Abstract
Introduction.
Adolescent depression is a significant mental health concern. Emotion regulation difficulties have been associated with subsequent depressive symptoms, though different facets of emotion regulation are rarely compared. This study examined the degree to which trajectories of change in different facets of emotion regulation (goal-directed behavior, impulse control, and regulation strategies) and depressive symptoms were associated across twelve months in a clinical adolescent sample.
Methods.
Participants included 110 adolescents from the US who were enrolled in a randomized trial that tested a cognitive-behavioral treatment for youth with co-occurring mental health and substance use concerns (Mage = 15.71 years; 57.3% male). Assessments were conducted at baseline, 3-, 6-, and 12-month follow-ups. Three separate bivariate latent basis growth curve analyses were conducted. Correlations between latent intercepts and latent slopes, as well as overall model fit, were examined.
Results.
Impulse control and goal-directed behavior were each associated with depressive symptoms at baseline. Additionally, change in impulse control over time was significantly associated with change in depressive symptoms. However, the same was not true for goal-directed behavior. Overall fit indices for models of emotion regulation strategies were below acceptable levels and thus could not be interpreted.
Conclusions.
Findings from the present study indicate that adolescents’ depressive symptoms appear to improve as their perceived ability to control impulses improves. These results suggest that addressing impulse control difficulties may be an important step in treating adolescent depression and co-occurring disorders.
Keywords: adolescence, depression, emotion regulation, impulse control
Depression is a serious mental health concern that impacts approximately 13% of adolescents aged 12–17 in the United States (National Institute of Mental Health, 2019). Depression often emerges in adolescence and negatively impacts a variety of domains, including academic performance, relationships with family and friends, and physical health (Thapar et al., 2012). Chronic depression, if untreated, can lead to the development of more severe psychological concerns, such as suicidal thoughts and behaviors and substance use (Gladstone & Beardslee, 2009; King et al., 2004). Numerous factors have been implicated in the onset and maintenance of depressive symptoms such as a genetic predisposition, pubertal and cognitive changes across adolescent development, early life adversity, trauma, chronic interpersonal conflict, and difficulties with emotion regulation (Thapar et al., 2012). Emotion regulation is particularly important in understanding adolescent depression. Indeed, chronic difficulties with adaptive emotion regulation in late childhood and early adolescence are associated with subsequent development of psychopathology, including depression (Clear et al., 2020; Feng et al., 2009; Folk et al., 2014; Silk et al., 2003; Turpyn et al., 2015). In contrast, adaptive emotion regulation is associated with resilience and is a protective factor against the development of depression (Cracco et al., 2017; Compas et al., 2017; Thapar et al., 2012). The present study examined the relation between trajectories of change in adolescent emotion regulation and depressive symptoms.
Emotion regulation is defined as a set of processes that contribute to the ability to use emotion regulation strategies and accomplish a goal, and include recognition, understanding, and acceptance of emotions as well as controlling impulses (Gross, 1998). In this respect, emotion regulation is considered multifaceted (Gratz & Roemer, 2004; Weinberg & Klonsky, 2009). With regard to use of emotion regulation strategies specifically, the use of both adaptive (i.e., effective) and maladaptive (i.e., ineffective) emotion regulation strategies increases from adolescence into adulthood. This change generally coincides with the development of more advanced cognitive abilities (Garnefski & Kraaij, 2006) though the process in not linear. Specifically, use of adaptive strategies declines from childhood into adolescence and increases again toward late adolescence into adulthood, while use of maladaptive strategies increases from childhood into adolescence and decreases again toward late adolescence into adulthood (Cracco et al., 2017). The relative lag in the use of adaptive coping strategies during early to middle adolescence is particularly problematic given that biological changes during this developmental period result in heightened frequency and intensity of negative emotions but cognitive capacity is not yet developed well enough to effectively regulate such feelings. This mismatch between strong emotion and emotion regulation strategy use (high maladaptive and low adaptive) may, in part, account for the emergence and maintenance of adolescent depressive symptoms (Cracco et al., 2017).
Examination of Depression and Emotion Regulation
Studies examining emotion regulation as a single construct have consistently demonstrated a positive association between emotion regulation difficulties and depressive symptoms. For example, a cross-sectional study of mother-adolescent relationships examined adolescent emotion regulation difficulties both via an observed family interaction task and self-report. Greater observed and self-reported emotion regulation difficulties were associated with greater adolescent depressive symptom severity (Yap et al., 2010). Similarly, greater emotion regulation difficulties have been shown to predict increases in adolescent depressive symptoms in longitudinal studies that span months (McLaughlin et al., 2009) to years (Masters et al., 2019).
Emotion regulation has also been studied as a multifaceted construct. According to Gratz and Roemer (2004), emotion regulation can be broken into six facets – emotional awareness, emotional clarity, acceptance of the emotional response, goal-directed behavior, impulse control, and access to adaptive emotion regulation strategies. The first three facets center on recognizing, understanding, and accepting the emotion and its generation process. The latter three center on altering the emotion or resulting behavior (Gratz & Roemer, 2004). Though related to one another, each of these facets plays a unique role in the overall process of emotion regulation (Gratz & Roemer, 2004; Gross, 1998). Numerous studies have demonstrated an association between these various facets of emotion regulation and depressive symptoms. Cross-sectional studies have found that less use of adaptive (and greater use of maladaptive) emotion regulation strategies is associated with greater adolescent depressive symptoms (Betts et al., 2009; Garnefski & Kraaij, 2006). Similarly, greater difficulties with impulsivity have been associated with greater depressive symptoms across community (Piko & Pinczés, 2014) and court-involved (Zhou et al., 2014) adolescent samples. In cross-sectional studies with adolescents, less use of adaptive (and greater use of maladaptive) regulation strategies were found to serve as an indirect pathway through which poor impulse control (d’Acremont & Van der Linden, 2007) as well as poor emotional awareness (Eastabrook et al., 2014; Van Bereven et al., 2019) were associated with greater depressive symptoms.
A similar pattern of findings is evident in longitudinal studies. For example, lower emotional awareness has been shown to predict elevated child and adolescent depressive symptoms across a one-year period (Kranzler et al., 2016). Rieffe and De Rooij (2012) found that individual variability in emotional awareness across two years predicted individual variability in depressive symptoms; improvement in emotional awareness was associated with decreases in depressive symptoms. Folk and colleagues (2014) examined emotional expression, emotion suppression, and adaptive coping strategies in the context of feelings of sadness, anger, and worry, respectively, as predictors of depression in older children. Results suggested that emotional suppression of anger and worry predicted higher depressive symptoms per caregiver report, while adaptive worry coping predicted fewer depressive symptoms per child-report over the course of two years. Cumulatively, this body of work demonstrates a relatively robust linear relation between difficulties with emotion regulation in general and adolescent depressive symptoms. However, as not all facets of emotion regulation hold the same relation with depressive symptoms, further study of individual facets in relation to depression is warranted. It will also be important to move beyond a linear examination of these constructs to better understand the true nature of the association of individual facets of emotion regulation and depressive symptoms across time, such as whether they vary in tandem.
Present Study
To date, research has not examined the degree to which facets of emotion regulation and depressive symptom change in tandem over time. Given the multifaceted nature of emotion regulation (Gratz & Roemer, 2004), some facets of emotion regulation may remain correlated with depressive symptoms over time, while others do not. Such information holds important implications for depression prevention and treatment planning. The purpose of the present study was to investigate the degree to which trajectories of change in different facets of emotion regulation and depressive symptoms remain correlated over the course of twelve months in a sample of adolescents being treated for co-occurring mental health and substance use concerns. We focused on three facets of difficulties with emotion regulation that center around alteration of the emotion or its corresponding behavior – goal-directed behavior, impulse control, and regulation strategies. These action-oriented facets of emotion regulation are crucial for healthy adolescent development (Modecki et al., 2017) and can be readily addressed in the context of mental health treatment. We examined these questions in a treatment-involved sample of adolescents in which some change over time would be expected.
Consistent with past research, we hypothesized that initial levels of each facet of emotion regulation (goal-directed behavior, impulse control, and access to adaptive emotion regulation strategies) and depressive symptoms would be significantly correlated with each other. We also hypothesized that this relationship would persist over time, such that the trajectories of change between each facet of emotion regulation and depressive symptoms would be significantly associated with each other over the course of twelve months. To provide a conservative test of study hypotheses, we controlled for sex, age, and treatment condition in study analyses. Prior research suggests females, relative to males, tend to experience overall higher depressive symptoms during adolescence (Salk et al., 2017), and show different trajectories of change in depressive symptoms over time as they age (Salk et al., 2016). Additionally, treatment condition was not of focus in the present study. Thus, sex, age, and treatment condition were included as covariates.
Methods
Participants
The present sample consisted of 110 adolescents enrolled in a randomized controlled trial comparing a cognitive-behavioral intervention to enhanced standard care for adolescents with co-occurring mental health and substance use concerns (Wolff et al.,2020). The current study is a secondary analysis of these data and not an examination of the main outcomes of this trial. Participants ranged in age from 13–18 years (M = 15.71, SD = 1.18) at the baseline assessment. Just over half of participants were male (57.3%; 42.7% female) and were predominantly White (70.9%; 10.9% African American, 11.8% multiracial, 2.7% other; 3.6% unreported) and non-Latino (67.3%; 30.0% Latino; 2.7% unreported).
The inclusion criteria for this parent study were: 1) English-speaking adolescent and legal guardian(s); 2) adolescent assent (consent for 18-year-olds); 3) consent of a legal guardian; and 4) enrolled in the Intensive Outpatient, home-based program (IOP) for co-occurring substance use and mental health problems at the clinic, with reported alcohol and/or substance use in the prior three months. Youth were ineligible if they exhibited serious psychiatric symptoms (e.g., active hallucinations, thought disorder), a primary diagnosis of obsessive-compulsive disorder or disordered eating, acute homicidality, or violent behavior upon screening, indicating need for a specialized and/or higher level of care. Though presence of a depressive or externalizing disorder was not a requirement for study inclusion, rates of these diagnoses in the present sample were notable (see Table 1).
