Abstract
Iron is an essential trace element in the body. However, in heart failure (HF), iron is only recognized as the cause of anemia. Actually, iron itself affects myocardial exercise tolerance and cardiac function via mitochondrial function. Therefore, it is necessary to clarify the pathological significance of iron in acute HF, irrespective of concomitant anemia. We investigated the impact of serum iron level at discharge on the prognosis of 615 patients emergently admitted with acute decompensated HF (ADHF). Patients were divided into two groups according to the median level of serum iron (62 µg/dL). The endpoint was the composite outcome, which included all-cause mortality and readmission for HF. During the mean follow-up period of 32.1 months, there were 333 events. Kaplan–Meier analysis showed that the incidence of the composite outcome was significantly higher in the Low iron group (P < 0.0001). In the multivariate analysis adjusted with factors including hemoglobin and ferritin levels, low serum iron was an independent predictor for the composite outcome (hazard ratio, 1.500; 95% confidence interval, 1.128–1.976; P = 0.0044). Low serum iron was an independent predictor of poor prognosis in ADHF, irrespective of hemoglobin or ferritin level, providing a new concept that iron may play a role in the pathophysiology of ADHF via non-hematopoietic roles.
Subject terms: Biomarkers, Cardiology, Risk factors
Introduction
Heart failure (HF) is a major public health issue worldwide. Recent guidelines on acute and chronic HF have classified HF into three groups according to left ventricular ejection fraction (LVEF): HF with reduced EF (HFrEF; LVEF < 40%), mid-range EF (HFmrEF; 40% ≤ LVEF < 50%), and preserved EF (HFpEF; 50% ≤ LVEF)1, 2. Despite optimal conventional therapy, patients with HF still show less improvement in symptoms as well as high readmission and mortality rates2–4. One reason for this may be the occurrence of comorbidities. In particular, it is well known that anemia is a strong factor associated with prognosis in HF, and iron is one of the major causes of anemia. Interestingly, iron is not only a factor of anemia, but also plays a crucial role in cardiac and skeletal muscle metabolism via mitochondrial function and affects myocardial exercise tolerance and cardiac function. However, little is known about the relationship between HF and iron itself beyond the cause of anemia. Therefore, it is necessary to clarify the pathological significance of iron in acute HF, irrespective of concomitant anemia.
Iron is an essential trace element in the body and is crucial for oxygen transport, delivery, and utilization. The regulation of systemic iron balance is also important for the homeostasis of myocytes and skeletal muscle cells, which depend on iron for their function and structural integrity5, 6. Interestingly, both iron deficiency (ID) and iron overload adversely affect cardiovascular health. ID is present in approximately 50% of patients with HF, regardless of whether it is HFrEF or HFpEF; ID is one of the representative comorbidities of HF7–9.
Previous studies have investigated the association between ferritin and chronic HF and demonstrated a significant association between ID, diagnosed based on ferritin levels, and poor outcomes7, 12–14. Ferritin is most frequently used as an indicator of ID, but some patients are diagnosed with functional ID despite high ferritin levels. Regarding this fact, the action of hepcidin has a great influence. Because hepcidin plays an important role in the regulation of iron metabolism, including the absorption of iron and liberation of iron stores within the body. Interestingly, the activity of hepcidin is enhanced by inflammation and previous studies have demonstrated that acute HF is associated with systemic inflammation10, 11. In short, the increasing hepcidin activity by inflammation in HF may lead to the development of functional ID despite high ferritin levels. Therefore, to better understand the pathophysiology of iron metabolism in HF, not only ferritin but also iron itself should be studied in more detail and the association between iron levels and clinical outcomes should be explore. In this study, we examined the impact of serum iron levels in patients with acute decompensated HF (ADHF).
Results
Baseline characteristics
As shown in Table 1, the mean age of the 615 patients was 74.3 ± 12.0 (mean ± SD) years, and the proportion of men was 56.9%. Median level of serum iron and ferritin were 62.0 (44.0–88.0) µg/dL and 107 (51–203) µg/L (medians (25th and 75th percentile)), respectively. To investigate the impact of serum iron level on the prognosis of ADHF, we divided patients into two groups according to the median serum iron level at discharge (62 mg/dL). Table 1 shows baseline clinical characteristics of patients in the Low and High iron groups. Compared to patients in the High iron group, those in the Low iron group were significantly older. There were no significant differences in the cause of HF or proportion of comorbidities between the groups, except for diabetes mellitus. The rate of ID based on ferritin level, which was defined as ferritin level < 100 ug/L or 100–299 ug/L if TSAT is < 20%, was significant higher in the Low iron group than in the High iron group. Moreover, vital signs at discharge and LVEF were similar, but the left ventricular end-diastolic diameter was shorter in the Low iron group. Regarding laboratory findings, the hemoglobin level and eGFR were lower and C-reactive protein (CRP) and BNP levels were higher in the Low iron group. TIBC, TSAT, ferritin and transferrin levels were lower in the Low iron group. The proportion of patients treated with angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, β-blockers, or diuretics was similar in both groups at discharge, except for mineralocorticoid receptor blockers. With regard to the rate of the rate of administration of iron tablets, it was significantly higher in the Low iron group than in the High iron group.
