Abstract
Risks associated with fatigue that accumulates during work shifts have historically been managed through working time arrangements that specify fixed maximum durations of work shifts and minimum durations of time off. By themselves, such arrangements are not sufficient to curb risks to performance, safety, and health caused by misalignment between work schedules and the biological regulation of waking alertness and sleep. Science-based approaches for determining shift duration and mitigating associated risks, while addressing operational needs, require: (1) a recognition of the factors contributing to fatigue and fatigue-related risks; (2) an understanding of evidence-based countermeasures that may reduce fatigue and/or fatigue-related risks; and (3) an informed approach to selecting workplace-specific strategies for managing work hours. We propose a series of guiding principles to assist stakeholders with designing a shift duration decision-making process that effectively balances the need to meet operational demands with the need to manage fatigue-related risks.
Key words: working time arrangements, shift scheduling, mental fatigue, sleepiness, alertness, productivity, circadian rhythms, sleep homeostasis, occupational medicine, policy making
Statement of Significance
There is a critical need for policies and regulations regarding shift duration to reliably manage risks related to fatigue and sleepiness in the workplace. Regulators, organizations, communities, and workers often struggle with how to manage shift duration and address associated risks from fatigue and sleepiness while continuing to meet the societal demands for work. Scientific evidence that is essential for designing effective shift duration solutions has grown substantially in recent years, and global practices have evolved, providing a foundation for making informed decisions about shift duration while preserving the integrity and feasibility of workplace operations. We present an ensemble of guiding principles, with reference to relevant resources and examples, to help devise tailored solutions pertaining to shift duration.
Definitions: Fatigue, Sleepiness, and Alertness
Science-based approaches for determining shift duration and mitigating associated risks are based, in part, on literature about sleep, sleep deprivation, circadian rhythmicity (i.e. timing on the biological clock in the brain), and the concepts of fatigue, sleepiness, and alertness. In the scientific literature, a variety of definitions for fatigue, sleepiness, and alertness can be found.1–3 In clinical and academic settings these terms have distinct meanings,3 with fatigue often used to refer to bodily symptoms associated with physical exertion, medical conditions such as anemia, thyroid disease, or cancer, and use of medications, such as blood pressurelowering drugs or chemotherapy. In these settings, fatigue is not generally used in relation to insufficient or displaced sleep. In operational contexts, however, the terms fatigue, sleepiness, and reduced alertness are often used interchangeably.3–5 To avoid confusion, the terminology used in this paper is based on the following definitions, which are typical in practice across operational settings.
Fatigue: A state of reduced mental or physical performance capability, resulting from sleep loss or extended wakefulness, circadian rhythmicity, workload, or other factors.6 As used in operational settings, fatigue manifests as performance impairment when engaging in a task. Mental fatigue implies decreased or degraded cognitive performance; physical fatigue implies decreased or degraded physical performance.
Sleepiness: A state of increased tendency to fall sleep, resulting from sleep loss or extended wakefulness, circadian rhythmicity, medications, or various sleep disorders.2,3 Sleepiness manifests objectively as an increased likelihood to fall asleep rapidly.2 and subjectively as an increased need or desire to sleep.3 Sleepiness is a contributor to mental fatigue.3,5
Alertness: The ability to direct and sustain attention, which is influenced by prior sleep and sleep loss, circadian rhythmicity, time on task (duration of continuous work), and other factors.7 Alertness manifests as the ability to maintain the attention necessary to perform a task at a specified level. Sleepiness is associated with reduced alertness.2
INTRODUCTION
The scheduling of work shifts has historically prioritized productivity, taking into account production costs and the available human resource pool, with little consideration of the effects of work schedules on workers.8 While acknowledging the importance of productivity, mounting evidence indicates that work schedules can have a negative impact on workers and their communities.9,10 The need to balance a demand for high work productivity at all hours of the day with the costs associated with long work hours fuels debate among employers, workers and policymakers about what the maximum durations of work shifts should be. This debate is complex, and a single solution would not be applicable to all work settings, industries or occupations.
During the 19th and part of the 20th century, when most work involved physical labor, the debate focused on physical fatigue as the main concern for work performance and safety. Because physical fatigue accumulates steadily across the duration of physical work, and dissipates progressively during rest breaks, regulations to limit fatigue focused on prescribing maximum durations for work shifts and minimum durations for time off.11 After World War II, the focus shifted from physical fatigue to mental fatigue as the primary concern in most industries.12 While mental fatigue, like physical fatigue, is exacerbated with increased work duration and reduced by rest breaks, mental fatigue does not simply accumulate and dissipate progressively with time on and off work.13 Other factors—especially time of day and the durations of wakefulness and prior sleep (see Appendix A) —also have a significant effect on mental fatigue.5 Nonetheless, regulations for shift duration are typically prescriptive and focused on shift maxima and break minima, along with limits on work hours aggregated over weeks to months.
Following deregulation efforts in the 1980s, many industries moved toward longer shifts and greater demands at work. Many factors contributed to this trend,14,15 including increased global competition; shortage of qualified employees; increased overtime and secondary employment to maintain a standard of living; increasing economic disparities; rising healthcare and retirement costs; and contingent work arrangements such as contract work. These trends have persisted into the 21st century. According to data from the American Time Use Survey in 2017 and 2018, 16% of U.S. wage and salary workers have non-standard working time arrangements.16 under a wide range of prevailing practices and regulations. Based on the 2019 Current Population Survey, 16.3% of the U.S. labor force works 49 h or more per week, and 6.6% works at least 60 h per week.17
Working longer hours has yielded economic prosperity and, on average, a higher standard of living, but has also resulted in increased levels of risk related to mental fatigue.11 Productivity requirements and financial incentives to work have grown substantially.15,18 Work hours are distributed increasingly across all hours of the day and infringe on the “biological night,” that is, the time period when the biological clock signals to the brain that it is time to sleep.19 Increasingly, work hours curtail the opportunity to obtain adequate sleep, with approximately 40% of workers in several major occupational sectors reporting short sleep duration.20 Other factors such as long commute times, skipped rest breaks, insufficiently regulated overtime, multiple jobs, caregiver duties, and social commitments also contribute to mental fatigue.5,21–24
Mental fatigue is associated with considerable risks to employees, employers, and society at large.5,9 Acute, short-term risks include reductions in performance, effectiveness, and productivity;5,25,26 increased errors and do-overs;26,27 absenteeism;24,28 “presenteeism,” wherein the worker is on task but performing below capacity;26,28 ineffective teamwork;29 immoral or unethical behavior;30,31 reduced job satisfaction;32 degraded quality of lif;33,34 decreased morale29 reduced safety;35,36 workplace accidents and injuries;4,37–39 motor vehicle crashes during the commute;40 and high-profile industrial catastrophes.41,42 In addition to degraded physical and mental health,43 long-term risks include reduced individual and community well-being as well as economic losses;44 Adverse fatigue-related outcomes are typically under-reported and under-recognized,45 and systematic approaches to attributing the causes of these outcomes to work schedules46,47are not widely used. While exact figures of the costs to society associated with fatigue are therefore not available, estimates for the United States exceed $100 billion annually.26
Mental fatigue is determined in large measure by time of day and the durations of wakefulness and prior sleep48 (see Appendix A). Prescriptive regulations for shift maxima and break minima alone are, therefore, not a dependable means of ensuring adequate sleep and/or mitigating risks associated with mental fatigue.49,50 In other words, the effectiveness of a rule set with fixed thresholds that restrict shift duration and protect time off depends on the circumstances. Such a rule set does not necessarily address fatigue and fatigue-related risks adequately and reliably, and the promulgation of such a rule set by a regulator should not be taken as a determination that work hours compliant with the rule set are automatically safe.11 Despite decades of implementation efforts and debate, no consensus exists on an appropriate maximum shift duration.51 Prescriptive regulations for work hours and rest can be effective to prevent work schedules that maximize productivity with no consideration for the biological need for sleep and other prerequisites for safety and health. However, prescriptive regulations alone are not the solution, and sometimes they can be counterproductive.52 Many work environments with prescriptive working time regulations show poor congruence between regulatory compliance and risk outcomes. On the one hand, a primary emphasis on productivity within the constraints of regulatory compliance incentivizes the creation of shift schedules that leave risks associated with fatigue/sleepiness poorly addressed. On the other hand, prescriptive regulations for work hours and rest do little to curb the long-term health risks associated with workers not getting enough sleep on a regular basis. Furthermore, some prescriptive regulations may involve limits from which even minor deviations to improve relevant outcomes such as productivity or worker well-being may be prohibited despite negligible increases in fatigue/sleepiness-related risks. If congruence between compliance with regulations and outcomes is poor, it threatens both the effectiveness of those regulations and the willingness of individuals and organizations to adhere to them, with potentially harmful consequences.11
A well-recognized need exists, therefore, for policies and regulations regarding shift duration that curb fatigue/sleepiness- related risks reliably. However, regulators, organizations, communities and workers often struggle with how to manage shift duration and manage fatigue/sleepiness-related risks while continuing to meet the societal demands for work. Guiding principles that inform policy and decision-making in this area have been difficult to access, so stakeholders are often put in a position of addressing work schedule issues with insufficient guidance. Industrial and regulatory agreements pertaining to shift duration should not be taken at face value as evidence of acceptable risk levels. Scientific evidence that is essential for designing effective shift duration solutions has grown substantially in recent years,8 and global practices have evolved.53,54 The evidence that is now available can help inform decisions about shift duration and timing, while also addressing the integrity and feasibility of workplace operations.
This document is a guide to help devise tailored solutions pertaining to shift duration. We present this information as an ensemble of guiding principles, with reference to relevant resources and examples. The guiding principles consider scientific evidence, values- and ethics-based contexts, goals and objectives of organizations and individuals, resource needs, and feasibility. Taken together, the guiding principles represent a framework from which decisions can be made. We encourage stakeholders - managers and their representatives, employees and their representatives, legislators, policy makers, and occupational medicine professionals - to consider the guiding principles, collectively (rather than separately), in designing effective, context-specific solutions regarding shift duration.
RISK FACTORS ASSOCIATED WITH SHIFT DURATION
While the mechanisms linking shift duration with health outcomes remain unclear,55 the relationship between shift duration and performance and safety outcomes is relatively well-understood. Work hours control the duration and timing of wakefulness and constrain the duration and timing of sleep, which affects the manifestation of mental fatigue, which in turn influences performance—including physical,56 mental,57 leadership,58 and team-based29—and safety risks,59,60 The relationship of wakefulness and sleep with fatigue is mediated by sleepiness, which is governed by two primary biological processes: the “circadian” wake drive and the “homeostatic” sleep drive.61 The “circadian” process promotes wakefulness during the day and sleep during the night, as driven by the brain’s biological clock. The “homeostatic” process seeks to balance the amounts of wakefulness and sleep by increasing sleep pressure as time awake accrues, and dissipating sleep pressure as time asleep accrues. At any given time during wakefulness, the interplay between these two processes determines sleepiness and thereby influences the level of mental fatigue (see Appendix A).48,62
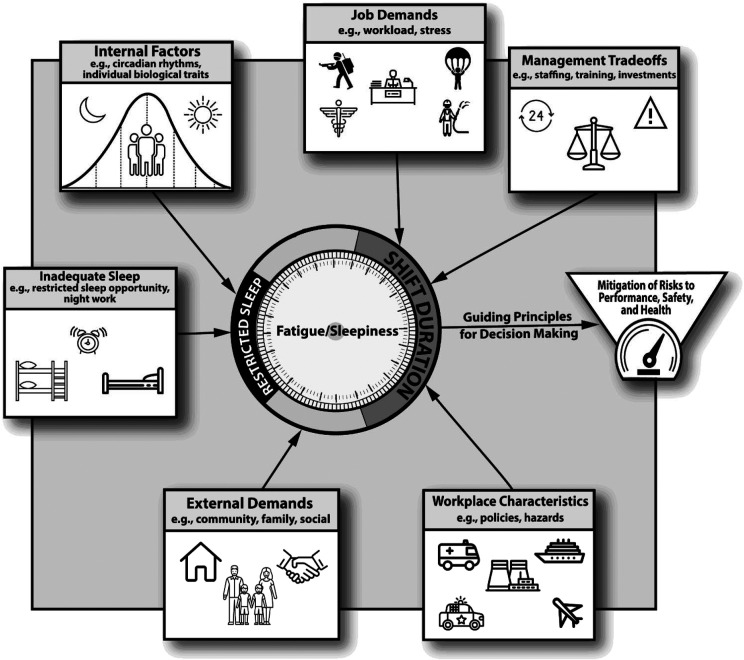
The manifestation of fatigue related to sleepiness driven by the two processes is exacerbated when working time arrangements limit and/or displace the time available for sleep.5 Other demands on a person’s time, including time needed for eating, personal hygiene, commuting, caregiver responsibilities, social activities, educational activities, secondary job, etc., may further constrain the time available for sleep and increase sleepiness and fatigue.23,24,63,64 Furthermore, the effects of repeated exposure to sleep loss and/or sleep displacement across consecutive days are cumulative.65,66 In the workplace, other factors, such as workload,67 stress,28,68 and inherent workplace hazards69,70 interact with fatigue/sleepiness to determine the overall fatigue-related risk levels associated with shift duration5 (see Figure 1). Collectively, these risk factors are captured in guiding principles 1.1–1.3 below.
Figure 1. Factors influencing the performance, safety and health risks associated with shift duration.
This diagram illustrates the multiple factors to be considered in balancing the needs of an operational setting, the human resource requirements to meet those needs, and the pivotal and complex role of shift duration. Shift duration competes with other demands on people’s time—for example, for commuting, eating, personal hygiene, non-work-related commitments, and social activities—and restricts the time available for sleep.23,24,63 Fatigue/sleepiness associated with reduced and displaced sleep and with the timing of the biological clock (circadian rhythm), in conjunction with individual traits (e.g. vulnerability to sleep loss) and workplace characteristics and hazards determines overall risk levels.124,144 Evaluation of these interconnected factors is pertinent to decision making about shift duration.
Guiding principle 1.1: The duration of work shifts is linked to adverse performance, safety, and health outcomes, especially when the shifts are not aligned with a worker’s biological clock to promote alertness during work and sleep during time off.
A primary cause of adverse outcomes associated with shift duration is misalignment of the timing and duration of work hours with the innate physiologic, temporal regulation of sleep and waking alertness.10,71 If sleep occurs during the night, when the circadian drive for wakefulness is low, and wakefulness and work occur during the day, when the circadian drive for wakefulness is high, the recuperative potential of sleep is generally high, and alertness during work hours is expected to be optimal. However, deviation of work hours from this optimal alignment may compromise the recuperative effect of sleep and increase sleepiness while awake, which contributes to mental fatigue and increased risk of adverse performance, safety and health outcomes.72,73
Although long work hours may cause fatigue due to the duration of continuous work alone, this effect is exacerbated when the work period causes the duration of wakefulness to be extended, such that the build-up of pressure for sleep from the homeostatic process increases, and/or pushes some of the work hours into the night, when the circadian drive for wakefulness is low. Such working time arrangements place work hours at times when sleepiness, and therefore mental fatigue, is intrinsically increased.5 They may also infringe on time available for sleep, thereby reducing the restorative effects of sleep for alertness, performance, safety, and health.23
For example, a professional driver may have an early morning duty start and then face traffic delays toward the end of the shift. Such a work schedule extends the waking period into the evening hours and may lead to sleepiness and contribute to fatigue, which could lead to errors and accidents.74 Fatigue/ sleepiness and related risks would be compounded by a night shift schedule, where the work period may end at a time when accumulated homeostatic pressure for sleep and reduced pressure for wakefulness from the biological clock act together to increase sleepiness coincident with the time of the commute home after work.40
Risks associated with fatigue/sleepiness are also compounded by chronic exposure to sleep loss or sleep displacement,65,66,75 and multiple days with recovery sleep may be needed to overcome the cumulative effects of sustained sleep insufficiency.65 Moreover, when sleep is chronically insufficient, self-monitoring of fatigue/sleepiness becomes less reliable.66,76 These issues are problematic in work schedules that cause sleep to be curtailed routinely, and emphasize the importance of offsetting even occasional sleep loss (e.g. to handle a work-related emergency) with ample recovery sleep opportunity in order to avoid risk accumulation.
