Abstract
The purpose of this study was to characterize the association between recent major life events and depressive symptoms during early adulthood, and to determine whether adolescents with chronically low positive affect or persistent sleep disturbance were more vulnerable to the link between stress and depressive symptoms. Adolescents (n = 147; 63.9% female; 33.7% non-Hispanic white) were recruited in 10th–11th grade and re-assessed 2 and 4 years later. At each assessment, adolescents completed measures of positive affect and sleep disturbances. At the final assessment, participants reported on their exposure to major life events in the past 12 months. Exposure to more major life events in the past year was associated with greater depressive symptoms in early adulthood. Chronically low positive affect and persistent sleep disturbances throughout adolescence each independently moderated this relationship. Specifically, only participants reporting low positive affect across the three assessments showed a positive and significant association between major life events and depressive symptoms. Further, only participants reporting sleep disturbances at all three assessments showed a positive and significant association between major life events and depressive symptoms. Chronically low positive affect and persistent sleep disturbances during adolescence may be useful indicators of risk for depression during early adulthood. Further, interventions targeting adolescent sleep disturbances and improving positive affect may be useful in reducing the risk for depression following life stress during this high risk developmental phase.
Keywords: Adolescent, Depression, Sleep disturbances, Positive affect
Depression remains one of the leading causes of global disease burden (Vos et al. 2017) and within adolescents this problem has been worsening since 2005 (Mojtabai et al. 2016). Further, depression tends to be a chronic and recurrent illness (Lewinsohn et al. 2000; Rohde et al. 2012), meaning that the global burden of depression may increase exponentially in the foreseeable future. One plausible path to mitigating the global burden of depression is preventing its onset. Given that 80% of depressive episodes occur in the wake of a major life stressor (Hammen 2005, 2015), identifying modifiable factors that attenuate this link may be particularly important for developing prevention strategies. Before the age of 12, the annual prevalence of depression is approximately 4%, increases throughout adolescence, and peaks at approximately 14% during early adulthood (Avenevoli et al. 2015; Mojtabai et al. 2016; Rohde et al. 2012). Thus, adolescence may be an ideal developmental phase for identifying promising intervention targets. Indeed, both low positive affect and sleep disturbance are intervention targets shown to reduce depressive symptoms when effectively engaged in treatment (Blake et al. 2016; Craske et al. 2016). In the current study, we examined whether two plausible and modifiable prevention targets during adolescence – chronically low positive affect and persistent sleep disturbance – moderate the link between stress and depressive symptoms in early adulthood.
Stress leads to depression (Hammen 2005, 2015). In fact, several studies have provided evidence that stress plays a causal role in the development of depression (Kendler et al. 1999). Given the ubiquity of stressful life events across the human lifespan, identifying modifiable factors that weaken the risk for depression in the wake of major life events may help to reduce the incidence of depression and other stress-related diseases. So far, effect sizes for depression prevention programs in youth have been encouraging but modest in targeted populations (Brent et al. 2015; Hetrick et al. 2016; Horowitz and Garber 2006; Werner-Seidler et al. 2017). Depression prevention programs may return larger effects if programs targeted factors that weakened the risk for depressive symptoms in the wake of life stress, rather than targeting symptoms alone. Positive affect and sleep have both been linked to how the body responds to stress (Minkel et al. 2014; Sin et al. 2015; Steptoe et al. 2005; Zautra et al. 2005). Further, both sleep and positive affect have been linked to resilience in youth at risk for depression (Silk et al. 2007). Thus, low positive affect and sleep disturbance are important moderators to investigate in the link between stressful life events and depression.
Low positive affect is associated with increased risk for depression for up to 10 years (Wood and Joseph 2010), and while negative affect tends to decline across adolescence in youth already at risk for depression, low positive affectivity persists (Conway et al. 2017). However, whether an individual’s tendency to experience positive affect mitigates the risk for depressive symptoms following major life events during developmental periods of high risk (e.g., adolescence and early adulthood) remains unknown. One promising study found that positive affect during adolescence can mitigate the link between low social support and later depression (Wetter and Hankin 2009), suggesting that this pathway is plausible. While experiencing positive emotions, cognitive abilities such as visuospatial attention and thought-action repertoires increase (Fredrickson and Branigan 2005; Rowe et al. 2007). As a result, people who experience more positive emotions develop larger repertoires of cognitive, behavioral, and social resources that aid in effective coping with stressors (Fredrickson 2000, 2001; Garland et al. 2010; Haeffel and Vargas 2011; Tugade and Fredrickson 2004; Tugade et al. 2004). Positive affect is a plausible prevention target for depression because there is preliminary evidence that it is modifiable in the short (McMakin et al. 2011) and the long-term (Cohn and Fredrickson 2010), although these effects have not yet been shown in adolescents. Nonetheless, there is now burgeoning evidence that mindfulness training (Cohn and Fredrickson 2010) and behavioral activation increase positive emotions (Mazzucchelli et al. 2010). Importantly, mindfulness-based interventions appear to promote increases in positive emotions through an “upward spiral” of cognition and positive emotions that serve to combat negative emotions (Garland et al. 2015; Goleman and Schwartz 1976). Indeed, interventions aimed specifically at increasing positive emotions can reduce the recurrence of depressive symptoms among adults (Seligman et al. 2006; Sin and Lyubomirsky 2009).
Whether the presence of persistent sleep disturbances across adolescence creates a vulnerability to depressive symptoms following major life events also remains unknown. Insomnia is a prospective risk factor for depression during adolescence (Roberts and Duong 2014) and in adulthood (Cho et al. 2008). Consistent with this idea, adolescents who regularly sleep 7.5–9.5 h per night are at the lowest risk for depression and anxiety (Fuligni et al. 2017a; Fuligni et al. 2017b; Ojio et al. 2016), and sleep disorders (e.g., pediatric sleep apnea) are prospectively associated with increased depression risk (Chang et al. 2017). This may be the case because sleep disturbances are associated with exaggerated psychological and biological responses to stress (Capaldi et al. 2005; Chiang et al. 2017; Hamilton et al. 2007; Meerlo et al. 2008). For example, in analyses of earlier waves of the present study, we demonstrated that poor sleep efficiency strengthened the association between daily family stress and negative affect (Chiang et al. 2017). Sleep is also a plausible prevention target for depression, given that interventions targeting sleep disturbances in adolescence are modestly effective (Blake et al. 2016).
Adolescence is a phase of development characterized by profound changes in affect as well as sleep (Carskadon 2011; Cicchetti and Rogosch 2002; Dahl 2004). Therefore, it is difficult to discern whether single assessments of these potential risk factors in cross-sectional studies reflect stable individual differences across adolescence or recent changes in the individual or their life. Therefore, trait-like difficulties experiencing positive affect or persistent problems with sleep measured repeatedly across this developmental phase may be a more reliable and clinically-meaningful indicator of risk.
In the present study, we examined the association between major life events in the past year (e.g., such as parental divorce, occupational problems at school or at work, interpersonal challenges with a friend or partner, financial difficulties) and depressive symptoms during early adulthood when risk for depressive episodes is highest (Kessler et al. 2005, 2012; Rohde et al. 2012). Based on the extant literature on the association between stress and depression, we hypothesized that individuals who reported more major life events would also report more depressive symptoms. Further, we hypothesized that the association between major life events and depressive symptoms would be the strongest among participants who reported chronically low positive affect and persistent sleep disturbances using reports of these factors across 6 years of adolescent development.
Method
Participants
Participants in the current study were from a three-wave longitudinal investigation designed to understand how psychosocial factors, family processes, and daily experiences contribute to early risk for poor health across adolescence (Chiang et al. 2017, 2019; Guan et al. 2016). The study enrolled 316 participants at Wave 1 of which 214 returned for Wave 2 and 180 returned for Wave 3; 148 participants participated in all three waves of data collection (Chiang et al. 2019). The analytic sample of the current study included 147 individuals, 63.9% female, Mage = 20.31, SDage = 0.69, with complete data for major life events and depressive symptoms at the third and final assessment. At this assessment, participants were 2–3 years post-high school. Of these participants, 59.2% (n = 87) were enrolled in either a 2- or 4-year college, 53.7% (n = 79) were working part-time, and 14.3% (n = 21) were working full-time (percentages add up to greater than 100% due to individuals both attending college and working). Participants were from diverse backgrounds: 46.3% of the sample was Latino, 15.0% was Asian-American, 33.7% was European-American, and 6.1% reported “other” for ethnicity. Adolescents came from families with a median income of $60,000, and had parents with a wide range of educational backgrounds; 14.2% had parents that did not complete high school, 11.7% had parents with a high school diploma, 46.7% had parents with some college including vocational training, and 27.5% had parents with a bachelor’s degree or higher.
Compared to the sample recruited initially (n = 316), the present analytic sample had a higher proportion of female participants, χ2 (315) = 6.33, p = 0.012, r = 0.36, and a lower proportion of Asian participants, χ2 (315) = 10.39, p = 0.016, r = 0.58. There were no differences in household income, p = 0.31, parent education, p = 0.09, BMI, p = 0.26, or depressive symptoms, p = 0.90 between the sample in the present analyses and the participants initially enrolled in the larger study.
