Abstract
Occupational lung diseases (OLDs) are caused, aggravated or exacerbated by exposures at the workplace. OLDs encompass a wide range of respiratory diseases similar to that found outside the work environment. Occupational asthma is the most commonly diagnosed OLD. Other OLDs may include acute and chronic conditions, ranging from hypersensitivity pneumonitis to chronic obstructive pulmonary disease (COPD) to pulmonary fibrosis. Historically, research into OLDs has centered on diseases resulting from exposures relevant to high-income countries and more obvious hazardous occupations, such as silicosis in coal miners. Peer-reviewed publications in 2019 have broadened the focus to include low- and middle-income countries and once-overlooked occupations such as dry cleaning and animal husbandry. Technological advances and greater understanding of disease etiology have allowed researchers and clinicians to implement improved risk analysis, screening and mitigation strategies to not only treat disease once it occurs, but to identify at-risk populations and institute protections to prevent or limit the negative impacts of workplace hazards. As recognition of OLDs as a worldwide threat in a variety of occupations increases, research is allowing for the development of better treatments and preventive measures that advance workers’ rights and ensure their continued good health.
Supplementary Information
The online version contains supplementary material available at 10.1007/s41030-020-00143-4.
Keywords: Asthma, COPD, Occupational lung disease, Pneumoconiosis, Pulmonary fibrosis, Small airways disease
Enhanced feature (slides, video, animation) (MP4 17252 kb)
Enhanced feature (slides, video, animation) (MP4 54866 kb)
Key Summary Points
| Workplace exposures contribute substantially to the burden of chronic respiratory diseases, including asthma, COPD, chronic bronchitis, idiopathic pulmonary fibrosis, hypersensitivity pneumonitis, other granulomatous diseases (including sarcoidosis), pulmonary alveolar proteinosis, tuberculosis, community-acquired pneumonia, and classic occupational pneumoconiosis. |
| Occupational lung diseases are often misattributed to non-occupational causes, leading to delayed or improper medical management of patients. |
| Respirable fine crystalline silica in coal mine dust has been implicated in the recent resurgence of coal workers’ pneumoconiosis in the United States. |
| The most common specific diagnosis in previously deployed US military personnel in Southwest Asia and Afghanistan is asthma. |
| Among patients with sensitizer-induced occupational asthma, 16% have severe disease, which is predicted by persistent exposure and longer duration of disease. |
| Occupational exposures are associated with incident chronic phlegm and chronic bronchitis, and the evidence is strongest for mineral dust exposure and metals. |
Digital Features
This article is published with digital features, including a summary slide and video abstracts, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13313066.
Introduction
Occupational lung diseases (OLDs) and non-occupational lung diseases are often clinically indistinguishable, but are differentiated from one another based upon etiology. Lung diseases are described as occupational if they are caused, aggravated or exacerbated by exposure in the workplace. Incriminating exposures might include respirable dusts (such as coal mine dust and silica), fumes, vapors, gases, volatile organic compounds, man-made vitreous fibers, chemicals, metals and infectious pathogenic materials. Inhalational hazards remain common in workplaces throughout the world, but they are largely avoidable. OLDs are a commonly diagnosed work-related illness, but in the absence of an occupational history they are indistinguishable from similarly named diseases that occur in the general population (Table 1). The distinction is important, however, because properly addressing a causative workplace exposure is often key to providing effective treatment. Unfortunately, to the detriment of patients, OLDs are frequently ignored, misdiagnosed and misattributed to non-occupational causes.
Table 1.
Common occupational diseases that may be misdiagnosed as non-occupational
| Non-occupational disease | Occupational disease |
|---|---|
| Asthma | Sensitizer-induced occupational asthma |
| Irritant-induced asthma/reactive airways dysfunction syndrome | |
| Work-exacerbated asthma | |
| COPD | Occupational COPD |
| Irritant (chronic) bronchitis | |
| Pneumonia | Hypersensitivity pneumonitis |
| Acute chemical pneumonitis | |
| Idiopathic pulmonary fibrosis | Asbestosis |
| Coal workers' pneumoconiosis | |
| Uranium workers' pneumoconiosis | |
| Hard metal disease | |
| Chronic hypersensitivity pneumonitis | |
| Sarcoidosis | Chronic beryllium disease |
| Chronic hypersensitivity pneumonitis | |
| Aluminum-induced pulmonary granulomatosis |
OLDs include a wide range of benign and malignant pathologies occurring anywhere from the upper respiratory tract to the alveoli. They encompass a range of pulmonary diseases including obstructive diseases such as chronic obstructive lung disease (COPD) and asthma; restrictive diseases such as pulmonary fibrosis (PF); mixed obstructive and restrictive lung diseases (such as pneumoconiosis and hypersensitivity pneumonitis); and cancers (such as mesothelioma and lung cancers). These diseases may be acute, subacute or chronic, and may occur with or without latency. While some OLDs cause permanent impairment, others may resolve with treatment or removal from the inciting work-related exposure.