Table 1.
Baseline characteristics of HF patients in the low vs. high iron group.
| Characteristic | Total (n = 615) | Low iron (n = 307) | High iron (n = 308) | P value |
|---|---|---|---|---|
| Demographic | ||||
| Age, years | 74.3 ± 12.0 | 76.3 ± 10.8 | 72.2 ± 12.8 | < 0.0001 |
| Male, % | 56.9 | 53.4 | 60.4 | 0.0808 |
| BMI, kg/m2 | 23.3 ± 4.4 | 23.0 ± 4.1 | 23.7 ± 4.6 | 0.1110 |
| Cause of HF, % | ||||
| Ischemic | 33.5 | 34.9 | 32.1 | 0.4764 |
| Valvular | 17.4 | 18.9 | 15.9 | 0.3289 |
| Dilated cardiomyopathy | 15.5 | 13.0 | 17.9 | 0.0970 |
| Hypertensive | 7.0 | 6.5 | 7.5 | 0.6430 |
| Medical history, % | ||||
| Hypertension | 74.3 | 76.9 | 71.8 | 0.1460 |
| Diabetes mellitus | 41.3 | 47.2 | 35.4 | 0.0028 |
| Dyslipidemia | 43.1 | 45.9 | 40.3 | 0.1557 |
| Smoking | 19.7 | 16.9 | 22.4 | 0.0879 |
| ID based on ferritin level | 57.4 | 40.5 | 74.6 | < 0.0001 |
| NYHA class on admission, % | ||||
| III or IV | 91.5 | 91.2 | 91.9 | 0.7625 |
| Vital sign at discharge | ||||
| Systolic blood pressure, mmHg | 111.0 ± 17.8 | 112.0 ± 18.6 | 110.1 ± 16.9 | 0.3052 |
| Heart rate, beats/minute | 71.4 ± 11.9 | 71.7 ± 11.7 | 71.1 ± 12.0 | 0.5946 |
| Echocardiographic parameters | ||||
| LVEF, % | 46.7 ± 16.0 | 47.6 ± 16.2 | 45.9 ± 15.7 | 0.1872 |
| HFpEF, % | 40.7 | 42.7 | 38.6 | 0.2986 |
| LVEDD, mm | 52.4 ± 9.3 | 51.3 ± 9.1 | 53.4 ± 9.4 | 0.0017 |
| Laboratory data at discharge | ||||
| C-reactive protein, mg/dL* | 0 .28 (0.10–0.90) | 0.50 (0.10–1.30) | 0.20 (0.10–0.50) | < 0.0001 |
| Hemoglobin, g/dL | 11.5 ± 2.1 | 10.8 ± 1.7 | 12.3 ± 2.2 | < 0.0001 |
| MCV, fl | 93.8 ± 6.7 | 92.6 ± 6.9 | 95.0 ± 6.2 | < 0.0001 |
| eGFR, mL/min/1.73m2 | 42.5 ± 22.2 | 37.2 ± 21.0 | 47.8 ± 22.1 | < 0.0001 |
| Sodium, mmol/L | 137.9 ± 4.0 | 138.0 ± 4.0 | 137.9 ± 4.0 | 0.7095 |
| Plasma BNP, pg/mL* | 272 (145–508) | 326 (182–626) | 225 (124–425) | < 0.0001 |
| Serum iron, µg/dL* | 62.0 (44.0–88.0) | 44.0 (33.0–53.0) | 88.0 (71.0–110.0) | < 0.0001 |
| TIBC, µg/dL | 287.9 ± 66.2 | 275.5 ± 71.8 | 300.3 ± 57.6 | < 0.0001 |
| TSAT, % | 24.8 ± 14.7 | 16.7 ± 12.5 | 32.8 ± 12.1 | < 0.0001 |
| Ferritin, µg/L | 107 (51–203) | 86 (40–175) | 128 (63–224) | < 0.0001 |
| Transferrin, mg/dL | 224.8 ± 52.2 | 217.5 ± 54.7 | 231.4 ± 49.0 | 0.0005 |
| Medication at discharge, % | ||||
| ACE inhibitors or ARBs | 87.3 | 85.3 | 89.3 | 0.1410 |
| MR blockers | 43.6 | 39.1 | 48.1 | 0.0249 |
| β-blockers | 74.5 | 71.7 | 77.3 | 0.1103 |
| Diuretics | 78.5 | 79.5 | 77.6 | 0.5698 |
| Iron tablets | 15.0 | 9.7 | 20.2 | 0.0003 |
ID based on ferritin level is defined as ferritin level < 100 ug/L or 100–299 ug/L if TSAT is < 20%.
HF heart failure; BMI body mass index; ID iron deficiency; NYHA New York Heart Association; LV left ventricular; EF ejection fraction; HFpEF heart failure with preserved ejection fraction; EDD end-diastolic diameter; MCV mean corpuscular volume; eGFR estimated glomerular filtration rate; BNP B-type natriuretic peptide; TIBC total iron-binding capacity; TSAT transferrin saturation; ACE angiotensin-converting enzyme; ARB angiotensin receptor blocker; MR mineralocorticoid receptor.