Procedures
All study procedures were reviewed and approved by the Institutional Review Board at UCLA. Adolescents and their primary caregivers were recruited from four high schools in the Los Angeles metropolitan area. Recruitment involved in-class presentations, distribution of study flyers and recruitment forms during presentations, and postal mailings to students’ homes. Enrollment for the larger study (n = 316) began in 10th and 11th grade and included follow-up assessments 2 and 4 years after enrollment. All participants and their parents provided written assent and consent, respectively, at the start of the initial study visit. Participants were compensated in cash for their time; $50 for the initial assessment, $75 for the second assessment, and $120 for the third and final assessment. All questionnaires were completed by youth on electronic tablets. The current study focused on the association between major life events and depressive symptoms assessed at the third assessment (i.e., 4 years after enrollment), and used positive affect and sleep data collected at all three study assessments. Trained research staff visited participants at home and all study questionnaires were completed via an electronic tablet. See Fig. 1 for timeline of study assessments.
Fig. 1.
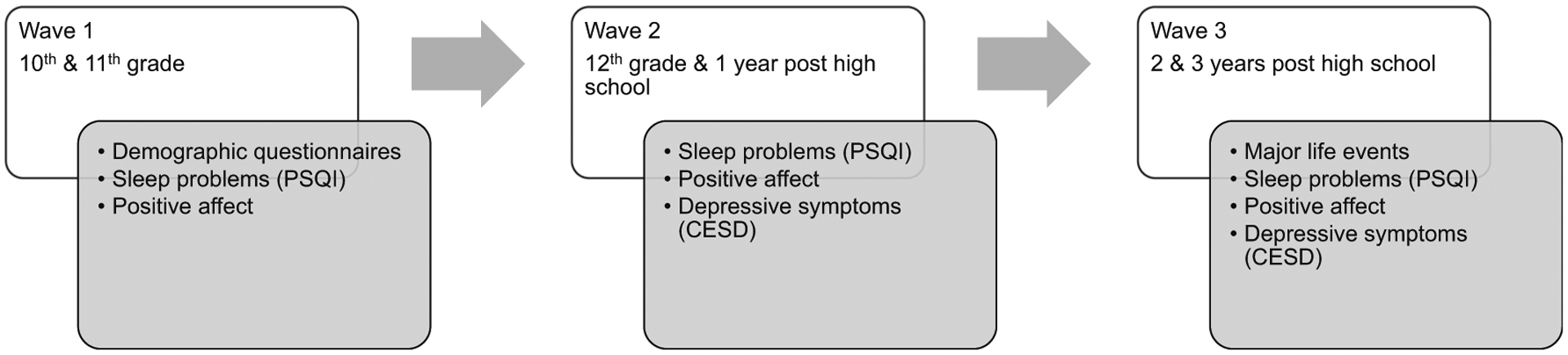
Timeline of study procedures
Measures
Major Life Events
Major life events in the past 12 months were queried at the Wave 3 assessment using a 21-item checklist developed from previous studies linking stressful life events across multiple domains (family, friends, school) to negative health outcomes (Chiang et al. 2019; Conger et al. 2002; Hammen 1991). See Table 1 for the list of items in the checklist and the frequency with which participants endorsed their occurrence. For each item, participants indicated whether each event had occurred during the past year with a no or yes. The number of yes responses was summed to create a total major life events score for each participant over the past year.
Table 1.
List of major life events (MLE) participants completed (n = 147)
| % (n) | |
|---|---|
| During the past 12 months, have any of the following occurred? | |
| Did not see your mother for one month or longer | 32.0 (47) |
| Did not see your father for one month or longer | 48.3 (71) |
| Became seriously ill | 5.4 (8) |
| A sister or brother had a drug or alcohol problem | 5.4 (8) |
| A close family friend was arrested | 7.5 (11) |
| A close friend moved quite far away | 28.6 (42) |
| Had a serious falling-out or ended a friendship with a close friend | 30.6 (45) |
| Got pregnant or your girlfriend got pregnant | 2.0 (3) |
| Your grades in school went down a lot | 15.0 (22) |
| Suspended or expelled from school | 1.4 (2) |
| Did not get into a club or sports team you really wanted to be involved in | 5.4 (8) |
| Your physical appearance got worse (e.g., weight, acne, etc.) | 26.5 (39) |
| Lost your job | 4.8 (7) |
| Did not get into a school or college that you wanted to attend | 4.8 (7) |
| Divorced or separated from your spouse or partner | 5.4 (8) |
| A parent lost his/her job | 11.6 (17) |
| Your parents divorced or separated | 2.7 (4) |
| A close family member or friend passed away | 28.6 (42) |
| Your parent suffered a financial loss or loss of property not related to work | 6.1 (9) |
| An immediate family member became seriously ill | 22.4 (33) |
| Your family experienced serious financial problems | 17.7 (26) |
Positive Affect
Positive affect was assessed at all 3 assessments via 8-items from the Positive and Negative Affect Scale (PANAS) (Watson and Clark 1999). In this measure, participants were asked to indicate the extent to which they have felt happy, joyful, delighted, cheerful, excited, enthusiastic, lively, and energetic during the past week according to a 5-point Likert scale from 1 = Very slightly or not at all to 5 = extremely. Participant scores on each item were averaged for each wave and then averaged across all waves as a measure of trait positive affect across adolescence. Internal reliability of positive affect in this sample was excellent, α > 0.95 at each wave, and did not change significantly across waves, b (437) = −0.1, SE = 0.02, p = 0.74.
Sleep Disturbance
At each assessment, participants completed the 19-item Pittsburgh Sleep Quality Index (PSQI) about their sleep over the past month (Buysse et al. 1989). The PSQI returns a global sleep disturbance score that ranges from 0 to 21 and scores greater than 5 indicate clinically meaningful problems with sleep (Backhaus et al. 2002; Dietch et al. 2016). Given that adolescence is a period characterized by atypical sleep (Carskadon 2011; Owens et al. 2014), we focused on youth reporting sleep disturbances that would be clinically meaningful. Therefore, participant scores on the PSQI at each assessment were recoded into a dichotomous variable reflecting individuals above and below the clinical threshold, and summed. The number of times a participant exceeded the clinical threshold at each of the three waves was used as their frequency of sleep disturbance across adolescence. Scores ranged from 0 to 3. The tendency to have clinically significant sleep problems across the three waves of data collection increased, b (437) = 0.04, SE = 0.01, p < 0.01.
Depressive Symptoms
Depressive symptoms during the past month were assessed at all study waves via the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff 1977). Symptoms at Wave 3 were used as the dependent variable in all models, and symptoms at Wave 2 were used as a covariate. The CES-D is a 20-question, self-report instrument with excellent reliability and validity (Radloff 1977). For each item, participants indicated the frequency of a given symptom according to a 4-point scale where 1 = rarely or none of the time and 4 = most or all of the time. Scores on the CES-D can range from 0 to 60, higher scores indicate more frequent and severe depressive symptoms, and scores greater than 15 suggest clinically significant symptoms of depression. The CES-D has demonstrated good sensitivity and specificity with major depressive episodes determined via semi-structured clinical interview (Mulrow et al. 1995; Stockings et al. 2015). The CES-D demonstrated excellent internal reliability in the current sample, α = 0.91, and depressive symptoms did not change significantly across the three waves of data collection, b (437) = −0.21, SE = 0.19, p = 0.28.
Data Analysis
All continuous variables were assessed for normality and heteroscedasticity and found to be normally distributed. Multiple linear regressions were used to determine the association between major life events during the 12 months prior to the Wave 3 assessment and depressive symptoms at Wave 3, as well as the moderating roles of positive affect and persistent sleep disturbances across adolescence on this association. All models were conducted with and without adjusting for age, sex, ethnicity, household income, and depressive symptoms at Wave 2. In order to determine the specificity of positive affect and persistent sleep problems in the association between MLE and depressive symptoms, our model of the interaction between trait positive affect and MLE on depressive symptoms controlled for persistent sleep problems and our model of the interaction between persistent sleep problems and MLE on depressive symptoms controlled for trait positive affect. When a significant interaction was observed in these regression models, we then computed simple slopes for the association between major life events and depressive symptoms at varying levels of the moderator to further characterize the interaction. All models where p < 0.05 were considered statistically significant, and all p-values less than 0.10 are reported to facilitate comparison with existing theoretical models and previously published findings.
Results
Participants in this sample reported exposure to between 0 and 10 major life events in the past year during young adulthood, MMLE = 3.12, SDMLE = 2.20. Each of the major life events in our assessment was endorsed by at least 3 participants, and the most commonly-reported events were separation from father, falling out with a friend, separation from mother, bereavement due to loss of a family member, and worsening physical appearance (See Table 1). Participants reported a wide range of depressive symptoms during young adulthood, RangeCESD 0–50, MCESD = 14.86, SDCESD = 0.83, and 35.4% (n = 52) participants reported clinically significant depressive symptoms.
