Abstract
Background:
The health and well-being of students in recovery from substance use disorder are increasingly being recognized as a priority on college campuses. This scoping review maps the state of the existing literature evaluating collegiate recovery programming to highlight research gaps and inform policy.
Method:
We conducted a systematic search of articles related to collegiate recovery programming published before August 2020. The 15 extracted study characteristics included publication type, study design, primary outcomes, reporting of behavioral addictions, mutual-help group attendance, sample demographic information, school size, ownership, and funding source.
Results:
The PRISMA-guided search strategy identified 357 articles for abstract review; of 113 articles retained for full-text review, 54 studies met criteria for inclusion. Primary outcomes were coded into four domains: clinical, recovery experience, program characterization, and stigma. Most (57%) used quantitative observational designs and 41% employed qualitative research designs. Government or foundation grants funded 11% of the studies.
Conclusion:
The domains identified offer a framework for healthcare providers, college administrators, and researchers to understand and improve programs, thereby better serving this vulnerable student group.
Keywords: collegiate recovery program, scoping review, college students, substance use disorder
1.0. Introduction
Approximately 600,000 college students describe themselves as in recovery from an alcohol and/or other drug use disorder (ACHA-NCHA II, 2019; National Center for Education Statistics, 2017; Substance Abuse and Mental Health Services Administration, 2019). Colleges and universities are beginning to provide support services intended to improve health and educational outcomes among this student population (Reed, Almaguer-botero, Grizzell, & Watts, 2020). Collegiate recovery programs (CRPs) create a recovery-friendly campus environment through peer support, on-campus mutual-help meetings, recovery/sober housing, alcohol/drug-free events, counseling staff, and dedicated student drop-in centers (Bugbee, Caldeira, Soong, Vincent, & Arria, 2016).
CRPs are built on three critical foundations: the need for continuing care of substance use disorders (SUDs), the importance of recovery-oriented systems of care (ROSC), and the value of peer-recovery support services. Continuing care refers to the recovery stage of healing and may include individual check-ups as well as mutual-help meetings and involvement in drug-free social events (Laitman, Kachur-Karavites, & Stewart, 2014). ROSCs are a framework for coordinating multiple systems, services, and supports that are person-centered and designed to readily adjust to meet the individual’s needs and chosen pathway to recovery (Kaplan, 2008). ROSC staff and health care professionals are increasingly emphasizing expanded peer support for individuals with SUD (Tracy & Wallace, 2016). CRPs are one venue where peer support services are being implemented, via both peer recovery coaching and recovery housing support services (Laudet & Humphreys, 2013).
The rapidly growing and novel resource of CRPs has attracted surprisingly little research interest, despite intense national concern about substance use on college campuses. Examining health and related outcomes for students in recovery is important for at least three reasons. First, lowering the risk for relapse on campus may lead to better continuous enrollment outcomes among students (Arria et al., 2013). Second, embracing students in recovery on campus helps normalize substance-free lifestyles, which can have radiating benefits to colleges. Lastly, understanding the unique health needs of students in recovery may allow colleges and universities to design programming that will be responsive to the healthcare and educational needs of this student group.
Brown University founded the first CRP in 1977 (Hennessy, Tanner‐Smith, Finch, Sathe, & Kugley, 2018; White & Finch, 2006). Soon after, Rutgers University, Texas Tech University, and Augsburg University initiated their own CRPs which included a mix of institutional programming, housing support, and clinical services for college students in SUD recovery (Botzet, Winters, & Fahnhorst, 2008; Cleveland, Harris, Baker, Herbert, & Dean, 2007; Laitman & Lederman, 2008). A more recent burst in CRP programming coincided with the 2005 release of a Texas Tech University/SAMHSA-authored guide designed to help students, college health workers, college administrators, and other professionals initiate programs across the US (Harris, Kimball, Casiraghi, & Maison, 2014). Today there are 138 CRPs in 40 states (Association for Recovery in Higher Education, 2020), each with its own programming and recovery community. CRPs exist at 4-year public and private institutions, and serve both undergraduate and graduate students (Laudet, Harris, Kimball, Winters, & Moberg, 2015). Though there is not an agreed-upon definition regarding recovery (Ashford, Brown, et al., 2019; Witkiewitz, Montes, Schwebel, & Tucker, 2020), the association representing CRPs, the Association for Recovery in Higher Education (ARHE), identifies abstinence-based recovery as a best-practices standard (Association for Recovery in Higher Education, 2020), while also recognizing that there are multiple pathways, some of which may not include abstinence (i.e., harm reduction, moderation). The studies included in this review examined both abstinence-based recovery and non-abstinence-based recovery.
College student substance use has long been identified as a strong indicator of adverse educational and public health outcomes (Musgrave-Marquart, Bromley, & Dalley, 1997; Substance Abuse and Mental Health Services Administration [SAMHSA], 2017). College students in recovery from SUD typically encounter a cultural milieu of excessive alcohol/drug consumption in which choosing between sustaining a program of recovery and a degree in higher education can be a dangerous, and sometimes life-threatening, decision. Specific challenges can include stigma, university assigned housing, media messaging, and binge alcohol use by peers. By offering accommodating services combined with a community supportive of recovery, CRPs may reduce the risk for relapse and reinforce and enhance remission rates and recovery. Notably, though SUD treatment facilities for college students address clinical symptomatology specifically, CRPs may be uniquely situated to address other recovery-related needs including resources for social support, spirituality, and mutual-help affiliation, collectively referred to as recovery capital (Laudet & White, 2008; Terrion, 2013; Vilsaint et al., 2017).
1.1. Prior reviews on CRPs and Study Aims
Early CRP reviews focused primarily on post-SUD treatment considerations (Morgan & Cavendish, 1988) and the recovery high school movement (White and Finch, 2006). More recent literature reviews have focused on how CRPs fit into the ROSC model (Bugbee et al., 2016; Harris, Baker, Kimball, & Shumway, 2008; Laudet, Harris, Kimball, Winters, & Moberg, 2014) and how CRPs help students succeed (Brown, Ashford, Heller, Whitney, & Kimball, 2018; Reed et al., 2020); however, none of these reviews were systematic. The two systematic reviews completed did not report any quantitative findings related to CRPs (Ashford et al., 2018b; Hennessy et al., 2018). One was a combined report (high school and college) on recovery schools, and though at least one controlled trial had been conducted and reported on recovery high schools (Finch, Moberg, & Krupp, 2014), no outcomes from controlled trials were found or reported on for CRPs (Hennessy et al., 2018). A second review paper reported major CRP themes identified from a meta-synthesis of qualitative findings (Ashford, Brown, Eisenhart, et al., 2018). The lack of controlled trials necessary for a systematic review in combination with the wide range of studies reporting CRP-related outcomes necessitates this scoping review.
Though there are previous descriptive reviews on collegiate recovery programming (e.g., Bugbee et al., 2016; Depue & Hagedorn, 2015; Laudet, Harris, Kimball, Winters, & Moberg, 2014), this is the first scoping review. As noted in Arksey and O’Malley (2005), scoping reviews are distinguishable due to their comprehensiveness and attendant ability to identify gaps in the literature and to inform policy. Scoping reviews provide a “lay of the land” of the research in an area of study, often without consideration of research quality (Daudt, van Mossel, & Scott, 2013; Levac, Colquhoun, & O’Brien, 2010). Conversely, systematic reviews provide a specific answer to a research question from a narrow range of quality-assessed studies. Following Arksey and O’Malley (2005), the purposes of this review were to identify the initial research question, search for relevant studies, select studies, chart the data, and collate, summarize and report the studies utilized in the review. Lastly, the review aimed to identify gaps in the research to be addressed in future investigations. The findings will be important for guiding policy and practice as they relate to college students in recovery at institutions of higher education. The reviewed literature will serve as a resource for CRP directors, college healthcare providers, college administrators, researchers, and other professionals who work with students in SUD recovery.