Table 1.
Sample Characteristics
| N | % | |
|---|---|---|
| Demographics | ||
| Sex | ||
| Male | 63 | 57.3 |
| Female | 47 | 42.7 |
| Race | ||
| White | 78 | 70.9 |
| African American | 12 | 10.9 |
| Multiracial | 13 | 11.8 |
| Other | 3 | 2.7 |
| Ethnicity | ||
| Latino | 33 | 30.0 |
| Non-Latino | 74 | 67.3 |
| Diagnoses at Baseline | ||
| Major Depressive Episode | 64 | 58.2 |
| Generalized Anxiety Disorder | 37 | 33.6 |
| Social Anxiety Disorder | 22 | 20.0 |
| Post-Traumatic Stress Disorder | 22 | 20.0 |
| Oppositional Defiant Disorder | 20 | 18.2 |
| Conduct Disorder | 62 | 56.4 |
| Attention Deficit/Hyperactivity Disorder | 60 | 54.5 |
| Alcohol Abuse/Dependence | 38 | 34.5 |
| Cannabis Abuse/Dependence | 94 | 85.5 |
| Other Substance Abuse/Dependence | 19 | 17.3 |
Note: Percentages do not total 100% as several participants chose to not report on these demographics.
Procedures
Prior to the start of data collection, all study procedures were approved by both university and hospital Institutional Review Boards. All adolescents and legal guardians who presented for intensive, home-based mental health services at a community-based facility located in the Northeastern United States were approached for recruitment. After consent/assent was obtained, a trained interviewer administered semi-structured diagnostic interviews (Schedule of Affective Disorders and Schizophrenia for School-Aged Children, Present and Lifetime Version [K-SADS-PL]; Kaufman et al., 1996) and research assistants administered the self-report assessments to adolescents and their guardians. This included screening, baseline, and follow-up assessments. After the baseline assessment, participants were randomized to one of two treatment conditions (Cognitive Behavioral Therapy experimental condition versus Treatment-as-Usual comparison condition). Intervention was conducted by clinicians employed in a community-based intensive outpatient setting that served youth with co-occurring substance misuse and mental health problems. The Cognitive-Behavioral Therapy condition included individual adolescent sessions, parent training sessions, and family sessions (Wolff et al., 2020). Follow-up assessments took place 3-, 6-, and 12-months post-baseline. All four time points are used in the present study.
Constructs and Measures
Facets of emotion regulation
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item self-report measure of clinically relevant difficulties with six facets of emotion regulation, corresponding to theoretically derived dimensions of emotion regulation. The DERS has a total scale and six subscales: Nonacceptance of emotional responses (6 items; e.g., “When I’m upset, I feel like I am weak”); Difficulties engaging in goal-directed behavior (5 items; e.g., “When I’m upset, I have difficulty getting work done”); Impulse control difficulties (6 items; e.g., “When I’m upset, I lose control over my behavior”); Lack of emotional awareness 6 items; e.g., “When I’m upset, I am attentive to my feelings,” reverse-coded); Limited access to emotion regulation strategies (8 items; e.g., “When I’m upset, I believe that wallowing in it is all I can do”); and Lack of emotional clarity (5 items; e.g., “When I’m upset, I have no idea how I am feeling”). Items on the DERS are rated on a scale from 1 (almost never) to 5 (almost always), with higher scores indicating greater difficulty with emotion regulation. A total score as well as six subscale scores can be derived. The DERS has demonstrated good to excellent internal consistency and construct validity when used with adolescents (Weinberg & Klonsky, 2009). The DERS subscales as well as total scale have been well-validated and widely used to examine the multifaced nature of emotion regulation across samples of community adolescents (Neumann et al., 2010) and adults (Bardeen et al., 2012; Lee et al., 2016), adults with severe mental illness (Fowler et al., 2014), and across cultures (Giromini et al., 2012; Ruganci & Gençöz, 2010). In the present study, internal consistency (∝) for the total score (.90 – .93) as well as the Nonacceptance of emotional responses (.91 – .92), Difficulties engaging in goal-directed behavior (.81 – .83), Impulse control difficulties (.79 – .85), Lack of emotional awareness (.83 – .84), and Limited access to emotion regulation strategies (.86 – .89) subscales was acceptable but low for the Lack of emotional clarity subscale across three of the four timepoints (.77, .74, .67; 12-month ∝ = .85).
In the present analyses, only the Difficulties engaging in goal-directed behavior, Impulse control difficulties, and Limited access to emotion regulation strategies subscales were used. This decision was made on theoretical and statistical grounds. Theoretically, these three facets focus on alteration of an emotion or resulting behavior, allowing for the examination of individual facets that are associated with action-oriented regulation (Skinner & Zimmer-Gembeck, 2007). Statistically, this decision was made to reduce multiple comparisons (Benjamini & Hochberg, 1995).
Depressive symptom severity
The Children’s Depression Inventory-2 (CDI-2; Kovacs, 2011) is a 28-item self-report measure of depressive symptoms during the past two weeks. Items on the CDI-2 are rated on a three-choice scale from 0 – 2 for each item, with higher scores indicating greater depressive symptoms (e.g., 0 = “I am sad once in a while,” 1 = “I am sad many times,” 2 = “I am sad all the time”). Possible raw scores ranged from 0 to 56. The CDI-2 has been shown to have good reliability and construct validity in adolescents (Kovacs, 2011). Internal consistency (∝) was good to excellent (.85 – .91) across all time points in this study.
Analysis Plan
Correlations among study variables were calculated using SPSS version 27. Skewness and kurtosis were also assessed. Missing data patterns can affect parameter estimates of structural equation models (Allison, 2003). Therefore, adolescents with complete versus missing data for emotion regulation difficulties and depressive symptom severity at any follow-ups (i.e., 3–12-months) were compared to baseline levels of each variable using independent t-tests. Adolescents were also compared across a variety of key demographic variables (i.e., age, sex, and treatment condition) with independent t-tests and chi-square tests. The Benjamini-Hochberg procedure, with the false discovery rate set at 5% was used to correct for multiple comparisons (see Benjamini & Hochberg, 1995).
Bivariate latent basis growth curve models (LGCMs; see Figure 1) were conducted in Mplus version 8.4 (Muthén & Muthén, 1998–2017) to examine the associations between trajectories of different facets of emotion regulation and depressive symptoms. LGCMs assume that a single trajectory underlies growth in a construct across time and provide estimation of a latent intercept, or initial level of the variable of interest, and a latent slope, or growth across time for the variable. LGCMs also allow for nonlinear growth across time (Bollen & Curran, 2006; Ferrer & McArdle, 2003). In a linear LGCM, the model is specified by setting slope loadings for all assessment time points. In a nonlinear LGCM, the model is specified by setting slope loadings for the first and last assessment time points, leaving all other loadings free to vary (Little, 2013). The initial slope loading also corresponds with the intercept (Little, 2013). First, linear and nonlinear univariate LGCMs (see Figure 2) were conducted for each facet of emotion regulation as well as for depressive symptoms to determine the best-fitting univariate models for each construct. Slope loadings for linear LGCMs were set at zero for (intercept) baseline, 3 for the first follow-up, 6 for the second follow-up, and 12 for the third follow-up to correspond with months across time. Slope loadings for nonlinear LGCMs were set at zero for (intercept) baseline and 12 for the final follow-up, with all other loadings freely estimated. This allows for interpretation of slope loadings for the first and second follow-ups (3- and 6-month) to be interpreted in terms of months. To determine whether a linear or nonlinear univariate LGCM was most appropriate for each construct, we examined the chi-square change from the nonlinear to the linear univariate LGCMs by constraining all non-significant slope loadings at 3- and 6-months. A non-significant difference in chi-square indicates that the linear model fits the data equally well and can thus be used as a more parsimonious representation of the data (Little, 2013).
Figure 1.
