Abstract
Objective/background:
Agitation is a common behaviour of Alzheimer’s Disease (AD). Although healing robots have previously been used for alleviating agitation for people with dementia in hospitals and other healthcare facilities, its effects remain unclear whether an information-support robot capable of disseminating information with user needs may have similar effects when it is applied in community dwellings. This study was to investigate the effects of information-support robots for reducing agitation in older people with AD residing alone in community-dwellings.
Methods
One participant with AD who lived alone in a community-dwelling was recruited. Participant’s frequencies, durations, and time courses of four patterns of agitation at home at baseline and during intervention were analysed. In this study, agitation was defined as: (a) restlessness going to the corridor (RLtoC), (b) restlessness going to the toilet (RLtoT), (c) restlessness going to the entrance (RLtoE), and (d) restlessness going to multiple places (RLtoMP). In the intervention phase, the information-support robot disseminated daily schedule or date information to the participant.
Results
RLtoC and RLtoMP were significantly reduced in frequency during the intervention. The durations of each episode of RLtoT and RLtoMP in the intervention were slightly reduced than those at the baseline. There were no differences in time courses of episodes of RLtoC and RLtoMP after the intervention.
Conclusion
This case study showed that information-support robot was useful to alleviate agitation of an older adult with AD living alone in a community-dwelling. Further study is warranted.
Keywords: Alzheimer’s disease, agitation, robot, living alone, assistive technology
Introduction
As society ages, the number of older people living alone is gradually increasing (Cabinet Office of Japan, 2018). In one community-based sample, 28% of people with dementia were found to be living alone (Nourhashemi et al., 2005). A previous study found that two thirds of older people with dementia in community-dwellings had psychiatric symptoms, such as psychosis, depression, and agitation (Chan et al., 2003). However, Lehmann et al. (2010) pointed out that knowledgeable informants and primary-care physicians, as well as patients themselves, were less likely to be aware of demented symptoms in patients who lived alone, as compared with those who live with other people.
Agitation is a neuropsychiatric symptom of Alzheimer’s Disease (AD), of which the prevalence is estimated to be 67.5% for sufferers in community-dwellings (Tractenberg et al., 2002). This leads to a lower quality of life in care-home residents with dementia (Livingston et al., 2017), increased admission rates to care facilities (Okura et al., 2011), and heightened monetary costs (Morris et al., 2015). According to the Agitation Definition Working Group formed by the International Psychogeriatric Association, agitation includes various behaviours, including rapid changes in mood, irritability, pacing, restlessness, yelling, speaking in an excessively loud voice, grabbing, and shoving (Cummings et al., 2015). While this symptom is known to be highly prevalent in hospitals or care facilities, an earlier study has suggested that it is also common among community-dwelling people with AD (Halpern et al., 2019).
Previous studies have reported the effects of non-pharmacological interventions for agitation. Music therapy reduced the agitation of people with AD, regardless of whether they had a music background (Brotons & Pickett-Cooper, 1996). Lighting intervention reduced the agitation-assessment score in people with AD and related dementias (Gfigueiro et al., 2014). Some studies have reported the effects of socially assistive robots upon agitation. Robotic cats indicated a trend toward decreasing agitated behaviour during intervention in a nursing home (Libin & Cohen-Mansfield, 2004). Therapy with a humanoid robot (NAO) resulted in improvements in the neuropsychiatric-inventory score, including agitation assessment, in a day-care center (Valentí Soler et al., 2015). Paro – a baby-seal robot – has been found to reduce agitation for people with major neurocognitive disorders in general hospitals (Demange et al., 2018). Moyle et al., (2017) showed that Paro was more effective for people with dementia in long-term-care facilities, as compared with the usual care in video data. Other studies have found improvements in the brief agitation-rating scale in the Paro group, as compared with the control group in the nursing home (Jøranson et al., 2015). Regarding information support devices for dementia, a previous study has reported that an IC recorder outputting the schedule reduced restless behaviours in the day-care center (Yasuda et al., 2006).
The above studies have reported some effects on improving agitation; however, the effects in home settings remain unclear. Moreover, as for overall studies of agitation, Livingston et al. (2014) have pointed out that future study was needed to clarify the effects on agitation in home settings, although the effects of non-pharmacological intervention upon agitation have been observed in hospitals or other facilities.
We have developed an information-support robot capable of distributing information needed by the user (Inoue et al., 2012). This robot has been developed to allow older people with cognitive disorders or dementia to live independently longer in community-dwellings, and allows families or caregivers to input information concerning the daily activities of older people via the cloud services, install it in the houses of older people living alone, and deliver the information at the time when it is needed. The robot system does not require users to complicated operations, and has been shown to attract the attention of older people with cognitive impairment at the rate of more than 90% (Nakayama et al., 2018). Occupational therapists have participated in the development of the information-support robot, and have evaluated the effects of the robot. The results showed that information-support incorporating to occupational therapy treatment enhanced the effects of the robot (Nishiura et al., 2014). Although the information-support robot may affect the performance of daily activities. it is not clear what impact it has upon the agitation of people with dementia. To our knowledge, there have been few reports about the effects of the information-support robot on people with agitation in home settings.
