Abstract
Adolescents and young adults (AYAs, 15–39 years) are the largest uninsured population in the Unites States, increasing the likelihood of late-stage cancer diagnosis and poor survival. We evaluated the associations between the Affordable Care Act (ACA), insurance coverage, stage at diagnosis, and survival among AYAs with lymphoma. We used data from the California Cancer Registry linked to Medicaid enrollment files on AYAs diagnosed with a primary non-Hodgkin (NHL; n=5,959) or Hodgkin (HL; n=5,378) lymphoma pre-ACA and in the early and full ACA eras. Health insurance was categorized as continuous Medicaid, discontinuous Medicaid, Medicaid enrollment at diagnosis/uninsurance, other public, and private. We used multivariable regression models for statistical analyses. The proportion of AYAs uninsured/Medicaid enrolled at diagnosis decreased from 13.4% pre-ACA to 9.7% with full ACA implementation, while continuous Medicaid increased from 9.3% to 29.6% during this time (p<0.001). After full ACA, AYAs with NHL were less likely to be diagnosed with stage IV disease (aOR=0.84, 95% CI 0.73–0.97). AYAs with lymphoma were more likely to receive care at National Cancer Institute-Designated Cancer Centers (aOR=1.42, 95% CI 1.28–1.57) and had lower likelihood of death (aHR=0.54, 95% CI 0.46–0.63) after full ACA. However, AYAs from the lowest socioeconomic neighborhoods, racial/ethnic minority groups, and those with Medicaid, continued to experience worse survival. In summary, AYAs with lymphomas experienced increased access to healthcare and better clinical outcomes following Medicaid expansion under the ACA. Yet, socioeconomic and racial/ethnic disparities remain, calling for additional efforts to decrease health inequities among underserved AYAs with lymphoma.
Keywords: adolescents and young adults, lymphoma, stage, survival, Affordable Care Act
Graphical Abstract
Introduction
Lymphoma is one of the most common malignancies in adolescents and young adults (AYAs) aged 15–39 years. Each year, over 4,000 AYAs are diagnosed with either Hodgkin lymphoma (HL) or non-Hodgkin lymphoma (NHL) in the United States (US).1 Most AYAs with lymphomas are diagnosed with late-stage disease.1, 2 Advances in risk-directed combination chemotherapy (associated or not with radiation) have led to significant improvement in lymphoma survival in the last three decades, even for patients with advanced stage disease at diagnosis.3, 4 Whereas 5-year survival for all stages combined currently exceeds 94% for HL and 83% for NHL across all AYA age groups, AYAs diagnosed with late-stage lymphoma experience significantly worse survival than those diagnosed with localized or regional disease, underscoring the importance of detecting cancer in earlier stages.1, 5, 6
AYAs are the largest uninsured population in the US. Despite improvement in insurance coverage after the implementation of the Patient Protection and Affordable Care Act of 2010 (ACA)7, data from 2018–2019 showed that 19–34 year-olds continue to be the most uninsured group (15.6%) compared with children ≤19 (5.7%) and older adults 35–64 years (11.3%).8 Lack of health insurance can lead to limited access to healthcare, adversely influencing AYAs cancer care and outcomes. Being uninsured or discontinuously insured may delay cancer screening or medical consultation when the first symptoms of cancer occur, resulting in cancer progression.9, 10 In addition, lack of insurance can delay cancer treatment initiation and prevent completion of treatment due to financial barriers, leading to increased cancer mortality.11
The ACA expanded health insurance for low-income AYAs in several ways: increasing Medicaid eligibility, creating individual and small-business marketplaces, allowing young adults to remain under their parent’s insurance until they turn 26 years (Dependent Coverage Expansion, DCE); and permitting consumers to buy coverage directly from insurance companies.12 Our previous study on AYAs diagnosed with cancer from 2005 to 2014 found that uninsured patients who obtained Medicaid insurance at cancer diagnosis were up to 2.5 times more likely to present with later stage disease than privately insured AYAs.13 In this study with updated data through 2017, we investigated whether ACA expansion was associated with increased insurance coverage and reduction of stage IV disease at diagnosis among AYAs with lymphoma. Our secondary aims were to examine changes in receipt of treatment at National Cancer Institute-Designated Cancer Centers (NCI-DCCs) and survival.
Material and Methods
We used data from the California Cancer Registry (CCR) linked to Medicaid enrollment files. Eligible patients were those aged 15–39 years when diagnosed with a first primary NHL or HL from March 2005 to December 2017 in California. Morphology codes were based on the Surveillance, Epidemiology, and End Results (SEER) AYA site recode. Health insurance was classified into private, Medicaid, other public, and unknown. Similar to a previous study,13 Medicaid insurance was categorized as continuous Medicaid (enrollment for at least 5 continuous months prior to lymphoma diagnosis), Medicaid at diagnosis (enrollment starts in the month prior to or within two months after diagnosis to account for reactive enrollment), and discontinuous Medicaid (enrollment that does not meet the definitions for continuous enrollees, Medicaid at diagnosis or Medicaid insurance recorded in the CCR but without a match in the Medicaid enrollment files). Because in California AYAs become eligible for Medicaid enrollment when diagnosed with cancer, in our analyses we combined AYAs who gained Medicaid insurance at diagnosis with those classified as uninsured in the CCR.
We categorized period of diagnosis according to ACA implementation, which started early in California: pre-ACA (March 2005–September 2010), early ACA (October 2010–December 2013) and full ACA (January 2014–December 2017). The early ACA includes the DCE and the Low-Income Health Plan, which expanded Medicaid eligibility to low-income individuals.12 The full ACA era includes full Medicaid expansion and insurance marketplaces. Clinical/hospital characteristics include stage at diagnosis based on the American Joint Commission of Cancer (AJCC) staging system (I–IV), Charlson comorbidity index, and treatment facility. Treatment facility (i.e., the hospital where the patient received lymphoma care) was classified as NCI-DCC or non-NCI-DCC. Sociodemographic covariates include sex, age at diagnosis, marital status, race/ethnicity [non-Hispanic (NH) White (White), NH Black (Black), Hispanic, Asian/Pacific Islander (Asian/PI), American Indian/Alaska Native (AI/AN)], and neighborhood socioeconomic status (nSES). The nSES index is a composite measure at the census block level, which contains information on education, occupation, unemployment, household income, poverty, rent and house values, information originated from the 2000 US Census and the 2006–2010 American Community Survey.14
We used descriptive analyses to evaluate changes in the proportion of health insurance categories and stage IV disease at diagnosis by ACA era, and the Kaplan-Meir approach to estimate overall (all-cause) survival. Multivariable logistic regression was used to examine the association of late-stage diagnosis (IV vs. I–III) with ACA and sociodemographic and clinical factors; as well as changes in treatment at NCI-DCCs over time. Results are presented as adjusted odds ratios (aOR) with corresponding 95% confidence intervals (CI). In the regression model for stage at diagnosis, patients with unknown stage (6.5% of the sample) were merged with those with stages I–III after Kaplan-Meier curves indicated these patients have survival trends similar to those with stages I/II at diagnosis. In a sensitivity analysis where we excluded patients with missing stage, we found similar results. Associations of survival with ACA, sociodemographic and clinical factors were evaluated with multivariable Cox proportional hazards models. Results are presented as adjusted hazard ratios (aHR) and associated 95% CIs. Patients were followed from lymphoma diagnosis to the date of death, last follow-up or end of study (12/31/2018), whichever occurred first. The proportional hazard assumption, assessed by log-log survival plots and confirmed using Schoenfeld residuals, was met for all variables but cancer type, which was used as a stratified variable for the analysis of all patients combined. Analyses were also performed separately for NHL and HL AYAs. All analyses were conducted using Stata software version 16.1.
