Abstract
Objective
A meta-analysis to investigate the risk factors for postoperative hypocalcaemia after thyroidectomy in adult patients.
Methods
A systematic search of publications in the electronic databases (PubMed®, The Cochrane Library, Web of Science, OVID and Embase®) from inception to June 2020 was conducted. Screening of titles, abstracts and full texts and data extraction were independently performed by two authors. The OR was selected as the pooled estimate.
Results
The analysis included 23 studies. Twelve significant risk factors for postoperative hypocalcaemia were identified: hypoparathyroidism, OR 5.58; total thyroidectomy, OR 3.59; hypomagnesaemia, OR 2.85; preoperative vitamin D deficiency, OR 2.32; female sex, OR 1.49; thyroid malignancy, OR 1.85; thyroiditis, OR 1.48; substernal multinodular goitres, OR 1.70; parathyroidectomy, OR 1.58; central compartment neck dissection, OR 1.17; modified radical neck dissection, OR 1.57; and central neck dissection, OR 1.54.
Conclusions
This meta-analysis provides moderate-to-high quality evidence that the 12 risk factors were predictive of postoperative hypocalcaemia, which should be monitored closely before thyroidectomy.
Keywords: Thyroid, prevalence, risk factor, hypocalcaemia, meta-analysis
Introduction
Thyroidectomy consists of total thyroidectomy (TT) and subtotal thyroidectomy. Although a widely used and relatively safe procedure, subsequent major complications such as incidental parathyroidectomy during thyroid resection, postoperative haemorrhage, hypocalcaemia and recurrent laryngeal nerve injury can threaten the postoperative quality of life of patients.1,2 Hypocalcaemia is the most common postoperative complication after thyroidectomy, with an overall prevalence of 7–51%.3,4 The prevalence of hypocalcaemia 6 months after surgery is 3.6% and the prevalence of permanent hypocalcaemia is 1.5–4%.5,6 However, what matters most to the patients is not only quality of life, but also prolonged hospital stays and an unfavourable prognosis.7Recent studies have identified various risk factors for postoperative hypocalcaemia, including perioperative parathyroid hormone (PTH) levels, incidental parathyroidectomy during thyroid resection, as well as postoperative vitamin D and magnesium levels.8–10 However, these studies have presented inconsistent findings as a consequence of study limitations such as the research subject, study design and sample size.11,12
This current meta-analysis aimed to summarize the most relevant risk factors, which can also be considered as predictive biomarkers, for postoperative hypocalcaemia after thyroidectomy in adult patients. It also aimed to estimate, if possible, the strength of any association between identified predictors and post-thyroidectomy hypocalcaemia.
Materials and methods
Search strategy
A systematic search of publications in the electronic databases (PubMed®, The Cochrane Library, Web of Science, OVID and Embase®) from inception to June 2020 was conducted. The search terms included: “thyroidectomy” or “thyroid resection” or “thyroid surgery” and “hypocalc*” or “low calcium” and “risk factors” or “influencing factors” and “association factors”. For PubMed®, the search terms included: “thyroidectomy or postoperative thyroidectomy or thyroid surgery” and “hypocalcemia or low calcium” and “risk factors or influencing factors or association factors”. As a consensus on the definition of hypocalcaemia had not been reached, all types of hypocalcaemia were included in the outcome indicators. Recent studies categorized hypocalcaemia into transient and permanent hypocalcaemia, or into biochemical and symptomatic hypocalcaemia. If transient and permanent hypocalcaemia were reported in an original study, the data on transient hypocalcaemia were extracted for analysis. If biochemical hypocalcaemia and symptomatic hypocalcaemia were reported in one of the original studies, the data on symptomatic hypocalcaemia were extracted for analysis. Biochemical hypocalcaemia was defined as serum calcium levels <2.0 mmol/l. Hypocalcaemia with concomitant symptoms in the extremities including numbness of hands, feet and mouth, muscle tremors, convulsion, arrhythmia, as well as Chvostek’s and Trousseau’s signs was defined as symptomatic hypocalcaemia. However, there was no generally accepted definitions of transient and permanent hypocalcaemia. Therefore, studies were included irrespective of the definitions. Only studies published in English were considered for inclusion.
Study selection
Studies were eligible for inclusion if they met the following criteria: (i) studies that enrolled patients > 18 years of age that received thyroidectomy and had no other complications; (ii) randomized control trials or observational studies on risk factors of hypocalcaemia after thyroidectomy; (iii) odds ratio (OR) values and the corresponding 95% confidence intervals (CIs) were directly provided or could be calculated indirectly. The exclusion criteria were as follows: (i) single case reports, reviews, video or multimedia literature; (ii) animal experiments; (iii) technique reports; (iv) duplicate reports; (v) articles written in non-English languages; (vi) studies lacking original data; (vii) studies with a sample size < 30.
Data extraction and quality assessment
Titles and abstracts were imported into Covidence, an established online screening and data extraction tool, and were independently screened for eligibility by two authors (Z.C. & Q.Z.). Any disagreement was resolved by discussion or the arbitration of a third author (J.D.) . Review of each candidate full text was undertaken by two authors (Y.W. & C.X.). Bibliographies of included studies were hand searched to include eligible studies. Two authors (R.H. & X.C.) independently extracted the following study data using a standardized Microsoft Excel form: study type and country, sample size, definition of postoperative hypocalcaemia and hypocalcaemia-related outcomes. Study quality was assessed using the Newcastle–Ottawa Scale (NOS) checklist.13 Studies that scored ≥7 stars (out of 9 stars) were considered to be of high quality, those with scores of 5–6 stars were of moderate quality and those that scored < 5 stars were of low quality.14
Statistical analyses
Data analysis was performed using RevMan software (version 5.3; Cochrane Collaboration, Oxford, UK). The OR was selected as the pooled estimate. The between-study heterogeneity was assessed using I2 statistics and Q statistics. A meta-analysis was performed when two or more studies reported a risk factor for postoperative hypocalcaemia after thyroidectomy. In the meta-analysis, a fixed-effects model was used when there was nonsignificant between-study heterogeneity (I2 < 50% and P > 0.1); otherwise, a random-effects model was employed (I2 > 50% and P < 0.1). The OR estimates are presented in forest plots. The presence of publication bias was evaluated via funnel plots and Egger’s test.