*Data are shown as percentages, means ± standard deviation, or medians (25th and 75th percentile).
Prognosis and outcome
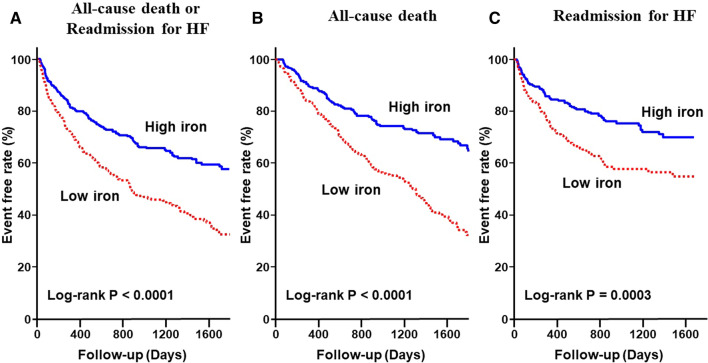
During the mean follow-up period of 32.1 months, there were 333 composite outcomes; among these, 153 were all-cause mortality and 180 were readmission for HF. As shown in the Kaplan–Meier survival curves, the Low iron group had a much higher rate of composite events (log-rank P < 0.0001) (Fig. 1A). Similarly, in each of all-cause mortality and readmission for HF, the event rate was higher in the Low iron group (log-rank P < 0.0001 and P = 0.0003, respectively) (Fig. 1B,C). In addition, the composite event rates were higher in the Low iron group than the High iron group at any of 90-days, 6-months and 1-year. (Supplemental Fig. S1).
Figure 1.
Kaplan–Meier event-free survival curves for (A) all-cause mortality or readmission for HF, (B) all-cause mortality, and (C) readmission for HF in the Low iron group (red line) compared with the High iron group (blue line). HF, heart failure.
Table 2 shows unadjusted and adjusted HRs for composite outcomes in the two groups. Compared to the High iron group, the unadjusted HR for composite outcome was significantly higher in the Low iron group (HR 1.956; 95% CI 1.570–2.444; P < 0.0001). Even after adjustment for covariates (age, sex, LVEF, Hb, eGFR, BNP, TSAT, and ferritin level) in the multivariable Cox proportional hazards models, this finding remained significant (HR 1.500; 95% CI 1.128–1.976; P = 0.0044). Moreover, in a further analysis of factors related to anemia and iron balance, including hemoglobin, MCV, ferritin, transferrin level, and TSAT, the low iron group was significantly associated with composite outcomes (HR 1.487; 95% CI 1.074–2.059; P = 0.0169) (Table 2 Model 5). In this study, a total of 74 patients had a history of blood transfusion within 3 months before enrollment and during hospitalization. The analysis was performed excluding these patients, but the results were similar. (Supplemental Table S1) Moreover, the Low iron group was associated with composite outcomes with or without ID based on ferritin level defined as ferritin level < 100 ug/L or 100–299 ug/L if TSAT is < 20%. (Supplemental Table S2).
Table 2.
Hazard ratios and 95% CI for composite events.
| All-cause death or readmission for HF | ||
|---|---|---|
| HR (95% CI) | P value | |
| Model 1 | ||
| Low iron (serum Fe < 62 µg/dL) | 1.956 (1.570–2.444) | < 0.0001 |
| Model 2 | ||
| Low iron (serum Fe < 62 µg/dL) | 1.739(1.392–2.179) | < 0.0001 |
| Age, year | 1.038 (1.027–1.049) | < 0.0001 |
| Male | 1.408 (1.128–1.757) | 0.0023 |
| Model 3 | ||
| Low iron (serum Fe < 62 µg/dL) | 1.454 (1.149–1.847) | 0.0020 |
| Age, year | 1.033 (1.022–1.044) | < 0.0001 |
| Male | 1.378 (1.100–1.726) | 0.0053 |
| Hemoglobin, g/dL | 0.856 (0.800–0.916) | < 0.0001 |
| eGFR, mL/min/1.73 m2 | 1.005 (0.999–1.010) | 0.1004 |
| Plasma BNP, 100 pg/mL | 1.028 (1.006–1.048) | 0.0082 |
| LVEF, % | 0.997 (0.989–1.004) | 0.3747 |
| Model 4 | ||
| Low iron (serum Fe < 62 µg/dL) | 1.500 (1.128–1.976) | 0.0044 |
| Age, year | 1.034 (1.023–1.047) | < 0.0001 |
| Male | 1.399 (1.108–1.766) | 0.0047 |
| Hemoglobin, g/dL | 0.866 (0.807–0.928) | < 0.0001 |
| eGFR, mL/min/1.73 m2 | 1.005 (0.999–1.011) | 0.0930 |
| Plasma BNP, 100 pg/Ll | 1.026 (1.004–1.047) | 0.0158 |
| LVEF, % | 0.996 (0.988–1.004) | 0.3244 |
| Ferritin, µg/L | 1.000 (1.000–1.001) | 0.5761 |
| TSAT, % | 1.001 (0.990–1.009) | 0.8392 |
| Model 5 | ||
| Low iron (serum Fe < 62 µg/dL) | 1.487 (1.074–2.059) | 0.0169 |
| Hemoglobin, g/dL | 0.856 (0.804–0.913) | < 0.0001 |
| MCV, fl | 1.038 (1.020–1.057) | < 0.0001 |
| Ferritin, µg/L | 1.000 (0.999–1.000) | 0.4769 |
| TSAT, % | 0.998 (0.986–1.011) | 0.7758 |
| Transferrin, mg/dL | 1.001 (0.998–1.004) | 0.5442 |
HF heart failure; eGFR estimated glomerular filtration rate; BNP B-type natriuretic peptide; LVEF, left ventricular ejection fraction; TSAT transferrin saturation; MCV mean corpuscular volume; HR hazard ratio; CI confidence interval.