Guiding principle 1.2: Work-related factors, such as workload and commute time, contribute to the impact of shift duration on performance, safety, and health outcomes.
Whereas the alignment of work hours with respect to the temporal regulation of sleep and waking alertness is the primary driver of performance, safety and health outcomes, a variety of other work-related factors also play a role. These include schedule configuration considerations, such as early starts,77 forward and (especially) backward rotating shifts,78,79 irregular shift schedules,72 quick returns,80 work breaks,81 number of consecutive shifts,82 time off between duty cycles,76,83 and cumulative work hours across weeks, months and years54—and the frequency and extent to which these factors occur alone or in combination. Furthermore, working conditions play a role, including physical, cognitive and/or emotional workload,84–87 environmental conditions,5 inherent hazard exposure,88 and workplace culture and policies.89–93
Commutes to and from work impose a demand on workers and may curtail sleep opportunity.63,94 As such, the duration of the commute, its timing, traffic exposure, and road, weather and light conditions are all relevant. The time required for commuting and other work-related time commitments outside of work (e.g. time to prepare and wind down from work) may accumulate to a degree that, combined with the work shift, leaves insufficient time for sleep and recuperation. For example, a worker who completes a 12-h shift preceded and followed by a 2-h commute, after managing activities of daily living (e.g. eating, personal hygiene), would have insufficient time between shifts to get adequate sleep.
These factors result in a demand on workers to manage extended hours of operation, often under conditions of circadian misalignment associated with shift work and with chronic restriction of sleep opportunities.9 This scenario affects or destabilizes the health and wellness of the worker.10 Depending on the operational setting and context, responsibility for addressing these factors may rest with employers, employees, regulators, or other stakeholders.11
Guiding principle 1.3: Biological, behavioral, and social factors contribute to the impact of shift duration on performance, safety, and health outcomes.
The impact of shift duration, shift schedules, and other work- related factors on performance, safety and health outcomes is moderated by biological, behavioral and social factors that influence sleep need, optimal sleep timing, response to sleep loss, tolerance to operating long hours, and overall resilience.95 The direction of the effects, whether protective or not, may vary within and between factors, and depends on the context.
Among the most impactful of these factors is “chronotype,” which represents the individual preference, partially biologically mediated, to be active early or late in the day and to sleep early or late in the night.96 Chronotype determines the optimal timing of sleep, and therefore the extent to which work hours may fall outside the alert waking hours and/or interfere with sleep.97 Individuals also vary in how well they tolerate work hours that are poorly aligned with their chronotype.98 Other relevant individual characteristics, most of which have been identified in the context of shift work, include age,99 sex,100 race/ethnicity,101 physical fitness,99 physical and mental health status,101 vulnerability to sleep loss,102 sensitivity to stress,103 and coping style.104 Social moderators such as family-related, cultural, societal, and socioeconomic factors are also relevant.9
Enduring or extended exposure to risk factors, whether biological, behavioral, individual, or societal, is likely to confer greater risk of adverse long-term consequences, compared against brief or short-term exposure. For example, there are well-documented risks to long-term health105 from sleeping during the day, at irregular times, or insufficiently;73 sleeping at least 7 h per night is recommended for the average adult.106 Epidemiologic studies of night shift work suggest that long-term health risks accumulate with the number of years of shift work exposure.10 The extent to which cumulative health risks are specifically a function of shift duration remains to be determined, but shared biological mechanisms underlying the impacts of shift duration and the duration and timing of sleep (see Appendix A) suggest that shift duration plays a role.
COUNTERMEASURES FOR RISKS ASSOCIATED WITH SHIFT DURATION
Tools and strategies that can be deployed in operational settings to reduce the adverse consequences of extended work shifts, collectively called “countermeasures,” are an integral component of mitigating the impact of work hours on performance, safety, and health.60,81 Although relatively little is known about countermeasures that pertain to health specifically, much more is known about countermeasures relevant to performance and safety or risks overall. Countermeasures that are backed by evidence of their effectiveness, at least in the short term, and generally expected to be feasible and acceptable to workers are summarized in Table 1. Because of their potential to offset the risks associated with work hours, the availability and implementation of countermeasures is an important consideration when discussing shift duration.5
Table 1.
Countermeasures for risks associated with shift duration. The table lists countermeasures that have evidence of their effectiveness, at least in the short term, and are generally expected to be feasible and acceptable to workers. See Appendix D for background information and references.
| Countermeasure | Timing of use | Short-term effects | Long-term effects | ||
|---|---|---|---|---|---|
| Before Shift | During Shift | After Shift | |||
Scheduling interventions to:
|
Providing employees with advance notice of working time arrangements allows for better preparation for a work shift (e.g. preparatory napping) | In shift work and extended shift operations, implementations of fixed (non-rotating) or forward rotating shift schedules, shorter shift durations, and reduced workload may constitute improvements Scheduling enough personnel to allow for rest breaks during work shifts facilitates the use of other counter- measures such as workplace napping, strategic caffeine use, and activity breaks | Providing employees with adequate time off between shifts allows for greater recovery |
Positive effects:
|
Positive effects:
|
| Napping (see Appendix D2) | Napping may be used to reduce sleep pressure before evening or night work (“prophylactic napping”) | Sanctioned workplace napping (on-the-job napping) can help alleviate unexpected sleepiness or sleepiness arising from extended shift duration | Napping may be advisable after a night or early morning shift to catch up on sleep or revert to a nighttime sleep schedule | Positive effects: • improved alertness and performance on the job, during the commute, and/or at home Negative effects: • sleep inertia, which is significantly reduced alertness and performance immediately upon waking, requiring a brief period (15–30 min) to reorient before engaging in work tasks or driving | Positive effects: • not well established Negative effects: • not well established |
| Caffeine use (see Appendix D3) | Caffeine use may be advisable before an extended commute to work or a long shift | Frequent, low-dose caffeine use may stabilize alertness and performance after sleep loss and during night and early morning shifts If consumed close to intended sleep time, caffeine can interfere with sleep onset | Caffeine use may be advisable before an extended commute home | Positive effects: • improved alertness and performance on the job, during the commute, and/or at home • when taken in conjunction with a nap, the time to overcome sleep inertia (see under “napping” above) may be reduced Negative effects: • large inter-individual differences in caffeine effectiveness and tolerance make it difficult to provide tailored advice on caffeine use | Positive effects: • not well established Negative effects: • habituation to caffeine can reduce its effectiveness • sustained, highdose caffeine use can cause side effects (e.g. anxiety, insomnia, tremor, arrhythmias, dehydration, withdrawal headaches) |
| Sleep hygiene and treatment of sleep disorders (see Appendix D4) | Sleep hygiene strategies may be used before a shift to help maximize sleep duration and improve the recuperative potential of sleep | Sleep hygiene strategies may be used to optimize benefit from on-the-job napping | Diagnosis and treatment of sleep disorders improves sleep’s recuperative potential and promotes health and well-being |
Positive effects:
|
Positive effects:
|
| Wake- and sleep-promoting medications (see Appendix D5) | In consultation with a medical specialist, wakepromoting medications may be considered for individuals who experience significantly reduced alertness during the commute to work | In consultation with a medical specialist, wake-promoting medications may be considered for individuals who experience significantly reduced alertness during a shift or during the subsequent commute home | In consultation with a medical specialist, sleeppromoting medications may be considered for individuals with difficulty sleeping between work shifts |
Positive effects:
|
Positive effects:
|
| Bright or blue light exposure (see Appendix D6) | Appropriately timed bright or blue light exposure may be advisable before an early morning shift or in the early morning before eastward transmeridian travel in order to help advance the biological clock Appropriately timed bright or blue light exposure may be advisable before a night shift or in the evening before westward transmeridian travel in order to help delay the biological clock | Appropriately timed bright or blue light exposure may be advisable during morning or evening hours to help advance or delay the biological clock, respectively Bright or blue light exposure can acutely improve alertness and may help night workers stay awake and alert during a shift | Appropriately timed bright or blue light exposure may be advisable after work to continue advancing or delaying the biological clock Appropriately timed bright or blue light exposure after transmeridian travel may help accelerate adjustment to a new time zone |
Positive effects:
|
Positive effects:
|
| Exercise and activity breaks (see Appendix D7) | Regular exercise is beneficial to employee health and wellness | Exercise breaks may transiently improve alertness Activity breaks may counteract adverse health consequences of prolonged sitting or poor posture Nightly exercise may facilitate adaptation of the biological clock to a night shift schedule | Exercising in the hour before bedtime may delay sleep onset |
Positive effects:
|
Positive effects:
|
| Fatigue prediction, detection and warning technologies (see Appendix D8) | Fatigue prediction, detection and warning technologies may be used before a shift to predict and help manage anticipated fatigue Fatigue prediction technologies may be used to help optimize work schedules and sleep schedules | Fatigue prediction, detection and warning technologies may be used during a shift to alert an employee or employer about elevated fatigue Fatigue prediction technologies may help guide the application of countermeasures | Fatigue prediction technologies may be used after a shift to help optimize sleep schedules Wearable technologies capable of detecting sleep may be used to monitor one’s sleep debt Fatigue prediction technologies may be used to help evaluate the role of fatigue in incidents that occurred during a shift |
Positive effects:
|
Positive effects:
|
| Risk mitigation tools, policies, and practices (see Appendix D9) | Risk mitigation practices may be useful before a shift to prepare for work or to allocate tasks based on expected fatigue levels | Risk mitigation tools, policies, and practices may be used to mitigate risks associated with fatigue even when long shifts and fatigue cannot be avoided Risk mitigation policies may guide and facilitate the availability and use of countermeasures in the workplace | Risk mitigation policies and practices may be used after a shift to guide proper hand-off to relief workers Risk mitigation systems may include a process to continually improve fatigue risk management strategies |
Positive effects:
|
Positive effects:
|
Some countermeasures reduce shift duration-related risks by increasing the amount of sleep or raising the level of waking alertness.107,108 Other countermeasures target operational risk outcomes; examples include checklists, quality control checks, warning systems, and team-based work strategies.69,91 Regardless of the approach, the goal is to manage fatigue/ sleepiness-related performance, safety and health outcomes associated with shift duration.60 The list of countermeasures in Table 1 is not meant to be exhaustive. Additional, context-specific countermeasures may be available for particular occupations (e.g. a wake-up call program for pilots taking advantage of nap opportunities while waiting for cargo planes to be loaded.109)
For the implementation of a given countermeasure, the benefits of decreasing fatigue/sleepiness or improving outcomes must be weighed against any unintended consequences.
For example, caffeine intake can decrease fatigue/sleepiness and improve alertness, performance and safety.110,111 However, consumption of caffeine close to bedtime, consumption of caffeine in high doses, and an individual’s sensitivity to caffeine, may lead to reduced recuperative potential of sleep.112 Similarly, naps can significantly improve alertness and performance.113,114 However, naps may also result in impaired cognition for a brief period immediately after awakening.115 a phenomenon known as “sleep inertia.” Thus, countermeasure use should be tailored to the context, recognizing that unintended consequences may reduce or negate effectiveness. Post-implementation monitoring of the positive and negative effects of countermeasures implemented in a given setting is important in order to assess (and, if necessary, address) the short- and long-term benefits and costs.11 These considerations are summarized in guiding principles 2.1–2.3 below.
Guiding principle 2.1: Countermeasures can reduce, but do not necessarily eliminate, adverse outcomes associated with shift duration.
The effectiveness of most countermeasures is influenced considerably by the specific circumstances and by inter-individual differences in their efficacy. For example, habitual caffeine users might not reap the same benefits of caffeine intake as those who only use caffeine strategically.116 Likewise, whereas some individuals could benefit greatly from napping in the workplace, others may have difficulty napping in the suboptimal conditions of the work environment or experience profound sleep inertia.117 As such, countermeasures are generally useful to help manage the effects of fatigue/sleepiness and related risks, but the availability of countermeasures should not, in itself, be used as a justification for making work shifts longer.
The application and effectiveness of countermeasures may be time-dependent. For example, caffeine as a fatigue countermeasure may not be helpful if used too early before a shift begins or too late during or after a shift.118 and it may interfere with sleep during the subsequent off-duty period.112 Workers should be provided guidance on when and how to use each available countermeasure for maximal effectiveness in a given work environment. Common countermeasures, and examples of when they may be applicable, are listed in Table 1.
The countermeasures presented in Table 1 are among those most commonly used in work environments. Some of these countermeasures are supported by a large body of laboratory and field research, while others, though implemented in specific environments, remain incompletely validated. For example, many studies conducted in both laboratory and field environments delineate the optimal times and circumstances for napping.119 By contrast, the use of exercise and activity breaks to improve alertness has limited support in the scientific literature, although these breaks may be helpful for improving health outcomes, especially for individuals working in sedentary occupations.120 The evidence base for various countermeasures is summarized in Table 1 and in the supplemental material.
Educating the workforce regarding the importance of adequate sleep and strategies to reduce the short- and long-term risks associated with fatigue/sleepiness is a central component of any countermeasure program.121,122 Workers should be educated about the countermeasures that are available and feasible for use in their work environment and how these countermeasures should be applied. However, the extent to which individuals can be required to use countermeasures, such as caffeine or other stimulants, is limited.123
Guiding principle 2.2: The development of policies regarding countermeasures and their application should be driven by an evaluation of the risks to be managed.
In some situations, a thorough evaluation may be needed to characterize the factors contributing to fatigue/sleepiness and related risks and inform the selection of the most appropriate countermeasure(s) and implementation of any incentives to promote their use. Adopting best practices that have already been established in comparable workplaces may be expedient.124 The operational, logistic and economic feasibility of specific countermeasures, and an assessment of whether the benefits are expected to be proportional to the costs, may determine which countermeasures are selected for implementation.
In settings that require 24-h operations, re-organizing the timing and duration of shifts can be helpful so that individual biological, behavioral and social factors are aligned with operational needs. Re-organizing working time arrangements may result in considerable return on investment, in the form of improved effectiveness, accidents avoided, reduced absenteeism and presenteeism, and greater retention.23,51Another option that may prove cost-effective is the use of caffeine. For example, an evidence-based guideline for emergency medical services (EMS) recommends wide availability of caffeine in EMS operations.111
Guiding principle 2.3: Monitoring the effects of countermeasures is important to determine their effectiveness, identify any unintended consequences, and evaluate opportunities for improvement.
Post-implementation monitoring of the effects, both positive and negative, of countermeasure implementation will inform whether any modifications are needed to better manage shift duration-related risks.11,125 Monitoring could involve the assessment of a variety of outcomes, including objective as well as self-report data from workers, productivity-related metrics, and fatigue/sleepiness-related incident reports and absenteeism rates.126
For example, the introduction of a dedicated nap room into a work environment has the potential to reduce fatigue/sleepiness, but practical aspects or work culture may serve as barriers to the use of the nap room.127 or sleep inertia may reduce the ability to perform after a nap.128 Post-implementation surveillance to determine when and how long employees are napping, coupled with objective performance indicators, may confirm that the nap room is working as intended, or that additional countermeasures are needed to address unintentional consequences.129 In this example, a formal hand-off protocol may be needed to facilitate the re-entry of an individual onto the work floor after a nap to address potential sleep inertia. Post-implementation surveillance assesses whether countermeasures are being used, whether they are beneficial, and what additional efforts may be needed to make them most effective.11
DECISION-MAKING ABOUT SHIFT DURATION
Multiple, potentially competing factors may play a role in decision-making about shift duration. To weigh such factors appropriately, the risks associated with shift duration and the countermeasures used to reduce these risks must be considered relative to a risk tolerance level—that is, the potential consequences that stakeholders are willing to accept in the context of what needs to be accomplished during the work shift and how important it may be that the work gets done.130 For example, the risk tolerance level for cross-continental organ transplant air transportation may be relatively high, so that stakeholders may be accepting of long shifts to make these kinds of life-saving operations possible, recognizing that they occur infrequently and are unlikely to incur cumulative risks from back-to-back operations.