Results
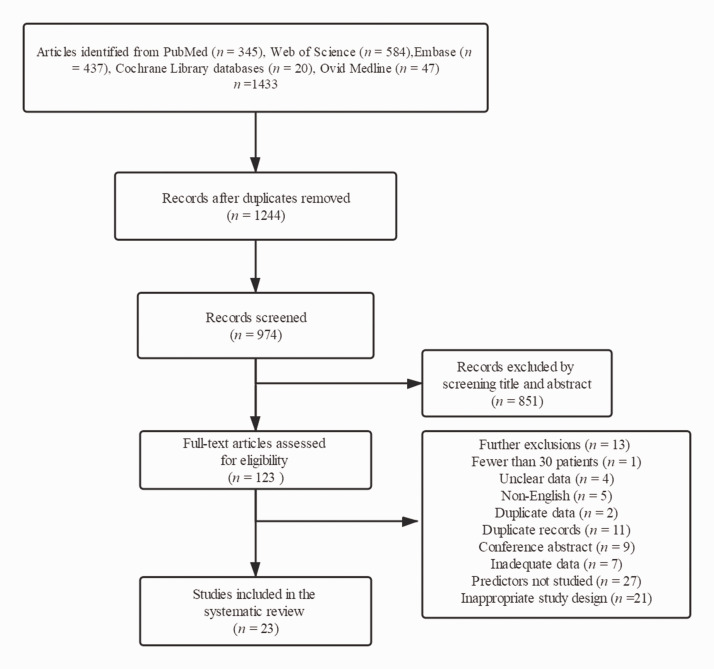
Initial searches identified 1433 unique papers. After removing duplicates and screening titles and abstracts, 123 studies remained for full-text analysis. A total of 23 studies that enrolled 877 356 participants were included for study quality assessment.3,9,10,15–34 The study selection procedure is presented in the flow chart (Figure 1). Of the included studies, three were prospective cohort studies, nine were retrospective cohort studies, 10 were retrospective case studies and one study was a retrospective cross-sectional analysis.3,9,10,15–34 Eight studies were conducted in European countries, 12 in Asian countries and three in the USA. The characteristics of the included studies are presented in Table 1.3,9,10,15–34
Figure 1.
Flow diagram of eligible studies showing the number of citations identified, retrieved and included in the final meta-analysis.
Table 1.
Characteristics of the 23 studies included in a meta-analysis to evaluate the risk factors for postoperative hypocalcaemia after thyroidectomy in adult patients.3,9,10,15–34
| Author | Country | Study design | Patientsn | Rate of postoperative hypocalcaemia, % | NOS score | Risk factors |
|---|---|---|---|---|---|---|
| Liu et al., 202015 | USA | Retrospective cross-sectional analysis | 126 766 | 30-day follow-up after surgery: 19.1% | 7 | Age, female, vitamin D deficiency, concurrent lateral neck dissection, concurrent central neck dissection, intraoperative parathyroid, recurrent laryngeal nerve injury, magnesium disorders |
| 1-year follow-up after surgery: 4.4% | ||||||
| Lale et al., 201916 | Turkey | Retrospective case control | 818 | Permanent hypocalcaemia (>1 year): 26.7% | 6 | Female, specimen weight, substernal localization, cervical lymph node dissection (CLND) |
| Transient hypocalcaemia (calcium level <8 mg/dl at 24 and 72 h after thyroidectomy): 1.7% | ||||||
| Carvalho et al., 201917 | Brazil | Retrospective cohort study | 1347 | Hypocalcaemia: 21% | 6 | Neck dissection, malignancy, sex, age, preoperative total calcium, preoperative parathyroid hormone (PTH); preoperative vitamin D, central compartment dissection |
| Wang W et al., 201918 | China | Retrospective cohort study | 242 | Hypocalcaemia: 60% | 6 | Sex, extent of surgery, hypoparathyroidism, lymph node dissection, hypomagnesemia, preoperative calcium |
| Falch et al., 201819 | Germany | Retrospective case study | 702 | Postoperative biochemical hypocalcaemia (48 h): 22.8% | 5 | Symptomatic hypocalcaemia, female, parathyroid reimplantation, surgery time (≥189 min), thyreostatic drug therapy |
| Persistent biochemical hypocalcaemia (>6 months): 6.8% | ||||||
| Docimo et al., 20179 | Italy | Retrospective case control | 328 | Symptomatic hypocalcaemia: 7.9% | 7 | Malignant pathology, central compartment neck dissection (CCND) |
| Transient hypocalcaemia: 14.6% | ||||||
| Permanent hypocalcaemia: 0.6% | ||||||
| Luo et al., 201720 | China | Retrospective case control | 304 | Biochemical hypocalcaemia: 26.9% | 5 | Female, postoperative hypomagnesaemia, postoperative iPTH < 1.6 pmol/l, relative decline of iPTH > 70% |
| Symptomatic hypocalcaemia: not reported | ||||||
| Wang X et al., 201721 | China | Retrospective case control | 237 | Biochemical hypocalcaemia: 52.3% | 6 | Bilateral CCND, modified radical neck dissection (MRND), parathyroid gland autotransplantation, hypoparathyroidism, hypomagnesaemia |
| Symptomatic hypocalcaemia: 33.8% | ||||||
| Cho et al., 201622 | Korea | Retrospective cohort study | 1030 | Transient hypocalcaemia: 28.2% | 6 | Age, female, central neck dissection (CND), MRND, extent of CND (bilateral), operation time, implant of parathyroid gland, parathyroid gland in pathology |
| Permanent hypocalcaemia: 2.6% | ||||||
| Nellis et al., 201623 | USA | Retrospective cohort study | 620 744 | Hypocalcaemia 6% | 8 | Magnesium disorder, phosphate disorder, female, age, Medicaid payor status, thyroid cancer, total thyroidectomy, neck dissection, recurrent laryngeal nerve injury, high-volume surgeon |
| Garrahy et al., 201610 | Ireland | Retrospective cohort study | 201 | Biochemical hypocalcaemia: 22.9% | 7 | Cancer diagnosis, central neck dissection, hypomagnesaemia, inadvertent parathyroid resection |
| Symptomatic hypocalcaemia: 12.4% | ||||||
| Bove et al., 201624 | Italy | Retrospective cohort study | 142 | Temporary hypocalcaemia: 33% | 6 | Substernal goitre |
| Permanent hypocalcaemia: 2.8% | ||||||
| Lee et al., 201525 | Korea | Retrospective case study | 134 | Laboratory preoperative calcaemia: 39% | 6 | Age, female, body mass index, preoperative calcium, preoperative PTH, vitamin D (< 20 ng/ml), vitamin D (< 10 ng/ml), selective neck dissection, incidental parathyroidectomy |
| Symptomatic preoperative calcaemia: 19% | ||||||
| Al-Khatib et al., 201526 | Saudi Arabia | Retrospective cohort study. | 213 | Laboratory hypocalcaemia: 19.7% | 6 | Postoperative serum PTH, preoperative serum 25(OH)D < 25 nmol/l |
| Clinical hypocalcaemia: 17.8% | ||||||
| Praženica et al., 201527 | Ireland | Prospective cohort study | 788 | Temporary hypocalcaemia: 23.9% | 8 | Sex, age, preoperative diagnosis benign, biclamp haemostasis, thyroid gland weight, substernal extension, tracheal deviation, operation time, multinodular goitre, Graves’ disease, Hashimoto thyroiditis, thyroid cancer, incidental parathyroidectomy |
| Symptomatic hypocalcaemia: 14.0% | ||||||
| Diez et al., 201328 | Spain | Prospective cohort study | 113 | Hypocalcaemia: 38.90% | 6 | Preoperative vitamin D < 15 ng/ml, postoperative PTH < 13 pg/ml |
| Baldassarre et al., 201229 | USA | Retrospective case study | 118 375 | Hypocalcaemia: 5.50% | 8 | Age, female, ethnicity, Hispanic, Asian or Pacific islander, native American, total thyroidectomy, thyroidectomy with unilateral neck dissection, thyroidectomy with bilateral neck dissection, complete substernal thyroidectomy, partial substernal thyroidectomy, substernal thyroidectomy, isthmectomy, partial thyroidectomy, length of stay (per day), nonteaching hospital, malignant neoplasm of thyroid gland |
| Turanli et al., 200930 | Turkey | Retrospective cohort study | 417 | Permanent hypocalcaemia: 7.7% | 7 | Incidental parathyroidectomy, extrathyroidal soft tissue invasion |
| Erbil et al., 200931 | Turkey | Prospective cohort study | 200 | Symptomatic hypocalcaemia: 73% | 6 | Age (> 50 years); preoperative serum 25-OHD level < 15 ng/ml |
| Asymptomatic hypocalcaemia: 27% | ||||||
| Wang Y et al., 201732 | China | Retrospective case study | 278 | Hypocalcaemia: 27.30% | 8 | Age (years), lateral lymph node dissection, lobectomy plus isthmusectomy versus lobectomy, near-total thyroidectomy versus lobectomy, total thyroidectomy versus lobectomy, injected versus non-injected, female, preoperative PTH levels |
| Aqtashi et al., 201733 | Switzerland | Retrospective cohort study | 34 | Hypocalcaemia: 33% | 6 | Operation interval, preoperative PTH, preoperative calcium |
| Lin et al., 20173 | Taiwan | Retrospective case study | 3186 | Hypocalcaemia: 30.90% | 7 | Age, female, multituberous goitre, Graves’ disease, malignant tumours, total thyroidectomy, reoperation, central cervical lymph node, thyroid malignancy |
| Tongol et al., 201634 | Philippines | Retrospective case study | 242 | Symptomatic hypocalcaemia: 10.74% | 7 | Age, sex, thyroid disease (toxic, nontoxic or malignant), thyroid gland weight in grams, presence concomitant complication of thyroidectomy Hoarseness and/or haematoma, type of surgery (total thyroidectomy), neck dissection, duration of surgery in hours, inadvertent parathyroidectomy |
| Asymptomatic hypocalcaemia: 1.24% |
NOS, Newcastle–Ottawa Scale.
