Abstract
Objectives:
A selective therapy for pancreatitis is total pancreatectomy and islet autotransplantation. Outcomes and geographical variability of patients who had total pancreatectomy (TP) alone or total pancreatectomy with islet autotransplantation (TPIAT) was assessed.
Methods:
Data was obtained from the Healthcare Cost and Utilization Project National Inpatient Sample database. Weighed univariate and multivariate analysis were performed to determine the effect of measured variables on outcomes.
Results:
Between 2002 and 2013 there were 1006 TP and 825 TPIAT in patients with a diagnosis of chronic pancreatitis, and 1705 TP and 830 TPIAT for any diagnosis of pancreatitis. The majority of the TP and TPIAT were performed in larger urban hospitals. Costs were similar for TP and TPIAT for chronic pancreatitis but were lower for TPIAT compared to TP for any type of pancreatitis. The trend for TP and TPIAT was significant in all geographical areas during the study period.
Conclusions:
There is an increasing trend of both TP and TPIAT. Certain groups are more likely to be offered TPIAT compared to TP alone. More data is needed to understand disparities and barriers to TPIAT, and long term outcomes of TPIAT such as pain control and glucose intolerance need further study.
Keywords: total pancreatectomy, total pancreatectomy with islet autotransplantation, chronic pancreatitis, pancreatitis, healthcare utilization
Introduction
Chronic pancreatitis is a progressive fibro-inflammatory disease which can lead to endocrine and exocrine gland failure. There are genetic, toxic, environmental, idiopathic etiologies, and other risk factors, including previous acute pancreatitis, which predispose to the disease.1,2,3 It can lead to substantial loss of quality of life, decreased productivity and unemployment, and narcotic dependence.4 The pain, which is frequently relapsing and incapacitating, is the most significant complaint of all quality of life measures, and thus remains the most significant target for treatment. The incidence of chronic pancreatitis varies from 4 to 14 per 100,000 per year with a prevalence of 13 to 52 per 100,000 persons.5,6,7
Treatment strategies involve pain control, behavioral modification (quitting alcohol and tobacco smoking), endoscopic interventions and surgical pancreas duct drainage or resection procedures.8,9,10 Total pancreatectomy is considered in highly selected patients with pain refractory to standard therapy.10 Concomitant pancreas islet autologous transplantation should be considered to prevent or lessen the severity of postoperative diabetes, and hypoglycemic unawareness.11–19
Total pancreatectomy and islet autotransplantation (TPIAT) is a low volume procedure performed in centers scattered throughout the United States and the world (see www.citregistry.org).20 Other indications include recurrent acute pancreatitis, anticipated large loss of islet mass due to surgery to treat benign disease (trauma, disconnected pancreas duct), potentially malignant lesions such as intra-papillary mucinous neoplasm, or pancreas malignancy of different etiologies.21–24
Disease duration affects islet yield, but other criteria to improve patient selection, and estimate outcomes are needed.25 Escalating costs of healthcare and a shift towards value based care make it important to assess the current state of TPIAT. Major collaborative efforts to better understand and characterize phenotypes to short and long term outcomes are underway including the National Institutes of Diabetes and Digestive and Kidney Diseases supported Prospective Observational Study of TPIAT (POST) consortium. (NIDDK, R01-DK109124, PI M. Bellin).26
The study aim was to assess the national use of total pancreatectomy with or without islet autotransplantation in a cohort with a diagnosis of chronic pancreatitis, and any diagnosis of pancreatitis, determine geographical variability, and compare healthcare utilization and outcomes in patients undergoing a total pancreatectomy with or without islet autotransplantation utilizing a large, validated database.
METHODS AND MATERIAL
Data Source
Data was extracted from the Healthcare Cost and Utilization Project (HCUP; www.hcup-us.ahrq.gov) National Inpatient Sample (NIS) database, which was previously named Nationwide Inpatient Sample until the methodology to capture data was revised in 2012. The HCUP is sponsored by the Agency for Healthcare Quality and Research (AHRQ) through a federal-state-industry partnership. The NIS database is an administrative, de-identified and publically accessible database which produces national estimates of hospital inpatient stays by compiling a 20% stratified sample of discharges which is extracted from the State Inpatient Databases. This represents more than 97% of the population of the United States. The sample size of diagnoses and outcomes obtained by the NIS are representative of national outcomes.27,28 Data is captured from the hospitals from 48 States and the District of Columbia which contribute data regardless of payer, so it also includes uninsured patients. The information is used in research and by policy-makers to estimate health care utilization, access to care, quality of care, financial charges, and outcomes, and for healthcare decision making at the national, state, and local levels.
Study Population
The study population consisted of patients who had a total pancreatectomy with a diagnosis of chronic pancreatitis, and who had islet autotransplantation or not. A secondary analysis for any diagnosis of pancreatitis was also performed. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes were used to perform a query on the NIS-HCUP database for adults (≥18 years old) who had a TP or TP-IAT between 2002 and 2013 for a diagnosis of pancreatitis, and for chronic pancreatitis specifically. ICD-9-CM codes 577.0 for acute and 577.1 for chronic pancreatitis were used, respectively. Patients with a concomitant diagnosis of any pancreas neoplasia, under age 18 or pregnant were excluded. The full list of codes and selection hierarchy is in Supplemental Table 1.
The Ohio State University Data and Specimen Policy and Human Subjects Research Policy does not require institutional review board approval for analyses conducted on a population-based public data set.
Patient Characteristics and Outcomes
Demographics (age, sex, and race), income status, type of insurance, comorbidities and hospital characteristics were analyzed. Income was stratified according to quartiles based on zip codes. Type of insurance was classified into private, Medicare, Medicaid, and uninsured. Elixhauser comorbidity index, <3 and ≥3 was used to stratify comorbidities. Differences in length of stay, mortality and cost of hospitalization over the study period were also studied.
