Abstract
Anxiety is experienced in response to threats that are distal or uncertain, involving changes in one’s subjective state, autonomic responses, and behavior. Defensive and physiologic responses to threats that involve the amygdala and brainstem are conserved across species. While anxiety responses typically serve an adaptive purpose, when excessive, unregulated, and generalized, they can become maladaptive, leading to distress and avoidance of potentially threatening situations. In primates, anxiety can be regulated by the prefrontal cortex (PFC), which has expanded in evolution. This prefrontal expansion is thought to underlie primates’ increased capacity to engage high-level regulatory strategies aimed at coping with and modifying the experience of anxiety. The specialized primate lateral, medial, and orbital PFC sectors are connected with association and limbic cortices, the latter of which are connected with the amygdala and brainstem autonomic structures that underlie emotional and physiological arousal. PFC pathways that interface with distinct inhibitory systems within the cortex, the amygdala, or the thalamus can regulate responses by modulating neuronal output. Within the PFC, pathways connecting cortical regions are poised to reduce noise and enhance signals for cognitive operations that regulate anxiety processing and autonomic drive. Specialized PFC pathways to the inhibitory thalamic reticular nucleus suggest a mechanism to allow passage of relevant signals from thalamus to cortex, and in the amygdala to modulate the output to autonomic structures. Disruption of specific nodes within the PFC that interface with inhibitory systems can affect the negative bias, failure to regulate autonomic arousal, and avoidance that characterize anxiety disorders.
Subject terms: Anxiety, Brain
Introduction
Anxiety is a state experienced in response to threats that are either distal or uncertain, and involves changes in an individual’s subjective state, behavior and physiology [1–3] that facilitate detection of a potential threat within the environment. These behavioral and physiological changes, which are collectively referred to as defensive responses [4], are conserved across species [5, 6], facilitating the use of translational models to characterize defensive circuitry. Decades of work, both in humans and animal models, converges upon a conserved set of brain regions necessary for executing adaptive defensive responses. This circuit includes the amygdala and other subcortical structures, which are necessary for identifying and coordinating behavioral and physiological responses to threats [1, 3].
The human brain is characterized by the significant expansion of association cortex, particularly the PFC. This expansion is thought to underlie the rich and elaborate subjective experience of anxiety in humans, as well as the capacity to engage in high-level strategies to regulate anxiety-associated responses [7]. While these PFC-based capabilities increase an organism’s chance for adaptive success within the environment, they also provide a more complex substrate upon which disordered processes can emerge [8], as is the case in anxiety disorders. Anxiety disorders are among the most prevalent psychiatric disorders and, as they emerge relatively early in life [9–11], can be chronic and recurrent across the lifespan, leading to a significant disease burden [12, 13].
Clarifying the role of the PFC in anxiety disorders has proven challenging, in part because the PFC is engaged across a broad range of anxiety-related neural processes. Here, we propose that the human PFC plays a role in predicting the likelihood of threats in the environment, using information aggregated from a variety of cortical and subcortical processing streams. Persistent biases towards threat prediction, leading to over-engagement of defensive systems, states of anxiety, and ultimately, avoidance, can create a self-reinforcing loop that influences the way anxious individuals gather and process information relevant to threat. First, we consider the organization of the frontal lobe, with a particular focus on the significant expansion of this lobe in primates. We discuss core symptoms associated with anxiety disorders and link these symptoms to aberrant prefrontal function. Finally, we consider how anatomical principles derived from studies in nonhuman primates (NHPs) can provide insight into the circuit basis for maladaptive cortical function in the context of anxiety.
Anxiety as an evolutionarily conserved, adaptive process
In general, the state of anxiety and the accompanying behavioral and physiological alterations serve an adaptive function. For example, hypervigilant scanning of the environment increases the likelihood of early threat detection, and can help an organism to engage the appropriate defensive strategy based on the proximity of the threat [14, 15]. However, when experienced in a manner that is extreme, out of context, and distressing, these responses can become maladaptive, interfering with an individual’s potential to engage with the world in the desired way. Indeed, extreme and inappropriate anxiety is a core feature of anxiety disorders. It is worth noting, however, that the source of anxiety is often related to an adaptive function (e.g., social interactions are critical for maintaining status within a group, but are the focus of anxiety in social phobia). A key challenge is understanding how and why these adaptive processes become disordered, producing distress and suffering. Central to this question is defining the boundaries between adaptive and pathological anxiety (see Box 1).
Characterization of the neural substrates of anxiety disorders can help guide the development of new treatments targeting mechanisms and pathophysiology. Animal models are essential in this regard, as they allow for specific manipulations of cells, molecules, and pathways within brain regions linked to anxiety [5, 16]. Much of the circuitry underlying defensive responses is conserved within model organisms, albeit with specializations unique to the environmental niche of the species [17], and has been described in several recent reviews [17–20]. For example, conserved across species, brainstem components of the defensive circuit, such as the periaqueductal grey, participate in the coordination of escape and freezing responses [21, 22]. These brainstem regions can be regulated by the amygdala which can respond to innate stimuli, and through associative learning processes [1, 23], can influence the selection and expression of defensive responses based on learned contingencies.
On the other hand, the structure and connections of frontal regions are less conserved. The rodent PFC is composed of agranular or dysgranular (limbic) cortex [24, 25]. From an evolutionary perspective, it is clear that both mice and rats, the most commonly used species, have a frontal cortical region that serves analogous functions to that of the primate PFC, particularly the agranular cortices within the cingulate gyrus [26–28]. Within rodent PFC, there are differentiated subdivisions that are specialized, preferentially supporting particular domains of functions (i.e., attention, reinforcement learning, etc.) via connections with subcortical structures, such as the amygdala and striatum [29–31]. Rodent models have made invaluable contributions in understanding how interactions among brains regions mediate defensive responses (see [14, 23, 32]). However, it is important to acknowledge the limitations of non-primate species in modeling features of human pathological anxiety, particularly with respect to functions subserved by the highly differentiated, granular portions of the primate PFC [27], which have no clear homolog in rodents.
In NHPs and humans, there is a marked expansion and reorganization of the PFC (reviewed in [33]), particularly the lateral and anterior granular portions [34], as well as within the anterior and midcingulate cortices [26, 27]. This expansion is thought to underlie the more complex regulatory strategies which humans and NHPs can engage to modulate subcortical portions of the defensive circuitry, as well as mediating components of the subjective states associated with anxiety. This prefrontal expansion, along with the existence of evolutionarily conserved, anxiety-related temperaments [5, 6, 16, 35, 36], supports the use of NHPs as a critical translational bridge between rodents and humans, particularly with respect to understanding symptoms of stress-related psychopathology linked to the PFC (for further discussion see Preuss and Wise, this volume, Chapter 1).
Box 1 Diagnosis in anxiety disorders.
The field of psychiatry has historically relied on categorical diagnoses (disordered versus healthy) to define the boundaries of anxiety and other psychiatric disorders, based on the combined presence of subsets of symptoms leading to functional impairment. Codified within the Diagnostic and Statistical Manual (DSM), there are several distinct diagnoses that comprise the Anxiety Disorder Category [284]. For the purposes of the current review, we limit our discussion of prefrontal-related dysfunction in relation to the major anxiety disorders defined within the DSM V: separation anxiety disorder (SAD), social phobia/social anxiety disorders, specific phobia, generalized anxiety disorder (GAD), and panic disorder (PD). These disorders have shared and unique features, primarily differing in relation to triggering stimuli, as well as the prominence and focus of different symptoms [285].
Despite the different manifestations, comorbidity among anxiety disorders (and, indeed, among all psychiatric disorders), is more of the rule than the exception [10, 286, 287]. Rates of comorbidity between anxiety disorders and other internalizing disorders, such as depression, are high across the lifespan [288] and this comorbidity negatively influences the rate of successful treatment [289, 290]. Additionally, there is generally a high degree of overlap between the brain regions implicated across diagnoses. A recent meta-analysis (see Fig. 1) combined scans from over 2,000 patients with various anxiety disorder diagnoses (GAD, PD, specific phobia, and social phobia). Hyperactivation in the insula and cingulate cortex, among other regions, was evident when data were pooled across diagnoses [188], a finding which is in line with previous meta-analyses [291]. Interestingly, some diagnostic differences were present: when analyzed independently for each diagnosis, deactivation was reported in the dACC for GAD, while hyperactivation of this region was reported in specific phobia [188], suggesting that some of the differences in symptoms displayed across disorders may be reflective of distinct dysfunction within cortical regions.
By nature, findings from meta-analyses are reliable and may be broadly applicable [292], but are constrained by several factors. Common task designs, such as the viewing of emotional faces, facilitate the cross-study aggregation of data necessary for meta-analyses. However, the utility and generalizability of these relatively simple tasks in relation to understanding the more complicated symptoms of psychopathology is unclear [293]. Smaller studies, which can use more involved tasks to selectively probe for various neural correlates of psychological and cognitive constructs, can reveal context-specific alterations in specific processes that otherwise may not be reflected when data from numerous studies are combined. Additionally, these smaller studies can be designed to capture anxiety responses to disorder-specific stimuli, as in [294], where prompts specific to the negative self-beliefs of individual participants were used to monitor emotion regulation success in the scanner. These and other more complex tasks can be useful in parsing symptom and disorder-specific neural correlates of anxiety disorders.
The prevalence of diagnostic [295, 296] and brain-based [188, 291, 297] overlaps suggest that the current diagnostic nosology may not reflect distinct underlying pathophysiological processes. Because of this, the field of psychiatry has begun to embrace dimensional approaches to complement diagnostic boundaries, which frame constructs associated with psychiatric disorders as continuous variables that span the population. This dimensional characterization is also in line with understanding the symptoms of anxiety disorders as extreme representations of adaptive traits. Perhaps the most prominent example is the Research Domain Criteria (RDoC; [298, 299], a research framework that encourages the probing of several core constructs related to mental illness at various levels of analysis (circuits, molecules, etc.). Most relevant to anxiety disorders are RDoC constructs contained within the Negative Valence Systems, including anxiety, fear, and sustained threat.
Dimensional approaches have not been restricted to the RDoC framework: many are moving beyond categorical approaches and incorporating dimensionality into their study of anxiety disorders [300, 301]. Novel approaches, based on factor analysis applied to transdiagnostic dimensional constructs have also become popular in recent years. Prominent among them is the Hierarchical Taxonomy of Psychopathology (HiTOP), which attempts to derive a hierarchical structure of psychopathology based on empirically derived clusters of disease features [302, 303]. For example, in the framework of HiTOP, social anxiety is considered, not as a disorder, but as a dimensional variable couched within the spectrum of internalizing [304].
Structure and function of the PFC in primates
The PFC is not a unitary entity. Functional specializations within regions of the PFC, which are delineated based on anatomical connectivity and laminar structure, make different contributions to processing related to anxiety [37]. Broadly, the PFC can be divided into lateral, orbital, and medial sectors, based on their architecture, global patterns of connectivity, and participation in functionally distinct networks (Fig. 1, reviewed in [38]). The phylogenetically conserved limbic cortex, which in rodents is the entirety of the PFC, in primates encompasses the anterior cingulate cortex (ACC) and posterior orbitofrontal cortex (pOFC). In primates, these regions are contiguous with the expanded granular cortex.
Fig. 1. Parcellation and threat-related activation in nonhuman primates and humans.
Top panel: Cytoarchitectonic parcellations of the human and rhesus monkey PFC, adapted from [282] with permission. Although several other parcellations have been proposed, the boundaries drawn here emphasize cross species homology. Overlaid on the human brain are the commonly used anatomical delineations (i.e., dorsolateral PFC), which are adapted from [37] with permission. Bottom panel: On the left, results from recent meta-analyses [188] show differences in functional activation patterns, assessed using fMRI, between individuals with pathological anxiety (n = 2554) and controls (n = 2348) while viewing emotion-related stimuli. On the right, threat-related metabolism using 18fluoro-deoxyglucose, a radioactively labeled analog of glucose, is visualized using positron emission tomography (FDG-PET). Individual differences in AT are associated with individual differences in metabolism in a large sample of 592 preadolescent rhesus monkeys, adapted from [128] with permission. There is substantial overlap in terms of the neural circuitry implicated across humans and rhesus monkeys in threat processing, as well as in the cytoarchitecture of prefrontal regions. OFC orbitofrontal cortex, AI anterior insula, BST bed nucleus of the stria terminalis, PAG periaqueductal grey.
The basal (orbital) surface of the PFC, which includes the orbital proisocortex (OPro), areas 13, 11, 47/12, and portions of areas 10 [39], is often referred to as the OFC. Through connections with sensory cortices of all modalities, as well as with the amygdala and the thalamus, the OFC is well poised to integrate information about the external world with valence and internal processes, such as homeostatic state [40]. The medial sector comprises both the ACC (areas 25, 32, and 24) and the medial PFC (mPFC, medial portions of areas 9 and 10). The ACC is specialized for communication with effector regions [41], directly influencing behavioral and autonomic expressions associated with anxiety through connections with motor systems, as well as for contextualization of threat, based on connections with the hippocampal formation [42, 43]. The medial PFC, particularly its ventral portion, is strongly linked to autonomic and interoceptive centers, such as the anterior insula and brainstem (reviewed in [44]). Together with the medial OFC, the ventral portions of the medial PFC (vmPFC) have been extensively linked to affect and emotion [45–47], while rostral and dorsal portions appear to be specialized for explicit appraisal of threat [48]. Finally, the lateral portion of the PFC (lPFC, areas 9/46 and lateral portions of areas 10 and 47/12) has been implicated in active emotion regulation strategies, as well as in the direction of attention and in the manipulation of task-relevant information in a way that is consistent with achieving high-level goals [7].
Within the medial and orbital PFC sectors, there is a rostro-caudal gradient: more posterior portions are composed of agranular cortex, which lacks the granular layer IV, or dysgranular cortex, which is characterized by an ill-defined layer IV. Agranular and dysgranular cortices are often referred to as limbic cortex (reviewed in [39]). More rostral portions of the medial and orbital PFC, as well as the entire lPFC, are composed of granular cortex, in which layer IV is defined, as are the boundaries between layers II/III and V/VI. In lPFC, the most differentiated cortices are found posteriorly, and include caudal areas 46 and 8 [49]. In addition to a gradient in lamination, anatomical connectivity also varies along the rostro-caudal axis, with more posterior portions of medial and orbital PFC sending and receiving more dense connections with subcortical structures. Interestingly, the ACC, a region associated with attention, a process that is often disrupted in anxiety disorders, has the strongest connections within the PFC (reviewed in [50]).
The complex interactions within and outside the PFC necessitate selection from a large array of information for decision and action, and this wealth of information increases uncertainty about which components are relevant. An understanding of these complex interactions begins with the phylogenetically ancient limbic cortices, which form a ring at the base of the cortex, placing them at the foot of each and every cortical system, but at the center of influence through strong connections with the expanded primate association system. The limbic pOFC and ACC cortices, which process the most basic drives and emotions, have strong connections with granular PFC [51, 52], the areas thought to be at the pinnacle of functional specialization and intellectual prowess. These pathways intricately link areas associated with emotion and cognition [53]. At the cellular and molecular level, limbic cortices have features that endow them with flexibility [54], enabling their engagement in functions that are in constant flux, including learning, memory, and emotions. At the same time, the malleable microarchitecture of limbic cortices renders them vulnerable to disruption in several psychiatric illnesses, including anxiety disorders. It is in this context that we highlight below how circuits that link the PFC with other cortical and subcortical structures may help explain how adaptive anxiety may cross into an abnormal state.