The risks associated with long work shifts may not fall on the same individuals as the benefits.11 As such, involving a sufficiently broad spectrum of potential stakeholders is important in the decision-making process regarding what shift durations, and what risks, are acceptable. Relevant stakeholders include but are not limited to employees, managers, unions, regulators, safety officers, medical directors, shareholders, communities, and/or their representatives.
Guiding principle 3.1: Determining maximum shift duration requires stakeholders to balance risk factors, countermeasures, and potentially competing goals.
Determining appropriate shift durations involves a potentially complex tradeoff between the competing goals of stakeholders or their representatives. For example, employers need to balance profitability and operational outcomes with the safety and health of employees or client and community expectations. Employees may need to balance their income and the organizational expectations they face against time spent with personal activities. Regulators may need to balance the competing demands of businesses and employees against the interests of the public. The community often has to balance their expectations for the availability of around-the-clock services against the costs associated with providing those services.
These tradeoffs are further complicated by competing demands related to extended shift durations. For example, employers may adopt a policy of extended work hours to address the occasional need to deliver urgent or emergency services, even though a different policy could be a better choice—for example, a policy that sets more limited work hours and allows for occasional exceptions in which the risk of cumulative sleep loss is mitigated with protected post-duty recovery periods. Short-term financial and operational considerations must be weighed against long-term consequences for worker health and well-being or costs borne by the broader community (e.g. increased accident rates, need for extended childcare services, demands on the health care system). Ensuring that all stakeholders understand and acknowledge these tradeoffs is critical to designing effective policies about appropriate shift durations.
Guiding principle 3.2: The decision-making process about shift duration should be fully informed, transparent, and based on scientific evidence.
Ideally, all stakeholders should participate responsibly in the decision-making process regarding the appropriate duration of shifts. The decision-making process requires stakeholders to consider all of the operational consequences, as well as identify and manage any associated risks. In determining appropriate shift durations and requirements for countermeasures to reduce risks, organizations should develop a stakeholder input process that clearly identifies the potential risks, costs and benefits to all stakeholders. The risks should be evaluated both on average (typical risks) and in the extreme (potential for catastrophic outcomes).
Decisions about shift duration are often made without a comprehensive assessment of the scientific evidence that can inform the decision-making process. All decision-makers should therefore be aware of the potential implications of their decisions and the often-competing nature of priorities and outcomes. Regulators have a key role in providing balanced guidance materials that identify likely costs and benefits and assist non-expert stakeholders in interpreting and applying the relevant scientific evidence.
The quality, relevance and generalizability of scientific evidence supporting decision-making about shift duration is highly variable.51 However, a lack of compelling scientific evidence for a given decision-making factor (e.g. that certain work practices cause fatigue, or that certain countermeasures are effective) should not be seen as evidence against that factor. Insufficient scientific evidence could be due to logistical or financial barriers to conducting the research, not because the factor is irrelevant or unimportant, and testimony from experts familiar with the operation may be required. The limits of the available knowledge base, and the extent to which that knowledge base generalizes to the organization or industry in question, should be discussed explicitly. Any uncertainty in supporting evidence should reinforce the necessity of post-implementation surveillance programs (see guiding principle 3.5). Such programs can yield information about the efficacy of specific practices, which should be publicized whenever possible so that the knowledge base is expanded for future efforts.
Guiding principle 3.3: The decision-making process about shift duration should faithfully represent the interests of all stakeholders and respect the legitimacy of these interests.
Conflicts of interest can often arise between stakeholders and their representatives. Decision-makers who act on behalf of others should be expected to demonstrate that they are promoting the declared interests of those they represent in an accurate manner. To ensure this, those whose lives and livelihoods would be directly impacted by changes to shift duration should be permitted and encouraged to participate in the decision-making process.
Decision-makers will often use dissimilar criteria or values to determine the most appropriate shift durations. Sometimes these criteria involve factors outside the workplace. Acknowledging concerns about the impact of work hours on non-work-related factors, and treating such concerns as legitimate, is critical. Though doing so may not change the decision, such acknowledgment enables organizations to predict and address post-implementation issues before they lead to significant negative outcomes, such as increased absenteeism or the loss of valuable employees.
The impact of changes in shift duration can manifest outside the workplace. For example, extending a shift from 8 to 12 h might impose difficulty in finding childcare. Inevitably, decisions to change shift duration will not be universally welcomed. Organizations should acknowledge any inconvenience caused and take reasonable steps to minimize the inconvenience, where possible, or provide reasonable time to adjust to altered working time arrangements.
Guiding principle 3.4: Deliberations, policies, and documentation regarding shift duration should be supported by an organization’s safety management architecture.
In many organizations and industries, policy regarding shift duration has been considered a matter to be addressed by labor law or human resource departments, rather than a workplace safety and health issue. However, shift duration is foremost a safety and health issue with legal implications, and policies and procedures pertaining to shift duration are best embedded within organizational risk and safety management systems.121 Many industries have pre-existing policy frameworks from which to draw, such as workplace health and safety policies, Safety Management System policies, or (Fatigue) Risk Management policies; see Appendix B. In most cases, employers and employees and their representatives should assign primacy to safety and health implications of shift duration over social and financial ones.
Guiding principle 3.5: Changes to rules and policies on shift duration should be monitored and evaluated, and corrective action should be taken in the event of unintended outcomes.
Emerging evidence indicates that changes in working time arrangements can produce unintended and paradoxical outcomes. The reasons for this often reflect unique aspects of the workplace, workforce or work tasks. Workplaces are complex environments whose responses to changes in the working time arrangement can be hard to predict. As a consequence, following changes in shift duration, organizations should monitor and respond to leading indicators of potential problems and both positive and negative outcomes to ensure the effectiveness of shift duration policies.11
Monitoring systems should identify, report, quantify and manage existing and emerging risks.121 Recommendations for the development of such systems are provided in Appendix C. Larger organizations should seek independent, third-party input in the evaluation of their policies and procedures for managing the risks associated with shift duration. The need for and timing of such input should be based on defined criteria, such as the typical level of operational risk, or the emergence of new or changing data that would benefit from this type of expertise.
CONCLUSION
Maximum work shift durations have historically been based on a balance between workplace productivity and physical fatigue- related risks, with insufficient consideration of the impact on mental fatigue and associated risks regarding performance, safety, and health. Based on the guiding principles with respect to shift duration-related risks as described in section “Risk Factors Associated with Shift Duration” and mitigations provided by countermeasures as described in section “Countermeasures for Risks Associated with Shift Duration,” policies regarding shift duration should be context-specific and based on a tradeoff analysis that incorporates a comprehensive assessment of needs and risks as described in section “Decision-Making About Shift Duration.” A variety of factors may increase or decrease shift duration-related risks, and conditions may exist that impact acceptable solutions, such as emergency operational needs, economic acceptability, and workplace, political or legal culture. Ultimately, solutions should be designed such that compliance with their content is congruent with desired outcomes; otherwise, not only would such approaches be ineffective, but individuals and organizations may be less willing to adhere to them, and remain vulnerable to harmful downstream risks.
A key question in determining shift duration is whether and when the risks of continuing to work become greater than the risks of ceasing to work.11 The relevant risks may occur along a spectrum of severity or acceptability, and may be multidimensional, impacting various functional domains and diverse individuals or groups of individuals.8 The assessment of these risks, therefore, includes consideration of their impact on the various stakeholders; indeed, those who may be most impacted may differ from those who reap the greatest benefits of a particular shift duration policy.11 A choice of whether to accept the risks or intervene to reduce the risks is then required. The guiding principles provided in this document are meant to help devise tailored solutions to address these issues.
ACKNOWLEDGMENTS
The shift length task force thanks Dr Claire Caruso (National Institute for Occupational Safety and Health), Dr Michael Hodgson (Occupational Safety and Health Administration), and Emily Whitcomb (National Safety Council) for lending their expertise and providing valuable feedback during the development of this manuscript. While the Occupational Safety and Health Administration (OSHA) does not have concerns with the content of the guiding principles, OSHA does not endorse them. The shift length task force also thanks two anonymous reviewers for valuable feedback on the paper, and Ginger Ellen Espinoza of the Naval Postgraduate School for the graphic design of Figure 1.
APPENDIX A
Biological Processes of Sleep/ Wake Regulation
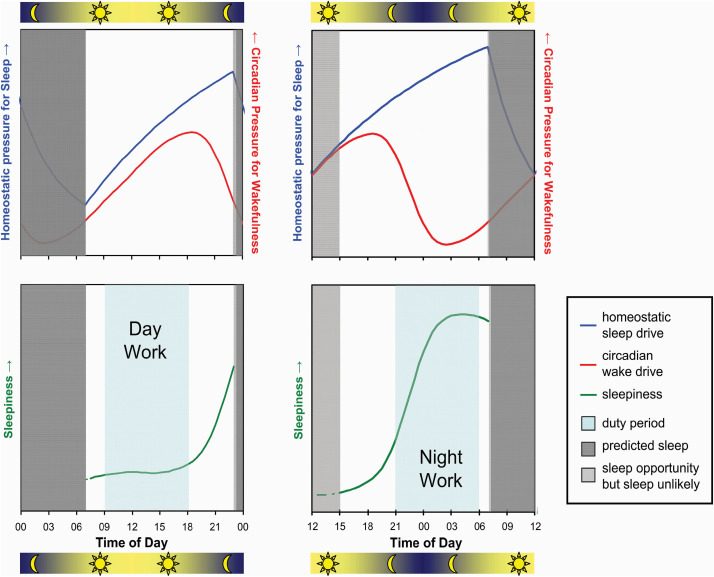
Mental fatigue, as defined earlier in this paper, is influenced strongly by sleepiness, and thereby by time of day and by the durations of wakefulness and prior sleep. This relationship is governed by two primary biological processes: the “circadian” wake drive and the “homeostatic” sleep drive.131–133 During the day, the circadian process produces rising pressure for wakefulness, which counteracts sleepiness. During the night, the circadian process withdraws this wake pressure, which promotes sleepiness and tendency to fall asleep. Simultaneously, during periods of wakefulness, the homeostatic process builds up pressure for sleep, which promotes sleepiness. During sleep periods, homeostatic pressure for sleep dissipates; the longer the sleep period, the less the remaining homeostatic sleep drive. Awakening from sleep occurs naturally when the remaining homeostatic sleep drive is overcome by the circadian wake drive. At any given time during wakefulness, sleepiness—and thereby mental fatigue as defined in this paper—is thus influenced by the interplay between the two processes, as illustrated in Figure A1.
Because the circadian process is a function of time of day, while the homeostatic process is a function of time awake and time asleep, the interplay between the two processes depends critically on the timing of periods of wakefulness and sleep. Figure A1 illustrates this for a healthy young adult in a day work scenario with daytime wakefulness and nighttime sleep (left panels), and in a night work scenario with nighttime wakefulness and daytime sleep (right panels). In the day work schedule, the interplay between the circadian and homeostatic processes maintains a stable, low level of sleepiness during most of the day, followed by a rapidly rising level of sleepiness in the late evening leading to the initiation of sleep. Furthermore, during nighttime sleep, the interplay between the two processes produces a consolidated sleep period. If the sleep period is not long enough, dissipation of the homeostatic pressure for sleep may be insufficient, and use of an alarm clock may be needed to wake up in time for work or other responsibilities.
Figure A1. Regulation of sleepiness by two biological processes.
A circadian process (red) produces a rising pressure for wakefulness, which counteracts fatigue, during the day; and a withdrawal of that pressure for wakefulness, thereby promoting sleepiness, during the night. Simultaneously, a homeostatic process (blue) builds up a pressure for sleep, thereby promoting sleepiness, during periods of wakefulness; and dissipated that pressure for sleep (dark gray), thereby providing recovery, during periods of sleep (top panels).131 The combined effect of the circadian and homeostatic processes on sleepiness may be calculated as the net difference between the homeostatic pressure for sleep and the circadian pressure for wakefulness (bottom panels, green),132 as illustrated here for a scenario with a daytime duty period (light blue) and an 8-h nighttime sleep opportunity (left panels) and for a scenario with a nighttime duty period (light blue) with an 8-h daytime sleep opportunity (right panels). Note that in the day work scenario, the sleep opportunity is ended (e.g. through use of an alarm clock) somewhat prematurely, as there is still some homeostatic pressure for sleep left to be dissipated (top left). In the night work scenario, however, sleep is curtailed much more, with the rising circadian wake pressure causing awakening from daytime sleep well before the end of the sleep opportunity. The early awakening leaves a higher level of homeostatic sleep pressure at the end of the shortened sleep period (dark gray) and causes a portion of time available for sleep in this scenario (light gray) to remain unutilized (top right). The combined effect of the two processes—sleepiness calculated as the net difference between the homeostatic pressure for sleep and the circadian pressure for wakefulness—is that sleepiness is low and stable throughout the duty period in the daytime duty scenario (bottom left), whereas sleepiness increases and peaks toward the end of the duty period in the nighttime duty scenario (bottom right). Note that the transient cognitive impairment immediately after awakening known as sleep inertia115 is not depicted in this figure.
By contrast, in a night work schedule, the interplay between the circadian and homeostatic processes produces a steady increase in sleepiness through most of the night. Furthermore, the rising circadian wake drive during daytime sleep causes early awakening and incomplete dissipation of the homeostatic pressure for sleep. High circadian wake drive during the late afternoon and early evening (the so-called “forbidden zone for sleep”134 or “wake maintenance zone”135) makes it difficult to obtain additional sleep during the afternoon. Thus, compared to a day work scenario, a night work scenario tends to produce sustained sleep loss and dynamically changing, higher levels of sleepiness.13
Given this biological regulation of sleepiness and its impact on mental fatigue, a prescriptive limit on work hours would not, by itself, prevent high fatigue levels during a night work schedule. (In fact, a prescriptive limit on work hours could inadvertently place the commute home at the time of greatest sleepiness, just before the rising circadian wake drive would partially reduce sleepiness again and mitigate fatigue.11)
APPENDIX B
Example Risk and Safety Management Policy Frameworks
Shift duration is a safety and health issue with legal implications, and policies and procedures pertaining to shift duration are best embedded within organizational risk and safety management systems.121 Many industries have pre-existing policy frameworks from which to draw, such as workplace health and safety policies, Safety Management System (SMS) policies, or Fatigue Risk Management (FRM) policies. Here we provide a few links to example frameworks and free resources (shared with permission), which may serve as a starting point for organizations to establish their own policies:
• The “Fatigue Risk Management Toolkit for Residents, Leaders, and Policy Makers in Canadian Postgraduate Medical Education” document contains practical tools and an implementation guide for managing fatigue in Canadian medical education. In large part it readily applies to U.S. medical education settings. It can be downloaded from: http://www.residentfatigue.ca/mssites/frm/PDF/Fatigue-Risk-Management-Toolkit-WEB5.pdf (last accessed on March 30, 2021).
• The “FRM Standard Operating Procedure for Utilities” document provides a straightforward but comprehensive standard operating procedure for a fatigue risk management system (FRMS) currently used in Australia. It may be adapted for U.S. operations and can be downloaded from: https://www.sleepresearchsociety.org/wp-content/uploads/2021/03/FRM-Standard-Operating-Procedure-for-Utilities.pdf (last accessed on March 30, 2021).
• The Fatigue Risk Management Systems Implementation Guide for Operators, 1st edition6 developed by the International Air Transport Association (IATA), the International Civil Aviation Organization (ICAO), and the International Federation of Airline Pilots’ Associations (IFALPA) is widely seen as a model for FRMS in larger operations. It can be downloaded from: https://www.icao.int/safety/fatiguemanagement/FRMS%20Tools/FRMS%20Implementation%20Guide%20for%20Operators%20July%202011.pdf (last accessed on March 30, 2021).
• The 2018 Fatigue Risk Management Guidelines for Emergency Medical Services Implementation Guidebook helps EMS administrators with the implementation of rigorously developed, evidence-based guidelines52 for fatigue risk management in EMS, with condensed summaries of recommendations and sample policy statements that may be tailored to the needs of local agencies. It can be downloaded from: https://nasemso.org/wp-content/uploads/Fatigue-Guidebook-FINAL-2018Oct.pdf (last accessed on March 30, 2021).
