Summary
Although numerous studies have investigated premature deaths attributable to temperature, effects of temperature on years of life lost (YLL) remain unclear. We estimated the relationship between temperatures and YLL, and quantified the YLL per death caused by temperature in China. We collected daily meteorological and mortality data, and calculated the daily YLL values for 364 locations (2013–2017 in Yunnan, Guangdong, Hunan, Zhejiang, and Jilin provinces, and 2006–2011 in other locations) in China. A time-series design with a distributed lag nonlinear model was first employed to estimate the location-specific associations between temperature and YLL rates (YLL/100,000 population), and a multivariate meta-analysis model was used to pool location-specific associations. Then, YLL per death caused by temperatures was calculated. The temperature and YLL rates consistently showed U-shaped associations. A mean of 1.02 (95% confidence interval: 0.67, 1.37) YLL per death was attributable to temperature. Cold temperature caused 0.98 YLL per death with most from moderate cold (0.84). The mean YLL per death was higher in those with cardiovascular diseases (1.14), males (1.15), younger age categories (1.31 in people aged 65–74 years), and in central China (1.34) than in those with respiratory diseases (0.47), females (0.87), older people (0.85 in people ≥75 years old), and northern China (0.64) or southern China (1.19). The mortality burden was modified by annual temperature and temperature variability, relative humidity, latitude, longitude, altitude, education attainment, and central heating use. Temperatures caused substantial YLL per death in China, which was modified by demographic and regional characteristics.
Keywords: temperature, years of life lost, mortality burden, distributed lag nonlinear model, multivariate meta-analysis, China
Graphical Abstract
Public Summary
-
•
Years of life lost (YLL) is used to estimate the effects of temperature
-
•
Both low and high temperatures can increase the YLLs
-
•
Average 1.02 YLL per death is attributed to temperature exposure
-
•
Temperature causes larger YLLs per death in males, younger people, and central China
Introduction
In the 21st century, climate change presents a global public health concern.1 In the context of climate change, the population around the world is becoming progressively more exposed to extreme temperatures.2 Numerous epidemiological studies have demonstrated the associations between ambient temperature exposure and mortality and morbidity.1,3, 4, 5, 6, 7, 8 These studies have found that temperatures could increase the risks of mortality from cardiovascular, respiratory, cerebrovascular, and other causes.9,10 However, most previous studies used death counts as a health outcome,11 which may not adequately represent the actual mortality burden attributable to temperature, as it provides an equal weight to every death regardless of age. Although all lives are valuable, the loss of young lives results in a larger potential loss of social contributions.12 Therefore, death counts may not capture the whole picture of mortality burden attributable to ambient temperature, which is not helpful for policy prioritization and decision making.
The years of life lost (YLL), an important component of disability-adjusted life years (DALYs), is an indicator of premature mortality. It considers the age at which a death occurs, and gives a greater weight to deaths at younger ages.13 Some studies have argued that the YLL is better than the death count as an indicator when assessing the mortality burden attributed to ambient temperature.14 However, few studies have estimated the exposure-response associations between temperature and YLL.12,15, 16, 17, 18, 19, 20, 21 Moreover, most of these studies employed the daily overall YLL as a health outcome, and did not adjust for the offset effect of population size. As a result, the city- or community-specific association between temperature and YLL cannot be simply combined. Therefore, the extent to which temperature exposure reduces life expectancy needs more examination.
China is the world's most populous country with over 1.4 billion people. In the context of global warming, the annual average surface air temperature in China increased at a rate of 0.32°C per decade during the period from 1961 to 2017, which is higher than the global average (0.12°C/decade) from 1951 to 2010.22,23 It is expected that the ambient temperature in China will continue to increase in the future.23 Many previous studies have also estimated the exposure-response associations of temperatures with death counts in China.9,24,25 However, the temperature-related mortality burden estimated using YLL has not been assessed in China.
In the current study, we employed a national dataset including 364 locations in China to examine the associations between temperature and YLL rates (YLL per 100,000 population) and to quantify the YLL per death attributable to temperature. Our findings will provide deep understanding of the magnitude of adverse health effects caused by ambient temperature, which is important for risk communication and interventions to reduce the mortality burden due to temperatures because YLL is a better indicator than death count to estimate mortality burden attributed to ambient temperature.
Results
General Characteristics of the Study Samples
Table 1 shows the general characteristics of the YLL rates (YLL per 100,000 population) and weather factors in the 364 study locations. The total YLL was 98.8 million, and the mean daily YLL rates for nonaccidental mortality, CVD-, cerebrovascular disease (CED)-, and RESP-related mortality were 22.5, 8.0, 3.9, and 2.2 per 100,000 per day, respectively. Geographically, the largest mean daily YLL rate was observed in central China (24.7), while the lowest was in southern China (21.6). The mean daily temperature, temperature variability, RH, and PM10 were 15.9°C, 9.3°C, 72.4%, and 81.6 μg/m3, respectively. Daily temperature was significantly associated with daily temperature variability (r = −0.13, p < 0.001), RH (r = 0.24, p < 0.001), and PM10 (r = −0.32, p < 0.001) in all included locations. Other characteristics are shown in Table S1 and Figure S5.
Table 1.
