Abstract
The long-term consequences of exposure to firearm injury – including suicide, assault, and mass shootings – on children’s mental and physical health is unknown. Using PRISMA-ScR guidelines, we conducted a scoping review of four databases (PubMed, Scopus, PsychINFO, and CJ abstract) between January 1, 1985 and April 2, 2018 for articles describing long-term outcomes of child or adolescent firearm injury exposure (n=3582). Among included studies (n=31), most used retrospective cohorts or cross-sectional studies to describe the correlation between firearm injury and post-traumatic stress. A disproportionate number of studies examined the effect of mass shootings, although few of these studies were conducted in the United States and none described the impact of social media. Despite methodologic limitations, youth firearm injury exposure is clearly linked to high rates of post-traumatic stress symptoms and high rates of future injury. Evidence is lacking on best practices for prevention of mental health and behavioral sequelae among youth exposed to firearm injury. Future research should use rigorous methods to identify prevalence, correlates, and intervention strategies for these at-risk youth.
Keywords: firearm, suicide, mass shooting, accidental injury, community violence, post-traumatic stress
Introduction
Firearm related deaths are the second leading cause of injury-related death in United States children and adolescents (Cunningham, Walton, & Carter, 2018) and a major global health burden (Naghavi et al., 2018). Most childhood firearm deaths result from suicide (38%) and homicide (53%); most non-fatal childhood firearm injuries, in contradiction, are due to assault or unintentional causes (Fowler et al., 2017; Srinivasan, Mannix, & Lee, 2014). An increasing number of children and adolescents (hereafter referred to as “youth” and referring to the age range of 0–17) are exposed to others’ injuries by firearms, with recent studies reporting that 5% of youth have directly witnessed a shooting in the past year (Finkelhor et al., 2015) and suggesting an increasing prevalence of mass shootings (Rand Corporation, 2018). The number of American youth who have access to firearms may also have increased in recent years (Karp, 2018; Levine & McKnight, 2017).
Youth injury by, or exposure to others’ injury by, firearms likely has multiple long-term behavioral and physical health consequences, ranging from post-traumatic stress, to substance use, to recurrent injury. Violent injuries, in general, are associated with higher rates of post-injury mental health symptoms and recurrent injury compared with non-violent injury (Cunningham et al., 2015; Fowler et al., 2009; Santiago et al., 2013; Shih et al., 2010). Exposure to violence (e.g., seeing high rates of violence in one’s community; parental domestic violence) is also associated with multiple negative long-term consequences (Bair-Merritt, Blackstone, & Feudtner, 2006)., including epigenetic changes (Jovanovic et al., 2017). However, firearm injury exposure of all types – including unintentional (“accidental”) injury, suicide, homicide or assault injuries, and mass shootings – may be qualitatively different from that of other types of violent injury, in that it is more likely to be life-threatening or lethal, may be associated with higher risk of future injury, and may threaten youths beliefs about the safety of their environment (Fowler et al., 2009). They may also contribute to adverse childhood experiences, a known It is also likely that the effects of firearm injury exposure on youth differ from those on adults, given developmental and biological differences (Benson & Elder Jr, 2011).
For instance, data from studies with adults suggests that a prior firearm injury significantly increases risk of future injury of all types, but particularly increases the risk of future firearm injury (Rowhani-Rahbar et al., 2015). A youth’s exposure to firearm injury in one’s community (regardless of the type) may engender greater fear and sense of danger than exposure to other types of violence (Netburn, 2018). Risk and protective factors for negative consequences (such as substance use, anxiety, and recurrent injury) may differ for firearm injury; for instance, in young adults, certain genetic variants correlate with risk of post-traumatic stress after exposure to a mass shooting (Mercer et al., 2012). Finally, simply identifying the consequences of firearm injury is insufficient; it is also important to understand how best to prevent these negative consequences from developing. Others have examined effect of interventions directed toward youth with all types of assault injury (Cheng et al., 2008; Walton et al., 2010), or towards adults with other types of injuries (Heinze et al., 2016). The effects of such interventions on firearm injury-exposed youth are largely unknown. Additionally, the effect of youth firearm injury exposure on their parents – and how best to engage parents to reduce long-term sequelae among youth – is, to our knowledge, unknown. This gap is particularly important given that parental PTSD is associated with worse childhood outcomes, and familial interventions have the potential to increase youth resilience in the face of firearm injury (Samuelson et al., 2017; Wise & Delahanty, 2017).
The Institute of Medicine developed a research agenda for firearm injury prevention after the mass shooting at Sandy Hook Elementary School in 2012 (Council, 2013), and similar agendas have been developed by other professional bodies (Ranney et al., 2017; Talley et al., 2018). Notable elements of these reports are the lack of evidence regarding long-term sequelae of firearm injuries and appropriate prevention thereof, as well as the lack of specific focus on youth firearm injury. To address the perceived lack of data on the behavioral and physical sequelae of firearm injury, and the prevention thereof, in youth, we conducted a scoping review of the literature. For the purpose of this review, we defined “long-term” sequelae of injury as those occurring 1+ month after injury (in concordance with definitions of post-traumatic stress disorder). The objective of this review, as recommended by established frameworks (Arksey & O’Malley, 2005), is to provide a summary of the existing literature within this area and identify gaps in the literature to set a research agenda moving forward.
Methods
Database Searches
Using PRISMA-ScR guidelines, we conducted a scoping review of four databases (PubMed, Scopus, PsychINFO, and CJ abstract) for English-language original research articles published between January 1, 1985 and May 25, 2018 that described longitudinal outcomes of child or adolescent firearm injury exposure, or the prevention thereof. The initial search was created in PubMed; searches in other databases were translations of that search (see APPENDIX for exemplar search strategy in PubMed). To enhance the scope of the search, researchers also reviewed reference lists of included articles, and forward citations of included articles were searched in Scopus. Dates of search and eligibility criteria were determined through consensus among our workgroup, which was part of the larger Firearm-safety Among Children and Teens (FACTS) Consortium (an NIH-funded consortium which aims to define new directions for youth firearm injury prevention research).
Eligibility Criteria
Inclusion criteria included original scientific articles focusing on either youth (age 0–17) or their parents that described consequences rather than precedents of firearm injury. We defined firearm injury “exposure” as personal injury or exposure to injury of another person by a firearm (including witnessing it or being in the same community); if a manuscript included populations with other types of injuries, we required that at least 1/3 of the population had a firearm-related injury. We defined a “focus on youth or their parents” as having at least 1/3 of the study population as youth age ≤ 17 years old. Exemplars of potential outcomes of firearm injury included medical, psycho-social, behavioral, injury-related, and criminal justice consequences, on either an individual or community level, following fatal or non-fatal youth firearm injury or exposure to such firearm injury. Exemplars of secondary prevention of firearm injury included any interventions to reduce risk of poor behavioral or physical health outcomes among youth after a firearm injury or exposure to such injury. We included articles from outside of the United States. We excluded non-English-language articles, studies describing patterns of injury as a primary outcome, policy studies, opinion pieces, review articles (although these were reviewed for references), studies describing airsoft guns or BB guns, and studies focusing on consequences of war given that firearm injury occurring within the war context reflects a broader societal conflict and is often associated with other traumas
Article Selection
All titles and abstracts were reviewed, independently and blindly, by at least two independent reviewers using the web-based program Rayyan (Ouzzani et al., 2016). The first 100 articles were reviewed by all authors, and discrepancies were discussed to ensure consensus. After the group achieved consensus, all further articles were reviewed, independently and blindly, by two independent reviewers (RK and KB). During the title and abstract screening, the independent reviewers erred on inclusion. Conflicting decisions among reviewers were discussed by the full team until consensus was reached. Full text articles were then independently reviewed for inclusion by two reviewers (various permutations of RK, KB, RB, and MR), with discrepancies again resolved through consensus discussion.