2.0. Methods
2.1. Data Sources and Searches
We conducted a scoping review to answer the following research question: “What is known from the existing literature about SUD recovery programming in higher education?” In adherence to guidelines for scoping reviews (Peters et al., 2015) and Preferred Reporting of Items for Systematic Reviews and Meta-Analyses (PRISMA) procedures (Moher, Liberati, Tetzlaff, & Altman, 2009), we developed a search scheme to identify articles related to collegiate recovery programming. Three online databases were searched–PsycInfo, PubMed, and Web of Science–using search terms including substance use, college, student, and recovery (See Appendix A for a full list of search strings) on July 8, 2020. Restrictions were not imposed based on dates, languages, or article types. To identify any further articles not located through these databases, we manually searched through relevant references, contacted experts in the field, and set up alerts on Google Scholar to notify us when any relevant new research was made available, concluding the search on August 14, 2020.
2.2. Study Selection
Figure 1 outlines the process of article selection utilizing the PRISMA guidelines (Moher et al., 2009). We excluded studies that did not focus on college students in recovery and studies that did not generate any definitive quantitative or qualitative results (outcomes given in numbers, percentages, or reporting common themes) regarding collegiate recovery programs or college students in recovery from substance use disorder (self-reported or diagnosed). Also excluded were systematic reviews, literature reviews, and book reviews. Case reports and case studies were generally excluded except for one study with rigorous experimental design and comprehensive results. One study, written in Spanish, examined counseling interventions among post-treatment college students in Mexico and was excluded because it was not recovery-focused. Finally, we examined all studies for the potential of duplicate results and eliminated any articles reporting findings on identical data. There were two instances of duplicate reporting: a dissertation later published as a book chapter (Cleveland, Harris, & Wiebe, 2010) and a chapter in the same book later published in a peer-reviewed journal (Cleveland & Harris, 2010b). Publicly available theses and dissertations were included but other unpublished works were not considered.
Figure 1.
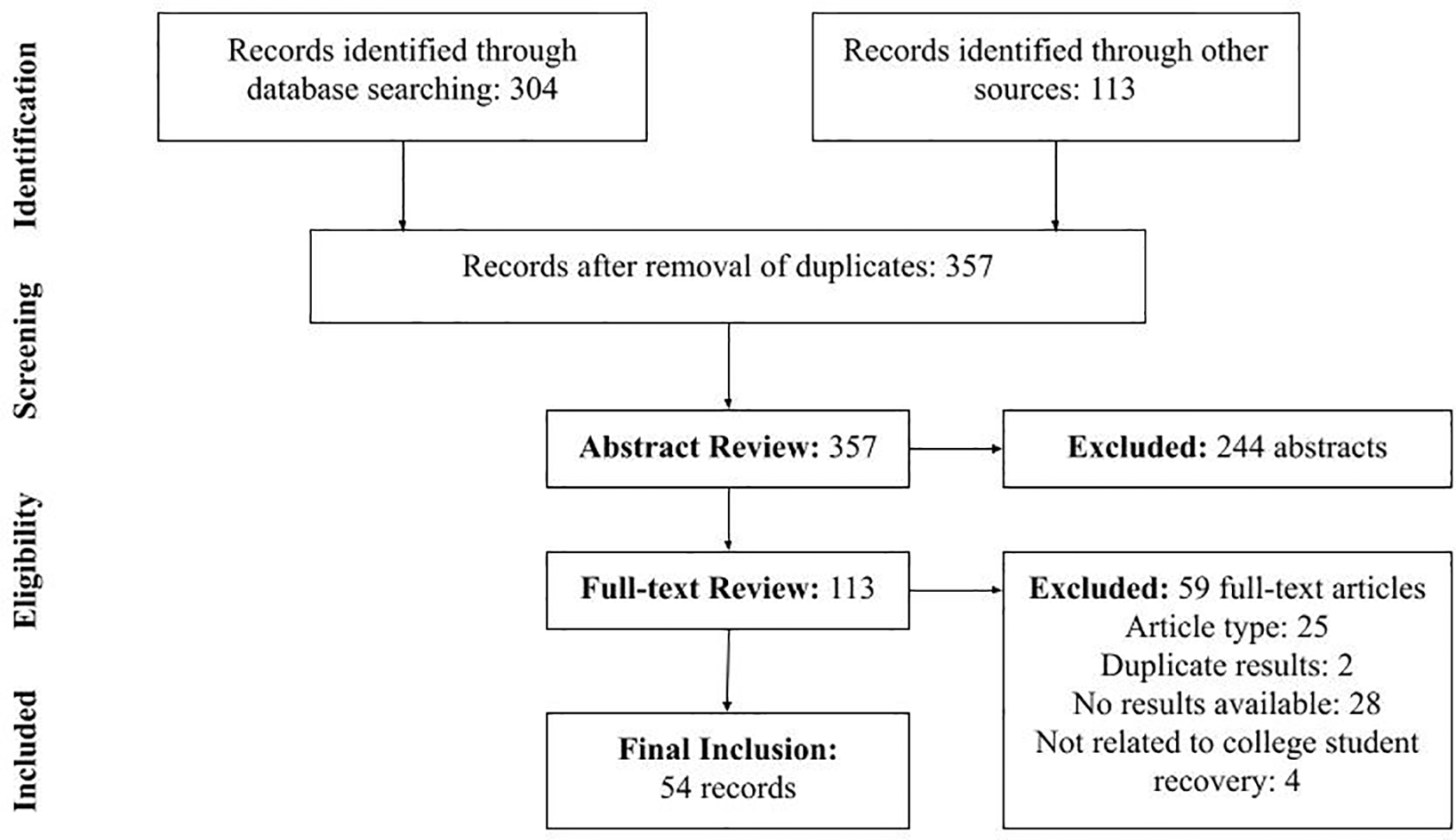
PRISMA flow chart
After any duplicate articles were removed, two researchers (NV, MR) independently reviewed all abstracts against the eligibility criteria. To be eligible, the abstract had to be (a) recovery-oriented (i.e., programming or services related to SUD recovery), and (b) focused on college students. Though we presumed that many of the studies would be focused on CRPs specifically, we did not limit the potential for non-CRP-related findings so that we could report on the full breadth of research pertaining to college students in recovery. Any dispute was resolved through discussion. Full-text articles were then obtained for all included abstracts and subsequently independently reviewed by two researchers (NV, MR). Articles that focused on college students in recovery, or recovery programming on college campuses, and reported thorough quantitative or qualitative results (outcomes given in numbers, percentages, or reporting themes) were included. To check for reliability and consistency, each researcher examined all of the articles separately and then charted the data individually using Microsoft Excel. The researchers then came together to identify any discrepancies between their spreadsheets (approximately 10 discrepancies [1.2%] were identified). Again, any disagreements were resolved through discussion between the researchers, and in the sole case that agreement was not attained, the senior author (KH) was brought in for resolution (Levac et al., 2010).
2.3. Data Extraction
For each included study, two researchers (NV & MR) independently extracted 15 study characteristics. Characteristics were initially based on those used in previous studies (e.g., study design, participants’ gender) and added to and refined (e.g., participants’ sexual orientation and behavioral addictions) using the iterative model presented in Arksey and O’Malley (2005). The final characteristics were (1) participant category (i.e., college student, college administrator, CRP Alumni, CRP director), (2, 3, 4) reporting of gender, race, and sexual orientation, (5) school size, (6) public or private school, (7) reporting of mutual-help group attendance (e.g., Alcoholics Anonymous, Narcotics Anonymous, SMART Recovery, All Recovery, and other 12-step/alternative to 12-step recovery groups), (8) reporting of behavioral addictions, (9) primary outcomes, (10) publication type (i.e., journal article, theses/dissertation, book chapter, case study), (11) year, (12) number of participants, (13) study design/statistical approach, (14) Institutional Review Board (IRB) approval, and (15) study funding source. We did not set out to systematically rate study quality as a data point, but IRB approval and external funding may be viewed as crude proxies for study quality. This is consistent with current scoping methods (Daudt et al., 2013). Studies that reported an IRB exemption (n=2) were considered to have attained IRB approval.
2.4. Data Synthesis and Analysis
The scoping review summarized and categorized articles across these 15 characteristics. It provides an overview of the literature without evaluation of article bias or research rigor. During the iterative review process, we found primary outcomes fell into four major domains: clinical, recovery experience (students in recovery answered open-ended questions regarding their experiences), program characterization, and non-clinical student outcomes.
