Abstract
Objective:
Depressive disorders are common among adults with alcohol use disorder and with suicidality; however, demographic differences in comorbid alcohol use disorder, binge drinking, and suicidality are understudied. The objective of this study was to determine the extent to which comorbid suicidality and alcohol use disorders and comorbid suicidality and binge drinking differ by age and gender among adults with depressive symptoms.
Method:
The sample included adults (unweighted N=29,460) in the United States who completed the 2015–2018 National Survey of Drug Use and Heath and screened positively for depression. Gender and age groups odds of alcohol use disorder only, suicidality only, and alcohol use disorder+suicidality were compared to neither problem. Similar analyses were conducted for binge drinking.
Results:
Men showed disproportional odds of alcohol use disorder only, all suicidality and alcohol use disorder comorbidities, and binge drinking+active suicidal ideation than women. Emerging adults showed higher odds of: passive and active suicidal ideation only and suicidality+alcohol use disorder than adults 35 and older; binge drinking only, binge drinking+passive suicidal ideation, and binge drinking+active suicidal ideation than all older adults; binge drinking+suicide planning and binge drinking+attempts than adults 50 and older.
Limitations:
Because participants all reported depression symptoms either at the subclinical or clinical level, demographic differences in suicidality, alcohol use disorder, and binge drinking found in this study cannot be generalized to non-depressed samples.
Conclusions:
Treatment providers should be aware of disproportionately higher odds of comorbid suicidality and alcohol use disorder, and suicidality and binge drinking among men and emerging adults.
Keywords: alcohol use disorders, binge drinking, suicidality, gender, emerging adults, depressive symptoms
In the US, over one in ten (13.9%) adults meet criteria for alcohol use disorder annually and almost a third (29.1%) meets criteria in their lifetime (Grant et al., 2015). Alcohol use costs roughly $250 billion annually in loss of life, lost work, medical care, and criminal justice, among other costs, with binge drinking accounting for 70% of costs; government funding covered about 40% of costs, with the remainder borne by persons who misuse alcohol, families, and society (Sacks et al., 2015). Suicidality (e.g., suicidal ideation and attempts) is highly comorbid with alcohol use disorder; adults with alcohol use disorder show 86% greater odds of suicidal ideation and approximately 3 times greater odds of suicide attempt (Darvishi et al., 2015). Understanding demographic differences in alcohol use disorder and binge drinking in representative samples and identifying key vulnerable groups, such as those with comorbid suicidality, can inform broad prevention and intervention efforts.
Depressive symptoms are correlates of both alcohol use disorder and suicidality. Adults with alcohol use disorder report elevated rates of past year major depressive disorder (16.6%) compared to the general population without alcohol use disorder (9.5%; Chen et al., 2016). Among adults with depressive disorders, depressive symptom severity and co-occurring alcohol or drug use disorder are related to suicide death (Hawton et al., 2013). Although comparatively little work has examined comorbidities of these problems, comorbid alcohol use disorder and depression increase risk of active suicidal ideation (Cohen et al., 2017). Alcohol intoxication is also related to greater suicide attempt lethality among those with alcohol use disorder and mood disorders (Sher et al., 2009).
Studies of suicidality risk factors often use clinical samples; however, suicidality is common in the general population, even in the absence of mental health diagnoses. For example, over half of people who die by suicide have no diagnosed mental health disorder as measured by psychological autopsy (Stone et al., 2018). Core depressive symptoms (i.e., depressed mood, anhedonia) are independently associated with suicidality. Specifically, depressed mood is proximally related to suicidal ideation among persons with depression (Ben-Zeev et al., 2012). Anhedonia is associated with suicidal ideation, even when controlling for other depressive symptoms (Ducasse et al., 2018). The current study investigates suicidality correlates among persons with any depressive symptoms, as subthreshold symptoms increase risk for suicidality.
Among those with depressive symptoms, men and emerging adults (i.e., ages 18–25) are two groups who may have higher rates of binge drinking, alcohol use disorder, suicidality, and their comorbidities. Gender differences in binge drinking and alcohol use disorder have been narrowing since the 1950s, with women’s rates increasing more rapidly than men’s (Dawson et al., 2015; Keyes et al., 2008). Data from the National Survey of Drug Use and Health (NSDUH) show adolescent girls were more likely than boys to initiate drinking every year from 2002–2013; however, males were more likely to continue drinking into their 20s (Cheng et al., 2016). Despite earlier initiation, females are not more likely to develop alcohol use disorder; instead males show a shorter time to alcohol use disorder after drinking initiation (Keyes et al., 2010). In population-based surveys, men continue to report higher rates of binge drinking than women (Wilsnack et al., 2018). Despite the narrowing gender gap in binge drinking and alcohol use disorder, men may still have greater risk for negative alcohol sequelae than women.
Gender differences in suicidality depend on suicidality severity, with more men dying by suicide and more women reporting suicidal ideation and attempts (Nock, Borges, Bromet, Cha, et al., 2008; Nock, Borges, Bromet, Alonso, et al., 2008). In the 2008 and 2009 NSDUH, women (3.9%) were more likely than men (3.5%) to report past year active suicidal ideation (Posner et al., 2011), but there were no gender differences in suicide planning or attempts (Crosby et al., 2011). In the 2014 NSDUH, there were no gender differences in past year active suicidal ideation, but women were more likely than men to report past year suicide planning (1.2% vs 1.0%) and attempts (0.5% vs 0.4%; Lipari et al., 2015).
For decades, binge drinking and alcohol use disorder have disproportionally affected emerging adults in the US compared to other ages (Schulenberg et al., 2019). Emerging adults show higher past month binge drinking (34.9% vs 25.1%) and past year alcohol use disorder (10.1% vs 5.1%) compared to adults over 25 (Substance Abuse and Mental Health Services Administration [SAMHSA], 2019). Emerging adults also report higher rates of suicidality compared to older ages. Suicidal ideation, planning, and attempts are higher among emerging adults (11%, 3.4%, and 1.9%, respectively) compared to older adults aged 26–49 (4.7%, 1.4%, 0.6%) and 50+ (2.1%, 0.6%, 0.2%; SAMHSA, 2019). Suicidal ideation, planning, and attempts increased from 2005–2017 in emerging adults, but not adults aged 26–49 and 50+ (Twenge et al., 2019). Increases in suicide attempts have disproportionally occurred in adults ages 18–34 and adults with depressive disorders (Olfson et al., 2017).
Demographic correlates of passive suicidal ideation are understudied. Passive suicidal ideation includes wishes for death and thoughts that life is not worthwhile, without intent or plans to engage suicidal behavior or thoughts of killing oneself (Posner et al., 2011). Two national samples of adults with depressive symptoms reported rates of passive suicidal ideation of 11.3% and 10.2% and risk of suicide attempts was similar among persons with passive and with active suicidal ideation (Baca-Garcia et al., 2011). Indeed, a recent meta-analysis found that passive and active suicidal ideation showed similarly strong relationships with suicide attempts and suicide death (Liu et al., 2020). Since suicidal ideation intensity can vary dramatically over days and hours (Kleiman et al., 2017), it is important to understand the spectrum of suicidality in relation to alcohol use disorder and binge drinking.
Women are more likely to have depressive symptoms and diagnoses compared to men (Salk et al., 2017), while men show consistently higher rates of alcohol use disorder (Grant et al., 2015). However, multiple theoretical frameworks suggest that male depression is under-detected because symptoms are masked by substance use, are under-reported, or are minimized by masculine expectations of affective expression (Addis, 2008). With alternative depression criteria that include substance use, risk taking, and aggression, rates of depression in men exceed that of women (Martin et al., 2013). If men tend to use substances in the context of depressive symptoms like suicidality, comorbid alcohol use disorders and suicidality may be more common in men than women. In addition, younger age of onset is associated with greater severity of alcohol use disorder (Grant et al., 2015) so emerging adults with alcohol use disorder may experience suicidality secondary to distress and impairment associated with severe alcohol use disorder symptoms. Normative and faster improvements in impulse control throughout emerging adulthood are associated with lower alcohol use disorder risk (Littlefield et al., 2010), and lower impulse control is associated with drinking and drinking to cope with emotions (Herman & Duka, 2019). Emerging adults with depressive symptoms may therefore show greater suicide attempt and alcohol use disorder comorbidity compared to older adults.
