Abstract
Purpose of Review
Arm care programs for baseball players are an increasingly popular area of interest for players, parents, coaches, sports performance staff, and team physicians. Once a general afterthought, the design of arm care programs is now heavily scrutinized in order to maximize performance and help reduce injury risk. Given the recent spike in interest for arm care programs for baseball players of all ages, the purpose of this work is to review the relevant literature regarding the efficacy of arm care programs and to discuss the authors’ preferred, evidence-based principles for arm care programs.
Recent Findings
Arm care programs appear to provide favorable results for performance, maintenance of strength and flexibility, and reduced injury risk. These programs should be tailored to the demands of the athlete, which can change based on the time of year and physical demands of the player’s position. A good program will incorporate flexibility, strengthening, proprioception, and joint mobility for the entire kinetic chain. Appropriate warm-up and cool-down periods are also important. Arm care programs should start with basic movement patterns before progressing to more advanced, coordinated exercises.
Summary
Arm care programs are an important piece of a holistic approach to caring for the throwing arm of baseball athletes. In general, they appear to be a safe and efficacious way to help prevent a portion of throwing arm injuries. Further research is needed to determine the optimal arm care program for each athlete.
Keywords: Arm care, Baseball, Injury prevention, Thrower, UCL, Recovery
Introduction
Arm care programs for injury prevention and performance enhancement in baseball pitchers continue to evolve rapidly. Once a foreign concept to the game of baseball, implementation of various arm care programs is now commonplace throughout all levels of play. This is likely due to the dramatic increase in upper extremity injuries in baseball pitchers during the past several decades [3, 6, 8, 13, 18, 29, 39]. Multiple risk factors have contributed to this rise, including but not limited to pitching while fatigued, year round pitching, glenohumeral internal rotation deficit, glenohumeral total arc of motion deficit, scapular dyskinesia, increased number of innings pitched during a season, and exceeding pitch count rules [4•, 7, 11, 14, 24, 32, 34, 51, 53].
Great effort has been made to combat this arm injury epidemic in baseball players through conscientious workload management and arm care programs. One example of this is the implementation of pitch count rules throughout most amateur baseball leagues after their introduction in Little League Baseball in 2006. In addition to workload management, specific pre- and post-outing arm care programs have been promoted as a way to decrease injury risk.
While individual programs may vary, there are a few key foundational elements in most programs. These include a dynamic warm-up, appropriate glenohumeral and elbow mobility, maintenance of rotator cuff strength, scapular stabilization strength and endurance, appropriate workload management, and recovery that promotes decreasing inflammation and maintenance of flexibility and strength. In general, arm care programs for baseball pitchers often have two primary goals: optimization of pitching performance and prevention of throwing arm injuries. Unfortunately, the influx of commercially driven arm care programs has made it more difficult for players, parents, and coaches to choose an appropriate evidence-based arm care program that accomplishes these critical goals. Therefore, the purpose of the current review article is to provide a thorough review of relevant literature that examines the efficacy of arm care programs in preventing throwing injuries. After a review of the literature, we will discuss our evidence-based fundamentals for a preferred arm care program for baseball athletes.
Efficacy of Existing Arm Care Programs
Strength, flexibility, and warm-up/recovery modalities remain the pillars of the most popular arm care programs. Several studies have evaluated the efficacy of various programs in the youth athlete specifically. Sakata et al. assessed 305 previously healthy baseball players ages 8–11, 136 of which were provided with a specific program, while 169 athletes comprised a control group [37]. The intervention group was instructed to perform nine strengthening exercises with a focus on rotator cuff, scapular control, and lower body strengthening/balance as well as nine stretching exercises. The intervention group endorsed a rate of 57% compliance, performing the exercises 1.3 times per week on average. The primary outcome was medial elbow injury. The authors found a 49.2% decreased incidence in subsequent elbow injury in the intervention group (P < 0.05). Increased total shoulder rotation, increased hip internal rotation of the non-dominant side, and decreased thoracic kyphosis angle were also predictive of lower rates of medial elbow injury. Of note, pitch counts were not a contributing factor to increased injury rates. Limitations of this study included lack of randomization and lack of evaluation for any preventative shoulder outcomes. Sakata et al. later went on to prospectively evaluate 237 youth baseball players ages 9–11 years old in a randomized controlled study utilizing a shorter, easier program in an effort to increase compliance [38••]. This 10-min program included 5 stretching exercises (10 s holds), 2 dynamic mobility exercises (scapular and thoracic), and 2 balance training exercises with 10 repetitions for each exercise. Compliance was reported to be as high as 73.4% with an average completion rate of 1.6 times per week. Shoulder and elbow injuries were monitored prospectively for 12 months and a 48.5% decreased risk of injury in the intervention group was found, which reached statistical significance. Furthermore, velocity increased in the intervention group (6.4 km/h vs 4.1 km/h in controls) as did shoulder horizontal adduction deficits on the dominant side, hip internal rotation on the non-dominant side, and thoracic kyphosis angle.
