Summary
Background
To assess the reproductive, maternal, newborn and child health (RMNCH) service coverage in Vietnam with trends in 2000−2014, projections and probability of achieving targets in 2030 at national and sub-national levels; and to analyze the socioeconomic, regional and urban-rural inequalities in RMNCH service indicators.
Methods
We used national population-based datasets of 44,624 households in Vietnam from 2000 to 2014. We applied Bayesian regression models to estimate the trends in and projections of RMNCH indicators and the probabilities of achieving the 2030 targets. Using the relative index, slope index, and concentration index of inequality, we examined the patterns and trends in RMNCH coverage inequality.
Findings
We projected that 9 out of 17 health service indicators (53%) would likely achieve the 2030 targets at the national level, including at least one and four ANC visits, BCG immunization, access to improved water and adequate sanitation, institutional delivery, skilled birth attendance, care-seeking for pneumonia, and ARI treatment. We observed very low coverages and zero chance of achieving the 2030 targets at national and sub-national levels in early initiation and exclusive breastfeeding, family planning needs satisfied, and oral rehydration therapy. The most deprived households living in rural areas and the Northwest, Northeast, North Central, Central Highlands, and Mekong River Delta regions would not reach the 80% immunization coverage of DPT3, Polio3, Measles and full immunization. We found socioeconomic, regional, and urban-rural inequalities in all RMNCH indicators in 2014 and no change in inequalities over 15 years in the lowest-coverage indicators.
Interpretation
Vietnam has made substantial progress toward UHC. By improving the government's health system reform efforts, re-allocating resources focusing on people in the most impoverished rural regions, and restructuring and enhancing current health programs, Vietnam can achieve the UHC targets and other health-related SDGs.
Funding
The authors did not receive any funds for conducting this study.
Keywords: RMNCH, Universal Health Coverage, Vietnam, trend, projection, progress, 2030 targets
Research in context.
Evidence before this study
We systematically searched PubMed for literature and research published in any language before January 1, 2021, about assessing Reproductive, maternal, newborn, and child health (RMNCH) service and progress toward Universal Health Coverage (UHC) in Vietnam. We found none study investigated the trends in and projections of RMNCH service coverage in Vietnam with national and sub-national levels and calculated the probability of reaching the 2030 targets. Also, none provided a comprehensive analysis of estimations, patterns, and trends in RMNCH service coverage inequalities between socioeconomic groups, living areas, and regional levels.
Added value of this study
This study is the first and most comprehensive study providing reliable estimates of RMNCH indicators for Vietnam, using multiple nationally representative surveys to the best of our knowledge. We used a Bayesian approach to present trends in and projections of RMNCH service coverage and the probabilities of achieving the 2030 targets, along with comprehensive inequality analyses. The overall coverage of prevention and treatment composite indices have both been significantly increasing from 2000 to 2014. Most indicators are projected to achieve the 2030 targets at the national level. However, we found decreasing trends in health-related behaviours of families and mothers with shallow coverage levels, which unlikely to reach the targets in 2030. Several health indicators and access to health services are more concentrated among the wealthiest than the poorest, with more significant gaps in rural than urban areas, showing that inequalities still exist. Additionally, our analyses suggest some regions lag and need to pay more attention and resources to maternal and child health in Vietnam.
Implications of all the available evidence
Our findings indicated that although Vietnam is moving toward UHC, maternal and child health and inequalities in healthcare coverage might pose barriers to achieve global UHC targets by 2030. Supportive policies are needed for improving women's empowerment and gender equality, focusing on the most impoverished rural people. The Vietnamese government must continue to improve and reform the healthcare system, re-allocate resources focusing on lagging localities and evaluate and enhance current health programs and interventions.
Alt-text: Unlabelled box
1. Background
Achieving Universal health coverage (UHC) is a global health priority and plays a central role in achieving other health-related targets in the Sustainable Development Goals (SDGs).1 The UHC targets include at least 80% population in each country covered for essential health services regardless of social-economic status or place of residence.2 World Health Organization (WHO) and the World Bank have developed a framework to monitor UHC progress, which measures expanded health services coverage and financial protection.2,3 Nevertheless, to accomplish the commitments toward health for all,4 each country should develop its plans and approaches to UHC, considering specific national social, economic, and political circumstances.
Women, newborns and children can experience particular difficulties in accessing quality care and financial protection.5 Primary healthcare, including reproductive, maternal, newborn and child health (RMNCH) services, are a critical part of the UHC framework with essential reproductive health services, care for pregnant women, preventive and curative interventions for newborns and children.6 Monitoring RMNCH service coverage in both national and sub-national groups plays a critical role in supporting government and policymakers in their efforts toward UHC progress. Vietnam was a "fast-track country" for health-related outcomes in the Millennium Development Goals (MDGs), given its comparatively low socioeconomic development. However, it faces difficulties and challenges in achieving UHC and health equity due to rapid demographic and social transition.7 According to World Bank's report, poor people are more likely to be ill and less likely to receive benefits from Vietnam's healthcare system.8 Previous analysis has identified inequities in health in Vietnam in multiple dimensions, including socioeconomic status and place of residence.9 Additionally, Vietnam has 63 provinces with diverse demographic, geographic, and socioeconomic characteristics, grouped into eight regions. This regional and provincial diversity might associate with significant geographical health inequalities.10 Monitoring and measuring these inequalities in RMNCH by socioeconomic status, regional level and living area are essential to achieving UHC in Vietnam. This will ensure not only appropriate resource allocation but also that disadvantaged populations are not left behind.
Previously, progress toward UHC in Vietnam has only been assessed superficially as part of multi-country analyses.11,12 However, a specific approach to comprehensive and informative measurements is required for a particular country using disaggregated data. Additionally, no previous study has presented national and sub-national trends in and projections of RMNCH indicators in Vietnam to 2030, neither offered comprehensive inequality analyses in multiple dimensions. This study investigated trends in and projections of RMNCH service coverage in Vietnam up to 2030 at national and sub-national levels and estimated the probability of achieving UHC targets by 2030. We also provided a comprehensive analysis of socioeconomic, regional, and urban-rural inequalities and changes from 2000–2014 to monitor RMNCH service coverage inequalities.
2. Methods
2.1. Data sources
We performed secondary data analysis using nationally representative household surveys, including the Demographic and Household Surveys (DHS) and Multiple Indicator Cluster Surveys (MICS). Finally, we included 44,624 households from five datasets from 2000 to 2014 (Supplementary Table S1). All selected data are open access, and ethical approval is not required.
2.2. Measurement of outcomes
All health service coverage indicators and inequality indices were measured using sampling weights and survey designs according to guidance of analysing data from DHS and MICS, and recommendations from World Health Organization (WHO) and World Bank.2,13,14
2.3. RMNCH service coverage
We selected RMNCH service indicators based on data availability and consistency with previous studies.15 The final indicator set included 12 prevention indicators and five treatment indicators (Supplementary Table S2). We estimated the composite prevention and treatment indices as the weighted mean of prevention and treatment indicators, respectively, using random-effects meta-analysis.16 We compared these results with the arithmetic mean proportions commonly used as an alternative measurement of coverage,15,17 and with geometric mean proportions recently used by the WHO.3 There were no notable differences among these methods (Supplementary Table S6, S7, S8). Following the previous formula of composite coverage, service coverage and SDG 3•8•1, and under the country context, we measured the health service coverage index by an equally weighted geometric average of prevention and treatment indicators.12,18
2.4. Inequality estimations
We performed a comprehensive analysis of socioeconomic, regional and urban-rural inequalities. Using regression-based methods, we calculated the relative index of inequality (RII), the slope index of inequality (SII), and the concentration index (CnI) to evaluate the degree of inequality between poor and wealthy households.19 The RII and SII correspond to the ratio and the absolute difference in predicted values of a health indicator between households in the top and bottom of socioeconomic status, while the CnI indicates the extent to which a health indicator is concentrated among the poorer or the richer groups.19 We conducted the same analysis to measure regional and rural-urban inequalities. We evaluated the patterns of inequality by using plots of wealth quintile-specific coverage based on previous works (Supplementary Methods).
