Abstract
Magnesium (Mg2+) is the 2nd most abundant intracellular cation, which participates in various enzymatic reactions; there by regulating vital biological functions. Magnesium (Mg2+) can regulate several cations, including sodium, potassium, and calcium; it consequently maintains physiological functions like impulse conduction, blood pressure, heart rhythm, and muscle contraction. But, it doesn’t get much attention in account with its functions, making it a “Forgotten cation”. Like other cations, maintenance of the normal physiological level of Mg2+ is important. Its deficiency is associated with various diseases, which point out to the importance of Mg2+ as a drug. The roles of Mg2+ such as natural calcium antagonist, glutamate NMDA receptor blocker, vasodilator, antioxidant and anti-inflammatory agent are responsible for its therapeutic benefits. Various salts of Mg2+ are currently in clinical use, but their application is limited. This review collates all the possible mechanisms behind the behavior of magnesium as a drug at different disease conditions with clinical shreds of evidence.
Keywords: Magnesium, Calcium antagonist, Hypomagnesemia, NMDA blocker, Forgotten cation, Vasodilator
Introduction
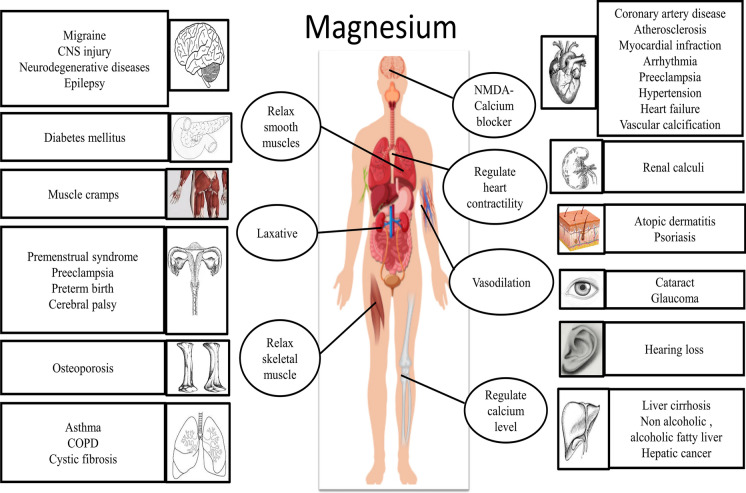
Macrominerals play important roles in regulating various vital functions in the human body and reducing risks for getting chronic diseases. Macroelements include elements such as calcium, magnesium, and phosphorous (Chronic et al. 1990). Magnesium (Mg2+) is an important divalent element belonging to the alkaline earth metal group. Magnesium is regarded as the 4th most abundant element in the body and the 2nd most intracellular cation (Romani 2011b; Jahnen-Dechent and Ketteler 2012). It plays various roles, such as acting as a cofactor for more than 300 enzymes, regulating physiological functioning of the heart and neurons, regulating blood pressure (BP), blood sugar level, etc. Besides, it also acts as a signaling molecule, reduces the neuronal excitotoxicity, maintains the level of potassium and calcium, regulates the synthesis, storage, and transport of ATP (Adenosine triphosphate) (McLean 1994; Rude 1989; Bharadwaj et al. 2014; Pham et al. 2014). Overall, magnesium (Mg2+) is considered as an important cation for maintaining normal physiological functions, as shown in Fig. 1 (Rude 1989; de Baaij et al. 2015; Pham et al. 2014). But magnesium (Mg2+) doesn’t get much attention due to two reasons. The first reason is that symptoms associated with altered Mg2+ levels appear only when the level becomes too low or too high. The second reason is that its exact role in maintaining normal physiology is poorly understood, making it a “forgotten cation.” (Bharadwaj et al. 2014; Ahmed and Mohammed 2019).
Fig. 1.
Physiological roles of magnesium on vital systems. Text in the circle represents the physiological role of Mg in various vital organs. Text in the rectangle indicate the diseases or disorders associated with magnesium deficiency
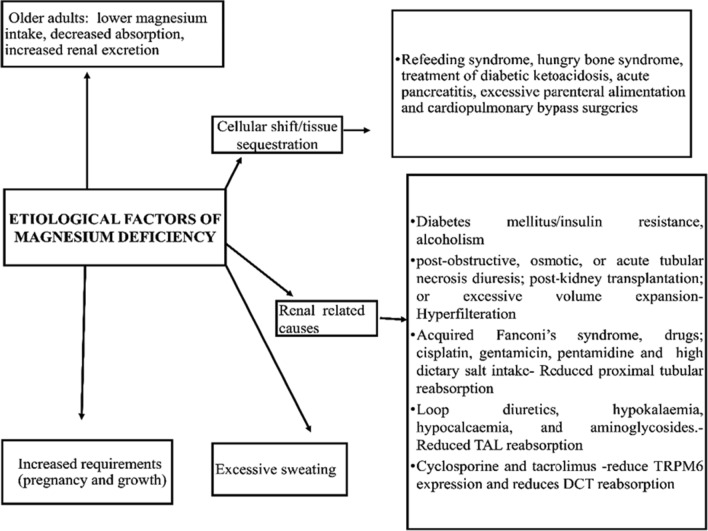
As per the United States Food and Nutrition, Recommended Daily Allowance (RDA) of Mg2+ is 420 mg for males and 320 mg for females. Around 10% of it is obtained through drinking water. Other sources of Mg2+ include green vegetables, unprocessed cereals, nuts, seeds, fish, meat, and milk products (Alexander et al. 2008). In the human body, Mg2+ mainly exists as storage form, and only a small amount is present extracellularly in serum. The concentration of Mg2+ in serum ranges from 0.5 to 1.05 mM, and its homeostasis is maintained through its absorption, reservoir, and excretion process by various organs such as the gut, bone, and kidney. Besides these organs, several hormones, namely vitamin D, parathyroid hormone, and estrogen, are involved in the regulation of normal level of Mg2+ (Al Alawi et al. 2018). Alteration in the level of Mg2+ may lead to hypomagnesemia or hypermagnesaemia. Hypermagnesaemia is characterized by neurologic and cardiac abnormalities like confusion, coma, widening of QRS complex, PR interval prolongation, and cardiac arrest. Whereas hypomagnesemia is manifested as tetany, convulsion, and cardiac arrhythmia (Alexander et al. 2008). Clinical and preclinical studies revealed that the Mg2+ level is found to be low in various pathological conditions such as migraine, diabetes, osteoporosis, asthma, preeclampsia, cardiovascular diseases (CVD), and its correction is an important treatment strategy for these conditions (Gröber et al. 2015; Dolati et al. 2019; Euser and Cipolla 2009; Li et al. 2017; DiNicolantonio et al. 2018b). Various factors may associate with Mg2+ deficiency (Fig. 2). In pathological conditions, various Mg2+ salts may also be used as a source of Mg2+(Table 1) (Pham et al. 2014; Gröber et al. 2015; Schwalfenberg and Genuis, 2017; Ahmed and Mohammed, 2019).
Fig. 2.
Factors associated with magnesium deficiency
Table 1.
Various clinically available magnesium supplements with their uses
| Magnesium supplement | Elemental content (%) | Bioavailability (%) | Particular uses |
|---|---|---|---|
| Magnesium oxide | 60 | 4 | Effervescent magnesium oxide is better absorbed (8%) than tablets |
| Magnesium carbonate | 45 | 15–40 | Treatment of hypomagnesaemia, heart burn, stomach upset and acid indigestion |
| Magnesium sulphate | 10 | 4 | Most commonly used clinical supplement |
| Magnesium hydroxide | 42 | 4 | Antacid and a cathartic |
| Magnesium citrate | 16 | 12 | Nephrolithiasis |
| Magnesium lactate | 12 | 12 | Treatment of hypomagnesaemia vomiting or diarrhoea or in gastrointestinal diseases |
| Magnesium chloride | 12 | 12 | Treatment or prevention of hypomagnesaemia |
| Magnesium aspartate | 10 | 41–45% (for 5 mg) | To treat fatigue and muscle hyper excitability |
Fate of magnesium in the body
Absorption
Even though 300 mg of Mg2+ is ingested under physiological conditions, only 24–75% is absorbed depending up on the its reserve and its level in consumed foods (Long and Romani 2014). Absorption occurs after 1 h of ingestion and becomes stable after 2–2.5 h for up to 4–8 h, and then it declines (Schuchardt and Hahn 2017). It is reported that about 65% of Mg2+ is absorbed upon its low intake, and only 11% is absorbed upon its high intake. Thus, the absorption rate is inversely linked with its intake (Rude 1989; Seo and Park 2008). Various exogenous and endogenous factors influence the absorption of Mg2+. Advanced age and endogenous factors like inflammatory bowel diseases, short bowel syndrome, etc., abate its absorption. Exogenous factors that increase its absorption include low or indigestible carbohydrates, namely inulin, mannitol, and lactose. Simultaneously, the presence of phylate, oxalate, and non-fermentable fibers impair its absorption (Schuchardt and Hahn 2017).
Mg2+ present in the diet is absorbed from the apical side of intestinal epithelial cells and it is then released into the blood through the basolateral side via Na+/Mg2+ exchanger (Long and Romani 2014). Mg2+ is absorbed through enterocytes into the bloodstream via two pathways, primarily by active transcellular transport (saturable) and secondarily by passive paracellular transport (not saturable). The major uptake (80–90%) mechanism is passive paracellular transport in the small intestine. This process is facilitated by a Mg2+concentration of about 1–5.0 mmol/L and a positive lumen voltage of about 15 mV (Gröber et al. 2015). The process is regulated by small transmembrane proteins referred as ‘Claudins’ (Schuchardt and Hahn 2017; Ahmed and Mohammed 2019; Gröber et al. 2015). Under reduced dietary intake of Mg2+, absorption switches to active transcellular transport, which occurs at large intestine mediated by Transient Receptor Potential Channel of Melastatin 6 and 7 (TRPM 6 and 7) (Ahmed and Mohammed 2019).
Storage, transport and exchange
An average adult human body contains about 24 g or 1000 mmol of Mg2+, of which 99% exist as storage form, 1% is available as in extracellular form in serum and red blood cells (RBC). Intracellular and serum magnesium concentrations range from 5 to 20 mmol/L and 0.76–1.15 mmol/L, respectively. Intracellular Mg2+ exists mainly as ionized form (1–5%), as bound with the proteins, and as in combination with the adenosine triphosphate (ATP) (Jahnen-Dechent and Ketteler 2012). Serum Mg2+ exists mainly as ionized form (55–70%), bound with the proteins (20–30%), and 5–15% of Mg2+ exist as sulphate, bicarbonate & phosphate salts (Swaminathan 2003). In RBCs, it is found to be relatively high with a range of around 1.65–2.65 mmol/L. In case of Mg2+ deficiency, a normal serum level is maintained by pulling it out from the RBCs. Thus RBC Mg2+ is considered as one of the good marker for Mg2+ deficiency (Razzaque 2018). The major storage sites for Mg2+ include bone (60%), muscle (20%), and soft tissues (19%) (Al Alawi et al. 2018). In bone, it exists as hydroxylapatite crystalline structure, which plays an important role in maintaining the normal serum level of Mg2+, and may get affected at the time of deficiency (Gröber 2019). Mg2+ content in bone is declined with age, and only one-third of it is available for ionic exchange to maintain the extracellular level (Jahnen-Dechent and Ketteler 2012; Gröber et al. 2015). The list of available Mg2+detection tests and significances are shown in Table 2 (Bharadwaj et al. 2014; Razzaque 2018; Al Alawi et al. 2018).
Table 2.
List of available magnesium detection tests with significances
| Laboratory tests | Importance |
|---|---|
| Red blood cell magnesium concentration | Reflect the actual magnesium status |
| Non-invasive intracellular mineral-electrolyte analysis (EXA) | To detect tissue level of magnesium |
| Hair mineral analysis test | Indicates the overall body chemistry and health status |
| Serum magnesium level | Less likely related with body magnesium content because it represent only 0.3% |
| 24 h excretion in urine or fractional excretion | More than 10–30 mg in 24 h excretion or above 2% in fractional excretion indicates renal wasting |
| Magnesium loading test | For the assessment of Intestinal and bone status of magnesium |
| Isotopic analysis of magnesium | 26Mg was used to evaluate absorption of magnesium from the gastrointestinal tract, But its limited to research purposes |
| Serum magnesium/calcium quotient | Sensitive indicator of magnesium status and turn over |
Different tissues respond in diverse ways towards the Mg2+ exchange. For example, in the heart, kidney, and adipocytes, the exchange of Mg2+occurs within 3–4 h. Conversely, in the brain (10%) and skeletal muscle (25%), the exchange of Mg2+ occurs after 16 h or more. In lymphocytes, it needs more than 40 h to exchange about 5–7% of Mg2+ (Vormann 2016; Romani 2011a, b; Maguire and Cowan 2002). Another reason for the limited exchange of Mg2+ is its binding with water, restricting the bare ion entry through the membrane. This situation is common to all ions but is greater for Mg2+ because the radius of its hydrated moiety formed with water is 400 times larger than its ionic radius(Maguire and Cowan 2002).
Excretion
The kidney plays an important role in the maintenance of serum Mg2+ level. In a day, around 2400 mg of Mg2+ is filtered by glomeruli; from that, only 100 mg is excreted, and 95% is reabsorbed back. The absorption process occurs at the thick ascending Loop of Henle (65%) and in distal convoluted Tube (DCT) (30%) (Saris et al. 2000; Seo and Park 2008; Al Alawi et al. 2018). The process at the thick ascending loop is facilitated by various transporters like paracellin1/claudin16 and 19. Transport in DCT is mediated by TRPM6 (Gröber 2019; Ahmed and Mohammed 2019; de Baaij et al. 2015). The abnormalities in the functioning of these transporters of Mg2+ may lead to various diseases and are listed in Table 3 (Kolte et al. 2014; de Baaij et al. 2015; Pham et al. 2014). Genetic disorders associated with the mutation of Mg2+transporters are listed in Table 4 (de Baaij et al. 2015; Seo and Park 2008).
Table 3.
List of magnesium transporters in different organs and diseasesassociated with its abnormalities
| Transporter | Expression | Associated diseases |
|---|---|---|
| Members of the Cyclin M (CNNM) | ||
| CNNM1 | Brain | Urofacial Syndrome 1 and Jalili Syndrome |
| CNNM2 | Kidney | Hypomagnesemia with seizure and mental retardation |
| CNNM3 | Ubiquitous expression | Pneumonic Tularemia and Jalili Syndrome |
| CNNM4 | Intestine | Jallili syndrome |
| Transient receptor potential melastatin cation channels | ||
| TRPM6 | Kidney, intestine | Hypomagnesemia with secondary hypocalcemia |
| TRPM7 | Ubiquitous | Cardiac fibrosis, atrial fibrillation, anoxic brain injury |
| Solute carrier family 41 member | ||
| SLC41A1 | Ubiquitous | Preeclampsia, nephronophthisis, Parkinson disease |
| SLC41A2 | Ubiquitous | Insulin-dependent diabetes mellitus, Epstein-Barr virus vnfection and Neoplasia |
| Mitochondrial RNA splicing 2 Mrs2 | Ubiquitous | Large congenital melanocytic mevus and Osteopetrosis |
| Paracellin-1 | Ascending limb of loop of Henle | Familial hypomagnesemia with hypercalciuria and nephrocalcinosis |
| Mg2 + transporter 1 MagT1 | Ubiquitous | X-linked Mg2 + deficiency with Epstein-Barr virus infection and neoplasia |
Table 4.
Examples of genetic disorders responsible for causing magnesium deficiency along with genes involved
| Diseases | Affected genes | Features |
|---|---|---|
| Familial hypomagnesemia with hypercalciuria and nephrocalcinosis type 1 (FHHNC1) | Claudin 16 (CLDN16) | Renal magnesium and calcium wasting, nephrocalcinosis and hypomagnesemia |
| Familial hypomagnesemia with hypercalciuria and nephrocalcinosis type 2 (FHHNC2) | Claudin 19 (CLDN16) |
Severe hypomagnesemia accompanied with nephrocalcinosis. and hypercalciuria Ocular defects such as significant myopia, macular colobomata, and horizontal nystagmus |
| Hypomagnesemia with secondary hypocalcemia (HSH) | Transient receptor potential melastatin type 6 (TRPM6) | Low levels of calcium and magnesium in serum leading to neurological and muscular complication |
| Isolated autosomal recessive hypomagnesemia (IRH) | Epidermal growth factor (EGF) | Declined serum and urine magnesium level, Seizure precipitation and psychomotor retardation |
| Autosomal dominant hypomagnesemia (ADH) | KCNA1 | Muscle cramps, weakness, tetanic episodes, and tremor. Reduced serum magnesium level |
| Hypomagnesemia with seizures and mental retardation (HSMR) | Cyclin M2; CNNM2 | Reduced serum magnesium level without affecting other electrolytes seizures, loss of consciousness, loss of muscle tone, headaches and staring |
| Seizures, sensorineural deafness, ataxia,mental retardation, and electrolyte imbalance/epilepsy, ataxia, sensory neural deafness and renal tubulopathy syndrome | KCNJ10 | Patients experiences electrolyte imbalance with hypokalemic metabolic alkalosis, severe hypomagnesemia, renal Na+, K+ and Mg2+ wasting |
| Isolated dominant hypomagnesemia (IDH) | FXYD domain containing ion transport regulator 2 (FXYD2) | Convulsions and hypomagnesemia |
| Renal cysts and diabetes syndrome (RCAD) | Hepatocyte nuclear factor 1B HNF1B | Hypomagnesemia, renal cyst genital and pancreatic abnormalities |
| Transient neonatal hyperphenyalaninemia and high urinary levels of primapterin HPABH4D | Pterin-4-alpha-carbinolamine dehydratase; PCBD1 | Hypomagnesemia, renal Mg2+ wasting, maturity-onset diabetes of the young(MODY5)-like diabetes |
| Gitelman’s syndrome | SLC, solute carrier; SLC12A3 | Hypomagnesemia and hypokalemia are the cardinal symptoms with tetany, paresthesias, and chondrocalcinosis |
| Bartter’s syndrome type 1 | SLC, solute carrier; SLC12A1 | Salt wasting, elevated plasma renin, aldosterone levels,hypokalemic alkalosis and low BP |
| Bartter’s syndrome type 2 | KCNJ1 | |
| Bartter’s syndrome type 3 | CLCNKB | |
| Bartter’s syndrome type 4 | BSND | |
| Kearns–Sayre syndrome | Mitochondrial deletion | Retinopathy, external ophthalmoplegia and cardiac conduction defects |
Cellular roles of magnesium
Extracellular and intracellular Mg2+ play various physiological roles. Usually, the concentration of negative ions in cells is higher than that of the cations; therefore, various metal ions can act as counter ions and intracellular buffers. This includes calcium, magnesium, sodium, and potassium. Positively charged Mg2+ serves as a counter ion to interact with negatively charged molecules such as ribonucleic acid (RNA), deoxyribonucleic acid (DNA), reactive oxygen species (ROS), and ATP. Mg2+ is thereby involved in the stabilization of DNA/RNA, modulation of enzyme activities, regulation of ion channel functioning, and protection of the cell from oxidative stress. So a disturbance in the Mg2+ level may impair these functions and contribute to pathological conditions (de Baaij et al. 2015; Wolf and Trapani 2008; Yamanaka et al. 2019).