Results
We identified 11,351 AYAs in California with lymphomas during the study period. Fourteen patients with lymphoma detected solely at autopsy were excluded; of the 11,337 AYAs analyzed, 5,959 had NHL and 5,378 HL. For the survival analysis, we further excluded patients with zero survival time (n=53) or incomplete dates of diagnosis and/or follow-up (n=63). Most patients were male (55.6%), White (44.5%), older (26–39 years, 62.8%), had private insurance (56.4%), and received initial care at non-NCI-DCCs (72.6%) (Table 1).
Table 1:
Characteristics of adolescents and young adults with lymphomas in California, 2005–2017, overall and by era of diagnosis
| Total (Mar 2005–Dec 2017) N=11,337 |
Pre-ACA (Mar 2005–Sep 2010) N=4,968 |
Early ACA (Oct 2010–Dec 2013) N=2,785 |
Full ACA (Jan 2014–Dec 2017) N=3,584 |
p-valueε | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Age at diagnosis | 0.106 | ||||||||
| 15–20 years | 1,936 | 17.1 | 860 | 17.3 | 463 | 16.6 | 613 | 17.1 | |
| 21–25 years | 2,284 | 20.1 | 1,047 | 21.1 | 561 | 20.2 | 676 | 18.9 | |
| 26–39 years | 7,117 | 62.8 | 3,061 | 61.6 | 1,761 | 63.2 | 2,295 | 64.0 | |
| Sex | 0.951 | ||||||||
| Female | 5,035 | 44.4 | 2,199 | 44.3 | 1,243 | 44.6 | 1,593 | 44.4 | |
| Male | 6,302 | 55.6 | 2,769 | 55.7 | 1,542 | 55.4 | 1,991 | 55.6 | |
| Health insurance | <0.001 | ||||||||
| Private | 6,395 | 56.4 | 3,004 | 60.5 | 1,622 | 58.2 | 1,769 | 49.4 | |
| Continuous Medicaid | 1,894 | 16.7 | 463 | 9.3 | 369 | 13.3 | 1,062 | 29.6 | |
| Discontinuous Medicaid | 1,129 | 10.0 | 513 | 10.3 | 278 | 10.0 | 338 | 9.4 | |
| Medicaid at diagnosis/uninsured | 1,424 | 12.6 | 667 | 13.4 | 407 | 14.6 | 350 | 9.7 | |
| Other Public* | 141 | 1.2 | 99 | 2.0 | 29 | 1.0 | 13 | 0.4 | |
| Unknown | 354 | 3.1 | 222 | 4.5 | 80 | 2.9 | 52 | 1.5 | |
| Lymphoma type | <0.001 | ||||||||
| Hodgkin Lymphoma | 5,378 | 47.4 | 2,460 | 49.5 | 1,330 | 47.8 | 1,588 | 44.3 | |
| Non-Hodgkin Lymphoma | 5,959 | 52.6 | 2,508 | 50.5 | 1,455 | 52.2 | 1,996 | 55.7 | |
| Stage at diagnosis | 0.085 | ||||||||
| Stage I | 2,496 | 22.0 | 1,086 | 21.9 | 608 | 21.8 | 802 | 22.4 | |
| Stage II | 3,764 | 33.2 | 1,679 | 33.8 | 931 | 33.5 | 1,154 | 32.2 | |
| Stage III | 1,728 | 15.2 | 761 | 15.3 | 438 | 15.7 | 529 | 14.8 | |
| Stage IV | 2,610 | 23.0 | 1,136 | 22.9 | 649 | 23.3 | 825 | 23.0 | |
| Unknown | 739 | 6.5 | 306 | 6.1 | 159 | 5.7 | 274 | 7.6 | |
| Treatment facility | <0.001 | ||||||||
| NCI-DCC | 3,107 | 27.4 | 1,196 | 24.1 | 796 | 28.6 | 1,115 | 31.1 | |
| Non-NCI-DCC | 8,230 | 72.6 | 3,772 | 75.9 | 1,989 | 71.4 | 2,469 | 68.9 | |
| Charlson Comorbidity Index | <0.001 | ||||||||
| None | 6,602 | 58.2 | 3,183 | 64.1 | 1,625 | 58.3 | 1,794 | 50.1 | |
| One | 1,013 | 8.9 | 415 | 8.3 | 245 | 8.8 | 353 | 9.8 | |
| More than one | 325 | 2.9 | 118 | 2.4 | 64 | 2.3 | 143 | 4.0 | |
| Unknown | 3,397 | 30.0 | 1,252 | 25.2 | 851 | 30.6 | 1,294 | 36.1 | |
| Race/ethnicity | <0.001 | ||||||||
| Non-Hispanic White | 5,046 | 44.5 | 2,338 | 47.1 | 1,240 | 44.5 | 1,468 | 41.0 | |
| Non-Hispanic Black | 873 | 7.7 | 403 | 8.1 | 226 | 8.1 | 244 | 6.8 | |
| Hispanic | 3,771 | 33.3 | 1,594 | 32.1 | 922 | 33.1 | 1,255 | 35.0 | |
| Asian/Pacific Islander | 1,376 | 12.1 | 523 | 10.5 | 334 | 12.0 | 519 | 14.5 | |
| American Indian/Alaska Native | 54 | 0.5 | 24 | 0.5 | 11 | 0.4 | 19 | 0.5 | |
| Other/Unknown | 217 | 1.9 | 86 | 1.7 | 52 | 1.9 | 79 | 2.2 | |
| Neighborhood SES | 0.100 | ||||||||
| Highest | 3,979 | 35.1 | 1,795 | 36.1 | 977 | 35.1 | 1,207 | 33.7 | |
| Medium | 3,878 | 34.2 | 1,695 | 34.1 | 926 | 33.2 | 1,257 | 35.1 | |
| Lowest | 3,480 | 30.7 | 1,478 | 29.8 | 882 | 31.7 | 1,120 | 31.2 | |
| Marital status | <0.001 | ||||||||
| Married | 3,533 | 31.2 | 1,667 | 33.5 | 810 | 29.1 | 1,056 | 29.5 | |
| Not Married | 7,163 | 63.2 | 3,015 | 60.7 | 1,813 | 65.1 | 2,335 | 65.1 | |
| Unknown | 641 | 5.2 | 286 | 5.8 | 162 | 5.8 | 193 | 5.4 | |
Abbreviations: SES: socioeconomic status; NCI-DCC, National Cancer Institute-Designated Cancer Center; ACA, Affordable Care Act.