2.5. Changes in inequalities
We estimated the difference of inequalities between two time points (the year 2014 and 2000) in three dimensions of relative terms (RII), absolute terms (SII), and magnitude (CnI). We computed the 95% Confidence Intervals (CIs) and p-value of the differences in RII, SII and CnI using each parameter's standard error. An indicator with statistically significant changes (p-value<0•05) in all three inequality measures was considered as having changes in inequality over 15 years.
2.6. Statistical analysis
We applied the Bayesian statistics, which required a choice of coefficient priors and provided the posterior predictive distributions, for calculating the probabilities of achieving targets, which are unobtainable from standard frequentist regression models.20 To investigate national trends in RMNCH service coverage, we used Bayesian linear regression models at aggregate unit of national levels with logit transformed values of RMNCH service coverages as the dependent variables and survey year as the covariate. In models that were disaggregated by wealth quintile or living areas, we also tested the inclusion of interaction terms between wealth index (or living areas) and survey year using the leave-one-out cross-validation method (Supplementary Table S3, S4). We applied Bayesian mixed-effect models to evaluate the variations between sub-national levels (regions) over time, as described elsewhere,21 with random slope tested (Supplementary Table S5). We fitted 182 Bayesian models using the Markov Chain Monte Carlo (MCMC) algorithm with 5000 samples, two chains, 1000 iterations burn-in, and 2x thinning for each. MCMC was diagnosed using trace plots and the potential scale reduction factor.20 From the fitted Bayesian models, we extracted posterior predictive distributions to estimate the probability of achieving UHC targets for all indicators and their 95% credible intervals (CrI) and the average annual percentage of change over the period. We applied a threshold of 80% coverage to define the UHC target achievement. We performed all the analyses using R and implemented Bayesian models in Stan via the brms package.22
2.7. Role of the funding source
The authors did not receive any funds for conducting this study. PTN, SG, HVN, MVH, and LQK had access to the raw data. PTN had full access to all the data and had final responsibility for submitting the manuscript for publication.
3. Results
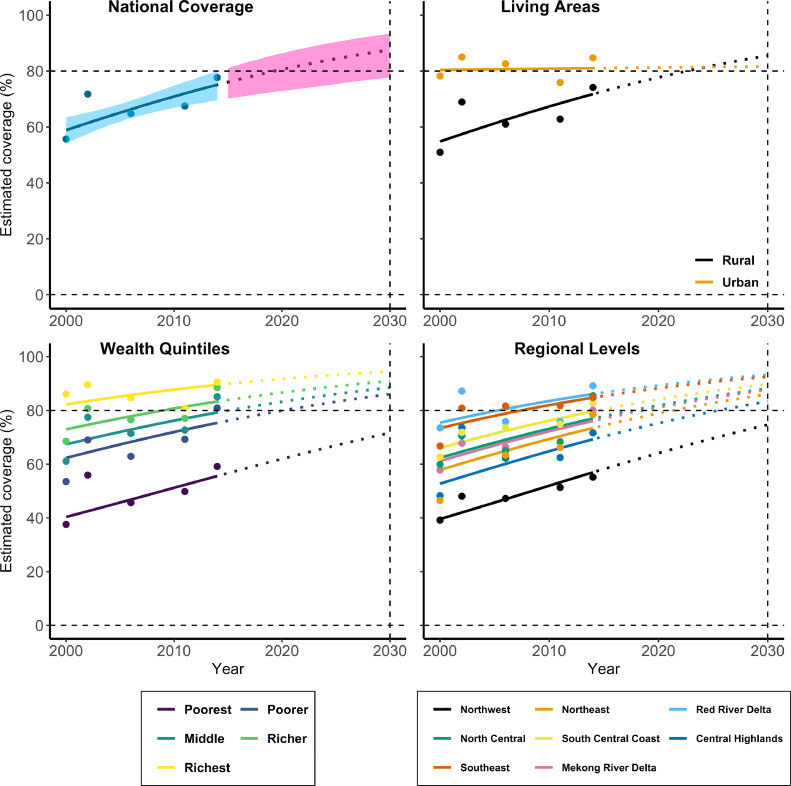
Figure 1 shows the trends in composite RMNCH service coverage at national and sub-national levels from 2000 and projections to 2030. We predicted RMNCH service coverage would reach the 80% target by 2030 at the national level and most of the wealth quintiles, except the poorest. We observed a gap in coverage between urban and rural areas in 2000 with its narrowing over time. Three regions of Northwest, Central Highlands and Northeast were projected having the lowest coverages in 2030, and the Northwest will not reach the 2030 targets. Those results are observed similarly in both composite prevention and treatment indices at national and wealth quintile levels (Supplementary Figure S1, S2). The sensitivity analysis of composite methods showed comparable results between meta-analysis random-effects, geometric mean, and arithmetic mean methods at wealth quintiles, living areas, and regional levels (Supplementary Table S6, S7, S8). Trends in and projections of all RMNCH service indicators to 2030 at national and sub-national levels are in Supplementary Figure S3–S19.
Figure 1.
Trends in and projections of RMNCH health service coverage in Vietnam at the national level and sub-national levels, 2000–2030
Notes: The coloured dots are the observed coverages; The solid lines are the estimated trends to 2014; The dashed lines are the projected trends in future from 2014; The shaded areas are the 95% Credible Intervals; the horizontal dotted lines present the UHC target of 80%; Top-left figure shows national coverage; Top-right figure shows coverage by living areas; Bottom-left figure shows coverage by wealth quintiles; Bottom-right figure shows coverage by regional levels.
Table 1 presented the national coverage of RMNCH indicators from 2000 to 2030 with both observed coverages (2000 and 2014) and projections (2020 and 2030). We observed very high probabilities (90%–100%) of achieving 2030 targets in 5/12 (42%) prevention indicators of at least one ANC (ANC1), at least four ANC (ANC4), BCG immunization, improved water, and adequate sanitation, and 4/5 (80%) treatment indicators of institutional delivery, skilled birth attendance (SBA), care-seeking for pneumonia (CSP), and ARI treatment. In contrast, we predicted 0% probability of achieving the 2030 target for early initiation of breastfeeding (EIBF) and exclusive breastfeeding (EBF), family planning needs satisfied (FPNS), full immunization and oral rehydration therapy (ORT) at national and all sub-national (socioeconomic, regional, and urban-rural) levels (Supplementary Table S10, S12, S14). EIBF, FPNS and ORT showed decreasing trends with a negative average annual percentage of change (AAPC) from 2000 to 2030. The AAPC of all RMNCH service coverages in three sub-periods of 2000–2010, 2010–2020, and 2020–2030 are in Supplementary Table S15.
Table 1.