General Characteristics of the Study Variables in 364 Locations across China
| Mean (SD) | Minimum | 25th Centile | Median | 75th Centile | Maximum | |
|---|---|---|---|---|---|---|
| Daily nonaccidental YLL ratea | ||||||
| Total | 22.5 (23.4) | 0.0 | 12.0 | 19.5 | 28.5 | 1,020.4 |
| Cardiovascular disease | 8.0 (12.5) | 0.0 | 2.5 | 5.8 | 10.4 | 799.1 |
| CED | 3.9 (6.6) | 0.0 | 0.0 | 2.3 | 5.3 | 324.3 |
| Respiratory disease | 2.2 (4.4) | 0.0 | 0.0 | 1.0 | 3.0 | 620.4 |
| Sex | ||||||
| Male | 26.6 (30.3) | 0.0 | 11.6 | 21.9 | 35.0 | 1,826.0 |
| Female | 18.2 (24.6) | 0.0 | 6.1 | 13.8 | 24.2 | 1,372.5 |
| Age (years) | ||||||
| 0–64 | 13.9 (18.0) | 0.0 | 4.2 | 10.8 | 19.2 | 994.7 |
| 65–74 | 69.7 (100.7) | 0.0 | 0.0 | 54.0 | 97.2 | 4,824.5 |
| ≥75 | 138.2 (142.3) | 0.0 | 66.1 | 119.3 | 182.7 | 5,077.2 |
| Region | ||||||
| Northern | 22.9 (15.9) | 0.0 | 11.8 | 20.4 | 30.7 | 359.0 |
| Central | 24.7 (38.6) | 0.0 | 11.9 | 19.2 | 28.0 | 1,020.4 |
| Southern | 21.6 (15.3) | 0.0 | 12.1 | 19.4 | 28.3 | 928.5 |
| Meteorological variable | ||||||
| Daily mean temperature (°C) | 15.9 (9.9) | −32.3 | 9.5 | 17.5 | 23.4 | 35.6 |
| Daily maximum temperature (°C) | 20.5 (10.0) | −27.2 | 14.1 | 22.3 | 28.1 | 41.2 |
| Daily minimum temperature (°C) | 11.8 (10.4) | −36.2 | 5.3 | 13.2 | 19.8 | 30.7 |
| Temperature variability (°C) | 9.3 (3.9) | 0.3 | 6.3 | 9.4 | 12.3 | 23.2 |
| Daily RH (%) | 72.4 (15.6) | 5.0 | 63.0 | 75.0 | 84.0 | 100.0 |
| PM10 (μg/m3) | 81.6 (41.1) | 8.3 | 51.4 | 76.7 | 103.0 | 767.3 |
YLL rate was the average YLL per 100,000 population.
Exposure-Response Associations of Temperatures with YLL Rates
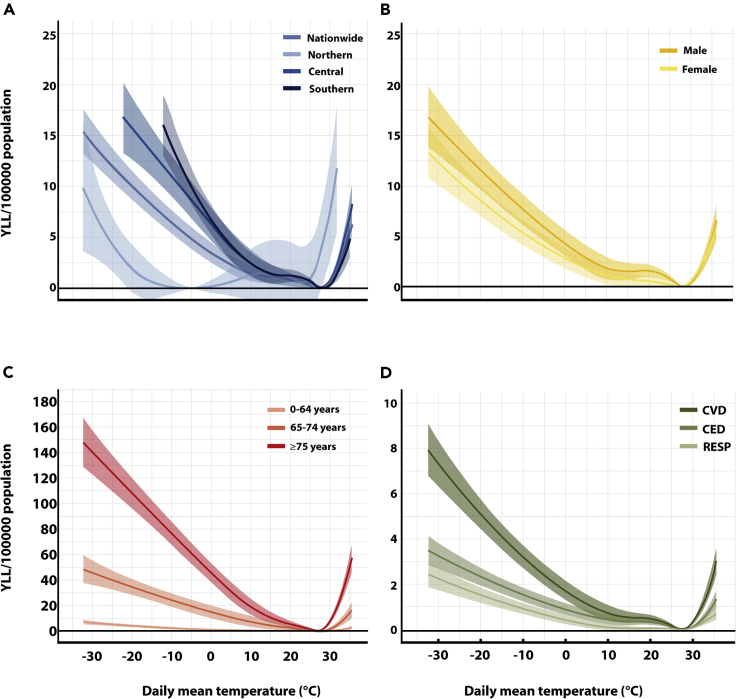
Figure 1 shows a U-shaped cumulative exposure-response relationship between temperatures and YLL rates. The MYT was 27.4°C nationwide with a higher MYT in southern China and a lower MYT in northern China. Cold temperature had a larger impact than hot temperature on the overall YLL rates. The overall YLL rates attributable to cold were greater in low-latitude regions than in high-latitude regions, while reverse patterns were found for heat-related YLL rates. We observed similar association patterns between temperature and cause-specific YLL rates among different geographic regions of China. For instance, cold temperatures had greater effects on the YLL rate from CVD in southern China, and hot temperatures had bigger effects on YLL rates from CVD in northern China. Temperature had a greater impact on YLL rates in males, populations ≥65 years old, and people with CVD than on females, populations ≤65 years old, and those with respiratory disease. The effects of extreme cold were more pronounced and lasted longer than those of extreme heat (Figures S6 and S7).
Figure 1.
