Abstract
Age-related macular degeneration (AMD) remains a leading cause of modifiable vision loss in older adults. Chronic oxidative injury and compromised antioxidant defenses represent essential drivers in the development of retinal neurodegeneration. Overwhelming free radical species formation results in mitochondrial dysfunction, as well as cellular and metabolic imbalance, which becomes exacerbated with increasing age. Thus, the depletion of systemic antioxidant capacity further proliferates oxidative stress in AMD-affected eyes, resulting in loss of photoreceptors, neuroinflammation, and ultimately atrophy within the retinal tissue. The aim of this systematic review is to examine the neuroprotective potential of the xanthophyll carotenoids lutein, zeaxanthin, and meso-zeaxanthin on retinal neurodegeneration for the purpose of adjunctive nutraceutical strategy in the management of AMD. A comprehensive literature review was performed to retrieve 55 eligible publications, using four database searches from PubMed, Embase, Cochrane Library, and the Web of Science. Epidemiology studies indicated an enhanced risk reduction against late AMD with greater dietary consumption of carotenoids, meanwhile greater concentrations in macular pigment demonstrated significant improvements in visual function among AMD patients. Collectively, evidence strongly suggests that carotenoid vitamin therapies offer remarkable synergic protection in the neurosensory retina, with the potential to serve as adjunctive nutraceutical therapy in the management of established AMD, albeit these benefits may vary among different stages of disease.
Keywords: carotenoids, macular pigment, macular pigment optical density, MPOD, lutein, zeaxanthin, meso-zeaxanthin, age-related macular degeneration, retinal neurodegeneration
1. Introduction
Age-related macular degeneration (AMD) is the leading cause of irreversible blindness among older adults in developed countries, affecting roughly one in eight individuals aged 60 years or greater [1,2,3,4]. Comprehensive reports estimate that 200 million people currently live with AMD globally, with this aggregate expected to increase further and approach 300 million by 2040 [3]. Similar rising trends in the U.S. are expected to reach 5.4 million people by the year 2050 [1,4,5]. Although the majority of these are of Caucasian descent, the disease is not limited to individuals of Caucasian origin; Asian, Hispanic, and African-American populations tend to develop intermediate dry AMD and wet polypoidal choroidal vasculopathy with greater incidence [5,6,7]. The projected growth in prevalence among adults developing noncommunicable eye diseases, such as AMD, can be attributed to the demographic transition consistent with an aging global population [1,3,8,9,10]. Due to its chronic nature, wherein this incurable disease requires steady long-term management, AMD has become, and will remain, a public health challenge for both high- and low-income countries, with considerable socio-economic implications and rises in healthcare expenditures [1,2,3,8,9,10,11,12,13,14].
Aging remains one of the primary risk factors in AMD [1,4,9,15]. While cellular senescence is inherent to biological aging, these perturbations in photoreceptor cells and retinal pigment epithelium (RPE) are thought to bring about the neurodegenerative onset characteristic of age-onset maculopathy. Additional non-modifiable risk factors include sex, confirmed family history of AMD, and strong genetic factors that may further predispose individuals to this condition [1,5,12,16,17,18,19,20,21]. Genetic variants associated with complement factor H (CFH) and AMD susceptibility gene 2 (ARMS2) are well-established risk factors for the development and progression of AMD [16,17,18,19,20,21,22,23,24,25] (single nucleotide polymorphisms that are found on chromosomes 1q31 and 10q26, respectively). Conversely, modifiable risk factors for AMD include dietary behaviors, smoking status, cardiovascular disease, as well as metabolic comorbidities [5,26,27,28,29,30]. Among these, individuals who currently smoke (and past-smokers) carry significantly greater risk of incident AMD [26,27,28,31].
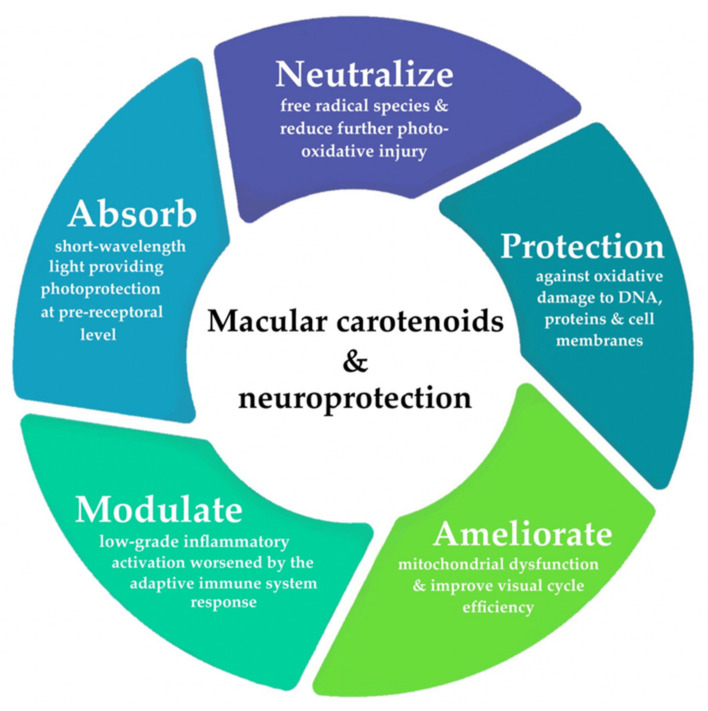
The etiopathogenesis of AMD is complex and multifactorial. It is postulated that early and intermediate stages of maculopathy are predominated by oxidative stress and low-grade inflammatory activation in aging retinae [32,33,34,35,36,37,38,39,40,41]. Figure 1 provides a summary of the neuroprotective mechanisms provided by macular carotenoids. A comprehensive review of the precise molecular processes, by which carotenoids offer protection against photo-oxidative damage, has been discussed in detail elsewhere [42]. As a consequence of its extremely high metabolic activity and constant exposure to light, the outer retina is known to be particularly vulnerable to photo-oxidative injury and mitochondrial dysfunction, prompting the overproduction of free radical species [42,43,44,45,46]. A growing body of evidence implicates that compromised antioxidant capacity may also serve a crucial role in AMD pathology, a sequela, which occurs predominantly in response to the chronic cycles of sustained oxidative stress, paired with the concomitant depletion of endogenous antioxidants [42,43,46,47,48]. Local inhibition of these antioxidant defense mechanisms (to counteract the accumulation of toxic byproducts and cellular debris) plays a significant role in perpetuating subsequent neurodegenerative damage onto the surrounding tissues through immunostimulatory activity [35,40,41,43,46]. In fact, outer retinal lesions originating from oxidative insult have been shown to mediate a para-inflammatory state or an adaptive immune response to dysregulated complement activation [32,33,34,35,36,37,38,40,41,45,49]. This interdependence between cellular senescence and redox imbalance likely represents essential facets contributing to neurodegenerative onset and disease progression in AMD.
Figure 1.
Overview of the neuroprotective mechanisms of xanthophylls lutein, zeaxanthin, and meso-zeaxanthin in the central retina.
The body’s intrinsic homeostatic mechanisms for maintaining redox control are comprised of both exogenous and endogenous antioxidant activity for neutralizing free radical species [42,43,46,47,48]. The mainstay of preventative nutritional therapies is aimed at the augmentation of exogenous antioxidant defenses through oral supplementation containing nutraceuticals and micronutrients. In particular, xanthophyll carotenoids possess unique properties, serving as potent antioxidants and anti-inflammatory mediators in the retina, and have been demonstrated to benefit the prevention of neurodegenerative retinopathies, such as AMD and diabetic eye disease [42,43,50,51,52,53]. Greater dietary intake of xanthophylls, via carotenoid supplementation, has been well-documented to offer clinically meaningful benefits in visual performance, in both healthy and diseased states [54,55,56,57,58]. However, the comprehensive neuroprotective capacity, afforded by macular carotenoids in clinical management of AMD, has not been thoroughly discussed. Hence, the purpose of this systematic review concentrates on summarizing the available evidence from observational studies and randomized controlled trials, reporting on carotenoid lutein, meso-zeaxanthin, and zeaxanthin (only in patients with AMD).
1.1. Age-Related Macular Degeneration
Traditionally, color fundus photography and slit lamp biomicroscopy have been the mainstay for the ophthalmic examination of fundus lesions associated with AMD [15,59,60]. Several disease classification systems have been developed over the years, from population studies [61,62,63] and clinical-based trials, of which the Age-Related Eye Disease Study (AREDS) clinical severity scale (Table 1) and its simplified severity scale are most notable [64,65,66,67]. However, inconsistency in disease terminology and ambiguous definitions, relating to the severity of maculopathy, highlight an overwhelming unmet clinical need. Thus, it is highly recommended for all those working in this field to adopt the single diagnosis of AMD proposed by the Beckman classification (Table 2) [68], which is then further classified according to disease severity, in agreement with AREDS [64,65,66,67].
Table 1.
AREDS clinical severity scale of age-related macular degeneration (AMD) [65].
| Category | Age-Related Eye Disease Study (AREDS) Classification |
|---|---|
| 1 | No drusen, or non-extensive small drusen only in both eyes |
| 2 | Extensive small drusen, non-extensive intermediate drusen, or the presence of pigment abnormalities in at least one eye |
| 3 | Extensive intermediate drusen, large drusen, or non-central geographic atrophy in at least one eye |
| 4 | Advanced AMD as defined by at least one of the following: geographic atrophy, retinal pigment epithelial detachment in one eye, choroidal neovascularization, or scars of confluent photocoagulation; or visual acuity less than 20/32 associated with lesions from non-advanced age-related macular degeneration, including large drusen in the fovea, in only one eye |
Abbreviations: AMD, age-related macular degeneration.
Table 2.
Beckman Classification System of AMD.
| Beckman Clinical Classification [68] | |||
|---|---|---|---|
| AMD Classification 1 | Drusen | Pigmentary Abnormalities 2 | Additional Features |
| No apparent aging | None | None | n/a |
| Normal aging changes | Small (≤63 μm) | None | n/a |
| Early AMD | Medium (>63 μm and ≤125 μm) | None | n/a |
| Intermediate AMD | Large (>125 μm) | Abnormalities present 2 | n/a |
| Late AMD | Large (>125 μm) | Abnormalities present 2 | Neovascular AMD and/or any geographic atrophy |
1 AMD classification based on lesions, assessed within 2 disc diameters of the fovea in either eye. 2 AMD pigmentary abnormalities defined as any hyper- or hypo-pigmentary abnormalities associated with at least some medium drusen but not associated with known disease entities. Abbreviations: AMD, age-related macular degeneration; n/a: not applicable.
Retinal drusen and basal laminar deposits are sine qua non features of early AMD [69,70,71,72]. Drusen is formed by the exudative accumulation of various cellular waste products and atherogenic debris (>40% of drusen volume) [69,70,71,72,73]. Notably, the detection of subretinal drusenoid deposits above the RPE, also known as reticular pseudodrusen, are correlated with a two-fold increase in the risk of developing late-stage geographic atrophy [72,74]. Further retinal injury is evident by the presence of pigmentary changes (depigmentation or hyperpigmentation) found in the RPE, indicating abnormalities associated with intermediate AMD [15,70]. Often, these more preliminary stages of AMD do not carry obvious changes in visual function or may present elusive symptoms of mild distortion in central vision, with greater difficulty under low light conditions, such as reading or seeing at night [15,65]. Some reports suggest that dark adaptation dysfunction, marked by impaired recovery of light sensitivity mediated by rod photoreceptors under mesopic conditions, may be one of the earliest indications of AMD onset [75,76,77,78,79,80].
According to its pathophysiology, late AMD can be divided into neovascular AMD and geographic atrophy (GA), based on distinct clinical manifestations [15]. Neovascular proliferations are characterized in accordance with the compartment wherein the choroidal neovascularization complex occupies, and the formation of chorioretinal anastomoses is found upon fluorescein angiography. With the advent of optical coherence tomography (OCT) imaging modalities, the anatomical classification of neovascular subtypes is made possible, which includes: type 1 neovascularization (NV) for submacular lesions confined below the RPE, type 2 NV for subretinal lesions found in the space between the photoreceptor layer and RPE, and type 3 NV for intraretinal lesions found within the retinal layers [15,81,82,83,84,85,86,87,88,89]. Subsequently, the aberrant angiogenesis of fragile vasculature is often accompanied by the presence of a retinal hemorrhage, a hard exudate, detachments of the RPE, and chorioretinal fibrotic scarring [15,82,83,84,87,89,90]. On the other hand, non-neovascular complications, seen in GA, are characterized by the demarcated regions of hypopigmentation, in consequence of the cumulative degeneration of the outer neurosensory retina, RPE, and choriocapillaris [15,64,68,90,91,92]. Perilesional hyperpigmentation delineates areas of ongoing atrophy and the confluent superimposition of RPE cells [93,94,95]. Both forms of late AMD result in severe visual defects, such as the formation of central scotoma, while peripheral vision remains relatively intact. Neovascular AMD often develops quite rapidly, leading to acute vision loss within a relatively short period of time (days to months); meanwhile, atrophic lesions progress more gradually and may take years, or decades, for symptoms to manifest [15].
Given the increasing prevalence and substantial implications on quality of life, the detection of these phenotypic lesions in each stage of AMD is of profound importance for disease management and clinical screening. Thus, apposite surrogates of AMD pathology will likely serve a cardinal role in preventing the onset of extensive neurodegeneration within outer retinal layers and irreversible loss of photoreceptor cells.
1.2. Macular Pigment Optical Density in AMD—Background
The xanthophyll carotenoids lutein and zeaxanthin, as well as an isomer of lutein meso-zeaxanthin, serve an important role in sustaining the integrity of the retina concomitant with optimizing central visual acuity [42,96,97]. Collectively, these lipid-soluble carotenoids comprise the macular pigment, which forms a yellow spot that is seen during ophthalmoscopy. A recent imaging study determined that the spatial profiles of lutein and zeaxanthin are both localized in the fovea, as previously described [42,96,97,98,99,100]; however, only zeaxanthin was primarily concentrated in the inner plexiform (IPL), outer plexiform (OPL), and outer nuclear layers [98]. Meanwhile, lutein distribution was more dispersed throughout the macula, in reduced concentrations, when compared to foveal zeaxanthin levels [98]. Humans are unable to naturally synthesize lutein and zeaxanthin [97,101,102]; therefore, they must be acquired through the dietary consumption of foods, such as spinach, kale, and cruciferous green leafy vegetables, as well as corn and egg yolks [42,97,103,104]. On the other hand, meso-zeaxanthin is a biochemical isomer, also found in the macula, that is configured from lutein metabolism via RPE65 isomerase activity [105,106] within the retinal pigment epithelial cells [42,97,98,101,107]. A growing body of evidence indicates that the depletion of these carotenoids, marked by low macular pigment optical density (MPOD), may be a clinical biomarker associated with greater risk of incident retinopathy and visual dysfunction [42,43,108,109,110].
Numerous reports have shown clinical benefits, by raising the levels of xanthophylls in the retina through dietary supplementation, thus, adjunctive carotenoid vitamin therapy may offer enhanced neuroprotection by augmenting MPOD and subsequently preventing further injury [42,96,97,101,107,111,112,113,114,115,116,117,118,119,120,121,122]. Higher levels of MPOD are thought to preserve retinal tissue, specifically the layers containing photoreceptors in the fovea, through two primary mechanisms: (1) serving as an innate optical filter against blue light and (2) as protective antioxidants, by neutralizing free radicals and reducing consequent oxidative injury [97,103,108,112,123,124,125]. The peak wavelength of the absorption spectrum of the macular (~460 nm) attenuate proliferation of reactive oxygen species is generated by photosensitizers, such as rod and cone cells, exposed to a range of visible blue light (400–500 nm) [96,123,126]. This optical filtration is particularly significant, as short-wavelength (blue) light is highly reactive and has the capacity to exacerbate photo-oxidative degeneration in the most sensitive layers of the neurosensory retina [42,97,123,124,125,126,127].
1.3. Measuring MPOD
While several imaging techniques are used to measure MPOD non-invasively within optometry settings, each possess their own set of advantages and disadvantages. The abilities and shortcomings of the MPOD measuring techniques are outlined in more detail elsewhere [42,95,99,103,127,128,129,130,131,132,133,134,135,136]. In brief, the standard routine methods of heterochromatic flicker photometry (HFP) and customized flicker photometry (cHFP) [42,99,103,128,129,130,131] utilize a psychophysical approach, wherein the determination of macular pigment levels is reliant upon subjective participation [137,138,139]. Objective techniques of fundus reflectometry [114,140,141,142,143,144], autofluorescence (AFI) [95,132,134,135,145], and resonance Raman spectroscopy [98,146,147,148,149] collect MPOD measurements, utilizing physical properties of light within the retina [42,95,103,128,133,136,150].
1.4. MPOD Biomarkers in Clinical AMD
There is an overwhelming need for developing improved biomarkers that underscore the diverse pathology and subtypes found in patients with AMD. While current treatments have shown success for late neovascular AMD, there are a lack of proven therapies involving the mechanisms underlying early/intermediate stages and late atrophic stages of disease; in such cases, AMD develops, in consequence of the compounding cycles of oxidative stress and para-inflammation [151,152,153]. Therefore, it is critical that therapeutic targets are aimed at ameliorating the perturbations contributing to lesion formation and preventing irreversible retinal neurodegeneration. Biomarkers are important tools, with the capacity to significantly aid the development of novel therapeutics, in addition to investigating the efficacy and overall safety of available treatments [154,155,156,157]. Given that a single biomarker may be appropriate for different clinical utility, it is deemed necessary to clearly define the situation-specific context of how a particular biomarker will be used accordingly [154,155,156].
While advancements in multimodality imaging have improved the prognosis for diagnosing retinal abnormalities, these modalities have also enabled the measurement of macular pigment status, to serve as a biomarker in multiple settings for AMD. It has been well-documented that MPOD levels are substantially reduced in AMD patients [107,110,158,159,160,161,162,163,164], which may be explained, at least in part, to similar risk factors shared between them [5,21,31,107,110,158,159,160,161,162,163,164,165,166,167,168]. Diagnostic assessment, incorporating MPOD measurements, in conjunction with standard fundoscopic imaging, may offer unique clinical insight into the current state of the individual’s retinal health. In fact, macular pigment levels represent the local equilibrium between pro-oxidant stressors and antioxidant defenses in the retina, which can be attributed to its slow biological turnover [42]. To this accord, MPOD measurement may function as: (1) a prognostic biomarker to appraise the health of neuroretinal layers, (2) a susceptibility/risk biomarker for screening those at risk of incident AMD, and (3) a pharmacodynamic/response biomarker to determine the clinical benefits of carotenoid vitamin therapy in AMD.
As a prognostic biomarker, MPOD levels may be used to monitor the progression of neurodegenerative changes in the photoreceptors and ganglion cells among patients with early or intermediate AMD. One study found that macular pigment levels were positively correlated with central retinal thickness, along with the neural volume of the ganglion cell layer (GCL), inner plexiform layer, and outer nuclear layer [169]. Previous reports have demonstrated differential morphology changes on OCT within the outer retinal layers in patients with early AMD, including the thickness and volume of the photoreceptor layer, as well as the RPE-Bruch’s membrane complex [71,92,170,171,172,173,174,175]. Similarly, inner retinal alterations are also found in the macular ganglion cell complex, comprised of the IPL, ganglion cell layer, and nerve fiber layer [175,176,177,178,179,180], which correspond to the dendrites, cell bodies, and axons of the neurosensory ganglion cells, respectively. Thus, MPOD depletion may serve to help prognosticate visual outcomes before severe impairment develops in early/intermediate AMD patients.
Given its bilateral nature, AMD fellow eyes may be considered to represent the pre-disease condition, in the absence of early retinal lesions, based on the incidence of fellow eye involvement, which increases significantly over time [158,159,181,182]. Recently, Nagai et al. determined the risk of late AMD fellow eyes developing incident maculopathy was significantly associated with the combination of reduced MPOD (<0.65 density units (DU), measured by HFP) and photoreceptor outer segment length (<35 μm on OCT) [183]. These results suggest MPOD screening may be an important susceptibility/risk biomarker used for the early detection of subclinical neurodegeneration among older adults and eyes with greater risk of developing AMD.
Furthermore, serial measurement of MPOD is used as pharmacodynamic/response biomarkers in randomized clinical trials to evaluate the protective benefits of carotenoid supplementation in patients with AMD, as discussed in more detail below. In summary, MPOD levels could be used to function as susceptibility/risk, monitoring, and pharmacodynamic/response biomarkers, in accordance with FDA-NIH guidelines [154,155].
2. Materials and Methods
This systematic review was conducted in accordance with the reporting guidelines outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [184]. The study was registered on PROSPERO (registration number: 269373).
2.1. Literature Search and Selection Strategy
We conducted a comprehensive literature review in PubMed, Embase, the Cochrane Library, and the Web of Science, utilizing a combination of the follow keywords and their variations in the search query: lutein, zeaxanthin, meso-zeaxanthin, carotenoids, macular pigment, macular pigment optical density, MPOD, age-related macular degeneration, AMD, and neurodegeneration. We extracted all relevant publications from clinical studies that published data on the relationship between MPOD/carotenoids (including lutein, and/or zeaxanthin, and/or meso-zeaxanthin) and AMD, prior to 25 July 2021. Records retrieved from the initial search were vetted individually, by two authors (PGD and DWL), for proper selection criteria and then further examined using English titles and abstracts. We carefully searched through the qualifying publications’ reference lists and cited references to ensure that all relevant material was included in this review. All eligible, full-text publications were individually examined, by the same two authors (PGD and DWL), for the appropriate inclusion and exclusion criteria, discussed below; any disagreements were resolved through discussions with the third and fourth authors (DLG and RBR).