The quality of all included studies was assessed using the NOS, of which 10 studies were rated as high quality (four with 8 stars and six with 7 stars) and 13 studies were rated as moderate quality (11 with 6 stars and two with 5 stars) (Table 1).3,9,10,15–34
According to the heterogeneity for the meta-analyses on preoperative vitamin D levels (I2 = 74%, P = 0.010), preoperative PTH (I2 = 92%, P < 0.0001) and preoperative calcium levels (I2= 79%, P < 0.0009), a random-effects model was used for the meta-analyses. According to the heterogeneity for the meta-analyses on sex (I2 = 49%, P = 0.03), age (I2 = 33%, P = 0.18), Graves’ diseases (I2= 42%, P = 0.19), hypomagnesaemia (I 2= 0.00%, P = 0.57), hypothyroidism (I2 = 30%, P < 0.23), thyroid malignant tumour (I2 = 0.00%, P < 0.43), thyroiditis (I2 = 0.00%, P < 0.47), TT (I2= 0.00%, P < 0.55), modified radical neck dissection (MRND) (I2 = 28%, P < 0.16), incidental parathyroidectomy (I2 = 0.00%, P = 0.41), multiple thyroid nodules (I2 = 2%, P < 0.31), central compartment neck dissection (CCND) (I2 = 26%, P < 0.23) and operative time (I2 = 0.00%, P < 0.63), a fixed-effects model was used for the meta-analyses.
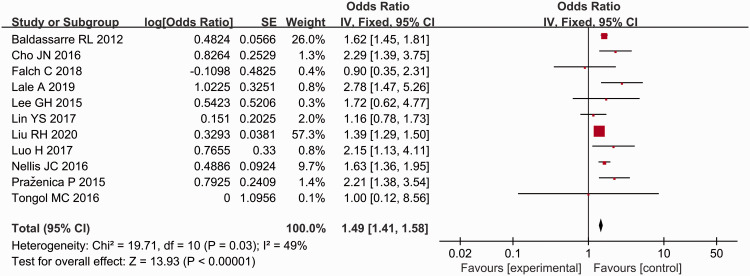
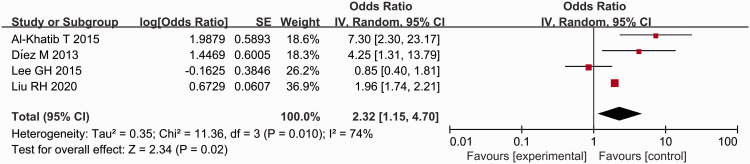
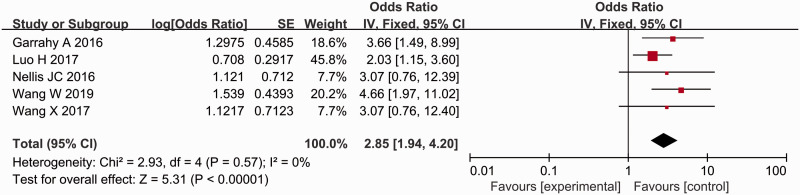
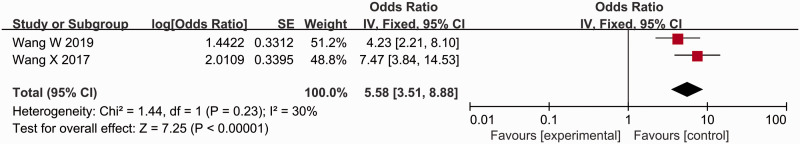
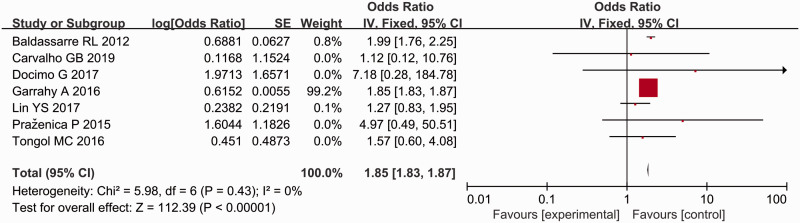
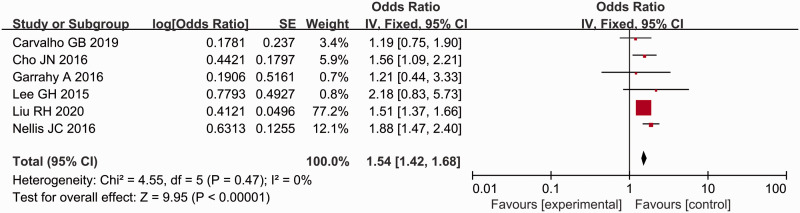
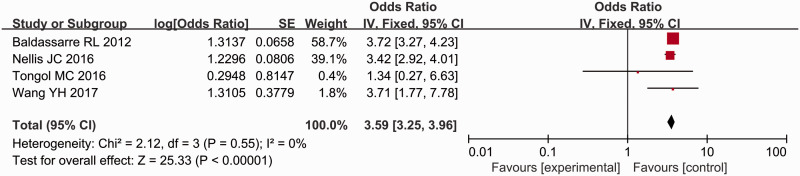
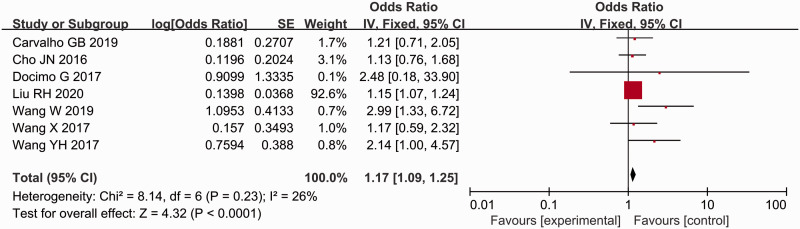
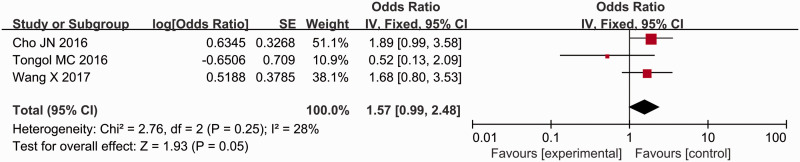
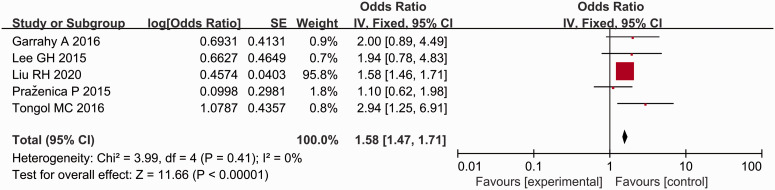
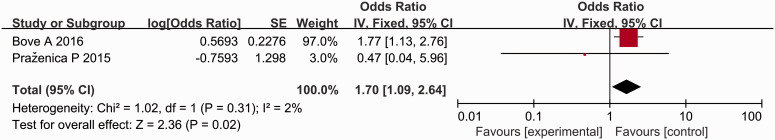
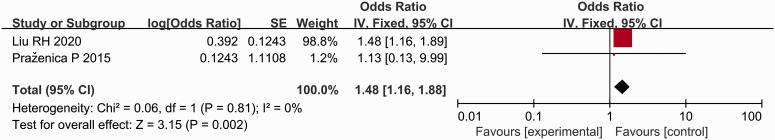
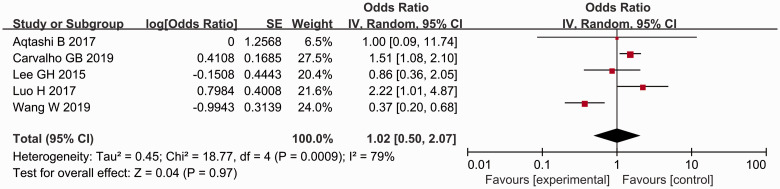
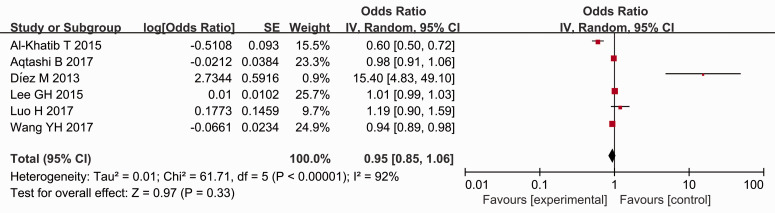
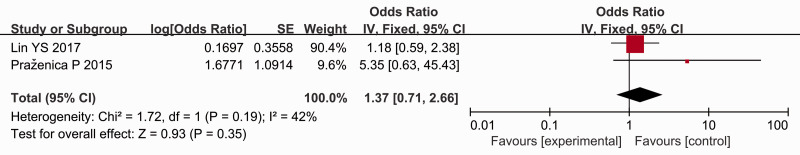
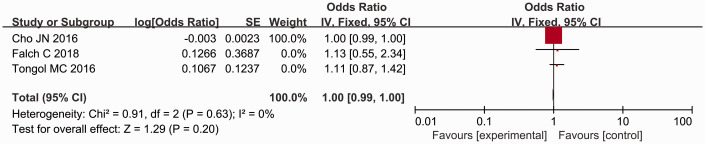
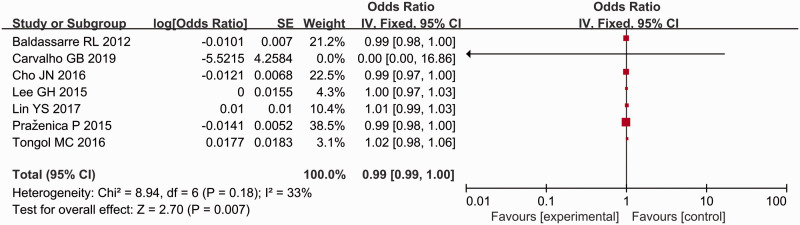
A total of 23 studies were included;3,9,10,15–34 and of these, 11 analysed the influence of sex (female) on postoperative thyroid function.3,15,16,19,20,22,23,25,27,29,34 The results showed that the incidence of postoperative hypocalcaemia in female patients was significantly higher than that in male patients (P < 0.00001, OR = 1.49, 95% CI 1.41, 1.58) (Figure 2). Four studies analysed the influence of preoperative vitamin D on postoperative thyroid function.15,25,26,28 Patients with