Pooled Cumulative Exposure-Response Relationships between Daily Mean Temperature and YLL Rate Over 0–21 Days lag in All 364 Locations and in Different Subgroups across China
Mortality Burden of Temperature Exposures
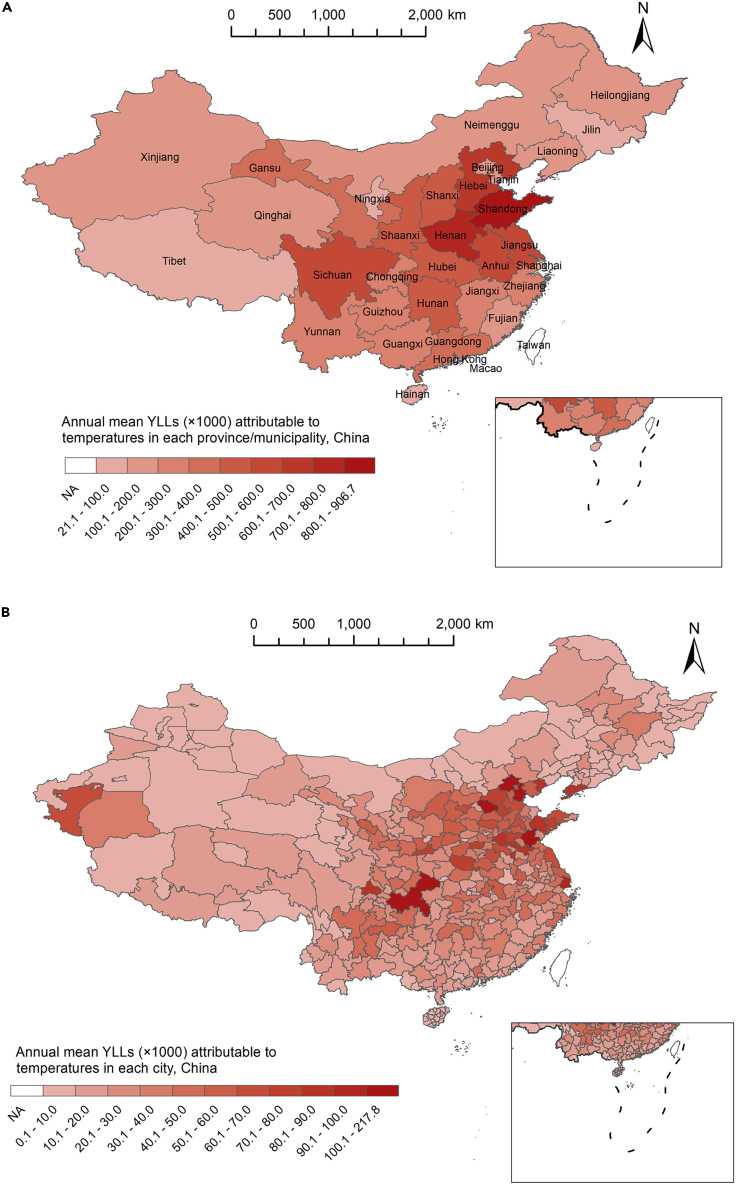
A mean of 1.02 (95% confidence interval [CI], 0.67–1.37) YLL per death was associated with temperature exposures nationwide, out of which 0.98 (95% CI, 0.65, 1.32) years were attributable to cold, particularly moderate cold (0.84; 95% CI, 0.52, 1.16). The mean YLL per death was higher in those with CED (1.37; 95% CI, 0.87, 1.87) or CVD (1.14; 95% CI; 0.77, 1.52) than in those with RESP (0.47; 95% CI, 0.26, 0.67), higher in the younger population (1.31 in people 65–74 years old; 95% CI, 0.75, 1.86) than in the oldest group (0.85 in people ≥75 years old; 95% CI, 0.64, 1.05), and higher in males (1.15; 95% CI, 0.71, 1.59) than in females (0.87; 95% CI, 0.43, 1.31) (Table 2 and S2). We found higher YLL per death in central China (1.34; 95% CI, 0.79, 1.89) than in southern China (1.19; 95% CI, 0.70, 1.68) and northern China (0.64; 95% CI, −0.98, 2.26), which was consistent with the spatial distribution of annual mean YLL attributable to temperatures in China. The highest YLL values were found in Shandong Province (906,700), and the lowest burden was found in Hainan Province (21,100). At the city level, we found that Chongqing city had the largest mortality burden (217,800), and Sansha city in Hannan Province had the lowest mortality burden (20) (Figure 2).
Table 2.
YLL per Death (Years, 95% CI) Attributable to Temperatures in China
| MYT (°C) | Total | Cold | Heat | |
|---|---|---|---|---|
| Causes of death | ||||
| Total mortality | 27.4 | 1.02 (0.67, 1.37) | 0.98 (0.65, 1.32) | 0.04 (0.03, 0.05) |
| CVD | 27.3 | 1.14 (0.77, 1.52) | 1.1 (0.74, 1.46) | 0.05 (0.03, 0.06) |
| CED | 27.6 | 1.37 (0.87, 1.87) | 1.33 (0.84, 1.82) | 0.04 (0.02, 0.05) |
| RESP | 26.8 | 0.47 (0.26, 0.67) | 0.43 (0.24, 0.61) | 0.04 (0.02, 0.06) |
| Geographic regions | ||||
| Northern | −5.2 | 0.64 (−0.98, 2.26) | 0.56 (−0.83, 1.96) | 0.07 (−0.15, 0.3) |
| Central | 27.5 | 1.34 (0.79, 1.89) | 1.28 (0.75, 1.82) | 0.06 (0.04, 0.08) |
| Southern | 28.1 | 1.19 (0.70, 1.68) | 1.16 (0.69, 1.64) | 0.02 (0.01, 0.04) |
| Age of death (years) | ||||
| 0–64 | 27.9 | 1.08 (0.46, 1.71) | 1.04 (0.44, 1.65) | 0.04 (0.02, 0.07) |
| 65–74 | 27.1 | 1.31 (0.75, 1.86) | 1.27 (0.73, 1.81) | 0.03 (0.02, 0.05) |
| ≥75 | 26.8 | 0.85 (0.64, 1.05) | 0.81 (0.62, 1.01) | 0.03 (0.03, 0.04) |
| Sex | ||||
| Male | 27.8 | 1.15 (0.71, 1.59) | 1.12 (0.69, 1.55) | 0.03 (0.02, 0.04) |
| Female | 26.9 | 0.87 (0.43, 1.31) | 0.82 (0.4, 1.24) | 0.05 (0.03, 0.07) |
Figure 2.
