Abstract
Background
Spending on cardiovascular disease and cardiovascular risk factors (cardiovascular spending) accounts for a significant portion of overall US healthcare spending. Our objective was to describe US adult cardiovascular spending patterns in 2016, changes from 1996 to 2016, and factors associated with changes over time.
Methods
We extracted information on adult cardiovascular spending from the Institute for Health Metrics and Evaluation’s disease expenditure project, which combines data on insurance claims, emergency department and ambulatory care visits, inpatient and nursing care facility stays, and drug prescriptions to estimate over 85% of all US healthcare spending. Cardiovascular spending (2016 USD) was stratified by age, sex, type of care, payer, and cardiovascular cause. Time trend and decomposition analyses quantified contributions of epidemiology, service price and intensity (spending per unit of utilization, e.g., spending per inpatient bed-day), and population growth and aging to the increase in cardiovascular spending from 1996 to 2016.
Results
Adult cardiovascular spending increased from $212 billion in 1996 to $320 billion in 2016, a period when the US population increased by over 52 million people, and median age increased from 33.2 to 36.9 years. Over this period, public insurance was responsible for the majority of cardiovascular spending (54%), followed by private insurance (37%), and out-of-pocket spending (9%). Health services for ischemic heart disease ($80 billion) and hypertension ($71 billion) led to the most spending in 2016. Increased spending between 1996 and 2016 was primarily driven by treatment of hypertension, hyperlipidemia, and atrial fibrillation/flutter, on which spending rose by $42 billion, $18 billion, and $16 billion, respectively. Increasing service price and intensity alone were associated with a 51%, or $88 billion, cardiovascular spending increase from 1996 through 2016, whereas changes in disease prevalence was associated with a 37%, or $36 billion, spending reduction over the same period, after taking into account population growth and population aging.
Conclusions
US adult cardiovascular spending increased by >$100 billion from 1996 to 2016. Policies tailored to control service price and intensity and preferentially reimburse higher quality care could help counteract future spending increases due to population aging and growth.
Keywords: Cardiovascular disease, health expenditures, health economics
INTRODUCTION
While cardiovascular disease (CVD) remains the leading cause of death in the United States, CVD mortality rates have been decreasing since the 1960’s only to begin rising again in the last decade1–3. Despite this, the population of older Americans is increasing, and nearly half of US adults are expected to have CVD by 20354–7. Commensurate with the large CVD burden, the US spends over $320 billion annually (15% of healthcare spending) managing and treating CVD and cardiovascular risk factors (cardiovascular spending)8. A detailed accounting of cardiovascular spending in the US can guide policy and management decisions, but it is difficult to quantify spending due to the multiple US healthcare system payers and data sets.
Recent work examined US healthcare spending overall and key drivers of changes over time, but, to our knowledge, no prior studies applied these methods to a detailed analysis of cardiovascular spending8–15. The Institute for Health Metrics and Evaluation’s Disease Expenditure Project (DEX) estimates US healthcare spending stratified by health condition, age and sex group, type of care, and payer8–10. We used DEX to describe patterns of cardiovascular spending in US adults in 2016, cardiovascular spending changes from 1996 to 2016, and to quantify key factors associated with cardiovascular spending changes over time.
METHODS
DEX estimates are publicly available on the Global Health Data Exchange (GHDx). The code used in the analysis is available upon request.
Data Sources
DEX Spending Data
Cardiovascular spending estimates came from the Institute for Health Metrics and Evaluations DEX project (Table I in the Supplement)8–10. DEX uses microdata from 5.9 billion unique insurance claims; 150.4 million ambulatory, dental, or emergency department visits; 1.5 billion inpatient and nursing care facility bed-days; and 5.9 million prescribed pharmaceuticals to estimate 85.2% of all US healthcare spending from 1996 to 2016 in 2016 US dollars (Table II in the Supplement). The spending that falls outside of the scope of the project includes home health care, durable medical equipment and non-durable medical products (including all over-the-counter medications, even those recommended by the American College of Cardiology for treatment of CVD16), government public health activities, unreimbursed charity care, and investments such as research and development. The spending captured in DEX is disaggregated into 154 health conditions, 38 age and sex groups, seven types of care – ambulatory, inpatient, nursing care facility, emergency department, dental care, prescribed pharmaceuticals purchased in the retail setting, and overhead category for insurance companies’ administrative costs. DEX also disaggregates spending into three payer categories: (1) public insurance, which includes Medicaid, Medicare, Veterans Affairs, as well as spending by other Federal and local programs; (2) private insurance; and (3) self or family out-of-pocket. The methods used in DEX have been reported elsewhere; a summary can be found in the Supplemental Methods8.
As causes for cardiovascular spending, we included eight CVD health conditions included in the DEX analysis (ischemic heart disease, cerebrovascular disease, atrial fibrillation/flutter, endocarditis, peripheral arterial disease, aortic aneurysm, rheumatic heart disease, and an “other heart disease” category that includes predominantly non-rheumatic valvular disease), two cardiovascular risk factors (hypertension and hyperlipidemia), and heart failure (comprised of heart failure, cardiomyopathy, and hypertensive heart disease) (Tables III–V in the Supplement). We extracted spending and volume estimates for adults (age ≥20 years) from the DEX database for each cardiovascular cause of spending. DEX provides separate estimates for spending on clinical care and for the administrative costs of running health insurance programs. We removed the estimates of administrative costs from our analysis to focus on the dollars spent to provide clinical care.
Epidemiological Data
We obtained estimates of population and disease prevalence from 1996–2016 from the 2017 Global Burden of Disease (GBD) study, which is disaggregated into the same age and sex groups used in DEX17. Prevalence estimates were extracted for all cardiovascular causes other than aortic aneurysms, for which GBD only estimates deaths. Data from both GBD and DEX are deidentified and aggregated. A waiver of informed consent was reviewed and approved by the University of Washington Institutional Review Board.
Statistical Analysis
Cardiovascular Spending in 2016
Estimates of cardiovascular spending in 2016 were reported for 28 age and sex groups, five types of care, and the three payer types. GBD population estimates were used to calculate per capita cardiovascular spending. Absolute and per capita spending estimates were analyzed for variation across age and sex groups, types of care, payer, and cardiovascular cause.
Changes in Cardiovascular Spending Over Time
Cardiovascular spending for each year from 1996 through 2016 was analyzed to determine how spending has varied over time. Changes in absolute spending and population-standardized annualized rates of change were calculated from 1996 to 2016. Annualized rate of change is defined as the constant yearly rate that spending would need to change to produce the overall change in spending over a longer period of time. Population-standardized annualized rates are commonly used to describe the change in spending that is independent of background changes in population size, age, and sex structure that occur over time8, 10, 18. We standardized our annualized rates using the 2016 population structure. To do this we multiplied the per person spending rate for each age and sex group for each cardiovascular cause of spending in 1996 by the 2016 age and sex population structure to estimate what cardiovascular spending would have been in 1996 if the population were structured as it was in 2016. Annualized rates of change were then calculated to estimate the rate of change needed to go from the hypothetical 1996 spending to the 2016 spending estimates.
Factors Associated with the Change in Cardiovascular Spending Over Time
We applied standard demographic decomposition methods in the same manner as Dieleman et al. to determine factors associated with changes in cardiovascular spending from 1996 to 201610, 19. We disaggregated the change in US healthcare spending into the changes associated with five factors: size of the total US population, age and sex structure of the population, disease prevalence, service utilization, and service price and intensity10, 19. Service utilization and service price and intensity are both defined differently for each type of care. For ambulatory and emergency care, service utilization is visits per prevalent case and service price and intensity is spending per visit; for inpatient and nursing home care, service utilization is number of bed-days per prevalent case and service price and intensity is spending per bed-day; and for retail pharmaceuticals service utilization is number of prescriptions per prevalent case and service price and intensity is mean spending per prescription10.
In the decomposition analysis, we estimated spending for each age, sex, cause, type of care, and year combination as the product of these five factors using population-level data derived from DEX and the 2017 GBD (Formula 1)10, 17, 19.
| (1) |
Where a indicates age; s, sex; c, condition; t, type of care; and y, year.
Uncertainty Estimates
We estimated uncertainty using 1,000 bootstrap draws of the GBD 2017 and DEX8, 10, 17. We report the mean of the 1,000 bootstrap draws and defined the 95% confidence intervals (95% CI) as the 2.5th to 97.5th percentile.