Table 2 provides key study variables and the bivariate associations between them. Positive affect scores were generally high at each Wave, Mpositive affect = 3.61–3.67, with a moderate amount of rank-order stability scores across the assessments, rs = 0.31–0.49. Sleep disturbance was pervasive in this sample such that 39.5% (n = 58) of participants reported clinically-meaningful sleep disturbance at study enrollment, 49.0% (n = 72) of participants reported clinically-meaningful sleep disturbance at the 2-year follow-up, 53.1% (n = 78) of participants reported clinically-meaningful sleep disturbance at the 4-year follow-up. Only 26.5% (n = 39) never exhibited clinically meaningful problems with sleep, and 18.4% (n = 27) exhibited clinically meaningful sleep problems at all three assessments. Notably, sleep latency and overall sleep quality were consistently among the highest correlated sleep components with global sleep disturbance scores at all three assessments, rs = 0.64–0.70, ps < 0.001 and rs = 0.67–0.73, ps < 0.001 respectively.
Table 2.
Means, standard deviations, and bivariate correlations between major life events, positivity, sleep disturbances, depressive symptoms (n = 147)
| Study Assessment | M (SD) | Correlations | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | ||
| Study enrollment | ||||||||||
| 1. Positivity | 3.67 (0.98) | 1.00 | ||||||||
| 2. Sleep disturbances | 5.18 (3.1) | −0.30** | 1.00 | |||||||
| 2-year follow-up | ||||||||||
| 3. Positivity | 3.61 (1.00) | 0.36** | −0.21* | 1.00 | ||||||
| 4. Sleep disturbances | 5.72 (2.93) | −0.04 | 0.47** | −0.34** | 1.00 | |||||
| 5. Depressive symptoms | 15.14 (9.82) | −0.23** | 0.38** | −0.59** | 0.46** | 1.00 | ||||
| 4-year follow-up | ||||||||||
| 6. Age | 20.31 (0.69) | −0.01 | 0.07 | −0.03 | −0.07 | −0.09 | 1.00 | |||
| 7. Positivity | 3.62 (0.99) | 0.31** | −0.28** | 0.49** | −0.22** | −0.32** | −0.04 | 1.00 | ||
| 8. Sleep disturbances | 5.97 (2.90) | −0.11 | 0.37** | −0.20* | 0.54 | 0.28** | −0.06 | −0.32** | 1.00 | |
| 9. Major life events | 3.12 (2.20) | −0.13 | 0.34** | −0.16+ | 0.21* | 0.27** | 0.06 | −0.16+ | 0.23** | 1.00 |
| 10. Depressive symptoms | 14.86 (10.10) | −0.34** | 0.33** | −0.39** | 0.21* | 0.45** | −0.05 | −0.65** | 0.40** | 0.27** |
p < 0.01,
p < 0.05,
p < 0.10
There were no significant differences between male and female participants in trait positivity, F(1,145) = 0.30, p = 0.59, or frequency of sleep disturbances, F(1,145) = 0.23, p = 0.63. Female participants reported slightly higher MLE exposure during the past year, MMLE (female) = 3.35, SDMLE (female) = 2.12 vs. MMLE (male) = 2.72, SDMLE (male) = 2.29, and slightly higher depressive symptoms, MMLE (female) = 15.90, SDMLE (female) = 10.49 vs. MMLE (male) = 13.02, SDMLE (male) = 9.19, although these differences were non-significant, F(1,145) = 2.86, p = 0.093 and F(1,145) = 2.80, p = 0.096 respectively.
Major Life Events Are Associated with more Depressive Symptoms in Young Adulthood
As expected, participants who reported more MLEs in the past year also reported higher depressive symptoms, b (145) = 1.24, SE = 0.37, p = 0.001, and the number of MLEs in the past year accounted for 7.3% of the variance in depressive symptoms, R2 = 0.073, p = 0.001. Exposure to each additional MLE was associated with a 1.24-point increase in total CESD score. The association between MLEs and depressive symptoms remained when accounting for age, sex, household income, ethnicity, and depressive symptoms at the Wave 2 assessment, b (141) = 0.80, SE = 0.37, p = 0.03. See Table 3 Model 1 for coefficient estimates for all covariates and MLEs predicting depressive symptoms in young adulthood.
Table 3.
Positivity and sleep disturbance during adolescence moderate the association between recent life stress and depressive symptoms
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| R2 | b (SE) | p | R2 | b (SE) | p | R2 | b (SE) | p | |
| 0.24 | <0.001 | 0.50 | <0.001 | 0.51 | < 0.001 | ||||
| Intercept | 12.56 (22.35) | 0.56 | 16.76 (18.72) | 0.37 | 30.87 (18.52) | 0.10 | |||
| Major life events | 0.80 (0.37) | 0.03 | 0.41 (0.31) | 0.19 | −0.73 (0.55) | 0.19 | |||
| Sleep Disturbance | – | – | 2.30 (0.67) | 0.001 | 2.26 (0.66) | 0.001 | |||
| Positive affect | – | – | −6.71 (0.96) | < 0.001 | −6.67 (0.95) | <0.001 | |||
| MLE × Positive affect | – | – | −0.97 (0.45) | 0.03 | – | – | |||
| MLE × Sleep Disturbances | – | – | – | – | 0.75 (0.28) | 0.008 | |||
| Covariates | |||||||||
| Depressive symptoms (Age 18) | 0.42 (0.08) | <0.001 | 0.08 (0.08) | 0.33 | 0.08 (0.08) | 0.31 | |||
| Sex | 1.95 (1.60) | 0.22 | 1.62 (1.31) | 0.22 | 2.11 (1.30) | 0.11 | |||
| Household income | <0.01 (0.00) | 0.67 | < 0.01 (0.00) | 0.75 | <0.01 (0.00) | 0.67 | |||
| Ethnicity | −0.90 (0.78) | 0.25 | −1.52 (1.31) | 0.22 | −1.51 (0.64) | 0.02 | |||
MLE Major Life Events. Additionally, we ran a 4th regression model that includes both interaction terms. In this model, the interaction between persistent sleep problems and MLEs remained significant, b = 0.62, SE = 0.30, p = 0.04, and the interaction between positive affect and MLEs did not, b = −0.65, SE = 0.47, p = 0.17. The results of this model seem to suggest that sleep problems more robustly moderate the link between MLEs and depressive symptoms in early adulthood than positive affect. However the collinearity statistic for the interaction between sleep problems and MLE’s was too low for us to interpret with any confidence, tolerance = 0.27
Chronically Low Positive Affect across Adolescence Moderates the Link between Stress and Depressive Symptoms in Young Adulthood
There was a main effect of positive affect on depressive symptoms. When accounting for MLEs in the past year, past depressive symptoms, age, sex, household income, ethnicity, and persistent sleep disturbance, higher average positive affect across the 4-year assessment period was associated with lower depressive symptoms, b (139) = −6.66, SE = 0.97, p < 0.001.
See Table 3 (Model 2) for detailed results of the interaction model. There was a significant interaction between positive affect across adolescence and major life events in the past year, b (138) = −0.97, SE = 0.45, p = 0.032, and the addition of the interaction between MLE and positive affect to the model contributed to a significant increase in variance accounted for, ΔF = 4.67, p = 0.030. The association between major life events and depressive symptoms among participants with above average positive affect across adolescence was non-significant, b = 0.06, SE = 0.45, p = 0.90, whereas the association among participants with below average positive affect was positive, b = 1.10, SE = 0.53, p = 0.04. See Fig. 2a for the associations between major life events and depressive symptoms in early adulthood at above and below average trait positive affect across adolescence.
Fig. 2.