The objective of this review is to provide a 2019 update on OLDs. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors. The sources of information contained in this review include peer-reviewed literature in PubMed (using search terms: occupational lung disease, work-related lung disease, occupational airway disease, work-related airway disease, lung disease at work, and airway disease at work, restricted to the year 2019).
Selected At-Risk Populations and Occupations
While many occupations put workers at risk for OLD, the iconic image is that of coal miners developing “black lung,” the popular and legal term for coal mine dust lung disease from inhalation of heterogeneous exposures in coal mines. While coal mining remains an important industry in the United States, domestic production is declining as other means of energy production gain favor. Some low- and middle-income countries (LMICs) also consider coal an important industry, but the trend worldwide is downward. With mining becoming less common, the economics and demographics associated with OLDs are changing away from black lung. A 2015 publication on the global burden of disease recorded the most pronounced rises for various occupational exposures, such as diesel engine exhaust, silica and benzene. Between 1990 and 2015, there were increases in average occupational exposure to diesel exhaust (72.1% men; 129.8% women), silica (72.6% men; 44.9% women) and benzene (48.5% men; 97.5% women) [1]. Current research reflects this, as investigators focus on new and once-neglected occupations and exposures associated with OLDs.
Coal Workers
Although once in decline, coal workers’ pneumoconiosis has seen a recent resurgence in prevalence and severity in the United States [2]. While the cause for this resurgence is not known, respirable fine crystalline silica, silicates and metal content of coal mine dust has been implicated. Hall et al. [3] assessed the prevalence of r-type opacities (rounded pneumoconiotic opacities measuring 3–10 mm in diameter typically associated with silicosis lung pathology) during 2010–2018 compared with earlier decades. Nationwide data from the US Coal Workers' Health Surveillance Program included chest radiographs of 106,506 working underground coal miners. Compared to chest radiographs of miners taken during 1980–1989, the prevalence of r-type opacities in similar radiographs had increased during the 2010–2018 period (prevalence ratio or PR 2.4). In central Appalachia, the relative increase in prevalence during these times periods was six times greater (PR 6.0). This study demonstrates the growing prevalence of r-type opacities in chest radiographs of Appalachian underground coal miners. The findings suggest significant occupational exposure to respirable crystalline silica in coal mine dust by workers. Therefore, there likely remains an ongoing need to control and monitor for silica exposure in US coal mines [3].
Silica-Exposed Workers in “Emerging” Industries
Silica-associated lung disease has long been recognized as a significant cause of morbidity and mortality in miners. Increasingly, silica-associated lung disease is being seen in workers in other industries, and often these workers are developing acute as well as chronic silicosis due to high exposures without appropriate protection. Barnes et al. examined silica-associated lung disease in several countries and in a variety of occupations that potentially expose workers to harmful amounts of silica dust. These industries ranged from stonemasons, to slate pencil workers, dental tool suppliers, jewelry makers, sandblasters and denim jean manufacturers, among others. These industries have been largely overlooked as risk factors for silica-related lung diseases in workers. As such, early and aggressive screening and interventions are needed to protect the health of workers in a variety of silica-using industries around the world [4]. As trends indicate a shift away from US-based manufacturing, particular focus should be directed toward workers in LMICs.
Equestrian Workers
Given that equestrian arenas and training facilities are often grounded with silica-containing sand, workers in this industry represent an at-risk group for OLDs. In a small study, Bulfin et al. examined the exposure of equestrian workers to respirable crystalline silica and dust. They determined that workers in these environments were exposed to clinically significant levels of respirable crystalline silica and dust. The highest levels of exposure occurred when the ground was not watered versus when it was. While recommending watering of arena grounds to reduce airborne particle exposure, the authors acknowledged this is a labor-intensive practice and therefore unlikely to be widely implemented. A comprehensive approach utilizing a group of efforts to reduce equestrian worker exposure to respirable crystalline silica and dust, such as occupational health training of these workers, is a more achievable solution [5].
Military Personnel
Since 2001, US military operations in Southwest Asia and Afghanistan have required the deployment of over 2.7 million personnel. Land-based personnel in these campaigns have been exposed to a complex mixture of airborne pollutants. These included elevated levels of particulate matter (PM2.5), desert dust, and various other organic and inorganic inhalational exposures from sources including combustion from burn pits. In a recent workshop held during the 2018 American Thoracic Society International Conference, epidemiologic studies and case series on this topic were reviewed. It was demonstrated that there were more frequent encounters for respiratory symptoms, airway diseases (predominantly asthma) and a variety of other abnormal respiratory tract findings in deployers versus non-deployers. When compared to the pulmonary system effects of airborne particulates seen in other populations, it is possible that due to exposures from their work in Southwest Asia and Afghanistan, deployers have developed lung diseases and a resultant decrease in pulmonary function. Other common symptoms present in both smokers and nonsmokers who sought medical evaluation included exertional dyspnea, cough, chest tightness and wheezing. The authors note that data from sources that regularly study this population showed that asthma is the most common specific diagnosis in previously deployed military populations. In fact, approximately 50% of deployers discharged from the military with asthma did not have an asthma diagnosis prior to enlistment [6].