In the present study, we focused on restlessness in the agitated behaviours and explored it. Restlessness has been shown to be presented in 29–44% of older people with dementia (Schonfeld et al., 2007; Woods et al., 2009), and associated with a greater burden on caregivers of people with dementia (Regier & Gitlin, 2018). Dealing with restlessness is essential for promoting the independence of older people with dementia, since it is associated with decline in cognitive function and independence of daily activities (Zahodne et al., 2015).
This study aimed to clarify the effect of the information-support robot upon the restless behaviours of older people living alone with dementia in community-dwellings. We hypothesised that the robot would result in a decrease in the frequency and duration of restless behaviour, as well as a declining tendency in the time course of such episodes depending on the time at which the robot’s support was given.
Methods
We recruited a participant from one city in Japan with the following characteristics: (a) having restless behaviours, (b) living alone, (c) able to listen, comprehend and follow the robot’s information and (d) consent to participate in the study. Exclusion criteria were: (a) having severe auditory impairment except those using hearing aids, and (b) having a risk that the robot might promote further restless behaviours. We explained the experiment to the participant and her family in written form, and observed an interaction between the participant and the robot prior to the experiment. The participant signed a consent form upon expressing the intention to participate. This study was approved by the ethics committee of the National Rehabilitation Center for Persons with Disabilities.
Case information
The participant was a 70-year-old woman who lived alone in a community-dwelling and was diagnosed with AD two years prior to the start of the study. In addition to AD, she had also been diagnosed as suffering from high blood pressure and took two medications – Aricept and Amlodipine – daily. According to the criteria for determining the daily-life-independence level (bedridden level) of the older people with disabilities (Ministry of Health Labor and Welfare of Japan, 2012), she had been rated A1, meaning that she could go outside with care and was out of bed for most of the day. In fact, she was not physically impaired and could move autonomously, but did not have the opportunity to go out without assistance. Although daily-living activities were at autonomous levels, she was unable to cook with fire. Thus, her daughter, who was her primary care giver, had helped to prepare meals. The participant’s cognitive function was assessed by the Mini-Mental State Examination – Japanese (MMSE-J) and the Japanese version of the Neurobehavioral Cognitive Status Examination (COGNISTAT) before and after the experiment. According to the results, she was rated as having dementia on the MMSE-J (a predictive validity classifying less than 24 scores into dementia has been identified (Sugishita & Hemmi, 2010)). Her COGNISTAT results showed cognitive impairments involving time orientation, attention, naming, constructional ability, memory, calculation, similarities, and judgment (scores below 9 are recognised as impaired (Matsuda et al., 2001)) before the intervention phase (Table 1). She used a public day service and helper service for four days and one day a week, respectively.
Table 1.
The cognitive function of a participant before and after the intervention.
| Before intervention | After intervention | |
|---|---|---|
| MMSE-J COGNISTAT | 14 | 18 |
| Orientation | 2 | 2 |
| Attention | 6 | 6 |
| Comprehension | 10 | 10 |
| Repetition | 11 | 11 |
| Naming | 5 | 7 |
| Constructional | 5 | 7 |
| Memory | 6 | 5 |
| Calculation | 4 | 4 |
| Similarities | 6 | 8 |
| Judgment | 8 | 7 |
An OT interviewed the participant, her daughter and her day-service staff in advance. According to this interview, we learned that the participant had missed meals and forgotten day services due to her time-orientation impairment, and previously had a heat stroke due to dehydration. However, the participant had not had any anxiety behaviour in activities of daily living, and had not had any sleep problem or moving around at night, had never developed delirium. Both her daughter and the day-service staff said that the participant was a bit rigid and inflexible in following daily routine. Her daughter also expressed a wish that the participant could live alone as independently as possible. The day-service staff noted that the participant frequently forgot the days upon which she was scheduled to receive service, such that she was sleeping or unprepared when the staff arrived in the morning, and often behaved in a restless or fidgeting manner during the service itself. Additionally, the day-service staff noted that the participant was very resistance to change her mind in daily life, and that she was quite restless both during the day service and returning home.
Assessment and intervention device
The MMSE-J and the COGNISTAT tests were administered twice by an OT at the end of baseline and intervention phases to assess cognitive function.