Finally, Shitara et al. evaluated 92 high school pitchers who were allowed to self-allocate into a flexibility and strength training group, a flexibility only group, and a group who did neither strengthening nor mobility work [42•]. The flexibility group performed 5 reps of 60 s holds of sleeper stretch after baseball activities. The strength training and flexibility group focused on ER strength using a standardized protocol with a load of 500 g, 20 reps, and 3 sets per day. Injury was defined as inability to play for at least 8 days, and injury rates were found to be 25% in the stretching only group, with average time to injury being 89 days and compliance rate of 77%. Injury rates were found to be 35% in the strength and flexibility group with average time to injury being 92 days and compliance rate of 65%. In the group that performed neither, 57% sustained an injury with average time to injury being 29.5 days. A 9% increase in dominant shoulder internal rotation resulted in 36% reduction in risk of injury. It is worth noting that post hoc analysis showed insufficient power to detect differences between the group who did neither and the group who did both strengthening and stretching as it pertains to strength and injury incidence. Furthermore, the self-selection design was a significant limitation of this study. Nonetheless, the trends provide compelling evidence that further investigation is needed to better understand the full benefits of arm care programs.
Baseline Assessments
Objectively measuring baseline shoulder strength and tracking it throughout the season is an essential component of injury prevention for throwers. Multiple early studies have examined concentric isokinetic shoulder strength in professional baseball pitchers [1, 10, 52]. Wilk assessed 150 professional baseball players using a Biodex isokinetic dynamometer showing an external/internal ratio of 61–65% [52]. This study also concluded that there was no significant difference between dominant and non-dominant IR and ER muscle strength. Ellenbecker showed a similar peak torque ER/IR ratio at 66.6% on the dominant arm, and significantly greater IR strength on the dominant shoulder [10]. No side to side difference for ER strength was appreciated.
With these generally accepted objective ratios in mind, targeted monitoring of specific athlete strength and endurance parameters, along with ranges of motion compared to baseline, provides greater opportunities for targeted treatment of altered movement patterns. It is also worth noting that, in the case of pitchers, differences in range of motion of the throwing shoulder typically exist before and after pitching. Some gain external rotation, others loose internal rotation, and some gain both [5, 17, 26]. Further, changes at the shoulder may be seen for a number of days after pitching [26].
Once flagged as abnormal, appropriate interventions can take place prior to reassessment. Tyler et al. prospectively evaluated 101 pitchers from 4 different high schools over 4 seasons and found that pre-season supraspinatus weakness in particular was a risk factor for subsequent major injury [48]. Targeted intervention with deficits of greater than 20% was recommended based on these findings. Furthermore, preseason external rotation and supraspinatus weakness have also been shown to be risk factors for injury at the professional level. In order to optimize and individualize arm care programs, practitioners must consider the inter-athlete and intra-athlete daily differences via screening as described above and workload inputs.
Approach to Strengthening
During the pitch, the rotator cuff works both concentrically to accelerate the arm and to provide glenohumeral stability, as well as eccentrically to decelerate the arm. Training the rotator cuff in a way that targets both of these contractions is ideal for arm care programs. Depending on the status of the athlete on any given day, the arm care program can consist of isometric, concentric, or eccentric exercises. The player’s daily workload, consisting of throwing and weight lifting exposure, can influence which type of muscle exercises is optimal for the athlete. If a player feels sore, then he might benefit from isometric contractions to minimize stress on the muscles through a more narrow range of motion. If the goal is to increase strength and promote tendon remodeling, then the athlete might benefit from strengthening through a larger range of motion with heavier resistance, as performed with concentric and eccentric contractions.