In addition, the “Fatigue at Work Employer Toolkit” developed by the National Safety Council (NSC) contains educational materials for human resources personnel, supervisors, and employees pertaining to fatigue-related safety risks. It can be downloaded from: https://safety.nsc.org/fatigue-risk-management-toolkit (last accessed on March 30, 2021).
APPENDIX C
Recommendations for the Development of Systems to Monitor the Outcomes of Changes in Shift Duration
After making changes in shift duration, organizations should monitor and respond to leading indicators of potential problems and both positive and negative outcomes to ensure the effectiveness of their shift duration policies. Monitoring systems should identify, report, quantify and manage existing and emerging risks. For the development of such systems, the following recommendations deserve consideration:
-
(1)
The degree (and likely cost) of monitoring should be proportional to the anticipated risk level. Where the risk level is low, monitoring may be relatively minimal. Where the risk level is high, however, monitoring should be more comprehensive, evidence-based and, in larger operations, bolstered by third-party oversight.
-
(2)Monitoring systems should identify and report key performance indicators. These indicators should enable the organization to demonstrate evidence for the following.
-
(a)There is appropriate knowledge of relevant policies, including personal and organizational roles and responsibilities in identifying, reporting, quantifying and mitigating the risks associated with extended shifts.
-
(b)There is appropriate training and education of staff in how to identify, report, quantify and manage the risks associated with extended shifts.
-
(c)Methodologies used for measuring, reporting and mitigating risks are evidence-based, subject to regular evaluation and, where appropriate, modified in light of local experience and/or relevant or emerging scientific evidence. These could include, and are not limited to, measures of:
-
^planned and actual working time arrangements for all at-risk employees, including planned and unplanned overtime, on-call work, secondary employment, or other activities likely to interfere with sleep;
-
^sleep-wake behavior of individual employees, as part of a shared-responsibility framework in which employer and employees have joint responsibility for ensuring adequate sleep;
-
^fatigue/sleepiness-related changes in behavior or task performance;
-
^self-report measures of fatigue, sleepiness, alertness, or fitness-for-duty;
-
^the efficacy and utilization rates of in situ countermeasures at the organizational level.
-
^
-
(a)
-
(3)
Based on data obtained in (2), organizations should respond appropriately to opportunities to apply corrective actions that will reduce risks associated with shift duration.
-
(4)
Monitoring systems should be cost-effective, so that the costs of implementation, or of the application of corrective actions, does not exceed the likely benefits. This guidance should, however, not be interpreted as advice to minimize resources dedicated to monitoring.
-
(5)
Organizations should implement a system that will enable them to identify and respond to any meaningful relationships between shift duration and risk outcomes including, but not limited to, productivity, performance, safety, health, and community and environmental consequences.
APPENDIX D
Background Information on Countermeasures for Risks Associated with Shift Duration
This Appendix provides background information and references that pertain to selected countermeasures for risks associated with shift duration as shown in Table 1. Implementation of these countermeasures can be complex, and consultation with an expert is generally recommended.
D1. Scheduling Improvements for Shift Work and Extended Shift Operations
Thoughtful and data-driven design of working time arrangements can contribute to risk mitigation by maximizing and protecting sleep opportunities, aligning work schedules with the circadian rhythm of the biological clock, and/or increasing time for recovery after extended duties or multiple shifts. While the primary focus of this paper is on shift duration, the timing of shift starts and ends, and other aspects of the working time arrangements are also important to consider in this regard.136,137 Scientific evidence pertaining to these issues is limited, and conclusive studies of scheduling improvements are largely lacking due to a wide range of possible confounds.138 Nonetheless, the following guidelines provide some insight into what kinds of scheduling practices affect performance, safety, and health risks and therefore present potential opportunities for improvement.
• Shift systems with backward rotation, in which the start times of consecutive shifts is advancing (i.e. the next block of shift starts at an earlier time of day than the current block), are generally less well tolerated than shift systems with forward rotation or fixed shift times.81 The speed of rotation (i.e. how many shifts in a block with the same start time) also plays a role in rotating shift systems, but the evidence on its effects is mixed.139
• Both night shifts and early morning starts curtail nighttime sleep opportunities, which increases risk levels relative to late morning and afternoon/evening shifts.77,140
• Shift durations beyond 12 h in duration tend to be associated with increased risk levels.80,140 Shift durations of 24 h or more without protected opportunities to nap while on duty are not recommended.51 Evidence is mixed, however, on 12-h shifts compared to 8-h shifts.51,141
• Risk levels tend to accumulate across consecutive shifts without days off.142,143
• Double (i.e. back-to-back) shifts and quick returns, overtime, and second jobs increase risk levels.22,144,145
• Irregular and unpredictable work hours and on-call duty schedules are often perceived as stressors and may also interfere with the ability to obtain adequate sleep, thereby increasing risk levels.9,146
• Whereas the impact of workload (or task load) is not well established,147,148 high workload may interfere with control over the pacing of work tasks and restrict time for rest breaks, which may increase risk levels.
D2. Napping
Taking a nap—a relatively short sleep period that may be (loosely) defined as less than half the duration of an individual’s typical nocturnal sleep length—is an effective way to supplement the daily amount of sleep and a powerful countermeasure to sleepiness and fatigue.149–153 Naps as short as 15 min and as long as several hours can be effective, whether before work (pre-emptive or prophylactic naps), during work (on-the-job or strategic naps), or after work (catch-up naps).112,154–156 Naps may facilitate adaptation to a shift work schedule and ease the return to daytime activity,157,158 and may offer cardiovascular health benefits.159,160 Split sleep schedules, in which a person takes a nap after a work shift and another nap before the next shift, have been associated with increased sleepiness,161 but few differences in performance relative to a consolidated post-shift sleep bout.162,163 For on-the-job napping to be implemented successfully as a countermeasure strategy, it is important that it be sanctioned164 and that there is access to a safe and quiet place to rest while on break.109,127
Importantly, napping may produce post-nap sleep inertia, a transient feeling of grogginess and impaired performance immediately upon awakening.115,165 Sleep inertia can be particularly problematic in on-call settings146 and may require a worker to delay the return to work for up to about 30 min after waking.166,167 Sleep inertia may be less intense after shorter (approximately 10–30 min) naps, but scientific evidence on this matter is inconclusive.168 Caffeine consumed just prior to a nap appears to be an effective countermeasure to performance impairment due to sleep inertia immediately after the nap.129 (see Appendix D3).
D3. Caffeine Use
There is abundant evidence that caffeine reduces sleepiness and fatigue and mitigates deficits in cognitive performance.116,169 When caffeine is used in conjunction with a nap, it may also reduce the time to overcome post-nap sleep inertia.170–173 Caffeine is widely available and found in many drinks and foods, either naturally occurring or as an additive; furthermore, caffeine can be obtained in the form of chewing gum and various over-the-counter medications. Available evidence suggests that moderate use of caffeine is compatible with a healthy lifestyle.174
The pharmacodynamics of caffeine are poorly understood, and large inter-individual differences in caffeine sensitivity, effectiveness, habituation, and tolerance exist.175–177 This limits the ability to provide tailored advice regarding dosing of caffeine to mitigate fatigue - although given the widespread presence of caffeine in foods and drinks, precise dosing could be difficult in practice regardless. Even so, the preponderance of scientific evidence indicates that caffeine is an effective fatigue countermeasure, and access to caffeine as part of a comprehensive fatigue risk management program is recommended.111
Caffeine present in the bloodstream just before bedtime may delay sleep onset and reduce the quality and quantity of subsequent sleep, although individuals differ considerably in their sensitivity to these effects.178 Sustained use of high-dose caffeine can cause additional undesirable effects, including anxiety, tremor, arrhythmias, insomnia, dehydration, and withdrawal headaches.179,180 For healthy adults, caffeine consumption up to about 400 mg per day (300 mg per day in pregnant women) is generally considered safe;181 however, the decision to use caffeine and the amount and frequency of use should be based on individual assessment of benefits versus undesirable side effects.
D4. Sleep Hygiene and Treatment of Sleep Disorders
Sleep disturbances that are not necessarily related to the work environment contribute to work-related errors and injuries.182 Sleep hygiene, which refers to a set of behavioral and environmental recommendations intended to promote good sleep,183 can help to obtain adequate duration of quality sleep. The recommended amount of sleep for the average adult is 7 h per night or more.105,106 Achieving this on a regular basis provides some degree of resilience against the adverse cognitive effects of subsequent sleep loss.184,185
Sleep hygiene environmental recommendations, which pertain to personal sleep spaces as well as any workplace sleep facilities, include ensuring a comfortable, appropriately sized bed; minimal light exposure and noise; comfortable temperature and humidity; and no sleep interruptions (unless there is an emergency).186,187 Sleep hygiene behavioral recommendations found in the literature, which are primarily focused on the habitual sleeping environment, include maintaining regular bed and wake times; avoiding daytime naps; avoiding bright light exposure during the 2–3 h prior to sleep; avoiding large meals or alcohol consumption for at least 2 h prior to bedtime; avoiding strenuous exercise immediately before bedtime; and avoiding caffeine, nicotine, and other stimulants for at least 6 h before bedtime.187,188
In operational settings, some or all of the behavioral recommendations may not be feasible or practical to implement (e.g. because irregular work schedules may interfere with maintaining regular bed and wake time) and may actually be at odds with effective fatigue risk management (e.g. because taking a daytime nap may be needed to mitigate fatigue). That is, some of the behavioral recommendations could be counterproductive for getting enough sleep or ensuring optimal performance and safety (especially in shift work settings). Also, although they are worthy sleep health recommendations in their own right, evidence of their effectiveness with regard to workplace performance, safety and health is limited.188 The behavioral recommendations should therefore not be seen as advice against pursuing catch-up sleep or naps, or using bright light or caffeine prior to bedtime, when doing so would be the better choice for safety.
Sleep disorders (e.g. obstructive sleep apnea, insomnia), medical conditions (e.g. diabetes mellitus, gastroesophageal reflux disease, back pain), and psychiatric disorders (e.g. depression, post-traumatic stress disorder) can transiently or chronically reduce the quality and quantity of sleep.189 For affected workers this can result in poor sleep quality, insufficient sleep, or excessive sleepiness, which can then negatively affect work performance. Additionally, some medications (e.g. hypnotics, antidepressants) incur side-effects that contribute to increased risk of fatigue during work hours, either through direct effects on sleepiness, or indirectly by worsening sleep quality or decreasing sleep duration.190 Workplace education regarding sleep disorders, treatment, and implications for safety and well-being has been found to reduce risk of occupational injuries.191 Furthermore, an employer-supported sleep disorder (obstructive sleep apnea) treatment program in the U.S. trucking industry has been shown to yield significant benefits in terms of crash risk, driver retention, and medical insurance costs.192,193
D5. Wake- and Sleep-Promoting Medications
Wake-promoting (stimulant) and sleep-promoting (hypnotic) medications should be used in consultation with and under supervision of a medical provider with expertise in management of sleep/wake disturbance associated with non-traditional work hours. A discussion of their pharmacological and clinical specifications is beyond the scope of this paper but can be found in the literature.194,195 The advantages and disadvantages of wake- and sleep-promoting medications and the legal and ethical considerations for their use in operational settings have also been discussed in the literature.123,196 Certain occupations have regulations or policies that prohibit the use of some or all of these medications.
Use of wake-promoting medications may interfere with the ability to obtain adequate sleep after bedtime.197 Use of sleep- promoting medications may result in next-day residual sedation, which could impair performance while at work or commuting to work,198 although caffeine intake may be helpful to mitigate this effect.199 Long-term use of wake- or sleep-promoting medications may have unintended effects on sleep, mood, and health.195,200 Interactions with other medications or with alcohol201 may increase the risk of side effects from wake- or sleep promoting medications. Alcohol, which some individuals use as a sleep aid, may degrade sleep quality, exacerbate sleep apnea, and cause next-day sleepiness.202
Melatonin, which in the United States is available over the counter as a dietary supplement, is usually marketed and used as a sleep aid. However, the primary effect of melatonin—a hormone that is also naturally produced by the pineal gland during the evening and night—is that it can shift the timing of the biological clock.203 As such, melatonin may be used to help realign sleep-wake timing and facilitate daytime sleep for night shift workers204 or to help overcome jet lag after travel across time zones.205 Optimizing the timing of melatonin administration is critical to achieving the desired effect, with morning administration leading to delays of the biological clock (shifting sleep later) and evening administration leading to advances of the biological clock (shifting sleep earlier).206 This makes achieving optimal effectiveness complicated in practice, and mistimed melatonin administration may even result in the opposite effect of what is desired. Melatonin use is generally considered safe and side effects are minimal,207 but it is not regulated in the United States and may contain additives with adverse health effects. As with other sleep-promoting medications, a medical provider with expertise in management of sleep/wake disturbance associated with non-traditional work hours should be consulted if melatonin is considered as a potential aid for sleep difficulties in the context of working time arrangements.
D6. Bright or Blue Light Exposure
Light has the potential to shift the biological clock, and it also affects alertness.208 Morning light exposure causes the biological clock to advance (shift earlier), and evening light exposure causes the clock to delay (shift later).209,210 The magnitude of these effects depends on the duration, brightness, and color of light exposure. The brighter the light and the longer the exposure, the greater the shifting,211,212 and light that is blue or blue-enriched is particularly effective for shifting the biological clock.213 Based on these principles, manipulation of light exposure can be used to shift the biological clock by some desired amount of time, for example to facilitate adaptation to a shift work schedule.214 Optimizing the timing of light exposure is critical to achieving the desired effect.208
The biological clock tends to shift no more than a few hours per day. This approach to shift work adaptation would therefore only work well for fixed or slowly rotating shift schedules, in which shift start or end times are expected to occur at approximately the same time for several consecutive days. Even then, additional measures may be required, such as wearing dark goggles or using technological solutions to reduce bright or blue light exposure at certain times,215 making the desired effect difficult to achieve.216 Strategies for mitigating risks in shift workers that rely on minimization of extended wakefulness and sleep loss, rather than shifting the biological clock, may be more effective in practice.
Light exposure has an acute alerting effect.217 To some extent the magnitude of this effect depends on the brightness level of the light,218 and light that is blue or blue-enriched is particularly effective for promoting alertness.219 Little is known about how long the alerting effect of light exposure lasts after the exposure has ended.220 That said, use of blue- enriched white light in the workplace has been reported to improve alertness, performance, and sleep quality.221 The acute alerting effect of light, however, cannot be separated from its effects on the biological clock. Especially in shift work settings, therefore, individuals exposed to bright or blue light to improve alertness may also experience a shift of the biological clock, which may or may not be problematic depending on the situation. Furthermore, inappropriate light exposure has the potential to adversely affect sleep. In many situations, therefore, light may not be a suitable countermeasure for risks associated with shift duration.
Exposure to light at night associated with shift work has been found to increase the risk of cancer.222–224 Additionally, chronic exposure to bright or blue light therapy has been linked to retinal damage later in life.225,226 This finding awaits corroboration with additional clinical studies.
D7. Exercise and Activity Breaks
In addition to the well-known benefits of physical activity from exercise and activity breaks with regard to skeletomuscular and overall health and wellness, physical activity has some potential to improve sleep.227,228 However, exercise less than 1 h before bedtime may delay sleep onset.229 Exercise also has the potential to shift the biological clock, with morning exercise facilitating advances and evening exercise facilitating delays of the biological clock.230 In the laboratory, nightly bouts of exercise have been found to promote adjustment of the biological clock to a night shift schedule.231
During sleep deprivation, physical activity may produce a modest short-term reduction in subjective sleepiness, but there may not be any concomitant improvement in cognitive performance.232 A review of continuous exercise at active workstations found minimal evidence for increased workplace performance or productivity.233 The extent to which exercise can be used effectively as a fatigue or risk countermeasure in operational settings remains to be investigated.