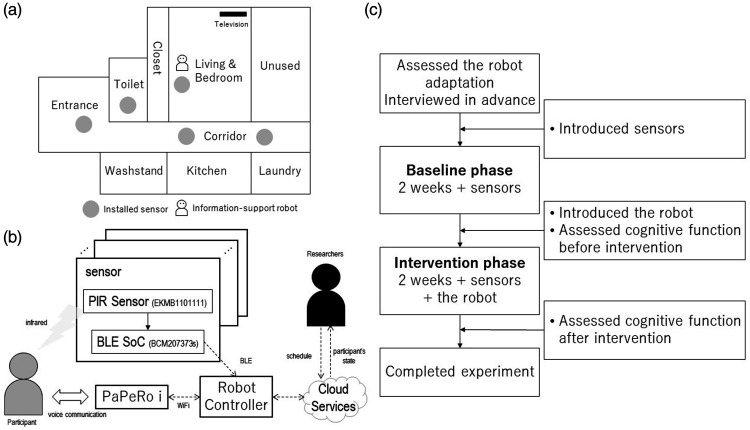
We adopted the motion sensor to detect transfers from room to room. The sensor is composed of BLE SoC (BCM207373s, Broadcom) and PIR motion sensor (EKMB1101111, Panasonic) that have been widely used in studies in smart home applications (Stucki et al., 2014). The sensors were 50.4-mm wide, 70.0-mm tall, and 38.0-mm thick and were operated by tablet via a Bluetooth function. They switched from off to on upon detecting a heat source. If no heat source is detected for 10 s, the sensors switch off. In the present study, five sensors were installed in the participant’s house: in living room, toilet, and entrance, as well as the corridor in front of kitchen and the corridor in front of washing machine (Figure 1(a)). Each sensor was mounted on the wall or ceiling, such that the participant would pay as little attention to it as possible.
Figure 1.
(a) The floor plan indicating the installed sensors and the information-support robot. (b) The system diagram including data collection and the flow that the robot distributed the information. (c) The research protocol.
We used PaPeRo i, which was manufactured by NEC, as a platform. It is equipped with voice synthesis, an intention-recognition module, and an interaction system consisting of a light indicator and a head motion. It can distribute necessary information for the case via the cloud and customise the information schedule by specifying the time and day of the week. Furthermore, it can record the participant’s response while the robot is distributing information. Figure 1(b) shows a system diagram that used in this study.
Experimental procedure
Before we introduced the information-support robot to the participant’s house, motion sensors were installed in each room for two weeks to measure the baseline-activity data, including the number of transfers and the time spent in rooms without the information-support robot. After completion of the baseline phase, the information-support robot was introduced to the living room and bedroom for two weeks. During the intervention phase, activity data were also measured by the motion sensors. The OT evaluated the participant’s cognitive function before and after the intervention. Figure 1(c) shows the research protocol.
Development of the information support contents
The information-support robot distributed necessary information that was determined in advance before the intervention in order to establish comfortable daily routine for the participant. First, an OT drafted the content of the information in line with the participant’s needs, her cognitive and interview performance. The OT adopted an information support approach that reliably deliver information to older people when drafting (Inoue et al., 2012). Next, another OT, one cultural anthropologist, and two engineers reviewed the draft, repeatedly revised and developed a provisional version. Finally, we asked the participant, her family and day-service staffs to confirm the provisional version and adopted the contents with their consent for the final version and the time of delivering the robotic intervention. Table 2 shows the distributing schedule and the information content.
Table 2.
The information distributing schedule and the contents.
| Distributing time | Contents |
|---|---|
| 7:00 | Good morning |
| 7:30 | Breakfast time notice |
| 8:00 | Encouraging hydration |
| 8:45 | Date information and Prepare the day service |
| 12:00 | Lunch time notice |
| 14:00 | Encouraging hydration |
| 16:00 | Encouraging hydration |
| 18:00 | Dinner time notice and Encouraging tooth brushing |
| 20:00 | Encouraging hydration |
| 21:00 | Good night |
Definition of restless behaviours
We defined restless behaviours as following four patterns: (a) The first was restlessness going to the corridor (RLtoC), which is sequential transfer from the living room to the corridor and back. (b) The second was restlessness going to the toilet (RLtoT), which was sequential transfer from the living room to the corridor to the toilet and back again. (c) The third was restlessness going to the entrance (RLtoE), which was sequential transfer from living room to the corridor to the entrance and back again. (d) The fourth was restlessness going to multiple places (RLtoMP), which was sequential transfer that did not fit the other three patterns, e.g. movement from the living room to the corridor, the entrance, the toilet, the corridor, and back to the living room.
Statistical analysis
We used a paired t-test to compare the number of episodes of restlessness between the baseline and intervention phases, and performed analysis using the IBM SPSS statistics 25 software.
Result
Robotic intervention was successfully implemented without problems over the course of the intervention phase. We confirmed that the participant mostly responded to the robot during the intervention phase by means of recorded utterances.
MMSE-J and COGNISTAT showed changed scores for cognitive function before and after the intervention (Table 1). Regarding MMSE-J, the total score increased on four points after intervention. The COGNISTAT showed improvements in the Naming, Constructional ability, and Similarities subcomponents after intervention. However, these subcomponents remained at an impaired level.