Intracellular Mg2+ is important to regulate various biochemical reactions involved in protein synthesis, energy metabolism, and signal transduction (Terasaki and Rubin 1985; Stangherlin and O’Neill 2018). Furthermore, it participates in the intracellular signaling process by promoting protein kinase activity. Phosphorylation of protein kinase is a vital step in signal transduction, which is carried out by transferring a phosphate group from ATP to residue side chain containing serine, threonine, or tyrosine. Mg2+ is involved in the transition phase of phosphate group transfer (Knape et al. 2015). Affinity analysis studies reported the need for a low binding free energy for ATP to bind with protein kinase in the presence of Mg2+, which points out its role in enhancing the binding affinity of ATP to protein kinase (Yu et al. 2011). It protects cells from free radicals due to its free radical scavenging property. Intracellular Mg2+ participates in the maintenance of genome stability by acting as a cofactor for enzymes involved in the DNA repair process and by acting as a competitive inhibitor of DNA damaging agents. Extracellular Mg2+ participate in the ion channel regulation, especially the NMDA receptor of glutamate and is important in maintaining normal neuronal functions (Yamanaka et al. 2019). Nerve cells are communicated through electrical and chemical signals. Mg2+ controls the strength of channel protein at the gap junction in the electrical synapse. Besides, Mg2+ influx is triggered in the neuron at the time of chemical synapse mediated activities. Hence Mg2+ is important for regulating electrical and chemical neuronal communication; it implies its role in synaptic plasticity and neuronal network generation (Yamanaka et al. 2019).
Role of magnesium in brain
The cytosolic Mg2+ level in the brain is estimated by P31 Magnetic resonance spectroscopy (31P MRS) and is found to be 0.182 mM; which is about half that in skeletal muscle; strengthens the report of lower ATP concentration in the brain. The decreased concentration of Mg2+ is associated with neurological diseases by triggering several biological and metabolic dysfunctions, which is further facilitated by diminished ATP production and altered Na+/K+ATPase activity (Iotti and Malucelli 2011). The blood–brain barrier (BBB) plays a major role in separating extracellular fluid (ECF) from blood circulation and facilitates the transport of materials across the brain. Various substances are transported across BBB to maintain the ionic concentration gradient between ECF and the extracellular space. Mg2+ concentration in ECF is higher than that in the cerebrospinal fluid (CSF) and plasma; this indicates that Mg2+ is actively transported to the brain. Similarly, the concentration of Mg2+ in CSF is higher than that in plasma, implying the active transport mechanism involved in Mg2+ transport. The concentration of Mg2+ in CSF is interrelated with various brain functions and reported to be altered in various neurological disorders. Although the mechanism involved in the transport process of Mg2+ across the brain is still not clear, in vitro studies indicate the expression of various transporters like Transient Receptor Potential Channel of Melastatin and Magnesium transporter 1 (MagT1) in human brain endothelial cells (Yamanaka et al. 2019). Administration as organic salts and as combined form with polyethylene glycol (PEG) were tried to improve the brain delivery of Mg2+, but, not found to be effective in correcting its altered level (Wang et al. 2017; Lee et al. 2010; Busingye et al. 2016).
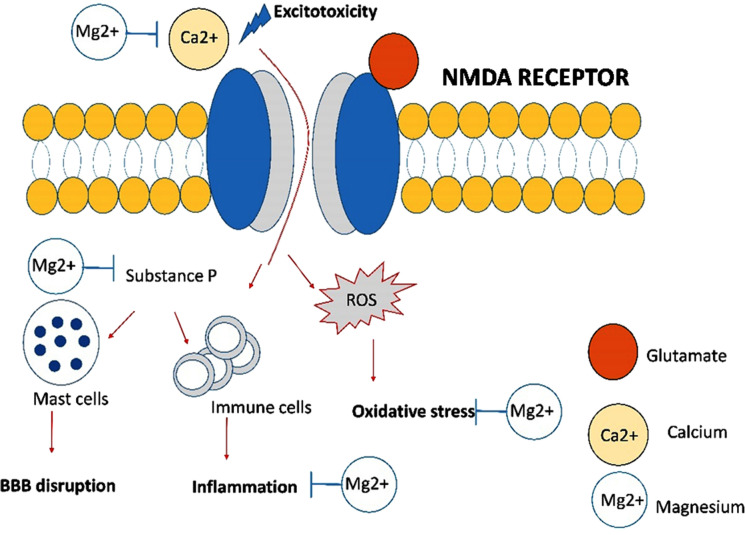
Mg2+ concentration in the brain is related to neuronal excitation, mediated by various neurotransmitters, including glutamate, which acts on the α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor (AMPA), N-methyl-d-aspartate receptor (NMDA), kainite, and metabotropic receptors present on the postsynaptic membranes. Physiologically at normal membrane potential (− 70 mV), the NMDA receptor is blocked by the Mg2+ so that glutamate can act only on the AMPA receptor. Activation of AMPA facilitates the ionic movement across the neuronal membranes, resulting in a rise in the potential to more than − 60 mV, which removes the Mg2+ block and thus activates NMDA receptors. Deficiency of extracellular Mg2+ results in the hyper-excitation of neurons due to NMDA over-activation. In addition to the NMDA receptor, Mg2+ can regulate the gamma-aminobutyric acid A receptor (GABAA) receptor, which is inhibitory in nature. The activation of GABAA receptor results in the influx of chloride ions, causing neuronal hyperpolarization and inhibition. Mg2+ is considered as a GABAA receptor agonist, can acts on this receptor-like benzodiazepines, and exhibits anxiolytic activity. This effect is antagonized by flumazenil; a GABA receptor antagonist, which confirms the agonistic property of Mg2+ on this receptor. The low central nervous system (CNS) level of Mg2+ may reduce GABAA receptor activity, resulting in higher membrane potential; may remove the Mg2+ blockade of the NMDA channel and contribute to excitotoxicity (Poleszak 2008; de Baaij et al. 2015). Further, if extracellular Mg2+ is found to be less, there is increased calcium influx, which increases the release of glutamate and hence causes excitotoxicity (Blanke and VanDongen 2008). Another vital activity of Mg2+ in the brain is its inhibitory effect on the oxidative stress and generation of vasoactive peptides, namely calcitonin gene-related peptide (CGRP), Substance P, etc. Deficiency of Mg2+ resulted in increased calcium concentration, increased production of ROS, and ROS-mediated cell death. Mg2+ deficiency promotes the release of inflammatory mediators like interleukin and tumor necrosis factor-α (TNF-α) via the activation of the substance P. Furthermore, Mg2+ is involved in the activation of nitric oxide synthase, increases the production of nitric oxide (NO); which is involved in various functions like vasodilation, channel regulation and release of neurotransmitters (de Baaij et al. 2015).
Magnesium and neurological diseases
Mg2+ deficiency has been reported in various brain-related diseases like migraine, stroke, neurodegenerative diseases, depression, epilepsy, etc. It is reported that the breakdown of BBB, edema, excitotoxicity and ROS production associated with neurological diseases can be corrected by the use of Mg2+ (Fig. 3).
Fig. 3.
Showing the relationship between excito-toxicity and the beneficial effect of magnesium in it. Excess of calcium influx in brain may cause causes various complication in brain such as excitotoxicity, BBB disruption, inflammation and oxidative stress. Magnesium is found to be beneficial in neurological diseases via correcting the above mentioned complications. i.e., inhibiting calcium influx, substance P production, inflammation and oxidative stress. ROS reactive oxygen species, NMDA receptor N methyl D aspartate receptor, BBB blood brain barrier
Migraine
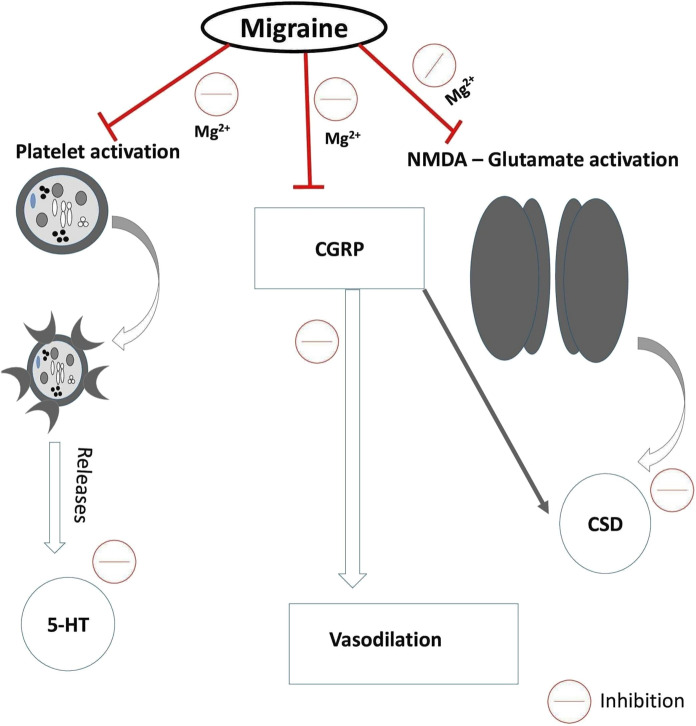
Migraine is a recurrent throbbing headache and is a common neurological cause of disability in the world. Migraine condition is associated with various complications like activation of NMDA receptor (may cause cortical spreading depression), the release of calcitonin Gene-Related Peptide-CGRP (causes vasodilatation), and 5-HT (Serotonin) from platelet, resulted in platelet activation. The disorder is characterized by symptoms like emesis, nausea, occasionally with photophobia and phonobia. The level of Mg2+ is found to be less in serum and CSF of patients with migraine (Dolati et al. 2019). Mg2+ exhibited anti-migraine activity by inhibiting the activation of NMDA receptor, CGRP release, and hyper aggregation of the platelet. Mg2+ acts in migraine by various mechanisms like counteracting cortical spreading depression, modulating neurotransmitter action (serotonin, nitric oxide, and glutamate), increasing ATP production, decreasing platelet aggregation, and by its neuroprotective and anti-inflammatory activity (Fig. 4) (Xue et al.2019; Sun-Edelstein and Mauskop 2009; Dolati et al. 2019). Intravenous magnesium can reduce the acute migraine attacks; meanwhile, oral administration of magnesium reduces the intensity and frequency of attack (Chiu et al. 2016). Research works reports revealed that the magnesium sulphate supplement is found to be effective in migraine with aura, but it is not effective in common attack. Whereas magnesium citrate is found to be effective in migraine without aura (Schwalfenberg and Genuis 2017; Chiu et al. 2016; Chen et al. 2016). Magnesium pidolate is reported to cross BBB rather than depositing on the bone; it has been tried to use in migraine (Maier et al. 2020).
Fig. 4.
Anti-migraine mechanism of action of magnesium: Migraine is due to mainly three reasons such as platelet activation, CGRP release and cortical spreading depression. Magnesium exhibiting its Antimigraine action through inhibiting platelet aggregation, serotonin release, inhibiting CGRP mediated vasodilation, and inhibiting CSD. 5 HT-serotonin, CGRP calcitonin gene related peptide, NMDA N methyl D aspartic acid receptor, CSD cortical spreading depression
CNS injury
Traumatic CNS injury may results in a decrease in intracellular Mg2+ level to 40–60% with a 10–15% decrease in total Mg2+ level; which may affect the entry of glutamate and calcium into the presynaptic neuron (Sperl et al. 2019; Cook et al. 2011). This results in neurodegeneration and cell death as secondary to brain injury (Institute of Medicine (US) Committee on Nutrition 2011). Secondary injuries include diffuse axonal injury, edema (both vasogenic and cytotoxic), extra-synaptic NMDA receptor-mediated toxicity, neurogenic inflammation, oxidative stress, mitochondrial dysfunction, and inflammation. The various studies reported that Mg2+ deficiency accelerates the release of substance P and pro-inflammatory mediators. There are various mechanisms that mediate the neuroprotective effect of Mg2+ in CNS injury. The first and most important among this is through the blockade of the NMDA receptor by Mg2+, which is otherwise responsible for the excitotoxicity. The second way is by providing protection against oxidative stress by reducing the generation of free radicals and hence lipid peroxidation. The third mechanism is by preserving mitochondrial membrane integrity through the decreased production of lactic acid and there by correcting mitochondrial dysfunction (Turner and Vink 2011).
Neurodegenerative diseases
Parkinson’s disease
Parkinson’s disease is a neurological disorder characterized by the loss of dopaminergic neurons in basal ganglia, resulted in the resting limb tremor, slowed and involuntary body movements, dyskinesia, impaired cognitive and non-motor functions (Yamanaka et al. 2019). Excitotoxicity is considered as one of the principal cause of Parkinson’s disease; that may lead to loss of dopaminergic neurons. An elevated level of inorganic phosphate along with declined cytosolic free Mg2+ and unchanged level of phosphocreatine is reported in Parkinson’s Patients. The possible mechanisms that cause Parkinson’s diseases are mitochondrial damage associated with increased free radical production, unfolded protein retention, and endoplasmic stress. Mitochondrial dysfunction resulted in the aggregation of α-synuclein, which is a presynaptic neuronal protein. Aggregation of α-synuclein with iron initiates oxidative stress, resulting in the combination of Parkin and DJ1genes, which prevent unfolded protein destruction. Usually, the misfolded protein aggregates and damaged organelles are degraded by autophagy, a process carried out by lysosomes. The impairment of this pathway leads to the accumulation of synuclein. Mg2+ transporter, SLC41A2 is located in PARK 16 gene, which is reported to have a role in Parkinson’s disease progression (de Baaij et al. 2015). Mg2+ is effective in the treatment of Parkinson’s disease via two mechanisms. Primarily by inhibiting the aggregation of α-synuclein with iron and other metals. The second mechanism is by having a regulatory effect on the mTOR pathway (mTOR pathway) involved in the deactivation of the autophagy process responsible for the accumulation of synuclein (Yamanaka et al. 2019). Mg2+, by regulating the mTOR pathway, reduces synuclein formation and protects the dopaminergic neurons. (Kirkland et al. 2018; Yamanaka et al. 2019). Furthermore, the prevention of neuro-inflammation by Mg2+ also contributes an additional protective effect in PD treatment.
Alzheimer’s disease
Alzheimer’s disease (AD) is a neurological disorder with loss of cholinergic transmitter in CNS and affects primarily the cognitive function. This disease is characterized by the accumulation of extracellular senile plaques and intracellular tangles within the brain cells, along with inflammation and atrophy (Yamanaka et al. 2019). A systemic review revealed a low level of Mg2+ in CSF and hair of AD patients, without any significant change in serum Mg2+ level, when compared with normal subjects (Veronese et al. 2016). Extracellular Mg2+ is reported to control the BBB permeability of amyloid β plaque to ECF and enhances its clearance. Mg2+ exhibits anti-inflammatory property via reducing the expression of TNF-α and production of pro-inflammatory mediators, which also contribute beneficial effect in Alzheimer’s condition. Low extracellular Mg2+ initiate the cleavage of Amyloid precursor protein (APP) by β secretase and γ secretase into C terminal fragment β (CTF β) and Aβ; which are neurotoxic. High extracellular Mg2+ switches the pathway to form soluble APP and CTFα, which is neurotrophic (Xue et al. 2019; Gröber et al. 2015; Kirkland et al. 2018). Further, Mg2+ inhibits glycogen synthase kinase-3 β (GSK-3β) enzyme (an enzyme involved in the cellular apoptotic process), reduces neuronal cell death, improves cognitive function and synaptic plasticity in sporadic rat’s model of AD (Xu et al. 2014).
Epilepsy
Anticonvulsant effect of Mg2+ is mediated by various mechanisms such as by antagonizing NMDA receptor, by increasing vasodilatory prostaglandin’s production, and by stabilizing neuronal membrane. Severe hypomagnesemia condition may precipitate generalized tonic–clonic seizures. Mg2+ is a potent modulator of seizure activity by inhibiting calcium influx through the NMDA receptor. Additionally, low Mg2+ content reduces the neuronal membrane surface charge and results in hyper-excitability (Yuen and Sander 2012). Mg2+ also has a role to act as a cofactor in the GABA synthesis, which also accounts for its anti-seizure activity. Higher intake of dietary Mg2+ is connected with a lower incidence of epilepsy and is thought to be mediated by decreased C reactive protein production (Yary and Kauhanen 2019). Na+/K+ATPase activity also changes with a decrease in the Mg2+ concentration and which increases the susceptibility to seizure (Haensch 2010). It is reported that depletion of Mg2+ prone to epileptic seizure by irritating the nervous system. Nuytten et al. 1991 studied two case reports; it indicates that intractable epilepsy is associated with Mg2+ deficiency (Nuytten et al. 1991). Supplementation of magnesium as magnesium sulphate has a beneficial effect in the pentylenetetrazol (PTZ) induced seizure model. Magnesium at an intermediate dose of 100 µg/mL
is effective in most epileptic conditions, whereas the low dose of 32 µg/mL is effective in partial complex seizures. Thus magnesium salt exhibit a dose-dependent effect in the treatment of epilepsy (de Oliveira et al. 2011). Mg2+ has a beneficial role in correcting the declined levels of synaptically released GABA associated with drug-resistant epilepsy (DRE). So that Mg2+ supplements decrease the number of days having seizures per month, in case of DRE patients. Thus, oral magnesium supplement therapy is used as an adjuvant in DRE treatment (Abdullahi et al. 2019). In epileptic patients, the low serum Mg2+ may associated with fatal cardiac events and causes sudden unexpected death (Terra et al. 2011). Magnesium sulphate is also found to be effective in the treatment of porphyria-associated seizures since most of the antiepileptic drugs are contraindicated in this situation (Sadeh et al. 1991). Magnesium sulphate is also effective in the treatment of refractory status epilepticus due to febrile illness-related epilepsy (Tan et al. 2015).
