 9.1) | 0.48 |
| Daily sedentary timec | 82.6 ± 5.8 | 82.5 ± 5.8 | 82.9 ± 5.9 | 82.7 ± 5.5 | 83.0 ± 5.9 | 83.3 ± 5.3 | 0.51 (–1.6; 2.6) | 0.63 | 0.35 (–0.5; 1.2) | 0.44 |
| Exercise self–efficacy Scale | 50.7 ± 17.7 | 57.7 ± 16.8 | 58.5 ± 16.5 | 51.5 ± 17.6 | 57.0 ± 17.3 | 59.0 ± 16.1 | –0.25 (–5.2; 4.7) | 0.92 | –0.71 (–4.6; 3.2) | 0.72 |
| PAM-13 | 59.1 ± 11.7 | 60.6 ± 14.0 | 61.5 ± 12.0 | 57.9 ± 12.4 | 59.9 ± 12.7 | 60.1 ± 13.9 | –1.25 (–5.1; 2.6) | 0.52 | –0.07 (–2.9; 3.1) | 0.96 |
|
Mean ± SD (ANCOVA) |
|
|
Standardised coefficients (95% CI) |
P value |
||||||
| EQ-5D-3L | 0.8 ± 0.2 | NA | 0.8 ± 0.2 | 0.8 ± 0.2 | NA | 0.8 ± 0.2 | 0.01 (0.0; 0.04) | 0.46 | ||
| EQ VAS score | 73.9 ± 14.5 | NA | 75.4 ± 14.7 | 67.7 ± 15.3 | NA | 70.0 ± 12.4 | 0.24 (–3.2; 3.6) | 0.89 | ||
CI: confidence interval; MD: mean difference; NA: not applicable; PAM-13: patient activation measure short form; VAS: visual analogue scale.
aDaily minutes of moderate to vigorous physical activity.
bObjective daily minutes of moderate to vigorous physical activity measured with the accelerometer added with self-reported cycling, swimming, strength training.
cPercentage of the wear time spent in the sedentary category (<1.8 METS).
*Adjusted for baseline measurement.
Excluding outliers from the analyses did not affect the results presented (data not shown). Adding patients’ self-reported additional activities to their objectively measured physical activity did not influence the findings (Tables 2 and 3). While adding these activities increased patients’ physical activity level in both groups, no statistical differences were observed between groups.
Effect modification
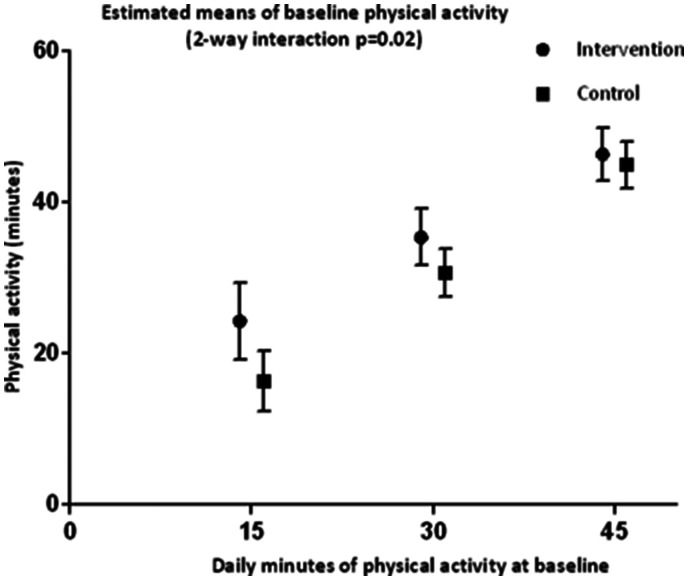
At 6 months, patients with a low acuity of perceived social support were more likely to benefit more from the intervention than patients with a moderate or a high acuity of perceived social support (P = 0.01; Figure 3). Patients with a low baseline physical activity level were more likely to have a larger increase in their activity level at 6 months compared with patients who were more active at baseline (P = 0.02; Figure 4). Other potential modifiers examined did not show an interaction with patients’ level of physical activity at 6 months (Supplementary file 4).