Current Study
This study investigated gender and age differences in alcohol use disorders independent of suicidality, suicidality independent of alcohol use disorders, and comorbid alcohol use disorders and suicidality in a national US sample. We aimed to understand relationships between alcohol use disorder and a spectrum of suicidality, ranging from passive suicidal ideation, active suicidal ideation, suicide planning, and suicide attempts. We hypothesized that men would demonstrate higher rates of alcohol use disorder and comorbid alcohol use disorder and suicide attempts, while women would report higher rates of each form of suicidality independent of alcohol use disorder. We expected emerging adults to show higher rates of alcohol use disorder, suicidality, and comorbidity relative to older ages. Second, we investigated gender and age differences in binge drinking independent of suicidality, suicidality independent of binge drinking, and comorbid binge drinking and suicidality. We hypothesized that men and emerging adults would have higher rates of binge drinking and comorbid binge drinking and suicidality, relative to women and older adults, respectively.
Methods
Participants
This study used publicly available data from the NSDUH, combining four consecutive years of data from 2015–2018. The NSDUH is a nationally representative, cross-sectional survey of the U.S. civilian population aged 12 or older, who live in non-institutionalized settings (e.g., households, group quarters including college dormitories, and civilians on military bases). SAMHSA conducts this survey annually using a multilevel stratified hierarchical sampling procedure to determine the prevalence of substance use and related disorders in the US. Multi-state area probability sampling creates a nationally representative sample. There are three stages of sample selection: first, within each state, state sampling regions are formed, roughly based on population. Second, segments are chosen within each census tract with aggregate adjacent census blocks. Third, out of the 48 segments formed, 8 are chosen for any given year of data collection. Lastly, all eligible dwelling units and persons are chosen from within segments (see Center for Behavioral Health Statistics and Quality, 2019 for detailed sampling procedures). Weighted interview response rates were 69.3% in 2015, 68.4% in 2016, 67.1% in 2017, and 66.56% in 2018. The adult representative sample includes 171,766 respondents. For the current analyses, data were restricted to adults who endorsed depression screening items (N = 29,936 unweighted) and were therefore administered suicidality items of interest. Of adults who reported depressive symptoms, 476 (1.6%) did not complete the passive suicidal ideation item and were excluded. The final sample (N=29,460 unweighted) is representative of adults with any depressive symptoms (17% of the total 2015–2018 NSDUH sample).
Procedures
The NSDUH is conducted face-to-face by professional interviewers using computer-assisted personal interviewing and audio computer-assisted self-interviewing. Sampling redesign was conducted in 2014 to redistribute sample sizes by state and age so that the sample derived from each state and age group was more proportional to their relative population sizes (see Center for Behavioral Health Statistics and Quality, 2015). Thus, the 2015–2018 datasets were used given their identical sampling and survey methods for variables of interest. Data collection for the NSDUH is sponsored by SAMHSA and conducted in compliance with the Research Triangle Institute International Institutional Review Board. Secondary analyses of this de-identified data are considered exempt from IRB oversight by the first and senior authors’ institution.
Measures
Gender.
Gender was recorded as male or female.
Age.
Age was categorized into six groups (18–25 years, 26–34 years, 35–49 years, 50–64 years, 65+).
Alcohol.
Diagnosis of either past year DSM-IV alcohol abuse or alcohol dependence indicated presence of an alcohol use disorder. Alcohol abuse was defined as six or more days of alcohol use in the past 12 months and one or more of the following, secondary to alcohol use: (1) problems at work, home, or school; (2) regularly using and engaging in physically dangerous behavior; (3) repeated legal trouble; and (4) continued use despite social problems. Alcohol dependence was defined as six or more days of alcohol use in the past 12 months and three or more of the following, secondary to alcohol use: (1) spent a lot of time on drinking activities, (2) used in greater quantities or for a longer time than intended, (3) developed tolerance, (4) made unsuccessful attempts to cut down or stop, (5) continued use despite physical health or emotional problems, (6) reduced or stopped participating in other activities, and (7) experienced withdrawal symptoms after cutting back or stopping.
Binge drinking was assessed in the prior month, defined as five or more drinks on the same occasion for men and four or more drinks on the same occasion for women.
Suicidality.
Four past-year suicidality variables were included: passive suicidal ideation, active suicidal ideation, suicide plans, and suicide attempts. These four items were administered within the depression screening and only to those who screened positively, as defined as endorsing past year depressed and/or anhedonic mood. The NSDUH depression module is based on DSM-IV diagnostic criteria (American Psychiatric Association, 2000). The current version was adapted from the National Comorbidity Survey-Replication interview, which has good concordance with the structured interview used by the World Health Organization and is related to psychosocial impairment (Kessler et al., 2003). Respondents were queried about suicidality during the month of worst depressed and/or anhedonic mood in the past year. Passive suicidal ideation was defined as endorsement of the item “Did you ever think that it would be better if you were dead?” Active suicidal ideation was defined as endorsement of the item “Did you think about committing suicide?” Only persons who active suicidal ideation were asked suicide plans and attempts items (i.e., “Did you make a suicide plan?”; “Did you make a suicide attempt?”).
Covariates.
Race and ethnicity responses were recoded into non-Hispanic White and Racial/Ethnic Minority (non-Hispanic Black/African American, non-Hispanic Native American/Alaskan Native, non-Hispanic Native Hawaiian or Pacific Islander, non-Hispanic Asian, non-Hispanic Multiracial, or Hispanic). For educational attainment, participants were asked their last completed grade and highest degree earned. Responses were recoded as high school graduate or less and compared to more than a high school diploma (e.g., some college, associate’s degree or higher). Household income was reported in $10,000 increments from $10,000 to $50,000, $50,000 to $74,000, and $75,000 and higher. Marital status was coded as married, never married, or separated/divorced/widowed. Sexual orientation was assessed by “Which one of the following do you consider yourself to be?” with responses “heterosexual, that is, straight”; “lesbian or gay”, or “bisexual”. For these analyses, lesbian/gay and bisexual responses were combined into sexual minority orientation. Responses of “don’t know”, refused, and blank responses were coded as a third category, as older adults may be more likely than younger adults to skip sexual orientation items (Fredriksen-Golsen & Kim, 2015). Substance use disorder was assessed with the same criteria as alcohol, with one exception; cannabis use disorder criteria did not include withdrawal. Year of NSDUH administration (2015–2018) was included, given increases in suicidality over time (SAMHSA, 2019).
Data analytic plan
Multinomial logistic regression models examined gender and age differences in four groups: neither suicidality nor alcohol use disorder, suicidality only, alcohol use disorder only, and both suicidality and alcohol use disorder. Adults with neither passive suicidal ideation nor alcohol use disorder were compared to those with passive suicidal ideation only, alcohol use disorder only, and both passive suicidal ideation and alcohol use disorder. Similar analyses were conducted with each active suicidal ideation, suicide plans, and suicide attempts. Adults with neither suicidality nor alcohol use disorders were the reference group in all four models. Similar models examined comorbid past-month binge drinking and the four suicidality groups. Regressions without covariates first tested the independent impact of gender and age on alcohol use disorder and suicidality, and binge drinking and suicidality. Due to relationships with alcohol use disorders and/or suicidality, we then controlled for race/ethnicity (Twenge et al., 2019; Vaeth et al., 2017; Williams et al., 2018), income (Grant et al., 2015), educational attainment (Olfson et al., 2017; Rosoff et al., 2019), marital status (Miller-Tutzauer et al., 1991), sexual orientation (Hottes et al., 2016; Medley et al., 2016), and other substance use disorders (Lipari et al., 2015; May & Klonsky, 2016) in all models. Since there were seven income categories, the distribution did not violate normality assumptions, and to reduce lost power from multiple comparisons, income was entered as a continuous variable.
Bonferroni-corrected p-values are reported for main effects to reduce Type 1 error risk. Odds ratios (ORs) were converted to percent likelihood odds by: (for ORs<1)%=OR/1+OR, or (for ORs 1–1.99)%=[(1–OR)x100]. SPSS Complex Samples Version 26 was used to account for NSDUH sampling procedures (SAMHSA, 2019). Population estimates were calculated across the four years included in this study.
Results
Preliminary Analyses
This sample is representative of adults in the US with depressive symptoms (Table 1). More than half (62.6%) was female. Age groups from 18–64 were roughly equal size, while fewer respondents were 65+. The majority identified as non-Hispanic White (74.3%), heterosexual (89.3%), unmarried (58.2%), with more than high school education (71.8%). Among adults with depressive symptoms, 48.4% reported passive suicidal ideation and 37.5% reported active suicidal ideation. Of those with active suicidal ideation, 34.9% reported suicide planning and 23.4% reported suicide attempt(s). Past year alcohol use disorder prevalence was 11.7% and past month binge drinking was 29.6%. Figures 1 and 2 depict rates of suicidality alone, alcohol use disorders alone, and their comorbidity, and of suicidality, binge drinking, and their comorbidity.