3.0. Results
The initial search revealed 357 articles for abstract review, 244 of which were excluded after examination (Figure 1). After separately reviewing the full texts of the remaining 113 articles, NV and MR collectively identified 54 studies for final inclusion and excluded 59. A list of the articles excluded and the reason for exclusion are provided in Appendix B. Table 1 offers a detailed summary of study characteristics. All of the included articles are listed in Table 2 and categorized by CRP primary outcome domain/category. The largest domains examined clinical outcomes (19/54, 35%) and recovery experiences (15/54, 28%) of college students in recovery. Most studies were published as journal articles (32/54, 59%) or dissertations/theses (17/54, 31%), with four book chapters and one case study. There were 12 studies published prior to 2010, 11 studies published from 2010 to 2015, and 31 studies published after 2015.
Table 1.
Description of included studies (n=54).
| Study Variable | Number of Studies (%) |
|---|---|
| Study Participants | |
| College students | 40 (74%) |
| College Administrators | 2 (4%) |
| CRP Alumni | 3 (5%) |
| CRP Directors | 1 (2%) |
| CRP Costs | 1 (2%) |
| Multiple Participant Groups | 7 (13%) |
| Characteristics of College Student Studies | |
| Basic Demographics | |
| Gender Reported* | 34 (85%) |
| Race/Ethnicity Reported* | 30 (75%) |
| Sexual Orientation Reported* | 3 (8%) |
| Research Settings | |
| University Size | |
| Large (10,000+) | 21 (39%) |
| Medium (2,000 to 10,000) | 9 (16%) |
| Small (less than 2,000) | 2 (4%) |
| Community College | 1 (2%) |
| Not applicable or Not Reported | 21 (39%) |
| University Type | |
| Public | 30 (55%) |
| Private | 2 (4%) |
| Not Applicable or Not Reported | 22 (41%) |
| Mutual-help Participation Reported | |
| Yes | 20 (37%) |
| Not Applicable or Not Reported | 34 (63%) |
| Behavioral Addictions Reported | |
| Eating | 6 (10%) |
| Gambling | 2 (4%) |
| Other (Including Internet/Gaming) | 3 (6%) |
| Not Applicable or Not Reported | 43 (80%) |
Note.
n=40 College Student Studies only.
Table 2.
Recovery programming primary outcome domains/categories.
3.0.1. Study designs
We offer a full reporting of the study design, primary outcome domain, number of participants, and IRB approval status in Figure 2. The scoping review identified one randomized controlled trial. However, this study did not randomize on CRP participation; rather all study participants were CRP students and were randomized into a biofeedback control and treatment condition to evaluate levels of craving (Eddie et al., 2018). The majority of studies in this scoping review used a quantitative observational design (31/54, 57%), that is, did not manipulate an independent variable. The remaining studies used a qualitative design (22/54, 41%).
Figure 2.
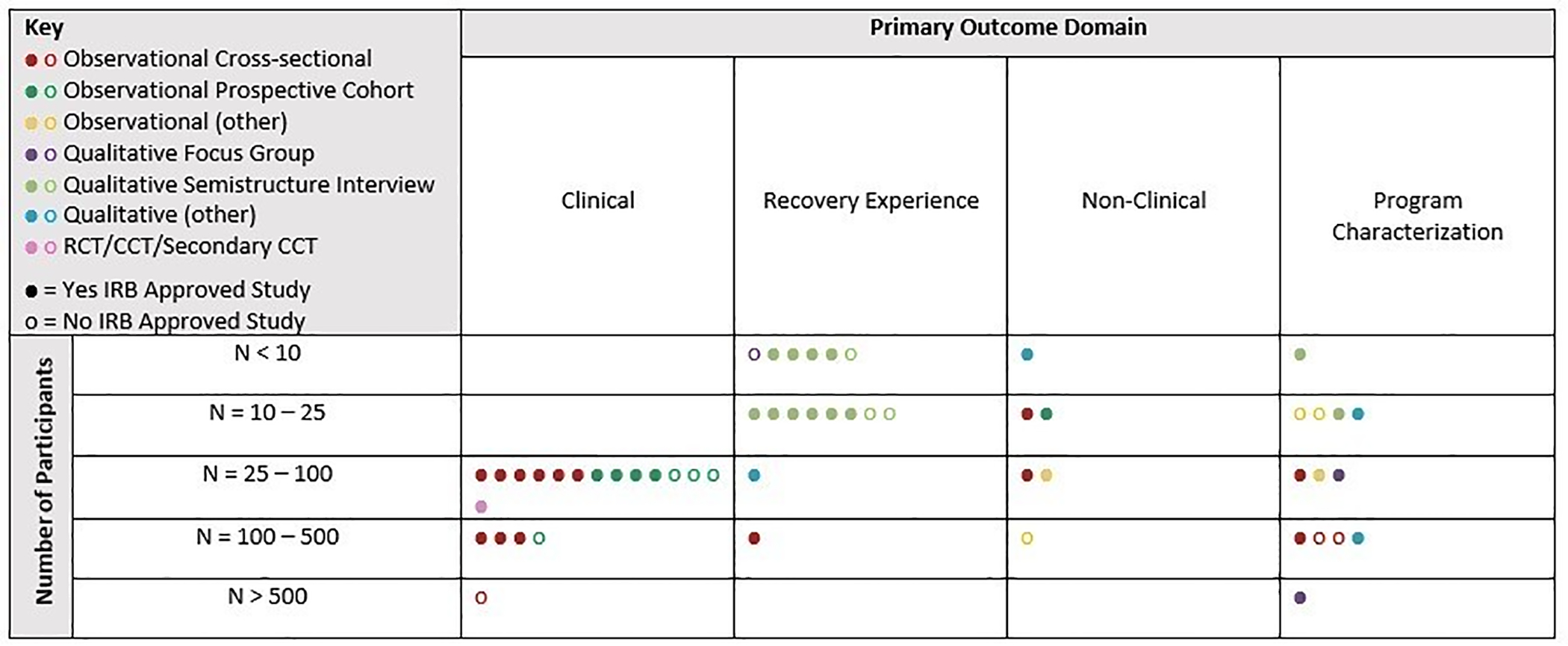
Studies charted on outcome, participants, design, and IRB status.
3.0.2. Funding source
Fifty-nine percent of studies either did not report whether they had funding (32/54) or reported that they were unfunded (7/54, 13%). When reported, funding was most often obtained from internal university funding sources (5/54, 9%) and philanthropic sources (4/54, 7%). Few studies reported government funding sources (6/54, 11%1), with two from the National Institute on Drug Abuse (NIDA - though these were from the same grant), one from the National Institute on Alcohol Abuse and Alcoholism (NIAAA), one from the Substance Abuse and Mental Health Services Administration (SAMHSA), and two from “other government” funding sources.
3.1. Primary outcome domain summaries
3.1.1. Recovery experience
Recovery experience refers to studies in which students answered open-ended questions about their lived experiences in recovery. Studies with the outcome of recovery experience that were qualitative designs and coded information collected in semi-structured interviews to identify themes reported among CRP students were identified (16/54, 30%) in the review (Bell et al., 2009; Iarussi, 2018; Kollath-Cattano et al., 2018; Terrion, 2013; Walker, 2017; Whitney, 2018; Woodford, 2001; Workman, 2020). A qualitative study using focus groups identified needs specific to students in recovery on campus (Worfler, 2016). Further studies of lived experience in recovery investigated themes among CRP alumni (Lovett, 2015), recovery discourses (Whitney, 2018), the role of recovery identities among CRP members (Hoffman, 2020), and what made student recovery possible (Washburn, 2016). Lastly, some studies examined why students joined a CRP (Harris et al., 2014; Laudet, Harris, Kimball, Winters, & Moberg, 2016). Reasons for joining a CRP included wanting a supportive network of peers, having a safe space on campus to deal with stress, and desiring to help others in their recovery.
