Abstract
Objectives
To understand and assess the degree of personalisation of tailored activities for people with dementia (PWD); and to estimate the magnitude of the effects of levels of personalisation on reducing behavioural and psychological symptoms of dementia (BPSD), improving quality of life (QoL) and level of engagement.
Design
Systematic review with meta-analysis.
Data sources
ProQuest, PubMed, Ovid, Cochrane Library, Web of Science and CINAHL were searched from the start of indexing to May 2020.
Eligibility criteria
We included randomised controlled trials and quasi-experimental studies assessing the effects of tailored activities for people aged 60 years or older with dementia or cognitive impairment on the outcomes of BPSD, QoL, depression and level of engagement with control groups.
Data extraction and synthesis
Two researchers screened studies, extracted data and assessed risks of bias. A rating scheme to assess the degree of personalisation of tailored activities was developed to classify tailored activities into high/medium/low groups. Effect sizes were expressed using standardised mean differences at 95% Confidence Interval (CI). Subgroup analyses were conducted to assess whether the degree of personalisation of tailored activities affected outcomes of interest.
Results
Thirty-five studies covering 2390 participants from 16 countries/regions were identified. Studies with a high-level of personalisation interventions (n=8) had a significant and moderate effect on reducing BPSD (standardised mean differences, SMD=−0.52, p<0.05), followed by medium (n=6; SMD=−0.38, p=0.071) and low-level personalisation interventions (n=6; SMD=−0.15, p=0.076). Tailored activities with a high-level of personalisation had a moderate effect size on improving QoL (n=5; SMD=0.52, p<0.05), followed by a medium level (n=3; SMD=0.41, p<0.05) of personalisation.
Conclusions
To develop high-level tailored activities to reduce BPSD and improve QoL among PWD, we recommend applying comprehensive assessments to identify and address two or more PWD characteristics in designed tailored activities and allow modification of interventions to respond to changing PWD needs/circumstances.
PROSPERO registration number
CRD42020168556.
Keywords: dementia, mental health, old age psychiatry
Strengths and limitations of this study.
The major contribution of this systematic review and meta-analyses is developing a rating scheme to assess the level of personalisation for interventions.
To assess whether the degree of personalisation of the tailored activities affects reduction of behavioural and psychological symptoms of dementia and improves quality of life among people with dementia or cognitive impairment.
Exclusion of papers not published in English may mean that important additional findings are missed.
Introduction
Dementia is particularly common among older adults, affecting 5%–8% of people aged 60 and over at any given time worldwide.1 Behavioural and psychological symptoms of dementia (BPSD) are common among people living with dementia (PWD), such as agitation, depression and resistance to care,2 which occur throughout the disease process, associated with decreased quality of life (QoL).3
Non-pharmacological interventions are recommended as first-line treatments over pharmacological approaches to treat BPSD and have less adverse effects.4 Tailored activities for PWD are promising non-pharmacological approaches that reduce BPSD and increase QoL. Two recently published National Institute for Health and Care Excellence (NICE) guidelines recommend that healthcare professionals offer activities to promote QoL that are tailored to personal preferences and consider using a structured tool to assess their likes, dislikes, routines and personal history.5 6
To our knowledge, six systematic reviews and meta-analyses (summarised in online supplemental table 1) have synthesised the effects of tailored activities on reducing BPSD and enhancing QoL among PWD, based on tailored strategies, activity types, personal characteristics, and frequency and duration of delivery.7–12 The first of these, incorporating studies published between 2000 and 2011, focused on the effectiveness of various tailored strategies to foster activity engagement and reduce BPSD in PWD.7 Changes to tools and materials used in activities were most common but yielded mixed outcomes of BSPD reduction; modifications to space and social demands were rarely tested but yielded consistently positive outcomes.7 In addition, a systematic review of studies published between 2000 and 2012 found that personalised pleasant activities yielded strong evidence for treating BPSD but limited evidence for physical and music activities.8Another meta-analysis found that individualised recreational activities were effective for reducing BPSD.9 Recently, Möhler and colleagues conducted three meta-analyses regarding the effects of tailored activities among PWD living in care facilities, communities and home settings, respectively, and found that, compared with usual care, tailored activities slightly reduced BPSD.10–12 However, no differences in other desired outcomes between intervention and control groups among different specific types of activity or duration of delivery were evident. Although different activity components (eg, activity types, PWD characteristics, frequency and duration of delivery) were discussed,7–12 no review further investigated the degree of personalisation among the tailored activities and synthesised its associations with the desired outcomes.
bmjopen-2021-048917supp001.pdf (795.6KB, pdf)
Understanding the degree of personalisation of tailored activities is important. We define the degree of personalisation of tailored activities as the extent to which non-pharmacological interventions are tailored, individualised or personalised for PWD. The conceptualisation of the degree of personalisation echoes the rationales and principles of effective interventions working on BPSD, level of engagement and QoL, embedded in occupational therapy,13 engagement in meaningful activities14 and person-centred care.15 Occupational therapy emphasises the fit between PWD capabilities and the occupation (eg, activities or roles) through task simplification and removing barriers in the physical and social environment.13 Environmental docility theory suggests that both underloading and overloading of external stimulations (e.g., cognitive activities and social interactions) may lead to PWD disengagement or excessive disability.16 Thus, maintaining PWD engagement in meaningful activities through tailored activities based on their physical strength, mental state and psychosocial needs is essential.14 The person-centred care approach stresses service providers’ and caregivers’ autonomy to determine specific ways of delivering care to maintain participants’ engagement during the intervention.15 These theories imply that the degree of personalisation can significantly influence the effectiveness of tailored activities for PWD. Thus, the degree of personalisation could depend on the assessment of PWD characteristics and their environment, the design of tailored activities based on PWD characteristics, and interventionists’ autonomy to address PWD spontaneous needs.
Conceptualising and quantifying the levels of personalisation of existing tailored activities can advance our knowledge on developing a high level of personalisation of tailored activities for PWD, deciding on the appropriate ‘dose’ of tailoring, and translating this cumulative evidence into clinical practice. However, existing literature provides little knowledge about assessing the degree of personalisation among tailored activities and their effectiveness on targeted outcomes.
Objectives
This systematic review and meta-analysis aimed to: (1) assess the degree of personalisation of existing tailored activities for PWD; (2) estimate the magnitude of the effects of existing tailored activities on reducing BPSD, improving QoL and the level of engagement among PWD and (3) assess whether the degree of personalisation of tailored activities affects the outcomes of interest.
Methods and analysis
We conducted the review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) procedure.17 Eligibility criteria required studies to: (1) include participants with dementia or cognitive impairment and aged 60 years or older; (2) include activities tailored to at least one of the participants’ characteristics (eg, needs, physical or/and mental ability, present or previous preferences for particular activities or interests, habits and physical living environments like housing conditions and caregiver management style); (3) report BPSD (measured by multi-domain scales, such as the Neuropsychiatric Inventory (NPI), and scales specific to agitation and depression/anxiety, such as the Cohen-Mansfield Agitation Inventory and the Cornell Scale for Depression in Dementia),18–20 QoL and level of engagement as outcomes; (4) include randomised controlled trials or quasi-experimental study design and (5) apply a control group (CG) (eg, usual care, wait-list, attention control, etc). The review included studies published in English from the start of indexing to May 2020.
We searched ProQuest (e.g., APA PsycInfo), PubMed, Ovid (e.g., Embase), Cochrane Library, Web of Science and CINAHL, using the search terms: (1) “cognitive impairment” OR “cognitive disorder” OR “dement*” OR “Alzheimer”; (2) “tailor*” OR “engag*” OR “individual*” OR “personal*”; and (3) “activit*” OR “program*” OR “therap*” OR “intervention*” OR “treatment*”. The full search strategy is shown in online supplemental table 2.