All analyses were conducted using Stata version 13.1 (StataCorp), R version 3.31 (R Foundation), and Excel (Microsoft). All spending was adjusted for inflation before any modeling using the economy-wide consumer price index from the Bureau of Economic Analysis. All estimates are reported in 2016 US dollars.
RESULTS
Cardiovascular Spending in 2016
In 2016, total spending on cardiovascular care in US adults was $320.1 billion (95% CI $299.2 to $345.6 billion). More than half of cardiovascular spending was paid by public payers at $180.1 billion (95% CI $167.2 to $194.3 billion), followed by private payers at $118.8 billion (95% CI $106.0 to $135.1 billion) and out-of-pocket spending at $21.2 billion (95% CI $17.0 to $25.7 billion) (Figure 1). Services for adults ≥65 years led to more than half of cardiovascular spending at $185.3 billion (95% CI $171.9 to $199.9 billion), followed by spending on adults aged 45 to 64 years at $113.3 billion (95% CI $104.3 to $125.9 billion) and adults aged 20 to 44 years at $21.4 billion (95% CI $20.0 to $22.8 billion).
Figure 1. Total cardiovascular spending in 2016 by payer, age, type of service, and cardiovascular cause.
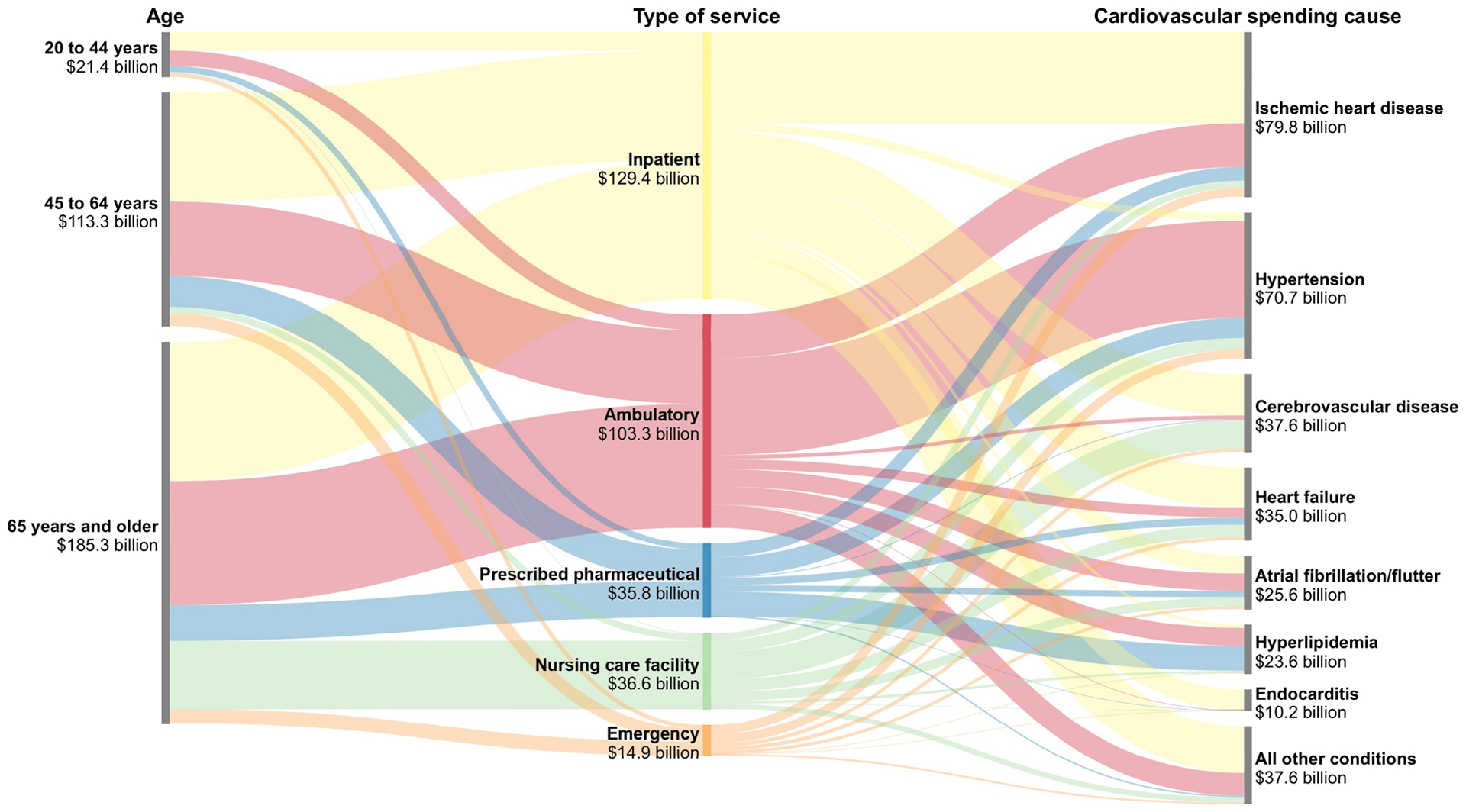
Notes: The figure shows the distribution of cardiovascular spending in 2016 by age, type of service, and cardiovascular spending cause (i.e., each column sums to the total cardiovascular spending in 2016). The first column shows the distribution of cardiovascular spending across age groups, and the pathways connecting the first and second columns indicate the cardiovascular spending by type of service within each age group. Similarly, the second column shows the distribution of cardiovascular spending across type of service, and the pathways connecting to the third column indicate the cardiovascular spending causes by type of service. The third column shows the distribution of cardiovascular spending by cardiovascular spending cause. “All other conditions” indicates all causes for which less than $10 billion was spent individually. All estimates are in 2016 USD.
The majority of cardiovascular spending was on inpatient care at $129.4 billion (95% CI $114.9 to $151.8 billion), followed by ambulatory care, nursing facility care, and prescribed retail pharmaceuticals at $103.3 billion (95% CI $95.4 to $112.0 billion), $36.6 billion (95% CI $31.7 to $42.8 billion), and $35.8 billion (95% CI $34.7 to $37.1 billion), respectively. The three largest cardiovascular causes of spending overall were ischemic heart disease at $79.8 billion (95% CI $72.3 to $85.4 billion), treatment of hypertension at $70.7 billion ($65.0 to $77.6 billion), and cerebrovascular disease at $37.6 billion (95% CI $33.8 to 42.0 billion) (Table 1). Cerebrovascular disease was unique in that a significant portion of spending (36.4%, 95% CI 32.0% to 43.0%) was for nursing facility care, which includes acute rehabilitation services.
Table 1.
Total Cardiovascular Spending and Aggregated Health Categories. Adult Cardiovascular Spending column is in 2016 $billions. All other columns present percentage of spending.