RMNCH service coverage in Vietnam from 2000–2030, and probability of achieving the 2030 targets
| Indicators | Observed coverages in percent(95% CI) | Predicted coverages in percent(95% CrI) | AAPC from 2000-2030(95% CrI) | Probability reach target (%) | ||
|---|---|---|---|---|---|---|
| Year 2000 | Year 2014 | Year 2020 | Year 2030 | |||
| Prevention Indicators | ||||||
| At least one ANC visit | 69•6 (65•7 to 73•3) | 94•5 (93•3 to 95•6) | 97•3 (96•6 to 98•0) | 99•2 (98•7 to 99•5) | 0•7 (0•6 to 0•8) | 100•0 |
| At least four ANC visit | 29•6 (27•2 to 32•1)† | 69•9 (67•5 to 72•2) | 83•6 (81•4 to 85•6) | 95•4 (94•0 to 96•4) | 2•4 (2•3 to 2•5) | 100•0 |
| Exclusive breastfeeding | 18•1 (14•1 to 22•9) | 20•7 (17•1 to 24•9) | 21•6 (16•5 to 27•2) | 26•3 (16•7 to 37•7) | 0•4 (0•0 to 0•9) | 0•0 |
| Early initiation of breastfeeding | 59.8 (57.2 to 62.4)† | 41.6 (39.2 to 44.2) | 39.5 (36.2 to 42.7) | 33.1 (28.0 to 38.6) | -0.7 (-0.9 to -0.4) | 0.0 |
| Family planning needs satisfied | 72•4 (71•1 to 73•8)† | 62•5 (61•2 to 63•8) | 56•9 (55•0 to 58•7) | 47•4 (43•8 to 51•0) | -0•9 (-1•0 to -0•7) | 0•0 |
| BCG immunization | 86•2 (83•1 to 88•9) | 95•5 (93•9 to 96•8) | 95•9 (94•3 to 97•1) | 97•8 (96•2 to 98•8) | 0•4 (0•3 to 0•5) | 100•0 |
| DPT3 immunization | 50•2 (46•0 to 54•4) | 75•9 (72•8 to 78•8) | 70•8 (66•8 to 74•4) | 76•5 (70•3 to 81•7) | 0•6 (0•4 to 0•9) | 10•1 |
| Polio3 immunization | 50•4 (46•2 to 54•6) | 84•3 (81•6 to 86•7) | 73•7 (69•9 to 77•1) | 80•7 (75•3 to 85•2) | 0•8 (0•6 to 1•1) | 61•4 |
| Measles immunization | 69•1 (65•1 to 72•9) | 81•9 (79•1 to 84•4) | 79•0 (75•3 to 82•4) | 81•6 (75•7 to 86•4) | 0•3 (0•0 to 0•5) | 70•8 |
| Full immunization | 35•1 (31•2 to 39•2) | 67•3 (63•9 to 70•5) | 61•0 (56•7 to 65•1) | 68•6 (61•4 to 74•7) | 0•8 (0•5 to 1•1) | 0•0 |
| Improved Water | 68•7 (68•3 to 69•2) | 91•9 (91•6 to 92•1) | 95•2 (95•1 to 95•4) | 98•2 (98•1 to 98•3) | 0•8 (0•8 to 0•8) | 100•0 |
| Adequate sanitation | 39•5 (39•0 to 40•0) | 80•4 (80•0 to 80•8) | 88•3 (88•0 to 88•6) | 95•1 (94•9 to 95•3) | 1•4 (1•4 to 1•4) | 100•0 |
| Treatment Indicators | ||||||
| Institutional delivery | 79•6 (77•4 to 81•7)† | 91•1 (89•5 to 92•4) | 94•3 (93•1 to 95•4) | 97•6 (96•6 to 98•4) | 0•8 (0•7 to 0•9) | 100•0 |
| Skilled birth attendance | 61•3 (57•1 to 65•3) | 92•2 (90•7 to 93•4) | 94•9 (93•8 to 95•8) | 98•1 (97•4 to 98•7) | 0•9 (0•8 to 1•0) | 100•0 |
| Care seeking for pneumonia | 62•6 (57•2 to 67•7) | 86•6 (79•6 to 91•5) | 89•0 (82•9 to 93•3) | 93•8 (87•0 to 97•2) | 0•8 (0•5 to 1•0) | 99•9 |
| ARI treatment | 50•3 (43•3 to 57•2)‡ | 82•7 (75•2 to 88•3) | 91•5 (84•9 to 95•6) | 98•4 (94•8 to 99•6) | 2•4 (1•9 to 2•8) | 100•0 |
| Oral rehydration therapy | 54•2 (49•0 to 59•4) | 30•0 (25•2 to 35•3) | 21•9 (17•2 to 27•3) | 11•7 (7•4 to 17•7) | -1•5 (-1•7 to -1•2) | 0•0 |
| Composite Indicators | ||||||
| Composite Prevention | 54•6 (48•9 to 60•2) | 77•1 (72•8 to 80•9) | 78•6 (74•0 to 82•8) | 85•4 (79•0 to 90•1) | 0•9 (0•6 to 1•1) | 95•3 |
| Composite Treatment | 59•5 (54•1 to 64•7) | 78•7 (70•8 to 85•0) | 82•1 (74•9 to 88•1) | 88•4 (79•3 to 94•1) | 0•9 (0•5 to 1•2) | 96•5 |
| Composite Coverage | 55•6 (49•9 to 61•2) | 78•0 (70•0 to 84•3) | 80•6 (72•9 to 86•4) | 87•6 (77•8 to 93•4) | 1•0 (0•5 to 1•3) | 93•9 |
Notes: The WHO's targets for Universal Health Coverage are by 2030 at least 80% health-services coverage for the entire population of a country, regardless of wealth status, place of residence or gender; † Data in the year 2002 was used due to unavailable data for 2000; ‡ Data in the year 2006 was used due to the unavailable data for 2000; AAPC=Average annual percentage change; ANC=Antenatal care; DPT=Three doses of diphtheria, pertussis, tetanus vaccine; BCG=Bacillus Calmette–Guérin vaccine; Polio3=Three doses of polio vaccine; ARI=Acute Respiratory Infections; The observed coverages during 2000–2014 were calculated based on the original datasets.