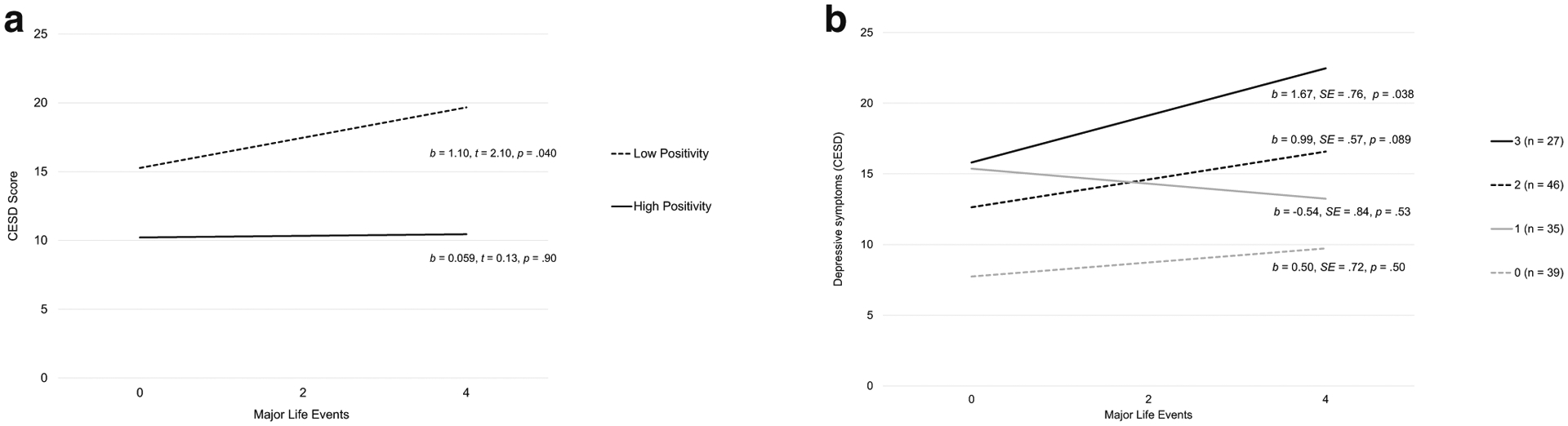
Association between major life events in the past 12 months and depressive symptoms for youth with a) above and below average trait positivity across adolescence and b) by the number of times the participant reported clinically significant symptoms of sleep disturbance across adolescence
Persistent Sleep Disturbance across Adolescence Moderates the Link between Stress and Depressive Symptoms in Early Adulthood
There was also a main effect of persistent sleep disturbance on depressive symptoms. When accounting for MLEs in the past year, past depressive symptoms, age, sex, ethnicity, household income, and trait positive affect, the presence of each additional occurrence of clinically-meaningful sleep disturbance across the four-year follow-up was associated with more depressive symptoms in young adulthood, b (139) = 2.27, SE = 0.67, p = 0.001.
See Table 3 (Model 3) for detailed results of this model. There was a significant interaction between the incidence of sleep disturbance across adolescence and major life events in the past year, b (139) = 0.75, SE = 0.28, p = 0.008, and the addition of the interaction between MLE and sleep disturbance to the model contributed to a significant increase in variance accounted for, ΔF = 7.15, p = 0.008. Specifically, participants reporting sleep disturbance at all three assessments exhibited a strong positive association between major life events and depressive symptoms, p = 0.038, participants reporting sleep disturbance at two of the three assessments exhibited a non-significant, positive association between major life events and depressive symptoms, p = 0.089, and participants reporting no or only one incidence of sleep disturbance across adolescence showed no relationship between major life events and depressive symptoms, p > 0.50. See Fig. 2b for the association between major life events and depressive symptoms in early adulthood at varying frequencies of sleep disturbance across adolescence.
Posthoc Analyses
Given that trait measures of positive affect and sleep disturbances included assessments at Wave 3 which co-occurred with our dependent variable, we conducted two additional models to test the temporal precedence of positive affect and sleep problems. Positive affect at Wave 2 alone moderated the link between life events and depression at wave 3, b = 1.02, p = 0.01, R2 = 0.35, p < 0.001, and sleep disturbances at Wave 2 also moderated the link between life events and depression at Wave 3, b = 1.60, p = 0.029, R2 = 0.28, p < 0.001.
Discussion
As hypothesized, and consistent with the extant literature, more major life events in the past year were associated with greater depressive symptoms during early adulthood in this sample. Yet, this association was only present in participants reporting lower average positive affect or persistent sleep disturbances across adolescence. The clinical implications of these findings are that efforts to increase experiences of positive affect or improve sleep in adolescents may reduce the risk of depressive symptoms following life stress in early adulthood. Perhaps more importantly, interventions that aim to either increase positive affect or improve sleep during adolescence may reduce the risk for developing symptoms in the wake of life stress among transitional age youth, when risk is highest.
Experiencing more major life events in the past year was associated with more depressive symptoms. This is consistent with decades of research on the etiology of depression (Hammen 2005, 2015). In this sample, the most commonly reported major life events were separation from father for more than one month, separation from mother for more than one month, having a serious falling out or ending to a friendship, having a close friend move far away, and death of a close family member or friend. These are uniformly interpersonal events, which have already been linked to risk for depression (Hammen 2005; Rudolph et al. 2000). Further, it is important to note that these interpersonal events are somewhat normative for adolescents transitioning to early adulthood. For example, it is not uncommon for adolescents to move away for college resulting in a disruption in their relationships with friends and family. Yet, little research has been done to acknowledge the role that normative stressors that occur in the transition from adolescence to early adulthood play in the high risk for depression observed in this phase of the lifespan.
Despite the robust association between major life events in the past year and depressive symptoms during early adulthood, participants who consistently reported high positive affect at each assessment throughout adolescence did not demonstrate an association between stress and depressive symptoms. This observation can be interpreted in several ways. First, adolescents who consistently demonstrate low positive affect may be particularly at risk for depression following major life events. Indeed, low positive affect carries increased risk for depression for up to 10 years (Wood and Joseph 2010) and there appears to be a distinct neural signature associated with high positive affect and low depressive symptoms in adolescents (Forbes et al. 2010). This finding could also implicate positive affect as a beneficial intervention target for adolescents to mitigate the well-documented risk for depression that increases across adolescence and into early adulthood. Increasing an adolescent’s capacity for positive affect may decrease the impact of negative events and other risk factors on their lives (e.g., Wetter and Hankin 2009), thus preventing increases in depressive symptoms in their wake. Indeed, a large experience sampling study of adult twins found that positive affect decreased the link between stressful experiences and negative affect throughout the day (Wichers et al. 2007). Indeed, there is early evidence that positive affect interventions can mitigate the negative behavioral effects of stress (Charlson et al. 2014). Yet, no study to our knowledge has tested the preventive efficacy of a positive affect intervention for depressive symptoms in adolescents. In one of the largest depression prevention programs in youth to date, the Penn Resiliency Program, effectiveness was mediated by improvements in explanatory style (Brunwasser et al. 2018). Indeed, humans naturally exhibit an attributional bias in positive compared to negative events. This phenomenon is diminished among depressed individuals and most exaggerated during phases of the lifespan when risk for depression is lowest (i.e., young children and older adults) (Mezulis et al. 2004). It is possible that persistently low capacity for positive affect may impede an adolescent’s experience of positive events as such, and therefore decrease their opportunities to engage this positive attributional bias.
We also observed that the association between stress and depressive symptoms in early adulthood was moderated by persistent sleep disturbance throughout adolescence. Only participants who reported clinically significant symptoms of sleep disturbance at all three assessments showed a positive and significant association between life events and depressive symptoms. Participants who reported sleep disturbance at two of the three assessments showed non-significant evidence of sensitization to life events (See Fig. 2b). Although, it is notable that participants who were exposed to more than 2 events in the past year reported depressive symptoms that exceeded the clinical threshold for depression (CESD >15) (See Fig. 2b), suggesting that this group may be clinically relevant even if not statistically so. Persistent sleep disturbance may contribute to depressive symptoms by increasing adolescent exposure to stressful life events through increased risk-taking (Owens et al. 2014; Shochat et al. 2014); but also through exaggerated biological processes (Capaldi et al. 2005; Irwin et al. 2016), that are activated by stressful events and have been independently linked to the pathogenesis of depression (Slavich and Irwin 2014). What’s notable is that youth reporting no problems with sleep across adolescence or at only one assessment were less vulnerable to the depressive effects of major life events in young adulthood. These observations underscore the utility of persistent sleep disturbances across adolescence as a reliable indicator of risk for depression, particularly following stressful life events. Screening for sleep disturbances regularly by healthcare providers with a high degree of continuity in adolescent populations (e.g., primary care physicians, dentists, school counselors) may be an effective way of triaging youth into preventive programs. In particular, persistent sleep problems in this sample were largely driven by difficulty falling asleep (sleep latency) and lower subjective sleep quality. These factors could be a useful guide to health care providers given that relatively simple behavioral factors such as media use before bed can be a major contributor to sleep latency (Lemola et al. 2015; Shochat et al. 2010). Treating these behavioral factors with sleep hygiene may also mitigate larger problems such as the association between family dysfunction and sleep latency (Billows et al. 2009). Yet, screening for sleep disturbances in pediatric primary care settings remains uncommon (Honaker and Meltzer 2016). It is well-established that effectively treating sleep disturbances leads to reductions in depressive symptoms (Ballesio et al. 2018). There is growing interest in using cognitive behavioral therapy for insomnia (CBTi) to prevent depression (Baglioni et al. 2011), and some preliminary evidence for its effectiveness (Christensen et al. 2016; See Irwin 2015 for review), although to our knowledge the evidence in adolescent populations remains limited.