a preoperative vitamin D level < 20 ng/ml were at a higher risk for postoperative hypocalcaemia (P = 0.02, OR = 2.32, 95% CI 1.15, 4.70) (Figure 3). Five studies analysed the influence of hypomagnesaemia on postoperative thyroid function.10,18,20,21,23 The incidence of postoperative hypocalcaemia after thyroidectomy was higher in patients with hypomagnesaemia (P < 0.00001, OR = 2.85, 95% CI 1.94, 4.20) (Figure 4). The meta-analysis including two studies on hypoparathyroidism demonstrated that the patients with hypoparathyroidism had a higher incidence of postoperative hypocalcaemia (P < 0.00001, OR = 5.58, 95% CI 3.51, 8.88) (Figure 5).18,21 Seven studies analysed the influence of malignant thyroid surgery.3,9,10,17,27,29,34 Patients receiving malignant thyroid surgery showed a higher risk of postoperative hypocalcaemia (P < 0.00001, OR = 1.85, 95% CI 1.83, 1.87) (Figure 6). Six studies analysed the influence of central neck dissection (CND).10,15,17,22,23,25 Patients experiencing CND showed a higher risk of postoperative hypocalcaemia (P < 0.00001, OR = 1.54, 95% CI 1.42, 1.68) (Figure 7). Four studies analysed the influence of TT.23,29,32,34 Patients that underwent TT showed a higher risk of postoperative hypocalcaemia (P < 0.00001, OR = 3.59, 95% CI 3.25, 3.96) (Figure 8). Seven studies analysed the influence of CCND.9,15,17,18,21,22,32 Patients that underwent CCND showed a higher risk of postoperative hypocalcaemia (P < 0.0001, OR = 1.17, 95% CI 1.09, 1.25) (Figure 9). Three studies analysed the influence of MRND.21,22,34 Patients that underwent MRND showed a higher risk of postoperative hypocalcaemia (P < 0.05, OR = 1.57, 95% CI 0.99, 2.48) (Figure 10). Five studies analysed the influence of incidental parathyroid resection.10,15,25,27,34 Patients that experienced incidental parathyroid resection showed a higher risk of postoperative hypocalcaemia (P < 0.00001, OR = 1.58, 95% CI 1.47, 1.71) (Figure 11). Two studies analysed the influence of substernal multinodular goitres.24,27 Patients with substernal multinodular goitres showed a higher risk of postoperative hypocalcaemia (P = 0.02, OR = 1.70, 95% CI 1.09, 2.64) (Figure 12). Two studies analysed the influence of thyroiditis.15,27 Patients with thyroiditis showed a higher risk of postoperative hypocalcaemia (P = 0.002, OR = 1.48, 95% CI 1.16, 1.88) (Figure 13).