Table 1.
Demographic Characteristics (N = 29,460)
| Unweighted n | Weighted SE | Weighted % | |
|---|---|---|---|
| Total | 29,460 | 1,206,320 | 100 |
| Year | |||
| 2015 | 7,153 | 678,934 | 24.1 |
| 2016 | 7,170 | 670,621 | 24.2 |
| 2017 | 7,530 | 804,123 | 26.1 |
| 2018 | 7,607 | 681,144 | 25.6 |
| Gender | |||
| Male | 10,524 | 669,403 | 37.4 |
| Female | 18,935 | 954,303 | 62.6 |
| Age | |||
| 18–25 years | 11,144 | 383,509 | 18.8 |
| 26–34 years | 6,321 | 391,051 | 18.8 |
| 35–49 years | 7,726 | 575,083 | 26.6 |
| 50–64 years | 3,016 | 686,170 | 24.5 |
| 65 and older | 1,253 | 697,055 | 11.3 |
| Race/Ethnicity | |||
| Non-Hispanic White | 20,429 | 1,161,468 | 74.2 |
| Racial/ethnic minority | 0.031 | 608,200 | 25.8 |
| Education | |||
| High school or less | 9,248 | 586,562 | 28.2 |
| > High school | 20,212 | 1,115,430 | 71.8 |
| Income | |||
| Less than $10,000 | 2,992 | 344,610 | 7.7 |
| $10,000-$19,999 | 3,580 | 432,619 | 10.6 |
| $20,000-$29,999 | 3,244 | 338,567 | 9.8 |
| $30,000-$39,000 | 3,031 | 366,029 | 9.7 |
| $40,000-$49,000 | 2,965 | 416,528 | 9.8 |
| $50,000-$74,000 | 4,554 | 538,665 | 16.2 |
| $75,000 or more | 9,050 | 795,732 | 36.2 |
| Marital Status | |||
| Married | 9,578 | 981,549 | 41.7 |
| Widowed/divorced/separated | 4,680 | 480,224 | 22.4 |
| Never been married | 15,202 | 656,978 | 35.9 |
| Sexual orientation | |||
| Heterosexual/Straight | 24,967 | 1,109,408 | 88.8 |
| Lesbian/Gay/Bisexual | 4,284 | 375,010 | 10.6 |
| Don’t know, did not answer | 209 | 97,924 | 0.6 |
| Substance Use Disorder | 2,733 | 287,335 | 7.3 |
| Passive Suicidal Ideation | 15,259 | 763,288 | 48.4 |
| Active Suicidal Ideation | 12,157 | 668,485 | 37.5 |
| Suicide Plan | 4,580 | 324,133 | 34.9 |
| Suicide Attempt | 3,091 | 323721 | 23.5 |
| Alcohol Use Disorder | 4,157 | 364,607 | 11.7 |
| Binge Drinking | 10,036 | 641,508 | 29.5 |
Notes. Alcohol and substance use disorders were assessed within the past year. Sample sizes for suicidality items differ: passive suicidal ideation = 29,460; active suicidal ideation = 29,415; suicide plan = 12,154; suicide attempt 12,139 (unweighted n’s). Suicide plan and attempt items were only answered by those who endorsed active suicidal ideation.
Figure 1.
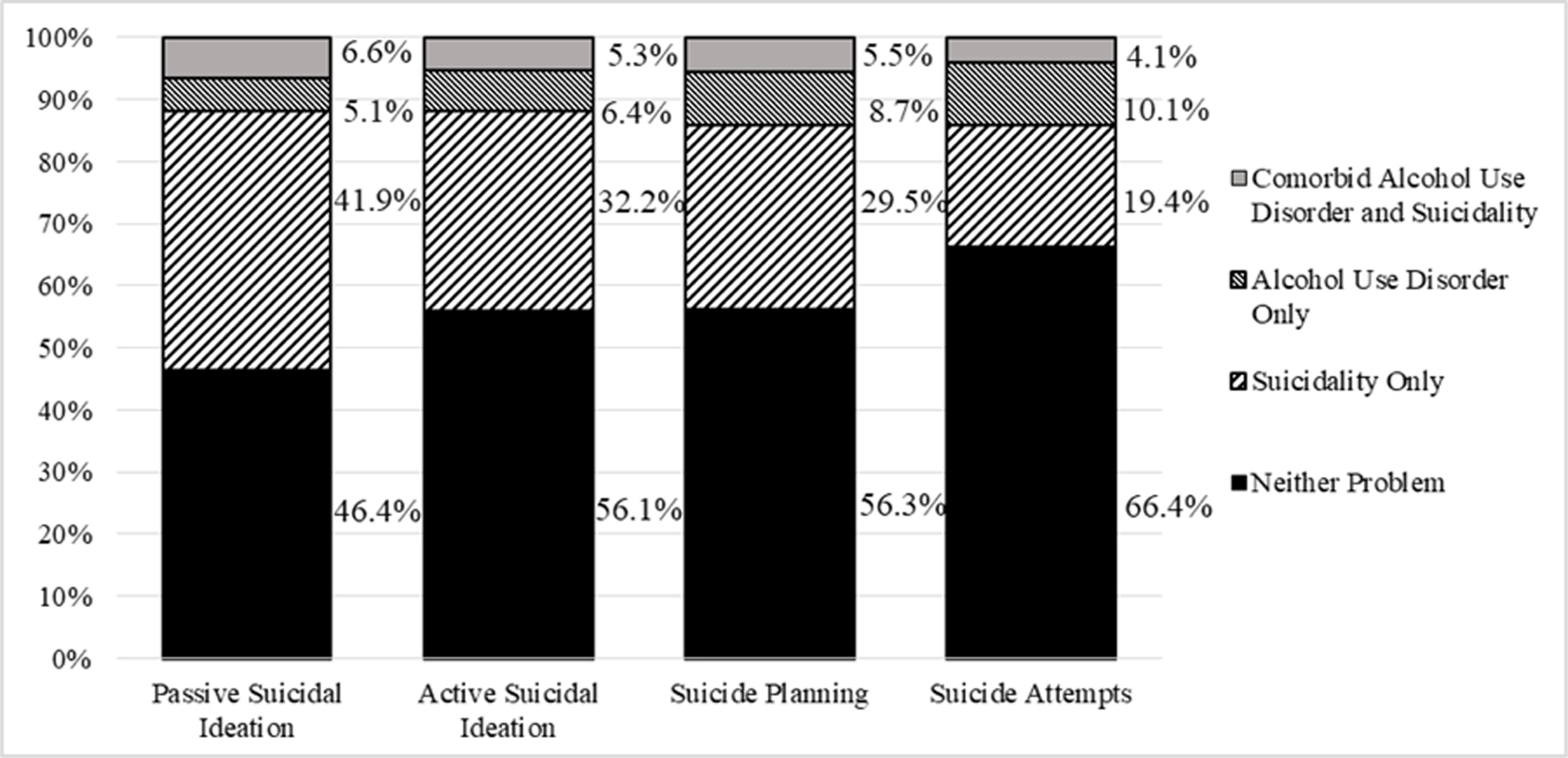
Rates of Alcohol Use Disorder Only, Suicidality Only, and Their Comorbidities across the Four Types of Suicidality
Note. Numbers on the vertical axis and in each subsection of the bars indicate the percent of the sample (i.e., adults who endorsed depressive symptoms) reporting each problem (e.g., 6.6% of the adults in the United States who report any depressive symptoms have comorbid alcohol use disorder and passive suicidal ideation). Each bar represents one of the four types of suicidality (passive suicidal ideation, active suicidal ideation, suicide planning or suicide attempts).
Figure 2.