The results of this study should be considered in the context of its strengths and limitations. Most importantly, this is a large longitudinal study in a diverse sample of adolescents that can only draw correlational, rather than causal, conclusions. Further, only 46.5% of the initially enrolled sample contributed data at all three assessments. We have covaried for factors that distinguish our present analytic sample from the initially enrolled sample, however it is possible that unmeasured factors contributing to study attrition may also influence our observations in ways that were not accounted for. Our MLE checklist only assessed for whether an event occurred and did not include any measures of subjective response to that event. It is therefore possible that some items in the checklist were not stressful or upsetting to our sample given their age (e.g., separation from parents), which may have resulted in an underestimation of the association between MLE and depressive symptoms. Additionally, exposure to MLEs and the final depressive symptom assessment occurred simultaneously which introduces the confound that stress and depression are bi-directionally related (Hazel et al. 2008; Liu and Alloy 2010; Uliaszek et al. 2012). Likewise, the clinically validated measures used in this study, CESD and PSQI, probe symptoms occurring in the past month rather than the entire period of time between each assessment. Thus it is possible that more participants experienced depressive episodes or sleep disturbances outside of these windows and are not captured in our data. To this point, no semi-structured clinical interview was used to complement the self-reported measures of depressive symptoms or sleep disturbances, which would help us to confirm the presence of depressive episodes and insomnia in this sample. Further, we have made the assumption that participants’ positive affect and sleep disturbances across the assessment periods were stable, although more frequent assessment of each of these constructs would be helpful to understand the degree to which adolescents fluctuate throughout the year. Finally, our final measure of sleep disturbance and positive affect temporally overlapped with the assessment of major life events and depressive symptoms, thus obscuring the possible roles of low positive affect and sleep problems in the etiology of depression.
Depression is a recurrent and debilitating disorder, particularly for individuals whose first depressive episode occurs early in lifespan development. Thus, prevention may be the most effective way of reducing the burden of depression on individuals and society. There is growing evidence that depression prevention programs can be effective for youth (Brent et al. 2015; Rohde et al. 2015; Stice et al. 2009; Werner-Seidler et al. 2017), particularly when delivered outside of a phase of acute distress (Biesheuvel-Leliefeld et al. 2015). However, there remains room for improvement given that existing programs are effective for preventing depressive symptoms but not necessarily depressive episodes (Hetrick et al. 2016; Rohde et al. 2015). We propose that the most effective depression prevention programs will mitigate the impact of stress on individuals. Yet, depression prevention trials often focus only on the presence or absence of symptoms over time. A more sensitive measure of program effectiveness may be an individual’s tendency to develop symptoms in the wake of life stress, rather than symptoms alone. This is particularly important given that the well-established sex differences observed in depression can be explained largely by differences in stress exposure by males and females (Hankin et al. 2007; Shih et al. 2006). Here we identify positive affect and sleep disturbance as two important factors in risk for depressive symptoms in early adulthood in the wake of recent major life events. Future studies are needed that test whether existing prevention programs are disproportionately effective for adolescents and transitional age youth with a history of low positive affect or sleep disturbances, or whether effective adolescent depression prevention programs engage these intervention targets. Further, investigations into whether interventions that increase positive affect or improve sleep are particularly effective in reducing the incidence of depression following stressful events during early adulthood could be instrumental in reducing the burden of depression across the lifespan.
Acknowledgements
The composition of this manuscript was made possible by the National Institute of Mental Health through a career development award that was awarded to Dr. Kuhlman (K08MH112773) and the collection of this data was made possible by the Eunice Kennedy Shriver Institute of Child Health & Human Development (R01HD062547; P2C-HD041022) and the National Institute on Aging (P30-AG017265; P30-AG028748).
Footnotes
Conflict of Interest The authors report no conflicts of interest.
Ethical Approval All study procedures were approved by the Institutional Review Board at UCLA.
References
- Avenevoli S, Swendsen J, He J-P, Burstein M, & Merikangas KR (2015). Major depression in the National Comorbidity Survey–Adolescent Supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child & Adolescent Psychiatry, 54(1), 37–44.e2. 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backhaus J, Junghanns K, Broocks A, Riemann D, & Hohagen F (2002). Test-retest reliability and validity of the Pittsburgh sleep quality index in primary insomnia. Journal of Psychosomatic Research, 53(3), 737–740. [DOI] [PubMed] [Google Scholar]
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Lombardo C, & Riemann D (2011). Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders, 135(1), 10–19. 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Ballesio A, Aquino MRJV, Feige B, Johann AF, Kyle SD, Spiegelhalder K, Lombardo C, Rücker G, Riemann D, & Baglioni C (2018). The effectiveness of behavioural and cognitive behavioural therapies for insomnia on depressive and fatigue symptoms: A systematic review and network meta-analysis. Sleep Medicine Reviews, 37, 114–129. 10.1016/j.smrv.2017.01.006. [DOI] [PubMed] [Google Scholar]
- Biesheuvel-Leliefeld KEM, Kok GD, Bockting CLH, Cuijpers P, Hollon SD, van Marwijk HWJ, & Smit F (2015). Effectiveness of psychological interventions in preventing recurrence of depressive disorder: Meta-analysis and meta-regression. Journal of Affective Disorders, 174, 400–410. 10.1016/j.jad.2014.12.016. [DOI] [PubMed] [Google Scholar]
- Billows M, Gradisar M, Dohnt H, Johnston A, McCappin S, & Hudson J (2009). Family disorganization, sleep hygiene, and adolescent sleep disturbance. Journal of Clinical Child & Adolescent Psychology, 38(5), 745–752. 10.1080/15374410903103635. [DOI] [PubMed] [Google Scholar]
- Blake MJ, Waloszek JM, Schwartz O, Raniti M, Simmons JG, Blake L, et al. (2016). The SENSE study: Post intervention effects of a randomized controlled trial of a cognitive-behavioral and mindfulness-based group sleep improvement intervention among at-risk adolescents. Journal of Consulting and Clinical Psychology, 84(12), 1039–1051. 10.1037/ccp0000142. [DOI] [PubMed] [Google Scholar]
- Brent DA, Brunwasser SM, Hollon SD, Weersing VR, Clarke GN, Dickerson JF, Beardslee WR, Gladstone TRG, Porta G, Lynch FL, Iyengar S, & Garber J (2015). Effect of a cognitive-behavioral prevention program on depression 6 years after implementation among at-risk adolescents: A randomized clinical trial. JAMA Psychiatry, 72(11), 1110–1118. 10.1001/jamapsychiatry.2015.1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunwasser SM, Freres DR, & Gillham JE (2018). Youth cognitive-behavioral depression prevention: Testing theory in a randomized controlled trial. Cognitive Therapy and Research, 1–15. 10.1007/s10608-018-9897-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF III, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Capaldi VF, Handwerger K, Richardson E, & Stroud LR (2005). Associations between sleep and cortisol responses to stress in children and adolescents: A pilot study. Behavioral Sleep Medicine, 3(4), 177–192. [DOI] [PubMed] [Google Scholar]