Based on ROC curve analysis, the serum iron cutoff value was 64 µg/dL in this study, with sensitivity of 66.1% and specificity of 58.2%. The area under the ROC curve was 0.6368. (Supplemental Fig. S2) The serum iron ≤ 64 ug/dl was an independent prognostic factor in multivariate analysis using Hemoglobin, BNP, and BUN that are well-known prognostic markers of mortality and readmission in HF. (Supplemental Table S3).
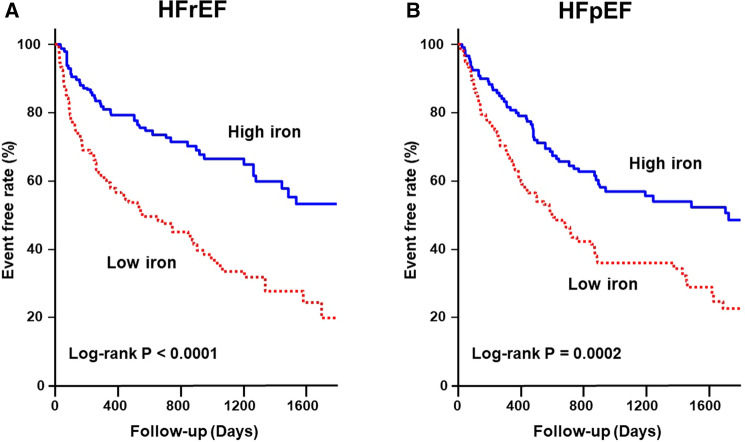
HFrEF and HFpEF
Figure 2 shows the Kaplan–Meier survival curves for composite events in HFrEF and HFpEF. The Low iron group had a much higher rate of composite events in both patients with HFrEF and HFpEF (log-rank P < 0.0001 and P = 0.0002, respectively).
Figure 2.
Kaplan–Meier event-free survival curves for all-cause mortality or readmission for HF in patients with HFrEF (A) and HFpEF (B) in the Low iron group (red line) compared to the High iron group (blue line). HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction.
Table 3 shows unadjusted and adjusted HRs for composite outcomes in HFrEF and HFpEF. In both HFrEF and HFpEF, the unadjusted HR for composite outcome was significantly higher in the Low iron group (HR 2.404; 95% CI 1.661–3.515; P < 0.0001 and HR 1.886; 95% CI 1.349–2.657; P = 0.0002, respectively). In multivariable Cox proportional hazards models, the Low iron group was independently related to composite outcomes in both HFrEF and HFpEF (HR 1.564; 95% CI 1.018–2.402; P = 0.0411 and HR 1.769; 95% CI 1.094–2.860; P = 0.0201, respectively). Moreover, in an analysis of factors related to anemia and iron balance, the Low iron group tended to be associated with composite outcomes in both HFrEF and HFpEF.
Table 3.
Hazard ratios and 95% CI for composite events in each of HFrEF and HFpEF.