Chi-square p-value; Jan, January; Mar, March Sep, September; Oct, October; Dec, December.
Other public includes Indian/Public Health Service, County Funded, not-otherwise specified (NOS), Medicare without supplement, Medicare, NOS.
From the pre-ACA to full ACA era, the proportion of AYAs with continuous Medicaid enrollment increased (9.3% to 29.6%) and Medicaid at diagnosis/uninsured decreased (13.4% to 9.7%), p-value<0.001 (Table 1). The proportion of AYAs with discontinuous Medicaid, private, and other public insurance also decreased over time.
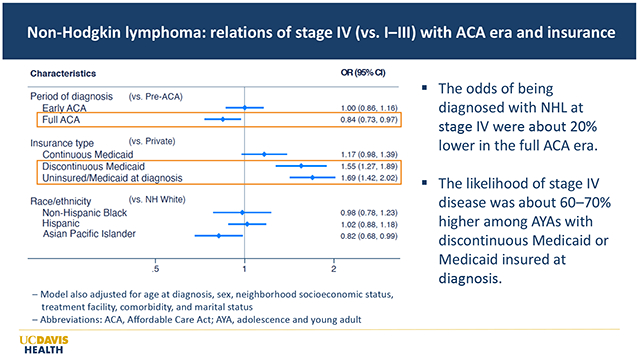
Among AYAs with NHL (but not HL), we observed a 3.6% reduction in stage IV disease at diagnosis (29.8% pre-ACA to 26.2% full ACA, p-value=0.033) (Supplemental Table S1). In multivariable models with all patients combined, the odds of stage IV disease were higher among AYAs with Medicaid at diagnosis/uninsured (aOR=1.69, CI 1.47–1.93) and discontinuous Medicaid (aOR=1.54, CI 1.33–1.80) vs. privately insured (Table 2). Those with continuous Medicaid were also more likely to present with stage IV (vs private, aOR=1.20, CI 1.05–1.38), although to a lesser extent. Patients with NHL were nearly twice as likely to present with stage IV than those with HL (aOR=1.81, CI 1.64–1.99). In stratified models, the odds of stage IV at diagnosis were lower among AYAs with NHL after full ACA implementation (vs. pre-ACA, aOR=0.84, CI 0.73–0.97), whereas no difference was observed among AYAs with HL (aOR=1.14, CI 0.96–1.37). Additionally, Black, Hispanic and Asian/PI patients with HL had 40% higher odds of stage IV at diagnosis than White patients.
Table 2:
Relation of ACA implementation, and sociodemographic and clinical factors to Stage IV lymphoma, overall and by lymphoma type, 2005–2017
| Characteristics | All patients N=11,337 |
Non-Hodgkin lymphoma N=5,959 |
Hodgkin lymphoma N=5,378 |
|---|---|---|---|
|
|
|||
| Stage IV (vs. I–III) aOR (95% CI) |
Stage IV (vs. I–III) aOR (95% CI) |
Stage IV (vs. I–III) aOR (95% CI) |
|
| Period of diagnosis | |||
| Pre-ACA (Mar 2005–Sep 2010) | Reference | Reference | Reference |
| Early ACA (Oct 2010–Dec 2013) | 0.99 (0.89–1.11) | 1.00 (0.86–1.16) | 0.99 (0.82–1.19) |
| Full ACA (Jan 2014–Dec 2017) | 0.94 (0.85–1.05) | 0.84 (0.73–0.97) | 1.14 (0.96–1.37) |
| Age at diagnosis, years | |||
| 15–20 | Reference | Reference | Reference |
| 21–25 | 0.99 (0.85–1.16) | 1.06 (0.84–1.33) | 0.93 (0.75–1.15) |
| 26–39 | 1.16 (1.01–1.33) | 1.25 (1.03–1.51) | 1.08 (0.88–1.31) |
| Sex | |||
| Females | Reference | Reference | Reference |
| Males | 1.33 (1.21–1.46) | 1.26 (1.12–1.43) | 1.40 (1.21–1.63) |
| Race/ethnicity& | |||
| Non-Hispanic White | Reference | Reference | Reference |
| Non-Hispanic Black | 1.13 (0.95–1.35) | 0.98 (0.78–1.23) | 1.40 (1.06–1.85) |
| Hispanic | 1.15 (1.03–1.29) | 1.02 (0.88–1.18) | 1.39 (1.16–1.66) |
| Asian/Pacific Islander | 1.00 (0.86–1.16) | 0.82 (0.68–0.99) | 1.40 (1.10–1.79) |
| American Indian/Alaska Native | 0.60 (0.28–1.26) | 0.56 (0.23–1.33) | 0.60 (0.14–2.61) |
| Neighborhood SES | |||
| Highest | Reference | Reference | Reference |
| Medium | 1.12 (0.99–1.25) | 1.19 (1.03–1.38) | 1.02 (0.85–1.23) |
| Lowest | 1.09 (0.96–1.24) | 1.13 (0.96–1.34) | 1.03 (0.84–1.27) |
| Insurance type& | |||
| Private | Reference | Reference | Reference |
| Continuous Medicaid | 1.20 (1.05–1.38) | 1.17 (0.98–1.39) | 1.25 (1.00–1.55) |
| Discontinuous Medicaid | 1.54 (1.33–1.80) | 1.55 (1.27–1.89) | 1.55 (1.22–1.98) |
| Medicaid at diagnosis/uninsured | 1.69 (1.47–1.93) | 1.69 (1.42–2.02) | 1.69 (1.36–2.11) |
| Other public* | 1.21 (0.81–1.81) | 1.43 (0.83–2.48) | 1.05 (0.57–1.95) |
| Charlson Comorbidity Index& | |||
| None | Reference | Reference | Reference |
| One | 1.14 (0.98–1.33) | 1.12 (0.93–1.37) | 1.17 (0.91–1.51) |
| More than one | 2.17 (1.71–2.75) | 1.92 (1.47–2.53) | 2.86 (1.81–4.52) |
| Treatment facility | |||
| NCI-DCC | Reference | Reference | Reference |
| Non-NCI-DCC | 0.63 (0.57–0.69) | 0.59 (0.53–0.67) | 0.70 (0.59– 0.82) |
| Lymphoma type | |||
| Hodgkin lymphoma | Reference | N/A | N/A |
| Non-Hodgkin lymphoma | 1.81 (1.64–1.99) | ||
| Marital status& | |||
| Married | Reference | Reference | Reference |
| Unmarried | 1.10 (0.98–1.22) | 1.08 (0.94–1.24) | 1.12 (0.93–1.36) |
Abbreviations: NCI-DCC: National Cancer Institute-Designated Cancer Center; SES: socioeconomic status; ACA: Affordable Care Act; aOR, adjusted odds ratio; CI, confidence interval; N/A: not applicable; Jan, January; Mar, March Sep, September; Oct, October; Dec, December.