- Carskadon MA (2011). Sleep in adolescents: The perfect storm. Pediatric Clinics of North America, 58(3), 637–647. 10.1016/j.pcl.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C-H, Chen S-J, & Liu C-Y (2017). Pediatric sleep apnea and depressive disorders risk: A population-based 15-year retrospective cohort study. PLoS One, 12(7), e0181430. 10.1371/journal.pone.0181430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson ME, Wells MT, Peterson JC, Boutin-Foster C, Ogedegbe GO, Mancuso CA, Hollenberg JP, Allegrante JP, Jobe J, & Isen AM (2014). Mediators and moderators of behavior change in patients with chronic cardiopulmonary disease: The impact of positive affect and self-affirmation. Translational Behavioral Medicine, 4(1), 7–17. 10.1007/s13142-013-0241-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang JJ, Kim JJ, Almeida DM, Bower JE, Dahl RE, Irwin MR, McCreath H, & Fuligni AJ (2017). Sleep efficiency modulates associations between family stress and adolescent depressive symptoms and negative affect. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 61(4), 501–507. 10.1016/j.jadohealth.2017.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang JJ, Park H, Almeida DM, Bower JE, Cole SW, Irwin MR, McCreath H, Seeman TE, & Fuligni AJ (2019). Psychosocial stress and C-reactive protein from mid-adolescence to young adulthood. Health Psychology, 38(3), 259–267. 10.1037/hea0000701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho HJ, Lavretsky H, Olmstead R, Levin MJ, Oxman MN, & Irwin MR (2008). Sleep disturbance and depression recurrence in community-dwelling older adults: A prospective study. The American Journal of Psychiatry, 165(12), 1543–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen H, Batterham PJ, Gosling JA, Ritterband LM, Griffiths KM, Thorndike FP, Glozier N, O’Dea B, Hickie IB, & Mackinnon AJ (2016). Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight study): A randomised controlled trial. The Lancet Psychiatry, 3(4), 333–341. 10.1016/S2215-0366(15)00536-2. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Rogosch FA (2002). A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology, 70(1), 6–20. 10.1037/0022-006X.70.1.6. [DOI] [PubMed] [Google Scholar]
- Cohn MA, & Fredrickson BL (2010). In search of durable positive psychology interventions: Predictors and consequences of long-term positive behavior change. The Journal of Positive Psychology, 5(5), 355–366. 10.1080/17439760.2010.508883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger RD, Wallace LE, Sun Y, Simons RL, McLoyd VC, & Brody GH (2002). Economic pressure in African American families: A replication and extension of the family stress model. Developmental Psychology, 38(2), 179–193. [PubMed] [Google Scholar]
- Conway CC, Zinbarg RE, Mineka S, & Craske MG (2017). Core dimensions of anxiety and depression change independently during adolescence. Journal of Abnormal Psychology, 126(2), 160–172. 10.1037/abn0000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Meuret AE, Ritz T, Treanor M, & Dour HJ (2016). Treatment for anhedonia: A neuroscience driven approach. Depression and Anxiety, 33(10), 927–938. 10.1002/da.22490. [DOI] [PubMed] [Google Scholar]
- Dahl RE (2004). Adolescent brain development: A period of vulnerabilities and opportunities. Keynote address. Annals of the New York Academy of Sciences, 1021(adolescent brain development: Vulnerabilities and opportunities), 1–22. 10.1196/annals.1308.001. [DOI] [PubMed] [Google Scholar]
- Dietch JR, Taylor DJ, Sethi K, Kelly K, Bramoweth AD, & Roane BM (2016). Psychometric evaluation of the PSQI in U.S. college students. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine, 12(8), 1121–1129. 10.5664/jcsm.6050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE, Ryan ND, Phillips ML, Manuck SB, Worthman CM, Moyles DL, et al. (2010). Healthy adolescents’ neural response to reward: Associations with puberty, positive affect, and depressive symptoms. Journal of the American Academy of Child & Adolescent Psychiatry, 49(2), 162–172.e5. 10.1016/j.jaac.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL (2000). Cultivating positive emotions to optimize health and well-being. Prevention & Treatment, 3(1), 1a. [Google Scholar]
- Fredrickson BL (2001). The Role of Positive Emotions in Positive Psychology., 56(3), 218–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, & Branigan C (2005). Positive emotions broaden the scope of attention and thought-action repertoires. Cognition and Emotion, 19(3), 313–332. 10.1080/02699930441000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni AJ, Arruda EH, Krull JL, & Gonzales NA (2017a). Adolescent sleep duration, variability, and peak levels of achievement and mental health. Child Development., 89, e18–e28. 10.1111/cdev.12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni AJ, Bai S, Krull JL, & Gonzales NA (2017b). Individual differences in optimum sleep for daily mood during adolescence. Journal of Clinical Child & Adolescent Psychology, 0(0), 1–11. 10.1080/15374416.2017.1357126, 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Fredrickson B, Kring AM, Johnson DP, Meyer PS, & Penn DL (2010). Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review, 30(7), 849–864. 10.1016/j.cpr.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Geschwind N, Peeters F, & Wichers M (2015). Mindfulness training promotes upward spirals of positive affect and cognition: Multilevel and autoregressive latent trajectory modeling analyses. Frontiers in Psychology, 6. 10.3389/fpsyg.2015.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goleman DJ, & Schwartz GE (1976). Meditation as an intervention in stress reactivity. Journal of Consulting and Clinical Psychology, 44(3), 456–466. [DOI] [PubMed] [Google Scholar]
- Guan S-SA, Bower JE, Almeida DM, Cole SW, Dahl RE, Irwin MR, Seeman TE, McDade T, & Fuligni AJ (2016). Parental support buffers the association of depressive symptoms with cortisol and C-reactive protein during adolescence. Brain, Behavior, and Immunity, 57, 134–143. 10.1016/j.bbi.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeffel GJ, & Vargas I (2011). Resilience to depressive symptoms: The buffering effects of enhancing cognitive style and positive life events. Journal of Behavior Therapy and Experimental Psychiatry, 42(1), 13–18. 10.1016/j.jbtep.2010.09.003. [DOI] [PubMed] [Google Scholar]
- Hamilton NA, Catley D, & Karlson C (2007). Sleep and the affective response to stress and pain. Health Psychology, 26(3), 288–295. 10.1037/0278-6133.26.3.288. [DOI] [PubMed] [Google Scholar]
- Hammen CL (1991). Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology, 100(4), 555–561. [DOI] [PubMed] [Google Scholar]
- Hammen CL (2005). Stress and depression. Annual Review of Clinical Psychology, 1, 293–319. 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hammen CL (2015). Stress and depression: Old questions, new approaches. Current Opinion in Psychology, 4, 80–85. 10.1016/j.copsyc.2014.12.024. [DOI] [Google Scholar]
- Hankin BL, Mermelstein R, & Roesch L (2007). Sex differences in adolescent depression: Stress exposure and reactivity models. Child Development, 78(1), 279–295. [DOI] [PubMed] [Google Scholar]
- Hazel NA, Hammen C, Brennan PA, & Najman J (2008). Early childhood adversity and adolescent depression: The mediating role of continued stress. Psychological Medicine, 38(04), 581–589. 10.1017/S0033291708002857. [DOI] [PubMed] [Google Scholar]
- Hetrick SE, Cox GR, Witt KG, Bir JJ, & Merry SN (2016). Cognitive behavioural therapy (CBT), third-wave CBTand interpersonal therapy (IPT) based interventions for preventing depression in children and adolescents. The Cochrane Database of Systematic Reviews, 8, CD003380. 10.1002/14651858.CD003380.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honaker SM, & Meltzer LJ (2016). Sleep in pediatric primary care: A review of the literature. Sleep Medicine Reviews, 25, 31–39. 10.1016/j.smrv.2015.01.004. [DOI] [PubMed] [Google Scholar]
- Horowitz JL, & Garber J (2006). The prevention of depressive symptoms in children and adolescents: A meta-analytic review. [DOI] [PubMed]
- Irwin MR (2015). Why sleep is important for health: A psychoneuroimmunology perspective. Annual Review of Psychology, 66(1), 143–172. 10.1146/annurev-psych-010213-115205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin MR, Olmstead R, & Carroll JE (2016). Sleep disturbance, sleep duration, and inflammation: A systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biological Psychiatry, 80(1), 40–52. 10.1016/j.biopsych.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, & Prescott CA (1999). Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry, 156(6), 837–841. 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen H-U (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21(3), 169–184. 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, & Grob A (2015). Adolescents’ electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. Journal of Youth and Adolescence, 44(2), 405–418. 10.1007/s10964-014-0176-x. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, & Gotlib IH (2000). Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. The American Journal of Psychiatry, 157(10), 1584–1591. 10.1176/appi.ajp.157.10.1584. [DOI] [PubMed] [Google Scholar]