SL and AYZ independently completed the title/abstract review and full-text review. We conducted title/abstract screening using Rayyan (https://www.rayyan.ai/) and full-text review using Endnote. The two researchers discussed disagreements in the title/abstract screening and full-text review to reach consensus. Data were extracted and checked by SL and MSLM. Where there were disagreements, data were rechecked for relevance and accuracy. Where available, raw data (eg, clinical interventions, strategies, outcomes and results) were extracted and entered into a spreadsheet.21 For each intervention, we additionally extracted the following information: PWD (including older people with cognitive impairment) characteristics taken into account, intervention delivery, and information about the tailoring process (the data extraction form is shown in online supplemental appendix 1).
Patient and public involvement
No patient involved.
Developing the tailoring and classification scheme
The authors formed an expert panel to develop a scheme for the level of personalisation interventions based on the included studies, comprising AYZ (a licensed social worker in Hong Kong with 2 years clinical experience of dementia care and 5 years research experience focusing on the mechanisms of non-pharmacological interventions for PWD), TLiu, JCPC and SL (each of whom had over 10-year experience in psychology and elderly care).
Based on the theories and approaches mentioned above, we hypothesised that tailoring is embedded in the whole process at three inter-related phases: assessment, design and implementation, and the degree of personalisation is determined by these three dimensions: (1) how to assess PWD characteristics before designing the intervention; (2) the extent to which interventions are tailored according to PWD characteristics and (3) the level of the interventionists’ autonomy to address PWD needs, as suggested by occupational therapy, engagement in meaningful activities, and the person-centred care approach (online supplemental figure 1).13–15 To this end, we developed three corresponding criteria to rate levels of personalisation (online supplemental table 3).
First, the level of assessment for tailoring refers to how comprehensive the PWD characteristics were considered and how systematically the assessment results were used for designing tailored activities. Operationally, we rated the level of assessment as ‘unclear/incomprehensive’, ‘semi-structured’ or ‘structured’. ‘Unclear/incomprehensive’ indicated that preassessment was missing/not clearly described, only a single domain of PWD characteristics was assessed, or no description of how the assessment results were used to inform the tailored activities design. ‘Semi-structured’ referred to preassessments conducted by unstructured/semi-structured interviews, with some descriptions on how the assessment results were used for activities design, ‘structured’ preassessments employed structured interviews with clear and detailed descriptions on how the assessment results were systematically used for the activities design.
Second, individualisation in intervention design refers to how the intervention design accounted for individuals’ uniqueness and variations of their needs. To avoid counting the number or arbitrarily weighting specific PWD characteristics, we distinguished the degree of individualisation based on whether the protocol tailored for one versus two or more PWD characteristics.
Third, the degree of person-centred care in implementation refers to how the interventionists were able to adjust the intervention based on their clinical knowledge and observation of participants’ performance in the intervention to maintain participants’ engagement and respond to participants’ spontaneous needs during the implementation. Intervention with a standardised protocol of tailored activities regardless of spontaneous needs of PWD were rated as low flexibility for pursuing person-centred care, and interventions encouraging and allowing great flexibility for interventionists to adjust the tailored activities based on clinical knowledge and observation of participants’ performance were rated as high flexibility.
Based on the dimensions mentioned above, we rated the level of personalisation of tailored activities as high, medium or low. A study was rated as high level only if it met all the following criteria: (1) structured assessments were used for systematically tailored activities plan; (2) interventions targeted two or more domains (eg, capabilities, preferences, interests, life experience and external environment) and (3) allowed the interventionists to exercise flexibility to adjust the intervention in accordance with PWD spontaneous needs. A study was rated as medium if: (1) unstructured/semi-structured assessments on participants’ characteristics were performed; (2) interventions targeted two or more domains and (3) some flexibility and modifications were allowed for adjusting the intervention in response to PWD needs. A study was rated as low if: (1) assessment was unclear/incomprehensive, or there was no clear description on how assessment results informed tailoring; (2) interventions targeted only one domain of participants’ characteristics and (3) low/marginal flexibility to pursue person-centred care for interventionists was allowed. AYZ and SL independently rated the level of personalisation for the included tailored activities. The inter-rater reliability was 88.8% in the initial stage of rating. Conflicting ratings were resolved through discussion.
Data synthesis and analysis
Given that outcomes in our review were continuous, effect sizes were expressed using standardised mean differences (SMD) at 95% CI,20 interpreted as Cohen’s d.22 Specifically, the values of 0.2, 0.5 and 0.8 reflected small, moderate and large effect sizes, respectively.22 Due to differences in settings and methods, we used the random-effects model to pool the results. Heterogeneity was determined by χ² and I² statistics.23 24 We classified subgroup analyses of the effectiveness of tailored activities according to the levels of personalisation of the interventions. All meta-analyses were conducted using Comprehensive Meta-Analysis Software. Where raw data are not provided, summary results are given in the text but not the forest plots. The meta-analyses included results from randomised controlled studies (RCTs) only because the findings from quasi-experimental studies were not comparable to those from RCTs. Sensitivity analyses were conducted to check the robustness of the findings.
Quality appraisal
SL and MSLM independently assessed the risk of bias for the studies using a revised Cochrane risk of bias tool for randomised trials,23 25 including: (1) bias arising from the randomisation process; (2) deviations from intended interventions; (3) bias due to missing outcome data; (4) bias in measurement of the outcome and (5) bias in selection of the reported results. Risk of Bias in Non-randomised Studies of Interventions was used to categorise the risk of bias as ‘low,’ ‘high’ or ‘some concerns’ for non-RCT studies.22 Conflicting results were resolved through discussions.
Results
Summary of search results
The search and study selection process is summarised in the PRISMA flow diagram (online supplemental figure 2). In the identification phase, 14 238 abstracts were identified and imported into Endnote; 7471 duplicate articles were removed. In the screening phase, the titles and abstracts of 6767 articles were screened, and 6476 irrelevant articles were excluded. In the eligibility phase, full-text screening was conducted for 291 articles according to the inclusion and exclusion criteria, and 35 studies were finally included in this review.
Included studies were conducted in 16 countries/regions: Australia, Brazil, Mainland China, Denmark, France, Germany, Hong Kong, Italy, Japan, Korea, the Netherlands, Norway, Switzerland, Taiwan, the UK and the USA, published between 2000 and 2020. The average age of participants ranged from 62.1 to 89.2 years. Twenty-nine studies included participants with dementia only, and the remaining studies included participants with mild to moderate levels of cognitive impairment. The total size of the intervention groups (IGs) was 1248 (range=6–158), and the total size of the CGs was 1142 (range=5–107). Fourteen studies (40%) had no more than 20 participants for each arm. Thirty studies were RCTs. Five applied a quasi-experimental study design. Twenty-two applied usual care as the comparison, and the remaining applied placebo control, active control or wait-list control. Twenty-four studies were conducted in care facilities (such as a nursing home, geriatric health service facility or hospital), and the remaining studies were conducted in community settings or home-based settings (online supplemental table 4).
Description of the interventions
The components of activities can be categorised into four groups: physical (n=3),26–28 cognitive (n=2),29 30 music (n=7)31–37 and multiple activities (n=23).16 38–59 Twenty-three studies reported their interventions as individual mode, five reported group-based mode and six reported mixed modes, while the remaining studies did not provide details. Intervention was provided by specialists (eg, occupational therapists, clinicians, psychologists, physical therapists and speech therapists), researchers and trained nursing home caregivers and staff. A detailed description of interventions is shown in online supplemental table 5.