D8. Fatigue Prediction, Detection and Warning Technologies
Technologies available to help manage risks from fatigue can be broadly categorized as biomathematical models of fatigue,234 tools for monitoring sleep and sleep debt,235 tools for detecting and warning about fatigue,236 and fitness-for-duty tests.237 Biomathematical models of fatigue make use of equations describing the regulation of sleep and wakefulness and the biological clock to provide predictions of sleepiness or performance impairment for a (hypothetical) average individual, based on a given sleep schedule or work schedule.238,239 Use of these models is commonplace before, during and after duty periods in commercial and military aviation,240,241 where shift scheduling is typically tightly managed. However, they are deemed to be of more limited utility in settings where shift scheduling is on demand or otherwise less strictly under operational control.242
Tools for monitoring sleep have become widely available in the consumer market over the last decade. Frequently integrated with physical activity and health monitoring systems, they usually consist of wearable sensors coupled with a smartphone-based software application.243 Such tools do not usually meet professionally accepted criteria for sleep assessment,244 but have been found helpful in allowing individuals to monitor and potentially improve their sleep245 or potentially seek medical evaluation. Tools for monitoring sleep may also serve to determine a person’s sleep schedule for use with a biomathematical model of fatigue in order to predict impending safety risks.246 A significant challenge with wearable technologies is user acceptability; people often do not tolerate wearing additional devices, especially if they are uncomfortable or obtrusive, interfere with work, or do not also fulfill other useful functions.247
Tools for detecting and warning about fatigue, commonly referred to as fatigue (or drowsiness) detection and warning systems, are manifold and diverse. Technologies for fatigue detection aim generally to measure fatigue continuously from unobtrusively observable signals that correlate with fatigue, such as various ocular measures, sleepiness-related variables derived from the electroencephalogram (EEG), indices of heart rate variability, changes in speech and voice, or facial expressions. A diversity of modalities for providing fatigue warnings have been implemented, including visual, auditory, and haptic alerts as well as warning messages transmitted to third parties for possible intervention. In cars and trucks, fatigue and error detection systems may activate driver assist technologies to help avoid accidents.69
In contrast to fatigue detection and warning systems, tests for fitness-for-duty (or readiness-to-perform) typically provide snapshot measures of fatigue and often require an individual’s active involvement such as performing a reaction time task248 or taking a balance test.249 While fatigue testing for fitness- for-duty provides an instant, objective estimate of a person’s level of fatigue, such testing does not track subsequent changes in fatigue over time unless the test is conducted repeatedly (although such changes could conceivably be predicted using a biomathematical model). Most fitness-for-duty tests are not specific for fatigue; other sources of impairment (e.g. distraction, alcohol intoxication) produce similar test results. For fitness-for- duty tests that rely on user response to assess fatigue, variations in motivation and effort may also influence test results.
Fatigue prediction, detection and warning technologies that have been shown to be both sensitive and specific to relevant levels of fatigue are rare. However, both of these accuracy attributes are important. Technologies need to be sensitive enough to detect or predict levels of fatigue that compromise performance and safety, as failures to identify these could have critical, even fatal consequences. At the same time, technologies need to be specific enough not to inadvertently trigger alerts when fatigue levels are low, as too many false alarms will quickly desensitize the user. Many of the currently available technologies are proprietary, and the extent to which they have been subjected to independent research is often limited. For most of these technologies, publicly accessible data on accuracy, reliability, and validity are limited or unavailable.
Collection of objective data in operational settings may have important implications for privacy and could carry liability for employers and employees. For example, following an accident in which fatigue is suspected to be a main contributor, sleep monitoring data may be subpoenaed to determine the amount of sleep obtained prior to the accident. This potential issue notwithstanding, when used as part of a comprehensive fatigue risk management system, fatigue prediction, detection and warning technologies may contribute to a worthwhile, data- driven process of continuous improvements in risk mitigation (see Appendix D9).
D9. Risk Mitigation Tools, Policies, and Practices
Even though shift duration and its attendant fatigue may be the source of risks to performance, safety, and health, countermeasures do not necessarily have to address the source of these risks to mitigate the risks themselves.70 There are many possibilities for “fatigue proofing” that mitigate or avoid risks through other means,250 such as use of task checklists and standard operating procedures (e.g. for end-of-shift hand-offs),5 team work strategies,29 extra staffing,144 scheduled rest breaks,81 providing safe transportation options after work shifts,251 engineering solutions (e.g. safety valves in factories, rumble strips on the road, automation in the operation of machines),5 and implementation of safety policies, procedures, and management systems23 (see also Appendix B). Furthermore, an educated workforce is a key component of risk mitigation. Fatigue risk management training should help workers, their managers, and other operational personnel (e.g. scheduling, human resources) understand how to manage work, sleep, and the application of countermeasures in order to maximize performance, safety, and health.122
Fatigue risk management training and other risk mitigation strategies may be incorporated into a fatigue risk management system (FRMS), which is a proactive, data-driven process whereby an organization undertakes a formal risk management approach to reducing the effects of fatigue in the workplace.121,252 An FRMS program involves all stakeholders (workers, management, unions, regulators), includes proactive data collection steps, and adapts to dynamically changing risks so as to be self-improving. The implementation of a FRMS is unique to the needs of a given industry and company, but the elements of FRMS programs are similar across industries (see also Appendix B). A FRMS is often embedded within a larger safety management system (SMS) to allow for integrated risk management. FRMS program managers are typically responsible for developing and implementing policies designed to mitigate fatigue-related risks (e.g. scheduling and rest requirements, and countermeasure use), investigating fatigue-related incidents and accidents, monitoring safety performance indicators, evaluating the impact of work schedules on performance and safety, providing mechanisms for individuals to report fatigue at work, providing recommendations for modifying schedules to improve fatigue-related outcomes, and providing regular training and resources to employees on best practices for managing work, sleep, and the application of countermeasures.121,124
DISCLOSURE STATEMENT
Financial Disclosure: The development of this paper was supported by the American Academy of Sleep Medicine (AASM) and the Sleep Research Society. Mr. Carandang and Ms. Kazmi are employed by the AASM. Mr. Heald was employed by the AASM during his work on this paper through July 2020. Dr Gurubhagavatula is the course director of the AASM Sleep Medicine Essentials Course (September 2021). She received a research grant from the AASM Foundation to study sleep apnea in law enforcement officers. She received royalties from UptoDate, Inc. for writing the article, “Drowsy driving: Risks, evaluation, and management.” Dr Barger served as a consultant for Boston Children’s Hospital and the University of Helsinki. She received research funding from Delta Airlines. Dr Boivin is the Founder and CEO of Alpha Logik Consultants Inc., a privately-owned small company that provides conferences and consultations on sleep and fatigue related issues. She served as a consultant for the following: Sunovion, Valéro, Merck Pharmaceutical, Canadian Space Agency, Rio Tinto, Comité Patronal de Négociation du Secteur de la Santé et des Services Sociaux (CPNSSS), Laurentian Pilotage Authority, Bel-Air Aviation, Mines Canadian Malartic, Canadian National, Aéroport de Montréal, Ministère des Transports du Québec. She received research contracts from Transport Canada, Société de l’Assurance automobile du Québec, NAV Canada Innovation Maritime, and Air Canada. Dr Dawson served as a consultant for LITA, Treasury Wine Estate, Energy Queensland, North Power, AngloAmerican, Z Energy, Zeroharm, PTA, BMA, Napier Port, and Lyttelton Port Company, and for workshops on shift work/ fatigue. He received research funding from Svitzer. Dr Drake served as a consultant for Eisai Inc., Jazz Pharmaceuticals, and Harmony Biosciences. He served as a speaker and a member of the speaker’s bureau for Merck, Inc. and Harmony Biosciences. He received research funding from Eisai Inc., Suven Life Sciences, Takeda Pharmaceuticals, Jazz Pharmaceuticals, Merck, Inc., and Procter & Gamble. Dr Flynn-Evans has a financial interest in Baby Sleep Science, a parent coaching company. Dr Mysliwiec has been contracted to serve as a speaker for Springer Healthcare LLC and Jazz Pharmaceuticals. He served as a consultant for CPAP Medical, Bluegrass Oxygen, NOCTEM, Sleep Care Inc., Ebb Therapeutics, and Nightware. Dr Samuels is the President and CEO of the Center for Sleep & Human Performance, and the sole owner of an online fatigue management training program for law enforcement. He currently serves as a consultant for Red Bull International, The Royal Canadian Mounted Police, FitGMR Ltd., Eisai Inc., Sunovian Pharmaceuticals, and Jazz Pharmaceuticals. He received research equipment donated from Cerebra Health Ltd. Dr Van Dongen serves as a consultant for Jazz Pharmaceuticals. He received research funding from Federal Express Corporation, Jazz Pharmaceuticals, and Mars Wrigley Confectionary. Non-financial Disclosure: Dr Basner is the President of the International Commission of Biological Effects of Noise (ICBEN). Dr Boivin received non-financial support from PPRS SAS. She provides expert opinion on clinical cases involving patients with circadian rhythm disorders. Dr Patterson served on the Board of Directors of the National Association of EMS Physicians. He is currently serving on the Board of Directors of the Pittsburgh Emergency Medicine Foundation. Dr Samuels is the Past President of the Canadian Sleep Society. He serves on the Board of Directors/Advisors for Cerebra Health Ltd, FitGMR Ltd, Eisai Inc., Sunovion Pharmaceuticals, and Jazz Pharmaceuticals.
COPYRIGHT STATEMENT
This article has been co-published with permission in JOURNAL OF CLINICAL SLEEP MEDICINE and SLEEP®. All rights reserved in respect of JOURNAL OF CLINICAL SLEEP MEDICINE, © American Academy of Sleep Medicine, and in respect of SLEEP®, © Sleep Research Society. The articles are identical except for minor differences in keeping with each journal's style. Either citation can be used when citing this article. Permission for reuse or republication can be obtained through Copyright Clearance Center.
REFERENCES
- 1. Skeiky L, et al . Circadian rhythms in sleepiness, alertness, and performance . In: Kryger MH, Roth T, Dement WC , eds. Principles and Practice of Sleep Medicine. 7th ed. Philadelphia: : Elsevier; , in press. . [Google Scholar]
- 2. Pigeon WR, et al . Distinguishing between excessive daytime sleepiness and fatigue: toward improved discovery and treatment . J Psychosom Res. 2003. ; 54 ( 1 ): 61 – 69 . [DOI] [PubMed] [Google Scholar]
- 3. Shen J, et al . Distinguishing sleepiness and fatigue: focus on definition and measurement . Sleep Med Rev. 2006. ; 10 ( 1 ): 63 – 76 . [DOI] [PubMed] [Google Scholar]
- 4. Åkerstedt T . Consensus statement: fatigue and accidents in transport operations . J Sleep Res. 2000. ; 9 ( 4 ): 395 . [DOI] [PubMed] [Google Scholar]
- 5. Satterfield BC, et al . Occupational fatigue, underlying sleep and circadian mechanisms, and approaches to fatigue risk management . Fatigue Biomed Health Behav 2013. ; 1 : 118 – 136 . [Google Scholar]
- 6. IATA , ICAO, IFALPA . Fatigue Risk Management Systems Implementation Guide for Operators. 1st ed . 2011. . https://www.icao.int/safety/fatiguemanagement/FRMS%20Tools/FRMS%20Implementation%20Guide%20for%20Operators%20July%202011.pdf (last accessed on March 30, 2021). [Google Scholar]
- 7. Van Dongen HPA, et al . Alertness level . In: Binder MD, Hirokawa N, Windhorst U , eds. Encyclopedia of Neuroscience. Berlin: : Springer; , 2008. : 75 – 77 . [Google Scholar]
- 8. Wong IS, et al . International consensus statements on non-standard working time arrangements and occupational health and safety . Ind Health. 2019. ; 57 ( 2 ): 135 – 138 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arlinghaus A, et al . Working time society consensus statements: evidence-based effects of shift work and non-standard working hours on workers, family and community . Ind Health. 2019. ; 57 ( 2 ): 184 – 200 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moreno CRC, et al . Working time society consensus statements: evidence-based effects of shift work on physical and mental health . Ind Health. 2019. ; 57 ( 2 ): 139 – 157 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Honn KA, et al . Working time society consensus statements: prescriptive rule sets and risk management-based approaches for the management of fatigue-related risk in working time arrangements . Ind Health. 2019. ; 57 ( 2 ): 264 – 280 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mackworth NH . Researches on the Measurement of Human Performance . Medical Research Council Special Report Series. London: : Privy Council; , 1950. . [Google Scholar]
- 13. Åkerstedt T . Work hours, sleepiness and the underlying mechanisms . J Sleep Res. 1995. ; 4 ( S2 ): 15 – 22 . [DOI] [PubMed] [Google Scholar]
- 14. Johnson JV, et al . Long working hours, occupational health and the changing nature of work organization . Am J Ind Med. 2006. ; 49 ( 11 ): 921 – 929 . [DOI] [PubMed] [Google Scholar]
- 15. Burke RJ, et al . The Long Work Hours Culture: Causes , Consequences and Choices. 1st ed. Bingley: : Emerald Group Publishing; ; 2008. [Google Scholar]
- 16.US Bureau of Labor Statistics. Job flexibilities and work schedules summary. 2019, https://www.bls.gov/news.release/flex2.nr0.htm (last accessed on March 30, 2021).
- 17.US Bureau of Labor Statistics. Labor force statistics from the Current Population Survey. 2020, https://www.bls.gov/cps/lfcharacteristics.htm#hours (last accessed on March 30, 2021).