Role of magnesium in cardio vascular system
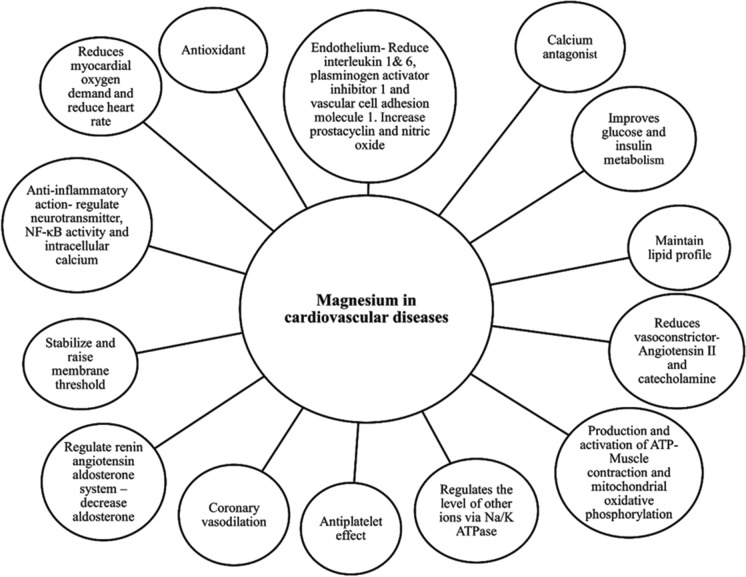
Mg2+ plays an important role in maintaining normal physiological functions of cardiac tissue through vasodilation by reducing vascular resistance, improving blood circulation, maintaining the electrical property of the myocardium, and by its anti-inflammatory activity (Kolte et al. 2014; de Baaij et al. 2015). Mg2+ also exhibits effects similar to clopidogrel by inhibiting platelet aggregation and adhesion (Tangvoraphonkchai and Davenport 2018). It is reported that Mg2+ deficiency can induce oxidative stress, which in turn activates the inflammatory process mediated via nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB). These inflammatory events trigger the transcription of various cytokines and pro-inflammatory mediators with increased expression of matrix metalloproteinase 2 and 9. This condition ultimately results in various pathological conditions like atherosclerosis, thrombus formation, and vascular calcification (Rude 1989; Chronic et al. 1990; Tangvoraphonkchai and Davenport 2018). Mg2+ can also affect the ionic concentration of calcium and potassium, which has a significant role in maintaining normal cardiac physiology (Chakraborti et al. 2002). Mg2+ competes with calcium-binding proteins and transporters, results in a change in the concentration of intracellular unbound calcium (de Baaij et al. 2015). Extracellular Mg2+ acts as a calcium antagonist, inhibit calcium channel conduction, increases the excitation threshold potential, and contributes to the membrane-stabilizing effect (Kolte et al. 2014). Mg2+ regulates K+, which plays a key role in myocardial conduction. Several clinical studies revealed the relationship between low intake of dietary magnesium with cardiac diseases, and it is reported that the maintenance of the normal physiological level of Mg2+ has a beneficial effect in various CVD (Geiger and Wanner 2012). In cardiac patients, magnesium supplementation reduces the Carotid Intima-Media Thickness (IMT), an index of atherosclerosis associated with various CVD (Kupetsky-Rincon et al. 2012; Pokan et al. 2006). The beneficial effects of Mg2+ on cardiac tissue are depicted in Fig. 5.
Fig. 5.
The beneficial role of magnesium in cardiac tissue
Magnesium and CVS disorders
Coronary artery diseases (CAD) and atherosclerosis
Atherosclerosis is one of the common risk factors for triggering various CVD. Like endothelial dysfunction and hyperlipidemia, hypomagnesemia is also considered as one of the risk factors for atherosclerosis. Mg2+ acts as a cofactor for many enzymes like pyrophosphatase, lipoprotein lipase, etc., which are involved in lipid metabolism. The deficiency of Mg2+ may affect the functioning of these enzymes, resulting in altered lipid metabolism and atherosclerosis (Deepti, and Nalini 2014; Geiger and Wanner 2012). Thus Mg2+ is effective in improving the lipid profile and endothelial dysfunction. Also, Mg2+ decreases the ROS production, reduces oxidative damage, and prevents the blood clots formation by inhibiting platelet aggregation. These factors provide advantages in the treatment of CAD. As per a study conducted on CAD patients, it is reported that administration of magnesium for 6 months offered an improvement in the maximal oxygen uptake, left ventricular ejection fraction, corrected endothelial dysfunctions, and reduces platelets induced thrombosis in CAD patients (Pokan et al. 2006).
Myocardial infarction
Myocardial infarction (MI) is resulted from the reduced blood flow to the cardiac tissue due to the formation of the plaques with interrupted myocardial oxygen supply. Commonly used treatment includes nitroglycerine and aspirin (Lu et al. 2015). Mg2+ provides beneficial effects through its vasodilatory effects and by preventing blood clot formation (Gröber et al. 2015; Pham et al. 2014). Anti-ischemic effect of Mg2+ is mediated through various mechanisms such as its calcium antagonistic property, by preserving the energy-dependent cellular process through the conservation of ATP, by decreasing the heart rate and contractility, by reducing the catecholamine-induced oxygen demand, and systemic afterload (Kolteet al. 2014). Second Leicester Intravenous Magnesium intervention trial (LIMIT 2) reported that Mg2+ effectively reduces mortality and left ventricular failure associated with acute mania (Gröber et al. 2015). Gyamlani et al. 2000 reported that magnesium administration after immediate post-infarction reduces the incidence of arrhythmia, pump dysfunction, and mortality associated with acute MI condition (Gyamlani et al. 2000). Studies conducted on various animal models revealed that Mg2+ deficiency is associated with decreased levels of endogenous antioxidants, elevated ROS levels, and increased susceptibility of the cardiovascular system to oxidative stress (Dinicolantonio et al. 2018; Kharb and Singh 2000). ROS can attack the cardiac cell membrane lipids, and cytoplasmic proteins cause nuclear and mitochondrial damage. Further, ROS can destruct the cell membrane poly-unsaturated fatty acids (PUFA), form lipid peroxides, fatty acid radicals and finally, fatty acid peroxy radicals. Thus, the free radical initiation and propagation reactions continued to form stable products like malondialdehyde (MDA); which is reported to inhibit the contractile functions of the heart and hence affect the myocardial oxygen supply. The PUFA of the subcellular organelles and sarcolemma of the cardiac myocytes are particularly susceptible to oxidative damage caused by ROS (Bandyopadhyay et al. 2005). A study conducted on 22 patients demonstrated that Mg2+ deficiency can exacerbate oxidative damage to post-ischemic myocardium, and the antioxidants are found to have beneficial effects in this condition (Freedman et al. 1990). A study report revealed that Mg2+ reduces the infarct size and mortality rate in MI patients (Antman 1996; Teo et al. 1991). A meta-analysis study indicates that Mg2+ has a beneficial effect in reducing arrhythmias in patients with MI (Salaminia et al. 2018). Thus magnesium supplementation is considered as an adjuvant in the treatment of MI (Rosique-Esteban et al. 2018). Some trials fail to prove its efficacy studies for introducing Mg2+ for MI; studies are still ongoing, owing to its low cost, ease of administration, good tolerability, and experimentally proven cardioprotective function (Kolteet al. 2014).
Arrhythmia
Cardiac arrhythmia is a condition characterized by an irregular heartbeat rhythm that may be either too slow (< 60 beats/min) or too fast (> 100 beats/min) and may occur at any age (Du-guan 2015). Normal cardiac rhythm is maintained by various ions like sodium, potassium, and calcium (Antzelevitch and Burashnikov 2011). Mg2+ deficiency is one of the risk factors for ventricular and supraventricular arrhythmia (Salaminia et al. 2018). The ECG changes observed in hypomagnesemia conditions include prolonged QT interval, depressed ST segment, and low amplitude of T waves. Hypomagnesaemia arises from stress or alcoholism is also responsible for inducing arrhythmias (Ramee et al. 1985; Topol and Lerman 1983). Mg2+ deficiency contributes to cardiac arrhythmia by disrupting the activity of Na+/K+ ATPase causes an imbalance between intracellular and extracellular potassium levels, impair the resting membrane and repolarization potential of normal cardiac electrophysiology (Dyckner and Wester 1981). The Mg2+ effectively prevents atrial fibrillation occurred after cardiac surgery, and intravenous magnesium is preferred as prophylaxis at this situation by the European association for cardiothoracic surgery and the Canadian cardiovascular society (Ho 2008; Onalan et al. 2007; Alghamdi et al. 2005; Miller et al. 2005). In addition, to this Mg2+ is also reported to be effective in treating Torsade’s des point, digoxin induced tachyarrhythmia’s, neuroleptic or tricyclic antidepressant-induced ventricular arrhythmia, and Wolff–Parkinson-White syndrome (Ho et al. 2007; Merrill et al. 1994; Sideris et al. 1996; Zehender 1996). It stabilizes the cardiac membranes and is considered as first-line in the treatment of Torsades de pointes. Intravenous magnesium regulates the cardiac electrophysiology via normalizing atrioventricular nodal conduction, by reducing automaticity, by prolonging sinus node refractory time, via preventing the antegrade and retrograde conduction over an accessory pathway and His ventricular conduction (Rasmussen and Thomsen 1989).
Preeclampsia
Preeclampsia is a condition associated with hypertension in pregnancy with proteinuria, contributing to an imbalance in angiogenic and anti-angiogenic growth factors (Li et al. 2017). Mg2+ is reported to have a beneficial effect in this situation by causing vasodilation mediated through NO production. In addition, Mg2+ offers beneficial effects and improve foetal outcome in preeclampsia; by down-regulating the expression of anti-angiogenic factors and by up-regulating the expression of angiogenic factors like vascular endothelial growth factor (VEGF), placental growth factor (PGF), etc. (Korish 2012; Al Alawi et al. 2018; Schwalfenberg and Genuis 2017). Mg2+ is also beneficial in eclampsia (seizure associated with preeclampsia) conditions by vascular and neurological mechanisms. That is, it acts as a vasodilator on peripheral and cerebral vasculature; can improve circulation and decrease peripheral vascular resistance. In addition, it protects the BBB, prevents edema formation, and has a central anti-convulsant activity (Esenet al. 2005; Euser et al. 2008; Kaya and Ahishali 2011; Hallak et al. 1992; Sibai, 2004). A coherent, systematic review suggested that Mg2+ reduces the risk of maternal mortality associated with eclampsia and documented the superior effect of Mg2+ over standard anticonvulsants. World health organization (WHO) advised to use Mg2+ as a standard treatment option for eclampsia and preeclampsia (Duley and Henderson-Smart 2003a,b; Fogleman 2011; Duley et al. 2006; Ayoubi 2011). Randomized, controlled trials in eclampsia patients disclosed that only 9.4% of Mg2+ treated women are prone to seizure when compared with 23.1% observed in the case of phenytoin treated patients (Lucas et al. 1995). Another randomized controlled trial in preeclampsia patients revealed that 2.8% of patients treated with anti-hypertensive drugs exhibit seizure episodes and in case of magnesium received patients it is only 0.9% (Witlin and Sibai 1998).
Hypertension
Hypertension is a major cause of morbidity and cardiovascular mortality (Kanthlal et al. 2020). Low intake of dietary magnesium and fewer amounts in the drinking water may cause Mg2+ deficiency, which is considered as a risk factor for developing CVD like hypertension, vasospasm, atherosclerosis, etc. Also, hypertension is frequently associated with a low serum level of Mg2+ (de Baaij et al. 2015; Gröber et al. 2015). Mg2+ deficiency results in an elevated level of vasopressin, aldosterone, and catecholamines, contributing to elevated BP (Jee et al. 2009). Besides this, hypomagnesemia results in the ineffective functioning of Mg2+-driven Na+/K+ATP ion pumps; causing dysregulation in sodium–potassium ratio, which is elevated in hypertensive conditions (Houston 2011; Touyz 2006). Apart from these, arterial plaque formation, inflammation, soft tissue calcification, and hardening of arteries also occurred in hypomagnesemia. The inflammation associated with Mg2+ deficiency triggers ROS-mediated hypertension (Long and Romani 2014). Both the extracellular and intracellular Mg2+ play a key role in maintaining BP via its vasodilatory property (Kolteet al. 2014; Dibaba et al.2017). Intracellular Mg2+ helps to reduce the level of vasoconstrictory calcium ions; extracellular Mg2+ acts by downregulating endothelin 1, which facilitates vasodilation through the activation of prostacyclin I2 (Kolte et al. 2014; Tangvoraphonkchai and Davenport 2018). The BP-lowering effect of magnesium is mainly suggested to be mediated via a decrease in peripheral vascular resistance associated with its vasodilatory effect (Touyz 2006). Magnesium supplementation is reported to effectively counteract the rise in BP associated with various conditions like pre-diabetics, insulin resistance, and CVD (Dibabaet al. 2017).
Heart failure
Mg2+ deficiency is commonly found in patients with congestive heart failure (CHF) (Gottlieb 1989). This may be due to several reasons like increased urinary excretion of Mg2+, increased extracellular volume, and due to the the effect of increased aldosterone(Dinicolantonio et al. 2018). Use of drugs like digoxin, ACE inhibitor, and diuretics also contributed to the deficiency of Mg2+ in congestive heart failure. In addition, in HF patients, it is essential to maintain the balanced level of Mg2+ as it palliates digitalis toxicity and other hemodynamic changes (Douban et al. 1996). The altered level of Mg2+ may prone to lethal arrhythmia followed by sudden death in CHF patients (Bashir et al. 1993). Oral supplementation of magnesium in HF patients reduces the inflammatory mediator C reactive protein, a marker for inflammatory reactions (Almoznino-Sarafian et al. 2007). Magnesium therapy is a promising approach to correct the pro-arrhythmic potential and to stabilize the cardiac repolarisation in heart failure patients (Ince et al. 2001). In line with this result, Stephen Gottlieb et al., 1993 reported that administration of intravenous magnesium sulphate reduces the frequency of occurrence of ventricular arrhythmia in CHF patients (Gottlieb et al. 1993). Magnesium orotate effectively improves the survival rate, clinical symptoms, and quality of life of patients with severe congestive heart failure (Stepura and Martynow 2009).
Vascular calcification
Vascular calcification is commonly observed in patients with chronic kidney diseases, which may also be associated with cardiovascular death (Zeper and De Baaij 2019). Vascular calcification is characterized by the up-regulation of genes like Runt-related transcription factor 2 (RUNX2), bone morphogenetic protein 2 (BMP2), and elevated levels of alkaline phosphatase (ALP) activity. Mg2+ primarily acts by inhibiting these genes, subsequently preventing the trans-differentiation and mineralization of vascular smooth muscle cells (Bressendorff et al. 2017). Patients with hypomagnesemia are more prone to vascular calcification; as Mg2+ is essential to prevent the formation and development of Ca/Pi (inorganic phosphate) and apatite crystals (Ter Braake et al. 2018,2017). In CALMAG study, it is reported that administration of MgCO3/Ca(OAc)2 and sevelamer-HCl are effective in reducing Inorganic phosphate (Pi) levels without elevating calcium levels (de Baaij et al. 2015).
Role of magnesium in lungs
Mg2+ and Ca2+ are two important cations involved in the regulation of normal bronchial functions with competing actions. Mg2+, the natural calcium antagonist, inhibits the entry of calcium in smooth muscle and is involved in releasing acetylcholine and histamine (Kercsmar 2006; Altinisik et al. 2016; Houston 2011). It also affects the bronchial vasomotor tone and lung structure (Landon and Young 1993; Mathew and Altura 1988). The therapeutic potential of Mg2+ in various lung disorders is mediated via reducing oxidative stress, impeding the release of substance P, inhibiting the voltage-gated calcium channel, and via its anti-inflammatory activity. Several study reports revealed that intravenous and dietary magnesium corrected the impaired pulmonary functions and improves the lung volume parameters such as vital capacity and forced expiratory volume (Britton et al. 1994). These factors help in contributing protection against various lung disorders like asthma and COPD (de Baaij et al. 2015).
Magnesium and respiratory disorders
Bronchial asthma
Asthma is a respiratory disease characterized by the narrowing of the airways with inflammatory reactions. Mg2+ deficiency is reported in serum and intracellular components of asthma patients (Kowal et al. 2007; Shaikh et al. 2016). Mg2+ reduces vasoconstriction and bronchoconstriction, so that its deficiency might result in the worsening of the asthmatic condition (Kelly 2003; Song and Chang 2012; Hill and Britton 1995). In 1936, magnesium is administrated for the first time for the treatment purpose in asthma patients by Victor Haury. Nebulized magnesium is also reported to improve respiratory function (Kowal et al. 2007; Song and Chang 2012; Mohammed and Goodacre 2007; Kokotajlo et al.2014). The anti-asthmatic effect of Mg2+ is mediated by various actions such as calcium antagonist property, by reducing the neutrophil respiratory burst and by altering the intracellular cyclic adenosine monophosphate (cAMP) level (Cairns and Kraft 1996; Das et al. 2010; Shivanthan and Rajapakse 2014). According to the magnesium trial, in children, administration of magnesium sulphate through inhalational route (MAGNETIC) provides an improvement in asthma score. Means the Yung Asthma Severity Score (ASS) showed a modest but statistically significant improvement after 60 min of use of nebulised MgSO4 and this effect is lasted for up to 240 min (Shan et al. 2013). Reports supported that magnesium sulphate, combined with standard treatment, improves breathlessness and reduces hospitalization with superior effect in acute asthma patients.(Schwalfenberg and Genuis 2017). According to the recent Cochrane review (2017), inhaled magnesium sulphate with β2 agonist improves the pulmonary functions in severe acute asthmatic patients (Knightly et al. 2017; Grober et al. 2015).
Cystic fibrosis
Cystic fibrosis is an autosomal recessive disorder due to mutation in the CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) gene, which is involved in the regulation of liquid volume in epithelial cells. In this disease, due to the defective CFTR gene, there is the formation of thick and sticky mucus which finally obstruct the respiratory pathways (Davies et al. 2007; Rafeeq and Murad 2017). Mg2+ deficiency is reported in patients with cystic fibrosis and is mainly due to four reasons; insufficient dietary intake, reduced intestinal absorption (due to pancreatic insufficiency associated with the disease), hyperglycemia associated with cystic fibrosis may trigger hypomagnesaemia and renal wasting associated with intake of drugs like β2 agonists, thiazides, loop diuretics, calcineurin inhibitor, amino-glycoside antibiotics etc. (Lee et al. 2015; Santi et al. 2016). Recombinant human DNase is used for treatment purposes, and magnesium is essential for its activation (Santi et al. 2016). Therefore the efficiency of the treatment is related to the Mg2+ status since Mg2+ can activate the endogenous Human DNase in sputum (Sanders et al. 2006). As per reports, oral magnesium can effectively treats cystic fibrosis in children via improving Shwachman-Kulczycki score and respiratory muscle strength. Furthermore, improvement of maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) is also reported in patients receiving magnesium (Gontijo-Amaral et al. 2012). Possible benefits of Mg2+ in cystic fibrosis treatments are improved respiratory muscle strength, pulmonary vasodilation in the case of pulmonary hypertension, and improved mucolytic activities of both endogenous and exogenous DNase (Santi et al. 2016).
