Abstract
Prostate cancer remains a life-threatening disease among men worldwide. The majority of PCa-related mortality results from metastatic disease that is characterized by metastasis of prostate tumor cells to various distant organs, such as lung, liver, and bone. Bone metastasis is most common in prostate cancer with osteoblastic and osteolytic lesions. The precise mechanisms underlying PCa metastasis are still being delineated. Intercellular communication is a key feature underlying prostate cancer progression and metastasis. There exists local signaling between prostate cancer cells and cells within the primary tumor microenvironment (TME), in addition to long range signaling wherein tumor cells communicate with sites of future metastases to promote the formation of pre-metastatic niches (PMN) to augment the growth of disseminated tumor cells upon metastasis. Over the last decade, exosomes/ extracellular vesicles have been demonstrated to be involved in such signaling. Exosomes are nanosized extracellular vesicles (EVs), between 30 and 150 nm in thickness, that originate and are released from cells after multivesicular bodies (MVB) fuse with the plasma membrane. These vesicles consist of lipid bilayer membrane enclosing a cargo of biomolecules, including proteins, lipids, RNA, and DNA. Exosomes mediate intercellular communication by transferring their cargo to recipient cells to modulate target cellular functions. In this review, we discuss the contribution of exosomes/extracellular vesicles in prostate cancer progression, in pre-metastatic niche establishment, and in organ-specific metastases. In addition, we briefly discuss the clinical significance of exosomes as biomarkers and therapeutic agents.
Keywords: exosomes/extracellular vesicles, tumor-derived exosomes, castration-resistance prostate cancer, tumor microenvironment, metastasis
1. Introduction
Prostate cancer (PCa) is the most prevalent cancer among males in United States (US) with an estimated 248,530 cases in 2021 [1]. It remains the second leading cause of male mortality with an estimated 34,130 deaths in 2021 in the US [1]. Serum prostate specific antigen (PSA) is used as a diagnostic biomarker for patients with PCa. However, it has been shown to lack specificity and therefore, lead to PCa overdiagnosis and overtreatment [2,3,4,5]. The survival rate of PCa patients is dependent on early disease diagnosis and available treatment options [6]. This malignancy is regulated by androgens acting via androgen receptor (AR) signaling. Therefore, AR signaling ablation via androgen deprivation therapy (ADT) is the goal of first line of therapies that result in cancer regression initially. However, after a period following hormonal therapy, the tumor progresses to metastatic castration-resistant prostate cancer (mCRPC) [7] with poor survival rates and limited therapeutic options. Hence, the search for new therapeutic regimens continue [8].
A majority of PCa-related mortality results from metastatic disease that is characterized by metastasis of prostate tumor cells to various distant organs, such as lung, liver, bone and lymph nodes. Bone metastasis is most common in prostate cancer with osteoblastic and osteolytic lesions [9]. The precise mechanisms underlying PCa metastasis remain unclear which has led scientists to further explore this area. Another area of utmost importance is the identification of alternate prognostic and diagnostic biomarkers which will help in better management of prostate cancer and also be of therapeutic relevance [10]. Some of these biomarkers include circulating tumor cells, microRNAs, and exosomes [5].
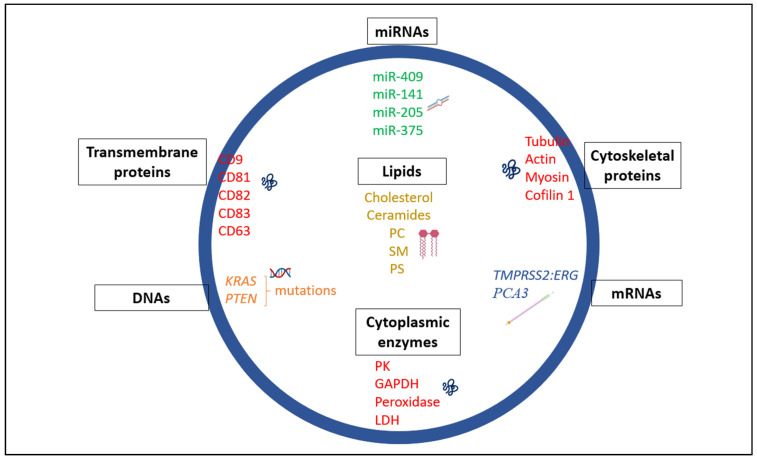
Exosomes are defined as nanosized extracellular vesicles (EVs), between 30 and 150 nm in thickness, that originate and are released from cells after multivesicular bodies (MVB) fuse with the plasma membrane [11,12]. Exosomes consist of a lipid bilayer membrane enclosing a cargo of biomolecules, including proteins, lipids, RNA, and DNA (Figure 1). Increasing evidence suggests that exosomes mediate intercellular communication by transferring their cargo to recipient cells to modulate target cell functions [13,14]. Intercellular communication is a key feature underlying tumor progression and metastasis. There exists local signaling between tumor cells and various cells within the primary tumor microenvironment (TME), in addition to long range signaling wherein tumor cells communicate with sites of future metastases. This latter signaling promotes the formation of pre-metastatic niches (PMN) that augments growth of disseminated tumor cells upon metastasis in distant organs. In this review, we discuss the contribution of exosomes in prostate cancer progression, in pre-metastatic niche establishment, and in organ-specific (organotropic) metastases. In addition, we briefly discuss the clinical significance of exosomes as biomarkers and therapeutic agents.
Figure 1.
Schematic of exosome heterogeneity. Exosomes typically serve as vehicles in shuttling a cargoes of proteins, miRNAs, mRNAs, DNAs, and lipids across cells. Phosphatidylcholine is abbreviated as PC, sphingomyelin as SM, phosphatidylserine as PS, Pyruvate Kinase as PK, lactate dehydrogenase as LDH, and glyceraldehyde 3-phosphate dehydrogenase as GAPDH.
2. Exosomes: Heterogeneity and Diverse Roles
Intercellular communication involving the shuttling of biological components such as microRNAs, long non-coding RNAs, DNA, and proteins via exosomes is essential in maintaining cellular homeostasis and normal functioning. However, there are instances whereby the transport of these biological substances across cells via exosomes can be detrimental resulting in pathological conditions. Over the last decade, exosomes have proven to be great export machinery in trafficking biological materials both in normal and diseased states such as in prostate cancer. Exosomes are cell-secreted and widely distributed in different biological or bodily fluids [15,16]. These vesicles consist of lipid bilayer membrane composed of cholesterol, phosphatidylserines, and sphingolipids which protect them against proteases and RNases [17,18]. Exosomes play key roles in different physiological processes, examples including erythrocyte maturation from reticulocytes, immune cell responses and also spreading of pathogens (virus and prions) from cell-to-cell [19,20]. In cancer, tumor-derived exosomes lead to malignancy, enhanced cell survival and proliferation, drug resistance and the creation of a PMN. The shuttling of the biological components contained in exosomes is thought to be a contributing factor to cancer development. According to Exocarta, a database for collating exosomal content, 9769 proteins, 3408 mRNAs, 2838 microRNAs and 1116 lipids have been identified in exosomes suggesting their crucial roles in intercellular communication [21,22,23,24]. Here we highlight some of the specific constituents in exosomes (Figure 1) and their key roles and functions. Also shown in Table 1 is a summary of exosomal markers that are specific to PCa and their roles.
Table 1.
Exosomal Markers in Prostate Cancer.
| Exosome Source(s) | Isolation Method | Component(s) in Exosome | Type | Application(s) | Role in PCa | Reference(s) |
|---|---|---|---|---|---|---|
| Serum | ExoMiR extraction kit | miR-375, miR-141 | miRNA | Diagnostic markers | Enhances tumor progression | [55] |
| Plasma | ExoQuick-based assay | miR-1290, miR-375 | miRNA | Prognostic markers | Contributes in the progression to CRPC | [89] |
| Urine | Ultracentrifugation | TM256,LAMTOR1, VATL, ADIRF | protein | Diagnostic markers | Upregulated in PCa; may contribute to disease progression | [90] |
| Urine | EXOPRO Urine Clinical Sample Concentrator Kit | ERG, PCA3,SPDEF | mRNA | Diagnostic markers | Promotes PCa aggressive phenotype | [91] |
| Plasma/serum | Differential ultracentrifugation | αvβ3 integrin | protein | Prognostic/diagnostic marker | Promotes PCa aggressive phenotype | [92] |
| Urine | Differential centrifugation | PCA3,TMPRSS2:ERG | mRNA | Diagnostic markers | Regulate AR signaling, mediate oncogenic signaling | [59,93] |
| Urine | Differential centrifugation | miR-196a-5p, miR-501-3p, miR34a-5p, miR-92a-1-5p, miR-143-3p | miRNA | Diagnostic markers | Downregulated in PCa | [94] |
| Urine | Differential centrifugation | miR-574-3p, miR-141-5p, miR-21-5p | miRNA | Diagnostic markers | Upregulated in PCa | [95] |
| Serum | Total Exosome Isolation Reagent | miR-1246 | miRNA | Diagnostic marker | Predicts aggressiveness in PCa | [96] |
| Bone metastasis | Ultracentrifugation | Annexins A1, A3 and A5, DDAH1 | proteins | Predictive markers | Contributes to angiogenesis in PCa | [97] |
| VCaP, LNCaP, C4–2 PCa cells | Ultracentrifugation | CLSTN1, FASN, LDHA | proteins | Diagnostic and prognostic markers | Enhances PCa progression | [42] |
| DU145, PC3 cells | Ultracentrifugation | ANXA2, CLU, ENO1, FN1, KRT8, LAMA5, NPM1, PRDX1, TFRC | proteins | Diagnostic and prognostic markers | Enhances PCa progression | [42] |
| DU145, PC3, VCaP, LNCaP, C4–2 prostate cancer cells, RWPE-1 benign prostate cells | Ultracentrifugation | Sphingolipid, glycosphingolipid | lipids | predictive markers | Enhances PCa progression | [42] |
| LNCaP, DU145, and PC3 cells | Density ultracentrifugation | PKM2 | protein | Therapeutic marker | Contributes to PCa metastasis to the bone | [98] |
| DU145 cells | Differential centrifugation | PCSEAT | lncRNA | Therapeutic marker | Plays an oncogenic role by contributing to growth and motility | [74] |
| Plasma | Total Exosome Isolation Reagent | SAP30L-AS1, SChLAP1 | lncRNA | Diagnostic markers | Biochemical recurrence and disease progression | [76] |
| Urine | Ultracentrifugation | lincRNA-p21 | lncRNA | Diagnostic marker | suppresses the progression of prostate cancer | [77] |
| Serum, PC3 cells | Differential centrifugation | P-glycoprotein | protein | Diagnostic marker | Contributes to docetaxel-resistance in PCa | [99] |
| Plasma | precipitation and ultracentrifugation | KLK3, AR-V7 | mRNA | Diagnostic and prognostic markers | Contributes to disease progression | [100,101] |
| Serum, DU145 cells | ultracentrifugation | ACTN4 | protein | Therapeutic marker | Contributes to disease progression and invasion | [45] |
Abbreviations of mRNA and proteins are as follows—Transmembrane protein 256 (TM256), Late Endosomal/Lysosomal Adaptor, MAPK And MTOR Activator 1 (LAMTOR1),V-type proton ATPase 16 kDa proteolipid subunit (VATL), Adipogenesis regulatory factor (ADIRF), ETS Transcription Factor ERG (ERG), Prostate Cancer Antigen 3 (PCA3), Sterile alpha motif-pointed domain-containing Ets transcription factor (SPDEF), dimethylarginine dimethylaminohydrolase 1(DDAH1), Calsyntenin 1 (CLSTN1), Fatty acid synthase (FASN), Lactate Dehydrogenase A (LDHA), Annexin A2 (ANXA2), Clusterin (CLU), Enolase 1 (ENO1), Fibronectin 1 (FN1), Keratin 8 (KRT8), Laminin Subunit Alpha 5 (LAMA5), Nucleophosmin 1 (NPM1), Peroxiredoxin 1 (PRDX1), Transferrin Receptor (TFRC), Pyruvate kinase M2 (PKM2), PCa specific expression and EZH2-associated transcript (PCSEAT), SAP30L Antisense RNA 1 (Head To Head)(SAP30L-AS1), second chromosome locus associated with prostate-1 (SChLAP1), Kallikrein Related Peptidase 3 (KLK3), Androgen receptor splice variant 7 (AR-V7), Actinin Alpha 4 (ACTN4).