Frequency of restlessness
Table 3 shows the average number of four restless episodes per day. It can be seen that the number of RLtoC episodes in the intervention phase was significantly lower than that in the baseline phase (t[12] = 2.25, r = .55, p = .044). Although the number of RLtoT episodes did not significantly differ between the baseline and intervention phases, there was a substantial decrease in their frequency in the intervention phase (t[12] = 2.14, r = .53, p = .054). The number of RLtoMP episodes significantly decreased during the intervention phase (t[12] = 2.96, r = .65, p = .012); on the other hand, the number of RLtoE episodes increased in the intervention phase (t[12] = −0.47, r = .14, p = .644).
Table 3.
The number of the four types of restless episodes and the duration.
| Baseline phase | Intervention phase | Effect size | p-values | |
|---|---|---|---|---|
| mean (SD) | mean (SD) | |||
| RL to C | ||||
| Frequency | 43.9 (17.2) | 32.6 (10.5) | .55 | .044 |
| Duration in second | 62.1 (64.5) | 73.8 (79.5) | ||
| RL to T | ||||
| Frequency | 13.5 (6.3) | 8.5 (4.9) | .53 | .054 |
| Duration in second | 306.5 (141.8) | 256.2 (95.8) | ||
| RL to E | ||||
| Frequency | 5.7 (3.3) | 6.2 (2.0) | .14 | .644 |
| Duration in second | 153.1 (100.0) | 198.0 (137.2) | ||
| RL to MP | ||||
| Frequency | 5.9 (2.9) | 3.2 (1.7) | .65 | .012 |
| Duration in second | 423.6 (222.4) | 420.5 (194.3) |
RL to C: restlessness going to the corridor; RL to T: restlessness going to the toilet; RL to E: restlessness going to the entrance; RL to MP: restlessness going to the multiple place.
Duration of restlessness
Table 3 shows the average duration of one restless action in the baseline and intervention phases. The durations of RLtoC episodes were mostly shorter than those of episodes of the other three types restlessness. The mean duration of RLtoC episodes increased in the intervention phase, as compared with the baseline phase (mean duration Bp: 62.1 ± 64.5 s/times, Ip: 73.8 ± 79.5 s/times). Regarding RLtoE episodes, the mean duration and standard deviation in the intervention phase also increased compared to their baseline values (mean duration Bp: 153.1 ± 100.0 s/times, Ip: 198.0 ± 137.2 s/times). By contrast, the mean duration of RLtoT episodes in the intervention phase was shorter than that in the baseline phase. Additionally, the deviation of duration in the intervention phase was narrower than that in the baseline phase (mean duration Bp: 306.5 ± 141.8 s/times, Ip: 256.2 ± 95.8 s/times). A similar deviation tendency was observed for RLtoMP episodes (Mean duration Bp: 423.6 ± 222.4 s/times, Ip: 420.5 ± 194.3 s/times).
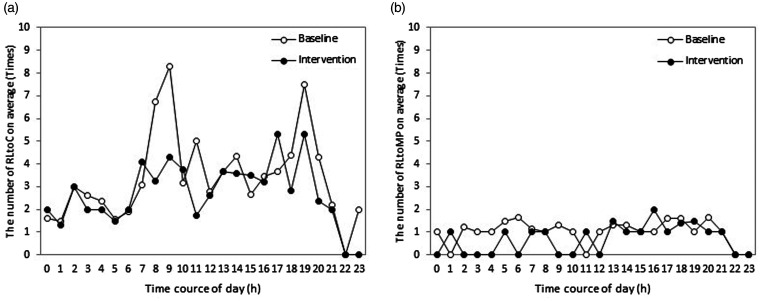
Time course of restless behaviours
We plotted RLtoC and RLtoMP episodes over the time course, which significantly decreased in frequency, to identify the effects of the time at which the robot distributed the information. There is no unambiguous evidence that the time of information distribution affected these time courses. As shown in Figure 2, the number of RLtoC episodes prominently decreased between 8:00 a.m. and 9:00 a.m., and that of RLtoMP episodes indicated a slight decrease from 2:00 a.m. to 6:00 a.m. and from 9:00 a.m. to 10:00 a.m.
Figure 2.
This shows the two restless episodes over the time course of a day. (a) RL to C: restlessness going to the corridor, and (b) RL to MP: restlessness going to the multiple place.
Discussion
We have conducted an intervention study to explore the effects of an information-support robot upon the restless behaviours of an older person with AD in a community-dwelling. Our findings showed that the robot’s intervention might significantly alleviate restless behaviours in the home and reduce the duration of restless actions.