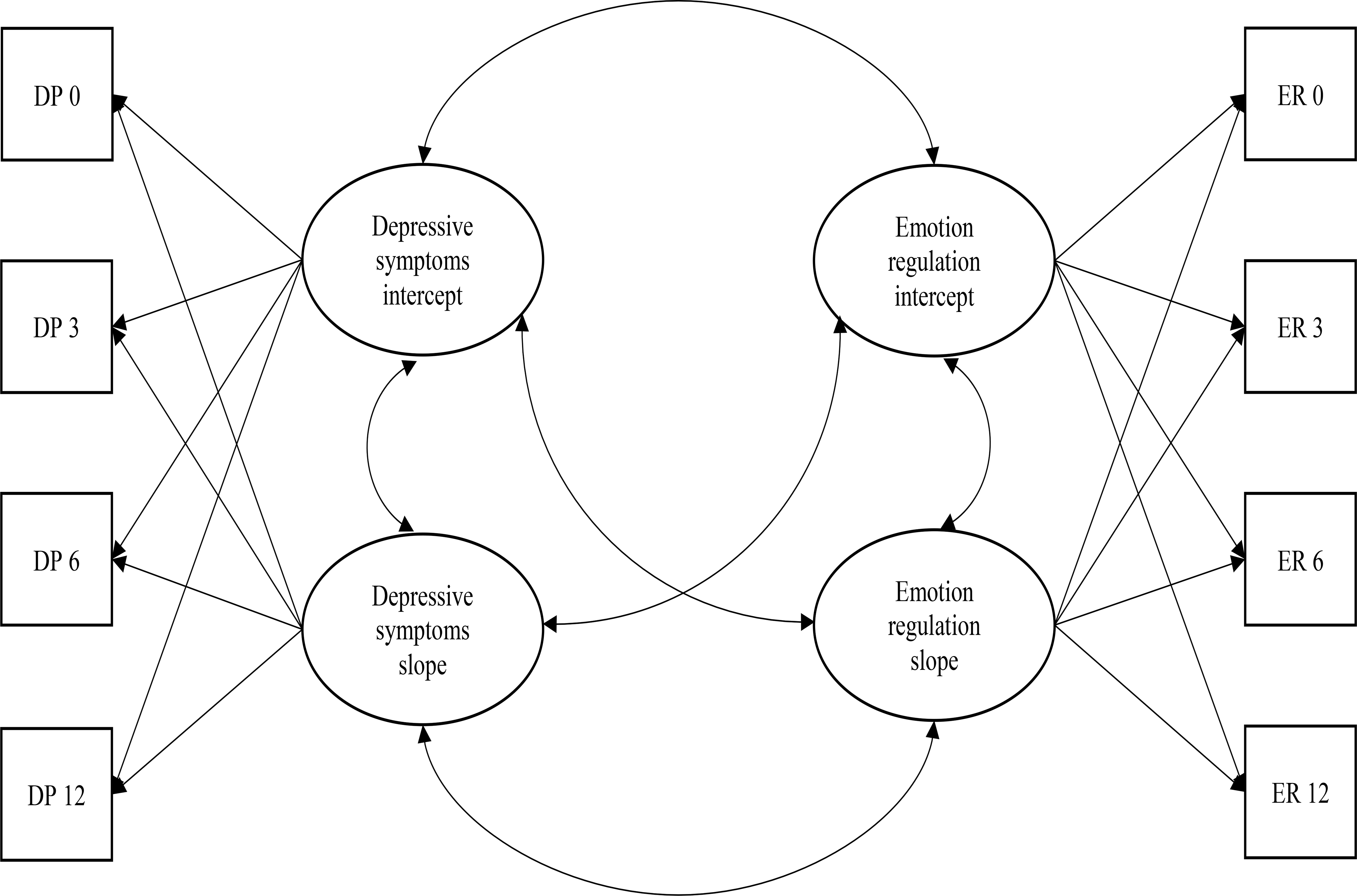
Bivariate latent basis growth curve model. This is a simplified depiction of the structural equation model used to estimate the latent basis growth curves of adolescent depressive symptoms (DP) and each facet of emotion regulation (ER). Covariates (age, sex, treatment group) on the latent intercepts and slopes are not depicted. The error structure is not shown.
Figure 2.
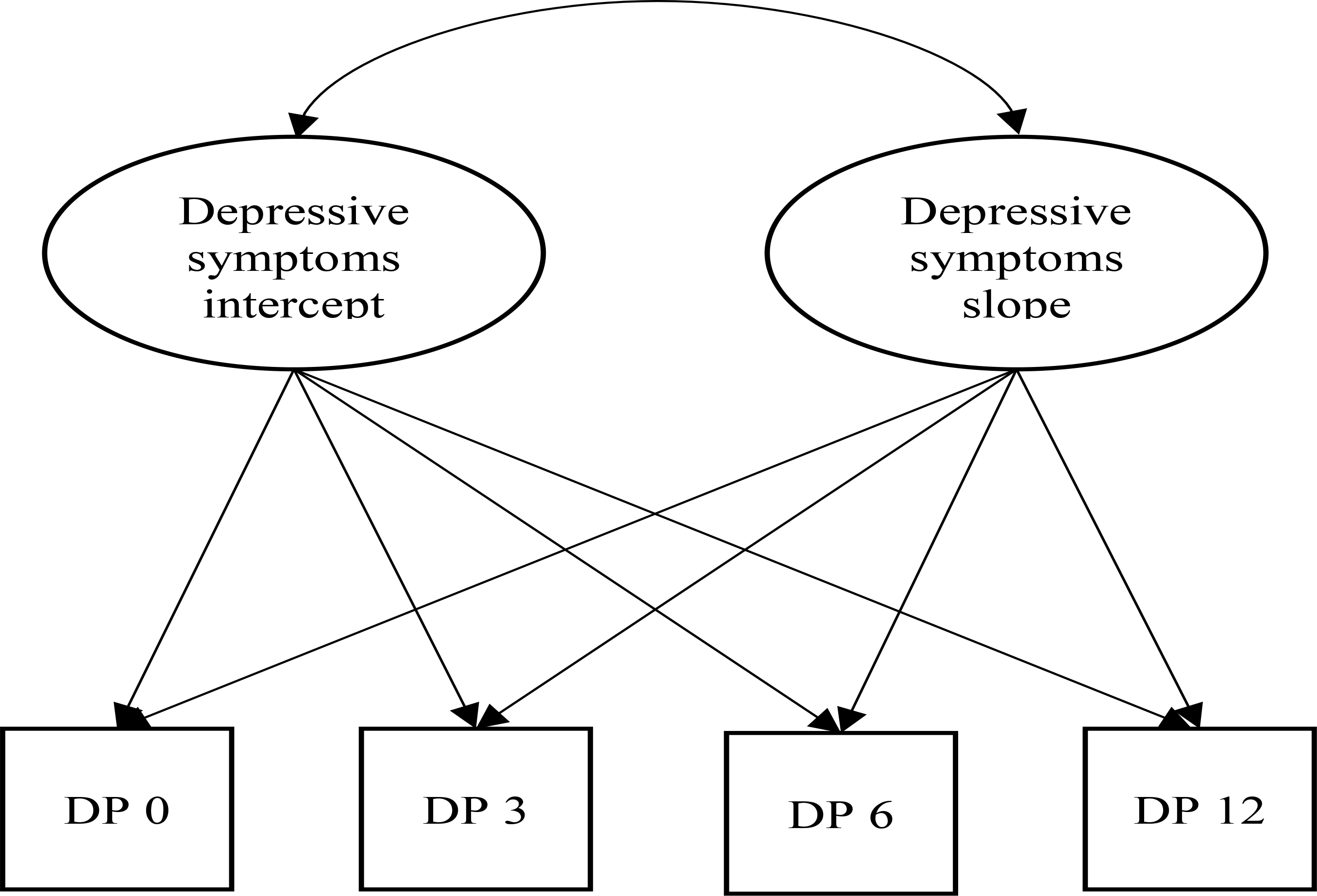
Univariate latent basis growth curve model. This depicts the structural equation model used to estimate the latent basis growth curve of adolescent depressive symptoms (DP). This model was also used for univariate latent basis growth curves for each facet of emotion regulation. The error structure is not shown.
To account for missing data, all models used full information likelihood estimation (FIML) and a maximum likelihood estimator (ML; Muthén & Muthén, 1998–2017). Individual model fit was assessed using the adjusted chi-square statistic, the comparative fit index (CFI), the Tucker-Lewis Index (TLI), and the root-mean-square error of approximation (RMSEA). A non-significant, chi-square suggests that the model fits the data well (Bentler & Bonnett, 1980). Additionally, based on rule of thumb criteria (Little, 2013), good fit is assumed for values ≥ .95 for CFI and TLI as well as ≤ .05 for RMSEA; acceptable fit is assumed by values ≥ .90 for CFI and TLI and ≤ .08 for RMSEA (Little, 2013). Because no one fit index determines whether a model optimally represents the data, we examined each model’s combination of fit indices (Wu et al., 2009) to determine whether each model functioned acceptably across multiple markers. Models with multiple fit indices below acceptable levels and that did not converge were not interpreted. Importantly, the CFI, TLI, and RMSEA address different dimensions of fit (e.g., sample- vs. population-based, absolute vs. relative fit, adjusted for model complexity vs. not), yet all three tend to be less affected by small sample size, relative to other indices (Sun, 2005; Wu et al., 2009).
Power analyses were conducted to ensure ample power to detect model fit with the stated number of participants. The MacCallum-Browne-Sugawara framework (MacCallum et al., 1996; MacCallum et al., 2010) was used, which allows for examination of power to detect overall model misfit, using RMSEA as the measure of effect, when the null hypothesis is specified as exact fit (that is, RMSEA = .00). Power estimates were conducted using R (R Core Team, 2020) with the RStudio development environment (RStudio Team, 2020), using a web utility code generator (Preacher & Coffman, 2006). We conducted a series of six power analyses with α = .05, N = 110, alternative RMSEA values set at .05 (“good”), .08 (“acceptable”), and .10 (“poor”), and degrees of freedom set at 36 (for bivariate LGCMs with two nonlinear constructs) and 38 (for bivariate LGCMs with one linear and one nonlinear construct). Results demonstrated that power is approaching .80 (1-β = .77, df = 36; 1-β = .79, df = 38) to detect acceptable fit (RMSEA = .08). Complete power results are presented in Supplementary Table 1.
To examine study hypotheses, we utilized three separate bivariate LGCMs (one for each facet of emotion regulation examined), which allow for examination of two different constructs and their interrelation across time. Correlations between the latent intercepts and latent slopes, as well as variability around the mean intercept and slope values, can also be derived (Bollen & Curran, 2006; Ferrer & McArdle, 2003). In the present study, correlations between latent intercepts were of interest to examine the relation between initial levels of emotion regulation and depressive symptoms. Correlations between latent slopes were of interest to examine whether trajectories of change in each facet of emotion regulation were related to depressive symptoms across time. To provide a stringent test of study hypotheses, adolescents’ age and sex, which have been shown to impact depressive symptoms and emotion regulation difficulties (Brummer et al., 2014; Gonçalves et al., 2019), as well as treatment condition, were regressed on all latent slopes and intercepts of the bivariate LCGMs. To correct for multiple comparisons, the Benjamini-Hochberg procedure, with the false discovery rate set at 5% was used (see Benjamini & Hochberg, 1995). This did not alter the pattern of significant results. Thus, the unadjusted p values and an alpha level of .05 is reported for ease of interpretation.
Results
Descriptive Statistics
Sample characteristics, including diagnoses as determined by the baseline semi-structured interview (K-SADS-PL), are presented in Table 1. As can be seen, the sample had high rates of both internalizing and externalizing diagnoses. Descriptive statistics and bivariate correlations among all model variables are presented in Tables 2 and 3, respectively. Additionally, skewness and kurtosis were within acceptable limits (see Lei & Lomax, 2005) for depressive symptoms and each facet of emotion regulation across all time points.