Prefrontal basis for pathological anxiety
Anxiety is a state that, when engaged adaptively, aids in the detection and appropriate response to potential, distal threats, as opposed to fear, which is experienced relative to a proximal, immediate threat. In order to adaptively engage states of anxiety, one has to be able to predict which contexts, cues, and sensations are likely to predict an aversive outcome. These predictions are made based on information gathered as one navigates the world, the extraction of which becomes more challenging in the complex and changing environments humans inhabit. Individual differences in the neural circuitry underlying these processes can bias an individual towards anxiety in several ways: first, excessive attention to, and incorporation of aversive information, can sway one’s perception of the likelihood of encountering threats, biasing an individual towards persistent anxiety in the absence of threat. Second, inability to downregulate the physiological and cognitive correlates of the anxious state based on the engagement of regulatory strategies further perpetuates the notion that potential threats and the anxious state they produce are uncontrollable and unavoidable. Finally, sensitivity to the uncertainty inherent to predicting threats in dynamic environments biases anxious individuals towards avoidance of situations that could potentially elicit aversive outcomes, restricting the ability to learn that the world is not as bad as was initially estimated. Here, we argue that the PFC is essential for the prediction, regulation and learning of threats, contributing to the pathological anxiety that characterizes anxiety disorders. Because of the differences in PFC structure and function between rodents and primates, we primarily focus on results from humans and NHP studies (for more detailed consideration of rodent models of pathological anxiety, see [55–57]).
Interpretation of the world: increased appraisal, learning, and generalization of threat
One of the key features of anxiety disorders is overvaluation of threat, which can manifest as increased resources dedicated to the processing of aversive or threatening information [58]. Children, adolescents, and adults with anxiety disorders have increased attentional bias towards threat [59–63]. Individuals with anxiety disorders also tend to have a negative bias in the interpretation of ambiguous scenarios [64]. This negative bias extends to perception of the self, as individuals with anxiety disorders and depression endorse more self-referential negative traits than positive traits [65, 66]. A meta-analysis of highly anxious individuals suggests that, in experimental paradigms involving viewing a virtual environment, they are hypervigilant and spend more time scanning for threat [67]. Studies in youth with anxiety disorders show increased activation of the lateral PFC during tasks that involve modulating attentional allocation (see [68] for a review of common tasks), most often the ventrolateral portions [69–72], but also the dorsolateral portions [73, 74], supporting a role for this region in the attentional bias to threat that anxious youths display.
In addition to increased attention towards threats, learning about threats is also impacted in anxiety disorders. This phenomenon is most often studied using fear conditioning paradigms, where a previously neutral stimulus is paired with aversive outcomes (unconditioned stimulus, US), eventually yielding defensive responses in the presence of the conditioned stimulus (CS+). A control stimulus (CS−), which is never presented with the aversive outcome, is used to test generalizability of the threat association. A recent meta-analysis revealed differential recruitment of a distributed cortical-subcortical network, which includes the insula, dACC, vmPFC and dlPFC, in individuals with anxiety disorders during fear conditioning [75]. Once negative associations are formed, they are more resistant to extinction in individuals with anxiety disorders [76–78] and the memory for extinction can also be impaired [79]. Extinction is typically achieved by repeated presentations of the CS+ in the absence of the aversive outcome until the new contingencies associated with the CS+ are learned. Acquisition of fear associations has been linked to the amygdala [80, 81], while the regulation and extinction of these associations rely on the medial PFC. Failure to extinguish has been linked to decreased activation within the vmPFC in anxiety disordered populations [81]. Fear conditioning paradigms are particularly valuable from a translational perspective, as they have been extensively used in rodents to characterize and manipulate the rodent analogs of these frontal regions across time, context, and development [82–84].
Anxiety disorders are also characterized by generalization of threat responses to non-threatening stimuli [85–89]. From a learning perspective, generalization is adaptive because it allows for the prediction of which unencountered stimuli are likely to be linked to aversive outcomes. However, excessive generalization of fear learning can lead to increased anxiety [90]. Parametrically modulating features of the conditioned stimulus can reveal the extent to which the fear association generalizes to stimuli with similar sensory features. Relative to healthy controls, individuals with panic disorder show broader generalization gradients, based on measures of physiological arousal [91]. A similar tendency to overgeneralize has been observed in generalized anxiety disorder [87] and is linked to neural activity within the vmPFC [92], ACC [93–95], and the hippocampal formation [96]. Generalization is not necessarily limited to sensory features and can occur across the concepts and contexts to which an initially phobogenic object is linked. For example, an initial phobia of dogs could lead to anxiety in places where an encounter with a dog could occur–parks, sidewalks, etc. While these concepts share minimal sensory features with a dog, their conceptual linkage, paired with the aversive association, facilitates the generalization of the phobia [97, 98]. The vmPFC/OFC has been linked to the encoding of “cognitive maps” [99, 100], which describe the relationship between linked objects in a conceptual space. With input from subcortical structures, it is conceivable that these prefrontal regions underlie the tendency for maladaptive generalization and its subjective, symptomatic components, such as diffuse anticipatory anxiety.
Together, this suggests that individuals with high anxiety attend to threat more readily, are biased in learning related to aversive outcomes, and tend to overgeneralize. Anxious states can also increase the capacity to detect threats within the environment, by priming and focusing attentional and sensory systems [101], further reinforcing one’s view of the world as a threatening place. These threat associations, once encoded, are more resistant to extinction and generalize more easily. Together, these threat and learning biases interact, providing a rationale for maintaining sustained hypervigilant states.
Excessive physiological arousal—failure to regulate
It is not surprising that individuals with anxiety disorders experience increased physiological arousal, as their ongoing hypervigilant state leads to the activation of subcortical structures that mediate threat-related autonomic and pituitary-adrenal responses. While these physiological responses are directly mediated by subcortical structures, such as the hypothalamus and brainstem, the PFC has the capacity to modulate these responses, by engaging a variety of regulatory strategies [102]. Cognitive regulation confers the ability to use internally maintained goals and cognitive strategies to shape behavior and emotion in response to a stressor [7, 103]. These goals and strategies can be used to alter the course of emotional and physiological responses. Anxiety and other internalizing disorders, such as depression, are associated with a shift from adaptive to maladaptive regulatory strategies in youth and adults [104–106]. As emotion regulation can lead to decreased physiological arousal and decreased subjective anxiety [107], failure to successfully regulate can sustain states of hyperarousal and anxiety.
Meta-analyses support the importance of prefrontal function in emotion regulation, particularly the dl-, vl- and dmPFC (see Fig. 1 for parcellation, [108]), as well as interactions between the PFC and amygdala [109–111]. A recent meta-analysis of emotion regulation in anxiety disorders revealed that, relative to healthy controls, individuals with anxiety disorders showed less activation in the dmPFC and dACC during reappraisal, a form of directed emotion regulation [112]. Studies in children with anxiety disorders and NHPs with high levels of temperamental anxiety demonstrate reduced functional coupling between dlFPC and amygdala regions [113]. Thus, decreased prefrontal recruitment, particularly of lateral and medial regions, can lead to unsuccessful downregulation of the persistent arousal associated with anxiety. This aberrant emotion regulation capacity would facilitate a shift from adaptive to maladaptive behaviors and a lack of perceived control over heightened states of physiological arousal and anxiety [114, 115] in response to stressors.
The PFC, particularly its most laminate, lateral, and anterior portions, develops its patterns of structural and functional connectivity comparatively late [116–118]. In line with this, there is a developmental shift in amygdala-dlPFC coupling from positive functional connectivity in younger children to negative functional connectivity later in childhood [119]. Similar developmental trends are observed in amygdala-dlPFC connectivity occurring during emotion regulation [120]. At a network level, trends towards increased functional connectivity between the frontoparietal network, which includes the dlPFC, and other brain networks, reflect increased integration across networks of the brain with maturation [121, 122]. Individual differences in hyperactivity of the amygdala early in life, based on genetic and early-life factors, paired with decreased regulatory capacity of the dlPFC through altered functional connectivity, can bias children towards excessive arousal [5].
Extreme behavioral inhibition (BI) is an early temperament characterized by marked inhibited responses in the face of novelty and uncertainty, paired with increased levels of autonomic arousal [123]. This phenotype, also referred to as anxious temperament (AT), is associated with a greater than 3.5 fold increase in the likelihood of developing a social anxiety disorder, as well as other forms of stress-related psychopathology [124, 125]. Extreme AT, and its accompanying activation of the anxiety circuit, early in life, may provide the substrate for later alterations in regulatory processes modulating emotional and autonomic reactivity [126]. Studies in NHP models of AT have shown that increased metabolism within the ventral PFC, particularly the subgenual ACC (sgACC) and pOFC, as well as the extended amygdala and periaqueductal grey (PAG), are associated with individual differences in AT [5, 127, 128]. Both AT and its neural substrates are influenced by heritable factors [127, 129, 130], and it is likely that individual differences in reactivity of the amygdala and other components of the AT neural circuit influence the developmental trajectory of this temperament and the transition to psychopathology.
Uncertainty and worry converge on avoidance
As individuals navigate an environment, they gather the information that allows them to facilitate their goals. Relevant information, such as the magnitude of positive and negative outcomes and the likelihood of encountering those outcomes given the state of the world, can be learned in order to maximize adaptive success [131, 132]. Upon encounter with conditions that are predictive of a potential threat, several decisions have to be made – what is the appropriate strategy to engage? Should I continue to engage with my current task to maximize reward (approach), despite this salient cue, or should I initiate an escape (avoid)?
The dynamic nature of the world, however, often precludes a straightforward mapping between predictors and outcomes, aversive or otherwise, imbuing each prediction with a certain degree of uncertainty. Computational modeling of value-based reinforcement learning (RL, see [133–136] for a discussion of various RL frameworks) has provided a formalism for describing the uncertainty inherent to the cognitive operations underlying value-based decision making. While RL frameworks have typically been used to describe how individuals make choices relative to positive outcomes, they can also be used to describe the prediction of negative or aversive outcomes (as in [137, 138]). High anxiety, both temperamental and induced, can affect the way individuals learn from salient outcomes, particularly under conditions of high uncertainty.
Uncertainty can be modulated at the level of predictor-outcome relationships, with the volatility of the environment influencing the optimal learning strategy. In stable environments, where the rules change at a slow rate, slow learning rates are favored [139], as they are resistant to updating adaptive strategies based on noise. When the environment is volatile, more recent information is more valuable, favoring a faster learning rate. Although healthy individuals can update learning rates based on the degree of uncertainty, individuals with high trait anxiety cannot do so as readily [140]. This inability to adapt learning rates may be due to difficulty in disambiguating signal (true changes in the hidden rules) from noise [141]. While RL, particularly related to positive outcomes, has typically been linked to corticostriatal circuits [142, 143], recent work suggests that the amygdala, striatum and OFC work together to guide decision making, both with respect to appetitive and aversive outcomes [144–147]. The OFC has been shown to interact with the amygdala and striatum during learning, encoding complementary task-relevant information [146, 148–150] that can guide choices during tasks [151] (for further discussion see Murray and Fellows, this volume, Chapter 10).
Uncertainty can also be modulated outside of an RL framework. For example, paradigms can leverage uncertainty about the timing of the delivery of an aversive picture or shock to induce a state of uncertain anticipation. Individuals with pathological anxiety have great difficulty tolerating this kind of uncertainty [152–155] and report subjective states of anxiety in these paradigms [156]. Interestingly, while the subcortical neural correlates of uncertain and certain anticipation of aversive events seem to be largely overlapping [156], uncertain anticipation tends to preferentially recruit frontal regions (dlPFC/frontal pole, dACC) for sustained periods of time, potentially reflecting the additional effort required to predict when the threat will occur.
Uncertainty about outcomes paired with bias towards threat can combine to create a persistently aroused and hypervigilant state, which can bias an individual towards avoidance. Avoidance is a core feature of anxiety disorders [157]. When faced with persistent hyperarousal and distress, as well as repeated unsuccessful attempts to downregulate these responses, there is a strong tendency to disengage from the source of aversive sensations. While avoidance can be adaptive in the face of real threats, excessive avoidance behavior can further reinforce anxiety, as it obviates the ability to engage successfully with the potential threat and resulting anxiety [114]. Avoidance is observed in humans with agoraphobia as they navigate real-world and virtual environments [158]. Under the threat of shock, individuals with anxiety disorders tend to favor an avoidant strategy in a decision-making paradigm [138]. Simulation experiments suggest that, given an overestimate of the likelihood of threat encounters, avoidance is the most adaptive strategy, in the short term [132, 159]. However, avoidance also decreases exposure to new information, maintaining and/or reinforcing the link between a situation and the physiological responses [160–162]. Avoidant behavior can also be susceptible to generalization in highly anxious individuals [90]. This can be the case with a variety of triggers (e.g., open spaces, social interactions, phobogenic objects), which in part correspond with extant diagnostic boundaries (e.g., agoraphobia, social anxiety disorder, specific phobia, respectively). Avoidance behavior is also translationally relevant [163], as many of the strategies interpreted as anxious in animal models involve some form of avoidance (e.g., avoidance of the open arm on the elevated plus maze). While it appears that the selection of avoidant strategies is linked to neural activity in subcortical structures, such as the amygdala [164] and striatum [165, 166], and implemented by the hypothalamus and brainstem [167, 168], the OFC, ACC and vmPFC have been shown to interact with these subcortical structures to flexibly regulate the selection of appropriate avoidance behaviors [17, 169–171].
The evidence presented above suggests that interactions between negative expectations and the failure to regulate autonomic arousal form the basis for the core symptoms of anxiety disorders, contributing to the preference of maladaptive avoidant strategies. While effective in reducing anxiety and distress in the short term, maladaptive avoidance leads to the reinforcement of negative associations both through the acute reduction in symptoms and also through the decreased sampling of information that can be used to learn new associations and strategies to cope with potential threat.
From symptoms to circuits in anxiety
Although neuroimaging has provided substantial insights into the general location and functional alterations associated with anxiety, these findings are limited by their correlational nature. The signals interpreted are not direct measurements of brain activity per se and constraints with respect to the low spatial and temporal resolution of these methods do not allow for an understanding of the functions of neurons and microcircuits. Characterizing the distribution and strength of specific neuronal pathways can provide insight at a mechanistic level into systems-level dysfunction within these circuits. Much of what we know about anatomical connectivity within the human brain is based on tract tracing studies in NHPs, which are particularly valuable models given the considerable homology between NHPs and humans with respect to the PFC [172–174]. Rodent studies directly manipulating circuit function with physiological, chemo- and optogenetic strategies provide critical insights that complement work in NHPs [4, 175, 176], although the homology between rodent and primate frontal regions is the subject of debate (see [25–27, 31, 177]).
In this context, drawing on neuroanatomical studies from primates, we highlight how connections within the PFC, as well as connections between the PFC and subcortical structures, can help inform the understanding of anxiety symptoms. We focus in particular on cortical connections of cingulate and pOFC regions, as well as connections between the PFC, amygdala and thalamus (summarized in Figs. 2 and 3). We do not suggest that the neural circuitry underlying anxiety is limited to these structures; indeed, dysfunction across other cortical regions and other subcortical structures has been linked to anxiety, the details of which are reviewed above and in [17, 23, 178, 179]. Instead, we highlight how anatomical connections can inform the understanding of the functional relationships between brain regions mediating anxiety.
Fig. 2. Relationship of PFC with thalamic, amygdalar, and autonomic structures.
Simplified schematic shows PFC bidirectional thalamic (MD) and amygdalar connections; special output of the posterior orbitofrontal cortex (top right) to the inhibitory amygdalar IM (red, bottom right); output from posterior medial (cingulate) areas (top, left) to hypothalamic and brainstem autonomic structures. The PFC and amygdala also project to the inhibitory thalamic reticular nucleus (TRN), which gates signals between the thalamus and cortex. The density of connections with the amygdala is shown for all prefrontal sectors, adapted from [197] with permission.