2.1. Exosome-Contained Proteins
The protein content of exosomes varies based on the cell types and bodily fluids from which they are produced [25]. They are typically purified and analyzed using Western blotting, fluorescence-activated cell sorting (FACS), mass spectrometry, and proteomics [26,27]. The endosomal sorting complex required for transport (ESCRT) consisting of four cytosolic protein complexes (ESCRT-0, ESCRT-I, ESCRT-II, and ESCRT-III) with about twenty proteins collectively including their accessory proteins such as programmed cell death 6-interacting protein (Alix), Tumor susceptibility gene 101 (TSG101), Vacuolar protein sorting 4 (VPS4), Vps twenty-associated-1 (VTA1), Heat shock cognate 71 kDa protein (HSC70), and Heat shock protein 90 β (HSP90β). In addition to these proteins, Ras-associated binding (Rab) family of proteins are major proteins in exosomes which contribute to exosomal biogenesis and serve as protein markers in identifying these exosomal vesicles [6,28,29]. Exosomes also consist of specific molecular components derived from their original cells which include transmembrane markers in the tetraspanin family (CD81, CD82, CD83, CD9, and CD63) [19,26,30,31]. These tetraspanins play diverse roles in biological processes such as cell adhesion, membrane fusion, motility, invasion, and exosome regulation [31,32,33]. Further, exosomes are enriched in other proteins such as cell adhesion molecules (e.g., integrins), growth factor receptors, phosphatidylserine-binding milk-fat globule-epidermal growth factor 8 (MFG-E8)/lactadherin and heterotrimeric G proteins [34,35,36]. Geis et al. reported that myeloid-derived suppressor cells (MDSC)-derived exosomes carry proteins, in addition to mRNAs and microRNAs (miRNAs) with some exosomes having different constituents than those of their parental cells [37]. They found that proteins such as annexins (A4, A6, and A7), histones (H2A.z, H2B, H3.1, H3.2, and H4), CD9, heat shock proteins (Hsp70 protein-4, Hsp cognate 71 kDa, heat shock protein 90α (Hsp90α), Hsp90β, major histocompatibility complex II (MHC II) molecules, Alix and vacuolar protein sorting-associated proteins Vps25, Vps4B, and Vps37B were enriched in exosomes with proteins CD9, Vps4B, and Vps37B only identified in exosomes in comparison with their parental cells [37,38]. In addition, proinflammatory proteins; S100A8 and S100A9 loaded in exosomes from MDSCs contributed to the immunosuppressive role of MDSC and enhanced tumor growth and metastasis [37,38]. In the tumor microenvironment, cancer stem cells and mesenchymal cells play integral roles in tumor progression [39]. Proteins loaded in exosomes derived from these two cell types have been shown to serve as intermediates of crosstalk between non-cancer stem cells and cancer stem cells thereby contributing to differentiation and dedifferentiation between these two cell types, respectively [39]. Moreover, analysis from Exocarta database revealed that exosomes from mesenchymal stem cells were enriched in proteins such as cytokines (LIF, CSF1–3, FAM3B), chemokines (CCL-2, -7, -20, and -28, CXCL -2 and -16), interleukins (IL-3, -5, -7, -9, -10, -17B, -19, -23A, -36G, OSM), and growth factors (VEGF, HGF, ITGB1, TGFB1, FGF18, PDGFA, TGFB2, ESM1, INHBB, FGF19, NRG2, GDF5, GDF3, INHBA, FGF16, GDF11, PDGFC, GDF1, GDF9) which may be involved in signaling [21,22,23,24,34]. Finally, exosomes are also enriched in cytoplasmic enzymes (pyruvate kinases, GAPDH, peroxidases, and lactate dehydrogenase) as well as cytoskeletal proteins (tubulin, actin, myosin, cofilin 1 and ezrin-radixin-moesin (ERM) proteins) [40,41].
In PCa, numerous studies have reported proteins that are selectively packaged into exosomes for different cellular and biological functions. Hosseini-Beheshti et al. identified several proteins that were enriched in exosomes in different PCa cells after proteomics profiling [42]. In their study, the authors reported that exosomes from RWPE-1; immortalized normal prostate cell line contained proteins such as Inter-Alpha-Trypsin Inhibitor Heavy Chain 4 (ITIH4), Laminin Subunit Gamma 2 (LAMC2), hemoproteins (HEMO), Keratin, Type II Cytoskeletal 6A (K2C6A), FAT Atypical Cadherin 2 (FAT2), Keratin, type II cytoskeletal 5 (K2C5), Keratin, type I cytoskeletal 14 (K1C14), and Small Heat Shock Protein Beta-1 (HSPB1) [42]. In addition, they identified exosomal proteins such as Endoplasmin (ENPL), Glucose-Regulated Protein, 78kD (GRP78), and Annexin A2-like protein (AXA2L) to be specific in AR negative PCa cells; DU145 and PC3 cells [42]. These proteins may contribute to the understanding of PCa and provide therapeutic targets in the management of the condition. Further, proteomic analyses of exosomes from PCa cell lines (PC346C and VCaP) and immortalized primary prostate epithelial cells (PNT2C2 and RWPE-1) revealed about 481 and 385 proteins respectively including Fatty acid synthase (FASN), Programmed Cell Death 6 Interacting Protein (PDCD6IP), Exportin 1 (XPO1) and Enolase 1 (ENO1) which could serve as biomarkers of PCa [43]. To identify exosome-rich proteins that contribute to the high Gleason Score in 18 men using liquid chromatography-tandem mass spectrometry, Fujiti et al. identified about 4710 proteins contained in exosomes isolated from urine from the patients [44]. Interestingly, among these lists of proteins, proteins such Charged multivesicular body protein 4a (CHMP4A), Charged multivesicular body protein 4c (CHMP4C), and Charged multivesicular body protein 2b (CHMP2B) which are components of ESCRT-III alongside proteins such as Granulin Precursor (GRN) and Alpha-1 microglycoprotein (AMBP) were found to be overexpressed in men with a Gleason Score of 8–9 suggesting that these proteins may con-tribute to dramatic PCa progression and metastasis [44]. Also, mass spectrometry analyses by Ishizuya et al. revealed 787 exosomal proteins, including Alpha-2-Macroglobulin (A2M), Immunoglobulin Heavy Constant Mu (IGHM), Calcium Release Activated Channel Regulator 2A (CRACR2A), Complement C1q Tumor Necrosis Factor-Related Protein 3 (C1QTNF3), CAMP Responsive Element Binding Protein 3 (CREB3), and Upstream Binding Transcription Factor (UBTF), from sera of 36 men with castration-resistant prostate cancer (CRPC), which may be contributing to PCa disease progression to CRPC [45].
2.2. Exosome-Contained MicroRNAs, Messenger RNAs, and Long Non-Coding RNAs
MicroRNAs (miRNAs), messenger RNAs (mRNAs), and long non-coding RNAs (lncRNAs) are essential components of exosomes involved in various biological functions in a variety of cancers [46]. miRNAs can play oncogenic and tumor-suppressive roles in cancer development underlying the importance of their study [47]. Exosomal miRNAs may communicate via gap junctions with neighboring cells of the same tissue or adjacent tissues [48]. He et al. demonstrated that exosomal miR-205 is a positive regulator of ovarian cancer metastasis [49]. By examining the expression of circulating miR-205 in the serum of ovarian cancer patients using the GEO database (GSE106817), the authors found that circulating exosomal miR-205 from serum of patients contributed to ovarian cancer metastasis [49]. They further found that exosomal miR-205 regulates angiogenesis in vitro and in vivo via regulation of PTEN/AKT signaling [49]. Teng et al. reported high levels of tumor suppressor miR-193a in exosomes from colon cancer patients [50]. The authors delineated that, miR-193a interacted with major vault protein (MVP) in cells and was selectively packaged into exosomes leading to colon cancer metastasis to the liver [50]. In another study, exosomal miR-21 and miR-29a were shown to contribute to tumor growth and metastasis by activating toll-like receptors 7 and 8 in immune cells thereby activating a premetastatic inflammatory response [51,52]. Examples of some miRNAs contained in exosomes in prostate cancer include miR-409 and miR-141 which are upregulated and can lead to epithelial-mesenchymal transition (EMT), tumorigenesis, bone metastasis, and AR activation by targeting small heterodimer partner (SHP) [48,53,54]. Exosomal miR-141 and miR-375 were also found to be present in serum of metastatic PCa patients [55]. Furthermore, exosomal miR-105 secreted by PCa, breast, ovarian, and gastric cancers was shown to enhance tumorigenesis and promote metastasis and invasion [56,57].
Exosomal mRNA composition is slightly different from donor cells due to the absence of ribosomal RNAs (18S and 28S) in them [14,57]. Valadi et al. reported that exosomes derived from mouse mast cell line, human mast cell line, and bone marrow-derived mouse mast cells (MC/9, HMC-1, BMMC respectively) contain functional mRNAs and microRNAs (let-7, miR-1, miR-15, miR-16,miR-17, miR-18, miR-181, and miR-375) [14,40]. The mRNAs contained in the exosomes derived from MC/9 coded for Cytochrome c oxidase subunit 5B (Cox5b), Heat shock 70 kDa protein 8 (Hspa8), Serine hydroxymethyltransferase 1 (Shmt1), Lactate dehydrogenase 1 (Ldh1), Zinc finger protein 125 (Zfp125), glucose-6-phosphate isomerase 1 (Gpi1) and Rad 23 homolog B nucleotide excision repair protein (Rad23b) proteins confirming their functional protein-coding abilities [14]. In addition, using Ingenuity Pathway Analysis, the mRNAs were identified to be significant in pathways contributing to cellular development, RNA post-translational modifications, protein synthesis and may also be mediating transport and communication across cells [14]. Also, specific exosomal miR-1, miR-17, miR-18, miR-181, and miR-375 from their study played diverse roles and functions including angiogenesis and tumorigenesis [14]. In a different study, the serum of patients with esophageal cancer contained high levels of esophageal cancer-related gene-4 (ECRG4) mRNA, a tumor suppressor gene that was found to inhibit tumor growth and angiogenesis [58]. Nilsson et al. showed the presence of mRNAs; prostate cancer antigen 3 (PCA3) and transmembrane protease serine 2:v-ets erythroblastosis virus E26 oncogene homolog (TMPRSS2:ERG) in tumor exosomes from the urine of PCa patients [59]. PCA3 gene is a segment of noncoding mRNA located on chromosome 9q21–22 that is expressed significantly, about 60–100 folds in PCa tissues as compared with normal tissues [60,61]. TMPRSS2:ERG is the predominant gene fusion in PCa where TMPRSS2 protein functions with overexpressed ERG; an ETS transcription factor thereby contributing to androgen-resistance in PCa [62,63,64]. A recent study showed that AR variant, AR-V7 RNA is present in exosomes in patients treated with AR pathway inhibitors Enzalutamide and Abiraterone as a primary therapy and is predictive of resistance to AR signaling inhibitors [65].