Level of personalisation
Based on the three-dimension rating scheme for the personalisation of tailored activities, we identified 12 studies as high level,16 26 35 39 40 46 49 51 53–56 11 as medium34 36 38 42 44 45 47 52 57–59 and 11 as low.27–33 37 43 48 50 One was rated as mixed because it had three-arm IGs with one medium and two low levels of tailoring activities for comparison.41 Table 1 shows the level of personalisation among the interventions reported in the reviewed studies.
Table 1.
Level of personalisation of tailored activities
| No. | Author | Level of assessment for tailoring | Degree of individualisation in design | Degree of person-centred care in intervention delivery | Level of personalisation |
| 1 | Orsulic-Jeras et al38 | Structured assessments of participants’ preferences using the Montessori-Based Assessment System developed by the authors for selecting appropriate activities for participants | Preserved abilities and preference (Two and above) | No description | Medium |
| 2 | Cohen-Mansfield et al39 | Structured assessments for tailoring relating to participants’ medical history, self-identity and social functioning | Identity roles, the severity of dementia and ability (Two and above) | High flexibility. The choice of intervention was affected by availability of materials, family members’ cooperation and the practicability of the intervention | High |
| 3 | Garland et al31 | No preassessments for tailoring | Music preference (One) | No description | Low |
| 4 | Cohen-Mansfield et al40 | Structured assessments for tailoring regarding participants’ medical history, self-identity and social functioning | Ability, history and preference (Two and above) | High flexibility. The study clearly indicated that flexibility was essential element of intervention | High |
| 5 | Gitlin et al16 | Semi-structured interviews to discern daily routines, and the Pleasant Event Schedule to identify previous/current activity interests. Interventionists observed dyadic communication and home environmental features and assessed dementia patients | Capabilities, previous roles, habits, interests, home environment and dyadic communication (Two and above) | High flexibility. Activity prescriptions were reviewed and modified if necessary, during the implementation | High |
| 6 | Lam et al26 | Structured assessments for tailoring. Individual functional profiles were mapped with personal selection | Abilities, preference and needs (Two and above) | High flexibility. Training content was dynamic and adjusted to the changing needs of PWD | High |
| 7 | Dechamps et al58 | Semi-structured assessments on physical/psychological functions | Abilities (One) | Some flexibility | Medium |
| 8 | Gitlin et al51 | Structured assessments of PWD capabilities, medical testing, home environment, caregiver communication and caregiver-identified concerns. Interventionists interviewed caregivers to identify patient’s routines, previous/current roles, habits and interest | Home environment, caregiver-identified concerns and capabilities, routines, previous/current roles, habits and interests (Two and above) | High flexibility | High |
| 9 | Sung et al32 | Semi-structured assessments of participants’ preferences and information on the importance of music to life | Music preference (One) | Low | Low |
| 10 | Kolanowski et al41 | Structured assessments of capacities and personality of interest | Capacity and preference (Two and above) | High flexibility. Great flexibility was allowed to use staff’s own clinical judgement and knowledge to implement individualised activities | Medium |
| a | Capacity (One) | No description | Low | ||
| b | Preference (One) | No description | Low | ||
| 11 | Lin et al33 | Semi-structured preassessment of participants’ music preference | Music preference (One) | No description | Low |
| 12 | Cohen-Mansfield et al59 | Structured assessments of participants’ medical history, self-identity and social functioning | Past identity, ability and preferences (Two and above) | Some flexibility. Interventionists were allowed to seek approval for possible adjustment if needed | Medium |
| 13 | van der Ploeg et al42 | Structured assessments (Myers Menorah Park/Montessori-Based Assessment System) for tailoring | Preserved abilities and interest (Two and above) | High flexibility. Flexibility to respond to patients’ perceived level of interest was allowed | Medium |
| 14 | Ridder et al34 | Semi-structured interviews to elicit life-story information either from journal or relatives | Life-story/history, psychosocial needs (Two and above) | Low/some flexibility. No specific description | Medium |
| 15 | Sakamoto et al35 | Structural assessments for tailoring to analyse participants’ personal life history, and interview with each participant and family member | Music preference, special memories (Two and above) | High flexibility | High |
| 16 | Van Haitsma et al57 | Incomprehensive preassessments | Interest and ability (Two and above) | Some flexibility. The intervention was adjusted according to the time when residents need stimulation | Medium |
| 17 | Yoon et al43 | Incomprehensive preassessments | Ability (One) | Low flexibility | Low |
| 18 | Toba et al44 | Preassessment of individuals’ abilities and disabilities to evaluate how to enhance abilities and compensate for disabilities | Abilities (One) | No description | Medium |
| 19 | Holthoff et al27 | Incomprehensive preassessments | Ability (One) | Low flexibility | Low |
| 20 | Telenius et al28 | Incomprehensive preassessments | Ability (One) | No description | Low |
| 21 | Davison et al29 | Preassessment. The researchers met with participants and their families to determine the preferred materials | Interest only (One) | Low flexibility | Low |
| 22 | Giuli et al30 | Incomprehensive preassessments on patients’ cognitive status | Cognition (One) | No description | Low |
| 23 | Lu et al45 | Preassessments on PWD functional ability, types and frequencies of meaningful activity, perceived barriers to engaging in activities | Functional ability, types and frequencies of meaningful activity (Two and above) | No description | Medium |
| 24 | Prick et al46 | Structured assessments for tailoring | Physical capacities, information about pleasant activities for the dyad (Two and above) | Medium to high | High |
| 25 | Bailey et al52 | No preassessments for tailoring | Interest and history (Two and above) | High flexibility. The group leaders had the flexibility to develop and tailor the individualised behavioural activity programmes during implementation | Medium |
| 26 | Li et al47 | The preliminary survey was implemented to investigate participants’ preferences, cultural background, cognitive function and abilities | Interest and capacities (Two and above) | Some flexibility. The interventionist was allowed to choose activities to match PWD ability and interest during personalised activity | Medium |
| 27 | Gitlin et al53 | Structured assessments of participants’ capacities, fall risk, daily routines, interests, caregivers (routines, employment, readiness) and environments (lighting, seating, clutter, noise) | Capabilities, functioning, interest, environment, caregivers (Two and above) | High flexibility (prescriptions were reviewed and modified if necessary during implementation) | High |
| 28 | Tanaka et al48 | Incomprehensive preassessments | Personal history (One) | No description | Low |
| 29 | Novelli et al54 | Structured assessments to identify preserved capacities, previous interests, frequency/intensity of BPSD in the PWD, daily care routines of caregivers and home environment features | Capabilities, previous interests, frequency and intensity of BPSD in PWD, daily care routines of the caregiver and home environment (Two and above) | High flexibility. Interventionists are allowed to tailor and adjust the chosen activities to match participants’ capabilities during implementation | High |
| 30 | Kwak et al36 | Unstructured interviews with participants and their family members as the best sources for identifying an individual’s music preferences | Music preference and songs significant to PWD life experience (Two and above) | High flexibility. The intervention allowed flexibility for facility staff to use their own clinical judgement and knowledge to tailor and implement the intervention | Medium |
| 31 | Jeon et al49 | Comprehensive individual assessment (physical, medical and psychosocial) and their environment, medication review and adherence, a review of communication with health service providers and cognitive needs and existing strategies. | Capacities/needs, environment (Two and above) | High flexibility. A multidisciplinary and interdisciplinary plan tailored to meet the client’s needs to enhance self-care ability using person-centred goal setting | High |
| 32 | de Oliveira et al 55 | Structured assessments. Semi structured investigator-developed interview to identify daily routines, and the Pleasant Event Schedule to identify previous and current activity interests | Cognitive and functional capacities, previous abilities, interests and roles (Two and above) | High flexibility (prescriptions were reviewed and modified if necessary during the implementation) | High |
| 33 | O’Connor et al56 | Structured assessments of participants’ capacities, fall risk, daily routines, interests, caregivers (routines, employment, readiness) and environments (lighting, seating, clutter, noise) | Capabilities, functioning, interest, environment, caregivers (Two and above) | High flexibility (prescriptions were reviewed and modified if necessary during implementation) | High |
| 34 | Weise et al37 | Preassessment of participants’ personal music preference from family members, nursing staff and directly from participants | Preference for music (One) | Low flexibility | Low |
| 35 | Huber et al50 | Incomprehensive preassessments | Preference (One) | Low flexibility | Low |
One=the intervention design was tailored for only one aspect of PWD characteristics; Two and above=the intervention design was tailored for two and above aspects of PWD characteristics.