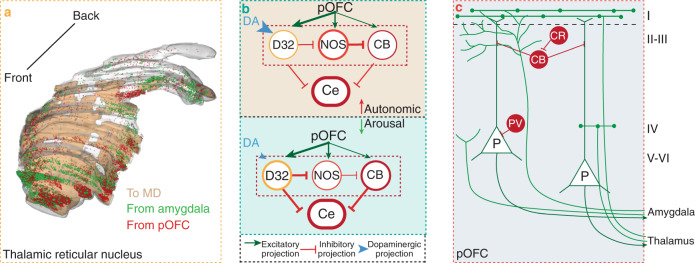
Fig. 3. Prefrontal, thalamic, and amygdalar pathway interactions with inhibitory systems.
a 3D reconstruction of the rhesus monkey inhibitory TRN shows its extent from anterior (lower left) to posterior (top right) levels. The image shows three superimposed pathways on TRN: Red dots, axon terminations from pOFC; green dots, axon terminations from the amygdala; brown shading, a map of projection neurons on TRN directed to the thalamic MD nucleus. Most PFC projections terminate on the anterior sector of TRN, but projections from the above pathways and some lateral PFC areas (not shown) project widely on TRN, suggesting that PFC and amygdala can gate thalamic inputs to cortex. Adapted from: [221] with permission. b A strong pathway from pOFC innervates the entirely inhibitory IM of the amygdala, which is composed of three types of inhibitory neurons. The circuit model shows predicted effects of high (large blue arrowhead) and low (small blue arrowhead) dopamine (DA) levels on the D32 (DARPP-32) neurons on the amygdalar IM and its projection to Ce. Elevated DA levels (large blue arrowhead) in stressful states is predicted to suppress D32 neurons and CB inhibitory neurons in IM, leading to disinhibition of the amygdalar Ce, and heightened autonomic drive. In contrast, in the presence of low DA levels (small blue arrowhead) D32 neurons can be depolarized and inhibit Ce, regulating downstream activity to autonomic structures. (Adapted from: [200, 207] with permission). c Schematic shows the cortical microcircuit, where about 20–30% of all neurons are inhibitory and show preferential laminar distributions. Pathways from the thalamic MDmc or the amygdala in pOFC terminate in distinct microenvironments in the upper versus the deep layers, where they encounter distinct neurochemical types of inhibitory neurons that express CR, CB, or PV, which innervate different elements of nearby neurons. Adapted from [232, 283] with permission.
PFC connections and inhibitory systems
The specialized PFC sectors (medial, orbital, and lateral), discussed above, are highly interconnected [49, 180], allowing the integration of information across a variety of cortical processing streams. Goal-directed behavior by the PFC plays a major role in selecting relevant and suppressing irrelevant signals, which depends on the engagement of neurons and systems with opposing functions.
While most cortical neurons are excitatory, the fewer (20–30%) inhibitory neurons have a key role in modulating the activity of nearby neurons. The various inhibitory neurons can be characterized by unique physiology, neurochemistry, and morphology, as well as the sites they innervate on a nearby pyramidal or other inhibitory neurons. The differences in inhibitory neurons and their connectivity provide the capacity to broadly influence cortical activation, ranging from mild modulation to strong inhibition (reviewed in [181, 182]). In primates, inhibitory neurons can be classified by the expression of calcium-binding proteins (calbindin (CB), calretinin (CR), or parvalbumin (PV)), which are largely non-overlapping from the standpoint of their laminar distributions (reviewed in [182]; Fig. 3c).
Cortico-cortical pathways in primates are excitatory, and can affect the excitability of neurons at the site of termination by innervating excitatory neurons or distinct types of inhibitory neurons. For example, feedforward pathways from lateral PFC primarily target neurons in the deep layers of the pregenual ACC (pgACC), which in turn project to neurons in the sgACC. About 20% of synapses in the pgACC to sgACC pathway are on inhibitory neurons [183]. Among these, axon terminals from the pgACC innervate PV neurons in the deep layers of the sgACC, which can exert strong perisomatic inhibition on local pyramidal neurons; the latter project to downstream autonomic regions in the hypothalamus and the brainstem [184, 185]. This serial pathway helps explain how activity in lPFC and pgACC can help regulate autonomic drive through sgACC. Conversely, inactivity of lPFC or in pgACC can remove powerful inhibition on sgACC and enhance arousal-related autonomic drive, as occurs in anxiety disorders.
There is also a feedback pathway from pgACC to lPFC, where targets on CB inhibitory neurons can exercise lateral inhibition on local pyramidal neurons [186]. This pathway is thought to be capable of silencing extraneous activity in neurons that flank active columns that are engaged in cognitive operations by increasing the signal-to-noise ratio [187]. In the deep layers, the pgACC pathway innervates PV neurons in lPFC, which may help change activity in a column of cortex when it is necessary to suspend an ongoing goal and assume another goal [186]. The pgACC has a key role in attentional mechanisms (reviewed in [50]), and its disruption in anxiety disorders [188] can have consequences for cognitive operations. Thus, in a laminar-specific manner, disruption of the pgACC to the upper layers of lPFC can increase noise and degrade attention to relevant stimuli for cognitive tasks. In the deep layers, it may disrupt the reappraisal of goals and the ability to reverse operations when needed, a process that is also affected in anxiety disorders.
Prefrontal interactions with subcortical circuitry
The evidence presented above supports an important role for the PFC in anxiety and its associated disorders, but the PFC does not interpret nor generate anxiety alone. Indeed, the PFC is interconnected with subcortical structures that are essential for providing information about and effecting changes in physiology, emotion, and behavior. Here, we discuss several key projection patterns from the PFC to emotion-related subcortical regions, focusing on pathways that may provide a neural basis for disruptions associated with anxiety disorders (Figs. 2, 3).
Connections with medial temporal lobe structures
Several structures within the medial temporal lobe, most notably the amygdala and hippocampus, participate extensively in anxiety, in part through connections with the PFC. The ACC especially receives unidirectional projections from the anterior hippocampus (ventral in rodents), which are strongest to subgenual area 25 [189]. Projections from the anterior hippocampus also reach the pOFC, but are comparatively sparser than to the ACC [190–193]. The pathway from hippocampus to ACC is thought to provide relevant information about the context of stimuli and events [194, 195], which is critical for decision making and selecting actions.
Among the temporal connections with PFC, the amygdala is the most prominent, and most consistently implicated in anxiety disorders. The amygdala projects to all PFC [196], but most robustly to pOFC and sgACC, which also uniquely and strongly project back to the amygdala [197, 198]. Moreover, the projections from the pOFC to the amygdala show a distinct pattern. The pOFC has bidirectional connections with all basal nuclei. In addition, the pOFC sends a dense and solely unidirectional projection to the entirely inhibitory neurons of the intercalated masses (IM) of the amygdala, interposed at the perimeters of the basal and central nuclei [199, 200] (Fig. 2).
In IM, the pOFC pathway targets strongly the class of inhibitory neurons that express DARPP-32, whose activity is known to be regulated dynamically by dopamine that originates from brainstem projections [201, 202]. Specifically, physiological studies have shown that the level of dopamine regulates the activity of DARPP-32 neurons via phosphorylation at distinct sites on the DARPP-32 protein [202]. In the presence of moderate levels of dopamine, DARPP-32 neurons can be depolarized, which project to, and inhibit the Ce, which activates downstream autonomic structures. On the other hand, high levels of dopamine hyperpolarize DARPP-32 neurons, effectively reducing the inhibitory input from IM neurons to the Ce. This evidence suggests that dopamine may act as a modulator of IM neurons: at optimal levels of dopamine neurons in IM are depolarized and inhibit their targets in the amygdalar Ce. On the other hand, at high levels of dopamine neuronal input from the IM is hypothesized to be reduced, leaving its Ce target unchecked, leading to upregulation of downstream autonomic structures during high emotional arousal, as seen in anxiety disorders. High dopamine levels accompanied by high autonomic drive are correlated with weakened regulatory influence by PFC [203–206].
It is noteworthy that the IM includes two other neurochemical types of inhibitory neurons, forming an intra-IM microcircuit that can have further consequences for Ce regulation. As shown in Fig. 3 on the intrinsic connections within IM, DARPP32 neurons project to and inhibit neighboring NOS neurons, which inhibit nearby CB neurons [207]. Because the Ce projects downstream to structures involved in threat-related physiological and autonomic responses, input from the inhibitory IM neurons, or the lack thereof, has the potential to modulate stress-related autonomic drive and physiological arousal [200].
Direct evidence for the functions of the pOFC to IM in regulating anxiety and autonomic arousal is challenging to acquire, as IM neurons are difficult to target in animal models and cannot be detected with neuroimaging methods in humans. Interestingly, selective ablation of IM cells blocks extinction [208], likely abolishing the increase in inhibition of Ce via IM connections that occur during extinction [209]. Advances in the application of opto- and chemogenetic methods to NHP models [210] could provide substantial insight into the functional significance of modulating these projections. Ultimately, specific targeting of this pathway could facilitate optimal inhibitory communication between the PFC and amygdala, therefore increasing the efficacy of the regulatory interaction between the two structures.
Thalamic interactions with the PFC
The goal-directed functions of PFC are guided by bidirectional signals with the dorsal thalamus, which includes the mediodorsal (MD) nucleus (e.g., [211]), and also other thalamic nuclei [212]. Goal-directed behavior requires attention to relevant stimuli and suppression of irrelevant signals, which is enabled by the thalamic reticular nucleus (TRN). Attentional mechanisms are affected in anxiety disorders, with phobias characterized by excessive focus on phobogenic objects or avoidance of conditions that evoke anxiety, such as social interactions.
Can the circuits connecting the thalamus and cortex inform what may be disrupted in anxiety? The features and connections of TRN provide important clues about normal function and disruption in anxiety. Topographically, the TRN envelops the thalamus on the dorsal and lateral sides, but differs from the dorsal thalamus by developmental origin and composition of entirely inhibitory neurons [213, 214]. The TRN is considered to be a hub for attentional regulation of signals passing through all of the dorsal thalamus [215], and preventing distracting stimuli from reaching the cortex ([216]; reviewed in [217]). This selective modulation is facilitated by bidirectional connections between the TRN and the dorsal thalamus, as well as unidirectional projections from the entire cortex to the TRN. Cortical projections to TRN from PFC, motor and sensory cortices, and their associated thalamic nuclei map on sequential sectors from the front to the back of TRN [218, 219]. Most projections from PFC terminate in the front sector of TRN, with some remarkable and intriguing exceptions: some lateral PFC areas, the pOFC, and the amygdala, innervate large swaths of TRN (Fig. 3a), extending to sectors that are the province of sensory or motor pathways [220, 221].
The inhibitory capacity of the TRN and distribution of connections suggest that it gates thalamocortical communication. What is the mechanism that confers specificity to this network? Physiologic studies have provided evidence that when cortico-thalamic firing by specific neurons is strong and persistent, there is transient plasticity that weakens inhibition from TRN on the active thalamic neurons and facilitates passage of their signals to the cortex [222]. Thalamic neurons that are not active can be silenced by TRN. In the sensory systems, neurons that respond to a specific stimulus exhibit this behavior. What is the signal that is targeted for passage in interactions between the thalamus and the PFC? We suggest that focused attention on a goal is the stimulus that initiates the physiological mechanism to select what is relevant for the task at hand. The projection of the amygdala to TRN suggests that stimuli with emotional import can activate MDmc for transmission to cortex [221, 223].
Synthesis of PFC circuits, decisions and anxiety
The tightly interconnected pOFC, MDmc, and the amygdala, and their broad projection onto the TRN have functional implications for maintaining a homeostatic state and its disruption in anxiety disorders. Computational modeling has shown that under normal conditions, the PFC and the amygdala work cooperatively to facilitate goal-directed behavior [224, 225]. Computational modeling reveals that in the face of uncertainty PFC input is necessary to facilitate information processing through the amygdalar IM [224]. Specifically, the model demonstrates that the pathway from IL cortex in rodents or pOFC in primates to the amygdalar IM can flexibly gauge responses in ambiguous and changing environments, in a pattern that is also suggested from human fMRI research [226].
In addition, through its strong projections to TRN [221], the amygdala can have a major influence on what goes from medial MD to cortex, and especially to its major target in pOFC. It is conceivable that in states of anxiety, as in phobias, excessive focus on phobogenic stimuli promotes their selective access to the PFC. In addition to innervating TRN directly, the amygdala also has a strong projection to MDmc. This pathway is highly unusual in strength and pattern of perisomatic synapses and adhesions on large dendritic segments that effectively isolate them from other inputs [227]. This pattern may ensure passage of amygdalar signals from thalamus to cortex during times of high arousal. Because individuals with anxiety disorders experience persistent arousal and anxiety, this may facilitate passage of aversive stimuli through thalamic gating to the cortex. Interestingly, the activity of a subset of limbic-associated TRN neurons is modulated by arousal [228]. Selective passage may account for the negative attentional bias of individuals with anxiety disorders, as they have more difficulty filtering out aversive stimuli relative to controls.
Thalamic nuclei that are connected with PFC receive dopaminergic axons, in a remarkably unique specialization in primates [229–231], reviewed in [232]). It is conceivable that differences in dopamine levels may influence the excitability of thalamic neurons as well. By extension of the thalamic computational model [224], high levels of dopamine may excite too many thalamic neurons associated with stimuli that must be considered or choices to be made, so that no neurons fire above others to gain selective access to cortex beyond those associated with threat. The specialized dopaminergic innervation in primates points to yet another way where high levels of dopamine in anxiety disorders can disrupt the thalamocortical motif that is critical for selection of information for decision and action.
Dopaminergic systems (see also discussion by Arnsten and Cools, this volume) have been implicated in many of the symptoms discussed in relation to anxiety disorders, such as value-based decision making [233, 234], the encoding of uncertainty [235–238], and fear generalization [239, 240]. The capability of dopamine to modulate these thalamocortical and amygdalocortical systems may be impacted in anxiety disorders, affecting both circuit function through PFC and contributing to the symptoms experienced by those with anxiety disorders. Continued work to characterize the influence of dopamine on these circuits, facilitated by pharmacological and promoter-based targeting of specific dopaminergic receptors (e.g. [241]) and projections (e.g., [242]) will help to further understand the complex and multifaceted role that dopamine and other neurotransmitter systems play in anxiety disorders.
Interactions between the cortex, thalamus, and amygdala can contribute to anxiety symptoms
The three major constructs discussed above, namely threat bias, hyperarousal, and avoidance, are all influenced by the function of the amygdala, thalamus, and PFC. Functional interactions among these structures, an understanding of which is informed by anatomy, can contribute to symptoms experienced by patients with anxiety disorders. We speculate that the pathophysiology underlying these symptom domains arises through recurrent interactions among these structures, resulting in a positive reinforcement loop. This idea is consistent with the strong bidirectional connections of the amygdala and MDmc with pOFC and ACC areas. For example, threat bias could be linked to amygdala hyperactivity, which signals to the rest of the brain that an imminent threat exists. Through bottom-up engagement of the PFC, via anatomical links to its posterior orbital and medial regions, the amygdala can bias the PFC to predict a higher likelihood of threat and exaggerate its potential magnitude. This, in turn, can influence top-down control of the brain by the PFC, as it is more likely to engage anxiety-related circuitry to respond to these altered perceptions of threat. Through interactions with the PFC and amygdala, the thalamus can also contribute to threat biases, favoring selective passage via filtering through TRN of thalamocortical signals related to threat to the exclusion of other relevant information. These subcortical regions, which have a special relationship with the PFC, by over-representation of aversive information can bias decisions and actions, and can lead to avoidance of thoughts and situations linked to perceived threats.
Treatment implications and future directions
The evidence presented above demonstrates the importance of the PFC in the complex expression of human anxiety, as well as in mediating the transition between adaptive and pathological anxiety. Anxiety, at its core, is an adaptive, protective state that promotes survival. Because of the substantially expanded capacity of the human PFC, there are far more opportunities for cognitive and psychological processes involved in mediating adaptive anxiety to become corrupted, resulting in PFC engagement of subcortical defensive circuitry in a way that is maladaptive. Above, we detail how exaggerated predictions about the magnitude and likelihood of threat, paired with aberrant learning under uncertain conditions, lead to persistent engagement of subcortical structures involved in anxiety. Avoidant strategies further reinforce these exaggerated threat predictions by eliminating opportunities to successfully learn from and cope with threat.