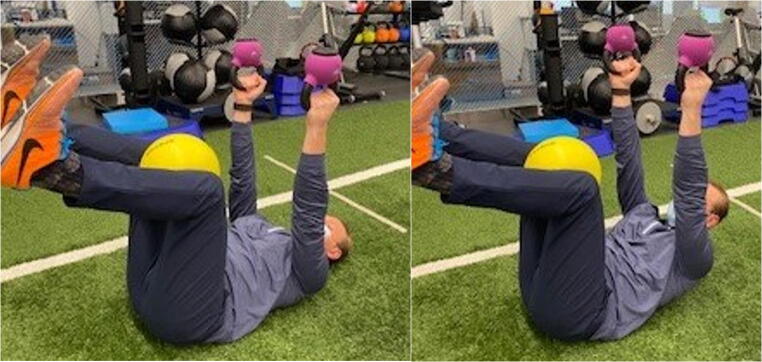
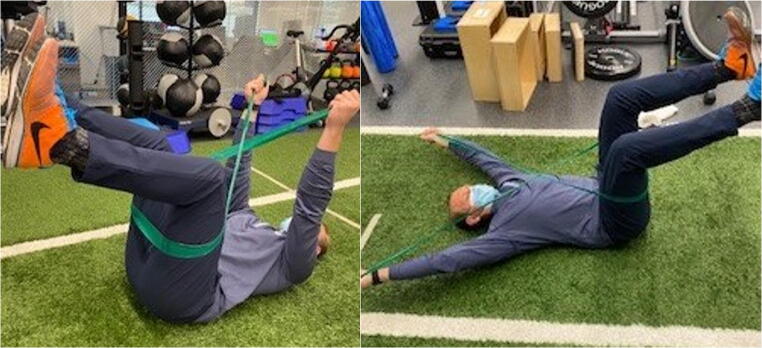
In general, a progression of rotator cuff exercises should start with ER and IR at 0° abduction with scaption on the opposite side, progressing to 90°of shoulder abduction (Fig. 1), followed by incorporation of rhythmic stabilization for neuromuscular control at both mid and end range of shoulder rotation. Side-lying external rotation in a side plank (Fig. 2) is also commonly used in daily arm care programs. All of these can be progressed by changing the athlete’s stance, adding more proximal challenges, as well as linking other muscle groups.
Fig. 1.
a Shoulder external rotation at 0° abduction with opposite arm scaption. b Shoulder external rotation at 90° abduction
Fig. 2.

Shoulder external rotation in modified side plank
Glenohumeral stability during the pitch and the ability to maximize rotator cuff activation depends on the control of its more proximal segment, the scapula. During the overhead pitch, the scapula has to retract during the cocking phase as well as protract during the acceleration phase [33]. It is important to constantly assess throwers for scapular winging or dyskinesia. Arm care programs should be inclusive of exercises that focus on strength and endurance of both scapular retractors along with protractors (Fig. 3).
Fig. 3.
Serratus protraction with adduction squeeze
The serratus anterior plays an especially important role in stability of the upper extremity and serves as an important link between the core and the shoulder. If an athlete lacks neuromuscular control of the scapula, they might be subject to increased stress and subsequent injury.
A stable core and appropriate rib cage positioning (Fig. 4) should be considered in all arm care programs in addition to hip mobility and lower extremity strength. A multifaceted approach should be utilized in assessing the core, as proximal foundational stability of the core is theorized to allow for enhanced distal mobility of segments such as the arm [25]. From a hip mobility perspective more specifically, Saito et al. demonstrated that limitations to hip flexion and internal rotation at 90 degrees of hip flexion were risk factors for elbow injury in the youth population [36], and Kantrowitz et al. have demonstrated a similar relationship between hip pathology and UCL tears in a professional cohort [23]. Furthermore, in the setting of performance, Kageyama et al. demonstrated that higher velocity pitchers generate greater momentum by hip extension/abduction and knee extension in the pivot leg for accelerating the body forward as well as by generating greater angular core velocities [22]. Therefore, stabilizing lower limbs during pitching plays an important role in order to increase rotation and forward trunk motion; and, therefore, lower extremity and core strength monitoring should not be neglected as part of arm care programs.
Fig. 4.
Core stabilization with shoulder elevation
Properly sequencing movement is a key task in overhead throwing [41]. Therefore, progressions in arm care programs include beginning with simple isolated single joint glenohumeral strengthening to eventually incorporating total body motions that engage the entire kinetic chain from toes to fingertips. This concept should be considered more globally and incorporated when programming arm care exercise selection. An application of this might include beginning arm care programs in a gravity reduced prone or supine position, working to establish proper firing and neuromuscular control, followed by progression to more challenging environments such as quadruped, kneeling, and eventually standing. Further progression would include incorporation of more segments throughout the kinetic chain that require greater coordination. For these reasons, the authors take a meticulous approach to assessment of other body segments, especially the ankle, hip, and the spine. This is in contrast to traditional arm care programs that do not typically consider the entire kinetic chain.