Other public includes Indian/Public Health Service, County Funded, not-otherwise specified (NOS), Medicare without supplement, Medicare, NOS.
Patients with unknown insurance, race/ethnicity, marital status, and comorbidity are not shown in the Table.
The proportion of AYAs who received initial care at NCI-DCCs increased from 24.1% pre-ACA to 31.1% after full ACA implementation, p<0.001 (Table 1). In multivariable models, compared with pre-ACA, AYAs were about 30–40% more likely to receive care at NCI-DCCs in the early (aOR=1.26, CI 1.13–1.41) and full (aOR=1.42, CI 1.28–1.57) ACA eras (Table 3). AYAs with NHL (vs. HL), stage IV at diagnosis, ≥1 comorbidity, with public insurance (vs. private), and of Asian/PI race/ethnicity (vs. Whites) were more likely to receive care at NCI-DCCs. By contrast, older AYAs (22–39 vs. 15–21), those of Black race/ethnicity and those residing in the middle and lowest SES neighborhoods had lower likelihood of receiving care at NCI-DCCs. These associations were similar for NHL and HL patients.
Table 3:
Relation of treatment at NCI-DCC to ACA implementation period, and clinical and sociodemographic factors among adolescents and young adults with lymphomas, California, 2005–2017
| All patients N=11,337 |
Non-Hodgkin lymphoma N=5,959 |
Hodgkin lymphoma N=5,378 |
|
|---|---|---|---|
|
| |||
| Characteristics (N=11,337) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) |
| Calendar period | |||
| Pre-ACA (Mar 2005–Sep 2010) | Reference | Reference | Reference |
| Early ACA (Oct 2010–Dec 2013) | 1.26 (1.13–1.41) | 1.33 (1.15–1.53) | 1.21 (1.03–1.42) |
| Full ACA (Jan 2014–Dec 2017) | 1.42 (1.28–1.57) | 1.39 (1.21–1.60) | 1.47 (1.26–1.72) |
| Insurance& | |||
| Private | Reference | Reference | |
| Continuous Medicaid | 1.20 (1.05–1.36) | 1.24 (1.05–1.48) | 1.14 (0.93–1.39) |
| Discontinuous Medicaid | 1.38 (1.19–1.61) | 1.51 (1.24–1.84) | 1.23 (0.97–1.56) |
| Medicaid at diagnosis/uninsured | 1.51 (1.32–1.72) | 1.53 (1.28–1.83) | 1.47 (1.19–1.81) |
| Other Public* | 1.76 (1.21–2.56) | 1.37 (0.79–2.40) | 2.16 (1.30–3.57) |
| Age at diagnosis, years | |||
| 15–21 | Reference | Reference | Reference |
| 22–25 | 0.57 (0.50–0.65) | 0.57 (0.46–0.71) | 0.57 (0.48–0.68) |
| 26–39 | 0.49 (0.43–0.55) | 0.46 (0.38–0.55) | 0.53 (0.45–0.63) |
| Sex | |||
| Female | Reference | Reference | Reference |
| Male | 1.03 (0.95–1.13) | 1.10 (0.98–1.24) | 0.96 (0.85–1.10) |
| Race/ethnicity& | |||
| Non-Hispanic White | Reference | Reference | Reference |
| Non-Hispanic Black | 0.74 (0.62–0.89) | 0.69 (0.55–0.88) | 0.80 (0.61–1.06) |
| Hispanic | 0.91 (0.82–1.02) | 0.91 (0.78–1.05) | 0.93 (0.79–1.10) |
| Asian/Pacific Islander | 1.26 (1.10–1.43) | 1.25 (1.05–1.48) | 1.26 (1.02–1.56) |
| American Indian/Alaska Native | 1.39 (0.77–2.50) | 1.85 (0.89–3.83) | 0.75 (0.25–2.25) |
| Neighborhood SES | |||
| Highest | Reference | Reference | Reference |
| Middle | 0.64 (0.58–0.71) | 0.67 (0.58–0.77) | 0.62 (0.53–0.73) |
| Lowest | 0.60 (0.53–0.68) | 0.58 (0.49–0.68) | 0.64 (0.53–0.76) |
| Marital status& | |||
| Married | Reference | Reference | Reference |
| Not married | 1.04 (0.93–1.15) | 1.02 (0.89–1.17) | 1.04 (0.88–1.24) |
| Type of cancer | |||
| Hodgkin lymphoma | Reference | ||
| Non-Hodgkin lymphoma | 1.61 (1.46–1.77) | N/A | N/A |
| Charlson comorbidity Index& | |||
| None | Reference | Reference | Reference |
| One | 0.89 (0.76–1.04) | 0.89 (0.73–1.09) | 0.87 (0.68–1.11) |
| More than one | 1.31 (1.02–1.67) | 1.36 (1.03–1.80) | 1.04 (0.62–1.74) |
| Stage at diagnosis& | |||
| I | Reference | Reference | Reference |
| II | 1.16 (1.02–1.32) | 0.99 (0.84–1.17) | 1.48 (1.15–1.89) |
| III | 1.06 (0.91–1.23) | 0.93 (0.76–1.13) | 1.37 (1.04–1.79) |
| IV | 1.63 (1.43–1.84) | 1.55 (1.34–1.80) | 1.90 (1.44–2.49) |
Abbreviations: NCI-DCC, National Cancer Institute-Designated Cancer Center; SES, socioeconomic status; ACA, Affordable Care Act; aOR, adjusted odds ratios; CI, confidence interval; N/A, not applicable; Jan, January; Mar, March; Sep, September; Oct, October; Dec, December.