3.1.2. Clinical
Studies were coded as clinical (19/54, 35%) if the primary outcome was determined to be part of the six American Society of Addiction Medicine criteria which include withdrawal potential, biomedical conditions, mental health, readiness to change, relapse/continued use, and recovery environment (Rastegar & Fingerhood, 2015). As would be expected, over a third (8/19, 42%) of the studies examining clinical outcomes looked specifically at substance use or abstinence. The majority of these studies were cross-sectional observational (10/19, 53%) research designs. Most examined current college students in recovery, though one study examined CRP alumni (Brown et al., 2019). Studies reporting relapse (return to use) found that 2.2% of current CRP students at a Midwestern university had returned to harmful use of alcohol or other drugs after six months in the program (Botzet et al. (2008), a 4.4% return to use rate at a university in Texas (Botzet et al. (2008), and that 10.2% of CRP alumni had returned to use since college graduation in a national sample (Brown et al. (2019). A study examining craving found that a subset of students in recovery displayed cascading negative affect that compounded levels of craving over several days (Zheng, Wiebe, Cleveland, Molenaar, & Harris (2013). Other craving studies found that facets of the 12-steps (action steps and everyday steps) were differentially associated with changes in craving (Wiebe, Griffin, Zheng, Harris, & Cleveland, 2018) and that heart rate variability biofeedback as an adjunct for students in recovery produced reduced levels of craving when compared to a waitlist control condition (Eddie, Conway, Alayan, Buckman, & Bates, 2018). Other clinical outcomes included recovery-related social support (J. A. Smith et al., 2018), coping with temptations (Wiebe, Cleveland, & Dean, 2010), disordered eating (Ashford, Wheeler, & Brown, 2019), and multiple medical/mental health conditions (Shumway, Bradshaw, Harris, & Baker, 2013; Watts, Tu, & O’Sullivan, 2019).
3.1.3. Non-clinical student outcomes
In 11% of the studies, primary outcomes were non-clinical in nature (6/54). These included academic performance (Moore, 1999), vocational expectations (Watts, Tu, et al., 2019), nutrition education (Wattick, Hagedorn, & Olfert, 2019), and reductions in stigma (Beeson et al., 2019; Gueci, 2018b). Five studies had qualitative designs and two had quantitative designs in the non-clinical domain.
3.1.4. Program characterization
About a quarter of the studies (13/54, 24%) examined the program characteristics of CRPs. Although some aimed to demonstrate the importance of the CRP as an essential resource on campus (Carlson, 2018; Watts, Chowdhury, & Holloway, 2019), others aimed to provide basic and program-specific information (Ashford, Brown, & Curtis, 2018; Beeson, Whitney, & Peterson, 2017; Gueci, 2018a). Study designs were a mix of qualitative and observational.
3.2. General findings
3.2.1. Evidence regarding the Efficacy of CRPs
Though there may be evidence regarding the essential components of recovery programming in research on adult populations, how those components operate specifically among college students has not been effectively evaluated in randomized trials. Hence, based on the available correlational results, it appears that a blending of evidence-based interventions including recovery housing (Jason & Ferrari, 2010), peer recovery supports (Laudet & Humphreys, 2013), continuing care treatment programming (McKay, 2009), and mutual-help group (Kelly, Humphreys, & Ferri, 2020) facilitation may be driving the rapid growth of CRPs nationwide. These evidence-based components in other contexts are commonly referred to as “active ingredients” or essential components of an intervention to promote recovery (Brownson, Fielding, & Maylahn, 2009). Similarly, the ARHE has recently identified CRP “best practices” such as peer recovery supports, student drop-in centers, and a full offering of mutual-help groups (ARHE, 2020). The proportion of CRPs that follows AHRE best practices or the presence of other evidence-based practices not identified by AHRE is currently unknown. The growth of CRPs in the past 15 years and available evidence points to the utility of CRP best practices, but without a clear understanding across multiple contexts, it may be difficult to formulate standardized interventions.
The multi-component nature of CRPs raises challenges for conducting comprehensive RCTs. Additionally, self-selection bias (e.g., students more motivated to change also may be more motivated to engage in CRPs) may cast doubt on CRP studies shown to improve student outcomes. This limitation has been overcome in adult studies on 12-step mutual-help organizations (Humphreys et al., 2020), and perhaps could also be handled in CRP research; for example, through studies that randomize arriving students to receive or not receive a tailored welcoming intervention to a CRP. Future studies could also exploit the exogeneity in availability (e.g., schools with and without CRPs) or using propensity score matching to evaluate CRP effectiveness while addressing the risk of selection bias. Future evaluations will also have to take account of the fact that CRPs attract current students interested in recovery as well as individuals in sustained recovery back to college. This potentially confounding developmental difference in students should be accounted for in future studies.
Though CRP research is still in its infancy, observational evidence suggests that programming for college students in recovery may be successful in helping students and CRP alumni to sustain abstinence (Bennett, McCrady, Keller, & Paulus, 1996; Botzet et al., 2008; Brown et al., 2019; Cleveland et al., 2007; Laudet et al., 2015). In addition, CRP participation’s association with higher GPA (3.2 for CRP students compared to 2.9 overall at Texas Tech University), retention in school, and graduation rate among students in recovery, compared to the general student population at the same schools, offers some moderate evidence of CRP efficacy in educational attainment (Ashford, Brown, & Curtis, 2018; Botzet et al., 2008; H. H. Cleveland et al., 2007; Harris et al., 2008; Moore, 1999; Watts, Tu, et al., 2019). Lastly, sobriety-related social support was associated with reduced alcohol and other drug-related cravings among CRP students (Cleveland & Harris, 2010a, 2010b; Wiebe et al., 2018; Zheng et al., 2013). These observational findings need replication but have encouraging implications for college administrators and researchers. For example, integrating interventions aimed at increasing social support for non-drinking lifestyles (e.g., sober tailgates and substance-free social outings) among students both in and not in recovery has the potential to create a safer campus environment for students, staff, and faculty.
Mutual-help group participation was reported in 37% of the studies. Because mutual-help (12-step and 12-step alternative programs) is effective among the general population (Kaskutas, 2009; Kelly et al., 2020; Timko, Cronkite, McKellar, Zemore, & Moos, 2013; Zemore, Lui, Mericle, Hemberg, & Kaskutas, 2018) and emerging adults (Bergman, Kelly, Fallah-Sohy, & Makhani, 2018; Kelly, Stout, & Slaymaker, 2013), the limited number of manuscripts reporting this data point suggests that mutual-help participation data should be gathered in all future CRP studies. Non-substance-related addictive behaviors (i.e., gaming/internet, sex, food, gambling) were recorded in 11/54 studies despite their high co-morbidity with SUDs (Cohen et al., 2010; Laudet et al., 2015), and the recent focus of examining these conditions in combination among CRP students (Ashford, Wheeler, et al., 2019; Monsour, Kimball, & Hensley, 2020). Future research should aim to record information on behavioral addictions among all CRP students.
3.2.2. Qualitative research
Common themes reported among qualitative studies of CRPs included the importance of on-campus mutual-help meetings (Whitney, 2018), the role of the student-drop-in center (Ashford, Brown, Eisenhart, et al., 2018), and the value of community and social support among CRP students (Harris et al., 2014). Likewise, other qualitative investigations looked at themes related to the importance of CRP seminars and addiction education programming (Bell et al., 2009; Casiraghi & Mulsow, 2010), managing emotions (Lovett, 2015), academic success (Terrion, 2013), enhancing overall wellness (Iarussi, 2018), and recovery housing and diversity in CRP programs (Woodford, 2001). These findings should act as a springboard for new quantitative research projects to further examine these themes.
3.2.3. Stigma
Research on stigma surrounding substance use disorder as it relates to college students was the primary focus of three studies (6%). One found that CRP-related “recovery ally” trainings to help faculty, staff and students learn how to support people in recovery reduced stigma and improved self-reported ally-related behaviors (i.e., use inclusive language, make others aware of CRP) (Beeson et al., 2019). A second study found that these trainings increased empathy for students in recovery among student allies (Gueci, 2018a). The final stigma-related study used a unique methodology incorporating photographs to capture common themes to identify sources and consequences of stigma among students in a CRP (Spencer, 2017). Sources of stigma included discrimination and expectation of rejection. Consequences of stigma included loneliness, isolation, and fear of missing out. Future studies should not only examine the personal experiences of stigma but also the overall level of stigma toward individuals with SUD among all students at schools with and without CRPs. These findings on school-level stigma may provide policy recommendations for school administrators and lawmakers contemplating CRP implementation at the university and state level.