PWD, people with dementia.
Level of assessment for tailoring
Sixteen studies assessed the full picture of PWD characteristics using structural assessments.16 26 35 38–42 46 49 51 53–56 59 For instance, five studies followed the protocol of the Tailored Activity Programme (TAP) incorporating the Progressive Lowered Stress Threshold Model.60 This posits that with disease progression, dementia patients become increasingly vulnerable to their environment and experience lower thresholds for tolerating stimuli that can result in behavioural disturbances. TAP applied systematic approaches to discern PWD and their caregivers’ daily routines, identify previous and current activity interests and collect information about dyadic communication and home environmental features to design activities for participants.
Degree of individualisation in design
Activities tailored according to PWD characteristics included cognitive or/and physical capacities (n=22),26–28 30 38 39 41–47 49 51 53–59 personal experience and history (n=2),34 48 role identity (n=3),39 51 55 preferences and interests (n=20)26 29 31–33 35–37 40–42 46 47 50 53–57 59 habits (n=2),51 54 cultural backgrounds (n=1)47 and living environment (n=5).49 51 53 54 56 Five studies also considered caregivers’ characteristics.46 51 53 54 56 Twelve studies tailored the intervention for a single aspect of PWD characteristics only, while the remainder tailored the activities for at least two. One study used a four-arm study design (three IGs plus one CG), with one tailoring both for PWD capacity and interests, the second only tailoring for the capacities yet opposite to PWD preference, and the third only tailoring for the interests yet challenging to PWD’ capacity in the three IGs.41
Degree of person-centred care in delivery
Twenty-six studies indicated the level of flexibility for modification of activities during the intervention. Sixteen studies explicitly permitted the interventionists to review and modify the intervention according to participants’ spontaneous needs and circumstances,16 26 35 36 39–42 46 49 51–56 thus were rated as offering a high degree of person-centred care. Five allowed some flexibility for adjusting interventions during implementation,34 47 57–59 thus were rated as offering some flexibility. Five studies enabled relatively limited adjustment of intervention to take account of changed PWD needs or circumstances.27 32 34 37 50 The remaining studies provided insufficient information to judge the extent of flexibility allowed during the intervention.
Quality appraisal
The risk bias of 10 RCT studies was judged as low, while that of 12 was rated as high, and the remainder was judged as giving some concern (online supplemental figure 3). Nineteen RCT studies reported the method of random sequence generation (eg, computer-generated programmes, random list generator, random allocation by an external researcher and block randomisation).16 28–30 33 34 37 41–43 46 49 51 53–56 58 59 Eleven were rated as high risk of deviation from intended intervention as they were judged as high risk of blinding participants, personnel and appropriate analysis used to estimate the effect of assignment to intervention.27–30 33 36 40 42 43 48 52 Five quasi-experimental studies were excluded from the meta-analysis since none were rated at low risk of bias and thus comparable to RCTs (online supplemental figure 4).
Meta-analysis: the effects of tailored interventions
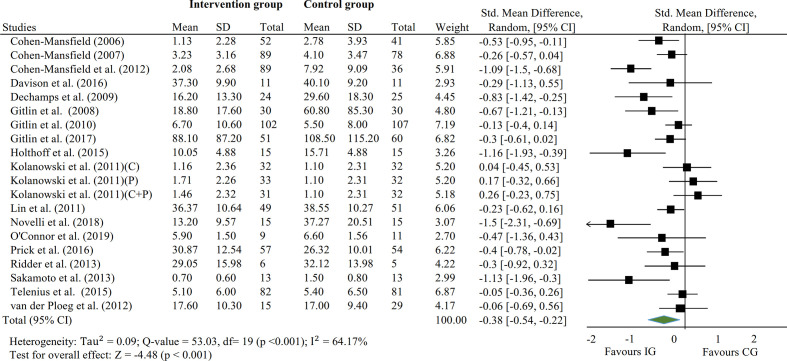
Twenty-six studies reported the outcomes of BPSD measured by multi-dimension or specific scales of agitation (figure 1).16 27–29 31 33–37 39–42 44 46 47 50 51 53–59 The measurements used for BPSD included the NPI, the Agitation Behavior Mapping Instrument, the Cohen-Mansfield Agitation Inventory, the Agitated Behaviors in Dementia Scale, the Behavioral Pathology in Alzheimer’s Disease rating scale and the short version of the Dementia Behavior Disturbance Scale.18 20 61–64 A higher score indicates more BPSD. According to our meta-analysis, 18 RCTs with 20 tailored activities had an overall small effect on BPSD at postintervention (SMDpooled=−0.38; 95% CI −0.54 to −0.22, p<0.001), although significant heterogeneity was found (I2=64.17%, p<0.001). Eight studies were excluded from the meta-analysis either because of their quasi-experimental design or for not reporting the raw data.31 36 37 44 47 50 55 57 Four of these identified no differences in reducing BPSD between IG and CG.31 36 37 50
Figure 1.
Effects of tailored interventions on challenging behaviour at postintervention (N=20). C=activities tailored for capacities of participants only, P=activities tailored for preference of participants only, C+P=activities tailored for capacities and preference of participants. Fixed effect: SMDpooled=−0.32, 95% CI −0.42 to −0.22, p<0.001. CG, control group; IG, intervention group.
Nine studies reported the outcome of QoL (figure 2).16 34 48 49 51 52 54 56 58 The measurements used for QoL included Quality of Life-Alzheimer’s Disease, the 3-Level version of the EuroQol five dimensions, the EuroQol 5-D, and the Health-related Quality of Life Questionnaire for the Elderly with Dementia.65–67 A higher score indicates higher QoL. Tailored interventions had an overall small effect on QoL at postintervention (SMDpooled=0.45; 95% CI 0.25 to 0.64, p<0.001), and no significant heterogeneity was found (I2=11.56%, p>0.05).
Figure 2.
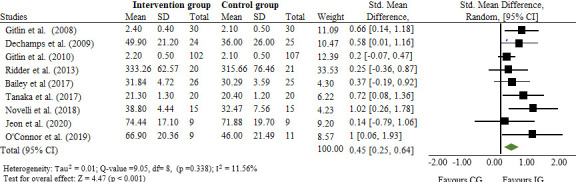
Effects of tailored interventions on quality of life at postintervention (N=9). Fixed effect: SMDpooled=0.42, 95% CI 0.24 to 0.59, p<0.001. CG, control group; IG, intervention group.