Other public includes Indian/Public Health Service, County Funded, not-otherwise specified (NOS), Medicare without supplement, Medicare, NOS.
Patients with unknown insurance, race/ethnicity, marital status, stage at diagnosis, and comorbidity are not shown in the Table.
Overall, five-year lymphoma survival increased from 87.4% pre-ACA to 91.1% full ACA, p-value<0.001 (Supplemental Figure S1). AYAs with stage IV disease experienced lower 5-year survival (77.6%) than those with stage I (92.7%), II (93.7%), or III (88.3%) (p-value<0.001; Supplemental Figure S2). In a stratified analysis, survival increased across eras for both NHL and HL, but was lower for AYAs with NHL. Likewise, survival was considerably worse for those with stage IV disease, with more pronounced differences among AYAs with NHL.
In multivariable Cox models, AYAs diagnosed in the early (aHR=0.76, CI 0.66–0.88) and full (aHR=0.54, CI 0.46–0.63) ACA eras had lower hazard of death than those diagnosed pre-ACA (Table 4). Compared to AYAs with private insurance, the hazard of death was higher among those with Medicaid at diagnosis/uninsured (aHR=2.14, CI 1.83–2.49), discontinuous Medicaid (aHR=2.17, CI 1.83–2.58), and continuous Medicaid (HR=1.93, CI 1.63–2.29). Regardless of health insurance status, older AYAs, males, unmarried, residents in the lowest SES neighborhoods, and those of Black (aHR=1.29, CI 1.07–1.57), Hispanic (aHR=1.26 CI 1.10–1.45), Asian/PI (aHR=1.22, CI 1.01–1.48), and AI/NA (aHR=2.16, CI 1.21–3.85) race/ethnicity (vs. White) experienced higher likelihood of death. We found similar associations when NHL and HL patients were considered separately.
Table 4:
Relation of ACA implementation period and sociodemographic and clinical factors to hazard of death, 2005–2017
| All patients N=11,221 | Non-Hodgkin lymphoma N=5,878 | Hodgkin lymphoma N=5,343 | |
|---|---|---|---|
|
| |||
| Characteristics | aHR (95% CI)§ | aHR (95% CI) | aHR (95% CI) |
| Age at diagnosis, years | |||
| 15–20 | Reference | Reference | Reference |
| 21–25 | 1.43 (1.16–1.78) | 1.43 (1.09–1.88) | 1.46 (1.02–2.10) |
| 26–39 | 1.91 (1.59–2.31) | 1.85 (1.47–2.33) | 2.06 (1.48–2.86) |
| Sex | |||
| Females | Reference | Reference | Reference |
| Males | 1.39 (1.24–1.56) | 1.43 (1.24–1.64) | 1.28 (1.02–1.61) |
| Period of diagnosis | |||
| Pre-ACA (Mar 2005–Sep 2010) | Reference | Reference | Reference |
| Early ACA (Oct 2010–Dec 2013) | 0.76 (0.66–0.88) | 0.80 (0.68–0.93) | 0.67 (0.51–0.89) |
| Full ACA (Jan 2014–Dec 2017) | 0.54 (0.46–0.63) | 0.56 (0.47–0.67) | 0.48 (0.34–0.70) |
| Stage at diagnosis& | |||
| I | Reference | Reference | Reference |
| II | 1.45 (1.19–1.76) | 1.35 (1.08–1.69) | 2.04 (1.15–3.62) |
| III | 2.07 (1.69–2.54) | 1.94 (1.53–2.45) | 3.00 (1.67–5.39) |
| IV | 3.03 (2.56–3.60) | 2.93 (2.45–3.50) | 4.13 (2.31–7.39) |
| Race/ethnicity& | |||
| Non-Hispanic White | Reference | Reference | Reference |
| Non-Hispanic Black | 1.29 (1.07–1.57) | 1.28 (1.03–1.60) | 1.31 (0.90–1.92) |
| Hispanic | 1.26 (1.10–1.45) | 1.23 (1.05–1.44) | 1.37 (1.05–1.80) |
| Asian/Pacific Islander | 1.22 (1.01–1.48) | 1.20 (0.96–1.48) | 1.26 (0.85–1.85) |
| American Indian/Alaska Native | 2.16 (1.21–3.85) | 1.75 (0.86–3.54) | 3.43 (1.25–9.40) |
| Neighborhood SES | |||
| Highest | Reference | Reference | Reference |
| Medium | 1.09 (0.94–1.26) | 1.10 (0.92–1.31) | 1.07 (0.81–1.41) |
| Lowest | 1.26 (1.08–1.47) | 1.40 (1.17–1.68) | 0.91 (0.67–1.24) |
| Insurance type& | |||
| Private | Reference | Reference | Reference |
| Continuous Medicaid | 1.93 (1.63–2.29) | 1.84 (1.52–2.23) | 2.18 (1.55–3.08) |
| Discontinuous Medicaid | 2.17 (1.83–2.58) | 2.06 (1.69–2.52) | 2.52 (1.81–3.50) |
| Medicaid at diagnosis/uninsured | 2.14 (1.83–2.49) | 2.10 (1.76–2.51) | 2.25 (1.64–3.08) |
| Other public* | 1.13 (0.66–1.93) | 1.25 (0.66–2.36) | 0.93 (0.34–2.54) |
| Charlson Comorbidity Index& | |||
| None | Reference | Reference | Reference |
| One | 1.26 (1.06–1.50) | 1.18 (0.97–1.45) | 1.51 (1.08–2.12) |
| More than one | 3.09 (2.55–3.74) | 2.88 (2.33–3.56) | 4.24 (2.70–6.65) |
| Treatment facility | |||
| NCI-DCC | Reference | Reference | Reference |
| Non-NCI-DCC | 1.04 (0.92–1.17) | 1.04 (0.91–1.20) | 0.98 (0.75–1.27) |
| Marital status& | |||
| Married | Reference | Reference | Reference |
| Unmarried | 1.24 (1.09–1.42) | 1.24 (1.07–1.44) | 1.23 (0.93–1.62) |
Abbreviations: SES, socioeconomic status; NCI-DCC, National Cancer Institute-Designated Cancer Center; ACA, Affordable Care Act; aHR, adjusted hazard ratios, CI, confidence interval; Jan, January; Mar, March; Sep September; Oct, October; Dec, December.