| Aggregate Age Group (years) | Type of Payer | Type of Care | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spending Rank | Cardiovascular Spending Cause | Adult Cardiovascular Spending, (95% CI) | 20–44 | 45–64 | 65+ | Public | Private | Out-of-pocket | Inpatient | Ambulatory | Nursing care facility | Prescribed pharmaceuticals | Emergency | |
| 1 | Ischemic Heart Disease | 79.8 | (72.3, 85.4) | 4.5 | 38.1 | 57.4 | 54.3 | 41.7 | 3.9 | 55.3 | 26.4 | 4.2 | 8.4 | 5.7 |
| 2 | Hypertension | 70.7 | (65.0, 77.6) | 7.8 | 40.5 | 51.7 | 57.0 | 35.7 | 7.3 | 5.5 | 66.8 | 7.9 | 13.4 | 6.2 |
| 3 | Cerebrovascular Disease | 37.6 | (33.8, 42.1) | 6.4 | 29.5 | 64.1 | 56.4 | 31.8 | 11.8 | 53.0 | 5.0 | 36.4 | 1.1 | 4.6 |
| 4 | Heart Failure | 35.0 | (32.5, 38.0) | 11.1 | 28.5 | 60.4 | 65.1 | 26.8 | 8.1 | 54.8 | 13.6 | 16.4 | 10.2 | 4.9 |
| 5 | Atrial Fibrillation/Flutter | 25.6 | (22.1, 30.4) | 2.2 | 22.6 | 75.2 | 56.4 | 36.2 | 7.4 | 33.1 | 32.6 | 16.9 | 11.7 | 5.7 |
| 6 | Hyperlipidemia | 23.6 | (21.7, 26.3) | 6.7 | 44.5 | 48.8 | 49.1 | 43.0 | 7.9 | 6.6 | 36.7 | 5.2 | 50.9 | 0.5 |
| 7 | Other Cardiovascular Disease | 22.6 | (19.6, 26.0) | 13.0 | 35.5 | 51.5 | 53.9 | 41.6 | 4.6 | 47.9 | 41.1 | 4.5 | 2.7 | 3.8 |
| 8 | Endocarditis | 10.2 | (5.1, 33.8) | 4.0 | 39.8 | 56.2 | 52.4 | 44.6 | 3.0 | 87.8 | 9.1 | 2.8 | 0.2 | 0.0 |
| 9 | Peripheral Arterial Disease | 6.3 | (5.5, 7.2) | 1.8 | 32.6 | 65.6 | 62.7 | 32.0 | 5.2 | 62.8 | 13.2 | 22.5 | 1.3 | 0.3 |
| 10 | Aortic Aneurysm | 5.0 | (4.5, 5.5) | 10.4 | 30.3 | 59.3 | 63.1 | 34.4 | 2.5 | 89.3 | 8.4 | 2.0 | 0.0 | 0.2 |
| 11 | Rheumatic Heart Disease | 3.8 | (1.4, 5.0) | 6.7 | 14.9 | 78.4 | 67.0 | 30.4 | 2.6 | 87.1 | 10.8 | 1.0 | 0.0 | 1.1 |
Total cardiovascular spending in 2016 was largest for those aged 60 to 64 years at $43.3 billion (95% CI $38.5 to $52.1 billion), with cardiovascular spending decreasing each following five-year age group to spending $38.9 billion (95% CI $35.8 to $42.6 billion) on those 80–84 years (Figure 2). Total per capita cardiovascular spending follows a different trend, with each age group spending more per capita than its adjacent younger group. For example, those 60 to 64 years old spent $2,229 (95% CI, $1,983 to $2,681) per capita in 2016, while those aged 85 and older spent $6,273 (95% CI, $5,782 to $6,873). Both total and per capita cardiovascular spending were higher for men across the majority of age groups. This additional spending was primarily due to increased inpatient care among men. Women age ≥80 years had higher cardiovascular spending than men ($43.6 billion [95% CI $39.8 to $47.5 billion] vs. $27.9 billion [95% CI $25.6 to $30.5 billion]), due mostly to increased nursing facility care. Unsurprisingly, public payers make up the majority of cardiovascular spending among those ≥65 years at 74.2% (95% CI 71.3% to 77.1%). However, public payers also comprise a significant portion across younger ages, making up 31.7% (95% CI 26.6% to 37.5%) of cardiovascular spending for those aged 45 to 64 years. Similar patterns are seen when examining spending per capita.
Figure 2. Total and per capita cardiovascular spending in 2016 by type of care and payer type.
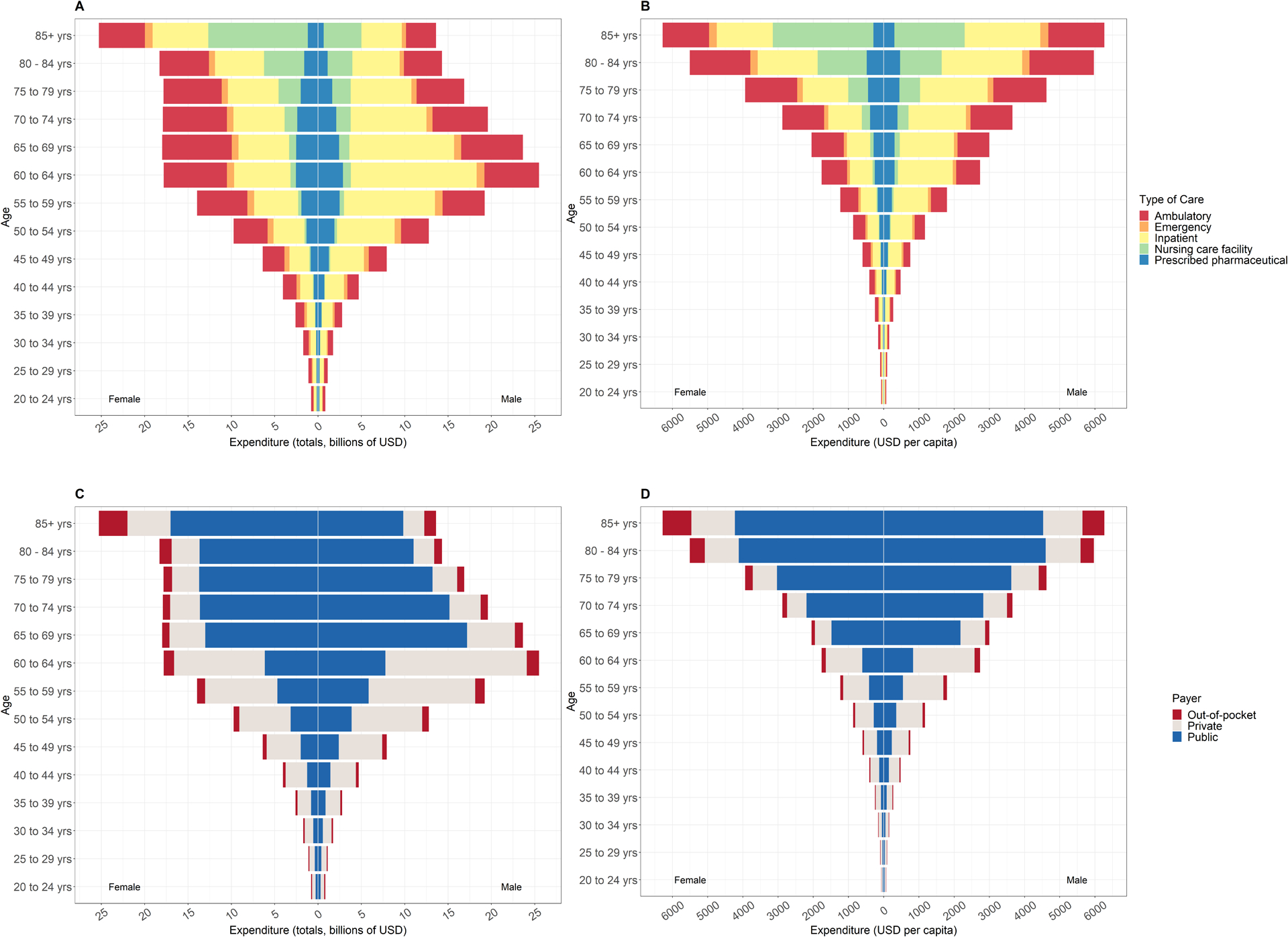
Notes: This figures shows 2016 cardiovascular spending. Panel A shows billions of USD by sex and type of care. Panel B shows USD per capita by sex and type of care. Panel C shows billions of USD by sex and payer. Panel D shows USD per capita by sex and payer. The figure shows 2016 absolute and per capita spending for each age and sex group, disaggregated by type of care and payer.
Changes in Cardiovascular Spending Over Time
From 1996 to 2010, total cardiovascular spending increased from $211.7 billion (95% CI $206.6 to $217.6 billion) to $318.4 billion (95% CI $306.8 to $331.7 billion) (Figure 3). However, cardiovascular spending decreased from 2010 to 2013, before increasing again from $306.1 billion (95% CI $292.5 to $321.7 billion) in 2013 to $320.1 billion (95% CI $299.2 to $345.6 billion) in 2016. Additionally, after accounting for population growth and population aging over time, the annualized rate of change of cardiovascular spending from 1996 through 2016 was 0.1% (95% CI −0.2% to 0.5%), relative to annualized rate of change of 2.6% (95% CI 2.6% to 2.6%) for all causes of US healthcare spending8.
Figure 3. Total US cardiovascular spending from 1996 to 2016 by type of care and payer type.