2.2. Study Selection Criteria
Observational clinical studies that adhered to the following criteria were included in this review: (1) epidemiological studies examining the association between the risk of incident AMD (including early or late AMD) and xanthophyll carotenoids, measured via dietary intake/consumption, serum concentrations, and/or by validated technique to quantify macular pigment optical density (MPOD) levels; (2) studies including adults with or without established AMD; and (3) original peer-reviewed publications available in English.
Prospective randomized clinical trials included in this review satisfied the following criteria: (1) interventional trials, investigating the effects of carotenoid vitamin therapy containing lutein, and/or zeaxanthin, and/or meso-zeaxanthin on clinical outcomes in eyes with AMD; (2) studies reporting on xanthophyll carotenoid levels in serum and/or by validated MPOD technique; (3) studies reporting on visual outcome measures, in response to carotenoid treatment; (4) must include adults with the presence of AMD; and (5) peer-reviewed, original research.
2.3. Data Extraction, Reliability and Risk of Bias Assessment
The authors carefully followed the PRISMA reporting guidelines, as closely as possible, as outlined above [184]. The risk of bias was assessed independently, by two authors (PGD and DWL), using the standardized metrics established to evaluate the interventional studies included in the present review. We used the Cochrane Collaboration’s tool for the assessment of risk of bias for randomized trials, which consists the following domains: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other sources of bias [185].
3. Results
3.1. Search and Selection of Eligible Studies
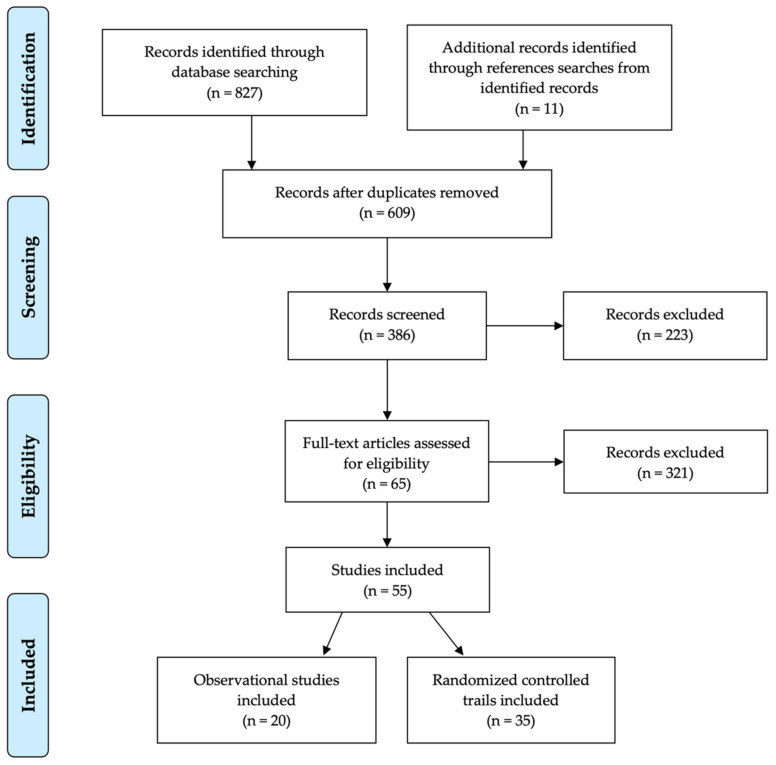
In total, 827 entries were collected from the primary search, using only scientific databases. After removing the duplicate entries and retrieving 11 additional records from the reference searches, a total of 609 studies remained for the further screening of titles and abstracts. From these, 223 entries were eliminated for further screening, based on the manuscript type, with an additional 321 records being excluded, in accordance with the inclusion/exclusion criteria described above. Finally, 65 eligible publications were selected for full-text assessment, of which 55 studies were included in the final evaluation (Figure 2): 20 observational clinical studies [16,51,109,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202] and 35 interventional clinical trials [50,53,115,117,119,120,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226,227,228,229,230,231].
Figure 2.
PRISMA flow chart, outlining the systematic review of xanthophyll carotenoids in the management of AMD.
3.2. Carotenoids and Risk of AMD (Observational Studies)
Currently, dietary modifications remain the mainstay of therapeutic strategies, to potentially delay or prevent both the development and progression of AMD. The Age-Related Eye Disease Study (AREDS) is considered to be among the most influential large-scale clinical trials highlighting the relationship between dietary antioxidants and the risk of AMD progression [181]. Reports indicate that regular consumption of the AREDS micronutrient formula (containing vitamin C, vitamin E, beta-carotene, and zinc) offered modest benefits, reducing the risk of late AMD progression by up to 25% during a five-year follow-up with at risk patients [181]. In aging retinae, it is believed that the depletion of endogenous and exogenous antioxidants represents a critical driver in exacerbating neurodegenerative mechanisms. In fact, there is substantial evidence in favor of the neuroprotective association, between greater dietary consumption of carotenoid nutraceuticals, increased lutein and zeaxanthin concentrations in serum, and AMD prevention. A summary of these observational epidemiology studies is outlined in Table 3.
Table 3.
Epidemiology studies on AMD risk associated with dietary intake and/or serum levels of lutein and zeaxanthin.
| Authors (Year) | Study Name | Participants | Follow-Up | Assessment of L/Z | Results |
|---|---|---|---|---|---|
| Seddon (1994) [197] | EDCCS | 356 AMD patients, 520 controls in USA; aged 55–80 years | - | Dietary L/Z | Highest quintile of L/Z intake, such as spinach and collard greens, strongly associated with reduced risk of late AMD |
| VandenLangenberg (1998) [201] | Beaver Dam Eye Study | 1709 individuals in USA; aged 43–84 years | 5 years | Dietary L/Z | No significant association reported between incident large drusen and dietary intake |
| Mares-Perlman (2001) [194] | NHANES III | 8596 individuals in USA; aged ≥40 years | - | Dietary L/Z | Significantly lower risk of pigmentary abnormalities and late AMD in highest L/Z quintiles |
| Snellen (2002) [198] | - | 72 AMD patients, 66 controls in Netherlands; aged ≥60 years | - | Dietary L/Z | Low dietary intake significantly associated with higher risk of neovascular AMD |
| Cho (2004) [188] | NHS and HPFS | 77,562 female and 40,866 male health professionals in USA; aged ≥50 years | 18 years; 12 years |
Dietary L/Z | No significant association between relative risk of age-related maculopathy and vegetable consumption or carotenoid intake |
| Van Leeuwen (2005) [200] | The Rotterdam Study | 4170 individuals in Netherlands; aged 55–95 years | 8 years | Dietary L/Z | No significant association reported between dietary L/Z intake and incident AMD |
| Moeller (2006) [196] | CAREDS | 1787 women in USA; aged 50–79 years | 7 years | Dietary L/Z | Protective association among adult women (<75 years) with stable dietary intake and no history of chronic disease |
| AREDS Research Group (2007) [51] | AREDS | 4159 AREDS participants in USA; aged 60–80 years | - | Dietary L/Z | Top quintile of dietary L/Z inversely associated with large drusen, neovascular AMD, and geographic atrophy |
| Tan (2008) [199] | Blue Mountains Eye Study | 2454 individuals in Australia; aged 49–93 years | 10.5 years | Dietary L/Z | Greater intake of L/Z saw reduced risk developing soft/reticular drusen and neovascular AMD progression |
| Cho (2008) [187] | NHS and HPFS | 71,494 female and 41,564 male health professionals in USA; aged 50–79 years | 18 years; 16 years |
Dietary L/Z | A non-linear, inverse association seen among top quintiles of L/Z intake and neovascular AMD in both cohorts |
| Ho (2011) [16] | The Rotterdam Study | 2167 individuals in Netherlands; aged ≥55 years | 8 years | Dietary L/Z | Top tertile of L/Z intake significantly reduced incident early AMD in those with greater genetic risk |
| Wu (2015) [202] | NHS and HPFS | 63,443 female and 38,603 male health professionals in USA; aged 50–90 years | 26 years; 24 years |
Dietary L/Z | Greater consumption of cooked spinach (0.5 cup, >1 serving/wk) inversely associated with intermediate AMD. Late AMD risk significantly lowered by up to 40% with higher L/Z intake |
| Arslan (2019) [186] | - | 100 AMD patients, 100 controls in Turkey; aged ≥50 years | - | Dietary L/Z | Non-significant association observed between serum L/Z |
| EDCCS Group (1993) [191] | EDCCS | 421 AMD patients, 615 controls in USA; aged 55–80 years | - | Serum L/Z | Protective association with greater serum L/Z levels and risk of neovascular AMD |
| Mares-Perlman (1995) [193] | Beaver Dam Eye Study | 167 AMD patients, 167 controls in USA; aged 43–84 years | - | Serum L/Z | No overall association between serum L/Z and risk of late AMD |
| Gale (2003) [192] | - | 380 individuals in Sheffield, United Kingdom; aged ≥60 years | - | Serum L/Z | Serum Z strongly associated with risk of incident early and late AMD |
| Dasch (2005) [189] | MARS | 586 AMD patients, 182 controls in Germany; aged 59–82 years | - | Serum L/Z | No significant association reported between serum L/Z levels |
| Delcourt (2006) [190] | POLA | 640 individuals in Sète, France; aged ≥60 years | - | Serum L/Z | Highest combined serum L/Z has significantly reduced risk |
| Michikawa (2009) [195] | - | 722 individuals in Karabuchi Town of Takasaki City, Japan; aged ≥65 years | - | Serum L/Z | No significant association found between serum L/Z |
| Zhou (2011) [109] | - | 174 AMD patients, 89 controls in China; aged 50–88 years | - | Serum L/Z | Significant inverse association between serum Z and neovascular AMD |
Abbreviations: L, lutein; Z, zeaxanthin; AMD, age-related macular degeneration; EDCCS, Eye Disease Case-Control Study; NHANES III, The Third National Health and Nutritional Examination Study; NHS, Nurse’ Health Study; HPFS, Health Professionals Follow-up Study; CAREDS, Carotenoids in Age-Related Eye Disease Study; AREDS, Age-Related Eye Disease Study; MARS, Muenster Aging and Retina Study; POLA, Pathologies Oculaires Liées à l’Âge Study.
It is evident that the relationship between dietary behaviors, lifestyle choices, and the risk of AMD is complex and multifaceted, wherein unhealthy lifestyles often carry an increased risk of consequent disease [232]. Among older adults, early lifestyle modifications for the systemic management of metabolic syndrome is vital for slowing disease progression, as it also represents another risk factor [65,233]. Additionally, the National Eye Institute encourages greater consumption of leafy green vegetables to lower AMD risk [1]. Multiple longitudinal cohort studies have demonstrated greater consumption of foods such as spinach, kale, and collard greens on a regular basis carry significant protection against incident late AMD [51,187,194,196,197,199]. In fact, these green leafy vegetables, from the cruciferous Brassica oleracea cabbage species, are recognized as an excellent sources of xanthophyll carotenoids, lutein and zeaxanthin [197,234,235,236,237]. A meta-analysis by Ma et al. found that individuals with the highest levels of carotenoid intake saw a significant reduction in the risk of late AMD (pooled relative risk (RR) = 0.74; 95% confidence interval (CI): 0.57–0.97) and saw a 32% risk reduction for neovascular AMD (RR = 0.68; 95% CI: 0.51–0.92) [238]. Using data from the AREDS cohort, the calculated odds ratios (OR) from one case-control study seemed to corroborate these findings, when comparing the highest versus lowest quintiles of carotenoid intake. Greater dietary consumption of lutein and zeaxanthin offered an enhanced protection against neovascular AMD (OR = 0.65; 95% CI: 0.45–0.93), geographic atrophy (OR = 0.45; 95% CI: 0.24–0.86), and large, or extensive, intermediate drusen (OR = 0.73; 95% CI: 0.56–0.96) [51]. Evidence from a large cohort of studies largely seemed to implicate that the protective benefits of greater carotenoid intake may be confined to late AMD. However, one report, from the population-based Rotterdam Study, found that higher dietary antioxidants (including lutein and zeaxanthin) may significantly attenuate early AMD incidence conferred by genetic risk variants [16,25]. These results are encouraging, given that the AMD risk, among carriers of the CFH Y402H variant, increased by up to 11-fold, and those with the ARMS2 (LOC387715 A69S) variant carried up to 15-times greater risk [16,17,18,19,20,21,22,23,24,25]. One school of thought suggests that xanthophyll carotenoids afford synergistic neuroprotection against these risk alleles by limiting the overactivation of the complement system concomitant with mitochondriotropic augmentation, respectively [239,240,241,242]. Furthermore, these findings highlight the importance of stable dietary behaviors, involving the frequent consumption of nutraceuticals rich in lutein and zeaxanthin, for the management of established AMD.
Observational studies investigating the relationship between the serum levels of macular carotenoids provide some evidence of the protective benefits against age-related maculopathy [109,190,191,192]. The 1993 Eye Disease Case-Control Study first reported that greater levels of lutein and zeaxanthin in serum were inversely associated with the risk of neovascular AMD [191]. However, a 1995 analysis from the Beaver Dam Eye Study was unable to reproduce these findings and did not find serum levels to correlate with late AMD prevention [193]. Variation among these initial reports may be explained, at least in part, by differences in the ethnogeography of the sample, and sample size, whereby influencing the interpretability of these results. Moreover, serum analyses from population-based cohorts in the United Kingdom, France, and China seemed to corroborate the protective association with systemic increases of lutein and zeaxanthin concentrations in circulation [109,190,192]. Surprisingly, two of these studies illustrated that the serum levels of zeaxanthin were strongly associated with the risk of incident AMD (both early and late AMD) [109,192]. It is well known that differential dietary habits have significant implications on their absorption from food matrices, as well as subsequent concentrations within the plasma [235,243,244,245,246,247,248,249,250], and may, therefore, account for some of the inconsistency among reports.
It is important to note that similar biological mechanisms, which greatly reduce the bioavailability of lutein and zeaxanthin, are also involved with established AMD risk factors. The cumulative effect of compromised antioxidant capacity, in consequence of prolonged oxidative injury, is thought to create an overwhelming, neurodegenerative environment. Mitochondrial dysfunction and photo-oxidation are known to trigger the proliferation of premature cellular senescence in RPE, which subsequently triggers the pathogenic cascade of AMD development [32,38,49,239,240,241,242,251,252,253,254,255,256,257,258,259,260,261,262]. Moreover, in diabetic retinopathy, the underlying causes of metabolic syndrome have been shown to substantially compromise the assimilation and transport of dietary carotenoids [30,43,263,264,265,266,267,268,269,270,271,272,273,274,275,276,277,278,279,280,281,282]. Metabolic perturbations, such as obesity, insulin resistance, and chronic hyperglycemia promote atherogenic metabolic imbalance, which further contributes to macular pigment depletion [102,250,276,277,278,279,280,281,282,283,284,285]. Therefore, low MPOD levels likely represent an essential factor in AMD development.
Conversely, some observational studies were unable to confirm these benefits [186,187,189,193,195,201]. For instance, the Beaver Dam Eye Study found that neither dietary intake nor serum carotenoid levels were significantly correlated with AMD [193,201], while the Muenster Aging and Retina Study (MARS), in Germany, also observed a non-statistically significant association between plasma concentrations and age-related maculopathy [189]. Inconsistency among large-scale cohort studies may be attributed, at least in part, to the persistent challenges of investigating insidious neurodegenerative conditions, such as AMD. Etiologically relevant exposures involve a combination of lifestyle choices and dietary habits, culminating over years or decades before the date of diagnosis, as clinical manifestations often present themselves only after incurring extensive damage to the retina. Thirteen out of twenty (13/20) reports from several large-scale epidemiological studies demonstrated the effects of xanthophylls in protecting against the progression of AMD [16,51,109,187,190,191,192,194,196,197,198,199,202]. Thus, it is appropriate to summarize that the majority of the observational studies discussed herein advocate the benefits of xanthophyll carotenoids in AMD.
3.3. Carotenoids in the Management of AMD (Interventional Studies)
Given the effectiveness of the AREDS supplement in slowing the course of AMD progression, randomized clinical trials have investigated the efficacy of carotenoid vitamin therapy, supplemented with or without additional antioxidants and micronutrients. It is important to note that the original AREDS formulation did not include xanthophyll carotenoids (i.e., lutein or zeaxanthin) [65]; instead, it contained β-carotene, which belongs to the subclass of provitamin A carotenes [286]. However, in response to the discovery that β-carotene may correlate with a greater risk of developing lung cancer among cigarette smokers [287,288], the Age-Related Eye Disease Study 2 (AREDS2) modified the original formula by removing β-carotene and substituting with lutein and zeaxanthin [50,289]. Primary analysis from the AREDS2 trial suggested xanthophyll supplementation did not offer further benefits against the rate of AMD progression, in comparison to the original AREDS formula [50]. However, secondary analysis showed that lutein and zeaxanthin supplementation significantly improved protection against late AMD (hazard ratio (HR): 0.82; 95% CI: 0.69–0.96) and particularly against neovascular AMD (HR: 0.78; 95% CI: 0.64–0.94), when substituted for β-carotene in the AREDS formulation [203]. The risk reduction was most significant among those with intermediate AMD lesions (bilateral large drusen) at baseline; direct comparisons showed HRs of 0.76 (95% CI: 0.61–0.96; p = 0.02) for developing late AMD and 0.65 (95% CI: 0.49–0.85; p = 0.002) for neovascular AMD [203]. From these reports, the AREDS2 suggests that supplementation with lutein and zeaxanthin could offer enhanced protection and are well-suited for therapeutic management using nutraceuticals in patients with established AMD, particularly in lieu of β-carotene.
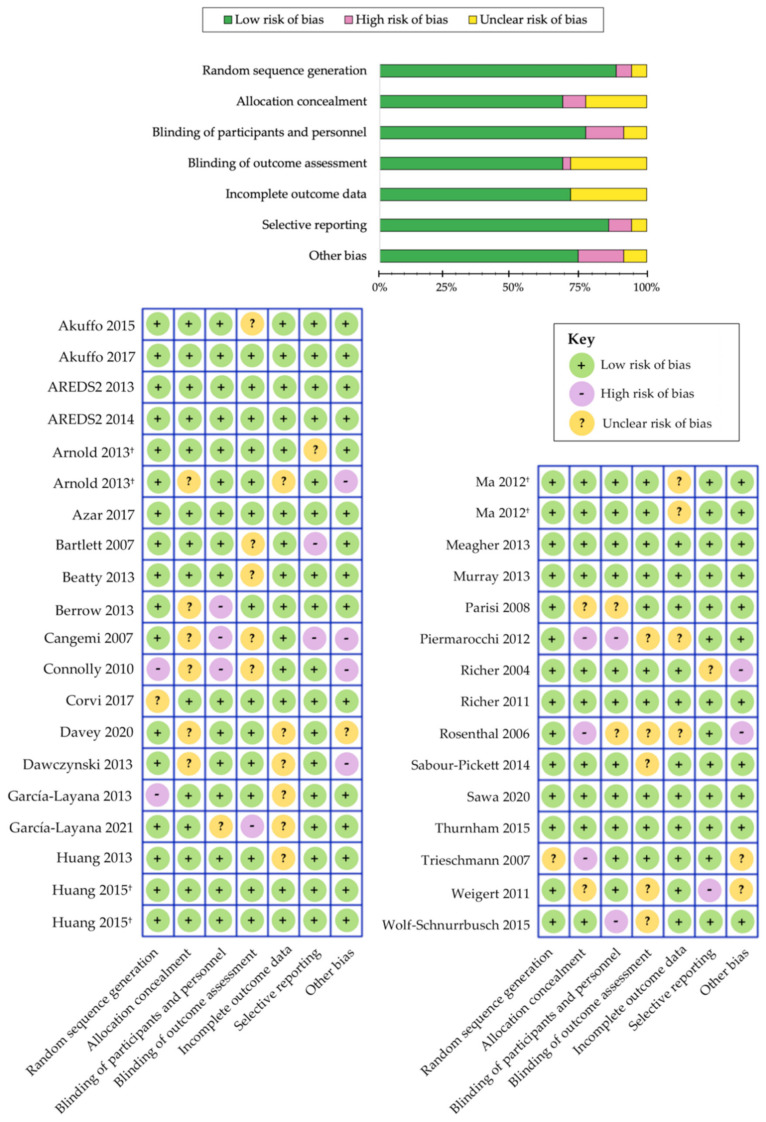
Numerous randomized clinical trials have been extremely consistent in demonstrating that xanthophyll carotenoid supplementation can greatly improve their concentrations in serum [50,115,119,204,205,206,207,213,217,219,221,222,227,229,231] and within the retinal tissue (i.e., MPOD) among patients with AMD [56,115,117,119,120,204,205,206,210,213,214,215,216,222,225,226,228,230,231]. A summary of these randomized clinical trials is outlined in Table 4 and Table 5. We have evaluated the risk of bias among the various randomized controlled trials using the Cochrane Collaboration’s tool [185] and a summary is shown in Figure 3. Overall, we determined that the risk of bias was low among the randomized controlled trials that evaluated the benefits of carotenoid vitamin therapy in AMD. A meta-analysis by Ma et al., comparing nine carotenoid interventional trials, revealed a dose-response relationship that was positively correlated with increased MPOD levels and changes in plasma concentrations, following supplementation with lutein, zeaxanthin, and/or meso-zeaxanthin [56]. Stratified analysis demonstrated that the augmentation of the macular pigment was most effective when supplementing with all three xanthophyll carotenoids during trials lasting longer than 12 months [56]. A stronger effect was also noted for studies containing higher doses of these carotenoids (per daily serving). Furthermore, reports from similar clinical trials seem to corroborate these findings, wherein treatment with macular carotenoids offered significant improvements to MPOD levels in eyes with AMD, upon measurement with both subjective and objective techniques [115,117,205,210,213,214,226,228,230,231]. Consistency among these results is highly significant because changes in the macular pigment measured, in response to carotenoid vitamin therapy, substantiate the role of MPOD status in representing a pharmacodynamic/response biomarker in the context of AMD.
Table 4.