Spatial Distribution of Annual Mean YLL Attributable to Temperatures in China
(A) At the provincial level.
(B) At the city level.
Effect Modification Analysis
We observed an increase in YLL per death related to temperatures in locations with moderate annual temperatures, high annual temperature variability, low annual RH, moderate latitude, small longitude, high altitude, and a short central heating period. The urbanization rate, GDP per capita, and education level were found to have weak modification effects on the YLL per death (Figure S8).
Sensitivity Analyses
The associations of temperature with YLL per death were generally robust to the changes in df for seasonality. The cold-attributed YLL rate and MYT reduced with a smaller maximum lag day (Figure S9).
Discussion
In this study, we found that temperatures were associated with an increased YLL rate, and a mean of 1.02 YLL per death was attributable to temperatures nationwide, with most from moderate cold. Higher YLL values per death caused by temperatures were found in individuals with CVD and CED than in individuals with RESP, in those from central China than in those from southern or northern China, in the group aged 65–74 years than in the group aged ≥75 years, and in males than in females. To the best of our knowledge, this is the first study involving a large number of locations and a large population size to estimate the temperature-related premature death indicated by YLL.
Although many studies have estimated the association between temperature and mortality rates,9,25,26 few studies have assessed the relationship between temperature and YLL.12,15, 16, 17, 18 In this study, we used the YLL rate to quantify the association, and observed U-shaped relationships between ambient temperatures and YLL rates with higher cold effects, which is consistent with several previous studies using death counts.27,28 Furthermore, we found higher MYTs and larger cold effects in southern China than in northern China, which also confirmed a similar pattern of minimum mortality temperature (MMT) in previous studies.24,29,30 For example, Ma et al.24 observed in 17 large Chinese cities that the MMT increased with decreasing latitude, with a Spearman correlation coefficient equal to 0.62. The spatial heterogeneity of cold effects is partially due to the differences in geography, adaptative capacity, and climatic characteristics among regions.29,31 For example, people in northern China generally have central heating in the winter season.32 The meta-regression results in this study also showed a lower mortality burden per death in locations with a central heating system than in other locations (Figure S8).
Our study first reported the mean YLL per death caused by temperature. We found that a mean of 1.02 YLL values per death was caused by exposure to temperature during the study period. We also analyzed YLL caused by different components of temperature, and found that cold temperatures, particularly moderate cold temperatures, were mainly responsible for the effects. Using mortality as the outcome, Chen et al.9 also found that moderate cold contributed to the largest fraction (ranging from 64.55% to 80.57%) of total temperature effects with only a small fraction of mortality effects from extreme cold (5.8%–10.16%) or extreme heat (2.73%–4.90%). The large fraction of moderate cold effects is related to the high frequency of moderate cold temperatures and their prolonged lag effects. The results of YLL per death caused by temperatures increase the body of evidence for the public and policy makers to better understand the magnitude of the health effects from temperature exposures and which populations and where are most at risk.
Previous studies based on daily mortality rates have found that exposure to temperature has a greater effect on females than on males.9,10 In contrast, we found a greater YLL per death in males than in females. This result indicates that the impact of temperatures on mortality burden was greater for males than for females.10 The reasons for this sex difference are not totally clear. Compared with females, males are more likely to have poor diets and unhealthy lifestyles, more mental stress, and other aspects of exposure such as occupational exposure to hazardous substances.33 Males therefore may be more susceptible to ambient temperature, and have a shorter life expectancy, which makes higher YLL values for males. In addition, it was suggested that females may have an innate enhanced potential to withstand immune challenges due to more highly activated innate immune pathways,34 which may attenuate the effects of inflammation induced by temperatures.35 Therefore, while using YLL per death as a measure, we should give more attention to males in planning public health interventions to mitigate the impact of temperature.
We also found some significant regional modifiers of YLL per death caused by temperatures, including annual mean temperature, temperature variability, and RH, latitude, longitude, altitude, level of education, and usage of central heating. These findings could not only help explain the spatial heterogeneous of temperature-related effects but also provide important information for policy makers to plan specifically tailored preventive actions to reduce the health impacts of temperatures.
This study also estimated the annual mean mortality burden attributable to temperatures at the province and city level in China, and observed substantial mortality burden caused by temperatures, particularly in central China. These findings have important implications for further understanding of the health impacts of temperatures. In the context of global warning, temperature-related deaths may increase in future in China.36 In addition, the rapid urbanization and population aging process may increase the impacts of temperature on human health.18,37 Therefore, efforts to adapt to climate change and reduce its health impacts are urgently needed in China. Chinese governments have conducted enormous health adaptation efforts to respond to climate change, including adaptation policies, health warning systems, risk communication, and the provision of healthcare and social services.38 However, there remain challenges for adaptation to climate change in China. For example, the integration or better collaboration across multiple government departments and improved community participation are needed to advance adaptation to climate change, and more research on adaptation interventions and their benefits and negative impacts is needed.
Strength and Limitations
The present study has several strengths. First, this study employed a large database with good-quality data, which increases the generalizability of our findings. Second, we applied a population-adjusted YLL rate to estimate the associations of temperature with the YLL rate, which was used to combine temperature effects across locations. Third, we estimated the mean YLL per death resulting from temperature. These measures provide novel insights because they provide an intuitive understanding of the health impact of temperature.