- 18. Belzer MH . The economics of long work hours: how economic incentives influence workplace practice . Ind Health. 2020. ; 58 ( 5 ): 399 – 402 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McMenamin T . A time to work: recent trends in shift work and flexible schedules . Monthly Labor Rev . 2007. ; 130 ( 12 ): 3 – 15 . [Google Scholar]
- 20. Shockey TM, et al . Short sleep duration by occupation group – 29 states, 2013–2014 . Morbid Mortal Weekly Rep . 2017. ; 66 ( 8 ): 207 – 213 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Basner M, et al . Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep . Sleep. 2014. ; 37 ( 12 ): 1889 – 1906 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Marucci-Wellman HR, et al . Differences in time use and activity patterns when adding a second job: implications for health and safety in the United States . Am J Public Health . 2014. ; 104 ( 8 ): 1488 – 1500 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wong IS, et al . Working Time Society consensus statements: a multi-level approach to managing occupational sleep- related fatigue . Ind Health . 2019. ; 57 ( 2 ): 228 – 244 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Riedy S, et al . Fatigue and short-term unplanned absences among police officers . Policing . 2020. ; 43 ( 3 ): 483 – 494 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Harrison Y, et al . The impact of sleep deprivation on decision making: a review . J Exp Psychol Appl . 2000. ; 6 ( 3 ): 236 – 249 . [DOI] [PubMed] [Google Scholar]
- 26. Ricci JA, et al . Fatigue in the U.S. workforce: prevalence and implications for lost productive work time . J Occup Environ Med . 2007. ; 49 ( 1 ): 1 – 10 . [DOI] [PubMed] [Google Scholar]
- 27. Landrigan CP, et al . Effect of reducing interns’ work hours on serious medical errors in intensive care units . N Engl J Med . 2004. ; 351 ( 18 ): 1838 – 1848 . [DOI] [PubMed] [Google Scholar]
- 28. Fischer FM, et al . Working Time Society consensus statements: psychosocial stressors relevant to the health and wellbeing of night and shift workers . Ind Health . 2019. ; 57 ( 2 ): 175 – 183 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Banks S, et al . Effects of fatigue on teams and their role in 24/7 operations . Sleep Med Rev . 2019. ; 48 : 101216 . [DOI] [PubMed] [Google Scholar]
- 30. Killgore WDS . Effects of sleep deprivation on cognition . Prog Brain Res . 2010. ; 185 : 105 – 129 . [DOI] [PubMed] [Google Scholar]
- 31. Barnes CM, et al . Lack of sleep and unethical behavior . Organ Behav Hum Decis Proc . 2011. ; 115 : 169 – 180 . [Google Scholar]
- 32. Estryn-Béhar M, et al .; NEXT Study Group . Effects of extended work shifts on employee fatigue, health, satisfaction, work/family balance, and patient safety . Work . 2012. ; 41 Suppl 1: 4283 – 4290 . [DOI] [PubMed] [Google Scholar]
- 33. Bell LB, et al . Effects of 13-hour 20-minute work shifts on law enforcement officers’ sleep, cognitive abilities, health, quality of life, and work performance: the Phoenix Study . Police Q . 2015. ; 18 ( 3 ): 293 – 337 . [Google Scholar]
- 34. Bazazan A, et al . Fatigue as a mediator of the relationship between quality of life and mental health problems in hospital nurses . Accid Anal Prev . 2019. ; 126 : 31 – 36 . [DOI] [PubMed] [Google Scholar]
- 35. Williamson A, et al . The link between fatigue and safety . Accid Anal Prev . 2011. ; 43 ( 2 ): 498 – 515 . [DOI] [PubMed] [Google Scholar]
- 36. Good CH, et al . Sleep in the United States Military . Neuropsychopharmacology . 2020. ; 45 ( 1 ): 176 – 191 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dembe AE, et al. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States . Occup Environ Med . 2005. ; 62 ( 9 ): 588 – 597 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wagstaff AS, et al . Shift and night work and long working hours—a systematic review of safety implications . Scand J Work Environ Health . 2011. ; 37 ( 3 ): 173 – 185 . [DOI] [PubMed] [Google Scholar]
- 39. Dawson D, et al . How much sleep do you need? A comprehensive review of fatigue related impairment and the capacity to work or drive safely . Accid Anal Prev . 2021. ; 151 : 105955 . [DOI] [PubMed] [Google Scholar]
- 40. Barger LK, et al .; Harvard Work Hours, Health, and Safety Group. Extended work shifts and the risk of motor vehicle crashes among interns . N Engl J Med . 2005. ; 352 ( 2 ): 125 – 134 . [DOI] [PubMed] [Google Scholar]
- 41. Mitler MM, et al . Catastrophes, sleep, and public policy: consensus report. Sleep . 1988. ; 11 ( 1 ): 100 – 109 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Dinges DF . An overview of sleepiness and accidents . J Sleep Res . 1995. ; 4 ( S2 ): 4 – 14 . [DOI] [PubMed] [Google Scholar]
- 43. Rivera AS, et al . Shift work and long work hours and their association with chronic health conditions: a systematic review of systematic reviews with meta-analyses . PLoS One . 2020. ; 15 ( 4 ): e0231037 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Caruso CC, et al . Long working hours, safety, and health: toward a National Research Agenda . Am J Ind Med . 2006. ; 49 ( 11 ): 930 – 942 . [DOI] [PubMed] [Google Scholar]
- 45. Rosekind MR . Underestimating the societal costs of impaired alertness: safety, health and productivity risks . Sleep Med . 2005. ; 6 Suppl 1 : S21 – S25 . [DOI] [PubMed] [Google Scholar]
- 46. Price JM, et al . A method for applying fatigue science to accident investigation . Rev Hum Factors Ergon . 2015. ; 10 : 79 – 114 . [Google Scholar]
- 47. Dawson D, et al . Determining the likelihood that fatigue was present in a road accident: a theoretical review and suggested accident taxonomy . Sleep Med Rev . 2018. ; 42 : 202 – 210 . [DOI] [PubMed] [Google Scholar]
- 48. Dijk DJ, et al . Circadian and sleep/wake dependent aspects of subjective alertness and cognitive performance . J Sleep Res . 1992. ; 1 ( 2 ): 112 – 117 . [DOI] [PubMed] [Google Scholar]
- 49. Gander PH . Evolving regulatory approaches for managing fatigue risk in transportation operations . Rev Hum Factors Ergon . 2015. ; 10 : 253 – 271 . [Google Scholar]
- 50. Flynn-Evans EE, et al .; American Academy of Sleep Medicine Public Safety Committee . Industrial regulation of fatigue: lessons learned from aviation . J Clin Sleep Med . 2019. ; 15 ( 4 ): 537 – 538 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Patterson PD, et al . Shorter versus longer shift durations to mitigate fatigue and fatigue-related risks in emergency medical services personnel and related shift workers: a systematic review . Prehosp Emerg Care . 2018. ; 22 ( Suppl 1 ): 28 – 36 . [DOI] [PubMed] [Google Scholar]
- 52. Patterson PD, et al . Evidence-based guidelines for fatigue risk management in emergency medical services . Prehosp Emerg Care . 2018. ; 22 ( Suppl 1 ): 89 – 101 . [DOI] [PubMed] [Google Scholar]
- 53. Lee S, et al . Working Time Around the World: Trends in Working Hours, Laws and Policies in a Global Comparative Perspective. . Geneva: : International Labour Office; ; 2007. . [Google Scholar]
- 54. Gärtner J, et al . Working Time Society consensus statements: regulatory approaches to reduce risks associated with shift work-a global comparison . Ind Health . 2019. ; 57 ( 2 ): 245 – 263 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kecklund G, et al . Health consequences of shift work and insufficient sleep . BMJ . 2016. ; 355 : i5210 . [DOI] [PubMed] [Google Scholar]
- 56. Grandou C, et al . The effects of sleep loss on military physical performance . Sports Med . 2019. ; 49 ( 8 ): 1159 – 1172 . [DOI] [PubMed] [Google Scholar]
- 57. Jackson ML, et al . Deconstructing and reconstructing cognitive performance in sleep deprivation . Sleep Med Rev . 2013. ; 17 ( 3 ): 215 – 225 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Barnes CM, et al . Too tired to inspire or be inspired: sleep deprivation and charismatic leadership . J Appl Psychol . 2016. ; 101 ( 8 ): 1191 – 1199 . [DOI] [PubMed] [Google Scholar]
- 59. Maia Q, et al . Short and long sleep duration and risk of drowsy driving and the role of subjective sleep insufficiency . Accid Anal Prev . 2013. ; 59 : 618 – 622 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Caldwell JA, et al . Fatigue and its management in the workplace . Neurosci Biobehav Rev . 2019. ; 96 : 272 – 289 . [DOI] [PubMed] [Google Scholar]
- 61. Borbély AA, et al . Sleep homeostasis and models of sleep regulation . J Biol Rhythms. . 1999. ; 14 ( 6 ): 557 – 568 . [DOI] [PubMed] [Google Scholar]
- 62. Van Dongen HPA, et al . Sleep, circadian rhythms, and psychomotor vigilance . Clin Sports Med . 2005. ; 24 ( 2 ): 237 – 49 , vii. [DOI] [PubMed] [Google Scholar]
- 63. Basner M, et al . American time use survey: sleep time and its relationship to waking activities. Sleep . 2007. ; 30 ( 9 ): 1085 – 1095 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Shattuck NL, et al . Does the quality of life differ for shift workers compared to day workers? Chronobiol Int . 2020. ; 37 ( 9 – 10 ): 1299 – 1303 . [DOI] [PubMed] [Google Scholar]
- 65. Belenky G, et al . Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study . J Sleep Res . 2003. ; 12 ( 1 ): 1 – 12 . [DOI] [PubMed] [Google Scholar]
- 66. Van Dongen HPA, et al . The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep . 2003. ; 26 ( 2 ): 117 – 126 . [DOI] [PubMed] [Google Scholar]
- 67. Grech MR, et al . An examination of the relationship between workload and fatigue within and across consecutive days of work: is the relationship static or dynamic? J Occup Health Psychol . 2009. ; 14 ( 3 ): 231 – 242 . [DOI] [PubMed] [Google Scholar]
- 68. Åkerstedt T, et al . Do sleep, stress, and illness explain daily variations in fatigue? A prospective study . J Psychosom Res . 2014. ; 76 ( 4 ): 280 – 285 . [DOI] [PubMed] [Google Scholar]
- 69. Sparrow AR, et al . Drowsiness measures for commercial motor vehicle operations . Accid Anal Prev . 2019. ; 126 : 146 – 159 . [DOI] [PubMed] [Google Scholar]
- 70. Dawson D, et al . Safety implications of fatigue and sleep inertia for emergency services personnel . Sleep Med Rev . 2021. ; 55 : 101386 . [DOI] [PubMed] [Google Scholar]
- 71. Baron KG, et al . Circadian misalignment and health . Int Rev Psychiatry . 2014. ; 26 ( 2 ): 139 – 154 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Boivin DB, et al . Impacts of shift work on sleep and circadian rhythms . Pathol Biol (Paris ). 2014. ; 62 ( 5 ): 292 – 301 . [DOI] [PubMed] [Google Scholar]
- 73. James SM, et al . Shift work: disrupted circadian rhythms and sleep-implications for health and well-being . Curr Sleep Med Rep . 2017. ; 3 ( 2 ): 104 – 112 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Soccolich SA, et al . An analysis of driving and working hour on commercial motor vehicle driver safety using naturalistic data collection . Accid Anal Prev . 2013. ; 58 : 249 – 258 . [DOI] [PubMed] [Google Scholar]
- 75. Van Dongen HPA, et al . The efficacy of a restart break for recycling with optimal performance depends critically on circadian timing . Sleep . 2011. ; 34 ( 7 ): 917 – 929 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Sparrow AR, et al . Naturalistic field study of the restart break in US commercial motor vehicle drivers: truck driving, sleep, and fatigue . Accid Anal Prev . 2016. ; 93 : 55 – 64 . [DOI] [PubMed] [Google Scholar]
- 77. Flynn-Evans EE, et al . Sleep and neurobehavioral performance vary by work start time during non-traditional day shifts. Sleep Health . 2018. ; 4 ( 5 ): 476 – 484 . [DOI] [PubMed] [Google Scholar]
- 78. Muecke S . Effects of rotating night shifts: literature review . J Adv Nurs . 2005. ; 50 ( 4 ): 433 – 439 . [DOI] [PubMed] [Google Scholar]
- 79. Sallinen M, et al . Shift work, sleep, and sleepiness - differences between shift schedules and systems . Scand J Work Environ Health . 2010. ; 36 ( 2 ): 121 – 133 . [DOI] [PubMed] [Google Scholar]
- 80. Dall’Ora C, et al . Characteristics of shift work and their impact on employee performance and wellbeing: a literature review . Int J Nurs Stud . 2016. ; 57 : 12 – 27 . [DOI] [PubMed] [Google Scholar]
- 81. Williamson A, Friswell R . Fatigue in the workplace: causes and countermeasures. Fatigue Biomed Health Behav. 2013. ; 1 : 81 – 98 . [Google Scholar]
- 82. Folkard S, et al . Shift work, safety and productivity . Occup Med (Lond ). 2003. ; 53 ( 2 ): 95 – 101 . [DOI] [PubMed] [Google Scholar]
- 83. Kandelaars KJ, et al . The impact of extended leave on sleep and alertness in the Australian rail industry. Ind Health . 2005. ; 43 ( 1 ): 105 – 113 . [DOI] [PubMed] [Google Scholar]
- 84. van den Berg TI, et al . The effects of work-related and individual factors on the Work Ability Index: a systematic review . Occup Environ Med . 2009. ; 66 ( 4 ): 211 – 220 . [DOI] [PubMed] [Google Scholar]
- 85. Henderson A . Emotional labor and nursing: an under-appreciated aspect of caring work . Nurs Inq . 2001. ; 8 ( 2 ): 130 – 138 . [DOI] [PubMed] [Google Scholar]
- 86. Honn KA, et al . Fatiguing effect of multiple take-offs and landings in regional airline operations . Accid Anal Prev . 2016. ; 86 : 199 – 208 . [DOI] [PubMed] [Google Scholar]
- 87. Arsintescu L, et al . The relationship between workload, performance and fatigue in a short-haul airline . Chronobiol Int . 2020. ; 37 ( 9 – 10 ): 1492 – 1494 . [DOI] [PubMed] [Google Scholar]
- 88. Jackson JE, et al . Fatigue in highway construction workers: Risks and countermeasures in rapid renewal project schedules . Transp Res Rec . 2013. ; 2347 : 11 – 18 . [Google Scholar]
- 89. Dekker S . Just Culture: Balancing Safety and Accountability . 2nd ed. Burlington: Ashgate Publishing: , 2008. . [Google Scholar]
- 90. Briner RB . Relationships between work environments, psychological environments and psychological well-being . Occup Med (Lond ). 2000. ; 50 ( 5 ): 299 – 303 . [DOI] [PubMed] [Google Scholar]
- 91. Dawson D, et al . Fatigue-proofing: a new approach to reducing fatigue-related risk using the principles of error management . Sleep Med Rev . 2012. ; 16 ( 2 ): 167 – 175 . [DOI] [PubMed] [Google Scholar]
- 92. Higgins JS, et al . Asleep at the wheel - the road to addressing drowsy driving . Sleep . 2017. ; 40 : zsx001 . [DOI] [PubMed] [Google Scholar]
- 93. Matsangas P, et al . Sleep quality, occupational factors, and psychomotor vigilance performance in U.S. Navy sailors. Sleep . 2020. ; 43 : zsaa118 . [DOI] [PubMed] [Google Scholar]
- 94. Petrov ME, et al . Commuting and sleep: results from the Hispanic community health study/study of Latinos Sueño ancillary study . Am J Prev Med . 2018. ; 54 ( 3 ): e49 – e57 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Ritonja J, et al . Working Time Society consensus statements: individual differences in shift work tolerance and recommendations for research and practice. Ind Health . 2019. ; 57 ( 2 ): 201 – 212 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Kerkhof GA . Inter-individual differences in the human circadian system: a review . Biol Psychol . 1985. ; 20 ( 2 ): 83 – 112 . [DOI] [PubMed] [Google Scholar]
- 97. Vetter C, et al . Aligning work and circadian time in shift workers improves sleep and reduces circadian disruption . Curr Biol . 2015. ; 25 ( 7 ): 907 – 911 . [DOI] [PubMed] [Google Scholar]