Table 2.
Descriptive Statistics of Model Variables
| M | SD | n | |
|---|---|---|---|
| Adolescent Depression (CDI-2) | |||
| Baseline | 16.66 | 10.10 | 110 |
| Month 3 | 12.75 | 7.64 | 90 |
| Month 6 | 11.38 | 7.29 | 90 |
| Month 12 | 10.01 | 8.46 | 94 |
| Difficulties with Goal-Directed Behaviora | |||
| Baseline | 16.50 | 4.95 | 109 |
| Month 3 | 14.77 | 5.32 | 85 |
| Month 6 | 14.70 | 5.37 | 87 |
| Month 12 | 13.88 | 5.27 | 89 |
| Difficulties with Impulse Controla | |||
| Baseline | 16.39 | 5.93 | 109 |
| Month 3 | 14.56 | 5.30 | 85 |
| Month 6 | 15.26 | 5.54 | 87 |
| Month 12 | 13.93 | 5.73 | 89 |
| Difficulties with Emotion Regulation Strategiesa | |||
| Baseline | 21.28 | 8.35 | 109 |
| Month 3 | 18.37 | 7.58 | 86 |
| Month 6 | 18.51 | 7.29 | 87 |
| Month 12 | 16.84 | 6.68 | 90 |
DERS subscale
Table 3.
Correlations Between Model Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | 19. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adolescent Depression (CDI-2) | |||||||||||||||||||
| 1. Dep. M0 | --- | ||||||||||||||||||
| 2. Dep. M3 | .56** | --- | |||||||||||||||||
| 3. Dep. M6 | .55** | .60** | --- | ||||||||||||||||
| 4. Dep. M12 | .54** | .55** | .66** | --- | |||||||||||||||
| Difficulties with Goal-Directed Behavior (DERS) | |||||||||||||||||||
| 5. Goal-Dir. M0 | .40** | .28** | .27* | .37** | --- | ||||||||||||||
| 6. Goal-Dir. M3 | .11 | .24* | −.06 | .12 | .41** | --- | |||||||||||||
| 7. Goal-Dir. M6 | .18 | .35** | .13 | .23* | .27* | .57** | --- | ||||||||||||
| 8. Goal-Dir. M12 | .11 | .34** | .15 | .32** | .31** | .38** | .50** | --- | |||||||||||
| Difficulties with Impulse Control (DERS) | |||||||||||||||||||
| 9. Impulse M0 | .38** | .23* | .30** | .25* | .60** | .31** | .37** | .23* | --- | ||||||||||
| 10. Impulse M3 | .16 | .30** | .08 | .15 | .24* | .64** | .54** | .23* | .46** | --- | |||||||||
| 11. Impulse M6 | .11 | .39** | .18 | .26* | .03 | .26* | .57** | .42** | .33** | .51** | --- | ||||||||
| 12. Impulse M12 | .17 | .29** | .19 | .36** | .22* | .24* | .39** | .65** | .36** | .35** | .60** | --- | |||||||
| Difficulties with Emotion Regulation Strategies (DERS) | |||||||||||||||||||
| 13. Strat. M0 | .58** | .31** | .26* | .36** | .64** | .24* | .33** | .19 | .71** | .29** | .22* | .28** | --- | ||||||
| 14. Strat. M3 | .25* | .46** | .06 | .19 | .32** | .65** | .52** | .28* | .39** | 74** | .42** | .24* | .38** | --- | |||||
| 15. Strat. M6 | .37** | .48** | .24* | .28* | .24* | .47** | .66** | .29* | .48** | .60** | .67** | .39** | .51** | 72** | --- | ||||
| 16. Strat. M12 | .32** | .40** | .30** | .44** | .33** | .24* | .33** | .55** | .37** | .25* | .47** | 73** | .45** | .36** | .43** | --- | |||
| Covariates | |||||||||||||||||||
| 17. Age | .31** | .27* | .18 | .25* | .16 | −.11 | −.04 | −.06 | .21* | −.10 | .06 | .13 | .28** | .05 | .08 | .24* | --- | ||
| 18. Sexa | .32** | .15 | .15 | .10 | .18 | −.14 | .16 | .08 | .14 | −.05 | .08 | .05 | .28** | .07 | .12 | .22* | .14 | --- | |
| 19. Treatment Groupb | .05 | .02 | .01 | −.03 | −.06 | −.06 | −.20 | −.06 | −.07 | −.08 | .01 | .001 | .02 | .11 | −.01 | .17 | .12 | .07 | --- |
0 = male and 1 = female
0 = Treatment-as-Usual comparison condition and 1 = Cognitive Behavioral Therapy experimental condition; M0 = Baseline; M3 = Month 3; M6 = Month 6; M12 = Month 12
p < .05
p < .01
Missing Data
Of the total 110 adolescents, approximately 18% had missing 3-month depressive symptom severity data, 18% at 6-months, and 15% at 12-months. Moreover, approximately 22% had missing 3-month emotion dysregulation data, 21% at 6-months, and 19% at 12-months. After correcting for multiple comparisons, adolescents with complete versus missing depressive symptom severity data at any follow-up did not differ significantly on depressive symptom severity or emotion regulation difficulties at baseline (p’s > .05). Similarly, adolescents with complete versus missing emotion regulation data at any follow-up did not differ significantly on emotion regulation abilities or depressive symptom severity at baseline (p’s > .05). Adolescents with missing versus complete data for either construct did not significantly differ across demographic variables (p’s > .05) or treatment condition (p’s > .05). Additionally, to determine if the pattern of missingness can be considered missing completely at random (MCAR), Little’s test (Li, 2013) using SPSS version 27 was conducted. A non-significant difference in chi-square value indicates that the pattern of missingness does not differ from what would be expected when data is MCAR (Li, 2013). Results suggest that the present data can be considered MCAR (χ2(187) = 194.55, p = .34).
Model Fit
All LGCM fit indices are presented in Table 4. Univariate LGCMs for each of the variables of interest indicated that depressive symptoms and goal-directed behavior each followed a nonlinear trajectory, while impulse control followed a linear trajectory. Model fit indices for emotion regulation strategies were below acceptable levels in both linear (CFI = .80, TLI = .85, RMSEA = .15) and nonlinear (CFI = .84, TLI = .84, RMSEA = .16) univariate LGCMs. Graphs of modeled growth trajectories based on nonlinear univariate LGCMs can be seen in Figure 3.
Table 4.
Univariate and bivariate latent growth curve model fit indices.
| Model descriptions | Model fit | Model comparisons | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Univariate models | χ2 (df) | p | CFI | TLI | RMSEA | AIC | BIC | Δχ2 (Δdf) | p |
| Nonlinear depressive symptom model | 8.34 (6) | .214 | .99 | .99 | .06 | 2600.90 | 2597.23 | – | – |
| Nonlinear goal-directed behavior model | 7.81 (6) | .252 | .97 | .97 | .05 | 2217.71 | 2214.03 | – | – |
| Nonlinear impulse control model | 10.37 (6) | .110 | .94 | .94 | .08 | 2270.12 | 2266.45 | – | – |
| Linear impulse control model | 14.47 (8) | .070 | .92 | .94 | .08 | 2270.23 | 2267.47 | 4.10 (2) | .129 |
| Nonlinear regulation strategies model | 22.51 (6) | .001 | .84 | .84 | .16 | 2482.16 | 2478.48 | – | – |
| Linear regulation strategies model | 27.93 (8) | .001 | .80 | .85 | .15 | 2483.57 | 2480.81 | 5.42 (2) | .067 |
| Bivariate models | |||||||||
| Depressive symptoms & goal-directed behavior | 58.97 (36) | .009 | .91 | .87 | .08 | 4793.82 | 4880.23 | – | – |
| Depressive symptoms & impulse control | 57.47 (38) | .022 | .93 | .90 | .07 | 4850.96 | 4837.17 | – | – |
| Depressive symptoms & regulation strategies | 73.34 (36) | <.001 | .89 | .83 | .10 | 5030.09 | 5015.39 | – | – |
Note. χ2 = Chi-square; df = degrees of freedom; CFI = comparative fit index; TLI = Tucker-Lewis index; RMSEA = root-mean-square error of approximation; AIC = Akaike information criteria; BIC = sample-size adjusted Bayesian information criteria; Δ = change in parameter.
Figure 3.