This study also has several limitations. First, similar to many previous studies, it was inherently an ecological study. Our findings should thus be interpreted with caution. Second, more locations were selected in several southern provinces in China, which may lead to selection bias in the results, such as the MYT and meta-regression results, since these five provinces may have more weight than the other provinces. For example, the higher MYT found in this study than in previous studies may be related to the unbalanced selection of locations.4,9 Third, climate change is a global public health concern. The present study included only locations in China (except for Hainan Province), which may limit the generalizability of our findings to other countries and regions. Fourth, we divided all study locations into three major zones based on their latitudes, which may potentially mask the difference in climate variability between provinces within the same zone. However, a meta-regression analysis was used to examine the effects of several location-level characteristics on the association of temperature with YLL rates. Fifth, we did not include the same study period in all locations due to the unavailability of mortality data. However, a study conducted in Shanghai indicated that both hot and cold effects on mortality did not substantially change during 2001–2012.39 Sixth, cancer is ranked top in the cause-of-death spectrum across many countries in the world.40 However, we did not estimate the association of temperature with cancer mortality in this study because daily cancer mortality data were not collected. Finally, the study locations were selected from both the DSPS and provincial mortality surveillance system. Although the provincial mortality surveillance system followed the DSPS standards, disparity between the two systems may potentially lead to bias.
Conclusions
Temperatures, especially moderate cold, have been found to be associated with substantial mortality burden of 1.02 YLL per death in China. The mortality effects of temperatures were modified by demographic and regional characteristics. Our findings add to the increasing body of knowledge to better inform policy making and adaptation intervention in the context of climate change.
Materials and Methods
Study Location Selection
Study locations in Yunnan, Guangdong, Hunan, Zhejiang, and Jilin provinces during 2013–2017 were selected from provincial mortality surveillance systems. Locations in other provinces during 2006–2011 were obtained from China's Disease Surveillance Points System (DSPS) (see the Appendix).25,41 The DSPS is administered by the Chinese Center for Disease Control and Prevention (China CDC), and the provincial mortality surveillance system was administered by the provincial CDC following the same protocol as that of DSPS. At each surveillance point, all deaths certified by clinical doctors or local CDC professionals are reported to the DSPS using an internet-based reporting system. The data from the DSPS have been widely applied in policy making and disease burden assessment.9,25,42
To ensure adequate statistical power, study locations from both provincial surveillance systems and DSPS were selected if they met either or both criteria: (1) a population size >200,000, and (2) an annual mortality rate >4‰.25 We set these two criteria because time-series analyses depend on both good quality of mortality data and adequate daily number of deaths. A total of 364 locations were selected and categorized into three groups:43 northern China (latitude ≥40°; 46 locations), central China (latitude ≥30° and <40°; 72 locations), and southern China (latitude <30°; 246 locations) (Figure S1). A total of 203.7 million people permanently live in the study locations.42
Data Collection
Daily nonaccidental mortality data during 2013–2017 were obtained from the corresponding provincial CDCs in the above five provinces. However, we only obtained the daily mortality data during 2006–2011 in locations beyond the five provinces.25 Therefore, there are two study periods in this study. The population and mortality data of all provinces were obtained from the 6th national population census conducted in 2010 (Census data: http://www.stats.gov.cn), which was used to calculate male and female life tables (<1 year, 1–4 years, and every 5 years from ages 5 to 100+ years) of each province using the methods provided by the World Health Organization.44 We then calculated the individual YLL by matching the death age and sex of each individual record to the province-specific life table. All deaths were classified into groups according to the International Classification of Diseases, 10th revision (ICD-10) categories: nonaccidental causes (codes: A00-R99), cardiovascular disease (CVD, codes I00-I99), respiratory disease (RESP, codes J00-J98), and cerebrovascular disease (RED, codes I60–I69). The daily total YLL for each cause was calculated by summing the YLL for all deaths on the same day. We also calculated the daily YLL by sex and age group (0–64 years, 65–74 years, and ≥75 years).
The annual mean population size during 2013–2017 for each study location in the five provinces was obtained from national or local statistical yearbooks, and population data for the other study locations were extracted from the 6th national population census, conducted in 2010 (Census data: http://www.stats.gov.cn). Based on these data, we calculated the daily YLL rate (YLL per 100,000 population) by dividing the daily recorded YLL by the corresponding population size of each location, which was used to estimate the association of temperature with YLL. Then, the association in every location was combined in a multivariate meta-analysis model. We also collected the annual mean population size during 2013–2017 for each city in China, which was used to estimate the total mortality burden in China.
Daily meteorological data including mean temperature and relative humidity (RH) from 698 weather stations across China were extracted from the China Meteorological Data Sharing Service System (Weather data: http://data.cma.cn/). We employed the Australian National University Splines (ANUSPLIN) thin plate smoothing software to interpolate the daily mean temperature, TMax, TMin, and RH at a 0.01 ° × 0.01 ° resolution across China. The results of 10-fold cross-validation showed that the R2 values of the daily mean temperature, TMax, TMin, and RH were 0.96, 0.94, 0.94, and 0.81, respectively, and the corresponding root mean squared errors (RMSEs) were 2.37°C, 2.8°C, 2.8°C, and 7.7%. These results suggest good prediction accuracy of the interpolation method (see the Appendix).45 We obtained the daily mean temperature, TMax, TMin, and RH of the grids where each selected location overlapped. We then calculated the daily temperature variability by estimating the standard deviation of daily maximum and minimum temperatures (TMaxlag0, TMaxlag1, TMinlag0, and TMinlag1) of the preceding 2 days.46 Here, we calculated the daily temperature variability as a potential cofounder of mean temperature, because previous studies showed that temperature variability was also an independent risk factor for mortality.46,47
The values of the daily mean particulate matter with an aerodynamic diameter of 10 μm or less (PM10) during 2006–2017 were obtained from the China National Environmental Monitoring Center. Since some studied locations were not covered by the air quality monitoring system, we employed a land-use-regression model to assess the daily PM10 value at each location using the following predictors: daily mean temperature, daily RH, latitude, longitude, altitude, population density, road density, types of land use, and gross domestic product (GDP) per capita. The fitness results showed that the R2 was 73.90%, and the RMSE was 16.49 μg/m3. The method has been described in our previous study48 (see the Appendix).