Figure 3.
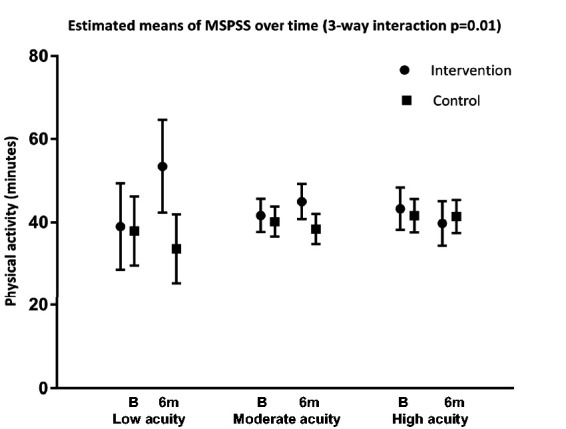
Estimated means of the multidimensional scale of perceived social support.
Figure 4.
Estimated means of baseline physical activity.
Discussion
In a cluster-randomised controlled trial, a nurse-led behaviour change intervention (Activate) in primary care patients at risk of CVD did not show a significant improvement in patients’ physical activity compared with usual care at 6 months of follow-up. No between-group differences were seen on secondary outcomes, including sedentary behaviour, self-efficacy for physical activity, patient activation for self-management and health status. Predefined subgroup analyses showed that patients with a low acuity of perceived social support and patients with a low baseline activity level were more likely to benefit more from the intervention.
The insignificant increase in patients’ physical activity is in contrast with other studies also using BCTs such as goal setting, action planning, self-monitoring, feedback and social support to increase physical activity by nurse-led consultations.25,26 Our results might be explained by several reasons. First, patients with a high baseline activity level might easily have reached a ceiling level. While an eligibility criterion of patients was insufficient physical activity, patients’ objectively measured mean physical activity level was remarkably high and the majority exceeded the Dutch guideline for physical activity. This was also seen in another Dutch trial.25 These high baseline levels may indicate invalid physical activity screening or a Hawthorne effect.27 Patients in the intervention group were used to wearing the accelerometer, which could have decreased patients’ socially desirable behaviour during the follow-up measurements compared with the control group. Second, the vast majority of baseline measurements occurred during summer in which physical activity levels are higher.28 A longer follow-up might have diminished the influence of seasonal changes. Third, nurses in the control group may have upgraded their usual care, resulting in diminished effectiveness of the intervention. Fourth, participating general practices might have been more prone to behaviour change support compared with general practices not participating. Fifth, treatment effects may have been more pronounced when nurses included more patients to enable them to master their skills in providing the intervention.29 Subsequently, insight into the intervention fidelity and the quality of delivery is crucial to further understanding of the effects30 and needs to be investigated.
We were not able to detect reductions in sedentary time, which is contrary to another study.31 Patients’ self-efficacy of being physically active increased in both groups. The results of the qualitative evaluation among patients, which we conducted parallel to the current study, revealed that patients increasingly felt more confident in goal attainment and highly valued included BCTs targeting self-efficacy.10 However, we could not explain patients’ increase in self-efficacy in the control group, rather than relating this increase to wearing the accelerometer during the follow-up measurements.