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a persistent and progressive disorder resulting from chronic inflammation in the lungs and airways (Mathew et al., 2017). According to various observational studies, hypomagnesemia is proportionally linked with the severity of chronic lung diseases and the duration of hospital stay (Do Amaral et al. 2008). Mg2+ exhibits anticholinergic and antihistaminic action by inhibiting acetylcholine release from cholinergic neurons and histamine from mast cells. Mg2+ is also responsible for reducing neutrophilic bursting in inflammation and thereby provides anti-inflammatory action. Thus the anti-inflammatory, anti-cholinergic, and anti-histaminic actions of Mg2+ provide favorable effects in COPD conditions (Ni et al. 2020). In a randomized, double-blind trial, it is reported that infusion of magnesium could contribute in correction of altered parameters like functional respiratory capacity, inspiratory capacity, MIP and MEP in COPD patients (Skorodin et al. 1995). Do Amaral et al.(2012) reported that the use of magnesium diminishes the static lung hyperinflation and improves exercise performance in COPD patients (Do Amaral et al. 2012).
Role of magnesium in skeletal muscles
Mg2+ is a cofactor for number of bio-chemical reactions, such as oxygen uptake, energy production, and electrolyte balance, which have important roles in maintaining normal muscle functions (Nielsen and Lukaski 2006). Muscle contraction is highly a Ca2+-dependent process; Ca2+ released from the sarcoplasmic reticulum binds with troponin C and myosin, resulting in the conformation change in the protein that mediates the contraction process. The Ca2+ antagonist nature of Mg2+causes an overall relaxant effect on skeletal muscle (Jahnen-Dechent and Ketteler 2012; Schwalfenberg and Genuis 2017; Al Alawi et al. 2018; Gröber et al. 2015). Under normal conditions, the concentration of Mg2+ is 1000 times higher than the calcium concentration and binds with the Ca2+-binding sites. Mg2+ is displaced by Ca2+; when it is released from the sarcoplasmic reticulum. In case of Mg2+ deficiency, there are more free Ca2+-binding sites, and hence excess binding of calcium to these sites occurs, results in hyper-contractility (de Baaij et al. 2015). Furthermore, ATP, which requires magnesium as a cofactor, is necessary for the function of the ryanodine receptor and calcium-ATPase of the sarcoplasmic reticulum (SERCA). These two are involved in releasing and reuptake of Ca2+ in the contraction process (Neumann et al. 2011). Mg2+ is required at both the resting stage and at exercise conditions. Increased Mg2+ turnover during exercise creates a state of its insufficiency, which causes hypertension (Kass and Poeira 2015). Increased dietary intake of magnesium or magnesium supplements by individuals with Mg2+ deficiency; offers beneficial effects in their exercise performances (Nielsen and Lukaski 2006).
Muscle cramps
Muscle cramps are one of the prominent and recurrent features of severe or chronic hypomagnesemia. The neuronal excitation caused by Mg2+ deficiency may contribute to muscle cramps. The beneficial role of Mg2+ in muscle cramps is not clear; it is believed that the calcium antagonist property of Mg2+ may be responsible for its relieving effect in muscle cramps (Pham et al. 2014; Schwalfenberg and Genuis 2017). Clinical studies have documented the beneficial effect of magnesium citrate in patients with chronic persistent leg cramps (Geiger and Wanner 2012). The efficacy of magnesium in pregnancy-associated muscle cramps is also reported; i.e., a mixture of magnesium lactate and citrate at morning (5 mmol) and evening (10 mmol) is reported to have a beneficial effect (Garrison et al. 2012). However, a Coherent systematic review and meta-analysis reported that magnesium supplementation doesn’t provide any beneficial prophylactic effect in older individuals suffering from muscle cramps (Schwalfenberg and Genuis 2017).
Role of magnesium in bones
About 50–60% of Mg2+ is stored in bones, out of which about 30% is at the surface as hydroxylapatite crystals along with calcium and inorganic phosphate (Pi). Mg2+ present at the surface of the bones is only available for ionic exchange. The remaining amount becomes an integral part of the bone and is released during the bone resorption process (Al Alawi et al., 2018). Mg2+ is involved in regulating the solubility of minerals, thereby maintaining the size of the crystals. Apart from this, Mg2+ also participates in osteoblast proliferation. Magnesium-deficient rats are reported to have declined bone mass and decreased osteoblast number. Mg2+ deficiency is associated with reduced vascular supply to the bones that promotes the release of tumor necrosis factor (TNFα), substance P, and interleukin 1β, which triggers osteoclastic bone resorption. The reduced level of parathyroid hormone and 1,25-dihydroxy vitamin D3 (1,25 (OH)2-D3) occurred in hypomagnesemia, which also worsens the bone resorption process (Castiglioni et al. 2013; Welch et al. 2017). Osteoporosis is reported to be often associated with hypomagnesemia. Osteoporosis is a multi-factorial disease that occurs due to the imbalance between the bone deposition and resorption mechanisms, associated with declined bone mass and increased fracture risks (Castiglioni et al. 2013). Immuno-histological results revealed the loss of osteoblast, diminished bone growth, augmented osteoclastic resorption, along with trabecular bone loss in magnesium-deficient rats model of osteoporosis. Since Mg2+ is a mitogenic agent for bone growth, its deficiency affects the growth and formation of bone cells and bone strength (Rude et al. 2009). Decreasing Osteocalcin, a protein essential for bone formation and high parathyroid hormone and deoxypyridinoline levels, is reported in the Mg2+ deficient animal models. Thus these altered variables affect bone mass and strength (Weng and Webster 2013). Also, increased interleukin1 (140%), TNFα (120%), and megakaryocytes (500%) count is reported in Mg2+ deficient animals, which indicates the increased activity of cytokines in the bone. The study indicates that Mg2+ has an important role in the prevention of osteoporosis (Rude et al. 2003; 1998). According to the Women’s Health Initiative Study, wrist fractures are common in those females with a low magnesium level. Another study reported that magnesium, when administered at a 600 mg dose for 12 months, resulted in an 11% increase in Bone mineral density (BMD) in osteoporosis patients (Orchard et al. 2014). But the factor that limits the use of magnesium in the treatment of osteoporosis in the general population is its detrimental effect on bone (Castiglioni et al. 2013). As per study reports, it is documented that a higher intake of magnesium increases BMD, with fewer fracture risks, meanwhile reduces bone turnover in postmenopausal women and adults. Thus an increase in magnesium level beyond an optimum value is harmful to bone health. Magnesium may adversely affect the osseous metabolism and parathyroid gland functioning, leading to defects in bone mineralization. High bone Mg2+ inhibits the development of hydroxyapatite crystals by competing with calcium and binding to insoluble salt-forming pyrophosphate, which is not degraded by enzymes. This condition leads to osteomalacic renal osteodystrophy (Castiglioni et al. 2013).
Role of magnesium in liver
Mg2+ is important to carry out the normal enzymatic reactions in the liver, including fat metabolism (Liu et al. 2019). Hypomagnesemia is reported to be associated with liver diseases. There are reports demonstrated that administration of magnesium to obese magnesium deficient woman leads to a reduction in aminotransferase (ALT) and systemic high-sensitivity C-reactive protein (hs-CRP) mediated inflammation; which is not observed in individuals with normal serum Mg2+ level (Rodriguez-Hernandez et al. 2010).
Magnesium and liver diseases
Liver cirrhosis
Liver cirrhosis is characterized by damage in liver structure, fibrosis with regenerative nodules and may occur as the end stage of various liver diseases (Vijayan 2014). Patients with liver cirrhosis have a lower level of intracellular and serum Mg2+ concentration (Liu et al. 2019). Various factors like the use of hepatotoxic drugs, exposure to toxic substances, type two diabetes, and obesity are the main reasons for non-alcoholic fatty liver diseases. At the same time, alcohol is the main factor responsible for the development of alcoholic fatty liver diseases. Mg2+ deficiency is associated with alcoholic and non-alcoholic fatty liver diseases (Li et al. 2018a, b). Consumption of alcohol resulted in Mg2+deficiency by two mechanisms; by increasing the excretion of magnesium through lactate production and organic acid accumulation and by affecting the normal functioning of Mg2+ transporter in the kidney. The release of endotoxins in alcoholic fatty liver conditions activates the kupffer cell via toll-like receptor type-2 (TLRT-2). This may promote the release of pro-inflammatory cytokines and chemokines, resulting in cirrhosis (Liu et al. 2019). Alcohol-induced liver cirrhosis also contribute to the altered fatty acid and carbohydrate metabolism (Cederbaum 2012). Mg2+ is important for maintenance of normal mitochondrial function as its deficiency is associated with the altered fatty acid metabolism in mitochondria (Altura et al. 1996). Apart from the above, Mg2+ deficiency detrimentally affects the citric acid cycle pathway and fatty acid metabolism by affecting the NADH/NAD + redox potential with ROS release (Liu et al. 2019).
Albumin synthesized by the liver plays a major role in the transport of Mg2+ through the circulatory system. Serum albumin level is low in cirrhotic patients, so the transport of Mg2+ becomes limited (Liu et al. 2019). Furthermore, elevated levels of various hormones like glucagon, growth hormone, and aldosterone also favor the excretion of Mg2+ (Burra 2013; Ferment and Touitou 1985). Hepatic Mg2+ deficiency is associated with increased collagen deposition (Liu et al. 2019). PKCε is the group of protein kinase enzymes that regulates the function of various cellular proteins. Low Mg2+ resulted in the defective cell membrane translocation of PKCε, which further limits the accumulation of Mg2+ in hepatocytes with increased deposition of collagen and fibrinogen, which aggravates cirrhosis (Liu et al. 2019). Mg2+ deficiency triggers the inflammatory processes by various mechanisms such as through the release of neuro-mediators like substance P, by up-regulating the transcription of NF-κβ activity and by increasing the calcium content within the cells (Nielsen 2018). Thus to counteract the inflammatory processes, the liver activates various protective mechanisms which contribute to fibrosis, followed by cirrhosis (Martínez-Esparza et al. 2015).
Use of alcohol, Hepatitis B viral infection, or chronic cholestasis initiates the generation of ROS (Kundu et al. 2012). ROS are directly involved in fibrogenesis through the proliferation of Hepatic stellate cells (HSCs) (Richter and Kietzmann 2016). Consequently, various signaling pathways also get activated, including mitogen-activated protein kinase (MAPK), NF-Κβ and C- myb. The expression of α-smooth muscle actin (α-SMA), pro-fibrotic cytokines, transforming growth factor –β1 and type I collagen are higher in activated HSCs (Zhang et al. 2016; Puche et al. 2013).
The beneficial effects of Mg2+ in the treatment of liver cirrhosis are evident from the use of magnesium as lithospermate B and acetylcysteine complex, which reduces the levels of TGF-β1, nitric oxide, infiltration of hepatic lymphocytes, and pseudo-lobule formation. Apart from this, magnesium lithospermate B alleviated the aspartate aminotransferase (AST) and alanine aminotransferase in serum. Further, Mg2+ effectively reduces H2O2 induced ROS production and reduces the transcriptional activation and expression of αSMA, TGFβ, type I collagen, etc. Normalizing these parameters may be responsible for its effectiveness in cirrhosis treatment (Tee et al. 2018). The third national health and nutrition examination study (NHANES III) with 13,504 patients reported that magnesium intake is beneficial in reducing mortality rate in 49% of patients with liver diseases at a border level of significance (Wu et al. 2017).
Nonalcoholic, alcoholic fatty liver and hepatic cancer
Non-alcoholic fatty liver diseases start as simple hepatic stenosis with non-alcoholic steatohepatitis, which then progresses to liver cirrhosis and finally results in hepatic cellular carcinomas (Eshraghian et al. 2018). One of the important mechanisms contributing to non-alcoholic fatty liver diseases (NAFLD) is insulin resistance (Park 2006). Mg2+ is involved in regulating the proper functioning of insulin by decreasing the tyrosine kinase activity, and its deficiency may cause insulin resistance. Mg2+ level is also altered in non-diabetic patients and in hepatic steatosis (Eshraghian et al. 2018).
Mg2+ plays an important role in enzyme reaction by mediating the stability of the genome, which is important in regulating cell proliferation, differentiation, and apoptosis (Jahnen-Dechent and Ketteler 2012). Thus Mg2+ deficiency may impair this mechanism, causes DNA mutation or initiation of the cancer process (Blaszczyk and Duda-Chodak 2013). Liver cancer is reported to be associated with Mg2+ deficiency, and magnesium supplementation through drinking water is reported to have a beneficial effect in it (Wu et al. 2017). Hepatitis B virus infection (HBV) is one of the reasons for hepatocellular carcinoma. During HBV infection, the regulatory protein in Hepatitis B virus X (HBx) intensifies the Tumor growth factor β (TGF-β) activity. TGF-β can acts as a tumour promoter to induce epithelial-mesenchymal transition (EMT), which is responsible for invasiveness and metastasis associated with hepatocellular carcinoma. Magnesium provides beneficial effects by pleiotropic mechanisms like up-regulating the activity of protein phosphatase magnesium-dependent 1a (PPM1a), by blocking TGF-β activity, and by inhibiting the transcription of tumour promoting genes (Liu et al. 2019).
Role of magnesium in the pancreas
Mg2+ participates in the endocrine and exocrine functions of the pancreas. The ex vivo model using rabbit pancreas revealed that Mg2+ regulates insulin secretion. The studies using rat pancreas and insulinoma cells also supported these reports. Furthermore, clinical reports indicated increased insulin resistance in magnesium-deficient patients (de Baaij et al. 2015). Mg2+ acts as a cofactor for the enzymes involved in carbohydrate metabolism. In magnesium-deficient animals, insulin receptor phosphorylation and glucose accumulations are found to be impaired (Al Alawi et al. 2018). Mg2+ level is inversely related with the homeostatic model assessment insulin resistance (HOMA-IR) test for β-cell function and insulin resistance, hemoglobin alpha 1 (HbA1), and plasma glucose levels (Long and Romani 2014). Low serum level of Mg2+ is reported in type 2 diabetes mellitus patients which is responsible for the decreased treatment outcome and increased mortality associated with the disease (Kostov 2019). Diabetic retinopathy, a chronic complication of diabetes, is also triggered by the inflammatory condition associated with hypomagnesemia (Kumar et al. 2019). Mg2+ is required to activate insulin receptors, which belong to the tyrosine class, and mediate the intracellular signaling process. Mg2+ deficiency disrupts the signaling process and results in insulin resistance (Barbagallo et al. 2003; Morakinyo et al. 2018).
Furthermore, hypomagnesemia facilitates the Ca2+ entry to adipocytes, causes oxidative stress and inflammation, which further contributes to insulin resistance (Zheltova et al. 2016). Insulin causes the Mg2+ to move from the extracellular to the intracellular compartment and decreases the renal tubular re-absorption process of Mg2+, resulting in hypomagnesemia (Al Alawi et al. 2018). Magnesium supplementation provides beneficial effects in type 1 patients by normalizing lipid profile, HbA1c, and by reducing neuropathic incidences associated with diabetes (Shahbah et al. 2017). Clinical trials proved that magnesium is effective in gestational diabetes mellitus by reducing plasma glucose levels and by maintaining a proper lipid profile (Maktabi et al. 2018). Various mechanisms suggested to be included under these beneficial effects are by down regulating the oxidized low-density lipoprotein receptor (LDLR) and by up regulating the peroxisome proliferator-activated receptor-gamma (PPAR-γ) and glucose transporter 1 (GLUT-1) (Jamilian et al. 2017) expressions. However, to establish the actual efficiency of magnesium in diabetic conditions, there is a need to conduct large sample-sized clinical trials.
Role of magnesium in skin
Atopic dermatitis patients are presented with declined levels of erythrocyte zinc and serum magnesium levels (Makiura et al. 2004). Magnesium supplements are effective by reducing inflammation, enhancing the proliferation and differentiation of epidermal cells, by enhancing skin hydration and dermal permeability (Proksch et al. 2005). Magnesium with ceramides has been beneficial in treating mild to moderate atopic dermatitis (Schwalfenberg and Genuis 2017). Also, magnesium can be administered through the transdermal route which can bypass the gastrointestinal tract and thereby helps to correct the serum Mg2+ level (Gröber et al. 2017). Magnesium is also reported to be beneficial in psoriasis therapy. Psoriasis is immune-related disease characterised by hyperproliferation with incomplete differentiation of keratinocytes (Rajitha et al. 2019). Mg2+ deficiency is reported in psoriatic patients, and topical magnesium therapy is one of the oldest treatment options for the disease (Shahidi-Dadras et al.2012; Chandrasekaran et al. 2014). Topically applied Mg2+ can cross the stratum corneum barrier depending upon the time and concentration of exposure. Hair follicle also contributes a significant role in this permeation (Chandrasekaran et al. 2016). The advantage of this delivery mechanism is the avoidance of diarrhoea, the most common problem associated with the oral use of magnesium (Razzaque 2018). Clinical observation revealed the beneficial effect of magnesium in patients with skin allergy (Błach et al. 2007). Oral magnesium chloride effectively treats familial benign chronic pemphigus or Hailey–Hailey disease, a rare skin disease (Barde et al. 2017). Besides, magnesium supplementation is reported to be effective in the pseudoxanthoma elasticum, a genetic disorder affecting skin, eye and blood vessels (Rose et al. 2019).