| All-cause death or readmission for HF | ||||
|---|---|---|---|---|
| HFrEF | HFpEF | |||
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Model 1 | ||||
| Low iron (serum Fe < 62 µg/dL) | 2.404 (1.661–3.515) | < 0.0001 | 1.886 (1.349–2.657) | 0.0002 |
| Model 2 | ||||
| Low iron (serum Fe < 62 µg/dL) | 2.082 (1.425–3.072) | 0.0002 | 1.741 (1.243–2.456) | 0.0014 |
| Age, year | 1.031 (1.012–1.051) | 0.0014 | 1.037 (1.020–1.055) | < 0.0001 |
| Male | 1.637 (1.072–2.499) | 0.0226 | 1.349 (0.967–1.881) | 0.0776 |
| Model 3 | ||||
| Low iron (serum Fe < 62 µg/dL) | 1.504 (1.006–2.269) | 0.0467 | 1.615 (1.121–2.347) | 0.0099 |
| Age, year | 1.019 (0.999–1.040) | 0.0597 | 1.034 (1.017–1.051) | < 0.0001 |
| Male | 1.687 (1.090–2.611) | 0.0148 | 1.358 (0.972–1.896) | 0.0733 |
| Hemoglobin, g/dL | 0.798 (0.713–0.891) | < 0.0001 | 0.888 (0.791–0.994) | 0.0391 |
| eGFR, mL/min/1.73 m2 | 0.999 (0.987–1.010) | 0.8059 | 1.007 (1.000–1.015) | 0.0617 |
| Plasma BNP, 100 pg/mL | 1.022 (0.987–1.055) | 0.2122 | 1.022 (0.974–1.061) | 0.3450 |
| LVEF, % | 0.976 (0.949–1.005) | 0.0972 | 1.007 (0.983–1.032) | 0.5614 |
| Model 4 | ||||
| Low iron (serum Fe < 62 µg/dL) | 1.564 (1.018–2.402) | 0.0411 | 1.769 (1.094–2.860) | 0.0201 |
| Age, year | 1.019 (0.999–1.041) | 0.0639 | 1.036 (1.018–1.055) | < 0.0001 |
| Male | 1.725 (1.100–2.706) | 0.0139 | 1.343 (0.952–1.894) | 0.0930 |
| Hemoglobin, g/dL | 0.796 (0.709–0.891) | < 0.0001 | 0.898 (0.798–1.011) | 0.0747 |
| eGFR, mL/min/1.73 m2 | 0.999 (0.988–1.010) | 0.8755 | 1.008 (0.999–1.016) | 0.0662 |
| Plasma BNP, 100 pg/mL | 1.019 (0.982–1.054) | 0.3052 | 1.023 (0.980–1.067) | 0.3029 |
| LVEF, % | 0.975 (0.948–1.004) | 0.0906 | 1.006 (0.981–1.032) | 0.6293 |
| Ferritin, µg/L | 1.000 (0.999–1.001) | 0.8929 | 1.000 (0.999–1.001) | 0.8627 |
| TSAT, % | 1.003 (0.991–1.011) | 0.5676 | 1.007 (0.989–1.025) | 0.4461 |
| Model 5 | ||||
| Low iron (serum Fe < 62 µg/dL) | 1.638 (1.037–2.563) | 0.0311 | 1.726 (0.998–2.985) | 0.0508 |
| Hemoglobin, g/dL | 0.808 (0.725–0.900) | 0.0001 | 0.882 (0.777–1.001) | 0.0515 |
| MCV, fl | 1.060 (1.025–1.097) | 0.0008 | 1.020 (0.992–1.050) | 0.1674 |
| Ferritin, µg/L | 0.999 (0.998–1.001) | 0.4057 | 1.000 (0.999–1.001) | 0.8305 |
| TSAT, % | 1.002 (0.985–1.011) | 0.7454 | 1.002 (0.982–1.022) | 0.8496 |
| Transferrin, mg/dL | 0.997 (0.993–1.002) | 0.2227 | 1.005 (1.000–1.009) | 0.0327 |
HF heart failure; HFrEF heart failure with reduced ejection fraction; HFpEF heart failure with preserved ejection fraction; eGFR estimated glomerular filtration rate; BNP B-type natriuretic peptide; LVEF left ventricular ejection fraction; TSAT transferrin saturation; MCV mean corpuscular volume, HR hazard ratio; CI confidence interval.
Factors related to low iron levels
In the analysis according to odds ratio, age, diabetes mellitus, CRP, eGFR, and BNP were related to low iron levels. Multivariate analysis using these factors revealed that all factors were independently associated with low iron levels (Supplemental Table S4).
Discussion
The present study investigated the significance of serum iron levels in patients with ADHF and demonstrated that serum iron level is independently associated with poor prognosis in patients with ADHF. To the best of our knowledge, this is the first report demonstrating an association of serum iron level per se with the prognosis of patients with ADHF. Compared to previous studies that investigated the relationship between ID based on ferritin level and HF, this study has several new advantages. First, the target patients had ADHF, not chronic HF. Second, we studied serum iron levels instead of ferritin levels. Finally, a low iron level was associated with adverse outcomes in both HFrEF and HFpEF.