Hospitals were classified into rural, urban non-academic, and urban academic. The geographical variability of TPIAT was studied using census information which divides the country into four regions (Northeast, Midwest, South and West, see https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf). A trend analysis was performed for TP and for TPIAT over the study period, and for each region to determine geographical variability.
Statistical Analysis
Patient and hospital characteristics were summarized with means and standard errors, for continuous variables, or frequencies and percentages, for categorical variables. Because of the large sample size Student t-test and chi-square were adequate to determine differences between the two study groups. All analyses were weighed to reflect national estimates. Multivariate linear regression models were used to determine the effect of length of stay and cost which were adjusted for hospital type and size. Multivariate logistic regression was used to determine independent predictors of receiving IAT. Confidence intervals (CI) were presented were appropriate. The Cochran-Armitage test was used to test for trends of associations during the study period from 2003 to 2013. All models were adjusted for age, gender, race, income, type of insurance, Elixhauser co-morbidity score, and geographical region using weighted data and survey procedures to produce national estimates. Significance was determined with a P < 0.05. All analyses were conducted with SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
Total Pancreatectomy Compared to Total Pancreatectomy and Islet Autotransplantation in Chronic Pancreatitis
Patient Characteristics
There were 1006 TP and 825 TPIAT between the years 2002–2013 in patients with a diagnosis of chronic pancreatitis. Univariate analysis showed that the TPIAT cohort was significantly younger (41 vs 55 years P < 0.001), and predominantly female (69 vs 55%, P < 0.001), and TPIAT was more likely to be performed in the Midwest region of the country. There was no clear racial disparity as most patients were described as “white” or “other”. Income was not different, but the TPIAT cohort was more likely to have private insurance (70% vs 46%, P < 0.001). TPIAT was not performed in rural, non-teaching urban hospitals, or small and medium hospitals. The majority (94%) of the surgeries were performed in urban, tertiary academic medical centers. Comorbidities were similar in both groups. See Table 1.
Table 1.
Chronic Pancreatitis Patient Characteristics, Hospital Settings, Outcomes, and Cost
| Overall (n = 1831) | TP (n = 1006) | TPIAT (n = 825) | P | |
|---|---|---|---|---|
| Age, mean ± SE | 46.35 ± 1.17 | 50.86 ± 1.16 | 40.86 ± 0.91 | <0.001 |
| Sex, n (%) | <0.001 | |||
| Male | 707 (38.63) | 450 (44.75) | 257 (31.17) | |
| Female | 1124 (61.37) | 556 (55.25) | 568 (68.83) | |
| Race, n (%) | <0.001 | |||
| White | 948 (51.78) | 584 (58.08) | 364 (44.11) | |
| Black | 96 (5.22) | 71 (7.03) | 25 (3.03) | |
| Hispanic | 46 (2.5) | 36 (3.54) | 10 (1.22) | |
| Other | 741 (40.49) | 315 (31.35) | 426 (51.64) | |
| Income Quartile, $US dollars,* n (%) | 0.160 | |||
| First (1–37,999) | 365 (20.32) | 229 (23.3) | 136 (16.74) | |
| Second (36,000–47,999) | 466 (25.92) | 226 (23.05) | 239 (29.36) | |
| Third (46,000–63,999) | 450 (25.04) | 258 (26.31) | 192 (23.52) | |
| Fourth (62,000–64,000+) | 516 (28.72) | 268 (27.34) | 248 (30.39) | |
| Insurance, n (%) | <0.001 | |||
| Medicare | 372 (21.01) | 319 (32.47) | 54 (6.79) | |
| Medicaid | 154 (8.71) | 126 (12.8) | 29 (3.62) | |
| Private | 998 (56.32) | 447 (45.55) | 551 (69.69) | |
| Other | 247 (13.96) | 90 (9.18) | 157 (19.9) | |
| Hospital type, n (%) | ||||
| Rural | 20 (1.09) | 20 (1.99) | 0 | |
| Urban non-teaching | 94 (5.16) | 94 (9.4) | 0 | |
| Urban teaching | 1713 (93.75) | 888 (88.6) | 825 (100) | |
| Hospital bed size, n (%) | ||||
| Small | 13 (0.71) | 13 (1.29) | 0 | |
| Medium | 124 (6.78) | 124 (12.36) | 0 | |
| Large | 1690 (92.51) | 865 (86.35) | 825 (100) | |
| Hospital region, n (%) | 0.002 | |||
| Northeast | 142 (7.76) | 100 (9.9) | 42 (5.15) | |
| Midwest | 827 (45.2) | 351 (34.87) | 477 (57.79) | |
| South | 599 (32.71) | 382 (37.95) | 217 (26.33) | |
| West | 262 (14.33) | 174 (17.28) | 89 (10.73) | |
| Elixhauser co-morbidity, n (%) | 0.784 | |||
| <3 | 996 (54,55) | 553 (55.31) | 443 (53.64) | |
| ≥3 | 830 (45,45) | 447 (44.69) | 382 (46.36) | |
| Mortality, n (%) | 34 (1.85) | 34 (3.36) | 0 | |
| LOS, mean ± SE, d | 16.24 ± 0.76 | 17.42 ± 1.23 | 14.79 ± 0.69 | 0.055 |
| Cost, mean ± SE, d | 59,613 ± 4243 | 57,609 ± 5859 | 61,998 ± 3282 | 0.389 |
Quartile ranges vary from 2002 to 2013.
SE indcates standard error; TPIAT, total pancreatectomy and islet autotransplantation; LOS, length of stay.