Another area of focus for this workshop was constrictive bronchiolitis. This topic was considered because of past reports that lung biopsies from selected deployers showed evidence of this diagnosis. However, workshop participants had a wide range of opinions concerning how to properly define and measure the frequency of constrictive bronchiolitis and other small airway pathology observed in the study populations. Some participants expressed concern that diagnostic criteria based on lung biopsies had not been consistently applied across the studies reviewed. The workshop found that airway disease, including constrictive bronchiolitis, may be related to exposures occurring while personnel were deployed. However, additional research is needed to fully characterize any potential causal relationships and to evaluate future risk of ex-servicemen developing OLDs as a consequence of their deployment [6].
Healthcare Workers
Because of the nature of their profession, healthcare workers (HCWs) are at increased risk for contracting many infectious respiratory diseases. In particular, HCWs are at increased risk for latent tuberculosis (TB) infection (LTBI) and active TB disease. A recent systematic review examined the prevalence and incidence of LTBI in HCWs in LMICs, using articles published from 2005 to 2017 [7]. Eighty-five studies (32,630 subjects) from 26 LMICs were examined using pooled estimates using random effects methods. The review determined that LMICs had a high prevalence and incidence of LTBI in HCWs and healthcare students (HCSs), as measured by positive tuberculin skin test (TST) or interferon gamma release assay (IGRA). TST positivity rates were approximately 50% for HCWs and 32% for HCSs, while IGRA was positive in 39% of HCWs and 25% of HCSs. The group with the highest prevalence of positive TST was nurses (pooled estimate 54%), while the highest prevalence of positive IGRAs was found in general service workers including cleaners, drivers and housekeepers (pooled estimate 60%). Physicians had the second highest prevalence of a positive TST or IGRA (48% and 35%, respectively) among HCW categories. LMICs with the highest TB incidence also had HCWs with the highest prevalence of LTBI. The annual incidence of LTBI as estimated from serial TSTs was 17% in HCWs and 5% in HCSs. In contrast, serial IGRA estimates showed an annual incidence of 18% and 8% in HCWs and HCSs, respectively. Variables with which the prevalence and incidence of test positivity was found to be associated with were: years of work, location of work, job type, and contact with TB. The study’s authors concluded that HCWs in LMICs in work settings with high TB incidence are at unacceptably high risk of developing LTBI. In resource-limited settings, it was found that effective and affordable basic control measures endorsed by the World Health Organization (WHO) are rarely implemented. It is imperative that TB programs in countries with high TB incidence make TB infection control measures in healthcare facilities a priority. Doing so will ensure HCWs and HCSs a safe work environment [7].
Cleaning Service Workers
Although asthma incidence in the general population has declined over time, the incidence of occupational asthma, the most commonly reported OLD in developed nations, has not. It is estimated that workplace exposures account for 16% of cases of adult-onset asthma [8]. Carder et al. [9] evaluated a variety of cleaning agents and the occupations at greatest risk of exposure and development of OLDs from 1999 to 2017. Launderers, dry cleaners and pressers were found to have the greatest risk of lung diseases resulting from occupational exposures to cleaning products. Asthma was the most commonly reported OLD in these workers, followed by acute inhalation incidents. The most frequently encountered chemicals were aldehydes and chlorine. The authors pointed out that while concerns over some chemicals have been addressed, workers are still encountering other chemicals that place them at increased risk for occupational pulmonary diseases. Action must be taken to address these new concerns and decrease the risk for workers developing these diseases [9].
Genetic/Epigenetic Factors
A minority of exposed workers develop OLDs, but determining who will develop disease as a result of an occupational exposure remains a challenge. Genetics and epigenetics are rapidly growing fields that may help explain worker susceptibility to OLDs. An example is chronic beryllium disease (CBD), an OLD that develops in a minority of about one million American workers exposed to beryllium dust each year. Yang et al. [10] investigated the role of environment, genetics and epigenetics in the development of pulmonary disease from beryllium exposure. Previous genetic association studies have indicated that some gene variants, such as HLA class II immune responses, can predispose to CBD. This, however, does not completely explain the differences in CBD progression. The researchers examined methylation patterns in lung cells from bronchoalveolar lavage specimens of patients exposed to beryllium and followed them over two years to evaluate epigenetic differences amongst those developing CBD versus beryllium sensitization without CBD. The groups were matched on age, sex, race and ethnicity. The researchers found significant differences in genes involved in immune responses, especially Th1 and Th17 responses, between the two groups. They also compared observed methylation patterns in patients with CBD to those with sarcoidosis, an idiopathic disease with granulomas similar to those found in CBD. Differences in methylation patterns were again found, although the results were less robust. This study was significant by being the first to examine epigenetic differences in the development of CBD, and lays the foundation for future research on worker susceptibility to OLDs [10]. This may lead the way to improved methods of prevention, disease screening and occupational health counseling.