- 98. Härmä M . Individual differences in tolerance to shiftwork: a review . Ergonomics . 1993. ; 36 ( 1–3 ): 101 – 109 . [DOI] [PubMed] [Google Scholar]
- 99. Härmä M . Ageing, physical fitness and shiftwork tolerance . Appl Ergon . 1996. ; 27 ( 1 ): 25 – 29 . [DOI] [PubMed] [Google Scholar]
- 100. Wirtz A, et al . Gender differences in the effect of weekly working hours on occupational injury risk in the United States working population . Scand J Work Environ Health . 2012. ; 38 ( 4 ): 349 – 357 . [DOI] [PubMed] [Google Scholar]
- 101. Baillargeon J . Characteristics of the healthy worker effect . Occup Med . 2001. ; 16 ( 2 ): 359 – 366 . [PubMed] [Google Scholar]
- 102. Van Dongen HPA . Shift work and inter-individual differences in sleep and sleepiness . Chronobiol Int . 2006. ; 23 ( 6 ): 1139 – 1147 . [DOI] [PubMed] [Google Scholar]
- 103. Kalmbach DA, et al . The impact of stress on sleep: pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders . J Sleep Res . 2018. ; 27 ( 6 ): e12710 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Tucker P, et al . Review of studies that have used the Standard Shiftwork Index: evidence for the underlying model of shiftwork and health . Appl Ergon . 2008. ; 39 ( 5 ): 550 – 564 . [DOI] [PubMed] [Google Scholar]
- 105. Watson NF, et al . Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: Methodology and discussion. Sleep . 2015. ; 38 ( 6 ): 1161 – 1183 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Watson NF, et al . Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep . 2015. ; 38 ( 6 ): 843 – 844 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Rosekind MR, et al . Managing fatigue in operational settings. 1: physiological considerations and countermeasures . Behav Med . 1996. ; 21 ( 4 ): 157 – 165 . [DOI] [PubMed] [Google Scholar]
- 108. Redeker NS, et al . Workplace interventions to promote sleep health and an alert, healthy workforce . J Clin Sleep Med . 2019. ; 15 ( 4 ): 649 – 657 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Rangan S, et al . Predictive and proactive fatigue risk management approaches in commercial aviation . Chronobiol Int . 2020. ; 37 ( 9 –10): 1479 – 1482 . [DOI] [PubMed] [Google Scholar]
- 110. Roehrs T, et al . Caffeine: sleep and daytime sleepiness . Sleep Med Rev . 2008. ; 12 ( 2 ): 153 – 162 . [DOI] [PubMed] [Google Scholar]
- 111. Temple JL, et al . Systematic review and meta-analysis of the effects of caffeine in fatigued shift workers: implications for emergency medical services personnel . Prehosp Emerg Care . 2018. ; 22 ( sup1 ): 37 – 46 . [DOI] [PubMed] [Google Scholar]
- 112. Drake C, et al . Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed . J Clin Sleep Med . 2013. ; 9 ( 11 ): 1195 – 1200 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Martin-Gill C, et al . Effects of napping during shift work on sleepiness and performance in emergency medical services personnel and similar shift workers: a systematic review and meta-analysis . Prehosp Emerg Care . 2018. ; 22 ( sup1 ): 47 – 57 . [DOI] [PubMed] [Google Scholar]
- 114. Alger SE, et al . Challenging the stigma of workplace napping . Sleep . 2019. ; 42 : zsz097 . [DOI] [PubMed] [Google Scholar]
- 115. Hilditch CJ, et al . Sleep inertia: current insights . Nat Sci Sleep . 2019. ; 11 : 155 – 165 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Snel J, et al . Effects of caffeine on sleep and cognition . Prog Brain Res . 2011. ; 190 : 105 – 117 . [DOI] [PubMed] [Google Scholar]
- 117. Milner CE, et al . Benefits of napping in healthy adults: impact of nap length, time of day, age, and experience with napping . J Sleep Res . 2009. ; 18 ( 2 ): 272 – 281 . [DOI] [PubMed] [Google Scholar]
- 118. Vital-Lopez FG, et al . Caffeine dosing strategies to optimize alertness during sleep loss . J Sleep Res . 2018. ; 27 ( 5 ): e12711 . [DOI] [PubMed] [Google Scholar]
- 119. Lovato N, et al . The effects of napping on cognitive functioning . Prog Brain Res . 2010. ; 185 : 155 – 166 . [DOI] [PubMed] [Google Scholar]
- 120. Commissaris DACM, et al . Interventions to reduce sedentary behavior and increase physical activity during productive work: a systematic review . Scand J Work Environ Health . 2016. ; 42 ( 3 ): 181 – 191 . [DOI] [PubMed] [Google Scholar]
- 121. Gander P, et al . Fatigue risk management: organizational factors at the regulatory and industry/company level . Accid Anal Prev . 2011. ; 43 ( 2 ): 573 – 590 . [DOI] [PubMed] [Google Scholar]
- 122. Barger LK, et al . Effect of fatigue training on safety, fatigue, and sleep in emergency medical services personnel and other shift workers: a systematic review and meta-analysis . Prehosp Emerg Care . 2018. ; 22 ( Suppl 1 ): 58 – 68 . [DOI] [PubMed] [Google Scholar]
- 123. Davenport N, Lowry C, Pinkston B . Use of stimulants in operational settings: Issues and considerations . In Wesensten NJ ed. , Sleep Deprivation, Stimulant Medications, and Cognition . Cambridge University Press, Cambridge: ; 2012. : 237 – 256 . [Google Scholar]
- 124. Lerman SE, et al .; American College of Occupational and Environmental Medicine Presidential Task Force on Fatigue Risk Management. Fatigue risk management in the workplace . J Occup Environ Med . 2012. ; 54 ( 2 ): 231 – 258 . [DOI] [PubMed] [Google Scholar]
- 125. Coplen MK, et al . From transportation fatigue research to effective practice: the case for evaluation . Rev Hum Fact Ergon. 2015. ; 10 : 272 – 302 . [Google Scholar]
- 126. Dawson D, et al . Managing fatigue: it’s about sleep . Sleep Med Rev . 2005. ; 9 ( 5 ): 365 – 380 . [DOI] [PubMed] [Google Scholar]
- 127. Wilson M, et al . Sleep quality, sleepiness and the influence of workplace breaks: a cross-sectional survey of health-care workers in two US hospitals . Chronobiol Int . 2018. ; 35 ( 6 ): 849 – 852 . [DOI] [PubMed] [Google Scholar]
- 128. Balkin TJ, et al . The process of awakening: a PET study of regional brain activity patterns mediating the re-establishment of alertness and consciousness . Brain . 2002. ; 125 ( Pt 10 ): 2308 – 2319 . [DOI] [PubMed] [Google Scholar]
- 129. Hilditch CJ, et al . Time to wake up: reactive countermeasures to sleep inertia . Ind Health . 2016. ; 54 ( 6 ): 528 – 541 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. International Organization for Standardization . Risk Management - Guidelines . 2nd ed. (ISO Standard No. 31000:2018). Geneva: : ISO Copyright Office; ; 2018. . [Google Scholar]
- 131. Borbély AA . A two process model of sleep regulation . Hum Neurobiol . 1982. ; 1 ( 3 ): 195 – 204 . [PubMed] [Google Scholar]
- 132. Daan S, et al . Timing of human sleep: recovery process gated by a circadian pacemaker . Am J Physiol . 1984. ; 246 ( 2 Pt 2): R161 – R183 . [DOI] [PubMed] [Google Scholar]
- 133. Dijk DJ, et al . Paradoxical timing of the circadian rhythm of sleep propensity serves to consolidate sleep and wakefulness in humans . Neurosci Lett . 1994. ; 166 ( 1 ): 63 – 68 . [DOI] [PubMed] [Google Scholar]
- 134. Lavie P . Ultrashort sleep-waking schedule. III. 'Gates’ and 'forbidden zones’ for sleep . Electroencephalogr Clin Neurophysiol . 1986. ; 63 ( 5 ): 414 – 425 . [DOI] [PubMed] [Google Scholar]
- 135. Strogatz SH, et al . Circadian pacemaker interferes with sleep onset at specific times each day: role in insomnia . Am J Physiol . 1987. ; 253 ( 1 Pt 2 ): R172 – R178 . [DOI] [PubMed] [Google Scholar]
- 136. Barger LK, et al . Neurobehavioral, health, and safety consequences associated with shift work in safety-sensitive professions . Curr Neurol Neurosci Rep . 2009. ; 9 ( 2 ): 155 – 164 . [DOI] [PubMed] [Google Scholar]
- 137. Fischer D, et al . Updating the “Risk Index”: a systematic review and meta-analysis of occupational injuries and work schedule characteristics . Chronobiol Int . 2017. ; 34 ( 10 ): 1423 – 1438 . [DOI] [PubMed] [Google Scholar]
- 138. Knutsson A . Methodological aspects of shift-work research . Chronobiol Int . 2004. ; 21 ( 6 ): 1037 – 1047 . [DOI] [PubMed] [Google Scholar]
- 139. Driscoll TR, et al. A systematic review of the neurobehavioural and physiological effects of shiftwork systems . Sleep Med Rev . 2007. ; 11 ( 3 ): 179 – 194 . [DOI] [PubMed] [Google Scholar]
- 140. Lockley SW, et al .; Harvard Work Hours, Health and Safety Group. Effects of health care provider work hours and sleep deprivation on safety and performance . Jt Comm J Qual Patient Saf . 2007. ; 33 ( 11 Suppl): 7 – 18 . [DOI] [PubMed] [Google Scholar]
- 141. Smith L, et al . Work shift duration: a review comparing eight hour and 12 hour shift systems . Occup Environ Med . 1998. ; 55 ( 4 ): 217 – 229 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Folkard S, et al . Trends in the risk of accidents and injuries and their implications for models of fatigue and performance . Aviat Space Environ Med . 2004. ; 75 ( 3 Suppl): A161 – A167 . [PubMed] [Google Scholar]
- 143. Geiger-Brown J, et al . Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses . Chronobiol Int . 2012. ; 29 ( 2 ): 211 – 219 . [DOI] [PubMed] [Google Scholar]
- 144. Vila B, Samuels C . Sleep loss in first responders and the military . In: Kryger MH, Roth T, Dement WC , eds. Principles and Practice of Sleep Medicine . 5th ed. St. Louis: : Elsevier Saunders; , 2011. : 799 – 808 . [Google Scholar]
- 145. Min A, et al . Work schedule characteristics and fatigue among rotating shift nurses in hospital setting: an integrative review . J Nurs Manag . 2019. ; 27 ( 5 ): 884 – 895 . [DOI] [PubMed] [Google Scholar]
- 146. Ferguson SA, et al . On-call work: to sleep or not to sleep? it depends . Chronobiol Int . 2016. ; 33 ( 6 ): 678 – 684 . [DOI] [PubMed] [Google Scholar]
- 147. Alghamdi MG . Nursing workload: a concept analysis . J Nurs Manag . 2016. ; 24 ( 4 ): 449 – 457 . [DOI] [PubMed] [Google Scholar]
- 148. Studnek JR, et al . Effect of task load interventions on fatigue in emergency medical services personnel and other shift workers: a systematic review . Prehosp Emerg Care . 2018. ; 22 ( sup1 ): 81 – 88 . [DOI] [PubMed] [Google Scholar]
- 149. Dinges DF, et al . The benefits of a nap during prolonged work and wakefulness . Work Stress. 1998 ; 2 : 139 – 153 . [Google Scholar]
- 150. Mollicone DJ, et al . Response surface mapping of neurobehavioral performance: testing the feasibility of split sleep schedules for space operations . Acta Astronaut . 2008. ; 63 ( 7 – 10 ): 833 – 840 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Ficca G, et al . Naps, cognition and performance . Sleep Med Rev . 2010. ; 14 ( 4 ): 249 – 258 . [DOI] [PubMed] [Google Scholar]
- 152. Faraut B, et al . Napping: a public health issue. From epidemiological to laboratory studies . Sleep Med Rev . 2017. ; 35 : 85 – 100 . [DOI] [PubMed] [Google Scholar]
- 153. Ruggiero JS, et al . Effects of napping on sleepiness and sleep-related performance deficits in night-shift workers: a systematic review . Biol Res Nurs . 2014. ; 16 ( 2 ): 134 – 142 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Dinges DF, et al . Temporal placement of a nap for alertness: contributions of circadian phase and prior wakefulness . Sleep . 1987. ; 10 ( 4 ): 313 – 329 . [PubMed] [Google Scholar]
- 155. Gillberg M, et al. The effects of a short daytime nap after restricted night sleep . Sleep. 1996. ; 19 ( 7 ): 570 – 575 . [DOI] [PubMed] [Google Scholar]
- 156. Sallinen M, et al . Promoting alertness with a short nap during a night shift . ] Sleep Res . 1998. ; 7 ( 4 ): 240 – 247 . [DOI] [PubMed] [Google Scholar]
- 157. Matsumoto K, et al . The effect of night-time naps on recovery from fatigue following night work . Ergonomics . 1994. ; 37 ( 5 ): 899 – 907 . [DOI] [PubMed] [Google Scholar]
- 158. Garbarino S, et al . Professional shift-work drivers who adopt prophylactic naps can reduce the risk of car accidents during night work . Sleep . 2004. ; 27 ( 7 ): 1295 – 1302 . [DOI] [PubMed] [Google Scholar]
- 159. Rotenberg L, et al . Work schedule and self-reported hypertension - the potential beneficial role of on-shift naps for night workers . Chronobiol Int . 2016. ; 33 ( 6 ): 697 – 705 . [DOI] [PubMed] [Google Scholar]
- 160. Patterson PD, et al . Ambulatory blood pressure monitoring among emergency medical services night shift workers . Occup Environ Med . 2021. ; 78 ( 1 ): 29 – 35 . [DOI] [PubMed] [Google Scholar]
- 161. Zhou X, et al . Do split sleep/wake schedules reduce or increase sleepiness for continuous operations? Accid Anal Prev . 2017. ; 99 (Pt B): 434 – 439 . [DOI] [PubMed] [Google Scholar]
- 162. Kosmadopoulos A, et al . The effects of a split sleep-wake schedule on neurobehavioural performance and predictions of performance under conditions of forced desynchrony . Chronobiol Int . 2014. ; 31 ( 10 ): 1209 – 1217 . [DOI] [PubMed] [Google Scholar]
- 163. Short MA, et al . The effect of split sleep schedules (6 h-on/6 h-off) on neurobehavioural performance, sleep and sleepiness . Appl Ergon . 2016. ; 54 : 72 – 82 . [DOI] [PubMed] [Google Scholar]
- 164. Geiger-Brown J, et al . CE: original research: napping on the night shift: a two-hospital implementation project . Am J Nurs . 2016. ; 116 ( 5 ): 26 – 33 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Tassi P, et al . Sleep inertia. Sleep Med Rev . 2000. ; 4 ( 4 ): 341 – 353 . [DOI] [PubMed] [Google Scholar]
- 166. Dinges DF, et al . Performance after naps in sleep-conducive and alerting environments . In: Johnson LC , ed. Biological Rhythms, Sleep and Shift Work: Advances in Sleep Research Vol. 7 . New York: : Spectrum; ; 1981. : 539 – 552 . [Google Scholar]
- 167. Ferrara M, et al. Time-course of sleep inertia upon awakening from nighttime sleep with different sleep homeostasis conditions . Aviat Space Environ Med . 2000. ; 71 ( 3 ): 225 – 229 . [PubMed] [Google Scholar]
- 168. Hilditch CJ, et al . A review of short naps and sleep inertia: do naps of 30 min or less really avoid sleep inertia and slow- wave sleep ? Sleep Med . 2017. ; 32 : 176 – 190 . [DOI] [PubMed] [Google Scholar]
- 169. Bonnet MH, et al . Utility of caffeine: Evidence from the laboratory . In: Wesensten NJ , ed. Sleep Deprivation, Stimulant Medications, and Cognition . New York: : Cambridge University Press; , 2012. : 82 – 92 . [Google Scholar]
- 170. Reyner LA, et al . Suppression of sleepiness in drivers: combination of caffeine with a short nap . Psychophysiology . 1997. ; 34 ( 6 ): 721 – 725 . [DOI] [PubMed] [Google Scholar]
- 171. Van Dongen HPA, et al . Caffeine eliminates psychomotor vigilance deficits from sleep inertia. Sleep . 2001. ; 24 ( 7 ): 813 – 819 . [DOI] [PubMed] [Google Scholar]
- 172. Newman RA, et al . Caffeine gum minimizes sleep inertia . Percept Mot Skills . 2013. ; 116 ( 1 ): 280 – 293 . [DOI] [PubMed] [Google Scholar]
- 173. Centofanti S, et al . A pilot study investigating the impact of a caffeine-nap on alertness during a simulated night shift . Chronobiol Int . 2020. ; 37 ( 9 – 10 ): 1469 – 1473 . [DOI] [PubMed] [Google Scholar]
- 174. van Dam RM, et al . Coffee, caffeine, and health . N Engl J Med . 2020. ; 383 ( 4 ): 369 – 378 . [DOI] [PubMed] [Google Scholar]
- 175. Evans SM, et al . Caffeine tolerance and choice in humans . Psychopharmacology (Berl) . 1992. ; 108 ( 1–2 ): 51 – 59 . [DOI] [PubMed] [Google Scholar]
- 176. Quartana PJ, et al . Genetic basis of individual vulnerability to sleep loss and responsivity to stimulants . In: Wesensten NJ , ed. Sleep Deprivation, Stimulant Medications, and Cognition . New York: : Cambridge University Press; ; 2012. : 43 – 57 . [Google Scholar]