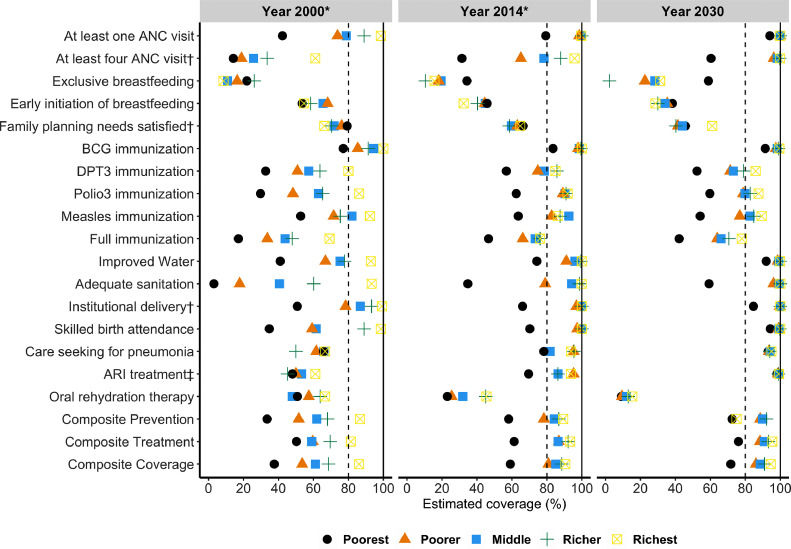
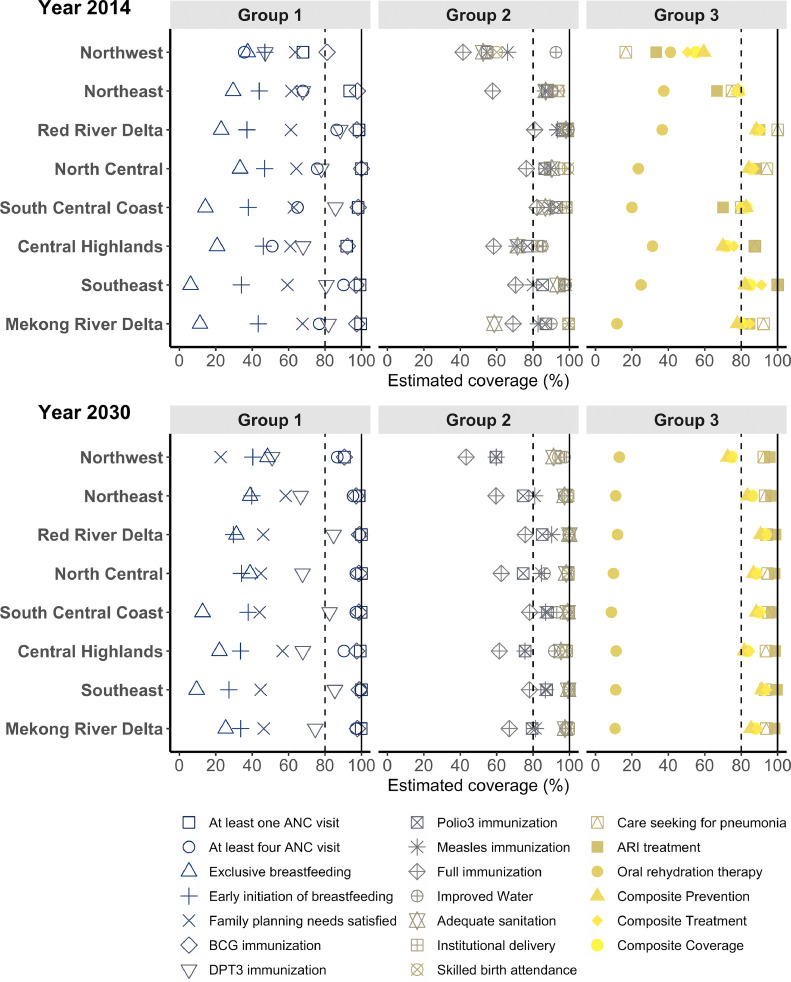
Figure 2 shows estimates of RMNCH service coverage at quintile-specific levels in the year 2000 and 2014 and projections to 2030. Three prevention indicators (ANC1, BCG, and access to improved water) and four treatment indicators (institutional delivery, SBA, CSP, and ARI treatment) will reach the 2030 targets across all quintiles. Although most indicators will reach the targets at the national level, there are substantial coverage gaps between socioeconomic groups with no achievement for the poorest quintile. Figure 3 presents RMNCH service coverages in eight regions in the years 2014 and 2030. The Northwest and Central highlands regions had the lowest coverages in most indicators in 2014 and 2030. We project that Northwest, Central Highlands, Northeast, and North Central regions will not reach the 2030 target in immunization indicators (DPT3, Polio3, Measles and Full immunization). The Mekong River Delta will not reach 80% coverage of DPT3 by 2030 (Supplementary Figure S20). Observed coverages of all indicators stratified by wealth quintiles, living areas and regional levels are in Supplementary Tables S9, S11, and S13, respectively.
Figure 2.
Health service coverage in Vietnam in the year 2000 and 2014 (observed) and year 2030 (projection) at wealth quintile levels
Notes: The coloured shapes are the estimated and projected values for wealth quintile levels; the horizontal axis shows coverage scales from 0 – 100%; the horizontal dotted lines present the UHC target of 80% coverage; † coverage in the year 2002 was used due to unavailable data for 2000; ‡ coverage in the year 2006 was used due to unavailable data for 2000; * Observed coverages;
Figure 3.
RMNCH service coverage in Vietnam in the year 2014 and 2030 at regional levels
Notes: The coloured shapes represent RMNCH indicators' values; the horizontal axis shows coverage scales from 0 – 100%; the horizontal dotted lines present the UHC target of 80% coverage.
Table 2 describes the comprehensive inequality analyses of all RMNCH service indicators in 2014 with socioeconomic, regional and urban-rural inequalities. We observed statistically significant socioeconomic inequalities in most indicators in all three indices of inequality (RII, SII, and CnI), except FPNS and CSP. All indicators showed higher concentrations of service coverage among wealthier groups, excluding EIBF and EBF. At least four ANC visits (ANC4) had the most significant gap between socioeconomic levels with RII of 2•52 (95% CI: 2•28−2•79), SII of 71•41 (65•52−77•31), and CnI of 0•19 (0•17−0•20). All RMNCH indicators experienced statistically significant regional inequalities with an enormous difference observed in exclusive breastfeeding with RII, SII and CnI of 5•26 (2•63−10•54), 33•97 (21•88−46•05), and 0•27 (0•16−0•37), respectively. We observed lower levels of urban-rural inequalities with the highest RII, SII, and CnI in ORT of 2•46 (1•25−4•83), 29•32 (5•89−52•74), and 0•10 (0•02− 0•18), respectively. The comprehensive inequality analyses of all RMNCH service indicators in all survey years (2000 to 2014) are in Supplementary Table S16. A sub-analysis of socioeconomic inequalities stratified by living areas is presented in Supplementary Table S17, with higher socioeconomic inequalities in rural areas than in urban areas in most indicators.
Table 2.
Inequality of RMNCH service coverage in Vietnam in year 2014
| Indicators | Socioeconomic Inequality | Regional Inequality | Urban-Rural Inequality | ||||||
|---|---|---|---|---|---|---|---|---|---|
| RII (95% CI) | SII (95% CI) | CnI (95% CI) | RII (95% CI) | SII (95% CI) | CnI (95% CI) | RII (95% CI) | SII (95% CI) | CnI (95% CI) | |
| Prevention Indicators | |||||||||
| At least one ANC visit | 1•14 (1•11 to 1•18)*** | 13•26 (10•35 to 16•17)*** | 0•04 (0•03 to 0•05)*** | 1•13 (1•10 to 1•16)*** | 12•01 (9•52 to 14•50)*** | 0•04 (0•03 to 0•04)*** | 1•15 (1•10 to 1•20)*** | 13•47 (9•52 to 17•42)*** | 0•02 (0•01 to 0•02)*** |
| At least four ANC visit | 2•52 (2•28 to 2•79)*** | 71•41 (65•52 to 77•31)*** | 0•19 (0•17 to 0•20)*** | 2•08 (1•87 to 2•31)*** | 54•52 (47•62 to 61•41)*** | 0•14 (0•12 to 0•15)*** | 1•79 (1•58 to 2•03)*** | 41•98 (33•14 to 50•81)*** | 0•07 (0•05 to 0•09)*** |
| Exclusive breastfeeding | 0•27 (0•14 to 0•55)*** | -22•63 (-35•82 to -9•44)*** | -0•20 (-0•30 to -0•09)*** | 5•26 (2•63 to 10•54)*** | 33•97 (21•88 to 46•05)*** | 0•27 (0•16 to 0•37)*** | 0•44 (0•19 to 1•03) | -15•96 (-31•41 to -0•50)* | -0•09 (-0•18 to 0•00) |
| Early initiation of breastfeeding | 0•70 (0•56 to 0•86)*** | -15•61 (-24•42 to -6•80)*** | -0•06 (-0•09 to -0•03)*** | 1•47 (1•19 to 1•81)*** | 16•28 (7•56 to 24•99)*** | 0•06 (0•03 to 0•10)*** | 0•62 (0•48 to 0•81)*** | -19•17 (-29•38 to -8•96)*** | -0•05 (-0•08 to -0•02)*** |