Impact of the information support robot upon the cognitive function
MMSE-J and three subscores of COGNISTAT showed an increase after the robot intervention. These findings suggested that the information-support robot changed the participant’s communication environment. Previous study has reported that a human-type communication robot improved the cognitive performance of older people living alone (Tanaka et al., 2012). An appropriate opportunity for communication has been reported to be useful to maintain cognitive function in community-dwelling older people (Kimura et al., 2019). Therefore, the information-support robot might be able to improve the MMSE-J and COGNISTAT scores due to the new opportunities for communication with the participant living alone.
Impact of the information-support robot upon the frequency of restlessness
In the present study, the frequency of RLtoC and RLtoMP episodes significantly decreased compared with the baseline. Previous studies have demonstrated that socially assistive robots influence the motor behaviour of older people with dementia; specifically, the intervention of Paro was shown to reduce the step count of older people with dementia during daytime (Moyle et al., 2018). Another study showed that Paro had an impact upon the agitated behaviour of people with dementia (Jøranson et al., 2015). These previous studies suggest that Paro can provide comfort to people with dementia. In terms of reducing the frequency of restless action, the present findings were consistent with those of previous studies.
It is notable that the robot used in this study distributed information needed by the participant. Furthermore, the OT established this information in line with the case’s cognitive impairment, especially in terms of time orientation and memory. Assistive technologies generally support people with dementia by focusing upon their real needs. A previous study developed COGKNOW, a cognitive device combined with smart-home technology, to help people with mild dementia (Meiland et al., 2007). Other studies have developed AP@LT, an application to compensate the memory problems of people with AD (Imbeault et al., 2014). Although these technologies have shown their effectiveness for planned activities such as medication taking, little is known about whether they affect unplanned daily activity around the home. From the findings in this study, we infer that information supports in line with the participant’s needs and the characteristics of cognitive function can impact on reducing the restlessness in the house.
Increase of MMSE-J and COGNISTAT scores might indicate that the information supports impacted on reducing the participant’s restlessness. One study has reported that older people with anxiety tented to decline the cognitive function and anxiety could be attributed to cognitive decline (Kassem et al., 2017). In this study, the information supports were in line with the participant’s needs, and might contribute to the improvement of cognitive function, leading to the reduction of restlessness.
Impact of the information-support robot upon the duration and time course of restlessness
Although most facets of restlessness decreased in frequency during the intervention phase, the mean duration of RL to C episodes showed an increase compared with the baseline phase. This means that the time spent in the corridor increased, even though the frequency decreased. This might indicate that the purposeful activities increased at the kitchen and the laundry area of the participant’s house. Additionally, the standard deviations of RL to T and RL to MP were narrower during the intervention phase than during the baseline. These results supplement the idea that the information-support robot may reduce restlessness not only quantitatively but qualitatively.
Moreover, the number of RL to C episodes prominently decreased from 8:00 a.m. to 9:00 a.m., and that of RL to MP episodes decreased from 2:00 a.m. to 6:00 a.m. There is a possibility that the participant might calm down in the certain time course with the information-supports due to some needs being met. Restlessness is associated with an increased neurological need arising from an inability to integrate various stimuli (Woods et al., 2009). Therefore, the present results suggest that either the information-support robot or the information itself met the participant’s needs, as a result, the participant calmed down from 8:00 a.m. to 9:00 a.m. Decline in RLtoMP episodes might indicate that sleep fragmentation decreased, since the participant is generally likely to be asleep from 2:00 a.m. to 6:00 a.m. Approximately 65% of people with AD have sleep disturbances attributable to change in circadian rhythms (Wennberg et al., 2017). The participant had not had any sleep problems but given that one or more RLtoMP episodes on average were recognised from 2:00 a.m. to 6:00 a.m. in the baseline phase, the results suggest that the intervention of the information-support robot might influence sleep conditions.
The time at which these results were represented may be significant. Agitated behaviours, such a pacing, were more disruptive in the morning than in the afternoon (Cohen-Mansfield, 2008). In general, people with dementia exhibit more time-orientation disruption in the morning than in the afternoon (Iwamoto & Hoshiyama, 2012). Therefore, an intervention by using the information-support robot might provide a solution for people with these symptoms, their families and caregivers.
Limitations
All the present results were obtained from a single case, making them difficult to generalise. Thus, we need to conduct a large-sample study to investigate the effects of the information-support robot. It is necessary to further investigate the quality of restless behaviours, since the behaviours defined in the present study may include daily-living activities. In particular, it is difficult to determine if the decrease in restless behaviour was positive. It should be noted that the present study focused on the restlessness. Agitation includes not only restlessness but various behaviours, and so we cannot infer that the information-support robot is effective for all agitation. In addition, assessments directly reflecting participant’s levels of independence should be required to clarify effects of the information-support robot on promoting the independence of older people living alone. In particular, sleep condition is necessary assessment for levels of the independence of older people with dementia, since it was associated with the independence and agitation in people with AD (De Oliveira et al., 2014). From the present study, it is, however, difficult to discuss effects of the information-support robot on the sleep conditions. Regarding an increase of the cognitive assessment scores, the present study cannot rule out the possibility of leaning effect due to the short-term intervention. The effects of the information support robot on cognitive function remains to be determined in future studies.