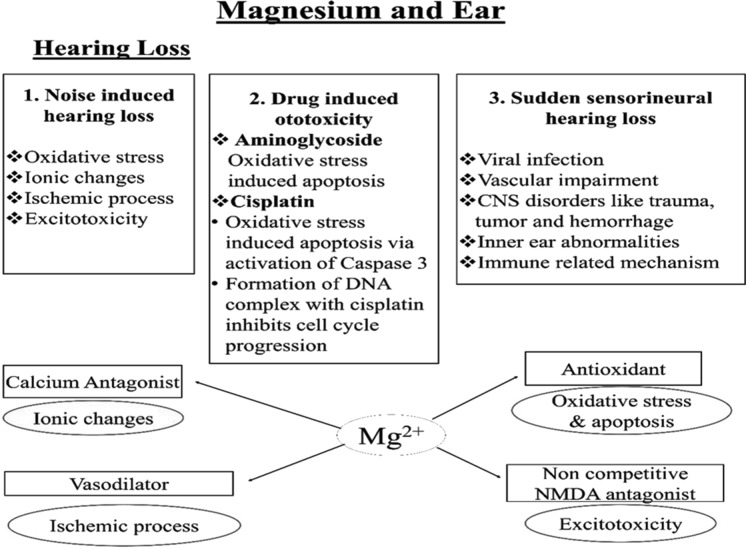
Role of magnesium in ear
Hearing loss may be associated with multiple etiological factors like noise or drug-induced hearing loss or sudden sensory neural hearing loss. The underlying cause of hearing loss is the imbalances in various metabolic processes like ischemic, ionic, excitotoxicity, and ROS. Mg2+ has therapeutic potential in hearing loss because of its vasodilatory, calcium, and NMDA antagonist actions and due to its antioxidant potential (Fig. 6). The neuroprotective effect of Mg2+ provides additional beneficial effects in the cellular death associated with hearing loss. Moreover, it can easily cross the perilymph blood barrier and reaches the organ of Corti than any other currently existing drugs (corticosteroids) (Sendowski et al. 2011). A study conducted on the US population revealed a correlation between magnesium intake and a lower risk of hearing loss (Choi et al. 2014). Another study conducted in 1994 reported that magnesium administration reduces noise-associated hearing damage (Attias et al. 1994). Mg2+, which easily crosses the hemato-cochlear barrier, has neuroprotective and vasodilatory effects and can minimise cochlear damage (Sendowski 2006). The magnesium-treated groups have a better tolerance to all sound frequencies tested (> 10 dB hearing level) (Nageris et al. 2004).
Fig. 6.
Showing factors leading to hearing loss and beneficial role of magnesium in it: hearing loss is mainly due to three main reasons; noise induced, drug induced and sudden sensioneural hearing loss. The ionic change associated with hearing loss is corrected by magnesium due to its calcium antagonist action and ischemic related problem are corrected by its vasodilatory property. Excitotoxicity in association with hearing loss is corrected by its non-competitive NMDA antagonist action. Additionally antioxidant action of magnesium is beneficial in oxidative stress and related apoptosis
Role of magnesium in eye
Mg2+ offers neurovascular protection in ocular diseases due to its vasodilatory effect achieved by reducing endothelin 1 production and by enhancing endothelial nitric oxide synthase activity (Ajith 2020). Furthermore, magnesium plays a vital role in maintaining lens homeostasis (Agarwal et al. 2013). Additionally, regulation of lens sodium pump activity, glutamate and calcium antagonist property, and the inhibitory effect on apoptosis of retinal ganglion cells; contribute to the efficacy of magnesium in ocular disease (Ajith 2020). Cataract is associated with magnesium deficiency which can be prevented and treated with magnesium supplementation (Agarwal et al. 2013; Nagai et al. 2006; 2007). Nagai et al., (2007) evaluated the effect of magnesium in cataract using the Shumiya cataract rat (SCR) model. The results showed that increased calcium content in the lens is responsible for the opacity associated with cataract, and administration of magnesium supplement is beneficial in ameliorating this effect due to its calcium antagonist property (Ekici et al. 2014). Furthermore, Mg2+ plays a vital role in maintaining lens homeostasis (Agarwal et al. 2013).
Glaucoma is the condition of chronic optic neuropathy that may often result in loss of vision. The rise in intraocular pressure with optic nerve damage is the main reason for glaucoma. Mg2+ regulates the ocular blood supply by its effect on endothelin-1 and endothelial nitric oxide expression. Additional neuro-protection is offered by its NMDA antagonistic effect (Ekici et al. 2014). The effectiveness of magnesium in correcting the blood flow and ganglion cell loss provides beneficial effects in glaucoma conditions (Iezhitsa and Agarwal 2018; Li et al. 2018a, b). Bioabsorbable coated magnesium alloy is a promising approach to develop a surgical assistive device for glaucoma (Li et al. 2018a, b). In glaucoma patients with vasospasm, magnesium improves peripheral circulation that is beneficial in the visual field (Zulema Gaspar et al. 1995).
Role of magnesium in immunity
Mg2+ is important in acquired immunity via regulating lymphocyte growth (Tam et al. 2003). An in vitro study carried out in chicken B cell line DT40 revealed that the removal of magnesium channel, TRPM7, results in cell death and can be partially corrected by magnesium supplementation (Schlingmann et al. 2007). Mutation in MagT1, a magnesium transporter, is reported in patients with X-linked immunodeficiency diseases, Epstein–Barr virus infection, and neoplasia (XMEN) (Ravell et al. 2014). Low CD4+ T cells and defective activation of T-lymphocytes are due to the decreased magnesium influx, which fails to activate PLCγ1 (Li et al. 2011a, b; Li et al. 2012). The importance of magnesium for CD4+ activation is also evident from reported studies conducted in asthma patients (Liang et al. 2012). However, further studies are essential to conclude the effect of Mg2+on T cell signaling. Mg2+ has an important role in synthesizing and releasing immune cells and other associated processes like cell adhesion and phagocytosis (Kubena 1994). Besides, it acts as a cofactor for the synthesis of immunoglobulin, CI 3 convertase, antibody-dependent cytolysis, macrophage responses to lymphocyte, IgM lymphocyte binding, T helper B cell adherence, substance P binding with lymphoblast, and binding of antigen to macrophage (Galland 1988; Laires and Monteiro 2008). Indeed, the deficiency affects various immune functions like the decline in NK cell level, monocytes and T cell ratio, increased oxidative stress after strenuous exercise, and elevated cytokine IL-6 level and inflammatory events. Deficiency of Mg2+ may be prone to recurrent bacterial and fungal infection (Nielsen 2018). Mg2+ deficient animal model exhibits inflammation as the first noticeable change with elevated levels of pro-inflammatory mediators like TNFα with declined anti-inflammatory cytokine levels (Galland 1988; Schmitz and Perraud 2017). The activation of immune cells like monocyte, macrophages, and polymorphonuclear cells are involved in the release of inflammatory mediators like cytokine, free radical and eicosanoids (Galland 1988). Administration of magnesium reduces leukocyte activation and oxidative damage to peripheral blood lymphocyte DNA in athletes and sedentary young men (Petrović et al. 2016). Thus, Mg2+ is an important factor for optimum immune cell functioning by regulating the proliferation and function of lymphocytes (Kubena 1994). In vitro studies also prove the role of magnesium in reducing leukocyte activation through its calcium antagonistic action (Laires and Monteiro 2008). Magnesium deficiency results in the stress condition that activate the sympathetic system and hypothalamic-pituitary axis causes fat accumulation and release of neuropeptides; results in the immune response followed by inflammatory cascades (Rayssiguier et al. 2010).
COVID 19 and magnesium
Mg2+ and other elements such as zinc, selenium, and iron play an important role in the immune system. Lack of consumption of these elements may reduce the tolerance to infections and increases the disease burdens (Calder et al. 2020). Mg2+ can inhibit cytokine storm and hyper oxidative stress in COVID 19 patients through various mechanisms such as its antioxidant, immune-modulatory, and anti-inflammatory activities (Moh’d Nour et al. 2020). Based on the basic and clinical research study, it is evident that Mg2+ effectively treats respiratory diseases like asthma and pneumonia because of its anti-inflammatory, antioxidant, and smooth muscle relaxant properties (Tang et al. 2020). A substantial decrease in the need for oxygen or intensive treatment assistance is reported in elderly COVID 19 patients upon the intake of vitamin D, magnesium, and vitamin B12 (DMB) in combination (Tan et al. 2020). Iran’s clinical trial registry (IRCT) confirmed that magnesium sulphate inhalation is effective in improving respiratory symptoms such as shortness of breath, cough and oxygen saturation in COVID 19 patients (Pourdowlat et al., 2021).
Newer formulation strategies for magnesium
Mg2+ deficiency is reported in number of neurological diseases and administration of intravenous magnesium sulphate is one of the treatment strategy for these conditions. But the CNS permeability of clinically using magnesium salts are reported to be less. To improve the CNS penetrability of Mg2+ few attempts are done and considered in this section. Magnesium threonate, newer organic salt of magnesium, is claimed to have greater BBB permeability than the inorganic salts. Shen et al. (2019) studied the effect of magnesium l threonate in 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine (MPTP) induced motor deficit and dopaminergic neuron loss in mouse (Shen et al. 2019). The efficacy of magnesium threonate is proven by its beneficial effect in memory deficit and neuropathic pain; which is mediated by reducing TNF-α production and by correcting the NMDA receptor dysfunction (Wang et al. 2013). Another study aims to improve the CNS availability of magnesium by combining it with PEG. This combination is found to be effective in treating unilateral cervical spinal cord injury and traumatic brain injury (Lee et al. 2010; Busingye et al. 2016). Magnesium oxide nanoparticle synthesised by the co-precipitation method exhibits good antibacterial activity against both gram-positive and negative bacteria (Imani and Safaei 2019). Another study reported that magnesium oxide nanoparticle is more effective in reducing anxiety induced by exercise than conventional magnesium oxide (Kesmati et al. 2014). The anti-cataract effect of liposomal magnesium taurate is checked in galactose-induced cataract model in rats. The formulation effectively prevents cataract genesis, which is mediated by maintaining the lens mineral homeostasis and by preventing the oxidative stress (Iezhitsa et al. 2016). A newer magnesium chloride supplement ‘ChronoMag’ as a dietary supplement is introduced for providing low-dose continuous magnesium with improved absorption, bioavailability, and GI tolerance for use in health conditions associated with low magnesium levels(Dualé et al. 2018).
Conclusion
Nutrients play major roles in regulating various vital functions of the physiological system. Magnesium is an important nutrient that plays several roles, such as to acts as a cofactor for more than 300 enzymatic reactions, promote growth via synthesis of DNA, RNA, and proteins, involved in muscle contraction, maintain normal cardiac and neurological functions. Magnesium performs various tasks as a drug through functions such as calcium antagonism, NMDA blocking, and vasodilatory action. The antioxidant and anti-inflammatory activities of magnesium provide additional protection in various disease conditions; as many diseases have oxidative stress or inflammatory reactions as background. Due to its versatility and universality in its functions, it can be considered a “master cation”. Even though it has a wide range of therapeutic activities, its functionality is not given the attention it deserves. Apart from the treatment beneficial, it also has lesser toxicity because of the body’s regulatory mechanism. The body maintains the normal level of magnesium via its absorption, storage, and excretion process. Hypomagnesemia is reported in various diseases like asthma, neurological diseases, preeclampsia, and CVD. Magnesium is obtained from various food materials and water under physiological conditions, but these sources are not satisfactory in a diseased state. There is a need for large sample size clinical trials to upgrade the use of magnesium as a standard drug. The future perspectives based on magnesium therapy strategies should include the development of the targeted delivery system to make the therapy more effective without deleteriously affecting other organ’s functions.
Acknowledgements
The authors gratefully acknowledge ‘Amrita School of Pharmacy, Kochi Kerala’ for providing support and facilities for this review.
Abbreviations
- ACE
Angiotensin converting enzyme
- AD
Alzheimer’s disease (AD)
- ALP
Alkaline phosphatase
- ALT
Aminotransferase
- AMPA
α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid
- APP
Amyloid precursor protein
- AST
Aspartate aminotransferase
- ATP
Adenosine triphosphate
- BBB
Blood brain barrier
- BMD
Bone mineral density
- BMP2
Bone morphogenetic protein 2
- BP
Blood pressure
- cAMP
Cyclic Adenosine mono phosphate
- CAD
Coronary arytery diseases
- CFTR
Cystic fibrosis transmembrane conductance regulator
- CGRP
Calcitonin gene related peptide
- CHF
Congestive heart Failure
- Claudin
CLDN
- CNS
Central nervous system
- CSD
Cortical spreading depression
- CSF
Cerebrospinal fluid
- CTF β
C terminal fragment β
- CVD
Cardiovascular diseases
- DRE
Drug resistant epilepsy
- ECF
Extracellular fluid
- ECG
Electrocardiogram
- EGF
Epidermal growth factor
- EMT
Epithelial-mesenchymal transition
- GABA
Gamma amino butyric acid
- GABAA
Gamma amino butyric acid receptor A
- GLUT-1
Glucose transporter 1
- GSK-3β
Glycogen synthase kinase-3 β
- HbA1
Haemoglobin, alpha 1
- HBV
Hepatitis B virus infection
- HCC
Hepatic cellular carcinoma
- HSC
Hepatic stellate cells
- IL 1
Interleukin 1
- IMT
Carotid Intima-Media Thickness
- LDLR
Low-density lipoprotein receptor LDLR
- MagT1
Magnesium transporter 1
- MAPK
Mitogen-activated protein kinase
- MEP
Maximal expiratory pressure
- Mg2+
Magnesium
- MI
Myocardial infarction
- MIP
Maximal Inspiratory Pressure
- Mrs2
Mitochondrial RNA splicing 2
- Mtor
Mammalian target of rapamycin
- Na+
Sodium
- NAFLD
Non-alcoholic fatty liver diseases
- NF-κB
Nuclear factor kappa light chain enhancer of activated B cells
- NMDA-N
Methyl D aspartate
- NO
Nitric oxide
- PEG
Polyethylene glycol
- PGF
Placental growth factor
- Pi
Inorganic phosphate
- PKCε
Protein kinase C epsilon type
- PLCγ1
Phosphoinositide phospholipase C
- PPAR-γ
Peroxisome proliferator- activated receptor gamma
- PUFA
Polyunsaturated Fatty Acids
- PD
Parkinson’s disease
- RBC
Red blood cells
- DCT
Distal convoluted tubule
- RDA
Recommended daily allowance dose
- TRPM
Transient receptor potential channel for melastatin
- RNA
Ribonucleic acid
- ROS
Reactive oxygen species
- RUNX2
Runt-related transcription factor 2
- SLC41
Solute Carrier Family transporter
- SOD
Superoxide dismutase
- TAL
Thick ascending limb of the Loop of Henle
- TGF-β
Transforming Growth Factor-β
- TLRT-2
Toll-like receptor type-2().