Characteristics of the interventional studies reporting on serum carotenoid levels in AMD.
| Authors (Year) | Study | Participants | Duration | Interventions | Serum | Main Findings |
|---|---|---|---|---|---|---|
| Rosenthal (2006) [227] | - | 30 patients with intermediate or late AMD; aged 60–91 years in USA | 6 months | 2.5 mg L; 5 mg L; 10 mg L | L and Z | Mean serum concentrations rose in each dosage group by 2-fold, 2.9-fold and 4-fold, respectively (p < 0.001 for all) |
| Trieschmann (2007) [119] | LUNA | 100 patients with AMD; aged (71.5 ± 7.1) years in Germany | 6 months | 12 mg L and 1 mg Z * (multivitamin); placebo | L and Z | Substantial increase in L (4-fold rise; p < 0.001) and Z (p = 0.007) concentrations |
| Connolly (2010) [213] | MOST | 5 patients with early AMD; aged (72.0 ± 11.0) years in Ireland | 2 months | 7.3 mg MZ, 3.7 mg L and 0.8 mg Z | L, Z and MZ | Significant time effect between rise in all three carotenoid serum levels (p < 0.003 for all) |
| AREDS2 Research Group (2013) [50] | AREDS2 | 4203 patients with intermediate or late AMD; aged (73.1 ± 7.7) years in USA | 5 years | 10 mg L and 2 mg Z * (multivitamin); 10 mg L, 2 mg Z and omega-3 fatty acids * (multivitamin); “placebo” | L and Z | Total serum L + Z levels increased by 190% to 210% from baseline (p < 0.001) |
| Arnold (2013) [206] | - | 20 patients with atrophic AMD; aged (66.0 ± 8.0) years in Germany | 4 weeks | 10 mg L and 3 mg Z, in oleaginous kale extract | L and Z | Statistically significant rise in serum L and serum Z after 4 weeks (p < 0.001 for both) |
| Arnold (2013) [207] | LUTEGA | 172 patients with atrophic AMD; aged (69.0 ± 10.0) years in Germany | 12 months | 10 mg L and 1 mg Z * (multivitamin); 20 mg L and 2 mg Z * (multivitamin); placebo | L and Z | Beneficial alterations seen in both treatment groups (p < 0.05) after one-month and values remained elevated until trial completion |
| Huang (2013) [219] | - | 108 patients with early AMD; aged 50–81 years in China | 48 weeks | 10 mg L; 20 mg L; 10 mg L and 10 mg Z; placebo | L and Z | Greater increase in serum L and Z with high-dose L (6.23-fold) and L + Z formula (3.11-fold), respectively (p < 0.001 for both) |
| Meagher (2013) [221] | - | 27 patients with early AMD; aged (66.0 ± 9.0) years in Ireland | 8 weeks | 20 mg L, 2 mg Z and 0.3 mg MZ; 10 mg L, 2 mg Z and 10 mg MZ; 3 mg L, 2 mg Z and 17 mg MZ |
L, Z and MZ | Serum L and Z increased only with higher-dose L (Groups 1 and 2; p < 0.001) while serum MZ increased in all three groups (p < 0.01 for all) |
| Murray (2013) [222] | CLEAR | 72 patients with early AMD; aged (70.5 ± 8.7) years in United Kingdom | 12 months | 10 mg L; placebo | L | Marked increase in serum L (p < 0.001) compared to placebo control |
| Akuffo (2015) [205] | MOST | 52 patients with early AMD; aged (66.0 ± 8.0) years in Ireland | 3 years | 20 mg L and 2 mg Z; 10 mg L, 2 mg Z and 10 mg MZ; 3 mg L, 2 mg Z and 17 mg MZ | L, Z and MZ | Statistically significant time x treatment effect revealed for changes serum L and MZ (p < 0.05 for both) concentrations |
| Huang (2015) [115] | - | 112 patients with early AMD; aged (69.1 ± 7.4) years in China | 24 months | 10 mg L; 20 mg L; 10 mg L and 10 mg Z; placebo | L and Z | Highly significant time x treatment interaction observed for both serum L and Z (p < 0.001 for both) |
| Wolf-Schnurrbusch (2015) [231] | - | 79 patients with early/intermediate AMD; aged 55–88 years in Switzerland | 6 months | 10 mg L and 1 mg Z * (multivitamin); 10 mg L, 1 mg Z and omega-3 fatty acids * (multivitamin); placebo | L and Z | Increases in serum L and Z (p < 0.05) only reported in Group 1 (carotenoid treatment without omega-3 fatty acids in formula) |
| Akuffo (2017) [204] | CREST | 121 patients with early/intermediate AMD; aged (64.7 ± 9.0) years in Ireland | 24 months | 10 mg L and 2 mg Z * (multivitamin); 10 mg L and 10 mg Z * (multivitamin); placebo | L, Z and MZ | Remarkable increase in all three serum concentrations (p < 0.0005); time x group interaction effect only for serum Z and MZ (p < 0.005 for both) |
| Sawa (2020) [229] | Sakai Lutein Study | 39 patients with neovascular AMD; aged (70.7 ± 5.3) years in Japan | 6 months | 20 mg L and 3 mg Z (beeswax capsule); 20 mg L and 3 mg Z (glycerol capsule) | L | Serum L increased in both treatment groups at 3- and 6 months (p < 0.01 for both) |
| García-Layana (2021) [217] | - | 109 patients with neovascular AMD; aged (77.1 ± 7.6) years in Spain | 12 months | 10 mg L and 2.6 mg Z * (multivitamin); original AREDS formula (no L/Z) | L and Z | Substantial increase in serum L and Z (p < 0.001 for both) with a large effect size after 12 months (Cohen’s d of ≥0.80 for both) |
* Multivitamin treatment containing carotenoids, in combination with other antioxidants. Abbreviations: L, lutein; Z, zeaxanthin; MZ, meso-zeaxanthin; AMD, age-related macular degeneration; LUNA, Lutein Nutrition effects (measured by autofluorescence); MOST, meso-zeaxanthin Ocular Supplementation Trial; LUTEGA, Lutein/zeaxanthin and omega-3 supplementation on optical density of AMD patients; CLEAR, Combination of Lutein Effects in the Aging Retina; CREST, Central Retinal Enrichment Supplementation Trials.
Table 5.
A summary of the eligible randomized clinical trials reporting on AMD.
| Authors (Year) | Study | Participants | Duration | Interventions | MPOD | Main Findings |
|---|---|---|---|---|---|---|
| Richer (2004) [225] | LAST | 90 patients with atrophic AMD; aged (74.7 ± 7.4) years in USA | 12 months | 10 mg L; 10 mg L * (multivitamin); placebo | HFP | Significant benefit in MPOD (p < 0.001), BCVA (p < 0.01) and CS at low/middle spatial frequencies (p < 0.05 for all) |
| Bartlett (2007) [209] | - | 25 patients with atrophic AMD; aged (69.2 ± 7.8) years in USA | 9 months | 6 mg L; placebo | - | Non-significant trend towards improvement in CS reported |
| Cangemi (2007) [212] | TOZAL | 37 patients with atrophic AMD; aged (76.3 ± 7.8) years in USA | 6 months | 8 mg L and 0.4 mg Z * (multivitamin) | - | Modest improvements observed in BCVA (p = 0.045) |
| Trieschmann (2007) [119] | LUNA | 100 patients with AMD; aged (71.5 ± 7.1) years in Germany | 6 months | 12 mg L and 1 mg Z * (multivitamin);placebo | Fundus AFI | Mean increase of +15.9% in MPOD measured at 0.5° eccentricity (p < 0.001) compared to control |
| Parisi (2008) [223] | CARMIS | 27 patients with atrophic AMD; aged (65.5 ± 5.1) years in Italy | 12 months | 10 mg L + 1 mg Z * (multivitamin); placebo | - | Enhanced improvement in central retinal function measures on mfERG (ring 1 and ring 2; p < 0.01 for both) |
| Connolly (2010) [213] | MOST | 5 patients with early AMD; aged (72.0 ± 11.0) years in Ireland | 2 months | 7.3 mg MZ, 3.7 mg L and 0.8 mg Z | cHFP | Significant increase in MPOD measured at 0.25° and 1° eccentricity with respect to time (p < 0.05 for all) |
| Richer (2011) [226] | ZVF | 60 patients with early/intermediate AMD; aged (74.9 ± 10.0) years in USA | 12 months | 8 mg Z; 8 mg and 9 mg L; 9 mg L | HFP | Central (1°) MPOD increased in all three groups (p < 0.03 for all); significant improvement in measures of foveal vision greater in Z-only group, while benefits in parafoveal vision were greater in L-only group |
| Weigert (2011) [120] | LISA | 126 patients with early/intermediate AMD; aged (71.6 ± 8.6) years in Austria | 6 months | 20 mg L for 3 months, then 10 mg L for 3 months; placebo | Reflectometry | Average increase of +27.9% in MPOD (p < 0.001); trend toward improvement in BCVA did not reach statistical significance |
| Ma (2012) [117] | - | 108 patients with early AMD; aged 50–81 years in China | 48 weeks | 10 mg L; 20 mg L; 10 mg L and 10 mg Z; placebo | Fundus AFI | Significant dose-response effect with increased MPOD (p < 0.01) positively related to benefits in CS (p < 0.05) and central retina function on mfERG (p < 0.01) |
| Piermarocchi (2012) [224] | CARMIS | 145 patients with atrophic AMD; aged (72.5 ± 7.0) years in Italy | 24 months | 10 mg L + 1 mg Z * (multivitamin); placebo | - | Reported significant benefits in BCVA and CS at 6-, 12-, and 24 months (p < 0.01 for all) compared to placebo |
| AREDS2 Research Group (2013) [50] | AREDS2 | 4203 patients with intermediate or late AMD; aged (73.1 ± 7.7) years in USA | 5 years | 10 mg L and 2 mg Z * (multivitamin); 10 mg L, 2 mg Z and omega-3 fatty acids * (multivitamin); “placebo” | - | Reduced hazard ratios of 0.82 (95% CI:0.69–0.96; p = 0.02) for late AMD and 0.76 (95% CI: 0.64–0.94; p = 0.01) for neovascular AMD compared to β-carotene in formulation † |
| Arnold (2013) [206] | - | 20 patients with atrophic AMD; aged (66.0 ± 8.0) years in Germany | 4 weeks | 10 mg L and 3 mg Z, in oleaginous kale extract | Reflectometry | Enhanced augmentation of macular pigment parameters including volume, area and maxOD (p < 0.001 for all) |
| Beatty (2013) [210] | CARMA | 433 patients with early AMD; aged (73.9 ± 8.1) years in Ireland | 12 months | 12 mg L and 0.6 mg Z * (multivitamin); placebo |
Raman spectroscopy | Statistically significant increase in MPOD with a positive linear trend during trial period (p < 0.01 for all) |
| Berrow (2013) [211] | - | 14 patients with early AMD; aged (67.6 ± 8.4) years in UK | 40 weeks | 12 mg L and 0.6 mg Z * (multivitamin); placebo |
- | Remarkable benefits in mfERG N1P1 response amplitude densities in ring 3 (p = 0.027); no differential changes observed in BCVA and CS |
| Dawczynski (2013) [215] | LUTEGA | 145 patients with atrophic AMD; aged (70.0 ± 10.0) years in Germany | 12 months | 10 mg L and 1 mg Z * (multivitamin); 20 mg L and 2 mg Z * (multivitamin); placebo | Reflectometry | Significant improvements observed for MPOD parameters (volume, area, maxOD and mean OD) and BCVA (p < 0.001 for all) in both treatment groups |
| García-Layana (2013) [216] | - | 44 patients with early AMD; aged (68.5 ± 8.5) years in Spain | 12 months | 12 mg L and 0.6 mg Z * (multivitamin); placebo |
HFP | Considerable rise in MPOD (+0.162 ODU; p < 0.01); however, no significant changes seen in BCVA and CS |
| Murray (2013) [222] | CLEAR | 72 patients with early AMD; aged (70.5 ± 8.7) years in United Kingdom | 12 months | 10 mg L; placebo | cHFP | Highly statistically significant increase in MPOD (+39.5%; p < 0.001) when compared to placebo |
| Sabour-Pickett (2014) [228] | MOST | 52 patients with early AMD; aged (66.0 ± 8.0) years in Ireland | 12 months | 20 mg L and 2 mg Z; 10 mg L, 2 mg Z and 10 mg MZ; 3 mg L, 2 mg Z and 17 mg MZ | cHFP | Robust improvements in MPOD spatial profile observed in those supplemented all three carotenoids in formulation (Group 2, p < 0.005; Group 3, p < 0.05) |
| Akuffo (2015) [205] | MOST | 52 patients with early AMD; aged (66.0 ± 8.0) years in Ireland | 3 years | 20 mg L and 2 mg Z; 10 mg L, 2 mg Z and 10 mg MZ; 3 mg L, 2 mg Z and 17 mg MZ | cHFP | Clinically meaningful CS benefits were seen in all three groups (p < 0.05 for all): Group 1 (15.15 cpd), Group 2 (1.2-, 6- and 9.6 cpd) and Group 3 (6-, 9.6- and 15.15 cpd) |
| Huang (2015) [115] | - | 112 patients with early AMD; aged (69.1 ± 7.4) years in China | 24 months | 10 mg L; 20 mg L; 10 mg L and 10 mg Z; placebo | Fundus AFI | Highly significant time x treatment interaction (p < 0.001) between changes in MPOD and central retinal function improvements (mfERG and MRS; p < 0.05 for both) |
| Thurnham (2015) [230] | - | 32 patients with early AMD; aged (66.0 ± 9.0) years in Ireland | 8 weeks | 20 mg L, 2 mg Z and 0.3 mg MZ; 10 mg L, 2 mg Z and 10 mg MZ; 3 mg L, 2 mg Z and 17 mg MZ | cHFP | Significant increase in all three groups (p < 0.05); Group 2 formulation (10 mg L, 2 mg Z and 10 mg MZ) may offer greater improvement to macular pigment spatial profile |
| Wolf-Schnurrbusch (2015) [231] | - | 79 patients with early/intermediate AMD; aged between 55–88 years in Switzerland | 6 months | 10 mg L and 1 mg Z * (multivitamin); 10 mg L, 1 mg Z and omega-3 fatty acids * (multivitamin); placebo | Fundus AFI | Demonstrable benefits in MPOD (p < 0.005) and CS scores (p < 0.01) observed in Group 1 only (carotenoid treatment without omega-3 fatty acids in formulation) |
| Akuffo (2017) [204] | CREST | 121 patients with early/intermediate AMD; aged (64.7 ± 9.0) years in Ireland | 24 months | 10 mg L, 2 mg Z and 10 mg MZ * (AREDS2 multivitamin); 10 mg L and 10 mg Z * (AREDS2 multivitamin) | cHFP | Augmentation of MPOD (p < 0.001) with clinically meaningful benefits in visual function (CS and GD under mesopic and photopic conditions, photostress recovery, and mean/max reading speed; p < 0.05 for all) |
| Azar (2017) [208] | - | 79 patients with neovascular AMD; aged (75.3 ± 7.6) years in France | 8 months | 5 mg L and 1 mg Z * (multivitamin); placebo |
Reflectometry | Non-significant trend toward greater MPOD levels reported in patients with neovascular AMD |
| Corvi (2017) [214] | - | 39 patients with early AMD; aged (78.0 ± 6.5) years in France | 3 months | 10 mg L and 2 mg Z * (multivitamin) | HFP | Significant rise in MPOD only in eyes with reticular pseudodrusen (n = 19; p = 0.002) after 3 months |
| Davey (2020) [53] | - | 56 patients with subclinical AMD; aged (68.4 ± 5.3) years in USA | 6 months | 15 mg L, 10 mg MZ and 2 mg Z * (Lumega-Z); 10 mg L and 2 mg Z * (AREDS-2 multivitamin); placebo | HFP | Statistically significant CS improvements for Lumega-Z group only (p < 0.001) with a positive linear trend with treatment time (p < 0.001) |
| Sawa (2020) [229] | Sakai Lutein Study | 39 patients with neovascular AMD; aged (70.7 ± 5.3) years in Japan | 6 months | 20 mg L and 3 mg Z (beeswax capsule); 20 mg L and 3 mg Z (glycerol capsule) | Fundus AFI | No significant changes were observed in CS, mesopic glare or MPOD in both treatment groups |
* Multivitamin treatment containing carotenoids in combination with other antioxidants; † Secondary analyses reported in AREDS2 Report No. 3 [203]; Abbreviations: MPOD, macular pigment optical density; L, lutein; Z, zeaxanthin; MZ, meso-zeaxanthin; AMD, age-related macular degeneration; LAST, Lutein Antioxidant Supplementation Trial; HFP, heterochromatic flicker photometry; ODU, optical density units; BCVA, best-corrected visual acuity; CS, contrast sensitivity; cpd, cycles per degree; TOZAL, Taurine, Omega-3 fatty acids, Zinc, Antioxidants and Lutein; LUNA, Lutein Nutrition effects measures by Autofluorescence; AFI, autofluorescence imaging; CARMIS, Carotenoids in Age-Related Maculopathy Italian Study; mfERG, multifocal electroretinogram; MOST, meso-zeaxanthin Ocular Supplementation Trial; cHFP, customized HFP; ZVF, Zeaxanthin and Visual Function; LISA, Lutein Intervention Study Austria; AREDS-2, Age-Related Eye Disease Study 2; CARMA, Carotenoids in Age-Related Maculopathy; LUTEGA, Lutein/zeaxanthin and omega-3 supplementation on optical density of AMD patients; CLEAR, Combination of Lutein Effects in the Aging Retina; CREST, Central Retinal Enrichment Supplementation Trials.
Figure 3.
Cochrane Collaboration’s tool for assessing risk of bias in randomized controlled trials [185]. Separate publications are indicated with a symbol (†) next to author name.
Based on the functional relationship between the macular pigments and sharp central vision, alterations in MPOD status have been postulated as a surrogate of visual performance in both healthy and diseased states [42]. In fact, a recent systematic review and meta-analysis by Johnson et al. found that MPOD was significantly correlated with visual function outcomes, including visual acuity, contrast sensitivity, photostress recovery, glare discomfort/disability, and dark adaptation in adults with healthy eyes [54]. Prior reports have also shown that improvements in visual function are positively associated with greater macular pigment levels [54,55,290,291,292,293,294,295,296,297,298,299], which can also be achieved through carotenoid supplementation in healthy eyes [55,57,58,111,112,114,116,298,299,300,301,302,303,304,305,306]. Thus, evidence from AMD trials, wherein carotenoid vitamin therapy is found to enrich MPOD concentrations concomitant with improvements in visual outcome measures, may be clinically beneficial for older adults and those with AMD, as it will likely render daily activities, such as reading or watching television, safer and easier [55,292].
In a meta-analysis by Liu et al. comparing data from several randomized, double-blind, placebo-controlled trials found that carotenoid supplementation resulted in significant improvements in best-corrected visual acuity (BCVA) and contrast sensitivity (CS) at all spatial frequencies in a dose-response relationship [307]. Correlation analysis revealed a linear association between the augmentation of MPOD levels and the observed benefits in BCVA. Several reports seem to mirror these findings, wherein xanthophyll carotenoids notably increased BCVA scores when supplemented for 12 months or longer [210,212,215,224,225,226]. Interestingly, Liu et al. noted that the magnitude of improvement in visual acuity among those with late AMD was substantially reduced, in comparison to those seen in eyes with early or intermediate AMD [307]. These findings likely underscore the mechanisms of action and criticality of the potential of xanthophyll carotenoids in ameliorating the integrity of the neurosensory retina before permanent loss of macular photoreceptors.
Although these improvements in visual acuity are encouraging, changes in CS function represent more comprehensive outcome measures for detecting subtle alterations in visual capacity, following treatment with carotenoid vitamin therapy. Indeed, CS is a more reliable measure of visual function that captures the essence of spatial visual sensitivity and is often prognosticative of poor visual performance, especially in eyes with maculopathy [308,309,310]. Furthermore, a significant linear association was shown between the positive changes in MPOD and the effects on CS at middle frequency [307]. In concordance with this meta-analysis, many AMD trials have also reported demonstrable improvements in CS at low and middle spatial frequencies, following significant enhancement in the macular pigment [53,115,117,204,205,224,225,226,228,231]. Similar to other reports, one study found that, in contrast to the considerable rise in MPOD from baseline to 24 weeks, statistically significant changes in CS were only observed after 48 weeks of supplementation [115]. Hence, these findings seem to suggest that MPOD status may represent a sine qua non for visual function improvement; for instance, contrast sensitivity would show significant improvement, only after MPOD had been sustained at greater concentrations [57,115,292]. This hypothesis is supported by the functional capacity of the macular pigments, wherein the preferential absorption of short-wavelength (blue) light provides pre-receptoral filtration, in addition to limiting the adverse effects of chromatic aberration [55,290,291,292,293,294,295,296,297,298,299]. Greater MPOD levels may also account for the improvements in glare disability [225,226] and photostress recovery [115,204,225]. Hence, carotenoid vitamin therapy was shown to significantly ameliorate several measures of visual performance that worsen, with respect to age and in patients with early or late AMD.
Several AMD trials also demonstrated remarkable improvements in objective measurement of macular function, following supplementation with xanthophyll carotenoids for twelve months or more [211,218,220,223]. Previous studies suggest that the functional integrity of the central retina, particularly the macular region, may be compromised during the early stages of disease progression [311,312,313,314,315,316,317,318,319,320,321]. Reports from AMD trials found that carotenoid vitamin therapy offered protection against early functional abnormalities within the central retina (between 0° and 5° eccentricity) [211,218,220,223]. In fact, two reports indicate that the improvements in central retinal function were positively correlated with MPOD augmentation [218,220]. These results may also be attributed, at least in part, to the enhanced neuroprotective capacity, afforded by these dietary antioxidants, to ameliorate pro-oxidative and pro-inflammatory mechanisms in the local tissue, particularly within the neurosensory layers of the macula [46,255,322,323,324]. In addition to improving the total antioxidant capacity, xanthophylls may also promote metabolic efficiency of the visual transduction cascade by augmenting mitochondrial dysfunction, a primary source of intracellular free radical formation in aging retina [42,46,47,48,255,298,324]. It has also been postulated that greater levels of carotenoids may help to promote the maintenance of synaptic network activity by enhancing cell survival and the viability of neurosensory cells [47,48,298]. However, additional studies are needed to further elucidate the potential role of the carotenoids involved with synaptic network activity and cognitive function [298,325]. These findings suggest that long-term treatment with carotenoids lutein and zeaxanthin in patients with AMD may promote enhanced retinal function by increasing macular pigment concentrations.