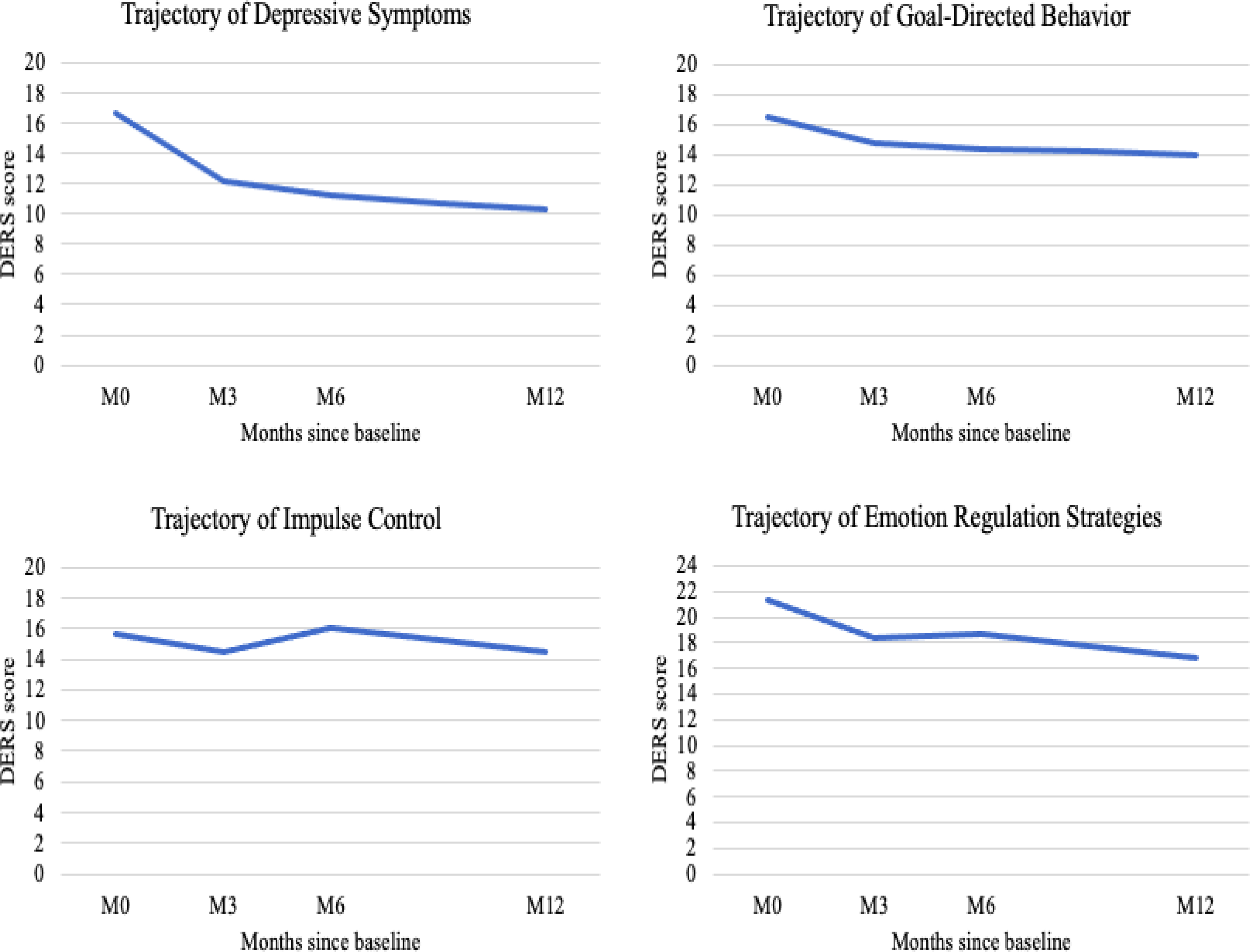
Trajectories of growth over time in adolescent depression and facets of emotion regulation. Modeled growth trajectories across twelve months for adolescent depressive symptoms, difficulties engaging in goal-directed behavior, impulse control difficulties, and limited access to emotion regulation strategies. Trajectories presented here are based on the nonlinear univariate latent growth curve models.
For the bivariate LGCM of depressive symptoms and goal-directed behavior, model fit indices suggested acceptable fit (CFI = .91, TLI = .87, RMSEA = .08). For the bivariate LGCM of depressive symptoms and impulse control, model fit indices also suggested good fit (CFI = .93, TLI = .90, RMSEA = .08). Though the univariate LGCM fit indices for emotion regulation strategies were below acceptable levels, the bivariate LGCM including depressive symptoms was still conducted, as it is directly relevant to study hypotheses. Model fit indices for the bivariate LGCM of depressive symptoms and emotion regulation strategies were also below acceptable levels (CFI = .89, TLI = .83, RMSEA = .10) and the model did not converge. As such, parameter estimates in this model cannot be interpreted. Results associated with emotion regulation strategies are therefore not presented further but are considered in the discussion.
Covariates
Age, sex, and treatment condition were regressed on the intercept and slope of both (goal-directed behavior and impulse control) final bivariate latent growth models (see Supplementary Table 2 for regression parameters). Across both bivariate LGCMs, older (versus younger) adolescents demonstrated greater initial depressive symptoms. Age did not affect the trajectories of any constructs of interest. Females (relative to males) demonstrated greater initial depressive symptoms and slower decreases in symptom severity over time. Treatment condition was not significantly related to initial levels or trajectories of depressive symptoms, goal-directed behavior, or impulse control. Thus, the rate at which adolescents experienced a change in depressive symptoms, goal-directed behavior, and impulse control did not vary between the experimental Cognitive-Behavioral Therapy and Treatment-as-Usual groups.
Correlations Between Depressive Symptoms and Difficulties with Emotion Regulation
Estimated intercept and slope values for the goal-directed behavior and impulse control bivariate LGCMs are presented in Table 5. Correlations between intercepts and slopes, on which study hypotheses are focused, are presented in Table 6. Consistent with study hypotheses, initial levels (intercepts) of goal-directed behavior and depressive symptoms were significantly correlated (r = .67, p < .001). Greater difficulty with engaging in goal-directed behavior was associated with higher depressive symptoms. Similarly, greater initial levels of impulse control were related to greater initial depressive symptoms (r = .46, p < .001). Results diverged with regard to the correlation between trajectories of change. Counter to hypotheses, change in goal-directed behavior over time was not significantly associated with change in depressive symptoms (r = .67, p = .21). Though this correlation is of a moderate magnitude, the standard error relative to the estimate (see Table 6) resulted in a critical ratio that is too low for this correlation to reach significance (Cohen et al., 2003). However, consistent with hypotheses, change in impulse control over time was significantly associated with change in depressive symptoms (r = .83, p = .008). That is, the rate of change in difficulties with impulse control was positively associated with the rate of change in depressive symptoms. Slope estimates were negative for both impulse control (B = −0.17, p = .003) and depressive symptoms (B = −0.54, p < .001), indicating a significant decline in both difficulty with impulse control and in depressive symptoms across the twelve-month study period.
Table 5.
Bivariate latent growth curve model intercepts and slopes.
| Model & parameter descriptions | Estimate (standard error) | Critical ratio | p |
|---|---|---|---|
| Depressive symptoms & goal-directed behavior | |||
| Depressive symptoms intercept | 16.75 (0.94) | 17.82 | <.001 |
| Depressive symptoms slope | −0.53 (0.07) | −7.17 | <.001 |
| Goal-directed behavior intercept | 16.57 (0.47) | 34.96 | <.001 |
| Goal-directed behavior slope | −0.19 (0.05) | −3.65 | <.001 |
| Depressive symptoms & impulse control model | |||
| Depressive symptoms intercept | 16.74 (0.94) | 17.85 | <.001 |
| Depressive symptoms slope | −0.54 (0.07) | −7.23 | <.001 |
| Impulse control intercept | 16.09 (0.50) | 32.29 | <.001 |
| Impulse control slope | −0.17 (0.06) | −2.98 | .003 |
Note. All parameter estimates presented here are unstandardized.
Table 6.
Correlations between intercepts and slopes in each bivariate latent growth curve model.
| Model & parameter descriptions | r | Estimate (standard error) | Critical ratio | p |
|---|---|---|---|---|
| Depressive symptoms & goal-directed behavior | ||||
| Depressive symptoms intercept ↔ depressive symptoms slope | −.64** | −1.99 (0.76) | −2.61 | <.001 |
| Goal-directed behavior intercept ↔ goal-directed behavior slope | .01 | 0.01 (0.36) | 0.01 | .987 |
| Depressive symptoms intercept ↔ goal-directed behavior slope | −.40 | −0.53 (0.42) | −1.26 | .265 |
| Goal-directed behavior intercept ↔ depressive symptoms slope | −.36 | −0.44 (0.34) | −1.32 | .173 |
| Depressive symptoms intercept ↔ goal-directed behavior intercept | .67** | 14.79 (4.37) | 3.38 | <.001 |
| Depressive symptoms slope ↔ goal-directed behavior slope | .67 | 0.05 (0.04) | 1.38 | .206 |
| Depressive symptoms & impulse control model | ||||
| Depressive symptoms intercept ↔ depressive symptoms slope | −.64** | −2.01 (0.77) | −2.61 | <.001 |
| Impulse control intercept ↔ impulse control slope | −.33 | −0.40 (0.34) | −1.17 | .100 |
| Depressive symptoms intercept ↔ impulse control slope | −.33 | −0.75 (0.51) | −1.49 | .133 |
| Impulse control intercept ↔ depressive symptoms slope | −.29 | −0.48 (0.35) | −1.40 | .152 |
| Depressive symptoms intercept ↔ impulse control intercept | .46** | 13.62 (4.53) | 3.01 | <.001 |
| Depressive symptoms slope ↔ impulse control slope | .83* | 0.11 (0.04) | 2.56 | .008 |
Note. Bolded pathways denote correlations comprising a primary research question.
significant at the .01 level
significant at the .001 level
Discussion
It is well established that difficulties with emotion regulation are associated with adolescent depressive symptoms both cross-sectionally (Betts et al., 2009; Piko & Pinczés, 2014; Yap et al., 2010) and longitudinally (Folk et al., 2014; Masters et al., 2019; McLaughlin et al., 2009). The present study sought to build on extant literature by examining the degree to which trajectories of change in different facets of emotion regulation (i.e., engaging in goal-directed behavior, impulse control, and access to emotion regulation strategies) and depressive symptoms co-vary over the course of twelve months. This was studied in a clinical sample of adolescents enrolled in a randomized controlled trial testing a cognitive-behavioral treatment for co-occurring mental health and substance use concerns, where some degree of change is expected over time.
Consistent with hypotheses, the growth curves of impulse control difficulties and depressive symptoms were related. Specifically, and consistent with prior cross-sectional research (d’Acremont & Van der Linden, 2007; Piko & Pinczés, 2014; Zhou et al., 2014), adolescents who reported greater difficulty with impulse control at baseline also had higher depressive symptoms at baseline. Extending this work, the present study also found that adolescents who evidenced a greater rate of decline in perceived impulse control difficulties (that is, a greater rate of improvement in impulse control) also showed a greater rate of decline in depressive symptoms across twelve months. Thus, adolescents’ depressive symptoms appear to improve as their perceived ability to control impulses improves. These findings should be interpreted in the context of the study sample. The majority of adolescents had a depressive disorder as well as a neurocognitive (Attention-Deficit Hyperactivity Disorder) and/or disruptive behavior disorder (Oppositional Defiant Disorder or Conduct Disorder) commonly characterized by high levels of impulsivity (Austerman, 2015; Long et al., 2015). Youth who are impulsive often receive negative feedback from adults and peers and experience significant negative consequences for their impulsive behavior (e.g., loss of prosocial peers, poor grades, conflictual familial relationships; Hofer et al., 2013; Koutamanis et al., 2015; Lozano et al., 2014; Saylor & Amann, 2016). Depressive symptoms can develop from the internalization of recurrent negative feedback (Zahn-Waxler et al., 2000). Negative consequences may further increase stress and lower self-esteem, both of which impact depression (Orth & Robins, 2013; Thapar et al., 2012). Therefore, it stands to reason that adolescents who report an improvement in their ability to control their behaviors, whether through therapy or other means, may also experience a decline in their depressive symptoms.