- TNFα
Tumor necrosis factor alpha
- VEGF
Vascular endothelial growth factor
- WHO
World Health Organisation
- XMEN-Epstein
Barr virus infection and neoplasia (XMEN)
- α-SMA
α-Smooth muscle actin
Declarations
Conflict of interest
There is no conflict of interest in this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abdullahi I, Watila MM, Shahi N, Nyandaiti Y, Bwala S. Serum magnesium in adult patients with idiopathic and symptomatic epilepsy in Maiduguri, Northeast Nigeria. Niger J Clin Pract. 2019;22(2):186–193. doi: 10.4103/njcp.njcp_252_18. [DOI] [PubMed] [Google Scholar]
- Agarwal R, Iezhitsa IN, Agarwal P, Spasov AA. Mechanisms of cataractogenesis in the presence of magnesium deficiency. Magnes Res. 2013;26:2–8. doi: 10.1684/mrh.2013.0336. [DOI] [PubMed] [Google Scholar]
- Ahmed F, Mohammed A. Magnesium: the forgotten electrolyte—a review on hypomagnesemia. Med Sci. 2019;7:56. doi: 10.3390/medsci7040056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajith TA. Possible therapeutic effect of magnesium in ocular diseases. JBCPP. 2020 doi: 10.1515/jbcpp-2019-0107. [DOI] [PubMed] [Google Scholar]
- Al Alawi AM, Majoni SW, Falhammar H. Magnesium and human health: perspectives and research directions. Int J Endocrinol. 2018 doi: 10.1155/2018/9041694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander RT, Hoenderop JG, Bindels RJ. Molecular determinants of magnesium homeostasis: insights from human disease. J Am Soc Nephrol. 2008;19:1451–1458. doi: 10.1681/ASN.2008010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alghamdi AA, Al-Radi OO, Latter DA. Intravenous magnesium for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and meta-analysis. J Card Surg. 2005;20:293–299. doi: 10.1111/j.1540-8191.2005.200447.x. [DOI] [PubMed] [Google Scholar]
- Almoznino-Sarafian D, Berman S, Mor A, Shteinshnaider M, Gorelik O, Tzur I, Alon I, Modai D, Cohen N. Magnesium and C-reactive protein in heart failure: an anti-inflammatory effect of magnesium administration? Eur J Nutr. 2007;46(4):230–237. doi: 10.1007/s00394-007-0655-x. [DOI] [PubMed] [Google Scholar]
- Altinisik HB, Kirdemir P, Altinisik U, Gokalp O. Effects of magnesium sulfate on airway smooth muscle contraction in rats. Med Glas. 2016;13(2):68–74. doi: 10.17392/862-16. [DOI] [PubMed] [Google Scholar]
- Altura BM, Gebrewold A, Altura BT, Brautbar N. Magnesium depletion impairs myocardial carbohydrate and lipid metabolism and cardiac bioenergetics and raises myocardial calcium content in-vivo: relationship to etiology of cardiac diseases. Biochem Mol Biol Int. 1996;40:1183–1190. doi: 10.1080/15216549600201823. [DOI] [PubMed] [Google Scholar]
- Amaral AF, Gallo L, Jr, Vannucchi H, Crescencio JC, Vianna EO, Martinez JA. The effect of acute magnesium loading on the maximal exercise performance of stable chronic obstructive pulmonary disease patients. Clinics. 2012;67:615. doi: 10.6061/clinics/2012(06)12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antman EM. Magnesium in acute myocardial infarction: overview of available evidence. Am Heart J. 1996;132:487–495. doi: 10.1016/S0002-8703(96)90341-5. [DOI] [PubMed] [Google Scholar]
- Antzelevitch C, Burashnikov A. Overview of Basic Mechanisms of Cardiac Arrhythmia. Card Electrophysiol Clin. 2011 doi: 10.1016/j.ccep.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attias J, Weisz G, Almog S, Shahar A, Wiener M, Joachims Z, Netzer A, Ising H, Rebentisch E, Guenther T. Oral magnesium intake reduces permanent hearing loss induced by noise exposure. Am J Otolaryngol Head Neck Med Surg. 1994;15(1):26–32. doi: 10.1016/0196-0709(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Ayoubi Pre-eclampsia: pathophysiology, diagnosis, and management. Vasc Health Risk Manag. 2011;7:467. doi: 10.2147/vhrm.s20181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandyopadhyay D, Chattopadhyay A, Ghosh G, Datta A. Oxidative stress-induced ischemic heart disease: protection by antioxidants. Curr Med. 2005;11(3):369–387. doi: 10.2174/0929867043456016. [DOI] [PubMed] [Google Scholar]
- Barbagallo M, Dominguez LJ, Galioto A, Ferlisi A, Cani C, Malfa L, Pineo A, Busardo’ A, Paolisso G. Role of magnesium in insulin action, diabetes and cardio-metabolic syndrome X. Mol Aspects Med. 2003;24:39–52. doi: 10.1016/S0098-2997(02)00090-0. [DOI] [PubMed] [Google Scholar]
- Barde NitinG, Mishra DharmendraB, Ingole ShraddhaO. Oral magnesium chloride: a novel approach in the management of Hailey-Hailey disease. Indian J Dermatol Venereol Leprol. 2017;83(2):259. doi: 10.4103/0378-6323.198459. [DOI] [PubMed] [Google Scholar]
- Bashir Y, Sneddon JF, Anne Staunton H, Haywood GA, Simpson IA, McKenna WJ, John Camm A. Effects of long-term oral magnesium chloride replacement in congestive heart failure secondary to coronary artery disease. Am J Cardiol. 1993;72(15):1156–1162. doi: 10.1016/0002-9149(93)90986-M. [DOI] [PubMed] [Google Scholar]
- Bharadwaj J, Darbari A, Naithani M. Magnesium: the fifth electrolyte. J Med Nutr Nutraceuticals. 2014;3:186. doi: 10.4103/2278-019x.131955. [DOI] [Google Scholar]
- Błach J, Nowacki W, Mazur A. Magnesium in skin allergy. Postpy Higieny i Medycyny Doświadczalnej (online) 2007;61:548. [PubMed] [Google Scholar]
- Blanke M, VanDongen A. Activation mechanisms of the NMDA receptor. In: VanDongen A, editor. Biology of the NMDA Receptor. Florida: CRC Press; 2008. pp. 283–312. [Google Scholar]
- Blaszczyk U, Duda-Chodak A. Magnesium: its role in nutrition and carcinogenesis. Rocz Państwowego ZakładuHig. 2013;64:165–171. [PubMed] [Google Scholar]
- Bressendorff I, Hansen D, Schou M, Kragelund C, Brandi L. The effect of magnesium supplementation on vascular calcification in chronic kidney disease—a randomised clinical trial (MAGiCAL-CKD): essential study design and rationale. BMJ Open. 2017 doi: 10.1136/bmjopen-2017-016795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton J, Pavord I, Richards K, Wisniewski Knox A, Lewis S, Tattersfield A, Weiss S. Dietary magnesium, lung function, wheezing, and airway hyper-reactivity in a random adult population sample. Lancet. 1994;344:357–362. doi: 10.1016/S0140-6736(94)91399-4. [DOI] [PubMed] [Google Scholar]
- Burra P. Liver abnormalities and endocrine diseases. Best Pract Res Clin Gastroenterol. 2013;27:553–563. doi: 10.1016/j.bpg.2013.06.014. [DOI] [PubMed] [Google Scholar]
- Busingye DS, Turner RJ, Vink R. Combined magnesium/polyethylene glycol facilitates the neuroprotective effects of magnesium in traumatic brain injury at a reduced magnesium dose. CNS Neurosci Ther. 2016;22:854–859. doi: 10.1111/cns.12591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairns CB, Kraft M. Magnesium attenuates the neutrophil respiratory burst in adult asthmatic patients. Acad Emerg Med. 1996;3:1093–1097. doi: 10.1111/j.1553-2712.1996.tb03366.x. [DOI] [PubMed] [Google Scholar]
- Calder PC, Carr AC, Gombart AF, Eggersdorfer M. Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections. Nutrients. 2020;12(4):1181. doi: 10.3390/nu12041181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castiglioni S, Cazzaniga A, Albisetti W, Maier JAM. Magnesium and osteoporosis: current state of knowledge and future research directions. Nutrients. 2013;5:3022–3033. doi: 10.3390/nu5083022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cederbaum AI. Alcohol Metabolism. Clin Liver Dis. 2012;16:667–685. doi: 10.1016/j.cld.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborti S, Chakraborti T, Mandal M, Mandal A, Das S, Ghosh S. Protective role of magnesium in cardiovascular diseases: a review. Mol Cell Biochem. 2002;238:163–179. doi: 10.1023/a:1019998702946. [DOI] [PubMed] [Google Scholar]
- Chandrasekaran NC, Weir C, Alfraji S, Grice J, Roberts MS, Barnard RT. Effects of magnesium deficiency—more than skin deep. Exp Biol Med. 2014;239:1280–1291. doi: 10.1177/1535370214537745. [DOI] [PubMed] [Google Scholar]
- Chandrasekaran NC, Sanchez WY, Mohammed YH, Grice JE, Roberts MS, Barnard RT. Permeation of topically applied magnesium ions through human skin is facilitated by hair follicles. Magnes Res. 2016;29(2):35–42. doi: 10.1684/mrh.2016.0402. [DOI] [PubMed] [Google Scholar]
- Chen PY, Chiu HY, Yeh TH, Huang YC. Meta-analysis effects of intravenous and oral magnesium on reducing migraine: a meta-analysis of randomized controlled trials. Pain Physician. 2016;19:97–112. doi: 10.36076/ppj/2016.19.E97. [DOI] [PubMed] [Google Scholar]
- Chiu HY, Yeh TH, Huang YC, Chen PY (2016) Effects of intravenous and oral magnesium on reducing migraine: a meta-analysis of randomized controlled trials. Pain Physician 19(1):E97–112. 10.36076/ppj/2016.19.e97 [PubMed]
- Choi YH, Miller JM, Tucker KL, Howard Hu, Park SK. Antioxidant vitamins and magnesium and the risk of hearing loss in the US general population. AJCN. 2014;99(1):148–155. doi: 10.3945/ajcn.113.068437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronic R, Risk D, Isbn C. Diet and health: implications for reducing chronic disease risk. Choice Rev Online. 1990 doi: 10.5860/choice.27-3332. [DOI] [Google Scholar]
- Cook NL, Corrigan F, van den Heuvel C. The role of magnesium in traumatic CNS injury. In: Vink R, Nechifor M, editors. Magnesium in the central nervous system. South Australia: University of Adelaide Press; 2011. pp. 167–180. [PubMed] [Google Scholar]
- Das SK, Haldar AK, Ghosh I, Saha SK, Das A, Biswas S. Serum magnesium and stable asthma: is there a link. Lung India. 2010;27:205–208. doi: 10.4103/0970-2113.71944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies JC, Alton EWFW, Bush A. Cystic fibrosis. Br Med J. 2007;335:1255–1259. doi: 10.1136/bmj.39391.713229.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Baaij JHF, Hoenderop JGJ, Bindels RJM. Magnesium in man: implications for health and disease. Physiol Rev. 2015;95:1–46. doi: 10.1152/physrev.00012.2014. [DOI] [PubMed] [Google Scholar]
- de Oliveira LDB, de Oliveira RWD, de Azevedo Futuro Neto H, Nakamura-Palacios EM. The role of magnesium sulfate in prevention of seizures induced by pentylenetetrazole in rats. Arq Neuropsiquiatr. 2011;69(2B):349–355. doi: 10.1590/s0004-282x2011000300016. [DOI] [PubMed] [Google Scholar]
- Deepti R, Nalini G. Relationship between hypomagnesemia and dyslipidemia in type 2 diabetes mellitus. Asian J Pharm Res Health Care. 2014;6(3):32–36. [Google Scholar]
- Dibaba DT, Xun P, Song Y, Rosanoff A, Mr S, He K. The effect of magnesium supplementation on blood pressure in individuals with insulin resistance, prediabetes, or noncommunicable chronic diseases: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2017;106:921–929. doi: 10.3945/ajcn.117.155291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNicolantonio JJ, Liu J, O’Keefe JH. Magnesium for the prevention and treatment of cardiovascular disease. Open Heart. 2018 doi: 10.1136/openhrt-2018-000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNicolantonio JJ, O’Keefe JH, Wilson W. Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Hear. 2018 doi: 10.1136/openhrt-2017-000668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do Amaral AF, Rodrigues AL, Terra Filho J, Vannucchi H, Martinez JAB. Effects of acute magnesium loading on pulmonary function of stable COPD patients. Med Sci Monit. 2008;14:524. [PubMed] [Google Scholar]
- Dolati S, Rikhtegar R, Mehdizadeh A, Yousefi M. The role of magnesium in pathophysiology and migraine treatment. Biol Trace Elem Res. 2019 doi: 10.1007/s12011-019-01931-z. [DOI] [PubMed] [Google Scholar]
- Douban S, Brodsky MA, Whang DD, Whang R. Significance of magnesium in congestive heart failure. Am Heart J. 1996;132(3):664–671. doi: 10.1016/S0002-8703(96)90253-7. [DOI] [PubMed] [Google Scholar]
- Dualé C, Cardot JM, Joanny F, Trzeciakiewicz A, Martin E, Pickering G, Dubray C. An advanced formulation of a magnesium dietary supplement adapted for a long-term use supplementation improves magnesium bioavailability: in vitro and clinical comparative studies. Biol Trace Elem Res. 2018;186:1. doi: 10.1007/s12011-018-1277-2. [DOI] [PubMed] [Google Scholar]
- Du-guan F. Cardiac arrhythmias: diagnosis, symptoms, and treatments. Cell Biochem Biophys. 2015;73(2):291–296. doi: 10.1007/s12013-015-0626-4. [DOI] [PubMed] [Google Scholar]
- Duley L, Henderson-Smart DJ. Magnesium sulphate versus diazepam for eclampsia. Cochrane Database Syst Rev. 2003 doi: 10.1002/14651858.cd000127. [DOI] [PubMed] [Google Scholar]
- Duley L, Henderson-Smart DJ. Magnesium sulphate versus phenytoin for eclampsia. Cochrane Database Syst Rev. 2003 doi: 10.1002/14651858.cd000128. [DOI] [PubMed] [Google Scholar]
- Duley L, Meher S, Abalos E. Management of pre-eclampsia. Br Med J. 2006;332:463–468. doi: 10.1136/bmj.332.7539.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyckner T, Ola Wester P. Relation between potassium, magnesium and cardiac arrhythmias. Acta Med Scand. 1981;209(S647):163–169. doi: 10.1111/j.0954-6820.1981.tb02652.x. [DOI] [PubMed] [Google Scholar]
- Ekici F, Korkmaz S, Karaca EE, Sül S, Tufan HA, Aydın B, Dileköz E. The role of magnesium in the pathogenesis and treatment of glaucoma. Int Sch Res Not. 2014 doi: 10.1155/2014/745439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esen F, Erdem T, Aktan D, Orhan M, Kaya M, Eraksoy H, Cakar N, Telci L. Effect of magnesium sulfate administration on blood-brain barrier in a rat model of intraperitoneal sepsis: a randomized controlled experimental study. Crit Care. 2005;9:18–23. doi: 10.1186/cc3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eshraghian A, Nikeghbalian S, Geramizadeh B, Malek-Hosseini SA. Serum magnesium concentration is independently associated with non-alcoholic fatty liver and non-alcoholic steatohepatitis. United Eur Gastroenterol J. 2018;6:97–103. doi: 10.1177/2050640617707863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euser AG, Cipolla MJ. Magnesium sulfate for the treatment of eclampsia: a brief review. Stroke. 2009;40:1169–1175. doi: 10.1161/STROKEAHA.108.527788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euser AG, Bullinger L, Cipolla MJ. Magnesium sulphate treatment decreases blood-brain barrier permeability during acute hypertension in pregnant rats. Exp Physiol. 2008;93:254–261. doi: 10.1113/expphysiol.2007.039966. [DOI] [PubMed] [Google Scholar]
- Ferment O, Touitou Y. Magnesium: metabolism and hormonal regulation in different species. Comp Biochem Physiol A. 1985;82:753–758. doi: 10.1016/0300-9629(85)90478-5. [DOI] [PubMed] [Google Scholar]
- Fogleman CD. Magnesium sulfate and other anticonvulsants for women with preeclampsia. Am Fam Physician. 2011;83:1269–1270. doi: 10.1002/14651858.cd000025.pub2. [DOI] [PubMed] [Google Scholar]
- Freedman AM, Atrakchi AH, Cassidy MM, Weglicki WB. Magnesium deficiency-induced cardiomyopathy: protection by vitamin E. Biochem Biophys Res Commun. 1990;170(3):1102–1106. doi: 10.1016/0006-291X(90)90506-I. [DOI] [PubMed] [Google Scholar]
- Galland L. Magnesium and immune function: an overview. Magnesium. 1988;7(5–6):290. [PubMed] [Google Scholar]
- Garrison SR, Allan GM, Sekhon RK, Musini VM, Khan KM. Magnesium for skeletal muscle cramps. Cochrane Database Syst Rev. 2012 doi: 10.1002/14651858.cd009402.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiger H, Wanner C. Magnesium in disease. Clin Kidney J. 2012;5:i25. doi: 10.1093/NDTPLUS/SFR165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gontijo-Amaral C, Guimarães EV, Camargos P. Oral magnesium supplementation in children with cystic fibrosis improves clinical and functional variables: a double-blind, randomized, placebo-controlled crossover trial. Am J Clin Nutr. 2012;96:50–56. doi: 10.3945/ajcn.112.034207. [DOI] [PubMed] [Google Scholar]
- Gottlieb SS. Importance of magnesium in congestive heart failure. Am J Cardiol. 1989 doi: 10.1016/0002-9149(89)90218-X. [DOI] [PubMed] [Google Scholar]
- Gottlieb SS, Fisher ML, Pressel MD, Patten RD, Weinberg M, Greenberg N. Effects of intravenous magnesium sulfate on arrhythmias in patients with congestive heart failure. Am Heart J. 1993;125(6):1645–1650. doi: 10.1016/0002-8703(93)90754-W. [DOI] [PubMed] [Google Scholar]
- Gröber U. Magnesium and drugs. Int J Mol Sci. 2019 doi: 10.3390/ijms20092094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gröber U, Schmidt J, Kisters K. Magnesium in prevention and therapy. Nutrients. 2015;7:8199–8226. doi: 10.3390/nu7095388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gröber U, Werner T, Vormann J, Kisters K. Myth or reality-transdermal magnesium? Nutrients. 2017 doi: 10.3390/nu9080813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyamlani G, Parikh C, Kulkarni AG. Benefits of magnesium in acute myocardial infarction: timing is crucial. Am Heart J. 2000;139:703. doi: 10.1016/S0002-8703(00)90051-6. [DOI] [PubMed] [Google Scholar]
- Haensch C-A. Cerebrospinal fluid magnesium level in different neurological disorders. Neurosci Med. 2010;01(02):60–63. doi: 10.4236/nm.2010.12009. [DOI] [Google Scholar]
- Hallak M, Berman RF, Irtenkauf SM, Evans MI, Cotton DB. Peripheral magnesium sulfate enters the brain and increases the threshold for hippocampal seizures in rats. Am J Obstet Gynecol. 1992;167:1605–1610. doi: 10.1016/0002-9378(92)91749-Z. [DOI] [PubMed] [Google Scholar]
- Hill J, Britton J. Dose-response relationship and time-course of the effect of inhaled magnesium sulphate on airflow in normal and asthmatic subjects. Br J Clin Pharmacol. 1995;40:539–544. doi: 10.1111/j.1365-2125.1995.tb05798.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho KM. Intravenous magnesium for cardiac arrhythmias: jack of all trades. Magnes Res. 2008;21:65–68. doi: 10.1684/mrh.2008.0130. [DOI] [PubMed] [Google Scholar]