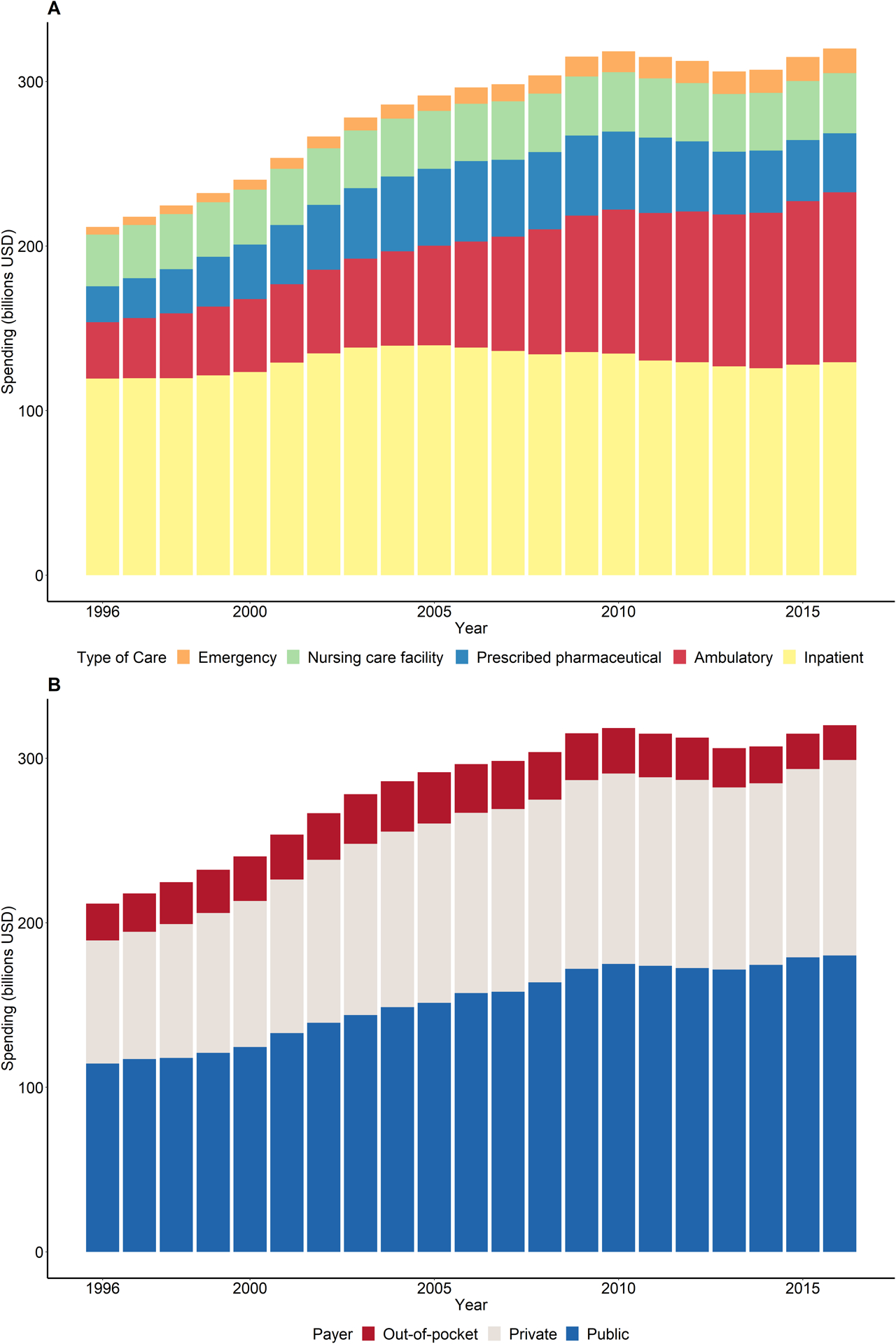
Notes: The figure shows cardiovascular spending over time, disaggregated by type of care (Panel A) and payer (Panel B). All estimates in 2016 USD.
Change in cardiovascular spending from 1996 to 2016 varied by type of care (Figure 3). The total increase in spending was driven largely by ambulatory care and prescribed retail pharmaceuticals, which accounted for 50.0% (95% CI 44.9% to 56.1%) and 24.0% (95% CI 21.0% to 27.4%) of the increase, respectively. While inpatient care accounted for the largest portion of cardiovascular spending each year, total spending on inpatient care was relatively flat over time. The change in cardiovascular spending over time did not vary greatly by payer. Both public payer and private payer spending increased slightly from 1996 to 2016, and out-of-pocket spending decreased proportionally.
Hypertension, hyperlipidemia, and atrial fibrillation/flutter were the conditions associated with the largest increases in overall spending between 1996 and 2016, at $42.1 billion (95% CI $36.6 to $48.9 billion), $17.9 billion (95% CI $16.0 to $20.7 billion), and $16.3 billion (95% CI $12.9 to $21.0 billion), respectively (Figure 4). These conditions, along with endocarditis, were also the fastest growing cardiovascular causes of spending after taking into account population changes. After accounting for growth population size and population aging over time, the annualized rate of change for treatment of hyperlipidemia was 5.0% (95% CI 4.4% to 5.6%), endocarditis was 4.4% (95% CI −1.1% to 9.9%), atrial fibrillation and atrial flutter was 3.2% (95% CI 2.3% to 4.1%), and treatment of hypertension was 2.6% (95% CI 2.2% to 3.1%), which compared to only 0.1% (95% CI −0.3% to 0.5%) for cardiovascular spending as a whole.
Figure 4. Absolute change and age-standardized annualized rate of change for total cardiovascular spending from 1996 to 2016.
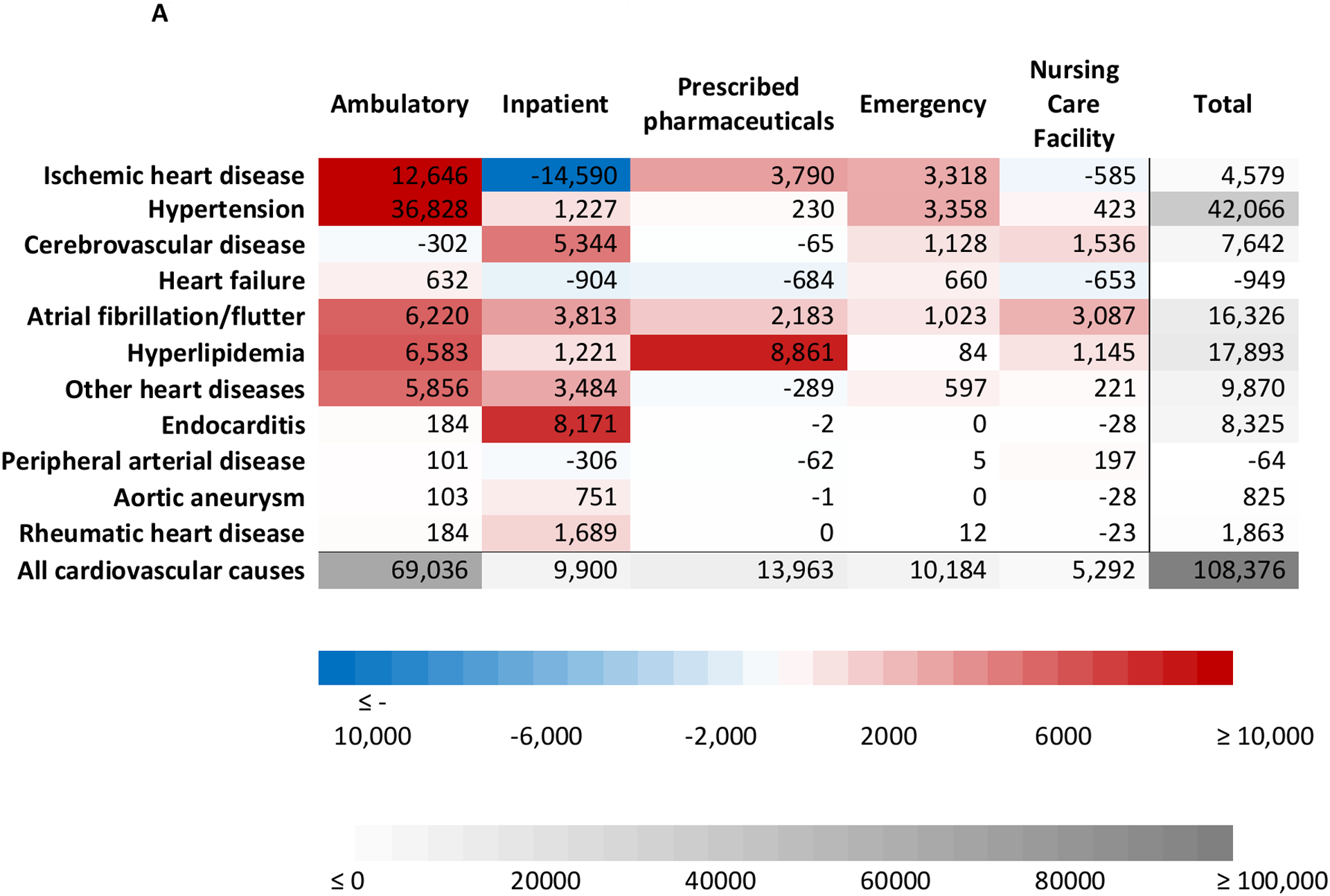
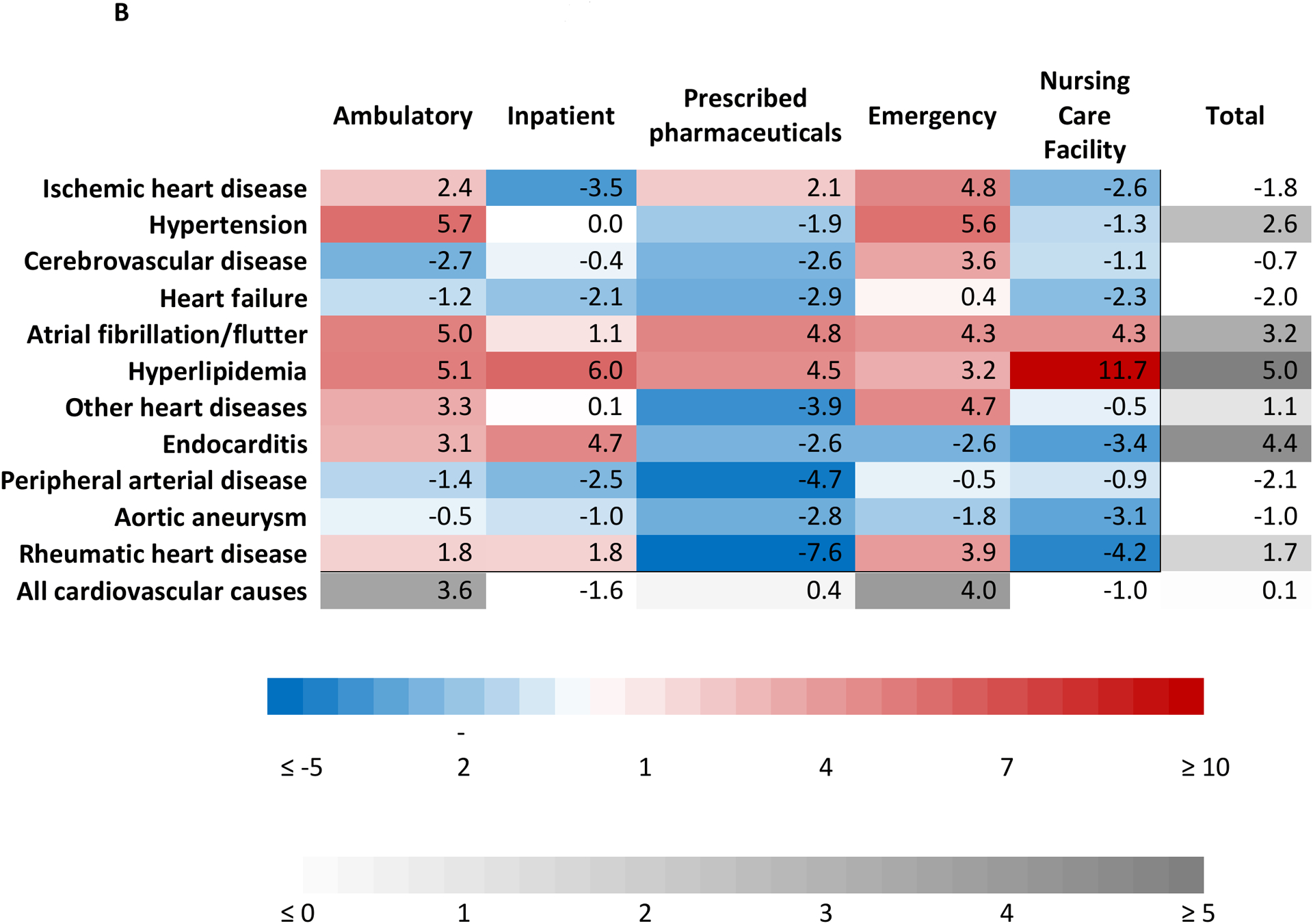
Notes: The figure shows the absolute change in spending (Panel A) and age-standardized annualized rate of change (Panel B) from 1996 through 2016. Cardiovascular causes are ranked by absolute spending in 2016. Absolute change is millions of 2016 USD.