Over the past decade, lncRNAs have gained attention in exosome research. LncRNAs are typically about >200 nucleotides in length and do not code for proteins however, they are able to interact with proteins, DNAs, and RNAs in the nucleus or cytoplasm [66,67]. Exosomal lncRNAs have been implicated in angiogenesis, tumor growth and migration, and reprogramming the TME [68,69,70]. Several studies have reported lncRNAs to be selectively packaged in exosomes for their biological functioning in recipient cells and could serve as biomarkers for various cancers such as PTENP1 (bladder cancer), MALAT1 (non-small cell lung cancer and breast cancer), HOTAIR (laryngeal squamous cell carcinoma), GAS5 (colorectal cancer), TUG1 and CCND1(cervical cancer and breast cancer) CCAT2 and POU3F3 (glioma), lnc-ROR, lnc-ROR, lnc TUC339 and lnc VLDLR (hepatocellular carcinoma) [40,67,69,70,71,72,73]. In prostate cancer, exosomal lncRNA MYU and PCSEAT function to enhance cell proliferation and migration, whereas exosomal lincRNA-p21, SAP30L-AS1, SChLAP1 function as diagnostic biomarkers [74,75,76,77].
2.3. Exosome-Contained Lipids
Lipids serve as very essential components of the plasma membrane of exosomes contributing to exosomes’ biogenesis, release, and function [78]. Exosomes purified from Oli-neu cells, a mouse oligodendroglial cell line were enriched in ceramides which triggered multivesicular endosome formation from endosome vesicles [79]. Further, exosomes isolated from B-lymphocytes contained acidic lipids (ganglioside GM3 with palmitoyl or nervonoyl residues, phosphatidylinositol, phosphatidylserine, and phosphatidic acid), and uncharged lipids (sphingomyelin, cholesterol, phosphatidylcholine, phosphatidylethanolamine, and ether lipids with an ethanolamine phosphoryl head group) [80]. Also, exosomes collected from two myeloid cell types; rat mast cells (RBL-2H3 mast cell line) and human dendritic cells and their parent cells showed similar lipid distribution; high sphingomyelin, lysophosphatidylcholine, and phosphatidylethanolamines suggesting a rigid lipid packaging in these exosomal membranes than their parent cells [81]. In addition, exosomes derived from reticulocytes were enriched in sphingomyelin than their parent cells although studies by Carayon et al. reported variations in lipid composition in a seven-day in vitro reticulocyte maturation experiment. This shows the participation of these lipids in different molecular mechanisms in exosome packaging during reticulocyte maturation into erythrocytes [11,82]. Finally, exosomes can also serve as carriers in transporting bioactive lipids (fatty acids, prostaglandins, and leukotrienes) and lipid metabolism enzymes (phospholipase A2, C, and D) to recipient cells [40,83,84]. In prostate cancer, Llorente et al. employed targeted lipidomic assays and reported 217 lipid species from exosomes isolated from PC3 cells [85]. They observed that exosomes were highly enriched in glycosphingolipids, cholesterol, sphingomyelin, and phosphatidylserine (1.2%, 43.5%, 16.3%, and 31.1%, respectively) as compared to their parent PC3 cells (0.5%, 19.2%, 6.9%, and 7.7%, respectively) suggesting that these lipids may play major roles in exosome regulation and could be potentially used as exosome biomarkers [85].
2.4. Exosome-Contained DNAs
Studies have shown that tumor-derived exosomes carry DNA. These exosomal DNAs may be used to classify mutations that exist in parental tumor cells [86,87]. In research conducted by Thakur et al., the authors reported the evidence of double-stranded DNA (dsDNA) enriched in tumor-derived exosomes specifically in melanoma, breast, lung, prostate, and pancreatic cancers [87]. Although the aforementioned tumors contained dsDNA, exosomes collected from pancreatic and lung cancer cell lines were lower in DNA content compared with the other cancers suggesting the variations in exosomal DNA packaging in different cancer cells [87]. The authors also showed exosomal DNA could carry BRAF mutations, common mutations in malignant melanoma, and mutations in epidermal growth factor receptor (EGFR) in NSCLC [87]. Performing allele-specific polymerase chain reaction (AS-PCR) on primary melanoma cell lines and NSCLC cell lines to characterize mutational status in BRAF and EGFR, respectively in exosomal DNA, their findings portrayed that exosomal DNA could be used to classify the mutational status of these two genes in parental cell lines [87]. Finally, circulating exosomal DNAs from serum of pancreatic cancer patients and healthy patients were identified to contain homozygous TP53 mutation at codon 273 and heterozygous KRAS mutation at codon 12 [88]. In prostate cancer, studies show that tumor genomic alterations, including copy number variations of genes frequently altered in metastatic PCa (i.e., MYC, AKT1, PTK2, KLF10, and PTEN), are represented in large EVs [86].
3. Tumor-Derived Exosomes: Role in Prostate Cancer Progression and Metastasis
Tumor-derived exosomes have been implicated in prostate cancer progression and metastasis to bone and other sites. Intercellular communication mediated by exosomes play an integral role in mediating both short-range and long-range communication between cancer cells, tumor microenvironment and metastatic sites. The following sections highlight the role of exosomes in these processes in prostate cancer.
3.1. Role of Exosome-Mediated Communication in Prostate Tumor Microenvironment and Angiogenesis
For cancer cells to maintain their hallmarks; sustain immortality, continue their proliferative activity, evade immune responses, resist cell death or apoptosis, initiate angiogenesis, continue invasion and metastasis, a medium is required [102,103,104]. Tumor microenvironment (TME) serves as this medium and it is composed of different cell types such as stromal cells (pericytes, fibroblasts, mesenchymal stromal cells, neuroendocrine cells, etc.), immune cells (T and B lymphocytes, dendritic cells, macrophages, etc.) and the extracellular matrix (ECM) which interact with the tumor cells to enhance their survival and growth. Tumor-derived exosomes from cells in the TME function as important participants or signals in maintaining cell-cell activity [17,105,106]. Tumor-derived exosomes in TME have been implicated as contributing factors in cancer therapy resistance mainly due to their involvement in the myriad of signaling activities across the different cell types in the TME, giving the tumor cells the ability to adapt and evade treatment [107,108]. Tumor-derived exosomes affect the ECM by disrupting cell adhesion via integrins and degrading collagen and fibronectin resulting in enhanced invasion and metastasis [109,110]. Furthermore, studies by DeRita et al. showed that prostate cancer cell exosomes contain the protein Src which activates focal adhesion kinase through integrin activation leading to angiogenesis and metastasis [111]. Also, studies showed that exosomes derived from prostate cancer cells enhance angiogenesis by promoting matrix metalloproteinases, under hypoxic conditions which leads to vascular leakiness and promotes circulating tumor cells (CTC) invasion [112,113,114].
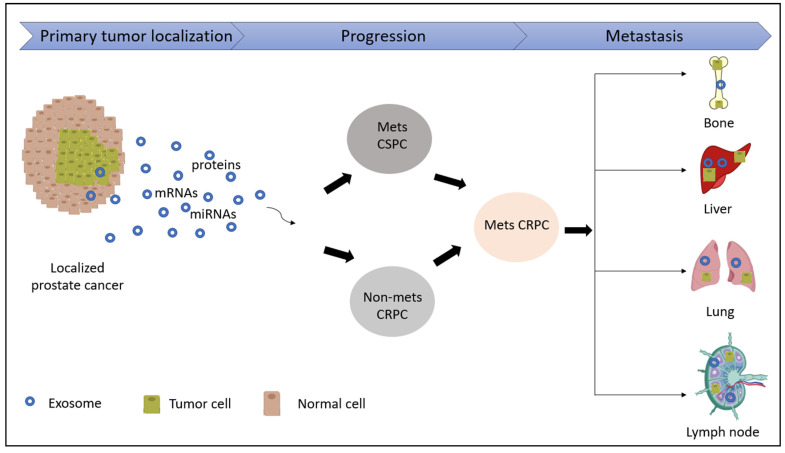
3.2. Tumor-Derived Exosome Mediated Communication in Pre-Metastatic Niche Formation and Organ-Specific Metastasis
Tumor-derived exosomes have been implicated in tumor growth, invasion and metastasis by communicating with cells at distant, pre-metastatic organ sites via the formation of tumor favoring microenvironments, a process referred to as ‘pre-metastatic niche’ formation, in addition to their role at metastatic sites [115] (Figure 2). The formation of PMN involves persistent long-range intercellular communication mediated by soluble or membrane-bound factors originating from the primary tumor [113,116]. These factors traverse through vascular and interstitial spaces and eventually engage with the cholesterol-rich plasma membrane of recipient cells at pre-metastatic organ sites [117]. Tumor-derived exosomes remodel the ECM by accumulating fibronectin and promoting ECM-modifying enzyme lysyl oxidase (LOX) crosslinking to enhance the adhesion of the bone-marrow-derived cells which are essential pre-metastatic niche components [113,118,119]. Interestingly, a recent study elegantly demonstrates that EV-mediated communication between PCa cells and bone marrow is mediated by cholesterol homeostasis in bone marrow myeloid cells [117]. They showed that PCa EV uptake by bone marrow myeloid cells in vitro and in vivo leads to activated NF-κB signaling, reduced myeloid thrombospondin-1 expression and enhanced osteoclast differentiation. A reduction of myeloid cell cholesterol in vitro and in vivo via a targeted, biomimetic approach prior to conditioning with PCa EVs prevented the uptake of PCa EVs by recipient myeloid cells, abolished NF-κB activity, decreased osteoclast differentiation, stabilized thrombospondin-1 expression and led to reduction of metastatic burden by 77% [117]. In another study, the authors demonstrate a role for phospholipase D2 in stimulating exosome secretion in PCa cell line models as well as a potential to increase osteoblast activity, thereby promoting the establishment of PCa bone metastasis [120].
Figure 2.
Schematic illustrating potential role of exosomes in prostate cancer progression. The release of tumor-derived exosomes enhances crosstalk across cells, leading to the progression of a localized PCa into either a metastatic Castration-Sensitive PCa (Mets CSPC) or a non-metastatic Castration-Resistant PCa (Non-mets CRPC). This ultimately leads to the advanced form of the disease; metastatic Castration-Resistant PCa (mCRPC) which can metastasize into various organs of the body such as bone, liver, lungs and lymph nodes.
Epithelial-to-mesenchymal transition (EMT) is a key step in the initiation of metastasis which is activated by autocrine and paracrine signaling by tumor-derived exosomes which can then target EMT-related factors such as β-catenin and transforming growth factor-beta (TGF-β) [121,122,123]. Prostate cancer-derived exosomes from DU145 and PC3 cells produce TGF-β capable of inducing transformation of fibroblasts into myofibroblasts by triggering the TGF-β/SMAD signaling pathway and also promoting tumorigenesis and suppressing immune response [124,125]. Exosomes secreted by prostate tumor cells contain a protein hyaluronidase 1 (Hyal1) which promotes the migration of prostate stromal cells; in effect enhancing prostate cancer progression [126]. Studies by Josson et al. have shown that stromal-derived exosomes contain miR-409, which contribute significantly to EMT in prostate cancer [54]. Similarly, exosomes collected from LNCaP and PC3 cells contained Integrin Subunit Alpha 3 (ITGA3) and Integrin Subunit Beta 1 (ITGB1) proteins which contribute to the migration and invasion of these tumors [127]. Interestingly, a study shows that miR-125b, miR-130b, and miR-155 derived from exosomes trigger neoplastic transformation and mesenchymal-epithelial transition (MET) of stem cells derived from adipose tissues of patients with prostate cancer [128]. miR-105 from tumor-derived exosomes functions as a tumor suppressor and prevents cell proliferation in prostate cancer by targeting cyclin-dependent kinase 6 (CDK6) [56,129].