| Family planning needs satisfied | 0•94 (0•88 to 1•02) | -3•45 (-8•02 to 1•13) | -0•01 (-0•02 to 0•00) | 1•15 (1•07 to 1•24)*** | 8•87 (4•35 to 13•39)*** | 0•02 (0•01 to 0•03)*** | 0•89 (0•82 to 0•97)* | -6•99 (-12•28 to -1•70)* | -0•01 (-0•02 to -0•00)** |
| BCG immunization | 1•12 (1•08 to 1•17)*** | 11•36 (7•76 to 14•96)*** | 0•03 (0•02 to 0•04)*** | 1•10 (1•07 to 1•14)*** | 9•69 (6•59 to 12•79)*** | 0•02 (0•01 to 0•03)*** | 1•13 (1•07 to 1•19)*** | 11•47 (6•47 to 16•47)*** | 0•01 (0•01 to 0•02)*** |
| DPT3 immunization | 1•49 (1•30 to 1•70)*** | 31•82 (21•90 to 41•74)*** | 0•07 (0•05 to 0•10)*** | 1•52 (1•33 to 1•73)*** | 32•75 (23•06 to 42•43)*** | 0•07 (0•05 to 0•10)*** | 1•17 (1•00 to 1•37) | 11•92 (-0•07 to 23•91) | 0•02 (-0•00 to 0•04) |
| Polio3 immunization | 1•34 (1•21 to 1•48)*** | 25•84 (17•66 to 34•01)*** | 0•06 (0•05 to 0•08)*** | 1•38 (1•25 to 1•51)*** | 27•81 (20•09 to 35•52)*** | 0•06 (0•04 to 0•08)*** | 1•24 (1•11 to 1•39)*** | 18•44 (8•68 to 28•21)*** | 0•03 (0•01 to 0•04)*** |
| Measles immunization | 1•28 (1•15 to 1•43)*** | 21•46 (12•36 to 30•57)*** | 0•05 (0•03 to 0•07)*** | 1•40 (1•26 to 1•55)*** | 28•18 (19•69 to 36•67)*** | 0•06 (0•04 to 0•08)*** | 1•02 (0•89 to 1•17) | 1•83 (-9•15 to 12•81) | 0•00 (-0•01 to 0•02) |
| Full immunization | 1•60 (1•35 to 1•90)*** | 33•94 (22•82 to 45•05)*** | 0•09 (0•06 to 0•11)*** | 1•70 (1•44 to 2•00)*** | 36•76 (25•95 to 47•57)*** | 0•09 (0•06 to 0•12)*** | 1•08 (0•89 to 1•32) | 5•17 (-8•21 to 18•55) | 0•01 (-0•01 to 0•03) |
| Improved Water | 1•25 (1•24 to 1•26)*** | 21•09 (20•41 to 21•76)*** | 0•05 (0•05 to 0•06)*** | 1•21 (1•20 to 1•22)*** | 17•85 (17•14 to 18•56)*** | 0•03 (0•03 to 0•03)*** | 1•23 (1•22 to 1•25)*** | 19•44 (18•47 to 20•40)*** | 0•03 (0•02 to 0•03)*** |
| Adequate sanitation | 1•84 (1•82 to 1•87)*** | 53•97 (53•03 to 54•92)*** | 0•16 (0•15 to 0•16)*** | 1•67 (1•65 to 1•70)*** | 44•13 (43•13 to 45•13)*** | 0•10 (0•10 to 0•11)*** | 1•62 (1•59 to 1•65)*** | 39•47 (38•05 to 40•89)*** | 0•06 (0•06 to 0•06)*** |
| Treatment Indicators | |||||||||
| Institutional delivery | 1•27 (1•22 to 1•33)*** | 23•00 (19•44 to 26•57)*** | 0•07 (0•06 to 0•08)*** | 1•24 (1•19 to 1•29)*** | 20•63 (17•19 to 24•08)*** | 0•06 (0•05 to 0•07)*** | 1•28 (1•21 to 1•35)*** | 22•77 (17•88 to 27•65)*** | 0•03 (0•02 to 0•04)*** |
| Skilled birth attendance | 1•23 (1•19 to 1•28)*** | 20•09 (16•73 to 23•46)*** | 0•06 (0•05 to 0•07)*** | 1•21 (1•16 to 1•25)*** | 17•91 (14•67 to 21•16)*** | 0•05 (0•05 to 0•06)*** | 1•24 (1•18 to 1•30)*** | 19•88 (15•27 to 24•50)*** | 0•03 (0•02 to 0•03)*** |
| Care seeking for pneumonia | 1•25 (1•00 to 1•56) | 19•58 (0•42 to 38•73)* | 0•04 (-0•00 to 0•08) | 1•40 (1•20 to 1•65)*** | 31•06 (18•06 to 44•06)*** | 0•08 (0•04 to 0•12)*** | 1•14 (0•87 to 1•49) | 11•54 (-11•90 to 34•98) | 0•01 (-0•02 to 0•05) |
| ARI treatment | 1•35 (1•05 to 1•75)* | 25•90 (4•71 to 47•09)* | 0•06 (0•01 to 0•10)* | 1•56 (1•30 to 1•89)*** | 38•98 (24•44 to 53•52)*** | 0•08 (0•04 to 0•12)*** | 1•43 (1•08 to 1•90)* | 30•42 (6•83 to 54•01)* | 0•04 (0•00 to 0•08)* |
| Oral rehydration therapy | 2•75 (1•50 to 5•04)*** | 29•63 (10•98 to 48•29)** | 0•15 (0•06 to 0•24)*** | 2•64 (1•44 to 4•85)** | 31•11 (14•07 to 48•14)*** | 0•16 (0•06 to 0•26)*** | 2•46 (1•25 to 4•83)** | 29•32 (5•89 to 52•74)* | 0•10 (0•02 to 0•18)* |
Notes: ***, **, * Statistically significant results with P<0•001, P<0•01, and P<0•05, respectively; RII=Relative Index of Inequality; SII=Slope Index of Inequality; CnI=Concentrate Index of Inequality; CI=Confidence Interval; The inequality analyses of UHC indicators at national and subnational levels during 2000–2014 are presented in the Supplementary.
The RII presents the ratio of health coverage between the top and bottom comparison groups (socioeconomic status, regional levels, and urban-rural areas). RII>1 indicates pro-rich inequality (higher coverage in the richest than in the poorest sub-groups); RII<1 indicates pro-poor inequality (higher coverage in the poorest than in the richest sub-groups); RII=1 suggests no inequality in the health indicator.
The SII indicates the difference in percentage points of health coverage between the top and bottom of comparing groups (socioeconomic status, regional levels, and urban-rural areas). SII>0 indicates pro-rich inequality (higher coverage in the richest than in the poorest sub-groups); SII<0 indicates pro-poor inequality (higher coverage in the poorest than in the richest sub-groups); SII=0 suggests unavailability of inequality in the health indicator.
The CnI determines the magnitude or extent of health inequality. CnI ranges from -1 to 1 with a positive value indicating a higher concentration of health coverage among the richer group and vice versa for a negative value. The closer value to 1 or -1, the higher degree of concentration. A zero value (0) of the CnI shows the unavailability of inequality in the health indicator.