In comparison to impulse control, the relation between goal-directed behavior and depressive symptoms did not endure. Consistent with study hypotheses, adolescents who reported greater difficulty engaging in goal-directed behavior also conveyed higher depressive symptoms at baseline. This finding is consistent with cross-sectional research which suggests that adolescents experiencing depression have trouble completing tasks, engaging in activities, and concentrating (Carr, 2015). However, counter to expectations, the trajectories of change in goal-directed behavior and depressive symptoms were not correlated across the twelve-month period. Interestingly, in the present sample, mean levels of perceived difficulties with engagement in goal-directed behavior (across months three, six, and twelve) were relatively equal to, and mean levels of perceived impulse control relatively greater than, those reported in community-based adolescent samples that also used the DERS to assess facets of emotion regulation (Neumann et al., 2010; Weinberg & Klonsky, 2009). Thus, it is possible that levels of goal directed behavior during follow-up time points were relatively normative and stable in the present sample, and thus did not correlate with depressive symptoms over time. Additionally, the difference in findings regarding the correlation between slopes across the goal-directed behavior and impulse control models suggest that the pattern of results differs by facet of emotion regulation.
Fit indices of latent basis growth curve models of difficulties with accessing emotion regulation strategies (both univariate and bivariate with depressive symptoms) were below acceptable levels. Additionally, the bivariate model did not properly converge, and thus could not be interpreted. Poor model fit may suggest that difficulty accessing adaptive emotion regulation strategies and adolescent depressive symptoms do not vary together across time. There are several other reasons for why a LGCM may demonstrate misfit (Wu et al., 2009). One possibility is that the model is misspecified; that is, there may be a degree of individual difference that is not accounted for in this model. Misfit can also be associated with the covariance structure (Wu et al., 2009). In the present study, the standard deviation of the emotion regulation strategies variable at each time point were higher than the standard deviations of the other two emotion regulation facets (i.e., impulse control and goal directed behavior). Taken together, study results may suggest that an important third variable was not accounted for in the emotion regulation strategies models.
Notably, as suggested above, the present study assessed adolescents’ perceptions of being able to effectively access and use emotion regulation strategies. Though other past work has documented an association between use of emotion regulation strategies and depressive symptoms, these studies have employed assessments of specific types of emotion regulation strategies (e.g., cognitive reframing, suppression; Betts et al., 2009; Garnefski & Kraaij, 2006). Thus, it is possible that this difference in assessment of emotion regulation strategies may help explain discrepancy in findings with past work. Further, use of specific emotion regulation strategies could be one missing factor that led to misspecification of the emotion regulation strategies growth models examined.
Clinical Implications
Findings from the present study hold important clinical implications. First, the link between perceptions of impulse control difficulties and depressive symptoms is useful for treatment planning. When working with adolescents with co-occurring depressive and externalizing symptoms, targeting skills to improve impulse control may be an important first step. For example, integration of mindfulness practices can promote improvements in impulse control by allowing the adolescent to stay present. Several recent reviews suggest that mindfulness practices for adolescents can result in a reduction of depressive symptoms and improvements in attention and emotion regulation, including impulse control (Biegel et al., 2009; Broderick & Jennings, 2012; Lin et al., 2019; Sanger & Dorjee, 2015). Moreover, mindfulness practices may have a neurobiological underpinning for promoting effective decision-making and regulating impulses. A recent study with adults (Taren et al., 2017) demonstrated that mindfulness practices are associated with increased functional connectivity between the dorsolateral prefrontal cortex, a region that is important in making cost-benefit comparisons and modulating behavior control (Basten et al., 2010; Hutcherson et al., 2012), and dorsal and ventral corticolimbic circuits, which play a role in cognitive control (Taren et al., 2017). Extension of neurobiological studies of mindfulness in adolescent samples has been encouraged (Sanger & Dorjee, 2015).
Second, the present findings suggest that perceptions of impulse control are important to consider in therapy. When adolescents believe that they are able to control their emotions and behaviors, they may be more likely to use their emotion regulation skills. Improvements in impulse control will, in turn, be observed by others (e.g., a parent, teacher, therapist) and yield positive responses. Under such conditions, adolescents may experience a concurrent decline in depressive symptoms. Several skills traditionally used in a cognitive-behavioral therapy approach to adolescent mental health treatment are relevant to this process. For example, the use problem solving, which includes an evaluation (pros and cons) of each potential solution generated (Friedberg & McClure, 2015), may help improve decision-making for those with impulse control difficulties. Affect regulation skills may be used to reduce heightened negative emotions that can impair effective decision-making (Friedberg & McClure, 2015). Cognitive restructuring can be used to help address unhelpful or untrue thoughts about one’s ability to control negative emotions and behavior (Friedberg & McClure, 2015). Together, the use of these skills may aid in addressing perceptions of impulse control difficulties.
Limitations and Future Directions
Although there are numerous strengths of the present study, including a multi-wave design, the use of repeated, well-validated self-report measures, and a stringent data analytic strategy, results should be interpreted within the context of several limitations. First, assessment of facets of emotion regulation was based on adolescent self-report. In the absence of objective assessments of engagement in goal-directed behavior, impulse control, and use of specific emotion regulation strategies, it cannot be concluded that adolescents actually evidenced changes in these components of emotion regulation. However, one recent study demonstrated that adolescent self-report, but not behavioral assessment, of impulsivity predicted adolescent behavior, such as substance use (Janssen et al., 2015). Moreover, the process model of emotion regulation posits that in order for effective emotion regulation to occur, an adolescent must be able to hold a mental representation of emotion regulation tactics, or the perception that he or she can engage in that tactic (Sheppes et al., 2015). Thus, adolescent self-report of emotion regulation may yield an accurate assessment of behavior. Nonetheless, use of multi-method approaches, including behavioral paradigms to assess facets of emotion regulation, in future research may offer a more comprehensive test of the questions under study. A second limitation of the present study is that causal inference cannot be drawn from latent basis growth curve modeling (Cohen et al., 2003; Curran et al., 2010). Rather, this model is limited to examining concurrent trajectories of change. Therefore, we cannot establish whether a change in perceptions of impulse control results in a change in depressive symptoms, or vice versa. Nevertheless, the current findings provide evidence for the interconnected nature of perceived impulse control (and difficulties thereof) and adolescent depressive symptoms. Future research using other longitudinal modeling approaches that allow for causal inference (e.g., Toh & Hernán, 2008) will be important to conduct.
Third, the generalizability of the present results may be limited. Though the use of a clinical sample of adolescents who are at heightened risk for severe negative outcomes in the absence of intervention is another clear strength of the present study, the sample is relatively unusual in that they had co-occurring substance use and mental health symptoms requiring intensive treatment. It is unclear whether results will generalize to less clinically severe (e.g., depressed adolescents without significant substance use) or community-based samples. Further, as noted above, the present clinical sample was characterized by high rates of depressive, externalizing (oppositional defiant, conduct disorders), neurodevelopmental (ADHD), and substance use disorders. Mean levels of difficulty with emotion regulation in the present sample were comparable to that found in another mixed clinical sample of adolescents without histories of nonsuicidal self-injury (though lesser than those with self-injury; Perez et al., 2012). Nonetheless, youth with primary diagnoses of other disorders commonly characterized by impulsivity, that would be better suited for another type of treatment, such as eating and obsessive-compulsive disorders, were excluded. Given research which suggests that degree of emotion regulation difficulties varies with different types of eating pathology (e.g., eating disorder with restriction versus binging/purging; Weinbach et al., 2018) as well as patterns of comorbidity (e.g., depressive symptoms) among individuals with obsessive-compulsive symptoms (Whitehead & Suveg, 2016), it is possible that results of the present study may have differed if youth with primary eating or obsessive-compulsive disorders were included. Additionally, the present sample was also comprised of predominantly White and non-Hispanic participants, and thus results may not generalize to a more ethnically and racially diverse sample. Further, data were gathered in the context of an intervention trial, though it was conducted in a real-world community mental health setting with clinicians employed in that setting.
Last, because this study employed secondary data analysis, the sample size was pre-fixed and the study slightly underpowered, which may have affected our ability to detect significant effects. Thus, results should be interpreted with caution. Nonetheless, the significant association found between perceived impulse control and depressive symptoms over time, speaks to the strength of the effects found in this area. Finally, given the novelty of studying the concurrent trajectory of difficulties with emotion regulation and adolescent depressive symptoms, results from the present study could not be compared to standardized benchmarks in this area.
Conclusion
The current study extends prior research to suggest that improvement in impulse control difficulties are associated with a concurrent decline in depressive symptoms over time in the context of mental health treatment. The same was not true for perceived goal directed behavior or use of general adaptive emotion regulation strategies. These results have meaningful implications for addressing depressive symptoms and perceptions of impulse control in the context of mental health treatment.
Supplementary Material
Acknowledgements
The authors thank the National Institute on Alcohol Abuse and Alcoholism (NIAAA; grant number R01AA020705) for the financial support and recognize that the findings and conclusions are those of the authors and do not necessarily reflect the opinions of NIAAA.
Funding:
This work was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA; grant number R01AA020705).