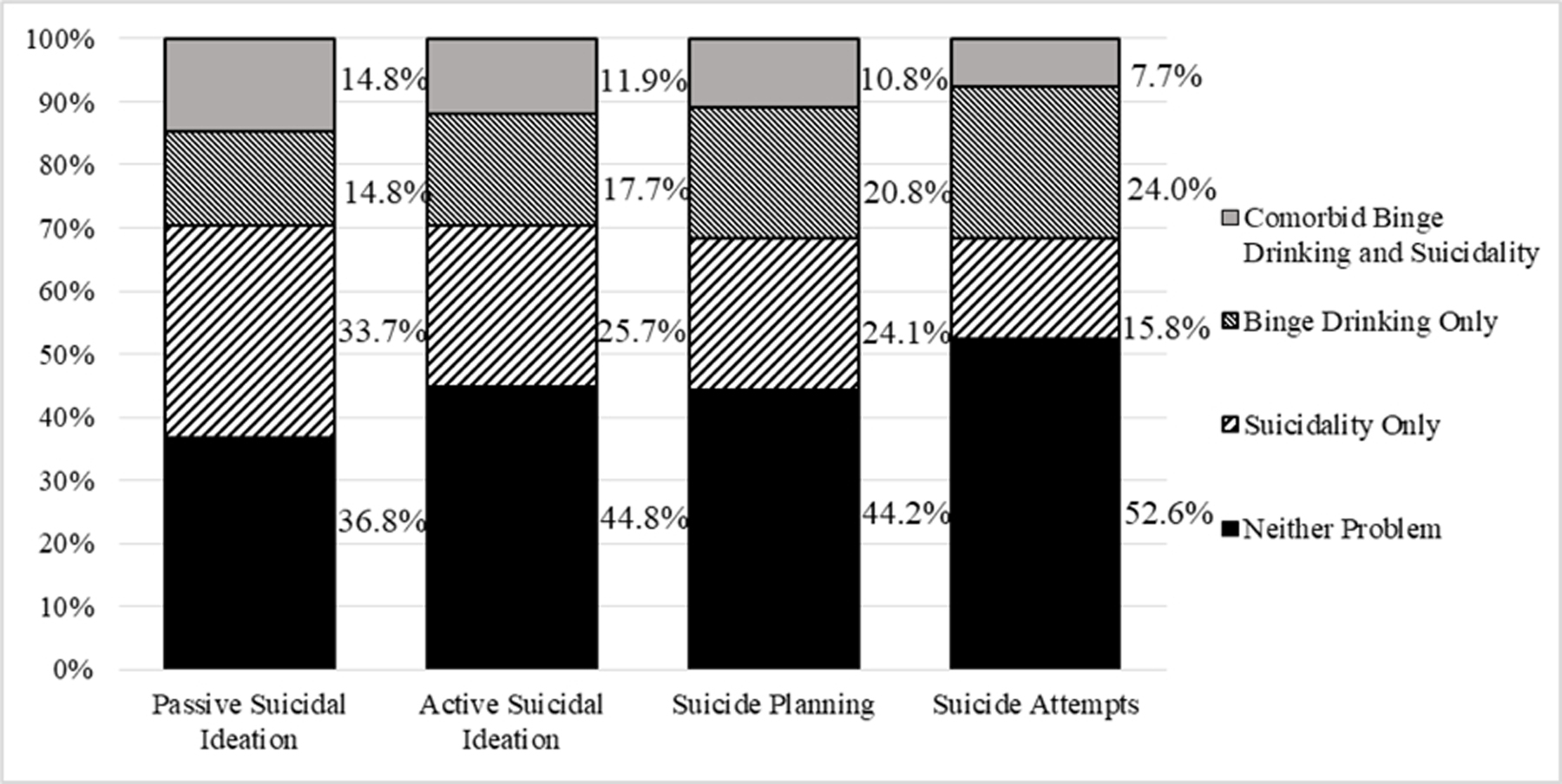
Rates of Binge Drinking Only, Suicidality Only, and Their Comorbidities across the Four Types of Suicidality
Note. Numbers on the vertical axis and in each subsection of the bars indicate the percent of the sample (i.e., adults who endorsed depressive symptoms) reporting each problem (e.g., 14.8% of the adults in the United States who report any depressive symptoms have comorbid binge drinking and passive suicidal ideation). Each bar represents one of the four types of suicidality (passive suicidal ideation, active suicidal ideation, suicide planning or suicide attempts).
Unadjusted Gender and Age Differences in Comorbid Alcohol Use Disorder, Binge Drinking, and Suicidality
Supplemental tables 1 and 2 show unadjusted models examining gender and age differences in alcohol use disorder and suicidality comorbidities, and in binge drinking and suicidality comorbidities, without accounting for relevant covariates. Men reported higher odds of active suicidal ideation and lower odds of suicide planning than women. Men reported lower odds of suicide attempts (independent of alcohol use disorders) than women. Out of 48 age comparisons, 41 were significant; all but one showed significantly higher odds of suicidality and alcohol use disorder in emerging adults. For binge drinking, men were more likely than women to report comorbid binge drinking and both passive and active suicidal ideation. Thirty-eight age comparisons were significant, all showing higher odds of outcomes in emerging adults. Bolded estimates in supplemental tables show estimates that fell to non-significance in adjusted models.
Gender and Age Differences in Comorbid Alcohol Use Disorder and Suicidality
Table 2 shows odds ratios for gender and age in alcohol use disorder only, suicidality only, and comorbid alcohol use disorder and suicidality, when accounting for covariates. Men reported 53%−92% increased odds of alcohol use disorder only compared to women. Men and women did not differ in passive suicidal ideation only or suicide attempts only. Men reported 22% higher odds of active suicidal ideation only, whereas women had 47% higher odds of suicide plans. Men were more likely than women to report all four types of suicidality comorbid with alcohol use disorders (ORs=1.38–1.84).
Table 2.
Alcohol Use Disorders and Suicidality Comorbidity by Gender and Age
| Gender | Age | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Wald χ2 | OR Male [95% CI] | Wald χ2 | OR 26–34 [95% CI] | OR 35–49 [95% CI] | OR 50–64 [95% CI] | OR 65+ [95% CI] | |||
| Passive SI and AUD | 80.85*** | 199.48*** | |||||||
| Passive SI Only | .96 [.90–1.04] | M=W | 1.18*** [1.08–1.30] | 1.31*** [1.16–1.48] | 1.28*** [1.14–1.45] | 1.83*** [1.53–2.19] | 18–25>26+ | ||
| AUD Only | 1.92*** [1.58–2.32] | M>W | .83* [.69–1.0] | 1.10 [.87–1.39] | 1.69** [1.23–2.31] | 4.49*** [2.51–8.04] | 18–25<26–34 1825>50+ | ||
| AUD+Passive SI | 1.53 [1.34–1.74]*** | M>W | 1.17 [.97–1.41] | 1.49*** [1.25–1.77] | 2.03*** [1.55–2.66] | 5.76*** [3.79–8.76] | 18–25>35+ | ||
| Active SI and AUD | 101.99*** | 213.59*** | |||||||
| Active SI Only | 1.22*** [1.12–1.32] | M>W | 1.24*** [1.13–1.36] | 1.42*** [1.27–1.58] | 1.52*** [1.33–1.74] | 2.06*** [1.68–2.54] | 18–25>26+ | ||
| AUD Only | 1.89*** [1.61–2.21] | M>W | .88 [.74–1.04] | 1.16 [.92–1.46] | 1.71*** [1.28–2.29] | 4.33*** [2.57–7.31] | 18–25>50+ | ||
| AUD+Active SI | 1.84*** [1.57–2.17] | M>W | 1.19 [.97–1.46] | 1.53** [1.26–1.85] | 2.34*** [1.73–3.16] | 6.26*** [3.32–11.81] | 18–25>35+ | ||
| Suicide Plan and AUD | 37.86*** | 37.56*** | |||||||
| Suicide Plan Only | .89* [.80–.99] | M<W | 1.12 [.96–1.32] | 1.09 [.94–1.26] | 1.16 [.93–1.44] | 1.55** [1.13–2.14] | 18–25>65+ | ||
| AUD Only | 1.49*** [1.25–1.78] | M>W | .94 [.71–1.24] | 1.00 [.79–1.27] | 1.65* [1.10–2.49] | 2.10* [1.02–4.30] | 18–25>50+ | ||
| AUD+Suicide Plan | 1.46* [1.09–1.95] | M>W | 1.09 [.85–1.41] | 1.23 [.92–1.64] | 1.62* [1.02–2.56] | 11.67* [1.74–78.31] | 18–25>50+ | ||
| Suicide Attempt and AUD | 30.50*** | 42.59** | |||||||
| Suicide Attempt Only | .86 [.75–1.00] | M=W | .99 [.83–1.18] | .99 [.79–1.23] | 1.09 [.84–1.41] | 1.40 [.93–2.10] | 18–25 = 26+ | ||
| AUD Only | 1.53*** [1.28–1.82] | M>W | .92 [.71–1.20] | .91 [.79–1.05] | 1.86*** [1.35–2.57] | 2.68* [1.20–5.60] | 18–25>50+ | ||
| AUD+Suicide Attempt | 1.38* [1.07–1.79] | M>W | 1.04 [.79–1.38] | 1.17 [.83–1.66] | 1.11 [.71–1.73] | 4.62 [.94–22.76] | 18–25=26+ | ||
Note.
p<.001,
p<.01,
p<.05.