The increase in spending on ambulatory care over time was driven predominantly by treatment of hypertension, ischemic heart disease, and atrial fibrillation/flutter (Figure 4). The increase in spending on prescribed retail pharmaceuticals was largely due to treatment of hyperlipidemia. However, spending on pharmaceuticals for hyperlipidemia began decreasing in 2009, consistent with increased use of generically priced statins. Decreased inpatient spending on ischemic heart disease was offset by increased endocarditis and cerebrovascular disease spending. When accounting for population size and structure, cardiovascular spending on inpatient care decreased from 1996 to 2016, with a population-adjusted annualized rate of change of −1.6% (95% CI −2.2% to −0.8%).
Factors Associated with Change in Cardiovascular Spending Over Time
Increased cardiovascular spending from 1996 to 2016 was associated with population growth and population aging and was partially offset by spending reductions associated with decreases in disease prevalence (Figure 5, Figures I–X in the Supplement). However, the details of these associations as well as the spending changes associated with service price and intensity and service utilization varied across cardiovascular causes and types of care. Changes in service price and intensity for ambulatory care was associated with a cardiovascular spending increase of 154.7% (95% CI 121.2% to 186.8%), or $53.2 billion (95% CI $44.0 to $62.2 billion), whereas decreasing pharmaceutical prices was associated with a spending reduction of 76.5% (95% CI 61.1% to 121.2%), or $14.0 billion (95% CI $10.7 to $22.3 billion). Decreased service utilization of inpatient care, meaning fewer bed-days per prevalent case, was associated with spending reductions of 62.7% (95% CI 45.0% to 72.1%), or $83.0 billion (95% CI $53.2 to $72.6 billion), but overall inpatient cardiovascular spending increased from 1996–2016 due to spending growth associated with population growth, population aging, and increased service price and intensity. Across all types of care, increasing service price and intensity alone were associated with a 51.2% (95% CI 41.2% to 60.9%), or an additional $87.7 billion (95% CI $71.9 to $103.7 billion) dollars, spent on cardiovascular causes in 2016 relative to 1996.
Figure 5. Decomposition of changes in cardiovascular spending from 1996 to 2016.