3.3. Role of Tumor-Derived Exosomes in PCa Lymphatic Metastasis
The lymphatic system is made up of the lymphatic vessels and lymphoid organs comprising of lymphocytes, lymph nodes, spleen, and tonsils. Over the years, a strong association has been found between tumor cells and tumor metastasis particularly in PCa [130,131]. An interesting route PCa-derived cells adapt during metastasis is through the lymphatic route where tumor cells intravasate into lymph nodes to get to their target sites thereby promoting aggressive phenotypes in PCa [131,132,133]. Therefore, research is gearing towards understanding how these PCa cells can metastasize into the lymph nodes. Although mechanisms by which tumor cells initiate this process seems to be a conundrum, one likely mediator contributing to lymph node metastasis to distant organs may possibly be via exosomes [134,135,136,137]. In a study by Khan et al. using tumor-derived samples from PCa patients, the authors identified significant expression of Survivin; a protein classified under inhibitor of apoptosis (IAP) family in exosomes collected from these patients [138]. Interestingly, increase in expression of Survivin was also identified in lymph node tissues from prostate carcinoma patients with high Gleason Score and was found to contribute to metastasis to lymph nodes and aggressive PCa behavior [139]. In another study by Maolake et al., the authors divulged that by activating Chemokine (C-C motif) ligand 21/C-C chemokine receptor 7 (CCL21/CCR7) axis, Tumor necrosis factor-α (TNF-α) contributed to PCa lymph node metastasis using DU145, PC3, LNCaP-SF, and LNCaP prostate cancer cell lines [140]. TNF-α has been reported to be packaged in exosomes [141] and this observation may mediate their effect shown in lymphatic metastasis. Further, Gaballa et al. recently demonstrated that integrin alpha 2 subunit (ITGA2) was packaged in exosomes isolated from DU145, PC3, LNCaP, and CWR-R1 PCa cells which are all metastatic PCa cell lines [142]. Inhibition of exosome release to recipient cells by knocking down ITGA2 in these metastatic PCa cells suggested the potential role of ITGA2 in contributing to disease progression and aggressive phenotypes observed in PCa [142]. In addition, although there were no significant changes in the protein expression levels of ITGA2 in 24 primary PCa tissues verses their matched metastatic lymph node tissues, lymph node metastatic tissues with a high Gleason Score of 9 was observed to have increased expression of ITGA2 in comparison with PCa tissues with lower Gleason Score of 7, indicating the likely role of ITGA2 in enhancing lymph node metastasis [142].
3.4. Role of Tumor-Derived Exosomes in Drug Resistance in Prostate Cancer
Chemotherapy remains one of the classical ways of treating advanced PCa [143]. However, several factors including tumor heterogeneity [144], epigenetic regulation by miRNAs [31], synergistic effects of multiple signaling pathways such as Akt/PI3K, MAPK/ERK, NF-κB/IL-6, mTOR, Hedgehog, and somatostatin receptor have been shown to contribute to drug resistance in these tumor cells. Thus, drug resistance has been one of the most daunting challenges in prostate cancer chemotherapy. The TME has also been implicated as one of the drivers of drug resistance in PCa [145] and the role of tumor-derived exosomes in modulating the TME remains an interesting area of study. We recently demonstrated that enzalutamide resistance and induction of therapy-induced neuroendocrine differentiation states in prostate cancer is mediated via exosomes [146]. Inhibition of exosome release could partly revert the sensitivity of enzalutamide resistant prostate cancer cells. Further, upon enzalutamide treatment, neural transcription factors BRN2 and BRN4 were released in prostate cancer exosomes that drive oncogenic reprogramming of prostate adenocarcinomas towards neuroendocrine states [146]. Corcoran et al. reported that exosomes contributed to docetaxel resistance in docetaxel-sensitive PCa cells (DU145, 22Rv1, and LNCaP) [147]. Release of multidrug resistance protein 1/P-glycoprotein (MDR-1/P-gp), a transporter protein that is associated with the efflux of many foreign substances including anti-cancer drugs from exosomes, was a likely factor in conferring resistance to the docetaxel-sensitive cells after the authors treated the cells with exosomes obtained from docetaxel-resistant variants of DU145 and 22Rv1 (DU145RD and 22Rv1RD), respectively [147]. Similarly, studies from Kato and colleagues demonstrated that MDR-1/P-gp released by serum exosomes in CRPC patients could be a marker for causing docetaxel resistance in PC3 cells [99]. Interestingly, knockdown of exosomal P-gp could decrease docetaxel resistance in the PC3 cells [99]. In addition, using nanoparticle tracking analysis, Kharaziha et al. revealed that docetaxel-resistant DU145 PCa cells released increased amount of exosomes as compared with docetaxel-sensitive DU145 PCa cells [148].
4. Clinical Utility of Exosomes as Biomarkers in Prostate Cancer Management
Over the years, exosomes and other EVs such as oncosomes, apoptotic bodies, microvesicles, and prostasomes are growing as rich sources of biomarkers for cancer diagnosis and as sources of tumor-derived proteins for cancer development [149,150,151]. Due to the involvement of exosomes in an array of biological signaling pathways and acting as cargoes in the tumor microenvironment, they can serve as an attractive source of biomarkers for PCa management. Exosomes are cell-secreted and detectable in biological fluids such as saliva, urine, serum, semen, prostatic secretions, etc., and can act as biomarkers for cancer detection and monitoring of response to therapies [20,43,151,152,153].
In a study conducted by Huang et al., profiling of plasma exosomal miRNA in CRPC patients identified exosomal miR-375 and miR-1290 as potential prognostic biomarkers for predicting survival in CRPC cases [89]. In identifying exosomal biomarkers, Bhagirath et al. reported exosomal miR-1246 as a potential exosomal biomarker in distinguishing between normal, benign, and aggressive form of PCa by showing a 31- and 23-fold increase in aggressive PCa in comparison with normal and benign prostatic hyperplasia (BPH), respectively [96]. Treatment of PC3 and LNCaP cells with exosomal inhibitor GW4869 further confirmed miR-1246 to be released specifically in PCa exosomes [96]. In addition, overexpression of miR-1246 in PCa xenograft mouse model in vivo highlighted the tumor-suppressive role of this miRNA suggesting its therapeutic relevance in managing aggressive PCa [96]. We recently reported exosomal thrombospondin 1 as a potential biomarker for detecting treatment-induced neuroendocrine differentiation (NED) in mCRPC patients (Bhagirath et al., Scientific Reports, under revision). Concurrently, after identifying myriad of altered miRNAs in CRPC-Neuroendocrine (CRPC-NE) and CRPC-Adenocarcinomas (CRPC-Adeno) exosomes/EVs, we used machine learning algorithms to next-generation sequencing miRNA dataset and identified a novel ‘EV-miRNA classifier’ consisting of miR-28-5p and miR-148a-3p that could have clinical advantage in distinguishing between CRPC-NE and CRPC-Adeno in patients non-invasively (Bhagirath et al., Scientific Reports, under revision). Since aberrant androgen receptor signaling can contribute to the development of resistance in PCa cells by expressing truncated AR variant 7 (AR-V7) proteins, detecting AR-V7 in exosomes, CTCs, and circulating tumor RNA (ctRNA) from PCa patients has proven to serve as a potential biomarker in CRPC. In a study conducted by Foj et al. [154], urinary exosomes containing miR-21 and miR-375 from 52 patients were identified as phenomenal non-invasive prognostic biomarkers in managing PCa. Following up on proteomics data of LNCaP- and PC3-exosomes from Sardana et al., Bijnsdorp et al. reported an increase in exosomal proteins ITGA3 and ITGB1 in urine of metastatic PCa patients which could serve as diagnostic metastasis biomarkers [127]. This study showed that exosomal ITGA3 and ITGB1 may play a role in manipulating non-cancerous surrounding cells [127]. Exosome-associated BRN2 and BRN4 were found to possess diagnostic potential for therapy-induced neuroendocrine prostate cancer [146]. Overall, preceding studies highlight the clinical significance of exosomes as prostate cancer biomarkers. Further, exosomes are also efficient and effective carriers of drugs that are used in PCa treatment [15,16].
5. Exosomes as Drug Carriers in Prostate Cancer Management
Chemotherapy remains one of the exacting tasks for researchers in the field especially due to their low bioavailability, drug resistance, immune response threats, and lack of specificity of the drugs used for treatment [155]. The use of nanotechnology has been explored by various scientists as a promising tool in the administration of these chemotherapeutic drugs to their target sites [155,156]. Several advantages accompany the use of these nanoparticles, not to mention but a few, including the protection of cargo from immune response, faster delivery and increase in its bioavailability, although there have been some drawbacks in their usage such as low specificity to tumors, and the induction of chemoresistance and radioresistance in tumor cells [155,157,158]. Nevertheless, due to their nanosized shape and multiple biological functions, exosomes have proven to be excellent carriers of miRNA, siRNA, mRNA, lncRNA, peptides, and synthetic drugs to target sites and this makes them interesting tools for use in cancer chemotherapy [159]. In loading these synthetic and small molecules into exosomes, studies by Batracova et al. showed three possible mechanisms—(1) naïve exosomes collected from parental cells can be loaded with cargoes ex vitro; (2) parental cells can be loaded with the cargoes which are then released into exosomes, and lastly (3) using transfection whereby parental cells absorb DNA encoding therapeutically active compounds which are then released in exosomes [160]. Kosaka et al. demonstrated that tumor suppressor miRNA, miR-143 from non-cancerous cells was delivered by exosomes to PCa cell line; PC-3M-luc cells thus inhibiting proliferation of the tumor cells in vitro and in vivo [161]. Also, extracellular vesicles (exosomes and microvesicles) derived from LNCaP and PC3 prostate cancer cell lines could serve as efficient carriers in delivering Paclitaxel, a drug for managing metastatic PCa to their parental cells by increasing its cytotoxic effect [16,162]. However, one major challenge observed by the authors was that EVs without the drug could increase cell viability [162].
6. Conclusions and Future Studies
Numerous studies conducted have shown that exosomes contribute to the cell-to-cell interactions within the tumor microenvironment, support pre-metastatic niche development and distant metastasis. However, several questions need to be addressed in future studies. Outstanding questions include: What exosome biogenesis pathways are active in prostate cancer cells that can eventually be targeted for therapeutic applications? How distinct are exosomal contents from primary prostate cancer versus metastatic prostate cancer? Do the primary prostate tumors continue supporting the metastatic tumors and vice-versa? It has been shown in prostate cancer and other tumors that pre-metastatic niche formation is mediated by exosomes, driven by continuous exchange of proteins and microRNAs in exosomes [115]. Future studies are needed to examine if pre-metastatic niche formation in PCa is reversible and if it can be exploited for therapeutic targeting of PCa metastasis. Also, it needs to be examined if exosomes from PCa metastatic sites favor development of further pre-metastatic niches in other distant organs like other tumor types [115]. Seeking answers to these outstanding questions will not only increase our understanding of exosomes in prostate cancer biology but will also pave the way for novel therapies for advanced prostate cancer that are urgently needed. Also, increased understanding will promote the optimized development of exosomes as alternate disease biomarkers, particularly for aggressive, metastatic prostate cancer.
Author Contributions
All authors have read and agreed to the published version of the manuscript.