The GDP per capita in 2010 for each location was obtained from the Data Center for Resources and Environmental Sciences (GDP data: http://www.resdc.cn). Other 2010 city-level characteristics, including the urbanization rate, mean years of education, and use of central heating, were collected from national and provincial statistical yearbooks.
We collected the daily mean temperatures, population size, and its components in each city during 2013–2017, using the same methods mentioned above. Based on the regional exposure-response associations between temperatures and the YLL rate in 364 locations, we estimated the annual mean YLL attributable to temperatures in each city in China.
Statistical Analysis
We used a two-stage approach in our study. In the first stage, we used a distributed lag nonlinear model (DLNM) linked with a Gaussian distribution function to estimate the associations of temperature with the YLL rate in each location.49 A cross-basis function was introduced to model the nonlinear and lag associations of temperature and temperature variability with the YLL rate, in which the temperature variability was adjusted for as a potential confounder. The DLNM can optimally adjust for other confounders, including those that change slowly over time expressed as seasonality, day of the week (DOW), other meteorological factors (e.g., RH), and air pollutants (e.g., PM10). We employed a natural cubic B-spline (ns) of time with seven degrees of freedom (df) per year to control for the seasonal and long-term trends in mortality, a categorical variable to control for the DOW, and a linear model to control for the same day PM10 concentration. An ns was also employed to adjust for the potential confounding effect of the present day RH with three df in the ns function, which can estimate the nonlinear effects of the RH on the YLL rate in the same day.9 We used 21 days as the maximum lag period for both mean temperature and temperature variability.4,25,46,48,50
In the second stage, we employed a multivariate meta-analysis to combine the location-specific cumulative associations of temperatures with the YLL rate at 21 lag days.51 The MYT (minimum YLL temperature) was identified in the combined curves of the YLL rate with temperature (see the Appendix).
Based on the overall cumulative YLL rate of temperature devised from the combined curve, we estimated the mean YLL per death caused by temperature and its components. We divided daily mean temperatures into four components, namely extreme cold, moderate cold, moderate heat, and extreme heat (defined as ≤2.5th percentile, the 2.5th percentile to the MYT, MYT to the 97.5th percentile, and >97.5th percentile of temperature, respectively). Similarly, we applied regional cumulative exposure-response associations between temperature and YLL rate to the daily mean temperatures and population data in each city (see the Appendix).
A univariable meta-regression model was employed to explore the impacts of location-level characteristics on YLL per death caused by temperature. These location-level variables included were the urbanization rate, mean years of education, annual mean temperature, annual mean temperature variability, annual mean RH, latitude, longitude, altitude, GDP per capita, and central heating.
All analyses were performed using R software (version 3.5.0, R Foundation for Statistical Computing, Vienna, Austria). The dlnm and mvmeta packages were the primary packages used. Two-tailed p values < 0.05 were considered to be statistically significant. All codes are available at https://github.com/gztt2002/YLL-of-Tm-and-Tv.
Sensitivity Analyses
A series of sensitivity analyses were conducted to test the robustness of the estimates nationwide. We employed alternative maximum lag periods of 14 and 28 days, and changed the df of time from 6 to 8 per year.
Web Resources
The mortality data can only be applied for through a government data sharing portal (www.phsciencedata.cn/Share/edtShare.jsp) or from the provincial mortality surveillance system. Data on the environment and location characteristics are available on the government's statistic yearbooks or websites listed in the methods section. All codes were available in https://github.com/gztt2002/YLL-of-Tm-and-Tv.
Ethical Approval
This study was approved by the Ethics Committee of Guangdong Provincial Center for Disease Control and Prevention (2019025). Data were analyzed at aggregate level and no participants were contacted.
Acknowledgments
We thank Professor Antonio Gasparrini for providing assistance during statistical analysis. This work was supported by the National Key Research and Development Program of China (2018YFA0606200), Guangzhou Science and Technology Project (201704020194), and the Guangdong Health Innovation Platform. The funders were not involved in the research and preparation of the article, including study design; collection, analysis, and interpretation of data; writing of the article; and the decision to submit it for publication.
Author Contributions
T.L., C.Z., H.Z., and B.H. are joint first authors. W.M. (mawj@gdiph.org.cn), M.Y., and M.Z. contributed equally to the correspondence work. W.M., M.Z., M.Y., C.Z., H.Z., and B.H. set up the collaborative network. T.L., C.Z., H.Z., and B.H. performed the statistical analysis and took the lead in drafting the manuscript and interpreting the results. T.L. provided substantial scientific insight into the interpretation of the results and drafting of the manuscript. Yanjun Xu, L.L., L.W., R.H., Z.H., Y. Xiao, J.L., X.X., D.J., M.Q., Q.Z., W.G., P.Y., Yiqing Xu, J.H., J.X., W.Z., X.L., S.C., L.G., Z.R., Y.Z., C.H., Y.D., S.R., and Y.G. provided the data and contributed to the interpretation of the results and the preparation of the submitted version of the manuscript. All authors contributed to the development of the manuscript and approved the final draft. W.M., M.Y., and M.Z. are study guarantors. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Declaration of Interests
The authors declare no competing interests.
Published Online: December 14, 2020
Footnotes
Supplemental Information can be found online at https://doi.org/10.1016/j.xinn.2020.100072.
Contributor Information
Min Yu, Email: myu@cdc.zj.cn.
Maigeng Zhou, Email: maigengzhou@126.com.
Wenjun Ma, Email: mawj@gdiph.org.cn.