Clinical and prognostic significance of ID in patients with HF has previously been recognized1, 8, 15. ID is associated with reduced exercise capacity, 6-min walk test values, and peak oxygen consumption13, 16, as well as poor prognosis and quality of life in patients with chronic HF13, 14, 17. Generally, ID is defined as ferritin level < 100 ug/L or 100–299 ug/L if TSAT is < 20%15, 18, 19. However, in patients with ADHF, it may be difficult to apply the ID criteria based on this definition due to the impaired iron action20. One of the reasons for impaired iron action is the effect of hepcidin. Hepcidin acts as a major homeostatic regulator of iron metabolism by blocking ferroportin, which is the only known mammalian iron exporting protein21, 22. ADHF is associated with a systemic inflammatory response whose sustained level over time is not linked to the decrease in mechanical myocardial stress, suggesting the unique role of inflammation in acute HF pathophysiology10, 11. Consequently, in patients with ADHF, the increasing hepcidin activity due to inflammation reduces duodenal iron absorption and simultaneously reduces iron release from stores in the reticulo-endothelial cells and hepatocytes, thereby causing functional ID. Our finding that CRP was associated with low iron levels supports this theory. Therefore, despite the widely accepted and reported above definitions in chronic HF, using ferritin as an indicator of functional ID may be challenging in patients with ADHF. Given that serum iron acts on the tissue, it can be argued that this is a more physiologically relevant variable; herein, we found a correlation between poor prognosis and low iron level. Notably, low iron level was an independent predictor of adverse outcomes even in multivariate analysis including hemoglobin and MCV. This finding is consistent with that from previous reports, which showed that ID was associated with poor prognosis in chronic HF, irrespective of whether anemia is present7, 13, 14, 17. These findings may imply that the significance of iron is shifting from the cause of anemia toward the more direct effects of iron itself on non-hematopoietic tissues such as cardiac muscle and skeletal muscles23. The oxygen-transport properties of hemoglobin depend on the binding of oxygen to ferrous iron within heme. Within the mitochondrion, iron is an essential component of several subunits of the electron transport chain. Recently, it was reported that augmented skeletal muscle energetics might be an important mechanism via which iron repletion confers benefits in HF despite minimal hemoglobin changes24. Therefore, serum iron may have important roles unrelated to anemia.
There are multiple mechanisms in addition to the action on hepcidin whereby serum iron levels may decrease in patients with HF, including excitation of the sympathetic nervous system, reduction of iron absorption by intestinal wall edema, and adverse effects from prescribed drugs such as histamine-2 receptor antagonists and proton-pump inhibitors25. Anemia due to ID reduces the ability of hemoglobin to transport oxygen and causes hypoxemia. Therefore, from the viewpoint of cardio-renal-anaemia syndrome, iron administration may be useful, especially in HF with anemia. In this study, the serum iron cutoff value was 64 µg/dL based on ROC curve analysis. Therefore, it may be better to consider intravenous iron therapy for the serum iron ≤ 64 µg/dL. Of course, large-scale studies and intervention studies are needed to set an appropriate reference value. In Japan, the length of hospital stay for HF is often longer than in other countries. Therefore, in patients with HF who have a short hospital stay, it may be necessary to pay attention to low iron not only at the time of discharge but also after discharge.
Moreover, in this study, low iron level was a prognostic factor in patients with HFrEF and HFpEF. Regarding HFrEF, the effectiveness of intravenous iron administration for chronic HF has been previously reported12, 26, 27. Our results suggest that intravenous iron administration may be useful even in the acute phase of HFrEF. However, caution is required to prevent iron overload. Some studies have demonstrated that iron overload can increase the risk of adverse cardiovascular events, such as HF and cardiomyopathy28. Therefore, frequent administration of iron agents should be avoided; in each case, it is necessary to carefully confirm the indications for iron administration. On the other hand, our findings suggest that iron administration may be a new therapeutic target in HFpEF. As is generally known, no useful treatment has been demonstrated for HFpEF. Therefore, it is a landmark finding if the efficacy of iron administration is demonstrated. However, this needs to be examined further in large-scale studies.
Limitations
There are several limitations to this study. First, the sample size was moderate, and the study was conducted at a single center. Second, we did not collect hepcidin, ferroportin, or biomarkers for inflammation, such as calcitonin or red cell distribution width except for CRP. Therefore, we could not directly examine hepcidin activity in this study population. Third, we had no data on other factors that influence hepcidin. Fourth, among the eligible study population, many patients were excluded in this study due to in-hospital deaths or absence of serum iron measurement at discharge. Although there was no difference between the baseline of the entire study patients and the baseline of this study patients, this may be a potential bias in the results.
Conclusion
We demonstrated that low iron level was an independent poor prognostic factor in ADHF, irrespective of hemoglobin or ferritin level. In acute HF, it is important to focus not only on ferritin but also on iron itself. Although further large-scale studies are warranted to verify the present results, our findings highlight a novel potential for iron replacement as a therapeutic target to further reduce adverse events in patients with HFpEF.
Methods
Patient selection
The NARA-HF study is a prospective and dynamic cohort study29, 30. The NARA-HF 4 study recruited 1012 consecutive patients emergently admitted to the cardiology wards or the coronary care unit at our hospital for the first time due to ADHF between January 2011 and December 2018. The diagnosis of HF was based on the Framingham criteria31. Patients with acute myocardial infarction (AMI), acute myocarditis, and acute HF with acute pulmonary embolism were excluded. Furthermore, re-registration at the time of readmission will not be performed.
Of the 1012 patients, 615 underwent serum iron measurement at discharge. Patients were divided into low (the Low iron group, n = 307) and high (the High iron group, n = 308) serum iron groups based on the median serum iron level (62 µg/dL). Baseline data for each patient included age, sex, body mass index (BMI), cause of HF, medical history, vital signs, laboratory and echocardiographic data, and medications on admission and at discharge.
The study was approved by the Ethics Committee of Nara Medical University, and written informed consent was obtained from all patients in accordance with the Declaration of Helsinki’s Ethical Principles for Medical Research Involving Human Subjects.