AUD = alcohol use disorders. SI = suicidal ideation. Neither suicidality nor alcohol use disorders are the dependent reference group in all four analyses. For gender, female = reference group. For age, 18–25-year-olds = reference group; odds ratios compare 18–25-year-olds to each older age group, with odds ratios over 1.0 meaning greater likelihood among 18–25-year-olds compared to older age groups. Analyses control for year, race/ethnicity, education, income, marital status, sexual orientation, and other substance use disorder. Bonferroni corrections are applied to p-values for main effects.
Emerging adults were more likely to report passive suicidal ideation only, active suicidal ideation only, comorbid alcohol use disorder and passive suicidal ideation, and comorbid alcohol use disorder and active suicidal ideation than most older ages. Emerging adults and 35–49-year-olds did not differ in likelihood of alcohol use disorder only. Adults aged 26–34 shows 45% higher odds of alcohol use disorder only compared to emerging adults in passive suicidal ideation analyses, but not other suicidality analyses. Emerging adults reported 65–86% increased odds of alcohol use disorder alone compared to adults aged 50–64 and 2.10–4.49 times the odds of alcohol use disorder alone compared to adults 65+. Emerging adults reported 18%−83% higher odds of passive suicidal ideation only and 1.24–2.06 times higher odds of active suicidal ideation only compared to older ages. Emerging adults reported 1.49–5.76 times higher odds of comorbid alcohol use disorder and passive suicidal ideation and 1.53–6.26 times higher odds of comorbid alcohol use disorder and active suicidal ideation compared to ages 35+. Emerging adults and 26–34-year-olds did not differ in suicide planning, suicide attempts, alcohol use disorder, or their comorbidities.
Emerging adults were 55% more likely than ages 65+ to report suicide planning only. Adults aged 35–49 were 45% more likely than emerging adults to report a suicide attempt only. Emerging adults showed 55% higher odds of comorbid alcohol use disorder and suicide planning compared to adults aged 50–64 and 11.67 times higher odds of comorbid alcohol use disorder and suicide plans compared to ages 65+. Emerging adults did not differ from older adults in either comorbid alcohol use disorder and suicide planning or attempts.
Gender and Age Differences in Comorbid Binge Drinking and Suicidality
Table 3 presents adjusted odds ratios for binge drinking and suicidality and their comorbidities. Men had 12–33% higher odds of binge drinking only compared to women. Men were 36% more likely than women to report active suicidal ideation only. Gender differences in passive suicidal ideation, suicide planning, and suicide attempts were not significant. Men reported 36% higher odds of comorbid binge drinking and active suicidal ideation compared to women. Gender differences in remaining comorbidities were not significant.
Table 3.
Binge Drinking and Suicidality Comorbidity by Gender and Age
| Gender | Age | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Wald χ2 | OR Male [95% CI] | Wald χ2 | OR 26–34 [95% CI] | OR 35–49 [95% CI] | OR 50–64 [95% CI] | OR 65+ [95% CI] | |||
| Passive SI and Binge Drinking | 28.71*** | 573.15*** | |||||||
| Passive SI Only | 1.02 [.94–1.49] | M=W | 1.19** [1.06–1.34] | 1.34*** [1.17–1.61] | 1.37*** [1.20–1.56] | 1.94*** [1.63–2.31] | 18–25>26+ | ||
| Binge Drinking Only | 1.33*** [1.19–1.49] | M>W | .94 [.81–1.09] | 1.37*** [1.17–1.61] | 2.30*** [1.92–2.75] | 4.33*** [3.09–6.07] | 18–25>35+ | ||
| Binge+Passive SI | 1.10 [.99–1.21] | M=W | 1.17* [1.04–1.33] | 1.79*** [1.52–2.12] | 2.56*** [2.15–3.05] | 6.67*** [5.05–8.80] | 18–25>26+ | ||
| Active SI and Binge Drinking | 59.95*** | 472.43*** | |||||||
| Active SI Only | 1.26*** [1.16–1.37] | M>W | 1.28*** [1.13–1.45] | 1.42*** [1.25–1.62] | 1.62*** [1.40–1.87] | 2.18*** [1.80–2.64] | 18–25>26+ | ||
| Binge Drinking Only | 1.29*** [1.17–1.42] | M>W | .98 [.86–1.12] | 1.37*** [1.19–1.58] | 2.27*** [1.91–2.68] | 4.30*** [3.16–5.85] | 18–25>35+ | ||
| Binge+Active SI | 1.36*** [1.22–1.52] | M>W | 1.20** [1.07–1.34] | 1.91*** [1.62–2.26] | 2.90*** [2.37–3.54] | 7.05*** [4.82–10.32] | 18–25>26+ | ||
| Suicide Plan and Binge Drinking | 5.65 | 137.77*** | |||||||
| Suicide Plan Only | .91 [.79–1.04] | M=W | 1.04 [.87–1.24] | 1.01 [.85–1.21] | 1.10 [.85–1.43] | 1.32 [.96–1.84] | 18–25~26+ | ||
| Binge Drinking Only | 1.08 [.93–1.26] | M=W | .87 [.73–1.04] | 1.22 [.99–1.49] | 1.73*** [1.36–2.21] | 2.24*** [1.46–3.44] | 18–25>50+ | ||
| Binge+Suicide Plan | 1.0 [.85–1.16] | M=W | 1.11 [.89–1.40] | 1.62*** [1.27–2.06] | 2.12*** [1.55–2.89] | 27.89*** [7.86–98.93] | 18–25>35+ | ||
| Suicide Attempt and Binge Drinking | 8.53 | 148.59*** | |||||||
| Suicide Attempt Only | .93 [.79–1.08] | M=W | .89 [.72–1.09] | .88 [.73–1.05] | .99 [.74–1.32] | 1.20 [.80–1.78] | 18–25=26+ | ||
| Binge Drinking Only | 1.12* [1.0–1.26] | M>W | .86 [.72–1.03] | 1.27* [1.05–1.55] | 1.79*** [1.42–2.26] | 2.72*** [1.78–4.16] | 18–25>35+ | ||
| Binge+Suicide Attempt | .90 [.74–1.10] | M=W | 1.08 [.82–1.43] | 1.37* [1.02–1.84] | 1.78** [1.20–2.64] | 9.55*** [3.23–28.26] | 18–25>35+ | ||
Note.
p<.001,
p<.01,
p<.05.
SI = Suicidal ideation. Neither suicidality nor binge drinking is the dependent reference group in all four analyses. For gender, female = reference group. For age, 18–25year-olds = reference group; odds ratios compare 18–25-year-olds to each older age group, with greater odds ratios over 1.0 meaning greater likelihood among 18–25-year-olds compared to older age groups. Analyses control for year, race/ethnicity, education, income, marital status, sexual orientation, and other substance use disorder. Bonferroni corrections are applied to p-values for main effects.
Emerging adults had 1.27–4.33 times higher odds of binge drinking only compared to 35+ age groups in all four analyses. Differences in binge drinking between emerging adults and 26–34-year-olds were not significant. Emerging adults reported 19%−94% higher odds of passive suicidal ideation only compared to older ages and 1.28–2.18 times higher odds of reporting active suicidal ideation only compared to older ages. Age differences in suicide planning only and suicide attempt only were not significant. Emerging adults reported 1.17–7.05 times higher odds of comorbid binge drinking and both passive and active suicidal ideation compared to older ages. With the exception of 26–34-year-olds, emerging adults reported 1.62–27.89 times higher odds of comorbid binge drinking and suicide planning compared to older ages. Emerging adults showed 78% higher odds of comorbid binge drinking and suicide attempts than 50–64-year-olds and 9.55 times higher odds of comorbid binge drinking and suicide attempts than adults 65+.
Discussion
Findings elucidate gender and age differences in comorbid alcohol use disorder and suicidality and in binge drinking and suicidality. Men were more likely to experience alcohol use disorder independent of suicidality and to experience alcohol use disorder and suicidality comorbidity across severity of suicidality from passive suicidal ideation to suicide attempts. Emerging adults consistently reported higher comorbid suicidal ideation, alcohol use disorder, and binge drinking than adults 35+. Emerging adults reported more severe suicidality and both alcohol use disorder and binge drinking than adults 50+.