Supplemental Information
References
- 1.Field, C.B., Barros, V.R., Dokken, D.J., et al. (2014). IPCC, 2014: Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the e Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom and New York, NY, USA.
- 2.Nick W., Markus A., Nigel A., et al. The 2019 report of the Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394:1836–1878. doi: 10.1016/S0140-6736(19)32596-6. [DOI] [PubMed] [Google Scholar]
- 3.Watts N., Adger W.N., Ayebkarlsson S., et al. The Lancet Countdown: tracking progress on health and climate change. Lancet. 2017;389:1151–1164. doi: 10.1016/S0140-6736(16)32124-9. [DOI] [PubMed] [Google Scholar]
- 4.Gasparrini A., Guo Y., Hashizume M., et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386:369–375. doi: 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Achebak H., Devolder D., Ballester J. Trends in temperature-related age-specific and sex-specific mortality from cardiovascular diseases in Spain: a national time-series analysis. Lancet Planet. Health. 2019;3:e297–e306. doi: 10.1016/S2542-5196(19)30090-7. [DOI] [PubMed] [Google Scholar]
- 6.Fu S.H., Gasparrini A., Rodriguez P.S., et al. Mortality attributable to hot and cold ambient temperatures in India: a nationally representative case-crossover study. Plos Med. 2018;15:e1002619. doi: 10.1371/journal.pmed.1002619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Medina-Ramón M., Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatisation and effect modification in 50 US cities. Occup. Environ. Med. 2007;64:827–833. doi: 10.1136/oem.2007.033175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ye X., Wolff R.C., Yu W., et al. Ambient temperature and morbidity: a review of epidemiological evidence. Environ. Health Perspect. 2011;120:19–28. doi: 10.1289/ehp.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen R., Yin P., Wang L., et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ. 2018;363:k4306. doi: 10.1136/bmj.k4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang Z., Lin H., Liu Y., et al. Individual-level and community-level effect modifiers of the temperature–mortality relationship in 66 Chinese communities. BMJ Open. 2015;5:e009172. doi: 10.1136/bmjopen-2015-009172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benmarhnia T., Deguen S., Kaufman J.S., et al. Vulnerability to heat-related mortality: a systematic review, meta-analysis, and meta-regression analysis. Epidemiology. 2015;26:781–793. doi: 10.1097/EDE.0000000000000375. [DOI] [PubMed] [Google Scholar]
- 12.Sewe M., Bunker A., Ingole V., et al. Estimated effect of temperature on years of life lost: a retrospective time-series study of low-, middle-, and high-income regions. Environ. Health Perspect. 2018;126:017004. doi: 10.1289/EHP1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steenland K., Armstrong B. An overview of methods for calculating the burden of disease due to specific risk factors. Epidemiology. 2006;17:512–519. doi: 10.1097/01.ede.0000229155.05644.43. [DOI] [PubMed] [Google Scholar]
- 14.Dalys G., Collaborators H. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1260–1344. doi: 10.1016/S0140-6736(17)32130-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang J., Ou C., Guo Y., et al. The burden of ambient temperature on years of life lost in Guangzhou, China. Sci. Rep. 2015;5:12250. doi: 10.1038/srep12250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang C., Barnett A.G., Wang X., et al. Effects of extreme temperatures on years of life lost for cardiovascular deaths: a time series study in Brisbane, Australia. Circ. Cardiovasc. Qual. Outcomes. 2012;5:609–614. doi: 10.1161/CIRCOUTCOMES.112.965707. [DOI] [PubMed] [Google Scholar]
- 17.Luan G., Yin P., Li T., et al. The years of life lost on cardiovascular disease attributable to ambient temperature in China. Sci. Rep. 2017;7:13531. doi: 10.1038/s41598-017-13225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu T., Ren Z., Zhang Y., et al. Modification effects of population expansion, ageing, and adaptation on heat-related mortality risks under different climate change scenarios in Guangzhou, China. Int. J. Environ. Res. Public Health. 2019;16:376. doi: 10.3390/ijerph16030376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y., Yu C., Peng M., et al. The burden of ambient temperature on years of life lost: a multi-community analysis in Hubei, China. Sci. Total Environ. 2018;621:1491–1498. doi: 10.1016/j.scitotenv.2017.10.079. [DOI] [PubMed] [Google Scholar]
- 20.Xu X., Chen Z., Huo X., et al. The effects of temperature on human mortality in a Chinese city: burden of disease calculation, attributable risk exploration, and vulnerability identification. Int. J. Biometeorol. 2019;63:1319–1329. doi: 10.1007/s00484-019-01746-6. [DOI] [PubMed] [Google Scholar]
- 21.Li G., Guo Q., Liu Y., et al. Projected temperature-related years of life lost from stroke due to global warming in a temperate climate city, Asia: disease burden caused by future climate change. Stroke. 2018;49:828–834. doi: 10.1161/STROKEAHA.117.020042. [DOI] [PubMed] [Google Scholar]
- 22.Stocker T.F., Qin D., Plattner G.-K., et al. Cambridge University Press; 2013. IPCC, 2013: Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. [Google Scholar]
- 23.Wang C., Zhao L. Springer Press; 2019. Overview of Climate Change in China. [Google Scholar]
- 24.Ma W., Chen R., Kan H. Temperature-related mortality in 17 large Chinese cities: how heat and cold affect mortality in China. Environ. Res. 2014;134:127–133. doi: 10.1016/j.envres.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 25.Ma W., Wang L., Lin H., et al. The temperature–mortality relationship in China: an analysis from 66 Chinese communities. Environ. Res. 2015;137:72–77. doi: 10.1016/j.envres.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 26.Gasparrini A., Guo Y., Hashizume M., et al. Temporal variation in heat-mortality associations: a multicountry study. Environ. Health Perspect. 2015;123:1200–1207. doi: 10.1289/ehp.1409070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luan G., Yin P., Wang L., et al. Association between ambient temperature and chronic obstructive pulmonary disease: a population-based study of the years of life lost. Int. J. Environ. Health Res. 2018;29:246–254. doi: 10.1080/09603123.2018.1533533. [DOI] [PubMed] [Google Scholar]