Sixteen studies reported the outcome of depression,16 26 28–30 32 39 43–46 48–50 52 58 measured by the Cornell Scale for Depression in Dementia, the Geriatric Depression Scale, the Multidimensional Observation Scale for Elderly Subjects, the Geriatric Depression Scale, the NPI subscale for depression or Patient Health Questionnaire-9.18 19 68–70 A higher score indicates more depression. Thirteen RCT studies with 14 tailored activities indicated those activities had a small overall effect on depression at postintervention (SMDpooled=−0.29; 95% CI −0.45 to −0.13, p<0.001), and no significant heterogeneity was found (online supplemental figure 5). The remaining three studies were excluded from the meta-analysis because of their quasi-experimental design or lack of comparable data,32 44 50 and only one study found no difference in reducing depression between IG and CG.44
Seven studies with nine interventions reported the outcome of engagement.16 38 39 41 42 51 52 The measurements of engagement included one item on the ABMI, the Menorah Park Engagement Scale, direct observation or caregiver report.61 71 A higher score indicates a higher level of engagement. The meta-analysis indicated that tailored interventions of eight matched IGs and CGs in six studies had an overall large effect on the level of engagement at postintervention (SMDpooled=0.86; 95% CI 0.23 to 1.48, p<0.001) (online supplemental figure 6). Significant heterogeneity was found, primarily generated by the outlier study whose intervention specifically targeted participants’ self-identity roles and which reported large effects on engagement (SMD=3.52; 95% CI 2.87 to 4.17, p<0.001).39 Removal of this study resulted in lower and non-significant heterogeneity with a significant small effect size (SMDadjusted pooled=0.47; 95% CI 0.23 to 0.60, p<0.001). One study with a quasi-experimental design reported increased engagement postintervention.38
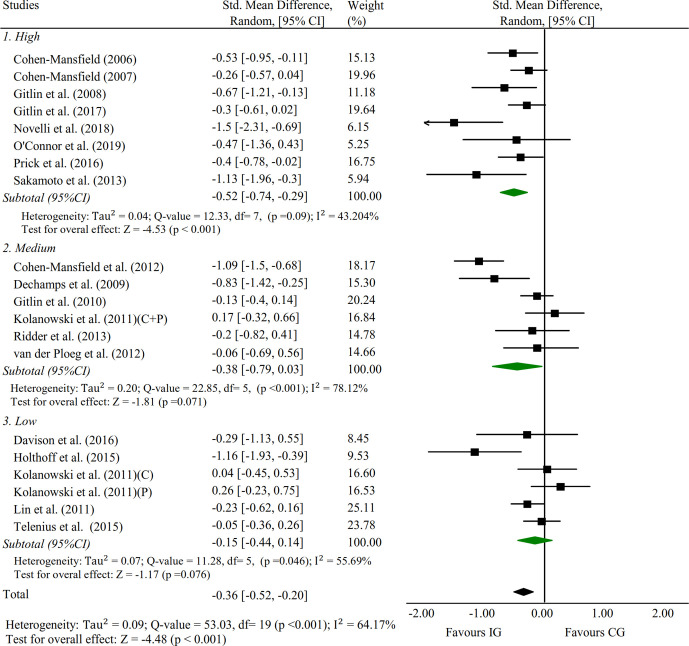
Subgroup analysis
Subgroup analysis was performed to test the difference of the effects of tailored activities with different levels of personalisation on outcomes (figures 3 and 4). Studies with a high level of personalisation tailored activities had a significant and the largest effect size regarding the reduction of BPSD (SMDpooled=−0.52, 95% CI −0.74 to −0.29, p<0.001) with non-significant heterogeneity, followed by medium (SMDpooled=−0.38, 95% CI −0.79 to 0.03, p=0.071) and low groups (SMDpooled=−0.15, 95% CI −0.44 to 0.14, p=0.076), although both the latter two groups had marginally significant effect sizes and significant heterogeneity. The high group had a moderate effect size on improvement in QoL (SMDpooled=0.52, 95% CI 0.16 to 0.89, p<0.01), followed by the medium group (SMDpooled=0.41, 95% CI 0.07 to 0.74, p<0.05). Only one study with a low level of personalisation tailored activities reported the outcome of QoL with moderate effect size (SMD=0.72, 95% CI 0.08 to 1.36, p<0.05).
Figure 3.
Subgroup analysis: effects of tailored interventions on challenging behaviour at postintervention by level of personalisation (N=20). C=activities tailored for capacities of participants only, P=activities tailored for preference of participants only, C+P=activities tailored for capacities and preference of participants. (1) High group. Fixed effect: SMDpooled=−0.46, 95% CI −0.62 to −0.30, p<0.001; middle group. Fixed effect: SMDpooled=−0.34, 95% CI −0.51 to −0.16, p<0.001; low group. Fixed effect: SMDpooled=−0.11, 95% CI −0.30 to 0.08, p=0.254. (2) Test for the difference across three subgroups: Q value=7.78, df(Q)=2, p value=0.02. CG, control group; IG, intervention group.
Figure 4.
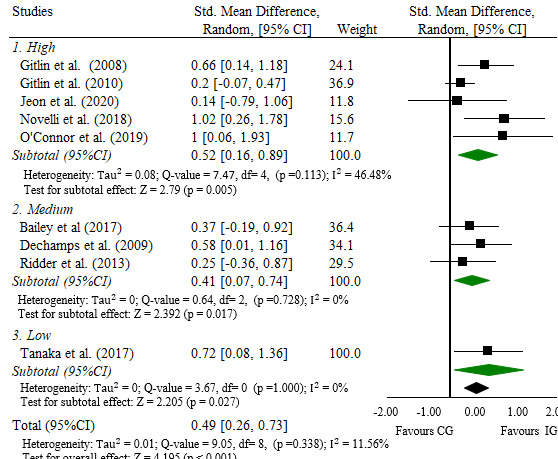
Subgroup analysis: effects of tailored interventions on quality of life at postintervention by level of personalisation (N=9). High group, fixed effect: SMDpooled=0.39, 95% CI 0.17 to 0.60, p<0.001; middle group, fixed effect: SMDpooled=0.41, 95% CI 0.07 to 0.74, p=0.017; low group, fixed effect: SMDpooled=0.72, 95% CI 0.08 to 1.36, p=0.027. (2) Test for the difference across three subgroups: Q value=0.94, df(Q)=2, p value=0.626. CG, control group; IG, intervention group.
Subgroup analysis was performed to test the difference of the effects of the level of personalisation on depression and engagement (online supplemental figures 7 and 8). The medium group had a moderate effect size regarding reduction in depression (SMDpooled=−0.64, 95% CI −1.14 to −0.15, p<0.05), followed by the high group (SMDpooled=−0.33, 95% CI −0.54 to −0.12, p<0.01). The three studies with a medium level of personalisation of tailored activities all involved social or group interaction components that have beneficial effects on PWD mental health. Only one study rated high on tailoring had a large effect on improving engagement level postintervention (SMD=0.85, 95% CI 0.32 to 1.38, p<0.01). The medium group had a small effect size (SMDpooled=0.44, 95% CI 0.07 to 0.80, p<0.05), followed by the low group (SMDpooled=0.39, 95% CI 0.04 to 0.74, p<0.05).