In summary, 21 randomized clinical trials reported on the efficacy of carotenoid vitamin therapy on augmenting MPOD levels (Table 5), of which 18 studies demonstrated statistically significant improvements [53,115,117,119,120,204,205,206,208,210,213,214,215,216,222,225,226,228,229,230,231]. Similarly, all 15 studies, highlighted in Table 4, saw demonstrable improvements in the serum concentrations of these xanthophylls, following oral supplementation [50,115,119,204,205,206,207,213,217,219,221,222,227,229,231]. Differential changes in visual performance measures were investigated among 18 studies reporting on visual acuity [50,53,115,117,120,205,208,210,211,212,214,215,216,217,222,224,225,226] and 15 studies reporting on contrast sensitivity function [53,115,117,204,205,209,210,211,216,224,225,226,228,229,231]. Improvements in BCVA were seen in six out of eighteen (6/18) trials [210,212,215,224,225,226]; meanwhile, remarkable benefits in CS were demonstrated in ten out of fifteen (10/15) randomized controlled trials [53,115,117,204,205,224,225,226,228,231]. Five studies evaluated changes in glare disability [204,209,225,226,229], of which four reports indicated significant improvement with carotenoid vitamin therapy [204,209,225,226]. Similarly, five clinical trials investigated the effect on photostress recovery time in AMD patients [115,117,204,225,226], wherein three reports saw changes of statistical significance [204,225,226]. Furthermore, each of the four studies, investigating the objective measures of retinal function through multifocal electroretinogram, showed significant improvements with carotenoid supplementation [211,218,220,223]. It is noteworthy to point out, as summarized in Table 5, that various randomized clinical trials demonstrated significant benefits of carotenoid vitamin supplementation in all stages of AMD.
Reports seem to indicate that AMD patients would likely require a minimum of twelve months of using carotenoid vitamin therapy and a higher dose of carotenoids before measurable benefits in visual function would become clinically apparent. The Carotenoids in Age-Related Maculopathy Italian Study (CARMIS) found that the relative risk of three or more letter visual loss was reduced by up to 76% (RR: 0.26; 95% CI: 0.11–0.59) among patients with atrophic AMD, following two years of carotenoid vitamin therapy [224]. Repeated measures analysis also demonstrated remarkable time effects were seen for the improvements in CS at 6, 12, and 24 months in the active treatment group [224]. This may explain, at least in part, why some trials with shorter durations reported increases in MPOD but only saw trends of improvement in visual function that did not achieve statistical significance [117,120,214,216,217,222]. However, more recent studies investigating the different ratios of xanthophyll carotenoids in formulation, namely the addition of meso-zeaxanthin, have largely shown that incorporating all three carotenoids may offer advantages for the management of early AMD [53,205,228,230].
It is important to note several potential limitations to these studies. In general, the consumption of any single micronutrient-containing vitamin does not appear to afford protection against AMD onset. Although, based on the current evidence, when combined with other antioxidants, dietary carotenoid supplementation with lutein, zeaxanthin, and/or meso-zeaxanthin does appear to substantially delay the disease progression in established AMD. The studies that looked at the addition of meso-zeaxanthin to the carotenoid formulation did not explore a separate group with meso-zeaxanthin alone. So, the exact benefit of including meso-zeaxanthin is not fully understood, as lutein should theoretically be converted to meso-zeaxanthin in all individuals that have the RPE65 isomerase. It is unknown (and additional research is needed) if greater amounts of lutein or zeaxanthin may be a sufficient and suitable substitute to meso-zeaxanthin or if meso-zeaxanthin is truly needed. It is noteworthy that xanthophyll carotenoids, plus antioxidants, did not exert similar treatment effects on geographic atrophy progression during the five-year follow-up in AREDS2 [203]. This may be attributed, at least in part, to advanced stages of disease and by poor micronutrient absorption rates, which likely represents a limiting factor and should not be ruled out from clinical trials [122,326]. However, one preliminary report indicated that oral zeaxanthin supplementation, as an adjunct to an aggressive triple combination therapy regimen (including bevacizumab, steroid, and photodynamic therapy with verteporfin) for patients with subfoveal choroidal neovascularization, enhanced therapeutic efficiency and decreased the number of treatment cycles required [327]. Similar benefits were reported in cultured human RPE cells, following hypoxia-induced VEGF secretion, whereby treatment with zeaxanthin was suggested to offer direction protection against the pro-angiogenic factors contributing to neovascular lesions [328]. Thus, improving carotenoid bioavailability should be among the primary aims for future interventional trials. The bioavailability of carotenoids, following assimilation and transport from dietary matrices, is also strongly influenced by age, gender, and ethnic origin, as well as anthropometric characteristics [43,47,250,266,270,275,277,278,279,281,329]. To overcome such limitations, advancements in micronized and nanoemulsion-based micronutrient delivery techniques have demonstrated improved bioavailability and accumulation of xanthophyll carotenoids in the retina, while maintaining overall safety [53,122,270,330,331,332]. Also, the measurement of MPOD longitudinally can provide a measure of “true bioavailability” at the end organ, which is targeted by the carotenoid vitamin therapy.
4. Conclusions
Age-related macular degeneration remains a leading cause of modifiable vision loss in older adults within developed countries. There is a strong rationale for the use of adjunctive carotenoid vitamin therapy in the clinical management strategies for established AMD. It appears that in the aging retina, the inhibition of the endogenous antioxidant capacity, marked by the depletion of macular carotenoids lutein, zeaxanthin, and meso-zeaxanthin, is a major contributing factor in disease progression. Additionally, systemic perturbations, associated with metabolic syndrome, inversely impact the bioavailability and localization of these carotenoids to the retina. It has been well-documented that these xanthophyll carotenoids possess profound antioxidant capacity, concomitant with their ability to serve as anti-inflammatory mediators, thereby limiting subsequent injury to surrounding tissues. Consistent evidence from large-scale epidemiology studies, and several randomized clinical trials, substantiate the synergic neuroprotective benefits afforded by carotenoid vitamin therapy in eyes with any stage of AMD. To this accord, the routine measurement of MPOD levels may be appropriate for monitoring retinal neurodegeneration caused by AMD and screening those at high-risk prior to the onset of clinical lesions associated with maculopathy. There is tremendous need for timely and prophylactic treatment strategies, whereby irreversible vision loss can be delayed or prevented. Hence, carotenoid vitamin therapy shows enhanced neuroprotection and clinical benefits in visual function, as an adjunctive nutraceutical strategy for patients with AMD.
Author Contributions
Conceptualization, D.W.L. and P.G.D.; methodology, D.W.L. and P.G.D.; data curation, D.W.L.; writing—original draft preparation, D.W.L. and P.G.D.; writing—review and editing, D.W.L., P.G.D., D.L.G., and R.B.R. All authors have read and agreed to the published version of the manuscript.
Funding
This systematic review received no external funding.
Conflicts of Interest
None directly related to the materials discussed. Drake Lem, none. Pinakin Davey serves as a consultant to ZeaVision LLC, which manufactures various nutritional supplements—none of which were used in this study. He has received an honorarium as a speaker at lectures provided by ZeaVision and Guardion Health Sciences. Dennis L. Gierhart is the Chief Scientific officer of, and is employed by, ZeaVision LLC. Richard B. Rosen has received research support from ZeaVision and Guardion Health. He is also a consultant to Optovue and is included on their Angiovue patent. He also consults for Boehringer-Ingelheim, Cellview, and Ocata.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Eye Institute Age-Related Macular Degeneration. [(accessed on 12 May 2021)]; Available online: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration.
- 2.Bourne R.R.A., Jonas J.B., Bron A.M., Cicinelli M.V., Das A., Flaxman S.R., Friedman D.S., Keeffe J.E., Kempen J.H., Leasher J., et al. Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe in 2015: Magnitude, temporal trends and projections. Br. J. Ophthalmol. 2018;102:575–585. doi: 10.1136/bjophthalmol-2017-311258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong W.L., Su X., Li X., Cheung C.M., Klein R., Cheng C.Y., Wong T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health. 2014;2:e106–e116. doi: 10.1016/S2214-109X(13)70145-1. [DOI] [PubMed] [Google Scholar]
- 4.Jonas J.B., Cheung C.M.G., Panda-Jonas S. Updates on the epidemiology of age-related macular degeneration. Asia Pac. J. Ophthalmol. 2017;6:493–497. doi: 10.22608/APO.2017251. [DOI] [PubMed] [Google Scholar]
- 5.Lambert N.G., ElShelmani H., Singh M.K., Mansergh F.C., Wride M.A., Padilla M., Keegan D., Hogg R.E., Ambati B.K. Risk factors and biomarkers of age-related macular degeneration. Prog. Retin. Eye Res. 2016;54:64–102. doi: 10.1016/j.preteyeres.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klein R., Klein B.E., Knudtson M.D., Wong T.Y., Cotch M.F., Liu K., Burke G., Saad M.F., Jacobs D.R., Jr. Prevalence of age-related macular degeneration in 4 racial/ethnic groups in the multi-ethnic study of atherosclerosis. Ophthalmology. 2006;113:373–380. doi: 10.1016/j.ophtha.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 7.Priya R.R., Chew E.Y., Swaroop A. Genetic studies of age-related macular degeneration: Lessons, challenges, and opportunities for disease management. Ophthalmology. 2012;119:2526–2536. doi: 10.1016/j.ophtha.2012.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chakrabarti M. Noncommunicable diseases and noncommunicable eye diseases: What is the way forward? Kerala J. Ophthalmol. 2020;32:224–231. doi: 10.4103/kjo.kjo_114_20. [DOI] [Google Scholar]
- 9.World Health Organization World Report on Vision 2019. [(accessed on 5 April 2021)]; Available online: https://www.who.int/publications/i/item/world-report-on-vision.
- 10.Resnikoff S., Kocur I. Non-communicable eye diseases: Facing the future. Community Eye Health. 2014;27:41–43. [PMC free article] [PubMed] [Google Scholar]
- 11.Kawasaki R., Yasuda M., Song S.J., Chen S.J., Jonas J.B., Wang J.J., Mitchell P., Wong T.Y. The prevalence of age-related macular degeneration in Asians: A systematic review and meta-analysis. Ophthalmology. 2010;117:921–927. doi: 10.1016/j.ophtha.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Klein R., Chou C.F., Klein B.E., Zhang X., Meuer S.M., Saaddine J.B. Prevalence of age-related macular degeneration in the US population. Arch. Ophthalmol. 2011;129:75–80. doi: 10.1001/archophthalmol.2010.318. [DOI] [PubMed] [Google Scholar]
- 13.Krishnan T., Ravindran R.D., Murthy G.V., Vashist P., Fitzpatrick K.E., Thulasiraj R.D., John N., Maraini G., Camparini M., Chakravarthy U., et al. Prevalence of early and late age-related macular degeneration in India: The INDEYE study. Investig. Ophthalmol. Vis. Sci. 2010;51:701–707. doi: 10.1167/iovs.09-4114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rein D.B. Forecasting age-related macular degeneration through the year 2050. Arch. Ophthalmol. 2009;127:533. doi: 10.1001/archophthalmol.2009.58. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell P., Liew G., Gopinath B., Wong T.Y. Age-related macular degeneration. Lancet. 2018;392:1147–1159. doi: 10.1016/S0140-6736(18)31550-2. [DOI] [PubMed] [Google Scholar]
- 16.Ho L., van Leeuwen R., Witteman J.C., van Duijn C.M., Uitterlinden A.G., Hofman A., de Jong P.T., Vingerling J.R., Klaver C.C. Reducing the genetic risk of age-related macular degeneration with dietary antioxidants, zinc, and omega-3 fatty acids: The Rotterdam study. Arch. Ophthalmol. 2011;129:758–766. doi: 10.1001/archophthalmol.2011.141. [DOI] [PubMed] [Google Scholar]
- 17.Jabbarpoor Bonyadi M.H., Yaseri M., Nikkhah H., Bonyadi M., Soheilian M. Association of risk genotypes of ARMS2/LOC387715 A69S and CFH Y402H with age-related macular degeneration with and without reticular pseudodrusen: A meta-analysis. Acta Ophthalmol. 2018;96:e105–e110. doi: 10.1111/aos.13494. [DOI] [PubMed] [Google Scholar]
- 18.Meyers K.J., Johnson E.J., Bernstein P.S., Iyengar S.K., Engelman C.D., Karki C.K., Liu Z., Igo R.P., Jr., Truitt B., Klein M.L., et al. Genetic determinants of macular pigments in women of the Carotenoids in Age-Related Eye Disease Study. Investig. Ophthalmol. Vis. Sci. 2013;54:2333–2345. doi: 10.1167/iovs.12-10867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khanamiri H.N., Falavarjani K.G., Sanati M.H., Aryan H., Irani A., Hashemi M., Modarres M., Parvaresh M.M., Nikeghbali A. Complement factor H Y402H and LOC387715 A69S polymorphisms in association with age-related macular degeneration in Iran. J. Ophthalmic Vis. Res. 2014;9:181–187. [PMC free article] [PubMed] [Google Scholar]
- 20.Vavvas D.G., Small K.W., Awh C.C., Zanke B.W., Tibshirani R.J., Kustra R. CFH and ARMS2 genetic risk determines progression to neovascular age-related macular degeneration after antioxidant and zinc supplementation. Proc. Natl. Acad. Sci. USA. 2018;115:E696–E704. doi: 10.1073/pnas.1718059115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seddon J.M., Cote J., Page W.F., Aggen S.H., Neale M.C. The US twin study of age-related macular degeneration: Relative roles of genetic and environmental influences. Arch. Ophthalmol. 2005;123:321–327. doi: 10.1001/archopht.123.3.321. [DOI] [PubMed] [Google Scholar]
- 22.Bonyadi M., Foruzandeh Z., Mohammadian T., Fotouhi N., Soheilian M., Jabbarpoor Bonyadi M.H., Javadzadeh A., Moein H., Yaseri M. Evaluation of CC-cytokine ligand 2 and complementary factor H Y402H polymorphisms and their interactional association with age-related macular degeneration. Acta Ophthalmol. 2016;94:e779–e785. doi: 10.1111/aos.13143. [DOI] [PubMed] [Google Scholar]
- 23.Rivera A., Fisher S.A., Fritsche L.G., Keilhauer C.N., Lichtner P., Meitinger T., Weber B.H. Hypothetical LOC387715 is a second major susceptibility gene for age-related macular degeneration, contributing independently of complement factor H to disease risk. Hum. Mol. Genet. 2005;14:3227–3236. doi: 10.1093/hmg/ddi353. [DOI] [PubMed] [Google Scholar]
- 24.Weeks D.E., Conley Y.P., Tsai H.J., Mah T.S., Schmidt S., Postel E.A., Agarwal A., Haines J.L., Pericak-Vance M.A., Rosenfeld P.J., et al. Age-related maculopathy: A genomewide scan with continued evidence of susceptibility loci within the 1q31, 10q26, and 17q25 regions. Am. J. Hum. Genet. 2004;75:174–189. doi: 10.1086/422476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang J.J., Buitendijk G.H., Rochtchina E., Lee K.E., Klein B.E., van Duijn C.M., Flood V.M., Meuer S.M., Attia J., Myers C., et al. Genetic susceptibility, dietary antioxidants, and long-term incidence of age-related macular degeneration in two populations. Ophthalmology. 2014;121:667–675. doi: 10.1016/j.ophtha.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 26.Caban-Martinez A.J., Davila E.P., Lam B.L., Dubovy S.R., McCollister K.E., Fleming L.E., Zheng D.D., Lee D.J. Age-related macular degeneration and smoking cessation advice by eye care providers: A pilot study. Prev. Chronic Dis. 2011;8:A147. [PMC free article] [PubMed] [Google Scholar]
- 27.Chakravarthy U., Augood C., Bentham G.C., de Jong P.T., Rahu M., Seland J., Soubrane G., Tomazzoli L., Topouzis F., Vingerling J.R., et al. Cigarette smoking and age-related macular degeneration in the EUREYE Study. Ophthalmology. 2007;114:1157–1163. doi: 10.1016/j.ophtha.2006.09.022. [DOI] [PubMed] [Google Scholar]
- 28.Handa S., Woo J.H., Wagle A.M., Htoon H.M., Eong K.A. Awareness of blindness and other smoking-related diseases and its impact on motivation for smoking cessation in eye patients. Eye. 2011;25:1170–1176. doi: 10.1038/eye.2011.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choudhury F., Varma R., McKean-Cowdin R., Klein R., Azen S.P. Risk factors for four-year incidence and progression of age-related macular degeneration: The Los Angeles Latino Eye Study. Am. J. Ophthalmol. 2011;152:385–395. doi: 10.1016/j.ajo.2011.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seddon J.M. Progression of age-related macular degeneration. Arch. Ophthalmol. 2003;121:785. doi: 10.1001/archopht.121.6.785. [DOI] [PubMed] [Google Scholar]
- 31.Hammond B.R., Jr., Wooten B.R., Snodderly D.M. Cigarette smoking and retinal carotenoids: Implications for age-related macular degeneration. Vis. Res. 1996;36:3003–3009. doi: 10.1016/0042-6989(96)00008-9. [DOI] [PubMed] [Google Scholar]
- 32.Kaarniranta K., Kajdanek J., Morawiec J., Pawlowska E., Blasiak J. PGC-1alpha protects RPE cells of the aging retina against oxidative stress-induced degeneration through the regulation of senescence and mitochondrial quality control. The significance for AMD pathogenesis. Int. J. Mol. Sci. 2018;19:2317. doi: 10.3390/ijms19082317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marazita M.C., Dugour A., Marquioni-Ramella M.D., Figueroa J.M., Suburo A.M. Oxidative stress-induced premature senescence dysregulates VEGF and CFH expression in retinal pigment epithelial cells: Implications for age-related macular degeneration. Redox Biol. 2016;7:78–87. doi: 10.1016/j.redox.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maugeri A., Barchitta M., Mazzone M.G., Giuliano F., Agodi A. Complement System and age-related macular degeneration: Implications of gene-environment interaction for preventive and personalized medicine. Biomed. Res. Int. 2018;2018:7532507. doi: 10.1155/2018/7532507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454:428–435. doi: 10.1038/nature07201. [DOI] [PubMed] [Google Scholar]
- 36.Nozaki M., Raisler B.J., Sakurai E., Sarma J.V., Barnum S.R., Lambris J.D., Chen Y., Zhang K., Ambati B.K., Baffi J.Z., et al. Drusen complement components C3a and C5a promote choroidal neovascularization. Proc. Natl. Acad. Sci. USA. 2006;103:2328–2333. doi: 10.1073/pnas.0408835103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu H., Chen M. Targeting the complement system for the management of retinal inflammatory and degenerative diseases. Eur. J. Pharmacol. 2016;787:94–104. doi: 10.1016/j.ejphar.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dong A., Xie B., Shen J., Yoshida T., Yokoi K., Hackett S.F., Campochiaro P.A. Oxidative stress promotes ocular neovascularization. J. Cell. Physiol. 2009;219:544–552. doi: 10.1002/jcp.21698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beatty S., Koh H., Phil M., Henson D., Boulton M. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv. Ophthalmol. 2000;45:115–134. doi: 10.1016/S0039-6257(00)00140-5. [DOI] [PubMed] [Google Scholar]
- 40.Chen M., Xu H. Parainflammation, chronic inflammation, and age-related macular degeneration. J. Leukoc. Biol. 2015;98:713–725. doi: 10.1189/jlb.3RI0615-239R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu H., Chen M., Forrester J.V. Para-inflammation in the aging retina. Prog. Retin. Eye Res. 2009;28:348–368. doi: 10.1016/j.preteyeres.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 42.Bernstein P.S., Li B., Vachali P.P., Gorusupudi A., Shyam R., Henriksen B.S., Nolan J.M. Lutein, zeaxanthin, and meso-zeaxanthin: The basic and clinical science underlying carotenoid-based nutritional interventions against ocular disease. Prog. Retin. Eye Res. 2016;50:34–66. doi: 10.1016/j.preteyeres.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lem D.W., Gierhart D.L., Davey P.G. Management of diabetic eye disease using carotenoids and nutrients. In: Waisundara V.Y., editor. Antioxidants—Benefits, Sources, and Mechanisms of Action. IntechOpen; London, UK: 2021. [Google Scholar]