Classification of Occupational Lung Disease
OLD is not a single diagnosis, but rather encompasses a range of pulmonary diseases. Multiple phenotypes of lung disease may coexist in a worker, as described with coal mine dust lung disease, which includes classic nodular pneumoconiosis, COPD, dust-related diffuse fibrosis, and small airways disease [11].
Overall Occupational Disease Burden
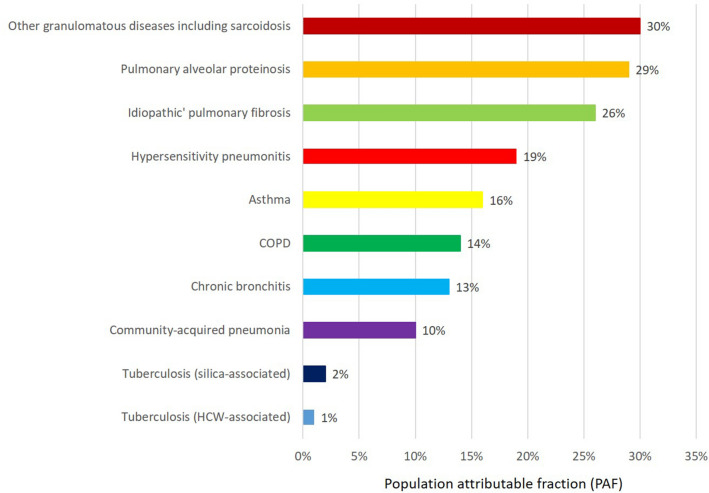
To examine trends in disease burden, Blanc et al. [8] performed an in-depth literature review and data synthesis of the occupational contribution to the burden of major nonmalignant respiratory diseases. For conditions for which there could be found sufficient population-based studies to permit pooled estimates, the occupational population attributable fraction (PAF) was estimated. For other conditions, occupational disease burden was estimated by attribution in case series, incidence rate ratios, or attributable fraction found in an exposed group. It was determined that exposures in the work environment substantially contribute to the burden of a range of chronic respiratory diseases. This includes idiopathic pulmonary fibrosis (PAF, 26%); asthma (PAF, 16%); COPD (PAF, 14%); chronic bronchitis (PAF, 13%); other granulomatous diseases such as sarcoidosis (occupational burden, 30%); pulmonary alveolar proteinosis (occupational burden, 29%); hypersensitivity pneumonitis (occupational burden, 19%); tuberculosis (occupational burden, 2.3% and 1% in silica-exposed workers and HCWs); and community-acquired pneumonia in working-age adults (PAF, 10%). Not counting the classic occupational pneumoconiosis (PAF, 100%), as shown in Fig. 1 [8], granulomatous diseases, such as sarcoidosis, have the highest occupational burden (30%), and can be seen among beryllium and other metal-exposed workers, as well as firefighters, workers in the lumber industry, rock or glass wool workers and emergency responders to the World Trade Center disaster in 2001. Pulmonary alveolar proteinosis, the disease with the second highest occupational burden (29%), was associated with a broad range of exposures including vapors or gases such as cleaning fluids and hair spray, inorganic dust such as silica (PAF for silica 5%), organic dust such as wood and metal dusts or fumes such as aluminum. “Idiopathic” pulmonary fibrosis, the disease with the third highest occupational burden (26%), was associated with exposure to vapors, gases, dusts or fumes (VGDF) (PAF of 26%), metal dust or fume (PAF 8%), wood dust (PAF 4%), silica dust (PAF 3%) and agricultural dust (PAF 4% not statistically significant). This analysis suggests that there exists a significant occupational burden for a variety of respiratory conditions that are not typically associated with work. An important limitation of this analysis is study heterogeneity [8].
Fig. 1.
Summary of the occupational burden of nonmalignant respiratory disease, by condition, using population attributable fractions
Asthma
Although sensitizer-induced occupational asthma (OA) accounts for a substantial amount of adult asthma, detailed study of asthma severity is lacking. A study by Vandenplas et al. [12] endeavored to describe the burden and determinants of severe sensitizer-induced OA. This was a retrospective study that looked at the period from 2006 to 2015. It involved 997 subjects with OA, as determined by a positive specific inhalation challenge performed in 20 tertiary centers in 11 European countries. The researchers defined severe asthma as that requiring a high level of treatment in addition to any one of the following criteria: (1) daily need for reliever medication, (2) two or more severe exacerbations in the previous year, or (3) spirometric airflow obstruction. In all, there were 162 (16.2%) subjects classified as having severe OA. Through a multivariable analysis, researchers determined that severe OA was associated with persistent exposure to a causal agent in the work environment (OR 2.78); longer disease duration (OR 1.04); a low level of education (OR 2.69); history of childhood asthma (OR 2.92); and sputum production (OR 2.86). This study indicates that in subjects with OA, a considerable proportion have severe asthma, and it identifies risk factors for severe disease that are modifiable [12]. The study supports the current recommendation of cessation of incriminating exposure in patients with sensitizer-induced OA.