Future development
In future, a randomised control study to generalise the findings of this study and a long-term intervention study should be conducted to investigate the long-term effects of the information-support robot.
This study investigated the possibility of using information-support robot might contribute to promoting the independence of older people living alone with dementia, since previous study has shown that agitated behaviours are associated with decline in the independence of AD (Zahodne et al., 2015). In this study, occupational therapists were responsible for developing the information-support contents distributed by the robot, the results of this case study would be significant to the occupational therapy in robot application.
Conclusion
We conducted a case study to clarify the effects of an information-support robot upon the restlessness of an older person living alone with AD in a community-dwelling. The information-support robot was found to alleviate restlessness in the house and reduce the duration of restless actions. These findings suggested that the information support robot can promote the independence of older people living alone with dementia. However, it is necessary to conduct a further large-sample study to investigate the effects of the information-support robot upon people with dementia.
Acknowledgements
We deeply are grateful to the staffs in Izu city hall staffs and to the members involved in this project.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by JST ‘Strategic Promotion of Innovation Research and Development’ Grant Number JPMJSV1011, Japan, and JSPS KAKENHI Grant Number JP19KT0004.
ORCID iD: Jumpei Mizuno https://orcid.org/0000-0002-4662-0526
References
- Brotons M., Pickett-Cooper P. K. (1996). The effects of music therapy intervention on agitation behaviors of Alzheimer’s disease patients. Journal of Music Therapy, 33, 2–18. 10.1093/jmt/33.1.2 [DOI] [Google Scholar]
- Cabinet Office of Japan (2018). Annual report on the ageing society: 2018. https://www8.cao.go.jp/kourei/english/annualreport/2018/pdf/c1-1.pdf
- Chan D. C., Kasper J. D., Black B. S., Rabins P. V. (2003). Prevalence and correlates of behavioral and psychiatric symptoms in community-dwelling elders with dementia or mild cognitive impairment: The memory and medical care study. Journal of Geriatric Psychiatry, 18, 174--182. 10.1002/gps.781 [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J. (2008). Agitated behavior in persons with dementia: The relationship between type of behavior, its frequency, and its disruptiveness. Journal of Psychiatric Research, 43, 64–69. 10.1016/j.jpsychires.2008.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings J., Mintzer J., Brodaty H., Sano M., Banerjee S., Devanand D. P., Gauthier S., Howard R, Lanctôt K., Lyketsos C. G., Peskind E., Porsteinsson A. P., Reich E., Sampaio C., Steffens D., Wortmann M., Zhong K.; International Psychogeriatric Association (2015). Agitation in cognitive disorders: International Psychogeriatric Association provisional consensus clinical and research definition. International Psychogeriatrics, 27, 7–17. 10.1017/S1041610214001963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Oliveira F. F., Bertolucci P. H. F., Chen E. S., De A., Cardoso Smith M. (2014). Assessment of sleep satisfaction in patients with dementia due to Alzheimer’s disease. Journal of Clinical Neuroscience, 21, 2112–2117. 10.1016/j.jocn.2014.05.041 [DOI] [PubMed] [Google Scholar]
- Demange M., Lenoir H., Pino M., Cantegreil-Kallen I., Rigaud A. S., Cristancho-Lacroix V. (2018). Improving well-being in patients with major neurodegenerative disorders: Differential efficacy of brief social robot-based intervention for 3 neuropsychiatric profiles. Clinical Interventions in Aging, 13, 1303–1311. 10.2147/CIA.S152561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gfigueiro M. G., Plitnick B. A., Lok A., Ejones G. E., Higgins P., Rhornick T. R., Srea M. S. (2014). Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clinical Interventions in Aging, 9, 1527–1537. 10.2147/CIA.S68557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern R., Seare J., Tong J., Hartry A., Olaoye A., Aigbogun M. S. (2019). Using electronic health records to estimate the prevalence of agitation in Alzheimer disease/dementia. International Journal of Geriatric Psychiatry, 34, 420–431. 10.1002/gps.5030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbeault H., Bier N., Pigot H., Gagnon L., Marcotte N., Fulop T., Giroux S. (2014). Electronic organiser and Alzheimer’s disease: Fact or fiction? Neuropsychological Rehabilitation, 24, 71–100. 10.1080/09602011.2013.858641 [DOI] [PubMed] [Google Scholar]