Data Extraction and Quality Ratings
A standard data abstraction form was created and refined by the authorship group using one agreed-upon full text article. This abstraction form captured the following data fields: country in which study was conducted, type of firearm injury studied, design, population, sample size, primary and secondary outcomes, main findings, and limitations. In keeping with other literature (Ranney et al., 2017), the independent variable of firearm injury was divided into the following types: peer and partner violence (i.e., homicide, non-fatal assault injury); suicide; mass shootings; unintentional injury; and other or multiple types of firearm injury. For each full-text review, data was abstracted into the form by one reviewer, and then verified by a second. Included studies were assessed for methodological quality using the “Risk of Bias” tools, as recommended by the Cochrane Collaborative (Higgins et al., 2016; Sterne et al., 2016). Given the heterogeneity of findings, qualitative summaries were made of all data.
Results
Search strategy identified a total of 3,582 articles (Figure 1). After removal of duplicates, 2,246 files were reviewed by title and abstract for potential inclusion. Of these, 59 abstracts were retained for full text review and forward citation searches. Twelve additional articles were included based on forward citations. After full text review, a total of 31 articles met full eligibility criteria and were included in the final sample for the scoping review.
Figure 1:
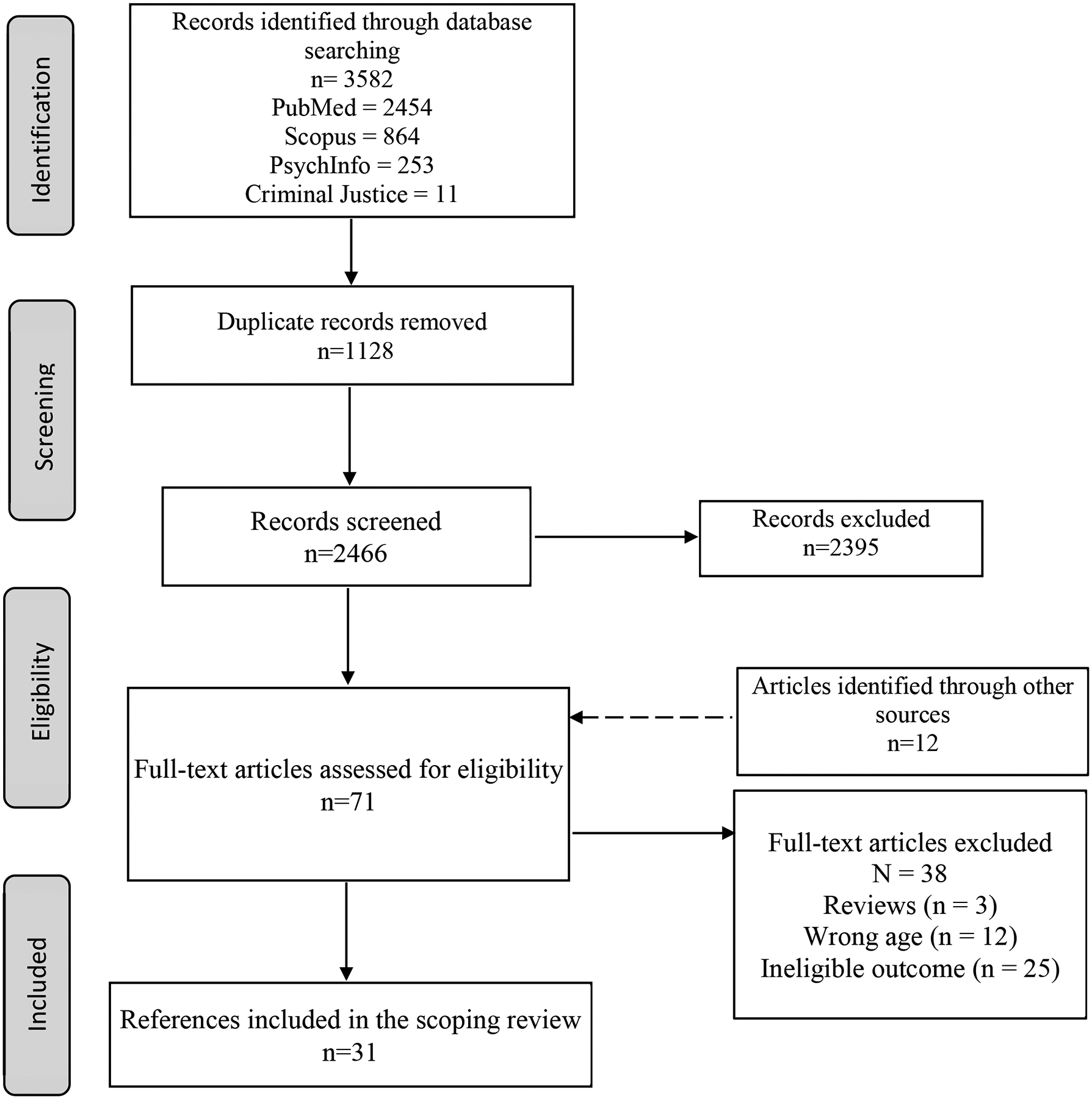
Flow Diagram of Article Selection for Scoping Review
The included manuscripts were categorized according to the type of youth firearm injury exposure: peer and partner violence (“assault” or “community violence”) (16%, n=5), suicide or suicide attempts (10%, n=3), mass shooting (45%, n=14), unintentional injury (3%, n=1) and studies that included multiple types of firearm injury (26%, n=8). Two-thirds of manuscripts (n=21) described the behavioral health sequelae of firearm violence, with the majority of focusing on post-traumatic stress symptoms. Sixteen percent (n=5) of the included manuscripts described physical health sequelae of firearm injury (e.g., headaches), and 32% (n=10) described patterns of recurrent injury (“recidivism”) following youth firearm injury. Only one article described outcomes of a secondary prevention intervention for firearm injury-exposed youth. All of the community firearm injury and suicide firearm injury-related articles, and all but one of the mixed or other types of firearm injury articles, used data from the U.S. Other articles originated from Norway (n=6, all describing outcomes of the same mass shooting event), Sweden (n=2), and Finland (n=3). Table 1 summarizes the characteristics of the reviewed study including type of firearm exposure, country of origin, and type of sequelae studied. Table 2 provides further details for each individual study including study design, outcome measures, relevant findings, and quality assessment.