- Liu RT, & Alloy LB (2010). Stress generation in depression: A systematic review of the empirical literature and recommendations for future study. Clinical Psychology Review, 30(5), 582–593. 10.1016/j.cpr.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzucchelli TG, Kane RT, & Rees CS (2010). Behavioral activation interventions for well-being: A meta-analysis. The Journal of Positive Psychology, 5(2), 105–121. 10.1080/17439760903569154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMakin DL, Siegle GJ, & Shirk SR (2011). Positive affect stimulation and sustainment (PASS) module for depressed mood: A preliminary investigation of treatment-related effects. Cognitive Therapy and Research, 35(3), 217–226. 10.1007/s10608-010-9311-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meerlo P, Sgoifo A, & Suchecki D (2008). Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Medicine Reviews, 12(3), 197–210. 10.1016/j.smrv.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Mezulis AH, Abramson LY, Hyde JS, & Hankin BL (2004). Is there a universal positivity bias in attributions? A meta-analytic review of individual, developmental, and cultural differences in the self-serving attributional bias. [DOI] [PubMed] [Google Scholar]
- Minkel J, Moreta M, Muto J, Htaik O, Jones C, Basner M, & Dinges D (2014). Sleep deprivation potentiates HPA axis stress reactivity in healthy adults. Health Psychology, 33(11), 1430–1434. 10.1037/a0034219. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, & Han B (2016). National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics, e20161878. 10.1542/peds.2016-1878,138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulrow CD, Williams JW, Gerety MB, Ramirez G, Montiel OM, & Kerber C (1995). Case-finding instruments for depression in primary care settings. Annals of Internal Medicine, 122(12), 913–921. 10.7326/0003-4819-122-12-199506150-00004. [DOI] [PubMed] [Google Scholar]
- Ojio Y, Nishida A, Shimodera S, Togo F, & Sasaki T (2016). Sleep duration associated with the lowest risk of depression/anxiety in adolescents. Sleep, 39(8), 1555–1562. 10.5665/sleep.6020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens J, Adolescent Sleep Working Group, & Committee on Adolescence. (2014). Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics, 134(3), e921–e932. 10.1542/peds.2014-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306. [DOI] [Google Scholar]
- Roberts RE, & Duong HT (2014). The prospective association between sleep deprivation and depression among adolescents. Sleep, 37(2), 239–244. 10.5665/sleep.3388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Klein DN, Seeley JR, & Gau JM (2012). Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood. Clinical Psychological Science, 1, 41–53. 10.1177/2167702612457599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, & Gau JM (2015). Effectiveness trial of an indicated cognitive-behavioral group adolescent depression prevention program versus Bibliotherapy and brochure control at 1-and 2-year follow-up. Journal of Consulting and Clinical Psychology, 83(4), 736–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe G, Hirsh JB, & Anderson AK (2007). Positive affect increases the breadth of attentional selection. Proceedings of the National Academy of Sciences, 104(1), 383–388. 10.1073/pnas.0605198104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C, Burge D, Lindberg N, Herzberg D, & Daley SE (2000). Toward an interpersonal life-stress model of depression: The developmental context of stress generation. Development and Psychopathology, 12(2), 215–234. [DOI] [PubMed] [Google Scholar]
- Seligman ME, Rashid T, & Parks AC (2006). Positive psychotherapy. The American Psychologist, 61(8), 774–788. [DOI] [PubMed] [Google Scholar]
- Shih JH, Eberhart NK, Hammen CL, & Brennan PA (2006). Differential exposure and reactivity to interpersonal stress predict sex differences in adolescent depression. Journal of Clinical Child & Adolescent Psychology, 35(1), 103–115. 10.1207/s15374424jccp3501_9. [DOI] [PubMed] [Google Scholar]
- Shochat T, Flint-Bretler O, & Tzischinsky O (2010). Sleep patterns, electronic media exposure and daytime sleep-related behaviours among Israeli adolescents. Acta Paediatrica, 99(9), 1396–1400. 10.1111/j.1651-2227.2010.01821.x. [DOI] [PubMed] [Google Scholar]
- Shochat T, Cohen-Zion M, & Tzischinsky O (2014). Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Medicine Reviews, 18(1), 75–87. 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Silk JS, Vanderbilt-Adriance E, Shaw DS, Forbes EE, Whalen DJ, Ryan ND, & Dahl RE (2007). Resilience among children and adolescents at risk for depression: Mediation and moderation across social and neurobiological contexts. Development and Psychopathology, 19(03), 841–865. 10.1017/S0954579407000417. [DOI] [PubMed] [Google Scholar]
- Sin NL, & Lyubomirsky S (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467–487. 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- Sin NL, Graham-Engeland JE, Ong AD, & Almeida DM (2015). Affective reactivity to daily stressors is associated with elevated inflammation. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 34(12), 1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, & Irwin MR (2014). From stress to inflammation and major depressive disorder: A social signal transduction theory of depression. Psychological Bulletin, 140(3), 774–815. 10.1037/a0035302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Wardle J, & Marmot M (2005). Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proceedings of the National Academy of Sciences, 102(18), 6508–6512. 10.1073/pnas.0409174102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, & Rohde P (2009). A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology, 77(3), 486–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockings E, Degenhardt L, Lee YY, Mihalopoulos C, Liu A, Hobbs M, & Patton G (2015). Symptom screening scales for detecting major depressive disorder in children and adolescents: A systematic review and meta-analysis of reliability, validity and diagnostic utility. Journal of Affective Disorders, 174(supplement C), 447–463. 10.1016/j.jad.2014.11.061. [DOI] [PubMed] [Google Scholar]
- Tugade MM, & Fredrickson BL (2004). Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology, 86(2), 320–333. 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tugade MM, Fredrickson BL, & Feldman Barrett L (2004). Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. Journal of Personality, 72(6), 1161–1190. 10.1111/j.1467-6494.2004.00294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uliaszek AA, Zinbarg RE, Mineka S, Craske MG, Griffith JW, Sutton JM, Epstein A, & Hammen C (2012). A longitudinal examination of stress generation in depressive and anxiety disorders. Journal of Abnormal Psychology, 121(1), 4–15. 10.1037/a0025835. [DOI] [PubMed] [Google Scholar]
- Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulkader RS, Abdulle AM, Abebo TA, Abera SF, Aboyans V, Abu-Raddad LJ, Ackerman IN, Adamu AA, Adetokunboh O, Afarideh M, Afshin A, Agarwal SK, Aggarwal R, Agrawal A, Agrawal S, Ahmadieh H, Ahmed MB, Aichour MTE, Aichour AN, Aichour I, Aiyar S, Akinyemi RO, Akseer N, al Lami FH, Alahdab F, al-Aly Z, Alam K, Alam N, Alam T, Alasfoor D, Alene KA, Ali R, Alizadeh-Navaei R, Alkerwi A’, Alla F, Allebeck P, Allen C, al-Maskari F, al-Raddadi R, Alsharif U, Alsowaidi S, Altirkawi KA, Amare AT, Amini E, Ammar W, Amoako YA, Andersen HH, Antonio CAT, Anwari P, Ärnlöv J, Artaman A, Aryal KK, Asayesh H, Asgedom SW, Assadi R, Atey TM, Atnafu NT, Atre SR, Avila-Burgos L, Avokphako EFGA, Awasthi A, Bacha U, Badawi A, Balakrishnan K, Banerjee A, Bannick MS, Barac A, Barber RM, Barker-Collo SL, Bärnighausen T, Barquera S, Barregard L, Barrero LH, Basu S, Battista B, Battle KE, Baune BT, Bazargan-Hejazi S, Beardsley J, Bedi N, Beghi E, Béjot Y, Bekele BB, Bell ML, Bennett DA, Bensenor IM, Benson J, Berhane A, Berhe DF, Bernabé E, Betsu BD, Beuran M, Beyene AS, Bhala N, Bhansali A, Bhatt S, Bhutta ZA, Biadgilign S, Bicer BK, Bienhoff K, Bikbov B, Birungi C, Biryukov S, Bisanzio D, Bizuayehu HM, Boneya DJ, Boufous S, Bourne RRA, Brazinova A, Brugha TS, Buchbinder R, Bulto LNB, Bumgarner BR, Butt ZA, Cahuana-Hurtado L, Cameron E, Car M, Carabin H, Carapetis JR, Cárdenas R, Carpenter DO, Carrero JJ, Carter A, Carvalho F, Casey DC, Caso