Logar-Henderson et al. [13] performed a large-scale evaluation of adult asthma in different occupations using the Occupational Disease Surveillance System in 575,379 individuals aged 15–65 years. Using this large dataset, they were able to identify linkages between asthma and various occupations. Increased disease risks were detected among common job classifications, including bakers (hazard ratio or HR 1.60), and painters and decorators (HR 1.67). Flour and isocyanates were associated with increased asthma risk in the job exposure matrix analysis. Increased risk was also demonstrated in concrete finishers (HR 1.93) and shipping and receiving clerks (HR 1.21), in contrast to groups of woodworkers whose results were variable. Decreased risks were found among nursing and farming groups. This large study was innovative in that it utilized purely administrative data. The authors were able to find connections between asthma and different occupations that would be impossible with a less comprehensive dataset [13].
COPD
As discussed previously, the occupational PAF is estimated at 14% and 13% for COPD and chronic bronchitis, respectively [8]. The Faces of Work-related COPD video series published in 2019 by the US National Occupational Research Agenda (NORA) provides useful information on causes, presentation, treatment and impact on patient quality of life of work-related COPD, available at: https://www.cdc.gov/nora/councils/resp/FacesCOPD.html.
Lytras et al. [14] examined chronic bronchitis specifically through a retrospective analysis of disease incidence, symptoms and exposure history. Chronic bronchitis (CB), defined by cough and phlegm production for most days for at least 3 months annually for two or more consecutive years, is an important COPD-related phenotype and has distinct clinical features and prognostic implications. CB risk has previously been associated with occupational exposures, but few studies have evaluated this association prospectively with objective assessments of exposure. Investigators in this study examined the effect of occupational exposures on CB incidence in the European Community Respiratory Health Survey. They randomly selected population samples aged 20–44 years in 1991–1993, and follow-up occurred twice over a 20-year period. Participants without baseline chronic cough or phlegm were analyzed prospectively. Coded job histories during follow-up were linked to a job exposure matrix. Then, occupational exposure estimates to 12 chemical agent categories were generated. A total of 8794 participants met inclusion criteria and contributed 13,185 total observations. Only participants who were exposed to metals had a higher incidence of CB (relative risk [RR] 1.7) compared with those not exposed to metals. Occupations involving any exposure to metals in the study included jobs such as motor vehicle mechanics, other machinery engineers and technicians, plumbers and pipefitters. Although metals are a heterogeneous category of exposure, one metal in particular, i.e., vanadium, present in steel and in fossil fuels, has both occupational epidemiologic and experimental evidence of an association with bronchitis. Mineral dust exposure similarly increased the incidence of chronic phlegm (RR 1.7). Occupations involving mineral dust exposure include truck and lorry drivers, and helpers/cleaners in offices, hotels and other establishments. Incidence of chronic phlegm was found to be increased in men exposed to gases/fumes and to solvents, and in women with exposure to pesticides. The strengths of the study include prospective design, long follow-up of 20 years and a large population size. The study demonstrates that occupational exposures are associated with chronic phlegm and CB, with the strongest evidence being for exposure to metals and mineral dust [14].
An important way to mitigate incidence of work-related COPD is to determine which occupations are at greatest risk. Utilizing the UK Biobank cohort, De Matteis et al. [15] evaluated an estimated 100,000 individuals with complete spirometry results and job histories to determine which professions were most at risk for developing COPD. Because of the unprecedentedly large sample size, the researchers were able to include only never-smokers (a positive tobacco smoking history was the largest confounder identified). Among never-smokers, they found six occupation categories to be at highest risk: “sculptor, painter, engraver, art restorer”; “gardener, groundsman, park keeper”; “food, drink and tobacco processor”; “plastics processor, moulder”; “agriculture, and fishing occupations not elsewhere classified”; and “warehouse stock handler, stacker.” Furthermore, these associations were confirmed among never-asthmatics as well. This information can aid in the development of focused preventive strategies in targeted occupations to reduce work-related COPD development [15].