Funding
Author’s laboratory is funded by the US Army Medical Research Acquisition Activity (USAMRAA) through the Idea Development Award under Award No. W81XWH-18-1-0303 and Augusta University. Funding support by the National Cancer Institute at the National Institutes of Health (Grant Number RO1CA177984) is also acknowledged. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense or U.S. Army or NIH.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siegel R.L., Miller K.D., Fuchs H.E., Jemal A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021;71:7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- 2.Adhyam M., Gupta A.K. A Review on the Clinical Utility of PSA in Cancer Prostate. Indian J. Surg. Oncol. 2012;3:120–129. doi: 10.1007/s13193-012-0142-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Semjonow A., Brandt B., Oberpenning F., Roth S., Hertle L. Discordance of assay methods creates pitfalls for the interpretation of prostate-specific antigen values. Prostate Suppl. 1996;7:3–16. doi: 10.1002/(SICI)1097-0045(1996)7+<3::AID-PROS1>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 4.Shahab A.A., Soebadi D.M., Djatisoesanto W., Hardjowijoto S., Soetojo S., Hakim L. Prostate-specific antigen and prostate-specific antigen density cutoff points among Indonesian population suspected for prostate cancer. Prostate Int. 2013;1:23–30. doi: 10.12954/PI.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saini S. PSA and beyond: Alternative prostate cancer biomarkers. Cell Oncol. (Dordr.) 2016;39:97–106. doi: 10.1007/s13402-016-0268-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang T., Deng C.-X. Current Progresses of Exosomes as Cancer Diagnostic and Prognostic Biomarkers. Int. J. Biol. Sci. 2019;15:1–11. doi: 10.7150/ijbs.27796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen M.M., Abate-Shen C. Molecular genetics of prostate cancer: New prospects for old challenges. Genes Dev. 2010;24:1967–2000. doi: 10.1101/gad.1965810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ingrosso G., Detti B., Scartoni D., Lancia A., Giacomelli I., Baki M., Carta G., Livi L., Santoni R. Current therapeutic options in metastatic castration-resistant prostate cancer. Semin. Oncol. 2018;45:303–315. doi: 10.1053/j.seminoncol.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Keller E.T., Brown J. Prostate cancer bone metastases promote both osteolytic and osteoblastic activity. J. Cell. Biochem. 2004;91:718–729. doi: 10.1002/jcb.10662. [DOI] [PubMed] [Google Scholar]
- 10.Kretschmer A., Tilki D. Biomarkers in prostate cancer—Current clinical utility and future perspectives. Crit. Rev. Oncol. Hematol. 2017;120:180–193. doi: 10.1016/j.critrevonc.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Skotland T., Hessvik N.P., Sandvig K., Llorente A. Exosomal lipid composition and the role of ether lipids and phosphoinositides in exosome biology. J. Lipid Res. 2019;60:9–18. doi: 10.1194/jlr.R084343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li F.-X.-Z., Liu J.-J., Xu F., Lin X., Zhong J.-Y., Wu F., Yuan L.-Q. Role of tumor-derived exosomes in bone metastasis. Oncol. Lett. 2019;18:3935–3945. doi: 10.3892/ol.2019.10776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Skog J., Wurdinger T., van Rijn S., Meijer D.H., Gainche L., Sena-Esteves M., Curry W.T., Jr., Carter B.S., Krichevsky A.M., Breakefield X.O. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat. Cell Biol. 2008;10:1470–1476. doi: 10.1038/ncb1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Valadi H., Ekstrom K., Bossios A., Sjostrand M., Lee J.J., Lotvall J.O. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 15.Jiang L., Gu Y., Du Y., Liu J. Exosomes: Diagnostic Biomarkers and Therapeutic Delivery Vehicles for Cancer. Mol. Pharm. 2019;16:3333–3349. doi: 10.1021/acs.molpharmaceut.9b00409. [DOI] [PubMed] [Google Scholar]
- 16.Pullan J.E., Confeld M.I., Osborn J.K., Kim J., Sarkar K., Mallik S. Exosomes as Drug Carriers for Cancer Therapy. Mol. Pharm. 2019;16:1789–1798. doi: 10.1021/acs.molpharmaceut.9b00104. [DOI] [PubMed] [Google Scholar]
- 17.Pan J., Ding M., Xu K., Yang C., Mao L.-J. Exosomes in diagnosis and therapy of prostate cancer. Oncotarget. 2017;8:97693–97700. doi: 10.18632/oncotarget.18532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Osaki M., Okada F. Exosomes and Their Role in Cancer Progression. Yonago Acta Med. 2019;62:182–190. doi: 10.33160/yam.2019.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Niel G., Porto-Carreiro I., Simoes S., Raposo G. Exosomes: A common pathway for a specialized function. J. Biochem. 2006;140:13–21. doi: 10.1093/jb/mvj128. [DOI] [PubMed] [Google Scholar]
- 20.Qin J., Xu Q. Functions and application of exosomes. Acta Pol. Pharm. 2014;71:537–543. [PubMed] [Google Scholar]
- 21.Keerthikumar S., Chisanga D., Ariyaratne D., Al Saffar H., Anand S., Zhao K., Samuel M., Pathan M., Jois M., Chilamkurti N., et al. ExoCarta: A Web-Based Compendium of Exosomal Cargo. J. Mol. Biol. 2016;428:688–692. doi: 10.1016/j.jmb.2015.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathivanan S., Fahner C.J., Reid G.E., Simpson R.J. ExoCarta 2012: Database of exosomal proteins, RNA and lipids. Nucleic Acids Res. 2012;40:D1241–D1244. doi: 10.1093/nar/gkr828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mathivanan S., Simpson R.J. ExoCarta: A compendium of exosomal proteins and RNA. Proteomics. 2009;9:4997–5000. doi: 10.1002/pmic.200900351. [DOI] [PubMed] [Google Scholar]
- 24.Simpson R.J., Kalra H., Mathivanan S. ExoCarta as a resource for exosomal research. J. Extracell. Vesicles. 2012;1 doi: 10.3402/jev.v1i0.18374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li W., Li C., Zhou T., Liu X., Liu X., Li X., Chen D. Role of exosomal proteins in cancer diagnosis. Mol. Cancer. 2017;16:145. doi: 10.1186/s12943-017-0706-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mathivanan S., Ji H., Simpson R.J. Exosomes: Extracellular organelles important in intercellular communication. J. Proteom. 2010;73:1907–1920. doi: 10.1016/j.jprot.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 27.Théry C., Zitvogel L., Amigorena S. Exosomes: Composition, biogenesis and function. Nat. Rev. Immunol. 2002;2:569–579. doi: 10.1038/nri855. [DOI] [PubMed] [Google Scholar]
- 28.Doyle L.M., Wang M.Z. Overview of Extracellular Vesicles, Their Origin, Composition, Purpose, and Methods for Exosome Isolation and Analysis. Cells. 2019;8:727. doi: 10.3390/cells8070727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Colombo M., Moita C., van Niel G., Kowal J., Vigneron J., Benaroch P., Manel N., Moita L.F., Théry C., Raposo G. Analysis of ESCRT functions in exosome biogenesis, composition and secretion highlights the heterogeneity of extracellular vesicles. J. Cell Sci. 2013;126:5553. doi: 10.1242/jcs.128868. [DOI] [PubMed] [Google Scholar]
- 30.Soung Y.H., Nguyen T., Cao H., Lee J., Chung J. Emerging roles of exosomes in cancer invasion and metastasis. BMB Rep. 2016;49:18–25. doi: 10.5483/BMBRep.2016.49.1.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Azmi A.S., Bao B., Sarkar F.H. Exosomes in cancer development, metastasis, and drug resistance: A comprehensive review. Cancer Metastasis Rev. 2013;32:623–642. doi: 10.1007/s10555-013-9441-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andreu Z., Yáñez-Mó M. Tetraspanins in extracellular vesicle formation and function. Front. Immunol. 2014;5:442. doi: 10.3389/fimmu.2014.00442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Simons M., Raposo G. Exosomes—Vesicular carriers for intercellular communication. Curr. Opin. Cell Biol. 2009;21:575–581. doi: 10.1016/j.ceb.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 34.Ferguson S.W., Nguyen J. Exosomes as therapeutics: The implications of molecular composition and exosomal heterogeneity. J. Control. Release. 2016;228:179–190. doi: 10.1016/j.jconrel.2016.02.037. [DOI] [PubMed] [Google Scholar]
- 35.Lötvall J., Hill A.F., Hochberg F., Buzás E.I., Di Vizio D., Gardiner C., Gho Y.S., Kurochkin I.V., Mathivanan S., Quesenberry P., et al. Minimal experimental requirements for definition of extracellular vesicles and their functions: A position statement from the International Society for Extracellular Vesicles. J. Extracell. Vesicles. 2014;3:26913. doi: 10.3402/jev.v3.26913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van der Vlist E.J., Nolte-’t Hoen E.N.M., Stoorvogel W., Arkesteijn G.J.A., Wauben M.H.M. Fluorescent labeling of nano-sized vesicles released by cells and subsequent quantitative and qualitative analysis by high-resolution flow cytometry. Nat. Protoc. 2012;7:1311–1326. doi: 10.1038/nprot.2012.065. [DOI] [PubMed] [Google Scholar]
- 37.Geis-Asteggiante L., Belew A.T., Clements V.K., Edwards N.J., Ostrand-Rosenberg S., El-Sayed N.M., Fenselau C. Differential Content of Proteins, mRNAs, and miRNAs Suggests that MDSC and Their Exosomes May Mediate Distinct Immune Suppressive Functions. J. Proteome Res. 2018;17:486–498. doi: 10.1021/acs.jproteome.7b00646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burke M., Choksawangkarn W., Edwards N., Ostrand-Rosenberg S., Fenselau C. Exosomes from myeloid-derived suppressor cells carry biologically active proteins. J. Proteome Res. 2014;13:836–843. doi: 10.1021/pr400879c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xu J., Liao K., Zhou W. Exosomes Regulate the Transformation of Cancer Cells in Cancer Stem Cell Homeostasis. Stem Cells Int. 2018;2018:4837370. doi: 10.1155/2018/4837370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rashed M.H., Bayraktar E., Helal G.K., Abd-Ellah M.F., Amero P., Chavez-Reyes A., Rodriguez-Aguayo C. Exosomes: From Garbage Bins to Promising Therapeutic Targets. Int. J. Mol. Sci. 2017;18:538. doi: 10.3390/ijms18030538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Théry C., Ostrowski M., Segura E. Membrane vesicles as conveyors of immune responses. Nat. Rev. Immunol. 2009;9:581–593. doi: 10.1038/nri2567. [DOI] [PubMed] [Google Scholar]
- 42.Hosseini-Beheshti E., Pham S., Adomat H., Li N., Tomlinson Guns E.S. Exosomes as biomarker enriched microvesicles: Characterization of exosomal proteins derived from a panel of prostate cell lines with distinct AR phenotypes. Mol. Cell Proteom. 2012;11:863–885. doi: 10.1074/mcp.M111.014845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duijvesz D., Burnum-Johnson K.E., Gritsenko M.A., Hoogland A.M., Vredenbregt-van den Berg M.S., Willemsen R., Luider T., Pasa-Tolic L., Jenster G. Proteomic profiling of exosomes leads to the identification of novel biomarkers for prostate cancer. PLoS ONE. 2013;8:e82589. doi: 10.1371/journal.pone.0082589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fujita K., Kume H., Matsuzaki K., Kawashima A., Ujike T., Nagahara A., Uemura M., Miyagawa Y., Tomonaga T., Nonomura N. Proteomic analysis of urinary extracellular vesicles from high Gleason score prostate cancer. Sci. Rep. 2017;7:42961. doi: 10.1038/srep42961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ishizuya Y., Uemura M., Narumi R., Tomiyama E., Koh Y., Matsushita M., Nakano K., Hayashi Y., Wang C., Kato T., et al. The role of actinin-4 (ACTN4) in exosomes as a potential novel therapeutic target in castration-resistant prostate cancer. Biochem. Biophys. Res. Commun. 2020;523:588–594. doi: 10.1016/j.bbrc.2019.12.084. [DOI] [PubMed] [Google Scholar]