Currently available treatments for anxiety disorders can be broadly divided into pharmacological and psychotherapeutic interventions, which target the circuits described above via differential initial mechanisms. For example, selective serotonin reuptake inhibitors (SSRIs), effect changes via initial action upon the serotonergic system, while cognitive-behavioral therapy (CBT) focuses on altering cognitive patterns associated with anxiety. Benzodiazepines, which are a highly effective pharmacological intervention for acute anxiety, produce their anxiolytic effects by facilitating inhibitory neurotransmission via their actions at GABAA receptors [243]. Despite differences in the initial route, the neural circuitry linked to successful treatment is largely overlapping [244–247], with normalized activation in the amygdala, insula and dACC associated with symptom amelioration.
Consistent with their convergent neural mechanisms, successful interventions also result in overlapping changes in anxiety symptoms. Treatments, both pharmacological and psychotherapeutic, have been shown to reduce negative bias and affect. New interventions, specifically centered around negative bias reduction, most notably Attention Bias Modification Treatment (ABMT), have shown promise in treating anxiety disorders [248, 249]. Effective interventions can also bolster emotion regulation capacities. For example, it has been demonstrated that CBT-based interventions [250–252], particularly those involving exposure-based methods, can lead to decreased autonomic arousal and increased perceived control over emotional and physiological states. Decreased avoidance behavior also accompanies successful treatment [253]. Novel research methods, such as ecological momentary assessment (EMA), a tool that allows for real-time tracking of patterns of movement [254, 255] and self-reported subjective states, could be used to better understand the inter-relation among negative cognition, associated arousal, and avoidance; this tool is currently being investigated to promote successful treatment [256, 257] for various psychiatric illnesses.
Despite the efficacy of current treatments, a considerable number of patients with anxiety disorders either partially or completely fail to respond [258, 259]. Additionally, ideal treatments would fundamentally impact the underlying neural circuit alterations in such a way as to reduce the ongoing vulnerabilities that underlie the recurrence and chronicity of anxiety disorders. Neuromodulation strategies, such as transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS), have the capacity to more directly target and normalize activation within relevant neural circuits [260]. While limited clinical trials have been performed with rTMS in patients with anxiety disorders [261], considerable work has shown efficacy in other internalizing disorders, particularly depression [262, 263], and forms of stress-related psychopathology, such as PTSD [264, 265]; (for further discussion see Chapter 15, this volume). Specific targeting of regions that exert control over anxiety-related cortical and subcortical regions, such as the dlPFC [266] or the medial PFC/ACC [267], could result in normalization of circuit function. For example, symptom reduction following TMS over the dlPFC in PTSD was associated with normalization of connectivity between the sgACC and various prefrontal regions, including the vlPFC and dmPFC, as well as the insula [268]. More direct targeting of subcortical structures could be potentially achieved via transcranial focused ultrasound stimulation, which has been used to target amygdala activity in primates in early studies [269], and by advances in neurofeedback technology, which could pair interventions with closed-loop reinforcement of regulatory brain activity [270]. Chemo- and optogenetic methods [271] using viral vector delivery systems also provide opportunities to ‘fine tune’ the activity of specific neurons and circuits. These methods have been extensively used in rodent models to modulate defensive responses, and recent efforts in NHPs suggest that specific targeting of amygdala neurons with chemogenetic methods could prove useful in the treatment of refractory and severely ill patients [272, 273], although significant progress will have to be made to establish the safety and long-term efficacy of these methods.
Because of the coordinated actions between key prefrontal and subcortical regions in mediating anxiety, effective treatments likely depend on the relative integrity of the anatomical and functional connections between nodes of the anxiety circuit. This is consistent with studies demonstrating that successful treatments are linked to functional connectivity patterns that are more similar to healthy controls [274–276]. From an anatomical perspective, the integrity of various white matter tracts, particularly the uncinate fasciculus, which contains the axons that convey signals between the PFC and the medial temporal lobe [277, 278], has been linked to pathological anxiety [279, 280]. It is interesting to speculate that interventions, pharmacological and/or experience-dependent [281] that modulate myelination within these tracts could prove to be effective treatments by normalizing prefrontal-subcortical connectivity.
Conclusion
Because of its importance in survival, anxiety and its underlying neural circuitry have been evolutionarily conserved, with the capacity to engage in more elaborate defensive and coping strategies increasing as the PFC has expanded. This expanded regulatory capacity, particularly evident in primates, depends on the interface between specialized PFC sectors with limbic cortical regions, as well as connectivity with subcortical structures involved in conveying relevant information about threats in the environment. While aberrant functioning within any of the components of the anxiety-related circuit contributes to the expression of maladaptive anxiety, the PFC is particularly relevant to human thoughts, feelings, disability, and suffering that characterize anxiety disorders. It is important to recognize that anxiety disorders commonly emerge during childhood and the pathophysiology related to anxiety disorders changes with the development and chronicity of symptoms. It is likely that over time, repeated and frequent activation of the anxiety circuit in response to exaggerated perceptions of threat results in ingrained and automatic activation of the cortical and subcortical structures mediating pathological anxiety. A deeper understanding of the developmental factors that influence the circuitry underlying maladaptive anxiety will provide new ideas for targeted, early-life interventions with the potential to obviate the recurrence and chronicity of anxiety disorders.
Acknowledgements
We thank Andrew S. Fox and Jonathan A. Oler for helpful discussions and comments on the manuscript. We thank Marissa Riedel, Patrick Roseboom, and the staff at the Harlow Center for Biological Psychology, the HealthEmotions Research Institute, the Waisman Center, the Waisman Laboratory for Brain Imaging and Behavior, the Lane Neuroimaging Laboratory, the Wisconsin National Primate Center, and the members of the Neural Systems Laboratory, Boston University, who participated in the original work.
Author contributions
MMK, NHK, HB conceptualized and wrote the manuscript.
Funding
This work was supported by the National Institutes of Mental Health (Grant Nos. R01MH081884, 3R01MH046729, 5R01MH107563, and R01MH046729 [to NHK], 5T32MH018931 [to MMK] and R01MH057414 and R01MH117785 [to HB]) and by grants to the Wisconsin National Primate Research Center (Grant Nos. P51-OD011106 and P51-RR000167).
Competing interests
NHK has received honoraria from CME Outfitters and the Pritzker Consortium; has served on scientific advisory boards for Skyland Trail; currently serves as an advisor to the Pritzker Neuroscience Consortium and consultant to Concept Therapeutics, the Early Adversity Research External Scientific Advisory Board at University of Texas – Austin, and currently serves as Editor-in-Chief of The American Journal of Psychiatry. All other authors report no biomedical financial interests or potential conflicts of interest.
Footnotes
The original online version of this article was revised due to errors into references
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
2/2/2022
A Correction to this paper has been published: 10.1038/s41386-021-01216-x
References
- 1.LeDoux JE. Emotion circuits in the brain. Annu Rev Neurosci. 2000;23:155–84. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- 2.Mobbs D, Adolphs R, Fanselow MS, Barrett LF, LeDoux JE, Ressler K, et al. Viewpoints: approaches to defining and investigating fear. Nat Neurosci. 2019;22:1205–16. doi: 10.1038/s41593-019-0456-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blanchard DC, Blanchard RJ. Defensive behaviors, fear, and anxiety. Handbook of anxiety and fear, San Diego, CA, US: Elsevier Academic Press; 2008. p. 63–79.
- 4.LeDoux JE, Pine DS. Using neuroscience to help understand fear and anxiety: a two-system framework. Am J Psychiatry. 2016;173:1083–93. doi: 10.1176/appi.ajp.2016.16030353. [DOI] [PubMed] [Google Scholar]
- 5.Fox AS, Kalin NH. A translational neuroscience approach to understanding the development of social anxiety disorder and its pathophysiology. Am J Psychiatry. 2014;171:1162–73. doi: 10.1176/appi.ajp.2014.14040449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalin NH. Mechanisms underlying the early risk to develop anxiety and depression: a translational approach. Eur Neuropsychopharmacol. 2017;27:543–53. doi: 10.1016/j.euroneuro.2017.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ochsner KN, Gross JJ. Cognitive emotion regulation: insights from social cognitive and affective neuroscience. Curr Dir Psychol Sci. 2008;17:153–8. doi: 10.1111/j.1467-8721.2008.00566.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pine DS, Wise SP, Murray EA. Evolution, emotion, and episodic engagement. The Am. Jo. of Psychiatry. 2021;in press. [DOI] [PMC free article] [PubMed]
- 9.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, et al. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2012;69:372–80. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–9. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffman DL, Dukes EM, Wittchen H-U. Human and economic burden of generalized anxiety disorder. Depress Anxiety. 2008;25:72–90. doi: 10.1002/da.20257. [DOI] [PubMed] [Google Scholar]
- 13.Greenberg PE, Fournier A-A, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010) J Clin Psychiatry. 2015;76:155–62. doi: 10.4088/JCP.14m09298. [DOI] [PubMed] [Google Scholar]
- 14.Fanselow MS, Lester LS. A functional behavioristic approach to aversively motivated behavior: predatory imminence as a determinant of the topography of defensive behavior. Evolution and learning, Hillsdale, NJ, US: Lawrence Erlbaum Associates, Inc; 1988. p. 185–212.
- 15.Mobbs D, Hagan CC, Dalgleish T, Silston B, Prévost C. The ecology of human fear: survival optimization and the nervous system. Front Neurosci. 2015;9:55. [DOI] [PMC free article] [PubMed]
- 16.Kenwood MM, Kalin NH. Nonhuman Primate Models to Explore Mechanisms Underlying Early-Life Temperamental Anxiety. Biol Psychiatry. 2021;89:659–671. [DOI] [PMC free article] [PubMed]
- 17.Mobbs D, Headley DB, Ding W, Dayan P. Space, time, and fear: survival computations along defensive circuits. Trends Cogn Sci. 2020;24:228–41. doi: 10.1016/j.tics.2019.12.016. [DOI] [PubMed] [Google Scholar]
- 18.Levy I, Schiller D. Neural computations of threat. Trends Cogn Sci. 2021;25:151–71. doi: 10.1016/j.tics.2020.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Headley DB, Kanta V, Kyriazi P, Paré D. Embracing complexity in defensive networks. Neuron. 2019;103:189–201. doi: 10.1016/j.neuron.2019.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Calhoon GG, Tye KM. Resolving the neural circuits of anxiety. Nat Neurosci. 2015;18:1394–404. doi: 10.1038/nn.4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker DL, Cassella JV, Lee Y, De Lima TCM, Davis M. Opposing roles of the amygdala and dorsolateral periaqueductal gray in fear-potentiated startle. Neurosci Biobehav Rev. 1997;21:743–53. doi: 10.1016/s0149-7634(96)00061-9. [DOI] [PubMed] [Google Scholar]
- 22.Lefler Y, Campagner D, Branco T. The role of the periaqueductal gray in escape behavior. Curr Opin Neurobiol. 2020;60:115–21. doi: 10.1016/j.conb.2019.11.014. [DOI] [PubMed] [Google Scholar]
- 23.LeDoux J. The emotional brain, fear, and the amygdala. Cell Mol Neurobiol. 2003;23:727–38. doi: 10.1023/A:1025048802629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wallis JD. Cross-species studies of orbitofrontal cortex and value-based decision-making. Nat Neurosci. 2011;15:13–19. doi: 10.1038/nn.2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.García-Cabezas MÁ, Zikopoulos B, Barbas H. The Structural Model: a theory linking connections, plasticity, pathology, development and evolution of the cerebral cortex. Brain Struct Funct. 2019;224:985–1008. doi: 10.1007/s00429-019-01841-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vogt BA, Vogt L, Farber NB, Bush G. Architecture and neurocytology of monkey cingulate gyrus. J Comp Neurol. 2005;485:218–39. doi: 10.1002/cne.20512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laubach M, Amarante LM, Swanson K, White SR. What, if anything, is rodent prefrontal cortex? ENeuro. 2018;5. [DOI] [PMC free article] [PubMed]
- 28.Evans DA, Stempel AV, Vale R, Branco T. Cognitive control of escape behaviour. Trends Cogn Sci. 2019;23:334–48. doi: 10.1016/j.tics.2019.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoover WB, Vertes RP. Anatomical analysis of afferent projections to the medial prefrontal cortex in the rat. Brain Struct Funct. 2007;212:149–79. doi: 10.1007/s00429-007-0150-4. [DOI] [PubMed] [Google Scholar]
- 30.Heilbronner SR, Rodriguez-Romaguera J, Quirk GJ, Groenewegen HJ, Haber SN. Circuit-based corticostriatal homologies between rat and primate. Biol Psychiatry. 2016;80:509–21. doi: 10.1016/j.biopsych.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sharma KK, Kelly EA, Pfeifer CW, Fudge JL. Translating Fear Circuitry: Amygdala Projections to Subgenual and Perigenual Anterior Cingulate in the Macaque. Cereb Cortex. 2020;30:550–62. [DOI] [PMC free article] [PubMed]
- 32.Davis M. The role of the amygdala in fear-potentiated startle: implications for animal models of anxiety. Trends Pharm Sci. 1992;13:35–41. doi: 10.1016/0165-6147(92)90014-w. [DOI] [PubMed] [Google Scholar]
- 33.Teffer K, Semendeferi K. Human prefrontal cortex: evolution, development, and pathology. Prog Brain Res. 2012;195:191–218. doi: 10.1016/B978-0-444-53860-4.00009-X. [DOI] [PubMed] [Google Scholar]
- 34.Semendeferi K, Teffer K, Buxhoeveden DP, Park MS, Bludau S, Amunts K, et al. Spatial organization of neurons in the frontal pole sets humans apart from great apes. Cereb Cortex. 2011;21:1485–97. doi: 10.1093/cercor/bhq191. [DOI] [PubMed] [Google Scholar]
- 35.Capitanio JP. Naturally occurring nonhuman primate models of psychosocial processes. ILAR J. 2017;58:226–34. doi: 10.1093/ilar/ilx012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bernardi S, Salzman CD. The contribution of nonhuman primate research to the understanding of emotion and cognition and its clinical relevance. Proc Natl Acad Sci USA. 2019;116:26305–12. doi: 10.1073/pnas.1902293116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dixon ML, Thiruchselvam R, Todd R, Christoff K. Emotion and the prefrontal cortex: an integrative review. Psychol Bull. 2017;143:1033–81. doi: 10.1037/bul0000096. [DOI] [PubMed] [Google Scholar]
- 38.Barbas H. Complementary roles of prefrontal cortical regions in cognition, memory, and emotion in primates. Adv Neurol. 2000;84:87–110. [PubMed] [Google Scholar]
- 39.Barbas H. General cortical and special prefrontal connections: principles from structure to function. Annu Rev Neurosci. 2015;38:269–89. doi: 10.1146/annurev-neuro-071714-033936. [DOI] [PubMed] [Google Scholar]
- 40.Stalnaker TA, Cooch NK, Schoenbaum G. What the orbitofrontal cortex does not do. Nat Neurosci. 2015;18:620–7. doi: 10.1038/nn.3982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shackman AJ, Salomons TV, Slagter HA, Fox AS, Winter JJ, Davidson RJ. The integration of negative affect, pain and cognitive control in the cingulate cortex. Nat Rev Neurosci. 2011;12:154–67. doi: 10.1038/nrn2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vogt BA, Pandya DN. Cingulate cortex of the rhesus monkey: II. Cortical afferents. J Comp Neurol. 1987;262:271–89. doi: 10.1002/cne.902620208. [DOI] [PubMed] [Google Scholar]
- 43.Devinsky O, Morrell MJ, Vogt BA. Contributions of anterior cingulate cortex to behaviour. Brain. 1995;118:279–306. doi: 10.1093/brain/118.1.279. [DOI] [PubMed] [Google Scholar]
- 44.Joyce MKP, Barbas H. Cortical connections position primate area 25 as a keystone for interoception, emotion, and memory. J Neurosci. 2018;38:1677–98. doi: 10.1523/JNEUROSCI.2363-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bechara A, Damasio H, Damasio AR. Emotion, decision making and the orbitofrontal cortex. Cereb Cortex. 2000;10:295–307. doi: 10.1093/cercor/10.3.295. [DOI] [PubMed] [Google Scholar]
- 46.Bechara A, Tranel D, Damasio H. Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain. 2000;123:2189–202. doi: 10.1093/brain/123.11.2189. [DOI] [PubMed] [Google Scholar]
- 47.Hiser J, Koenigs M. The multifaceted role of the ventromedial prefrontal cortex in emotion, decision making, social cognition, and psychopathology. Biol Psychiatry. 2018;83:638–47. doi: 10.1016/j.biopsych.2017.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mechias M-L, Etkin A, Kalisch R. A meta-analysis of instructed fear studies: implications for conscious appraisal of threat. Neuroimage. 2010;49:1760–8. doi: 10.1016/j.neuroimage.2009.09.040. [DOI] [PubMed] [Google Scholar]
- 49.Barbas H, Pandya DN. Architecture and intrinsic connections of the prefrontal cortex in the rhesus monkey. J Comp Neurol. 1989;286:353–75. doi: 10.1002/cne.902860306. [DOI] [PubMed] [Google Scholar]
- 50.Barbas H, Bunce JG, Medalla M. Prefrontal pathways that control attention. Principles of frontal lobe functions. Oxford University Press; 2013;31–48.