V, Castañeda-Orjuela CA, Castle CD, Catalá-López F, Chang HY, Chang JC, Charlson FJ, Chen H, Chibalabala M, Chibueze CE, Chisumpa VH, Chitheer AA, Christopher DJ, Ciobanu LG, Cirillo M, Colombara D, Cooper C, Cortesi PA, Criqui MH, Crump JA, Dadi AF, Dalal K, Dandona L, Dandona R, das Neves J, Davitoiu DV, de Courten B, de Leo DD, Defo BK, Degenhardt L, Deiparine S, Dellavalle RP, Deribe K, Des Jarlais DC, Dey S, Dharmaratne SD, Dhillon PK, Dicker D, Ding EL, Djalalinia S, Do HP, Dorsey ER, dos Santos KPB, Douwes-Schultz D, Doyle KE, Driscoll TR, Dubey M, Duncan BB, el-Khatib ZZ, Ellerstrand J, Enayati A, Endries AY, Ermakov SP, Erskine HE, Eshrati B, Eskandarieh S, Esteghamati A, Estep K, Fanuel FBB, Farinha CSES, Faro A, Farzadfar F, Fazeli MS, Feigin VL, Fereshtehnejad SM, Fernandes JC, Ferrari AJ, Feyissa TR, Filip I, Fischer F, Fitzmaurice C, Flaxman AD, Flor LS, Foigt N, Foreman KJ, Franklin RC, Fullman N, Fürst T, Furtado JM, Futran ND, Gakidou E, Ganji M, Garcia-Basteiro AL, Gebre T, Gebrehiwot TT, Geleto A, Gemechu BL, Gesesew HA, Gething PW, Ghajar A, Gibney KB, Gill PS, Gillum RF, Ginawi IAM, Giref AZ, Gishu MD, Giussani G, Godwin WW, Gold AL, Goldberg EM, Gona PN, Goodridge A, Gopalani SV, Goto A, Goulart AC, Griswold M, Gugnani HC, Gupta R, Gupta R, Gupta T, Gupta V, Hafezi-Nejad N, Hailu GB, Hailu AD, Hamadeh RR, Hamidi S, Handal AJ, Hankey GJ, Hanson SW, Hao Y, Harb HL, Hareri HA, Haro JM, Harvey J, Hassanvand MS, Havmoeller R, Hawley C, Hay SI, Hay RJ, Henry NJ, Heredia-Pi IB, Hernandez JM, Heydarpour P, Hoek HW, Hoffman HJ, Horita N, Hosgood HD, Hostiuc S, Hotez PJ, Hoy DG, Htet AS, Hu G, Huang H, Huynh C, Iburg KM, Igumbor EU, Ikeda C, Irvine CMS, Jacobsen KH, Jahanmehr N, Jakovljevic MB, Jassal SK, Javanbakht M, Jayaraman SP, Jeemon P, Jensen PN, Jha V, Jiang G, John D, Johnson SC, Johnson CO, Jonas JB, Jürisson M, Kabir Z, Kadel R, Kahsay A, Kamal R, Kan H, Karam NE, Karch A, Karema CK, Kasaeian A, Kassa GM, Kassaw NA, Kassebaum NJ, Kastor A, Katikireddi SV, Kaul A, Kawakami N, Keiyoro PN, Kengne AP, Keren A, Khader YS, Khalil IA, Khan EA, Khang YH, Khosravi A, Khubchandani J, Kiadaliri AA, Kieling C, Kim YJ, Kim D, Kim P, Kimokoti RW, Kinfu Y, Kisa A, Kissimova-Skarbek KA, Kivimaki M, Knudsen AK, Kokubo Y, Kolte D, Kopec JA, Kosen S, Koul PA, Koyanagi A, Kravchenko M, Krishnaswami S, Krohn KJ, Kumar GA, Kumar P, Kumar S, Kyu HH, Lal DK, Lalloo R, Lambert N, Lan Q, Larsson A, Lavados PM, Leasher JL, Lee PH, Lee JT, Leigh J, Leshargie CT, Leung J, Leung R, Levi M, Li Y, Li Y, Li Kappe D, Liang X, Liben ML, Lim SS, Linn S, Liu PY, Liu A, Liu S, Liu Y, Lodha R, Logroscino G, London SJ, Looker KJ, Lopez AD, Lorkowski S, Lotufo PA, Low N, Lozano R, Lucas TCD, Macarayan ERK, Magdy Abd el Razek H, Magdy Abd el Razek M, Mahdavi M, Majdan M, Majdzadeh R, Majeed A, Malekzadeh R, Malhotra R, Malta DC, Mamun AA, Manguerra H, Manhertz T, Mantilla A, Mantovani LG, Mapoma CC, Marczak LB, Martinez-Raga J, Martins-Melo FR, Martopullo I, März W, Mathur MR, Mazidi M, McAlinden C, McGaughey M, McGrath JJ, McKee M, McNellan C, Mehata S, Mehndiratta MM, Mekonnen TC, Memiah P, Memish ZA, Mendoza W, Mengistie MA, Mengistu DT, Mensah GA, Meretoja TJ, Meretoja A, Mezgebe HB, Micha R, Millear A, Miller TR, Mills EJ, Mirarefin M, Mirrakhimov EM, Misganaw A, Mishra SR, Mitchell PB, Mohammad KA, Mohammadi A, Mohammed KE, Mohammed S, Mohanty SK, Mokdad AH, Mollenkopf SK, Monasta L, Montico M, Moradi-Lakeh M, Moraga P, Mori R, Morozoff C, Morrison SD, Moses M, Mountjoy-Venning C, Mruts KB, Mueller UO, Muller K, Murdoch ME, Murthy GVS, Musa KI, Nachega JB, Nagel G, Naghavi M, Naheed A, Naidoo KS, Naldi L, Nangia V, Natarajan G, Negasa DE, Negoi RI, Negoi I, Newton CR, Ngunjiri JW, Nguyen TH, Nguyen QL, Nguyen CT, Nguyen G, Nguyen M, Nichols E, Ningrum DNA, Nolte S, Nong VM, Norrving B, Noubiap JJN, O’Donnell MJ, Ogbo FA, Oh IH, Okoro A, Oladimeji O, Olagunju TO, Olagunju AT, Olsen HE, Olusanya BO, Olusanya JO, Ong K, Opio JN, Oren E, Ortiz A, Osgood-Zimmerman A, Osman M, Owolabi MO, PA M, Pacella RE, Pana A, Panda BK, Papachristou C, Park EK, Parry CD, Parsaeian M, Patten SB, Patton GC, Paulson K, Pearce N, Pereira DM, Perico N, Pesudovs K, Peterson CB, Petzold M, Phillips MR, Pigott DM, Pillay JD, Pinho C, Plass D, Pletcher MA, Popova S, Poulton RG, Pourmalek F, Prabhakaran D, Prasad NM, Prasad N, Purcell C, Qorbani M, Quansah R, Quintanilla BPA, Rabiee RHS, Radfar A, Rafay A, Rahimi K, Rahimi-Movaghar A, Rahimi-Movaghar V, Rahman MHU, Rahman M, Rai RK, Rajsic S, Ram U, Ranabhat CL, Rankin Z, Rao PC, Rao PV, Rawaf S, Ray SE, Reiner RC, Reinig N, Reitsma MB, Remuzzi G, Renzaho AMN, Resnikoff S, Rezaei S, Ribeiro AL, Ronfani L, Roshandel G, Roth GA, Roy A, Rubagotti E, Ruhago GM, Saadat S, Sadat N, Safdarian M, Safi S, Safiri S, Sagar R, Sahathevan R, Salama J, Saleem HOB, Salomon JA, Salvi SS, Samy AM, Sanabria JR, Santomauro D, Santos IS, Santos JV, Santric Milicevic MM, Sartorius B, Satpathy M, Sawhney M, Saxena S, Schmidt MI, Schneider IJC, Schöttker B, Schwebel DC, Schwendicke F, Seedat S, Sepanlou SG, Servan-Mori EE, Setegn T, Shackelford KA, Shaheen A, Shaikh MA, Shamsipour M, Shariful Islam SM, Sharma J, Sharma R, She J, Shi P, Shields C, Shifa GT, Shigematsu M, Shinohara Y, Shiri R, Shirkoohi R, Shirude S, Shishani K, Shrime MG, Sibai AM, Sigfusdottir ID, Silva DAS, Silva JP, Silveira DGA, Singh JA, Singh NP, Sinha DN, Skiadaresi E, Skirbekk V, Slepak EL, Sligar A, Smith DL, Smith M, Sobaih BHA, Sobngwi E, Sorensen RJD, Sousa TCM, Sposato LA, Sreeramareddy CT, Srinivasan V, Stanaway JD, Stathopoulou V, Steel N, Stein MB, Stein DJ, Steiner TJ, Steiner C, Steinke S, Stokes MA, Stovner LJ, Strub B, Subart M, Sufiyan MB, Sunguya BF, Sur PJ, Swaminathan S, Sykes BL, Sylte DO, Tabarés-Seisdedos R, Taffere GR, Takala JS, Tandon N, Tavakkoli M, Taveira N, Taylor HR, Tehrani-Banihashemi A, Tekelab T, Terkawi AS, Tesfaye DJ, Tesssema B, Thamsuwan O, Thomas KE, Thrift AG, Tiruye TY, Tobe-Gai R, Tollanes MC, Tonelli M, Topor-Madry R, Tortajada M, Touvier M, Tran BX, Tripathi S, Troeger C, Truelsen T, Tsoi D, Tuem KB, Tuzcu EM, Tyrovolas S, Ukwaja KN, Undurraga EA, Uneke CJ, Updike R, Uthman OA, Uzochukwu BSC, van Boven JFM, Varughese S, Vasankari T, Venkatesh S, Venketasubramanian N, Vidavalur R, Violante FS, Vladimirov SK, Vlassov VV, Vollset SE, Wadilo F, Wakayo T, Wang YP, Weaver M, Weichenthal S, Weiderpass E, Weintraub RG, Werdecker A, Westerman R, Whiteford HA, Wijeratne T, Wiysonge CS, Wolfe CDA, Woodbrook R, Woolf AD, Workicho A, Xavier D, Xu G, Yadgir S, Yaghoubi M, Yakob B, Yan LL, Yano Y, Ye P, Yimam HH, Yip P, Yonemoto N, Yoon SJ, Yotebieng M, Younis MZ, Zaidi Z, Zaki MES, Zegeye EA, Zenebe ZM, Zhang X, Zhou M, Zipkin B, Zodpey S, Zuhlke LJ, & Murray CJL (2017). Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the global burden of disease study 2016. The Lancet, 390(10100), 1211–1259. 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1999). The PANAS-X: Manual for the positive and negative affect schedule-expanded form. Retrieved from http://ir.uiowa.edu/cgi/viewcontent.cgi?article=1011&context=psychology_pubs [Google Scholar]
- Werner-Seidler A, Perry Y, Calear AL, Newby JM, & Christensen H (2017). School-based depression and anxiety prevention programs for young people: A systematic review and meta-analysis. Clinical Psychology Review, 51, 30–47. 10.1016/j.cpr.2016.10.005. [DOI] [PubMed] [Google Scholar]
- Wetter EK, & Hankin BL (2009). Mediational pathways through which positive and negative emotionality contribute to anhedonic symptoms of depression: A prospective study of adolescents. Journal of Abnormal Child Psychology, 37(4), 507–520. 10.1007/s10802-009-9299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichers M. c., Myin-Germeys I, Jacobs N, Peeters F, Kenis G, Derom C, et al. (2007). Evidence that moment-to-moment variation in positive emotions buffer genetic risk for depression: A momentary assessment twin study. Acta Psychiatrica Scandinavica, 115(6), 451–457. 10.1111/j.1600-0447.2006.00924.x. [DOI] [PubMed] [Google Scholar]
- Wood AM, & Joseph S (2010). The absence of positive psychological (eudemonic) well-being as a risk factor for depression: A ten year cohort study. Journal of Affective Disorders, 122(3), 213–217. 10.1016/j.jad.2009.06.032. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Affleck GG, Tennen H, Reich JW, & Davis MC (2005). Dynamic approaches to emotions and stress in everyday life: Bolger and Zuckerman reloaded with positive as well as negative affects. Journal of Personality, 73(6), 1511–1538. 10.1111/j.0022-3506.2005.00357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