Patients’ activation for self-management might not have been affected by the intervention as their activation scores indicated that patients were already taking an active role in building self-management skills and were considered to strive for behaviour change.20
Patients’ health status did not change at 6 months, which is in line with the trial of van der Weegen et al.25
The subgroup analysis showed that patients with a low acuity of perceived social support tend to favour more effect from the intervention, which could be partially explained by patients’ inability to elicit social support themselves.32 Patients with an inactive baseline activity level tend to benefit more from the intervention, which is consistent with another study.26 No interaction effect was shown for age, BMI, education level, patient–nurses’ relationship and depression, which is also seen in other studies.26,33 However, these results urged caution due to the lack of power of the analyses leaving the complex question unanswered of which patients benefit from self-management interventions. Subsequently, the baseline characteristics of patients might shed light on further hypothesising this question. Relatively active patients with an average age of 60 years, moderate educational level and overweight or obese were well represented, assuming the results are substantially representative of patients having these characteristics. However, patients with low health literacy levels and ethnic minorities were underrepresented as they were more likely not to participate due to language barriers and difficulties in understanding the intervention.
The results of qualitative studies conducted among patients and nurses alongside the Activate trial revealed pivotal insights in the effectiveness.10,29 Patients emphasised that, irrespective of their objective changes in physical activity, participating increased their awareness of health benefits of physical activity and their physical activity level.10 Both studies identified the contribution of individual factors to nurses’ and patients’ perceived success of the intervention,10,29 which often result in tiny changes that produce marginal gains accumulating in meaningful successes.34
Strengths and limitations
The use of the BCW as a theoretical framework enhances reproducibility and our understanding of the active ingredients of the intervention to unravel further the black box of the effectiveness of self-management interventions. In the design, several methodological challenges were addressed to improve the methodological rigor and generalisability, such as cluster randomisation at the level of the general practice to prevent contamination; a sample from general practices throughout The Netherlands; the modified informed consent procedure to postponed information to reduce attrition bias and contamination in the control group as patients could not be blinded for the intervention; patients’ own nurse rather than researchers or exercise specialists delivered the intervention; objective physical activity measurements using a blank screen accelerometer; self-reported measurements using validated questionnaires; and a thorough conducted process evaluation parallel to the trial. Some limitations should be considered. Despite our expectations and efforts, the number of patients according to the power calculation proved unattainable, which forces a careful interpretation of the results, particularly the effect modification analyses. Despite the commitment of general practices and nurses to recruit sufficient patients, the recruitment rate of patients was 27.6%, which is lower than another patient-based trial25 but showed a higher patient recruitment rate than population-based physical activity trials.26 Including insufficient patients might have diluted the effect of the intervention. The low recruitment rate might have resulted in a higher intraclass correlation than anticipated (0.12 instead of 0.05). The low recruitment rate of patients was due to reporting sufficient physical activity, other priorities, and/or already being involved in research. The low recruitment rate of general practices was due to busy daily practices, sick leave, other priorities, and already being involved in other research. These low recruitment rates raise issues about generalisability.
To reduce selective inclusion, broad selection criteria were chosen. However, nurses indicated that patients, who they experienced as unmotivated to change their behaviour during prior consultations, were less likely to be included, suggesting that selective inclusion might have occurred. The dropout rate was somewhat higher than anticipated (19.4% instead of 15%). However, it is unlikely that drop-outs biased our results as patients’ baseline characteristics were comparable and the multilevel analysis flexibly dealt with drop-out.
Finally, the accelerometer itself had some limitations, such as the inability to measure cycling, swimming and strength training properly, patients frequently lost the accelerometer and technical issues occurred, which caused loss of data.
In conclusion, the nurse-led Activate intervention did not increase the level of physical activity and other patient-related outcomes in patients at risk of CVD in primary care. To understand better the absence of a significant effect, a thorough process evaluation, concerning patients’ and nurses’ perceptions towards the intervention was performed. The fidelity of delivery of the intervention and active components for effective self-management require further investigation.
Implications for practice
A nurse-led behaviour change intervention did not increase patients’ level of physical activity.
Patients with a low social support were prone to benefit from the intervention.
Patients with a low baseline physical activity were likely to increase their activity level.