- 51.Nauta WJH. The problem of the frontal lobe: a reinterpretation. J Psychiatr Res. 1971;8:167–87. doi: 10.1016/0022-3956(71)90017-3. [DOI] [PubMed] [Google Scholar]
- 52.Nauta W. Neural associations of the frontal cortex. Acta Neurobiologiae Experimentalis. 1972;32:125–40. [PubMed] [Google Scholar]
- 53.Barbas H. Anatomic basis of cognitive-emotional interactions in the primate prefrontal cortex. Neurosci Biobehav Rev. 1995;19:499–510. doi: 10.1016/0149-7634(94)00053-4. [DOI] [PubMed] [Google Scholar]
- 54.Garcia-Cabezas MA, Joyce MKP, John YJ, Zikopoulos B, Barbas H. Mirror trends of plasticity and stability indicators in primate prefrontal cortex. Eur J Neurosci. 2017;46:2392–405. doi: 10.1111/ejn.13706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nestler EJ, Hyman SE. Animal models of neuropsychiatric disorders. Nat Neurosci. 2010;13:1161–9. doi: 10.1038/nn.2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Blanchard DC, Summers CH, Blanchard RJ. The role of behavior in translational models for psychopathology: Functionality and dysfunctional behaviors. Neurosci Biobehav Rev. 2013;37:1567–77. doi: 10.1016/j.neubiorev.2013.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Klengel T, Dias BG, Ressler KJ. Models of intergenerational and transgenerational transmission of risk for psychopathology in mice. Neuropsychopharmacology. 2016;41:219–31. doi: 10.1038/npp.2015.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Carlisi CO, Robinson OJ. The role of prefrontal–subcortical circuitry in negative bias in anxiety: translational, developmental and treatment perspectives. Brain Neurosci Adv. 2018;2:2398212818774223. doi: 10.1177/2398212818774223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mogg K, Bradley BP. A cognitive-motivational analysis of anxiety. Behav Res Ther. 1998;36:809–48. doi: 10.1016/s0005-7967(98)00063-1. [DOI] [PubMed] [Google Scholar]
- 60.Roy AK, Vasa RA, Bruck M, Mogg K, Bradley BP, Sweeney M, et al. Attention bias toward threat in pediatric anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2008;47:1189–96. doi: 10.1097/CHI.0b013e3181825ace. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van IJzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. 2007;133:1–24. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- 62.Abend R, de Voogd L, Salemink E, Wiers RW, Pérez-Edgar K, Fitzgerald A, et al. Association between attention bias to threat and anxiety symptoms in children and adolescents. Depress Anxiety. 2018;35:229–38. doi: 10.1002/da.22706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Abend R, Bajaj MA, Matsumoto C, Yetter M, Harrewijn A, Cardinale EM, et al. Converging multi-modal evidence for implicit threat-related bias in pediatric anxiety disorders. Res Child Adolesc Psychopathol. 2021;49:227–40. doi: 10.1007/s10802-020-00712-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stuijfzand S, Creswell C, Field AP, Pearcey S, Dodd H. Research review: Is anxiety associated with negative interpretations of ambiguity in children and adolescents? A systematic review and meta-analysis. J Child Psychol Psychiatry. 2018;59:1127–42. doi: 10.1111/jcpp.12822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Goldin PR, Ziv M, Jazaieri H, Hahn K, Heimberg R, Gross JJ. Impact of cognitive behavioral therapy for social anxiety disorder on the neural dynamics of cognitive reappraisal of negative self-beliefs: randomized clinical trial. JAMA Psychiatry. 2013;70:1048–56. doi: 10.1001/jamapsychiatry.2013.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Thurston MD, Goldin P, Heimberg R, Gross JJ. Self-views in social anxiety disorder: the impact of CBT versus MBSR. J Anxiety Disord. 2017;47:83–90. doi: 10.1016/j.janxdis.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Armstrong T, Olatunji BO. Eye tracking of attention in the affective disorders: a meta-analytic review and synthesis. Clin Psychol Rev. 2012;32:704–23. doi: 10.1016/j.cpr.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cisler JM, Koster EHW. Mechanisms of attentional biases towards threat in anxiety disorders: an integrative review. Clin Psychol Rev. 2010;30:203–16. doi: 10.1016/j.cpr.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Browning M, Holmes EA, Murphy SE, Goodwin GM, Harmer CJ. Lateral prefrontal cortex mediates the cognitive modification of attentional bias. Biol Psychiatry. 2010;67:919–25. doi: 10.1016/j.biopsych.2009.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Monk CS, Nelson EE, McClure EB, Mogg K, Bradley BP, Leibenluft E, et al. Ventrolateral prefrontal cortex activation and attentional bias in response to angry faces in adolescents with generalized anxiety disorder. AJP. 2006;163:1091–7. doi: 10.1176/ajp.2006.163.6.1091. [DOI] [PubMed] [Google Scholar]
- 71.Sylvester CM, Barch DM, Corbetta M, Power JD, Schlaggar BL, Luby JL. Resting state functional connectivity of the ventral attention network in children with a history of depression or anxiety. J Am Acad Child Adolesc Psychiatry. 2013;52:1326–36.e5. doi: 10.1016/j.jaac.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sylvester CM, Corbetta M, Raichle ME, Rodebaugh TL, Schlaggar BL, Sheline YI, et al. Functional network dysfunction in anxiety and anxiety disorders. Trends Neurosci. 2012;35:527–35. doi: 10.1016/j.tins.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bishop S, Duncan J, Brett M, Lawrence AD. Prefrontal cortical function and anxiety: controlling attention to threat-related stimuli. Nat Neurosci. 2004;7:184–8. doi: 10.1038/nn1173. [DOI] [PubMed] [Google Scholar]
- 74.Fu X, Taber-Thomas BC, Pérez-Edgar K. Frontolimbic functioning during threat-related attention: relations to early behavioral inhibition and anxiety in children. Biol Psychol. 2017;122:98–109. doi: 10.1016/j.biopsycho.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fullana MA, Harrison BJ, Soriano-Mas C, Vervliet B, Cardoner N, Àvila-Parcet A, et al. Neural signatures of human fear conditioning: an updated and extended meta-analysis of fMRI studies. Mol Psychiatry. 2016;21:500–8. doi: 10.1038/mp.2015.88. [DOI] [PubMed] [Google Scholar]
- 76.Lissek S, Powers AS, McClure EB, Phelps EA, Woldehawariat G, Grillon C, et al. Classical fear conditioning in the anxiety disorders: a meta-analysis. Behav Res Ther. 2005;43:1391–424. doi: 10.1016/j.brat.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 77.Duits P, Cath DC, Lissek S, Hox JJ, Hamm AO, Engelhard IM, et al. Updated meta-analysis of classical fear conditioning in the anxiety disorders. Depression Anxiety. 2015;32:239–53. doi: 10.1002/da.22353. [DOI] [PubMed] [Google Scholar]
- 78.Pittig A, Treanor M, LeBeau RT, Craske MG. The role of associative fear and avoidance learning in anxiety disorders: Gaps and directions for future research. Neurosci Biobehav Rev. 2018;88:117–40. doi: 10.1016/j.neubiorev.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 79.Gold AL, Abend R, Britton JC, Behrens B, Farber M, Ronkin E, et al. Age differences in the neural correlates of anxiety disorders: An fMRI Study of Response to Learned Threat. Am J Psychiatry. 2020;177:454–63. doi: 10.1176/appi.ajp.2019.19060650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Delgado MR, Nearing KI, LeDoux JE, Phelps EA. Neural circuitry underlying the regulation of conditioned fear and its relation to extinction. Neuron. 2008;59:829–38. doi: 10.1016/j.neuron.2008.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Indovina I, Robbins TW, Núñez-Elizalde AO, Dunn BD, Bishop SJ. Fear-conditioning mechanisms associated with trait vulnerability to anxiety in humans. Neuron. 2011;69:563–71. doi: 10.1016/j.neuron.2010.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Delgado MR, Olsson A, Phelps EA. Extending animal models of fear conditioning to humans. Biol Psychol. 2006;73:39–48. doi: 10.1016/j.biopsycho.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 83.Sullivan RM, Opendak M. Neurobiology of infant fear and anxiety: impacts of delayed amygdala development and attachment figure quality. Biol Psychiatry. 2021;89:641–50. doi: 10.1016/j.biopsych.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shechner T, Hong M, Britton JC, Pine DS, Fox NA. Fear conditioning and extinction across development: evidence from human studies and animal models. Biol Psychol. 2014;100:1–12. doi: 10.1016/j.biopsycho.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dymond S, Dunsmoor JE, Vervliet B, Roche B, Hermans D. Fear generalization in humans: systematic review and implications for anxiety disorder research. Behav Ther. 2015;46:561–82. doi: 10.1016/j.beth.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 86.van Meurs B, Wiggert N, Wicker I, Lissek S. Maladaptive behavioral consequences of conditioned fear-generalization: a pronounced, yet sparsely studied, feature of anxiety pathology. Behav Res Ther. 2014;57:29–37. doi: 10.1016/j.brat.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lissek S, Kaczkurkin AN, Rabin S, Geraci M, Pine DS, Grillon C. Generalized anxiety disorder is associated with overgeneralization of classically conditioned fear. Biol Psychiatry. 2014;75:909–15. doi: 10.1016/j.biopsych.2013.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dunsmoor JE, Paz R. Fear generalization and anxiety: behavioral and neural mechanisms. Biol Psychiatry. 2015;78:336–43. doi: 10.1016/j.biopsych.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 89.El-Bar N, Laufer O, Yoran-Hegesh R, Paz R. Over-generalization in youth with anxiety disorders. Soc Neurosci. 2017;12:76–85. doi: 10.1080/17470919.2016.1167123. [DOI] [PubMed] [Google Scholar]
- 90.Norbury A, Robbins TW, Seymour B. Value generalization in human avoidance learning. ELife. 2018;7:e34779. doi: 10.7554/eLife.34779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lissek S, Rabin S, Heller RE, Lukenbaugh D, Geraci M, Pine DS, et al. Overgeneralization of conditioned fear as a pathogenic marker of panic disorder. Am J Psychiatry. 2010;167:47–55. doi: 10.1176/appi.ajp.2009.09030410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lissek S, Bradford DE, Alvarez RP, Burton P, Espensen-Sturges T, Reynolds RC, et al. Neural substrates of classically conditioned fear-generalization in humans: a parametric fMRI study. Soc Cogn Affect Neurosci. 2014;9:1134–42. doi: 10.1093/scan/nst096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nitschke JB, Sarinopoulos I, Oathes DJ, Johnstone T, Whalen PJ, Davidson RJ, et al. Anticipatory activation in the amygdala and anterior cingulate in generalized anxiety disorder and prediction of treatment response. AJP. 2009;166:302–10. doi: 10.1176/appi.ajp.2008.07101682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bian X-L, Qin C, Cai C-Y, Zhou Y, Tao Y, Lin Y-H, et al. Anterior cingulate cortex to ventral hippocampus circuit mediates contextual fear generalization. J Neurosci. 2019;39:5728–39. doi: 10.1523/JNEUROSCI.2739-18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cullen PK, Gilman TL, Winiecki P, Riccio DC, Jasnow AM. Activity of the anterior cingulate cortex and ventral hippocampus underlie increases in contextual fear generalization. Neurobiol Learn Mem. 2015;124:19–27. doi: 10.1016/j.nlm.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 96.Besnard A, Sahay A. Adult hippocampal neurogenesis, fear generalization, and stress. Neuropsychopharmacology. 2016;41:24–44. doi: 10.1038/npp.2015.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dunsmoor JE, Murphy GL. Stimulus typicality determines how broadly fear is generalized. Psychol Sci. 2014;25:1816–21. doi: 10.1177/0956797614535401. [DOI] [PubMed] [Google Scholar]
- 98.Bennett M, Vervoort E, Boddez Y, Hermans D, Baeyens F. Perceptual and conceptual similarities facilitate the generalization of instructed fear. J Behav Ther Exp Psychiatry. 2015;48:149–55. doi: 10.1016/j.jbtep.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 99.Constantinescu AO, O’Reilly JX, Behrens TEJ. Organizing conceptual knowledge in humans with a gridlike code. Science. 2016;352:1464–8. doi: 10.1126/science.aaf0941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wilson RC, Takahashi YK, Schoenbaum G, Niv Y. Orbitofrontal cortex as a cognitive map of task space. Neuron. 2014;81:267–79. doi: 10.1016/j.neuron.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Robinson OJ, Charney DR, Overstreet C, Vytal K, Grillon C. The adaptive threat bias in anxiety: amygdala–dorsomedial prefrontal cortex coupling and aversive amplification. NeuroImage. 2012;60:523–9. doi: 10.1016/j.neuroimage.2011.11.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Annu Rev Neurosci. 2001;24:167–202. doi: 10.1146/annurev.neuro.24.1.167. [DOI] [PubMed] [Google Scholar]
- 103.Ochsner KN, Gross JJ. The neural bases of emotion and emotion regulation: a valuation perspective. Handbook of emotion regulation, 2nd ed, New York, NY, US: The Guilford Press; 2014. p. 23–42.
- 104.Schäfer JÖ, Naumann E, Holmes EA, Tuschen-Caffier B, Samson AC. Emotion regulation strategies in depressive and anxiety symptoms in youth: a meta-analytic review. J Youth Adolesc. 2017;46:261–76. doi: 10.1007/s10964-016-0585-0. [DOI] [PubMed] [Google Scholar]
- 105.Mennin DS, McLaughlin KA, Flanagan TJ. Emotion regulation deficits in generalized anxiety disorder, social anxiety disorder, and their co-occurrence. J Anxiety Disord. 2009;23:866–71. doi: 10.1016/j.janxdis.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mcclure EB, Pine DS. Social anxiety and emotion regulation: a model for developmental psychopathology perspectives on anxiety disorders. Developmental Psychopathology, John Wiley & Sons, Ltd; 2015. p. 470–502.