Other public includes Indian/Public Health Service, County Funded, not-otherwise specified (NOS), Medicare without supplement, Medicare, NOS.
Model stratified by cancer site (Hodgkin and non-Hodgkin lymphomas) due to violation of the Cox proportional hazards assumption.
Not included patients with unknown insurance, race/ethnicity, marital status, stage at diagnosis, and comorbidity.
Discussion
Using data from 2005 to 2017, we found that after the ACA implementation in California, AYAs diagnosed with lymphoma had increased Medicaid insurance coverage, were more likely to receive care at NCI-DCCs and experienced better survival. Importantly, AYAs with NHL (albeit not HL) experienced lower likelihood of stage IV disease at diagnosis. However, even after consideration for stage and health insurance, important socioeconomic and racial/ethnic disparities persisted. AYAs residing in the lowest SES neighborhoods and racial/ethnic minority groups experienced worse cancer outcomes, highlighting the need for interventions aimed at decreasing health inequities among underserved AYAs with lymphoma.
The marked increase in continuous Medicaid coverage and decrease of those who were uninsured/gained Medicaid coverage at the time of lymphoma diagnosis is consistent with recent studies in California that evaluated insurance coverage changes in AYAs with cancer in the pre-/post-ACA eras.15, 16 The overall decrease we observed in private insurance coverage may be, in part, due to low-income AYAs changing from private insurance with high patient cost-sharing (i.e., deductibles, copayments, and coinsurance charges) to public insurance when they become eligible for Medicaid coverage.17
Overall, we observed that AYAs with Medicaid insurance were more likely to present with stage IV disease than privately insured AYAs, but this association was more pronounced among AYAs with Medicaid at diagnosis/uninsured or discontinuous Medicaid. Notably, when we analyzed NHL and HL separately, AYAs with continuous Medicaid were not more likely to be diagnosed with stage IV disease than privately insured AYAs. This finding is consistent with our prior study, which suggested that continuous insurance coverage positively influences cancer stage at diagnosis, including lymphomas.13 Our findings are also supported by a recent review which showed that insurance coverage disruption was associated with late-stage cancer diagnosis in all 13 included studies, and this was especially significant for NHL and HL, along with selected solid cancers.11
Late-stage diagnosis remains a strong predictor of cancer survival in AYAs.6 Our findings showed that AYAs with stage IV lymphoma were 3-fold more likely to die than those with stage I disease. To increase the chance of curative treatment, health policy and educational strategies should focus on diagnosing lymphoma at earlier stages. Health insurance mandates and removal of costs associated with preventive health services can reduce barriers to care prior to or as soon as the first signs and symptoms of the disease appear (e.g., painless enlarged lymph nodes, weight loss, fevers, night sweats or shortness of breath), leading to improved stage at diagnosis.18 In addition, educational campaigns for AYAs and clinicians to improve awareness of cancer in this population can increase knowledge of symptoms and importance of care for AYAs19 and facilitate referral from primary care physicians to oncologists.20 Our finding of decreased likelihood of stage IV disease among AYAs with NHL in the full ACA era is encouraging and suggests improved AYA access to healthcare.
Despite increased Medicaid insurance coverage, we observed that AYAs with private insurance had better survival than those with public insurance. This finding is consistent with previous studies in AYAs with cancer.21, 22 Our prior work21 found that among over 60,000 AYAs diagnosed with common cancers, including lymphoma, those with Medicaid insurance had significantly worse cancer-specific survival than those with private insurance. Likewise, Colton et al22 observed that independent of stage, AYAs with public or no insurance (vs private) had lower survival, and this association was particularly significant among those with NHL and HL. This may relate to several factors, including the high rate of socioeconomically disadvantaged AYAs with cancer enrolled in Medicaid, significant Medicaid disenrollment with time from cancer diagnosis,23, 24 and that cancer is a high-cost condition and AYAs face several barriers during the cancer care continuum leading to financial toxicity.25, 26 More specifically, patients with lower SES often present with more advanced disease and have poorer general health than those with higher SES.27 In addition, studies have shown that AYA cancer survivors have unhealthier lifestyle behaviors (e.g., higher smoking rates) than the general population.28
Despite the positive health outcomes we observed in our study, the benefits were not shared equally across all AYA groups. Specifically, AYAs residing in the lowest SES neighborhoods and those of racial/ethnic minority groups had higher likelihood of late stage at diagnosis and worse survival, consistent with prior studies.13, 29 Additionally, in a recent population-based analysis, Moke and colleagues6 examined the risk of death among AYAs diagnosed with 22 of the most common cancers during 1988–2000 and 2001–2014 and found that survival disparities increased, rather than decreased, between the early and late periods, with higher hazard of death among Blacks, Asians/PIs and Latinos (vs Whites) and among those who lived in low SES neighborhoods. These results highlight the disturbing and persistent disparities in health outcomes among AYAs with cancer (including lymphomas) and the urgent need for health policies aimed at mitigating these disparities. For example, policies should focus on improving AYA enrollment into cancer treatment trials and evaluating quality of care metrics for racial/ethnic minority groups. The joint initiative of the American Society of Clinical Oncology (ASCO) and Association of Community Cancer Centers (ACCC) was designed to achieve the goal of improving accrual of underrepresented racial/ethnic groups in cancer clinical trials.30 ASCO has also worked on ensuring that patients with all health insurance plans, including Medicaid, have access to all phases of clinical trials.31 Another key policy is to mandate the real-time exchange of health information among healthcare entities and government agencies to evaluate and improve timely and optimal care for all patients.32
Finally, we found that the proportion of AYAs with lymphomas who received care at NCI-DCCs increased across ACA eras. Following ACA implementation, AYAs were 30–40% more likely to receive initial care at NCI-DCCs, in the early and full ACA, respectively. Previous studies have shown that AYAs with leukemias cared for at NCI-DCCs (vs non-NCI-DCCs) had better survival.33, 34 Multiple factors may contribute to better outcomes at NCI-DCCs, including greater participation in clinical trials, higher patient volume (which may provide better medical expertise and more medical resources), and more adherence to guideline-concordant care.35 We did not find a significant difference in survival by treatment facility, but this may be partially explained by the higher proportion of AYAs with stage IV lymphoma cared for at NCI-DCCs. In addition, multiple factors influence the AYA decision to pursue care at a NCI-DCC. For example, financial concerns about non-medical costs (e.g., transportation to the treating facility, costs of housing, childcare) and lack of social support can impede AYAs to travel long distances to receive care at NCI-DCCs.36 In addition, access of privately insured AYAs to NCI-DCCs will depend on the type of insurance they have, e.g., health maintenance organization (HMO) or preferred provider organization.37 In particular, the proportion of employee sponsored workers covered by HMO plans that provide care withing a local network is much higher in California (46–55%, 2012–2020) than in the United States (13–16%), impacting where cancer care is received.38
Our study has several limitations. First, we did not have data from another state (Medicaid expansion or non-expansion state) or another age group for comparison. Second, we had insurance information at initial diagnosis/treatment, but did not have information on insurance changes over time. Third, we lacked detailed information on treatment, consistent with what is collected by cancer registries in the US. Although these data could have provided additional information, our findings are important and contribute to the growing literature that shows positive health outcomes after ACA implementation.39 Notably, we used data on virtually all AYAs diagnosed with lymphoma in California during the study period and expanded upon our prior findings13 by adding 3 additional years of data, allowing for the investigation of trends in health outcomes by ACA era. Furthermore, we had new information on time of Medicaid enrollment, permitting us to differentiate AYAs with continuous (or discontinuous) Medicaid coverage from those enrolled in Medicaid at the time of lymphoma diagnosis.