Table 1:
Overview
| Type of Outcome | ||||||
|---|---|---|---|---|---|---|
| Type of Firearm Exposure | First Author (Year) | Country | Mental Health | Injury Recidivism | Physical Health | Other |
| Peer/Partner Violence | Carter, PM (2015) | United States | ✓ | |||
| Chong, VE (2015a) | United States | ✓ | ||||
| Chong, VE (2015b) | United States | ✓ | ||||
| Davis, J (2013) | United States | ✓ | ||||
| Tellez, MG (1995) | United States | ✓ | ||||
| Suicide and Self-Harm | Brent, DA (1993a) | United States | ✓ | |||
| Brent, DA (1993b) | United States | ✓ | ||||
| Olfson, M (2018) | United States | ✓ | ||||
| Mass Shooting | Bugge, I (2015) | Norway | ✓ | |||
| Dyb, G (2014) | Norway | ✓ | ✓ | |||
| Hafstad, GS (2014) | Norway | ✓ | ||||
| Haravuori, H (2011) | Finland | ✓ | ||||
| Haravuori, H (2016) | Finland | ✓ | ||||
| Hawkins, NA (2008) | United States | ✓ | ||||
| Nader (1990) | United States | ✓ | ||||
| Omar, HA (1999) | United States | ✓ | ||||
| Pynoos (1987) | United States | ✓ | ||||
| Schwarz, ED (1991) | United States | ✓ | ||||
| Stene, LE (2015) | Norway | ✓ | ||||
| Stensland, SO (2018) | Norway | ✓ | ||||
| Suomalainen, L. (2011) | Finland | ✓ | ||||
| Thoresen, S (2016) | Norway | ✓ | ||||
| Unintentional Injury | Ponzer, S (1997) | Sweden | ✓ | ✓ | ✓ | |
| Unspecified or Multiple Intent | Bergman, B (1996) | Sweden | ✓ | ✓ | ✓ | ✓ |
| Boynton-Jarrett, R (2008) | United States | ✓ | ✓ | |||
| Carter, PM (2017) | United States | ✓ | ||||
| Gibson, PD (2016) | United States | ✓ | ||||
| Gill, AC (2002) | United States | ✓ | ||||
| Hamrin, V (1998) | United States | ✓ | ||||
| Hamrin, V (2004) | United States | ✓ | ||||
| Slovak, K (2001) | United States | ✓ | ||||
Table 2:
Synthesis of Results, According to Type of Firearm Exposure and Type of Study
| First author (year) | Population | Sample Size | Primary Outcome | Main Findings | Limitations/Notable Strengths | |
|---|---|---|---|---|---|---|
| Peer/Partner Violence | ||||||
| Retrospective Cohort | Chong, VE (2015a) | Patients treated at trauma center for injuries due to interpersonal violence between 2005–2010, median age 20 | 1,890 | Recurrent violent injury |
|
Single center; approximation of socioeconomic status; chart review |
| Davis, J.S. (2013) | All patients admitted to a level 1 pediatric trauma center with violent injury between 1991 and 2010, age 0–19 | 12,235 | Recurrent violent injury |
|
Single center; chart review | |
| Tellez, M.G. (1995) | Admissions to trauma center for violent injury from 1991–1993, age <25 | 552 | Characteristics of recidivists, cost of reinjury |
|
Single center; chart review | |
| Prospective Cohort (with random control group) | Carter, P.M. (2015) | 14-to-24-year-olds with drug use in the past 6 months presenting to urban trauma center with assault injury (n=349; n=70 with firearm injury) matched to 250 controls (drug-using nonassaulted youth) | 599 | Subsequent firearm aggression or victimization within 24 months of baseline assessment |
|
Single center (but extremely high follow-up) |
| Sensitivity analysis | Chong, V.E. (2015b) | Markov model of outcomes of patients aged 12 to 20 presenting to urban trauma center with violent firearm injury, based on examination of all patients treated for violent injury 2005–2008 | 155 | One year violent injury recidivism; cost-effectiveness |
|
Non-randomized convenience sample; single center; unreported follow-up rate |
| Suicide and Self-Harm | ||||||
| Retrospective Cohort | Brent, DA (1993a) | Close friends and acquaintances of 26 adolescent suicide victims between 1988–1991, age-race-gender matched to controls from communities without recent adolescent suicides | 146 | Depression (K-SADS-E), PTSD (PTSD-RI), suicidal ideation and attempts, in the 7 months following peer suicide |
|
Low participation rate (but standardized interviews) |
| Brent, DA (1993b) | 28 high school students exposed to a peer suicide on a bus compared to 28 demographically similar peers from another community | 56 | Depression/Anxiet y (K-SADS-E), PTSD (Post Traumatic Stress Disorder Reaction Inventory) assessed 2 months after event |
|
Small sample (but Standardized interviews) | |
| Olfson, M. (2018) | 12–24 year olds in Medicaid Analytic Extract from 2001–2007 with clinical diagnosis of self-harm | 32,395 | Repeat non-fatal self-harm or suicide in the year following index event |
|
Limited to patients receiving Medicaid; relies on hospital billing codes (but excellent outcome capture) | |
| Mass Shooting | ||||||
| Qualitative or cross-sectional | Hawkins, N.A. (2008) | Students (age 15–17) and parents (age 41–49) from Columbine High School in 1999 | 11 | Qualitative analysis of emotional, cognitive, social responses in the weeks following the shooting |
|
Small convenience sample; non-standard qualitative methods |
| Nader (1990) | Long-term follow up of the original sample from Pynoos (1987) | 100 | Score on the DSM-III PTSD Reaction Index 14 months following the sniper attack |
|
Non-systematic sample (but validated assessments) | |
| Omar, H.A. (1999) | Students age 15–17 from 2 high schools in Lexington, KY | 412 | Emotional responses 10 days following Columbine shooting |
|
Convenience sample; non-standardized assessments | |
| Pynoos (1987) | Students (age 5–13) exposed to a sniper attack on the school playground | 159 | Score on the DSM-III PTSD Reaction Index one month following the sniper attack |
|
Non-systematic sample (but validated assessments) | |
| Schwarz, E.D. (1991) | Children and adults exposed to shooting at an “upper middle class” suburban elementary school | 128 | PTSD at 8–14 months post-shooting (DSM III criteria), using self-report measures |
|
Non-systematic sample (but validated assessments) | |
| Prospective Cohort | Bugge, I. (2015) | Survivors of 2011 mass shooting at youth summer camp in Norway | 325 | Post traumatic stress symptoms (measured using PTSD-RI) |
|
Non-systematic sample (but validated assessments) |
| Dyb, G. (2014) | Survivors of 2011 mass shooting at youth summer camp in Norway | 325 | Correlation between use of by nationally deployed mental health services and mental health symptoms (post-traumatic stress, depression/anxiety, and somatic illness) |
|
Non-systematic sample (but validated assessments) | |
| Hafstad, GS (2014) | Survivors of 2011 mass shooting at youth summer camp in Norway | 325 | Post traumatic stress disorder, measured using PTSD-RI (DSM IV and V criteria) |
|
Non-systematic sample (but validated assessments) | |
| Haravuori, H (2011) | Survivors of 1 school shooting in Finland in 2007, compared to youth from another high school | 231/526 | Post traumatic stress symptoms (measured using Impact of Events Scale) |
|
Non-systematic sample (but validated assessments) | |
| Haravuori, H (2016) | Survivors of 2 school shootings in Finland in 2007 and 2008, mean age 17.6 | 228 | Post Traumatic Stress Disorder (assessed using K-SADS-PL) |
|
Non-systematic sample (but validated assessments) | |
| Stene, L. E. (2015) | Survivors of 2011 mass shooting at youth summer camp in Norway | 285 | Health services utilization and mental health symptoms |
|
Non-systematic sample (but validated assessments) | |
| Stensland, S.O. (2018) | Survivors of 2011 mass shooting at youth summer camp in Norway, matched to controls from population based Young-HUNT3 study | 1,917 | Recurrent migraine and tension-type headache |
|
Non-systematic sample (but validated assessments) | |
| Suomalainen, L. 2011 | Survivors of 1 school shooting in Finland in 2007, compared to youth from another high school | 231/526 | Post traumatic stress symptoms (measured using Impact of Events Scale) |
|
Non-systematic sample (but validated assessments) | |
| Thoresen, S (2016) | Parents of survivors of 2011 youth mass shooting in Norway | 531 | Post traumatic stress symptoms and depression/anxiety assessed at 4–5 months and 14–15 months following the event, using self-report measures (PTSD-RI and HSCL) |
|
Non-systematic sample (but validated assessments) | |
| Unintentional Injury | ||||||
| Retrospective Cohort | Ponzer, S. (1997) | All non-fatal accidental firearm injuries in children under 18 in Stockholm from 1972–1993 (n=141), age and gender matched to controls, mean age 13.2 | 282 | Injury recidivism, hospitalization, conviction of crime |