- 46.Che Y., Shi X., Shi Y., Jiang X., Ai Q., Shi Y., Gong F., Jiang W. Exosomes Derived from miR-143-Overexpressing MSCs Inhibit Cell Migration and Invasion in Human Prostate Cancer by Downregulating TFF3. Mol. Ther. Nucleic Acids. 2019;18:232–244. doi: 10.1016/j.omtn.2019.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 47.Akoto T., Bhagirath D., Saini S. MicroRNAs in treatment-induced neuroendocrine differentiation in prostate cancer. Cancer Drug Resist. 2020;3:804–818. doi: 10.20517/cdr.2020.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rajagopal C., Harikumar K.B. The Origin and Functions of Exosomes in Cancer. Front. Oncol. 2018;8:66. doi: 10.3389/fonc.2018.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.He L., Zhu W., Chen Q., Yuan Y., Wang Y., Wang J., Wu X. Ovarian cancer cell-secreted exosomal miR-205 promotes metastasis by inducing angiogenesis. Theranostics. 2019;9:8206–8220. doi: 10.7150/thno.37455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Teng Y., Ren Y., Hu X., Mu J., Samykutty A., Zhuang X., Deng Z., Kumar A., Zhang L., Merchant M.L., et al. MVP-mediated exosomal sorting of miR-193a promotes colon cancer progression. Nat. Commun. 2017;8:14448. doi: 10.1038/ncomms14448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fabbri M., Paone A., Calore F., Galli R., Gaudio E., Santhanam R., Lovat F., Fadda P., Mao C., Nuovo G.J., et al. MicroRNAs bind to Toll-like receptors to induce prometastatic inflammatory response. Proc. Natl. Acad. Sci. USA. 2012;109:E2110–E2116. doi: 10.1073/pnas.1209414109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Malla B., Zaugg K., Vassella E., Aebersold D.M., Dal Pra A. Exosomes and Exosomal MicroRNAs in Prostate Cancer Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2017;98:982–995. doi: 10.1016/j.ijrobp.2017.03.031. [DOI] [PubMed] [Google Scholar]
- 53.Xiao J., Gong A.Y., Eischeid A.N., Chen D., Deng C., Young C.Y., Chen X.M. miR-141 modulates androgen receptor transcriptional activity in human prostate cancer cells through targeting the small heterodimer partner protein. Prostate. 2012;72:1514–1522. doi: 10.1002/pros.22501. [DOI] [PubMed] [Google Scholar]
- 54.Josson S., Gururajan M., Hu P., Shao C., Chu G.Y., Zhau H.E., Liu C., Lao K., Lu C.L., Lu Y.T., et al. miR-409-3p/-5p promotes tumorigenesis, epithelial-to-mesenchymal transition, and bone metastasis of human prostate cancer. Clin. Cancer Res. 2014;20:4636–4646. doi: 10.1158/1078-0432.CCR-14-0305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bryant R.J., Pawlowski T., Catto J.W.F., Marsden G., Vessella R.L., Rhees B., Kuslich C., Visakorpi T., Hamdy F.C. Changes in circulating microRNA levels associated with prostate cancer. Br. J. Cancer. 2012;106:768–774. doi: 10.1038/bjc.2011.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhou W., Fong M.Y., Min Y., Somlo G., Liu L., Palomares M.R., Yu Y., Chow A., O’Connor S.T., Chin A.R., et al. Cancer-secreted miR-105 destroys vascular endothelial barriers to promote metastasis. Cancer Cell. 2014;25:501–515. doi: 10.1016/j.ccr.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Milane L., Singh A., Mattheolabakis G., Suresh M., Amiji M.M. Exosome mediated communication within the tumor microenvironment. J. Control. Release. 2015;219:278–294. doi: 10.1016/j.jconrel.2015.06.029. [DOI] [PubMed] [Google Scholar]
- 58.Mao L., Li X., Gong S., Yuan H., Jiang Y., Huang W., Sun X., Dang X. Serum exosomes contain ECRG4 mRNA that suppresses tumor growth via inhibition of genes involved in inflammation, cell proliferation, and angiogenesis. Cancer Gene Ther. 2018;25:248–259. doi: 10.1038/s41417-018-0032-3. [DOI] [PubMed] [Google Scholar]
- 59.Nilsson J., Skog J., Nordstrand A., Baranov V., Mincheva-Nilsson L., Breakefield X.O., Widmark A. Prostate cancer-derived urine exosomes: A novel approach to biomarkers for prostate cancer. Br. J. Cancer. 2009;100:1603–1607. doi: 10.1038/sj.bjc.6605058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bussemakers M.J., van Bokhoven A., Verhaegh G.W., Smit F.P., Karthaus H.F., Schalken J.A., Debruyne F.M., Ru N., Isaacs W.B. DD3: A new prostate-specific gene, highly overexpressed in prostate cancer. Cancer Res. 1999;59:5975–5979. [PubMed] [Google Scholar]
- 61.Marks L.S., Bostwick D.G. Prostate Cancer Specificity of PCA3 Gene Testing: Examples from Clinical Practice. Rev. Urol. 2008;10:175–181. [PMC free article] [PubMed] [Google Scholar]
- 62.Yu J., Yu J., Mani R.-S., Cao Q., Brenner C.J., Cao X., Wang X., Wu L., Li J., Hu M., et al. An Integrated Network of Androgen Receptor, Polycomb, and TMPRSS2-ERG Gene Fusions in Prostate Cancer Progression. Cancer Cell. 2010;17:443–454. doi: 10.1016/j.ccr.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tomlins S.A., Laxman B., Varambally S., Cao X., Yu J., Helgeson B.E., Cao Q., Prensner J.R., Rubin M.A., Shah R.B., et al. Role of the TMPRSS2-ERG gene fusion in prostate cancer. Neoplasia. 2008;10:177–188. doi: 10.1593/neo.07822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang Z., Wang Y., Zhang J., Hu Q., Zhi F., Zhang S., Mao D., Zhang Y., Liang H. Significance of the TMPRSS2:ERG gene fusion in prostate cancer. Mol. Med. Rep. 2017;16:5450–5458. doi: 10.3892/mmr.2017.7281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Del Re M., Conteduca V., Crucitta S., Gurioli G., Casadei C., Restante G., Schepisi G., Lolli C., Cucchiara F., Danesi R., et al. Androgen receptor gain in circulating free DNA and splicing variant 7 in exosomes predict clinical outcome in CRPC patients treated with abiraterone and enzalutamide. Prostate Cancer Prostatic Dis. 2021 doi: 10.1038/s41391-020-00309-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Perkel J.M. Visiting “Noncodarnia”. BioTechniques. 2013;54:301–304. doi: 10.2144/000114037. [DOI] [PubMed] [Google Scholar]
- 67.Sun Z., Yang S., Zhou Q., Wang G., Song J., Li Z., Zhang Z., Xu J., Xia K., Chang Y., et al. Emerging role of exosome-derived long non-coding RNAs in tumor microenvironment. Mol. Cancer. 2018;17:82. doi: 10.1186/s12943-018-0831-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang P., Zhou H., Lu K., Lu Y., Wang Y., Feng T. Exosome-mediated delivery of MALAT1 induces cell proliferation in breast cancer. OncoTargets Ther. 2018;11:291–299. doi: 10.2147/OTT.S155134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lang H.L., Hu G.W., Chen Y., Liu Y., Tu W., Lu Y.M., Wu L., Xu G.H. Glioma cells promote angiogenesis through the release of exosomes containing long non-coding RNA POU3F3. Eur. Rev. Med. Pharm. Sci. 2017;21:959–972. [PubMed] [Google Scholar]
- 70.Wang M., Zhou L., Yu F., Zhang Y., Li P., Wang K. The functional roles of exosomal long non-coding RNAs in cancer. Cell. Mol. Life Sci. 2019;76:2059–2076. doi: 10.1007/s00018-019-03018-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gezer U., Özgür E., Cetinkaya M., Isin M., Dalay N. Long non-coding RNAs with low expression levels in cells are enriched in secreted exosomes. Cell Biol. Int. 2014;38:1076–1079. doi: 10.1002/cbin.10301. [DOI] [PubMed] [Google Scholar]
- 72.Zheng R., Du M., Wang X., Xu W., Liang J., Wang W., Lv Q., Qin C., Chu H., Wang M., et al. Exosome-transmitted long non-coding RNA PTENP1 suppresses bladder cancer progression. Mol. Cancer. 2018;17:143. doi: 10.1186/s12943-018-0880-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhao W., Liu Y., Zhang C., Duan C. Multiple Roles of Exosomal Long Noncoding RNAs in Cancers. Biomed. Res. Int. 2019;2019:1460572. doi: 10.1155/2019/1460572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yang X., Wang L., Li R., Zhao Y., Gu Y., Liu S., Cheng T., Huang K., Yuan Y., Song D., et al. The long non-coding RNA PCSEAT exhibits an oncogenic property in prostate cancer and functions as a competing endogenous RNA that associates with EZH2. Biochem. Biophys. Res. Commun. 2018;502:262–268. doi: 10.1016/j.bbrc.2018.05.157. [DOI] [PubMed] [Google Scholar]
- 75.Varambally S., Dhanasekaran S.M., Zhou M., Barrette T.R., Kumar-Sinha C., Sanda M.G., Ghosh D., Pienta K.J., Sewalt R.G.A.B., Otte A.P., et al. The polycomb group protein EZH2 is involved in progression of prostate cancer. Nature. 2002;419:624–629. doi: 10.1038/nature01075. [DOI] [PubMed] [Google Scholar]
- 76.Wang Y.H., Ji J., Wang B.C., Chen H., Yang Z.H., Wang K., Luo C.L., Zhang W.W., Wang F.B., Zhang X.L. Tumor-Derived Exosomal Long Noncoding RNAs as Promising Diagnostic Biomarkers for Prostate Cancer. Cell. Physiol. Biochem. 2018;46:532–545. doi: 10.1159/000488620. [DOI] [PubMed] [Google Scholar]
- 77.Işın M., Uysaler E., Özgür E., Köseoğlu H., Şanlı Ö., Yücel Ö.B., Gezer U., Dalay N. Exosomal lncRNA-p21 levels may help to distinguish prostate cancer from benign disease. Front. Genet. 2015;6:168. doi: 10.3389/fgene.2015.00168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Skotland T., Sandvig K., Llorente A. Lipids in exosomes: Current knowledge and the way forward. Prog. Lipid Res. 2017;66:30–41. doi: 10.1016/j.plipres.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 79.Trajkovic K., Hsu C., Chiantia S., Rajendran L., Wenzel D., Wieland F., Schwille P., Brügger B., Simons M. Ceramide Triggers Budding of Exosome Vesicles into Multivesicular Endosomes. Science. 2008;319:1244. doi: 10.1126/science.1153124. [DOI] [PubMed] [Google Scholar]
- 80.Wubbolts R., Leckie R.S., Veenhuizen P.T.M., Schwarzmann G., Möbius W., Hoernschemeyer J., Slot J.-W., Geuze H.J., Stoorvogel W. Proteomic and Biochemical Analyses of Human B Cell-derived Exosomes: Potential implications for their function and multivesicular body formation. J. Biol. Chem. 2003;278:10963–10972. doi: 10.1074/jbc.M207550200. [DOI] [PubMed] [Google Scholar]