Outcomes
Mortality was higher for TP compared to TPIAT (3.4 vs 0%, P < 0.01). Crude length of stay was similar, 17 days for TP, and 15 days for TPIAT (P = 0.55), but became statistically longer by 4.86 days (P = 0.013) for TP alone after adjusting for demographics and hospital characteristics. Cost for both interventions was similar, TP USD$4782, TPIAT was the reference (95% CI, −8691 to 18,255, P = 0.483). See Table 2.
Table 2.
Adjusted Length of Stay and Cost for Patients With Chronic Pancreatitis Who Had TP Alone Compared to TPIAT
| Adjusted Coefficient (95% CI) |
P | |
|---|---|---|
| Length of stay, d | 4.86 (1.03–8.70) | 0.013 |
| Costs, $US dollars | 4782 (−8691 to 18,255) | 0.483 |
TPIAT was cost reference.
CI indicates confidence interval; TP, total pancreatectomy; TPIAT total pancreatectomy and islet autotransplantation.
Trend Analysis
A significant trend of total pancreatectomy alone in patients with chronic pancreatitis was noted during the study period. See Supplemental Table 2. This trend was numerically higher in the Midwest. The trend of undergoing autotransplantation after total pancreatectomy for chronic pancreatitis also increased significantly during the study period, and this trend was numerically also higher in the Midwest. See Figures 1, 2, 3, and Supplemental Figure 1 and Supplemental Table 2.
FIGURE 1.
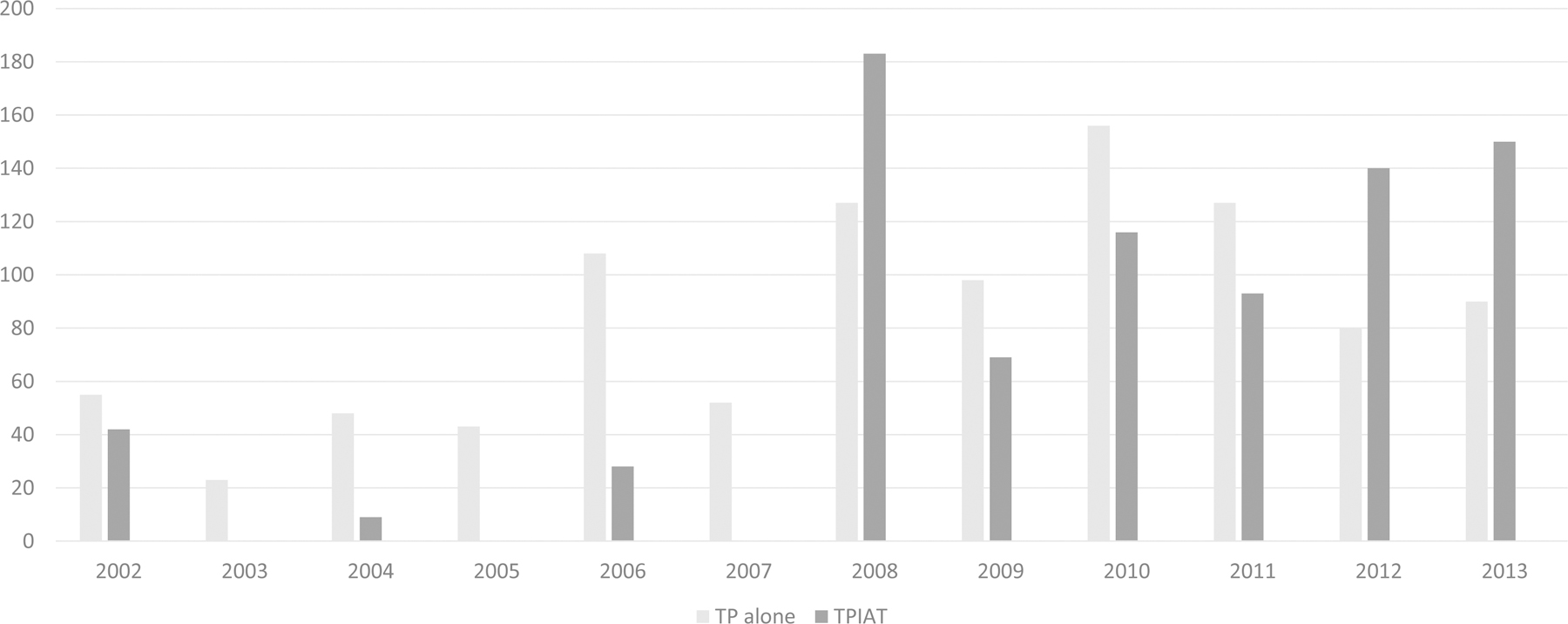
The bar-graph depicts the trend of TP alone and TPIAT in patients with chronic pancreatitis during the study period. Cell sizes <10 were not reported as they might not reflect a difference between groups. TP indicates total pancreatectomy; TPIAT, total pancreatectomy and islet autotransplantation. Cochran-Armitage test indicates a significant trend for TPIAT, P < 0.01
FIGURE 2.