|
Determination of intent by chart review (but systematic sample, excellent follow-up) |
| Unspecified/Mixed | ||||||
| Cross sectional | Slovak, K. (2001) | Rural public school students in grades 3–8 in 1998 in Ohio, mean age 11.4 | 549 | Anxiety, depression, PTSD, anger, dissociation (measured by Trauma Symptom Checklist for Children) |
|
Cross-sectional (but strong sampling, validated assessments) |
| Retrospective Cohort | Carter, P.M. (2017) | Children <19 yo presenting to 16 Pediatric Emergency Departments between 2004–2008 with firearm injuries of any type | 1,758 | Recurrent injury in the next 12 months |
|
Chart review (but multi-center) |
| Gill, A.C. (2002) | Pediatric patients 12 months-17 years treated at a multidisciplinary trauma clinic following hospitalization for traumatic injury, mean age 8.55 | 337 | Post traumatic stress disorder (DSM IV) |
|
Single site; only hospitalized patients presenting to trauma clinic | |
| Prospective Cohort | Bergman, B. (1996) | All non-fatal pediatric firearm injuries from 1972–1993 in Stockholm, age and gender matched to uninjured controls, mean age 13.9 yrs | 192 | Recurrent injury, hospitalization due somatic injury or psychiatric illness, conviction of crime |
|
Chart review (but excellent follow-up rates) |
| Boynton-Jarrett, R. (2008) | NLSY- Nationally representative sample of adolescents aged 12–18 at baseline followed for 8 years (1997–2004) | 8,224 | Self-rated health (SRH) |
|
Non-validated measures of gun violence exposure (but strong sampling methods) | |
| Gibson, P.D. (2016) | Patients 0–18 presenting evaluated by the trauma service for any type of firearm injury from 2000–2011 | 896 | Recurrent firearm injury |
|
Single center, non-standard follow-up | |
| Hamrin, V. (1998) | All patients admitted to pediatric trauma center from June 1994-Sept 1995 with firearm-related injury, ages 11–15 | 16 | Acute stress disorder (DSM III criteria) |
|
Small sample; likely assessing trauma prior to the event as assessed too early for ASD | |
| Hamrin, V. (2004) | Patients admitted to pediatric trauma center for firearm injury between 1995–1999, matched to medically hospitalized controls, mean age 14.7 | 56 | Acute stress disorder (ASDS) (measured by Child Posttraumatic Stress Disorder Reaction Index) |
|
Convenience sample; non-standardized assessment; assessed too early for ASD |
Below, we describe qualitative conclusions from this scoping review about long-term behavioral and physical sequelae of youth firearm injury, and the prevention of such consequences, divided by the type of firearm violence exposure. We also comment on particular methodologic strengths and weaknesses of the reviewed literature.
Peer and Partner Violence
Seven manuscripts included in this scoping review described the longitudinal consequences of peer or partner firearm injury among youth who presented to a hospital for care of this injury. The majority (n=4) of these manuscripts were prospective or retrospective cohort studies examining rates and/or predictors of future injury following an initial firearm injury event. In all of these manuscripts, children and adolescents with an index firearm-related injury were significantly more likely to experience a subsequent injury compared to those who presented with other types of violent injury, or compared to those who presented to the hospital for other reasons (Carter et al., 2015; Chong, Lee, & Victorino, 2015; Davis et al., 2013; Tellez et al., 1995). However, many of these studies were limited by multiple potential biases in study design (including convenience samples, potential missed outcomes, and unmeasured confounders). The Carter (2015) study was notable for systematic recruitment strategies, a well-designed comparison group, high follow-up rates, and standardized assessment methodologies.
A single study reported the outcomes of an intervention directed at hospitalized gunshot wound patients (mean age 17.8 years) (Chong, Smith, et al., 2015). This study examined frequency of recurrent hospitalization for a violent injury among youth enrolled in a hospital-based violence intervention program (HVIP) after a violent firearm injury, compared to youth receiving usual care after a violent firearm injury. They found no significant intervention effects. Conclusions were limited by the fact that patient enrollment was non-randomized (with multiple potential biases in assignment to one intervention group versus the other) and due to limitations in follow-up and outcome assessment.
No manuscripts described longitudinal consequences or secondary prevention of adolescent firearm injury exposures related to dating violence or family violence.
Suicide and Self-Harm
Of the three manuscripts in this scoping review that described consequences of firearm suicide, one examined the prevalence of repeat self-injury or suicide following an initial presentation for self-harm with a firearm. Olfson (2018) used a large, nationally representative cohort of adolescents insured by Medicaid who presented to the hospital with a self-harm injury and survived the initial injury. Among this sample, adolescents who were seen for self-injury using firearms were significantly more likely to die from suicide within a year compared to adolescents who presented with other forms of self harm (hazard ratio 33.45, 95% CI 13.31–84.06) (Olfson et al., 2018). The other 2 manuscripts described the longitudinal consequences of a peer firearm suicide; both reported that adolescents exposed to peer firearm suicide (either through directly witnessing it, or through community affiliation or peer network affiliation with the decedent) had higher subsequent rates of depression, anxiety, PTSD, and suicidal thoughts (Brent et al., 1993a; Brent et al., 1993b). These studies, however, were limited by small number and by the nature of the case-control design.
Mass Shooting
Of the 14 manuscripts in this scoping review that examined the sequalae of mass shooting events, the majority (64%) were studies conducted outside the U.S. Of the 5 studies conducted within the US, all data collection was prior to the year 2000. All except one study used quantitative assessments; most used validated assessments of mental health symptoms, but all used a non-systematic sample of exposed youth.
In general, among youth directly exposed to a mass shooting, rates of post-traumatic stress assessed using standardized assessments were consistently significantly higher compared to control populations. The rate of post-traumatic stress ranged from 11% to 62%, depending on the type of assessment used, nature of the exposure, and the time from the traumatic event (Bugge et al., 2015; Hafstad et al., 2014; Haravuori et al., 2011; Schwarz & Kowalski, 1991; Suomalainen et al., 2011). Physical proximity to the shooting correlated with severity of post-traumatic stress at one month and one year following the event (Nader et al., 1990; Pynoos et al., 1987a; Pynoos et al., 1987b). Media exposure to an event did not correlate with severity of post-traumatic stress symptoms (Haravuori et al., 2011).
Six manuscripts included in this scoping review specifically reported on sequelae of a 2011 mass shooting at a summer camp for adolescents on a small island in Norway, in which 69 people were killed, and 495 survived (many of whom sustained nonfatal injuries). Following the attacks, a nationally coordinated program was initiated to screen survivors and provide necessary health and psychosocial services. Almost 87% of the survivors reported having contact with the outreach team, and 73% received specialized mental health services (Dyb et al., 2014). Almost all survivors (95%) reported having contact with any health care service following the attack (Stene & Dyb, 2015). Rates of post-traumatic stress disorder following the event were found to be between 11–12% by conservative criteria (Hafstad et al., 2014). Survivors had significantly higher rates of migraines (OR 6.1) and tension-type headaches (OR 4.67), as well as a higher frequency of headaches (OR 4.51) compared to the general population (Stensland et al., 2018).