- 107.Hofmann SG, Heering S, Sawyer AT, Asnaani A. How to handle anxiety: the effects of reappraisal, acceptance, and suppression strategies on anxious arousal. Behav Res Ther. 2009;47:389–94. doi: 10.1016/j.brat.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Buhle JT, Silvers JA, Wager TD, Lopez R, Onyemekwu C, Kober H, et al. Cognitive reappraisal of emotion: a meta-analysis of human neuroimaging studies. Cereb Cortex. 2014;24:2981–90. doi: 10.1093/cercor/bht154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Quirk GJ, Beer JS. Prefrontal involvement in the regulation of emotion: convergence of rat and human studies. Curr Opin Neurobiol. 2006;16:723–7. doi: 10.1016/j.conb.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 110.Lee H, Heller AS, van Reekum CM, Nelson B, Davidson RJ. Amygdala–prefrontal coupling underlies individual differences in emotion regulation. NeuroImage. 2012;62:1575–81. doi: 10.1016/j.neuroimage.2012.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Morawetz C, Bode S, Baudewig J, Heekeren HR. Effective amygdala-prefrontal connectivity predicts individual differences in successful emotion regulation. Soc Cogn Affect Neurosci. 2017;12:569–85. doi: 10.1093/scan/nsw169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cisler JM, Olatunji BO. Emotion regulation and anxiety disorders. Curr Psychiatry Rep. 2012;14:182–7. doi: 10.1007/s11920-012-0262-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Birn RM, Shackman AJ, Oler JA, Williams LE, McFarlin DR, Rogers GM, et al. Evolutionarily conserved prefrontal-amygdalar dysfunction in early-life anxiety. Mol Psychiatry. 2014;19:915–22. doi: 10.1038/mp.2014.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Barlow DH. Anxiety and its disorders: the nature and treatment of anxiety and panic. Guilford Press; 2004.
- 115.Gallagher MW, Bentley KH, Barlow DH. Perceived control and vulnerability to anxiety disorders: a meta-analytic review. Cogn Ther Res. 2014;38:571–84. [Google Scholar]
- 116.Rakic P, Goldman-Rakic PS. The development and modifiability of the cerebral cortex. Overv Neurosci Res Program Bull. 1982;20:433–8. [PubMed] [Google Scholar]
- 117.Bourgeois JP, Goldman-Rakic PS, Rakic P. Synaptogenesis in the prefrontal cortex of rhesus monkeys. Cereb Cortex. 1994;4:78–96. doi: 10.1093/cercor/4.1.78. [DOI] [PubMed] [Google Scholar]
- 118.Darlington RB, Dunlop SA, Finlay BL. Neural development in metatherian and eutherian mammals: variation and constraint. J Comp Neurol. 1999;411:359–68. [PubMed] [Google Scholar]
- 119.Gee DG, Humphreys KL, Flannery J, Goff B, Telzer EH, Shapiro M, et al. A developmental shift from positive to negative connectivity in human amygdala–prefrontal circuitry. J Neurosci. 2013;33:4584–93. doi: 10.1523/JNEUROSCI.3446-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Silvers JA, Insel C, Powers A, Franz P, Helion C, Martin RE, et al. vlPFC–vmPFC–amygdala interactions underlie age-related differences in cognitive regulation of emotion. Cereb Cortex. 2017;27:3502–14. doi: 10.1093/cercor/bhw073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fair DA, Cohen AL, Power JD, Dosenbach NUF, Church JA, Miezin FM, et al. Functional brain networks develop from a “local to distributed” organization. PLOS Computational Biol. 2009;5:e1000381. doi: 10.1371/journal.pcbi.1000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Fair DA, Dosenbach NUF, Church JA, Cohen AL, Brahmbhatt S, Miezin FM, et al. Development of distinct control networks through segregation and integration. PNAS. 2007;104:13507–12. doi: 10.1073/pnas.0705843104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral inhibition: linking biology and behavior within a developmental framework. Annu Rev Psychol. 2005;56:235–62. doi: 10.1146/annurev.psych.55.090902.141532. [DOI] [PubMed] [Google Scholar]
- 124.Clauss JA, Blackford JU. Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study. J Am Acad Child Adolesc Psychiatry. 2012;51:1066–75.e1. doi: 10.1016/j.jaac.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Clauss JA, Avery SN, Blackford JU. The nature of individual differences in inhibited temperament and risk for psychiatric disease: a review and meta-analysis. Prog Neurobiol. 2015;0:23–45. doi: 10.1016/j.pneurobio.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Henderson HA, Pine DS, Fox NA. Behavioral inhibition and developmental risk: a dual-processing perspective. Neuropsychopharmacology. 2015;40:207–24. doi: 10.1038/npp.2014.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Oler JA, Fox AS, Shelton SE, Rogers J, Dyer TD, Davidson RJ, et al. Amygdalar and hippocampal substrates of anxious temperament differ in their heritability. Nature. 2010;466:864–8. doi: 10.1038/nature09282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Fox AS, Oler JA, Shackman AJ, Shelton SE, Raveendran M, McKay DR, et al. Intergenerational neural mediators of early-life anxious temperament. PNAS. 2015;112:9118–22. doi: 10.1073/pnas.1508593112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Robinson JL, Kagan J, Reznick JS, Corley R. The heritability of inhibited and uninhibited behavior: a twin study. Developmental Psychol. 1992;28:1030–7. [Google Scholar]
- 130.Williamson DE, Coleman K, Bacanu S-A, Devlin BJ, Rogers J, Ryan ND, et al. Heritability of fearful-anxious endophenotypes in infant rhesus macaques: a preliminary report. Biol Psychiatry. 2003;53:284–91. doi: 10.1016/s0006-3223(02)01601-3. [DOI] [PubMed] [Google Scholar]
- 131.Gagne C, Dayan P, Bishop SJ. When planning to survive goes wrong: predicting the future and replaying the past in anxiety and PTSD. Curr Opin Behav Sci. 2018;24:89–95. [Google Scholar]
- 132.Zorowitz S, Momennejad I, Daw ND. Anxiety, avoidance, and sequential evaluation. computational. Psychiatry. 2020;4:1–17. doi: 10.1162/cpsy_a_00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bishop SJ, Gagne C. Anxiety, depression, and decision making: a computational perspective. Annu Rev Neurosci. 2018;41:371–88. doi: 10.1146/annurev-neuro-080317-062007. [DOI] [PubMed] [Google Scholar]
- 134.Huys QJM, Maia TV, Frank MJ. Computational psychiatry as a bridge from neuroscience to clinical applications. Nat Neurosci. 2016;19:404–13. doi: 10.1038/nn.4238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Soltani A, Izquierdo A. Adaptive learning under expected and unexpected uncertainty. Nat Rev Neurosci. 2019;20:635–44. doi: 10.1038/s41583-019-0180-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yau JO-Y, McNally GP. Rules for aversive learning and decision-making. Curr Opin Behav Sci. 2019;26:1–8. [Google Scholar]
- 137.Pulcu E, Shkreli L, Holst CG, Woud ML, Craske MG, Browning M, et al. The effects of the angiotensin II receptor antagonist losartan on appetitive versus aversive learning: a randomized controlled trial. Biol Psychiatry. 2019;86:397–404. doi: 10.1016/j.biopsych.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 138.Mkrtchian A, Aylward J, Dayan P, Roiser JP, Robinson OJ. Modeling avoidance in mood and anxiety disorders using reinforcement learning. Biol Psychiatry. 2017;82:532–9. doi: 10.1016/j.biopsych.2017.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Behrens TEJ, Woolrich MW, Walton ME, Rushworth MFS. Learning the value of information in an uncertain world. Nat Neurosci. 2007;10:1214–21. doi: 10.1038/nn1954. [DOI] [PubMed] [Google Scholar]
- 140.Browning M, Behrens TE, Jocham G, O’Reilly JX, Bishop SJ. Anxious individuals have difficulty learning the causal statistics of aversive environments. Nat Neurosci. 2015;18:590–6. doi: 10.1038/nn.3961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Huang H, Thompson W, Paulus MP. Computational dysfunctions in anxiety: failure to differentiate signal from noise. Biol Psychiatry. 2017;82:440–6. doi: 10.1016/j.biopsych.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Niv Y. Reinforcement learning in the brain. J Math Psychol. 2009;53:139–54. [Google Scholar]
- 143.Wang JX, Kurth-Nelson Z, Kumaran D, Tirumala D, Soyer H, Leibo JZ, et al. Prefrontal cortex as a meta-reinforcement learning system. Nat Neurosci. 2018;21:860–8. doi: 10.1038/s41593-018-0147-8. [DOI] [PubMed] [Google Scholar]
- 144.Saddoris MP, Gallagher M, Schoenbaum G. Rapid associative encoding in basolateral amygdala depends on connections with orbitofrontal cortex. Neuron. 2005;46:321–31. doi: 10.1016/j.neuron.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 145.Li J, Schiller D, Schoenbaum G, Phelps EA, Daw ND. Differential roles of human striatum and amygdala in associative learning. Nat Neurosci. 2011;14:1250–2. doi: 10.1038/nn.2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Morrison SE, Saez A, Lau B, Salzman CD. Different time courses for learning-related changes in amygdala and orbitofrontal cortex. Neuron. 2011;71:1127–40. doi: 10.1016/j.neuron.2011.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Rudebeck PH, Ripple JA, Mitz AR, Averbeck BB, Murray EA. Amygdala contributions to stimulus–reward encoding in the macaque medial and orbital frontal cortex during learning. J Neurosci. 2017;37:2186–202. doi: 10.1523/JNEUROSCI.0933-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Christakou A, Robbins TW, Everitt BJ. Prefrontal cortical–ventral striatal interactions involved in affective modulation of attentional performance: implications for corticostriatal circuit function. J Neurosci. 2004;24:773–80. doi: 10.1523/JNEUROSCI.0949-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Haber SN, Knutson B. The reward circuit: linking primate anatomy and human imaging. Neuropsychopharmacology. 2010;35:4–26. doi: 10.1038/npp.2009.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Taub AH, Perets R, Kahana E, Paz R. Oscillations synchronize amygdala-to-prefrontal primate circuits during aversive learning. Neuron. 2018;97:291–98.e3. doi: 10.1016/j.neuron.2017.11.042. [DOI] [PubMed] [Google Scholar]
- 151.Rich EL, Wallis JD. Decoding subjective decisions from orbitofrontal cortex. Nat Neurosci. 2016;19:973–80. doi: 10.1038/nn.4320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Dugas MJ, Buhr K, Ladouceur R. The role of intolerance of uncertainty in etiology and maintenance. generalized anxiety disorder: advances in research and practice, New York, NY, US: The Guilford Press; 2004. p. 143–63.
- 153.Carleton RN, Mulvogue MK, Thibodeau MA, McCabe RE, Antony MM, Asmundson GJG. Increasingly certain about uncertainty: Intolerance of uncertainty across anxiety and depression. J Anxiety Disord. 2012;26:468–79. doi: 10.1016/j.janxdis.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 154.Grupe DW, Nitschke JB. Uncertainty and anticipation in anxiety: an integrated neurobiological and psychological perspective. Nat Rev Neurosci. 2013;14:488–501. doi: 10.1038/nrn3524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lee JK, Orsillo SM, Roemer L, Allen LB. Distress and avoidance in generalized anxiety disorder: exploring the relationships with intolerance of uncertainty and worry. Cogn Behav Ther. 2010;39:126–36. doi: 10.1080/16506070902966918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hur J, Smith JF, DeYoung KA, Anderson AS, Kuang J, Kim HC, et al. Anxiety and the neurobiology of temporally uncertain threat anticipation. J Neurosci. 2020;40:7949–64. doi: 10.1523/JNEUROSCI.0704-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Arnaudova I, Kindt M, Fanselow M, Beckers T. Pathways towards the proliferation of avoidance in anxiety and implications for treatment. Behav Res Ther. 2017;96:3–13. doi: 10.1016/j.brat.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 158.Walz N, Mühlberger A, Pauli P. A human open field test reveals thigmotaxis related to agoraphobic fear. Biol Psychiatry. 2016;80:390–97. doi: 10.1016/j.biopsych.2015.12.016. [DOI] [PubMed] [Google Scholar]
- 159.Bach DR. Anxiety-like behavioural inhibition is normative under environmental threat-reward correlations. PLOS Computational Biol. 2015;11:e1004646. doi: 10.1371/journal.pcbi.1004646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bolles RC. Species-specific defense reactions and avoidance learning. Psychological Rev. 1970;77:32–48. [Google Scholar]
- 161.Bouton ME, Mineka S, Barlow DH. A modern learning theory perspective on the etiology of panic disorder. Psychol Rev. 2001;108:4–32. doi: 10.1037/0033-295x.108.1.4. [DOI] [PubMed] [Google Scholar]
- 162.Salkovskis PM, Clark DM, Hackmann A, Wells A, Gelder MG. An experimental investigation of the role of safety-seeking behaviours in the maintenance of panic disorder with agoraphobia. Behav Res Ther. 1999;37:559–74. doi: 10.1016/s0005-7967(98)00153-3. [DOI] [PubMed] [Google Scholar]
- 163.Kirlic N, Young J, Aupperle RL. Animal to human translational paradigms relevant for approach avoidance conflict decision making. Behav Res Ther. 2017;96:14–29. doi: 10.1016/j.brat.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gründemann J, Bitterman Y, Lu T, Krabbe S, Grewe BF, Schnitzer MJ, et al. Amygdala ensembles encode behavioral states. Science. 2019;364:eaav8736. [DOI] [PubMed]
- 165.Wenzel JM, Oleson EB, Gove WN, Cole AB, Gyawali U, Dantrassy HM, et al. Phasic dopamine signals in the nucleus accumbens that cause active avoidance require endocannabinoid mobilization in the midbrain. Curr Biol. 2018;28:1392–404.e5. doi: 10.1016/j.cub.2018.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Ramirez F, Moscarello JM, LeDoux JE, Sears RM. Active avoidance requires a serial basal amygdala to nucleus accumbens shell circuit. J Neurosci. 2015;35:3470–7. doi: 10.1523/JNEUROSCI.1331-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Lovett-Barron M, Chen R, Bradbury S, Andalman AS, Wagle M, Guo S, et al. Multiple convergent hypothalamus-brainstem circuits drive defensive behavior. Nat Neurosci. 2020;23:959–67. [DOI] [PMC free article] [PubMed]
- 168.Gu Y, Piper WT, Branigan LA, Vazey EM, Aston-Jones G, Lin L, et al. A brainstem-central amygdala circuit underlies defensive responses to learned threats. Mol Psychiatry. 2020;25:640–54. doi: 10.1038/s41380-019-0599-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Franklin TB, Silva BA, Perova Z, Marrone L, Masferrer ME, Zhan Y, et al. Prefrontal cortical control of a brainstem social behavior circuit. Nat Neurosci. 2017;20:260–70. doi: 10.1038/nn.4470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Warden MR, Selimbeyoglu A, Mirzabekov JJ, Lo M, Thompson KR, Kim S-Y, et al. A prefrontal cortex–brainstem neuronal projection that controls response to behavioural challenge. Nature. 2012;492:428–32. doi: 10.1038/nature11617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Diehl MM, Iravedra-Garcia JM, Morán-Sierra J, Rojas-Bowe G, Gonzalez-Diaz FN, Valentín-Valentín VP, et al. Divergent projections of the prelimbic cortex bidirectionally regulate active avoidance. ELife. 2020;9:e59281. doi: 10.7554/eLife.59281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ongür D, Price JL. The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cereb Cortex N Y N 1991. 2000;10:206–19. [DOI] [PubMed]
- 173.Pandya D, Seltzer B, Petrides M, Cipolloni PB. Cerebral cortex: architecture, connections, and the dual origin concept. Oxford University Press; 2015.