- 177. Spaeth AM, et al . Cumulative neurobehavioral and physiological effects of chronic caffeine intake: individual differences and implications for the use of caffeinated energy products . Nutr Rev . 2014. ; 72 (Suppl 1): 34 – 47 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Clark I, et al . Coffee, caffeine, and sleep: a systematic review of epidemiological studies and randomized controlled trials . Sleep Med Rev. . 2017. ; 31 : 70 – 78 . [DOI] [PubMed] [Google Scholar]
- 179. Leonard TK, et al . The effects of caffeine on various body systems: a review . J Am Diet Assoc . 1987. ; 87 ( 8 ): 1048 – 1053 . [PubMed] [Google Scholar]
- 180. Bruce M, et al . Caffeine withdrawal: a contrast of withdrawal symptoms in normal subjects who have abstained from caffeine for 24 hours and for 7 days . J Psychopharmacol . 1991. ; 5 ( 2 ): 129 – 134 . [DOI] [PubMed] [Google Scholar]
- 181. Wikoff D, et al . Systematic review of the potential adverse effects of caffeine consumption in healthy adults, pregnant women, adolescents, and children . Food Chem Toxicol . 2017. ; 109 (Pt 1): 585 – 648 . [DOI] [PubMed] [Google Scholar]
- 182. Shahly V, et al . The associations of insomnia with costly workplace accidents and errors: results from the America Insomnia Survey . Arch Gen Psychiatry . 2012. ; 69 ( 10 ): 1054 – 1063 . [DOI] [PubMed] [Google Scholar]
- 183. Hauri P. Sleep hygiene . In: Hauri P , ed. Current Concepts: The Sleep Disorders . Kalamazoo, MI: : Upjohn Company; , 1977. : 21 – 35 . [Google Scholar]
- 184. Rupp TL, et al . Banking sleep: realization of benefits during subsequent sleep restriction and recovery. Sleep . 2009. ; 32 ( 3 ): 311 – 321 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Patterson PD, et al . Does evidence support “banking/ex- tending sleep” by shift workers to mitigate fatigue, and/or to improve health, safety, or performance? A systematic review . Sleep Health. 2019. ; 5 ( 4 ): 359 – 369 . [DOI] [PubMed] [Google Scholar]
- 186. Caddick ZA, et al . A review of the environmental parameters necessary for an optimal sleep environment . Build Environ . 2018. ; 132 : 11 – 20 . [Google Scholar]
- 187. Stepanski EJ, et al . Use of sleep hygiene in the treatment of insomnia . Sleep Med Rev . 2003. ; 7 ( 3 ): 215 – 225 . [DOI] [PubMed] [Google Scholar]
- 188. Irish LA, et al . The role of sleep hygiene in promoting public health: a review of empirical evidence . Sleep Med Rev . 2015. ; 22 : 23 – 36 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189. Bixler EO, et al . Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression . J Clin Endocrinol Metab . 2005. ; 90 ( 8 ): 4510 – 4515 . [DOI] [PubMed] [Google Scholar]
- 190. Pagel JF . Drug-induced hypersomnolence . Sleep Med Clin . 2017. ; 12 ( 3 ): 383 – 393 . [DOI] [PubMed] [Google Scholar]
- 191. Melamed S, et al . Excessive daytime sleepiness and risk of occupational injuries in non-shift daytime workers. Sleep . 2002. ; 25 ( 3 ): 315 – 322 . [DOI] [PubMed] [Google Scholar]
- 192. Burks SV, et al . Nonadherence with employer-mandated sleep apnea treatment and increased risk of serious truck crashes. Sleep . 2016. ; 39 ( 5 ): 967 – 975 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Burks SV, et al . Employer-mandated obstructive sleep apnea treatment and healthcare cost savings among truckers . Sleep . 2020. ; 43 :zsz262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Czeisler CA, et al. ; et al. S. Modafinil in Shift Work Sleep Disorder Study Group. Modafinil for excessive sleepiness associated with shift-work sleep disorder . N Engl J Med . 2005. ; 353 ( 5 ): 476 – 486 . [DOI] [PubMed] [Google Scholar]
- 195. Sateia MJ, et al . Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med . 2017. ; 13 ( 2 ): 307 – 349 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Caldwell JA . Optimizing alertness with medications: The case for hypnotics . In: Ackerman PL , ed. Cognitive Fatigue: Multidisciplinary Perspectives on Current Research and Future Applications . Washington, D.C: .: American Psychological Association; ; 2011. : 231 – 246 . [Google Scholar]
- 197. Gill M, et al . Cognitive performance following modafinil versus placebo in sleep-deprived emergency physicians: a double-blind randomized crossover study . Acad Emerg Med . 2006. ; 13 ( 2 ): 158 – 165 . [DOI] [PubMed] [Google Scholar]
- 198. van der Sluiszen NNJJM, et al . Driving performance and neurocognitive skills of long-term users of benzodiazepine anxiolytics and hypnotics . Hum Psychopharmacol . 2019. ; 34 ( 6 ): e2715 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Johnson LC, et al . Benzodiazepines and caffeine: effect on daytime sleepiness, performance, and mood . Psychopharmacology (Berl) . 1990. ; 101 ( 2 ): 160 – 167 . [DOI] [PubMed] [Google Scholar]
- 200. Cressman AM, et al .; Canadian Drug Safety and Effectiveness Research Network. Prescription stimulant use and hospitalization for psychosis or mania: a population-based study . J Clin Psychopharmacol . 2015. ; 35 ( 6 ): 667 – 671 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Roth T, et al . Pharmacological effects of sedative-hypnotics, narcotic analgesics, and alcohol during sleep . Med Clin North Am . 1985. ; 69 ( 6 ): 1281 – 1288 . [DOI] [PubMed] [Google Scholar]
- 202. Roehrs T, et al . Sleep, sleepiness, and alcohol use . Alcohol Res Health . 2001. ; 25 ( 2 ): 101 – 109 . [PMC free article] [PubMed] [Google Scholar]
- 203. Auld F, et al . Evidence for the efficacy of melatonin in the treatment of primary adult sleep disorders . Sleep Med Rev . 2017. ; 34 : 10 – 22 . [DOI] [PubMed] [Google Scholar]
- 204. Sharkey KM, et al . Effects of melatonin administration on daytime sleep after simulated night shift work . J Sleep Res . 2001. ; 10 ( 3 ): 181 – 192 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Herxheimer A, et al . Melatonin for the prevention and treatment of jet lag . Cochrane Database Syst Rev . 2002. ; 2 :CD001520. [DOI] [PubMed] [Google Scholar]
- 206. Lewy AJ, et al . Melatonin shifts human circadian rhythms according to a phase-response curve . Chronobiol Int . 1992. ; 9 ( 5 ): 380 – 392 . [DOI] [PubMed] [Google Scholar]
- 207. Andersen LP, et al . The safety of melatonin in humans . Clin Drug Investig . 2016. ; 36 ( 3 ): 169 – 175 . [DOI] [PubMed] [Google Scholar]
- 208. Chellappa SL, et al . Can light make us bright? Effects of light on cognition and sleep . Prog Brain Res . 2011. ; 190 : 119 – 133 . [DOI] [PubMed] [Google Scholar]
- 209. Minors DS, et al . A human phase-response curve to light . Neurosci Lett . 1991. ; 133 ( 1 ): 36 – 40 . [DOI] [PubMed] [Google Scholar]
- 210. Khalsa SBS, et al . A phase response curve to single bright light pulses in human subjects . J Physiol . 2003. ; 549 (Pt 3 ): 945 – 952 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Boivin DB, et al . Dose-response relationships for resetting of human circadian clock by light . Nature . 1996. ; 379 ( 6565 ): 540 – 542 . [DOI] [PubMed] [Google Scholar]
- 212. Czeisler CA, et al . Sleep and circadian rhythms in humans . Cold Spring Harb Symp Quant Biol . 2007. ; 72 : 579 – 597 . [DOI] [PubMed] [Google Scholar]
- 213. Lockley SW, et al . High sensitivity of the human circadian melatonin rhythm to resetting by short wavelength light . J Clin Endocrinol Metab . 2003. ; 88 ( 9 ): 4502 – 4505 . [DOI] [PubMed] [Google Scholar]
- 214. Lee C, et al . A compromise phase position for permanent night shift workers: circadian phase after two night shifts with scheduled sleep and light/dark exposure . Chronobiol Int . 2006. ; 23 ( 4 ): 859 – 875 . [DOI] [PubMed] [Google Scholar]
- 215. Shechter A, et al . Interventions to reduce short-wavelength (“blue”) light exposure at night and their effects on sleep: a systematic review and meta-analysis . Sleep Adv . 2020. : 1 : zpaa002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Eastman CI, et al . How to use light and dark to produce circadian adaptation to night shift work . Ann Med . 1999. ; 31 ( 2 ): 87 – 98 . [DOI] [PubMed] [Google Scholar]
- 217. Cajochen C . Alerting effects of light . Sleep Med Rev . 2007. ; 11 ( 6 ): 453 – 464 . [DOI] [PubMed] [Google Scholar]
- 218. Smolders KCHJ, et al . Investigation of dose-response relationships for effects of white light exposure on correlates of alertness and executive control during regular daytime working hours . J Biol Rhythms . 2018. ; 33 ( 6 ): 649 – 661 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Rahman SA, et al . Diurnal spectral sensitivity of the acute alerting effects of light . Sleep . 2014. ; 37 ( 2 ): 271 – 281 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. Phipps-Nelson J, et al . Daytime exposure to bright light, as compared to dim light, decreases sleepiness and improves psychomotor vigilance performance. Sleep . 2003. ; 26 ( 6 ): 695 – 700 . [DOI] [PubMed] [Google Scholar]
- 221. Viola AU, et al . Blue-enriched white light in the workplace improves self-reported alertness, performance and sleep quality . Scand J Work Environ Health . 2008. ; 34 ( 4 ): 297 – 306 . [DOI] [PubMed] [Google Scholar]
- 222. Kloog I, et al . Global co-distribution of light at night (LAN) and cancers of prostate, colon, and lung in men . Chronobiol Int . 2009. ; 26 ( 1 ): 108 – 125 . [DOI] [PubMed] [Google Scholar]
- 223. Yang WS, et al . Light exposure at night, sleep duration, melatonin, and breast cancer: a dose-response analysis of observational studies . Eur J Cancer Prev . 2014. ; 23 ( 4 ): 269 – 276 . [DOI] [PubMed] [Google Scholar]
- 224. International Agency for Research on Cancer. Night Shift Work. IARC Monographs on the Identification of Carcinogenic Hazards to Humans. vol. 124 . Lyon, France: : IARC; , 2020. . [Google Scholar]
- 225. Mainster MA . Light and macular degeneration: a biophysical and clinical perspective . Eye (Lond). 1987. ; 1 ( Pt 2 ): 304 – 310 . [DOI] [PubMed] [Google Scholar]
- 226. Tosini G, et al . Effects of blue light on the circadian system and eye physiology . Mol Vis . 2016. ; 22 : 61 – 72 . [PMC free article] [PubMed] [Google Scholar]
- 227. Kredlow MA, et al . The effects of physical activity on sleep: a meta-analytic review . J Behav Med . 2015. ; 38 ( 3 ): 427 – 449 . [DOI] [PubMed] [Google Scholar]
- 228. Kelley GA, et al . Exercise and sleep: a systematic review of previous meta-analyses . J Evid Based Med . 2017. ; 10 ( 1 ): 26 – 36 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Stutz J, et al . Effects of evening exercise on sleep in healthy participants: a systematic review and meta-analysis . Sports Med . 2019. ; 49 ( 2 ): 269 – 287 . [DOI] [PubMed] [Google Scholar]
- 230. Youngstedt SD, et al . Human circadian phase-response curves for exercise . J Physiol . 2019. ; 597 ( 8 ): 2253 – 2268 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. Barger LK, et al . Daily exercise facilitates phase delays of circadian melatonin rhythm in very dim light . Am J Physiol Regul Integr Comp Physiol . 2004. ; 286 ( 6 ): R1077 – R1084 . [DOI] [PubMed] [Google Scholar]
- 232. Matsumoto Y, et al . Physical activity increases the dissociation between subjective sleepiness and objective performance levels during extended wakefulness in human . Neurosci Lett . 2002. ; 326 ( 2 ): 133 – 136 . [DOI] [PubMed] [Google Scholar]
- 233. Ojo SO, et al . The impact of active workstations on workplace productivity and performance: a systematic review . Int J Environ Res Public Health . 2018. ; 15 : 417 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Riedy SM, et al. , sleepiness, and performance prediction modeling . In: Kryger MH, Roth T, Dement WC , eds. Principles and Practice of Sleep Medicine . 7th ed. Philadelphia: : Elsevier; , in press. . [Google Scholar]
- 235. Bianchi MT . Sleep devices: wearables and nearables, informational and interventional, consumer and clinical . Metabolism . 2018. ; 84 : 99 – 108 . [DOI] [PubMed] [Google Scholar]
- 236. Abe T, et al . Sleepiness and safety: where biology needs technology. Sleep Biol Rhythms. . 2014. ; 12 ( 2 ): 74 – 84 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Burns M, et al . Fitness-for-duty testing: a new approach to workplace safety . Alcohol Health Res World . 1995. ; 19 ( 2 ): 159 – 160 . [PMC free article] [PubMed] [Google Scholar]
- 238. Mallis MM, et al . Summary of the key features of seven biomathematical models of human fatigue and performance . Aviat Space Environ Med . 2004. ; 75 ( 3 Suppl):A4–14. [PubMed] [Google Scholar]
- 239. Van Dongen HPA . Comparison of mathematical model predictions to experimental data of fatigue and performance . Aviat Space Environ Med . 2004. ; 75 ( 3 Suppl):A15–A36. [PubMed] [Google Scholar]
- 240. Rangan S, et al . Integrated fatigue modeling in crew rostering and operations . Can Aeronaut Space J . 2013. ; 59 : 1 – 6 . [Google Scholar]
- 241. Gunzelmann G, et al . Basic and applied science interactions in fatigue understanding and risk mitigation . Prog Brain Res . 2019. ; 246 : 177 – 204 . [DOI] [PubMed] [Google Scholar]
- 242. James FO, et al . Does implementation of biomathematical models mitigate fatigue and fatigue-related risks in emergency medical services operations? a systematic review . Prehosp Emerg Care . 2018. ; 22 ( sup1 ): 69 – 80 . [DOI] [PubMed] [Google Scholar]
- 243. Roomkham S, et al . Promises and challenges in the use of consumer-grade devices for sleep monitoring . IEEE Rev Biomed Eng . 2018. ; 11 : 53 – 67 . [DOI] [PubMed] [Google Scholar]
- 244. Guillodo E, et al .; HUGOPSY Network . Clinical applications of mobile health wearable-based sleep monitoring: systematic review . JMIR Mhealth Uhealth . 2020. ; 8 ( 4 ): e10733 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Berryhill S, et al . Effect of wearables on sleep in healthy individuals: a randomized crossover trial and validation study . J Clin Sleep Med . 2020. ; 16 ( 5 ): 775 – 783 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Mollicone D, et al . Predicting performance and safety based on driver fatigue . Accid Anal Prev . 2019. ; 126 : 142 – 145 . [DOI] [PubMed] [Google Scholar]
- 247. Loncar-Turukalo T, et al . Literature on wearable technology for connected health: scoping review of research trends, advances, and barriers . J Med Internet Res . 2019. ; 21 ( 9 ): e14017 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Basner M, et al . Fitness for duty: a 3-minute version of the psychomotor vigilance test predicts fatigue-related declines in luggage-screening performance . J Occup Environ Med . 2011. ; 53 ( 10 ): 1146 – 1154 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Forsman P, et al . Posturographic sleepiness monitoring . J Sleep Res . 2007. ; 16 ( 3 ): 259 – 261 . [DOI] [PubMed] [Google Scholar]
- 250. Thomas M, et al . Fatigue proofing . In: Kryger MH, Roth T, Dement WC , eds. Principles and Practice of Sleep Medicine . 7th ed. Philadelphia: : Elsevier; , in press. . [Google Scholar]
- 251. Rainey D, et al . Sleep and transportation safety: role of the employer. Sleep Med Clin . 2019. ; 14 ( 4 ): 499 – 508 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252. Gander PH, et al . 2017 . Fatigue risk management systems . In: Kryger MH, Roth T, Dement WC , eds. Principles and Practice of Sleep Medicine . 6th ed. Philadelphia: : Elsevier; , 2017. : 697 – 707 . [Google Scholar]