Other studies reported high rates of anxiety and sadness among youth in the community of the shooting, parents in the community of a shooting, and in communities exposed to media reports about the shooting (Hawkins et al., 2007; Omar, 1999; Schwarz & Kowalski, 1991). A single non-U.S. based study reported that survivors of a mass shooting had no difference in rates of substance abuse, after adjustment for overall mental health (Suomalainen et al., 2011). Parents of survivors had five times higher post-traumatic stress and two times higher depressive symptoms than parents of the general population in a single study based on the Norway mass shooting (Thoresen et al., 2016).
No studies described the sequelae of mass shootings for teachers or healthcare providers who care for the exposed youth.
Unintentional Injury
Our review identified one manuscript that specifically examined the longitudinal effects of unintentional firearm injury. This study, conducted using population-wide databases in Sweden with average follow-up period of 10 years, reported that childhood victims of unintentional firearm injury were more likely to have future hospitalizations for violent injury (OR 2.42) and for other disease processes (OR 4.0), were more likely to be perpetrators of crimes such as assault (OR 6.33), and more likely to be imprisoned (OR 14.0) (Ponzer et al., 1997). Although the use of a national database for longitudinal outcomes was a major strength of the study, the primary limitation of this study is that it relied on medical chart review to determine the intent of the injury, thus potentially misclassifying assault related injuries.
General Firearm Injury Exposure
Of the remaining eight manuscripts, the type of firearm exposure was either not specified, or was explicitly defined as a mix of firearm assault (peer or partner), self-harm, and unintentional firearm injury. Among these manuscripts, six reported on mental health sequelae of firearm injury; these manuscripts all reported high levels of post traumatic stress symptoms, including acute stress disorder, depression, and anxiety (Gill, 2002; Hamrin, 1998; Hamrin, Jonker, & Scahill, 2004; Slovak & Singer, 2001); high levels of somatic disease (Bergman, Ponzer, & Brismar, 1996); and low overall self-rated health (Boynton-Jarrett et al., 2008). Recurrent injury following both unintentional and intentional assault injury were high (Bergman et al., 1996; Carter et al., 2017; Gibson et al., 2016), although rates of recurrent firearm injury were low (Carter et al., 2017). Firearm injury was also associated with higher risk of future criminal convictions (Bergman et al., 1996). With the exception of Bergman and Carter, most studies were limited by high risk of confounding in inclusion or outcomes measurements, lack of validated outcomes measurements, and limited time periods of follow-up.
Quality Assessments
None of the manuscripts in this scoping review were randomized controlled trials, and few were high quality cohort studies. Overall, the quality of the conclusions was low, due to limitations in study design, unmeasured confounders, and missingness of both independent and dependent variables, as described in more detail in the individual sections above. All except three studies (Bergman et al., 1996; Carter et al., 2015; Olfson et al., 2018) were deemed to exhibit high risk of bias, due to factors including bias in selection of participants (e.g., only including participants from a certain hospital in a city; having low response rate), lack of concurrent comparison groups (e.g., leading to lack of clarity over whether firearm injury exposure was actually the cause of the observed outcome), bias in assignment to intervention groups (e.g., non-randomized or convenience samples for interventions), high risk of missing outcome data (e.g., non-systematic follow-up), lack of standardized assessment instruments for outcome measurements (e.g., using non-validated measures), and lack of measurement of potential confounders of the outcomes (e.g., not adjusting analyses for well-established risk factors for post-traumatic stress disorders).
Discussion
This scoping review summarizes the current evidence about the epidemiology and prevention of behavioral and physical health sequelae among youth exposed to firearm injury. We identified a total of 31 articles over three decades that met inclusion criteria; the overall quality of these studies was low to moderate. Despite the paucity of research and relatively weak methodological rigor of conducted studies, the behavioral and physical health consequences of youth exposure to firearm injury are consistently reported as high, after all types of firearm injury. Youth firearm injury exposure is clearly linked to high rates of post-traumatic stress symptoms and high rates of future injury. Almost no literature to date describes potential secondary prevention interventions to mitigate these negative longitudinal effects among children or their parents, likely due to the lack of adequate funding for research in this area. A primary objective of this scoping review was to provide recommendations for future research based on what can be gleaned by the existing literature; we provide these recommendations below.
Most importantly, our review identified a glaring need for more methodologically rigorous studies of the epidemiology and prevention of post-firearm-injury sequelae among adolescents. Existing studies rarely used prospective cohorts, objective outcome measures, or rigorous assessments of exposure, and rarely compare outcomes between youth who are exposed to firearm injury versus those who are exposed to other forms of trauma. Almost half of the included studies used cross-sectional, retrospective cohort, or case-control designs. This study design type is frequently biased by unmeasured confounders. Although almost all of the remainder of the studies (n=15) used prospective cohorts, this study design has limitations including the methodology for the selection of subjects and potential attrition bias (Song & Chung, 2010). Only eight studies had a comparison group, limiting ability to draw conclusions about the impact of the firearm injury (versus of injury in general, or other unmeasured confounders). Additionally, many of the studies were limited by response bias, lack of diagnostic interviews, and non-standard follow-up periods. We note that the limitations are at least partly due to systematic underfunding and understudy of firearm injury in general, and pediatric firearm injury in particular, over the last 22 years (Alcorn, 2017; Stark & Shah, 2017). Although the presence of the Firearm-safety Among Children and Teens (FACTS) Consortium (an NIH-funded consortium which aims to define new directions for youth firearm injury prevention research) through which this manuscript was written is an important first step in addressing the lack of literature, it is insufficient. Improved public and private funding of firearm injury research is critical in the quest to reduce the impact of firearm injury on youth.
Although our ability to draw conclusions from methodologically weak studies is limited, the review of these 31 studies confirms that firearm injury exposure is associated with high rates of post-traumatic stress among youth. The specific risk factors for development of such sequelae, however, are not well reported in the literature. For example, we identified no rigorous examinations of the psychophysiologic correlates, biologic outcomes, or phenotypic and genetic mechanisms of post-firearm-injury consequences. The exploration of mechanisms is a major gap to be addressed by future literature (The National Institute of Mental Health, 2017). We also note the lack of evaluation of mental health sequelae beyond post-traumatic stress symptoms; very few included manuscripts described prevalence or correlates of, for example, depression, other anxiety disorders, substance use, or quality of life. We urge future researchers to consider outcomes other than post-traumatic stress that are important to youth and their families (Wanner, 2015).
Importantly, we identified only one manuscript that evaluated an intervention to specifically prevent consequences of firearm injury among youth. This gap in the youth literature is particularly glaring, given that an extensive literature describes effective interventions and preventative interventions for other types of trauma and youth violence (David-Ferdon et al., 2016; Schneider, Grilli, & Schneider, 2013); additionally, a growing body of literature provides preliminary evidence on hospital-based post-injury intervention programs to reduce consequences of firearm injury and other types of injuries among adults (Affinati et al., 2016; Zatzick et al., 2013). Rather than develop new interventions - and given that many of the manuscripts in this scoping review identified heightened post traumatic stress symptoms in youth exposed to firearm injury - we recommend that future trials specifically examine the efficacy and effectiveness of existing evidence-based secondary prevention and interventions for youth that have not yet focused on firearm injury. An efficient use of scarce resources such trials could be conducted with interventions in their original format, or in an adapted format specific to youth firearm injury.
We also note that the reviewed studies disproportionately examine the consequences of mass shootings (45% of included studies, <1% of youth firearm deaths), compared to articles about the effects of firearm suicide injuries and death (10% of studies, 38% of youth firearm deaths) or firearm assault (16% of studies, 53% of youth firearm deaths). Assault-related firearm injury is the leading cause of death for minority males in the U.S. (Center for Disease Control and Prevention, 2014; Fowler et al., 2017; Srinivasan et al., 2014), but assessment of the consequences and prevention of these types of injuries is preliminary at best. Youth with an initial assault-related firearm injury have a high likelihood of recurrent injury (Carter et al., 2015). Yet we identified only one study providing preliminary data on efficacy of violence intervention programs to reduce recurrent injury among firearm-injured youth (Chong, Lee, et al., 2015). Rigorous evaluation of such programs following best methods practice to ensure adequate recruitment and retention, controlling for both confounders and intervention dose, is needed (Roche et al., 2018).