Outcomes
The endpoint was set as the composite outcome, which included all-cause mortality and readmission for HF. Medical records were reviewed to determine vital status and the cause of death. When this information was unavailable in the medical record, we telephoned patients or their families. Information regarding cardiovascular events such as non-fatal AMI, stroke, and re-hospitalization due to recurrence of ADHF was also obtained. Furthermore, we reanalyzed these examinations in each case of HFrEF and HFpEF.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and compared using Student’s t-test. Categorical variables were summarized with frequency percentages and analyzed using a chi-square test. Cumulative event-free rates during follow-up were derived using the Kaplan–Meier method. Univariate and multivariable analyses of events were performed using Cox proportional hazards models. We implemented five models for the adjustment of covariates: model 1, unadjusted; model 2, adjusted for age and sex; model 3, adjusted for all factors in model 2 plus hemoglobin, estimated glomerular filtration rate (eGFR), brain natriuretic peptide (BNP), and LVEF; model 4, adjusted for all factors in model 3 plus ferritin level and transferrin saturation (TSAT); and model 5, adjusted for factors related to anemia and iron balance including hemoglobin, mean corpuscular volume (MCV), ferritin, transferrin level, and TSAT.
Results were reported as hazard ratios (HR), 95% confidence intervals (CI), and P-values. The HR for outcomes in the Low iron group was compared with that for outcomes in the High iron group, which served as the reference group. Variables with P-values < 0.05 were retained in the model. JMP version 14 for Windows (SAS Institute, Cary, NC, USA) was used for all statistical analyses.
Supplementary Information
Acknowledgements
The authors thank Y. Wada, Y. Kamada, and I Yoshida for their support in the data collection process.
Author contributions
T.U. and R.K. performed the statistical analysis; T.U., R.K., K.N., M.N., S.I., Y.N., T.N., Y.H., H.N., T.N., K.O., T.S., S.O., and M.W. acquired the data; T.U. and Y.S. conceived and designed the research; T.U. and Y.S. drafted the manuscript and made critical revisions of the manuscript for key intellectual content. All authors reviewed the manuscript and have approved the submitted version (and any substantially modified version that involves the author's contribution to the study). All authors have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. All authors have certified the author list and author contributions.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-82063-0.
References
- 1.Ponikowski P, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016;18:891–975. doi: 10.1002/ejhf.592. [DOI] [PubMed] [Google Scholar]
- 2.Yancy CW, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136:e137–e161. doi: 10.1161/CIR.0000000000000509. [DOI] [PubMed] [Google Scholar]
- 3.Ueda T, et al. Differences in blood pressure riser pattern in patients with acute heart failure with reduced mid-range and preserved ejection fraction. ESC Heart Fail. 2019;6:1057–1067. doi: 10.1002/ehf2.12500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakada Y, et al. Simple risk score to predict survival in acute decompensated heart failure-A2B score. Circ. J. 2019;83:1019–1024. doi: 10.1253/circj.CJ-18-1116. [DOI] [PubMed] [Google Scholar]
- 5.Melenovsky V, et al. Myocardial iron content and mitochondrial function in human heart failure: A direct tissue analysis. Eur. J. Heart Fail. 2017;19:522–530. doi: 10.1002/ejhf.640. [DOI] [PubMed] [Google Scholar]
- 6.Jankowska EA, Ponikowski P. Molecular changes in myocardium in the course of anemia or iron deficiency. Heart Fail. Clin. 2010;6:295–304. doi: 10.1016/j.hfc.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Klip IT, et al. Iron deficiency in chronic heart failure: An international pooled analysis. Am. Heart J. 2013;165(575–582):e3. doi: 10.1016/j.ahj.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 8.von Haehling S, Jankowska EA, van Veldhuisen DJ, Ponikowski P, Anker SD. Iron deficiency and cardiovascular disease. Nat. Rev. Cardiol. 2015;12:659–669. doi: 10.1038/nrcardio.2015.109. [DOI] [PubMed] [Google Scholar]
- 9.Martens P, et al. Impact of iron deficiency on exercise capacity and outcome in heart failure with reduced, mid-range and preserved ejection fraction. Acta Cardiol. 2018;73:115–123. doi: 10.1080/00015385.2017.1351239. [DOI] [PubMed] [Google Scholar]
- 10.Boulogne M, et al. Inflammation versus mechanical stretch biomarkers over time in acutely decompensated heart failure with reduced ejection fraction. Int. J. Cardiol. 2017;226:53–59. doi: 10.1016/j.ijcard.2016.10.038. [DOI] [PubMed] [Google Scholar]