Figure 2.
Forest plot of a meta-analysis to evaluate the relationship between female sex and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.3,15,16,19,20,22,23,25,27,29,34
Figure 3.
Forest plot of a meta-analysis to evaluate the relationship between preoperative vitamin D and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.15,25,26,28
Figure 4.
Forest plot of a meta-analysis to evaluate the relationship between hypomagnesaemia and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.10,18,20,21,23
Figure 5.
Forest plot of a meta-analysis to evaluate the relationship between hypoparathyoidism and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.18,21
Figure 6.
Forest plot of a meta-analysis to evaluate the relationship between thyroid malignancy and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.3,9,10,17,27,29,34
Figure 7.
Forest plot of a meta-analysis to evaluate the relationship between central neck dissection and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.10,15,17,22,23,25
Figure 8.
Forest plot of a meta-analysis to evaluate the relationship between total thyroidectomy and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.23,29,32,34
Figure 9.
Forest plot of a meta-analysis to evaluate the relationship between central compartment neck dissection and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.9,15,17,18,21,22,32
Figure 10.
Forest plot of a meta-analysis to evaluate the relationship between modified radical neck dissection and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.21,22,34
Figure 11.
Forest plot of a meta-analysis to evaluate the relationship between incidental parathyroidectomy and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.10,15,25,27,34
Figure 12.
Forest plot of a meta-analysis to evaluate the relationship between substernal multinodular goitre and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.24,27
Figure 13.
Forest plot of a meta-analysis to evaluate the relationship between thyroiditis and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.15,27
There was no significant association between the risk of postoperative hypocalcaemia and preoperative calcium levels, preoperative PTH levels, Graves' disease, surgery time and age (Figures 14, 15, 16, 17, 18).
Figure 14.
Forest plot of a meta-analysis to evaluate the relationship between preoperative calcium level and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.17,18,20,25,33
Figure 15.
Forest plot of a meta-analysis to evaluate the relationship between preoperative parathyroid hormone and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.20,25,26,28,32,33
Figure 16.
Forest plot of a meta-analysis to evaluate the relationship between Graves’ disease and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.3,27
Figure 17.
Forest plot of a meta-analysis to evaluate the relationship between surgery time and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.19,22,34
Figure 18.
Forest plot of a meta-analysis to evaluate the relationship between age and the risk for postoperative hypocalcaemia after thyroidectomy in adult patients. CI, confidence interval.3,17,22,25,27,29,34
Funnel plots (see supplementary materials, Figure 19) and Egger’s regression test (see supplementary materials, Figure 20) were used to examine if publication bias existed. The results demonstrated that no publication bias existed for other markers and measurement outcomes.
Discussion
This current meta-analysis, which systematically reviewed 23 studies and analysed non-overlapping data from 877 356 participants, identified 12 risk factors for postoperative hypocalcaemia after thyroidectomy, including female sex, preoperative vitamin D deficiency, hypomagnesaemia, hypoparathyroidism, thyroid malignancies, thyroiditis, substernal multinodular goitres, parathyroidectomy, total thyroidectomy, CCND, MRND and CND. Among them, hypoparathyroidism, total thyroidectomy, hypomagnesaemia, and preoperative vitamin D deficiency were the most important risk factors. In contrast, age, preoperative PTH levels, preoperative calcium levels, Graves’ disease and surgery time were not significantly associated with the risk of postoperative hypocalcaemia.
Hypoparathyroidism has been confirmed as an independent risk factor for hypocalcaemia after thyroid surgery because the function of the parathyroid gland directly affects serum calcium levels.17,20 Damage to the parathyroid gland may be primarily due to the anatomical location of the parathyroid gland. Most parathyroid glands are located at the posterior margin of the lateral lobe of the thyroid in the loose connective tissue between the true and false capillaries. The blood supply of the parathyroid gland comes from the inferior thyroid artery and its anastomotic branch with the superior thyroid artery. However, 80% of the inferior thyroid artery is the only blood vessel supplying the parathyroid gland. The parathyroid gland may be damaged if the inferior thyroid artery is ligated near the inferior pole of the thyroid gland or if vascular spasm is caused by careless surgical procedures. This meta-analysis demonstrated that the worse the parathyroid gland function is, the higher the incidence of postoperative hypocalcaemia will be. Since all included studies on hypoparathyroidism were from Asia,18,21 more studies conducted in other countries and in different ethnic groups are needed to verify this finding. In addition, the accidental excision of the parathyroid gland is also relatively common in clinical practice and studies have shown that incidental parathyroidectomy (IP) during thyroid surgery is significantly associated with an increased incidence of postoperative hypocalcaemia.4,35 Meanwhile, it is been shown that the reduction in the number of retained parathyroid glands is another critical risk factor for postoperative hypocalcaemia and that the retention of at least one parathyroid gland can prevent the occurrence of permanent postoperative hypocalcaemia.36 All of these previous findings are consistent with the current results.4,35,36 Therefore, preventing the occurrence of IP as much as possible and the close monitoring for postoperative PTH levels are conducive to reducing hypocalcaemia risks in clinical practice.
Total thyroidectomy is the main treatment for thyroid cancer and malignant lymphoma as it offers complete tumour resection and a low recurrence rate.37 However, prolonged surgical stimulation boosts the release of calcitonin due to the large surgical scope of malignant thyroid disease and the need for lymph node dissection, leading to a decrease in blood calcium.38 In addition, the parathyroid glands, especially the two pairs of parathyroid glands in the lower pole, are not easy to retain during total thyroidectomy for lymph node dissection because the upper parathyroid glands are located on the posterior and upper side of the upper pole of the thyroid. The position is relatively fixed and can be easily identified. The position of the parathyroid gland varies considerably between patients. If the scope of surgery is large and the surgical field of view is unclear, it is easy to mishandle the parathyroid glands.39 The removal of lymph and adipose tissue may cause avascular necrosis of the parathyroid glands, which may result in hypocalcaemia in patients with TT after surgery.40 Studies have indicated that the incidence of transient hypocalcaemia after TT is 27.5%.41 A previous study reported that the incidence of hypocalcaemia in patients undergoing TT (38.8%) was significantly higher than that in patients undergoing lobectomy (13.8%).38 The results of the current meta-analysis demonstrate that TT is one of the main risk factors for postoperative hypocalcaemia. The incidence of parathyroid gland damage during surgery can be significantly increased by extensive thyroidectomy and lymphatic dissection. Therefore, appropriate surgical methods should be selected based on the patient's disease type to avoid the unnecessary expansion of the scope of surgery.