Footnotes
Declarations of interest: none.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allison PD (2003). Missing data techniques for structural equation modeling. Journal of Abnormal Psychology , 112(4), 545–557. 10.1037/0021-843X.112.4.545 [DOI] [PubMed] [Google Scholar]
- Austerman J (2015). ADHD and behavioral disorders: Assessment, management, and an update from DSM-5. Cleveland Clinic Journal of Medicine, 82(S1), S2–S7. 10.3949/ccjm.82.s1.01 [DOI] [PubMed] [Google Scholar]
- Bardeen JR, Fergus TA, & Orcutt HK (2012). An examination of the latent structure of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 34, 382–392. 10.1007/s10862-012-9280-y [DOI] [Google Scholar]
- Basten U, Biele G, Heekeren HR, & Fiebach CJ (2010). How the brain integrates costs and benefits during decision making. Proceedings of the National Academy of Sciences of the United States of America, 107(50), 21767–21772. 10.1073/pnas.0908104107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Methodological), 57(1), 289–300. 10.1111/j.2517-6161.1995.tb02031.x [DOI] [Google Scholar]
- Bentler PM, & Bonett DG (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin, 88(3), 588–606. 10.1037/0033-2909.88.3.588 [DOI] [Google Scholar]
- Betts J, Gullone E, & Sabura Allen J (2010). An examination of emotion regulation, temperament, and parenting style as potential predictors of adolescent depression risk status: A correlational study. British Journal of Developmental Psychology, 27(2), 473–485. 10.1348/026151008X314900 [DOI] [PubMed] [Google Scholar]
- Biegel GM, Brown KW, Shapiro SL, Schubert CM (2009). Mindfulness-based stress reduction for the treatment of adolescent psychiatric outpatients: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 77(5), 855–866. 10.1037/a0016241 [DOI] [PubMed] [Google Scholar]
- Bollen KA, & Curran PJ (2006). Latent curve models: A structural equation perspective (Vol. 467). John Wiley & Sons. [Google Scholar]
- Broderick PC, & Jennings PA (2012). Mindfulness for adolescents: A promising approach to supporting emotion regulation and preventing risky behavior. New Directions for Youth Development, 136, 111–126. 10.1002/yd.20042 [DOI] [PubMed] [Google Scholar]
- Brummer L, Stopa L, & Bucks R (2014). The influence of age on emotion regulation strategies and psychological distress. Behavioural and Cognitive Psychotherapy, 42(6), 668–681. 10.1017/S1352465813000453 [DOI] [PubMed] [Google Scholar]
- Carr A (2015). The handbook of child and adolescent clinical psychology: A contextual approach. Routledge. [Google Scholar]
- Cohen J, Cohen P, West SG, & Aiken LS (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Erlbaum. [Google Scholar]
- Clear SJ, Gardner AA, Webb HJ, & Zimmer-Gembeck MJ (2020). Common and distinct correlates of depression, anxiety, and aggression: Attachment and emotion regulation of sadness and anger. Journal of Adult Development, 27(3), 181–191. 10.1007/s10804-019-09333-0 [DOI] [Google Scholar]
- Compas BE, Jaser SS, Bettis AH, Watson KH, Gruhn MA, Dunbar JP, Williams E, & Thigpen JC (2017). Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychological Bulletin, 143(9), 939–991. 10.1037/bul0000110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cracco E, Goossens L, & Braet C (2017). Emotion regulation across childhood and adolescence: evidence for a maladaptive shift in adolescence. European Child & Adolescent Psychiatry, 26(8), 909–921. 10.1007/s00787-017-0952-8 [DOI] [PubMed] [Google Scholar]
- Curran PJ, Obeidat K, & Losardo D (2010). Twelve frequently asked questions about growth curve modeling. Journal of Cognition and Development, 11(2), 121–136. 10.1080/15248371003699969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- d’Acremont M, & Van der Linden M (2007). How is impulsivity related to depression in adolescence? Evidence from a French validation of the cognitive emotion regulation questionnaire. Journal of Adolescence, 30(2), 271–282. 10.1016/j.adolescence.2006.02.007 [DOI] [PubMed] [Google Scholar]
- Eastabrook JM, Flynn JJ, & Hollenstein T (2014). Internalizing symptoms in female adolescents: Associations with emotional awareness and emotion regulation. Journal of Child and Family Studies, 23(3), 487–496. 10.1007/s10826-012-9705-y [DOI] [Google Scholar]
- Feng X, Keenan K, Hipwell AE, Henneberger AK, Rischall MS, Butch J, Boeldt C, Boeldt D, Hinze AK, Babinski DE (2009). Longitudinal associations between emotion regulation and depression in preadolescent girls: Moderation by the caregiving environment. Developmental Psychology , 45(3), 798–808. 10.1037/a0014617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer E, & McArdle J (2009). Alternative structural models for multivariate longitudinal data analysis. Structural Equation Modeling: A Multidisciplinary Journal, 10(4), 493–524. 10.1207/S15328007SEM1004_1 [DOI] [Google Scholar]
- Folk JB, Zeman JL, Poon JA, & Dallaire DH (2014). A longitudinal examination of emotion regulation: Pathways to anxiety and depressive symptoms in urban minority youth. Child and Adolescent Mental Health, 19(4), 243–250. 10.1111/camh.12058 [DOI] [PubMed] [Google Scholar]
- Fowler JC, Charak R, Elhai JD, Allen JG, Frueh BC, & Oldham JM (2014). Construct validity and factor structure of the Difficulties in Emotion Regulation Scale among adults with severe mental illness. Journal of Psychiatric Research, 58, 175–180. 10.1016/j.jpsychires.2014.07.029 [DOI] [PubMed] [Google Scholar]
- Friedberg RD, & McClure JM (2015). Clinical practice of cognitive therapy with children and adolescents: The nuts and bolts (2nd ed.). Guilford Press. [Google Scholar]
- Garnefski N, Kraaij V, & van Etten M (2005). Specificity of relations between adolescents’ cognitive emotion regulation strategies and internalizing and externalizing psychopathology. Journal of Adolescence, 28(5), 619–631. 10.1016/j.adolescence.2004.12.009 [DOI] [PubMed] [Google Scholar]
- Garnefski N, & Kraaiji V (2006). Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Personality and Individual Differences, 40(8), 1659–1669. 10.1016/j.paid.2005.12.009 [DOI] [Google Scholar]
- Giromini L, Velotti P, de Campora G, Bonalume L, & Zavattini GC (2012). Cultural adaptation of the Difficulties in Emotion Regulation Scale: Reliability and validity of an Italian version. Journal of Clinical Psychology, 68(9), 989–1007. 10.1002/jclp.21876 [DOI] [PubMed] [Google Scholar]
- Gladstone TRG, & Beardslee WR (2009). The prevention of depression in children and adolescents: A review. The Canadian Journal of Psychiatry, 54(4), 212–221. 10.1177/070674370905400402 [DOI] [PubMed] [Google Scholar]
- Gonçalves SF, Chaplin TM, Turpyn CC, Niehaus CE, Curby TW, Sinha R, & Ansell EB (2019). Difficulties in emotion regulation predict depressive symptom trajectory from early to middle adolescence. Child Psychiatry and Human Development, 50, 618–630. 10.1007/s10578-019-00867-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment , 26, 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Gross JJ (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2(3), 271–299. 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- Hofer C, Eisenberg N, Spinrad TL, Morris AS, Gershoff E, Valiente C, Kupfer A, & Eggum ND (2013). Mother-adolescent conflict: Stability, change, and relations with externalizing and internalizing behavior problems. Social Development, 22(2), 259–279. 10.1111/sode.12012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope TL, Adams C, Reynolds L, Powers D, Perez RA, & Kelley ML (1999). Parent vs. self-report: Contributions toward diagnosis of adolescent psychopathology. Journal of Psychopathology and Behavioral Assessment, 21, 349–363. 10.1023/A:1022124900328 [DOI] [Google Scholar]
- Hutcherson CA, Plassmann H, Gross JJ, & Rangel A (2012). Cognitive regulation during decision making shifts behavioral control between ventromedial and dorsolateral prefrontal value systems. Journal of Neuroscience, 32(39), 13543–13554. 10.1523/JNEUROSCI.6387-11.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen T, Larsen H, Peeters M, Boendermaker WJ, Vollebergh WAM, & Wiers RW (2015). Do online assessed self-report and behavioral measures of impulsivity-related constructs predict onset of substance use in adolescents? Addictive Behaviors Reports, 1, 12–18. 10.1016/j.abrep.2015.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, & Ryan N (1996). Diagnostic Interview: Kiddie-SADS-Present and Lifetime Version (K-SADS-PL). Kaufman, Birmaher, Rao, &Ryan. [Google Scholar]
- Kaufman AS, & Kaufman NL (1990). K-BIT: Kaufman Brief Intelligence Test: Manual. American Guidance Service. [Google Scholar]
- King SM, Iacono WG, & McGue M (2004). Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction, 99(12), 1548–1559. 10.1111/j.1360-0443.2004.00893.x [DOI] [PubMed] [Google Scholar]
- Koutamanis M, Vossen HGM, & Valkenburg PM (2015). Adolescents’ comments in social media: Why do adolescents receive negative feedback and who is most at risk? Computers in Human Behavior, 53, 486–494. 10.1016/j.chb.2015.07.016 [DOI] [Google Scholar]
- Kovacs M (2011). Children’s Depression Inventory 2nd Edition: Technical manual. Multi-Health System. [Google Scholar]
- Kranzler A, Young JF, Hankin BL, Abela JRZ, Elias MJ, & Selby EA (2015). Emotional awareness: A transdiagnostic predictor of depression and anxiety for children and adolescents. Journal of Clinical Child & Adolescent Psychology, 45(3), 262–269. 10.1080/15374416.2014.987379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee DJ, Witte TK, Bardeen JR, Davis MT, & Weathers FW (2016). A factor analytic evaluation of the Difficulties in Emotion Regulation Scale. Journal of Clinical Psychology, 72(9), 933–946. 10.1002/jclp.22297 [DOI] [PubMed] [Google Scholar]