- 44.Beatty S., Boulton M., Henson D., Koh H.H., Murray I.J. Macular pigment and age related macular degeneration. Br. J. Ophthalmol. 1999;83:867–877. doi: 10.1136/bjo.83.7.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cai J., Nelson K.C., Wu M., Sternberg P., Jr., Jones D.P. Oxidative damage and protection of the RPE. Prog. Retin. Eye Res. 2000;19:205–221. doi: 10.1016/S1350-9462(99)00009-9. [DOI] [PubMed] [Google Scholar]
- 46.Georgieva E., Ivanova D., Zhelev Z., Bakalova R., Gulubova M., Aoki I. Mitochondrial dysfunction and redox imbalance as a diagnostic marker of “free radical diseases”. Anticancer Res. 2017;37:5373–5381. doi: 10.21873/anticanres.11963. [DOI] [PubMed] [Google Scholar]
- 47.Lem D.W., Gierhart D.L., Davey P.G. Carotenoids in the management of glaucoma: A systematic review of the evidence. Nutrients. 2021;13:1949. doi: 10.3390/nu13061949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lem D.W., Gierhart D.L., Davey P.G. A systematic review of carotenoids in the management of diabetic retinopathy. Nutrients. 2021;13:2441. doi: 10.3390/nu13072441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shimomachi M., Hasan M.Z., Kawaichi M., Oka C. HtrA1 is induced by oxidative stress and enhances cell senescence through p38 MAPK pathway. Exp. Eye Res. 2013;112:79–92. doi: 10.1016/j.exer.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 50.Age-Related Eye Disease Study 2 Research Group. Chew E.Y., Clemons T.E., SanGiovanni J.P., Danis R., Ferris F.L., 3rd, Elman M., Antoszyk A., Ruby A., Orth D., et al. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: The Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA. 2013;309:2005–2015. doi: 10.1001/jama.2013.4997. [DOI] [PubMed] [Google Scholar]
- 51.Age-Related Eye Disease Study Research Group. SanGiovanni J.P., Chew E.Y., Clemons T.E., Ferris F.L., 3rd, Gensler G., Lindblad A.S., Milton R.C., Seddon J.M., Sperduto R.D. The relationship of dietary carotenoid and vitamin A, E, and C intake with age-related macular degeneration in a case-control study: AREDS Report No. 22. Arch. Ophthalmol. 2007;125:1225–1232. doi: 10.1001/archopht.125.9.1225. [DOI] [PubMed] [Google Scholar]
- 52.Chous A.P., Richer S.P., Gerson J.D., Kowluru R.A. The diabetes visual function supplement study (DiVFuSS) Br. J. Ophthalmol. 2016;100:227–234. doi: 10.1136/bjophthalmol-2014-306534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davey P.G., Henderson T., Lem D.W., Weis R., Amonoo-Monney S., Evans D.W. Visual function and macular carotenoid changes in eyes with retinal drusen—An open label randomized controlled trial to compare a micronized lipid-based carotenoid liquid supplementation and AREDS-2 formula. Nutrients. 2020;12:3271. doi: 10.3390/nu12113271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Johnson E.J., Avendano E.E., Mohn E.S., Raman G. The association between macular pigment optical density and visual function outcomes: A systematic review and meta-analysis. Eye. 2020;35:1620–1628. doi: 10.1038/s41433-020-01124-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Loughman J., Nolan J.M., Howard A.N., Connolly E., Meagher K., Beatty S. The impact of macular pigment augmentation on visual performance using different carotenoid formulations. Investig. Ophthalmol. Vis. Sci. 2012;53:7871–7880. doi: 10.1167/iovs.12-10690. [DOI] [PubMed] [Google Scholar]
- 56.Ma L., Liu R., Du J.H., Liu T., Wu S.S., Liu X.H. Lutein, zeaxanthin and meso-zeaxanthin supplementation associated with macular pigment optical density. Nutrients. 2016;8:426. doi: 10.3390/nu8070426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nolan J.M., Loughman J., Akkali M.C., Stack J., Scanlon G., Davison P., Beatty S. The impact of macular pigment augmentation on visual performance in normal subjects: COMPASS. Vis. Res. 2011;51:459–469. doi: 10.1016/j.visres.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 58.Nolan J.M., Power R., Stringham J., Dennison J., Stack J., Kelly D., Moran R., Akuffo K.O., Corcoran L., Beatty S. Enrichment of macular pigment enhances contrast sensitivity in subjects free of retinal disease: Central retinal enrichment supplementation trials—Report 1. Investig. Ophthalmol. Vis. Sci. 2016;57:3429–3439. doi: 10.1167/iovs.16-19520. [DOI] [PubMed] [Google Scholar]
- 59.Guymer R., Wu Z. Age-related macular degeneration (AMD): More than meets the eye. The role of multimodal imaging in today’s management of AMD-A review. Clin. Exp. Ophthalmol. 2020;48:983–995. doi: 10.1111/ceo.13837. [DOI] [PubMed] [Google Scholar]
- 60.Miller J.W., Bagheri S., Vavvas D.G. Advances in Age-related macular degeneration understanding and therapy. US Ophthalmic Rev. 2017;10:119–130. doi: 10.17925/USOR.2017.10.02.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bird A.C., Bressler N.M., Bressler S.B., Chisholm I.H., Coscas G., Davis M.D., de Jong P.T., Klaver C.C., Klein B.E., Klein R., et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv. Ophthalmol. 1995;39:367–374. doi: 10.1016/S0039-6257(05)80092-X. [DOI] [PubMed] [Google Scholar]
- 62.Klein R., Davis M.D., Magli Y.L., Segal P., Klein B.E., Hubbard L. The Wisconsin age-related maculopathy grading system. Ophthalmology. 1991;98:1128–1134. doi: 10.1016/S0161-6420(91)32186-9. [DOI] [PubMed] [Google Scholar]
- 63.Klein R., Meuer S.M., Myers C.E., Buitendijk G.H., Rochtchina E., Choudhury F., de Jong P.T., McKean-Cowdin R., Iyengar S.K., Gao X., et al. Harmonizing the classification of age-related macular degeneration in the three-continent AMD consortium. Ophthalmic Epidemiol. 2014;21:14–23. doi: 10.3109/09286586.2013.867512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Age-Related Eye Disease Study Group. Davis M.D., Gangnon R.E., Lee L.Y., Hubbard L.D., Klein B.E., Klein R., Ferris F.L., Bressler S.B., Milton R.C. The Age-Related Eye Disease Study severity scale for age-related macular degeneration: AREDS report No. 17. Arch. Ophthalmol. 2005;123:1484–1498. doi: 10.1001/archopht.123.11.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Age-Related Eye Disease Study Research Group Risk factors associated with age-related macular degeneration. A case-control study in the age-related eye disease study: Age-related eye disease study report number 3. Ophthalmology. 2000;107:2224–2232. doi: 10.1016/s0161-6420(00)00409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Age-Related Eye Disease Study Research Group. Ferris F.L., Davis M.D., Clemons T.E., Lee L.Y., Chew E.Y., Lindblad A.S., Milton R.C., Bressler S.B., Klein R. A simplified severity scale for age-related macular degeneration: AREDS report no. 18. Arch. Ophthalmol. 2005;123:1570–1574. doi: 10.1001/archopht.123.11.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liew G., Joachim N., Mitchell P., Burlutsky G., Wang J.J. Validating the AREDS simplified severity scale of age-related macular degeneration with 5- and 10-year incident data in a population-based sample. Ophthalmology. 2016;123:1874–1878. doi: 10.1016/j.ophtha.2016.05.043. [DOI] [PubMed] [Google Scholar]
- 68.Ferris F.L., 3rd, Wilkinson C.P., Bird A., Chakravarthy U., Chew E., Csaky K., Sadda S.R., Beckman Initiative for Macular Research Classification Committee Clinical classification of age-related macular degeneration. Ophthalmology. 2013;120:844–851. doi: 10.1016/j.ophtha.2012.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sarks S., Cherepanoff S., Killingsworth M., Sarks J. Relationship of Basal laminar deposit and membranous debris to the clinical presentation of early age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2007;48:968–977. doi: 10.1167/iovs.06-0443. [DOI] [PubMed] [Google Scholar]
- 70.Garrity S.T., Sarraf D., Freund K.B., Sadda S.R. Multimodal imaging of nonneovascular age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2018;59:AMD48–AMD64. doi: 10.1167/iovs.18-24158. [DOI] [PubMed] [Google Scholar]
- 71.Huisingh C., McGwin G., Jr., Neely D., Zarubina A., Clark M., Zhang Y., Curcio C.A., Owsley C. The association between subretinal drusenoid deposits in older adults in normal macular health and incident age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2016;57:739–745. doi: 10.1167/iovs.15-18316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Spaide R.F., Ooto S., Curcio C.A. Subretinal drusenoid deposits AKA pseudodrusen. Surv. Ophthalmol. 2018;63:782–815. doi: 10.1016/j.survophthal.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 73.Wang L., Clark M.E., Crossman D.K., Kojima K., Messinger J.D., Mobley J.A., Curcio C.A. Abundant lipid and protein components of drusen. PLoS ONE. 2010;5:e10329. doi: 10.1371/journal.pone.0010329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wightman A.J., Guymer R.H. Reticular pseudodrusen: Current understanding. Clin. Exp. Optom. 2019;102:455–462. doi: 10.1111/cxo.12842. [DOI] [PubMed] [Google Scholar]
- 75.Owsley C., McGwin G., Jr., Clark M.E., Jackson G.R., Callahan M.A., Kline L.B., Witherspoon C.D., Curcio C.A. Delayed rod-mediated dark adaptation is a functional biomarker for incident early age-related macular degeneration. Ophthalmology. 2016;123:344–351. doi: 10.1016/j.ophtha.2015.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dimitrov P.N., Guymer R.H., Zele A.J., Anderson A.J., Vingrys A.J. Measuring rod and cone dynamics in age-related maculopathy. Investig. Ophthalmol. Vis. Sci. 2008;49:55–65. doi: 10.1167/iovs.06-1048. [DOI] [PubMed] [Google Scholar]
- 77.Owsley C., Huisingh C., Clark M.E., Jackson G.R., McGwin G., Jr. Comparison of visual function in older eyes in the earliest stages of age-related macular degeneration to those in normal macular health. Curr. Eye Res. 2016;41:266–272. doi: 10.3109/02713683.2015.1011282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Owsley C., Jackson G.R., White M., Feist R., Edwards D. Delays in rod-mediated dark adaptation in early age-related maculopathy. Ophthalmology. 2001;108:1196–1202. doi: 10.1016/S0161-6420(01)00580-2. [DOI] [PubMed] [Google Scholar]
- 79.Owsley C., McGwin G., Jr., Jackson G.R., Kallies K., Clark M. Cone- and rod-mediated dark adaptation impairment in age-related maculopathy. Ophthalmology. 2007;114:1728–1735. doi: 10.1016/j.ophtha.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 80.Steinmetz R.L., Haimovici R., Jubb C., Fitzke F.W., Bird A.C. Symptomatic abnormalities of dark adaptation in patients with age-related Bruch’s membrane change. Br. J. Ophthalmol. 1993;77:549–554. doi: 10.1136/bjo.77.9.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bhutto I., Lutty G. Understanding age-related macular degeneration (AMD): Relationships between the photoreceptor/retinal pigment epithelium/Bruch’s membrane/choriocapillaris complex. Mol. Aspects Med. 2012;33:295–317. doi: 10.1016/j.mam.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Freund K.B., Ho I.V., Barbazetto I.A., Koizumi H., Laud K., Ferrara D., Matsumoto Y., Sorenson J.A., Yannuzzi L. Type 3 neovascularization: The expanded spectrum of retinal angiomatous proliferation. Retina. 2008;28:201–211. doi: 10.1097/IAE.0b013e3181669504. [DOI] [PubMed] [Google Scholar]
- 83.Kim J.H., Kim J.W., Kim C.G., Lee D.W. Long-term treatment outcomes in type 3 neovascularization: Focus on the difference in outcomes between geographic atrophy and fibrotic scarring. J. Clin. Med. 2020;9:1145. doi: 10.3390/jcm9041145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Naysan J., Jung J.J., Dansingani K.K., Balaratnasingam C., Freund K.B. Type 2 (subretinal) neovascularization in age-related macular degeneration associated with pure reticular pseudodrusen phenotype. Retina. 2016;36:449–457. doi: 10.1097/IAE.0000000000000758. [DOI] [PubMed] [Google Scholar]
- 85.Seddon J.M., McLeod D.S., Bhutto I.A., Villalonga M.B., Silver R.E., Wenick A.S., Edwards M.M., Lutty G.A. Histopathological insights into choroidal vascular loss in clinically documented cases of age-related macular degeneration. JAMA Ophthalmol. 2016;134:1272–1280. doi: 10.1001/jamaophthalmol.2016.3519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yeo N.J.Y., Chan E.J.J., Cheung C. Choroidal neovascularization: Mechanisms of endothelial dysfunction. Front. Pharmacol. 2019;10:1363. doi: 10.3389/fphar.2019.01363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Biesemeier A., Taubitz T., Julien S., Yoeruek E., Schraermeyer U. Choriocapillaris breakdown precedes retinal degeneration in age-related macular degeneration. Neurobiol. Aging. 2014;35:2562–2573. doi: 10.1016/j.neurobiolaging.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 88.Yannuzzi L.A., Negrao S., Iida T., Carvalho C., Rodriguez-Coleman H., Slakter J., Freund K.B., Sorenson J., Orlock D., Borodoker N. Retinal angiomatous proliferation in age-related macular degeneration. Retina. 2001;21:416–434. doi: 10.1097/00006982-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 89.Spaide R.F., Jaffe G.J., Sarraf D., Freund K.B., Sadda S.R., Staurenghi G., Waheed N.K., Chakravarthy U., Rosenfeld P.J., Holz F.G., et al. Consensus nomenclature for reporting neovascular age-related macular degeneration data: Consensus on neovascular age-related macular degeneration nomenclature study group. Ophthalmology. 2020;127:616–636. doi: 10.1016/j.ophtha.2019.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.McLeod D.S., Grebe R., Bhutto I., Merges C., Baba T., Lutty G.A. Relationship between RPE and choriocapillaris in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2009;50:4982–4991. doi: 10.1167/iovs.09-3639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sparrow J.R., Boulton M. RPE lipofuscin and its role in retinal pathobiology. Exp. Eye Res. 2005;80:595–606. doi: 10.1016/j.exer.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 92.Curcio C.A., Medeiros N.E., Millican C.L. Photoreceptor loss in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 1996;37:1236–1249. [PubMed] [Google Scholar]
- 93.Pilotto E., Benetti E., Convento E., Guidolin F., Longhin E., Parrozzani R., Midena E. Microperimetry, fundus autofluorescence, and retinal layer changes in progressing geographic atrophy. Can. J. Ophthalmol. 2013;48:386–393. doi: 10.1016/j.jcjo.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 94.Rudolf M., Vogt S.D., Curcio C.A., Huisingh C., McGwin G., Jr., Wagner A., Grisanti S., Read R.W. Histologic basis of variations in retinal pigment epithelium autofluorescence in eyes with geographic atrophy. Ophthalmology. 2013;120:821–828. doi: 10.1016/j.ophtha.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yung M., Klufas M.A., Sarraf D. Clinical applications of fundus autofluorescence in retinal disease. Int. J. Retina Vitr. 2016;2:12. doi: 10.1186/s40942-016-0035-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bernstein P.S., Delori F.C., Richer S., van Kuijk F.J., Wenzel A.J. The value of measurement of macular carotenoid pigment optical densities and distributions in age-related macular degeneration and other retinal disorders. Vis. Res. 2010;50:716–728. doi: 10.1016/j.visres.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gruszecki W.I., Sielewiesiuk J. Orientation of xanthophylls in phosphatidylcholine multibilayers. Biochim. Biophys. Acta. 1990;1023:405–412. doi: 10.1016/0005-2736(90)90133-9. [DOI] [PubMed] [Google Scholar]
- 98.Li B., George E.W., Rognon G.T., Gorusupudi A., Ranganathan A., Chang F.Y., Shi L., Frederick J.M., Bernstein P.S. Imaging lutein and zeaxanthin in the human retina with confocal resonance Raman microscopy. Proc. Natl. Acad. Sci. USA. 2020;117:12352–12358. doi: 10.1073/pnas.1922793117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Leung I.Y. Macular pigment: New clinical methods of detection and the role of carotenoids in age-related macular degeneration. Optometry. 2008;79:266–272. doi: 10.1016/j.optm.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 100.De Kinkelder R., van der Veen R.L., Verbaak F.D., Faber D.J., van Leeuwen T.G., Berendschot T.T. Macular pigment optical density measurements: Evaluation of a device using heterochromatic flicker photometry. Eye. 2011;25:105–112. doi: 10.1038/eye.2010.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bone R.A., Landrum J.T., Hime G.W., Cains A., Zamor J. Stereochemistry of the human macular carotenoids. Investig. Ophthalmol. Vis. Sci. 1993;34:2033–2040. [PubMed] [Google Scholar]
- 102.Scripsema N.K., Hu D.N., Rosen R.B. Lutein, zeaxanthin, and meso-zeaxanthin in the clinical management of eye disease. J. Ophthalmol. 2015;2015:865179. doi: 10.1155/2015/865179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Howells O., Eperjesi F., Bartlett H. Measuring macular pigment optical density in vivo: A review of techniques. Graefes Arch. Clin. Exp. Ophthalmol. 2011;249:315–347. doi: 10.1007/s00417-010-1577-5. [DOI] [PubMed] [Google Scholar]
- 104.Li L.H., Lee J.C., Leung H.H., Lam W.C., Fu Z., Lo A.C.Y. Lutein supplementation for eye diseases. Nutrients. 2020;12:1721. doi: 10.3390/nu12061721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gorusupudi A., Shyam R., Li B., Vachali P., Subhani Y.K., Nelson K., Bernstein P.S. Developmentally regulated production of meso-zeaxanthin in chicken retinal pigment epithelium/choroid and retina. Investig. Ophthalmol. Vis. Sci. 2016;57:1853–1861. doi: 10.1167/iovs.16-19111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Shyam R., Gorusupudi A., Nelson K., Horvath M.P., Bernstein P.S. RPE65 has an additional function as the lutein to meso-zeaxanthin isomerase in the vertebrate eye. Proc. Natl. Acad. Sci. USA. 2017;114:10882–10887. doi: 10.1073/pnas.1706332114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bone R.A., Landrum J.T., Mayne S.T., Gomez C.M., Tibor S.E., Twaroska E.E. Macular pigment in donor eyes with and without AMD: A case-control study. Investig. Ophthalmol. Vis. Sci. 2001;42:235–240. [PubMed] [Google Scholar]
- 108.Howells O., Eperjesi F., Bartlett H. Improving the repeatability of heterochromatic flicker photometry for measurement of macular pigment optical density. Graefes Arch. Clin. Exp. Ophthalmol. 2013;251:871–880. doi: 10.1007/s00417-012-2127-0. [DOI] [PubMed] [Google Scholar]
- 109.Zhou H., Zhao X., Johnson E.J., Lim A., Sun E., Yu J., Zhang Y., Liu X., Snellingen T., Shang F., et al. Serum carotenoids and risk of age-related macular degeneration in a chinese population sample. Investig. Ophthalmol. Vis. Sci. 2011;52:4338–4344. doi: 10.1167/iovs.10-6519. [DOI] [PubMed] [Google Scholar]
- 110.Nolan J.M., Stack J., O’Donovan O., Loane E., Beatty S. Risk factors for age-related maculopathy are associated with a relative lack of macular pigment. Exp. Eye Res. 2007;84:61–74. doi: 10.1016/j.exer.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 111.Landrum J.T., Bone R.A., Joa H., Kilburn M.D., Moore L.L., Sprague K.E. A one year study of the macular pigment: The effect of 140 days of a lutein supplement. Exp. Eye Res. 1997;65:57–62. doi: 10.1006/exer.1997.0309. [DOI] [PubMed] [Google Scholar]
- 112.Bone R.A., Landrum J.T., Cao Y., Howard A.N., Alvarez-Calderon F. Macular pigment response to a supplement containing meso-zeaxanthin, lutein and zeaxanthin. Nutr. Metab. 2007;4:12. doi: 10.1186/1743-7075-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Akuffo K.O., Beatty S., Stack J., Dennison J., O’Regan S., Meagher K.A., Peto T., Nolan J. Central retinal enrichment supplementation trials (CREST): Design and methodology of the CREST randomized controlled trials. Ophthalmic Epidemiol. 2014;21:111–123. doi: 10.3109/09286586.2014.888085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Berendschot T.T., Goldbohm R.A., Klopping W.A., van de Kraats J., van Norel J., van Norren D. Influence of lutein supplementation on macular pigment, assessed with two objective techniques. Investig. Ophthalmol. Vis. Sci. 2000;41:3322–3326. [PubMed] [Google Scholar]