- Inoue T., Nihei M., Narita T., Onoda M., Ishiwata R., Mamiya I., Shino, M., Kojima, H., Ohnaka, S., Fujita, Y., & Kamata M. (2012). Field-based development of an information support robot for persons with dementia. Technology and Disability, 24, 263–271. 10.3233/TAD-120357 [DOI] [Google Scholar]
- Iwamoto Y., Hoshiyama M. (2012). Time orientation during the day in the elderly with dementia. Physical & Occupational Therapy in Geriatrics, 30, 202–213. 10.3109/02703181.2012.713453 [DOI] [Google Scholar]
- Jøranson N., Pedersen I., Rokstad A. M. M., Ihlebæk C. (2015). Effects on symptoms of agitation and depression in persons with dementia participating in robot-assisted activity: A cluster-randomized controlled trial. Journal of the American Medical Directors Association, 16, 867–873. 10.1016/j.jamda.2015.05.002 [DOI] [PubMed] [Google Scholar]
- Kassem A. M., Ganguli M., Yaffe K., Hanlon J. T., Lopez O. L., Wilson J. W., Cauley J. A.; Osteoporotic Fractures in Men (MrOS) Study Research Group (2017). Anxiety symptoms and risk of cognitive decline in older community-dwelling men. International Psychogeriatrics, 29, 1137–1145. 10.1017/S104161021700045X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura N., Aso Y., Yabuuchi K., Ishibashi M., Hori D., Sasaki Y., Nakamichi A., Uesugi S., Fujioka H., Iwao S., Jikumaru M., Katayama T., Sumi K., Eguchi A., Nonaka S., Kakumu M, Matsubara E. (2019). Modifiable lifestyle factors and cognitive function in older people: A cross-sectional observational study. Frontiers in Neurology, 10, 401–412. 10.3389/fneur.2019.00401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann S. W., Black B. S., Shore A., Kasper J., Rabins P. V. (2010). Living alone with dementia: Lack of awareness adds to functional and cognitive vulnerabilities. International Psychogeriatrics, 22, 778–784. 10.1017/S1041610209991529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libin A., Cohen-Mansfield J. (2004). Therapeutic robocat for nursing home residents with dementia: Preliminary inquiry. American Journal of Alzheimer’s Disease and Other Dementias, 19, 111–116. 10.1177/153331750401900209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston G., Barber J., Marston L., Rapaport P., Livingston D., Cousins S., Robertson S., La Frenais F., Cooper C. (2017). Prevalence of and associations with agitation in residents with dementia living in care homes: MARQUE cross-sectional study. BJPsych Open, 3, 171–178. 10.1192/bjpo.bp.117.005181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston G., Kelly L., Lewis-Holmes E., Baio G., Morris S., Patel N., Omar R. Z., Katona C., Cooper C. (2014). A systematic review of the clinical effectiveness and cost-effectiveness of sensory, psychological and behavioural interventions for managing agitation in older adults with dementia. Health Technology Assessment (Winchester, England), 18, 1. 10.3310/hta18390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuda O., Saito M., Kurokawa Y., Miyamoto N., Maruyama K., Matsuda H., Nakatani M. (2001). A study of the reliability and validity of the Japanese version of the neurobehavioral cognitive status examination (NCSE). Japanese Journal of Geriatric Psychiatry, 12, 1177–1187. [Google Scholar]
- Meiland F. J., Reinersmann A., Bergvall-Kareborn B., Craig D., Moelaert F., Mulvenna M. D., Nugent C., Scully T., Bengtsson J. E., Dröes R. M. (2007). COGKNOW: Development of an ICT device to support people with dementia. Journal on Information Technology in Healthcare, 5, 324–334. [PubMed] [Google Scholar]
- Ministry of Health Labour and Welfare of Japan (2012). Overview of survey results of long term care facility and establishment. Ministry of Health Labour and Welfare (in Japanese). https://www.mhlw.go.jp/toukei/saikin/hw/kaigo/service10/dl/gaikyo.pdf
- Morris S., Patel N., Baio G., Kelly L., Lewis-Holmes E., Omar R. Z., Katona C., Cooper C., Livingston G. (2015). Monetary costs of agitation in older adults with Alzheimer’s disease in the UK: Prospective cohort study. BMJ Open, 5, e007382– e00738-7. 10.1136/bmjopen-2014-007382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyle W., Jones C. J., Murfield J. E., Thalib L., Beattie E. R. A., Shum D. K. H., O’Dwyer S. T., Mervin M. C., Draper B. M. (2017). Use of a robotic seal as a therapeutic tool to improve dementia symptoms: A cluster-randomized controlled trial. Journal of the American Medical Directors Association, 18, 766–773. 10.1016/j.jamda.2017.03.018 [DOI] [PubMed] [Google Scholar]
- Moyle W., Jones C. J., Murfield J. E., Thalib L., Beattie E. R. A., Shum D. K. H., O’Dwyer S., Mervin M. C., Draper B. M. (2018). Effect of a robotic seal on the motor activity and sleep patterns of older people with dementia, as measured by wearable technology: A cluster-randomised controlled trial. Maturitas, 110, 10–17. 10.1016/j.maturitas.2018.01.007 [DOI] [PubMed] [Google Scholar]