One potential explanation for why there are fewer studies on suicide related firearm-injury is that 85% of suicide attempts with a firearm are lethal (Spicer & Miller, 2000); there are, therefore, few survivors to study. However, as one of the reviewed articles describes, survivors are particularly high risk for dying from suicide within a year (Olfson et al., 2018), and friends and families of youth who commit suicide with a firearm may be at high risk for future problems themselves (Brent et al., 1993a; Brent et al., 1993b). Future studies should elucidate the sequelae of adolescent suicide attempts and/or completion by firearm amongst family members, peers, schools, and communities of the identified proband, particularly given preliminary evidence for suicide contagion (Brent et al., 1993a; Brent et al., 1993b); secondary prevention interventions for this group are warranted.
Most studies describing sequelae of mass shootings for youth investigate events in other countries (i.e., Norway, Finland) or describe events in the United States prior to 2000. Given that the rate of shootings with casualties of four or more individuals is occurring regularly and may be increasing in the United States (Follman, Aronsen, & Pan, 2018), additional research on the behavioral and physical health consequences of mass shootings are warranted. Early research on mass shootings were consistent with the Population Exposure Model which posits that individuals closest in proximity to trauma are likely to be affected the most (DeWolfe, 2004; Health & Services, 2005). The way in which information is disseminated to the United States population has changed dramatically over the past twenty years. Social network sites such as Facebook, Instagram, and Twitter are a significant source for news, particularly for young people (Barthel et al., 2015; Bergström & Jervelycke Belfrage, 2018; Kümpel, Karnowski, & Keyling, 2015; Shultz et al., 2013). In fact, in the 2018 school shooting at Stoneman Douglas High School in Florida, youth at the school live-tweeted their experiences and videos of the event. This may suggest that the Population Exposure Model may no longer be the best way to understand the experience of trauma on a community given that many individuals not at a mass shooting may experience the event as if they are physically there. Future research addressing the virtual impact of such shootings, and interventions to reduce long-term consequences of exposure among youth and their communities, is needed.
Finally, we recommend that more recent studies be conducted in the United States, given that the largest global burden of firearm injury is experienced domestically (Naghavi et al., 2018). The lack of research is likely at least in part due to a longstanding freeze on firearm research instituted in the United States in 1996 via the Dickey Amendment (Betz, Ranney, & Wintemute, 2016).
Limitations.
This scoping review has three main limitations. First, by virtue of design, scoping reviews are not systematic, given that their purpose is to identify the key areas within a research agenda and to identify research gaps in the existing literature, which is consistent with our primary objectives (Arksey & O’Malley, 2005). Although we conducted our search within four databases and followed suggested methods for scoping reviews, it is likely that all sources were not identified; given our methods, however, we are doubtful that additional articles would quantitatively or qualitatively change our conclusions. Second, this review does not focus on the literature of witnessing violence in a child’s community or family (McGill et al., 2014), and instead explicitly focuses on studies of firearm injury; moreover, analysis according to type of injury (peer, partner, unintentional, mass shooting) may limit generalizability. Third, we did not include non-English literature, which has the potential to exclude articles that would be relevant.
Conclusion.
Firearm injuries of all types (peer and partner assault injury, suicide, accidental, and mass shooting) are associated with increased risk of both behavioral and physical health sequelae among youth. However, the methodologic rigor of the existing corpus of research is limited, and a mismatch is observed between patterns of injury and death, and types of firearm injury studied. In particular, empirically studied secondary prevention interventions need to be designed, tested, and widely implemented (Fowler et al., 2017). It is our hope that this scoping review maps the gaps in the literature in a way that allows the prevention science of youth firearm injury to move forward.
Supplementary Material
Acknowledgements:
The authors wish to acknowledge Lynn Massey for assistance with the literature search, organizing data abstraction, and manuscript preparation. We would also like to acknowledge Gurpreet Kaur Rana, Informationist at the Taubman Health Sciences Library, University of Michigan, for creating the search strategies for the scoping review.
Funding:
This review was funded by NIH/NICHD 1R24HD087149-01A1. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agencies.
Footnotes
Financial Disclosure Statement: The authors have no financial relationships relevant to this article to disclose.
References
- Affinati S, Patton D, Hansen L, Ranney M, Christmas AB, Violano P, … Crandall M (2016). Hospital-based violence intervention programs targeting adult populations: an Eastern Association for the Surgery of Trauma evidence-based review. Trauma surgery & acute care open, 1(1), e000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcorn T (2017). Trends in research publications about gun violence in the United States, 1960 to 2014. JAMA internal medicine, 177(1), 124–126. [DOI] [PubMed] [Google Scholar]
- Arksey H, & O’Malley L (2005). Scoping studies: towards a methodological framework. International journal of social research methodology, 8(1), 19–32. [Google Scholar]
- Bair-Merritt MH, Blackstone M, & Feudtner C (2006). Physical health outcomes of childhood exposure to intimate partner violence: a systematic review. Pediatrics, 117(2), e278–e290. [DOI] [PubMed] [Google Scholar]
- Barthel M, Shearer E, Gottfried J, & Mitchell A (2015). The evolving role of news on Twitter and Facebook. Pew Research Center, 14. [Google Scholar]
- Benson JE, & Elder GH Jr (2011). Young adult identities and their pathways: A developmental and life course model. Developmental Psychology, 47(6), 1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman B, Ponzer S, & Brismar B (1996). Criminality and Morbidity in Young Victims of Firearm Injuries: A Follow-up Study. Annals of the New York Academy of Sciences, 794(1), 334–335. [DOI] [PubMed] [Google Scholar]
- Bergström A, & Jervelycke Belfrage M (2018). News in Social Media: Incidental consumption and the role of opinion leaders. Digital Journalism, 6(5), 583–598. [Google Scholar]
- Betz ME, Ranney ML, & Wintemute GJ (2016). Frozen Funding on Firearm Research:“Doing Nothing Is No Longer an Acceptable Solution”. Western journal of emergency medicine, 17(1), 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boynton-Jarrett R, Ryan LM, Berkman LF, & Wright RJ (2008). Cumulative Violence Exposure and Self-Rated Health: Longitudinal Study of Adolescents in the United States. Pediatrics, 122(5), 961–970. doi: 10.1542/peds.2007-3063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Perper J, Moritz G, Friend A, Schweers J, Allman C, … Balach L (1993a). Adolescent witnesses to a peer suicide. Journal of the American Academy of Child & Adolescent Psychiatry, 32(6), 1184–1188. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Schweers J, Roth C, … Liotus L (1993b). Psychiatric sequelae to the loss of an adolescent peer to suicide. Journal of the American Academy of Child & Adolescent Psychiatry, 32(3), 509–517. [DOI] [PubMed] [Google Scholar]
- Bugge I, Dyb G, Stensland SØ, Ekeberg Ø, Wentzel-Larsen T, & Diseth TH (2015). Physical injury and posttraumatic stress reactions. A study of the survivors of the 2011 shooting massacre on Utøya Island, Norway. Journal of psychosomatic research, 79(5), 384–390. [DOI] [PubMed] [Google Scholar]
- Carter PM, Cook LJ, Macy ML, Zonfrillo MR, Stanley RM, Chamberlain JM, … Network, P. E. C. A. R. (2017). Individual and neighborhood characteristics of children seeking emergency department care for firearm injuries within the PECARN Network. Academic emergency medicine, 24(7), 803–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Roehler DR, Goldstick J, Zimmerman MA, Blow FC, & Cunningham RM (2015). Firearm violence among high-risk emergency department youth after an assault injury. Pediatrics, 135(5), 805–815. doi: 10.1542/peds.2014-3572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention, C. (2014). Web-based injury statistics query and reporting systems: Fatal Injury Data (WISQARS). Retrieved from https://www.cdc.gov/injury/wisqars/fatal.html
- Cheng TL, Wright JL, Markakis D, Copeland-Linder N, & Menvielle E (2008). Randomized trial of a case management program for assault-injured youth: impact on service utilization and risk for reinjury. Pediatric emergency care, 24(3), 130–136. [DOI] [PubMed] [Google Scholar]
- Chong VE, Lee WS, & Victorino GP (2015a). Neighborhood socioeconomic status is associated with violent reinjury. Journal of surgical research, 199(1), 177–182. [DOI] [PubMed] [Google Scholar]
- Chong VE, Smith R, Garcia A, Lee WS, Ashley L, Marks A, … Victorino GP (2015b). Hospital-centered violence intervention programs: a cost-effectiveness analysis. The American Journal of Surgery, 209(4), 597–603. [DOI] [PubMed] [Google Scholar]
- Council NR (2013). Priorities for research to reduce the threat of firearm-related violence: National Academies Press. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Carter PM, Ranney M, Zimmerman MA, Blow FC, Booth BM, … Walton MA (2015). Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA Pediatr, 169(1), 63–70. doi: 10.1001/jamapediatrics.2014.1900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Walton MA, & Carter PM (2018). The Major Causes of Death in Children and Adolescents in the United States New England Journal of Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David-Ferdon C, Vivolo-Kantor AM, Dahlberg LL, Marshall KJ, Rainford N, & Hall JE (2016). A comprehensive technical package for the prevention of youth violence and associated risk behaviors.