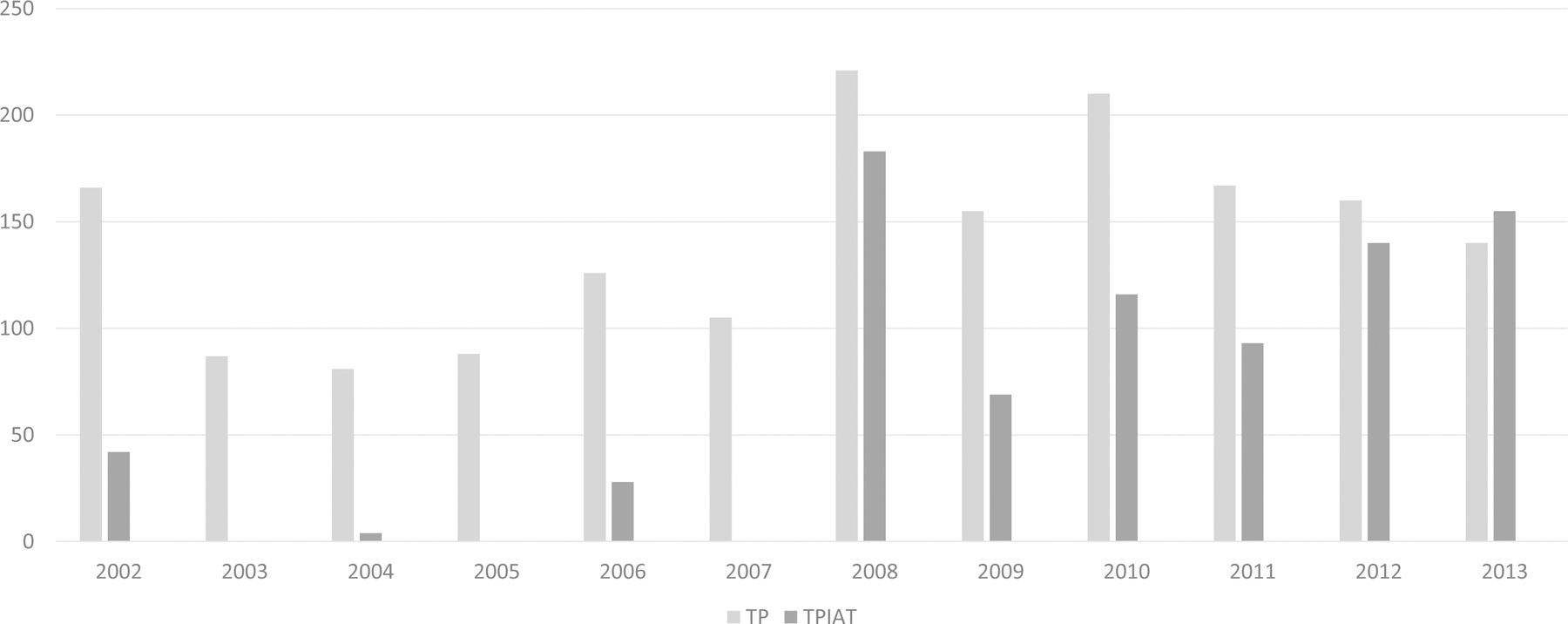
The bar-graph shows the trend of TP and TPIAT in patients with chronic pancreatitis during the study period 2002–2013 according to census derived geographical areas of the United States. Cell sizes <10 were not reported as they might not reflect a difference between groups. Cochran-Armitage test indicates a significant trend for TPIAT in all regions, P < 0.001
FIGURE 3.
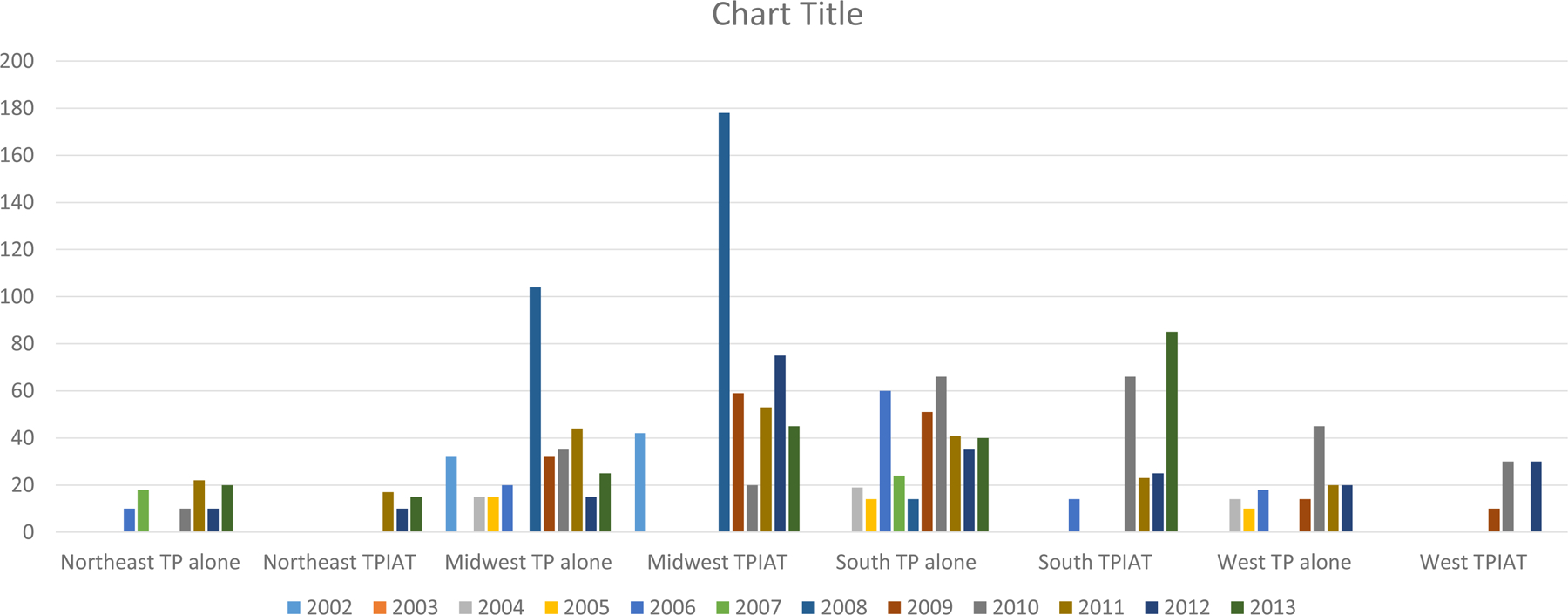
The bar-graph shows the trend of TP alone and TPIAT in patients with any type of pancreatitis during the study period. Cell sizes <10 were not reported as they might not reflect a difference between groups. Cochran-Armitage test indicates a significant trend for TPIAT in all regions, P < 0.001
Subset Analyses of Total Pancreatectomy Compared to Total Pancreatectomy and Islet Autotransplantation for Any Type of Pancreatitis
Patient Characteristics
There were 1705 TP and 830 TPIAT between the years 2002–2013. Forty-eight percent of the cohort who had a total pancreatectomy alone had a diagnosis of acute pancreatitis, whereas 12% of the TPIAT cohort had a diagnosis of acute pancreatitis. Univariate analysis showed that the TPIAT cohort was significantly younger (41 vs 50 years, P < 0.001), and predominantly female (69 vs 50%, P < 0.001). High/very high income individuals were more likely to have TPIAT instead of TP alone. No differences were observed based on type of medical insurance. The majority (90%) of the surgeries were performed in tertiary academic medical centers. Comorbidities were similar in both groups. See Table 3.