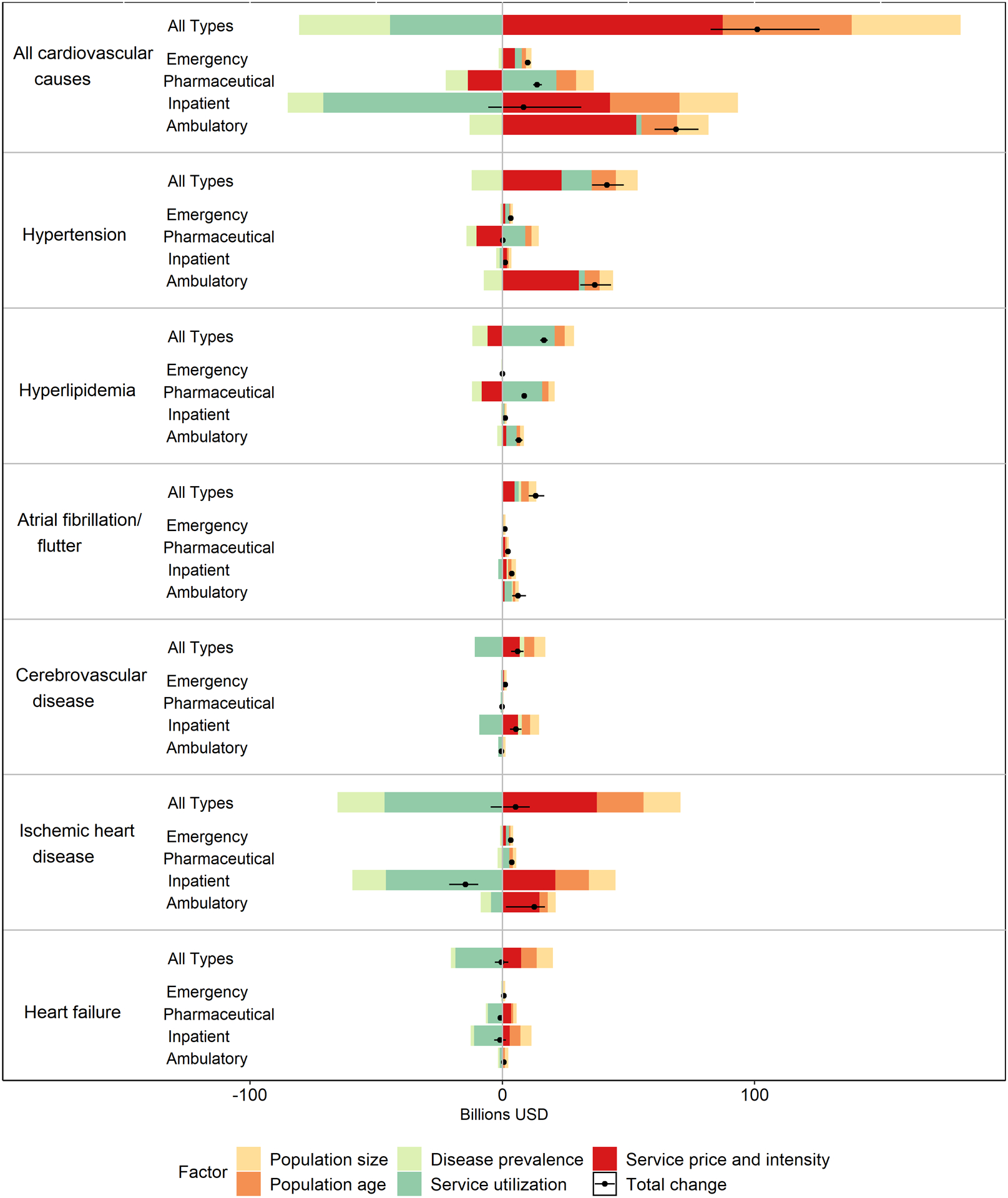
Notes: Figure shows the results of the decomposition analysis for the six largest causes of cardiovascular spending in 2016 as well as all cardiovascular causes cumulatively. The change associated with each factor is independent of the change associated with all other factors. All estimates are in 2016 USD.
DISCUSSION
Based on data from the Institute for Health Metrics and Evaluations DEX project, we estimated that cardiovascular healthcare spending for US adults was $320.1 billion in 2016. Cardiovascular spending increased from 1996 to 2016, primarily driven by increased spending on ambulatory care and prescribed retail pharmaceuticals. After accounting for background population growth and aging, increased service price and intensity together were responsible for an additional $88 billion dollars of cardiovascular spending in 2016 compared to 1996.
Our estimate of total US cardiovascular spending is higher than the estimate reported in the most recent American Heart Association (AHA) annual report20. We estimated $307.1 billion in cardiovascular spending in 2014, compared to the AHA’s $213.8 billion estimate20. This discrepancy may be due in part to the differences in data sources, scope, and methodology, such as a comorbidity adjustment used to create the DEX project’s estimates. The AHA uses the Medical Expenditure Panel Survey (MEPS), which only covers the non-institutionalized civilian US population and does not account for the $36.6 billion nursing care facility spending included in our analysis. Additionally, the DEX project scales all estimates to fit within the overall envelope of the National Health Expenditure Accounts (NHEA), which are the official government estimates of health spending in the US. MEPS is known to underestimate health spending compared with the NHEA, and our estimates closely align with previous work using a similar framework14, 21. For example, Roehrig et al. independently attributed $294 billion to circulatory conditions in 2013, similar to our cardiovascular spending estimate of $306 billion spent that same year14.
Our findings add to previous work that attributes a large share of the slowdown in US healthcare spending growth through 2013 to a slowdown in cardiovascular spending12–14. We found that this slow growth continued through 2016. The slowing of growth for heart and cerebrovascular disease spending has been attributed to fewer acute events, changes in clinical practice (e.g., decline in coronary revascularization), improved treatment of CVD risk factors, decreased smoking rates, and generic medications becoming more available12–14, 22–24. Our analysis is consistent with these hypotheses, showing that inpatient spending growth was largely attenuated by decreasing disease prevalence and fewer bed-days per prevalent case. We also found that decreased spending on prescribed retail cardiovascular pharmaceuticals played a substantial role in the overall trend of cardiovascular spending since 2010, consistent with increased use of generically priced statins.
Although our results reflect the shifting of some cardiovascular care from inpatient to ambulatory settings, we cannot quantify to what extent the overall slowdown in cardiovascular spending specifically can be attributed to these changes in clinical practice. For example, spending on ambulatory care of ischemic heart disease increased by over $12 billion from 1996 to 2016, while spending on inpatient care of ischemic heart disease decreased by over $14 billion over that same time period. We cannot quantify the change in this spending that is due to increased same-day discharge for elective percutaneous coronary interventions or use of “observation stays”25. Overall, the combination of medications going off-patent, a shift from inpatient care to ambulatory care, and improved treatment of risk factors that likely explains our finding that population-standardized cardiovascular spending grew more slowly than overall US healthcare spending.
Although cardiovascular spending on inpatient care grew at a slower rate relative to spending on other types of care, it did grow despite favorable epidemiologic trends and decreased service utilization. Reduced cardiovascular spending associated with fewer bed-days per prevalent case of CVD was offset by increased spending per bed-day. This could reflect more efficient hospital stays. For example, it is well-established that the length-of-stay for an admission for a myocardial infarction has decreased over time despite more aggressive treatment26–29. However, it may also suggest that the health system’s appetite for revenue is constant, such that more efficient clinical decision making and insurers’ efforts to curb utilization have triggered compensatory changes in services provided in the hospital and the amount charged for them. The question of which phenomenon is predominant, changes in price or changes in services provided, is not clear. For example, from 1998 to 2008 Medicare fee-for-service claims for noninvasive testing and monitoring grew dramatically, with the number of claims for nuclear stress tests growing 3-fold and claims for echocardiograms growing 2-fold, and the appropriateness of these is debated30. A similar trend may be occurring in the inpatient setting. At the same time, hospital overhead costs have increased at a greater rate than medical inflation, so it may be that the cost of capital investments and the procurement of devices and equipment is being shifted onto patients in the form of higher facility fees and corresponding increases in spending per bed-day31. Additionally, examination is needed of the impact on cardiovascular spending of other changes in the way insurers have tried to mitigate increased costs (e.g., prior authorization and utilization reviews) and access to health insurance (e.g., approval and adoption of the Affordable Care Act).
It is difficult to project whether the trend of increased cardiovascular spending from 2013 to 2016 will continue into future years. The increase in spending may be perpetuated by the approval of costly cardiovascular drugs in recent years, such as valsartan/sacubitril and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, which have seen increased utilization since 2016. Additionally, the recent approvals of tafamidis for transthyretin amyloid cardiomyopathy, which comes at a cost of $225,000 per year and is the most expensive cardiovascular drug ever approved, and of icosapent ethyl, which costs around $4,800 per year, indicate that cardiovascular spending on pharmaceuticals may increase32–36. Finally, the favorable epidemiologic trends responsible for significant savings on inpatient care are changing and may be worsened as the number of elderly in the US is expected to rise significantly in coming decades3–5. Our finding that spending per bed-day increased from 1996 through 2016 (an increase in service price and intensity), coupled with the growing number of US adults living with cardiovascular disease, may lead to increased inpatient spending overall despite decreased utilization of inpatient cardiovascular health services per prevalent case of CVD. This suggests that continued efforts to decrease hospital length of stay may be insufficient in controlling future inpatient cardiovascular spending. The difference between per capita cardiovascular spending on men and women also merits further investigation. The prevalence of ischemic heart disease among men in 2016 was 65.6% higher than among women, explaining at least some of the variation, but higher spending for men may also reflect gender biases in both frequency of diagnostic work up for suspected cardiovascular disease and intensity of treatment of cardiovascular disease1, 37–40.