Causation and Diagnosis of Occupational Lung Disease
Diagnosis of OLDs may be difficult due to a challenge in determining causation. For instance, work-related and non-work-related asthma may be clinically indistinguishable from one another, in the absence of a carefully taken occupational history and confirmatory data. Diagnosis of OLD must therefore rely upon interpreting the occupational history and confirmatory data in relation to the epidemiologic evidence of an association between a particular causative agent in the workplace and a particular pulmonary pathology. Disease causation may, however, be confounded by co-exposures. An example would be that of COPD in a miner co-exposed to smoking. Epidemiologic evidence shows that smoking coal workers have higher rates of and more severe COPD than do tobacco smokers who are not coal workers or coal workers who are not smokers, implying an additive effect of dust and smoking on risk for COPD [16]. Sometimes, the co-exposures may be environmental, and involve large segments of the working and non-working population. For example, both environmental and occupational exposure to asbestos is a relevant health problem in Turkey, a country with high rates of exposure to naturally occurring asbestos [17. This could logically extend to many types of occupational exposures beyond asbestos, and surveillance systems must be adequately aware of risks in order to be able to assess them. Another common difficulty is the confusion regarding the level of certainty required to establish causation—usually > 50%, as opposed to > 95% used in scientific research [18]. In addition to the strength of epidemiological association, the cardinal principles that are considered in determining causation include the latency, intensity and duration of exposure, as obtained by a careful occupational history [18]. The foundation of objective confirmation of OLD is spirometry. In 2019, the American and European respiratory organizations issued new guidelines regarding the use and interpretation of spirometry. This represented a fundamental change to various aspects of how spirometry was used and interpreted, changing the criteria for test acceptability and for grading test quality, and introducing the new concept of usability of test [19].
Prevention and Treatment of Occupational Lung Disease
OLDs are typically treated by primary care providers, occupational medical physicians and/or pulmonologists. Acute-onset diseases may resolve on their own, once the employee is removed from the offending exposure. Chronic diseases are often indolent, often with a latency period, and show a slow progression over many years or decades. Often, by the time of diagnosis, many pulmonary conditions have sufficiently progressed so that the most effective treatments are symptomatic.
Treatments for OLDs are largely the same as that for non-OLDs. For instance, occupational and non-occupational asthma are similarly treated with inhaled bronchodilators, inhaled corticosteroids, mast cell stabilizers, among other common medications. Asthma does have effective treatments, although no cure. Other diseases also have treatments, but the effectiveness of these treatments may be to slow progression or treat symptoms, but they are not disease-modifying. For instance, occupational COPD is treated like non-occupational COPD with modalities such as supplemental oxygen, outpatient pulmonary rehabilitation, vaccinations, lifestyle changes with exercise and diet, medications and surgical interventions such as lung transplantation or lung volume reduction. Some progressive fibrotic diseases, for instance, have recently developed anti-fibrosis treatments, such as the tyrosine kinase inhibitor nintedanib, that may help mitigate lung function decline [20]. However, even with such treatments, these diseases will typically progress over time and lead to significant mortality. Because of difficulties in treatment, preventing OLD remains the most effective strategy.
Most surveillance programs use symptom questionnaires, spirometry and/or chest radiographs classified using the International Labor Organization Classification of Chest Radiographs for Pneumoconiosis (i.e., B-reads). Cancers of the lung and pleura are diseases for which computed tomography (CT) screening programs are in place to catch disease early. These screening programs are in line with the current professional guidelines to perform yearly CT lung scans to screen for lung cancer in “asymptomatic adults aged 55–80 years who have a 30 pack-year smoking history and currently smoke or have quit smoking within the past 15 years” [21]. Although large studies on occupational cohorts have not been performed, high-risk workers may be similarly screened.
Unfortunately, one hurdle to overcome is identifying who is at risk for OLD in the first place. This comes down to identifying hazardous exposures in places they may not have previously been recognized, and identifying those who might be predisposed to having an adverse response from an exposure. Researchers have therefore examined niche industries or looked more closely at occupations where disease outbreaks have been observed in order to uncover unknown exposures. More scientifically advanced approaches, such as gene analysis, are being used to identify workers potentially at greater risk than others from a particular hazard.
Economic Consequences of Occupational Lung Disease
OLDs place a significant economic burden upon workers, employers, insurers and the general population. Although removal from the workplace exposure may help improve or resolve OLD, removal from work may not always be practical. It is difficult to ask someone who has made a career in a certain field to suddenly alter the course of their life and choose another profession. The consequences of these are wide-ranging, affecting sense of personal worth, intimate relationships, social circles and finances. In recognition of the economic impacts that OLDs can have, several remedies have been put in place. In addition to government workers’ compensation programs, government programs aimed at restituting workers in certain industries have been established. This includes special compensation and healthcare provision for workers exposed to coal, uranium, radiation and other harmful workplace exposures.