- 115.Huang Y.M., Dou H.L., Huang F.F., Xu X.R., Zou Z.Y., Lin X.M. Effect of supplemental lutein and zeaxanthin on serum, macular pigmentation, and visual performance in patients with early age-related macular degeneration. Biomed. Res. Int. 2015;2015:564738. doi: 10.1155/2015/564738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Koh H.H., Murray I.J., Nolan D., Carden D., Feather J., Beatty S. Plasma and macular responses to lutein supplement in subjects with and without age-related maculopathy: A pilot study. Exp. Eye Res. 2004;79:21–27. doi: 10.1016/j.exer.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 117.Ma L., Yan S.F., Huang Y.M., Lu X.R., Qian F., Pang H.L., Xu X.R., Zou Z.Y., Dong P.C., Xiao X., et al. Effect of lutein and zeaxanthin on macular pigment and visual function in patients with early age-related macular degeneration. Ophthalmology. 2012;119:2290–2297. doi: 10.1016/j.ophtha.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 118.Richer S., Devenport J., Lang J.C. LAST II: Differential temporal responses of macular pigment optical density in patients with atrophic age-related macular degeneration to dietary supplementation with xanthophylls. Optometry. 2007;78:213–219. doi: 10.1016/j.optm.2006.10.019. [DOI] [PubMed] [Google Scholar]
- 119.Trieschmann M., Beatty S., Nolan J.M., Hense H.W., Heimes B., Austermann U., Fobker M., Pauleikhoff D. Changes in macular pigment optical density and serum concentrations of its constituent carotenoids following supplemental lutein and zeaxanthin: The LUNA study. Exp. Eye Res. 2007;84:718–728. doi: 10.1016/j.exer.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 120.Weigert G., Kaya S., Pemp B., Sacu S., Lasta M., Werkmeister R.M., Dragostinoff N., Simader C., Garhofer G., Schmidt-Erfurth U., et al. Effects of lutein supplementation on macular pigment optical density and visual acuity in patients with age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2011;52:8174–8178. doi: 10.1167/iovs.11-7522. [DOI] [PubMed] [Google Scholar]
- 121.Khachik F., Bernstein P.S., Garland D.L. Identification of lutein and zeaxanthin oxidation products in human and monkey retinas. Investig. Ophthalmol. Vis. Sci. 1997;38:1802–1811. [PubMed] [Google Scholar]
- 122.Bone R.A., Davey P.G., Roman B.O., Evans D.W. Efficacy of commercially available nutritional supplements: Analysis of Serum uptake, macular pigment optical density and visual functional response. Nutrients. 2020;12:1321. doi: 10.3390/nu12051321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kijlstra A., Tian Y., Kelly E.R., Berendschot T.T. Lutein: More than just a filter for blue light. Prog. Retin. Eye Res. 2012;31:303–315. doi: 10.1016/j.preteyeres.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 124.Junghans A., Sies H., Stahl W. Macular pigments lutein and zeaxanthin as blue light filters studied in liposomes. Arch. Biochem. Biophys. 2001;391:160–164. doi: 10.1006/abbi.2001.2411. [DOI] [PubMed] [Google Scholar]
- 125.Krinsky N.I., Johnson E.J. Carotenoid actions and their relation to health and disease. Mol. Aspects Med. 2005;26:459–516. doi: 10.1016/j.mam.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 126.Landrum J.T., Bone R.A. In: Mechanistic Evidence for Eye Disease and Carotenoids. Krinsky N.I., Mayne S.T., Sies H., editors. CRC Press; New York, NY, USA: 2004. [Google Scholar]
- 127.Li S.Y., Fu Z.J., Lo A.C. Hypoxia-induced oxidative stress in ischemic retinopathy. Oxid. Med. Cell. Longev. 2012;2012:426769. doi: 10.1155/2012/426769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Suarez-Berumen K., Davey P.G. Macular pigments optical density: A Review of techniques of measurements and factors influencing their levels. JSM Ophthalmol. 2014;3:4. [Google Scholar]
- 129.Bartlett H., Eperjesi F. Apparent motion photometry: Evaluation and reliability of a novel method for the measurement of macular pigment. Br. J. Ophthalmol. 2011;95:662–665. doi: 10.1136/bjo.2009.178137. [DOI] [PubMed] [Google Scholar]
- 130.Davey P.G., Alvarez S.D., Lee J.Y. Macular pigment optical density: Repeatability, intereye correlation, and effect of ocular dominance. Clin. Ophthalmol. 2016;10:1671–1678. doi: 10.2147/OPTH.S111708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bartlett H., Howells O., Eperjesi F. The role of macular pigment assessment in clinical practice: A review. Clin. Exp. Optom. 2010;93:300–308. doi: 10.1111/j.1444-0938.2010.00499.x. [DOI] [PubMed] [Google Scholar]
- 132.Delori F.C. Autofluorescence method to measure macular pigment optical densities fluorometry and autofluorescence imaging. Arch. Biochem. Biophys. 2004;430:156–162. doi: 10.1016/j.abb.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 133.Bartlett H., Eperjesi F. Use of fundus imaging in quantification of age-related macular change. Surv. Ophthalmol. 2007;52:655–671. doi: 10.1016/j.survophthal.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 134.Delori F.C., Goger D.G., Hammond B.R., Snodderly D.M., Burns S.A. Macular pigment density measured by autofluorescence spectrometry: Comparison with reflectometry and heterochromatic flicker photometry. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 2001;18:1212–1230. doi: 10.1364/JOSAA.18.001212. [DOI] [PubMed] [Google Scholar]
- 135.Dennison J.L., Stack J., Beatty S., Nolan J.M. Concordance of macular pigment measurements obtained using customized heterochromatic flicker photometry, dual-wavelength autofluorescence, and single-wavelength reflectance. Exp. Eye Res. 2013;116:190–198. doi: 10.1016/j.exer.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 136.Lapierre-Landry M., Carroll J., Skala M.C. Imaging retinal melanin: A review of current technologies. J. Biol. Eng. 2018;12:29. doi: 10.1186/s13036-018-0124-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bone R.A., Mukherjee A. Innovative Troxler-free measurement of macular pigment and lens density with correction of the former for the aging lens. J. Biomed. Opt. 2013;18:107003. doi: 10.1117/1.JBO.18.10.107003. [DOI] [PubMed] [Google Scholar]
- 138.Lee B.B., Martin P.R., Valberg A. The physiological basis of heterochromatic flicker photometry demonstrated in the ganglion cells of the macaque retina. J. Physiol. 1988;404:323–347. doi: 10.1113/jphysiol.1988.sp017292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Obana A., Gohto Y., Moriyama T., Seto T., Sasano H., Okazaki S. Reliability of a commercially available heterochromatic flicker photometer, the MPS2, for measuring the macular pigment optical density of a Japanese population. Jpn. J. Ophthalmol. 2018;62:473–480. doi: 10.1007/s10384-018-0588-3. [DOI] [PubMed] [Google Scholar]
- 140.Berendschot T.T., van Norren D. Objective determination of the macular pigment optical density using fundus reflectance spectroscopy. Arch. Biochem. Biophys. 2004;430:149–155. doi: 10.1016/j.abb.2004.04.029. [DOI] [PubMed] [Google Scholar]
- 141.Davey P.G., Ngo A., Cross J., Gierhart D.L. Macular pigment reflectometry: Development and evaluation of a novel clinical device for rapid objective assessment of the macular carotenoids. In: Manns F., Soderberg P.G., Ho A., editors. Proceedings of the Ophthalmic Technologies XXIX; San Francisco, CA, USA. 2–3 February 2019; Bellingham, WA, USA: SPIE—International Society for Optics and Photonics; 2019. [Google Scholar]
- 142.Huang H., Guan C., Ng D.S., Liu X., Chen H. Macular Pigment optical density measured by a single wavelength reflection photometry with and without mydriasis. Curr. Eye Res. 2019;44:324–328. doi: 10.1080/02713683.2018.1542735. [DOI] [PubMed] [Google Scholar]
- 143.Kilbride P.E., Alexander K.R., Fishman M., Fishman G.A. Human macular pigment assessed by imaging fundus reflectometry. Vis. Res. 1989;29:663–674. doi: 10.1016/0042-6989(89)90028-X. [DOI] [PubMed] [Google Scholar]
- 144.Sanabria J.C., Bass J., Spors F., Gierhart D.L., Davey P.G. Measurement of carotenoids in perifovea using the macular pigment reflectometer. J. Vis. Exp. 2020:9. doi: 10.3791/60429. [DOI] [PubMed] [Google Scholar]
- 145.You Q.S., Bartsch D.U., Espina M., Alam M., Camacho N., Mendoza N., Freeman W.R. Reproducibility of macular pigment optical density measurement by two-wavelength autofluorescence in a clinical setting. Retina. 2016;36:1381–1387. doi: 10.1097/IAE.0000000000000893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bernstein P.S., Zhao D.Y., Sharifzadeh M., Ermakov I.V., Gellermann W. Resonance Raman measurement of macular carotenoids in the living human eye. Arch. Biochem. Biophys. 2004;430:163–169. doi: 10.1016/j.abb.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 147.Gellermann W., Ermakov I.V., Ermakova M.R., McClane R.W., Zhao D.Y., Bernstein P.S. In vivo resonant Raman measurement of macular carotenoid pigments in the young and the aging human retina. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 2002;19:1172–1186. doi: 10.1364/JOSAA.19.001172. [DOI] [PubMed] [Google Scholar]
- 148.Obana A., Gohto Y., Tanito M., Okazaki S., Gellermann W., Bernstein P.S., Ohira A. Effect of age and other factors on macular pigment optical density measured with resonance Raman spectroscopy. Graefes Arch. Clin. Exp. Ophthalmol. 2014;252:1221–1228. doi: 10.1007/s00417-014-2574-x. [DOI] [PubMed] [Google Scholar]
- 149.Obana A., Tanito M., Gohto Y., Gellermann W., Okazaki S., Ohira A. Macular pigment changes in pseudophakic eyes quantified with resonance Raman spectroscopy. Ophthalmology. 2011;118:1852–1858. doi: 10.1016/j.ophtha.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 150.Christaras D., Ginis H., Pennos A., Mompean J., Artal P. Objective method for measuring the macular pigment optical density in the eye. Biomed. Opt. Express. 2019;10:3572–3583. doi: 10.1364/BOE.10.003572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Fasler K., Fu D.J., Moraes G., Wagner S., Gokhale E., Kortuem K., Chopra R., Faes L., Preston G., Pontikos N., et al. Moorfields AMD database report 2: Fellow eye involvement with neovascular age-related macular degeneration. Br. J. Ophthalmol. 2020;104:684–690. doi: 10.1136/bjophthalmol-2019-314446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Rozing M.P., Durhuus J.A., Nielsen M.K., Subhi Y., Kirkwood T.B., Westendorp R.G., Sorensen T.L. Age-related macular degeneration: A two-level model hypothesis. Prog. Retin. Eye Res. 2020;76:100825. doi: 10.1016/j.preteyeres.2019.100825. [DOI] [PubMed] [Google Scholar]
- 153.Sene A., Chin-Yee D., Apte R.S. Seeing through VEGF: Innate and adaptive immunity in pathological angiogenesis in the eye. Trends Mol. Med. 2015;21:43–51. doi: 10.1016/j.molmed.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Califf R.M. Biomarker definitions and their applications. Exp. Biol. Med. 2018;243:213–221. doi: 10.1177/1535370217750088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.FDA-NIH Biomarker Working Group . BEST (Biomarkers, EndpointS, and Other Tools) Resource. Food and Drug Administration; Silver Spring, MD, USA: 2016. [PubMed] [Google Scholar]
- 156.Wickstrom K., Moseley J. Biomarkers and surrogate endpoints in drug development: A European regulatory view. Investig. Ophthalmol. Vis. Sci. 2017;58:BIO27–BIO33. doi: 10.1167/iovs.17-21778. [DOI] [PubMed] [Google Scholar]
- 157.Robb M.A., McInnes P.M., Califf R.M. Biomarkers and surrogate endpoints: Developing common terminology and definitions. JAMA. 2016;315:1107–1108. doi: 10.1001/jama.2016.2240. [DOI] [PubMed] [Google Scholar]
- 158.Obana A., Hiramitsu T., Gohto Y., Ohira A., Mizuno S., Hirano T., Bernstein P.S., Fujii H., Iseki K., Tanito M., et al. Macular carotenoid levels of normal subjects and age-related maculopathy patients in a Japanese population. Ophthalmology. 2008;115:147–157. doi: 10.1016/j.ophtha.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 159.Beatty S., Murray I.J., Henson D.B., Carden D., Koh H., Boulton M.E. Macular pigment and risk for age-related macular degeneration in subjects from a Northern European population. Investig. Ophthalmol. Vis. Sci. 2001;42:439–446. [PubMed] [Google Scholar]
- 160.Bernstein P.S., Zhao D.Y., Wintch S.W., Ermakov I.V., McClane R.W., Gellermann W. Resonance Raman measurement of macular carotenoids in normal subjects and in age-related macular degeneration patients. Ophthalmology. 2002;109:1780–1787. doi: 10.1016/S0161-6420(02)01173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Dietzel M., Zeimer M., Heimes B., Claes B., Pauleikhoff D., Hense H.W. Determinants of macular pigment optical density and its relation to age-related maculopathy: Results from the Muenster Aging and Retina Study (MARS) Investig. Ophthalmol. Vis. Sci. 2011;52:3452–3457. doi: 10.1167/iovs.10-6713. [DOI] [PubMed] [Google Scholar]
- 162.LaRowe T.L., Mares J.A., Snodderly D.M., Klein M.L., Wooten B.R., Chappell R., Group C.M.P.S. Macular pigment density and age-related maculopathy in the carotenoids in age-related eye disease study. An ancillary study of the women’s health initiative. Ophthalmology. 2008;115:876–883. doi: 10.1016/j.ophtha.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 163.Mares J.A., LaRowe T.L., Snodderly D.M., Moeller S.M., Gruber M.J., Klein M.L., Wooten B.R., Johnson E.J., Chappell R.J., Group C.M.P.S., et al. Predictors of optical density of lutein and zeaxanthin in retinas of older women in the Carotenoids in Age-Related Eye Disease Study, an ancillary study of the Women’s Health Initiative. Am. J. Clin. Nutr. 2006;84:1107–1122. doi: 10.1093/ajcn/84.5.1107. [DOI] [PubMed] [Google Scholar]
- 164.Raman R., Biswas S., Gupta A., Kulothungan V., Sharma T. Association of macular pigment optical density with risk factors for wet age-related macular degeneration in the Indian population. Eye. 2012;26:950–957. doi: 10.1038/eye.2012.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.American Optometric Association Macular pigment and healthy vision. Optometry. 2009;80:592–598. doi: 10.1016/j.optm.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 166.Hammond B.R., Jr., Curran-Celentano J., Judd S., Fuld K., Krinsky N.I., Wooten B.R., Snodderly D.M. Sex differences in macular pigment optical density: Relation to plasma carotenoid concentrations and dietary patterns. Vis. Res. 1996;36:2001–2012. doi: 10.1016/0042-6989(95)00290-1. [DOI] [PubMed] [Google Scholar]
- 167.Hammond B.R., Jr., Fuld K., Snodderly D.M. Iris color and macular pigment optical density. Exp. Eye Res. 1996;62:293–297. doi: 10.1006/exer.1996.0035. [DOI] [PubMed] [Google Scholar]
- 168.Ozawa Y., Shigeno Y., Nagai N., Suzuki M., Kurihara T., Minami S., Hirano E., Shinoda H., Kobayashi S., Tsubota K. Absolute and estimated values of macular pigment optical density in young and aged Asian participants with or without age-related macular degeneration. BMC Ophthalmol. 2017;17:161. doi: 10.1186/s12886-017-0557-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Nagai N., Asato T., Minami S., Suzuki M., Shinoda H., Kurihara T., Sonobe H., Watanabe K., Uchida A., Ban N., et al. Correlation between macular pigment optical density and neural thickness and volume of the retina. Nutrients. 2020;12:888. doi: 10.3390/nu12040888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Brandl C., Brucklmayer C., Gunther F., Zimmermann M.E., Kuchenhoff H., Helbig H., Weber B.H.F., Heid I.M., Stark K.J. Retinal layer thicknesses in early age-related macular degeneration: Results from the German AugUR study. Investig. Ophthalmol. Vis. Sci. 2019;60:1581–1594. doi: 10.1167/iovs.18-25332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lamin A., Oakley J.D., Dubis A.M., Russakoff D.B., Sivaprasad S. Changes in volume of various retinal layers over time in early and intermediate age-related macular degeneration. Eye. 2019;33:428–434. doi: 10.1038/s41433-018-0234-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ferrara D., Silver R.E., Louzada R.N., Novais E.A., Collins G.K., Seddon J.M. Optical Coherence tomography features preceding the onset of advanced age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2017;58:3519–3529. doi: 10.1167/iovs.17-21696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Curcio C.A., Messinger J.D., Sloan K.R., Mitra A., McGwin G., Spaide R.F. Human chorioretinal layer thicknesses measured in macula-wide, high-resolution histologic sections. Investig. Ophthalmol. Vis. Sci. 2011;52:3943–3954. doi: 10.1167/iovs.10-6377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Jackson G.R., Owsley C., Curcio C.A. Photoreceptor degeneration and dysfunction in aging and age-related maculopathy. Ageing Res. Rev. 2002;1:381–396. doi: 10.1016/S1568-1637(02)00007-7. [DOI] [PubMed] [Google Scholar]
- 175.Medeiros N.E., Curcio C.A. Preservation of ganglion cell layer neurons in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2001;42:795–803. [PubMed] [Google Scholar]
- 176.Lee E.K., Yu H.G. Ganglion cell-inner plexiform layer and peripapillary retinal nerve fiber layer thicknesses in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2015;56:3976–3983. doi: 10.1167/iovs.15-17013. [DOI] [PubMed] [Google Scholar]
- 177.Muftuoglu I.K., Ramkumar H.L., Bartsch D.U., Meshi A., Gaber R., Freeman W.R. Quantitative analysis of the inner retinal layer thicknesses in age-related macular degeneration using corrected optical coherence tomography segmentation. Retina. 2018;38:1478–1484. doi: 10.1097/IAE.0000000000001759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Savastano M.C., Minnella A.M., Tamburrino A., Giovinco G., Ventre S., Falsini B. Differential vulnerability of retinal layers to early age-related macular degeneration: Evidence by SD-OCT segmentation analysis. Investig. Ophthalmol. Vis. Sci. 2014;55:560–566. doi: 10.1167/iovs.13-12172. [DOI] [PubMed] [Google Scholar]
- 179.Yenice E., Sengun A., Demirok G.S., Turacli E. Ganglion cell complex thickness in nonexudative age-related macular degeneration. Eye. 2015;29:1076–1080. doi: 10.1038/eye.2015.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Zucchiatti I., Parodi M.B., Pierro L., Cicinelli M.V., Gagliardi M., Castellino N., Bandello F. Macular ganglion cell complex and retinal nerve fiber layer comparison in different stages of age-related macular degeneration. Am. J. Ophthalmol. 2015;160:602–607. doi: 10.1016/j.ajo.2015.05.030. [DOI] [PubMed] [Google Scholar]
- 181.Age-Related Eye Disease Study Research Group A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch. Ophthalmol. 2001;119:1417–1436. doi: 10.1001/archopht.119.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Amissah-Arthur K.N., Panneerselvam S., Narendran N., Yang Y.C. Optical coherence tomography changes before the development of choroidal neovascularization in second eyes of patients with bilateral wet macular degeneration. Eye. 2012;26:394–399. doi: 10.1038/eye.2011.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Nagai N., Minami S., Suzuki M., Shinoda H., Kurihara T., Sonobe H., Watanabe K., Uchida A., Ban N., Tsubota K., et al. Macular pigment optical density and photoreceptor outer segment length as predisease biomarkers for age-related macular degeneration. J. Clin. Med. 2020;9:1347. doi: 10.3390/jcm9051347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 185.Higgins J.P., Altman D.G., Gotzsche P.C., Juni P., Moher D., Oxman A.D., Savovic J., Schulz K.F., Weeks L., Sterne J.A., et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Arslan S., Kadayifcilar S., Samur G. The potential role of dietary antioxidant capacity in preventing age-related macular degeneration. J. Am. Coll. Nutr. 2019;38:424–432. doi: 10.1080/07315724.2018.1538830. [DOI] [PubMed] [Google Scholar]
- 187.Cho E., Hankinson S.E., Rosner B., Willett W.C., Colditz G.A. Prospective study of lutein/zeaxanthin intake and risk of age-related macular degeneration. Am. J. Clin. Nutr. 2008;87:1837–1843. doi: 10.1093/ajcn/87.6.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Cho E., Seddon J.M., Rosner B., Willett W.C., Hankinson S.E. Prospective study of intake of fruits, vegetables, vitamins, and carotenoids and risk of age-related maculopathy. Arch. Ophthalmol. 2004;122:883–892. doi: 10.1001/archopht.122.6.883. [DOI] [PubMed] [Google Scholar]
- 189.Dasch B., Fuhs A., Schmidt J., Behrens T., Meister A., Wellmann J., Fobker M., Pauleikhoff D., Hense H.W. Serum levels of macular carotenoids in relation to age-related maculopathy: The Muenster Aging and Retina Study (MARS) Graefes Arch. Clin. Exp. Ophthalmol. 2005;243:1028–1035. doi: 10.1007/s00417-005-1176-z. [DOI] [PubMed] [Google Scholar]