Supplemental Material
Supplemental material, sj-pdf-1-cnu-10.1177_1474515120919547 for Effectiveness of the nurse-led Activate intervention in patients at risk of cardiovascular disease in primary care: a cluster-randomised controlled trial by Heleen Westland, Marieke J Schuurmans, Irene D Bos-Touwen, Marjolein A de Bruin-van Leersum, Evelyn M Monninkhof, Carin D Schröder, Daphne A de Vette and Jaap CA Trappenburg: on behalf of the STAAB consortium* in European Journal of Cardiovascular Nursing
Supplemental material, sj-pdf-2-cnu-10.1177_1474515120919547 for Effectiveness of the nurse-led Activate intervention in patients at risk of cardiovascular disease in primary care: a cluster-randomised controlled trial by Heleen Westland, Marieke J Schuurmans, Irene D Bos-Touwen, Marjolein A de Bruin-van Leersum, Evelyn M Monninkhof, Carin D Schröder, Daphne A de Vette and Jaap CA Trappenburg: on behalf of the STAAB consortium* in European Journal of Cardiovascular Nursing
Supplemental material, sj-pdf-3-cnu-10.1177_1474515120919547 for Effectiveness of the nurse-led Activate intervention in patients at risk of cardiovascular disease in primary care: a cluster-randomised controlled trial by Heleen Westland, Marieke J Schuurmans, Irene D Bos-Touwen, Marjolein A de Bruin-van Leersum, Evelyn M Monninkhof, Carin D Schröder, Daphne A de Vette and Jaap CA Trappenburg: on behalf of the STAAB consortium* in European Journal of Cardiovascular Nursing
Supplemental material, sj-pdf-4-cnu-10.1177_1474515120919547 for Effectiveness of the nurse-led Activate intervention in patients at risk of cardiovascular disease in primary care: a cluster-randomised controlled trial by Heleen Westland, Marieke J Schuurmans, Irene D Bos-Touwen, Marjolein A de Bruin-van Leersum, Evelyn M Monninkhof, Carin D Schröder, Daphne A de Vette and Jaap CA Trappenburg: on behalf of the STAAB consortium* in European Journal of Cardiovascular Nursing
Acknowledgements
The authors gratefully thank the general practices, nurses and patients who participated in this study. They also thank Annika Haanstra for her contribution to the data collection and Peter Zuithoff for the statistical support.
Author contribution
All authors declare that they made a substantial contribution to the concept or design of the work; or acquisition, analysis or interpretation of data, drafted the article or revised it critically for important intellectual content, and approved the version to be published. Each author participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Dutch Ministry of Health, Welfare and Sports, ZonMw grant (grant number 520001002).
Supplemental material
Supplemental material for this article is available online.
References
- 1.Bodenheimer T, Lorig K, Holman H, et al. Patient self-management of chronic disease in primary care. JAMA 2002; 288: 2469–2475. [DOI] [PubMed] [Google Scholar]
- 2.Barlow J, Wright C, Sheasby J, et al. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns 2002; 48: 177–187. [DOI] [PubMed] [Google Scholar]
- 3.Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud 2013; 50: 587–592. [DOI] [PubMed] [Google Scholar]
- 4.Jonkman N, Westland H, Groenwold RHH, et al. Do self-management interventions work in patients with heart failure? An individual patient data meta-analysis. Circulation 2016; 133: 1189–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jonkman NH, Westland H, Trappenburg JC, et al. Characteristics of effective self-management interventions in patients with COPD: individual patient data meta-analysis. Eur Respir J 2016; 48: 55–68. [DOI] [PubMed] [Google Scholar]