There are currently efforts to keep the growing numbers of older workers in employment. Strategies meant to achieve this goal face the challenge of making provisions for the increasing prevalence of COPD with age. Schofield et al. [22] presented findings of the first longitudinal study of the impact of COPD on subsequent economic activity. Investigators recruited men and women in their 50s who were employed full-time and followed them for 18 months. Of the participants who responded to the follow-up questionnaire (1656 of 1773 [93%]), the majority (78.5%) continued in full-time employment, 10.6% were part-time employees and 10.9% were no longer in paid employment. There was an increased adjusted risk of loss of employment for respondents who had spirometrically defined moderate or severe COPD (risk ratio 2.9) or self-reported breathlessness (risk ratio 3.1) at baseline. Sex or manual/nonmanual work was not found to modify this risk. This study demonstrated that in older workers, airway obstruction and breathlessness are independently associated with premature loss from the workforce. The prospective design lends strong support to the association being casual. The authors felt that the results of this study pose important questions and challenges for policy makers. This includes determining how to enable those with COPD and with significant breathlessness to remain economically active. In this study population, the pensionable age in the country under study was on average 10 years above the average age of those in the study who dropped out of the workforce. This indicates the existence of a need to evaluate interventions that are aimed at retaining individuals with COPD in work [22].
Algamdi et al. [23] similarly looked at the economic impact of fibrotic interstitial lung diseases (ILDs), including workplace productivity loss and the associated costs. The researchers used the Work Productivity and Activity Impairment questionnaire in patients in the six-center Canadian Registry for Pulmonary Fibrosis (CARE-PF) and compared them to Canadian population census data. A total of 148 out of 650 eligible patients were employed. Of the employed patients, productivity loss was reported by 55%. An average productivity loss of 7.8 ± 0.9 h per week was found. Presenteeism accounted for the majority of this loss (5.5 ± 0.6 h per week), while absenteeism accounted for a smaller proportion (2.3 ± 0.6 h per week) [23]. This study demonstrates the significant economic impact of fibrotic interstitial lung diseases.
Conclusion
A substantial occupational burden exists for multiple respiratory conditions, with clinical, policy and research implications. There is an urgent need to increase clinical recognition and public health awareness of OLDs. Increased attention should be directed toward reducing OLD burden through identification and implementation of effective preventive strategies. For this to happen, it is imperative that policy makers across the globe, especially those who establish regulatory standards and oversee their enforcement, reevaluate protections currently in place for workers exposed to recognized inhalational hazards. Additionally, LMICs can learn from the experience of more economically advanced countries and vice versa, and implement protections known to prevent OLDs and protect worker health. Medical research must continue to elucidate the pathogenesis of OLDs while continuing to examine once-overlooked parts of the world and occupations that have been poorly studied. Advances in genetic research and the understanding of gene-environment interactions and the epigenome are opening up fields of study that may help bring about advances in prevention and more focused treatments. Standards concerning how tests are performed and results are interpreted continue to change based upon experience and understanding of disease etiology, progression and management. As science advances, emerging technologies pose new potential risks to workers. There should be an increased focus on work with nanotechnology, in the aerospace industry and mobile technologies. Drawing upon current knowledge, we may be able to avert potential complications from new occupational hazards and prevent a recurrence of mistakes from being made in parts of the world that are just now adopting technologies and industries that are familiar to more economically advanced areas of the world.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Akshay Sood and Kevin Vlahovich have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659–724. [DOI] [PMC free article] [PubMed]
- 2.Blackley DJ, Halldin CN, Laney AS. Continued increase in prevalence of coal workers' pneumoconiosis in the United States, 1970–2017. Am J Public Health. 2018;108(9):1220–1222. doi: 10.2105/AJPH.2018.304517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hall NB, Blackley DJ, Halldin CN, Laney AS. Continued increase in prevalence of r-type opacities among underground coal miners in the USA. Occup Environ Med. 2019;76(7):479–481. doi: 10.1136/oemed-2019-105691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnes H, Goh NSL, Leong TL, Hoy R. Silica-associated lung disease: An old-world exposure in modern industries. Respirology. 2019;24(12):1165–1175. doi: 10.1111/resp.13695. [DOI] [PubMed] [Google Scholar]