Recovery
Recovery is a pivotal component of arm care in the pitching athlete, especially within the competitive season. Commonly used modalities include the following: active recovery, contrast and cryotherapies, soft tissue massage, stretching and mobility work, compression, and blood flow restriction. While a detailed review of these modalities is beyond the scope of this article, modalities are generally targeted to have one or more of the following effects: blood flow changes, tissue temperature changes, altered nerve conduction velocity, and changes in hydrostatic pressure affecting capillary and cellular permeability. The belief is that these methods may have benefits in reducing inflammation/edema, increasing removal of metabolic waste, and shortening the recovery time frame [43, 45]. Acutely, these methods have been shown to have mixed results on improving performance [9, 35, 44, 47]. However, numerous studies have shown the perceived benefits in muscle soreness, fatigue, and readiness [35, 49, 50]. Historically, conjecture exists on the utility of these modalities, as training theory suggests that post-exercise inflammation is essential for promotion of positive long-term adaptations. Therefore, in theory, recovery modalities may have a “dampening” effect. While the research exploring this effect is scarce, the authors believe that recovery modalities should be individualized based on the timing within the season and training plan as well as the athlete’s needs and preferences.
Workload Management
Athlete workload has become widely discussed within the literature and greater sports media. A number of studies have shown that injured players pitch more months, games, innings, and pitches per year [15, 32]. As expected, with increased exposure comes increased injury. This hypothesis was supported by Lazu et al. in 2019 who demonstrated significant correlation between arm soreness and pitch volume in collegiate pitchers throughout an entire season [28]. However, this correlation of workload to injury risk has not been consistently demonstrated in Major League pitchers [12]. Made popular by the work of Blanch and Gabbett, who explored the acute to chronic workload ratio and (ACWR) association with injury, workload management has become commonplace in professional sports [2]. Recently, these methods have come under scrutiny due to possible inappropriate statistical properties and conceptual issues that may complicate interpretations for practical applications [19]. However, a recent systematic review concluded that despite the high variability, ACWR calculations for external (e.g., total distance) and internal (e.g., heart rate) loads may be related to injury risk. That said, the authors called for standardized methods and more objective conclusions from multiple populations before such models can be used confidently to mitigate injury risk [30]. Nonetheless, the exploration of rolling average counts and potential for inclusion of ratios provides practitioners the opportunity to understand a pitcher’s throwing volume and rate of change of volume, which can help better periodize the training regimen. Within these calculations, it is important to consider the competition and role-specific time cycles of the pitcher (i.e., 5-day rotation starting pitcher versus relief pitcher).
It is plausible that a sudden increase in workload leads to fatigue and negative performance/musculoskeletal effects. ACWR calculations may be used as a guide, with numbers greater than one being concerning for accumulating fatigue. Currently, there is a relative paucity of literature supporting the utility and efficacy of ACWR in baseball specifically, but it may still serve as a useful metric for physical stress. It is also important to consider that workload ratios will be different for players based on defensive position played, especially between relief and starting pitchers who clearly have unique demands.
Historically, workload has been managed by pitch counts and inning limits. Pitch counts in isolation exemplify an unrefined external workload representation for pitchers. They fail to consider the intra-pitch type mechanical differences and do not include the multitude of throwing drills pitchers complete (i.e., catch play, long-toss, flat ground pitching, towel drills, plyo-ball work, warm-up throws, and bullpen drills) [54]. Akin to global position system (GPS) monitoring in invasion sports, microsensor technology developments have opened the door for deeper analysis of pitcher workload. Further research is required to build out models to better understand the stressors placed on the neurological and musculoskeletal systems within the different pitcher training practices. Finally, while objective data is invaluable as it pertains to trends and workload management, perceived exertion by the athlete should not be neglected as a subjective intensity marker.
Individualizing Arm Care
A periodized approach in the long- and short-term manipulation of training and competition stress and recovery is thought to be essential for optimal athletic performance and success in competition [20]. Opportunities exist within the day-to-day management of the athlete to titrate appropriate care in an integrated periodization fashion [31••]. A team- or athlete-specific exercise continuum can be developed and adopted to daily needs. For example, athletes with limited throwing exposures may benefit from supplementation with more challenging stimuli, such as plyometric and eccentric exercises. These replicate the demands of throwing to promote a well-controlled and appropriate dosage of physiological stressors, such as tendon mechanical stress and exercise-induced muscle damage, which leads to positive training effects [16, 21, 27•, 46]. On the contrary, athletes undertaking significant throwing workloads may benefit from a higher percentage of recovery modalities, as fatigue and physiological changes may influence performance and training in the near future [16]. Creating a daily tailored approach may mitigate risk of placing additional undue stress on athletes that may be created by a structured block periodization program. Furthermore, a personalized approach can increase perceived benefits of recovery modalities with appropriately timed exposures [31••]. Subjective screening questionnaires provide an avenue for the quantification of the athlete-perceived workload (i.e., rating of perceived exertion) and response to workloads and intervention (i.e., muscle soreness) [40]. These measures can be used in concert with external load data to appropriate arm care. Long-term investigations are needed to better understand individual responses to workload and arm care intervention.