Table 3.
All Pancreatitis Patient Characteristics, Hospital Settings, Outcomes and Cost
| Overall (n = 2535) | TP (n = 1705) | TPIAT (n = 830) | P | |
|---|---|---|---|---|
| Age, mean ± SE, y | 47.28 ± 1.03 | 50.42 ± 0.84 | 40.81 ± 0.90 | <0.001 |
| Sex, n (%) | <0.001 | |||
| Male | 1104 (43.5) | 847 (49.67) | 257 (30.98) | |
| Female | 1431 (56.45) | 858 (50.33) | 573 (69.02) | |
| Race, n (%) | <0.001 | |||
| White | 1373 (54.15) | 1004 (58.87) | 369 (44.44) | |
| Black | 153 (6.05) | 129 (7.54) | 25 (3.01) | |
| Hispanic | 75 (2.94) | 65 (3.78) | 10 (1.22) | |
| Other | 934 (36.85) | 508 (29.81) | 426 (51.33) | |
| Insurance, n (%) | 0.147 | |||
| Medicare | 504 (20.36) | 367 (22.04) | 136 (16.63) | |
| Medicaid | 657 (26.41) | 412 (24.74) | 244 (29.79) | |
| Private | 642 (25.81) | 450 (27.01) | 192 (23.37) | |
| Other | 684 (27.53) | 437 (26.21) | 248 (30.2) | |
| Income Bracket, n (%) | <0.001 | |||
| Low | 639 (25.81) | 585 (34.83) | 54 (6.75) | |
| Moderate | 203 (8.22) | 170 (10.11) | 34 (4.23) | |
| High | 1334 (53.89) | 784 (46.62) | 551 (69.25) | |
| Very high | 299 (12.09) | 142 (8.45) | 157 (19.77) | |
| Hospital Type, n (%) | ||||
| Rural | 34 (1.35) | 34 (2) | 0 | |
| Urban Non-Teaching | 209 (8.26) | 209 (12.3) | 0 | |
| Urban Teaching | 2288 (90.39) | 1458 (85.7) | 830 (100) | |
| Hospital Bed Size, n (%) | ||||
| Small | 51 (2) | 51 (2.97) | 0 | |
| Medium | 197 (7.79) | 197 (11.58) | 0 | |
| Large | 2284 (90.22) | 1454 (85.45) | 830 (100) | |
| Hospital Region, n (%) | 0.002 | |||
| Northeast | 244 (9.62) | 201 (11.81) | 42 (5.12) | |
| Midwest | 1071 (42.26) | 590 (34.58) | 482 (58.05) | |
| South | 833 (32.84) | 615 (36.09) | 217 (26.17) | |
| West | 387 (15.28) | 299 (17.53) | 89 (10.67) | |
| Elixhauser Co-Morbidity, n (%) | 0.941 | |||
| <3 | 1347 (53.6) | 904 (53.74) | 443 (53.32) | |
| ≥3 | 1166 (46.4) | 778 (46.26) | 387 (46.68) | |
| Acute Pancreatitis, n (%) | 916 (36.15) | 814 (47.74) | 102 (12.33) | <0.001 |
| Chronic Pancreatitis, n (%) | 1831 (72.21) | 1006 (58.98) | 825 (99.4) | <0.001 |
| Mortality, n (%) | 129 (5.09) | 129 (7.58) | 0 | |
| LOS, mean ± SE, d | 20.67 ± 1.08 | 23.53 ± 1.22 | 14.80 ± 0.69 | <0.001 |
| Cost, mean ± SE, $US dollars | 68,462 ± 3495 | 71,808 ± 4839 | 62,001 ± 3262 | 0.066 |
Outcomes
After adjustment, TP had a statistically longer length of stay (24 vs 15 days, P < 0.001) and a higher mortality (7.5% vs 0 %, P < 0.001) compared to TPIAT. The cost of TP was also significantly higher compared to TPIAT, with a cost difference of USD$19,050 (95% CI, 2408–35,691; P = 0.025). See Supplemental Table 3.
Trend Analysis
A significant trend for TP and for TPIAT for patients with any type of pancreatitis was noted for the study period, see Supplemental Figure 2. As mentioned previously for the cohort with chronic pancreatitis, the Midwest was numerically more represented for both procedures compared to the other regions.