In contrast to higher rates of active suicidal ideation among women in general population samples (Nock et al., 2008) but similar adults with major depressive disorder in the NSDUH (Cheek et al., 2016), this study found higher rates of active suicidal ideation among men with depressive symptoms. Similar to higher rates of suicide attempts in women compared to men in the NSDUH (Crosby et al., 2011) and the National Comorbidity Survey–Replication (Nock & Kessler, 2006), women in this study showed higher rates of suicide planning compared to men. However, gender differences in suicide attempts were not significant when accounting for covariates, suggesting other demographic factors may account for women’s increased odds of suicide attempts. Notably, the present study included only those with depressive symptoms. Men’s suicidal ideation may have increased, as the current study used data from 2015–2018, while Crosby and colleagues (2011) analyzed 2008 NSDUH data. Men showed higher likelihood of comorbid alcohol use disorder and suicide planning and attempts than women, but not comorbid binge drinking and suicide planning or attempts. Alcohol use disorder, compared to binge drinking, may have stronger relationships with severe suicidality. Binge drinking may be more normative and not infer the same level of predisposition or shared genetic risk as alcohol use disorder and suicidality (Brady, 2006).
Emerging adults showed striking profiles of suicidal ideation and both comorbid alcohol use disorder and binge drinking. Emerging adults were also overrepresented in comorbidities with more severe suicidality (i.e., alcohol use disorder and suicide planning, binge drinking and suicide planning, binge drinking and suicide attempt). Adults with chronic suicidality may have died by suicide or other causes by later adulthood, which would mean this study compared emerging adults to older adults who may think about, but not engage in suicidal behavior. However, higher rates of suicidality and alcohol use disorders observed during emerging adulthood likely highlight this developmental stage as a true period of risk, in line with elevated rates of mental health and substance use disorders in this age group (Kessler et al., 2007); such problems tend to subside over time for many people (Gustavson et al., 2018). Arnett (2005) suggests that emerging adults use alcohol because of developmental processes, such as the stress of feeling ‘in-between’ adolescence and adulthood, experimentation and risk taking, living with peers rather than family, and low consideration of consequences. Stress and instability in emerging adulthood may contribute to suicidality; however, alcohol use may also contribute to suicidality and vice versa, or these two problems could present concurrently.
Although we have discussed these findings primarily in terms of age effects, cohort effects may be impacting results. For example, participants who were emerging adults during the time of data collection fall into either Generation Z or Generation Y/Millennials. These cohorts may have increased incidence of mental health problems and greater stress related to gun violence, climate change, rising suicide rates, separation and deportation of immigrant families, and sexual harassment relative to older cohorts (American Psychological Association, 2018). The study design does not allow for disentangling age and cohort effects so findings may not fully apply to future or past cohorts of emerging adults.
This study expands the knowledge base on passive suicidal ideation, which many have argued is clinically distinct from active suicidal ideation (Baca-Garcia et al., 2011). Passive suicidal ideation literature has focused on veterans (Kimbrel et al., 2015; May et al., 2015; Pfeiffer et al., 2014) and emergency department patients (Allen et al., 2013) and primarily in relation to suicidal behavior (Baca-Garcia et al., 2011). The current study extends this research by identifying relatively high rates of comorbid passive suicidal ideation and both alcohol use disorder and binge drinking in a representative US sample with depressive symptoms. Notably, men reported higher rates of comorbid alcohol use disorder and passive suicidal ideation than women, but similar rates of passive suicidal ideation alone. Men reported higher rates of active suicidal ideation alone, comorbid alcohol use disorder and active suicidal ideation, and comorbid binge drinking and active suicidal ideation. Similarities across men and women in passive suicidal ideation, and differences in active suicidal ideation (independent of alcohol use disorder and binge drinking), supports conceptualizing passive and active suicidality as distinct experiences with different correlates.
Underlying processes related to binge drinking, alcohol use disorder, and suicidality may overlap and contribute to comorbidity. Alcohol use disorder increases predisposition for suicide attempts (e.g., social problems, impulsivity, aggression), and intoxication directly increases risk for suicide attempt by lowering inhibitions and increasing depressed mood, hopelessness, stressful events, and suicidal ideation (Lamis & Malone, 2012; Norström & Rossow, 2016). In one clinical study in Germany, comorbid alcohol use disorder and suicide attempts were more common among men and older adults than women and younger adults (Boenisch et al., 2010). In the present study of adults with depressive symptoms in the US, men and younger adults were most likely to have comorbid alcohol use disorder and suicide attempts, but no age differences were apparent for comorbid binge drinking and suicide attempts. Men and emerging adults may have more psychological vulnerability for suicidality or are more prone to interpersonal conflict, life stressors, hopelessness or aggression while drinking, which in turn increase risk for suicidality. Alcohol use disorder is also associated with impulsive suicide attempts (i.e., no reported premeditation; Spokas et al., 2012); emerging adults do not yet possess fully developed executive functioning capacity for impulse-control (Littlefield et al., 2010) and may therefore be more prone to suicide attempts secondary to alcohol use.
Several limitations are worth mentioning. First, death by suicide or from complications due to alcohol use disorder were not considered; both causes of death are higher in middle-age and older adults compared to emerging adults (Hedegaard et al., 2020; White et al., 2020). Second, respondents needed to be willing to participate in an audio-assisted self-guided interview and report depressive symptoms. Although suicidality is common among persons with depressive disorders, it is not pathognomonic of depression and occurs across psychopathology (e.g., anxiety disorders; Bomyea et al., 2013) and independent of mental health diagnosis (Nock et al., 2019). Therefore, findings apply specifically to those with subclinical and clinical depression. Age by gender interactions were attempted, but did not run, perhaps due to categorical age groups in the public NSDUH data. Additionally, some distinct covariate groups were collapsed into less specific groupings to provide stable estimates (e.g., separated, divorced, and widowed people were collapsed into a single marital status group; racial/ethnic groups had to be collapsed into a dichotomous variable in order for models to converge). Lastly, mechanisms that may explain gender and age differences in alcohol use disorder, binge drinking, and suicidality, such as experiences of sexism, gendered emotional expression, and developmental stressors, were not assessed.
Future studies should examine comorbidity between alcohol use disorder and suicidality in population-based samples irrespective of depressive symptoms. Studies with additional years (i.e., at least seven years for joint point regressions) could test longitudinal differences in prevalence of alcohol use disorder, suicidality, and their comorbidity by gender and age. Additional theory-driven research could elucidate why men and emerging adults were more likely to report comorbid alcohol use disorder and suicidality and binge drinking and suicidality, such as differences in constructs proposed by the interpersonal psychological theory (Joiner, 2005; Van Orden et al., 2010).
Results have important public health and clinical implications. This study strengthens the rationale for recommendations for depression screenings on college campuses (American College Health Association, 2010) and in primary care (Siu et al., 2016), as well as alcohol and suicide screenings in these settings (American College Health Association, 2010; Curry et al., 2018; Kaplan et al., 2014; LeFevre & Force, 2014; Siu et al., 2016). Healthcare providers should be aware of the higher prevalence of comorbid alcohol use disorder and suicidal ideation among men and emerging adults. Interventions for binge drinking should include skills to manage passive and active suicidal ideation, to prevent worsening suicidality. The consistent risk profile for emerging adults suggests that, while college campuses are directing resources toward alcohol safety and reducing alcohol consumption (Carey et al., 2016; Scott-Sheldon et al., 2014), such interventions should be bolstered with suicide safety planning. Large scale depression screening efforts on college campuses and clinical settings may need to increase their capacity for alcohol and suicidality screenings as well as access to interventions for alcohol, depression, and suicidality. Public health efforts, like the truth® campaign which was associated with reductions in tobacco use among young adults (Vallone et al., 2017), should be applied to binge drinking. Population-level initiatives are needed to support the millions of adults struggling with suicidality, alcohol use disorder, and binge drinking.
Supplementary Material
Highlights.
In adults with depressive symptoms, rates of alcohol use disorder, binge drinking, and suicidality are higher is some groups
Men and emerging adults were more likely than women and older adults to have both alcohol use disorder and suicidality
Men and emerging adults showed higher rates of both binge drinking and suicidal thoughts than women and older adults
Clinicians should be aware of high rates of suicidality in adults with alcohol use disorders, particularly men and emerging adults
Suicide prevention should be part of alcohol use disorder prevention and treatment
Role of Funding Sources
Data used in the current study are publicly available from the Substance Abuse and Mental Health Data Archive (https://datafiles.samhsa.gov/info/browse-studies-nid3454). Manuscript preparation for this study was funded in part by the T32AA007290 that covered Dr. Kelly’s time, as well as K23DA034879, R01MD013550, RF1MH120830, R01MH101138, and R01MH115905. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or SAMHSA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Competing Interests
The authors do not have any conflicts of interests to report.