The patterns of socioeconomic inequality in RMNCH service coverage are shown in Figure 2. In 2000, most indicators showed linear patterns (or queuing), except for ANC4. In 2014, there were tremendous transformations in most indicators with bottom inequality patterns. We predicted the year 2030 would end up with bottom inequality patterns among 7/11 (63•6%) prevention indicators. Figure 4 shows the RMNCH service indicators with statistically significant changes in all three indices (RII, SII, CnI) of socioeconomic, regional and urban-rural inequalities from 2000−2014, omitting non-significant indicators for simplicity. We found that adequate sanitation, Polio3, and SBA had the highest reductions in all socioeconomic, regional and urban-rural inequalities in a combination of relative, absolute and magnitude terms. Detailed estimates of changes in inequalities for all RMNCH service indicators with 95% CIs and p-values are in Supplementary Table S18. We observed no statistically significant changes in socioeconomic, regional and urban-rural inequalities in EBF, CSP, ARI treatment and ORT. In contrast, the indicator FPNS showed an increase in socioeconomic inequality but a decrease in regional inequality. Socioeconomic and regional inequalities in ANC4 decreased in relative terms but increased in absolute terms (Supplementary Table S18). Changes in socioeconomic inequalities over the period 2000−2014 stratified by living areas are in Supplementary Table S19 with more substantially reduced inequalities in rural areas than urban areas.
Figure 4.
Changes in inequalities of RMNCH service coverage in Vietnam from 2000 - 2014
Notes: The coloured squares are the RMNCH service indicators; The horizontal axis shows changes in relative index of inequality (RII), the vertical axis shows changes in slope index of inequality (SII), while the size of the squares indicates the absolute changes in concentration index of inequality (CnI); Only statistically significant changes in all three indices of RII, SII, and CnI were presented in the figure; Positive values express an increase in inequalities between two-time points, and negative values indicate a reduction in inequality; † data in the year 2002 was used due to unavailable of data for 2000.
4. Discussion
This study is the first comprehensive picture of RMNCH service coverage and progress toward UHC in Vietnam at national and sub-national levels. We found that most prevention and treatment indicators improved significantly from 2000–2014, and most indicators will achieve the global targets by 2030 at the national level. However, the analysis of wealth quintile-specific coverage showed significant gaps between the most disadvantaged and wealthiest groups. Additionally, our analyses suggest some regions are lagging and need to pay more attention and resources to progress in maternal and child health. Despite the significant improvements we identified in this study, socioeconomic, regional, and urban-rural inequalities still exist in several RMNCH service indicators with different patterns and trends, impeding UHC achievement in Vietnam.
In the present study, the majority (9/17) of RMNCH indicators and all three composite RMNCH indicators will certainly (90%–100%) reach the 2030 target at the national level. However, we found that the most deprived groups were still left behind with no chance of reaching 2030 targets in promoting maternal care (ANC4) and ensuring adequate sanitation. Improved and adequate sanitation are essential in improving the quality of life and preventing many infectious diseases. Low ability and willingness to pay for improved sanitation of poor households require implementation of policies/interventions in both economy and education that extend beyond individual efforts to improve sanitation environments.23 Three WHO's key family behaviour indicators (ORT, FPNS, and exclusive breastfeeding) have zero projected chance of achieving the 2030 target at national levels and all sub-national levels. The global coverage of using ORT for children with diarrhoea in 2015 was 41%, indicating that Vietnam's inadequate national coverage is not an exception.24 Previous works showed that traditional experience and self-treatment might affect people's healthcare practices, typically reducing the proportion using ORT in Vietnam.25 The low coverage of and a decreasing trend in FPNS calls for a long term commitment from the Vietnamese government to family planning policy.26 Early initiation of breastfeeding and exclusive breastfeeding show slow national progress and pro-poor inequality with higher coverage in the poorest than in the wealthiest subgroups.5 It probably dues to rapid urbanization, caesarean deliveries, inappropriate maternal leave policies, and other socio-cultural determinants.27,28 Knowing that early initiation and exclusive breastfeeding are the most effective intervention to reduce neonatal and early infant mortality,29,30 the low national coverages may pose a serious obstacle to achieving health equity in Vietnam. Achievement of adequate breastfeeding has been estimated to potentially prevent more than 3000 child and maternal deaths, saving US$1.5 million in health system costs and generating US$1.8 billion for the economy annually for Vietnam.31 However, improving health outcomes related to WHO's key family behaviours is greatly affected by households' socioeconomic and health literacy characteristics.32 Interventions for improving mother's health literacy and education and integrating husband's and elder's participation could be sufficient for the short-term goals. Given the lessons learned from other countries by targeting women's empowerment and gender equality,33 Vietnam should integrate these aspects into its national action plan to improve UHC and other health-related SDG outcomes in the long run.
Our findings showed that the poorest households in rural areas and the regions of Northwest, Northeast, North Central, Central Highlands, and Mekong River Delta would not reach the 80% coverage of DPT3, Polio3, Measles and full immunization. Notably, the vaccination program's ultimate goal is to reach herd immunity to prevent the transmission of infectious diseases, and it usually needs a higher coverage than UHC targets. The mandatory vaccination coverage for herd immunity can be roughly calculated based on the reproductive number (R0) of specific diseases in a population and the vaccine effectiveness (VE). For example, measles has an R0 of 16 for Asian populations, and the MMR vaccine has 97% efficacy for protecting people from measles after two doses.34 Thus, it will require at least (1-1/R0)/VE ~ 97% coverage among children to eliminate or prevent measles among school-aged populations. The gap between current coverage and the required coverage for herd immunity could explain the recent outbreaks of measles in remote and poor areas in Vietnam.35 The establishment of Vietnam's Expanded Programme on Immunization showed a massive impact on improving child mortality.36 However, to eliminate or interrupt highly contagious diseases like measles, vaccination coverage at the level required for herd immunity among new birth cohorts (children less than 24 months) is essential but may not enough. Vietnam should also maintain herd immunity in all birth cohorts at sub-national levels by (i) routinely monitoring population immunity to identify the left-behind groups; and (ii) exploring context-specific school entry checks of immunization status with strong collaboration between the ministry of health and the ministry of education.37 Further, multi-component interventions in improving knowledge and awareness surrounding vaccination need to be carefully considered and integrated into national health programs for coping with vaccine hesitancy, one of the ten global health threats.
Since the early 2000s, the Vietnamese government has made substantial changes to the healthcare system, specifically promoting a decentralized system with autonomous providers,38 reforming health insurance, and enhancing primary healthcare.39,40 The pyramid healthcare system in Vietnam worked well with fewer requirements for resources and individual efforts and was a major contributor to Vietnam's COVID-19 successes.41 However, despite those advantages and benefits, such decentralization does come to the risk of increasing inequalities between regions or widening poverty gaps within the country. The low-quality maternal health services in poor areas and the big gaps in personnel and equipment between and within localities may pose barriers to maternal health service utilization.42 The present study showed inequalities in all RMNCH indicators in 2014. There was no change in inequalities over 15 years in some of the lowest-coverage indicators in socioeconomic, regional, and urban-rural levels. This suggests that some of the current health programs have been ineffective in these areas, and the need for health system improvements before Vietnam can achieve the UHC targets. To achieve sustainable and equitable development, Vietnam should focus on government reforms to improve economic equality and complete the poverty alleviation goals across localities. The Vietnamese government could learn the lessons of managing government decentralization reforms from China, a neighbouring country with similar political institutions and administrative divisions, including (i) enhancing investment and resource competition between local governments; (ii) granting additional autonomy to high-performance local governments; and (iii) awarding more resources and more central control to low-performance governments to support them in competitive reforms. This "performance-based" decentralization reform could promote economic growth in all localities with diverse capacities and characteristics, reduce absolute poverty, and improve rural health and regional development.43 Additionally, perceptions of low quality in primary healthcare facilities among disadvantaged rural women and primary healthcare providers could be a potential barrier to the RMNCH service utilization.44 Vietnam's healthcare system needs to prepare for the complexity of disease patterns in rural areas and the growing demand for high-quality and high-tech healthcare services at primary healthcare facilities in the future. Doing so will avoid the concentration of health technology in the most advantaged urban areas and guarantee all parts of the country can benefit from future investments in advanced health technology. Further, it will ensure the achievement of effective UHC in Vietnam with high-quality and people-centred healthcare services.