In conclusion, following the ACA implementation in California, AYAs with lymphoma experienced increased Medicaid insurance coverage, were more likely to be treated at NCI-DCCs, were less likely to be diagnosed with NHL at stage IV, and had better survival. Our study contributes to the growing literature showing positive health outcomes following the ACA implementation, which has substantially increased health insurance coverage for low-income AYAs in the US. However, the persistent socioeconomic and racial/ethnic disparities we identified underscore the ongoing need for strategies aimed to decrease disparities in outcomes among AYAs with lymphoma.
Supplementary Material
Novelty and Impact.
Following the Affordable Care Act (ACA) implementation in California, adolescents and young adults (AYAs) diagnosed with lymphomas experienced increased Medicaid insurance coverage, improved access to National Cancer Institute-Designated Cancer Centers, were less likely to present with stage IV disease, and had better survival, reinforcing the importance of the ACA provisions.
Despite health insurance status, racial/ethnic and socioeconomic survival disparities persisted, highlighting the need for health policy strategies focused on decreasing health inequities among underserved AYAs with lymphomas.
Acknowledgement
The collection of cancer incidence data used in this study was supported by the California Department of Public Health pursuant to California Health and Safety Code Section 103885; Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries, under cooperative agreement 5NU58DP006344; the NCI’s Surveillance, Epidemiology and End Results (SEER) Program under contract HHSN261201800032I awarded to the University of California, San Francisco, contract HHSN261201800015I awarded to the University of Southern California, and contract HHSN261201800009I awarded to the Public Health Institute.
The ideas and opinions expressed herein are those of the authors and do not necessarily reflect the opinions of the State of California, Department of Public Health, the NCI, and the CDC or their Contractors and Subcontractors. Likewise, it should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Funding
This work was supported in part by the Cancer Research Coordinating Committee (grant number CRR-17-420784). Dr Abrahão’s work was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number T32HP30037 for Research in Primary Care. Dr Keegan was supported by the UC Davis Comprehensive Cancer Center (P30CA093373). Dr Wun was supported by UL1 TR001860, National Center for Advancing Translational Science (NCATS), National Institute of Health.
List of abbreviations
- ACA
Affordable Care Act
- ACCC
Association of Community Cancer Centers
- aHR
Adjusted hazard ratios
- AI/AN
American Indian/Alaska Native
- aOR
Adjusted odds ratios
- ASCO
American Society of Clinical Oncology
- AYA
Adolescent and young adult
- CCR
California Cancer Registry
- CI
Confidence interval
- DCE
Dependent Coverage Expansion
- HL
Hodgkin lymphoma
- NCI-DCC
National Cancer Institute-Designated Cancer Centers
- NH
Non-Hispanic
- NHL
Non-Hodgkin lymphoma
- nSES
Neighborhood socioeconomic status
- PI
Pacific Islander
- SEER
Surveillance, Epidemiology, and End Results
- US
United States
Footnotes
Conflict of Interest: We declare no conflict of interest.
Ethics Statement
Ethical approval was obtained by the Institutional Review Board of the University of California, Davis and by the California Committee for the Protection of Human Subjects.
Conference presentation
Abstract was presented (poster) at the American Society of Clinical Oncology (ASCO) virtual annual meeting on June 4, 2021 and published in the online supplement of the Journal of Clinical Oncology.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.
References
- 1.Miller KD, Fidler-Benaoudia M, Keegan TH, Hipp HS, Jemal A, Siegel RL. Cancer statistics for adolescents and young adults, 2020. CA Cancer J Clin. 2020. [DOI] [PubMed] [Google Scholar]
- 2.Smith EC, Ziogas A, Anton-Culver H. Association between insurance and socioeconomic status and risk of advanced stage Hodgkin lymphoma in adolescents and young adults. Cancer. 2012;118: 6179–6187. [DOI] [PubMed] [Google Scholar]
- 3.Shanbhag S, Ambinder RF. Hodgkin lymphoma: A review and update on recent progress. CA Cancer J Clin. 2018;68: 116–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Armitage JO, Gascoyne RD, Lunning MA, Cavalli F. Non-Hodgkin lymphoma. Lancet. 2017;390: 298–310. [DOI] [PubMed] [Google Scholar]
- 5.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70: 7–30. [DOI] [PubMed] [Google Scholar]
- 6.Moke DJ, Tsai K, Hamilton AS, et al. Emerging Cancer Survival Trends, Disparities, and Priorities in Adolescents and Young Adults: A California Cancer Registry-Based Study. JNCI Cancer Spectr. 2019;3: pkz031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Government. US. The Patient Protection and Affordable Care Act, Public Law No: 111-148. Available from URL: https://www.congress.gov/111/plaws/publ148/PLAW-111publ148.pdf.