DISCUSSION
The study showed an increasing trend for total pancreatectomy and total pancreatectomy with islet autotransplantation for patients with chronic pancreatitis and with any type of pancreatitis for the study period. Unlike a previous study on TPIAT only, this study also included subjects who had a total pancreatectomy without islet autotransplantation.29 The number of national TPIAT became similar to, or surpassed TP alone starting in 2008, but increased trend for both was noted in all geographical zones. The South region showed a substantial increase in TPIAT in 2013, but all regions performed more TPIAT over time probably indicating more active programs. The higher activity for TPIAT in the Midwest may indicate higher volume programs in the United States, and could also be due to referral bias. Not surprisingly, all TPIAT were performed in large and urban teaching hospitals. Most of the TP alone were also performed in similar settings but about 10% of the cases were carried out in small to medium, and rural or urban non-teaching hospitals. The large number of TP alone still being performed for patients with chronic pancreatitis is intriguing, and could indicate a lack of patient or physician access to referral centers, a cohort with exclusion criteria for TPIAT, a need to educate patients and healthcare workers of the indications for TPIAT, or a need to establish more centers performing TPIAT. Most of the TPIAT were performed in subjects with a diagnosis of chronic pancreatitis, as only 12% were coded as acute pancreatitis or other (and probably most patients had recurrent acute pancreatitis). Interestingly, 47% of the TP alone were performed in patients with acute pancreatitis. The database cannot establish an etiology of the acute pancreatitis, and there are limitations with the current ICD classifications so this code may have included subjects with severe acute pancreatitis, pancreas necrosis, iatrogenic or trauma induced acute pancreatitis, pancreas leaks or abscesses, and others, which could have led to a total pancreatectomy. It is also possible that patients who had extensive pancreatic debridements or resections were coded as TP. The data on TP compared to TPIAT for all types of pancreatitis has to be interpreted with caution.
In this study patients with chronic pancreatitis and TPIAT were associated with a shorter length of stay, and no mortality compared to those undergoing TP alone. Subjects with any type of pancreatitis undergoing TPIAT also had a shorter hospitalization, no mortality, and lower cost compared to those that had a total pancreatectomy alone. These results are different to a study using the National Surgical Quality Improvement Program (NSQIP) data which described that TPIAT was associated with increased post-operative morbidity and longer length of stay without any difference in mortality. Differences may be explained by methodologies between NSQIP and NIS, and not identifying subjects with chronic pancreatitis alone in comparison to this study.30,31 The improved outcomes of a shorter length of stay and no mortality in this TPIAT cohort could be a result of selection bias of healthier patients because TPIAT is usually an elective procedure, whereas TP may have been performed acutely, and for other indications already discussed. The Elixhauser co-morbidity score was similar in both groups so other differences not measured in the database may have existed. The lower cost for TPIAT found in the any pancreatitis group could be due to the shorter duration of hospitalization. No cost difference was found in the chronic pancreatitis cohorts, but at least one previous study indicated that for minimal change chronic pancreatitis TPIAT was cost-effective and increased quality adjusted survival compared to medical management.32 More studies to understand the costs associated with TPIAT are needed.
A few factors favored TPIAT for patients with chronic pancreatitis, and this included younger age, female sex, and having private insurance. These results are not unexpected. Case series of TPIAT show a higher prevalence of females in this age group. TPIAT is not covered by Medicare or Medicaid but it is by most private insurers which limits the procedure availability [see https://www.cms.gov/medicare-coverage-database], and may bias towards a younger, and presumably healthier group.18,33,34 For all types of pancreatitis, TPIAT was associated with younger age, female sex, and higher income bracket. While insurance coverage did not predict TPIAT in this group, the higher income bracket could be associated with an increased likelihood of having private insurance, and thus access to TPIAT. The younger age may indicate a selection bias that may affect suitability for TPIAT. For example, the presence of diabetes mellitus is usually a latter occurrence in chronic pancreatitis, so patients are usually older, and may disqualify patients for TPIAT. Also noteworthy, 45% of the patients who had TP alone in the any type of pancreatitis cohort were covered by Medicare or Medicaid. It would be concerning if these patients had a TP alone due to lack of insurance coverage. More than half of the patients were coded as “other race”, followed by whites, so it is not possible to determine racial disparity with certainty, a known limitation of the database.35 The role of factors associated with TPIAT need to be studied further to determine the disparities that affect patient selection which may prevent other groups from receiving TPIAT, possibly including insurance coverage.
It was interesting to note the regional variability of TPIAT. Improving referral opportunities, patient and caregiver education, and possibly having more centers performing TPIAT could improve access. While the number of smaller and rural hospitals performing TP alone was small it would be interesting to know possible factors that deterred referral to a higher level of care.