- Ho KM, Sheridan DJ, Paterson T. Use of intravenous magnesium to treat acute onset atrial fibrillation: a meta-analysis. Heart. 2007;93:1433–1440. doi: 10.1136/hrt.2006.111492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston M. The role of magnesium in hypertension and cardiovascular disease. J Clin Hypertens. 2011;13:843–847. doi: 10.1111/j.1751-7176.2011.00538.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezhitsa I, Agarwal R. Magnesium acetyl taurate as a potential agent for retinal and optic nerve protection in glaucoma. Neural Regen Res. 2018;13:807–808. doi: 10.4103/1673-5374.232470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezhitsa I, Agarwal R, Saad SDB, Zakaria FKB, Agarwal P, Krasilnikova A, Rahman THA, Bin Rozali KN, Spasov A, Ozerov A, Alyautdin R, Ismail NM. Mechanism of the anticataract effect of liposomal MgT in galactose-fed rats. Mol vis. 2016;22:734–747. [PMC free article] [PubMed] [Google Scholar]
- Imani MM, Safaei M. Optimized synthesis of magnesium oxide nanoparticles as bactericidal agents. J Nanotechnol. 2019 doi: 10.1155/2019/6063832. [DOI] [Google Scholar]
- Ince C, Schulman SP, Quigley JF, Berger RD, Kolasa M, Ferguson R, Silver B, Haigney MCP. Usefulness of magnesium sulfate in stabilizing cardiac repolarization in heart failure secondary to ischemic cardiomyopathy. Am J Cardiol. 2001;88(3):224–229. doi: 10.1016/S0002-9149(01)01630-7. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (US) (2011) Committee on nutrition, trauma, and the brain, John Erdman, Maria Oria, and Laura Pillsbury. “Magnesium” https://www.ncbi.nlm.nih.gov/books/NBK209305/. Accessed 20 June 2020
- Iotti S, Malucelli E. Free magnesium concentration in the human brain. In: Vink R, Nechifor M, editors. Magnesium in the central nervous system. South Australia: University of Adelaide Press; 2011. pp. 3–12. [PubMed] [Google Scholar]
- Jahnen-Dechent W, Ketteler M. Magnesium basics. CKJ Clin Kidney J. 2012;5:i3–i14. doi: 10.1093/ndtplus/sfr163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamilian M, Samimi M, Faraneh AE, Aghadavod E, Shahrzad HD, Chamani M, Mafi A, Asemi Z. Magnesium supplementation affects gene expression related to insulin and lipid in patients with gestational diabetes. Magnes Res. 2017;30:71–79. doi: 10.1684/mrh.2017.0425. [DOI] [PubMed] [Google Scholar]
- Jee D, Lee D, Yun S, Lee C. Magnesium sulphate attenuates arterial pressure increase during laparoscopic cholecystectomy. Br J Anaesth. 2009;103:484–489. doi: 10.1093/bja/aep196. [DOI] [PubMed] [Google Scholar]
- Kanthlal SK, Joseph J, Paul B, Vijayakumar M, Uma Devi P. Antioxidant and vasorelaxant effects of aqueous extract of large cardamom in L-NAME induced hypertensive rats. Clin Exp Hypertens. 2020 doi: 10.1080/10641963.2020.1739699. [DOI] [PubMed] [Google Scholar]
- Kass LS, Poeira F. The effect of acute vs chronic magnesium supplementation on exercise and recovery on resistance exercise, blood pressure and total peripheral resistance on normotensive adults. J Int Soc Sports Nutr. 2015 doi: 10.1186/s12970-015-0081-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaya M, Ahishali B. The role of magnesium in edema and blood-brain barrier disruption. In: Vink R, Nechifor M, editors. Magnesium in the central nervous system. Adelaide: University of Adelaide Press; 2011. pp. 135–144. [PubMed] [Google Scholar]
- Kelly HW. Magnesium sulfate for severe acute asthma in children. J Pediatr Pharmacol Ther. 2003;8:40–45. doi: 10.5863/1551-6776-8.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kercsmar CM. Wheezing in older children: asthma. In: Wilmott R, Bush A, Deterding R, Ratjen F, Sly P, Zar H, Li A, editors. Kendig’s disorders of the respiratory tract in children. Amsterdam: Elsevier Inc; 2006. pp. 810–838. [Google Scholar]
- Kesmati M, Torabi MHT. Interaction between anxiolytic effects of magnesium oxide nanoparticles and exercise in adult male rat. Nanomed J. 2014;1:324–330. [Google Scholar]
- Kharb S, Singh V. Magnesium deficiency potentiates free radical production associated with myocardial infarction. J Assoc Phys India. 2000;48(5):484. [PubMed] [Google Scholar]
- Kirkland AE, Sarlo GL, Holton KF. The role of magnesium in neurological disorders. Nutrients. 2018;10:1–23. doi: 10.3390/nu10060730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knape MJ, Ahuja LG, Bertinetti D, Burghardt NCG, Zimmermann B, Taylor SS, Herberg FW. Divalent metal ions Mg2+ and Ca2+ have distinct effects on protein kinase a activity and regulation. ACS Chem Biol. 2015;10(10):2303–2315. doi: 10.1021/acschembio.5b00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knightly R, Milan SJ, Hughes R, Knopp Sihota JA, Rowe BH, Normansell R, Powell C (2017) Inhaled magnesium sulfate in the treatment of acute asthma Cochrane Database Syst Rev 2017(11):CD003898 [DOI] [PMC free article] [PubMed]
- Kokotajlo S, Degnan L, Meyers R, Siu A, Robinson C. Use of intravenous magnesium sulfate for the treatment of an acute asthma exacerbation in pediatric patients. J Pediatr Pharmacol Ther. 2014;19:91–97. doi: 10.5863/1551-6776-19.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolte D, Vijayaraghavan K, Khera S, Sica DA, Frishman WH. Role of magnesium in cardiovascular diseases. Cardiol Rev. 2014;22:182–192. doi: 10.1023/A:1016058229972. [DOI] [PubMed] [Google Scholar]
- Korish AA. Magnesium sulfate therapy of preeclampsia: an old tool with new mechanism of action and prospect in management and prophylaxis. Hypertens Res. 2012;35:1005–1011. doi: 10.1038/hr.2012.103. [DOI] [PubMed] [Google Scholar]
- Kostov K. Effects of magnesium deficiency on mechanisms of insulin resistance in type 2 diabetes: focusing on the processes of insulin secretion and signaling. Int J Mol Sci. 2019 doi: 10.3390/ijms20061351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowal A, Panaszek B, Barg W, Obojski A. The use of magnesium in bronchial asthma: a new approach to an old problem. Arch Immunol Ther Exp (warsz) 2007;55:35–39. doi: 10.1007/s00005-007-0008-8. [DOI] [PubMed] [Google Scholar]
- Kubena KS. The role of magnesium in immunity. J Nutr Immunol. 1994;2(3):107–126. doi: 10.1300/J053v02n03_07. [DOI] [Google Scholar]
- Kumar P, Bhargava S, Agarwal P, Garg A, Khosla A. Association of serum magnesium with type 2 diabetes mellitus and diabetic retinopathy. J Fam Med Prim Care. 2019;8:1671. doi: 10.4103/jfmpc.jfmpc_83_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kundu D, Roy A, Mandal T, Bandyopadhyay U, Ghosh E, Ray D. Oxidative stress in alcoholic and viral hepatitis. N Am J Med Sci. 2012;4:412–415. doi: 10.4103/1947-2714.100993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kupetsky-Rincon EA, Li Q, Uitto J. Magnesium reduces carotid intima-media thickness in a mouse model of pseudoxanthoma elasticum: a novel treatment biomarker. Clin Transl Sci. 2012;5:259–264. doi: 10.1111/j.1752-8062.2011.00390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laires MJ, Monteiro C. Exercise, magnesium and immune function. Magnes Res. 2008;21(2):92–96. doi: 10.1684/mrh.2008.0136. [DOI] [PubMed] [Google Scholar]
- Landon RA, Young EA. Role of magnesium in regulation of lung function. J Am Diet Assoc. 1993;93:674–677. doi: 10.1016/0002-8223(93)91675-G. [DOI] [PubMed] [Google Scholar]
- Lee JHT, Roy J, Moon Sohn H, Cheong M, Liu J, Stammers AT, Tetzlaff W, Kwon BK. Magnesium in a polyethylene glycol formulation provides neuroprotection after unilateral cervical spinal cord injury. Spine (phila Pa 1976) 2010;35(2010):2041–2048. doi: 10.1097/BRS.0b013e3181d2d6c5. [DOI] [PubMed] [Google Scholar]
- Lee MJ, Alvarez JA, Smith EM, Killilea DW, Chmiel JF, Joseph PM, Grossmann RE, Gaggar A, Ziegler TR, Tangpricha V. Changes in mineral micronutrient status during and after pulmonary exacerbation in adults with cystic fibrosis. Nutr Clin Pract. 2015;30:838–843. doi: 10.1177/0884533615589991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li FY, Lenardo MJ, Chaigne-Delalande B. Loss of MAGT1 abrogates the Mg 2+ flux required for T cell signaling and leads to a novel human primary immunodeficiency. Magnes Res. 2011;24:S109. doi: 10.1684/mrh.2011.0286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li FY, Chaigne-Delalande B, Kanellopoulou C, Davis JC, Matthews HF, Douek DC, Cohen JI, Uzel G, Su HC, Lenardo MJ. Second messenger role for Mg 2+ revealed by human T-cell immunodeficiency. Nature. 2011;475:471–476. doi: 10.1038/nature10246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Chaigne-delalande B, Kanellopoulou C, Jeremiah C, Lenardo MJ. Signaling role for Mg2+ revealed by immunodeficiency due to loss of MagT1. Nature. 2012;475:471–476. doi: 10.1038/nature10246.Signaling. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Han X, Yang J, Bao J, Di X, Zhang G, Liu H. Magnesium sulfate provides neuroprotection in eclampsia-like seizure model by ameliorating neuroinflammation and brain edema. Mol Neurobiol. 2017;54:7938–7948. doi: 10.1007/s12035-016-0278-4. [DOI] [PubMed] [Google Scholar]
- Li W, Zhu X, Song Y, Fan L, Wu L, Kabagambe EK, Hou L, Shrubsole MJ, Liu J, Dai Q. Intakes of magnesium, calcium and risk of fatty liver disease and prediabetes. Vic Lit Cult. 2018;21:2088–2095. doi: 10.1017/S1368980018000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li XJ, Xie L, Pan FS, Wang Y, Liu H, Tang YR, Hutnik CML. A feasibility study of using biodegradable magnesium alloy in glaucoma drainage device. Int J Ophthalmol. 2018;11:135–142. doi: 10.18240/ijo.2018.01.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang RY, Wu W, Huang J, Jiang SP, Lin Y. Magnesium affects the cytokine secretion of CD4+ T lymphocytes in acute asthma. J Asthma. 2012;49:1012–1015. doi: 10.3109/02770903.2012.739240. [DOI] [PubMed] [Google Scholar]
- Liu M, Yang H, Mao Y. Magnesium and liver disease. Ann Transl Med. 2019;7:578–578. doi: 10.21037/atm.2019.09.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long S, Romani AM. Role of cellular magnesium in human diseases. 22Austin J Nutr Food Sci. 2014;2:1–19. [PMC free article] [PubMed] [Google Scholar]
- Lu L, Liu M, Sun RR, Zheng Y, Zhang P. Myocardial infarction: symptoms and treatments. Cell Biochem Biophys. 2015;72:865–867. doi: 10.1007/s12013-015-0553-4. [DOI] [PubMed] [Google Scholar]
- Lucas MJ, Leveno KJ, Cunningham FG. A comparison of magnesium sulfate with phenytoin for the prevention of eclampsia. N Engl J Med. 1995;333:201–205. doi: 10.1056/NEJM199507273330401. [DOI] [PubMed] [Google Scholar]
- Maguire ME, Cowan JA. Magnesium chemistry and biochemistry. Biometals. 2002;15:203–210. doi: 10.1023/A:1016058229972. [DOI] [PubMed] [Google Scholar]
- Maier JA, Pickering G, Giacomoni E, Cazzaniga A, Pellegrino P. Headaches and magnesium: mechanisms, bioavailability, therapeutic efficacy and potential advantage of magnesium pidolate. Nutrients. 2020;12(9):2660. doi: 10.3390/nu12092660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makiura M, Akamatsu H, Akita H, Yagami A, Shimizu Y, Eiro H, Kuramoto M, Suzuki K, Matsunaga K. Atopic dermatitis-like symptoms in HR-1 hairless mice fed a diet low in magnesium and zinc. J Int Med Res. 2004;32:392–399. doi: 10.1177/147323000403200407. [DOI] [PubMed] [Google Scholar]
- Maktabi M, Jamilian M, Amirani E, Chamani M, Asemi Z. The effects of magnesium and vitamin e co-supplementation on parameters of glucose homeostasis and lipid profiles in patients with gestational diabetes. Lipids Health Dis. 2018 doi: 10.1186/s12944-018-0814-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-Esparza M, Tristán-Manzano M, Ruiz-Alcaraz AJ, García-Peñarrubia P. Inflammatory status in human hepatic cirrhosis. World J Gastroenterol. 2015;21:11522–11541. doi: 10.3748/wjg.v21.i41.11522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathew R, Altura BM. Magnesium and the lungs. Magnesium. 1988;7:173–187. [PubMed] [Google Scholar]
- Mathew IE, Baby A, Joseph S, Gireesh Kumar KP, Anila KN. Study on clinical pharmacist initiated interventions on COPD and asthma patients. J Pharm Sci Res. 2017;9:1212–1216. [Google Scholar]
- McLean RM. Magnesium and its therapeutic uses: a review. Am J Med. 1994;96:63–76. doi: 10.1016/0002-9343(94)90117-1. [DOI] [PubMed] [Google Scholar]
- Merrill JJ, DeWeese G, Wharton JM. Magnesium reversal of digoxin-facilitated ventricular rate during atrial fibrillation in the Wolff-Parkinson-White syndrome. Am J Med. 1994;97:25–28. doi: 10.1016/0002-9343(94)90044-2. [DOI] [PubMed] [Google Scholar]
- Miller S, Crystal E, Garfinkle M, Lau C, Lashevsky I, Connolly SJ. Effects of magnesium on atrial fibrillation after cardiac surgery: a meta-analysis. Heart. 2005;91:618–623. doi: 10.1136/hrt.2004.033811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moh’d Nour MBY, Alshawabkeh AD, Jadallah ARR, et al. Magnesium sulfate extended infusion as an adjunctive treatment for complicated Covid-19 infected critically ill patients. EAS J Anesthesiol Crit Care. 2020 doi: 10.36349/easjacc.2020.v02i03.17. [DOI] [Google Scholar]
- Mohammed S, Goodacre S. Intravenous and nebulised magnesium sulphate for acute asthma: systematic review and meta-analysis. Emerg Med J. 2007;24:823–830. doi: 10.1136/emj.2007.052050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morakinyo AO, Samuel TA, Adekunbi DA. Magnesium upregulates insulin receptor and glucose transporter-4 in streptozotocin-nicotinamide-induced type-2 diabetic rats. Endocr Regul. 2018;52:6–16. doi: 10.2478/enr-2018-0002. [DOI] [PubMed] [Google Scholar]
- Nagai N, Ito Y, Inomata M, Shumiya S, Tai H, Hataguchi Y, Nakagawa K. Delay of cataract development in the Shumiya cataract rat by the administration of drinking water containing high concentration of magnesium ion. Biol Pharm Bull. 2006;29:1234–1238. doi: 10.1248/bpb.29.1234. [DOI] [PubMed] [Google Scholar]
- Nagai N, Ito Y, Tai H, Hataguchi Y, Nakagawa K. Effects of magnesium content in the feed on cataract development in shumiya cataract rat. J Oleo Sci. 2007;56:29–33. doi: 10.5650/jos.56.29. [DOI] [PubMed] [Google Scholar]
- Nageris BI, Ulanovski D, Attias J. Magnesium treatment for sudden hearing loss. Ann Otol Rhinol. 2004;113(8):672–675. doi: 10.1177/000348940411300814. [DOI] [PubMed] [Google Scholar]
- Neumann JT, Diaz-Sylvester PL, Fleischer S, Copello JA. CGP-37157 inhibits the sarcoplasmic reticulum Ca 2+ ATPase and activates ryanodine receptor channels in striated muscle. Mol Pharmacol. 2011;79:141–147. doi: 10.1124/mol.110.067165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni H, Naing C, Aye SZ. Magnesium sulfate for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2020 doi: 10.1002/14651858.CD013506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen FH. Magnesium deficiency and increased inflammation: current perspectives. J Inflamm Res. 2018;11:25–34. doi: 10.2147/JIR.S136742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen FH, Lukaski HC. Update on the relationship between magnesium and exercise. Magnes Res. 2006;19:180–189. doi: 10.1684/mrh.2006.0060. [DOI] [PubMed] [Google Scholar]
- Nuytten D, Van Hees J, Meulemans A, Carton H. Magnesium deficiency as a cause of acute intractable seizures. J Neurol. 1991;238(5):262–264. doi: 10.1007/BF00319737. [DOI] [PubMed] [Google Scholar]
- Onalan O, Crystal E, Daoulah A, Lau C, Crystal A, Lashevsky I. Meta-analysis of magnesium therapy for the acute management of rapid atrial fibrillation. Am J Cardiol. 2007;99:1726–1732. doi: 10.1016/j.amjcard.2007.01.057. [DOI] [PubMed] [Google Scholar]
- Orchard TS, Larson JC, Alghothani N, Bout-Tabaku S, Cauley JA, Chen Z, LaCroix AZ, Wactawski-Wende J, Jackson RD. Magnesium intake, bone mineral density, and fractures: results from the women’s health initiative observational study. Am J Clin Nutr. 2014;99:926–933. doi: 10.3945/ajcn.113.067488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JH. Insulin resistance in non-alcoholic fatty liver disease. Korean J Hepatol. 2006;12:16–30. doi: 10.2174/138161210791208875. [DOI] [PubMed] [Google Scholar]
- Petrović J, Stanić D, Dmitrašinović G, Plećaš-Solarović B, Ignjatović S, Batinić B, Popović D, Pešić V. Magnesium supplementation diminishes peripheral blood lymphocyte DNA oxidative damage in athletes and sedentary young man. Oxid Med Cell Longev. 2016 doi: 10.1155/2016/201964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham PCT, Pham PAT, Pham SV, Pham PTT, Pham PMT, Pham PTT. Hypomagnesemia: a clinical perspective. Int J Nephrol Renovasc Dis. 2014 doi: 10.2147/IJNRD.S42054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokan R, Hofmann P, Von Duvillard SP, Smekal G, Wonisch M, Lettner K, Schmid P, Shechter M, Von Duvillard SP. Oral magnesium therapy, exercise heart rate, exercise tolerance, and myocardial function in coronary artery disease patients. Br J Sport Med. 2006;40:773–778. doi: 10.1136/bjsm.2006.027250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poleszak E (2008) Benzodiazepine/GABAA receptors are involved in magnesium-induced anxiolytic-like behavior in mice. Pharmacol Rep 60:483–489. https://pubmed.ncbi.nlm.nih.gov/18799816/ [PubMed]
- Pourdowlat G, Mousavinasab SR, Farzanegan B, Kashefizadeh A, Meybodi ZA, Jafarzadeh M, Baniasadi S. Evaluation of the efficacy and safety of inhaled magnesium sulphate in combination with standard treatment in patients with moderate or severe COVID-19: a structured summary of a study protocol for a randomised controlled trial. Trials. 2021;22:60. doi: 10.1186/s13063-021-05032-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proksch E, Nissen HP, Bremgartner M, Urquhart C. Bathing in a magnesium-rich dead sea salt solution improves skin barrier function, enhances skin hydration, and reduces inflammation in atopic dry skin. Int J Dermatol. 2005;44:151–157. doi: 10.1111/j.1365-4632.2005.02079.x. [DOI] [PubMed] [Google Scholar]
- Puche JE, Saiman Y, Friedman SL. Hepatic stellate cells and liver fibrosis. Compr Physiol. 2013;3:1473–1492. doi: 10.1002/cphy.c120035. [DOI] [PubMed] [Google Scholar]
- Rafeeq MM, Murad HAS. Cystic fibrosis: current therapeutic targets and future approaches. J Transl Med. 2017 doi: 10.1186/s12967-017-1193-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajitha P, Shammika P, Aiswarya S, Gopikrishnan A, Jayakumar R, Sabitha M. Chaulmoogra oil-based methotrexate loaded topical nanoemulsion for the treatment of psoriasis. J Drug Deliv Sci Technol. 2019;49:463–476. doi: 10.1016/j.jddst.2018.12.020. [DOI] [Google Scholar]