- 8.Conway D Health Insurance Coverage Among Young Adults Aged 19 to 34: 2018 and 2019. Washington, D.C., 2020. [Google Scholar]
- 9.Martin S, Ulrich C, Munsell M, Taylor S, Lange G, Bleyer A. Delays in cancer diagnosis in underinsured young adults and older adolescents. Oncologist. 2007;12: 816–824. [DOI] [PubMed] [Google Scholar]
- 10.Dawes AJ, Louie R, Nguyen DK, et al. The impact of continuous Medicaid enrollment on diagnosis, treatment, and survival in six surgical cancers. Health Serv Res. 2014;49: 1787–1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yabroff KR, Reeder-Hayes K, Zhao J, et al. Health Insurance Coverage Disruptions and Cancer Care and Outcomes: Systematic Review of Published Research. J Natl Cancer Inst. 2020;112: 671–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blumenthal D, Collins SR. Health Care Coverage under the Affordable Care Act — A Progress Report. New England Journal of Medicine. 2014;371: 275–281. [DOI] [PubMed] [Google Scholar]
- 13.Keegan THM, Parsons HM, Chen Y, et al. Impact of Health Insurance on Stage at Cancer Diagnosis Among Adolescents and Young Adults. J Natl Cancer Inst. 2019;111: 1152–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12: 703–711. [DOI] [PubMed] [Google Scholar]
- 15.Abrahão R, Maguire FB, Morris CR, Parikh-Patel A, Parsons HM, Keegan THM. The influence of the Affordable Care Act-Dependent Care Expansion on insurance coverage among young cancer survivors in California: an updated analysis. Cancer Causes Control. 2020. [DOI] [PubMed] [Google Scholar]
- 16.Abrahão R, Ribeiro RC, Malogolowkin MH, Wun T, Keegan THM. Early mortality and survival improvements for adolescents and young adults with acute promyelocytic leukemia in California: an updated analysis. In press. Haematologica. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salazar MC, Canavan ME, Walters SL, et al. Evaluation of Cancer Care After Medicaid Expansion Under the Affordable Care Act. JAMA Network Open. 2020;3: e2017544–e2017544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.HealthCare.gov. Preventive health services. Available from URL: https://www.healthcare.gov/coverage/preventive-care-benefits/ [accessed 10/27/2021].
- 19.Magni C, Segrè C, Finzi C, et al. Adolescents’ Health Awareness and Understanding of Cancer and Tumor Prevention: When and Why an Adolescent Decides to Consult a Physician. Pediatr Blood Cancer. 2016;63: 1357–1361. [DOI] [PubMed] [Google Scholar]
- 20.Zebrack B, Mathews-Bradshaw B, Siegel S. Quality cancer care for adolescents and young adults: a position statement. J Clin Oncol. 2010;28: 4862–4867. [DOI] [PubMed] [Google Scholar]
- 21.Parsons HM, Maguire FB, Morris CR, et al. Impact of insurance type and timing of Medicaid enrollment on survival among adolescents and young adults with cancer. Pediatr Blood Cancer. 2020;67: e28498. [DOI] [PubMed] [Google Scholar]
- 22.Colton MD, Goulding D, Beltrami A, et al. A U.S. population-based study of insurance disparities in cancer survival among adolescents and young adults. Cancer Med. 2019;8: 4867–4874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liao JM, Sommers BD, Navathe AS. Medicaid’s Path to Value-Based Reform. N Engl J Med. 2018;379: 105–108. [DOI] [PubMed] [Google Scholar]
- 24.Parsons HM, Schmidt S, Harlan LC, et al. Young and uninsured: Insurance patterns of recently diagnosed adolescent and young adult cancer survivors in the AYA HOPE study. Cancer. 2014;120: 2352–2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu AD, Zheng Z, Han X, et al. Medical Financial Hardship in Survivors of Adolescent and Young Adult Cancer in the United States. JNCI: Journal of the National Cancer Institute. 2021;113: 997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salsman JM, Bingen K, Barr RD, Freyer DR. Understanding, measuring, and addressing the financial impact of cancer on adolescents and young adults. Pediatr Blood Cancer. 2019;66: e27660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKelvie RS, Benedict CR, Yusuf S. Evidence based cardiology: prevention of congestive heart failure and management of asymptomatic left ventricular dysfunction. BMJ. 1999;318: 1400–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Warner EL, Nam GE, Zhang Y, et al. Health behaviors, quality of life, and psychosocial health among survivors of adolescent and young adult cancers. J Cancer Surviv. 2016;10: 280–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kent EE, Morris RA, Largent JA, Ziogas A, Sender LS, Anton-Culver H. Socioeconomic Impacts on Survival Differ by Race/Ethnicity among Adolescents and Young Adults with Non-Hodgkin’s Lymphoma. J Cancer Epidemiol. 2010;2010: 824691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Society of Clinical Oncology. ASCO & ACCC Join Forces to Increase Participation of Racial and Ethnic Minority Populations in Cancer Treatment Trials. Available from URL: https://www.asco.org/about-asco/press-center/news-releases/asco-accc-join-forces-increase-participation-racial-and-ethnic [accessed 10/10/2021].
- 31.Patel MI, Lopez AM, Blackstock W, et al. Cancer Disparities and Health Equity: A Policy Statement From the American Society of Clinical Oncology. J Clin Oncol. 2020;38: 3439–3448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.California Legislative Information. Assembly Bill No. 133. Available from URL: https://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=202120220AB133 [accessed 10/23/2021].
- 33.Wolfson J, Sun CL, Wyatt L, Stock W, Bhatia S. Adolescents and Young Adults with Acute Lymphoblastic Leukemia and Acute Myeloid Leukemia: Impact of Care at Specialized Cancer Centers on Survival Outcome. Cancer Epidemiol Biomarkers Prev. 2017;26: 312–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muffly L, Alvarez E, Lichtensztajn D, Abrahão R, Gomez SL, Keegan T. Patterns of care and outcomes in adolescent and young adult acute lymphoblastic leukemia: a population-based study. Blood Adv. 2018;2: 895–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Muffly L, Lichtensztajn D, Shiraz P, et al. Adoption of pediatric-inspired acute lymphoblastic leukemia regimens by adult oncologists treating adolescents and young adults: A population-based study. Cancer. 2017;123: 122–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andrews M For Some Patients In Marketplace Plans, Access To Cancer Centers Is Elusive. Available from URL: https://khn.org/news/for-some-patients-in-marketplace-plans-access-to-cancer-centers-is-elusive/ [accessed 10/12/2021].
- 37.Health for California Insurance Center. California Health Insurance Plan Options: HMO, PPO or EPO. Available from URL: (https://www.healthforcalifornia.com/california-health-insurance-plan-options-hmo-ppo-epo). [accessed 10/22/2021].
- 38.Whitmore H, Satorius J. 2021. Edition – California Employer Health Benefits. Available from URL: https://www.chcf.org/publication/2021-edition-california-employer-health-benefits/ [accessed 10/21/2021].
- 39.Guth M, Garfield R, Rudowitz R. The Effects of Medicaid Expansion under the ACA: Updated Findings from a Literature Review. San Francisco-CA, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.