There are several limitations worth reviewing. As large as the NIS database is, it is retrospective, and weighted to represent national estimates using a 20% sample, so lack of data may only indicate that patients who may have actually had TP alone or TPIAT were not in the sample, and not that the procedures were not performed. Samples with less than 10 patients were excluded from statistical analysis.36 Still, the trend of both procedures showed that both are being performed more frequently, and that TPIAT is becoming more commonplace. As an administrative database the results are dependent on the accuracy of the billing codes which are subject to error. 35 For this study subjects were found by selecting total pancreatectomy, then islet autotransplantation, and then chronic (or any) pancreatitis so it is likely that patients with this diagnosis actually had the disease. The number of evaluable variables in the NIS is large, but more specific data to understand etiologies, patient characteristics, and co-morbidities which may have affected suitability for TPIAT and outcomes are not available.37
In conclusion, this study shows an increasing trend of both TP and TPIAT, and suggests that some geographical variance exists. Barriers to access TPIAT need to be explored because it appears that certain groups are more likely to be offered the procedure. TP without islet autotransplantation is still being performed regularly so more data to understand if this is related to disease activity, access, or knowledge about TPIAT, would be helpful. Expanding TPIAT insurance coverage to Medicare and Medicaid patients should also be explored. Further studies to understand when to pursue TP alone, and how to select patients for TPIAT, barriers to TPIAT access, potential racial disparities, and long term outcomes such as improvement in pain, quality of life, productivity, and euglycemia, are necessary.33,34, 38–41
Supplementary Material
ACKNOWLEDGMENTS
POST Study Consortium: The authors would like to acknowledge the efforts of the supporting team members James S. Hodges (University of Minnesota School of Public Health), Helen Voelker (University of Minnesota, DCC database management), Yi Yang (University of Minnesota, Biostatistics), Joshua J. Wilhelm (University of Minnesota, islet lab), Dr. Kenneth Washburn (The Ohio State University, Surgery), Dr. Amer Rajab (The Ohio State University, Surgery and Islet Isolation), Dr. Shumei Meng (The Ohio State University, Endocrinology), and the following study coordinators: Peggy Ptacek (University of Minnesota), Jayne Pederson (University of Minnesota), Anne Elizabeth Farrow (Baylor), Jovana Valdez (Baylor), Misty Troutt (Cincinnati Children’s Hospital), Amanda Schreibeis (Cincinnati Children’s Hospital), Jessica Chevalier (Dartmouth Hitchcock), Jessica Hiscoe (Dartmouth Hitchcock), Mahya Faghih (John Hopkins), Sheila Fedorek (University of Pittsburgh), Lindsay Basto (University of Chicago), Mortadha Abd (Medical University of South Carolina), Caitlin Schaffner (Medical University of South Carolina), Casey McClurkin (The Ohio State University), Brianna Conley (The Ohio State University), Alejandra Cervantes (The Ohio State University), Alice Hinton (The Ohio State University-Graduate Research), and Jill Buss (The Ohio State University).
Grant Support: None
Abbreviations:
- TP
total pancreatectomy
- TPIAT
total pancreatectomy with islet autotransplantation
- HCUP
Healthcare Cost and Utilization Project
- NIS
National Inpatient Sample
- AHRQ
Agency for Healthcare Quality and Research
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
Footnotes
The authors have no conflicts of interest to disclose relevant to this manuscript.
Disclosures: Luis F. Lara, MD, Consultant, Medtronic; Speaker, Abbvie, Allergan. The other authors did not disclose conflicts of interest related to the manuscript.
REFERENCES
- 1.Whitcomb DC, Frulloni L, Garg P, et al. Chronic pancreatitis: An international draft consensus proposal for a new mechanistic definition. Pancreatology. 2016:2:218–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chari ST, Singer MV. The problem of classification and staging of chronic pancreatitis. Proposals based on current knowledge of its natural history. Scand J Gastroenterol 1994;29:949–960. [DOI] [PubMed] [Google Scholar]
- 3.Sankaran SJ, Xiao AY, Wu LM, et al. Frequency of progression from acute to chronic pancreatitis and risk factors:a meta-analysis. Gastroenterology. 2015;149:1490–1500. [DOI] [PubMed] [Google Scholar]
- 4.Pezzilli R, Bini L, Fantini L, et al. Quality of life in chronic pancreatitis. World J Gastroenterol 2006;12:6249–6251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Machicado JD, Yadav D. Epidemiology of recurrent acute and chronic pancreatitis: similarities and differences. Dig Dis Sci 2017;62:1683–1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jupp J, Fine D, Johnson CD. The epidemiology and socioeconomic impact of chronic pancreatitis. Best Pract Res Clin Gastroenterol 2010; 24:219–231. [DOI] [PubMed] [Google Scholar]
- 7.Conwell DL, Lee LS, Yadav D, et al. American Pancreatic Association practice guidelines in chronic pancreatitis: evidence-based report on diagnostic guidelines. Pancreas 2014;43:1143–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lankisch PG, Löhr-Happe A, Otto J, et al. Natural course in chronic pancreatitis. Pain, exocrine and endocrine pancreatic insufficiency and prognosis of the disease. Digestion 1993;54:148–155. [DOI] [PubMed] [Google Scholar]
- 9.Yadav D, Hawes RH, Brand RE, et al. Alcohol consumption, cigarette smoking, and the risk of recurrent acute and chronic pancreatitis. Arch Intern Med 2009;169:1035–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andersen DK, Frey CF. The evolution of the surgical treatment of chronic pancreatitis. Ann Surg 2010;251:18–32. [DOI] [PubMed] [Google Scholar]
- 11.Blondet JJ, Carlson AM, Kobayashi T, et al. The role of total pancreatectomy and islet autotransplantation for chronic pancreatitis. Surg Clin North Am 2007;87:1477–1501. [DOI] [PubMed] [Google Scholar]
- 12.Garcea G, Weaver J, Phillips J, et al. Total pancreatectomy with and without islet cell transplantation for chronic pancreatitis: a series of 85 consecutive patients. Pancreas 2009;38:1–7. [DOI] [PubMed] [Google Scholar]