Sensitivity analysis
We conducted a series of sensitivity analyses that excluded studies that combined participants with dementia and those with cognitive impairment. No substantial differences were found between the findings of studies focussing exclusively on PWD and studies that included participants with dementia and participants with cognitive impairment (online supplemental table 6). Sensitivity analyses were also conducted to examine whether the effect sizes of tailored activities on the outcomes of interest were associated with each study’s sample size. The only significant association was found between sample size and effect size on QoL. We also tested whether a study’s intervention mode (individual, group and mixed with mixed mode set as the reference group) would be associated with its findings. No significant associations were found between intervention mode and the outcomes.
Discussion
Our systematic review aimed to assess the degree of personalisation of tailored activities and estimate the effect of levels of personalisation of tailored activities on reducing BPSD, improving QoL and other relevant outcomes among PWD. Thirty-five studies met our inclusion criteria, covering a total of 2390 participants from 16 countries/regions. The activities included in the interventions comprised physical, cognitive, music and multiple activities.
We employed meta-analysis to estimate the overall effects of tailored activities on the outcomes of BPSD, QoL, depression and engagement. Our findings on the effect sizes of tailored activities of the outcomes of interests differ from previous review studies. First, we found that tailored activities slightly reduced BPSD, consistent with previous meta-analyses targeting facilities, communities and PWD living in their own home.10–12 Second, we found that tailored activities had a small effect on improving QoL, compared with previous reviews that found inconclusive evidence regarding QoL: no effect in facilities, and a slight improvement in both community-based and home-based settings.10–12 Third, our findings showed that tailored activities had small effects on depression, and large effects on engagement, contradicting previous reviews reporting little or no effect on these outcomes.11 12
Unlike previous review studies, we further developed the rating scheme of tailoring level based on three essential components: assessment for tailoring, individualisation in intervention design and person-centred care in implementation. Based on our rating scheme, the activities with optimal tailoring conditions possess the following characteristics. In the assessment stage, systematic interviews on individuals’ characteristics were conducted. In the design stage, two or more domains of individuals’ characteristics were targeted in the activity plan, including capabilities, preferences, interests, life experience and external environment. In the implementation stage, interventionists were allowed high flexibility and any modifications based on their professional judgement to accommodate the spontaneous needs of PWD during the intervention. Overall, we rated only 12 studies as high level of personalisation of tailored activities, 11 as medium, 11 as low and 1 study was rated as mixed because it had three-arm IGs with one medium and two low levels of tailoring activities for comparison.
Based on our rating scheme, we extended previous review studies to investigate how the degree of tailoring influenced intervention effectiveness on the outcomes of interest. Interventions with a high level of personalisation of tailored activities had a significant and moderate effect, followed by medium (small) and low groups (trivial); the latter two groups had significant heterogeneity and marginally significant effect sizes. Interventions rated as having a high level of personalisation had a moderate effect size on improving QoL, followed by the medium group. Only one study with a low level of personalisation of tailored activities reported the outcome of QoL with moderate effect size. These findings support our rating scheme as the overall goals of tailoring activities are to reduce BPSD and improve QoL.54 56 A similar pattern was found in the level of engagement. However, because the degree of personalisation was rated high in one study only, this should be interpreted with caution.
This systematic review has several limitations. The generalisability of our results may be limited since we included English-language studies only. The included studies had risks of bias that may undermine the quality of evidence. Furthermore, noticeable heterogeneity was found among studies with outcomes of BPSD and engagement, which may affect the conclusions synthesised from these studies. Thus, these results must be interpreted with caution. In addition, the rating scheme for the level of personalisation was subjective regarding the level of assessments for tailoring and the degree of person-centred care in implementation.
This review has implications for clinical practice. It provides new insights into non-pharmacological tailored activities by developing a rating scheme for the level of personalisation and tested its validity by investigating the effectiveness of interventions with different levels of tailoring on BPSD and QoL. Healthcare professionals and practitioners can use our findings to tailor interventions to benefit patients’ outcomes. We recommend the application of structural and comprehensive assessment approaches to identify and address two or more PWD characteristics (capacities, preferences, habits and living environment, etc) in designing tailored activities, and allow interventionists to use their professional judgement to modify the interventions to respond to spontaneous needs of PWD to develop tailored activities with a high level of personalisation.
Our systematic review has implications for future intervention research. Fourteen studies had no more than 20 participants for each arm, and only 10 RCTs were judged as low risk. Evaluation studies should adhere to current methodological standards, for example, a randomised and concealed allocation, adequate blinding (at least participants and outcome assessors), and recruitment of adequate samples.23
Conclusion
This systematic review shows that tailored activities slightly reduced BPSD and depression, had a small effect on improving QoL and had large effects on facilitating the level of engagement among PWD. Additionally, we advanced existing literature by proposing and testing the validity of a rating scheme for the level of personalisation. Additional high-quality tailored intervention studies with sufficient samples are needed.
Supplementary Material
Footnotes
Twitter: @TerryLum
Contributors: SL was responsible for the overall content of the systematic review. SL wrote the systematic review, performed the preliminary searches and data extraction, conducted quality assessments and drafted the systematic review paper. SL, AYZ, T Liu and JCPC designed the rating scheme for the level of personalisation. MSLM cross-checked data extraction and performed quality ratings independently. GW and T Lum made substantial contributions to the conception and design of the systematic review and assisted SL, AYZ, T Liu and JCPC to resolve any discrepancies regarding study inclusion, data extraction and quality ratings. All authors offered critical revisions for the systematic review manuscript.
Funding: This work was supported by a donation from Tin Hing-Sin Sam to promote non-pharmacological interventions for people with dementia and their caregivers in the community.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1.World Health Organization . Dementia, 2019. Available: https://www.who.int/news-room/fact-sheets/detail/dementia