Calcium and magnesium ions have similar chemical properties and share the same homeostasis regulatory system, including intestinal absorption, renal tubule reabsorption and excretion.42 In these regulatory systems, magnesium ions interact with calcium ions.43 Magnesium ions can regulate the synthesis and/or secretion of PTH, affect the sensitivity of target organs to PTH and participate in the synthesis of 1,25-dihydroxyvitamin D3 to affect calcium balance in vivo.44 Magnesium influences the serum levels of calcium ions by promoting PTH secretion and regulating the sensitivity of PTH receptors and renal calcium excretion.45 Therefore, hypomagnesaemia or lowering serum magnesium could increase the risk of hypomagnesaemia after thyroidectomy. A previous study demonstrated that magnesium levels in patients after thyroidectomy generally decreased and 16% of patients developed hypocalcaemia with hypomagnesaemia.46 The incidence of postoperative hypocalcaemia in patients with serum magnesium disorder was 12.71 times higher than that in normal patients.23 These previous studies have demonstrated that hypomagnesaemia is one of the independent risk factors for hypocalcaemia after thyroid surgery,23,46 consistent with the results of the current meta-analysis. At present, several studies have confirmed that hypomagnesaemia is an independent risk factor for hypocalcaemia and close monitoring of serum magnesium concentration in patients with severe hypocalcaemia is recommended.10,20,21 However, the role of magnesium in alleviating severe hypocalcaemia needs to be further investigated.
Vitamin D is a fat-soluble vitamin that plays a vital role in the regulation of serum calcium.47Preoperative vitamin D deficiency is a risk factor for postoperative hypocalcaemia after thyroid surgery.16The results of this current meta-analysis suggested that preoperative vitamin D deficiency was one of the major risk factors for hypocalcaemia. Preoperative vitamin D deficiency reduces the conversion of 1,25-dihydroxyvitamin D3 under the action of PTH. As a result, phosphorus excretion from the kidney of patients is obstructed and calcium cannot be absorbed in the renal tubules and intestines.48 Simultaneously, the calcium in the bone cannot be mobilized, resulting in an imbalance of plasma calcium and phosphorus regulation leading to postoperative hypocalcaemia.28,48 Therefore, vitamin D levels should be monitored and vitamin D supplementation should be given to avoid the occurrence of hypocalcaemia after surgery.
The findings from this current meta-analysis have several potential explanations. Being female is a risk factor of hypocalcaemia, which might be due to the influence of sex steroids on PTH secretion, genetic variations of cell signalling pathways or anatomical differences between males and females.34 Studies report that females have a higher incidence of hypocalcaemia after thyroidectomy.15,32,49 In addition, accidental parathyroid gland removal can easily occur during surgery owing to the high proportion of female parathyroid glands that are located in the thyroid parenchyma, contributing to a significantly higher incidence of postoperative hypocalcaemia in patients with thyroidectomy.50,51 Although numerous studies have indicated that women are an independent risk factor after thyroidectomy,3,15,16,19,20,22,23,25,27,29,34 the incidence of hypocalcaemia in premenopausal and postmenopausal women needs to be further investigated.
Pathological type is one of the most important risk factors because of the large scope of surgery and the need for neck lymph node removal, which increases the probability of hypocalcaemia and persistent hypoparathyroidism in patients with malignant tumours undergoing thyroid surgery alone.52 The current meta-analysis also demonstrated that thyroid malignancy that requires extensive surgery and cervical lymph node dissection is a risk factor for postoperative hypocalcaemia. A previous cross-sectional case–control study demonstrated that the incidence of postoperative hypocalcaemia was higher in patients with malignant tumours compared with patients with benign tumours,49 which was consistent with the current findings that TT, cervical lymph node dissection, thyroiditis and multiple thyroid nodules are the major risk factors for postoperative hypocalcaemia. Another study confirmed that cervical lymph node dissection, thyroiditis and multiple thyroid nodules are the major risk factors for IP.3 Furthermore, the safe retention of parathyroid glands and complete preservation of parathyroid function are of vital importance for the prevention of hypocalcaemia. This explains why patients with cervical lymph node dissection, thyroiditis, thyroid nodules and TT are more likely to have hypocalcaemia after surgery.
With regard to whether age is a risk factor for hypocalcaemia after thyroid surgery, a previous study reported that the risk of hypocalcaemia after thyroid surgery in patients over 50 years of age was 20 times higher than that in younger patients.53 However, studies on the age-specific prevalence of postoperative hypocalcaemia have yielded inconsistent results. For example, a study reported that young patients have an increased risk for temporary hypocalcaemia.54 The results of a large study also suggested that patients younger than 50 years of age were at a higher risk for symptomatic hypocalcaemia.6 Furthermore, an age <28.5 years was reported as a key risk factor for postoperative hypocalcaemia.55 The variations observed in the ages between these studies might be due to differences in subject selection, study design and sample size.53–55 This current meta-analysis demonstrated that there was a nonsignificant difference in the prevalence of postoperative hypocalcaemia based on age. Whether age is a risk factor for hypocalcaemia after thyroid surgery requires further investigation.
Although it has been reported that age, preoperative low calcium levels, Graves’ disease, surgery time and preoperative low PTH levels may increase the risk for postoperative hypocalcaemia after thyroidectomy,3,15,19,25,27,34 this current meta-analysis demonstrated no significant relationship between these factors and the risk of postoperative hypocalcaemia. This may be partially attributable to the high degree of heterogeneity between the included studies. Further research is required. It should be noted that the current meta-analysis was not able to investigate the role of parathyroid autologous transplantation, perioperative fluid replacement and thyroidectomy on lactation because of insufficient published studies.
In conclusion, this current meta-analysis provides moderate-to-high quality evidence that female sex, preoperative vitamin D deficiency, hypomagnesaemia, hypoparathyroidism, thyroid malignancies, incidental parathyroidectomy, thyroiditis, thyroid nodules, total thyroidectomy, CCND, MRND and CND are risk factors for postoperative hypocalcaemia. These current findings will underpin further prevention or timely treatment of postoperative hypocalcaemia after thyroid surgery.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_0300060521996911 for Risk factors for postoperative hypocalcaemia after thyroidectomy: A systematic review and meta-analysis by Zhimei Chen, Qiyuan Zhao, Jinlei Du, Ya Wang, Rongrong Han, Caijuan Xu, Xiaofang Chen and Min Shu in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_0300060521996911 for Risk factors for postoperative hypocalcaemia after thyroidectomy: A systematic review and meta-analysis by Zhimei Chen, Qiyuan Zhao, Jinlei Du, Ya Wang, Rongrong Han, Caijuan Xu, Xiaofang Chen and Min Shu in Journal of International Medical Research
Footnotes
Declaration of conflicting interests: The authors declare that there are no conflicts of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Zhimei Chen https://orcid.org/0000-0002-6133-7163
Supplemental material: Supplemental material for this article is available online.