4.0. Discussion
This scoping review summarizes the research literature regarding college student substance use disorder recovery-related programming. Nearly all of the studies to date have used either observational or qualitative research designs. Like many other emergent literatures, randomized clinical trials generating efficacy estimates are rare in the CRP literature. Sample sizes were generally small. Nearly one-quarter of the studies did not report IRB approval, though some of these may have had such approval. Extramural funding was scarce among CRP investigations with 11% reporting investment from a National Institute of Health funding organization, foundations, or other government funders. The lack of international studies on programming relating to university students in recovery suggests that CRPs may not be flourishing at the same rate in countries outside the US. Alternatively, the gap in literature could be due to a lack of interest in CRPs from international researchers or an English-language bias in CRP-related international studies. This highlights the need for future projects to determine the number of CRPs operating outside the US (programs have been identified at the University of Windsor in Canada and the University of Teesside in the United Kingdom) and how they may differ in scope, funding, and effectiveness.
4.1. Knowledge gaps and informing policy, practice, and research
This scoping review identified numerous gaps in the CRP literature. Notably, there is a lack of controlled trials (on CRPs and their best practices/active ingredients) and implementation science research designs. Other important gaps in the literature included a lack of research on sociodemographic differences among students in CRPs, racial disparities among students in CRPs, and community college programming. Simply understanding how many CRP programs are currently operating and basic programming information would be a step forward for research in this area. Though we did not implement a data point for studies examining CRP participants with co-occurring conditions and criminal justice involvement, a lack of studies in these areas was apparent. Additionally, conceptual models were seldom applied to inform research design and data collection. Remedying these gaps is an important next step in this area of inquiry.
4.1.1. Controlled trials and implementation science studies
As noted, there has been one randomized controlled trial including CRP students to date. This likely reflects the practical challenges of conducting such studies as well as the lack of funding for them (e.g., from NIH). The lone NIH-funded study aimed specifically at college students in recovery is now more than 7 years old and was not a controlled trial (Laudet et al., 2015, 2016; Laudet, Harris, Winters, Moberg, & Kimball, 2014; Laudet et al., 2014). Research funders have an important role to play in providing support for identifying the most effective elements of CRPs and understanding of the recovery phase of SUD among college students.
Implementation science, the study of methods to promote the systematic uptake of research findings and other evidence-based practices, also seeks to increase the use of scientific findings to enhance routine practice and improve the quality and effectiveness of health services (Eccles & Mittman, 2006). Colleges represent a unique context in which to conduct implementation research due to their differing models of leadership, school year calendar, and student culture, and the diversity of students and staff (Owens et al., 2014). Likewise, colleges themselves may be influenced by the local community, alumni, the U.S. Department of Education, and funding at state and federal levels (Clotfelter, 2003; Jongbloed & Vossensteyn, 2016). Unfortunately, these contexts through which universities operate often do not necessarily work in harmony to support implementation of SUD recovery programming (Harris et al., 2014). For example, school administrators may denounce CRPs in an effort to avoid public admission that a drug or alcohol problem exists on campus. The first step of determining the implementation strategy for CRPs is identifying a framework to guide data collection, analyses, and interpretation such that contextual factors can be identified and studied. Hence, implementation science investigations are needed to identify barriers and facilitators to the implementation of CRP best practices using well-validated frameworks (i.e., Consolidated Framework for Implementation Research [CFIR] or Reach Effectiveness Adoption Implementation Maintenance [RE-AIM]). The final step would be a Hybrid Type 2 effectiveness and implementation study (Curran, Bauer, Mittman, Pyne, & Stetler, 2012) to examine CRP implementation outcomes while continuing to examine the effectiveness of CRP best practices. The hybrid design would involve program selection at the school level and measurement of key uptake variables such as reach, retention, adoption, and fidelity while also examining key student outcomes (as an RCT does) such as GPA and relapse.
4.1.2. Sociodemographic differences, racial disparities, and gender differences
This scoping review exposed a lack of research on underserved student groups and highlights the need to know more about CRP students of color, women students, and low-income and first-generation students. We found no articles examining differences between socio-economic groups, though one study reported that one-third of students had experienced homelessness in their lifetime (Laudet et al., 2015). In addition, 25% of the studies did not report CRP participants’ racial/ethnic background, and none examined racial disparities or racial differences on any outcomes. One study focused specifically on women (Walker, 2017) and one examined sex differences (J. A. Smith et al., 2018). Though most studies (85%) reported gender, 15% of the studies did not, and two studies reported the number of transgender/non-binary students (Carlson, 2018; Watts, Tu, et al., 2019). Likewise, three studies reported student sexual orientation (Ashford, Brown, & Curtis, 2018; Ashford, Wheeler, et al., 2019; Watts, Tu, et al., 2019). To inform college healthcare providers and policy, research is needed on these underrepresented students in terms of their use and outcomes of CRP participation. These findings would provide guidance on the unique programming needs and inform tailored intervention programs for these underserved student populations.
4.1.3. Co-occurring conditions and criminal justice involvement
Though the evidence is preliminary, it appears that co-occurring conditions (mental health disorders and multiple SUDs) are the norm among CRP participants. In connection with the findings presented on non-substance focused addictive behaviors, multiple studies have documented a relationship between SUD and eating disorders (Ashford et al., 2019; Laudet et al., 2015), SUD and other mental health conditions (Ashford, Brown, & Curtis, 2018; Laudet et al., 2015; Odefemi-Azzan, 2020), and poly-substance use disorders (more than one reported SUD - Cleveland et al., 2007; Laudet et al., 2015). How these conditions shape CRP involvement or influence recovery-related outcomes will be vital for future research to investigate.
Findings of a high level of previous criminal justice involvement (58%−66%) among CRP members (Cleveland et al., 2007; Laudet et al., 2015) have implications for both CRP and criminal justice system researchers. First, among CRP researchers, investigations are warranted into internal processes among students that lead to engagement in CRPs and desistance from criminal activity. Second, the cost savings associated with desistance from the criminal justice system among these students deserves attention. Relatedly, research examining the effectiveness of reallocation of resources from the criminal justice system into CRPs should be prioritized.
4.1.4. Conceptual models
Studies that implemented a conceptual model to guide findings used a systems-based community approach (Harris et al., 2008), the continuum of care model to treat addiction (Laitman et al., 2014; Laitman & Lederman, 2008), an integrated behavioral health model to treat mental health disorders that co-occur with SUD (Ashford, Brown, & Curtis, 2018), a recovery model specifically for community colleges (DiRosa & Scoles, 2020), and a socio-economic model that categorizes CRPs into outcomes at the individual, interpersonal, organizational, and community levels (Beeson et al., 2017). Unfortunately, none of these models comprehensively conceptualize CRP programming. Because CRPs can draw from research in different disciplines, including criminal justice, public health, and education, and each discipline has its own models and preferred outcomes (i.e., recidivism, relapse, retention), it would be helpful to create a socioecological model of CRP outcomes to guide future research.
5.0. Limitations
We did not review the quality of the studies included or investigate the research methods for potential bias; thus, we are limited in the conclusions we can draw. Though we intended to review a large amount of the literature with broader inclusion criteria than the previous systematic review (Hennessy et al., 2018), the decision not to specifically evaluate or limit inclusion based upon study quality likely influenced interpretation. This review was also limited by the amount of research available, an English language bias in science, and the focus on predominately large public universities in North America. Lastly, we recorded mutual-help attendance as an all-encompassing data point for 12-step programs and alternatives such as SMART Recovery and Celebrate Recovery. Future reviews may further delineate among the different types of mutual-help groups.
6.0. Conclusions
This scoping review mapped the lay of the land in research on collegiate recovery programming. The studies included in the review are intended to provide an expansive overview of the literature and add to the general understanding of students in recovery from SUD (self-reported and diagnosed). The review identified gaps in research on programming for students in recovery and highlighted areas for future inquiry. The available evidence on CRPs is minimal when compared to the extensive literature base on prevention and reduction of substance use on college campuses. Given such a disparity and the growing need for recovery-oriented services on college campuses, evaluations of CRP effectiveness are needed. The domains identified in this review offer a potential framework for healthcare providers and researchers and will help to inform policy and practice to improve outcomes for this underserved student group.