- 13.Sutherland DER, Gruessner AC, Carlson AM, et al. Islet autotransplant outcomes after total pancreatectomy: a contrast to islet allograft outcomes. Transplantation. 2008;86:1799–1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Digon BJ. History of islet transplantation. Curr Diab Rep 2009;9:312–316. [DOI] [PubMed] [Google Scholar]
- 15.Andren-Sandberg A, Hoem D, Gislason H. Pain management in chronic pancreatitis. Eur J Gastroenterol Hepatol 2002;14:957–970. [DOI] [PubMed] [Google Scholar]
- 16.Warnock GL, Thompson DM, Meloche RM, et al. A multi-year analysis of islet transplantation compared with intensive medical therapy on progression of complications in type 1 diabetes. Transplantation 2008;86:1762–1766. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez Rilo HL, Ahmad SA, D’Alessio D, et al. Total pancreatectomy and autologous islet cell transplantation as a means to treat severe chronic pancreatitis. J Gastrointest Surg 2003;7:978–989. [DOI] [PubMed] [Google Scholar]
- 18.Sutherland DE, Radosevich DM, Bellin MD, et al. Total pancreatectomy and islet autotransplantation for chronic pancreatitis. J Am Coll Surg 2012;214:409–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chinnakotla S, Beilman GJ, Dunn TB, et al. Factors predicting outcomes after total pancreatectomy and islet autotransplantation lessons learned from over 500 cases. Ann Surg 2015;262:610–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sutherland DE. Report from the International Pancreas Transplant Regisry. Diabetologia. 1991;34:Supple1: S28–S39 [DOI] [PubMed] [Google Scholar]
- 21.Bellin MD, Balamurugan AN, Pruett TL, et al. No islets left behind: islet autotransplantation for surgery-induced diabetes. Curr Diab Rep 2012;12:580–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jindal RM, Riccordi C, Shriver CD. Autologous pancreatic islet transplantation for severe trauma. N Engl J Med 2010;22:362:1550. [DOI] [PubMed] [Google Scholar]
- 23.Gala-Lopez BL, Semlacher E, Manouchehri N, et al. Autologous islet transplantation after total pancreatectomy for renal cell carcinoma metastases. Am J Transplant 2011;11:2708–2714. [DOI] [PubMed] [Google Scholar]
- 24.Kobayashi T, Sato Y, Hirukawa H, et al. Total pancreatectomy combined partial pancreas autotransplantation for recurrent pancreatic cancer: a case report. Transplant Proc 2012;44:1176–1179. [DOI] [PubMed] [Google Scholar]
- 25.Takita M, Lara LF, Naziruddin B, et al. Effect of the duration of chronic pancreatitis on pancreas islet yield and metabolic outcome following iselt autotransplantation. J Gastrointest Surg 2015;19:1236–1246. [DOI] [PubMed] [Google Scholar]
- 26.Bellin MD, Abu-El-Haija M, Morgan K, et al. A multicenter study of total pancreatectomy with islet autotransplantation (TPIAT): POST (Prospective Observational Study of TPIAT). Pancreatology. 2018;18:286–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.AHRQ, AHRQ comparative analysis of HCUP and NHDS inpatient discharge data [AHRQ Web site] 2015. Available at: https://www.ahrq.gov/research/data/hcup/nhds/niscomp.html. Accessed October 15, 2018.
- 28.AHRQ, HCUP quality control procedures [HCUP Web site] 2016. Available at: https://www.hcup-us.ahrq.gov/db/quality.jsp. Accessed October 15, 2018.
- 29.Fazlalizade R, Moghadamyeeghaneh Z, Demirjian AN, et al. Total pancreatectomy and islet autotransplantation: A decade nationwide analysis. World J Transplant 2016;6:233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhayani NH, Enomoto LM, Miller JL, et al. Morbidity of total pancreatectomy with islet cell auto-transplantation compared to total pancreatectomy alone. HPB (Oxford). 2014;16:522–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiss A, Anderson JE, Chang DC. Comparing the National Surgical Quality Improvement Program with the Nationwide Inpatient Sample database. JAMA Surg 2015;150:815–816. [DOI] [PubMed] [Google Scholar]
- 32.Wilson GC, Ahmad SA, Schauer DP, et al. Cost-effectiveness of total pancreatectomy and islet cell autotransplantation for the treatment of minimal change chronic pancreatitis. J Gastrointest Surg 2015;19:46–54. [DOI] [PubMed] [Google Scholar]
- 33.Bellin MD, Kerdsirichairat T, Beilman GJ, et al. Total pancreatectomy with islet autotransplantation improves quality of life in patients with refractory recurrent acute pancreatitis. Clin Gastroenterol Hepatol 2016;14:1317–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bellin MD, Gelrud A, Arreaza-Rubin G, et al. Total pancreatectomy with islet autotransplantation: summary of an NIDDK workshop. Ann Surg 2015;261:21–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krishna SG, Kamboj AK, Hart PA, et al. The changing epidemiology of acute pancreatitis hospitalizations: a decade of trends and the impact of chronic pancreatitis. Pancreas 2017;46:482–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dimick JB, Welch HG, Birkmeyer JD. Surgical mortality as an indicator of hospital quality: the problem with small sample size. JAMA 2004;292:847–851. [DOI] [PubMed] [Google Scholar]
- 37.Genta RM, Sonnenberg A. Big data in gastroenterology research. Nat Rev Gastroenterol Hepatol 2014;11:386–390. [DOI] [PubMed] [Google Scholar]
- 38.Solomina J, Gołębiewska J, Kijek MR, et al. Pain control, glucose control, and quality of life in patients with chronic pancreatitis after total pancreatectomy with islet autotransplantation: a preliminary report. Transplant Proc 2017;49:2333–2339. [DOI] [PubMed] [Google Scholar]
- 39.Morgan K, Owczarski SM, Borckardt J, et al. Pain control and quality of life after pancreatectomy with islet autotransplantation for chronic pancreatitis. J Gastrointest Surg 2012;16:129–133. [DOI] [PubMed] [Google Scholar]
- 40.Garcea G, Pollard CA, Illouz S, et al. Patient satisfaction and cost-effectiveness following total pancreatectomy with islet cell transplantation for chronic pancreatitis. Pancreas 2013;42:322–328. [DOI] [PubMed] [Google Scholar]
- 41.Wilson GC, Sutton JM, Abbott DE, et al. Long-term outcomes after total pancreatectomy and islet cell autotransplantation: is it a durable operation? Ann Surg 2014;260:659–665. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