By evaluating inequality changes in multiple dimensions, we were able to identify the true improvements in RMNCH service indicators, which are defined as significant reductions in all relative, absolute, and magnitude of inequalities. For example, ANC4 inequalities decreased in relative terms but increased in absolute terms, indicating that gaps in receiving four antenatal care visits between socioeconomic groups and regions became wider over time, even as levels of coverage improved across all groups. The reduction in ratio due to the improved coverages in all sub-groups created a false improvement in inequality of ANC4 if we only assess it in relative terms. We, therefore, highlight the use of all three dimensions to comprehensively and accurately evaluate inequalities in health. We recognized the government's efforts and initial achievements in enhancing health equality between urban-rural areas with the appropriate resource allocation to rural areas. However, our analyses identified the spurious improvements in urban-rural inequalities among DPT3, Measles, Full-immunization, which mainly occurred due to the slow progress in urban areas. Thus, these results may raise concerns about health interventions' effectiveness over time and suggest a rebalancing of the vaccination program between urban and rural areas is needed. Additionally, the target groups for future interventions may be different between RMNCH indicators depending on the patterns of inequalities.45
Our study has numerous strengths. First, it presents reliable and systematic estimates of RMNCH service indicators in Vietnam at national and sub-national levels based on high-quality population-based household data. Second, by using Bayesian methods, we could estimate the probability of achieving the 2030 targets.20 Third, our study comprehensively estimates patterns and trends in socioeconomic, regional, and urban-rural inequalities in RMNCH service indicators. It can help the government and policymakers in tailoring plans for future programs. Several limitations may also be inherent. Our study included all publicly available population-based data to 2014 when the last survey was completed and released. No post-2014 data and fewer data points in some indicators drove wide credible intervals of long-term trends and projections. The integration of data with different recall periods (two years in MICS and five years in DHS) posed some potential risks to our trend analyses.46 However, our sensitivity analysis of change in trends by matching DHS recall periods showed comparable results between unmatched- and matched-DHS recall period, suggested the low risk of bias in our trends and projections (Supplementary Table S20). Further, all our predictions of 2015−2030 were calculated based on the current trends of 2000−2014 and the assumption of unchanging future policy. Our projections are therefore unable to account for improvements in policies happening after 2020. However, they still offer a baseline estimate of progress against which the next 10 years of policy changes can be assessed. The improvement in data completeness and reliability of Viet Nam's national routine health management information system,47 the ongoing 2021 Multiple Indicator Cluster Surveys, and the possibility of meta-analysis from currently available literature warrant further investigation to update the estimated trends and projections of RMNCH coverage in Vietnam.
5. Conclusions
Vietnam is progressing toward UHC in most RMNCH service indicators given, despite its challenges. The Vietnamese government must continue to improve and reform the healthcare system, re-allocate resources focusing on vulnerable people (e.g., the most impoverished rural people), and evaluate and enhance current health programs and interventions. It is also essential to design a national plan that integrates a more social perspective on gender equality, women's empowerment, and other related SDGs. There is still a long way to go, but by strengthening both the health system and social approach to healthcare, we believe that Vietnam will achieve the UHC targets, which also helps the country achieve health for all.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
Author and contributors
Literature search: PTN, PML
Study concept: PTN, SG, SR
Study design: PTN
Data collection: PTN, HVN, LQK, MVH
Figures: PTN
Data analysis: PTN, SG, SR
Data interpretation: PTN
Writing first draft of manuscript: PTN, PML
Critical revision of the manuscript for important intellectual content: PTN, SR, PML, HVN, KV, HLN, AD, LQK, MVH, SG
Administrative, technical, or material support: PML, HVN, LQK, MVH
Supervision: SG
Data Availability statement
All data analysed in this study are publicly available from DHS (https://dhsprogram.com) and MICS program (https://mics.unicef.org). The R codes for statistical analysis and data visualization are available for research purposes upon reasonable request to the corresponding author.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2021.100230.
Appendix. Supplementary materials
References
- 1.UN General Assembly. Transforming our world: The 2030 Agenda for Sustainable Development. 2015 https://sustainabledevelopment.un.org/content/documents/21252030 Agenda for Sustainable Development web.pdf (accessed Oct 16, 2019).
- 2.WHO and World Bank . World Health Organization; 2015. Tracking universal health coverage: First global monitoring report. [Google Scholar]
- 3.WHO and World Bank . World Health Organization; 2017. Tracking universal health coverage: 2017 Global Monitoring Report. [Google Scholar]
- 4.Gilmour S, Le Mai P, Nguyen P, Dhungel B, Tomizawa M, Nguyen H. Progress towards Health for All: Time to End Discrimination and Marginalization. Int J Environ Res Public Health. 2020;17:1696. doi: 10.3390/ijerph17051696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization (WHO) 2015. State of inequality: Reproductive, maternal, newborn and child health. Geneva. [Google Scholar]
- 6.World Health Organization (WHO) 2019. 2019 Global Monitoring Report: Primary Health Care on the Road to Universal Health Coverage. Geneva, Switzerland. https://www.who.int/healthinfo/universal_health_coverage/report/uhc_report_2019.pdf?ua=1 (accessed March 25, 2020) [Google Scholar]
- 7.World Bank Group. Moving toward UHC : Vietnam - national initiatives, key challenges, and the role of collaborative activities. 2017.
- 8.Bredenkamp C, Buisman LR, Prencipe LM, Wagstaff A. 2012. Vietnam - Health equity and financial protection report. Washington, DC. [Google Scholar]
- 9.PAHE . 2014. Health system in Vietnam: Towards target with equity. Hanoi, Vietnam. www.isds.org.vn (accessed May 4, 2020) [Google Scholar]
- 10.World Bank . 2012. Well Begun, Not Yet Done: Vietnam's Remarkable Progress on Poverty Reduction and the Emerging Challenges. Hanoi, Vietnam. https://openknowledge.worldbank.org/handle/10986/12326 (accessed April 16, 2021) [Google Scholar]
- 11.Van Minh H, Pocock NS, Chaiyakunapruk N. Progress toward universal health coverage in ASEAN. Glob Health Action. 2014;7 doi: 10.3402/gha.v7.25856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wagstaff A, Neelsen S. A comprehensive assessment of universal health coverage in 111 countries: a retrospective observational study. Lancet Glob Heal. 2020;8:e39–e49. doi: 10.1016/S2214-109X(19)30463-2. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization, The World Bank . 2014. Monitoring progress towards universal health coverage at country and global level: Framework, measures and targets. Geneva, Switzerland. https://www.who.int/healthinfo/universal_health_coverage/report/2014/en/ (accessed April 5, 2020) [Google Scholar]
- 14.World Health Organization (WHO). Toward a global action plan for healthy lives and well-being for all: Uniting to accelerate progress towards the health-related SDGs. 2018 https://www.who.int/sdg/global-action-plan/Global_Action_Plan_Phase_I.pdf (accessed Oct 16, 2019).