- 2.Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ 2015;350:h369. 10.1136/bmj.h369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gitlin LN, Kales HC, Lyketsos CG. Nonpharmacologic management of behavioral symptoms in dementia. JAMA 2012;308:2020–9. 10.1001/jama.2012.36918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oliveira AMde, Radanovic M, Mello PCHde, et al. Nonpharmacological interventions to reduce behavioral and psychological symptoms of dementia: a systematic review. Biomed Res Int 2015;2015:1–9. 10.1155/2015/218980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NICE . Dementia: assessment, management and support for people living with dementia and their carers [NG97], 2018. Available: https://www.nice.org.uk/guidance/ng97 [PubMed]
- 6.NICE . Dementia: Quality standard [QS184], 2019. Available: https://www.scie-socialcareonline.org.uk/dementia-qs-184/r/a110f00000THdtRAAT
- 7.Trahan MA, Kuo J, Carlson MC, et al. A systematic review of strategies to foster activity engagement in persons with dementia. Health Educ Behav 2014;41:70S–83. 10.1177/1090198114531782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Testad I, Corbett A, Aarsland D, et al. The value of personalized psychosocial interventions to address behavioral and psychological symptoms in people with dementia living in care home settings: a systematic review. Int Psychogeriatr 2014;26:1083–98. 10.1017/S1041610214000131 [DOI] [PubMed] [Google Scholar]
- 9.Travers C, Brooks D, Hines S, et al. Effectiveness of meaningful occupation interventions for people living with dementia in residential aged care: a systematic review. JBI Database System Rev Implement Rep 2016;14:163–225. 10.11124/JBISRIR-2016-003230 [DOI] [PubMed] [Google Scholar]
- 10.Möhler R, Renom A, Renom H, et al. Personally tailored activities for improving psychosocial outcomes for people with dementia in long-term care. Cochrane Database Syst Rev 2018;2:CD009812. 10.1002/14651858.CD009812.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Möhler R, Renom A, Renom H, et al. Personally tailored activities for improving psychosocial outcomes for people with dementia in community settings. Cochrane Database Syst Rev 2020;8:CD010515. 10.1002/14651858.CD010515.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Möhler R, Renom A, Renom H. Personally tailored activities for people with dementia living in their own homes. Cochrane Database Syst Rev 2020;8. 10.1002/14651858.CD010515.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bennett S, Laver K, Voigt-Radloff S, et al. Occupational therapy for people with dementia and their family carers provided at home: a systematic review and meta-analysis. BMJ Open 2019;9:e026308. 10.1136/bmjopen-2018-026308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Macaulay S. The broken lens of BPSD: why we need to rethink the way we label the behavior of people who live with alzheimer disease. J Am Med Dir Assoc 2018;19:177–80. 10.1016/j.jamda.2017.11.009 [DOI] [PubMed] [Google Scholar]
- 15.Chenoweth L, King MT, Jeon Y-H, et al. Caring for aged dementia care resident study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: a cluster-randomised trial. Lancet Neurol 2009;8:317–25. 10.1016/S1474-4422(09)70045-6 [DOI] [PubMed] [Google Scholar]
- 16.Gitlin LN, Winter L, Burke J, et al. Tailored activities to manage neuropsychiatric behaviors in persons with dementia and reduce caregiver burden: a randomized pilot study. Am J Geriatr Psychiatry 2008;16:229–39. 10.1097/01.JGP.0000300629.35408.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cummings JL, Mega M, Gray K, et al. The neuropsychiatric inventory: comprehensive assessment of psychopathology in dementia. Neurology 1994;44:2308–14. 10.1212/wnl.44.12.2308 [DOI] [PubMed] [Google Scholar]
- 19.Alexopoulos GS, Abrams RC, Young RC, et al. Cornell scale for depression in dementia. Biol Psychiatry 1988;23:271–84. 10.1016/0006-3223(88)90038-8 [DOI] [PubMed] [Google Scholar]
- 20.Cohen-Mansfield J, Billig N. Agitated behaviors in the elderly. I. a conceptual review. J Am Geriatr Soc 1986;34:711–21. 10.1111/j.1532-5415.1986.tb04302.x [DOI] [PubMed] [Google Scholar]
- 21.Cochrane Effective Practice and Organisation of Care (EPOC) . Describing interventions in EPOC reviews, 2017. Available: https://epoc.cochrane.org/resources/epoc-resources-review-authors
- 22.Cohen J. Statistical power analysis for the behavioral sciences. Academic Press, 2013. [Google Scholar]
- 23.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Chichester: John Wiley & Sons, 2011. [Google Scholar]
- 24.Higgins JP, Li T, Deeks JJ. Choosing effect measures and computing estimates of effect: the cochrane collaboration, 2019. Available: www.training.cochrane.org/handbook
- 25.Sterne JAC, Savović J, Page MJ, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;2:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 26.Lam LCW, Lui VWC, Luk DNY, et al. Effectiveness of an individualized functional training program on affective disturbances and functional skills in mild and moderate dementia-a randomized control trial. Int J Geriatr Psychiatry 2010;25:133–41. 10.1002/gps.2309 [DOI] [PubMed] [Google Scholar]
- 27.Holthoff VA, Marschner K, Scharf M, et al. Effects of physical activity training in patients with alzheimer's dementia: results of a pilot RCT study. PLoS One 2015;10:e0121478. 10.1371/journal.pone.0121478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Telenius EW, Engedal K, Bergland A. Effect of a high-intensity exercise program on physical function and mental health in nursing home residents with dementia: an assessor blinded randomized controlled trial. PLoS One 2015;10:e0126102. 10.1371/journal.pone.0126102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davison TE, Nayer K, Coxon S, et al. A personalized multimedia device to treat agitated behavior and improve mood in people with dementia: a pilot study. Geriatr Nurs 2016;37:25. 10.1016/j.gerinurse.2015.08.013 [DOI] [PubMed] [Google Scholar]
- 30.Giuli C, Papa R, Lattanzio F, et al. The effects of cognitive training for elderly: results from my mind project. Rejuvenation Res 2016;19:485–94. 10.1089/rej.2015.1791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garland K, Beer E, Eppingstall B, et al. A comparison of two treatments of agitated behavior in nursing home residents with dementia: simulated family presence and preferred music. Am J Geriatr Psychiatry 2007;15:514–21. 10.1097/01.JGP.0000249388.37080.b4 [DOI] [PubMed] [Google Scholar]
- 32.Sung H-C, Chang AM, Lee W-L. A preferred music listening intervention to reduce anxiety in older adults with dementia in nursing homes. J Clin Nurs 2010;19:1056–64. 10.1111/j.1365-2702.2009.03016.x [DOI] [PubMed] [Google Scholar]
- 33.Lin Y, Chu H, Yang C-Y, et al. Effectiveness of group music intervention against agitated behavior in elderly persons with dementia. Int J Geriatr Psychiatry 2011;26:670–8. 10.1002/gps.2580 [DOI] [PubMed] [Google Scholar]
- 34.Ridder HMO, Stige B, Qvale LG, et al. Individual music therapy for agitation in dementia: an exploratory randomized controlled trial. Aging Ment Health 2013;17:667–78. 10.1080/13607863.2013.790926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sakamoto M, Ando H, Tsutou A. Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. Int Psychogeriatr 2013;25:775–84. 10.1017/S1041610212002256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kwak J, Anderson K. Findings from a prospective randomized controlled trial of an individualized music listening program for persons with dementia. J Appl Gerontol 2020;39:567–75. 10.1177/0733464818778991 [DOI] [PubMed] [Google Scholar]
- 37.Weise L, Töpfer NF, Deux J, et al. Feasibility and effects of individualized recorded music for people with dementia: a pilot RCT study. Nordic J Music Ther 2020;29:39–56. 10.1080/08098131.2019.1661507 [DOI] [Google Scholar]
- 38.Orsulic-Jeras S, Judge KS, Camp CJ. Montessori-based activities for long-term care residents with advanced dementia: effects on engagement and affect. Gerontologist 2000;40:107–11. 10.1093/geront/40.1.107 [DOI] [PubMed] [Google Scholar]
- 39.Cohen-Mansfield J, Parpura-Gill A, Golander H. Utilization of self-identity roles for designing interventions for persons with dementia. J Gerontol B Psychol Sci Soc Sci 2006;61:P202–12. 10.1093/geronb/61.4.p202 [DOI] [PubMed] [Google Scholar]