- 174.Zikopoulos B, García-Cabezas MÁ, Barbas H. Parallel trends in cortical gray and white matter architecture and connections in primates allow fine study of pathways in humans and reveal network disruptions in autism. PLOS Biol. 2018;16:e2004559. doi: 10.1371/journal.pbio.2004559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Perusini JN, Fanselow MS. Neurobehavioral perspectives on the distinction between fear and anxiety. Learn Mem. 2015;22:417–25. doi: 10.1101/lm.039180.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Diehl MM, Bravo-Rivera C, Quirk GJ. The study of active avoidance: a platform for discussion. Neurosci Biobehav Rev. 2019;107:229–37. doi: 10.1016/j.neubiorev.2019.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Heukelum S, van, Mars RB, Guthrie M, Buitelaar JK, Beckmann CF, Tiesinga PHE, et al. Where is cingulate cortex? a cross-species view. Trends Neurosci. 2020;43:285–99. doi: 10.1016/j.tins.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 178.Pessoa L, Adolphs R. Emotion processing and the amygdala: from a ‘low road’ to ‘many roads’ of evaluating biological significance. Nat Rev Neurosci. 2010;11:773–83. doi: 10.1038/nrn2920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Fox AS, Oler JA, Tromp DPM, Fudge JL, Kalin NH. Extending the amygdala in theories of threat processing. Trends Neurosci. 2015;38:319–29. doi: 10.1016/j.tins.2015.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Carmichael ST, Price JL. Connectional networks within the orbital and medial prefrontal cortex of macaque monkeys. J Comp Neurol. 1996;371:179–207. doi: 10.1002/(SICI)1096-9861(19960722)371:2<179::AID-CNE1>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 181.DeFelipe J. Types of neurons, synaptic connections and chemical characteristics of cells immunoreactive for calbindin-D28K, parvalbumin and calretinin in the neocortex. J Chem Neuroanat. 1997;14:1–19. doi: 10.1016/s0891-0618(97)10013-8. [DOI] [PubMed] [Google Scholar]
- 182.Barbas H, Wang J, Joyce MKP, García-Cabezas MÁ. Pathway mechanism for excitatory and inhibitory control in working memory. J Neurophysiol. 2018;120:2659–78. doi: 10.1152/jn.00936.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Joyce MKP, García-Cabezas MÁ, John YJ, Barbas H. Serial prefrontal pathways are positioned to balance cognition and emotion in primates. J Neurosci. 2020;40:8306–28. doi: 10.1523/JNEUROSCI.0860-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.An X, Bandler R, Ongür D, Price JL. Prefrontal cortical projections to longitudinal columns in the midbrain periaqueductal gray in macaque monkeys. J Comp Neurol. 1998;401:455–79. [PubMed] [Google Scholar]
- 185.Rempel-Clower NL, Barbas H. Topographic organization of connections between the hypothalamus and prefrontal cortex in the rhesus monkey. J Comp Neurol. 1998;398:393–419. doi: 10.1002/(sici)1096-9861(19980831)398:3<393::aid-cne7>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 186.Medalla M, Barbas H. Synapses with inhibitory neurons differentiate anterior cingulate from dorsolateral prefrontal pathways associated with cognitive control. Neuron. 2009;61:609–20. doi: 10.1016/j.neuron.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Wang X-J, Tegner J, Constantinidis C, Goldman-Rakic PS. Division of labor among distinct subtypes of inhibitory neurons in a cortical microcircuit of working memory. Proc Natl Acad Sci. 2004;101:1368–73. doi: 10.1073/pnas.0305337101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Chavanne AV, Robinson OJ. The overlapping neurobiology of induced And pathological anxiety: A meta-analysis of functional neural activation. Am J Psychiatry. 2021;178:156–64. doi: 10.1176/appi.ajp.2020.19111153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Wang J, John Y, Barbas H. Pathways for contextual memory: the primate hippocampal pathway to anterior cingulate cortex. Cereb Cortex. 2021;31:1807–26. doi: 10.1093/cercor/bhaa333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Aggleton JP, Wright NF, Rosene DL, Saunders RC. Complementary patterns of direct amygdala and hippocampal projections to the macaque prefrontal cortex. Cereb Cortex. 2015;25:4351–73. doi: 10.1093/cercor/bhv019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Barbas H, Blatt GJ. Topographically specific hippocampal projections target functionally distinct prefrontal areas in the rhesus monkey. Hippocampus. 1995;5:511–33. doi: 10.1002/hipo.450050604. [DOI] [PubMed] [Google Scholar]
- 192.Insausti R, Muñoz M. Cortical projections of the non-entorhinal hippocampal formation in the cynomolgus monkey (Macaca fascicularis): Nonentorhinal hippocampal output to cortex in primates. Eur J Neurosci. 2001;14:435–51. doi: 10.1046/j.0953-816x.2001.01662.x. [DOI] [PubMed] [Google Scholar]
- 193.Rosene D, Van Hoesen G. Hippocampal efferents reach widespread areas of cerebral cortex and amygdala in the rhesus monkey. Science. 1977;198:315–7. doi: 10.1126/science.410102. [DOI] [PubMed] [Google Scholar]
- 194.Eichenbaum H. Prefrontal–hippocampal interactions in episodic memory. Nat Rev Neurosci. 2017;18:547–58. doi: 10.1038/nrn.2017.74. [DOI] [PubMed] [Google Scholar]
- 195.Leblanc H, Ramirez S. Linking social cognition to learning and memory. J Neurosci. 2020;40:8782–98. doi: 10.1523/JNEUROSCI.1280-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Barbas H, De Olmos J. Projections from the amygdala to basoventral and mediodorsal prefrontal regions in the rhesus monkey. J Comp Neurol. 1990;300:549–71. doi: 10.1002/cne.903000409. [DOI] [PubMed] [Google Scholar]
- 197.Ghashghaei HT, Hilgetag CC, Barbas H. Sequence of information processing for emotions based on the anatomic dialogue between prefrontal cortex and amygdala. Neuroimage. 2007;34:905–23. doi: 10.1016/j.neuroimage.2006.09.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Porrino LJ, Crane AM, Goldman-Rakic PS. Direct and indirect pathways from the amygdala to the frontal lobe in rhesus monkeys. J Comp Neurol. 1981;198:121–36. doi: 10.1002/cne.901980111. [DOI] [PubMed] [Google Scholar]
- 199.Ghashghaei HT, Barbas H. Pathways for emotion: interactions of prefrontal and anterior temporal pathways in the amygdala of the rhesus monkey. Neuroscience. 2002;115:1261–79. doi: 10.1016/s0306-4522(02)00446-3. [DOI] [PubMed] [Google Scholar]
- 200.Zikopoulos B, Höistad M, John Y, Barbas H. Posterior orbitofrontal and anterior cingulate pathways to the amygdala target inhibitory and excitatory systems with opposite functions. J Neurosci. 2017;37:5051–64. doi: 10.1523/JNEUROSCI.3940-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Greengard P. The neurobiology of slow synaptic transmission. Science. 2001;294:1024–30. doi: 10.1126/science.294.5544.1024. [DOI] [PubMed] [Google Scholar]
- 202.Svenningsson P, Nishi A, Fisone G, Girault J-A, Nairn AC, Greengard P. DARPP-32: an Integrator of Neurotransmission. Annu Rev Pharm Toxicol. 2004;44:269–96. doi: 10.1146/annurev.pharmtox.44.101802.121415. [DOI] [PubMed] [Google Scholar]
- 203.Inglis FM, Moghaddam B. Dopaminergic innervation of the amygdala is highly responsive to stress. J Neurochemistry. 2008;72:1088–94. doi: 10.1046/j.1471-4159.1999.0721088.x. [DOI] [PubMed] [Google Scholar]
- 204.Rosenkranz JA, Grace AA. Cellular mechanisms of infralimbic and prelimbic prefrontal cortical inhibition and dopaminergic modulation of basolateral amygdala neurons in vivo. J Neurosci. 2002;22:324–37. doi: 10.1523/JNEUROSCI.22-01-00324.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Correll CM, Rosenkranz JA, Grace AA. Chronic cold stress alters prefrontal cortical modulation of amygdala neuronal activity in rats. Biol Psychiatry. 2005;58:382–91. doi: 10.1016/j.biopsych.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 206.Yokoyama M, Suzuki E, Sato T, Maruta S, Watanabe S, Miyaoka H. Amygdalic levels of dopamine and serotonin rise upon exposure to conditioned fear stress without elevation of glutamate. Neurosci Lett. 2005;379:37–41. doi: 10.1016/j.neulet.2004.12.047. [DOI] [PubMed] [Google Scholar]
- 207.Zikopoulos B, John YJ, García-Cabezas MÁ, Bunce JG, Barbas H. The intercalated nuclear complex of the primate amygdala. Neuroscience. 2016;330:267–90. doi: 10.1016/j.neuroscience.2016.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Likhtik E, Popa D, Apergis-Schoute J, Fidacaro GA, Paré D. Amygdala intercalated neurons are required for expression of fear extinction. Nature. 2008;454:642–5. doi: 10.1038/nature07167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Amano T, Unal CT, Paré D. Synaptic correlates of fear extinction in the amygdala. Nat Neurosci. 2010;13:489–94. doi: 10.1038/nn.2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Galvan A, Caiola MJ, Albaugh DL. Advances in Optogenetic and Chemogenetic Methods to Study Brain Circuits in Non-human Primates. J Neural Transm Vienna Austria 1996. 2018;125:547–63. [DOI] [PMC free article] [PubMed]
- 211.Goldman-Rakic PS, Porrino LJ. The primate mediodorsal (MD) nucleus and its projection to the frontal lobe. J Comp Neurol. 1985;242:535–60. doi: 10.1002/cne.902420406. [DOI] [PubMed] [Google Scholar]
- 212.Dermon CR, Barbas H. Contralateral thalamic projections predominantly reach transitional cortices in the rhesus monkey. J Comp Neurol. 1994;344:508–31. doi: 10.1002/cne.903440403. [DOI] [PubMed] [Google Scholar]
- 213.Puelles L, Rubenstein JLR. Forebrain gene expression domains and the evolving prosomeric model. Trends Neurosci. 2003;26:469–76. doi: 10.1016/S0166-2236(03)00234-0. [DOI] [PubMed] [Google Scholar]
- 214.Wells AM, García-Cabezas MÁ, Barbas H. Topological atlas of the hypothalamus in adult rhesus monkey. Brain Struct Funct. 2020;225:1777–803. doi: 10.1007/s00429-020-02093-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.McAlonan K, Cavanaugh J, Wurtz RH. Attentional modulation of thalamic reticular neurons. J Neurosci. 2006;26:4444–50. doi: 10.1523/JNEUROSCI.5602-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Crick F. Function of the thalamic reticular complex: the searchlight hypothesis. Proc Natl Acad Sci. 1984;81:4586–90. doi: 10.1073/pnas.81.14.4586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Zikopoulos B, Barbas H. Circuits for multisensory integration and attentional modulation through the prefrontal cortex and the thalamic reticular nucleus in primates. Reviews in the Neurosciences. 2007;18:1–25. [DOI] [PMC free article] [PubMed]
- 218.Pinault D. The thalamic reticular nucleus: structure, function and concept. Brain Res Brain Res Rev. 2004;46:1–31. doi: 10.1016/j.brainresrev.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 219.Lam Y-W, Sherman SM. Functional organization of the thalamic input to the thalamic reticular nucleus. J Neurosci. 2011;31:6791–9. doi: 10.1523/JNEUROSCI.3073-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Zikopoulos B, Barbas H. Prefrontal projections to the thalamic reticular nucleus form a unique circuit for attentional mechanisms. J Neurosci. 2006;26:7348–61. doi: 10.1523/JNEUROSCI.5511-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Zikopoulos B, Barbas H. Pathways for emotions and attention converge on the thalamic reticular nucleus in primates. J Neurosci. 2012;32:5338–50. doi: 10.1523/JNEUROSCI.4793-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Crandall SR, Cruikshank SJ, Connors BW. A corticothalamic switch: controlling the thalamus with dynamic synapses. Neuron. 2015;86:768–82. doi: 10.1016/j.neuron.2015.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Kosciessa JQ, Lindenberger U, Garrett DD. Thalamocortical excitability modulation guides human perception under uncertainty. Nat Commun. 2021;12:2430. doi: 10.1038/s41467-021-22511-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.John YJ, Bullock D, Zikopoulos B, Barbas H. Anatomy and computational modeling of networks underlying cognitive-emotional interaction. Front Hum Neurosci. 2013;77, Article 101:1–26. [DOI] [PMC free article] [PubMed]
- 225.John YJ, Zikopoulos B, Bullock D, Barbas H. The emotional gatekeeper: a computational model of attentional selection and suppression through the pathway from the amygdala to the inhibitory thalamic reticular nucleus. PLoS Comput Biol. 2016;12:e1004722. doi: 10.1371/journal.pcbi.1004722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Schiller D, Levy I, Niv Y, LeDoux JE, Phelps EA. From fear to safety and back: reversal of fear in the human brain. J Neurosci. 2008;28:11517–25. doi: 10.1523/JNEUROSCI.2265-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Timbie C, García-Cabezas MÁ, Zikopoulos B, Barbas H. Organization of primate amygdalar–thalamic pathways for emotions. PLoS Biol. 2020;18:e3000639. doi: 10.1371/journal.pbio.3000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Halassa MM, Chen Z, Wimmer RD, Brunetti PM, Zhao S, Zikopoulos B, et al. State-dependent architecture of thalamic reticular subnetworks. Cell. 2014;158:808–21. doi: 10.1016/j.cell.2014.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Sánchez-González MÁ, García-Cabezas MÁ, Rico B, Cavada C. The primate thalamus is a key target for brain dopamine. J Neurosci. 2005;25:6076–83. doi: 10.1523/JNEUROSCI.0968-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.García-Cabezas MA, Rico B, Sánchez-González MA, Cavada C. Distribution of the dopamine innervation in the macaque and human thalamus. Neuroimage. 2007;34:965–84. doi: 10.1016/j.neuroimage.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 231.García-Cabezas MA, Martínez-Sánchez P, Sánchez-González MA, Garzón M, Cavada C. Dopamine innervation in the thalamus: monkey versus rat. Cereb Cortex. 2009;19:424–34. doi: 10.1093/cercor/bhn093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Barbas H, García-Cabezas MÁ, Zikopoulos B. Frontal-thalamic circuits associated with language. Brain Lang. 2013;126:49–61. doi: 10.1016/j.bandl.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Dabney W, Kurth-Nelson Z, Uchida N, Starkweather CK, Hassabis D, Munos R, et al. A distributional code for value in dopamine-based reinforcement learning. Nature. 2020;577:671–5. doi: 10.1038/s41586-019-1924-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Radulescu A, Niv Y, Ballard I. Holistic reinforcement learning: the role of structure and attention. Trends Cogn Sci. 2019;23:278–92. doi: 10.1016/j.tics.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Fiorillo CD, Tobler PN, Schultz W. Discrete coding of reward probability and uncertainty by dopamine neurons. Science. 2003;299:1898–902. doi: 10.1126/science.1077349. [DOI] [PubMed] [Google Scholar]