- 28.Egondi T., Kyobutungi C., Rocklov J. Temperature variation and heat wave and cold spell impacts on years of life lost among the urban poor population of Nairobi, Kenya. Int. J. Environ. Res. Public Health. 2015;12:2735–2748. doi: 10.3390/ijerph120302735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guo Y., Li S., Zhang Y., et al. Extremely cold and hot temperatures increase the risk of ischaemic heart disease mortality: epidemiological evidence from China. Heart. 2013;99:195–203. doi: 10.1136/heartjnl-2012-302518. [DOI] [PubMed] [Google Scholar]
- 30.Li Y., Cheng Y., Cui G. Association between high temperature and mortality in metropolitan areas of four cities in various climatic zones in China: a time-series study. Environ. Health. 2014;13:65. doi: 10.1186/1476-069X-13-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderson B.G., Bell M.L. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20:205–213. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen Y., Ebenstein A., Greenstone M., et al. Evidence on the impact of sustained exposure to air pollution on life expectancy from China’s Huai River policy. Proc. Natl. Acad. Sci. USA. 2013;110:12936–12941. doi: 10.1073/pnas.1300018110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Du H., Li L., Bennett D., et al. Fresh fruit consumption and major cardiovascular disease in China. N. Engl. J. Med. 2016;374:1332–1343. doi: 10.1056/NEJMoa1501451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shani T.G., Barbara M., Hideyuki Y., et al. ImmGen report: sexual dimorphism in the immune system transcriptome. Nat. Commun. 2019;10:4295. doi: 10.1038/s41467-019-12348-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paolo G., Paolo D.G., Marco P., et al. Climate changes and human health: a review of the effect of environmental stressors on cardiovascular diseases across epidemiology and biological mechanisms. Curr. Pharm. Des. 2017;23:3247–3261. doi: 10.2174/1381612823666170317143248. [DOI] [PubMed] [Google Scholar]
- 36.Zhang B., Li G., Ma Y., et al. Projection of temperature-related mortality due to cardiovascular disease in Beijing under different climate change, population, and adaptation scenarios. Environ. Res. 2018;162:152–159. doi: 10.1016/j.envres.2017.12.027. [DOI] [PubMed] [Google Scholar]
- 37.Sun R., Cao H., Zhu X., et al. Current aging research in China. Protein Cell. 2015;6:314–321. doi: 10.1007/s13238-015-0145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He Y., Ma R., Ren M., et al. Springer Press; 2019. Public Health Adaptation to Heat Waves in Response to Climate Change in China. [Google Scholar]
- 39.Yang C., Meng X., Chen R., et al. Long-term variations in the association between ambient temperature and daily cardiovascular mortality in Shanghai, China. Sci. Total Environ. 2015;538:524–530. doi: 10.1016/j.scitotenv.2015.08.097. [DOI] [PubMed] [Google Scholar]
- 40.Global Burden of Disease Cancer Collaboration. Fitzmaurice C., Allen C., et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study. JAMA Oncol. 2019;5:1749–1768. doi: 10.1001/jamaoncol.2019.2996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu S., Wu X., Lopez A.D., et al. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ. 2016;94:46–57. doi: 10.2471/BLT.15.153148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhou M., Wang H., Zhu J., et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 43.Xiao J., Peng J., Zhang Y., et al. How much does latitude modify temperature–mortality relationship in 13 eastern US cities? Int. J. Biometeorol. 2014;59:1–8. doi: 10.1007/s00484-014-0848-y. [DOI] [PubMed] [Google Scholar]
- 44.World Health Organization Global Health Observatory data repository: life tables by country, China. 2013. http://apps.who.int/gho/data/?theme=main&vid=60340
- 45.Hutchinson M.F., Xu T. ANUSPLIN VERSION 4.4 USER GUIDE. The Australian national University, Fenner School of environment and Society, Canberra, Australia. 2013. http://fennerschool.anu.edu.au/files/anusplin44.pdf
- 46.Guo Y., Gasparrini A., Armstrong B.G., et al. Temperature variability and mortality: a multi-country study. Environ. Health Perspect. 2016;124:1554–1559. doi: 10.1289/EHP149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheng J., Xu Z., Bambrick H., et al. Impacts of heat, cold, and temperature variability on mortality in Australia, 2000-2009. Sci. Total Enviro. 2019;651:2558–2565. doi: 10.1016/j.scitotenv.2018.10.186. [DOI] [PubMed] [Google Scholar]
- 48.Chen S., Hu J., Gong W., et al. Developing a novel indicator to estimate years of life lost attributable to temperature variability between neighboring days. 2020. https://iopscience.iop.org/article/10.1088/1748-9326/abb10c
- 49.Gasparrini A., Armstrong B., Kenward M.G. Distributed lag non-linear models. Stat. Med. 2010;29:2224–2234. doi: 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang Y., Xiang Q., Yu C., et al. Mortality risk and burden associated with temperature variability in China, United Kingdom and United States: comparative analysis of daily and hourly exposure metrics. Environ. Res. 2019;179:108771. doi: 10.1016/j.envres.2019.108771. [DOI] [PubMed] [Google Scholar]
- 51.Gasparrini A., Armstrong B., Kenward M.G. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat. Med. 2012;31:3821–3839. doi: 10.1002/sim.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.