Supplementary Material
Highlights:
A scoping review of collegiate recovery programming in the U.S.
The review identified four sub-groups of relevant primary outcomes
Across studies, programs improved relapse, educational, and social support outcomes
Government and foundation funded research was infrequent in the literature
Research is needed, particularly prospective cohort and matching trials
Role of Funding Source:
Noel Vest was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number T32DA035165. In addition, this research was supported by a Senior Research Career Scientist Awards (RCS 00-001 to Dr. Timko; RCS 14-141 to Dr. Humphreys) from the Department of Veterans Affairs (VA) Health Services Research and Development (HSR&D) Service. Dr. Kelly reported funding from the National Institute on Alcohol Abuse and Alcoholism under award K24AA022136. The views expressed are the authors’ and do not necessarily reflect the official position of any government agency.
Footnotes
Note that percentages may not add to 100% due to rounding error.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- ACHA-NCHA II. (2019). Undergaduate Student Reference Group Data Report Spring 2019. American College Health Association, 1–60. Retrieved from https://www.acha.org/documents/ncha/NCHA-II_SPRING_2019_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf [Google Scholar]
- Arksey H, & O’Malley L (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology: Theory and Practice. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Arria AM, Caldeira KM, Vincent KB, Winick ER, Baron RA, & O’Grady KE (2013). Discontinuous college enrollment: Associations with substance use and mental health. Psychiatric Services, 64(2), 165–172. 10.1176/appi.ps.201200106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashford RD, Brown A, Brown T, Callis J, Cleveland HH, Eisenhart E, … Whitney J (2019). Defining and operationalizing the phenomena of recovery: a working definition from the recovery science research collaborative. Addiction Research and Theory, 27(3), 179–188. 10.1080/16066359.2018.1515352 [DOI] [Google Scholar]
- Ashford RD, Brown AM, & Curtis B (2018). Collegiate Recovery Programs: The Integrated Behavioral Health Model. Alcoholism Treatment Quarterly, 36(2), 274–285. 10.1080/07347324.2017.1415176 [DOI] [Google Scholar]
- Ashford RD, Brown AM, Eisenhart E, Thompson-Heller A, & Curtis B (2018). What we know about students in recovery: meta-synthesis of collegiate recovery programs, 2000–2017. Addiction Research and Theory, 26(5), 405–413. 10.1080/16066359.2018.1425399 [DOI] [Google Scholar]
- Ashford RD, Wheeler B, & Brown AM (2019). Collegiate recovery programs and disordered eating: exploring subclinical behaviors among students in recovery. Alcoholism Treatment Quarterly, 37(1), 99–108. 10.1080/07347324.2018.1475206 [DOI] [Google Scholar]
- Association for Recovery in Higher Education. (2020). ARHE - Standards and Recommendations. Retrieved from https://collegiaterecovery.org/standards-recommendations/ [Google Scholar]
- Beeson ET, Ryding R, Peterson HM, Ansell KL, Aideyan B, & Whitney JM (2019). RecoveryZone: A Pilot Study Evaluating the Outcomes of an Online Ally Training Program. Journal of Student Affairs Research and Practice, 56(3), 284–297. 10.1080/19496591.2018.1474765 [DOI] [Google Scholar]
- Beeson ET, Whitney JM, & Peterson HM (2017). The Development of a Collegiate Recovery Program: Applying Social Cognitive Theory within a Social Ecological Framework. American Journal of Health Education, 48(4), 226–239. 10.1080/19325037.2017.1317304 [DOI] [Google Scholar]
- Bell N, Kanitkar K, Kerksiek K, Watson W, Das A, Kostina-Ritchey E, … Harris K (2009). “it has made college possible for Me”: Feedback on the impact of a university-based center for students in recovery. Journal of American College Health, 57(6), 650–658. 10.3200/JACH.57.6.650-658 [DOI] [PubMed] [Google Scholar]
- Bennett ME, McCrady BS, Keller DS, & Paulus MD (1996). An intensive program for collegiate substance abusers: Progress six months after treatment entry. Journal of Substance Abuse Treatment, 13(3), 219–225. 10.1016/S0740-5472(96)00045-1 [DOI] [PubMed] [Google Scholar]
- Bergman BG, Kelly JF, Fallah-Sohy N, & Makhani S (2018). Emerging adults, mutual-help organizations, and addiction recovery: What does the science tell us? In Smith DC (Ed.), Emerging adults and substance use disorder treatment: Developmental considerations and innovative approaches (pp. 167–195). Oxford University Press. [Google Scholar]
- Botzet AM, Winters K, & Fahnhorst T (2008). An exploratory assessment of a college substance abuse recovery program: Augsburg College’s StepUP program. Journal of Groups in Addiction and Recovery, 2(2–4), 257–270. 10.1080/15560350802081173 [DOI] [Google Scholar]
- Brown A, Ashford R, Heller AT, Whitney J, & Kimball T (2018). Collegiate Recovery Students and Programs: Literature Review from 1988–2017. Journal of Recovery Science, 1(1), 1–11. 10.31886/jors.11.2018.8 [DOI] [Google Scholar]
- Brown AM, Ashford RD, Figley N, Courson K, Curtis B, & Kimball T (2019). Alumni Characteristics of Collegiate Recovery Programs: A National Survey. Alcoholism Treatment Quarterly, 37(2), 149–162. 10.1080/07347324.2018.1437374 [DOI] [Google Scholar]
- Brownson RC, Fielding JE, & Maylahn CM (2009). Evidence-based public health: A fundamental concept for public health practice. Annual Review of Public Health, 30, 175–201. 10.1146/annurev.publhealth.031308.100134 [DOI] [PubMed] [Google Scholar]
- Bugbee BA, Kimberly Caldeira MM, Andrea Soong MM, Kathryn Vincent MB, & Amelia Arria MM (2016). Collegiate Recovery Programs: A Win-Win Proposition for Students and Colleges About the Center on Young Adult Health and Development Suggested Citation. (August). 10.13140/RG.2.2.21549.08160 [DOI] [Google Scholar]
- Carlson M (2018). RECOVERY SUPPORT SERVICES FOR YOUNG ADULTS : A NEEDS ASSESSMENT FOR A COLLEGIATE RECOVERY PROGRAM AT A MIDSIZED PUBLIC UNIVERSITY LOCATED IN SOUTHERN CALIFORNIA by. California State University, San Bernardino. [Google Scholar]
- Casiraghi AM, & Mulsow M (2010). Building Support for Recovery into an Academic Curriculum: Student Reflections on the Value of Staff Run Seminars. In Cleveland H, Harris K, & Wiebe R (Eds.), Substance abuse recovery in college: Community supported abstinence (1st ed., pp. 113–144). Boston, MA: Springer. [Google Scholar]
- Cleveland HH, & Harris K (2010a). Conversations about recovery at and away from a drop-in center among members of a collegiate recovery community. Alcoholism Treatment Quarterly, 28(1), 78–94. 10.1080/07347320903436268 [DOI] [Google Scholar]
- Cleveland HH, & Harris KS (2010b). The role of coping in moderating within-day associations between negative triggers and substance use cravings: A daily diary investigation. Addictive Behaviors, 35(1), 60–63. 10.1016/j.addbeh.2009.08.010 [DOI] [PubMed] [Google Scholar]
- Cleveland HH, Harris KS, Baker AK, Herbert R, & Dean LR (2007). Characteristics of a collegiate recovery community: Maintaining recovery in an abstinence-hostile environment. Journal of Substance Abuse Treatment, 33(1), 13–23. 10.1016/j.jsat.2006.11.005 [DOI] [PubMed] [Google Scholar]
- Cleveland HH, Harris KS, & Wiebe RP (2010). Substance Abuse Recovery in College. In Substance Abuse Recovery in College. 10.1007/978-1-4419-1767-6 [DOI] [Google Scholar]
- Clotfelter CT (2003). Alumni giving to elite private colleges and universities. Economics of Education Review. 10.1016/S0272-7757(02)00028-6 [DOI] [Google Scholar]