Limitations
This study has several limitations. First, we may overestimate ambulatory spending on hypertension due to misattribution of the primary clinical focus of individual office visits. This is because MEPS does not provide the primary diagnosis recorded by healthcare providers at clinical encounters and instead lists the causes in the order reported by the patient. We assumed the first listed diagnosis was the primary diagnosis. While a comorbidity adjustment in DEX usually accounts for some of the bias introduced by this assumption, treatment of hypertension is excluded from the adjustment. Second, spending on non-rheumatic valvular disease is included in the “Other cardiovascular causes” category and is not individually identifiable. The DEX causes were derived from the GBD cause list, which focuses on worldwide populations, and the global epidemiology of non-rheumatic valvular disease is quite different than in the US. Given the complex and costly interventions, future analyses would benefit from specifically identifying spending on non-rheumatic valvular heart disease in the US. Third, spending on diabetes and obesity were excluded as cardiovascular causes from this study. Although DEX includes a comorbidity adjustment that redistributes excess spending on diabetes to comorbid conditions, including CVD, this likely does not fully address the overlap in spending on these diseases. With the advent of sodium-glucose cotransporter-2 (SGLT-2) inhibitors, which first demonstrated CVD benefit in 2015, the overlap in spending on diabetes and CVD will likely increase41. Future research examining spending on cardiometabolic disease, including obesity and diabetes, or that disentangles how much spending on obesity and diabetes can be attributed to cardiovascular spending is warranted. Fourth, we were unable to separate spending on procedures as a component of spending on medical care overall. Fifth, our study relies on survey data, which may miss outlier expensive but rare cases and also fails to represent certain populations by design. Sixth, the current study does not have information on the distribution of cardiovascular spending by geography or race and ethnicity, or spending after 2016.
Conclusion
US adult cardiovascular spending increased substantially from 1996 through 2016, despite a slowdown in growth starting in the mid-2000s and a near-plateau in spending since 2010.
The results of this detailed analysis of cardiovascular spending indicate that CVD costs increased substantially despite decreased utilization of services by healthcare providers, and increases in service price and intensity (e.g., spending per inpatient bed-day) were a major reason. Efforts to control service price and intensity of healthcare services, as well as novel approaches to incentivize prevention and high-value care, may be needed to contain anticipated increases in spending due to population aging and growth and increasing cardiovascular mortality in the US. Specific policy proposals would benefit from both cost-effectiveness analyses and budget impact analyses in local health systems.
Supplementary Material
CLINICAL PERSPECTIVE.
- What is new?
- Adult US cardiovascular spending (2016 USD) increased from $212 billion in 1996 to $320 billion in 2016, with most growth occurring between 1996 and 2010; a slowdown in spending on prescribed retail pharmaceuticals and inpatient care tempered later growth.
- Although ischemic heart disease remained the largest cause of cardiovascular spending in 2016 ($79.8 billion), spending on hypertension ($70.7 billion), hyperlipidemia ($23.6 billion), and atrial fibrillation/flutter ($25.6 billion) grew at substantially faster rates.
- Increasing service price and intensity was associated with an $88-billion-dollar cardiovascular spending increase from 1996–2016, whereas changes in disease prevalence was associated with a $36-billion-dollar spending reduction.
- What are the clinical implications?
- Factors associated with cardiovascular spending reductions from 1996 to 2016 – namely decreasing disease prevalence, inpatient resource utilization, and pharmaceutical prices – may be unable to contain future cardiovascular spending increases due to new pharmaceuticals and cardiac devices, increased spending per inpatient bed-day, and an increasing population of older Americans.
- As shown by our analysis of ischemic heart disease, where costs rose despite large decreases in inpatient service utilization, policies designed to control service price and intensity (e.g., spending per inpatient bed-day) and promote high-quality, cost-effective care may better contain cardiovascular spending than policies designed to reduce inpatient length of stay.
ACKNOWLEDGEMENTS
The Scholarly Project Program at The Columbia University Vagelos College of Physicians and Surgeons. Carina Chen, who provided guidance on using data from DEX and GBD.
SOURCES OF FUNDING
Dr. Bellows is supported by the National Heart, Lung, and Blood Institute (NHLBI) (K01HL140170).
Non-standard Abbreviations and Acronyms
- DEX
The Institute for Health Metrics and Evaluation’s Disease Expenditure Project
- GHDx
Global Health Data Exchange
- GBD
Global Burden of Disease study
- AHA
American Heart Association
- MEPS
Medical Expenditure Panel Survey
- NHEA
National Health Expenditure Accounts
Footnotes
DISCLOSURES
All authors declare no relevant conflicts of interest to disclose.
REFERENCES
- 1.GBD Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–1210. DOI: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mensah GA, Wei GS, Sorlie PD, Fine LJ, Rosenberg Y, Kaufmann PG, Mussolino ME, Hsu LL, Addou E, Engelgau MM, et al. Decline in Cardiovascular Mortality: Possible Causes and Implications. Circ Res. 2017;120:366–380. DOI: 10.1161/CIRCRESAHA.116.309115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah NS, Molsberry R, Rana JS, Sidney S, Capewell S, O’Flaherty M, Carnethon M, Lloyd-Jones DM, Khan SS. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999–2018: observational analysis of vital statistics. BMJ. 2020;370:m2688. DOI: 10.1136/bmj.m2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mensah GA, Brown DW. An overview of cardiovascular disease burden in the United States. Health Aff (Millwood). 2007;26:38–48. DOI: 10.1377/hlthaff.26.1.38. [DOI] [PubMed] [Google Scholar]
- 5.Sidney S, Quesenberry CP Jr., Jaffe MG, Sorel M, Nguyen-Huynh MN, LH Kushi, Go AS, Rana JS. Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals. JAMA Cardiol. 2016;1:594–599. DOI: 10.1001/jamacardio.2016.1326. [DOI] [PubMed] [Google Scholar]
- 6.Nelson S, Whitsel L, Khavjou O, Phelps D, Leib A. Projections of cardiovascular disease prevalence and costs: 2015–2035 - Technical Report. http://www.heart.org/idc/groups/heart-public/@wcm/@adv/documents/downloadable/ucm_491513.pdf. Accessed: February 17, 2017.
- 7.Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M, Pletcher MA, Smith AE, Tang K, Yuan CW, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet. 2018;392:2052–2090. DOI: 10.1016/S0140-6736(18)31694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, Horst C, Kaldjian A, Matyasz T, Scott KW, et al. US Health Care Spending by Payer and Health Condition, 1996–2016. JAMA. 2020;323:863–884. DOI: 10.1001/jama.2020.0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dieleman JL, Baral R, Birger M, Bui AL, Bulchis A, Chapin A, Hamavid H, Horst C, Johnson EK, Joseph J, et al. US Spending on Personal Health Care and Public Health, 1996–2013. JAMA. 2016;316:2627–2646. DOI: 10.1001/jama.2016.16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dieleman JL, Squires E, Bui AL, Campbell M, Chapin A, Hamavid H, Horst C, Li Z, Matyasz T, Reynolds A, et al. Factors Associated With Increases in US Health Care Spending, 1996–2013. JAMA. 2017;318:1668–1678. DOI: 10.1001/jama.2017.15927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheiner L Health spending growth: The effects of the great recession. https://www.brookings.edu/wp-content/uploads/2016/06/HealthSpendingGrowth.pdf. Accessed: November 6, 2020.