- Davis JS, Pandya RK, Sola JE, Perez EA, Neville HL, & Schulman CI (2013). Pediatric trauma recidivism in an urban cohort. Journal of surgical research, 182(2), 326–330. [DOI] [PubMed] [Google Scholar]
- DeWolfe DJ (2004). Mental health response to mass violence and terrorism: A training manual: Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration, US Department of Health and Human Services. [Google Scholar]
- Dyb G, Jensen T, Glad KA, Nygaard E, & Thoresen S (2014). Early outreach to survivors of the shootings in Norway on the 22nd of July 2011. European journal of psychotraumatology, 5(1), 23523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2015). Prevalence of childhood exposure to violence, crime, and abuse: Results from the national survey of children’s exposure to violence. JAMA pediatrics, 169(8), 746–754. [DOI] [PubMed] [Google Scholar]
- Follman M, Aronsen G, & Pan D (2018). US mass shootings, 1982–2018: Data from Mother Jones’ investigation. Mother Jones. [Google Scholar]
- Fowler KA, Dahlberg LL, Haileyesus T, Gutierrez C, & Bacon S (2017). Childhood firearm injuries in the United States. Pediatrics, e20163486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler PJ, Tompsett CJ, Braciszewski JM, Jacques-Tiura AJ, & Baltes BB (2009). Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Development and Psychopathology, 21(1), 227–259. [DOI] [PubMed] [Google Scholar]
- Gibson PD, Ippolito JA, Shaath MK, Campbell CL, Fox AD, & Ahmed I (2016). Pediatric gunshot wound recidivism: Identification of at-risk youth. Journal of Trauma and Acute Care Surgery, 80(6), 877–883. [DOI] [PubMed] [Google Scholar]
- Gill AC (2002). Risk factors for pediatric posttraumatic stress disorder after traumatic injury. Archives of Psychiatric Nursing, 16(4), 168–175. [DOI] [PubMed] [Google Scholar]
- Hafstad GS, Dyb G, Jensen TK, Steinberg AM, & Pynoos RS (2014). PTSD prevalence and symptom structure of DSM-5 criteria in adolescents and young adults surviving the 2011 shooting in Norway. Journal of Affective Disorders, 169, 40–46. [DOI] [PubMed] [Google Scholar]
- Hamrin V (1998). Psychiatric interviews with pediatric gunshot patients. Journal of Child and Adolescent Psychiatric Nursing, 11(2), 61–68. [DOI] [PubMed] [Google Scholar]
- Hamrin V, Jonker B, & Scahill L (2004). Acute Stress Disorder Symptoms in Gunshot-Injured Youth. Journal of Child and Adolescent Psychiatric Nursing, 17(4), 161–172. [DOI] [PubMed] [Google Scholar]
- Haravuori H, Suomalainen L, Berg N, Kiviruusu O, & Marttunen M (2011). Effects of media exposure on adolescents traumatized in a school shooting. Journal of traumatic stress, 24(1), 70–77. [DOI] [PubMed] [Google Scholar]
- Hawkins NA, McIntosh DN, Silver RC, & Holman EA (2007). Early responses to school violence: A qualitative analysis of students’ and parents’ immediate reactions to the shootings at Columbine High School. Journal of Emotional Abuse, 4(3–4), 197–223. [Google Scholar]
- Health, U. D. o., & Services, H. (2005). Terrorism and other public health emergencies: A reference guide for media. Washington, DC: Department of Health and Human Services. [Google Scholar]
- Heinze JE, Reischl TM, Bai M, Roche JS, Morrel-Samuels S, Cunningham RM, & Zimmerman MA (2016). A Comprehensive Prevention Approach to Reducing Assault Offenses and Assault Injuries among Youth. Prevention science : the official journal of the Society for Prevention Research, 17(2), 167–176. doi: 10.1007/s11121-015-0616-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J, Sterne J, Savović J, Page M, Hróbjartsson A, Boutron I, … Eldridge S (2016). A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev, 10(Suppl 1), 29–31. [Google Scholar]
- Jovanovic T, Vance LA, Cross D, Knight AK, Kilaru V, Michopoulos V, … Smith AK (2017). Exposure to violence accelerates epigenetic aging in children. Scientific reports, 7(1), 8962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karp A (2018). Estimating Global Civilian-Held Firearms Numbers. Small Arms Survey. [Google Scholar]
- Kümpel AS, Karnowski V, & Keyling T (2015). News sharing in social media: A review of current research on news sharing users, content, and networks. Social media+ society, 1(2), 2056305115610141. [Google Scholar]
- Levine PB, & McKnight R (2017). Firearms and accidental deaths: Evidence from the aftermath of the Sandy Hook school shooting. Science, 358(6368), 1324–1328. [DOI] [PubMed] [Google Scholar]
- McGill T, Self-Brown SR, Lai BS, Cowart M, Tiwari A, LeBlanc M, & Kelley ML (2014). Effects of exposure to community violence and family violence on school functioning problems among urban youth: The potential mediating role of posttraumatic stress symptoms. Frontiers in public health, 2, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercer KB, Orcutt HK, Quinn JF, Fitzgerald CA, Conneely KN, Barfield RT, … Ressler KJ (2012). Acute and posttraumatic stress symptoms in a prospective gene× environment study of a university campus shooting. Archives of General Psychiatry, 69(1), 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nader K, Pynoos R, Fairbanks L, & Frederick C (1990). Children’s PTSD reactions one year after a sniper attack at their school. The American journal of psychiatry, 147(11), 1526. [DOI] [PubMed] [Google Scholar]
- Naghavi M, Marczak LB, Kutz M, Shackelford KA, Arora M, Miller-Petrie M, … Alam K (2018). Global mortality from firearms, 1990–2016. JAMA, 320(8), 792–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netburn D (2018, November 10). The role of PTSD in mass shootings: Let’s separate myth from reality. Los Angeles Times. Retrieved from http://www.latimes.com/science/sciencenow/la-sci-sn-ptsd-mass-shootings-20181110-story.html [Google Scholar]
- Olfson M, Wall M, Wang S, Crystal S, Bridge JA, Liu S-M, & Blanco C (2018). Suicide after deliberate self-harm in adolescents and young adults. Pediatrics, e20173517. [DOI] [PubMed] [Google Scholar]
- Omar HA (1999). Adolescent violence as viewed by high school students. International journal of adolescent medicine and health, 11(3–4), 153–158. [DOI] [PubMed] [Google Scholar]
- Ouzzani M, Hammady H, Fedorowicz Z, & Elmagarmid A (2016). Rayyan—a web and mobile app for systematic reviews. Systematic reviews, 5(1), 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponzer S, Bergman B, Brismar B, & Johansson S (1997). Accidental firearm injury in childhood--a predictor of social and medical outcome? European journal of emergency medicine: official journal of the European Society for Emergency Medicine, 4(3), 125–129. [DOI] [PubMed] [Google Scholar]