- 15.Boerma T, AbouZahr C, Evans D, Evans T. Monitoring Intervention Coverage in the Context of Universal Health Coverage. PLoS Med. 2014;11 doi: 10.1371/journal.pmed.1001728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rahman MS, Rahman MM, Gilmour S, Swe KT, Krull Abe S, Shibuya K. Trends in, and projections of, indicators of universal health coverage in Bangladesh, 1995–2030: a Bayesian analysis of population-based household data. Lancet Glob Heal. 2018;6:e84–e94. doi: 10.1016/S2214-109X(17)30413-8. [DOI] [PubMed] [Google Scholar]
- 17.Lim SS, Allen K, Dandona L. Measuring the health-related Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015. Lancet. 2016;388:1813–1850. doi: 10.1016/S0140-6736(16)31467-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hogan DR, Stevens GA, Hosseinpoor AR, Boerma T. Monitoring universal health coverage within the Sustainable Development Goals: development and baseline data for an index of essential health services. Lancet Glob Heal. 2018;6:e152–e168. doi: 10.1016/S2214-109X(17)30472-2. [DOI] [PubMed] [Google Scholar]
- 19.O'Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. The World Bank; Washington DC: 2007. Analyzing Health Equity Using Household Survey Data: a guide to techniques and their implementation. [DOI] [Google Scholar]
- 20.Gelman A, Carlin JB, Stern HS, Dunson DB, Vehtari A, Rubin DB. Chapman and Hall/CRC; London, UK: 2013. Bayesian data analysis, third. https://www.crcpress.com/Bayesian-Data-Analysis/Gelman-Carlin-Stern-Dunson-Vehtari-Rubin/p/book/9781439840955 (accessed Sept 15, 2019) [Google Scholar]
- 21.Nguyen PT, Gilmour S, Le PM, Onishi K, Kato K, Nguyen HV. Progress toward HIV elimination goals: trends in and projections of Annual HIV testing and Condom use in Africa. AIDS. 2021 doi: 10.1097/qad.0000000000002870. published online March 16. [DOI] [PubMed] [Google Scholar]
- 22.Bürkner P-C. brms : An R Package for Bayesian Multilevel Models Using Stan. J Stat Softw. 2017;80:1–28. [Google Scholar]
- 23.Van Minh H, Hung NV, Thanh NH, Yang JC. Assessing willingness to pay for improved sanitation in rural Vietnam. Environ Health Prev Med. 2013;18:275–284. doi: 10.1007/s12199-012-0317-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.UNICEF. The state of the World's Children 2016: A fair chance for every child. New York, 2016 www.soapbox.co.uk (accessed June 15, 2020).
- 25.Rheinländer T, Samuelsen H, Dalsgaard A, Konradsen F. Perspectives on child diarrhoea management and health service use among ethnic minority caregivers in Vietnam. BMC Public Health. 2011;11 doi: 10.1186/1471-2458-11-690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hellwig F, Coll CV, Ewerling F, Barros AJ. Time trends in demand for family planning satisfied: analysis of 73 countries using national health surveys over a 24-year period. J Glob Health. 2019;9 doi: 10.7189/jogh.09.020423. –020423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Almroth S, Arts M, Quang ND, Hoa PTT, Williams C. Exclusive breastfeeding in Vietnam: an attainable goal. Acta Pdiatrica. 2008;97:1066–1069. doi: 10.1111/j.1651-2227.2008.00844.x. [DOI] [PubMed] [Google Scholar]
- 28.Le QNT, Phung KL, Nguyen VTT. Factors associated with a low prevalence of exclusive breastfeeding during hospital stay in urban and semi-rural areas of southern Vietnam. Int Breastfeed J. 2018;13:46. doi: 10.1186/s13006-018-0188-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edmond K, Newton S, Hurt L. Timing of initiation, patterns of breastfeeding, and infant survival: Prospective analysis of pooled data from three randomised trials. Lancet Glob Heal. 2016;4:e266–e275. doi: 10.1016/S2214-109X(16)00040-1. [DOI] [PubMed] [Google Scholar]
- 30.Gilmour S, Shibuya K. Simple steps to equity in child survival. BMC Med. 2013;11:261. doi: 10.1186/1741-7015-11-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walters DD, Phan LTH, Mathisen R. The cost of not breastfeeding: Global results from a new tool. Health Policy Plan. 2019;34:407–417. doi: 10.1093/heapol/czz050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization (WHO). The World Health Report 2005: Make every mother and child count. Geneva, 2005.
- 33.Remme M, Vassall A, Fernando G, Bloom DE. Investing in the health of girls and women: a best buy for sustainable development. BMJ. 2020;369:m1175. doi: 10.1136/bmj.m1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guerra FM, Bolotin S, Lim G. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017;17:e420–e428. doi: 10.1016/S1473-3099(17)30307-9. [DOI] [PubMed] [Google Scholar]
- 35.The World Health Organization (WHO) WHO; 2019. Measles – Global situation: Disease outbreak news.http://www.who.int/csr/don/26-november-2019-measles-global_situation/en/ published online Nov 27. (accessed April 16, 2021) [Google Scholar]
- 36.Jit M, Huyen DTT, Friberg I. Thirty years of vaccination in vietnam: Impact and cost-effectiveness of the national expanded programme on immunization. Vaccine. 2015;33:A233–A239. doi: 10.1016/j.vaccine.2014.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization Regional Office for the Western Pacific. Regional strategy and plan of action for measles and rubella elimination in the Western Pacific. Manila, Philippines, 2017 http://iris.wpro.who.int/handle/10665.1/14227.
- 38.Lieberman SS, Capuno JJ, Van Minh H. East Asia Decentralizes: Making Local Government Work. World Bank, Washington, DC; Washington, DC: 2005. Decentralizing Health: Lessons from Indonesia, the Philippines, and Vietnam; p. 267. [Google Scholar]
- 39.Fritzen SA. Legacies of primary health care in an age of health sector reform: Vietnam's commune clinics in transition. Soc Sci Med. 2007;64:1611–1623. doi: 10.1016/j.socscimed.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 40.Jowett M, Contoyannis P, Vinh ND. The impact of public voluntary health insurance on private health expenditures in Vietnam. Soc Sci Med. 2003;56:333–342. doi: 10.1016/s0277-9536(02)00031-x. [DOI] [PubMed] [Google Scholar]
- 41.Van Nguyen H, Van Hoang M, Dao ATM. An adaptive model of health system organization and responses helped Vietnam to successfully halt the Covid-19 pandemic: What lessons can be learned from a resource-constrained country. Int J Health Plann Manage. 2020;35:988–992. doi: 10.1002/hpm.3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heo J, Kim SY, Yi J. Maternal, neonatal, and child health systems under rapid urbanization: A qualitative study in a suburban district in Vietnam. BMC Health Serv Res. 2020;20:90. doi: 10.1186/s12913-019-4874-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu X, Ramesh M, Yu J. Autonomy and Performance: Decentralization Reforms in Zhejiang Province, China. Public Adm Dev. 2017;37:94–109. [Google Scholar]
- 44.McKinn S, Linh DT, Foster K, McCaffery K. A qualitative analysis of factors that influence Vietnamese ethnic minority women to seek maternal health care. BMC Pregnancy Childbirth. 2019;19:1–12. doi: 10.1186/s12884-019-2375-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barros AJD, Victora CG. Measuring Coverage in MNCH: Determining and Interpreting Inequalities in Coverage of Maternal, Newborn, and Child Health Interventions. PLoS Med. 2013;10 doi: 10.1371/journal.pmed.1001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ngandu NK, Manda S, Besada D, Rohde S, Oliphant NP, Doherty T. Does adjusting for recall in trend analysis affect coverage estimates for maternal and child health indicators? An analysis of DHS and MICS survey data. Glob Health Action. 2016;9 doi: 10.3402/GHA.V9.32408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hong TT, Hoa NP, Walker SM, Hill PS, Rao C. Completeness and reliability of mortality data in Viet Nam: Implications for the national routine health management information system. PLoS One. 2018;13 doi: 10.1371/journal.pone.0190755. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data analysed in this study are publicly available from DHS (https://dhsprogram.com) and MICS program (https://mics.unicef.org). The R codes for statistical analysis and data visualization are available for research purposes upon reasonable request to the corresponding author.