- 190.Delcourt C., Carriere I., Delage M., Barberger-Gateau P., Schalch W., The POLA Study Group Plasma lutein and zeaxanthin and other carotenoids as modifiable risk factors for age-related maculopathy and cataract: The POLA Study. Investig. Ophthalmol. Vis. Sci. 2006;47:2329–2335. doi: 10.1167/iovs.05-1235. [DOI] [PubMed] [Google Scholar]
- 191.Eye Disease Case-Control Study Group Antioxidant status and neovascular age-related macular degeneration. Eye Disease Case-Control Study Group. Arch. Ophthalmol. 1993;111:104–109. doi: 10.1001/archopht.1993.01090010108035. [DOI] [PubMed] [Google Scholar]
- 192.Gale C.R., Hall N.F., Phillips D.I., Martyn C.N. Lutein and zeaxanthin status and risk of age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2003;44:2461–2465. doi: 10.1167/iovs.02-0929. [DOI] [PubMed] [Google Scholar]
- 193.Mares-Perlman J.A., Brady W.E., Klein R., Klein B.E., Bowen P., Stacewicz-Sapuntzakis M., Palta M. Serum antioxidants and age-related macular degeneration in a population-based case-control study. Arch. Ophthalmol. 1995;113:1518–1523. doi: 10.1001/archopht.1995.01100120048007. [DOI] [PubMed] [Google Scholar]
- 194.Mares-Perlman J.A., Fisher A.I., Klein R., Palta M., Block G., Millen A.E., Wright J.D. Lutein and zeaxanthin in the diet and serum and their relation to age-related maculopathy in the third national health and nutrition examination survey. Am. J. Epidemiol. 2001;153:424–432. doi: 10.1093/aje/153.5.424. [DOI] [PubMed] [Google Scholar]
- 195.Michikawa T., Ishida S., Nishiwaki Y., Kikuchi Y., Tsuboi T., Hosoda K., Ishigami A., Iwasawa S., Nakano M., Takebayashi T. Serum antioxidants and age-related macular degeneration among older Japanese. Asia Pac. J. Clin. Nutr. 2009;18:1–7. [PubMed] [Google Scholar]
- 196.Moeller S.M., Parekh N., Tinker L., Ritenbaugh C., Blodi B., Wallace R.B., Mares J.A., CAREDS Research Study Group Associations between intermediate age-related macular degeneration and lutein and zeaxanthin in the Carotenoids in Age-related Eye Disease Study (CAREDS): Ancillary study of the Women’s Health Initiative. Arch. Ophthalmol. 2006;124:1151–1162. doi: 10.1001/archopht.124.8.1151. [DOI] [PubMed] [Google Scholar]
- 197.Seddon J.M., Ajani U.A., Sperduto R.D., Hiller R., Blair N., Burton T.C., Farber M.D., Gragoudas E.S., Haller J., Miller D.T., et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. Eye Disease Case-Control Study Group. JAMA. 1994;272:1413–1420. doi: 10.1001/jama.1994.03520180037032. [DOI] [PubMed] [Google Scholar]
- 198.Snellen E.L., Verbeek A.L., Van Den Hoogen G.W., Cruysberg J.R., Hoyng C.B. Neovascular age-related macular degeneration and its relationship to antioxidant intake. Acta Ophthalmol. Scand. 2002;80:368–371. doi: 10.1034/j.1600-0420.2002.800404.x. [DOI] [PubMed] [Google Scholar]
- 199.Tan J.S., Wang J.J., Flood V., Rochtchina E., Smith W., Mitchell P. Dietary antioxidants and the long-term incidence of age-related macular degeneration: The Blue Mountains Eye Study. Ophthalmology. 2008;115:334–341. doi: 10.1016/j.ophtha.2007.03.083. [DOI] [PubMed] [Google Scholar]
- 200.Van Leeuwen R., Boekhoorn S., Vingerling J.R., Witteman J.C., Klaver C.C., Hofman A., de Jong P.T. Dietary intake of antioxidants and risk of age-related macular degeneration. JAMA. 2005;294:3101–3107. doi: 10.1001/jama.294.24.3101. [DOI] [PubMed] [Google Scholar]
- 201.VandenLangenberg G.M., Mares-Perlman J.A., Klein R., Klein B.E., Brady W.E., Palta M. Associations between antioxidant and zinc intake and the 5-year incidence of early age-related maculopathy in the Beaver Dam Eye Study. Am. J. Epidemiol. 1998;148:204–214. doi: 10.1093/oxfordjournals.aje.a009625. [DOI] [PubMed] [Google Scholar]
- 202.Wu J., Cho E., Willett W.C., Sastry S.M., Schaumberg D.A. Intakes of lutein, zeaxanthin, and other carotenoids and age-related macular degeneration during 2 decades of prospective follow-up. JAMA Ophthalmol. 2015;133:1415–1424. doi: 10.1001/jamaophthalmol.2015.3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Age-Related Eye Disease Study 2 Research Group. Chew E.Y., Clemons T.E., Sangiovanni J.P., Danis R.P., Ferris F.L., 3rd, Elman M.J., Antoszyk A.N., Ruby A.J., Orth D., et al. Secondary analyses of the effects of lutein/zeaxanthin on age-related macular degeneration progression: AREDS2 report no. 3. JAMA Ophthalmol. 2014;132:142–149. doi: 10.1001/jamaophthalmol.2013.7376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Akuffo K.O., Beatty S., Peto T., Stack J., Stringham J., Kelly D., Leung I., Corcoran L., Nolan J.M. The impact of supplemental antioxidants on visual function in nonadvanced age-related macular degeneration: A head-to-head randomized clinical trial. Investig. Ophthalmol. Vis. Sci. 2017;58:5347–5360. doi: 10.1167/iovs.16-21192. [DOI] [PubMed] [Google Scholar]
- 205.Akuffo K.O., Nolan J.M., Howard A.N., Moran R., Stack J., Klein R., Klein B.E., Meuer S.M., Sabour-Pickett S., Thurnham D.I., et al. Sustained supplementation and monitored response with differing carotenoid formulations in early age-related macular degeneration. Eye. 2015;29:902–912. doi: 10.1038/eye.2015.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Arnold C., Jentsch S., Dawczynski J., Bohm V. Age-related macular degeneration: Effects of a short-term intervention with an oleaginous kale extract—A pilot study. Nutrition. 2013;29:1412–1417. doi: 10.1016/j.nut.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 207.Arnold C., Winter L., Frohlich K., Jentsch S., Dawczynski J., Jahreis G., Bohm V. Macular xanthophylls and omega-3 long-chain polyunsaturated fatty acids in age-related macular degeneration: A randomized trial. JAMA Ophthalmol. 2013;131:564–572. doi: 10.1001/jamaophthalmol.2013.2851. [DOI] [PubMed] [Google Scholar]
- 208.Azar G., Quaranta-El Maftouhi M., Masella J.J., Mauget-Faysse M. Macular pigment density variation after supplementation of lutein and zeaxanthin using the Visucam((R)) 200 pigment module: Impact of age-related macular degeneration and lens status. J. Fr. Ophtalmol. 2017;40:303–313. doi: 10.1016/j.jfo.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 209.Bartlett H.E., Eperjesi F. Effect of lutein and antioxidant dietary supplementation on contrast sensitivity in age-related macular disease: A randomized controlled trial. Eur. J. Clin. Nutr. 2007;61:1121–1127. doi: 10.1038/sj.ejcn.1602626. [DOI] [PubMed] [Google Scholar]
- 210.Beatty S., Chakravarthy U., Nolan J.M., Muldrew K.A., Woodside J.V., Denny F., Stevenson M.R. Secondary outcomes in a clinical trial of carotenoids with coantioxidants versus placebo in early age-related macular degeneration. Ophthalmology. 2013;120:600–606. doi: 10.1016/j.ophtha.2012.08.040. [DOI] [PubMed] [Google Scholar]
- 211.Berrow E.J., Bartlett H.E., Eperjesi F., Gibson J.M. The effects of a lutein-based supplement on objective and subjective measures of retinal and visual function in eyes with age-related maculopathy—A randomised controlled trial. Br. J. Nutr. 2013;109:2008–2014. doi: 10.1017/S0007114512004187. [DOI] [PubMed] [Google Scholar]
- 212.Cangemi F.E. TOZAL study: An open case control study of an oral antioxidant and omega-3 supplement for dry AMD. BMC Ophthalmol. 2007;7:3. doi: 10.1186/1471-2415-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Connolly E.E., Beatty S., Thurnham D.I., Loughman J., Howard A.N., Stack J., Nolan J.M. Augmentation of macular pigment following supplementation with all three macular carotenoids: An exploratory study. Curr. Eye Res. 2010;35:335–351. doi: 10.3109/02713680903521951. [DOI] [PubMed] [Google Scholar]
- 214.Corvi F., Souied E.H., Falfoul Y., Georges A., Jung C., Querques L., Querques G. Pilot evaluation of short-term changes in macular pigment and retinal sensitivity in different phenotypes of early age-related macular degeneration after carotenoid supplementation. Br. J. Ophthalmol. 2017;101:770–773. doi: 10.1136/bjophthalmol-2016-309115. [DOI] [PubMed] [Google Scholar]
- 215.Dawczynski J., Jentsch S., Schweitzer D., Hammer M., Lang G.E., Strobel J. Long term effects of lutein, zeaxanthin and omega-3-LCPUFAs supplementation on optical density of macular pigment in AMD patients: The LUTEGA study. Graefes Arch. Clin. Exp. Ophthalmol. 2013;251:2711–2723. doi: 10.1007/s00417-013-2376-6. [DOI] [PubMed] [Google Scholar]
- 216.Garcia-Layana A., Recalde S., Alaman A.S., Robredo P.F. Effects of lutein and docosahexaenoic Acid supplementation on macular pigment optical density in a randomized controlled trial. Nutrients. 2013;5:543–551. doi: 10.3390/nu5020543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Garcia-Layana A., Recalde S., Hernandez M., Abraldes M.J., Nascimento J., Hernandez-Galilea E., Olmedilla-Alonso B., Escobar-Barranco J.J., Zapata M.A., Silva R., et al. A randomized study of nutritional supplementation in patients with unilateral wet age-related macular degeneration. Nutrients. 2021;13:1253. doi: 10.3390/nu13041253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Huang Y.M., Dou H.L., Huang F.F., Xu X.R., Zou Z.Y., Lu X.R., Lin X.M. Changes following supplementation with lutein and zeaxanthin in retinal function in eyes with early age-related macular degeneration: A randomised, double-blind, placebo-controlled trial. Br. J. Ophthalmol. 2015;99:371–375. doi: 10.1136/bjophthalmol-2014-305503. [DOI] [PubMed] [Google Scholar]
- 219.Huang Y.M., Yan S.F., Ma L., Zou Z.Y., Xu X.R., Dou H.L., Lin X.M. Serum and macular responses to multiple xanthophyll supplements in patients with early age-related macular degeneration. Nutrition. 2013;29:387–392. doi: 10.1016/j.nut.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 220.Ma L., Dou H.L., Huang Y.M., Lu X.R., Xu X.R., Qian F., Zou Z.Y., Pang H.L., Dong P.C., Xiao X., et al. Improvement of retinal function in early age-related macular degeneration after lutein and zeaxanthin supplementation: A randomized, double-masked, placebo-controlled trial. Am. J. Ophthalmol. 2012;154:625–634. doi: 10.1016/j.ajo.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 221.Meagher K.A., Thurnham D.I., Beatty S., Howard A.N., Connolly E., Cummins W., Nolan J.M. Serum response to supplemental macular carotenoids in subjects with and without age-related macular degeneration. Br. J. Nutr. 2013;110:289–300. doi: 10.1017/S0007114512004837. [DOI] [PubMed] [Google Scholar]
- 222.Murray I.J., Makridaki M., van der Veen R.L., Carden D., Parry N.R., Berendschot T.T. Lutein supplementation over a one-year period in early AMD might have a mild beneficial effect on visual acuity: The CLEAR study. Investig. Ophthalmol. Vis. Sci. 2013;54:1781–1788. doi: 10.1167/iovs.12-10715. [DOI] [PubMed] [Google Scholar]
- 223.Parisi V., Tedeschi M., Gallinaro G., Varano M., Saviano S., Piermarocchi S., Group C.S. Carotenoids and antioxidants in age-related maculopathy italian study: Multifocal electroretinogram modifications after 1 year. Ophthalmology. 2008;115:324–333. doi: 10.1016/j.ophtha.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 224.Piermarocchi S., Saviano S., Parisi V., Tedeschi M., Panozzo G., Scarpa G., Boschi G., Lo Giudice G., Carmis Study G. Carotenoids in Age-related Maculopathy Italian Study (CARMIS): Two-year results of a randomized study. Eur. J. Ophthalmol. 2012;22:216–225. doi: 10.5301/ejo.5000069. [DOI] [PubMed] [Google Scholar]
- 225.Richer S., Stiles W., Statkute L., Pulido J., Frankowski J., Rudy D., Pei K., Tsipursky M., Nyland J. Double-masked, placebo-controlled, randomized trial of lutein and antioxidant supplementation in the intervention of atrophic age-related macular degeneration: The Veterans LAST study (Lutein Antioxidant Supplementation Trial) Optometry. 2004;75:216–230. doi: 10.1016/S1529-1839(04)70049-4. [DOI] [PubMed] [Google Scholar]
- 226.Richer S.P., Stiles W., Graham-Hoffman K., Levin M., Ruskin D., Wrobel J., Park D.W., Thomas C. Randomized, double-blind, placebo-controlled study of zeaxanthin and visual function in patients with atrophic age-related macular degeneration: The Zeaxanthin and Visual Function Study (ZVF) FDA IND #78, 973. Optometry. 2011;82:667–680. doi: 10.1016/j.optm.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 227.Rosenthal J.M., Kim J., de Monasterio F., Thompson D.J., Bone R.A., Landrum J.T., de Moura F.F., Khachik F., Chen H., Schleicher R.L., et al. Dose-ranging study of lutein supplementation in persons aged 60 years or older. Investig. Ophthalmol. Vis. Sci. 2006;47:5227–5233. doi: 10.1167/iovs.05-1513. [DOI] [PubMed] [Google Scholar]
- 228.Sabour-Pickett S., Beatty S., Connolly E., Loughman J., Stack J., Howard A., Klein R., Klein B.E., Meuer S.M., Myers C.E., et al. Supplementation with three different macular carotenoid formulations in patients with early age-related macular degeneration. Retina. 2014;34:1757–1766. doi: 10.1097/IAE.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 229.Sawa M., Shunto T., Nishiyama I., Yokoyama A., Shigeta R., Miura S., Kawasaki R. Effects of lutein supplementation in Japanese patients with unilateral age-related macular degeneration: The Sakai lutein Study. Sci. Rep. 2020;10:5958. doi: 10.1038/s41598-020-62483-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Thurnham D.I., Nolan J.M., Howard A.N., Beatty S. Macular response to supplementation with differing xanthophyll formulations in subjects with and without age-related macular degeneration. Graefes Arch. Clin. Exp. Ophthalmol. 2015;253:1231–1243. doi: 10.1007/s00417-014-2811-3. [DOI] [PubMed] [Google Scholar]
- 231.Wolf-Schnurrbusch U.E., Zinkernagel M.S., Munk M.R., Ebneter A., Wolf S. Oral lutein supplementation enhances macular pigment density and contrast sensitivity but not in combination with polyunsaturated fatty acids. Investig. Ophthalmol. Vis. Sci. 2015;56:8069–8074. doi: 10.1167/iovs.15-17586. [DOI] [PubMed] [Google Scholar]
- 232.Meyers K.J., Liu Z., Millen A.E., Iyengar S.K., Blodi B.A., Johnson E., Snodderly D.M., Klein M.L., Gehrs K.M., Tinker L., et al. Joint associations of diet, lifestyle, and genes with age-related macular degeneration. Ophthalmology. 2015;122:2286–2294. doi: 10.1016/j.ophtha.2015.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Age-Related Eye Disease Study Research Group. Clemons T.E., Milton R.C., Klein R., Seddon J.M., Ferris F.L., 3rd Risk factors for the incidence of Advanced Age-Related Macular Degeneration in the Age-Related Eye Disease Study (AREDS) AREDS report no. 19. Ophthalmology. 2005;112:533–539. doi: 10.1016/j.ophtha.2004.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Abdel-Aal E.-S.M., Akhtar H., Zaheer K., Ali R. Dietary sources of lutein and zeaxanthin carotenoids and their role in eye health. Nutrients. 2013;5:1169–1185. doi: 10.3390/nu5041169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Eisenhauer B., Natoli S., Liew G., Flood V.M. Lutein and zeaxanthin-food sources, bioavailability and dietary variety in age-related macular degeneration protection. Nutrients. 2017;9:120. doi: 10.3390/nu9020120. [DOI] [Google Scholar]
- 236.Mageney V., Baldermann S., Albach D.C. Intraspecific variation in carotenoids of Brassica oleracea var. sabellica. J. Agric. Food Chem. 2016;64:3251–3257. doi: 10.1021/acs.jafc.6b00268. [DOI] [PubMed] [Google Scholar]
- 237.Perry A., Rasmussen H., Johnson E.J. Xanthophyll (lutein, zeaxanthin) content in fruits, vegetables and corn and egg products. J. Food Compos. Anal. 2009;22:9–15. doi: 10.1016/j.jfca.2008.07.006. [DOI] [Google Scholar]
- 238.Ma L., Dou H.L., Wu Y.Q., Huang Y.M., Huang Y.B., Xu X.R., Zou Z.Y., Lin X.M. Lutein and zeaxanthin intake and the risk of age-related macular degeneration: A systematic review and meta-analysis. Br. J. Nutr. 2012;107:350–359. doi: 10.1017/S0007114511004260. [DOI] [PubMed] [Google Scholar]
- 239.Huang C.P., Lin Y.W., Huang Y.C., Tsai F.J. Mitochondrial dysfunction as a novel target for neuroprotective nutraceuticals in ocular diseases. Nutrients. 2020;12:1950. doi: 10.3390/nu12071950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Barot M., Gokulgandhi M.R., Mitra A.K. Mitochondrial dysfunction in retinal diseases. Curr. Eye. Res. 2011;36:1069–1077. doi: 10.3109/02713683.2011.607536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Armstrong J.S. Mitochondrial medicine: Pharmacological targeting of mitochondria in disease. Br. J. Pharmacol. 2007;151:1154–1165. doi: 10.1038/sj.bjp.0707288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Feher J., Papale A., Mannino G., Gualdi L., Gabrieli C.B. Mitotropic compounds for the treatment of age-related macular degeneration. The metabolic approach and a pilot study. Ophthalmologica. 2003;217:351–357. doi: 10.1159/000071351. [DOI] [PubMed] [Google Scholar]
- 243.Bohn T. Bioavailability of non-provitamin A carotenoids. Curr. Nutr. Food Sci. 2008;4:240–258. doi: 10.2174/157340108786263685. [DOI] [Google Scholar]
- 244.Bray G.A., Nielsen S.J., Popkin B.M. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am. J. Clin. Nutr. 2004;79:537–543. doi: 10.1093/ajcn/79.4.537. [DOI] [PubMed] [Google Scholar]
- 245.Castenmiller J.J., West C.E. Bioavailability and bioconversion of carotenoids. Annu. Rev. Nutr. 1998;18:19–38. doi: 10.1146/annurev.nutr.18.1.19. [DOI] [PubMed] [Google Scholar]
- 246.Gross L.S., Li L., Ford E.S., Liu S. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: An ecologic assessment. Am. J. Clin. Nutr. 2004;79:774–779. doi: 10.1093/ajcn/79.5.774. [DOI] [PubMed] [Google Scholar]
- 247.Ludwig D.S., Majzoub J.A., Al-Zahrani A., Dallal G.E., Blanco I., Roberts S.B. High glycemic index foods, overeating, and obesity. Pediatrics. 1999;103:E26. doi: 10.1542/peds.103.3.e26. [DOI] [PubMed] [Google Scholar]
- 248.Nagao A. Absorption and metabolism of dietary carotenoids. BioFactors. 2011;37:83–87. doi: 10.1002/biof.151. [DOI] [PubMed] [Google Scholar]
- 249.O’Connell O.F., Ryan L., O’Brien N.M. Xanthophyll carotenoids are more bioaccessible from fruits than dark green vegetables. Nutr. Res. 2007;27:258–264. doi: 10.1016/j.nutres.2007.04.002. [DOI] [Google Scholar]
- 250.Van het Hof K.H., West C.E., Weststrate J.A., Hautvast J.G.A.J. Dietary factors that affect the bioavailability of carotenoids. J. Nutr. 2000;130:503–506. doi: 10.1093/jn/130.3.503. [DOI] [PubMed] [Google Scholar]
- 251.Barreau E., Brossas J.Y., Courtois Y., Tréton J.A. Accumulation of mitochondrial DNA deletions in human retina during aging. Investig. Ophthalmol. Vis. Sci. 1996;37:384–391. [PubMed] [Google Scholar]
- 252.Decanini A., Nordgaard C.L., Feng X., Ferrington D.A., Olsen T.W. Changes in select redox proteins of the retinal pigment epithelium in age-related macular degeneration. Am. J. Ophthalmol. 2007;143:607–615. doi: 10.1016/j.ajo.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Dunaief J.L. The role of apoptosis in age-related macular degeneration. Arch. Ophthalmol. 2002;120:1435. doi: 10.1001/archopht.120.11.1435. [DOI] [PubMed] [Google Scholar]
- 254.Feher J., Kovacs I., Artico M., Cavallotti C., Papale A., Gabrieli C.B. Mitochondrial alterations of retinal pigment epithelium in age-related macular degeneration. Neurobiol. Aging. 2006;27:983–993. doi: 10.1016/j.neurobiolaging.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 255.Kaarniranta K., Pawlowska E., Szczepanska J., Jablkowska A., Blasiak J. Role of mitochondrial DNA damage in ROS-mediated pathogenesis of age-related macular degeneration (AMD) Int. J. Mol. Sci. 2019;20:2374. doi: 10.3390/ijms20102374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Kennedy C.J., Rakoczy P.E., Constable I.J. Lipofuscin of the retinal pigment epithelium: A review. Eye. 1995;9:763–771. doi: 10.1038/eye.1995.192. [DOI] [PubMed] [Google Scholar]
- 257.Liang F.-Q., Godley B.F. Oxidative stress-induced mitochondrial DNA damage in human retinal pigment epithelial cells: A possible mechanism for RPE aging and age-related macular degeneration. Exp. Eye Res. 2003;76:397–403. doi: 10.1016/S0014-4835(03)00023-X. [DOI] [PubMed] [Google Scholar]
- 258.Nordgaard C.L., Berg K.M., Kapphahn R.J., Reilly C., Feng X., Olsen T.W., Ferrington D.A. Proteomics of the retinal pigment epithelium reveals altered protein expression at progressive stages of age-related macular degeneration. Investig. Opthalmol. Vis. Sci. 2006;47:815. doi: 10.1167/iovs.05-0976. [DOI] [PubMed] [Google Scholar]