- Ramee SR, White CJ, Svinarich JT, Watson TD, Fox RF. Torsade de pointes and magnesium deficiency. Am Heart J. 1985;109:164–167. doi: 10.1016/0002-8703(85)90432-6. [DOI] [PubMed] [Google Scholar]
- Rasmussen HS, Thomsen PEB. The electrophysiological effects of intravenous magnesium on human sinus node, atrioventricular node, atrium, and ventricle. Clin Cardiol. 1989;12:85–90. doi: 10.1002/clc.4960120204. [DOI] [PubMed] [Google Scholar]
- Ravell J, Chaigne-Delalande B, Lenardo M. X-linked immunodeficiency with magnesium defect, Epstein-Barr virus infection, and neoplasia disease: a combined immune deficiency with magnesium defect. Curr Opin Pediatr. 2014;26:713–719. doi: 10.1097/MOP.0000000000000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayssiguier Y, Libako P, Nowacki W, Rock E. Magnesium deficiency and metabolic syndrome: stress and inflammation may reflect calcium activation. Magnes Res. 2010;23(2):73–80. doi: 10.1684/mrh.2010.0208. [DOI] [PubMed] [Google Scholar]
- Razzaque MS. Magnesium: are we consuming enough? Nutrients. 2018;10:1–8. doi: 10.3390/nu10121863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter K, Kietzmann T. Reactive oxygen species and fibrosis: further evidence of a significant liaison. Cell Tissue Res. 2016;365:591–605. doi: 10.1007/s00441-016-2445-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Hernandez H, Cervantes-Huerta M, Rodriguez-Moran M, Guerrero-Romero F. Oral magnesium supplementation decreases alanine aminotransferase levels in obese women. Magnes Res. 2010;23:90–96. doi: 10.1684/mrh.2010.0204. [DOI] [PubMed] [Google Scholar]
- Romani AMP. Cellular magnesium homeostasis. Arch Biochem Biophys. 2011;512:1–23. doi: 10.1016/j.abb.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romani AMP. Intracellular magnesium homeostasis. Magnes Cent Nerv Syst. 2011;512:13–58. doi: 10.1017/UPO9780987073051.003. [DOI] [Google Scholar]
- Rose S, Jim On S, Fuchs W, Chen C, Phelps R, Kornreich D, Haddican M, et al. Magnesium supplementation in the treatment of pseudoxanthoma elasticum: a randomized trial. JADD. 2019;81(1):263–265. doi: 10.1016/j.jaad.2019.02.055. [DOI] [PubMed] [Google Scholar]
- Rosique-Esteban N, Guasch-Ferré M, Hernández-Alonso P, Salas-Salvadó J. Dietary magnesium and cardiovascular disease: a review with emphasis in epidemiological studies. Nutrients. 2018 doi: 10.3390/nu10020168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rude RK. Physiology of magnesium metabolism and the important role of magnesium in potassium deficiency. Am J Cardiol. 1989;63:G13–G34. doi: 10.1016/0002-9149(89)90216-6. [DOI] [PubMed] [Google Scholar]
- Rude RK, Kirchen ME, Gruber HE, Stasky AA, Meyer MH. Magnesium deficiency induces bone loss in the rat. Miner Electrolyte Metab. 1998;24:314–320. doi: 10.1159/000057389. [DOI] [PubMed] [Google Scholar]
- Rude RK, Gruber HE, Wei LY, Frausto A, Mills BG. Magnesium deficiency: effect on bone and mineral metabolism in the mouse. Calcif Tissue Int. 2003;72:32–41. doi: 10.1007/s00223-001-1091-1. [DOI] [PubMed] [Google Scholar]
- Rude RK, Singer FR, Gruber HE. Skeletal and hormonal effects of magnesium deficiency. ACN. 2009;28(2):131–141. doi: 10.1080/07315724.2009.10719764. [DOI] [PubMed] [Google Scholar]
- Sadeh M, Blatt I, Martonovits G, Karni A, Goldhammer Y. Treatment of porphyric convulsions with magnesium sulfate. Epilepsia. 1991;32(5):712–715. doi: 10.1111/j.1528-1157.1991.tb04714.x. [DOI] [PubMed] [Google Scholar]
- Salaminia S, Sayehmiri F, Angha P, Sayehmiri K, Motedayen M. Evaluating the effect of magnesium supplementation and cardiac arrhythmias after acute coronary syndrome: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2018 doi: 10.1186/s12872-018-0857-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders NN, Franckx H, De Boeck K, Haustraete J, De Smedt SC, Demeester J. Role of magnesium in the failure of rhDNase therapy in patients with cystic fibrosis. Thorax. 2006;61:962–968. doi: 10.1136/thx.2006.060814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santi M, Milani GP, Simonetti GD, Fossali EF, Bianchetti MG, Lava SAG. Magnesium in cystic fibrosis—systematic review of the literature. Pediatr Pulmonol. 2015;51:196–202. doi: 10.1002/ppul.23356. [DOI] [PubMed] [Google Scholar]
- Saris NEL, Mervaala E, Karppanen H, Khawaja JA, Lewenstam A. Magnesium: an update on physiological, clinical and analytical aspects. Clin Chim Acta. 2000;294:1–26. doi: 10.1016/S0009-8981(99)00258-2. [DOI] [PubMed] [Google Scholar]
- Schlingmann KP, Waldegger S, Konrad M, Chubanov V, Gudermann T. TRPM6 and TRPM7-gatekeepers of human magnesium metabolism. Biochim Biophys Acta. 2007;1772:813–821. doi: 10.1016/j.bbadis.2007.03.009. [DOI] [PubMed] [Google Scholar]
- Schmitz C, Anne-Laure P. Molecular, genetic, and nutritional aspects of major and trace minerals. In: Collins J, editor. Magnesium and the immune response. Amsterdam: Elsevier Inc; 2017. pp. 319–331. [Google Scholar]
- Schuchardt JP, Hahn A. Intestinal absorption and factors influencing bioavailability of magnesium—an update. Curr Nutr Food Sci. 2017;13:260–278. doi: 10.1155/2017/4179326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwalfenberg GK, Genuis SJ. The importance of magnesium in clinical healthcare. Scientifica (cairo) 2017 doi: 10.1155/2017/4179326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sendowski I. Magnesium therapy in acoustic trauma. Magnes Res. 2006;19(4):244–254. doi: 10.1684/mrh.2006.0075. [DOI] [PubMed] [Google Scholar]
- Sendowski I, Holy X, Raffin F, Cazals Y. Magnesium and hearing loss. In: Vink R, Nechifor M, editors. Magnesium in the central nervous system. Adelaide: University of Adelaide Press; 2011. pp. 145–156. [PubMed] [Google Scholar]
- Seo JW, Park TJ. Magnesium metabolism. electrolyte. Blood Press. 2008;6:86–95. doi: 10.5049/EBP.2008.6.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahbah D, Hassan T, Morsy S, Saadany HEI, Fathy M, Al-Ghobashy A, Elsamad N, Emam A, Elhewala A, Ibrahim B, El Gebaly S, El Sayed H, Ahmed H. Oral magnesium supplementation improves glycemic control and lipid profile in children with type 1 diabetes and hypomagnesaemia. Medicine (united States) 2017;96:e6352. doi: 10.1097/MD.0000000000006352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahidi-Dadras M, Namazi N, Khalilazar S, Younespour S. Trace elements status in psoriasis and their relationship with the severity of the disease. Iran J Dermatol. 2012;15:38–41. [Google Scholar]
- Shaikh MN, Malapati BR, Gokani R, Patel B, Chatriwala M. Serum magnesium and vitamin D levels as indicators of asthma severity. Pulm Med. 2016 doi: 10.1155/2016/1643717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shan Z, Rong Y, Yang W, Wang D, Yao P, Xie J, Liu L. Intravenous and nebulized magnesium sulfate for treating acute asthma in adults and children: a systematic review and meta-analysis. Respir Med. 2013;107:321–330. doi: 10.1016/j.rmed.2012.12.001. [DOI] [PubMed] [Google Scholar]
- Shen Y, Dai L, Tian H, Xu R, Li F, Li Z, Zhou J, Wang L, Dong J, Sun L. Treatment of magnesium-l-threonate elevates the magnesium level in the cerebrospinal fluid and attenuates motor deficits and dopamine neuron loss in a mouse model of Parkinson’s disease. Neuropsychiatr Dis Treat. 2019;15:3143–3153. doi: 10.2147/NDT.S230688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shivanthan MC, Rajapakse S. Magnesium for acute exacerbation of chronic obstructive pulmonary disease: a systematic review of randomised trials. Ann Thorac Med. 2014;9:77–80. doi: 10.4103/1817-1737.128844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibai BM. Magnesium sulfate prophylaxis in preeclampsia: lessons learned from recent trials. Am J Obstet Gynecol. 2004;190:1520–1526. doi: 10.1016/j.ajog.2003.12.057. [DOI] [PubMed] [Google Scholar]
- Sideris AM, Galiatsu E, Filippatos GS, Kappos K, Anthopoulos LP. Effects of magnesium and potassium on Wolff–Parkinson-White syndrome. J Electrocardiol. 1996;29:11–15. doi: 10.1016/S0022-0736(96)80106-3. [DOI] [PubMed] [Google Scholar]
- Skorodin MS, Tenholder MF, Yetter B, Owen KA, Waller RF, Khandelwahl S, Maki K, Rohail T, D’alfonso N. Magnesium sulfate in exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 1995;155:496–500. doi: 10.1001/archinte.1995.00430050072008. [DOI] [PubMed] [Google Scholar]
- Song WJ, Chang YS. Magnesium sulfate for acute asthma in adults: a systematic literature review. Asia Pac Allergy. 2012;2:76. doi: 10.5415/apallergy.2012.2.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperl A, Heller RA, Biglari B, Haubruck P, Seelig J, Schomburg L, Bock T, Moghaddam A. The role of magnesium in the secondary phase after traumatic spinal cord injury. A prospective clinical observer study. Antioxidants. 2019;8(11):509. doi: 10.3390/antiox8110509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangherlin A, O’Neill JS. Signal transduction: magnesium manifests as a second messenger. Curr Biol. 2018;28:R1403–R1405. doi: 10.1016/j.cub.2018.11.0. [DOI] [PubMed] [Google Scholar]
- Stepura OB, Martynow AI. Magnesium orotate in severe congestive heart failure (MACH) Int J Cardiol. 2009;131:293–295. doi: 10.1016/j.ijcard.2007.11.022. [DOI] [PubMed] [Google Scholar]
- Sun-Edelstein C, Mauskop A. Role of magnesium in the pathogenesis and treatment of migraine. Expert Rev Neurother. 2009;9(3):369–379. doi: 10.1586/14737175.9.3.369. [DOI] [PubMed] [Google Scholar]
- Swaminathan R. Magnesium metabolism and its disorders. Clin Biochem Rev. 2003;24:47–66. [PMC free article] [PubMed] [Google Scholar]
- Tam M, Gómez S, González-Gross M, Marcos A. Possible roles of magnesium on the immune system. Eur J Clin Nutr. 2003;57:1193–1197. doi: 10.1038/sj.ejcn.1601689. [DOI] [PubMed] [Google Scholar]
- Tan WW, Chan DWS, Lee JH, Thomas T, Menon AP, Chan YH. Use of magnesium sulfate infusion for the management of febrile illness-related epilepsy syndrome: a case series. Child Neurol Open. 2015 doi: 10.1177/2329048x14550067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan CW, Ho LP, Kalimuddin S, Cherng BPZ, Teh YE, Thien SY, Wong HM, Tern PJW, et al. A cohort study to evaluate the effect of combination vitamin D, magnesium and vitamin B12 (DMB) on progression to severe outcome in older COVID-19 patients. MedRxiv. 2020 doi: 10.1101/2020.06.01.20112334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang CF, Ding H, Jiao RQ, Xing Xin Wu, Kong LD. Possibility of magnesium supplementation for supportive treatment in patients with COVID-19. Eur J Pharmacol. 2020;886:173546. doi: 10.1016/j.ejphar.2020.173546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangvoraphonkchai K, Davenport A. Magnesium and cardiovascular disease. Adv Chronic Kidney Dis. 2018;25:251–260. doi: 10.1053/j.ackd.2018.02.010. [DOI] [PubMed] [Google Scholar]
- Tee JK, Peng F, Tan YL, Yu B, Ho HK. Magnesium isoglycyrrhizinate ameliorates fibrosis and disrupts TGF-β-Mediated SMAD pathway in activated hepatic stellate cell line LX2. Front Pharmacol. 2018 doi: 10.3389/fphar.2018.01018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teo KK, Yusuf S, Collins R, Held PH, Peto R, Rory Collins O. Effects of intravenous magnesium in suspected acute myocardial infarction: overview of randomised trials. BMJ. 1991;303:1499–1503. doi: 10.1136/bmj.303.6816.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ter Braake AD, Shanahan CM, De Baaij JHF. Magnesium counteracts vascular calcification: passive interference or active modulation? Arterioscler Thromb Vasc Biol. 2017;37:1431–1445. doi: 10.1161/ATVBAHA.117.309182. [DOI] [PubMed] [Google Scholar]
- Ter Braake AD, Tinnemans PT, Shanahan CM, Hoenderop JGJ, De Baaij JHF. Magnesium prevents vascular calcification in vitro by inhibition of hydroxyapatite crystal formation. Sci Rep. 2018;8:1–11. doi: 10.1038/s41598-018-20241-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terasaki M, Rubin H. Evidence that intracellular magnesium is present in cells at a regulatory concentration for protein synthesis. Proc Natl Acad Sci USA. 1985;82:7324–7326. doi: 10.1073/pnas.82.21.7324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terra VC, de Albuquerque M, Scorza CA, Arida RM, Scorza FA. Serum magnesium: a clinical biomarker for sudden unexpected death in epilepsy? J Epilepsy Clin Neurophysiol. 2011;17(2):77–77. doi: 10.1590/S1676-26492011000200008. [DOI] [Google Scholar]
- Teymoor Y, Kauhanen J. “Dietary intake of magnesium and the risk of epilepsy in middle-aged and older finnish men: A 22-year follow-up study in a general population. Nutrition. 2019;58:36–39. doi: 10.1016/j.nut.2018.06.019. [DOI] [PubMed] [Google Scholar]
- Topol EJ, Lerman BB. Hypomagnesemic torsades de pointes. Am J Cardiol. 1983;52:1367–1368. doi: 10.1016/0002-9149(83)90611-2. [DOI] [PubMed] [Google Scholar]
- Touyz RM. Magnesium and hypertension. Curr Opin Nephrol Hypertens. 2006;15:141–144. doi: 10.1097/01.mnh.0000214773.34480.d4. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Vink R (2011) Magnesium and traumatic brain injury. In: Vink R, Nechifor M (eds) University of Adelaide Press, South Australia, pp 255–267
- Veronese N, Zurlo A, Solmi M, Luchini C, Trevisan C, Bano G, Manzato E, Sergi G, Rylander R. Magnesium status in Alzheimer’s disease: a systematic review. Am J Alzheimers Dis Other Demen. 2016;31(3):208–213. doi: 10.1177/1533317515602674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayan M, Anisha KA, Arjun SKS, Roshni PR. Clinical profile and prescribing pattern of cirrhosis in a tertiary care hospital. Indian J Pharm Pract. 2014;7:69–74. doi: 10.5530/ijopp.7.3.12. [DOI] [Google Scholar]
- Vormann J. Magnesium: nutrition and homoeostasis. AIMS Public Health. 2016;3:329–340. doi: 10.3934/publichealth.2016.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Liu Y, Zhou LJ, Wu Y, Li F, Shen KF, Pang RP, Wei XH, Li YY, Liu XG. Magnesium l-threonate prevents and restores memory deficits associated with neuropathic pain by inhibition of TNF-α. Pain Physician. 2013;16:563–575. [PubMed] [Google Scholar]
- Wang P, Yu X, Guan PP, Guo JW, Wang Y, Zhang Y, Zhao H, Wang ZY. Magnesium ion influx reduces neuroinflammation in Aβ precursor protein/presenilin 1 transgenic mice by suppressing the expression of interleukin-1β. Cell Mol Immunol. 2017;14:451–464. doi: 10.1038/cmi.2015.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch AA, Skinner J, Hickson M. Dietary magnesium may be protective for aging of bone and skeletal muscle in middle and younger older age men and women: cross-sectional findings from the UK biobank cohort. Nutrients. 2017 doi: 10.3390/nu9111189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weng L, Webster TJ. Nanostructured magnesium has fewer detrimental effects on osteoblast function. Int J Nanomedicine. 2013;8:1773–1781. doi: 10.2147/IJN.S39031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witlin AG, Sibai BM. Magnesium sulfate therapy in preeclampsia and eclampsia. Obstet Gynecol. 1998;92:883–889. doi: 10.1016/S0029-7844(98)00277-4. [DOI] [PubMed] [Google Scholar]
- Wolf FI, Trapani V. Cell (patho)physiology of magnesium. Clin Sci. 2008;114:27–35. doi: 10.1042/CS20070129. [DOI] [PubMed] [Google Scholar]
- Wu L, Zhu X, Fan L, Kabagambe EK, Song Y, Tao M, Zhong X, Hou L, Shrubsole MJ, Liu J, Da Q. Magnesium intake and mortality due to liver diseases: results from the third national health and nutrition examination survey cohort. Sci Rep. 2017 doi: 10.1038/s41598-017-18076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu ZP, Li L, Bao J, Wang ZH, Zeng J, Liu EJ, Li XG, Huang RX, Gao D, Li MZ, Zhang Y, Liu GP, Wang JZ. Magnesium protects cognitive functions and synaptic plasticity in streptozotocin-induced sporadic Alzheimer’s model. PLoS ONE. 2014;9:1–11. doi: 10.1371/journal.pone.0108645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue W, You J, Su Y, Wang Q. The effect of magnesium deficiency on neurological disorders: a narrative review article. Iran J Public Health. 2019;48:379–387. [PMC free article] [PubMed] [Google Scholar]
- Yamanaka R, Shindo Y, Okak K. Magnesium is a key player in neuronal maturation and neuropathology. Int J Mol Sci. 2019 doi: 10.3390/ijms20143439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Lu, Lizhe Xu, Min Xu, Wan Bo, Long Yu, Huang Q. Role of Mg2+ ions in protein kinase phosphorylation: insights from molecular dynamics simulations of ATP-kinase complexes. Mol Simul. 2011;37(14):1143–1150. doi: 10.1080/08927022.2011.561430. [DOI] [Google Scholar]
- Yuen AWC, Sander JW. Can magnesium supplementation reduce seizures in people with epilepsy? Hypothesis Epilepsy Res. 2012;100(1–2):152–156. doi: 10.1016/j.eplepsyres.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Zehender M. Magnesium as an anti-arrhythmic therapy principle in supraventricular and ventricular cardiac arrhythmias. Z Kardiol. 1996;85(6):135–145. [PubMed] [Google Scholar]
- Zeper LW, De Baaij JHF. Magnesium and calciprotein particles in vascular calcification: the good cop and the bad cop. Curr Opin Nephrol Hypertens. 2019;28:368–374. doi: 10.1097/MNH.0000000000000509. [DOI] [PubMed] [Google Scholar]
- Zhang CY, Yuan WG, He P, Lei JH, Wang CX. Liver fibrosis and hepatic stellate cells: etiology, pathological hallmarks and therapeutic targets. World J Gastroenterol. 2016;22:10512–10522. doi: 10.3748/wjg.v22.i48.10512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheltova AA, Kharitonova MV, Iezhitsa IN, Spasov AA. Magnesium deficiency and oxidative stress: an update. Biomed. 2016;6:8–14. doi: 10.7603/s40681-016-0020-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zulema Gaspar A, Gasser P, Flammer J. The influence of magnesium on visual field and peripheral vasospasm in glaucoma. Ophthalmologica. 1995;209(1):11–13. doi: 10.1159/000310566. [DOI] [PubMed] [Google Scholar]