- Pynoos RS, Frederick C, Nader K, Arroyo W, Steinberg A, Eth S, … Fairbanks L (1987a). Life threat and posttraumatic stress in school-age children. Archives of General Psychiatry, 44(12), 1057–1063. [DOI] [PubMed] [Google Scholar]
- Pynoos RS, Nader K, Frederick C, Gonda L, & Stuber M (1987b). Grief reactions in school age children following a sniper attack at school. Israel Journal of Psychiatry and Related Sciences. [PubMed] [Google Scholar]
- Rand Corporation. (2018). Mass Shootings: Definitions and Trends Retrieved from https://www.rand.org/research/gun-policy/analysis/supplementary/mass-shootings.html
- Ranney ML, Fletcher J, Alter H, Barsotti C, Bebarta VS, Betz ME, … Acep Technical Advisory Group on Firearm Injury Research, a. S. o. t. A. R. C. (2017). A Consensus-Driven Agenda for Emergency Medicine Firearm Injury Prevention Research. Ann Emerg Med, 69(2), 227–240. doi: 10.1016/j.annemergmed.2016.08.454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche JS, Clery MJ, Carter PM, Dora-Laskey A, Walton MA, Ngo QM, & Cunningham RM (2018). Tracking Assault-injured, Drug-using Youth in Longitudinal Research: Follow-up Methods. Academic emergency medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowhani-Rahbar A, Zatzick D, Wang J, Mills BM, Simonetti JA, Fan MD, & Rivara FP (2015). Firearm-related hospitalization and risk for subsequent violent injury, death, or crime perpetration: a cohort study. Annals of Internal Medicine, 162(7), 492–500. [DOI] [PubMed] [Google Scholar]
- Samuelson KW, Wilson CK, Padrón E, Lee S, & Gavron L (2017). Maternal PTSD and children’s adjustment: Parenting stress and emotional availability as proposed mediators. Journal of clinical psychology, 73(6), 693–706. [DOI] [PubMed] [Google Scholar]
- Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, … Fullerton CS (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: intentional and non-intentional traumatic events. PloS one, 8(4), e59236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider SJ, Grilli SF, & Schneider JR (2013). Evidence-based treatments for traumatized children and adolescents. Current Psychiatry Reports, 15(1), 332. [DOI] [PubMed] [Google Scholar]
- Schwarz ED, & Kowalski JM (1991). Malignant memories: PTSD in children and adults after a school shooting. Journal of the American Academy of Child & Adolescent Psychiatry, 30(6), 936–944. [DOI] [PubMed] [Google Scholar]
- Shih RA, Schell TL, Hambarsoomian K, Marshall GN, & Belzberg H (2010). Prevalence of PTSD and major depression following trauma-center hospitalization. The Journal of trauma, 69(6), 1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shultz JM, Muschert GW, Dingwall A, & Cohen AM (2013). The Sandy Hook Elementary School shooting as tipping point: “This Time Is Different”. Disaster health, 1(2), 65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slovak K, & Singer M (2001). Gun violence exposure and trauma among rural youth. Violence and Victims, 16(4), 389. [PubMed] [Google Scholar]
- Song JW, & Chung KC (2010). Observational studies: cohort and case-control studies. Plastic and reconstructive surgery, 126(6), 2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spicer RS, & Miller TR (2000). Suicide acts in 8 states: incidence and case fatality rates by demographics and method. American Journal of Public Health, 90(12), 1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan S, Mannix R, & Lee LK (2014). Epidemiology of paediatric firearm injuries in the USA, 2001–2010. Archives of disease in childhood, 99(4), 331–335. [DOI] [PubMed] [Google Scholar]
- Stark DE, & Shah NH (2017). Funding and publication of research on gun violence and other leading causes of death. JAMA, 317(1), 84–85. [DOI] [PubMed] [Google Scholar]
- Stene LE, & Dyb G (2015). Health service utilization after terrorism: a longitudinal study of survivors of the 2011 Utøya attack in Norway. BMC health services research, 15(1), 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stensland SØ, Zwart J-A, Wentzel-Larsen T, & Dyb G (2018). The headache of terror: a matched cohort study of adolescents from the Utøya and the HUNT Study. Neurology, 90(2), e111–e118. [DOI] [PubMed] [Google Scholar]
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, … Boutron I (2016). ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Bmj, 355, i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suomalainen L, Haravuori H, Berg N, Kiviruusu O, & Marttunen M (2011). A controlled follow-up study of adolescents exposed to a school shooting–Psychological consequences after four months. European Psychiatry, 26(8), 490–497. [DOI] [PubMed] [Google Scholar]
- Talley CL, Campbell BT, Jenkins DH, Barnes SL, Sidwell RA, Timmerman G, … Eastman A (2018). Recommendations from the American College of Surgeons Committee on Trauma’s Firearm Strategy Team (FAST) Workgroup: Chicago Consensus I. Journal of the American College of Surgeons. [DOI] [PubMed] [Google Scholar]
- Tellez MG, Mackersie RC, Morabito D, Shagoury C, & Heye C (1995). Risks, costs, and the expected complication of re-injury. The American Journal of Surgery, 170(6), 660–664. [DOI] [PubMed] [Google Scholar]
- The National Institute of Mental Health. (2017). Strategic Research Priorities Overview. Transforming the understanding and treatment of mental illnesses. Retrieved from https://www.nimh.nih.gov/about/strategic-planning-reports/strategic-research-priorities/index.shtml
- Thoresen S, Jensen TK, Wentzel-Larsen T, & Dyb G (2016). Parents of terror victims. A longitudinal study of parental mental health following the 2011 terrorist attack on Utøya Island. Journal of anxiety disorders, 38, 47–54. [DOI] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, & Cunningham RM (2010). Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA, 304(5), 527–535. doi: 10.1001/jama.2010.1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanner JP (2015). Development of a Trauma-Specific Quality of Life Measurement. The journal of trauma and acute care surgery, 79(2), 275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wise AE, & Delahanty DL (2017). Parental factors associated with child post-traumatic stress following injury: a consideration of intervention targets. Frontiers in psychology, 8, 1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D, Jurkovich G, Rivara FP, Russo J, Wagner A, Wang J, … O’Connor SS (2013). A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Annals of surgery, 257(3), 390. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