References
- 1.Gunn A, Oyekunle T, Stang M, et al . Recurrent Laryngeal Nerve Injury After Thyroid Surgery: An Analysis of 11,370 Patients. J Surg Res 2020; 255: 42–49. doi: 10.1016/j.jss.2020.05.017. [DOI] [PubMed] [Google Scholar]
- 2.Khan Bhettani M, Rehman M, Ahmed M, et al . Role of pre-operative vitamin D supplementation to reduce post-thyroidectomy hypocalcemia; Cohort study. Int J Surg 2019; 71: 85–90. doi: 10.1016/j.ijsu.2019.08.035. [DOI] [PubMed] [Google Scholar]
- 3.Lin YS, Hsueh C, Wu HY, et al. Incidental parathyroidectomy during thyroidectomy increases the risk of postoperative hypocalcemia. Laryngoscope 2017; 127: 2194–2200. doi: 10.1002/lary.26448. [DOI] [PubMed] [Google Scholar]
- 4.Sitges-Serra A, Gallego-Otaegui L, Suárez S, et al. Inadvertent parathyroidectomy during total thyroidectomy and central neck dissection for papillary thyroid carcinoma. Surgery 2017; 161: 712–719. doi: 10.1016/j.surg.2016.08.021. [DOI] [PubMed] [Google Scholar]
- 5.Almquist M, Hallgrimsson P, Nordenström E, et al. Prediction of permanent hypoparathyroidism after total thyroidectomy. World J Surg 2014; 38: 2613–2620. doi: 10.1007/s00268-014-2622-z. [DOI] [PubMed] [Google Scholar]
- 6.Arman S, Vijendren A, Mochloulis G. . The incidence of post-thyroidectomy hypocalcaemia: a retrospective single-centre audit. Ann R Coll Surg Engl 2019; 101: 273–278. doi: 10.1308/rcsann.2018.0219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.An CM, Tang PZ, Zhang B. . Prediction and treatment of the hypocalcemia after total thyroidectomy. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2009; 44: 698–700 [Article in Chinese, English abstract]. [PubMed] [Google Scholar]
- 8.Kim WW, Chung SH, Ban EJ, et al . Is Preoperative Vitamin D Deficiency a Risk Factor for Postoperative Symptomatic Hypocalcemia in Thyroid Cancer Patients Undergoing Total Thyroidectomy Plus Central Compartment Neck Dissection? Thyroid 2015; 25: 911–918. doi: 10.1089/thy.2014.0522. [DOI] [PubMed] [Google Scholar]
- 9.Docimo G, Ruggiero R, Casalino G, et al. Risk factors for postoperative hypocalcemia. Updates Surg 2017; 69: 255–260. doi: 10.1007/s13304-017-0452-x. [DOI] [PubMed] [Google Scholar]
- 10.Garrahy A, Murphy MS, Sheahan P. Impact of postoperative magnesium levels on early hypocalcemia and permanent hypoparathyroidism after thyroidectomy. Head Neck 2016; 38: 613–619. doi: 10.1002/hed.23937. [DOI] [PubMed] [Google Scholar]
- 11.Antakia R, Edafe O, Uttley L, et al . Effectiveness of preventative and other surgical measures on hypocalcemia following bilateral thyroid surgery: a systematic review and meta-analysis. Thyroid 2015; 25: 95–106. doi: 10.1089/thy.2014.0101. [DOI] [PubMed] [Google Scholar]
- 12.Vasileiadis I, Charitoudis G, Vasileiadis D, et al . Clinicopathological characteristics of incidental parathyroidectomy after total thyroidectomy: The effect on hypocalcemia. A retrospective cohort study. Int J Surg 2018; 55: 167–174. doi: 10.1016/j.ijsu.2018.05.737. [DOI] [PubMed] [Google Scholar]
- 13.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25: 603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 14.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2008, accessed January 2019).
- 15.Liu RH, Razavi CR, Chang HY, et al. Association of Hypocalcemia and Magnesium Disorders With Thyroidectomy in Commercially Insured Patients. JAMA Otolaryngol Head Neck Surg 2020; 146: 237–246. doi: 10.1001/jamaoto.2019.4193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lale A, Öz B, Akcan AC, et al. Determination of risk factors causing hypocalcaemia after thyroid surgery. Asian J Surg 2019; 42: 883–889. doi: 10.1016/j.asjsur.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Carvalho GB, Giraldo LR, Lira RB, et al. Preoperative vitamin D deficiency is a risk factor for postoperative hypocalcemia in patients undergoing total thyroidectomy: retrospective cohort study. Sao Paulo Med J 2019; 137: 241–247. doi: 10.1590/1516-3180.2018.0336140319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang W, Meng C, Ouyang Q, et al. Magnesemia: an independent risk factor of hypocalcemia after thyroidectomy. Cancer Manag Res 2019; 11: 8135–8144. doi: 10.2147/CMAR.S218179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Falch C, Hornig J, Senne M, et al. Factors predicting hypocalcemia after total thyroidectomy – A retrospective cohort analysis. Int J Surg 2018; 55: 46–50. doi: 10.1016/j.ijsu.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Luo H, Yang H, Zhao W, et al. Hypomagnesemia predicts postoperative biochemical hypocalcemia after thyroidectomy. BMC Surg 2017; 17: 62. doi: 10.1186/s12893-017-0258-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang X, Zhu J, Liu F, et al. Postoperative hypomagnesaemia is not associated with hypocalcemia in thyroid cancer patients undergoing total thyroidectomy plus central compartment neck dissection. Int J Surg 2017; 39: 192–196. doi: 10.1016/j.ijsu.2017.01.085. [DOI] [PubMed] [Google Scholar]
- 22.Cho JN, Park WS, Min SY. Predictors and risk factors of hypoparathyroidism after total thyroidectomy. Int J Surg 2016; 34: 47–52. doi: 10.1016/j.ijsu.2016.08.019. [DOI] [PubMed] [Google Scholar]
- 23.Nellis JC, Tufano RP, Gourin CG. Association between Magnesium Disorders and Hypocalcemia following Thyroidectomy. Otolaryngol Head Neck Surg 2016; 155: 402–410. doi: 10.1177/0194599816644594. [DOI] [PubMed] [Google Scholar]
- 24.Bove A, Di Renzo RM, D'Urbano G, et al. Preoperative risk factors in total thyroidectomy of substernal goiter. Ther Clin Risk Manag 2016; 12: 1805–1809. doi: 10.2147/TCRM.S110464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee GH, Ku YH, Kim HI, et al. Vitamin D level is not a predictor of hypocalcemia after total thyroidectomy. Langenbecks Arch Surg 2015; 400: 617–622. DOI: 10.1007/s00423-015-1311-1. [DOI] [PubMed] [Google Scholar]
- 26.Al-Khatib T, Althubaiti AM, Althubaiti A, et al. Severe vitamin D deficiency: a significant predictor of early hypocalcemia after total thyroidectomy. Otolaryngol Head Neck Surg 2015; 152: 424–431. doi: 10.1177/0194599814561209. [DOI] [PubMed] [Google Scholar]
- 27.Praženica P, O'Keeffe L, Holý R. Dissection and identification of parathyroid glands during thyroidectomy: association with hypocalcemia. Head Neck 2015; 37: 393–399. doi: 10.1002/hed.23613. [DOI] [PubMed] [Google Scholar]