References
- Addis ME (2008). Gender and depression in men. Clinical Psychology: Science and Practice, 15(3), 153–168. 10.1111/j.1468-2850.2008.00125.x [DOI] [Google Scholar]
- Allen MH, Abar BW, McCormick M, Barnes DH, Haukoos J, Garmel GM, & Boudreaux ED (2013). Screening for suicidal ideation and attempts among emergency department medical patients: instrument and results from the Psychiatric Emergency Research Collaboration. Suicide & Life-Threatening Behavior, 43(3), 313–323. 10.1111/sltb.12018 [DOI] [PubMed] [Google Scholar]
- American College Health Association (2010). Considerations for integration of counseling and health services on college and university campuses. Journal of American College Health, 58(6), 583–596. 10.1080/07448481.2010.482436 [DOI] [PubMed] [Google Scholar]
- Baca-Garcia E, Perez-Rodriguez MM, Oquendo MA, Keyes KM, Hasin DS, Grant BF, & Blanco C (2011). Estimating risk for suicide attempt: Are we asking the right questions? Passive suicidal ideation as a marker for suicidal behavior. Journal of Affective Disorders, 134(1–3), 327–332. 10.1016/j.jad.2011.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Young MA, & Depp CA (2012). Real-time predictors of suicidal ideation: mobile assessment of hospitalized depressed patients. Psychiatry Research, 197(1–2), 55–59. 10.1016/j.psychres.2011.11.025 [DOI] [PubMed] [Google Scholar]
- Boenisch S, Bramesfeld A, Mergl R, Havers I, Althaus D, Lehfeld H, Niklewski G, & Hegerl U (2010). The role of alcohol use disorder and alcohol consumption in suicide attempts-A secondary analysis of 1921 suicide attempts. European Psychiatry, 25(7), 414–420. 10.1016/j.eurpsy.2009.11.007 [DOI] [PubMed] [Google Scholar]
- Bomyea J, Lang AJ, Craske MG, Chavira D, Sherbourne CD, Rose RD, Golinelli D, Campbell-Sills L, Welch SS, Sullivan G, Bystritsky A, Roy-Byrne P, & Stein MB (2013). Suicidal ideation and risk factors in primary care patients with anxiety disorders. Psychiatry Research, 209(1), 60–65. 10.1016/j.psychres.2013.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady J (2006). The association between alcohol misuse and suicidal behaviour. Alcohol and Alcoholism, 41(5), 473–478. 10.1093/alcalc/agl060 [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Garey L, Elliott JC, & Carey MP (2016). Alcohol interventions for mandated college students: a meta-analytic review. Journal of Consulting and Clinical Psychology, 84(7), 619–632. 10.1037/a0040275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2015) National Survey on Drug Use and Health: 2014 and 2015 redesign changes. Substance Abuse and Mental Health Services Administration. Rockville, MD. [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2019). 2018 National Survey on Drug Use and Health: methodological resource book (section 2, sample design report). Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Cheek SM, Nestor BA & Liu RT (2016). Substance use and suicidality: Specificity of substance use by injection to suicide attempts in a nationally representative sample of adults with major depression. Depression & Anxiety, 33, 541–548. 10.1002/da.22407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng HG, Cantave MD, & Anthony JC (2016). Taking the first full drink: epidemiological evidence on male–female differences in the United States. Alcoholism: Clinical and Experimental Research, 40(4), 816–825. 10.1111/acer.13028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen GH, Fink DS, Sampson L, Tamburrino M, Liberzon I, Calabrese JR, & Galea S (2017). Coincident alcohol dependence and depression increases risk of suicidal ideation among Army National Guard soldiers. Annals of Epidemiology, 27(3), 157–163.e1. 10.1016/j.annepidem.2016.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosby AE, Han B, Ortega LAG, Parks SE, & Gfroerer J (2011). Suicidal thoughts and behaviors among adults aged >/=18 years--United States, 2008–2009. Morbidity and Mortality Weekly Report. Surveillance summaries, 60(13), 1–22. [PubMed] [Google Scholar]
- Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, Doubeni CA, Epling JW, Kemper AR, Kubik M, Landefeld CS, Mangione CM, Silverstein M, Simon MA, Tseng CW, & Wong JB (2018). Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force recommendation statement. JAMA, 320(18), 1899–1909. 10.1001/jama.2018.16789 [DOI] [PubMed] [Google Scholar]
- Darvishi N, Farhadi M, Haghtalab T, & Poorolajal J (2015). Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide: a meta-analysis. PloS One, 10(5), e0126870–e0126870. 10.1371/journal.pone.0126870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Saha TD, & Grant BF (2015). Changes in alcohol consumption: United States, 2001–2002 to 2012–2013. Drug and Alcohol Dependence, 148, 56–61. 10.1016/j.drugalcdep.2014.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducasse D, Loas G, Dassa D, Gramaglia C, Zeppegno P, Guillaume S, Olié E, & Courtet P (2018). Anhedonia is associated with suicidal ideation independently of depression: a meta-analysis. Depression and Anxiety, 35(5), 382–392. 10.1002/da.22709 [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, & Hasin DS (2015). Epidemiology of DSM-5 Alcohol Use Disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. Journal of the American Medical Association, 72(8), 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustavson K, Knudsen AK, Nesvåg R, Knudsen GP, Vollset SE, & Reichborn-Kjennerud T (2018). Prevalence and stability of mental disorders among young adults: findings from a longitudinal study. BMC Psychiatry, 18(1), 65. 10.1186/s12888-018-1647-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Casañas I Comabella C, Haw C, & Saunders K (2013). Risk factors for suicide in individuals with depression: a systematic review. Journal of Affective Disorders, 147(1–3), 17–28. 10.1016/j.jad.2013.01.004 [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, & Warner M (2020). Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief, no 356. Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Herman AM, & Duka T (2019). Facets of impulsivity and alcohol use: What role do emotions play? Neuroscience and Biobehavioral Reviews, 106, 202–216. 10.1016/j.neubiorev.2018.08.011 [DOI] [PubMed] [Google Scholar]
- Hottes TS, Bogaert L, Rhodes AE, Brennan DJ, & Gesink D (2016). Lifetime prevalence of suicide attempts among sexual minority adults by study sampling strategies: a systematic review and meta-analysis. American Journal of Public Health, 106(5), e1–e12. 10.2105/AJPH.2016.303088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, McFarland BH, Caetano R, Conner KR, Giesbrecht N, & Nolte KB (2014). Use of alcohol before suicide in the United States. Annals of Epidemiology, 24(8), 588–592.e2. 10.1016/j.annepidem.2014.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Amminger GP, Aguilar - Gaxiola S, Alonso Caballero J, Lee S, & Ustun TB (2007). Age of onset of mental disorders: a review of recent literature. Current Opinion in Psychiatry, 20(4), 359–364. 10.1097/YCO.0b013e32816ebc8c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, & Wang PS (2003). The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA, 289(23), 3095–3105. 10.1001/jama.289.23.3095 [DOI] [PubMed] [Google Scholar]
- Keyes KM, Grant BF, & Hasin DS (2008). Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug and Alcohol Dependence, 93(1–2), 21–29. 10.1016/j.drugalcdep.2007.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Martins SS, Blanco C, & Hasin DS (2010). Telescoping and gender differences in alcohol dependence: new evidence from two national surveys. The American Journal of Psychiatry, 167(8), 969–976. 10.1176/appi.ajp.2009.09081161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Gratz KL, Tull MT, Morissette SB, Meyer EC, DeBeer BB, Silvia PJ, Calhoun PC, & Beckham JC (2015). Non-suicidal self-injury as a predictor of active and passive suicidal ideation among Iraq/Afghanistan war veterans. Psychiatry Research, 227(2–3), 360–362. 10.1016/j.psychres.2015.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, & Nock MK (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726–738. 10.1037/abn0000273 [DOI] [PubMed] [Google Scholar]
- Lamis DA, & Malone PS (2012). Alcohol use and suicidal behaviors among adults: a synthesis and theoretical model. Suicidology Online, 3, 4–23. [PMC free article] [PubMed] [Google Scholar]
- LeFevre ML, & Force USPT (2014). Screening for suicide risk in adolescents, adults, and older adults in primary care: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine, 160(10), 613–620. [DOI] [PubMed] [Google Scholar]
- Lipari R, Piscopo K, Kroutil LA, & Miller GK (2015). Suicidal thoughts and behavior among adults: results from the 2014 National Survey on Drug Use and Health. NSDUH Data Review. Substance Abuse and Mental Health Services Administration: Rockville, MD. [Google Scholar]