Conclusion
Arm care programs can be enhanced by taking a multifaceted approach to monitoring and strengthening. Arm care should be periodized through the year, depending on the specific demands of the sport. An off-season arm care program should look dramatically different than an in-season program, as the athlete is taxed in a much different way in these two situations. Within season, arm care dosage should be prescribed based on the load that the athlete is encountering. Adjustments in volume and intensity of arm care exercises should undulate accordingly with pitch count, total throwing volume, subjective reports of fatigue, objective tracking of measures such as strength and range of motion, and consideration of internal and external load that the athlete is experiencing. Constant reassessment on a daily or weekly basis should be implemented to determine the response to both competition and training, and frequent adjustments should be made. Further research is required to determine the ideal arm care programs for performance and injury risk mitigation.
Compliance with Ethical Standards
Conflict of Interest
Kathryn McElheny, James Carr II, and Terrance Sgroi declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Injuries in Overhead Athletes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kathryn McElheny, Email: mcelhenyk@hss.edu.
Terrance Sgroi, Email: sgroit@hss.edu.
James B. Carr, II, Email: carrja@hss.edu.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Alderink GJ, Kuch DJK. Isokinetic shoulder strength of high school and college-aged pitchers. J Orthop Sports Phys Ther. 1986;7:163–172. doi: 10.2519/jospt.1986.7.4.163. [DOI] [PubMed] [Google Scholar]
- 2.Blanch P, Gabbett TJ. Has the athlete trained enough to return to play safely? The acute:chronic workload ratio permits clinicians to quantify a player’s risk of subsequent injury. Br J Sports Med. 2016;50:471–475. doi: 10.1136/bjsports-2015-095445. [DOI] [PubMed] [Google Scholar]
- 3.Camp CL, Conte S, D’Angelo J, Fealy SA. Epidemiology of ulnar collateral ligament reconstruction in major and minor league baseball pitchers: comprehensive report of 1429 cases. J Shoulder Elb Surg. 2018;27:871–878. doi: 10.1016/j.jse.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 4.• Camp CL, Sinatro A, Spiker A, Werner BC, Altchek DW, Coleman SH, Dines JS (2017) Decreased shoulder external rotation and flexion are greater predictors of injury than internal rotation deficits: analysis of 132 pitcher-seasons in professional baseball. Orthop J Sport Med SAGE Publications 5:2325967117S0022. Although prior work has supported the importance of reducing glenohumeral internal rotation deficits in pitchers, this study demonstrates that deficits in shoulder ER and flexion are more significant predictors of subsequent elbow injury. [DOI] [PubMed]
- 5.Case JM, Mannava S, Fallin JH, Stone AV, Freehill MT. Acute changes in glenohumeral range-of-motion following in-season minor league pitching starts. Phys Sportsmed. 2015;43:360–365. doi: 10.1080/00913847.2015.1059249. [DOI] [PubMed] [Google Scholar]
- 6.Conte SA, Fleisig GS, Dines JS, Wilk KE, Aune KT, Patterson-Flynn N, Elattrache N. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43:1764–1769. doi: 10.1177/0363546515580792. [DOI] [PubMed] [Google Scholar]
- 7.Coughlin RP, Lee Y, Horner NS, Simunovic N, Cadet ER, Ayeni OR (2019) Increased pitch velocity and workload are common risk factors for ulnar collateral ligament injury in baseball players: a systematic review. J. ISAKOS.