- 259.Terluk M.R., Kapphahn R.J., Soukup L.M., Gong H., Gallardo C., Montezuma S.R., Ferrington D.A. Investigating mitochondria as a target for treating age-related macular degeneration. J. Neurosci. 2015;35:7304–7311. doi: 10.1523/JNEUROSCI.0190-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Terman A., Brunk U.T. Oxidative stress, accumulation of biological ‘garbage’, and aging. Antioxid. Redox Signal. 2006;8:197–204. doi: 10.1089/ars.2006.8.197. [DOI] [PubMed] [Google Scholar]
- 261.Mukhopadhyay A., Weiner H. Delivery of drugs and macromolecules to mitochondria. Adv. Drug Deliv. Rev. 2007;59:729–738. doi: 10.1016/j.addr.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Neroev V.V., Archipova M.M., Bakeeva L.E., Fursova A., Grigorian E.N., Grishanova A.Y., Iomdina E.N., Ivashchenko Z.N., Katargina L.A., Khoroshilova-Maslova I.P., et al. Mitochondria-targeted plastoquinone derivatives as tools to interrupt execution of the aging program. 4. Age-related eye disease. SkQ1 returns vision to blind animals. Biochemistry. 2008;73:1317–1328. doi: 10.1134/S0006297908120043. [DOI] [PubMed] [Google Scholar]
- 263.Al-Aubaidy H.A., Jelinek H.F. Oxidative DNA damage and obesity in type 2 diabetes mellitus. Eur. J. Endocrinol. 2011;164:899–904. doi: 10.1530/EJE-11-0053. [DOI] [PubMed] [Google Scholar]
- 264.Castro A.M., Macedo-de la Concha L.E., Pantoja-Meléndez C.A. Low-grade inflammation and its relation to obesity and chronic degenerative diseases. Rev. Méd. Hosp. Gen. México. 2017;80:101–105. doi: 10.1016/j.hgmx.2016.06.011. [DOI] [Google Scholar]
- 265.Chung H.Y., Ferreira A.L., Epstein S., Paiva S.A., Castaneda-Sceppa C., Johnson E.J. Site-specific concentrations of carotenoids in adipose tissue: Relations with dietary and serum carotenoid concentrations in healthy adults. Am. J. Clin. Nutr. 2009;90:533–539. doi: 10.3945/ajcn.2009.27712. [DOI] [PubMed] [Google Scholar]
- 266.Connor W.E., Duell P.B., Kean R., Wang Y. The prime role of HDL to transport lutein into the retina: Evidence from HDL-deficient WHAM chicks having a mutant ABCA1 transporter. Investig. Ophthalmol. Vis. Sci. 2007;48:4226–4231. doi: 10.1167/iovs.06-1275. [DOI] [PubMed] [Google Scholar]
- 267.Fernandez-Sanchez A., Madrigal-Santillan E., Bautista M., Esquivel-Soto J., Morales-Gonzalez A., Esquivel-Chirino C., Durante-Montiel I., Sanchez-Rivera G., Valadez-Vega C., Morales-Gonzalez J.A. Inflammation, oxidative stress, and obesity. Int. J. Mol. Sci. 2011;12:3117–3132. doi: 10.3390/ijms12053117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Frayn K.N., Coppack S.W., Fielding B.A., Humphreys S.M. Coordinated regulation of hormone-sensitive lipase and lipoprotein lipase in human adipose tissue in vivo: Implications for the control of fat storage and fat mobilization. Adv. Enzyme Regul. 1995;35:163–178. doi: 10.1016/0065-2571(94)00011-Q. [DOI] [PubMed] [Google Scholar]
- 269.Kwon H., Pessin J.E. Adipokines mediate inflammation and insulin resistance. Front. Endocrinol. 2013;4:71. doi: 10.3389/fendo.2013.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Lim C., Kim D.-W., Sim T., Hoang N.H., Lee J.W., Lee E.S., Youn Y.S., Oh K.T. Preparation and characterization of a lutein loading nanoemulsion system for ophthalmic eye drops. J. Drug Deliv. Sci. Technol. 2016;36:168–174. doi: 10.1016/j.jddst.2016.10.009. [DOI] [Google Scholar]
- 271.Loane E., Nolan J.M., Beatty S. The respective relationships between lipoprotein profile, macular pigment optical density, and serum concentrations of lutein and zeaxanthin. Investig. Ophthalmol. Vis. Sci. 2010;51:5897–5905. doi: 10.1167/iovs.09-4878. [DOI] [PubMed] [Google Scholar]
- 272.Rosen B.S., Cook K.S., Yaglom J., Groves D.L., Volanakis J.E., Damm D., White T., Spiegelman B.M. Adipsin and complement factor D activity: An immune-related defect in obesity. Science. 1989;244:1483–1487. doi: 10.1126/science.2734615. [DOI] [PubMed] [Google Scholar]
- 273.Savini I., Catani M.V., Evangelista D., Gasperi V., Avigliano L. Obesity-associated oxidative stress: Strategies finalized to improve redox state. Int. J. Mol. Sci. 2013;14:10497–10538. doi: 10.3390/ijms140510497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Tilg H., Moschen A.R. Adipocytokines: Mediators linking adipose tissue, inflammation and immunity. Nat. Rev. Immunol. 2006;6:772–783. doi: 10.1038/nri1937. [DOI] [PubMed] [Google Scholar]
- 275.Wang W., Connor S.L., Johnson E.J., Klein M.L., Hughes S., Connor W.E. Effect of dietary lutein and zeaxanthin on plasma carotenoids and their transport in lipoproteins in age-related macular degeneration. Am. J. Clin. Nutr. 2007;85:762–769. doi: 10.1093/ajcn/85.3.762. [DOI] [PubMed] [Google Scholar]
- 276.Bovier E.R., Lewis R.D., Hammond B.R., Jr. The relationship between lutein and zeaxanthin status and body fat. Nutrients. 2013;5:750–757. doi: 10.3390/nu5030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Broekmans W.M., Berendschot T.T., Klopping-Ketelaars I.A., de Vries A.J., Goldbohm R.A., Tijburg L.B., Kardinaal A.F., van Poppel G. Macular pigment density in relation to serum and adipose tissue concentrations of lutein and serum concentrations of zeaxanthin. Am. J. Clin. Nutr. 2002;76:595–603. doi: 10.1093/ajcn/76.3.595. [DOI] [PubMed] [Google Scholar]
- 278.Johnson E.J., Hammond B.R., Yeum K.J., Qin J., Wang X.D., Castaneda C., Snodderly D.M., Russell R.M. Relation among serum and tissue concentrations of lutein and zeaxanthin and macular pigment density. Am. J. Clin. Nutr. 2000;71:1555–1562. doi: 10.1093/ajcn/71.6.1555. [DOI] [PubMed] [Google Scholar]
- 279.Hammond B.R., Jr., Ciulla T.A., Snodderly D.M. Macular pigment density is reduced in obese subjects. Investig. Ophthalmol. Vis. Sci. 2002;43:47–50. [PubMed] [Google Scholar]
- 280.Nieves D.J., Cnop M., Retzlaff B., Walden C.E., Brunzell J.D., Knopp R.H., Kahn S.E. The atherogenic lipoprotein profile associated with obesity and insulin resistance is largely attributable to intra-abdominal fat. Diabetes. 2003;52:172–179. doi: 10.2337/diabetes.52.1.172. [DOI] [PubMed] [Google Scholar]
- 281.Nolan J., O’Donovan O., Kavanagh H., Stack J., Harrison M., Muldoon A., Mellerio J., Beatty S. Macular pigment and percentage of body fat. Investig. Ophthalmol. Vis. Sci. 2004;45:3940–3950. doi: 10.1167/iovs.04-0273. [DOI] [PubMed] [Google Scholar]
- 282.Nolan J.M., Feeney J., Kenny R.A., Cronin H., O’Regan C., Savva G.M., Loughman J., Finucane C., Connolly E., Meagher K., et al. Education is positively associated with macular pigment: The Irish Longitudinal Study on Ageing (TILDA) Investig. Ophthalmol. Vis. Sci. 2012;53:7855–7861. doi: 10.1167/iovs.11-9367. [DOI] [PubMed] [Google Scholar]
- 283.Flammer J., Konieczka K., Flammer A.J. The primary vascular dysregulation syndrome: Implications for eye diseases. EPMA J. 2013;4:14. doi: 10.1186/1878-5085-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Jeganathan V.S., Kawasaki R., Wang J.J., Aung T., Mitchell P., Saw S.M., Wong T.Y. Retinal vascular caliber and age-related macular degeneration: The Singapore Malay Eye Study. Am. J. Ophthalmol. 2008;146:954–959. doi: 10.1016/j.ajo.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 285.Kumari N., Cher J., Chua E., Hamzah H., Wong T.Y., Cheung C.Y. Association of serum lutein and zeaxanthin with quantitative measures of retinal vascular parameters. PLoS ONE. 2018;13:e0203868. doi: 10.1371/journal.pone.0203868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Parker R.S. Carotenoids in human blood and tissues. J. Nutr. 1989;119:101–104. doi: 10.1093/jn/119.1.101. [DOI] [PubMed] [Google Scholar]
- 287.Alpha-Tocopherol Beta Carotene Cancer Prevention Study Group The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N. Engl. J. Med. 1994;330:1029–1035. doi: 10.1056/NEJM199404143301501. [DOI] [PubMed] [Google Scholar]
- 288.Middha P., Weinstein S.J., Männistö S., Albanes D., Mondul A.M. β-carotene supplementation and lung cancer incidence in the alpha-tocopherol, beta-carotene cancer prevention study: The role of tar and nicotine. Nicotine Tob. Res. 2019;21:1045–1050. doi: 10.1093/ntr/nty115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Age-Related Eye Disease Study 2 Research Group. Chew E.Y., Clemons T., SanGiovanni J.P., Danis R., Domalpally A., McBee W., Sperduto R., Ferris F.L. The Age-Related Eye Disease Study 2 (AREDS2): Study design and baseline characteristics (AREDS2 report number 1) Ophthalmology. 2012;119:2282–2289. doi: 10.1016/j.ophtha.2012.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Hammond B.R., Jr., Fletcher L.M., Elliott J.G. Glare disability, photostress recovery, and chromatic contrast: Relation to macular pigment and serum lutein and zeaxanthin. Investig. Ophthalmol. Vis. Sci. 2013;54:476–481. doi: 10.1167/iovs.12-10411. [DOI] [PubMed] [Google Scholar]
- 291.Hammond B.R., Fletcher L.M., Roos F., Wittwer J., Schalch W. A double-blind, placebo-controlled study on the effects of lutein and zeaxanthin on photostress recovery, glare disability, and chromatic contrast. Investig. Ophthalmol. Vis. Sci. 2014;55:8583–8589. doi: 10.1167/iovs.14-15573. [DOI] [PubMed] [Google Scholar]
- 292.Loughman J., Akkali M.C., Beatty S., Scanlon G., Davison P.A., O’Dwyer V., Cantwell T., Major P., Stack J., Nolan J.M. The relationship between macular pigment and visual performance. Vis. Res. 2010;50:1249–1256. doi: 10.1016/j.visres.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 293.Stringham J.M., Garcia P.V., Smith P.A., Hiers P.L., McLin L.N., Kuyk T.K., Foutch B.K. Macular pigment and visual performance in low-light conditions. Investig. Ophthalmol. Vis. Sci. 2015;56:2459–2468. doi: 10.1167/iovs.14-15716. [DOI] [PubMed] [Google Scholar]
- 294.Stringham J.M., Garcia P.V., Smith P.A., McLin L.N., Foutch B.K. Macular pigment and visual performance in glare: Benefits for photostress recovery, disability glare, and visual discomfort. Investig. Ophthalmol. Vis. Sci. 2011;52:7406–7415. doi: 10.1167/iovs.10-6699. [DOI] [PubMed] [Google Scholar]
- 295.Stringham J.M., Hammond B.R., Jr. The glare hypothesis of macular pigment function. Optom. Vis. Sci. 2007;84:859–864. doi: 10.1097/OPX.0b013e3181559c2b. [DOI] [PubMed] [Google Scholar]
- 296.Stringham J.M., Hammond B.R. Macular pigment and visual performance under glare conditions. Optom. Vis. Sci. 2008;85:82–88. doi: 10.1097/OPX.0b013e318162266e. [DOI] [PubMed] [Google Scholar]
- 297.Stringham J.M., O’Brien K.J., Stringham N.T. Macular carotenoid supplementation improves disability glare performance and dynamics of photostress recovery. Eye Vis. 2016;3:30. doi: 10.1186/s40662-016-0060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Stringham J.M., O’Brien K.J., Stringham N.T. Contrast sensitivity and lateral inhibition are enhanced with macular carotenoid supplementation. Investig. Ophthalmol. Vis. Sci. 2017;58:2291–2295. doi: 10.1167/iovs.16-21087. [DOI] [PubMed] [Google Scholar]
- 299.Stringham J.M., Stringham N.T., O’Brien K.J. Macular carotenoid supplementation improves visual performance, sleep quality, and adverse physical symptoms in those with high screen time exposure. Foods. 2017;6:47. doi: 10.3390/foods6070047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Khachik F., de Moura F.F., Chew E.Y., Douglass L.W., Ferris F.L., 3rd, Kim J., Thompson D.J. The effect of lutein and zeaxanthin supplementation on metabolites of these carotenoids in the serum of persons aged 60 or older. Investig. Ophthalmol. Vis. Sci. 2006;47:5234–5242. doi: 10.1167/iovs.06-0504. [DOI] [PubMed] [Google Scholar]
- 301.Bone R.A., Landrum J.T. Dose-dependent response of serum lutein and macular pigment optical density to supplementation with lutein esters. Arch. Biochem. Biophys. 2010;504:50–55. doi: 10.1016/j.abb.2010.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Bovier E.R., Hammond B.R. A randomized placebo-controlled study on the effects of lutein and zeaxanthin on visual processing speed in young healthy subjects. Arch. Biochem. Biophys. 2015;572:54–57. doi: 10.1016/j.abb.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 303.Johnson E.J., Chung H.Y., Caldarella S.M., Snodderly D.M. The influence of supplemental lutein and docosahexaenoic acid on serum, lipoproteins, and macular pigmentation. Am. J. Clin. Nutr. 2008;87:1521–1529. doi: 10.1093/ajcn/87.5.1521. [DOI] [PubMed] [Google Scholar]
- 304.Kvansakul J., Rodriguez-Carmona M., Edgar D.F., Barker F.M., Kopcke W., Schalch W., Barbur J.L. Supplementation with the carotenoids lutein or zeaxanthin improves human visual performance. Ophthalmic Physiol. Opt. 2006;26:362–371. doi: 10.1111/j.1475-1313.2006.00387.x. [DOI] [PubMed] [Google Scholar]
- 305.Landrum J., Bone R., Mendez V., Valenciaga A., Babino D. Comparison of dietary supplementation with lutein diacetate and lutein: A pilot study of the effects on serum and macular pigment. Acta Biochim. Pol. 2012;59:167–169. doi: 10.18388/abp.2012_2198. [DOI] [PubMed] [Google Scholar]
- 306.Yao Y., Qiu Q.H., Wu X.W., Cai Z.Y., Xu S., Liang X.Q. Lutein supplementation improves visual performance in Chinese drivers: 1-year randomized, double-blind, placebo-controlled study. Nutrition. 2013;29:958–964. doi: 10.1016/j.nut.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 307.Liu R., Wang T., Zhang B., Qin L., Wu C., Li Q., Ma L. Lutein and zeaxanthin supplementation and association with visual function in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2014;56:252–258. doi: 10.1167/iovs.14-15553. [DOI] [PubMed] [Google Scholar]
- 308.Buhren J., Terzi E., Bach M., Wesemann W., Kohnen T. Measuring contrast sensitivity under different lighting conditions: Comparison of three tests. Optom. Vis. Sci. 2006;83:290–298. doi: 10.1097/01.opx.0000216100.93302.2d. [DOI] [PubMed] [Google Scholar]
- 309.Chen X., Li Q., Liu X., Yang L., Xia W., Tao L. Visual acuity evaluated by pattern-reversal visual-evoked potential is affected by check size/visual angle. Neurosci. Bull. 2012;28:737–745. doi: 10.1007/s12264-012-1292-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Stangos N., Voutas S., Topouzis F., Karampatakis V. Contrast sensitivity evaluation in eyes predisposed to age-related macular degeneration and presenting normal visual acuity. Ophthalmologica. 1995;209:194–198. doi: 10.1159/000310612. [DOI] [PubMed] [Google Scholar]
- 311.Berrow E.J., Bartlett H.E., Eperjesi F., Gibson J.M. The electroretinogram: A useful tool for evaluating age-related macular disease? Doc. Ophthalmol. 2010;121:51–62. doi: 10.1007/s10633-010-9226-1. [DOI] [PubMed] [Google Scholar]
- 312.Chen C., Wu L., Wu D., Huang S., Wen F., Luo G., Long S. The local cone and rod system function in early age-related macular degeneration. Doc. Ophthalmol. 2004;109:1–8. doi: 10.1007/s10633-004-1041-0. [DOI] [PubMed] [Google Scholar]
- 313.Feigl B., Lovie-Kitchin J., Brown B. Objective functional assessment of age-related maculopathy: A special application for the multifocal electroretinogram. Clin. Exp. Optom. 2005;88:304–312. doi: 10.1111/j.1444-0938.2005.tb06714.x. [DOI] [PubMed] [Google Scholar]
- 314.Gerth C., Delahunt P.B., Alam S., Morse L.S., Werner J.S. Cone-mediated multifocal electroretinogram in age-related macular degeneration: Progression over a long-term follow-up. Arch. Ophthalmol. 2006;124:345–352. doi: 10.1001/archopht.124.3.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Gin T.J., Luu C.D., Guymer R.H. Central retinal function as measured by the multifocal electroretinogram and flicker perimetry in early age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2011;52:9267–9274. doi: 10.1167/iovs.11-8517. [DOI] [PubMed] [Google Scholar]
- 316.Hood D.C., Frishman L.J., Saszik S., Viswanathan S. Retinal origins of the primate multifocal ERG: Implications for the human response. Investig. Ophthalmol. Vis. Sci. 2002;43:1673–1685. [PubMed] [Google Scholar]
- 317.Hood D.C., Odel J.G., Chen C.S., Winn B.J. The multifocal electroretinogram. J. Neuroophthalmol. 2003;23:225–235. doi: 10.1097/00041327-200309000-00008. [DOI] [PubMed] [Google Scholar]
- 318.Huang S., Wu D., Jiang F., Ma J., Wu L., Liang J., Luo G. The multifocal electroretinogram in age-related maculopathies. Doc. Ophthalmol. 2000;101:115–124. doi: 10.1023/A:1026587103165. [DOI] [PubMed] [Google Scholar]
- 319.Li J., Tso M.O., Lam T.T. Reduced amplitude and delayed latency in foveal response of multifocal electroretinogram in early age related macular degeneration. Br. J. Ophthalmol. 2001;85:287–290. doi: 10.1136/bjo.85.3.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Parisi V., Perillo L., Tedeschi M., Scassa C., Gallinaro G., Capaldo N., Varano M. Macular function in eyes with early age-related macular degeneration with or without contralateral late age-related macular degeneration. Retina. 2007;27:879–890. doi: 10.1097/IAE.0b013e318042d6aa. [DOI] [PubMed] [Google Scholar]
- 321.Sutter E.E., Tran D. The field topography of ERG components in man—I. The photopic luminance response. Vis. Res. 1992;32:433–446. doi: 10.1016/0042-6989(92)90235-B. [DOI] [PubMed] [Google Scholar]
- 322.Droge W. Free radicals in the physiological control of cell function. Physiol. Rev. 2002;82:47–95. doi: 10.1152/physrev.00018.2001. [DOI] [PubMed] [Google Scholar]
- 323.Pinazo-Durán M.D., Zanón-Moreno V., Gallego-Pinazo R., García-Medina J.J. Chapter 6—Oxidative stress and mitochondrial failure in the pathogenesis of glaucoma neurodegeneration. In: Bagetta G., Nucci C., editors. Progress in Brain Research. Volume 220. Elsevier; Amsterdam, The Netherlands: 2015. pp. 127–153. [DOI] [PubMed] [Google Scholar]
- 324.Toma C., De Cilla S., Palumbo A., Garhwal D.P., Grossini E. Oxidative and nitrosative stress in age-related macular degeneration: A Review of their role in different stages of disease. Antioxidants. 2021;10:653. doi: 10.3390/antiox10050653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Johnson E.J., Vishwanathan R., Johnson M.A., Hausman D.B., Davey A., Scott T.M., Green R.C., Miller L.S., Gearing M., Woodard J., et al. Relationship between serum and brain carotenoids, alpha-tocopherol, and retinol concentrations and cognitive performance in the oldest old from the Georgia Centenarian Study. J. Aging Res. 2013;2013:951786. doi: 10.1155/2013/951786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Johnson E.J. Role of lutein and zeaxanthin in visual and cognitive function throughout the lifespan. Nutr. Rev. 2014;72:605–612. doi: 10.1111/nure.12133. [DOI] [PubMed] [Google Scholar]
- 327.Olk R.J., Peralta E., Gierhart D.L., Brown G.C., Brown M.M. Triple combination therapy and zeaxanthin for the treatment of neovascular age-related macular degeneration: An interventional comparative study and cost-effectiveness analysis. Int. J. Retina Vitr. 2015;1:22. doi: 10.1186/s40942-015-0019-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Rosen R., Vagaggini T., Chen Y., Hu D.N. Zeaxanthin inhibits hypoxia-induced VEGF secretion by RPE cells through decreased protein levels of hypoxia-inducible factors-1alpha. Biomed. Res. Int. 2015;2015:687386. doi: 10.1155/2015/687386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Lima V.C., Rosen R.B., Maia M., Prata T.S., Dorairaj S., Farah M.E., Sallum J. Macular pigment optical density measured by dual-wavelength autofluorescence imaging in diabetic and nondiabetic patients: A comparative study. Investig. Ophthalmol. Vis. Sci. 2010;51:5840–5845. doi: 10.1167/iovs.09-4695. [DOI] [PubMed] [Google Scholar]
- 330.Conti B., Bucolo C., Giannavola C., Puglisi G., Giunchedi P., Conte U. Biodegradable microspheres for the intravitreal administration of acyclovir: In vitro/in vivo evaluation. Eur. J. Pharm. Sci. 1997;5:287–293. doi: 10.1016/S0928-0987(97)00023-7. [DOI] [Google Scholar]
- 331.Jaiswal M., Dudhe R., Sharma P.K. Nanoemulsion: An advanced mode of drug delivery system. 3 Biotech. 2015;5:123–127. doi: 10.1007/s13205-014-0214-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Wu M., Feng Z., Deng Y., Zhong C., Liu Y., Liu J., Zhao X., Fu Y. Liquid antisolvent precipitation: An effective method for ocular targeting of lutein esters. Int. J. Nanomed. 2019;14:2667–2681. doi: 10.2147/IJN.S194068. [DOI] [PMC free article] [PubMed] [Google Scholar]