- 28.Díez M, Vera C, Ratia T, et al. Effect of vitamin D deficiency on hypocalcaemia after total thyroidectomy due to benign goitre. Cir Esp 2013; 91: 250–256 [Article in Spanish, English abstract]. doi: 10.1016/j.ciresp.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 29.Baldassarre RL, Chang DC, Brumund KT, et al. Predictors of hypocalcemia after thyroidectomy: results from the nationwide inpatient sample. ISRN Surg 2012; 2012: 838614. doi: 10.5402/2012/838614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Turanli S, Karaman N, Ozgen K. Permanent hypocalcemia in patients operated for thyroid carcinoma. Indian J Otolaryngol Head Neck Surg 2009; 61: 280–285. doi: 10.1007/s12070-009-0083-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Erbil Y, Barbaros U, Temel B, et al. The impact of age, vitamin D(3) level, and incidental parathyroidectomy on postoperative hypocalcemia after total or near total thyroidectomy. Am J Surg 2009; 197: 439–446. doi: 10.1016/j.amjsurg.2008.01.032. [DOI] [PubMed] [Google Scholar]
- 32.Wang YH, Bhandari A, Yang F, et al. Risk factors for hypocalcemia and hypoparathyroidism following thyroidectomy: a retrospective Chinese population study. Cancer Manag Res 2017; 9: 627–635. doi: 10.2147/CMAR.S148090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aqtashi B, Ahmad N, Frotzler A, et al . Risk factors for hypocalcaemia after completion hemithyroidectomy in thyroid cancer. Swiss Med Wkly 2017; 147: w14513. doi: 10.4414/smw.2017.14513. [DOI] [PubMed] [Google Scholar]
- 34.Tongol MC, Mirasol R. Incidence and Risk Factors for Post-thyroidectomy Hypocalcemia. Journal of the ASEAN Federation of Endocrine Societies 2016; 31: 30–36. doi: 10.15605/jafes.031.01.06. [Google Scholar]
- 35.Bai B, Chen Z, Chen W. Risk factors and outcomes of incidental parathyroidectomy in thyroidectomy: A systematic review and meta-analysis. PLoS One 2018; 13: e207088. doi: 10.1371/journal.pone.0207088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim YS. Impact of preserving the parathyroid glands on hypocalcemia after total thyroidectomy with neck dissection. J Korean Surg Soc 2012; 83: 75–82. doi: 10.4174/jkss.2012.83.2.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bellantone R, Lombardi CP, Bossola M, et al. Total thyroidectomy for management of benign thyroid disease: review of 526 cases. World J Surg 2002; 26:1468–1471. doi: 10.1007/s00268-002-6426-1. [DOI] [PubMed] [Google Scholar]
- 38.Del Rio P, Rossini M, Montana CM, et al. Postoperative hypocalcemia: analysis of factors influencing early hypocalcemia development following thyroid surgery. BMC Surg 2019; 18: 25. doi: 10.1186/s12893-019-0483-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perrier ND, Edeiken B, Nunez R, et al. A novel nomenclature to classify parathyroid adenomas. World J Surg 2009; 33: 412–416. doi: 10.1007/s00268-008-9894-0. [DOI] [PubMed] [Google Scholar]
- 40.Tian W, Jiang Y, Gao B, et al . Application of nano-carbon in lymph node dissection for thyroid cancer and protection of parathyroid glands. Med Sci Monit 2014; 20: 1925–1930. doi: 10.12659/MSM.890721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nam KH, Yun JS, Lee YS, et al. Hypocalcemia after Total Thyroidectomy: Incidence and Risk Factors. J Korean Surg Soc 2008; 74: 182–186. [Google Scholar]
- 42.Law PH, Sun Y, Bhattacharya SK, et al . Calcium and magnesium homeostasis in aldosteronism: response to diuretics. Journal of Investigative Medicine 2005; 53: S266. [Google Scholar]
- 43.Chattopadhyay N, Mithal A, Brown EM. . The calcium-sensing receptor: a window into the physiology and pathophysiology of mineral ion metabolism. Endocr Rev 1996; 17: 289–307. doi: 10.1210/edrv-17-4-289. [DOI] [PubMed] [Google Scholar]
- 44.Rodríguez-Ortiz ME, Canalejo A, Herencia C, et al . Magnesium modulates parathyroid hormone secretion and upregulates parathyroid receptor expression at moderately low calcium concentration. Nephrol Dial Transplant 2014; 29: 282–289. doi: 10.1093/ndt/gft400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodelo-Haad C, Pendón-Ruiz de Mier MV, Díaz-Tocados JM, et al . The Role of Disturbed Mg Homeostasis in Chronic Kidney Disease Comorbidities. Front Cell Dev Biol 2020; 8: 543099. doi: 10.3389/fcell.2020.543099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sebastian M, Rudnicki J, Jakubaszko W, et al. Clinical and biochemical factors affecting postoperative hypocalcemia after near-total thyroidectomy. Adv Clin Exp Med 2013; 22: 675–682. doi: 10.1038/mtna.2013.51. [PubMed] [Google Scholar]
- 47.Hewison M, Zehnder D, Chakraverty R, et al . Vitamin D and barrier function: a novel role for extra-renal 1 alpha-hydroxylase. Mol Cell Endocrinol 2004; 215: 31–38. 10.1016/j.mce.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 48.Gloor HJ, Bonjour JP, Caverzasio J, et al . Resistance to the phosphaturic and calcemic actions of parathyroid hormone during phosphate depletion. Prevention by 1,25-dihydroxyvitamin D3. J Clin Invest 1979; 63: 371–377. doi: 10.1172/JCI109312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Easterbrook PJ, Berlin JA, Gopalan R, et al. Publication bias in clinical research. Lancet 1991; 337: 867–872. doi: 10.1016/0140-6736(91)90201-y. [DOI] [PubMed] [Google Scholar]
- 50.Manouras A, Markogiannakis H, Lagoudianakis E, et al. Unintentional parathyroidectomy during total thyroidectomy. Head Neck 2008; 30: 497–502. doi: 10.1002/hed.20728. [DOI] [PubMed] [Google Scholar]
- 51.Rajinikanth J, Paul MJ, Abraham DT, et al. Surgical audit of inadvertent parathyroidectomy during total thyroidectomy: incidence, risk factors, and outcome. Medscape J Med 2009; 11: 29. doi: 10.1111/j.1445-2197.2009.04916_23.x. [PMC free article] [PubMed] [Google Scholar]
- 52.Roh JL, Park JY, Park CI. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 2007; 245: 604–610. doi: 10.1097/01.sla.0000250451.59685.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tolone S, Roberto R, del Genio G, et al. The impact of age and oral calcium and vitamin D supplements on postoperative hypocalcemia after total thyroidectomy. A prospective study. BMC Surg 2013; 13: S11. doi: 10.1186/1471-2482-13-S2-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu YR, Fallon SC, Carpenter JL, et al. Perioperative determinants of transient hypocalcemia after pediatric total thyroidectomy. J Pediatr Surg 2017; 52: 684–688. doi: 10.1016/j.jpedsurg.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 55.Karadeniz E, Akcay MN. . Risk Factors of Incidental Parathyroidectomy and its Relationship with Hypocalcemia after Thyroidectomy: A Retrospective Study. Cureus 2019; 11: e5920. doi: 10.7759/cureus. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_0300060521996911 for Risk factors for postoperative hypocalcaemia after thyroidectomy: A systematic review and meta-analysis by Zhimei Chen, Qiyuan Zhao, Jinlei Du, Ya Wang, Rongrong Han, Caijuan Xu, Xiaofang Chen and Min Shu in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_0300060521996911 for Risk factors for postoperative hypocalcaemia after thyroidectomy: A systematic review and meta-analysis by Zhimei Chen, Qiyuan Zhao, Jinlei Du, Ya Wang, Rongrong Han, Caijuan Xu, Xiaofang Chen and Min Shu in Journal of International Medical Research