- 8.Degen RM, Camp CL, Bernard JA, Dines DM, Altchek DW, Dines JS. Current trends in ulnar collateral ligament reconstruction surgery among newly trained orthopaedic surgeons. J Am Acad Orthop Surg. 2017;25:140–149. doi: 10.5435/JAAOS-D-16-00102. [DOI] [PubMed] [Google Scholar]
- 9.Eguchi Y, Jinde M, Murooka K, Konno Y, Ohta M, Yamato H. Stretching versus transitory icing: which is the more effective treatment for attenuating muscle fatigue after repeated manual labor? Eur J Appl Physiol. 2014;114:2617–2623. doi: 10.1007/s00421-014-2983-x. [DOI] [PubMed] [Google Scholar]
- 10.Ellenbecker TS, Mattalino AJ. Concentric isokinetic shoulder internal and external rotation strength in professional baseball pitchers. J Orthop Sports Phys Ther. 1997;25:323–328. doi: 10.2519/jospt.1997.25.5.323. [DOI] [PubMed] [Google Scholar]
- 11.Erickson BJ, Chalmers PN, Axe MJ, Romeo AA (2017) Exceeding pitch count recommendations in little league baseball increases the chance of requiring Tommy John surgery as a professional baseball pitcher. Orthop J Sport Med 5 [DOI] [PMC free article] [PubMed]
- 12.Erickson BJ, Chalmers PN, Bush-Joseph CA, Romeo AA (2016) Predicting and preventing injury in Major League Baseball. Am J Orthop (Belle Mead NJ). [PubMed]
- 13.Erickson BJ, Nwachukwu BU, Rosas S, Schairer WW, McCormick FM, Bach BR, Bush-Joseph CA, Romeo AA. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43:1770–1774. doi: 10.1177/0363546515580304. [DOI] [PubMed] [Google Scholar]
- 14.Fleisig GS, Andrews JR. Prevention of elbow injuries in youth baseball pitchers. Sports Health. 2012;4:419–424. doi: 10.1177/1941738112454828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fleisig GS, Andrews JR, Cutter GR, Weber A, Loftice J, McMichael C, Hassell N, Lyman S. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39:253–257. doi: 10.1177/0363546510384224. [DOI] [PubMed] [Google Scholar]
- 16.Fouré A, Nordez A, Cornu C. Plyometric training effects on Achilles tendon stiffness and dissipative properties. J Appl Physiol. 2010;109:849–854. doi: 10.1152/japplphysiol.01150.2009. [DOI] [PubMed] [Google Scholar]
- 17.Freehill MT, Archer KR, Diffenderfer BW, Ebel BG, Cosgarea AJ, Mcfarland EG. Changes in collegiate starting pitchers’ range of motion after single game and season. Phys Sportsmed. 2014;42:69–74. doi: 10.3810/psm.2014.02.2049. [DOI] [PubMed] [Google Scholar]
- 18.Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of medial ulnar collateral ligament reconstruction. Am J Sports Med. 2016;44:729–734. doi: 10.1177/0363546515622407. [DOI] [PubMed] [Google Scholar]
- 19.Impellizzeri FM, Ward P, Coutts AJ, Bornn L, McCall A. Training load and injury: part 2—questionable research practices hijack the truth and mislead well-intentioned clinicians. J Orthop Sport Phys Ther. 2020;0:1–17. doi: 10.2519/jospt.2020.9211. [DOI] [PubMed] [Google Scholar]
- 20.Issurin VB (2010) New horizons for the methodology and physiology of training periodization. Sport Med [DOI] [PubMed]
- 21.Jamurtas AZ, Fatouros IG, Buckenmeyer P, Kokkinidis E, Taxildaris K, Kambas A, Kyriazis G. Effects of plyometric exercise on muscle soreness and plasma creatine kinase levels and its comparison with eccentric and concentric exercise. J Strength Cond Res. 2000;14:68–74. [Google Scholar]
- 22.Kageyama M, Sugiyama T, Takai Y, Kanehisa H, Maeda A. Kinematic and kinetic profiles of trunk and lower limbs during baseball pitching in collegiate pitchers. J Sport Sci Med. 2014;13:742–750. [PMC free article] [PubMed] [Google Scholar]
- 23.Kantrowitz DE, Trofa DP, Woode DR, Ahmad CS, Lynch TS (2018) Athletic hip injuries in Major League Baseball pitchers associated with ulnar collateral ligament tears. Orthop J Sport Med 6 [DOI] [PMC free article] [PubMed]
- 24.Keller RA, De Giacomo AF, Neumann JA, Limpisvasti O, Tibone JE. Glenohumeral internal rotation deficit and risk of upper extremity injury in overhead athletes: a meta-analysis and systematic review. Sports Health SAGE Publications Inc. 2018;10:125–132. doi: 10.1177/1941738118756577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ben KW, Press J, Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36:189–198. doi: 10.2165/00007256-200636030-00001. [DOI] [PubMed] [Google Scholar]