- Cohen LR, Greenfield SF, Gordon S, Killeen T, Jiang H, Zhang Y, & Hien D (2010). Survey of eating disorder symptoms among women in treatment for substance abuse. American Journal on Addictions. 10.1111/j.1521-0391.2010.00038.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran GM, Bauer M, Mittman B, Pyne JM, & Stetler C (2012). Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care, 50(3), 217–226. 10.1097/MLR.0b013e3182408812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daudt HM, van Mossel C, & Scott SJ (2013). Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Medical Research Methodology, 13(1), 48. 10.1186/1471-2288-13-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depue MK, & Hagedorn WB (2015). Facilitating college students’ recovery through the use of collegiate recovery programs. Journal of College Counseling, 18(1), 66–81. 10.1002/j.2161-1882.2015.00069.x [DOI] [Google Scholar]
- DiRosa F, & Scoles P (2020). The Healing Pillars of Collegiate Recovery: A Community College Model of Recovery and Education. Journal of Student Affairs Research and Practice, 57(1), 69–76. 10.1080/19496591.2019.1644116 [DOI] [Google Scholar]
- Eccles MP, & Mittman BS (2006). Welcome to Implementation Science. Implementation Science, 1(1), 1. 10.1186/1748-5908-1-1 [DOI] [Google Scholar]
- Eddie D, Conway FN, Alayan N, Buckman J, & Bates ME (2018). Assessing heart rate variability biofeedback as an adjunct to college recovery housing programs. Journal of Substance Abuse Treatment, 92(January 2018), 70–76. 10.1016/j.jsat.2018.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch AJ, Moberg DP, & Krupp AL (2014). Continuing Care in High Schools: A Descriptive Study of Recovery High School Programs. Journal of Child and Adolescent Substance Abuse, 23(2), 116–129. 10.1080/1067828X.2012.751269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gueci N (2018). Collegiate Recovery Program (CRP): Student Needs and Employee Roles. Building Healthy Academic Communities Journal, 2(2), 33. 10.18061/bhac.v2i2.6393 [DOI] [Google Scholar]
- Gueci V (2018). Recovery 101 : Providing Peer-to-Peer Support to Students in Recovery. Arizona State University. [Google Scholar]
- Harris KS, Baker AK, Kimball TG, & Shumway ST (2008). Achieving systems-based sustained recovery: A comprehensive model for collegiate recovery communities. Journal of Groups in Addiction and Recovery, 2(2–4), 220–237. 10.1080/15560350802080951 [DOI] [Google Scholar]
- Harris KS, Kimball TG, Casiraghi AM, & Maison SJ (2014). Collegiate Recovery Programs. Peabody Journal of Education, 89(2), 229–243. 10.1080/0161956X.2014.897095 [DOI] [Google Scholar]
- Hennessy EA, Tanner‐Smith EE, Finch AJ, Sathe N, & Kugley S (2018). Recovery schools for improving behavioral and academic outcomes among students in recovery from substance use disorders: a systematic review. Campbell Systematic Reviews. 10.4073/csr.2018.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman DE (2020). EXPERIENCES OF COLLEGE STUDENTS IN ADDICTION RECOVERY: A CRITICAL CASE STUDY. University of South Carolina. [Google Scholar]
- Humphreys K, Barreto NB, Alessi SM, Carroll KM, Crits-Christoph P, Donovan DM, … Wagner TH (2020). Impact of 12 step mutual help groups on drug use disorder patients across six clinical trials. Drug and Alcohol Dependence, 215, 108213. 10.1016/j.drugalcdep.2020.108213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iarussi MM (2018). The Experiences of College Students in Recovery From Substance Use Disorders. Journal of Addictions and Offender Counseling. 10.1002/jaoc.12040 [DOI] [Google Scholar]
- Jason LA, & Ferrari JR (2010). Oxford House Recovery Homes: Characteristics and Effectiveness. Psychological Services. 10.1037/a0017932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongbloed B, & Vossensteyn H (2016). University funding and student funding: International comparisons. Oxford Review of Economic Policy. 10.1093/oxrep/grw029 [DOI] [Google Scholar]
- Kaplan L (2008). The role of recovery support services in recovery-oriented systems of care (DHHS Publication No. SMA 08–4315). Rockville, MD. [Google Scholar]
- Kaskutas LA (2009). Alcoholics Anonymous Effectiveness: Faith Meets Science. Journal of Addictive Diseases, 28(2), 145–157. 10.1080/10550880902772464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Humphreys K, & Ferri M (2020). Alcoholics Anonymous and other 12-step programs for alcohol use disorder. Cochrane Database of Systematic Reviews. 10.1002/14651858.CD012880.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, & Slaymaker V (2013). Emerging adults’ treatment outcomes in relation to 12-step mutual-help attendance and active involvement. Drug and Alcohol Dependence, 129(1–2), 151–157. 10.1016/j.drugalcdep.2012.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kollath-Cattano C, DeMaria AL, Sundstrom B, Kooper A, Manzi H, McInnis SM, & Cabot JO (2018). ‘Everyone wants a community’: a qualitative investigation of the challenges and service needs among college students in recovery. Addiction Research and Theory, 26(5), 369–376. 10.1080/16066359.2017.1414199 [DOI] [Google Scholar]
- Laitman L, Kachur-Karavites B, & Stewart LP (2014). Building, Engaging, and Sustaining a Continuum of Care From Harm Reduction to Recovery Support: The Rutgers Alcohol and Other Drug Assistance Program. Journal of Social Work Practice in the Addictions, 14(1), 64–83. 10.1080/1533256X.2014.872010 [DOI] [Google Scholar]
- Laitman L, & Lederman LC (2008). The need for a continuum of care: The rutgers comprehensive model. Journal of Groups in Addiction and Recovery, 2(2–4), 238–256. 10.1080/15560350802080993 [DOI] [Google Scholar]
- Laudet AB, Harris K, Kimball T, Winters KC, & Moberg DP (2015). Characteristics of Students Participating in Collegiate Recovery Programs: A National Survey. Journal of Substance Abuse Treatment, 51, 38–46. 10.1016/j.jsat.2014.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, Harris K, Kimball T, Winters KC, & Moberg DP (2016). In college and in recovery: Reasons for joining a Collegiate Recovery Program. Journal of American College Health : J of ACH, 64(3), 238–246. 10.1080/07448481.2015.1117464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A, Harris K, Winters K, Moberg D, & Kimball T (2014). Nationwide survey of collegiate recovery programs: Is there a single model? Drug and Alcohol Dependence, 140(2014), e117. 10.1016/j.drugalcdep.2014.02.335 [DOI] [Google Scholar]
- Laudet Alexandre, Harris K, Kimball T, Winters KC, & Moberg DP (2014a). Collegiate Recovery Communities Programs: What Do We Know and What Do We Need to Know? Journal of Social Work Practice in the Addictions, 14(1), 84–100. 10.1080/1533256X.2014.872015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet Alexandre, Harris K, Kimball T, Winters KC, & Moberg DP (2014b). Collegiate Recovery Communities Programs: What Do We Know and What Do We Need to Know? Journal of Social Work Practice in the Addictions, 14(1), 84–100. 10.1080/1533256X.2014.872015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet Alexandre, & Humphreys K (2013). Promoting recovery in an evolving policy context: What do we know and what do we need to know about recovery support services? Journal of Substance Abuse Treatment, 45(1), 126–133. 10.1016/j.jsat.2013.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet Alexandre, & White WL (2008). Recovery capital as prospective predictor of sustained recovery, life satisfaction, and stress among former poly-substance users. Substance Use and Misuse, 43(1), 27–54. 10.1080/10826080701681473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac D, Colquhoun H, & O’Brien KK (2010). Scoping studies: Advancing the methodology. Implementation Science. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovett J (2015). MAINTAINING LASTING RECOVERY AFTER GRADUATING FROM A COLLEGIATE RECOVERY COMMUNITY. University of Alabama. [Google Scholar]