- 81.Laulagnier K., Motta C., Hamdi S., Roy S., Fauvelle F., Pageaux J.F., Kobayashi T., Salles J.P., Perret B., Bonnerot C., et al. Mast cell- and dendritic cell-derived exosomes display a specific lipid composition and an unusual membrane organization. Biochem. J. 2004;380:161–171. doi: 10.1042/bj20031594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Carayon K., Chaoui K., Ronzier E., Lazar I., Bertrand-Michel J., Roques V., Balor S., Terce F., Lopez A., Salomé L., et al. Proteolipidic Composition of Exosomes Changes during Reticulocyte Maturation. J. Biol. Chem. 2011;286:34426–34439. doi: 10.1074/jbc.M111.257444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Record M., Carayon K., Poirot M., Silvente-Poirot S. Exosomes as new vesicular lipid transporters involved in cell–cell communication and various pathophysiologies. Biochim. Biophys. Acta (BBA) Mol. Cell Biol. Lipids. 2014;1841:108–120. doi: 10.1016/j.bbalip.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 84.Subra C., Grand D., Laulagnier K., Stella A., Lambeau G., Paillasse M., De Medina P., Monsarrat B., Perret B., Silvente-Poirot S., et al. Exosomes account for vesicle-mediated transcellular transport of activatable phospholipases and prostaglandins. J. Lipid Res. 2010;51:2105–2120. doi: 10.1194/jlr.M003657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Llorente A., Skotland T., Sylvänne T., Kauhanen D., Róg T., Orłowski A., Vattulainen I., Ekroos K., Sandvig K. Molecular lipidomics of exosomes released by PC-3 prostate cancer cells. Biochim. Biophys. Acta (BBA) Mol. Cell Biol. Lipids. 2013;1831:1302–1309. doi: 10.1016/j.bbalip.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 86.Vagner T., Spinelli C., Minciacchi V.R., Balaj L., Zandian M., Conley A., Zijlstra A., Freeman M.R., Demichelis F., De S., et al. Large extracellular vesicles carry most of the tumour DNA circulating in prostate cancer patient plasma. J. Extracell. Vesicles. 2018;7:1505403. doi: 10.1080/20013078.2018.1505403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Thakur B.K., Zhang H., Becker A., Matei I., Huang Y., Costa-Silva B., Zheng Y., Hoshino A., Brazier H., Xiang J., et al. Double-stranded DNA in exosomes: A novel biomarker in cancer detection. Cell Res. 2014;24:766–769. doi: 10.1038/cr.2014.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yang S., Che S.P., Kurywchak P., Tavormina J.L., Gansmo L.B., Correa de Sampaio P., Tachezy M., Bockhorn M., Gebauer F., Haltom A.R., et al. Detection of mutant KRAS and TP53 DNA in circulating exosomes from healthy individuals and patients with pancreatic cancer. Cancer Biol. Ther. 2017;18:158–165. doi: 10.1080/15384047.2017.1281499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Huang X., Yuan T., Liang M., Du M., Xia S., Dittmar R., Wang D., See W., Costello B.A., Quevedo F., et al. Exosomal miR-1290 and miR-375 as prognostic markers in castration-resistant prostate cancer. Eur. Urol. 2015;67:33–41. doi: 10.1016/j.eururo.2014.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Øverbye A., Skotland T., Koehler C.J., Thiede B., Seierstad T., Berge V., Sandvig K., Llorente A. Identification of prostate cancer biomarkers in urinary exosomes. Oncotarget. 2015;6:30357–30376. doi: 10.18632/oncotarget.4851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fujita K., Nonomura N. Urinary biomarkers of prostate cancer. Int. J. Urol. 2018;25:770–779. doi: 10.1111/iju.13734. [DOI] [PubMed] [Google Scholar]
- 92.Krishn S.R., Singh A., Bowler N., Duffy A.N., Friedman A., Fedele C., Kurtoglu S., Tripathi S.K., Wang K., Hawkins A., et al. Prostate cancer sheds the αvβ3 integrin in vivo through exosomes. Matrix Biol. 2019;77:41–57. doi: 10.1016/j.matbio.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Semaan L., Mander N., Cher M.L., Chinni S.R. TMPRSS2-ERG fusions confer efficacy of enzalutamide in an in vivo bone tumor growth model. BMC Cancer. 2019;19:972. doi: 10.1186/s12885-019-6185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rodríguez M., Bajo-Santos C., Hessvik N.P., Lorenz S., Fromm B., Berge V., Sandvig K., Linē A., Llorente A. Identification of non-invasive miRNAs biomarkers for prostate cancer by deep sequencing analysis of urinary exosomes. Mol. Cancer. 2017;16:156. doi: 10.1186/s12943-017-0726-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Samsonov R., Shtam T., Burdakov V., Glotov A., Tsyrlina E., Berstein L., Nosov A., Evtushenko V., Filatov M., Malek A. Lectin-induced agglutination method of urinary exosomes isolation followed by mi-RNA analysis: Application for prostate cancer diagnostic. Prostate. 2016;76:68–79. doi: 10.1002/pros.23101. [DOI] [PubMed] [Google Scholar]
- 96.Bhagirath D., Yang T.L., Bucay N., Sekhon K., Majid S., Shahryari V., Dahiya R., Tanaka Y., Saini S. microRNA-1246 Is an Exosomal Biomarker for Aggressive Prostate Cancer. Cancer Res. 2018;78:1833–1844. doi: 10.1158/0008-5472.CAN-17-2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ronquist K.G., Ronquist G., Larsson A., Carlsson L. Proteomic Analysis of Prostate Cancer Metastasis-derived Prostasomes. Anticancer Res. 2010;30:285. [PubMed] [Google Scholar]
- 98.Dai J., Escara-Wilke J., Keller J.M., Jung Y., Taichman R.S., Pienta K.J., Keller E.T. Primary prostate cancer educates bone stroma through exosomal pyruvate kinase M2 to promote bone metastasis. J. Exp. Med. 2019;216:2883–2899. doi: 10.1084/jem.20190158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kato T., Mizutani K., Kameyama K., Kawakami K., Fujita Y., Nakane K., Kanimoto Y., Ehara H., Ito H., Seishima M., et al. Serum exosomal P-glycoprotein is a potential marker to diagnose docetaxel resistance and select a taxoid for patients with prostate cancer. Urol. Oncol. Semin. Orig. Investig. 2015;33 doi: 10.1016/j.urolonc.2015.04.019. [DOI] [PubMed] [Google Scholar]
- 100.Paliouras M., Borgono C., Diamandis E.P. Human tissue kallikreins: The cancer biomarker family. Cancer Lett. 2007;249:61–79. doi: 10.1016/j.canlet.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 101.Joncas F.H., Lucien F., Rouleau M., Morin F., Leong H.S., Pouliot F., Fradet Y., Gilbert C., Toren P. Plasma extracellular vesicles as phenotypic biomarkers in prostate cancer patients. Prostate. 2019;79:1767–1776. doi: 10.1002/pros.23901. [DOI] [PubMed] [Google Scholar]
- 102.Fouad Y.A., Aanei C. Revisiting the hallmarks of cancer. Am. J. Cancer Res. 2017;7:1016–1036. [PMC free article] [PubMed] [Google Scholar]
- 103.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 104.Gutschner T., Diederichs S. The hallmarks of cancer: A long non-coding RNA point of view. RNA Biol. 2012;9:703–719. doi: 10.4161/rna.20481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Roma-Rodrigues C., Mendes R., Baptista P.V., Fernandes A.R. Targeting Tumor Microenvironment for Cancer Therapy. Int. J. Mol. Sci. 2019;20:840. doi: 10.3390/ijms20040840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Chen F., Zhuang X., Lin L., Yu P., Wang Y., Shi Y., Hu G., Sun Y. New horizons in tumor microenvironment biology: Challenges and opportunities. BMC Med. 2015;13:45. doi: 10.1186/s12916-015-0278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Li I., Nabet B.Y. Exosomes in the tumor microenvironment as mediators of cancer therapy resistance. Mol. Cancer. 2019;18:32. doi: 10.1186/s12943-019-0975-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Quail D.F., Joyce J.A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med. 2013;19:1423–1437. doi: 10.1038/nm.3394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mashouri L., Yousefi H., Aref A.R., Ahadi A.M., Molaei F., Alahari S.K. Exosomes: Composition, biogenesis, and mechanisms in cancer metastasis and drug resistance. Mol. Cancer. 2019;18:75. doi: 10.1186/s12943-019-0991-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mu W., Rana S., Zöller M. Host matrix modulation by tumor exosomes promotes motility and invasiveness. Neoplasia. 2013;15:875–887. doi: 10.1593/neo.13786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.DeRita R.M., Zerlanko B., Singh A., Lu H., Iozzo R.V., Benovic J.L., Languino L.R. c-Src, Insulin-Like Growth Factor I Receptor, G-Protein-Coupled Receptor Kinases and Focal Adhesion Kinase are Enriched Into Prostate Cancer Cell Exosomes. J. Cell. Biochem. 2017;118:66–73. doi: 10.1002/jcb.25611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Deep G., Jain A., Kumar A., Agarwal C., Kim S., Leevy W.M., Agarwal R. Exosomes secreted by prostate cancer cells under hypoxia promote matrix metalloproteinases activity at pre-metastatic niches. Mol. Carcinog. 2020;59:323–332. doi: 10.1002/mc.23157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Peinado H., Zhang H., Matei I.R., Costa-Silva B., Hoshino A., Rodrigues G., Psaila B., Kaplan R.N., Bromberg J.F., Kang Y., et al. Pre-metastatic niches: Organ-specific homes for metastases. Nat. Rev. Cancer. 2017;17:302–317. doi: 10.1038/nrc.2017.6. [DOI] [PubMed] [Google Scholar]
- 114.Ramteke A., Ting H., Agarwal C., Mateen S., Somasagara R., Hussain A., Graner M., Frederick B., Agarwal R., Deep G. Exosomes secreted under hypoxia enhance invasiveness and stemness of prostate cancer cells by targeting adherens junction molecules. Mol. Carcinog. 2015;54:554–565. doi: 10.1002/mc.22124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wortzel I., Dror S., Kenific C.M., Lyden D. Exosome-Mediated Metastasis: Communication from a Distance. Dev. Cell. 2019;49:347–360. doi: 10.1016/j.devcel.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 116.Liu Y., Cao X. Characteristics and Significance of the Pre-metastatic Niche. Cancer Cell. 2016;30:668–681. doi: 10.1016/j.ccell.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 117.Henrich S.E., McMahon K.M., Plebanek M.P., Calvert A.E., Feliciano T.J., Parrish S., Tavora F., Mega A., De Souza A., Carneiro B.A., et al. Prostate cancer extracellular vesicles mediate intercellular communication with bone marrow cells and promote metastasis in a cholesterol-dependent manner. J. Extracell. Vesicles. 2020;10:e12042. doi: 10.1002/jev2.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhang C., Ji Q., Yang Y., Li Q., Wang Z. Exosome: Function and Role in Cancer Metastasis and Drug Resistance. Technol. Cancer Res. Treat. 2018;17 doi: 10.1177/1533033818763450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Guise T. Examining the metastatic niche: Targeting the microenvironment. Semin. Oncol. 2010;37(Suppl. S2):S2–S14. doi: 10.1053/j.seminoncol.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 120.Borel M., Lollo G., Magne D., Buchet R., Brizuela L., Mebarek S. Prostate cancer-derived exosomes promote osteoblast differentiation and activity through phospholipase D2. Biochim. Biophys. Acta Mol. Basis Dis. 2020;1866:165919. doi: 10.1016/j.bbadis.2020.165919. [DOI] [PubMed] [Google Scholar]