- 26.Ben KW, Sciascia A, Moore S. An acute throwing episode decreases shoulder internal rotation. Clin Orthop Relat Res, pp. 2012:1545–51. [DOI] [PMC free article] [PubMed]
- 27.• Kubo K, Ishigaki T, Ikebukuro T (2017) Effects of plyometric and isometric training on muscle and tendon stiffness in vivo. Physiol Rep 5. Results suggest that plyometric training (but not isometric training) enhances the extensibility of tendon structures during ballistic contractions and active muscle stiffness during fast stretching. [DOI] [PMC free article] [PubMed]
- 28.Lazu AL, Love SD, Butterfield TA, English R, Uhl TL. The relationship between pitching volume and arm soreness in collegiate baseball pitchers. Int J Sports Phys Ther. 2019;14:97–106. doi: 10.26603/ijspt20190097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mahure SA, Mollon B, Shamah SD, Kwon YW, Rokito AS. Disproportionate trends in ulnar collateral ligament reconstruction: projections through 2025 and a literature review. J Shoulder Elb Surg Mosby Inc. 2016;25:1005–1012. doi: 10.1016/j.jse.2016.02.036. [DOI] [PubMed] [Google Scholar]
- 30.Maupin D, Schram B, Canetti E, Orr R. The relationship between acute: chronic workload ratios and injury risk in sports: a systematic review. Open Access J Sport Med Volume. 2020;11:51–75. doi: 10.2147/OAJSM.S231405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.•• Mujika I, Halson S, Burke LM, Balagué G, Farrow D (2018) An integrated, multifactorial approach to periodization for optimal performance in individual and team sports. Int. J. Sports Physiol. Perform. Review of the available evidence related to integrated periodization with particular focus on exercise training, recovery, nutrition, psychological skills, and skill acquisition. [DOI] [PubMed]
- 32.Olsen SJ, Fleisig GS, Dun S, Loftice J, Andrews JR. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34:905–912. doi: 10.1177/0363546505284188. [DOI] [PubMed] [Google Scholar]
- 33.Provencher CDRMT, Makani A, McNeil JW, Pomerantz ML, Golijanin P, Gross D (2014) The role of the scapula in throwing disorders. Sports Med Arthrosc [DOI] [PubMed]
- 34.Reiman MP, Walker MD, Peters S, Kilborn E, Thigpen CA, Garrigues GE (2019) Risk factors for ulnar collateral ligament injury in professional and amateur baseball players: a systematic review with meta-analysis. J Shoulder Elb Surg [DOI] [PubMed]
- 35.Richendollar ML, Darby LA, Brown TM. Ice bag application, active warm-up, and 3 measures of maximal functional performance. J Athl Train. 2006;41:364–370. [PMC free article] [PubMed] [Google Scholar]
- 36.Saito M, Kenmoku T, Kameyama K, Murata R, Yusa T, Ochiai N, Kijima T, Takahira N, Fukushima K, Ishige N, Takaso M. Relationship between tightness of the hip joint and elbow pain in adolescent baseball players. Orthop J Sport Med. 2014;2:1–6. doi: 10.1177/2325967114532424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sakata J, Nakamura E, Suzuki T, Suzukawa M, Akaike A, Shimizu K, Hirose N. Efficacy of a prevention program for medial elbow injuries in youth baseball players. Am J Sports Med. 2018;46:460–469. doi: 10.1177/0363546517738003. [DOI] [PubMed] [Google Scholar]
- 38.•• Sakata J, Nakamura E, Suzuki T, Suzukawa M, Akeda M, Yamazaki T, Ellenbecker TS, Hirose N (2019) Throwing injuries in youth baseball players: can a prevention program help? A randomized controlled trial. Am J Sports Med 47:2709–2716. Randomized controlled trial demonstrating that a prevention program decreases throwing injuries of the shoulder and elbow and enhances the parameter of pitching performance in 237 youth baseball players ages 9–11. [DOI] [PubMed]
- 39.Saper MG, Pierpoint LA, Liu W, Comstock RD, Polousky JD, Andrews JR. Epidemiology of shoulder and elbow injuries among United States high school baseball players: school years 2005-2006 through 2014-2015. Am J Sports Med. 2018;46:37–43. doi: 10.1177/0363546517734172. [DOI] [PubMed] [Google Scholar]