- 5.Bulfin K, Cowie H, Galea KS, Connolly A, Coggins MA. Occupational exposures in an equestrian centre to respirable dust and respirable crystalline silica. Int J Environ Res Public Health. 2019;16:17. doi: 10.3390/ijerph16173226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garshick E, Abraham JH, Baird CP, Ciminera P, Downey GP, Falvo MJ, et al. Respiratory health after military service in Southwest Asia and Afghanistan. An official American thoracic society workshop report. Ann Am Thorac Soc. 2019;16(8):e1–16. doi: 10.1513/AnnalsATS.201904-344WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Apriani L, McAllister S, Sharples K, Alisjahbana B, Ruslami R, Hill PC, et al. Latent tuberculosis infection in healthcare workers in low- and middle-income countries: an updated systematic review. Eur Respir J. 2019;53:4. doi: 10.1183/13993003.01789-2018. [DOI] [PubMed] [Google Scholar]
- 8.Blanc PD, Annesi-Maesano I, Balmes JR, Cummings KJ, Fishwick D, Miedinger D, et al. The occupational burden of nonmalignant respiratory diseases. An Official American Thoracic Society and European Respiratory Society statement. Am J Respir Crit Care Med. 2019;199(11):1312–1334. doi: 10.1164/rccm.201904-0717ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carder M, Seed MJ, Money A, Agius RM, van Tongeren M. Occupational and work-related respiratory disease attributed to cleaning products. Occup Environ Med. 2019;76(8):530–536. doi: 10.1136/oemed-2018-105646. [DOI] [PubMed] [Google Scholar]
- 10.Yang IV, Konigsberg I, MacPhail K, Li L, Davidson EJ, Mroz PM, et al. DNA methylation changes in lung immune cells are associated with granulomatous lung disease. Am J Respir Cell Mol Biol. 2019;60(1):96–105. doi: 10.1165/rcmb.2018-0177OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Petsonk EL, Rose C, Cohen R. Coal mine dust lung disease. New lessons from old exposure. Am J Respir Crit Care Med. 2013;187(11):1178–1185. doi: 10.1164/rccm.201301-0042CI. [DOI] [PubMed] [Google Scholar]
- 12.Vandenplas O, Godet J, Hurdubaea L, Rifflart C, Suojalehto H, Walusiak-Skorupa J, et al. Severe occupational asthma: insights from a multicenter European cohort. J Allergy Clin Immunol Pract. 2019;7(7):2309–2318. doi: 10.1016/j.jaip.2019.03.017. [DOI] [PubMed] [Google Scholar]
- 13.Logar-Henderson C, MacLeod JS, Arrandale VH, Holness DL, McLeod CB, Peter A, et al. Adult asthma among workers in Ontario. Results from the occupational disease surveillance system. Ann Am Thorac Soc. 2019;16(5):563–571. doi: 10.1513/AnnalsATS.201810-701OC. [DOI] [PubMed] [Google Scholar]
- 14.Lytras T, Kogevinas M, Kromhout H, Carsin AE, Antó JM, Bentouhami H, et al. Occupational exposures and incidence of chronic bronchitis and related symptoms over two decades: the European Community Respiratory Health Survey. Occup Environ Med. 2019;76(4):222–229. doi: 10.1136/oemed-2018-105274. [DOI] [PubMed] [Google Scholar]
- 15.De Matteis S, Jarvis D, Darnton A, Hutchings S, Sadhra S, Fishwick D, et al. The occupations at increased risk of COPD: analysis of lifetime job-histories in the population-based UK Biobank Cohort. Eur Respir J. 2019;54:1. doi: 10.1183/13993003.00186-2019. [DOI] [PubMed] [Google Scholar]
- 16.Department of Health and Humans Services Centers for Disease Control and Prevention NIfOSaH. Coal Mine Dust Exposures and Associated Health Outcomes. https://www.cdc.gov/niosh/docs/2011-172/pdfs/2011-172.pdf. Current Intelligence Bulletin. 2011;p. 64.
- 17.Bayram M, Ozkan D, Hayat E, Bilgin M, Mehdi E, Bilgin S, et al. Asbestos-related diseases in Turkey: caused not only by naturally occurring fibers but also by industrial exposures. Am J Respir Crit Care Med. 2019;199(5):656–659. doi: 10.1164/rccm.201810-1922LE. [DOI] [PubMed] [Google Scholar]
- 18.Sood A. Performing a lung disability evaluation: how, when, and why? J Occup Environ Med. 2014;56(Suppl 10):S23–S29. doi: 10.1097/JOM.0000000000000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update. An official American thoracic society and european respiratory society technical statement. Am J Respir Crit Care Med. 2019;200(8):e70–e88. doi: 10.1164/rccm.201908-1590ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flaherty KR, Wells AU, Cottin V, Devaraj A, Walsh SLF, Inoue Y, et al. Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med. 2019;381(18):1718–1727. doi: 10.1056/NEJMoa1908681. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Preventive Services Task Force. USPSTF A and B Recommendations. 2017. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/.
- 22.Schofield SJ, Woods A, Szram J, Newman-Taylor AJ, Cullinan P. Chronic obstructive pulmonary disease and breathlessness in older workers predict economic inactivity. A prospective cohort Study. Am J Respir Crit Care Med. 2019;200(10):1228–1233. doi: 10.1164/rccm.201902-0297OC. [DOI] [PubMed] [Google Scholar]
- 23.Algamdi M, Sadatsafavi M, Fisher JH, Morisset J, Johannson KA, Fell CD, et al. Costs of workplace productivity loss in patients with fibrotic interstitial lung disease. Chest. 2019;156(5):887–895. doi: 10.1016/j.chest.2019.04.016. [DOI] [PubMed] [Google Scholar]