- 40.Cohen-Mansfield J, Libin A, Marx MS. Nonpharmacological treatment of agitation: a controlled trial of systematic individualized intervention. J Gerontol A Biol Sci Med Sci 2007;62:908–16. 10.1093/gerona/62.8.908 [DOI] [PubMed] [Google Scholar]
- 41.Kolanowski A, Litaker M, Buettner L, et al. A randomized clinical trial of theory-based activities for the behavioral symptoms of dementia in nursing home residents. J Am Geriatr Soc 2011;59:1032–41. 10.1111/j.1532-5415.2011.03449.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van der Ploeg ES, Eppingstall B, Camp CJ, et al. A randomized crossover trial to study the effect of personalized, one-to-one interaction using Montessori-based activities on agitation, affect, and engagement in nursing home residents with dementia. Int Psychogeriatr 2013;25:565–75. 10.1017/S1041610212002128 [DOI] [PubMed] [Google Scholar]
- 43.Yoon JE, Lee SM, Lim HS, et al. The effects of cognitive activity combined with active extremity exercise on balance, walking activity, memory level and quality of life of an older adult sample with dementia. J Phys Ther Sci 2013;25:1601–4. 10.1589/jpts.25.1601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Toba K, Nakamura Y, Endo H, et al. Intensive rehabilitation for dementia improved cognitive function and reduced behavioral disturbance in geriatric health service facilities in Japan. Geriatr Gerontol Int 2014;14:206–11. 10.1111/ggi.12080 [DOI] [PubMed] [Google Scholar]
- 45.Lu YY-F, Bakas T, Yang Z, et al. Feasibility and effect sizes of the revised daily engagement of meaningful activities intervention for individuals with mild cognitive impairment and their caregivers. J Gerontol Nurs 2016;42:45–58. 10.3928/00989134-20160212-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Prick A-E, Scherder E, et al. The effects of a multicomponent dyadic intervention on the mood, behavior, and physical health of people with dementia: a randomized controlled trial. Clin Interv Aging 2016;11:383–95. 10.2147/CIA.S95789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li D-M, Li X-X. The effect of folk recreation program in improving symptoms: a study of Chinese elder dementia patients. Int J Geriatr Psychiatry 2017;32:901–8. 10.1002/gps.4543 [DOI] [PubMed] [Google Scholar]
- 48.Tanaka S, Honda S, Nakano H, et al. Comparison between group and personal rehabilitation for dementia in a geriatric health service facility: single-blinded randomized controlled study. Psychogeriatrics 2017;17:177–85. 10.1111/psyg.12212 [DOI] [PubMed] [Google Scholar]
- 49.Jeon Y-H, Krein L, Simpson JM, et al. Feasibility and potential effects of interdisciplinary home-based reablement program (I-HARP) for people with cognitive and functional decline: a pilot trial. Aging Ment Health 2020;24:1916-1925. 10.1080/13607863.2019.1642298 [DOI] [PubMed] [Google Scholar]
- 50.Huber A, Oppikofer S, Meister L, et al. Music & memory: the impact of individualized music listening on depression, agitation, and positive emotions in persons with dementia. Act Adapt Aging 2021;45:70–84. 10.1080/01924788.2020.1722348 [DOI] [Google Scholar]
- 51.Gitlin LN, Winter L, Dennis MP, et al. A biobehavioral home-based intervention and the well-being of patients with dementia and their caregivers: the cope randomized trial. JAMA 2010;304:983–91. 10.1001/jama.2010.1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bailey EM, Stevens AB, LaRocca MA, et al. A randomized controlled trial of a therapeutic intervention for nursing home residents with dementia and depressive symptoms. J Appl Gerontol 2017;36:895–908. 10.1177/0733464815627956 [DOI] [PubMed] [Google Scholar]
- 53.Gitlin LN, Arthur P, Piersol C, et al. Targeting behavioral symptoms and functional decline in dementia: a randomized clinical trial. J Am Geriatr Soc 2018;66:339–45. 10.1111/jgs.15194 [DOI] [PubMed] [Google Scholar]
- 54.Novelli MMPC, Machado SCB, Lima GB, et al. Effects of the tailored activity program in Brazil (TAP-BR) for persons with dementia: a randomized pilot trial. Alzheimer Dis Assoc Disord 2018;32:339–45. 10.1097/WAD.0000000000000256 [DOI] [PubMed] [Google Scholar]
- 55.de Oliveira AM, Radanovic M, Homem de Mello PC, et al. An intervention to reduce neuropsychiatric symptoms and caregiver burden in dementia: preliminary results from a randomized trial of the tailored activity program-outpatient version. Int J Geriatr Psychiatry 2019;34:1301–7. 10.1002/gps.4958 [DOI] [PubMed] [Google Scholar]
- 56.O'Connor CM, Clemson L, Brodaty H, et al. The tailored activity program (TAP) to address behavioral disturbances in frontotemporal dementia: a feasibility and pilot study. Disabil Rehabil 2019;41:299–310. 10.1080/09638288.2017.1387614 [DOI] [PubMed] [Google Scholar]
- 57.Van Haitsma KS, Curyto K, Abbott KM, et al. A randomized controlled trial for an individualized positive psychosocial intervention for the affective and behavioral symptoms of dementia in nursing home residents. J Gerontol B Psychol Sci Soc Sci 2015;70:35–45. 10.1093/geronb/gbt102 [DOI] [PubMed] [Google Scholar]
- 58.Dechamps A, Alban R, Jen J, et al. Individualized cognition-action intervention to prevent behavioral disturbances and functional decline in institutionalized older adults: a randomized pilot trial. Int J Geriatr Psychiatry 2009;25:850–60. 10.1002/gps.2427 [DOI] [PubMed] [Google Scholar]
- 59.Cohen-Mansfield J, Thein K, Marx MS, et al. Efficacy of nonpharmacologic interventions for agitation in advanced dementia: a randomized, placebo-controlled trial. J Clin Psychiatry 2012;73:1255–61. 10.4088/JCP.12m07918 [DOI] [PubMed] [Google Scholar]
- 60.Hall GR, Buckwalter KC. Progressively lowered stress threshold: a conceptual model for care of adults with Alzheimer's disease. Arch Psychiatr Nurs 1987;1:399–406. [PubMed] [Google Scholar]
- 61.Cohen-Mansfield J, Werner P, Marx MS. An observational study of agitation in agitated nursing home residents. Int Psychogeriatr 1989;1:153–65. 10.1017/s1041610289000165 [DOI] [PubMed] [Google Scholar]
- 62.Logsdon RG, Teri L, Weiner MF, et al. Assessment of agitation in alzheimer’s disease: the agitated behavior in dementia scale. J Am Geriatr Soc 1999;47:1354–8. 10.1111/j.1532-5415.1999.tb07439.x [DOI] [PubMed] [Google Scholar]
- 63.Reisberg B, Borenstein J, Salob SP, et al. Behavioral symptoms in alzheimer's disease: phenomenology and treatment. J Clin Psychiatry 1987;48 Suppl:9–15. [PubMed] [Google Scholar]
- 64.Machida A. [Estimation of the reliability and validity of the short version of the 28-item dementia behavior disturbance scale]. Nihon Ronen Igakkai Zasshi 2012;49:463–7. 10.3143/geriatrics.49.463 [DOI] [PubMed] [Google Scholar]
- 65.Logsdon RG, Gibbons LE, McCurry SM. Quality of life in Alzheimer’s disease: patient and caregiver reports. J Ment Health Aging 1999;5:21–32 https://www.researchgate.net/publication/232417911_Quality_of_Life_in_Alzheimer's_disease_Patient_and_Caregiver_Reports [Google Scholar]
- 66.EuroQol Group . EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199–208. 10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- 67.Terada S, Ishizu H, Fujisawa Y, et al. Development and evaluation of a health-related quality of life questionnaire for the elderly with dementia in Japan. Int J Geriatr Psychiatry 2002;17:851–8. 10.1002/gps.711 [DOI] [PubMed] [Google Scholar]
- 68.Yesavage JA. Geriatric depression scale. Psychopharmacol Bull 1988;24:709–11. [PubMed] [Google Scholar]
- 69.Helmes E, Csapo KG, Short JA. Standardization and validation of the multidimensional observation scale for elderly subjects (moses). J Gerontol 1987;42:395–405. 10.1093/geronj/42.4.395 [DOI] [PubMed] [Google Scholar]
- 70.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Skrajner MJ, Camp CJ. Resident-assisted Montessoriprogramming (RAMP™): use of a small group reading activity run by persons with dementia in adult day health care and long-term care settings. Am J Alzheimers Dis Other Demen 2007;22:27–36. 10.1177/1533317506297895 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-048917supp001.pdf (795.6KB, pdf)
Data Availability Statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.