- 40.Saw AE, Main LC, Gastin PB. Monitoring the athlete training response: subjective self-reported measures trump commonly used objective measures: a systematic review. Br J Sports Med. 2016;50:281–291. doi: 10.1136/bjsports-2015-094758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scarborough DM, Bassett AJ, Mayer LW, Berkson EM. Kinematic sequence patterns in the overhead baseball pitch. Sport Biomech. 2020;19:569–586. doi: 10.1080/14763141.2018.1503321. [DOI] [PubMed] [Google Scholar]
- 42.• Shitara H, Yamamoto A, Shimoyama D, Ichinose T, Sasaki T, Hamano N, Ueno A, Endo F, Oshima A, Sakane H, Tachibana M, Tomomatsu Y, Tajika T, Kobayashi T, Osawa T, Iizuka H, Takagishi K (2017) Shoulder stretching intervention reduces the incidence of shoulder and elbow injuries in high school baseball players: a time-to-event analysis. Sci Rep 7. Non-randomized prospective evaluation of the effects of a prevention program on the incidence of shoulder and elbow injuries in high school baseball pitchers with that demonstrated decreased injury incidence with regular stretching and potentially strengthening. [DOI] [PMC free article] [PubMed]
- 43.Singh DP, Lonbani ZB, Woodruff MA, Parker TJ, Steck R, Peake JM. Effects of topical icing on inflammation, angiogenesis, revascularization, and myofiber regeneration in skeletal muscle following contusion injury. Front Physiol. 2017;8. [DOI] [PMC free article] [PubMed]
- 44.Thain PK, Bleakley CM, Mitchell ACS. Muscle reaction time during a simulated lateral ankle sprain after wet-ice application or cold-water immersion. J Athl Train. 2015;50:697–703. doi: 10.4085/1062-6050-50.4.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tipton MJ, Collier N, Massey H, Corbett J, Harper M. Cold water immersion: kill or cure? Exp Physiol. 2017;102:1335–1355. doi: 10.1113/EP086283. [DOI] [PubMed] [Google Scholar]
- 46.Tofas T, Jamurtas AZ, Fatouros I, Nikolaidis MG, Koutedakis Y, Slnouris EA, Papageorgakopoulou N, Theocharis DA. Plyometric exercise increases serum indices of muscle damage and collagen breakdown. J Strength Cond Res. 2008;22:490–496. doi: 10.1519/JSC.0b013e31816605a0. [DOI] [PubMed] [Google Scholar]
- 47.Tseng CY, Lee JP, Tsai YS, Da Lee S, Kao CL, Liu TC, Lai CH, Harris MB, Kuo CH. Topical cooling (icing) delays recovery from eccentric exercise-induced muscle damage. J Strength Cond Res. 2013;27:1354–1361. doi: 10.1519/JSC.0b013e318267a22c. [DOI] [PubMed] [Google Scholar]
- 48.Tyler TF, Mullaney MJ, Mirabella MR, Nicholas SJ, McHugh MP. Risk factors for shoulder and elbow injuries in high school baseball pitchers: the role of preseason strength and range of motion. Am J Sports Med, pp. 2014;42:1993–1999. doi: 10.1177/0363546514535070. [DOI] [PubMed] [Google Scholar]
- 49.Versey NG, Halson SL, Dawson BT. Water immersion recovery for athletes: effect on exercise performance and practical recommendations. Med: Sport; 2013. [DOI] [PubMed] [Google Scholar]
- 50.Webb NP. The use of post-game recovery modalities following team contact sport: a review. J Aust Strength Cond. 2013;21:70–79. [Google Scholar]
- 51.Whiteside D, Martini DN, Lepley AS, Zernicke RF, Goulet GC. Predictors of ulnar collateral ligament reconstruction in major league baseball pitchers. Am J Sports Med. 2016;44:2202–2209. doi: 10.1177/0363546516643812. [DOI] [PubMed] [Google Scholar]
- 52.Wilk KE, Andrews JR, Arrigo CA, Keirns MA, Erber DJ. The strength characteristics of internal and external rotator muscles in professional baseball pitchers. Am J Sports Med. 1993;21:61–66. doi: 10.1177/036354659302100111. [DOI] [PubMed] [Google Scholar]
- 53.Wilk KE, MacRina LC, Fleisig GS, Aune KT, Porterfield RA, Harker P, Evans TJ, Andrews JR. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: a prospective study. Am J Sports Med. 2014;42:2075–2081. doi: 10.1177/0363546514538391. [DOI] [PubMed] [Google Scholar]
- 54.Zaremski JL, Zeppieri G, Jones DL, Tripp BL, Bruner M, Vincent HK, Horodyski M. Game-day pitch counts in high school baseball pitchers—an observational study. Orthop J Sport Med. 2018;6:232596711876525. doi: 10.1177/2325967118765255. [DOI] [PMC free article] [PubMed] [Google Scholar]