- 11.Logeart D, et al. Current aspects of the spectrum of acute heart failure syndromes in a real-life setting: The OFICA study. Eur. J. Heart Fail. 2013;15:465–476. doi: 10.1093/eurjhf/hfs189. [DOI] [PubMed] [Google Scholar]
- 12.Anker SD, et al. Effects of ferric carboxymaltose on hospitalisations and mortality rates in iron-deficient heart failure patients: An individual patient data meta-analysis. Eur. J. Heart Fail. 2018;20:125–133. doi: 10.1002/ejhf.823. [DOI] [PubMed] [Google Scholar]
- 13.Okonko DO, Mandal AK, Missouris CG, Poole-Wilson PA. Disordered iron homeostasis in chronic heart failure: Prevalence, predictors, and relation to anemia, exercise capacity, and survival. J. Am. Coll. Cardiol. 2011;58:1241–1251. doi: 10.1016/j.jacc.2011.04.040. [DOI] [PubMed] [Google Scholar]
- 14.van Veldhuisen DJ, Anker SD, Ponikowski P, Macdougall IC. Anemia and iron deficiency in heart failure: Mechanisms and therapeutic approaches. Nat. Rev. Cardiol. 2011;8:485–493. doi: 10.1038/nrcardio.2011.77. [DOI] [PubMed] [Google Scholar]
- 15.Anand IS, Gupta P. Anemia and iron deficiency in heart failure: Current concepts and emerging therapies. Circulation. 2018;138:80–98. doi: 10.1161/CIRCULATIONAHA.118.030099. [DOI] [PubMed] [Google Scholar]
- 16.Ebner N, et al. The impact of iron deficiency and anaemia on exercise capacity and outcomes in patients with chronic heart failure. Results from the studies investigating co-morbidities aggravating heart failure. Int. J. Cardiol. 2016;205:6–12. doi: 10.1016/j.ijcard.2015.11.178. [DOI] [PubMed] [Google Scholar]
- 17.Comín-Colet J, et al. Iron deficiency is a key determinant of health-related quality of life in patients with chronic heart failure regardless of anaemia status. Eur. J. Heart Fail. 2013;15:1164–1172. doi: 10.1093/eurjhf/hft083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Aelst LNL, et al. Iron status and inflammatory biomarkers in patients with acutely decompensated heart failure: Early in-hospital phase and 30-day follow-up. Eur. J. Heart Fail. 2017;19:1075–1076. doi: 10.1002/ejhf.837. [DOI] [PubMed] [Google Scholar]
- 19.von Haehling S, Ebner N, Evertz R, Ponikowski P, Anker SD. Iron deficiency in heart failure: An overview. JACC Heart Fail. 2019;7:36–46. doi: 10.1016/j.jchf.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 20.Nanas JN, et al. Etiology of anemia in patients with advanced heart failure. J. Am. Coll. Cardiol. 2006;48:2485–2489. doi: 10.1016/j.jacc.2006.08.034. [DOI] [PubMed] [Google Scholar]
- 21.Ganz T. Cellular iron: Ferroportin is the only way out. Cell. Metab. 2005;1:155–157. doi: 10.1016/j.cmet.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 22.Lakhal-Littleton S, et al. Cardiac ferroportin regulates cellular iron homeostasis and is important for cardiac function. Proc. Natl. Acad. Sci. USA. 2015;112:3164–3169. doi: 10.1073/pnas.1422373112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van der Meer P, van der Wal HH, Melenovsky V. Mitochondrial function, skeletal muscle metabolism, and iron deficiency in heart failure. Circulation. 2019;139:2399–2402. doi: 10.1161/CIRCULATIONAHA.119.040134. [DOI] [PubMed] [Google Scholar]
- 24.Charles-Edwards G, et al. Effect of iron isomaltoside on skeletal muscle energetics in patients with chronic heart failure and iron deficiency. Circulation. 2019;139:2386–2398. doi: 10.1161/CIRCULATIONAHA.118.038516. [DOI] [PubMed] [Google Scholar]
- 25.Lam JR, Schneider JL, Quesenberry CP, Corley DA. Proton pump inhibitor and Histamine-2 receptor antagonist use and iron deficiency. Gastroenterology. 2017;152(821–829):e1. doi: 10.1053/j.gastro.2016.11.023. [DOI] [PubMed] [Google Scholar]
- 26.Anker SD, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N. Engl. J. Med. 2009;361:2436–2348. doi: 10.1056/NEJMoa0908355. [DOI] [PubMed] [Google Scholar]
- 27.Ponikowski P, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency. Eur. Heart J. 2015;36:657–668. doi: 10.1093/eurheartj/ehu385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murphy CJ, Oudit GY. Iron-overload cardiomyopathy: Pathophysiology, diagnosis, and treatment. J. Card. Fail. 2010;16:888–900. doi: 10.1016/j.cardfail.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 29.Ueda T, et al. Plasma renin activity is a strong and independent prognostic indicator in patients with acute decompensated heart failure treated with renin-angiotensin system inhibitors. Circ. J. 2015;79:1307–1314. doi: 10.1253/circj.CJ-14-1203. [DOI] [PubMed] [Google Scholar]
- 30.Ueda T, et al. Worsening of renal function during 1 year after hospital discharge is a strong and independent predictor of all-cause mortality in acute decompensated heart failure. J. Am. Heart. Assoc. 2014;3:e001174. doi: 10.1161/JAHA.114.001174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ho KK, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: The Framingham Study. J. Am. Coll. Cardiol. 1993;22:6A–13A. doi: 10.1016/0735-1097(93)90455-A. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.