- 121.Valastyan S., Weinberg R.A. Tumor metastasis: Molecular insights and evolving paradigms. Cell. 2011;147:275–292. doi: 10.1016/j.cell.2011.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Syn N., Wang L., Sethi G., Thiery J.P., Goh B.C. Exosome-Mediated Metastasis: From Epithelial-Mesenchymal Transition to Escape from Immunosurveillance. Trends Pharm. Sci. 2016;37:606–617. doi: 10.1016/j.tips.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 123.Spugnini E.P., Logozzi M., Di Raimo R., Mizzoni D., Fais S. A Role of Tumor-Released Exosomes in Paracrine Dissemination and Metastasis. Int. J. Mol. Sci. 2018;19:3968. doi: 10.3390/ijms19123968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Webber J., Steadman R., Mason M., Tabi Z., Clayton A. Cancer Exosomes Trigger Fibroblast to Myofibroblast Differentiation. Cancer Res. 2010;70:9621–9630. doi: 10.1158/0008-5472.CAN-10-1722. [DOI] [PubMed] [Google Scholar]
- 125.Diana B.-D., Donald J.T. TGF-β/Smad Signaling in Prostate Cancer. Curr. Drug Targets. 2003;4:197–207. doi: 10.2174/1389450033491118. [DOI] [PubMed] [Google Scholar]
- 126.McAtee C.O., Booth C., Elowsky C., Zhao L., Payne J., Fangman T., Caplan S., Henry M.D., Simpson M.A. Prostate tumor cell exosomes containing hyaluronidase Hyal1 stimulate prostate stromal cell motility by engagement of FAK-mediated integrin signaling. Matrix Biol. 2019;78–79:165–179. doi: 10.1016/j.matbio.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bijnsdorp I.V., Geldof A.A., Lavaei M., Piersma S.R., van Moorselaar R.J., Jimenez C.R. Exosomal ITGA3 interferes with non-cancerous prostate cell functions and is increased in urine exosomes of metastatic prostate cancer patients. J. Extracell. Vesicles. 2013;2 doi: 10.3402/jev.v2i0.22097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Abd Elmageed Z.Y., Yang Y., Thomas R., Ranjan M., Mondal D., Moroz K., Fang Z., Rezk B.M., Moparty K., Sikka S.C., et al. Neoplastic reprogramming of patient-derived adipose stem cells by prostate cancer cell-associated exosomes. Stem Cells. 2014;32:983–997. doi: 10.1002/stem.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Honeywell D.R., Cabrita M.A., Zhao H., Dimitroulakos J., Addison C.L. miR-105 inhibits prostate tumour growth by suppressing CDK6 levels. PLoS ONE. 2013;8:e70515. doi: 10.1371/journal.pone.0070515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Oliveira-Ferrer L., Milde-Langosch K., Eylmann K., Rossberg M., Müller V., Schmalfeldt B., Witzel I., Wellbrock J., Fiedler W. Mechanisms of Tumor-Lymphatic Interactions in Invasive Breast and Prostate Carcinoma. Int. J. Mol. Sci. 2020;21:602. doi: 10.3390/ijms21020602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Datta K., Muders M., Zhang H., Tindall D.J. Mechanism of lymph node metastasis in prostate cancer. Future Oncol. 2010;6:823–836. doi: 10.2217/fon.10.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sepúlveda L., Gorgal T., Pires V., Rodrigues F. Prostate Cancer Metastatic to the Cervical Lymph Nodes. Case Rep. Urol. 2015;2015:263978. doi: 10.1155/2015/263978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zang G., Mu Y., Gao L., Bergh A., Landstrom M. PKCzeta facilitates lymphatic metastatic spread of prostate cancer cells in a mice xenograft model. Oncogene. 2019;38:4215–4231. doi: 10.1038/s41388-019-0722-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Clayton A., Turkes A., Navabi H., Mason M.D., Tabi Z. Induction of heat shock proteins in B-cell exosomes. J. Cell Sci. 2005;118:3631. doi: 10.1242/jcs.02494. [DOI] [PubMed] [Google Scholar]
- 135.Yen E.-Y., Miaw S.-C., Yu J.-S., Lai I.R. Exosomal TGF-β1 is correlated with lymphatic metastasis of gastric cancers. Am. J. Cancer Res. 2017;7:2199–2208. [PMC free article] [PubMed] [Google Scholar]
- 136.Weidle U.H., Birzele F., Kollmorgen G., Rüger R. The Multiple Roles of Exosomes in Metastasis. Cancer Genom. Proteom. 2017;14:1–15. doi: 10.21873/cgp.20015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Liu S.-L., Sun P., Li Y., Liu S.-S., Lu Y. Exosomes as critical mediators of cell-to-cell communication in cancer pathogenesis and their potential clinical application. Transl. Cancer Res. 2019;8:298–311. doi: 10.21037/tcr.2019.01.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Khan S., Jutzy J.M.S., Valenzuela M.M.A., Turay D., Aspe J.R., Ashok A., Mirshahidi S., Mercola D., Lilly M.B., Wall N.R. Plasma-Derived Exosomal Survivin, a Plausible Biomarker for Early Detection of Prostate Cancer. PLoS ONE. 2012;7:e46737. doi: 10.1371/journal.pone.0046737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Shariat S.F., Lotan Y., Saboorian H., Khoddami S.M., Roehrborn C.G., Slawin K.M., Ashfaq R. Survivin expression is associated with features of biologically aggressive prostate carcinoma. Cancer. 2004;100:751–757. doi: 10.1002/cncr.20039. [DOI] [PubMed] [Google Scholar]
- 140.Maolake A., Izumi K., Natsagdorj A., Iwamoto H., Kadomoto S., Makino T., Naito R., Shigehara K., Kadono Y., Hiratsuka K., et al. Tumor necrosis factor-α induces prostate cancer cell migration in lymphatic metastasis through CCR7 upregulation. Cancer Sci. 2018;109:1524–1531. doi: 10.1111/cas.13586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kodidela S., Ranjit S., Sinha N., McArthur C., Kumar A., Kumar S. Cytokine profiling of exosomes derived from the plasma of HIV-infected alcohol drinkers and cigarette smokers. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0201144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gaballa R., Ali H.E.A., Mahmoud M.O., Rhim J.S., Ali H.I., Salem H.F., Saleem M., Kandeil M.A., Ambs S., Abd Elmageed Z.Y. Exosomes-Mediated Transfer of Itga2 Promotes Migration and Invasion of Prostate Cancer Cells by Inducing Epithelial-Mesenchymal Transition. Cancers. 2020:2300. doi: 10.3390/cancers12082300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Mahon K.L., Henshall S.M., Sutherland R.L., Horvath L.G. Pathways of chemotherapy resistance in castration-resistant prostate cancer. Endocr. Relat. Cancer. 2011;18:R103–R123. doi: 10.1530/ERC-10-0343. [DOI] [PubMed] [Google Scholar]
- 144.Mansoori B., Mohammadi A., Davudian S., Shirjang S., Baradaran B. The Different Mechanisms of Cancer Drug Resistance: A Brief Review. Adv. Pharm. Bull. 2017;7:339–348. doi: 10.15171/apb.2017.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Semenas J., Allegrucci C., Boorjian S.A., Mongan N.P., Persson J.L. Overcoming drug resistance and treating advanced prostate cancer. Curr. Drug Targets. 2012;13:1308–1323. doi: 10.2174/138945012802429615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bhagirath D., Yang T.L., Tabatabai Z.L., Majid S., Dahiya R., Tanaka Y., Saini S. BRN4 Is a Novel Driver of Neuroendocrine Differentiation in Castration-Resistant Prostate Cancer and Is Selectively Released in Extracellular Vesicles with BRN2. Clin. Cancer Res. 2019;25:6532–6545. doi: 10.1158/1078-0432.CCR-19-0498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Corcoran C., Rani S., O’Brien K., O’Neill A., Prencipe M., Sheikh R., Webb G., McDermott R., Watson W., Crown J., et al. Docetaxel-resistance in prostate cancer: Evaluating associated phenotypic changes and potential for resistance transfer via exosomes. PLoS ONE. 2012;7:e50999. doi: 10.1371/journal.pone.0050999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Kharaziha P., Chioureas D., Rutishauser D., Baltatzis G., Lennartsson L., Fonseca P., Azimi A., Hultenby K., Zubarev R., Ullén A., et al. Molecular profiling of prostate cancer derived exosomes may reveal a predictive signature for response to docetaxel. Oncotarget. 2015;6:21740–21754. doi: 10.18632/oncotarget.3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Vlaeminck-Guillem V. Extracellular Vesicles in Prostate Cancer Carcinogenesis, Diagnosis, and Management. Front. Oncol. 2018;8:222. doi: 10.3389/fonc.2018.00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Aalberts M., Stout T.A., Stoorvogel W. Prostasomes: Extracellular vesicles from the prostate. Reproduction. 2014;147:R1–R14. doi: 10.1530/REP-13-0358. [DOI] [PubMed] [Google Scholar]
- 151.Drake R.R., Kislinger T. The proteomics of prostate cancer exosomes. Expert Rev. Proteom. 2014;11:167–177. doi: 10.1586/14789450.2014.890894. [DOI] [PubMed] [Google Scholar]
- 152.Tian W., Liu S., Li B. Potential Role of Exosomes in Cancer Metastasis. Biomed. Res. Int. 2019;2019 doi: 10.1155/2019/4649705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Barcelo M., Castells M., Bassas L., Vigues F., Larriba S. Semen miRNAs Contained in Exosomes as Non-Invasive Biomarkers for Prostate Cancer Diagnosis. Sci. Rep. 2019;9:13772. doi: 10.1038/s41598-019-50172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Foj L., Ferrer F., Serra M., Arévalo A., Gavagnach M., Giménez N., Filella X. Exosomal and Non-Exosomal Urinary miRNAs in Prostate Cancer Detection and Prognosis. Prostate. 2017;77:573–583. doi: 10.1002/pros.23295. [DOI] [PubMed] [Google Scholar]
- 155.Arrighetti N., Corbo C., Evangelopoulos M., Pastò A., Zuco V., Tasciotti E. Exosome-like Nanovectors for Drug Delivery in Cancer. Curr. Med. Chem. 2019;26:6132–6148. doi: 10.2174/0929867325666180831150259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Elsharkasy O.M., Nordin J.Z., Hagey D.W., de Jong O.G., Schiffelers R.M., Andaloussi S.E., Vader P. Extracellular vesicles as drug delivery systems: Why and how? Adv. Drug Deliv. Rev. 2020;159:332–343. doi: 10.1016/j.addr.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 157.Xu X., Saw P.E., Tao W., Li Y., Ji X., Bhasin S., Liu Y., Ayyash D., Rasmussen J., Huo M., et al. ROS-Responsive Polyprodrug Nanoparticles for Triggered Drug Delivery and Effective Cancer Therapy. Adv. Mater. 2017;29 doi: 10.1002/adma.201700141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Di C., Zhang Q., Wang Y., Wang F., Chen Y., Gan L., Zhou R., Sun C., Li H., Zhang X., et al. Exosomes as drug carriers for clinical application. Artif. Cells Nanomed. Biotechnol. 2018;46:S564–S570. doi: 10.1080/21691401.2018.1501381. [DOI] [PubMed] [Google Scholar]
- 159.Barile L., Vassalli G. Exosomes: Therapy delivery tools and biomarkers of diseases. Pharmacol. Ther. 2017;174:63–78. doi: 10.1016/j.pharmthera.2017.02.020. [DOI] [PubMed] [Google Scholar]
- 160.Batrakova E.V., Kim M.S. Using exosomes, naturally-equipped nanocarriers, for drug delivery. J. Control. Release Off. J. Control. Release Soc. 2015;219:396–405. doi: 10.1016/j.jconrel.2015.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kosaka N., Iguchi H., Yoshioka Y., Hagiwara K., Takeshita F., Ochiya T. Competitive Interactions of Cancer Cells and Normal Cells via Secretory MicroRNAs. J. Biol. Chem. 2012;287:1397–1405. doi: 10.1074/jbc.M111.288662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Saari H., Lázaro-Ibáñez E., Viitala T., Vuorimaa-Laukkanen E., Siljander P., Yliperttula M. Microvesicle- and exosome-mediated drug delivery enhances the cytotoxicity of Paclitaxel in autologous prostate cancer cells. J. Control. Release. 2015;220:727–737. doi: 10.1016/j.jconrel.2015.09.031. [DOI] [PubMed] [Google Scholar]