- Lei M, & Lomax RG (2009). The effect of varying degrees of nonnormality in structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal, 12(1), 1–27. 10.1207/s15328007sem1201_1 [DOI] [Google Scholar]
- Li C (2013). Little’s test of missing completely at random. The Stata Journal, 13(4), 795–809. 10.1177/1536867X1301300407 [DOI] [Google Scholar]
- Lin J, Chadi N, & Shrier L (2019). Mindfulness-based interventions for adolescent health. Current Opinion in Pediatrics, 31(4), 469–475. 10.1097/MOP.0000000000000760 [DOI] [PubMed] [Google Scholar]
- Little TD (2013). Longitudinal Structural Equation Modeling. New York, NY: Guilford Press. [Google Scholar]
- Long EC, Hill J, Luna B, Verhulst B, & Clark DB (2015). Disruptive behavior disorders and indicators of disinhibition in adolescents: The BRIEF-SR, anti-saccade task, and D-KEFS color-word interference test. Journal of Adolescence, 44, 182–190. 10.1016/j.adolescence.2015.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano JH, Gordillo F, & Pérez MA (2014). Impulsivity, intelligence, and academic performance: Testing the interaction hypothesis. Personality and Individual Differences, 61–62, 63–68. 10.1016/j.paid.2014.01.013 [DOI] [Google Scholar]
- MacCallum RC, Browne MW, & Sugawara HM (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods, 1(2), 130–149. 10.1037/1082-989x.1.2.130 [DOI] [Google Scholar]
- MacCallum R, Lee T, & Browne MW (2010). The issue of isopower in power analysis for tests of structural equation models. Structural Equation Modeling, 17(1), 23–41. 10.1080/10705510903438906 [DOI] [Google Scholar]
- Masters MR, Zimmer-Gembeck MJ, & Farrell LJ (2019). Transactional associations between adolescents’ emotion dysregulation and symptoms of social anxiety and depression: A longitudinal study. The Journal of Early Adolescence, 39(8), 1085–1109. 10.1177/0272431618806053 [DOI] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, & Hilt LM (2009). Emotion dysregulation as a mechanism linking peer victimization to internalizing symptoms in adolescents. Journal of Consulting and Clinical Psychology, 77(5), 894–904. 10.1037/a0015760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezulis A, Salk RH, Hyde JS, Priess-Groben HA, & Simonson JL (2014). Affective, biological, and cognitive predictors of depressive symptom trajectories in adolescence. Journal of Abnormal Child Psychology, 42(4), 539–550. 10.1007/s10802-013-9812-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modecki KL, Zimmer-Gembeck MJ, & Guerra N (2017). Emotion regulation, coping, and decision making: Three linked skills for preventing externalizing problems in adolescence. Child Development, 88(2), 417–426. 10.1111/cdev.12734 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998-2017). Mplus User’s Guide (8th Ed). Muthén & Muthén. [Google Scholar]
- Neumann A, van Lier PAC, Gratz KL, & Koot HM (2010). Multidimensional assessment of emotion regulation difficulties in adolescents using the difficulties in emotion regulation scale. Assessment, 17(1), 138–149. 10.1177/1073191109349579 [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. (2019). Past Year Prevalence of Major Depressive Episode Among U.S. Adolescents (2017) [Figure]. https://www.nimh.nih.gov/health/statistics/major-depression.shtml#part_155031
- Orth U, & Robins RW (2013). Understanding the link between low self-esteem and depression. Current Directions in Psychological Science, 22(6), 455–460. 10.1177/0963721413492763 [DOI] [Google Scholar]
- Perez J, Venta A, Garnaat S, & Sharp C (2012). The Difficulties in Emotion Regulation Scale: Factor structure and associations with nonsuicidal self-injury in adolescent inpatients. Journal of Psychopathology and Behavioral Assessment, 34, 393–404. 10.1007/s10862-012-9292-7 [DOI] [Google Scholar]
- Piko BF, & Pinczés T (2014). Impulsivity, depression and aggression among adolescents. Personality and Individual Differences, 69, 33–37. 10.1016/j.paid.2014.05.008 [DOI] [Google Scholar]
- Preacher KJ, & Coffman DL (2006, May). Computing power and minimum sample size for RMSEA [Computer software]. Available from http://quantpsy.org/.
- R Core Team (2020). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Rieffe C, & De Rooij M (2012). The longitudinal relationship between emotion awareness and internalizing symptoms during late childhood. European Child & Adolescent Psychiatry, 21(6), 349–356. 10.1007/s00787-012-0267-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- RStudio Team (2020). RStudio: Integrated development environment for R. RStudio, PBC. http://www.rstudio.com/ [Google Scholar]
- Ruganci RN, & Gençöz T (2010). Psychometric properties of a Turkish version of the Difficulties in Emotion Regulation Scale. Journal of Clinical Psychology, 66(4), 442–455. 10.1002/jclp.20665 [DOI] [PubMed] [Google Scholar]
- Salk RH, Hyde JS, & Abramson LY (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin, 143(8), 783–822. 10.1037/bul0000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk RH, Petersen JL, Abramson LY, & Hyde JS (2016). The contemporary face of gender differences and similarities in depression throughout adolescence: Development and chronicity. Journal of Affective Disorders, 205, 28–35. 10.1016/j.jad.2016.03.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanger KL, & Dorjee D (2015). Mindfulness training for adolescents: A neurodevelopmental perspective on investigating modifications in attention and emotion regulation using event-related brain potentials. Cognitive, Affective, & Behavioral Neuroscience, 15, 696–711. 10.3758/s13415-015-0354-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saylor KE, & Amann BH (2016). Impulsive aggression as a comorbidity or attention-deficit/hyperactivity disorder in children and adolescents. Journal of Child and Adolescent Psychopharmacology, 26(1), 19–25. 10.1089/cap.2015.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppes G, Suir G, & Gross JJ (2015). Emotion regulation and psychopathology. Annual Review of Clinical Psychology, 11, 379–405. 10.1146/annurev-clinpsy-032814-112739 [DOI] [PubMed] [Google Scholar]
- Silk JS, Steinberg L, & Morris AS (2003). Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development, 74(6), 1869–1880. 10.1046/j.1467-8624.2003.00643.x [DOI] [PubMed] [Google Scholar]
- Skinner EA, & Zimmer-Gembeck MJ (2007). The development of coping. Annual Review of Psychology, 58, 119–144. 10.1146/annurev.psych.58.110405.085705 [DOI] [PubMed] [Google Scholar]
- Sun J (2005). Assessing goodness of fit in confirmatory factor analysis. Measurement and Evaluation in Counseling and Development, 37, 240–256. 10.1080/07481756.2005.11909764 [DOI] [Google Scholar]
- Taren AA, Gianaros PJ, Greco CM, Lindsay EK, Fairgrieve A, Brown KW, Rosen RK, Ferris JL, Julson E, Marsland AL, Creswell JD (2017). Mindfulness meditation training and executive control network resting state functional connectivity: A randomized controlled trial. Psychosomatic Medicine, 79(6), 674–683. 10.1097/PSY.0000000000000466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A, Collishaw S, Pine DS, & Thapar AK (2012). Depression in adolescence. The Lancet, 379(9820), 1056–1067. 10.1016/S0140-6736(11)60871-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toh S, & Hernán MA (2008). Causal inference from longitudinal studies with baseline randomization. The International Journal of Biostatistics, 4(1), 22. 10.2202/1557-4679.1117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turpyn CC, Chaplin TM, Cook EC, & Martelli AM (2015). A person-centered approach to adolescent emotion regulation: Associations with psychopathology and parenting. Journal of Experimental Child Psychology, 136, 1–16. 10.1016/j.jecp.2015.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bereven M-L, Goossens L, Volkaert B, Grassmann C, Wante L, Vandeweghe L, Verbeken S, Braet C (2019). How do I feel right now? Emotional awareness, emotion regulation, and depressive symptoms in youth. European Child & Adolescent Psychiatry, 28, 389–398. 10.1007/s00787-018-1203-3 [DOI] [PubMed] [Google Scholar]
- Weinbach N, Sher H, & Bohon C (2018). Differences in emotion regulation difficulties across types of eating disorders during adolescence. Journal of Abnormal Child Psychology, 46, 1351–1358. 10.1007/s10802/017-0365-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg A, & Klonsky ED (2009). Measurement of emotion dysregulation in adolescents. Psychological Assessment, 21(4), 616–621. 10.1037/a0016669 [DOI] [PubMed] [Google Scholar]
- Whitehead MR, & Suveg C (2016). Difficulties in emotion regulation differentiate depressive and obsessive-compulsive symptoms and their co-occurrence. Anxiety, Stress, & Coping, 29(5), 507–518. 10.1080/10615806.2015.1088523 [DOI] [PubMed] [Google Scholar]
- Wu W, West SG, & Taylor AB (2009). Evaluating model fit for growth curve models: Integration of fit indices from SEM and MLM frameworks. Psychological Methods, 14(3), 183–201. 10.1037/a0015858 [DOI] [PubMed] [Google Scholar]
- Yap MBH, Schwartz OS, Byrne ML, Simmons JG, & Allen NB (2010). Maternal positive and negative interaction behaviors and early adolescents’ depressive symptoms: Adolescent emotion regulation as a mediator. Journal of Research on Adolescence, 20(4), 1014–1043. 10.1111/j.1532-7795.2010.00665.x [DOI] [Google Scholar]
- Zahn-Waxler C, Klimes-Dougan B, & Slattery MJ (2000). Internalizing problems of childhood and adolescence: Prospects, pitfalls, and progress in understanding the development of anxiety and depression. Development and Psychopathology, 12(3), 443–466. 10.1017/S0954579400003102 [DOI] [PubMed] [Google Scholar]
- Zhou J, Witt K, Chen C, Zhang S, Zhang Y, Qiu C, Cao L, Wang X (2014). High impulsivity as a risk factor for the development of internalizing disorders in detained juvenile offenders. Comprehensive Psychiatry, 55(5), 1157–1164. 10.1016/j.comppsych.2014.03.022 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