- 6.Jonkman N, Groenwold RHH, Trappenburg JCA, et al. Complex self-management interventions in chronic disease unravelled: a review of lessons learnt from an individual patient data meta-analysis. J Clin Epidemiol 2017; 83: 48–56. [DOI] [PubMed] [Google Scholar]
- 7.Kemper HGC, Ooijendijk WTM, Stiggelbout M. Consensus over de Nederlandse Norm voor Gezond Bewegen. Tijdschr Soc Gezondheidsz 2000; 78: 180–183. [Google Scholar]
- 8.Williams PT. Physical fitness and activity as separate heart disease risk factors: a meta-analysis. Med Sci Sports Exerc 2001; 33: 754–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burke LE, Dunbar-Jacob JM, Hill MN. Compliance with cardiovascular disease prevention strategies: a review of the research. Ann Behav Med 1997; 19: 239–263. [DOI] [PubMed] [Google Scholar]
- 10.Westland H, Sluiter J, Te Dorsthorst S, et al. Patients’ experiences with a behaviour change intervention to enhance physical activity in primary care: a mixed methods study. PLoS One 2019; 14: e0212169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baan CA, Hutten JBF, Rijken PM. Afstemming in de zorg: een achtergrondstudie naar de zorg voor mensen met een chronische aandoening. [Coordination of care: a study into the care for people with a chronic condition]. Bilthoven, The Netherlands: RIVM, 2003. [Google Scholar]
- 12.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011; 6:42,5908–6–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Westland H, Bos Touwen I, Trappenburg JCA, et al. Unravelling effectiveness of a nurse-led behaviour change intervention to enhance physical activity in patients at risk for cardiovascular disease in primary care: study protocol for a cluster randomised controlled trial. Trials 2017; 18: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boter H, van Delden JJ, de Haan RJ, et al. Modified informed consent procedure: consent to postponed information. BMJ 2003; 327: 284–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nederlands Huisartsen Genootschap. Multidisciplinaire richtlijn Cardiovasculair risicomanagement. Houten, The Netherlands: Bohn Stafleu van Loghum, 2011. [Google Scholar]
- 16.Slootmaker SM, Chin A Paw MJM, Schuit AJ, et al. Concurrent validity of the PAM accelerometer relative to the MTI Actigraph using oxygen consumption as a reference. Scand J Med Sci Sports 2009; 19: 36–43. [DOI] [PubMed] [Google Scholar]
- 17.Everett B, Salamonson Y, Davidson PM. Bandura’s exercise self-efficacy scale: validation in an Australian cardiac rehabilitation setting. Int J Nurs Stud 2009; 46: 824–829. [DOI] [PubMed] [Google Scholar]
- 18.Shin Y, Jang H, Pender NJ. Psychometric evaluation of the exercise self-efficacy scale among Korean adults with chronic diseases. Res Nurs Health 2001; 24: 68–76. [DOI] [PubMed] [Google Scholar]
- 19.van der Heijden MMP, Pouwer F, Pop VJM. Psychometric properties of the Exercise Self-efficacy Scale in Dutch Primary care patients with type 2 diabetes mellitus. Int J Behav Med 2014; 21: 394–401. [DOI] [PubMed] [Google Scholar]
- 20.Hibbard J, Mahoney E, Stockard J, et al. Development and testing of a short form of the patient activation measure. Health Serv Res 2005; 40: 1918–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kind P. The EuroQol instrument: an index of health-related quality of life. In: Spilker B (ed.) Quality of life and pharmacoeconomics in clinical trials, 2nd edn. Lippincott-Raven, 1996.