- 12.Cutler DM, Ghosh K, Messer KL, Raghunathan TE, Stewart ST, Rosen AB. Explaining The Slowdown In Medical Spending Growth Among The Elderly, 1999–2012. Health Aff (Millwood). 2019;38:222–229. DOI: 10.1377/hlthaff.2018.05372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunn A, Rittmueller L, Whitmire B. Health Care Spending Slowdown From 2000 To 2010 Was Driven By Lower Growth In Cost Per Case, According To A New Data Source. Health Aff (Millwood). 2016;35:132–140. DOI: 10.1377/hlthaff.2015.1109. [DOI] [PubMed] [Google Scholar]
- 14.Roehrig C Mental Disorders Top The List Of The Most Costly Conditions In The United States: $201 Billion. Health Aff (Millwood). 2016;35:1130–1135. DOI: 10.1377/hlthaff.2015.1659. [DOI] [PubMed] [Google Scholar]
- 15.Roehrig C, Miller G, Lake C, Bryant J. National health spending by medical condition, 1996–2005. Health Aff (Millwood). 2009;28:w358–w367. DOI: 10.1377/hlthaff.28.2.w358. [DOI] [PubMed] [Google Scholar]
- 16.Siscovick DS, Barringer TA, Fretts AM, Wu JH, Lichtenstein AH, Costello RB, Kris-Etherton PM, Jacobson TA, Engler MB, Alger HM, et al. Omega-3 Polyunsaturated Fatty Acid (Fish Oil) Supplementation and the Prevention of Clinical Cardiovascular Disease: A Science Advisory From the American Heart Association. Circulation. 2017;135:e867–e884. DOI: 10.1161/CIR.0000000000000482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.GBD Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. DOI: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Preston S, Heuveline P, Guillot M. Basic concepts and measures. demography: measuring and modeling population processes. Oxford: Blackwell Publishing Ltd; 2001. [Google Scholar]
- 19.Gupta PD. Standardization and decomposition of rates: a user’s manual. Washington, DC: US Bureau of the Census; 1993. [Google Scholar]
- 20.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141:e139–e596. DOI: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 21.Bernard D, Cowan C, Selden T, Cai L, Catlin A, Heffler S. Reconciling medical expenditure estimates from the MEPS and NHEA, 2007. Medicare Medicaid Res Rev. 2012;2:mmrr.002.04.a09. DOI: 10.5600/mmrr.002.04.a09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Riley RF, Don CW, Powell W, Maynard C, Dean LS. Trends in coronary revascularization in the United States from 2001 to 2009: recent declines in percutaneous coronary intervention volumes. Circ Cardiovasc Qual Outcomes. 2011;4:193–197. DOI: 10.1161/CIRCOUTCOMES.110.958744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aitken M, Berndt ER, Cutler DM. Prescription drug spending trends in the United States: looking beyond the turning point. Health Aff (Millwood). 2009;28:w151–w160. DOI: 10.1377/hlthaff.28.1.w151. [DOI] [PubMed] [Google Scholar]
- 24.Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. JAMA. 2011;305:1769–1776. DOI: 10.1001/jama.2011.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amin AP, Patterson M, House JA, Giersiefen H, Spertus JA, Baklanov DV, Chhatriwalla AK, Safley DM, Cohen DJ, Rao SV, et al. Costs Associated With Access Site and Same-Day Discharge Among Medicare Beneficiaries Undergoing Percutaneous Coronary Intervention: An Evaluation of the Current Percutaneous Coronary Intervention Care Pathways in the United States. JACC Cardiovasc Interv. 2017;10:342–351. DOI: 10.1016/j.jcin.2016.11.049. [DOI] [PubMed] [Google Scholar]
- 26.Every NR, Spertus J, Fihn SD, Hlatky M, Martin JS, Weaver WD. Length of hospital stay after acute myocardial infarction in the Myocardial Infarction Triage and Intervention (MITI) Project registry. J Am Coll Cardiol. 1996;28:287–293. DOI: 10.1016/0735-1097(96)00168-4. [DOI] [PubMed] [Google Scholar]
- 27.Fang J, Alderman MH, Keenan NL, Ayala C. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. Am J Med. 2010;123:259–266. DOI: 10.1016/j.amjmed.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 28.Krumholz HM, Normand ST, Wang Y. Twenty-Year Trends in Outcomes for Older Adults With Acute Myocardial Infarction in the United States. JAMA Netw Open. 2019;2:e191938. DOI: 10.1001/jamanetworkopen.2019.1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spencer FA, Lessard D, Gore JM, Yarzebski J, Goldberg RJ. Declining length of hospital stay for acute myocardial infarction and postdischarge outcomes: a community-wide perspective. Arch Intern Med. 2004;164:733–740. DOI: 10.1001/archinte.164.7.733. [DOI] [PubMed] [Google Scholar]
- 30.Andrus BW, Welch HG. Medicare services provided by cardiologists in the United States: 1999–2008. Circ Cardiovasc Qual Outcomes. 2012;5:31–36. DOI: 10.1161/CIRCOUTCOMES.111.961813. [DOI] [PubMed] [Google Scholar]
- 31.Kalman NS, Hammill BG, Schulman KA, Shah BR. Hospital overhead costs: the neglected driver of health care spending? J Health Care Finance. 2015;41:1–15. [Google Scholar]
- 32.Gurwitz JH, Maurer MS. Tafamidis-A Pricey Therapy for a Not-So-Rare Condition. JAMA Cardiol. 2020;5:247–248. DOI: 10.1001/jamacardio.2019.5233. [DOI] [PubMed] [Google Scholar]
- 33.Maurer MS, Schwartz JH, Gundapaneni B, Elliott PM, Merlini G, Waddington-Cruz M, Kristen AV, Grogan M, Witteles R, Damy T, et al. Tafamidis Treatment for Patients with Transthyretin Amyloid Cardiomyopathy. N Engl J Med. 2018;379:1007–1016. DOI: 10.1056/NEJMoa1805689. [DOI] [PubMed] [Google Scholar]
- 34.Cuddy SAM, Coyle ML, Falk RH. Initial Monthly Cost of Tafamidis-the Real Price for Patients. JAMA Cardiol. 2020;5:847–848. DOI: 10.1001/jamacardio.2020.0863. [DOI] [PubMed] [Google Scholar]
- 35.Kazi DS, Bellows BK, Baron SJ, Shen C, Cohen DJ, Spertus JA, Yeh RW, Arnold SV, Sperry BW, Maurer MS, et al. Cost-Effectiveness of Tafamidis Therapy for Transthyretin Amyloid Cardiomyopathy. Circulation. 2020;141:1214–1224. DOI: 10.1161/CIRCULATIONAHA.119.045093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jia X, Akeroyd JM, Nasir K, Nambi V, Ballantyne CM, Petersen LA, Virani SS. Eligibility and Cost for Icosapent Ethyl Based on the REDUCE-IT Trial. Circulation. 2019;139:1341–1343. DOI: 10.1161/CIRCULATIONAHA.118.038691. [DOI] [PubMed] [Google Scholar]
- 37.Ayanian JZ, Epstein AM. Differences in the use of procedures between women and men hospitalized for coronary heart disease. N Engl J Med. 1991;325:221–225. DOI: 10.1056/NEJM199107253250401. [DOI] [PubMed] [Google Scholar]
- 38.Blomkalns AL, Chen AY, Hochman JS, Peterson ED, Trynosky K, Diercks DB, Brogan GX Jr., Boden WE, Roe MT, Ohman EM, et al. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45:832–837. DOI: 10.1016/j.jacc.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 39.Daugherty SL, Peterson PN, Magid DJ, Ho PM, Bondy J, Hokanson JE, Ross CA, Rumsfeld JS, Masoudi FA. The relationship between gender and clinical management after exercise stress testing. Am Heart J. 2008;156:301–307. DOI: 10.1016/j.ahj.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 40.Tobin JN, Wassertheil-Smoller S, Wexler JP, Steingart RM, Budner N, Lense L, Wachspress J. Sex bias in considering coronary bypass surgery. Ann Intern Med. 1987;107:19–25. DOI: 10.7326/0003-4819-107-1-19. [DOI] [PubMed] [Google Scholar]
- 41.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373:2117–2128. DOI: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 42.Centers for Medicare and Medicaid Services. National Health Expenditure Accounts Historical. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical.html. Accessed: February 1, 2017.
- 43.International Monetary Fund. World Economic Outlook. https://www-imf-org.offcampus.lib.washington.edu/external/pubs/ft/weo/2015/01/weodata/index.aspx. Accessed: February 17, 2017.
- 44.World Health Organization. Health Accounts methodology. https://www.who.int/healthaccounts/methodology/en/. Accessed: August 31, 2019.
- 45.Centers for Medicare and Medicaid Services. Quick Definitions for National Health Expenditure Accounts Categories. http://www.cms.gov/Research-Statistics-Data-andSystems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/quickref.pdf. Accessed: May 12, 2015.
- 46.Gupta PD. Decomposition of the difference between two rates and its consistency when more than two populations are involved. Mathematical Population Studies. DOI: 1991;3:105–125. 10.1080/08898489109525329. [DOI] [Google Scholar]
- 47.Iglewicz B, Hoaglin DC. How to Detect and Handle Outliers. Milwaukee, WI, USA: ASQC Quality Press; 1993. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