- 236.Lafuente V, de, Romo R. Dopamine neurons code subjective sensory experience and uncertainty of perceptual decisions. PNAS. 2011;108:19767–71. doi: 10.1073/pnas.1117636108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Gershman SJ, Uchida N. Believing in dopamine. Nat Rev Neurosci. 2019;20:703–14. doi: 10.1038/s41583-019-0220-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Starkweather CK, Gershman SJ, Uchida N. The medial prefrontal cortex shapes dopamine reward prediction errors under state uncertainty. Neuron. 2018;98:616–29.e6. doi: 10.1016/j.neuron.2018.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Kahnt T, Tobler PN. Dopamine regulates stimulus generalization in the human hippocampus. ELife. 2016;5:e12678. doi: 10.7554/eLife.12678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Jo YS, Heymann G, Zweifel LS. Dopamine neurons reflect the uncertainty in fear generalization. Neuron. 2018;100:916–25.e3. doi: 10.1016/j.neuron.2018.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Abraham AD, Neve KA, Lattal KM. Activation of D1/5 dopamine receptors: a common mechanism for enhancing extinction of fear and reward-seeking behaviors. Neuropsychopharmacology. 2016;41:2072–81. doi: 10.1038/npp.2016.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Luo R, Uematsu A, Weitemier A, Aquili L, Koivumaa J, McHugh TJ, et al. A dopaminergic switch for fear to safety transitions. Nat Commun. 2018;9:2483. doi: 10.1038/s41467-018-04784-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Insel TR, Ninan PT, Aloi J, Jimerson DC, Skolnick P, Paul SM. A benzodiazepine receptor—mediated model of anxiety: studies in nonhuman primates and clinical implications. Arch Gen Psychiatry. 1984;41:741–50. doi: 10.1001/archpsyc.1984.01790190015002. [DOI] [PubMed] [Google Scholar]
- 244.Brooks SJ, Stein DJ. A systematic review of the neural bases of psychotherapy for anxiety and related disorders. Dialogues Clin Neurosci. 2015;17:261–79. doi: 10.31887/DCNS.2015.17.3/sbrooks. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Ma Y. Neuropsychological mechanism underlying antidepressant effect: a systematic meta-analysis. Mol Psychiatry. 2015;20:311–9. doi: 10.1038/mp.2014.24. [DOI] [PubMed] [Google Scholar]
- 246.Gorka SM, Young CB, Klumpp H, Kennedy AE, Francis J, Ajilore O, et al. Emotion-based brain mechanisms and predictors for SSRI and CBT treatment of anxiety and depression: a randomized trial. Neuropsychopharmacology. 2019;44:1639–48. doi: 10.1038/s41386-019-0407-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Paulus MP, Feinstein JS, Castillo G, Simmons AN, Stein MB. Dose-dependent decrease of activation in bilateral amygdala and insula by lorazepam during emotion processing. Arch Gen Psychiatry. 2005;62:282–8. doi: 10.1001/archpsyc.62.3.282. [DOI] [PubMed] [Google Scholar]
- 248.Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox N, Leibenluft E, et al. Attention bias modification treatment: a meta-analysis towards the establishment of novel treatment for anxiety. Biol Psychiatry. 2010;68:982–90. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Linetzky M, Pergamin-Hight L, Pine DS, Bar-Haim Y. Quantitative evaluation of the clinical efficacy of attention bias modification treatment for anxiety disorders. Depression Anxiety. 2015;32:383–91. doi: 10.1002/da.22344. [DOI] [PubMed] [Google Scholar]
- 250.Berking M, Wupperman P, Reichardt A, Pejic T, Dippel A, Znoj H. Emotion-regulation skills as a treatment target in psychotherapy. Behav Res Ther. 2008;46:1230–7. doi: 10.1016/j.brat.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 251.Aldao A, Jazaieri H, Goldin PR, Gross JJ. Adaptive and maladaptive emotion regulation strategies: interactive effects during CBT for social anxiety disorder. J Anxiety Disord. 2014;28:382–9. doi: 10.1016/j.janxdis.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Jazaieri H, Goldin PR, Gross JJ. Treating social anxiety disorder with CBT: impact on emotion regulation and satisfaction with life. Cogn Ther Res. 2017;41:406–16. [Google Scholar]
- 253.Hofmann SG, Hay AC. Rethinking avoidance: toward a balanced approach to avoidance in treating anxiety disorders. J Anxiety Disord. 2018;55:14–21. doi: 10.1016/j.janxdis.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Bos FM, Schoevers RA, aan het Rot M. Experience sampling and ecological momentary assessment studies in psychopharmacology: a systematic review. Eur Neuropsychopharmacol. 2015;25:1853–64. doi: 10.1016/j.euroneuro.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 255.Smith AR, Kircanski K, Brotman MA, Do QB, Subar AR, Silk JS, et al. Advancing clinical neuroscience through enhanced tools: pediatric social anxiety as an example. Depression Anxiety. 2019;36:701–11. doi: 10.1002/da.22937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Schueller SM, Aguilera A, Mohr DC. Ecological momentary interventions for depression and anxiety. Depression Anxiety. 2017;34:540–5. doi: 10.1002/da.22649. [DOI] [PubMed] [Google Scholar]
- 257.Colombo D, Fernández-Álvarez J, Patané A, Semonella M, Kwiatkowska M, García-Palacios A, et al. Current state and future directions of technology-based ecological momentary assessment and intervention for major depressive disorder: a systematic review. J Clin Med. 2019;8:465. doi: 10.3390/jcm8040465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Gomez AF, Barthel AL, Hofmann SG. Comparing the efficacy of benzodiazepines and serotonergic anti-depressants for adults with generalized anxiety disorder: a meta-analytic review. Expert Opin Pharmacother. 2018;19:883–94. doi: 10.1080/14656566.2018.1472767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Springer KS, Levy HC, Tolin DF. Remission in CBT for adult anxiety disorders: a meta-analysis. Clin Psychol Rev. 2018;61:1–8. doi: 10.1016/j.cpr.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 260.Ferrarelli F, Phillips ML. Examining and modulating neural circuits in psychiatric disorders with transcranial magnetic stimulation and electroencephalography: present practices and future developments. Am J Psychiatry. 2021:In Press. [DOI] [PMC free article] [PubMed]
- 261.Sagliano L, Atripaldi D, De Vita D, D’Olimpio F, Trojano L. Non-invasive brain stimulation in generalized anxiety disorder: A systematic review. Prog Neuro-Psychopharmacol Biol Psychiatry. 2019;93:31–38. doi: 10.1016/j.pnpbp.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 262.Berlim MT, van den Eynde F, Tovar-Perdomo S, Daskalakis ZJ. Response, remission and drop-out rates following high-frequency repetitive transcranial magnetic stimulation (rTMS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. Psychol Med. 2014;44:225–39. doi: 10.1017/S0033291713000512. [DOI] [PubMed] [Google Scholar]
- 263.Chen L, Hudaib A-R, Hoy KE, Fitzgerald PB. Is rTMS effective for anxiety symptoms in major depressive disorder? An efficacy analysis comparing left-sided high-frequency, right-sided low-frequency, and sequential bilateral rTMS protocols. Depression Anxiety. 2019;36:723–31. doi: 10.1002/da.22894. [DOI] [PubMed] [Google Scholar]
- 264.Berlim MT, Van den Eynde F. Repetitive transcranial magnetic stimulation over the dorsolateral prefrontal cortex for treating posttraumatic stress disorder: an exploratory meta-analysis of randomized, double-blind and sham-controlled trials. Can J Psychiatry. 2014;59:487–96. doi: 10.1177/070674371405900905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Yesavage JA, Fairchild JK, Mi Z, Biswas K, Davis-Karim A, Phibbs CS, et al. Effect of repetitive transcranial magnetic stimulation on treatment-resistant major depression in us veterans: a randomized clinical trial. JAMA Psychiatry. 2018;75:884–93. doi: 10.1001/jamapsychiatry.2018.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Diefenbach GJ, Assaf M, Goethe JW, Gueorguieva R, Tolin DF. Improvements in emotion regulation following repetitive transcranial magnetic stimulation for generalized anxiety disorder. J Anxiety Disord. 2016;43:1–7. doi: 10.1016/j.janxdis.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 267.Carmi L, Tendler A, Bystritsky A, Hollander E, Blumberger DM, Daskalakis J, et al. Efficacy and safety of deep transcranial magnetic stimulation for obsessive-compulsive disorder: a prospective multicenter randomized double-blind placebo-controlled trial. AJP. 2019;176:931–8. doi: 10.1176/appi.ajp.2019.18101180. [DOI] [PubMed] [Google Scholar]
- 268.Philip NS, Barredo J, van’t Wout-Frank M, Tyrka AR, Price LH, Carpenter LL. Network mechanisms of clinical response to transcranial magnetic stimulation in posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 2018;83:263–72. doi: 10.1016/j.biopsych.2017.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Folloni D, Verhagen L, Mars RB, Fouragnan E, Constans C, Aubry J-F, et al. Manipulation of subcortical and deep cortical activity in the primate brain using transcranial focused ultrasound stimulation. Neuron. 2019;101:1109–16.e5. doi: 10.1016/j.neuron.2019.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Cohen A, Keynan JN, Jackont G, Green N, Rashap I, Shani O, et al. Multi-modal virtual scenario enhances neurofeedback learning. Front Robot AI. 2016;3:52.
- 271.Roth BL. DREADDs for neuroscientists. Neuron. 2016;89:683–94. doi: 10.1016/j.neuron.2016.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Raper J, Murphy L, Richardson R, Romm Z, Kovacs-Balint Z, Payne C, et al. Chemogenetic inhibition of the amygdala modulates emotional behavior expression in infant rhesus monkeys. ENeuro. 2019;6. [DOI] [PMC free article] [PubMed]
- 273.Roseboom PH, Mueller SAL, Oler JA, Fox AS, Riedel MK, Elam VR, et al. Evidence in primates supporting the use of chemogenetics for the treatment of human refractory neuropsychiatric disorders. Molecular Therapy. 2021;In Press. [DOI] [PMC free article] [PubMed]
- 274.Whitfield-Gabrieli S, Ghosh SS, Nieto-Castanon A, Saygin Z, Doehrmann O, Chai XJ, et al. Brain connectomics predict response to treatment in social anxiety disorder. Mol Psychiatry. 2016;21:680–5. doi: 10.1038/mp.2015.109. [DOI] [PubMed] [Google Scholar]
- 275.Gillan CM, Whelan R. What big data can do for treatment in psychiatry. Curr Opin Behav Sci. 2017;18:34–42. [Google Scholar]
- 276.Etkin A, Maron-Katz A, Wu W, Fonzo GA, Huemer J, Vértes PE, et al. Using fMRI connectivity to define a treatment-resistant form of post-traumatic stress disorder. Sci Transl Med. 2019;11:eaal3236. [DOI] [PMC free article] [PubMed]
- 277.Ungerleider LG, Gaffan D, Pelak VS. Projections from inferior temporal cortex to prefrontal cortex via the uncinate fascicle in rhesus monkeys. Exp Brain Res. 1989;76:473–84. doi: 10.1007/BF00248903. [DOI] [PubMed] [Google Scholar]
- 278.Ebeling U, von Cramon D. Topography of the uncinate fascicle and adjacent temporal fiber tracts. Acta Neurochir (Wien) 1992;115:143–8. doi: 10.1007/BF01406373. [DOI] [PubMed] [Google Scholar]
- 279.Tromp DPM, Grupe DW, Oathes DJ, McFarlin DR, Hernandez PJ, Kral TRA, et al. Reduced structural connectivity of a major frontolimbic pathway in generalized anxiety disorder. Arch Gen Psychiatry. 2012;69:925–34. doi: 10.1001/archgenpsychiatry.2011.2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Tromp DPM, Williams LE, Fox AS, Oler JA, Roseboom PH, Rogers GM, et al. Altered Uncinate Fasciculus Microstructure in Childhood Anxiety Disorders in Boys But Not Girls. Am J Psychiatry. 2019;176:208–16. [DOI] [PMC free article] [PubMed]
- 281.Fields RD. A new mechanism of nervous system plasticity: activity-dependent myelination. Nat Rev Neurosci. 2015;16:756–67. doi: 10.1038/nrn4023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Petrides M, Tomaiuolo F, Yeterian EH, Pandya DN. The prefrontal cortex: comparative architectonic organization in the human and the macaque monkey brains. Cortex. 2012;48:46–57. doi: 10.1016/j.cortex.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 283.Timbie C, Barbas H. Pathways for emotions: specializations in the amygdalar, mediodorsal thalamic, and posterior orbitofrontal network. J Neurosci. 2015;35:11976–87. doi: 10.1523/JNEUROSCI.2157-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fifth Edition. American Psychiatric Association; 2013.
- 285.Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017;19:93–107. doi: 10.31887/DCNS.2017.19.2/bbandelow. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Brown TA, Barlow DH. Comorbidity among anxiety disorders: implications for treatment and DSM-IV. J Consulting Clin Psychol. 1992;60:835–44. doi: 10.1037//0022-006x.60.6.835. [DOI] [PubMed] [Google Scholar]
- 287.Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. Child Adolesc Psychiatr Clin N. Am. 2005;14:631–48. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 288.Lamers F, van Oppen P, Comijs HC, Smit JH, Spinhoven P, van Balkom AJLM, et al. Comorbidity patterns of anxiety and depressive disorders in a large cohort study: the Netherlands Study of Depression and Anxiety (NESDA) J Clin Psychiatry. 2011;72:341–8. doi: 10.4088/JCP.10m06176blu. [DOI] [PubMed] [Google Scholar]
- 289.Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 290.Farabaugh A, Alpert J, Wisniewski SR, Otto MW, Fava M, Baer L, et al. Cognitive therapy for anxious depression in STAR(*) D: what have we learned? J Affect Disord. 2012;142:213–8. doi: 10.1016/j.jad.2012.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. 2007;164:1476–88. doi: 10.1176/appi.ajp.2007.07030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Button KS, Ioannidis JPA, Mokrysz C, Nosek BA, Flint J, Robinson ESJ, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14:365–76. doi: 10.1038/nrn3475. [DOI] [PubMed] [Google Scholar]
- 293.Wilhelm FH, Grossman P. Emotions beyond the laboratory: theoretical fundaments, study design, and analytic strategies for advanced ambulatory assessment. Biol Psychol. 2010;84:552–69. doi: 10.1016/j.biopsycho.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 294.Dixon ML, Moodie CA, Goldin PR, Farb N, Heimberg RG, Gross JJ. Emotion Regulation in Social Anxiety Disorder: Reappraisal and Acceptance of Negative Self-beliefs. Biol Psychiatry Cogn Neurosci Neuroimaging. 2020;5:119–29. [DOI] [PubMed]
- 295.Watson D. Differentiating the mood and anxiety disorders: a quadripartite model. Annu Rev Clin Psychol. 2009;5:221–47. doi: 10.1146/annurev.clinpsy.032408.153510. [DOI] [PubMed] [Google Scholar]
- 296.Zinbarg RE, Barlow DH. Structure of anxiety and the anxiety disorders: a hierarchical model. J Abnorm Psychol. 1996;105:181–93. doi: 10.1037//0021-843x.105.2.181. [DOI] [PubMed] [Google Scholar]
- 297.Zald DH, Lahey BB. Implications of the hierarchical structure of psychopathology for psychiatric neuroimaging. Biol Psychiatry: Cogn Neurosci Neuroimaging. 2017;2:310–7. doi: 10.1016/j.bpsc.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research Domain Criteria (RDoC): toward a new classification framework for research on mental disorders. AJP. 2010;167:748–51. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 299.Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11:126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Hudziak JJ, Achenbach TM, Althoff RR, Pine DS. A dimensional approach to developmental psychopathology. Int J Methods Psychiatr Res. 2007;16:S16–23. doi: 10.1002/mpr.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.McLaughlin KA, Sheridan MA. Beyond cumulative risk: a dimensional approach to childhood adversity. Curr Dir Psychol Sci. 2016;25:239–45. doi: 10.1177/0963721416655883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, et al. The hierarchical taxonomy of psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017;126:454–77. doi: 10.1037/abn0000258. [DOI] [PubMed] [Google Scholar]
- 303.Kotov R, Krueger RF, Watson D, Cicero DC, Conway CC, DeYoung CG, et al. The hierarchical taxonomy of psychopathology (HiTOP): a quantitative nosology based on consensus of evidence. Annu Rev Clin Psychol. 2021;17:null. doi: 10.1146/annurev-clinpsy-081219-093304. [DOI] [PubMed] [Google Scholar]
- 304.Ruggero CJ, Kotov R, Hopwood CJ, First M, Clark LA, Skodol AE, et al. Integrating the hierarchical taxonomy of psychopathology (HiTOP) into clinical practice. J Consulting Clin Psychol. 2019;87:1069–84. doi: 10.1037/ccp0000452. [DOI] [PMC free article] [PubMed] [Google Scholar]