- Littlefield AK, Sher KJ, & Steinley D (2010). Developmental trajectories of impulsivity and their association with alcohol use and related outcomes during emerging and young adulthood I. Alcoholism, Clinical and Experimental Research, 34(8), 1409–1416. 10.1111/j.1530-0277.2010.01224.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Bettis AH, & Burke TA (2020). Characterizing the phenomenology of passive suicidal ideation: a systematic review and meta-analysis of its prevalence, psychiatric comorbidity, correlates, and comparisons with active suicidal ideation. Psychological Medicine, 50(3), 367–383. 10.1017/S003329171900391X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LA, Neighbors HW, & Griffith DM (2013). The experience of symptoms of depression in men vs women: analysis of the national comorbidity survey replication. JAMA Psychiatry, 70(10), 1100–1106. 10.1001/jamapsychiatry.2013.1985 [DOI] [PubMed] [Google Scholar]
- May AM, & Klonsky ED (2016). What distinguishes suicide attempters from suicide ideators? a meta-analysis of potential factors. Clinical Psychology: Science and Practice, 23(1), 5–20. 10.1111/cpsp.12136 [DOI] [Google Scholar]
- May CN, Overholser JC, Ridley J, & Raymond D (2015). Passive suicidal ideation: A clinically relevant risk factor for suicide in treatment-seeking veterans. Illness Crisis and Loss, 23(3), 261–277. 10.1177/1054137315585422 [DOI] [Google Scholar]
- Medley G, Lipari RN, Bose J, Rti,;, Cribb DS, Kroutil LA, & Mchenry G (2016). Sexual orientation and estimates of adult substance use and mental health: results from the 2015 National Survey on Drug Use and Health. Publication No. SMA 16–4984, NSDUH Series H-51). https://doi.org/(HHS Publication No. SMA 16–4984, NSDUH Series H-51
- Miller-Tutzauer C, Leonard KE, & Windle M (1991). Marriage and alcohol use: a longitudinal study of “maturing out”. Journal of Studies on Alcohol, 52(5), 434–440. 10.15288/jsa.1991.52.434 [DOI] [PubMed] [Google Scholar]
- Miller T, Chandler L, & Mouttapa M (2015). A needs assessment, development, and formative evaluation of a health promotion smartphone application for college students. American Journal of Health Education, 46(4), 207–215. 10.1080/19325037.2015.1044138 [DOI] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Bruffaerts R, Chiu WT, de Girolamo G, Gluzman S, de Graaf R, Gureje O, Haro JM, Huang Y, Karam E, Kessler RC, Lepine JP, Levinson D, Medina-Mora ME, … Williams D (2008). Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. The British Journal of Psychiatry: The Journal of Mental Science, 192(2), 98–105. 10.1192/bjp.bp.107.040113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, & Lee S (2008). Suicide and suicidal behavior. Epidemiologic Reviews, 30, 133–154. 10.1093/epirev/mxn002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Ramirez F, & Rankin O (2019). Advancing our understanding of the who, when, and why of suicide risk. JAMA Psychiatry, 76(1), 11–12. 10.1001/jamapsychiatry.2018.3164 [DOI] [PubMed] [Google Scholar]
- Nock M, & Kessler R (2006). Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. Journal of Abnormal Psychology, 115, 616–623. 10.1037/0021-843X.115.3.616 [DOI] [PubMed] [Google Scholar]
- Norström T, & Rossow I (2016). Alcohol consumption as a risk factor for suicidal behavior: A systematic review of associations at the individual and at the population level. Archives of Suicide Research, 20(4), 489–506. 10.1080/13811118.2016.1158678 [DOI] [PubMed] [Google Scholar]
- Olfson M, Blanco C, Wall M, Liu SM, Saha TD, Pickering RP, & Grant BF (2017). National trends in suicide attempts among adults in the United States. JAMA Psychiatry, 74(11), 1095–1103. 10.1001/jamapsychiatry.2017.2582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer PN, Brandfon S, Garcia E, Duffy S, Ganoczy D, Myra Kim H, & Valenstein M (2014). Predictors of suicidal ideation among depressed Veterans and the interpersonal theory of suicide. Journal of Affective Disorders, 152–154, 277–281. 10.1016/j.jad.2013.09.025 [DOI] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, & Mann JJ (2011). The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. The American Journal of Psychiatry, 168(12), 1266. 10.1176/appi.ajp.2011.10111704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosoff DB, Clarke T-K, Adams MJ, McIntosh AM, Davey Smith G, Jung J, & Lohoff FW (2019). Educational attainment impacts drinking behaviors and risk for alcohol dependence: results from a two-sample Mendelian randomization study with ~780,000 participants. Molecular Psychiatry. 10.1038/s41380-019-0535-9 [DOI] [PMC free article] [PubMed]
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, & Brewer RD (2015). 2010 national and state costs of excessive alcohol consumption. American Journal of Preventive Medicine, 49(5), e73–e79. 10.1016/j.amepre.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Salk RH, Hyde JS, & Abramson LY (2017). Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychological Bulletin, 143(8), 783–822. 10.1037/bul0000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley P, Bachman JG, Miech RA, & Patrick ME (2019). Monitoring the Future National Survey Results on Drug Use, 1975–2018 Volume II College Students and Adults Ages 19–60. Ann Arbor: Institute for Social Research, The University of Michigan [Google Scholar]
- Scott-Sheldon LAJ, Carey KB, Elliott JC, Garey L, & Carey MP (2014). Efficacy of alcohol interventions for first-year college students: a meta-analytic review of randomized controlled trials. Journal of Consulting and Clinical Psychology, 82(2), 177–188. 10.1037/a0035192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher L, Oquendo M. a, Richardson-vejlgaard R, Makhija NM, Posner K, Mann JJ, & Stanley BH (2009). Effect of acute alcohol use on the lethality of suicide attempts in patients with mood disorders. Journal of Psychiatry Resaerch, 43(10), 901–905. 10.1016/j.jpsychires.2009.01.005.Effect [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu AL, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, García FAR, Gillman M, Herzstein J, Kemper AR, Krist AH, Kurth AE, Owens DK, Phillips WR, Phipps MG, & Pignone MP (2016). Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA, 315(4), 380–387. 10.1001/jama.2015.18392 [DOI] [PubMed] [Google Scholar]
- Spokas M, Wenzel A, Brown GK, & Beck AT (2012). Characteristics of individuals who make impulsive suicide attempts. Journal of Affective Disorders, 136(3), 1121–1125. 10.1016/j.jad.2011.10.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone DM, Simon TR, Fowler KA, Kegler SR, Yuan K, Holland KM, Ivey-Stephenson AZ, & Crosby AE (2018). Vital signs: Trends in state suicide rates — United states, 1999–2016 and circumstances contributing to suicide — 27 states, 2015. Morbidity and Mortality Weekly Report, 67(22), 617–624. 10.15585/mmwr.mm6722a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health, HHS Publication No. PEP19–5068, NSDUH Series H-54. Rockville, MD. [Google Scholar]
- Twenge JM, Cooper AB, Joiner TE, Duffy ME, & Binau SG (2019). Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. Journal of Abnormal Psychology, 128(3), 185–199. 10.1037/abn0000410 [DOI] [PubMed] [Google Scholar]
- Vaeth PAC, Wang-Schweig M, & Caetano R (2017). Drinking, alcohol use disorder, and treatment access and utilization among U.S. racial/ethnic groups. Alcoholism, Clinical and Experimental Research, 41(1), 6–19. 10.1111/acer.13285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallone D, Greenberg M, Xiao H, Bennett M, Cantrell J, Rath J, & Hair E (2017). The effect of branding to promote healthy behavior: Reducing tobacco use among youth and young adults. International Journal of Environmental Research and Public Health, 14(12), 1–13. 10.3390/ijerph14121517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TEJ (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AM, Castle I-JP, Hingson RW, & Powell PA (2020). Using death certificates to explore changes in alcohol-related mortality in the United States, 1999 to 2017. Alcoholism, Clinical and Experimental Research, 44(1), 178–187. 10.1111/acer.14239 [DOI] [PubMed] [Google Scholar]
- Williams E, Mulia N, Karriker-Jaffe KJ, & Lui CK (2018). Changing racial/ethnic disparities in heavy drinking trajectories through young adulthood: a comparative cohort study. Alcoholism: Clinical and Experimental Research, 42(1), 135–143. 10.1111/acer.13541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsnack RW, Wilsnack SC, Gmel G, & Kantor LW (2018). Gender differences in binge drinking. Alcohol Research: Current Reviews, 39(1), 57–76. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