- 22.Pedersen SS, Spinder H, Erdman RA, et al. Poor perceived social support in implantable cardioverter defibrillator (ICD) patients and their partners: cross-validation of the multidimensional scale of perceived social support. Psychosomatics 2009; 50: 461–467. [DOI] [PubMed] [Google Scholar]
- 23.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 24.Makoul G, Krupat E, Chang C. Measuring patient views of physician communication skills: development and testing of the Communication Assessment Tool. Patient Educ Couns 2007; 67: 333–342. [DOI] [PubMed] [Google Scholar]
- 25.van der Weegen S, Verwey R, Spreeuwenberg M, et al. It’s LiFe! Mobile and web-based monitoring and feedback tool embedded in primary care increases physical activity: a cluster randomized controlled trial. J Med Internet Res 2015; 17: e184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris T, Kerry S, Limb E, et al. Effect of a primary care walking intervention with and without nurse support on physical activity levels in 45- to 75-year-olds: the Pedometer and Consultation Evaluation (PACE-UP) cluster randomised clinical trial. PLoS Med 2017; 14: e1002210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pedišic Ž, Bauman A. Accelerometer-based measures in physical activity surveillance: current practices and issues. Br J Sports Med 2015; 49: 219–223. [DOI] [PubMed] [Google Scholar]
- 28.Kimura T, Kobayashi H, Nakayama E, et al. Seasonality in physical activity and walking of healthy older adults. J Physiol Anthropol 2015; 34: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Westland H, Koop Y, Schröder C, et al. Nurses’ perceptions towards the delivery and feasibility of a behaviour change intervention to enhance physical activity in patients at risk for cardiovascular disease in primary care: a qualitative study. BMC Fam Pract 2018; 19: 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bellg A, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 2004; 23: 443–451. [DOI] [PubMed] [Google Scholar]
- 31.Mutrie N, Doolin O, Fitzsimons C, et al. Increasing older adults’ walking through primary care: results of a pilot randomized controlled trial. Fam Pract 2012; 29: 633–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.French D, Olander E, Chisholm A, et al. Which behaviour change techniques are most effective at increasing older adults’ self-efficacy and physical activity behaviour? A systematic review. Ann Behav Med 2014; 48: 225–234. [DOI] [PubMed] [Google Scholar]
- 33.Fitzsimons C, Baker G, Gray S, et al. Does physical activity counselling enhance the effects of a pedometer-based intervention over the long-term: 12-month findings from the Walking for Wellbeing in the west study. BMC Public Health 2012; 12: 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richards D. Complex interventions and the amalgamation of marginal gains: a way forward for understanding and researching essential nursing care? Int J Nurs Stud 2015; 52: 1143–1145. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cnu-10.1177_1474515120919547 for Effectiveness of the nurse-led Activate intervention in patients at risk of cardiovascular disease in primary care: a cluster-randomised controlled trial by Heleen Westland, Marieke J Schuurmans, Irene D Bos-Touwen, Marjolein A de Bruin-van Leersum, Evelyn M Monninkhof, Carin D Schröder, Daphne A de Vette and Jaap CA Trappenburg: on behalf of the STAAB consortium* in European Journal of Cardiovascular Nursing
Supplemental material, sj-pdf-2-cnu-10.1177_1474515120919547 for Effectiveness of the nurse-led Activate intervention in patients at risk of cardiovascular disease in primary care: a cluster-randomised controlled trial by Heleen Westland, Marieke J Schuurmans, Irene D Bos-Touwen, Marjolein A de Bruin-van Leersum, Evelyn M Monninkhof, Carin D Schröder, Daphne A de Vette and Jaap CA Trappenburg: on behalf of the STAAB consortium* in European Journal of Cardiovascular Nursing
Supplemental material, sj-pdf-3-cnu-10.1177_1474515120919547 for Effectiveness of the nurse-led Activate intervention in patients at risk of cardiovascular disease in primary care: a cluster-randomised controlled trial by Heleen Westland, Marieke J Schuurmans, Irene D Bos-Touwen, Marjolein A de Bruin-van Leersum, Evelyn M Monninkhof, Carin D Schröder, Daphne A de Vette and Jaap CA Trappenburg: on behalf of the STAAB consortium* in European Journal of Cardiovascular Nursing
Supplemental material, sj-pdf-4-cnu-10.1177_1474515120919547 for Effectiveness of the nurse-led Activate intervention in patients at risk of cardiovascular disease in primary care: a cluster-randomised controlled trial by Heleen Westland, Marieke J Schuurmans, Irene D Bos-Touwen, Marjolein A de Bruin-van Leersum, Evelyn M Monninkhof, Carin D Schröder, Daphne A de Vette and Jaap CA Trappenburg: on behalf of the STAAB consortium* in European Journal of Cardiovascular Nursing