- Nakayama Y., Saito D., Nishiura Y., Mizuno J., Ohnaka S., Watabe K., Sadohara K., Hamada H., Nihei M., Ohta Y., Inoue T. (2018). Information acquisition from a communication robot in older persons with cognitive impairments [Paper presentation]. 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society Program, Honolulu, HI, United States. https://embs.papercept.net/conferences/conferences/EMBC18/program/EMBC18_ContentListWeb_2.html
- Nishiura Y., Inoue T., Nihei M. (2014). Appropriate talking pattern of an information support robot for people living with dementia: A case study. Journal of Assistive Technologies, 8, 177–187. 10.1108/JAT-12-2013-0035 [DOI] [Google Scholar]
- Nourhashemi F., Amouyal-Barkate K., Gillette-Guyonnet S., Cantet C., Vellas B.; REAL.FR Group (2005). Living alone with Alzheimer’s disease: Cross-sectional and longitudinal analysis in the REAL.FR study. The Journal of Nutrition, Health & Aging, 9, 117–120. [PubMed] [Google Scholar]
- Okura T., Plassman B. L., Steffens D. C., Llewellyn D. J., Potter G. G., Langa K. M. (2011). Neuropsychiatric symptoms and the risk of institutionalization and death: The aging, demographics, and memory study. Journal of the American Geriatrics Society, 59, 473–481. 10.1111/j.1532-5415.2011.03314.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regier N. G., Gitlin L. N. (2018). Dementia-related restlessness: Relationship to characteristics of persons with dementia and family caregivers. International Journal of Geriatric Psychiatry, 33, 185–192. 10.1002/gps.4705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonfeld L., King-Kallimanis B., Brown L. M., Davis D. M., Kearns W. D., Molinari V. A., Werner D. H., Beattie E. R., Nelson A. L. (2007). Wanderers with cognitive impairment in department of veterans affairs nursing home care units. Journal of the American Geriatrics Society, 55, 692–699. 10.1111/j.1532-5415.2007.01135.x [DOI] [PubMed] [Google Scholar]
- Stucki R. A., Urwyler P., Rampa L., Müri R., Mosimann U. P., Nef T. (2014). A web-based non-intrusive ambient system to measure and classify activities of daily living. Journal of Medical Internet Research, 16, e175. 10.2196/jmir.3465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugishita M., Hemmi I. (2010). Validity and reliability of the min mental state examination-Japanese (MMSE-J): A preliminary report. Japanese Journal of Cognitive Neuroscience, 12, 186–190. 10.11253/ninchishinkeikagaku.12.186 [DOI] [Google Scholar]
- Tanaka M., Ishii A., Yamano E., Ogikubo H., Okazaki M., Kamimura K., Konishi Y., Emoto S., Watanabe Y. (2012). Effect of a human-type communication robot on cognitive function in elderly women living alone. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 18, CR550–CR557. 10.12659/MSM.883350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tractenberg R. E., Weiner M. F., Thal L. J. (2002). Estimating the prevalence of agitation in community-dwelling persons with Alzheimer’s disease. The Journal of Neuropsychiatry and Clinical Neurosciences, 14, 11–18. 10.1176/jnp.14.1.11 [DOI] [PubMed] [Google Scholar]
- Valentí Soler M., Agüera-Ortiz L., Olazarán Rodríguez J., Mendoza Rebolledo C., Pérez Muñoz A., Rodríguez Pérez I., Ruiz E. O., Sánchez A. B., Cano V. H., Chillón L. C., Ruiz S. F., Alvarez J. L., Salas B. L., Plaza J. M. C., Rico F. M., Dago G. A., Martín P. M. (2015). Social robots in advanced dementia. Frontiers in Aging Neuroscience, 7, 133. 10.3389/fnagi.2015.00133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg A., Wu M., Rosenberg P., Spira A. (2017). Sleep disturbance, cognitive decline, and dementia: A review. Seminars in Neurology, 37, 395–406. 10.1055/s-0037-1604351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods D. L., Beck C., Sinha K. (2009). The effect of therapeutic touch on behavioral symptoms and cortisol in persons with dementia. Forschende Komplementärmedizin/Research in Complementary Medicine, 16, 181–189. 10.1159/000220479 [DOI] [PubMed] [Google Scholar]
- Yasuda K., Beckman B., Yoneda M., Yoneda H., Iwamoto A., Nakamura T. (2006). Successful guidance by automatic output of music and verbal messages for daily behavioural disturbances of three individuals with dementia. Neuropsychological Rehabilitation, 16, 66–82. 10.1080/09602010443000191 [DOI] [PubMed] [Google Scholar]
- Zahodne L. B., Ornstein K., Cosentino S., Devanand D. P., Stern Y. (2015). Longitudinal relationships between Alzheimer disease progression and psychosis, depressed mood, and agitation/aggression. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 23, 130–140. 10.1016/j.jagp.2013.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]