- McKay JR (2009). Continuing care research: What we have learned and where we are going. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG (2009). Academia and Clinic Annals of Internal Medicine Preferred Reporting Items for Systematic Reviews and Meta-Analyses : Annals of Internal Medicine, 151(4), 264–269. [DOI] [PubMed] [Google Scholar]
- Monsour D, Kimball T, & Hensley E (2020). Navigating challenges to providing eating disorder support in collegiate recovery programs. Journal of American College Health, 1–4. 10.1080/07448481.2020.1790576 [DOI] [PubMed] [Google Scholar]
- Moore M (1999). An archival investigation of factors impacting a substance-abuse intervention program. Texas Tech University. [Google Scholar]
- Morgan EJ, & Cavendish JM (1988). Medical, ethical, and legal issues in treating college student substance abusers. Alcoholism Treatment Quarterly, 4(4), 141–149. 10.1300/J020V04N04_10 [DOI] [Google Scholar]
- Musgrave-Marquart D, Bromley SP, & Dalley MB (1997). Personality, academic attribution, and substance use as predictors of academic achievement in college students. Journal of Social Behavior and Personality, 12(2), 501–511. [Google Scholar]
- National Center for Education Statistics. (2017). College enrollment rates. The Condition of Education 2018, 2010, 1–3. Retrieved from https://nces.ed.gov/programs/coe/pdf/coe_cha.pdf [Google Scholar]
- Odefemi-Azzan O (2020). Factors that affect students enrolled in a midsize collegiate recovery program in the United States. Saint Peter’s University. [Google Scholar]
- Owens JS, Lyon AR, Brandt NE, Masia Warner C, Nadeem E, Spiel C, & Wagner M (2014). Implementation Science in School Mental Health: Key Constructs in a Developing Research Agenda. School Mental Health, 6(2), 99–111. 10.1007/s12310-013-9115-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, & Soares CB (2015). Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare, 13(3), 141–146. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- Rastegar D, & Fingerhood M (2015). The American Society of Addiction Medicine Handbook of Addiction Medicine. In The American Society of Addiction Medicine Handbook of Addiction Medicine. 10.1093/med/9780190214647.001.0001 [DOI] [Google Scholar]
- Reed BJ, Almaguer-botero AP, Grizzell S, & Watts J (2020). Collegiate Recovery Programs : Helping College Students in Recovery Succeed. 34(2), 58–72. [Google Scholar]
- Shumway ST, Bradshaw SD, Harris KS, & Baker AK (2013). Important factors of early addiction recovery and inpatient treatment. Alcoholism Treatment Quarterly, 31(1), 3–24. 10.1080/07347324.2013.747313 [DOI] [Google Scholar]
- Smith JA, Franklin S, Asikis C, Knudsen S, Woodruff A, & Kimball T (2018). Social Support and Gender as Correlates of Relapse Risk in Collegiate Recovery Programs. Alcoholism Treatment Quarterly, 36(3), 354–365. 10.1080/07347324.2018.1437372 [DOI] [Google Scholar]
- Spencer KM (2017). Voices of Recovery: An Exploration of Stigma Experienced by College Students in Recovery from Alcohol and/or Other Drug Addiction through Photovoice. University of North Carolina at Greensboro. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. HHS Publication No. PEP19–5068, NSDUH Series H-54, 170, 51–58. 10.1016/j.drugalcdep.2016.10.042 [DOI] [Google Scholar]
- Terrion JL (2013). The experience of post-secondary education for students in recovery from addiction to drugs or alcohol: Relationships and recovery capital. Journal of Social and Personal Relationships, 30(1), 3–23. 10.1177/0265407512448276 [DOI] [Google Scholar]
- Timko C, Cronkite RC, McKellar J, Zemore S, & Moos RH (2013). Dually diagnosed patients’ benefits of mutual-help groups and the role of social anxiety. Journal of Substance Abuse Treatment, 44(2), 216–223. 10.1016/j.jsat.2012.05.007 [DOI] [PubMed] [Google Scholar]
- Tracy K, & Wallace S (2016). Benefits of peer support groups in the treatment of addiction. Substance Abuse and Rehabilitation. 10.2147/sar.s81535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilsaint CL, Kelly JF, Bergman BG, Groshkova T, Best D, & White W (2017). Development and validation of a Brief Assessment of Recovery Capital (BARC-10) for alcohol and drug use disorder. Drug and Alcohol Dependence, 177(February), 71–76. 10.1016/j.drugalcdep.2017.03.022 [DOI] [PubMed] [Google Scholar]
- Walker M (2017). Women in Recovery : Perceptions in Transition to Community College. [Google Scholar]
- Washburn SC (2016). Trajectories, Transformations, and Transitions: A Phenomenological Study of College Students in Recovery Finding Success. ProQuest Dissertations and Theses, 333. Retrieved from https://vpn.utm.my/docview/1830471095?accountid=41678 [Google Scholar]
- Wattick RA, Hagedorn RL, & Olfert MD (2019). ARTICLE IN PRESS GEM No. XXX Enhancing College Student Recovery Outcomes Through Nutrition and Culinary Therapy : Mountaineers for Recovery and Resilience. 000(000), 0–3. 10.1016/j.jneb.2019.11.006 [DOI] [PubMed] [Google Scholar]
- Watts JR, Chowdhury D, & Holloway L (2019). Success in collegiate recovery programs: results from a phenomenological investigation. Alcoholism Treatment Quarterly, 37(2), 163–180. 10.1080/07347324.2018.1532776 [DOI] [Google Scholar]
- Watts JR, Tu WM, & O’Sullivan D (2019). Vocational Expectations and Self-Stigmatizing Views Among Collegiate Recovery Students: An Exploratory Investigation. Journal of College Counseling, 22(3), 240–255. 10.1002/jocc.12140 [DOI] [Google Scholar]
- White WL, & Finch AJ (2006). The Recovery School Movement: Its History and Future. Counselor. [Google Scholar]
- Whitney J (2018). STUDENTS’ LIVED EXPERIENCES IN COLLEGIATE RECOVERY PROGRAMS AT THREE LARGE PUBLIC RESEARCH UNIVERSITIES. Pennsylvania State University. [Google Scholar]
- Wiebe R, Cleveland H, & Dean L (2010). Maintaining abstinence in college: Temptations and tactics. In Cleveland H, Harris K, & Wiebe R (Eds.), Substance abuse recovery in college (1st ed., pp. 57–55). Boston, MA: Springer. [Google Scholar]
- Wiebe RP, Griffin AM, Zheng Y, Harris KS, & Cleveland HH (2018). Twelve Steps, Two Factors: Coping Strategies Moderate the Association Between Craving and Daily 12-Step Use in a College Recovery Community. Substance Use and Misuse, 53(1), 114–127. 10.1080/10826084.2017.1325904 [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Montes KS, Schwebel FJ, & Tucker JA (2020). What Is Recovery? Alcohol Research : Current Reviews, 40(3), 01. 10.35946/arcr.v40.3.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodford M (2001). Recovering College Students’ Perspectives: Investigating the Phenomena of Recovery from Substance Abuse among Undergraduate Students. University of Virginia. [Google Scholar]
- Worfler K (2016). EXAMINING COLLEGE STUDENTS IN RECOVERY FROM A SUBSTANCE USE DISORDER THROUGH INTERPRETATIVE PHENOMENOLOGICAL ANALYSIS. Colorado State University. [Google Scholar]
- Workman C (2020). “KNOWING WHERE WE’VE BEEN, AND WHAT WE’VE OVERCOME IS KEY”: THE ROLE OF CAMPUS ENVIRONMENT ON DEVELOPMENT OF RECOVERY IDENTITY IN MEMBERS OF A COLLEGIATE RECOVERY PROGRAM. University of Wisconsin - La Crosse. [Google Scholar]
- Zemore SE, Lui C, Mericle A, Hemberg J, & Kaskutas LA (2018). A longitudinal study of the comparative efficacy of Women for Sobriety, LifeRing, SMART Recovery, and 12-step groups for those with AUD. Journal of Substance Abuse Treatment, 88, 18–26. 10.1016/j.jsat.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y, Wiebe RP, Cleveland HH, Molenaar PCM, & Harris KS (2013). An Idiographic Examination of Day-to-Day Patterns of Substance Use Craving, Negative Affect, and Tobacco Use Among Young Adults in Recovery. Multivariate Behavioral Research, 48(2), 241–266. 10.1080/00273171.2013.763012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


